Abstract
Background:
Burnout among postgraduate medical trainees (PMTs) is increasingly being recognized as a crisis in the medical profession. We aimed to establish the prevalence of burnout among PMTs, identify risk and protective factors, and assess whether burnout varied by country of training, year of study and specialty of practice.
Methods:
We systematically searched MEDLINE, Embase, PsycINFO, the Cochrane Database of Systematic Reviews, Web of Science and Education Resources Information Center from their inception to Aug. 21, 2018, for studies of burnout among PMTs. The primary objective was to identify the global prevalence of burnout among PMTs. Our secondary objective was to evaluate the association between burnout and country of training, year of study, specialty of training and other sociodemographic factors commonly thought to be related to burnout. We employed random-effects meta-analysis and meta-regression techniques to estimate a pooled prevalence and conduct secondary analyses.
Results:
In total, 8505 published studies were screened, 196 met eligibility and 114 were included in the meta-analysis. The pooled prevalence of burnout was 47.3% (95% confidence interval 43.1% to 51.5%), based on studies published over 20 years involving 31 210 PMTs from 47 countries. The prevalence of burnout remained unchanged over the past 2 decades. Burnout varied by region, with PMTs of European countries experiencing the lowest level. Burnout rates among medical and surgical PMTs were similar.
Interpretation:
Current wellness efforts and policies have not changed the prevalence of burnout worldwide. Future research should focus on understanding systemic factors and leveraging these findings to design interventions to combat burnout.
Study registration:
PROSPERO no. CRD42018108774
We are in a critical period within the medical profession as alarming rates of suicide among physicians bring burnout to the forefront.1–3 The effects of burnout are widespread, affecting physician wellness and productivity as well as patient health outcomes.2,4 Burnout is characterized by physical, emotional and mental exhaustion, resulting from long-term involvement in emotionally taxing situations.5 In the United States, about half of practising physicians experience an episode of burnout during their career.1,6,7 Canadian data report a slightly lower prevalence; about 30% of the surveyed physicians endorsed burnout.8
Residency is a particularly stressful time; the trainee is tasked with a tremendous responsibility of consistently providing high-quality care while learning and integrating new skills. Adapting to these job demands has a direct consequence on one’s emotional and intellectual reserve, and the ability to establish a healthy home–work interface.9 The prevalence of burnout among postgraduate medical trainees (PMTs) varies widely from 3% to 88%. 7,10–13 However, existing attempts at systematic investigation of burnout in this group have been limited by methodological flaws including restrictive search strategies, lack of evaluation of temporal and associated factors, and lack of global investigation.7,10–13
The objective of our study was twofold; our main aim was to establish the prevalence of burnout among PMTs based on a meta-analysis of studies from across the world. Second, we used the extracted data to explore whether commonly studied factors, such as age, sex and relationship status, are shown to protect against or increase risk for burnout as well as to understand, using meta-regression, whether country of training, year of study and specialty of training were associated with burnout, as these factors may explain heterogeneity in the prevalence of burnout.
Methods
Study design and data sources
We conducted a systematic review of the literature to identify all studies evaluating burnout among PMTs. The search strategy was developed and conducted by a health research librarian (L.B.) at McMaster University. We searched MEDLINE (1946 to Aug. 21, 2018), Embase (1974 to Aug. 21, 2018), PsycINFO (1987 to Aug. 21, 2018), the Cochrane Database of Systematic Reviews (2005 to Aug. 21, 2018), Web of Science (1976 to Aug. 21, 2018) and Education Resources Information Center database (ERIC) (1966 to Aug. 21, 2018). The search encompassed terms used to refer to PMTs worldwide (e.g., resident, intern, junior physician and house officer), burnout and its components (emotional exhaustion, physical exhaustion, depersonalization and cynicism) and the setting (medical, hospital and clinical).
MEDLINE was used to develop the initial search and the search strategy was used to search the other databases. Results were exported from each database after all searches had been made and finalized. The reference lists of reviews identified were searched for relevant articles. No restrictions on geography or date were applied. The full search strategy is provided in Appendix 1, available at www.cmajopen.ca/content/9/1/E189/suppl/DC1. The protocol was registered in PROS-PERO (CRD42018108774).
Study selection
All studies measuring burnout among PMTs were included regardless of country of training, specialty, year of training or setting.
The Maslach Burnout Inventory (MBI) is a validated and commonly used tool to measure burnout.14 Although this tool was used by most included studies, there is a lack of unified and standardized definition for burnout in the current literature. Therefore, we accepted the definition of burnout as used in the study, recognizing that it is measured and defined variably across the literature.
The MBI measures burnout in the context of emotional exhaustion, depersonalization and lack of personal accomplishment. This is a 22-item self-administered questionnaire whereby respondents are asked to rank their responses on a 7-point Likert scale (ranging from 0 to 6, or less commonly, from 1 to 7). Although the MBI was initially created to assess burnout on a continuum, it has commonly been adapted to dichotomize burnout.14 However, there is a lack of standardization regarding which of the 3 dimensions are necessary to constitute burnout or specific cut-off values for each of these dimensions.2 In addition, modified versions of the MBI, including single item measures, are sometimes employed.15,16
We included studies that either reported or provided data necessary to quantify burnout, such as through the prevalence of burnout, PMTs’ scores on a burnout scale or their classifications into percentiles based on score. We included studies published in English only. Studies investigating doctors of osteopathic medicine were excluded, as were case studies, dissertations and opinion papers.
All titles, abstracts and full-text articles were evaluated for eligibility independently and in duplicate by 5 reviewers (L.N., B.S., A.S., O.K. and F.N.) using the Covidence software. 17 Discrepancies were discussed and resolved by consensus; if consensus was not reached, the decision was taken by an independent reviewer (L.N. or B.S.). In addition, we reviewed the reference list of each identified study.
Data extraction and quality assessment
From each study, we extracted study characteristics, participant demographic characteristics, definition and measurement of burnout, burnout rates and factors associated with burnout. Definitions for the following extracted associated factors were accepted as they were reported by study authors: depression, job satisfaction and income satisfaction.
Data were extracted independently and in duplicate by 4 reviewers (L.N., B.S., A.S. and F.N.). As before, discrepancies were resolved by an independent reviewer (L.N. or B.S.). There is a lack of a validated tool to assess the risk of bias in cross-sectional studies, and this prohibited us from assessing risk systematically. However, using the general framework of the Newcastle–Ottawa Scale, a well-established tool to assess risk of bias, the same reviewers also rated the quality of included studies based on representativeness of the sample, sample size, ascertainment of outcome and reporting of findings.18
Statistical analysis
Primary analysis
For our analyses, we accepted the reported value of burnout as defined by each individual study, regardless of the tool employed. We estimated a random-effects pooled prevalence for all included studies using a restricted maximum-likelihood estimator. We used raw proportions without transforming the data based on recommendations by Lipsey and Wilson, since most of our proportions were between 0.2 and 0.8.19 The meta-analysis was conducted in R using the metafor package.20
As we anticipated systematic differences among the results of studies (heterogeneity), we report both the τ2 values of heterogeneity and calculated I2. We sought to understand whether prevalence of burnout changed depending on the tool used to ascertain the prevalence. Therefore, we conducted a meta-regression analysis with the use of the MBI as a categorical moderator variable (yes v. no). We hypothesized that since use of the MBI decreases heterogeneity in how burnout is defined, it would be a significant predictor in our meta-regression.21,22 If use of the MBI was found to be a significant variable, we intended to adjust all additional analyses for the use of the MBI.
We conducted a subgroup analysis of North American studies to establish a pooled estimate of burnout among North American PMTs. As before, we employed a random-effects model to pool data.
Secondary analysis
We conducted 2 secondary analyses. First, we extracted data on reported risk and protective factors, including age, sex, relationship status (single v. having a partner), depression, level of stress, work hours, frequency of call shifts, job satisfaction, wage or income satisfaction, family or network support, sleep and level of training. We present a descriptive summary of associations found for these factors in the literature. Second, we employed meta-regression, a regression technique of aggregate data which allows for study of the impact of moderator variables on pooled effect size, to study the effect of region of training, program of residency (medicine v. surgery) and the year burnout data were collected on the pooled measure of burnout.
