Abstract
Cognitive status has been reported to affect the peri-operative and post-operative outcomes of certain surgical procedures. This prospective study investigated the effect of preoperative cognitive impairment on the postoperative course of elderly patients (n = 122, >65 years), following spine surgery for degenerative spinal disease. Data on demographic characteristics, medical history, and blood analysis results were collected. Preoperative cognition was assessed using the mini-mental state examination, and patients were divided into three groups: normal cognition, mild cognitive impairment, and moderate-to-severe cognitive impairment. Discharge destinations (p = 0.014) and postoperative cardiopulmonary complications (p = 0.037) significantly differed based on the cognitive status. Operation time (p = 0.049), white blood cell count (p = 0.022), platelet count (p = 0.013), the mini-mental state examination score (p = 0.033), and the Beck Depression Inventory score (p = 0.041) were significantly associated with the length of hospital stay. Our investigation demonstrated that improved understanding of preoperative cognitive status may be helpful in surgical decision-making and postoperative care of elderly patients with degenerative spinal disease.
Keywords: cognitive status, degenerative spinal disease, geriatrics, MMSE
1. Introduction
Cognitive status is one of the most important perioperative risk factors related to clinical outcomes in geriatric patients [1,2]. The elderly population has recently been increasing due to extended life expectancy, leading to an increase in the number of patients with degenerative spinal diseases and, thus, the number of spine surgeries. Therefore, spine surgeons are managing an increasing number of elderly people with spinal disorders and aging of the spine [3,4,5,6]. Moreover, these patients usually have an increased number of comorbidities, severe spinal degeneration, and reduced bone mineral density [7]. Furthermore, impaired cognitive status is common in elderly patients.
Previous studies have shown that cognitive impairment within the surgical population is associated with prolonged hospital stays, increased postoperative complications, and higher total medical cost [1,8]. However, preoperative cognitive status has been reported as one of the positive predictors of better outcomes after lumbar discectomy [9]. In addition, some authors have reported that cognitive-behavioral factors play an important role in postsurgical outcomes [10]. However, the effect of preoperative cognitive impairment on outcomes in elderly patients undergoing spine surgery for degenerative spinal disease has not yet been reported. Furthermore, the lack of accurate knowledge on the impact of preoperative cognitive status on the course of patients undergoing spine surgery restricts surgeons from planning adequate therapeutic strategies and providing appropriate postoperative care. Therefore, the aim of this study was to investigate the relationship between preoperative cognitive status and postoperative clinical outcomes in geriatric patients undergoing surgery for degenerative lumbar disease.
2. Materials and Methods
2.1. Patient Enrollment
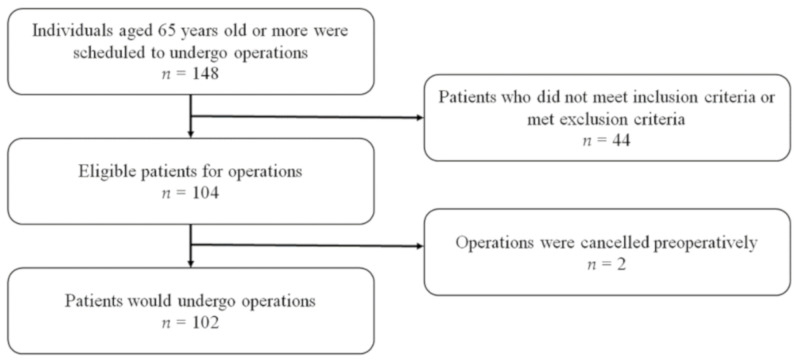
Patients older than 65 years who underwent spine surgery for degenerative lumbar conditions between October 2015 and July 2016 at a single institution were enrolled in this study (Figure 1). The investigative protocol was approved by our hospital’s Institutional Review Board (NCT 02550626), and informed consent was obtained from all patients.
Figure 1.
Participant enrollment. Exclusion from the study was based on the following criteria: (I) patients did not meet inclusion criteria (n = 44); (II) surgeries were cancelled before operations (n = 2).
Among the 148 patients who underwent lumbar surgeries, we selected and prospectively studied 102 patients (68.9%) who met the inclusion criteria. Of these, 44 patients did not meet the inclusion criteria, and surgery was postponed for two patients. The inclusion criteria included the following: (I) patients aged ≥ 65 years who were scheduled to undergo spine surgeries, including discectomy, laminectomy, and fusion; (II) hospital stay of more than 3 days; and (III) indication for surgery including herniated nucleus pulposus, degenerative disc disease, spondylolisthesis, and spinal stenosis. We excluded patients with conditions that could affect general health such as spinal tumor-like lesions, infection, or trauma. Patients with known brain conditions, including cerebral contusions and Alzheimer’s disease, all of which can cause disorientation, were also excluded.
