Abstract
Since the early days of the pandemic, there have been several reports of cerebrovascular complications during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Numerous studies proposed a role for SARS-CoV-2 in igniting stroke. In this review, we focused on the pathoetiology of stroke among the infected patients. We pictured the results of the SARS-CoV-2 invasion to the central nervous system (CNS) via neuronal and hematogenous routes, in addition to viral infection in peripheral tissues with extensive crosstalk with the CNS. SARS-CoV-2 infection results in pro-inflammatory cytokine and chemokine release and activation of the immune system, COVID-19-associated coagulopathy, endotheliitis and vasculitis, hypoxia, imbalance in the renin-angiotensin system, and cardiovascular complications that all may lead to the incidence of stroke. Critically ill patients, those with pre-existing comorbidities and patients taking certain medications, such as drugs with elevated risk for arrhythmia or thrombophilia, are more susceptible to a stroke after SARS-CoV-2 infection. By providing a pictorial narrative review, we illustrated these associations in detail to broaden the scope of our understanding of stroke in SARS-CoV-2-infected patients. We also discussed the role of antiplatelets and anticoagulants for stroke prevention and the need for a personalized approach among patients with SARS-CoV-2 infection.
Keywords: SARS-CoV-2, COVID-19, stroke, pathophysiology, pharmacology, neuroimmunomodulation, renin-angiotensin system, blood coagulation
Introduction
As a member of the coronavirus family, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the etiological agent of coronavirus disease of 2019 (COVID-19), is an enveloped virus with a positive-sense single-stranded RNA genome, that exhibits ~80 and 50% genetic similarity with severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1) and Middle East respiratory syndrome coronavirus (MERS-CoV), respectively (1, 2). While the pathogenesis of SARS-CoV-2 remains to be clarified, its similarities with SARS-CoV-1 and MERS-CoV pathogenesis may provide insights into SARS-CoV-2 pathogenesis. With few exceptions, coronaviruses are generally associated with respiratory infections. Reports of a wide range of neurologic symptoms including stroke (3, 4), in addition to reports of virus detection in the cerebrospinal fluid (CSF) (5) and brain tissues from autopsies (6–8) introduced a neuroinvasive potential of SARS-CoV-2. Although a causal relationship between coronaviruses and stroke has not yet been established, supporting evidence exists in several publications. First, there is an independent association between COVID-19 and acute ischemic stroke after controlling for other vascular risk factors (9). Further, in a study of 17,799 hospitalized patients with SARS-CoV-2 infection, our team reported a pooled stroke risk of 0.9% while ischemic stroke occurred in 79% of patients, hemorrhagic stroke in 17%, and 4% had cerebral venous thrombosis (10). Other meta-analyses reported a stroke incidence rate of 1.1–1.6% among patients with COVID-19 (11–14) which appears higher than 0.6–0.8% incidence in the general population (15). Evidence has shown a significant decrease in the rate of myocardial infarction and ischemic stroke in the emergency department during the pandemic (16). This phenomenon, which may be attributable to the fear of SARS-CoV-2 infection among the population, suggests the underdiagnosis of stroke and a possible higher incidence of stroke in SARS-CoV-2 infected patients. Moreover, the risk of stroke in SARS-CoV-2 infection is 7.6-fold higher than that of influenza infection (17). Finally, cerebrovascular diseases were an independent predictor of severity and fatality of COVID-19 illness based on adjusted effect estimates (18).
Moreover, stroke in SARS-CoV-2 infected patients is reported to have specific features. It is more commonly reported in young patients (mean age <55 years) without classic vascular risk factors (19–21), with a high prevalence of cryptogenic stroke (11, 22), and an increased incidence of large vessel stroke (11, 21, 23, 24), even in patients with mild SARS-CoV-2 infection (25). These reports highlight the importance of acknowledging the association between stroke and SARS-CoV-2 infection.
Given the former considerations, we conducted a narrative review of possible pathways responsible for neuroinvasion by SARS-CoV-2. We also provided a pictorial overview of the topic to better summarize the potential etiopathogenic mechanisms underlying the stroke in patients with SARS-CoV-2 infections.