We first categorized regions as continents, but as only a few studies were conducted in Africa, Asia, Australia, the Middle East and South America, we collapsed these regions into one and compared them against Europe and North America, which had larger samples.
A random-effect inverse-variance weighted model was used to conduct the meta-regression. A 2-tailed Q-statistic was used to test the significance of the slope in a multivariate analysis and the standard Z-statistic in a univariate analysis. We used the Comprehensive Meta-Analysis software (version 3) to conduct our analysis. Because of the post hoc nature of this analysis, we did not take a significant finding to be definitive, but rather to promote a direction for future research.
Ethics approval
In keeping with research ethics board guidelines at McMaster University, ethics approval was not required for this systematic review.
Results
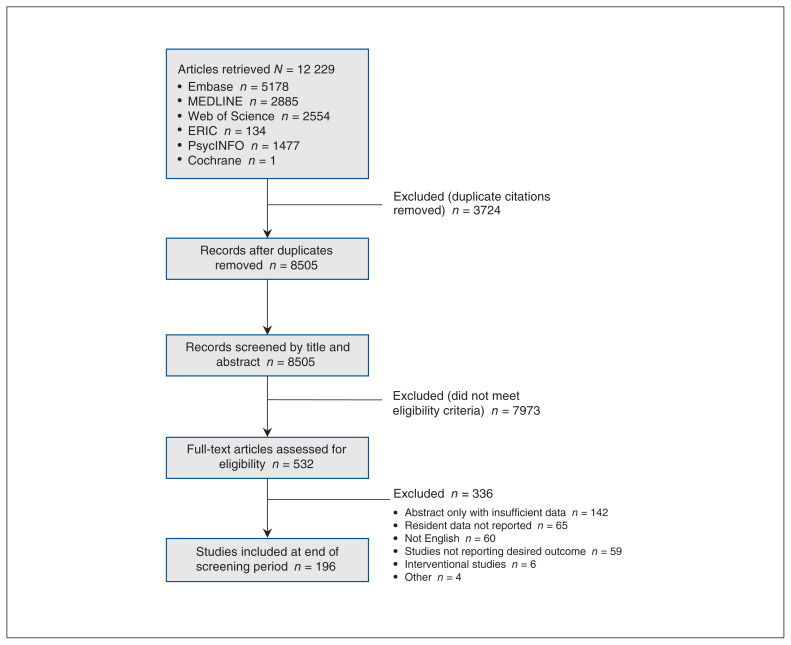
Upon completion of screening, 196 of the 8505 studies met our eligibility criteria (Figure 1). These studies were published between 1987 and 2018 and represent data from 44 128 PMTs across 47 countries; a large proportion of studies (82/196) were conducted in the US. The studies included PMTs from a variety of programs and at different levels of training. Of the 196 studies meeting eligibility criteria, an overall proportion of burnout was reported for 31 210 PMTs in 114 studies conducted between 2001 and 2017. Four of these 114 studies report burnout in 2 separate populations of PMTs, rendering 118 data sets eligible for our meta-analysis (Appendix 2, available at www.cmajopen.ca/content/9/1/E189/suppl/DC1). Therefore, our analysis of risk and protective factors is based on 44 128 PMTs from 196 studies, whereas our meta-analysis includes 31 210 PMTs from 114 studies.
Figure 1:
Flow diagram based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline overviewing selection of studies for inclusion in the systematic review. Note: ERIC = Education Resources Information Center.
Measurement of burnout
Among the studies included in our review, burnout was measured using a variety of tools, detailed in Appendix 3, available at www.cmajopen.ca/content/9/1/E189/suppl/DC1. The most commonly used tool to assess burnout was the MBI (138 of 196 studies). Among the 138 studies that used the MBI, 83 studies reported an overall proportion of PMTs experiencing burnout. These studies defined burnout using 9 different definitions, with the most common one being a high score in either emotional exhaustion or depersonalization (42 of 83). Five of the 83 studies did not report how overall burnout was determined. The cut-off values for the individual dimensions also varied, as described in Appendix 2. For instance, there were 6 different definitions for high emotional exhaustion, whereas 24 of 83 studies did not report a cut-off value for emotional exhaustion.
Some studies (29 of 196) used a modified version of the MBI. A single item measure for emotional exhaustion and depersonalization was the most commonly employed modified version. Thirty-one of 196 studies used a different tool altogether, as described in Appendix 3.
Pooled prevalence of burnout
Overall
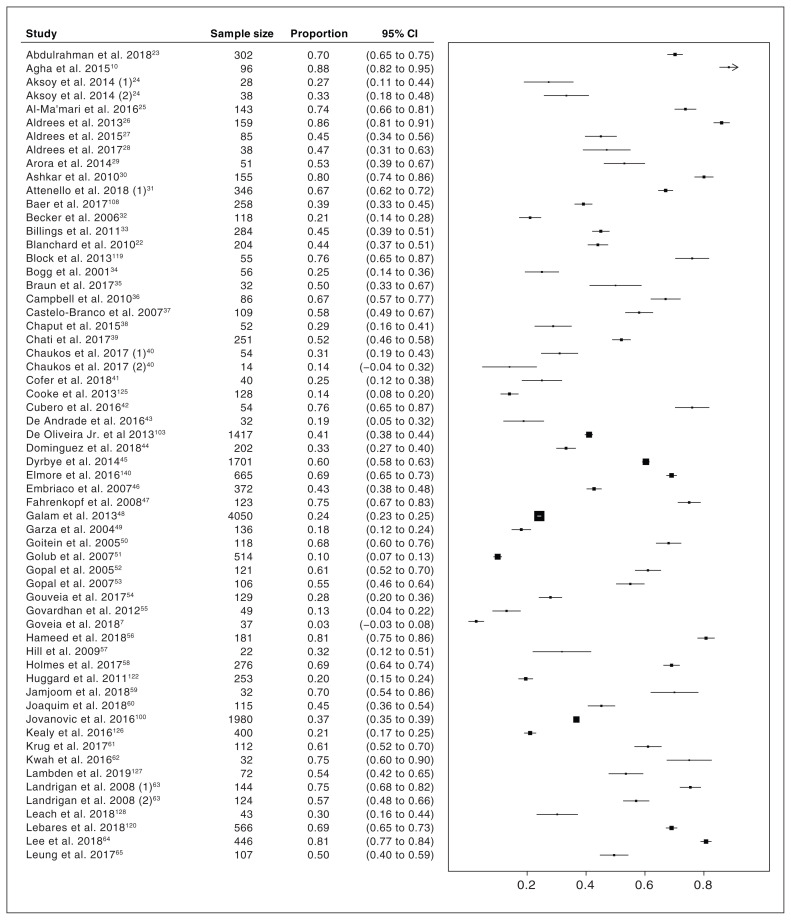
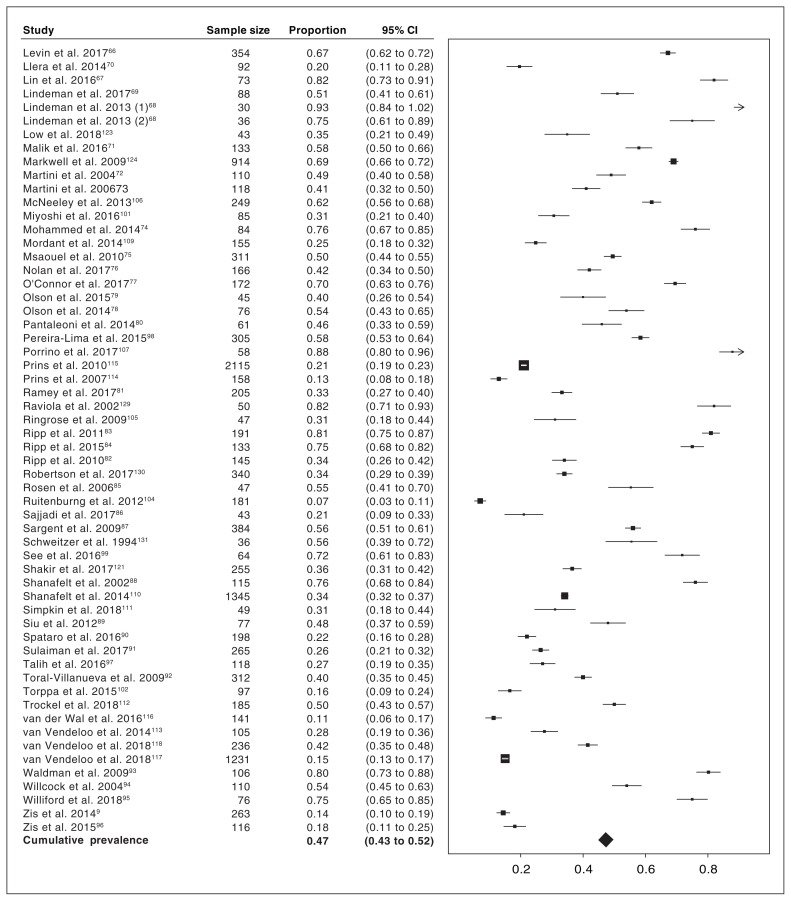
As mentioned previously, 114 studies were included in our meta-analysis. These data came from 31 210 PMTs from 47 countries. The pooled random-effects estimate of burnout was 47.3% (95% confidence interval [CI] 43.1% to 51.5%). An analysis of heterogeneity suggests significant differences among the pooled studies; τ2 was 0.052 (phet < 10−16) and I2 was 98.56%. A forest plot of all studies is presented in Figure 2 and Figure 3.7,9,10,22–132 We then sought to understand whether capturing burnout in a standardized manner using the MBI would explain heterogeneity in prevalence. Thus, we conducted a meta-regression analysis with the MBI use as a categorical variable. As expected, use of the MBI to capture burnout significantly explained heterogeneity in the prevalence (meta-regression β 0.117, 95% CI 0.027 to 0.207. We therefore adjusted our future analyses for use of the MBI.