2.2. Perioperative Patient Assessment
Cognitive status of patients was evaluated using the Korean version of the mini-mental state examination (K-MMSE) [11]. The MMSE is one of the most widely used screening tests in clinical trials and in general practice for the detection of cognitive impairment in older adults [12]. In addition, it is easy to implement and has good test-retest reliability (0.80–0.95) [12,13,14]. The K-MMSE tests five cognitive functional areas: orientation, registration, attention-calculation, recall, and language. The maximum score is 30, with higher scores indicating better cognition. The patients were divided into three groups according to the K-MMSE score. Mild cognitive impairment (MCI) was defined as an MMSE score between 21 and 26 points, while moderate-to-severe cognitive impairment (MSCI) was defined as an MMSE score of ≤20 points. Normal cognition (NC) was defined as an MMSE score of ≥27 points. Baseline examinations were performed preoperatively to assess the postoperative clinical prognosis. These examinations were performed by two independent, trained research assistants who did not participate in the surgical care of the patients to reduce potential subjective bias. Patients were not evaluated on the day of surgery because of the potential confounding influence of intraoperative anesthetic medications.
Patient characteristics, MMSE scores, comorbidities, number of medications, and preoperative laboratory findings were examined to identify potential associations with preoperative cognitive status. Patient education level was assessed, and non-educated patients were assigned a score of 0; other patients were assigned points according to each additional year of education. We estimated patient degree of depression using the Beck Depression Inventory (BDI) [15], one of the most widely used psychometric tests for measuring the severity of depression. This inventory comprises a 0 to 63 rating system, and the higher the score, the higher the severity of depression. We also collected data about clinical outcomes related to postoperative prognosis. The data included the following: intraoperative estimated blood loss (EBL), admission to intensive care unit (ICU) after surgery, re-admission and revision, and presence of postoperative delirium. These factors were examined for identifying potential associations with preoperative cognitive status.
2.3. Statistical Analysis
Statistical analysis was performed with SPSS version 19 for Windows (IBM, Armonk, NY, USA). Data are presented as the mean ± standard deviation (SD). A Student’s t test, χ2 test, univariate linear regression analysis, and multivariate linear regression analysis with an enter method were used for statistical analysis. All variables with a significance level of p < 0.05 in the univariate analysis were included as independent variables in a forward stepwise regression method in the multivariate analysis. A value of p < 0.05 was considered statistically significant.
3. Results
3.1. Patient Data
Following study recruitment criteria, 102 patients who underwent spine surgeries for degenerative disease were enrolled in this study. The baseline characteristics of these 102 patients are presented in Table 1. At enrollment, 54 (52.9%) patients showed NC, 43 (42.2%) showed MCI, and five (4.9%) showed MSCI. There were no significant differences between the three groups in terms of demographic data, medical history, surgical method, or preoperative laboratory findings.
Table 1.
Baseline characteristics.
| Characteristic | 0 < MMSE < 20 | 21 ≤ MMSE ≤ 26 | MMSE ≥ 27 | p-Value |
|---|---|---|---|---|
| Demographic data | ||||
| Number of patients | 5 | 43 | 54 | - |
| Age (years) | 73.6 ± 3.3 | 72.3 ± 4.7 | 70.9 ± 4.7 | 0.323 |
