Abstract
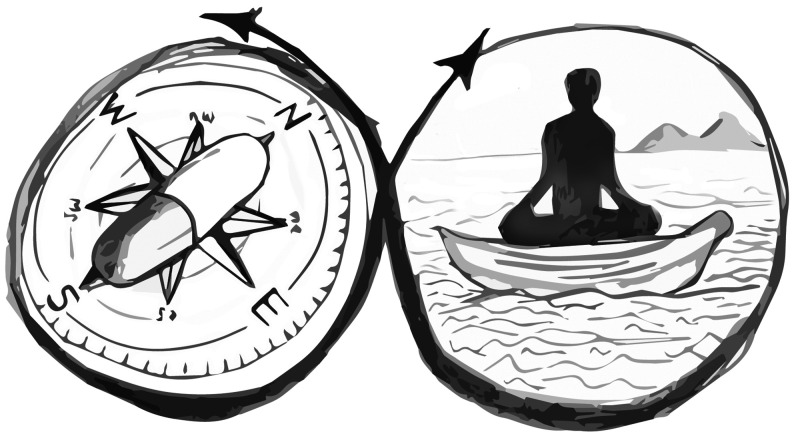
Psychedelic and mindfulness interventions have been shown to improve mental ill-health and wellbeing, with a range of clinical processes and effects in common. However, each appear to contain specific challenges in the context of mental health treatment. In this Perspective, we focus on a set of distinct affordances, “useful differences”, within psychedelic and mindfulness interventions that might address common challenges within the other intervention. Accordingly, we propose a set of applied synergies, indicating specific ways in which these two promising interventions might be combined for greater benefit. Metaphorically, on the journey toward mental health and wellbeing, we propose that psychedelic treatments may serve the role of Compass (initiating, motivating, and steering the course of mindfulness practice), with mindfulness interventions serving the role of Vehicle (integrating, deepening, generalizing, and maintaining the novel perspectives and motivation instigated by psychedelic experience). We outline a set of testable hypotheses and future research associated with the synergistic action of psychedelic and mindfulness interventions toward improved clinical outcomes.
Keywords: mindfulness, meditation, psychedelics, psychedelic-assisted psychotherapy, psilocybin, LSD, mental health, psychiatry, psychotherapy
1. Psychedelic and Mindfulness-Based Interventions and Effects
Psychedelic and mindfulness-based interventions have both been shown independently to improve mental health and psychological wellbeing.1,2 While distinct, both psychedelics and mindfulness are associated with a range of similar phenomenological, psychological, and neurobiological changes.3,4 These similarities reflect potential compatibility as combined interventions.5,6 Yet certain differences, we propose, highlight potential ways in which psychedelic and mindfulness-based interventions can address key challenges faced by the other. This Perspective proposes ways to combine both interventions towards synergistic and improved outcomes.
1.1. Mindfulness Meditation and Mindfulness-Based Interventions
Mindfulness refers to the awareness that emerges when deliberately paying attention to the experience of the present moment with curiosity and without judgment.7 It is a quality that can be enhanced through systematic training known as mindfulness meditation (MM). Formal MM practice generally involves sitting with the eyes closed, attending to the changing flow of sensory phenomena (e.g., the breath entering and leaving the body) without evaluation or selection.
The term mindfulness has been used to refer to a state of awareness, a psychological trait, or a mental activity,8 resulting in some confusion among researchers. In this Perspective, we use the term “mindfulness” when referring to the psychological construct and MM when referring to the set of attention training exercises commonly employed to enhance mindfulness. Originally developed within Buddhism and other wisdom traditions to alleviate mental suffering and gain insight, mindfulness has been incorporated into mindfulness-based interventions (MBIs) such as mindfulness-based stress reduction and mindfulness-based cognitive therapy.9,10 Meta-analyses show that mindfulness-based interventions can reduce clinical symptoms of psychiatric disorders compared to either active or nonactive comparison conditions, with small to moderate effect sizes, respectively, at post-treatment (d = 0.23; d = 0.35) and 6 month follow-up (d = 0.29; d = 0.52)2. Mindfulness-based interventions appear to be particularly effective in reducing depressive symptoms, pain, and addiction.2
Acute subjective effects of MM training include positive experiences such as relaxation, nonreactivity, attentiveness, gratitude, love, and joy,11 as well as challenging experiences such as restlessness, boredom, confusion, pain, sadness, and anger.12 Reports from long-term meditators describe a variety of ongoing effects, including heightened mindful awareness, reductions in automatic behavior, increased gratitude, and reduced stress reactivity.11,13
Extensive and intensive MM practice has also been associated with nonordinary states of consciousness, including profound alterations to the experience of time and self11 and, in rare cases, hallucinations, unusual thinking, and depersonalization.14 The latter are often experienced as unpleasant and can be associated with negative long-term effects, although within some traditional contexts such experiences can also be considered a sign of progress.15
1.2. Psychedelics and Psychedelic Interventions
The “classical” psychedelics are a class of serotonergic tryptamines that exert the majority of their psychoactive effects via the 5HT2A receptor subtype (e.g., lysergic acid diethylamide or LSD, psilocybin, ayahuasca) and reliably produce nonordinary states of consciousness with subjective changes that entail dramatic changes in sensory perception, distortions of time, reduced cognitive control, awe experience, novel perspectives on familiar phenomena, labile emotions, heightened empathy, and compassion.16−19
Psychedelic-assisted psychotherapy (PP) includes a range of related approaches that combine the ingestion of a psychedelic substance with various forms of professional support or psychotherapy. A common PP treatment protocol within a research trial includes 1–3 dosing sessions alongside 6–12 psychotherapy sessions utilizing various therapeutic modalities and delivered over a 1–3 month period. For the dosing sessions, considerable care is taken to ensure a conducive participant mindset, physical context, and therapeutic alliance.20 Recent research indicates that even relatively short-term PP can safely produce rapid and sustained clinical benefits for severe and intractable psychological and behavioral disorders1 including depression,21 tobacco addiction,22 alcohol dependence,23 and anxiety and depressive symptoms within terminal cancer patients.24
Within modern clinical psychedelic trials, many patients report a peak state sometimes referred to as a “mystical-type experience”, an experience that can appear devoid of space, time aentails a dramatic reduction and the destinction between self and nonself, conveys “noetic qualities” (acquisition of new knowledge or perspectives), and wherein many of the notable features of this experience are impossible to convey in language.25 The magnitude of mystical-type experience during the acute psychedelic experience appears to be a key predictor of sustained positive changes in psychological functioning.26 Participants in clinical psychedelic trials also commonly report challenging experiences during the acute drug effects, including anxiety, hyperarousal, confusion, and fear, alongside difficulties integrating insights from the dosing session.27 However, while the majority of PP participants indicate that their psychedelic sessions were among the most challenging experiences of their lives, these experiences are also rated among the most personally meaningful.24,28
2. Potential Synergies between Mindfulness and Psychedelic Interventions
2.1. Previous Research Linking Mindfulness Meditation and Psychedelics
Some preliminary evidence has shown interesting links between the effects of mindfulness and psychedelics. For example, administration of psychedelics has been found to increase both state and trait mindfulness.17,29−34 Also, Smigielski and colleagues6 found that psilocybin, administered to experienced MM practitioners during a meditation retreat, was associated with increased meditation depth, higher post-intervention trait mindfulness, and improved psychosocial functioning at 4 months follow-up, compared to a placebo condition. Furthermore, Smigielski and colleagues6 noted that, compared to non-meditators receiving the same dose of psilocybin, MM practitioners indicated higher ratings of blissful state, spiritual experience, and feelings of unity associated with their psilocybin session, as well as lower anxiety around “ego-dissolution” (an experience of fragmenting and dissipating selfhood).