Figure 2:
Forest plot with prevalence of burnout among postgraduate medical trainees reported by included studies in the meta-analysis and pooled prevalence based on all data. Forest plot continues in Figure 3. Note: CI = confidence interval.
Figure 3:
Forest plot with prevalence of burnout among postgraduate medical trainees reported by included studies in the meta-analysis and pooled prevalence based on all data. Forest plot continued from Figure 2; contains cumulative frequencies of Figure 2 and Figure 3. Note: CI = confidence interval.
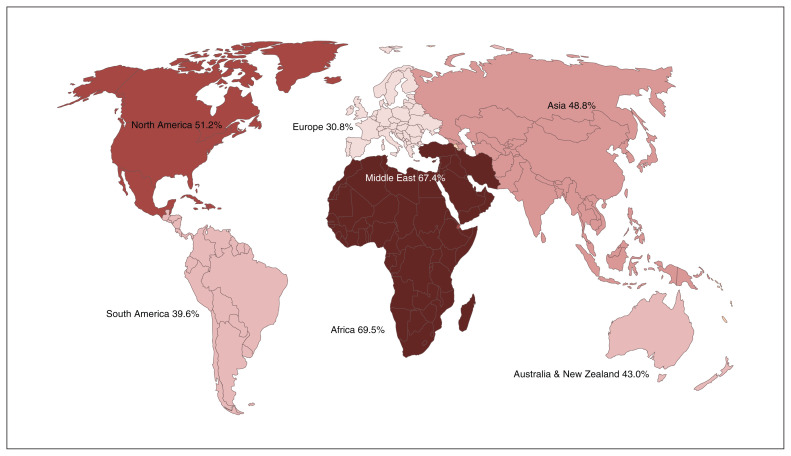
North America
Sixty studies captured North American data; the pooled random-effects estimate of burnout among North American PMTs was 51.2% (95% CI 45.9% to 56.6%). We further explored regional variation in burnout across the world and results of this analysis are presented below.
Meta-regression
Year of study
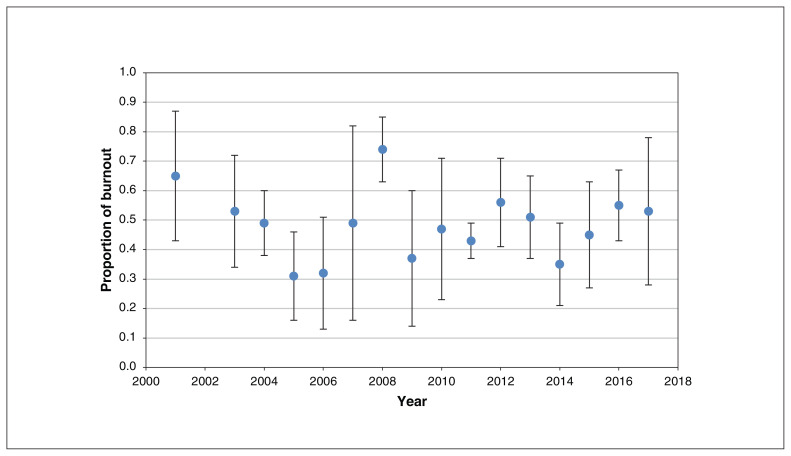
We undertook a meta-regression of burnout with the year in which a study was conducted to evaluate whether heterogeneity in the prevalence of burnout was explained by time (i.e., whether burnout changed over time). Data for this analysis were available from 100 studies; 14 did not report the year of survey. Our analysis, adjusted for MBI use, found that the year of study was not a significant moderator of burnout (estimate of meta-regression β 0.002, 95% CI −0.009 to 0.013). Burnout prevalence over the years is presented in Figure 4.
Figure 4:
Mean prevalence of burnout by year of data collection. Error bars represent 95% confidence intervals.
Medical versus surgical training
We also investigated whether prevalence of burnout was affected by the choice of specialty; specifically, we were interested in understanding whether medical PMTs experienced differing rates of burnout compared with surgical PMTs. Data were available from 82 studies. Our meta-regression analysis, adjusted for MBI use, showed no evidence that specialty of training was associated with burnout prevalence (estimate of meta-regression β −0.005, 95% CI −0.110 to 0.099).
Geographic region
We anticipated that geographic region of study would be an important predictor of burnout prevalence. We categorized regions by continents, but due to limited studies conducted in some of these regions, we collapsed Africa, Asia, Australia, Middle East and South America into 1 category. Therefore, we conducted an analysis with region as a 3-category variable (North America, Europe and rest of the world). Data from all 114 studies were available for this analysis. Our analysis, adjusted for MBI use, found that region was a significant predictor of variation in burnout prevalence (estimate of meta-regression p < 0.001). Appendix 2 includes details of studies from each region, and Table 1 presents the results of our meta-analysis of burnout prevalence by region. As limited data were available for other regions, stronger conclusions can be made about burnout only among North American and European residents; the prevalence of burnout among European PMTs was 30.8% versus 51.2% in North America. Figure 5 illustrates burnout prevalence by region.
Table 1:
Results of meta-regression of burnout prevalence by region of source data*
| Region | No. of PMTs | No. of studies | Estimate of β coefficient (95% CI)† |
|---|---|---|---|
| Europe | 12 782 | 24 | Reference |
| Africa | 86 | 2 | 0.20 (0.10 to 0.30) |
| Asia | 914 | 8 | |
| Australia and New Zealand | 1563 | 6 | |
| Middle East and North Africa | 1250 | 10 | |
| South America | 957 | 8 | |
| North America | 14 004 | 60 | 0.18 (0.09 to 0.28) |
Note: CI = confidence interval, PMT = postgraduate medical trainee.
Meta-analyzed estimates for each region.
β coefficients were calculated using meta-regression with Europe as the reference group.
Figure 5:
Mean prevalence of burnout among postgraduate medical trainees by continent of source data. Figure is shaded by gradient of burnout prevalence.