| Sex; male, n (%) | 0 | 13 | 21 | 0.083 |
| Graduate | 1.20 ± 2.68 | 6.40 ± 4.22 | 9.83 ± 4.07 | 0.424 |
| Medical history | ||||
| Height (cm) | 152.6 ± 2.8 | 156.1 ± 8.1 | 159.4 ± 8.6 | 0.083 |
| Weight (kg) | 53.6 ± 12.0 | 60.2 ± 7.5 | 62.2 ± 9.4 | 0.208 |
| BMI (kg/m2) | 22.9 ± 4.4 | 24.8 ± 2.8 | 24.4 ± 2.8 | 0.332 |
| Number of medications | 5.8 ± 2.8 | 5.5 ± 3.3 | 4.8 ± 3.1 | 0.866 |
| HTN | 4 (80%) | 28 (65.1%) | 35 (64.8%) | 0.787 |
| DM | 0 (0%) | 12 (27.9%) | 11 (20.4%) | 0.315 |
| Cardiovascular disease | 1 (20.0%) | 9 (20.9%) | 13 (24.1%) | 0.925 |
| Cerebrovascular disease | 0 (0%) | 6 (14.0%) | 2 (3.7%) | 0.140 |
| Parkinson’s disease | 1 (20.0%) | 4 (9.3%) | 8 (14.8%) | 0.637 |
| NP related disease | 1 (20.0%) | 3 (7.0%) | 9 (16.7%) | 0.321 |
| BDI score | 9.40 ± 4.83 | 14.58 ± 8.06 | 14.32 ± 8.68 | 0.329 |
| Surgical method | ||||
| Spinal fusion, n | 2 | 29 | 34 | 0.489 |
| Decompression, n | 3 | 14 | 20 | |
| Laboratory findings | ||||
| Hemoglobin | 13.2 ± 1.7 | 13.3 ± 1.3 | 13.8 ± 1.4 | 0.931 |
| WBC | 6.77 k ± 0.71 k | 7.28 k ± 1.64 k | 6.84 k ± 1.80 k | 0.111 |
| PLT | 212.6 k ± 33.2 k | 233.3 k ± 50.3 k | 233.7 k ± 64.8 k | 0.091 |
| BUN | 17.0 ± 2.9 | 17.1 ± 6.2 | 16.7 ± 4.1 | 0.064 |
| Creatinine | 0.65 ± 0.11 | 0.78 ± 0.22 | 0.78 ± 0.19 | 0.160 |
| Albumin | 3.9 ± 0.3 | 4.1 ± 0.3 | 4.2 ± 0.35 | 0.764 |
Abbreviations: BMI, body mass index; HTN, hypertension; DM, diabetes mellitus; NP, neuropsychiatric; BDI, Beck Depression Inventory; WBC, white blood cell; PLT, platelet; BUN, blood urea nitrogen.
3.2. Outcome Data
The three study groups based on cognitive function (NC, MCI, and MSCI) did not differ significantly in terms of median length of stay, admission to ICU after surgery, total medical cost, or mean medical cost per day (Table 2). However, discharge destinations were significantly different in the three groups according to MMSE score (p = 0.014). The mean EBL was not significantly different in the three groups: 540 ± 454 mL in the MSCI group, 609 ± 521 mL in the MCI group, and 563 ± 641 mL in the NC group (p = 0.762). In addition, rates of re-admission, revision, and postoperative overall complications were not significantly different among the three groups. However, a significant difference was seen in cardiopulmonary complications among the three groups based on the MMSE score (p = 0.037).
Table 2.
Outcome data.
| 0 < MMSE < 20 | 21 ≤ MMSE ≤ 26 | MMSE ≥ 27 | p-Value | |
|---|---|---|---|---|
| Number of patients | 5 | 43 | 54 | |
| Length of stay | 10.6 ± 4.9 | 11.2 ± 5.8 | 9.4 ± 5.4 | 0.488 |
| Admission to ICU after surgery, n (%) | 1 (20.0%) | 7 (16.3%) | 5 (9.3%) | 0.520 |
| Discharged to home, n (%) | 3 (60%) | 39 (91%) | 52 (96.3%) | 0.014 |
| Total medical costs ($) | 7483.2 ± 2529.2 | 8644.9 ± 3446.8 | 7319 ± 3403.4 | 0.944 |
| Mean medical cost per day ($) | 765.3 ± 287.5 | 830.7 ± 271.6 | 814.4 ± 260.3 | 0.837 |
| EBL (mL) | 540 ± 454 | 609 ± 521 | 563 ± 641 | 0.762 |
| OT (minutes) | 186.2 ± 25.0 | 197.3 ± 67.6 | 192.3 ± 97.9 | 0.937 |
| Re-admissions, n (%) | 2 (40.0%) | 11 (25.6%) | 14 (25.9%) | 0.796 |
| Revision, n (%) | 0 (0%) | 7 (16.3%) | 4 (7.4%) | 0.273 |
| Overall complications, n (%) | 2 (40.0%) | 16 (37.2%) | 14 (25.9%) | 0.450 |
| Cardiopulmonary, n (%) | 2 (40.0%) | 1 (2.3%) | 2 (3.7%) | 0.037 |
| Stroke, n (%) | 0 (0%) | 0 (0%) | 1 (1.0%) | 0.527 |
| Wound infection, n (%) | 0 (0%) | 1 (1.3%) | 2 (3.7%) | 0.794 |
| Postoperative pain, n (%) | 0 (0%) | 2 (4.7%) | 1 (1.9%) | 0.628 |
| ASD, n (%) | 0 (0%) | 2 (4.7%) | 4 (7.4%) | 0.624 |
| Postoperative delirium, n (%) | 0 (0%) | 10 (23.3%) | 5 (9.3%) | 0.098 |
Abbreviations: ICU, intensive care unit; EBL, estimated blood loss; OT, operation time; ASD, adjacent segment disease.