Relatedly, Griffiths and colleagues5 found that administering psilocybin to healthy participants alongside supported “spiritual practice” (which included some MM) led to greater improvements across many key outcomes, including positive mood and attitudes and life satisfaction at 6 months follow-up, compared to active placebo. Furthermore, the provision of more intensive support for this “spiritual practice” was associated with greater increases in acute “mystical experience” during psilocybin dosing, as well as more personally profound meditation experiences, self-reported and observed positive behaviors, and increased meaning in life at 6 months follow-up.
Interestingly, MM and PP may be associated with certain neurobiological changes in common, including reduced Default Mode Network (DMN) activation, and greater functional connectivity between DMN structures and task-positive networks such as the dorsolateral prefrontal cortex.35−37 Some of these structural changes have been associated with the therapeutic benefits of these interventions.37−40
While these early trials indicate that combining psychedelics and mindfulness may produce complementary effects, it remains unclear whether, why, or how to combine these interventions toward improved therapeutic outcomes. Here, we outline a set of potential applied synergies that can be tested in trials and, where useful, implemented in practice.
2.2. Psychedelics and Mindfulness: The Compass and the Vehicle
In the sections below, we explore potential synergies of psychedelics and mindfulness; many of these can be depicted within an overarching metaphor: on a journey toward mental health and wellbeing, psychedelics may act as a Compass and mindfulness meditation as a Vehicle. That is, psychedelics appear particularly effective at temporarily initiating an often-dramatic reorientation toward more adaptive values, attitudes, and behaviors41−43 through the production of a personally profound nonordinary state of consciousness; however, psychedelics may be limited in their longer-term use. The often profound reorientation afforded by PP can be incrementally overwhelmed by the re-emergence of previous maladaptive thoughts and behaviors (e.g., despite a large short-term reduction in depressive symptoms following psilocybin-assisted psychotherapy in one trial, 58% of depressed patients had relapsed by 3 months44).
Indeed, while some studies suggest that psychedelic interventions can have sustained effects,94 others have found declining clinical effects in the longer term,21,22 with the lasting effects of PP likely dependent on numerous factors, including type and dosage of psychedelic substance, type and duration of psychotherapeutic support, specific symptomatic profiles, acute subjective effects, demographic variables, and life context. In addition, many studies suffer from small sample sizes, self-selection biases and other potential “inflationary effects” (e.g., a likely greater placebo component due to the novelty of the agent, heightened participant expectations, and increases in suggestibility linked to psychedelics). That is, while sustained clinical benefits in psychedelic trials are often impressive, for most patients it may be unreasonable to expect that one or a few doses of a psychedelic alongside brief psychotherapy would produce clinically significant effects that endure for many months or years. One possible approach to sustaining outcomes may be to offer psychedelic treatment regularly to patients who are relapsing or at risk of relapse. However, setting aside a range of potential psychological and physical health concerns that may be associated with frequent psychedelic dosing over the long-term, and the risk of diminishing benefit with repeated dosing, the clinical and economic burden of providing regular and ongoing psychedelic treatment is a substantial impediment to this being a viable treatment model. Accordingly, substantial nonpsychedelic elements of the treatment program may be important in sustaining the benefits of psychedelics for many people.
In contrast, MM may be particularly effective for sustaining therapeutic change45,46 through integrating, deepening, generalizing, and maintaining the often-temporary changes to belief, attitude, affect, behavior, and relationship following psychedelic dosing; however, the initiation and ongoing maintenance of MM practice is difficult,47 with mindfulness-based interventions typically showing high attrition rates in the treatment of psychiatric conditions.48 Thus, as we will explore in more depth later in this Perspective, psychedelics may afford reliable, robust, yet transient changes that may overcome key early hurdles to practicing mindfulness, increasing motivation to practice and perhaps even boosting the quality of the practice.
Below, we outline ways in which psychedelics may aid in the recognition, motivation, depth, and compassion associated with intensive or extensive mindfulness practice and conversely the way mindfulness may aid in lowering anxiety and psychological defenses during psychedelic experiences and in sustaining the changes in the longer-term following psychedelics. Through these nonexhaustive synergies, we suggest that the psychedelic encounter can provide a reliable map to guide and motivate a mindfulness practice in navigating the territory of one’s relationship to daily life.
2.3. Synergy 1: Mindful State Recognition
While mindfulness may initially appear to be a simple practice,49 it can be challenging for novice meditators to know the specific target mental processes that reflect progress along a path of deepening meditation practice.50 While skillful mindfulness teachers and clinicians attempt to guide individuals to desired states, individuals must rely on their own subjective experience to ascertain the effectiveness of their approach.51 This can lead to confusion and potentially reduced motivation to practice.47
Interestingly, high doses of psychedelics more reliably produce potent nonordinary states of consciousness and psychological effects that resemble those associated with deep meditative states. Accordingly, these experiences might act as a point of reference to orient MM practice, particularly for novice meditators. For example, psychedelics without MM have been found to increase facets of trait mindfulness, such as heightened present-moment awareness, increased ability to articulate momentary experience, and the capacities of nonjudgement and nonreactivity.17,29,31,32 In addition, acute psychedelic effects include decreased self-referential thinking,40,52 increased decentering,17 feelings of interpersonal connectedness,53 and non-dual experience,18 each also associated with prolonged meditation.
Qualitative accounts from both meditative and psychedelic experience further reflect this resemblance. For example, paradigmatic accounts from experienced meditators (e.g., “there is no “I”...no sense of ego...this is just dissolving...there is just the universe”13) often resemble reports following high dose psychedelics (e.g., “I was everybody, unity, one life...the one asking for love and giving love, I was swimming in the sea, and the sea was me”54). These subjective experiences of alterations to self-experience may be in part associated with reduced DMN activation and internal functional connectivity, which is evident during both MM55−57 and psychedelic exposure.38,58,59 Further research is required to understand the relationship between the DMN and these subjective effects.