Risk and protective factors
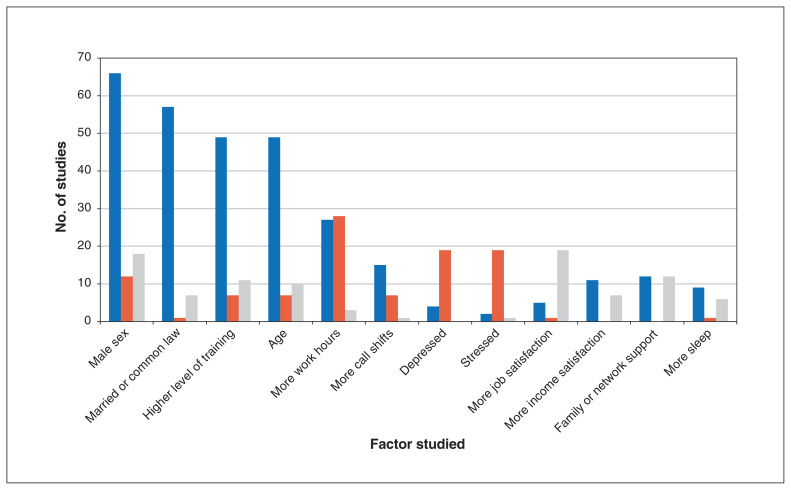
We aimed to study the following factors and their role in burnout: age, sex, relationship status, depression, level of stress, work hours, frequency of call shifts, job satisfaction, wage or income satisfaction, family or network support, sleep and level of training. However, because of heterogeneity in how these factors are studied and reported in literature, we were unable to pool results but rather present only a descriptive analysis of our findings (Figure 6). In brief, we found that most studies did not find a significant association between burnout and age, sex, relationship status and level of training. However, stress and lower job satisfaction were commonly associated with higher rates of burnout in the literature. In addition, although 28 of 58 studies investigating the association between work hours and burnout found a positive association, 27 of 58 concluded that no significant association existed. Similarly, only 7 of 23 studies found that burnout was positively and significantly associated with more call shifts.
Figure 6:
Bar graph depicting studies in the systematic review reporting a type of association between commonly studied factors and burnout among postgraduate medical trainees. Blue bars represent the number of studies finding no association between the studied factor and burnout. Orange bars represent the number of studies finding that the studied factor increased burnout. Grey bars represent the number of studies finding that the studied factor decreased burnout.
Risk-of-bias assessment
Many of the included studies had methodological flaws, limiting the reliability of their findings. Specifically, 30.6% (60/196) of studies included a consecutive or obviously representative sample of PMTs, and only 9.7% (19/196) of studies justified their sample size by using a sample size calculation. In addition, 25.5% (50/196) of studies compared respondents’ characteristics to those of nonrespondents or had a satisfactory response rate of greater than 80%. Although 98.5% (193/196) of studies used a well-described validated tool to measure burnout, this is of doubtful significance given the heterogeneity in interpreting the tool and establishing cut-off values highlighted above. A total of 44.9% (88/196) appropriately reported on descriptive statistics to describe the population with proper measures of dispersion. Lastly, 49.5% (97/196) of studies provided adequate statistics to describe burnout with proper measures of dispersion.
Interpretation
Our analyses underscore 4 key findings: the prevalence of burnout has not changed significantly over time; prevalence of burnout is associated with region; burnout rates among medical and surgical PMTs were similar; and most of the commonly studied risk and protective factors were not associated with burnout.
First, although policies over the past 2 decades have aimed to circumvent systemic causes of burnout by limiting work hours, on-call responsibilities and, more recently, instituting wellness programs, our results show that the prevalence of burnout has not significantly changed over time.133 Our results are consistent with the equivocal findings of a recent systematic review.134 Notably, our findings are likely more reflective of policy changes around work hours, rather than wellness programs, as these are more recent additions to the battle against burnout. Taken together, our findings suggest that unknown or underrecognized systemic factors are likely major contributors, and efforts should be aimed to uncover these. To this end, considerable qualitative work has focused on understanding the pitfalls of medical training, the hidden curriculum and challenges within the medical culture. Some training programs have sought to overcome the potential toxic culture by incorporating mentorship programs to promote collegiality135 and create platforms to give voice to PMTs.136 It is likely that answers lie at the intersection of further quantitative research of structural differences between geographically diverse training systems and qualitative work understanding the prevailing toxic culture of medicine and its impact on physicians and patients alike.137
Second, we report that burnout is associated with region, suggesting a role of systemic factors on PMT wellness. Among North American and European PMTs, the regions for which we had the most data available, there exists a stark difference in the prevalence of burnout. Although there is a paucity of research comparing health care systems among these regions, a study of general workplace trends finds that factors such as more involved unions and longer paid vacations, among other such social policies, contribute to overall improved work–life balance and less burnout.138 It is possible that our findings are biased by methodological considerations such as the possibility that the MBI may be filled out in a different manner across cultures, contributing to the observed variation in prevalence. Nonetheless, our findings warrant future research to identify cultural and systemic differences that may explain our results, both within and outside the training environment. The possible effect of cultural and systemic differences is supported by other recent work; a cross-sectional study reports that physicians as a group are more resilient than the general population, lending less credence to the view that individual factors lead to burnout.139 Furthermore, a systematic review by Panagioti and colleagues evaluating strategies to mitigate burnout emphasized the need for organizational level change.4
Third, our meta-regression suggests that whether a PMT is a surgical trainee or medical trainee does not significantly explain the heterogeneity in burnout prevalence. Although there may exist differences between the 2 training programs, they are likely small in comparison to other determinants of burnout. It is often hypothesized that surgical residents experience greater stress and harassment during their training, leading to high rates of burnout.132,140–142 However, our findings suggest that rates likely do not differ and support alliance of efforts, both policy and research, by medical and surgical training programs to address a crisis that affects all PMTs equally.
Lastly, with the exception of stress and depression, our descriptive analysis of the literature failed to identify any consistent relation between commonly studied risk and protective factors with burnout. For example, although commonly believed to be associated with burnout, we found that most literature does not support an association between relationship status and level of training with burnout. We also found an equivocal relation between work hours and burnout. Given the cross-sectional nature of the included studies and the likely between-study variance in how these factors are measured, it is difficult to make strong conclusions; nevertheless, our results suggest that research to date into causes of burnout has failed to yield definitive risk factors that can be mitigated or protective factors that can be enhanced to combat the increasing prevalence.
Although previous reviews have aimed to summarize rates of burnout among resident physicians, these studies have been limited by restrictive search terms; have included largely North American studies, have been quite small (e.g., the review by Rodriguez and colleagues including only 26 studies); or have focused on attending physicians, excluding trainees.2,11–13 The comprehensiveness of our data makes our results generalizable and provides a solid platform on which additional data can be added to make more robust conclusions.
Our results propose a clear direction for future research on burnout among trainees. Our study suggests that the key to mitigating burnout lies in systemic changes that may be uncovered by studying regional variation in the medical culture. Our study highlights that we do not yet have a grasp on what factors cause burnout among physicians; it is critical that we amend research efforts to gain a better understanding of burnout so that appropriate interventions can be developed to alleviate this crisis.
Limitations
There are 2 key limitations to our study. First, we included only studies published in English. This limitation is reflected in our reduced sample size from continents outside Europe and North America. Future studies should focus on translating non-English studies and searching the grey literature to gain a better understanding of burnout among all regions worldwide. Nonetheless, even with our geographically limited sample size, we observed that significant variation in burnout exists globally. This supports our view that the next steps in burnout research should focus on understanding differences between health care and education systems. To be cautious, we predominantly limit the discussion in this paper to North America and Europe.
Second, there is significant heterogeneity in the measurement of burnout, subsequently leading to pooled estimates that are less reliable and should be interpreted with caution. Notably, use of the MBI to define burnout explained some heterogeneity and we subsequently adjusted our meta-regression accordingly to ensure robustness of our findings. As previously noted, some studies used a modified version of the MBI. While the one most commonly employed — using single item measures for emotional exhaustion and depersonalization — has previously been validated and found to correlate strongly with the full version of the MBI,15,16 many of these studies used arbitrary versions that are of questionable validity. Therefore, we encourage readers to assess the results critically. The bias resulting from substantial heterogeneity is a limitation that exists in literature and highlights the need for standardized measurement of burnout. The MBI is the most commonly used and widely validated tool; we encourage its use by future researchers to facilitate further research in this field and to assess adequately temporal trends in burnout globally.
Conclusion
Despite burnout’s substantial impact, interventions appear to have had little effect on its prevalence over the last few decades. We provide a comprehensive characterization of burnout within our profession and a new direction for future research.