SARS-CoV-2 Cellular Entry
The main transmission route for SARS-CoV-2 is the direct contamination of mucosal linings (26) (Figure 1). Epithelial cells in the mucosal linings of the respiratory and gastrointestinal tracts can spread the virus by expressing the main receptor of SARS-CoV-2—angiotensin-converting enzyme-2 (ACE2)—and the main cofactor—transmembrane serine protease 2 (TMPRSS2) (27). TMPRSS2 is an activating protease that is necessary for cleaving the spike protein of SARS-CoV-2, facilitating the viral binding to the receptor, and leading to viral internalization (28). In addition to ACE2, the cluster of differentiation 147 (CD147), which acts through interaction with spike glycoprotein, was introduced as a novel receptor for SARS-CoV-2 (29). A furin cleavage site, which was not present in the spike glycoprotein of SARS-CoV-1, has also been discovered in SARS-CoV-2 as a host factor participating in viral infection (30). Furin is a ubiquitous protease that participates in activating surface proteins of viruses such as coronaviruses and influenza (31, 32). Although not consistently expressed in all cell types, ACE2, TMPRSS2, CD147, and furin are present in the human respiratory tract (33). Furthermore, neuropilin-1 (NRP1), a cellular transmembrane receptor, has been introduced to act as a specific receptor for SARS-CoV-2 (34, 35). Epithelial cells of respiratory and gastrointestinal linings highly express NRP1 (34). NRP1 has been shown to mediate viral infection even in the absence of TMPRSS2 and ACE2. However, the infection is milder compared to the sole expression of ACE2 (34).
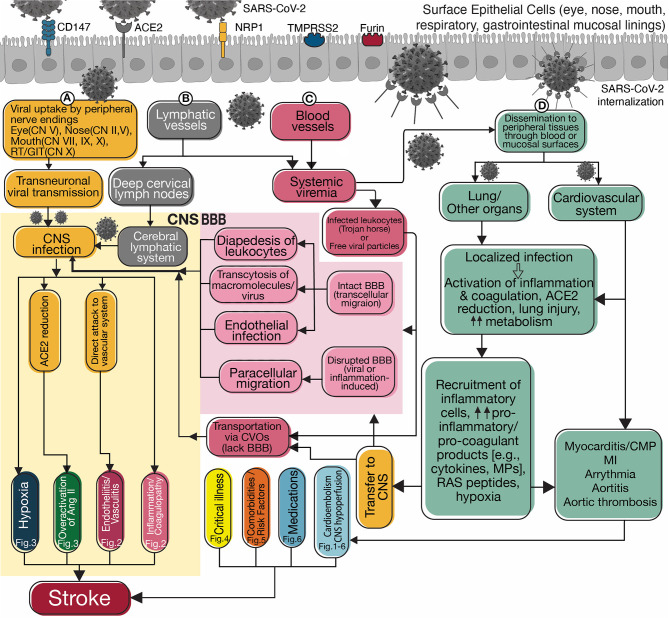
Figure 1.