Table 3 shows the results of the univariate and multivariate linear regression analyses for length of stay. From the univariate linear regression model, covariates with p < 0.2 (EBL, operation time (OT), hemoglobin (Hb) count, WBC count, platelet count, MMSE score, and BDI score) were included in the multivariate linear regression model. After the enter method analysis, OT (coefficient: 0.244, 95% confidence interval (CI) (0.000, 0.032), p = 0.049), WBC count (coefficient: −0.229, 95% CI (−0.001, 0.000), p = 0.022), platelet count (coefficient: 0.250, 95% CI (0.005, 0.043), p = 0.013), MMSE score (coefficient: −0.196, 95% CI (−0.763, −0.032), p = 0.033), and BDI score (coefficient: 0.190, 95% CI (0.005, 0.238), p = 0.041) were found to be significantly associated with length of stay.
Table 3.
Univariate and multivariate linear regression analysis of length of stay and other continuous variables.
| Variables | Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|---|
| β-Coefficients | 95.0% CI | p-Value | β-Coefficients | 95.0% CI | p-Value | |||
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | |||||
| Age | −0.049 | −0.292 | 0.176 | 0.623 | ||||
| EBL | 0.312 | 0.001 | 0.005 | 0.001 | 0.046 | −0.002 | 0.003 | 0.716 |
| OT | 0.321 | 0.009 | 0.034 | 0.001 | 0.244 | 0.000 | 0.032 | 0.049 |
| WBC | −0.136 | −0.001 | −0.000 | 0.174 | −0.229 | −0.001 | 0.000 | 0.022 |
| Hb | −0.147 | −10.411 | 0.200 | 0.139 | −0.031 | −0.912 | 0.657 | 0.748 |
| PLT | 0.241 | 0.005 | 0.042 | 0.015 | 0.250 | 0.005 | 0.043 | 0.013 |
| MMSE | −0.169 | −0.737 | 0.055 | 0.090 | −0.196 | −0.763 | −0.032 | 0.033 |
| BDI | 0.240 | 0.030 | 0.277 | 0.015 | 0.190 | 0.005 | 0.238 | 0.041 |
Abbreviations: EBL, estimated blood loss; OT, operation time; WBC, white blood cell; Hb, hemoglobin; PLT, platelet; MMSE, mini-mental state examination; BDI, Beck Depression Inventory.
4. Discussion
Cognitive decline is associated with a higher prevalence of several chronic medical conditions and may necessitate higher rates of procedures and surgeries [16,17]. Moreover, preoperative cognitive status has also been linked to the incidence of other adverse outcomes, including postoperative complications, longer hospital stays, and functional decline [16,18]. Robinson et al. reported that baseline cognitive impairment in older adults undergoing major elective surgery was related to adverse postoperative outcomes, including increased complications, prolonged hospital stays, and long-term mortality. [19]. Nonetheless, studies on the association between preoperative cognitive status and postoperative outcomes in adults who undergo surgery for degenerative spinal conditions are limited. As the frequency of spine surgery is increasing in parallel with the aging population and spinal degenerative diseases, a more comprehensive understanding of the relationship between preoperative cognitive status and clinical outcomes is important for predicting general prognosis and determining treatment plans following the spine surgery. In this prospective study, we discovered that discharge destination and OT were significantly different in patients with different preoperative cognitive status. Additionally, MMSE score, an indicator of cognitive status, was independently associated with the length of hospital stay in elderly patients following lumbar surgery.
In this analysis, we compared three groups of patients divided according to the preoperative cognitive status (NC, MCI, and MSCI as per the K-MMSE) who underwent elective surgery, and the three groups had significantly different discharge destinations (p = 0.014). Although these results were not statistically quantitatively correlated, we found that the better the preoperative cognitive status, the more likely it was for the patient to be discharged home (60% for MSCI vs. 91% for MCI vs. 96% for NC). This was not a surprising outcome because individuals with cognitive impairment would be less likely to function independently after surgery. Furthermore, patients with cognitive impairment are at a high risk of hospitalization due to a range of issues including the presence of complex medical illnesses, poor ability to manage chronic diseases, poor medication compliance, higher medication adverse effects, and lack of required social support [20,21]. Adogwa et al. reported that patients undergoing spine surgery for deformity with preoperative cognitive impairment were four times more likely to be discharged to a facility compared with patients with normal cognitive status [22]. Robinson et al. showed that geriatric patients with impaired cognition had a higher rate of discharge to institutions following surgery [19]. Furthermore, Nazir et al. suggested that discharge destination should be included in any model that seeks to predict hospitalization or rehospitalization risk for cognitively impaired individuals [23]. In addition, Capua et al. showed that the factors affecting the discharge destination after elective anterior cervical discectomy and fusion were older age (over 65 years), poorer patient functional status, OT over 4 h, and more severe American Society of Anesthesiology (ASA) class [24]. Since the preoperative cognitive status affects the discharge destination, it may be helpful for surgeons to consider this to plan the postoperative patient care.