Supplementary Material
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Leen Naji, Zahra Sohani, Brendan Singh and Jason Profetto conceived the research question. Leen Naji, Brendan Singh, Brittany Dennis, Zahra Sohani, Zainab Samaan and Lehana Thabane designed the review protocol. Leen Naji and Laura Banfield designed the search strategy, which was completed by Laura Banfield. Leen Naji, Brendan Singh, Ajay Shah, Faysal Naji and Owen Kavanagh completed the systematic screening of studies for inclusion independently and in duplicate. Leen Naji, Brendan Singh, Ajay Shah, Faysal Naji and Owen Kavanagh performed data extraction and quality assessment of included studies independently and in duplicate. Leen Naji, Akram Alyass and Zahra Sohani performed data analyses. Fahad Razak reviewed the manuscript. All authors contributed to the writing and revision of the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. Leen Naji and Zahra Sohani accept full responsibility for the finished article, had access to any data, and controlled the decision to publish. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work. Lehana Thabane and Zahra Sohani are co-senior authors.
Funding: No funding was received for this study.
Data sharing: All extracted data are available for sharing. Data may be accessed by contacting (Zahra Sohani, zahra.sohani@mail.mcgill.ca or Leen Naji, leen.naji@medportal.ca).
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/9/1/E189/suppl/DC1.
References
- 1.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work–life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600–13. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 2.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians. JAMA. 2018;320:1131–50. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yaghmour NA, Brigham TP, Richter T, et al. Causes of death of residents in ACGME-accredited programs 2000 through 2014: implications for the learning environment. Acad Med. 2017;92:976–83. doi: 10.1097/ACM.0000000000001736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians. JAMA Intern Med. 2017;177:195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 5.Kuremyr D, Kihlgren M, Norberg A, et al. Emotional experiences, empathy and burnout among staff caring for demented patients at a collective living unit and a nursing home. J Adv Nurs. 1994;19:670–9. doi: 10.1111/j.1365-2648.1994.tb01137.x. [DOI] [PubMed] [Google Scholar]
- 6.Geelan-Hansen K, Anne S, Benninger MS. Burnout in otolaryngology — head and neck surgery: a single academic center experience. Otolaryngol Head Neck Surg. 2018;159:254–7. doi: 10.1177/0194599818774740. [DOI] [PubMed] [Google Scholar]
- 7.Govêia CS, Cruz TTMD, de Miranda DB, et al. Association between burnout syndrome and anxiety in residents and anesthesiologists of the Federal District. Rev Bras Anestesiol. 2018;68:442–6. doi: 10.1016/j.bjane.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CMA National Physician Health Survey: a national snapshot. Ottawa: Canadian Medical Association; 2018. [Google Scholar]
- 9.Zis P, Anagnostopoulos F, Sykioti P. Burnout in medical residents: a study based on the job demands-resources model. Scientific World Journal. 2014;2014 doi: 10.1155/2014/673279. 673279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agha A, Mordya A, Anwar E, et al. Burnout among middle-grade doctors of tertiary care hospital in Saudi Arabia. Work. 2015;51:839–47. doi: 10.3233/WOR-141898. [DOI] [PubMed] [Google Scholar]
- 11.Thomas NK. Resident burnout. JAMA. 2004;292:2880–9. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 12.Prins JT, Gazendam-Donofrio SM, Tubben BJ, et al. Burnout in medical residents: a review. Med Educ. 2007;41:788–800. doi: 10.1111/j.1365-2923.2007.02797.x. [DOI] [PubMed] [Google Scholar]
- 13.Rodrigues H, Cobucci R, Oliveira A, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018;13:e0206840. doi: 10.1371/journal.pone.0206840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maslach C, Jacson S, Leiter M. Maslach Burnout Inventory manual. 3rd ed. Palo Alto (CA): Consulting Psychologists Press; 1996. [Google Scholar]
- 15.West CP, Dyrbye LN, Sloan JA, et al. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24:1318–21. doi: 10.1007/s11606-009-1129-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.West CP, Dyrbye LN, Satele DV, et al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27:1445–52. doi: 10.1007/s11606-012-2015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Covidence systematic review software. Melbourne (AU): Veritas Health Innovation; [Google Scholar]
- 18.Wells G, Tugwell P, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa: The Ottawa Hospital Research Institute; 2015. [Google Scholar]
- 19.Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks (CA): Sage; 2001. p. 49. [Google Scholar]
- 20.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48. [Google Scholar]
- 21.Taris TW, Le Blanc PM, Schaufeli WB, et al. Are there causal relationships between the dimensions of the Maslach Burnout Inventory? A review and two longitudinal tests. Work Stress. 2005;19:238–55. [Google Scholar]
- 22.Blanchard P, Truchot D, Albiges-Sauvin L, et al. Prevalence and causes of burnout amongst oncology residents: a comprehensive nationwide cross-sectional study. Eur J Cancer. 2010;46:2708–15. doi: 10.1016/j.ejca.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 23.Abdulrahman M, Farooq MM, Al Kharmiri A, et al. Burnout and depression among medical residents in the United Arab Emirates: a multicenter study. J Family Med Prim Care. 2018;7:435–41. doi: 10.4103/jfmpc.jfmpc_199_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aksoy DY, Durusu Tanriover M, Dizdar O, et al. Burnout syndrome during residency in internal medicine and pediatrics in a country without working time directive. Int J Health Care Qual Assur. 2014;27:223–30. doi: 10.1108/IJHCQA-12-2012-0127. [DOI] [PubMed] [Google Scholar]
- 25.Al-Ma’mari NO, Naimi AI, Tulandi T. Prevalence and predictors of burnout among obstetrics and gynecology residents in Canada. Gynecol Surg. 2016;13:323–7. [Google Scholar]
- 26.Aldrees TM, Aleissa S, Zamakhshary M, et al. Physician well-being: prevalence of burnout and associated risk factors in a tertiary hospital, Riyadh, Saudi Arabia. Ann Saudi Med. 2013;33:451–6. doi: 10.5144/0256-4947.2013.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aldrees T, Badri M, Islam T, et al. Burnout among otolaryngology residents in Saudi Arabia: a multicenter study. J Surg Educ. 2015;72:844–8. doi: 10.1016/j.jsurg.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 28.Aldrees T, Hassouneh B, Alabdulkarim A, et al. Burnout among plastic surgery residents: National survey in Saudi Arabia. Saudi Med J. 2017;38:832–6. doi: 10.15537/smj.2017.8.18346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arora M, Diwan AD, Harris IA. Prevalence and factors of burnout among Australian orthopaedic trainees: a cross-sectional study. J Orthop Surg (Hong Kong) 2014;22:374–7. doi: 10.1177/230949901402200322. [DOI] [PubMed] [Google Scholar]
- 30.Ashkar K, Romani M, Musharrafieh U, et al. Prevalence of burnout syndrome among medical residents: experience of a developing country. Postgrad Med J. 2010;86:266–71. doi: 10.1136/pgmj.2009.092106. [DOI] [PubMed] [Google Scholar]
- 31.Attenello FJ, Buchanan IA, Wen T, et al. Factors associated with burnout among US neurosurgery residents: a nationwide survey. J Neurosurg. 2018;129:1349–63. doi: 10.3171/2017.9.JNS17996. [DOI] [PubMed] [Google Scholar]
- 32.Becker JL, Milad MP, Klock SC. Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol. 2006;195:1444–9. doi: 10.1016/j.ajog.2006.06.075. [DOI] [PubMed] [Google Scholar]
- 33.Billings ME, Lazarus ME, Wenrich M, et al. The effect of the hidden curriculum on resident burnout and cynicism. J Grad Med Educ. 2011;3:503–10. doi: 10.4300/JGME-D-11-00044.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bogg J, Gibbs T, Bundred P. Training, job demands and mental health of pre-registration house officers. Med Educ. 2001;35:590–5. doi: 10.1046/j.1365-2923.2001.00951.x. [DOI] [PubMed] [Google Scholar]