Thus, psychedelics may provide a reliable, albeit transient, subjective experience that appears to substantially overlap with deep meditative states, which typically require considerable practice to achieve.11,60 Such experiences may better orient mindfulness practitioners toward these states in their ongoing daily meditation practice.
2.4. Synergy 2: Motivation for Mindfulness Practice
Sustaining MM over the longer term is a crucial factor in achieving the intended benefits.61−63 However, MM can be challenging to practice and without rapid benefits,47 leading to demotivation to practice and high attrition rates.48
By transiently inducing a peak experience and “afterglow” that resembles aspects of deep meditative states and the results of effective and prolonged practice, psychedelics may motivate people to sustain their mindfulness practice over time. Indeed, research indicates that awareness of the potential benefits is a significant predictor of sustained meditation.47,64 Furthermore, PP has been associated with revised priorities65 and increased motivation to act congruently with ones values,41,66 which may contribute to the motivation for ongoing MM practice.
2.5. Synergy 3: Depth of Mindfulness
During mindfulness practice, practitioners commonly encounter challenging thoughts and emotions (e.g., forgotten memories) that can trigger psychological defenses67,68 and experiential avoidance,69 potentially limiting meditative depth and beneficial effects. Indeed, links between experiential avoidance and psychopathology are well-established.70
Psychedelics may address reactive impediments to meditation depth through transiently and potently lowering psychological defenses, provoking insights and new perspectives, and compelling the individual to face their fears, difficult memories, or insights.27,71−74 Psychedelics have also been shown to increase the personality trait of Openness,16,75,76 which may further contribute to the key mindfulness attitudes of meta-cognitive curiosity and nonavoidance. Thus, psychedelics may calibrate the individual to an attitude of less defensiveness and greater openness, allowing them to better navigate difficult experiences that arise through deep states of meditation, and to continually deepen their practice through mindful attention and curiosity. Such transient psychedelic experiences may thereby improve both the quality of the meditative state and therefore its long-term benefits.
2.6. Synergy 4: Mindful Compassion
Mindfulness without kindness and self-compassion can take on a “cold, critical quality”77 that can paradoxically lead to maladaptive emotional regulation strategies such as repression.67,78 Compassion appears to enhance the capacity to approach and process difficult emotions instead of avoiding them.49,79 Self-compassion is an important part of practicing mindfulness7 is strongly related to psychological wellbeing.80 It has been found to mediate the relationship between meditation practice and subsequent positive affect81 and to more strongly predict psychological wellbeing than trait mindfulness.82 However, mindfulness practitioners can find it difficult to cultivate and maintain such qualities due to patterns of self-critical rumination, feelings of unworthiness, insecure attachment styles, difficulty processing strong emotions, and resistance.83−86
Psychedelics have been found to reliably increase self-compassion, prosocial attitudes, and emotional empathy.87−89 Therefore, psychedelics may instigate a more compassionate type of mindfulness practice, potentially enhancing its therapeutic utility.
2.7. Synergy 5: Psychedelic Non-avoidance
The barrage of substantial phenomenological, cognitive, affective, and perceptual changes common during psychedelic experiences can trigger confusion and distress.27,90 Although the literature on adverse events in clinical applications of psychedelics is nascent, psychologically challenging experiences during psychedelic dosing are common, with about two-thirds of participants describing aspects of the experience as being among the top ten most challenging of their lives.27 Commonly reported challenging experiences include feelings of grief, panic, physical distress, paranoia, and fear of insanity, isolation, or death.90 However, working through such experiences during the acute effects can facilitate positive therapeutic outcomes.26,27
A key factor differentiating beneficial from counterproductive psychedelic experiences is whether the participant is open to and accepting of the experience or whether they resist it.26,27,91 While preparatory sessions for psychedelics often include a discussion of the importance of maintaining a nonavoidant attitude during the dosing session,92 this can be challenging for many people when they are actually confronted by this material during the acute effects.
MM during the dosing session may assist in lowering negative reactivity and avoidant responding, thereby decreasing the chance of a therapeutically ineffective or even harmful “bad trip”. MM explicitly trains a nonreactive and accepting attitude and has been found to reduce experiential avoidance49,93 and decrease emotional reactivity and bias for negative emotional stimuli. The challenge of remaining mindfully attentive during intense and confronting psychedelic experiences may be addressed by extensive MM practice during the preparatory phase of PP.
It is, however, important to ensure that mindfulness practice is conducted in a way that genuinely cultivates qualities such as acceptance and nonreactivity. While research suggests the combination of MM and psychedelics may be safe,5,6 MM could inadvertently increase reactivity to mental events, which could potentially compromise subsequent psychedelic dosing. Close supervision by experienced therapists during any such training may be warranted.
2.8. Synergy 6: Sustained Psychedelic Proximity and Generalization
PP has been associated with a short period of “afterglow”,32 which tends to dissipate over a period of days or weeks. Mindfulness practice may help maintain such positive changes in thoughts and behaviors following administration of psychedelics through further developing or strengthening insights, defusing from maladaptive thoughts and behaviors, maintaining a sense of the priorities of one’s values, renewing one’s commitments to relevant changes in behavior, and generalizing these changes into more aspects of one’s life.
Given the leading role of subjective psychedelic experiences in predicting and possibly driving therapeutic change,24 retaining a sense of “proximity” to the shifts in perspective and experience afforded by psychedelics may be key to sustaining the therapeutic benefits. The ability for extensive or intensive MM to occasion mystical-type experiences that in part resemble those associated with psychedelics may serve to maintain “experiential proximity” to the psychedelic encounter, which may in turn help to maintain clinical effects. For example, MM can occasion nonordinary state experiences that resemble those commonly associated with high dose psychedelics, including reports of Oceanic Boundlessness13,60 and feelings of awe and wonder.95,96 Indeed, MM aims to explicitly cultivate the capacity for these experiences.97
Well-supported psychedelic experiences are often psychotherapeutically dense, efficient, and useful. While certain qualities of the acute psychedelic experience predict clinical benefit across a number of trials,43 these specific qualities are mostly difficult to describe (representing a hallmark of such experiences, ineffability). We speculate that should these nonordinary state experiences fade over time into verbalized “lessons” devoid of key phenomenology, such cognitive artifacts would be limited in the degree to which they can drive or maintain changes relevant to mental illness.98 MM may assist in better sustaining the effects of psychedelics through its ability to occasion nonordinary state experiences (albeit often less intense) with overlapping qualities that might allow for an ongoing sense of proximity to nonverbal and noncognitive aspects of the encounter that appear therapeutically important.