Flowchart diagram summarizes possible routes for neuroinvasion and potential mechanisms of stroke. SARS-CoV-2 penetrates through its receptors, ACE2, CD147, or NRP1 and co-receptors, TMPRSS2, or FURIN present on the epithelial cells of the surface mucosal lining. Transportation occurs via viral invasion into (A) peripheral nerve endings and transneuronal transmission, (B) peripheral lymphatic vessels connected to the blood or cerebral lymphatic circulation, and (C) the blood vessels and invasion into the CNS (yellow box on the left). In blood, the virus spreads inside infected leukocytes (aka “Trojan horse”) or as free particles. Viral invasion through the hematogenous route requires crossing the intact blood-brain barrier (BBB) or penetrating the CNS through circumventricular organs (CVOs) that lack BBB. Intact BBB may allow a limited number of leukocytes to enter the CNS via transcellular diapedesis. Viral particles and macro-molecules can breach the BBB via receptor-mediated transcytosis or adsorptive transcytosis. Finally, SARS-CoV-2 can directly infect the endothelium and cross. A disrupted BBB enables unlimited paracellular transportation. Once In the CNS, the virus can invade the vascular system and increase stroke risk by causing endotheliitis/vasculitis (Figure 2), activating the inflammation and coagulation cascades (Figure 2), overactivation of angiotensin II signaling pathways (Figure 3), or causing local hypoxia (Figure 3). There is crosstalk between the inflammatory and coagulation systems in the central and peripheral environments because their products are transported bidirectionally. Viral invasion into peripheral tissues, including pulmonary and cardiovascular systems, occurs through direct mucosal surfaces or hematogenous dissemination (D). Activation of inflammation and coagulation systems increases pro-inflammatory and pro-coagulant products, which are then transported to the CNS accompanying angiotensin II through BBB and CVOs. Lung and cardiovascular injury and elevated metabolism cause systemic hypoxia increasing the risk of stroke. Cardiovascular damage (Figures 1–6) can cause a stroke by arrhythmia and cardioembolism or by decreased cardiac output resulting in cerebral hypoperfusion. Clinical features of critical illness (Figure 4), especially in patients with some comorbidities or risk factors (Figure 5) and side effects of certain medications (Figure 6) may be related to increased risk of stroke. SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2; CD147, Cluster of differentiation 147; ACE2, Angiotensin-converting enzyme 2; NRP1, Neuropilin-1; TMPRSS2, Transmembrane Serine Protease 2; CN, Cranial Nerve; RT, Respiratory tract; GIT, Gastrointestinal tract; CNS, Central nervous system; Fig, Figure; Ang II, Angiotensin 2; BBB, Blood-brain barrier; CVOs, Circumventricular organs; MPs, Microparticles; RAS, Renin-angiotensin system; CMP, Cardiomyopathy; MI, Myocardial infarction.
After passing through the mucosal linings, the systemic spread of SARS-CoV-2 to tissues, blood and lymphatic circulation, and peripheral nerve endings can enable the spread to the central nervous system (CNS). The brain is privileged by having various barriers such as the blood-brain barrier (BBB) and the blood-cerebrospinal fluid barrier (36). However, the integrity of these barriers is not complete and pathologic conditions may disrupt them (37). After crossing the barriers, SARS-CoV-2 neuroinvasion needs the presence of viral receptors in the host brain cells. Human brain cell lines express ACE2, CD147, NRP1, and TMPRSS2 (38, 39).
Proposed Mechanisms for Neuroinvasion
Two possible routes can be hypothesized for SARS-CoV-2 neuroinvasion, including neuronal and hematogenous transmission. Figure 1 pictures the possible mechanisms of stroke associated with SARS-CoV-2 in each of these routes.
Neuronal Route of Neuroinvasion
Transneuronal transport of the SARS-CoV-2 through peripheral nerve endings can occur via specific viral receptors (40) (Figure 1A). In addition, peripheral nerve endings may use other mechanisms for uptake of the virus. For example, viral uptake can occur via trans-synaptic membranous-coating-mediated endocytosis (similar to other coronaviruses) (41) or fusion of virus envelope with the host neuron via the axonal membrane of the next-order-neuron (similar to herpesviruses) (42).
Like other mucosal linings, nasal mucosa (the respiratory mucosa and olfactory mucosa) may be an entry site for SARS-CoV-2. The human nasal mucosa and olfactory bulb express different levels of NRP1, ACE2, CD147, TMPRSS2, and Furin, which may explain the smell and taste disturbance (34, 43–45). The expression of ACE2 and TMPRSS2 was not obvious in the neurons of the olfactory mucosa and olfactory bulb, however, they were detected in the non-neuronal cells (such as support cells, stem cells, and perivascular cells) (43). Neuropathological analysis of COVID-19 deceased patients showed high expression of NRP1 in SARS-CoV-2 infected cells of the olfactory epithelium, and tracts (34).