We found the overall postoperative complications were not significantly different in the three MMSE groups, except for the cardiopulmonary complication (p = 0.037). Two of five patients in the MSCI group who underwent simple laminectomy developed complications of pneumonia and stable angina, respectively. Viramontes et al. demonstrated that there were strong associations between patients with pre-cognitive impairments undergoing total hip arthroplasty and increased hospital complications such as aspiration pneumonia [25].
Length-of-hospital stay (LOS) is a complex and multifaceted parameter with numerous measurable and intangible factors [26]. Some of the significant predictors of LOS are age, preoperative hemoglobin level, comorbidities, ASA score, type of surgery, fluid balance, volume of fluid transfused, postoperative pain intensity, dependency score, and postoperative complications [27,28,29,30]. However, some of these variables were omitted from the final model because of their modest effect and collinearity with other variables. Although previous studies have indicated that age was associated with LOS after surgery [31,32], age did not have any effect in our LOS model. In the present study, the linear regression models, including univariate and multivariate analyses, revealed that OT and LOS were positively correlated. This finding is consistent with the study of Kudo et al., which demonstrated that patients with long surgery time were more likely to have complications and subsequently have longer LOS [33]. In addition, our study showed that WBC count and platelet count were also associated with LOS. Some previous studies reported that low preoperative hemoglobin levels are associated with long LOS, but in our present study, including the linear regression models, WBC and thrombocyte counts, instead of hemoglobin levels, were associated with LOS [34,35]. In addition, Lakomkin et al. reported that platelet count was a significant predictor of postoperative complications following posterolateral lumbar fusion [35]. Although we did not directly compare the association between platelet count and occurrence of postoperative complications [34], patients who developed postoperative complications required longer hospitalization. Moreover, MMSE score and BDI score had significant effects on LOS in this study. Our results showed that as the MMSE score decreases and BDI score increases, the probability of that patient requiring a longer hospital stay increases. Some prior studies have demonstrated that a cut-off value of 24 points on the MMSE was predictive of a longer hospital stay [36]. MMSE scores tend to be lower with increasing age, and the decreased cognitive function leads to longer LOS [36]. Regarding depression, our findings are similar to those of the previous studies showing that higher the degree of depression [37], poorer the postoperative prognosis, including pain control, which might affect LOS.
Several factors contribute to the cost of spinal surgery: the specific type of spine surgery performed; the number of levels; comorbidities; and surgeon’s choices, such as implant selection [38]. Previous studies demonstrated that various patient factors, such as age, sex, race, insurance status, severity of illness, and length of stay, were also associated with the cost of lumbar spine surgery [39]. In our study, the linear regression models, including univariate and multivariate analyses, revealed that OT was the only variable associated with total medical cost. The longer the OT, the greater was the usage of drugs or complex procedures, which resulted in increased medical costs.
Although some studies comparing the cost of spine surgery have been performed [40,41,42], they did not particularly focus on the specific drivers of hospitalization cost or the prediction of its magnitude. However, while this was not investigated in our study, it was meaningful to identify the factors that affect the cost of medical care in terms of the clinical aspects of spine surgery. Estimation of the hospitalization cost for each patient undergoing spine surgery and the identification of the modifiable drivers of cost could allow physicians to understand the economic aspects of spine surgery and improve their clinical practice. Although the influence was not statistically significant, preoperative cognitive status measured by the MMSE is a possible factor that influences total medical cost in degenerative spine surgery.
Our study had some limitations that must be acknowledged. First, because of the small sample size, especially the number of patients in the MSCI group, and the fact that patients were recruited from a single institution in Korea, the generalizability of our findings may be limited, especially for patients with cultural differences and those with degeneration and higher BMI, such as in the United States or Europe. In the future, multicenter well-designed randomized studies with large samples may help further identify the risk factors associated with preoperative cognitive status in degenerative lumbar surgery. Second, this study was also limited by our inability to completely adjust for characteristics—known and unknown—that may have influenced the results. Although biases were reduced by controlling for significant variables via multivariate analysis, they could not be eliminated. Third, we did not investigate functional parameters, such as physical and social activity before and after surgery in the elderly patients who underwent surgery; we have considered including these parameters in future studies.