Psychedelic experiences within modern clinical trials are rated among life’s most personally meaningful and profound experiences by a large majority of participants,24 with participants reporting dramatic alterations in their beliefs, affect, and motivation to change. However, the gradual worsening of symptoms in many patients and the risk of “spiritual bypassing” (a tendency to use “peak” or “transcendent” experiences to avoid facing unresolved psychological, developmental, interpersonal, vocational, physical, or other issues99) suggest that it may be important to frequently ground, generalize, and apply these personally profound experiences within daily life. Mindfulness practice may provide the bridge between psychedelic experience and the everyday, thereby aiding in the integration and generalization of insights into relationships, attitudes, affect, and behaviors, and reducing the resumption of maladaptive habits.
3. Future Research: Combining Mindfulness and Psychedelics
Here, we propose a set of research hypotheses that could be tested to ascertain ways in which mindfulness and psychedelics might fruitfully be combined, including scales and other tools that could be employed to explore these (see Supporting Information for scale references). These questions highlight both the speculative or preliminary nature of this Perspective’s proposals and their clinical implications.
Compared to no psychedelic experience, controlled and supported exposure of novice meditators to a high dose classical psychedelic will:
decrease confusion about how to practice mindfulness and increase confidence in the methods and benefits of practice (e.g., as measured by the Determinants of Meditation Practice Inventory-Revised (DMPI-R))
increase the depth of meditation practice and subsequent mindful awareness, controlling for practice time (e.g., as measured by the Five Facet Mindfulness Questionnaire and the Meditation Depth Index)
increase motivation to practice mindfulness (e.g., as measured by the DMPI-R) and increase the amount of overall practice (e.g., as measured by the Mindful Adherence Questionnaire and experience sampling metrics extracted from meditation smartphone apps)
increase compassion for self and others, both within MM practice and in daily life (e.g., as measured by the Self-Compassion Scale and the Compassion Scale)
increase reported benefits of mindfulness on behavior, relationships, affect, and cognition (e.g., as measured by the Warwick-Edinburgh Mental Wellbeing Scale)
In addition, we hypothesise that compared to no mindfulness training, intensive or extensive mindfulness training and practice in people naive to psychedelics will:
reduce anxiety and avoidant responding during challenging psychedelic dosing sessions and the occurrence of unresolved “bad trips” (e.g., as measured by the 5-Dimensional Altered States of Consciousness Rating Scale and the Emotional Breakthrough Inventory)
sustain for a longer period of time the felt sense of proximity to changes in attitude, perspective, and affect experienced during the acute psychedelic experience
lead to a more generalized influence within daily attitudes, feelings, relationships, and behaviors of psychedelic perspectives (e.g., as measured by the Persisting Effects Questionnaire)
sustain a range of mental health benefits associated with psychedelic dosing and PP for a longer period (e.g., as measures by various mental illness and wellbeing questionnaires)
4. Common Ground, Useful Differences
In summary, this Perspective outlined a number of applied ways in which mindfulness and psychedelics may work clinically in complementary, synergistic ways to address key limitations in each intervention. We employ a Compass and Vehicle metaphor to describe the broad synergy. That is, the Compass of psychedelics may serve to initiate, motivate, and steer the course of mindfulness practice; conversely, the Vehicle of mindfulness may serve to integrate, deepen, generalize, and maintain the novel perspectives and motivation instigated by psychedelics.
Above, we have briefly sketched a set of possible, yet by no means exhaustive, applied synergies between psychedelics and mindfulness. These include a role for psychedelics to substantively contribute to multiple aspects of mindfulness through providing a first-hand experience that resembles deep meditative states, thereby potentially reducing confusion, inefficiency, and resultant demotivation (e.g., progress is more recognizable), increasing the depth and psychotherapeutic utility of mindfulness experiences (e.g., lowered psychological defenses, increasing insight), and enhancing compassion for self and others (an important and often underemphasized approach to using mindfulness practice toward psychotherapeutic ends). Conversely, mindfulness may aid various aspects of psychedelic dosing, including reducing anxiety and associated experiential-avoidance during intense and challenging psychedelic experiences (e.g., training for greater acceptance and lower reactivity), maintaining proximity to nonordinary psychedelic perspectives and thereby sustaining clinical effects (e.g., MM-induced experiences, including nonordinary states), and integrating and generalizing psychedelic perspectives and motivation to change in an applied way (e.g., bridging from peak psychedelic experiences into the challenges and habits of daily life).
Psychedelics and mindfulness are clearly and substantially aligned in terms of the contextual, methodological, experiential, neurobiological, and clinical outcomes they have in common, allowing for a range of feasible combinations between them. Yet crucially, the key limitations within each intervention appear diametrically opposed: psychedelics represent an intervention that can reliably instigate substantial therapeutic change while being limited in terms of sustaining that change; mindfulness represents an intervention that presents a range of initial hurdles to engagement but increasing benefits over time.
Further research into the potential of combining psychedelics and mindfulness to enhance important elements of each other is warranted, with implications for clinical practice. To this end, the development of new measures would aid in detecting synergistic effects between psychedelic and mindfulness interventions. Herein we have suggested the possibility of a “fruitful marriage” between two promising mental health interventions, and highlighted some initial research questions to explore. Our hope is that this Perspective contributes to further empirical work combining psychedelic and mindfulness interventions, and consequently to improved mental health outcomes.
Supporting Information Available
The Supporting Information is available free of charge at https://pubs.acs.org/doi/10.1021/acsptsci.1c00034.
References for the scales mentioned in the Future Research section (PDF)
Author Contributions
The manuscript was written through equal contributions of all authors. All authors have approved the final version of the manuscript.
This research received no funding.
The authors declare the following competing financial interest(s): P.L. is a member of the Medical Advisory Board of Incannex Healthcare Ltd. This company was not involved in any aspect of this paper, including the decision to write it, drafting the paper, or its publication.