- 35.Braun SE, Auerbach SM, Rybarczyk B, et al. Mindfulness, burnout, and effects on performance evaluations in internal medicine residents. Adv Med Educ Pract. 2017;8:591–7. doi: 10.2147/AMEP.S140554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Campbell J, Prochazka AV, Yamashita T, et al. Predictors of persistent burnout in internal medicine residents: a prospective cohort study. Acad Med. 2010;85:1630–4. doi: 10.1097/ACM.0b013e3181f0c4e7. [DOI] [PubMed] [Google Scholar]
- 37.Castelo-Branco C, Figueras F, Eixarch E, et al. Stress symptoms and burnout in obstetric and gynaecology residents. BJOG. 2007;114:94–8. doi: 10.1111/j.1471-0528.2006.01155.x. [DOI] [PubMed] [Google Scholar]
- 38.Chaput B, Bertheuil N, Jacques J, et al. Professional burnout among plastic surgery residents: Can it be prevented? Outcomes of a national survey. Ann Plast Surg. 2015;75:2–8. doi: 10.1097/SAP.0000000000000530. [DOI] [PubMed] [Google Scholar]
- 39.Chati R, Huet E, Grimberg L, et al. Factors associated with burnout among French digestive surgeons in training: results of a national survey on 328 residents and fellows. Am J Surg. 2017;213:754–62. doi: 10.1016/j.amjsurg.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 40.Chaukos D, Chad-Friedman E, Mehta DH, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41:189–94. doi: 10.1007/s40596-016-0628-6. [DOI] [PubMed] [Google Scholar]
- 41.Cofer KD, Hollis RH, Goss L, et al. Burnout is associated with emotional intelligence but not traditional job performance measurements in surgical residents. J Surg Educ. 2018;75:1171–9. doi: 10.1016/j.jsurg.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 42.Cubero DIG, Fumis RRL, de Sa TH, et al. Burnout in medical oncology fellows: a prospective multicenter cohort study in Brazilian institutions. J Cancer Educ. 2016;31:582–7. doi: 10.1007/s13187-015-0850-z. [DOI] [PubMed] [Google Scholar]
- 43.de Andrade APM, Amaro E, Farhat SCL, et al. Higher burnout scores in paediatric residents are associated with increased brain activity during attentional functional magnetic resonance imaging task. Acta Paediatr. 2016;105:705–13. doi: 10.1111/apa.13371. [DOI] [PubMed] [Google Scholar]
- 44.Dominguez LC, Stassen L, de Grave W, et al. Taking control: Is job crafting related to the intention to leave surgical training? PLoS One. 2018;13:e0197276. doi: 10.1371/journal.pone.0197276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dyrbye LN, West CP, Satele D, et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. 2014;89:443–51. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 46.Embriaco N, Azoulay E, Barrau K, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175:686–92. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- 47.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488–91. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Galam E, Komly V, Le Tourneur A, et al. Burnout among French GPs in training: a cross-sectional study. Br J Gen Pract. 2013;63:e217–24. doi: 10.3399/bjgp13X664270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garza JA, Schneider KM, Promecene P, et al. Burnout in residency: statewide study. South Med J. 2004;97:1171–3. doi: 10.1097/01.SMJ.0000129926.66568.10. [DOI] [PubMed] [Google Scholar]
- 50.Goitein L, Shanafelt TD, Wipf JE, et al. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005;165:2601–6. doi: 10.1001/archinte.165.22.2601. [DOI] [PubMed] [Google Scholar]
- 51.Golub JS, Weiss PS, Ramesh AK, et al. Burnout in residents of otolaryngology-head and neck surgery: a national inquiry into the health of residency training. Acad Med. 2007;82:596–601. doi: 10.1097/ACM.0b013e3180556825. [DOI] [PubMed] [Google Scholar]
- 52.Gopal R, Glasheen JJ, Miyoshi TJ, et al. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005;165:2595–600. doi: 10.1001/archinte.165.22.2595. [DOI] [PubMed] [Google Scholar]
- 53.Gopal RK, Carreira F, Baker WA, et al. Internal medicine residents reject “longer and gentler” training. J Gen Intern Med. 2007;22:102–6. doi: 10.1007/s11606-007-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gouveia PAdC, Ribeiro Neta MHC, Aschoff CA, et al. Factors associated with burnout syndrome in medical residents of a university hospital. Rev Assoc Med Bras. 2017;63:504–11. doi: 10.1590/1806-9282.63.06.504. [DOI] [PubMed] [Google Scholar]
- 55.Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med. 2012;76:389–95. [PubMed] [Google Scholar]
- 56.Hameed TK, Masuadi E, Al Asmary NA, et al. A study of resident duty hours and burnout in a sample of Saudi residents. BMC Med Educ. 2018;18:180. doi: 10.1186/s12909-018-1300-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hill JD, Smith RJH. Monitoring stress levels in postgraduate medical training. Laryngoscope. 2009;119:75–8. doi: 10.1002/lary.20013. [DOI] [PubMed] [Google Scholar]
- 58.Holmes EG, Connolly A, Putnam KT, et al. Taking care of our own: a multi-specialty study of resident and program director perspectives on contributors to burnout and potential interventions. Acad Psychiatry. 2017;41:159–66. doi: 10.1007/s40596-016-0590-3. [DOI] [PubMed] [Google Scholar]
- 59.Jamjoom RS, Park YS. Assessment of pediatric residents’ burnout in a tertiary academic centre. Saudi Med J. 2018;39:296–300. doi: 10.15537/smj.2018.3.22328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Joaquim A, Custodio S, Savva-Bordalo J, et al. Burnout and occupational stress in the medical residents of oncology, haematology and radiotherapy: a prevalence and predictors study in Portugal. Psychol Health Med. 2018;23:317–24. doi: 10.1080/13548506.2017.1344256. [DOI] [PubMed] [Google Scholar]
- 61.Krug MF, Golob AL, Wander PL, et al. Changes in resident well-being at one institution across a decade of progressive work hours limitations. Acad Med. 2017;92:1480–4. doi: 10.1097/ACM.0000000000001675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kwah J, Weintraub J, Fallar R, et al. The effect of burnout on medical errors and professionalism in first-year internal medicine residents. J Grad Med Educ. 2016;8:597–600. doi: 10.4300/JGME-D-15-00457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Landrigan CP, Fahrenkopf AM, Lewin D, et al. Effects of the Accreditation Council for Graduate Medical Education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122:250–8. doi: 10.1542/peds.2007-2306. [DOI] [PubMed] [Google Scholar]
- 64.Lee PT, Loh J, Sng G, et al. Empathy and burnout: a study on residents from a Singapore institution. Singapore Med J. 2018;59:50–4. doi: 10.11622/smedj.2017096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leung J, Rioseco P. Burnout, stress and satisfaction among Australian and New Zealand radiation oncology trainees. J Med Imaging Radiat Oncol. 2017;61:146–55. doi: 10.1111/1754-9485.12541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Levin KH, Shanafelt TD, Keran CM, et al. Burnout, career satisfaction, and well-being among US neurology residents and fellows in 2016. Neurology. 2017;89:492–501. doi: 10.1212/WNL.0000000000004135. [DOI] [PubMed] [Google Scholar]
- 67.Lin DT, Liebert CA, Tran J, et al. Emotional intelligence as a predictor of resident well-being. J Am Coll Surg. 2016;223:352–8. doi: 10.1016/j.jamcollsurg.2016.04.044. [DOI] [PubMed] [Google Scholar]
- 68.Lindeman BM, Sacks BC, Hirose K, et al. Multifaceted longitudinal study of surgical resident education, quality of life, and patient care before and after July 2011. J Surg Educ. 2013;70:769–76. doi: 10.1016/j.jsurg.2013.06.018. [DOI] [PubMed] [Google Scholar]
- 69.Lindeman B, Petrusa E, McKinley S, et al. Association of burnout with emotional intelligence and personality in surgical residents: Can we predict who is most at risk? J Surg Educ. 2017;74:e22–30. doi: 10.1016/j.jsurg.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 70.Llera J, Durante E. Correlation between the educational environment and burn-out syndrome in residency programs at a university hospital. Arch Argent Pediatr. 2014;112:6–11. doi: 10.5546/aap.2014.eng.6. [DOI] [PubMed] [Google Scholar]