5. Conclusions
In conclusion, the role of preoperative cognitive impairment in elderly patients with degenerative spinal disease has not yet been elucidated. However, our data suggest that preoperative cognitive status is associated with discharge destination in such patients. Preoperative cognitive status, as measured by the MMSE, is one of the risk factors for LOS. Improved understanding of baseline cognition before surgery can help surgical decision-making, prediction of outcomes, and planning of postoperative care in elderly degenerative spine patients.
Author Contributions
Conceptualization, H.C.K., S.Y.K., and Y.H.; methodology, H.C.K. and Y.H.; software, H.C.K.; validation, S.B.A., H.J., T.W.K., and J.K.O.; formal analysis, H.C.K. and Y.H.; investigation, H.C.K., S.B.A., H.J., and T.W.K.; resources, H.C.K.; data curation, H.C.K.; writing—original draft preparation, H.C.K.; writing—review and editing, H.C.K., S.Y.K., and Y.H.; visualization, H.C.K.; supervision, D.A.S., S.Y., K.N.K., and P.H.L.; project administration, S.Y.K. and Y.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the ethics committee of Yonsei University Severance Hospital.
Informed Consent Statement
Written informed consent was obtained from all the participants.
Data Availability Statement
Data available on request due to restrictions eg privacy or ethical. The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gajdos C., Kile D., Hawn M.T., Finlayson E., Henderson W.G., Robinson T.N. The significance of preoperative impaired sensorium on surgical outcomes in nonemergent general surgical operations. JAMA Surg. 2015;150:30–36. doi: 10.1001/jamasurg.2014.863. [DOI] [PubMed] [Google Scholar]
- 2.Kim S., Brooks A.K., Groban L. Preoperative assessment of the older surgical patient: Honing in on geriatric syndromes. Clin. Interv. Aging. 2015;10:13–27. doi: 10.2147/CIA.S75285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fehlings M.G., Tetreault L., Nater A., Choma T., Harrop J., Mroz T., Santaguida C., Smith J.S. The aging of the global population: The changing epidemiology of disease and spinal disorders. Neurosurgery. 2015;77(Suppl. 4):S1–S5. doi: 10.1227/NEU.0000000000000953. [DOI] [PubMed] [Google Scholar]
- 4.Lee C.-H., Chung C.K., Kim C.H., Kwon J.-W. Health care burden of spinal diseases in the republic of korea: Analysis of a nationwide database from 2012 through 2016. Neurospine. 2018;15:66–76. doi: 10.14245/ns.1836038.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tan J.Y.-W., Kaliya-Perumal A.-K., Oh J.Y.-L. Is spinal surgery safe for elderly patients aged 80 and above? Predictors of mortality and morbidity in an asian population. Neurospine. 2019;16:764–769. doi: 10.14245/ns.1836336.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takami T. Spine surgeons are facing the great challenge of contributing to the realization of a society of health and longevity. Neurospine. 2019;16:770–771. doi: 10.14245/ns.19edi.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Umekawa M., Takai K., Taniguchi M. Complications of spine surgery in elderly japanese patients: Implications for future of world population aging. Neurospine. 2019;16:780–788. doi: 10.14245/ns.1938184.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee Y.S., Kim Y.B., Lee S.H., Park Y.S., Park S.W. The prevalence of undiagnosed presurgical cognitive impairment and its postsurgical clinical impact in older patients undergoing lumbar spine surgery. J. Korean Neurosurg. Soc. 2016;59:287–291. doi: 10.3340/jkns.2016.59.3.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson C.A., Roffey D.M., Chow D., Alkherayf F., Wai E.K. A systematic review of preoperative predictors for postoperative clinical outcomes following lumbar discectomy. Spine J. 2016;16:1413–1422. doi: 10.1016/j.spinee.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Voorhies R.M., Jiang X., Thomas N. Predicting outcome in the surgical treatment of lumbar radiculopathy using the pain drawing score, mcgill short form pain questionnaire, and risk factors including psychosocial issues and axial joint pain. Spine J. 2007;7:516–524. doi: 10.1016/j.spinee.