Supplementary Material
References
- Aday J. S.; Mitzkovitz C. M.; Bloesch E. K.; Davoli C. C.; Davis A. K. (2020) Long- term effects of psychedelic drugs: A systematic review. Neurosci. Biobehav. Rev. 113, 179–189. 10.1016/j.neubiorev.2020.03.017. [DOI] [PubMed] [Google Scholar]
- Goldberg S. B.; Tucker R. P.; Greene P. A.; Davidson R. J.; Wampold B. E.; Kearney D. J.; Simpson T. L. (2018) Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review 59, 52–60. 10.1016/j.cpr.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuschkel K.; Kuypers K. P. C. (2020) Depression, Mindfulness, and Psilocybin: Possible Complementary Effects of Mindfulness Meditation and Psilocybin in the Treatment of Depression. A Review. Frontiers in Psychiatry 11, 224. 10.3389/fpsyt.2020.00224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milliere R.; Carhart-Harris R.; Roseman L.; Trautwein F.-M.; Berkovich-Ohana A. (2018) Psychedelics, Meditation, and Self-Consciousness. Frontiers in Psychology 9, 1475. 10.3389/fpsyg.2018.01475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths R. R.; Johnson M. W.; Richards W. A.; Richards B. D.; Jesse R.; Maclean K. A.; Klinedinst M. A.; et al. (2018) Psilocybin-occasioned mystical-type experience in combination with meditation and other spiritual practices produces enduring positive changes in psychological functioning and in trait measures of prosocial attitudes and behaviors. J. Psychopharmacol. 32 (1), 49–69. 10.1177/0269881117731279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smigielski L.; Kometer M.; Scheidegger M.; Krahenmann R.; Huber T.; Vollenweider F. X. (2019) Characterization and prediction of acute and sustained response to psychedelic psilocybin in a mindfulness group retreat. Sci. Rep. 9 (1), 14914. 10.1038/s41598-019-50612-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. (1994) Wherever you go, there you are: mindfulness meditation in everyday life, 1st ed., Hyperion, New York. [Google Scholar]
- Van Dam N. T.; van Vugt M. K.; Vago D. R.; Schmalzl L.; Saron C. D.; Olendzki A.; Meyer D. E.; et al. (2018) Mind the Hype: A Critical Evaluation and Prescriptive Agenda for Research on Mindfulness and Meditation. Perspectives on Psychological Science 13 (1), 36–61. 10.1177/1745691617709589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal Z. V., Williams J. M. G., and Teasdale J. D. (2002) Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse, Guilford Press, New York, NY, US. [Google Scholar]
- Miller J. J.; Fletcher K.; Kabat-Zinn J. (1995) Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. General Hospital Psychiatry 17 (3), 192–200. 10.1016/0163-8343(95)00025-M. [DOI] [PubMed] [Google Scholar]
- Sedlmeier P.; Loße C.; Quasten L. C. (2018) Psychological Effects of Meditation for Healthy Practitioners: an Update. Mindfulness 9 (2), 371–387. 10.1007/s12671-017-0780-4. [DOI] [Google Scholar]
- Farias M.; Maraldi E.; Wallenkampf K. C.; Lucchetti G. (2020) Adverse events in meditation practices and meditation-based therapies: a systematic review. Acta Psychiatr. Scand. 142 (5), 374–393. 10.1111/acps.13225. [DOI] [PubMed] [Google Scholar]
- Gifford-May D.; Thompson N. (1994) “Deep states” of meditation: Phenomenological reports of experience. Journal of Transpersonal Psychology 26 (2), 117. [Google Scholar]
- Lindahl J. R.; Fisher N. E.; Cooper D. J.; Rosen R. K.; Britton W. B. (2017) The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLoS One 12 (5), e0176239–e0176239. 10.1371/journal.pone.0176239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compson J. (2018) Adverse Meditation Experiences: Navigating Buddhist and Secular Frameworks for Addressing Them. Mindfulness 9 (5), 1358–1369. 10.1007/s12671-017-0878-8. [DOI] [Google Scholar]
- Carhart-Harris R.; Kaelen M.; Bolstridge M.; Williams T. M.; Williams L. T.; Underwood R.; Nutt D. J.; Feilding A. (2016) The paradoxical psychological effects of lysergic acid diethylamide (LSD). Psychol. Med. 46 (7), 1379–1390. 10.1017/S0033291715002901. [DOI] [PubMed] [Google Scholar]
- Soler J.; Elices M.; Franquesa A.; Barker S.; Friedlander P.; Feilding A.; Riba J.; Pascual J. C. (2016) Exploring the therapeutic potential of Ayahuasca: acute intake increases mindfulness- related capacities. Psychopharmacology 233 (5), 823–829. 10.1007/s00213-015-4162-0. [DOI] [PubMed] [Google Scholar]
- Studerus E.; Kometer M.; Hasler F.; Vollenweider F. X. (2011) Acute, subacute and long-term subjective effects of psilocybin in healthy humans: a pooled analysis of experimental studies. J. Psychopharmacol. 25 (11), 1434–1452. 10.1177/0269881110382466. [DOI] [PubMed] [Google Scholar]
- Riba J.; Rodríguez-Fornells A.; Urbano G.; Morte A.; Antonijoan R.; Montero M.; Barbanoj M. J.; Callaway M. J. (2001) Subjective effects and tolerability of the South American psychoactive beverage Ayahuasca in healthy volunteers. Psychopharmacology 154 (1), 85–95. 10.1007/s002130000606. [DOI] [PubMed] [Google Scholar]
- Johnson M. W.; Richards W.; Griffiths R. R. (2008) Human hallucinogen research: guidelines for safety. J. Psychopharmacol. 22 (6), 603–620. 10.1177/0269881108093587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris R.; Bolstridge M.; Day C. M. J.; Rucker J.; Watts R.; Erritzoe D. E.; Kaelen M.; et al. (2018) Psilocybin with psychological support for treatment-resistant depression: six-month follow-up. Psychopharmacology 235 (2), 399. 10.1007/s00213-017-4771-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M. W.; Garcia-Romeu A.; Griffiths R. R. (2017) Long-term follow-up of psilocybin-facilitated smoking cessation. Am. J. Drug Alcohol Abuse 43 (1), 55–60. 10.3109/00952990.2016.1170135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielson E. M.; May D. G.; Forcehimes A. A.; Bogenschutz M. P. (2018) The Psychedelic Debriefing in Alcohol Dependence Treatment: Illustrating Key Change Phenomena through Qualitative Content Analysis of Clinical Sessions. Front. Pharmacol. 9, 132. 10.3389/fphar.2018.00132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths R. R.; Johnson M. W.; Carducci M. A.; Umbricht A.; Richards W. A.; Richards B. D.; Klinedinst M. A.; Cosimano M. P. (2016) Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double- blind trial. J. Psychopharmacol. 30 (12), 1181–1197. 10.1177/0269881116675513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett F. S.; Johnson M. W.; Griffiths R. R. (2015) Validation of the revised Mystical Experience Questionnaire in experimental sessions with psilocybin. J. Psychopharmacol. 