- 71.Malik AA, Bhatti S, Shafiq A, et al. Burnout among surgical residents in a lower-middle income country — Are we any different? Ann Med Surg (Lond) 2016;9:28–32. doi: 10.1016/j.amsu.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Martini S, Arfken CL, Churchill A, et al. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004;28:240–2. doi: 10.1176/appi.ap.28.3.240. [DOI] [PubMed] [Google Scholar]
- 73.Martini S, Arfken CL, Balon R. Comparison of burnout among medical residents before and after the implementation of work hours limits. Acad Psychiatry. 2006;30:352–5. doi: 10.1176/appi.ap.30.4.352. [DOI] [PubMed] [Google Scholar]
- 74.Mohammed KA-M, Ali EG, Youssef IM, et al. Depression and burnout among residents. Arab J Psychiatry. 2014;25:40–51. [Google Scholar]
- 75.Msaouel P, Keramaris NC, Tasoulis A, et al. Burnout and training satisfaction of medical residents in Greece: Will the European Work Time Directive make a difference? Hum Resour Health. 2010;8:16. doi: 10.1186/1478-4491-8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nolan KJ, Writer H, Ladhani M. Wellness in Canadian paediatric residents and their program directors. Paediatr Child Health. 2017;22:199–202. doi: 10.1093/pch/pxx050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.O’Connor P, Lydon S, O’Dea A, et al. A longitudinal and multicentre study of burnout and error in irish junior doctors. Postgrad Med J. 2017;93:660–4. doi: 10.1136/postgradmedj-2016-134626. [DOI] [PubMed] [Google Scholar]
- 78.Olson SM, Odo NU, Duran AM, et al. Burnout and physical activity in minnesota internal medicine resident physicians. J Grad Med Educ. 2014;6:669–74. doi: 10.4300/JGME-D-13-00396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Olson K, Kemper KJ, Mahan JD. What factors promote resilience and protect against burnout in first-year pediatric and medicine-pediatric residents? J Evid Based Complementary Altern Med. 2015;20:192–8. doi: 10.1177/2156587214568894. [DOI] [PubMed] [Google Scholar]
- 80.Pantaleoni JL, Augustine EM, Sourkes BM, et al. Burnout in pediatric residents over a 2-year period: a longitudinal study. Acad Pediatr. 2014;14:167–72. doi: 10.1016/j.acap.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 81.Ramey SJ, Ahmed AA, Takita C, et al. Burnout evaluation of radiation residents nationwide: results of a survey of United States residents. Int J Radiat Oncol Biol Phys. 2017;99:530–8. doi: 10.1016/j.ijrobp.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 82.Ripp J, Fallar R, Babyatsky M, et al. Prevalence of resident burnout at the start of training. Teach Learn Med. 2010;22:172–5. doi: 10.1080/10401334.2010.488194. [DOI] [PubMed] [Google Scholar]
- 83.Ripp J, Babyatsky M, Fallar R, et al. The incidence and predictors of job burnout in first-year internal medicine residents: a five-institution study. Acad Med. 2011;86:1304–10. doi: 10.1097/ACM.0b013e31822c1236. [DOI] [PubMed] [Google Scholar]
- 84.Ripp JA, Bellini L, Fallar R, et al. The impact of duty hours restrictions on job burnout in internal medicine residents: a three-institution comparison study. Acad Med. 2015;90:494–9. doi: 10.1097/ACM.0000000000000641. [DOI] [PubMed] [Google Scholar]
- 85.Rosen IM, Gimotty PA, Shea JA, et al. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81:82–5. doi: 10.1097/00001888-200601000-00020. [DOI] [PubMed] [Google Scholar]
- 86.Sajjadi S, Norena M, Wong H, et al. Moral distress and burnout in internal medicine residents. Can Med Educ J. 2017;8:e36–43. [PMC free article] [PubMed] [Google Scholar]
- 87.Sargent MC, Sotile W, Sotile MO, et al. Quality of life during orthopaedic training and academic practice. Part 1: Orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2009;91:2395–405. doi: 10.2106/JBJS.H.00665. [DOI] [PubMed] [Google Scholar]
- 88.Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–67. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 89.Siu C, Yuen SK, Cheung A. Burnout among public doctors in Hong Kong: cross-sectional survey. Hong Kong Med J. 2012;18:186–92. [PubMed] [Google Scholar]
- 90.Spataro BM, Tilstra SA, Rubio DM, et al. The toxicity of self-blame: sex differences in burnout and coping in internal medicine trainees. J Womens Health (Larchmt) 2016;25:1147–52. doi: 10.1089/jwh.2015.5604. [DOI] [PubMed] [Google Scholar]
- 91.Sulaiman CFC, Henn P, Smith S, et al. Burnout syndrome among non-consultant hospital doctors in Ireland: relationship with self-reported patient care. Int J Qual Health Care. 2017;29:679–84. doi: 10.1093/intqhc/mzx087. [DOI] [PubMed] [Google Scholar]
- 92.Toral-Villanueva R, Aguilar-Madrid G, Juarez-Perez CA. Burnout and patient care in junior doctors in Mexico City. Occup Med (Lond) 2009;59:8–13. doi: 10.1093/occmed/kqn122. [DOI] [PubMed] [Google Scholar]
- 93.Waldman SV, Lopez Diez JC, Arazi HC, et al. Burnout, perceived stress, and depression among cardiology residents in Argentina. Acad Psychiatry. 2009;33:296–301. doi: 10.1176/appi.ap.33.4.296. [DOI] [PubMed] [Google Scholar]
- 94.Willcock SM, Daly MG, Tennant CC, et al. Burnout and psychiatric morbidity in new medical graduates. Med J Aust. 2004;181:357–60. doi: 10.5694/j.1326-5377.2004.tb06325.x. [DOI] [PubMed] [Google Scholar]
- 95.Williford ML, Scarlet S, Meyers MO, et al. Multiple-institution comparison of resident and faculty perceptions of burnout and depression during surgical training. JAMA Surg. 2018;153:705–11. doi: 10.1001/jamasurg.2018.0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zis P, Artemiadis AK, Lykouri M, et al. Residency training: determinants of burnout of neurology trainees in Attica, Greece. Neurology. 2015;85:e81–4. doi: 10.1212/WNL.0000000000001924. [DOI] [PubMed] [Google Scholar]
- 97.Talih F, Warakian R, Ajaltouni J, et al. Correlates of depression and burnout among residents in a Lebanese academic medical center: a cross-sectional study. Acad Psychiatry. 2016;40:38–45. doi: 10.1007/s40596-015-0400-3. [DOI] [PubMed] [Google Scholar]
- 98.Pereira-Lima K, Loureiro SR. Burnout, anxiety, depression, and social skills in medical residents. Psychol Health Med. 2015;20:353–62. doi: 10.1080/13548506.2014.936889. [DOI] [PubMed] [Google Scholar]
- 99.See KC, Lim TK, Kua EH, et al. Stress and burnout among physicians: prevalence and risk factors in a Singaporean internal medicine programme. Ann Acad Med Singapore. 2016;45:471–4. [PubMed] [Google Scholar]
- 100.Jovanovic N, Podlesek A, Volpe U, et al. Burnout syndrome among psychiatric trainees in 22 countries: Risk increased by long working hours, lack of supervision, and psychiatry not being first career choice. Eur Psychiatry. 2016;32:34–41. doi: 10.1016/j.eurpsy.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 101.Miyoshi R, Matsuo H, Takeda R, et al. Burnout in Japanese residents and its associations with temperament and character. Asian J Psychiatr. 2016;24:5–9. doi: 10.1016/j.ajp.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 102.Torppa MA, Kuikka L, Nevalainen M, et al. Emotionally exhausting factors in general practitioners’ work. Scand J Prim Health Care. 2015;33:178–83. doi: 10.3109/02813432.2015.1067514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.de Oliveira GS, Jr, Chang R, Fitzgerald PC, et al. The prevalence of burnout and depression and their association with adherence to safety and practice standards: a survey of united states anesthesiology trainees. Anesth Analg. 2013;117:182–93. doi: 10.1213/ANE.0b013e3182917da9. [DOI] [PubMed] [Google Scholar]
- 104.Ruitenburg MM, Frings-Dresen MH, Sluiter JK. The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: a cross-sectional study. BMC Health Serv Res. 2012;12:292. doi: 10.1186/1472-6963-12-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ringrose R, Houterman S, Koops W, et al. Burnout in medical residents: a questionnaire and interview study. Psychol Health Med. 2009;14:476–86. doi: 10.1080/13548500903012822. [DOI] [PubMed] [Google Scholar]