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Shin M.H., Lee Y.M., Park J.M., Kang C.J., Lee B.D., Moon E., Chung Y.I. A combination of the korean version of the mini-mental state examination and korean dementia screening questionnaire is a good screening tool for dementia in the elderly. Psychiatry Investig. 2011;8:348–353. doi: 10.4306/pi.2011.8.4.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Folstein M.F., Folstein S.E., McHugh P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 13.Tombaugh T.N., McIntyre N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 14.O’Connor D.W., Pollitt P.A., Hyde J.B., Fellows J.L., Miller N.D., Brook C.P., Reiss B.B. The reliability and validity of the mini-mental state in a british community survey. J. Psychiatr. Res. 1989;23:87–96. doi: 10.1016/0022-3956(89)90021-6. [DOI] [PubMed] [Google Scholar]
- 15.Beck A.T., Steer R.A., Carbin M.G. Psychometric properties of the beck depression inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988;8:77–100. doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- 16.Duthie A., Chew D., Soiza R.L. Non-psychiatric comorbidity associated with alzheimer’s disease. QJM. 2011;104:913–920. doi: 10.1093/qjmed/hcr118. [DOI] [PubMed] [Google Scholar]
- 17.Bynum J.P., Rabins P.V., Weller W., Niefeld M., Anderson G.F., Wu A.W. The relationship between a dementia diagnosis, chronic illness, medicare expenditures, and hospital use. J. Am. Geriatr. Soc. 2004;52:187–194. doi: 10.1111/j.1532-5415.2004.52054.x. [DOI] [PubMed] [Google Scholar]
- 18.Phelan E.A., Borson S., Grothaus L., Balch S., Larson E.B. Association of incident dementia with hospitalizations. JAMA. 2012;307:165–172. doi: 10.1001/jama.2011.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robinson T.N., Wu D.S., Pointer L.F., Dunn C.L., Moss M. Preoperative cognitive dysfunction is related to adverse postoperative outcomes in the elderly. J. Am. Coll. Surg. 2012;215:12–17. doi: 10.1016/j.jamcollsurg.2012.02.007. discussions 17–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gray S.L., Mahoney J.E., Blough D.K. Medication adherence in elderly patients receiving home health services following hospital discharge. Ann. Pharmacother. 2001;35:539–545. doi: 10.1345/aph.10295. [DOI] [PubMed] [Google Scholar]
- 21.Preyde M., Chapman T. Psychosocial profile of elderly patients discharged from a community hospital. Soc. Work Health Care. 2007;45:77–95. doi: 10.1300/J010v45n02_05. [DOI] [PubMed] [Google Scholar]
- 22.Adogwa O., Elsamadicy A.A., Sergesketter A., Vuong V.D., Moreno J., Cheng J., Karikari I.O., Bagley C.A. Independent association between preoperative cognitive status and discharge location after surgery: A strategy to reduce resource use after surgery for deformity. World Neurosurg. 2018;110:e67–e72. doi: 10.1016/j.wneu.2017.10.081. [DOI] [PubMed] [Google Scholar]
- 23.Nazir A., LaMantia M., Chodosh J., Khan B., Campbell N., Hui S., Boustani M. Interaction between cognitive impairment and discharge destination and its effect on rehospitalization. J. Am. Geriatr. Soc. 2013;61:1958–1963. doi: 10.1111/jgs.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Di Capua J., Somani S., Kim J.S., Lee N.J., Kothari P., Phan K., Lugo-Fagundo N., Cho S.K. Predictors for patient discharge destination after elective anterior cervical discectomy and fusion. Spine. 2017;42:1538–1544. doi: 10.1097/BRS.0000000000002140. [DOI] [PubMed] [Google Scholar]
- 25.Viramontes O., Luan Erfe B.M., Erfe J.M., Brovman E.Y., Boehme J., Bader A.M., Urman R.D. Cognitive impairment and postoperative outcomes in patients undergoing primary total hip arthroplasty: A systematic review. J. Clin. Anesth. 2019;56:65–76. doi: 10.1016/j.jclinane.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 26.Kanaan S.F., Waitman L.R., Yeh H.W., Arnold P.M., Burton D.C., Sharma N.K. Structural equation model analysis of the length-of-hospital stay after lumbar spine surgery. Spine J. 2015;15:612–621. doi: 10.1016/j.spinee.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walid M.S., Robinson E.C., Robinson J.S., Jr. Higher comorbidity rates in unemployed patients may significantly impact the cost of spine surgery. J. Clin. Neurosci. 2011;18:640–644. doi: 10.1016/j.jocn.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 28.Deyo R.A., Mirza S.K., Martin B.I., Kreuter W., Goodman D.C., Jarvik J.G. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siemionow K., Pelton M.A., Hoskins J.A., Singh K. Predictive factors of hospital stay in patients undergoing minimally invasive transforaminal lumbar interbody fusion and instrumentation. Spine. 2012;37:2046–2054. doi: 10.1097/BRS.0b013e31825c6688. [DOI] [PubMed] [Google Scholar]