29 (11), 1182–1190. 10.1177/0269881115609019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roseman L.; Nutt D. J.; Carhart-Harris R. (2018) Quality of Acute Psychedelic Experience Predicts Therapeutic Efficacy of Psilocybin for Treatment-Resistant Depression. Front. Pharmacol. 8, 974. 10.3389/fphar.2017.00974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonaro T. M.; Bradstreet M. P.; Barrett F. S.; MacLean K. A.; Jesse R.; Johnson M. W.; Griffiths R. R. (2016) Survey study of challenging experiences after ingesting psilocybin mushrooms: Acute and enduring positive and negative consequences. J. Psychopharmacol. 30 (12), 1268–1278. 10.1177/0269881116662634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths R. R.; Richards W.; Johnson M. W.; McCann U.; Jesse R. (2008) Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later. J. Psychopharmacol. 22 (6), 621–632. 10.1177/0269881108094300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen M. K.; Fisher P. M.; Stenbæk D. S.; Kristiansen S.; Burmester D.; Lehel S.; Knudsen G. M.; et al. (2020) A single psilocybin dose is associated with long-term increased mindfulness, preceded by a proportional change in neocortical 5-HT2A receptor binding. Eur. Neuropsychopharmacol. 33, 71–80. 10.1016/j.euroneuro.2020.02.001. [DOI] [PubMed] [Google Scholar]
- Uthaug M. V.; Lancelotta R.; van Oorsouw K.; Kuypers K. P. C.; Mason N.; Rak J.; Ramaekers J. G.; et al. (2019) A single inhalation of vapor from dried toad secretion containing 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) in a naturalistic setting is related to sustained enhancement of satisfaction with life, mindfulness-related capacities, and a decrement of psychopathological symptoms. Psychopharmacology 236 (9), 2653–2666. 10.1007/s00213-019-05236-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampedro F.; de la Fuente Revenga M.; Valle M.; Roberto N.; Domínguez-Clavé E.; Elices M.; Riba J.; et al. (2017) Assessing the Psychedelic “After-Glow” in Ayahuasca Users: Post-Acute Neurometabolic and Functional Connectivity Changes Are Associated with Enhanced Mindfulness Capacities. Int. J. Neuropsychopharmacol. 20 (9), 698–711. 10.1093/ijnp/pyx036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy-Beiner A.; Soar K. (2020) Ayahuasca’s ‘afterglow’: improved mindfulness and cognitive flexibility in ayahuasca drinkers. Psychopharmacology 237 (4), 1161–1169. 10.1007/s00213-019-05445-3. [DOI] [PubMed] [Google Scholar]
- Speth J.; Speth C.; Kaelen M.; Schloerscheidt A. M.; Feilding A.; Nutt D. J.; Carhart- Harris R. (2016) Decreased mental time travel to the past correlates with default-mode network disintegration under lysergic acid diethylamide. J. Psychopharmacol. 30 (4), 344–353. 10.1177/0269881116628430. [DOI] [PubMed] [Google Scholar]
- Mian M. N.; Altman B. R.; Earleywine M. (2020) Ayahuasca’s Antidepressant Effects Covary with Behavioral Activation as Well as Mindfulness. J. Psychoact. Drugs 52 (2), 130–137. 10.1080/02791072.2019.1674428. [DOI] [PubMed] [Google Scholar]
- Fox K. C. R.; Dixon M. L.; Nijeboer S.; Girn M.; Floman J. L.; Lifshitz M.; Christoff K.; et al. (2016) Functional neuroanatomy of meditation: A review and meta-analysis of 78 functional neuroimaging investigations. Neurosci. Biobehav. Rev. 65, 208. 10.1016/j.neubiorev.2016.03.021. [DOI] [PubMed] [Google Scholar]
- Josipovic Z. (2014) Neural correlates of nondual awareness in meditation. Ann. N. Y. Acad. Sci. 1307 (1), 9–18. 10.1111/nyas.12261. [DOI] [PubMed] [Google Scholar]
- Barrett F. S.; Griffiths R. R. (2017) Classic Hallucinogens and Mystical Experiences: Phenomenology and Neural Correlates. Curr. Top. Behav. Neurosci. 36 (1), 393–430. 10.1007/7854_2017_474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smigielski L.; Scheidegger M.; Kometer M.; Vollenweider F. X. (2019) Psilocybin-assisted mindfulness training modulates self-consciousness and brain default mode network connectivity with lasting effects. NeuroImage 196, 207–215. 10.1016/j.neuroimage.2019.04.009. [DOI] [PubMed] [Google Scholar]
- Palhano-Fontes F.; Andrade K. C.; Tofoli L. F.; Santos A. C.; Crippa J. A. S.; Hallak J. E.; de Araujo D. B.; Ribeiro S. (2015) The psychedelic state induced by ayahuasca modulates the activity and connectivity of the default mode network. PLoS One 10 (2), e0118143. 10.1371/journal.pone.0118143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebedev A. V.; Lövdén M.; Rosenthal G.; Feilding A.; Nutt D. J.; Carhart-Harris R. L. (2015) Finding the self by losing the self: Neural correlates of ego-dissolution under psilocybin. Human Brain Mapping 36 (8), 3137–53. 10.1002/hbm.22833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinspoon L.; Doblin R. (2001) Psychedelics as catalysts of insight-oriented psychotherapy. Social Research 68 (3), 677–695. [Google Scholar]
- Lerner M.; Lyvers M. (2006) Values and beliefs of psychedelic drug users: a cross-cultural study. J. Psychoact. Drugs 38 (2), 143–147. 10.1080/02791072.2006.10399838. [DOI] [PubMed] [Google Scholar]
- Ross S.; Bossis A.; Guss J.; Agin-Liebes G.; Malone T.; Cohen B.; Schmidt B. L.; et al. (2016) Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J. Psychopharmacol. 30 (12), 1165–1180. 10.1177/0269881116675512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris R.; Bolstridge M.; Rucker J.; Day C. M. J.; Erritzoe D.; Kaelen M.; Nutt D. J.; et al. (2016) Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry 3 (7), 619–627. 10.1016/S2215-0366(16)30065-7. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K.; Bowen S. (2010) Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention. Journal of Consulting and Clinical Psychology 78 (3), 362–374. 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piet J.; Hougaard E. (2011) The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: A systematic review and meta-analysis. Clinical Psychology Review 31 (6), 1032–1040. 10.1016/j.cpr.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Hunt C. A.; Hoffman M. A.; Mohr J. J.; Williams A. l. (2020) Assessing Perceived Barriers to Meditation: the Determinants of Meditation Practice Inventory-Revised (DMPI-R). Mindfulness 11 (1), 1139–1149. 10.1007/s12671-020-01308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuyken W.; Byford S.; Taylor R. S.; Watkins E.; Holden E.; White K.; Teasdale J. D.; et al. (2008) Mindfulness-Based Cognitive Therapy to Prevent Relapse in Recurrent Depression. Journal of Consulting and Clinical Psychology 76 (6), 966–978. 10.1037/a0013786. [DOI] [PubMed] [Google Scholar]