The neuroinvasive potential of respiratory coronaviruses through the olfactory nerve was previously examined in mice models inoculated with intranasal SARS-CoV-1. Viral antigens were primarily detected in the olfactory bulb, areas of the brain connected directly to the olfactory bulb, and then dissemination throughout the brain (46). Further studies on the autopsy of a COVID-19 patient with anosmia, dysgeusia, and seizure revealed diffuse tissue damage in the olfactory pathway, rectus gyrus, and medulla oblongata. Neurons, glial cells, axons, and nerve sheaths were damaged, and particles resembling virions of SARS-CoV-2 were detected in these structures (47). In another study, asymmetric olfactory bulb with or without olfactory cleft obliteration was present in 4 out of 19 early postmortem MRI examinations of patients who died from COVID-19; however, downstream olfactory tract changes were not evident (48). Moreover, a recent MRI study reported that persistent anosmia in COVID-19 patients evaluated with objective olfactory tests may be associated with olfactory bulb atrophy (49).
Intranasal inoculation of murine coronavirus resulted in widespread infection, including the detection of viral genome in the trigeminal and olfactory nerves, and areas in the brain connected to them (50). Observing this pattern of viral spread by following known neuroanatomical pathways supports trans-neural transmission through this nerve (50). Trigeminal nerve involvement was proposed as a possible mechanism of headache in COVID-19 patients (51).
ACE2 and TMPRSS2 are present in the human conjunctiva and the cornea (52). Ocular manifestations (53) and SARS-CoV-2 presence in tears and conjunctival secretions (54) were reported. Eyes may provide an entry for SARS-CoV-2 through the trigeminal nerve into the CNS.
The involvement of trigeminal, facial, glossopharyngeal, and vagus nerves in the nasal and oral mucosa, which are responsible for the detection and transport of taste signals, maybe the reason for a high incidence of taste disturbance in the COVID-19 patients up to 88% (55, 56). As presented in animal models of influenza virus, viral spread to reach the brain via the vagus nerve is possible (57). The virus may hypothetically invade the vagus nerve in respiratory and gastrointestinal tracts and retrogradely infect the CNS (58).
Hematogenous Route for Neuroinvasion
Infection of mucosal linings may provide access to the lymphatic system (Figure 1B) and the bloodstream (Figure 1C) as endothelial cells express the SARS-CoV-2 receptors (59, 60). These pathways may disseminate the virus to the peripheral tissues such as the lungs and cardiovascular system (Figure 1D), or end up in the CNS. The brain has a functional lymphatic pathway connected to the deep cervical lymph nodes which is capable of transferring fluid and immune cells (61). The lymphatic pathway can be hypothesized to be an entry for the SARS-CoV-2.
BBB tightly protects the CNS micro-environment. However, peripheral leukocytes can minimally cross the BBB via transcellular diapedesis (37). During an inflammation, damaged tight junctions of endothelial cells make trafficking via paracellular routes possible (37). SARS-CoV-2 might cross the intact BBB and cause BBB damage directly or through induction of pro-inflammatory cytokines (e.g., IFN-γ) and chemokines (62). A monolayer culture of human endothelial cells showed low ACE2 levels. However, ACE2 upregulation has been noted due to shear stress in the 3-dimensional model of the middle cerebral artery, particularly in stenotic portions. In this model, recombinant SARS-CoV-2 spike protein attachment to ACE2 of endothelial cells induced various gene expression including the offending proteins in COVID-19 such as IL-4, IL-10, and complement C3. These findings further support the susceptibility of human brain endothelial cells to SARS-CoV-2 infection (63). Moreover, a model of human BBB showed disruption of endothelial barrier after introduction of SARS-CoV-2 spike protein via inducing a pro-inflammatory response on brain endothelium. This model added another evidence for neuroinvasive nature of the virus (64). Investigation of cadavers revealed SARS-CoV-2 particles packed in vesicles capillary endothelial cells and the neurons of the frontal lobe (6). Exocytosis and endocytosis of viral particles were also observed in endothelial cells which support the hematogenous route for viral invasion (6).