- 30.Mayo B.C., Haws B.E., Bohl D.D., Louie P.K., Hijji F.Y., Narain A.S., Massel D.H., Khechen B., Singh K. Postoperative fever evaluation following lumbar fusion procedures. Neurospine. 2018;15:154–162. doi: 10.14245/ns.1836026.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hauck K., Zhao X. How dangerous is a day in hospital? A model of adverse events and length of stay for medical inpatients. Med. Care. 2011;49:1068–1075. doi: 10.1097/MLR.0b013e31822efb09. [DOI] [PubMed] [Google Scholar]
- 32.Neatherlin J.S., Brillhart B., Henry J.J. Factors determining length of hospitalization for patients having laminectomy surgery. J. Neurosci. Nurs. 1988;20:39–41. doi: 10.1097/01376517-198802000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Kudo D., Miyakoshi N., Hongo M., Kasukawa Y., Ishikawa Y., Mizutani T., Shimada Y. Relationship between preoperative serum rapid turnover proteins and early-stage surgical wound infection after spine surgery. Eur. Spine J. 2017;26:3156–3161. doi: 10.1007/s00586-016-4855-z. [DOI] [PubMed] [Google Scholar]
- 34.Leu S., Kamenova M., Mehrkens A., Mariani L., Scharen S., Soleman J. Preoperative and postoperative factors and laboratory values predicting outcome in patients undergoing lumbar fusion surgery. World Neurosurg. 2016;92:323–338. doi: 10.1016/j.wneu.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 35.Lakomkin N., Goz V., Cheng J.S., Brodke D.S., Spiker W.R. The utility of preoperative laboratories in predicting postoperative complications following posterolateral lumbar fusion. Spine J. 2018;18:993–997. doi: 10.1016/j.spinee.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 36.Wobith M., Acikgoz A., Grosser K., Weimann A. Preoperative cognitive function in very old patients: Influence on the complication rate and length of hospitalization. Chir. Z. Geb. Oper. Medizen. 2019;90:930–935. doi: 10.1007/s00104-019-01028-2. [DOI] [PubMed] [Google Scholar]
- 37.Pinheiro M.B., Ferreira M.L., Refshauge K., Maher C.G., Ordonana J.R., Andrade T.B., Tsathas A., Ferreira P.H. Symptoms of depression as a prognostic factor for low back pain: A systematic review. Spine J. 2016;16:105–116. doi: 10.1016/j.spinee.2015.10.037. [DOI] [PubMed] [Google Scholar]
- 38.Menger R.P., Savardekar A.R., Farokhi F., Sin A. A cost-effectiveness analysis of the integration of robotic spine technology in spine surgery. Neurospine. 2018;15:216–224. doi: 10.14245/ns.1836082.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zygourakis C.C., Liu C.Y., Wakam G., Moriates C., Boscardin C., Ames C.P., Mummaneni P.V., Ratliff J., Dudley R.A., Gonzales R. Geographic and hospital variation in cost of lumbar laminectomy and lumbar fusion for degenerative conditions. Neurosurgery. 2017;81:331–340. doi: 10.1093/neuros/nyx047. [DOI] [PubMed] [Google Scholar]
- 40.Lad S.P., Babu R., Baker A.A., Ugiliweneza B., Kong M., Bagley C.A., Gottfried O.N., Isaacs R.E., Patil C.G., Boakye M. Complications, reoperation rates, and health-care cost following surgical treatment of lumbar spondylolisthesis. J. Bone Joint Surg. Am. 2013;95:e162. doi: 10.2106/JBJS.L.00730. [DOI] [PubMed] [Google Scholar]
- 41.McCarthy I.M., Hostin R.A., Ames C.P., Kim H.J., Smith J.S., Boachie-Adjei O., Schwab F.J., Klineberg E.O., Shaffrey C.I., Gupta M.C., et al. Total hospital costs of surgical treatment for adult spinal deformity: An extended follow-up study. Spine J. 2014;14:2326–2333. doi: 10.1016/j.spinee.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 42.Udeh B.L., Costandi S., Dalton J.E., Ghosh R., Yousef H., Mekhail N. The 2-year cost-effectiveness of 3 options to treat lumbar spinal stenosis patients. Pain Pract. 2015;15:107–116. doi: 10.1111/papr.12160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to restrictions eg privacy or ethical. The data presented in this study are available on request from the corresponding author.