- Chambers R.; Gullone E.; Allen N. B. (2009) Mindful emotion regulation: An integrative review. Clinical Psychology Review 29 (6), 560–572. 10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Mikulas W. L. (2011) Mindfulness: Significant Common Confusions. Mindfulness 2 (1), 1–7. 10.1007/s12671-010-0036-z. [DOI] [Google Scholar]
- Shapiro D. H. (1992) Adverse effects of meditation: a preliminary investigation of long- term meditators. International Journal of Psychosomatics 39 (1–4), 62–67. [PubMed] [Google Scholar]
- Farb N. A. S.; Segal Z. V.; Mayberg H.; Bean J.; McKeon D.; Fatima Z.; Anderson A. K. (2007) Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Social Cognitive and Affective Neuroscience 2 (4), 313. 10.1093/scan/nsm030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krippner S. (1968) The psychedelic state, the hypnotic trance, and the creative act. Journal of Humanistic Psychology 8 (1), 49–67. 10.1177/002216786800800105. [DOI] [Google Scholar]
- Watts R.; Day C.; Krzanowski J.; Nutt D.; Carhart-Harris R. (2017) Patients’ Accounts of Increased “Connectedness” and “Acceptance” After Psilocybin for Treatment- Resistant Depression. Journal of Humanistic Psychology 57 (5), 520–564. 10.1177/0022167817709585. [DOI] [Google Scholar]
- Brewer J. A.; Worhunsky P. D.; Gray J. R.; Tang Y.-Y.; Weber J.; Kober H. (2011) Meditation experience is associated with differences in default mode network activity and connectivity. Proc. Natl. Acad. Sci. U. S. A. 108 (50), 20254. 10.1073/pnas.1112029108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkovich-Ohana A.; Glicksohn J.; Goldstein A. (2012) Mindfulness-induced changes in gamma band activity – Implications for the default mode network, self-reference and attention. Clin. Neurophysiol. 123 (4), 700–710. 10.1016/j.clinph.2011.07.048. [DOI] [PubMed] [Google Scholar]
- Garrison K. A.; Zeffiro T. A.; Scheinost D.; Constable R. T.; Brewer J. A. (2015) Meditation leads to reduced default mode network activity beyond an active task. Cognitive, Affective & Behavioral Neuroscience 15 (3), 712–720. 10.3758/s13415-015-0358-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris R.; Erritzoe D.; Williams T.; Stone J. M.; Reed L. J.; Colasanti A.; Nutt D. J.; et al. (2012) Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. Proc. Natl. Acad. Sci. U. S. A. 109 (6), 2138. 10.1073/pnas.1119598109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasquini L.; Palhano-Fontes F.; Araujo D. B. (2020) Subacute effects of the psychedelic ayahuasca on the salience and default mode networks. J. Psychopharmacol. 34 (6), 623–635. 10.1177/0269881120909409. [DOI] [PubMed] [Google Scholar]
- Piron H. (2001) The meditation depth index (MEDI) and the meditation depth questionnaire (MEDEQ). Journal for Meditation and Meditation Research 1 (1), 69–92. [Google Scholar]
- Parsons C. E.; Crane C.; Parsons L. J.; Fjorback L. O.; Kuyken W. (2017) Home practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behaviour Research and Therapy 95, 29–41. 10.1016/j.brat.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strohmaier S. (2020) The Relationship Between Doses of Mindfulness-Based Programs and Depression, Anxiety, Stress, and Mindfulness: a Dose-Response Meta-Regression of Randomized Controlled Trials. Mindfulness 11, 1315–1335. 10.1007/s12671-020-01319-4. [DOI] [Google Scholar]
- Bowen S.; Kurz A. S. (2012) Between-session practice and therapeutic alliance as predictors of mindfulness after mindfulness-based relapse prevention. J. Clin. Psychol. 68 (3), 236–245. 10.1002/jclp.20855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears S.; Kraus S.; Carlough K.; Treat E. (2011) Perceived Benefits and Doubts of Participants in a Weekly Meditation Study. Mindfulness 2 (3), 167–174. 10.1007/s12671-011-0055-4. [DOI] [Google Scholar]
- Belser A. B.; Agin-Liebes G.; Swift T. C.; Terrana S.; Devenot N.; Friedman H. L.; Ross S.; et al. (2017) Patient experiences of psilocybin-assisted psychotherapy: an interpretative phenomenological analysis. Journal of Humanistic Psychology 57 (4), 354–388. 10.1177/0022167817706884. [DOI] [Google Scholar]
- Noorani T.; Garcia-Romeu A.; Swift T. C.; Griffiths R. R.; Johnson M. W. (2018) Psychedelic therapy for smoking cessation: qualitative analysis of participant accounts. J. Psychopharmacol. 32 (7), 756–769. 10.1177/0269881118780612. [DOI] [PubMed] [Google Scholar]
- Lomas T.; Cartwright T.; Edginton T.; Ridge D. (2015) A Qualitative Analysis of Experiential Challenges Associated with Meditation Practice. Mindfulness 6 (4), 848–860. 10.1007/s12671-014-0329-8. [DOI] [Google Scholar]
- Cohen-Katz J.; Wiley S.; Capuano T.; Baker D. M.; Deitrick L.; Shapiro S. (2005) The Effects of Mindfulness-based Stress Reduction on Nurse Stress and Burnout: A Qualitative and Quantitative Study, Part III. Holistic Nursing Practice 19 (2), 78. 10.1097/00004650-200503000-00009. [DOI] [PubMed] [Google Scholar]
- Hayes S. C.; Wilson K. G.; Gifford E. V.; Follette V. M.; Strosahl K. (1996) Experiential Avoidance and Behavioral Disorders: A Functional Dimensional Approach to Diagnosis and Treatment. Journal of Consulting and Clinical Psychology 64 (6), 1152–1168. 10.1037/0022-006X.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Chawla N.; Ostafin B. (2007) Experiential avoidance as a functional dimensional approach to psychopathology: an empirical review. J. Clin. Psychol. 63 (9), 871–890. 10.1002/jclp.20400. [DOI] [PubMed] [Google Scholar]
- Johnson M. W.; Hendricks P. S.; Barrett F. S.; Griffiths R. R. (2019) Classic psychedelics: An integrative review of epidemiology, therapeutics, mystical experience, and brain network function. Pharmacol. Ther. 197, 83–102. 10.1016/j.pharmthera.2018.11.010. [DOI] [PubMed] [Google Scholar]
- Zeifman R. J.; Wagner A. C.; Watts R.; Kettner H.; Mertens L. J.; Carhart-Harris R. L. (2020) Post-Psychedelic Reductions in Experiential Avoidance Are Associated With Decreases in Depression Severity and Suicidal Ideation. Frontiers in psychiatry 11, 782. 10.3389/fpsyt.2020.00782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks P. S. (2018) Awe: a putative mechanism underlying the effects of classic psychedelic-assisted psychotherapy. International Review of Psychiatry 30 (4), 331–342. 10.1080/09540261.2018.1474185. [DOI] [PubMed] [Google Scholar]