SARS-CoV-2 invasion to the lung appears to happen directly through viral disruption of alveolar and bronchial epithelial cells and macrophages, and indirectly via systemic inflammatory mediators. The type II alveolar epithelial cells and macrophages found in alveoli and pulmonary hilum lymphoid tissues are infected by SARS-CoV-2. COVID-19 patients with severe signs of pneumonia and acute respiratory distress syndrome (ARDS) have characteristics of systemic hyper-inflammation known as “cytokine storm” with exaggerated production of pro-inflammatory cytokines and chemokines, and also pro-coagulant factors (1, 65). Infection of respiratory epithelial cells, dendritic cells, and alveolar macrophages by SARS-CoV-2 might drive the cytokine storm (1, 65, 66). Pro-inflammatory products might result in damages in pulmonary tissues, and transfer of these products in the systemic circulation to other organs and failure of multiple organs such as cardio- and cerebrovascular systems. Mast cells, which are found in the submucosa of the respiratory system, are also hypothesized to have a crucial role in SARS-CoV-2 hyper-inflammation by releasing histamine and proteases and pro-inflammatory cytokines and chemokines (67). Through various mechanisms such as the expression of ACE2, mast cells recognize SARS-CoV-2 and recruit immune cells (68). Hypoxia, an outcome of respiratory failure and elevated metabolism, and elevated levels of angiotensin 2 may also link the pulmonary infection with cardiovascular events and stroke. Indirect effects of peripheral infection via transportation of these local products to the CNS may trigger a stroke even in the absence of viral neuroinvasion.
Moreover, reallocation of SARS-CoV-2-containing macrophages migrating out of the lungs to other tissues such as CNS is plausible in the context of viral spread. Infecting the leukocytes and using them as a reservoir was known in SARS-CoV-1 and some other neuroinvasive viruses (69, 70).
In addition to disruption of BBB, circumventricular organs (CVOs) are a candidate for entry to the brain. CVOs are specialized sensory areas of the brain participating in fluid homeostasis, cardiovascular regulation, and energy balance. CVOs have fenestrated capillaries that make them windows for the entrance of blood-borne products and pathogens to the brain (71). CNS infection through CVOs has not been reported in humans; however, animal models have demonstrated CVOs as a route for pathogens to invade the CNS (72).
Factors Associated With Stroke in Patients Infected With SARS-CoV-2
Endothelial Cells
Endothelial cells maintain vascular hemostasis and blood flow. Due to a large surface area, cells are exposed to intravascular signals from pathogens and inflammatory products (Figure 2C). Cells actively respond to stimuli by structural alterations, leading to increased vascular permeability and secretion of the pro-inflammatory cytokines. Cytokines recruit immune cells, such as neutrophils and platelets, and combine with pro-coagulant factors to form a thrombus that encases pathogens (73). Activated endothelial cells also influence the balance of vascular tone, resulting in diminished blood flow and ischemia (74). In addition to chemical signals from the virus, inflammatory cells, and platelets, direct viral invasion to endothelial cells also happens in SARS-CoV-2 infection. Diffuse endotheliitis, presence of viral particles in endothelial cells, and tissue infarction in various organs, including the lungs, heart, kidney, small intestine, liver (59), and brain (6), were reported in patients with SARS-CoV-2. Biomarkers associated with activated endothelial cells and platelets were significantly higher in SARS-CoV-2 infected ICU patients than non-ICU admitted patients (75). These markers were also associated with mortality, highlighting the prominent role of endotheliopathy in COVID-19 (75).