- 106.McNeeley MF, Perez FA, Chew FS. The emotional wellness of radiology trainees: prevalence and predictors of burnout. Acad Radiol. 2013;20:647–55. doi: 10.1016/j.acra.2012.12.018. [DOI] [PubMed] [Google Scholar]
- 107.Porrino J, Mulcahy MJ, Mulcahy H, et al. Emotional wellness of current musculoskeletal radiology fellows. Acad Radiol. 2017;24:682–93. doi: 10.1016/j.acra.2016.12.024. [DOI] [PubMed] [Google Scholar]
- 108.Baer TE, Feraco AM, Tuysuzoglu Sagalowsky S, et al. Pediatric resident burnout and attitudes toward patients. Pediatrics. 2017;139:e20162163. doi: 10.1542/peds.2016-2163. [DOI] [PubMed] [Google Scholar]
- 109.Mordant P, Deneuve S, Rivera C, et al. Quality of life of surgical oncology residents and fellows across Europe. J Surg Educ. 2014;71:222–8. doi: 10.1016/j.jsurg.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 110.Shanafelt TD, Raymond M, Horn L, et al. Oncology fellows’ career plans, expectations, and well-being: Do fellows know what they are getting into? J Clin Oncol. 2014;32:2991–7. doi: 10.1200/JCO.2014.56.2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Simpkin AL, Khan A, West DC, et al. Stress from uncertainty and resilience among depressed and burned out residents: a cross-sectional study. Acad Pediatr. 2018;18:698–704. doi: 10.1016/j.acap.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 112.Trockel M, Bohman B, Lesure E, et al. A brief instrument to assess both burnout and professional fulfillment in physicians: reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Acad Psychiatry. 2018;42:11–24. doi: 10.1007/s40596-017-0849-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.van Vendeloo SN, Brand PLP, Verheyen CCPM. Burnout and quality of life among orthopaedic trainees in a modern educational programme: importance of the learning climate. Bone Joint J. 2014;96-B:1133–8. doi: 10.1302/0301-620X.96B8.33609. [DOI] [PubMed] [Google Scholar]
- 114.Prins JT, Hoekstra-Weebers J, van de Wiel HBM, et al. Burnout among Dutch medical residents. Int J Behav Med. 2007;14:119–25. doi: 10.1007/BF03000182. [DOI] [PubMed] [Google Scholar]
- 115.Prins JT, Hoekstra-Weebers JEHM, Gazendam-Donofrio SM, et al. Burnout and engagement among resident doctors in the Netherlands: a national study. Med Educ. 2010;44:236–47. doi: 10.1111/j.1365-2923.2009.03590.x. [DOI] [PubMed] [Google Scholar]
- 116.van der Wal RAB, Bucx MJL, Hendriks JCM, et al. Psychological distress, burnout and personality traits in Dutch anaesthesiologists: a survey. Eur J Anaesthesiol. 2016;33:179–86. doi: 10.1097/EJA.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 117.van Vendeloo SN, Prins DJ, Verheyen C, et al. The learning environment and resident burnout: a national study. Perspect Med Educ. 2018;7:120–5. doi: 10.1007/s40037-018-0405-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.van Vendeloo SN, Godderis L, Brand PLP, et al. Resident burnout: evaluating the role of the learning environment. BMC Med Educ. 2018;18:54. doi: 10.1186/s12909-018-1166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Block L, Wu AW, Feldman L, et al. Residency schedule, burnout and patient care among first-year residents. Postgrad Med J. 2013;89:495–500. doi: 10.1136/postgradmedj-2012-131743. [DOI] [PubMed] [Google Scholar]
- 120.Lebares CC, Guvva EV, Ascher NL, et al. Burnout and stress among US surgery residents: psychological distress and resilience. J Am Coll Surg. 2018;226:80–90. doi: 10.1016/j.jamcollsurg.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 121.Shakir HJ, McPheeters MJ, Shallwani H, et al. The prevalence of burnout among US neurosurgery residents. Neurosurgery. 2018;83:582–90. doi: 10.1093/neuros/nyx494. [DOI] [PubMed] [Google Scholar]
- 122.Huggard P, Dixon R. “Tired of caring”: the impact of caring on resident doctors. Australas J Disaster Trauma Stud. 2011;2011:105–11. [Google Scholar]
- 123.Low JM, Tan MY, See KC, et al. Sleep, activity and fatigue reported by postgraduate year 1 residents: a prospective cohort study comparing the effects of night-float versus traditional overnight on-call. Singapore Med J. 2018;59:652–5. doi: 10.11622/smedj.2018036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Markwell AL, Wainer Z. The health and wellbeing of junior doctors: insights from a national survey. Med J Aust. 2009;191:441–4. doi: 10.5694/j.1326-5377.2009.tb02880.x. [DOI] [PubMed] [Google Scholar]
- 125.Cooke GP, Doust JA, Steele MC. A survey of resilience, burnout, and tolerance of uncertainty in Australian general practice registrars. BMC Med Educ. 2013;13:2. doi: 10.1186/1472-6920-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kealy D, Halli P, Ogrodniczuk JS, et al. Burnout among Canadian psychiatry residents: a national survey. Can J Psychiatry. 2016;61:732–6. doi: 10.1177/0706743716645286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lambden JP, Chamberlin P, Kozlov E, et al. Association of perceived futile or potentially inappropriate care with burnout and thoughts of quitting among health-care providers. Am J Hosp Palliat Care. 2019;36:200–6. doi: 10.1177/1049909118792517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Leach PK, Nygaard RM, Chipman JG, et al. Impostor phenomenon and burnout in general surgeons and general surgery residents. J Surg Educ. 2019;76:99–106. doi: 10.1016/j.jsurg.2018.06.025. [DOI] [PubMed] [Google Scholar]
- 129.Raviola G, Machoki M, Mwaikambo E, et al. HIV, disease plague, demoralization and “burnout”: resident experience of the medical profession in Nairobi, Kenya. Cult Med Psychiatry. 2002;26:55–86. doi: 10.1023/a:1015289132151. [DOI] [PubMed] [Google Scholar]
- 130.Robertson SL, Robinson MD, Reid A. Electronic health record effects on work-life balance and burnout within the I3 population collaborative. J Grad Med Educ. 2017;9:479–84. doi: 10.4300/JGME-D-16-00123.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Schweitzer B. Stress and burnout in junior doctors. S Afr Med J. 1994;84:352–4. [PubMed] [Google Scholar]
- 132.Elmore LC, Jeffe DB, Jin L, et al. National survey of burnout among US general surgery residents. J Am Coll Surg. 2016;223:440–51. doi: 10.1016/j.jamcollsurg.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Temple J. Resident duty hours around the globe: Where are we now? BMC Med Educ. 2014;14(Suppl 1):S8. doi: 10.1186/1472-6920-14-S1-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Busireddy KR, Miller JA, Ellison K, et al. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ. 2017;9:294–301. doi: 10.4300/JGME-D-16-00372.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Butcher L. Stanford program takes 3-pronged approach to burnout. Neurol Today. 2019;19:30–1. [Google Scholar]
- 136.Post MD education annual report. Toronto: University of Toronto; 2016. [accessed 2020 July 9]. Voice of the resident — PGME annual report 2016. Available: https://annualreport.postmd.ca/pgme-2016/voice-of-the-resident/ [Google Scholar]
- 137.Montgomery A. The inevitability of physician burnout: implications for interventions. Burn Res. 2014;1:50–6. [Google Scholar]
- 138.Alesina A, Glaeser E, Sacerdote B. Work and leisure in the US and Europe: Why so different? Cambridge (MA): 2005. [Google Scholar]
- 139.West CP, Dyrbye LN, Sinsky C, et al. Resilience and burnout among physicians and the general US working population. JAMA Netw Open. 2020;3:e209385. doi: 10.1001/jamanetworkopen.2020.9385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hu Y-Y, Ellis RJ, Hewitt DB, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381:1741–52. doi: 10.1056/NEJMsa1903759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons. Arch Surg. 2009;144:371–6. doi: 10.1001/archsurg.2008.575. [DOI] [PubMed] [Google Scholar]
- 142.Rodrigues H, Cobucci R, Oliveira A, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018;13:e0206840. doi: 10.1371/journal.pone.0206840. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.