- Roseman L.; Haijen E.; Idialu-Ikato K.; Kaelen M.; Watts R.; Carhart-Harris R. (2019) Emotional breakthrough and psychedelics: Validation of the Emotional Breakthrough Inventory. J. Psychopharmacol. 33 (9), 1076–1087. 10.1177/0269881119855974. [DOI] [PubMed] [Google Scholar]
- MacLean K. A.; Johnson M. W.; Griffiths R. R. (2011) Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. J. Psychopharmacol. 25 (11), 1453–1461. 10.1177/0269881111420188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebedev A. V.; Kaelen M.; Lövdén M.; Nilsson J.; Feilding A.; Nutt D. J.; Carhart- Harris R. L. (2016) LSD-induced entropic brain activity predicts subsequent personality change. Human Brain Mapping 37 (9), 3203–3213. 10.1002/hbm.23234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro S. L.; Carlson L. E.; Astin J. A.; Freedman B. (2006) Mechanisms of mindfulness. J. Clin. Psychol. 62 (3), 373–386. 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- Jazaieri H.; McGonigal K.; Jinpa T.; Doty J. R.; Gross J. J.; Goldin P. R. (2014) A randomized controlled trial of compassion cultivation training: Effects on mindfulness, affect, and emotion regulation. Motivation and Emotion 38 (1), 23–35. 10.1007/s11031-013-9368-z. [DOI] [Google Scholar]
- Neff K. (2003) Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self and Identity 2 (2), 85–101. 10.1080/15298860309032. [DOI] [Google Scholar]
- Zessin U.; Dickhäuser O.; Garbade S. (2015) The relationship between self-compassion and well-being: A meta-analysis. Applied Psychology: Health and Well-Being 7 (3), 340–364. 10.1111/aphw.12051. [DOI] [PubMed] [Google Scholar]
- Campos D.; Cebolla A.; Quero S.; Bretón-López J.; Botella C.; Soler J.; Baños R. M.; et al. (2016) Meditation and happiness: Mindfulness and self-compassion may mediate the meditation–happiness relationship. Personality and Individual Differences 93, 80–85. 10.1016/j.paid.2015.08.040. [DOI] [Google Scholar]
- Van Dam N. T.; Sheppard S. C.; Forsyth J. P.; Earleywine M. (2011) Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. Journal of Anxiety Disorders 25 (1), 123–130. 10.1016/j.janxdis.2010.08.011. [DOI] [PubMed] [Google Scholar]
- Hofmann S. G.; Petrocchi N.; Steinberg J.; Lin M.; Arimitsu K.; Kind S.; Stangier U. (2015) Loving-Kindness Meditation to Target Affect in Mood Disorders: A Proof-of- Concept Study. Evidence-Based Complementary and Alternative Medicine 269126. 10.1155/2015/269126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearney D. J.; Malte C. A.; McManus C.; Martinez M. E.; Felleman B.; Simpson T. L. (2013) Loving-Kindness Meditation for Posttraumatic Stress Disorder: A Pilot Study. Journal of Traumatic Stress 26 (4), 426–434. 10.1002/jts.21832. [DOI] [PubMed] [Google Scholar]
- Shahar B.; Szepsenwol O.; Zilcha-Mano S.; Haim N.; Zamir O.; Levi-Yeshuvi S.; Levit- Binnun N. (2015) A Wait-List Randomized Controlled Trial of Loving-Kindness Meditation Programme for Self-Criticism. Clinical Psychology & Psychotherapy 22 (4), 346–356. 10.1002/cpp.1893. [DOI] [PubMed] [Google Scholar]
- Seppala E. M.; Hutcherson C. A.; Nguyen D. T. H.; Doty J. R.; Gross J. J. (2014) Loving-kindness meditation: a tool to improve healthcare provider compassion, resilience, and patient care. Journal of Compassionate Health Care 1 (1), 9–9. 10.1186/s40639-014-0005-9. [DOI] [Google Scholar]
- Preller K.; Vollenweider F. (2019) Modulation of Social Cognition via Hallucinogens and “Entactogens”. Frontiers in Psychiatry 10, 881. 10.3389/fpsyt.2019.00881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Mulukom V.; Patterson R. E.; van Elk M. (2020) Broadening Your Mind to Include Others: The relationship between serotonergic psychedelic experiences and maladaptive narcissism. Psychopharmacology 237 (9), 2725–2737. 10.1007/s00213-020-05568-y. [DOI] [PubMed] [Google Scholar]
- Pokorny T.; Preller K. H.; Kometer M.; Dziobek I.; Vollenweider F. X. (2017) Effect of Psilocybin on Empathy and Moral Decision-Making. Int. J. Neuropsychopharmacol. 20 (9), 747–757. 10.1093/ijnp/pyx047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett F. S.; Bradstreet M. P.; Leoutsakos J.-M. S.; Johnson M. W.; Griffiths R. R. (2016) The Challenging Experience Questionnaire: Characterization of challenging experiences with psilocybin mushrooms. J. Psychopharmacol. 30 (12), 1279. 10.1177/0269881116678781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis A. K.; Barrett F. S.; Griffiths R. R. (2020) Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. Journal of Contextual Behavioral Science 15, 39–45. 10.1016/j.jcbs.2019.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mithoefer M. C. (2017). A Manual for MDMA-Assisted Psychotherapy in the Treatment of Posttraumatic Stress Disorder., version 8.1. Retrieved from: https://maps.org/research/mdma/mdma-research-timeline/4887-a-manual-for-mdma-assisted-psychotherapy-in-the-treatment-of-ptsd.
- Moore S. D.; Brody L. R.; Dierberger A. E. (2009) Mindfulness and experiential avoidance as predictors and outcomes of the narrative emotional disclosure task. J. Clin. Psychol. 65 (9), 971–988. 10.1002/jclp.20600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agin-Liebes G. I.; Malone T.; Yalch M. M.; et al. (2020) Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. J. Psychopharmacol. 34 (2), 155–166. 10.1177/0269881119897615. [DOI] [PubMed] [Google Scholar]
- Preston J. L.; Shin F. (2017) Spiritual experiences evoke awe through the small self in both religious and non-religious individuals. Journal of Experimental Social Psychology 70, 212–221. 10.1016/j.jesp.2016.11.006. [DOI] [Google Scholar]
- Fredrickson B. L.; Cohn M. A.; Coffey K. A.; Pek J.; Finkel S. M. (2008) Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology 95 (5), 1045–1062. 10.1037/a0013262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falb M. D.; Pargament K. I. (2012) Relational mindfulness, spirituality, and the therapeutic bond. Asian Journal of Psychiatry 5 (4), 351–354. 10.1016/j.ajp.2012.07.008. [DOI] [PubMed] [Google Scholar]
- Tursi M. F. d. S.; Baes C. v. W.; Camacho F. R. d. B.; Tofoli S. M. d. C.; Juruena M. F. (2013) Effectiveness of psychoeducation for depression: A systematic review. Australian and New Zealand Journal of Psychiatry 47 (11), 1019–1031. 10.1177/0004867413491154. [DOI] [PubMed] [Google Scholar]
- Welwood J. (2002) Toward a psychology of awakening: Buddhism, psychotherapy, and the path of personal and spiritual transformation, Shambhala Publications. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.