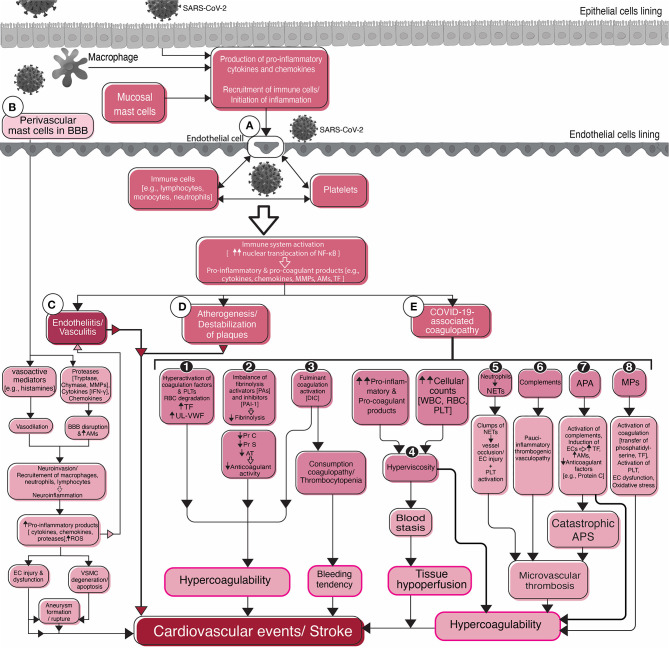
Figure 2.
Flowchart diagram shows the roles of endothelial cells, platelets, the inflammatory system, and the coagulation system in SARS-CoV-2-associated stroke and cardiovascular events. Viral infection of epithelial cells of the mucosal linings stimulates them for the production of pro-inflammatory cytokines and activation of the immune system. Macrophages and mast cells residing in the mucosal tissues also participate in the activation of the immune system in the early stages of infection. Activation of and interaction between the immune system, endothelial cells, and platelets (A) in circulation result in stroke complications. Common sequelae include endotheliitis, or vasculitis (C), atherogenesis, or destabilization of pre-existing atherosclerotic plaques (D), and COVID-19-associated coagulopathy (E). Different mechanisms that are attributable to COVID-19-associated coagulopathy are depicted in detail (1–8). The possible role of mast cells in the blood-brain barrier (BBB) disruption, initiation and/or aggravation of inflammation, neuroinvasion, and stroke are summarized in the left side of the figure (B). Mast cells, one of the two resident immune cells (microglia is the second one), cause BBB damage leading to the recruitment of peripheral immune cells and the virus into the brain and inflammation in the cerebral vasculature and subsequent stroke. SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2; BBB, Blood-brain barrier; NF-κB, Nuclear factor-kappa B; MMPs, Matrix metallopeptidases; AMs, Adhesion molecules; TF, Tissue factor; IFN-γ, Interferon-gamma; ROS, Reactive oxygen species; EC, endothelial cell; VSMC, Vascular smooth muscle cell; PLT, Platelet; RBC, Red blood cell; UL-VWF, Ultra large-von Willebrand factor; PA, Plasminogen activator; PAI-1, Plasminogen activator inhibitor-1; Pr, Protein; AT, Antithrombin; DIC, Disseminated intravascular coagulation; WBC, White blood cell; NETs, Neutrophil extracellular traps; APA, Antiphospholipid antibodies; APS, Antiphospholipid syndrome; MPs, Microparticles.
Viral-induced vasculopathy was reported in different viruses and may be a predisposing factor for stroke in SARS-CoV-2 infection as well. For instance, the varicella-zoster infection that has been associated with vasculopathy of large and small vessels may induce transmural involvement of the vessels, which in turn leads to ischemic and hemorrhagic strokes (76). SARS-CoV-1 infections are associated with systemic vasculitis, featuring leukocyte infiltration and endothelial cell proliferation, swelling, and apoptosis (77). Similarly, there are reports of patients with SARS-CoV-2 presenting with cerebral vasculitis and vasculopathy with micro- and macrohemorrhage (48, 78–80).
Platelets
Platelets can restrict pathogens by releasing pro-coagulant and pro-inflammatory mediators, forming thrombus, and directly interacting with pathogens, endothelium, and immune cells (81) (Figure 2). Thrombocytopenia is a common complication of viral infections, with diverse etiologies including SARS-CoV-2, (82) and may increase bleeding tendency. Thrombocytopenia and thrombocytosis were both associated with the severity and mortality of COVID-19 (83, 84). Thrombocytosis may be induced by thrombopoietin, released in the presence of pro-inflammatory cytokines such as IL-6 (85). Platelet count elevation was reported as a distinctive feature in SARS-CoV-2-induced pneumonia vs. other etiologies (86). There is a low risk of venous and arterial thrombus formation following reactive thrombocytosis (87, 88). In a group of hospitalized SARS-CoV-2 patients, platelet counts >450 × 109/L, were predictive of thrombotic events and platelet counts below 150 × 109/L were predictive of hemorrhagic events (89).
Inflammatory System
Direct activation of the immune system, platelets, and endothelial cells by SARS-CoV-2 appears to play a pivotal role in further activation of the inflammatory system and chemical release (Figure 2A). The exaggerated inflammatory responses may cause vascular events including stroke through various mechanisms that are being further discussed.
Mast Cells
Mast cells that reside in the cerebral perivascular spaces and are presumed to be the first responders in inflammatory reactions in the CNS have a key role in the disruption of BBB (90) (Figure 2B). Mast cells produce various types of vasoactive mediators such as histamine, proteases (e.g., tryptase and chymase), cytokines, and chemokines. Release of these products causes endothelial dysfunction, BBB disruption, expression of adhesion molecules leading to leukocyte trafficking to the affected tissue, and neuroinflammation (90, 91). Therefore, they may be implicated in the initiation or deterioration of stroke. Activated mast cells participate in the pathogenesis of ischemic and hemorrhagic stroke, and hemorrhagic transformation of ischemic stroke after treatment with recombinant tissue plasminogen activator (92). Release of vasodilatory and proinflammatory substances, damage to the BBB, recruitment of immune cells, and neuroinflammation have been related to the role of mast cells in stroke (92, 93). Although it has not been observed in the CNS, degranulating mast cells were observed in the vessel wall of an infarcted spleen associated with SARS-CoV-2 vasculitis (94). Moreover, experimental models revealed the role of mast cells in the pathogenesis of cerebral aneurysm via induction of inflammation in the vessel wall. The inhibition of activated mast cells successfully prevented the progression of an aneurysm (95). Human studies confirmed abundant mast cells in the cerebral aneurysm wall and significant elevation in ruptured aneurysms (96). The formation of a cerebral aneurysm was also associated with the activation of macrophages, neutrophils, and leukocytes with the production of pro-inflammatory cytokines and matrix metalloproteinases (MMPs). In addition, endothelial dysfunction and vascular smooth muscle cell degeneration, and apoptosis leading to vessel wall thinning were also linked with cerebral aneurysm (97).
Atherogenesis and Destabilization of Plaques
Infection increases pro-inflammatory cytokines that in turn activate inflammatory cells inside the atherosclerotic plaques (98) (Figure 2D). Cytokines and intraplaque inflammatory cells destabilize the preexisting atherosclerotic plaques via increasing proteins such as metalloproteinases and oxidative stress (98, 99). Moreover, hyper-secretion of cytokines and chemokines during SARS-CoV-2 infection are hypothesized to stimulate the formation of new-onset vascular plaques (100). Inflammatory products cause oxidative stress, damage the endothelium and overlying fibrous cap of atherosclerotic plaques, activate the platelets and stimulate the vascular smooth muscle cells to migrate into the intima, and produce fibrous products which lead to the production of fatty streaks (100). In addition, acute infection and inflammation increase pro-coagulant products and cause a hypercoagulable state. Arterial surface breakdown at the site of plaque rupture in the presence of a hypercoagulability state increases the risk for acute thrombogenesis (98, 99).
COVID-19-Associated Coagulopathy
Although not completely understood, COVID-19-associated coagulopathy (CAC, Figure 2E) shares characteristics with sepsis-induced coagulopathy, disseminated intravascular coagulopathy (DIC), or thrombotic microangiopathies (101). Nonetheless, CAC has distinctive features, such as a higher incidence of thrombotic events than sepsis, the prominent role of inflammatory cytokines, complements, and antiphospholipid antibodies (101). Moreover, despite frequent thrombotic events in severe COVID-19, milder thrombocytopenia, and milder prolongation of prothrombin time (PT) compared to sepsis-induced DIC occurs (101). Important characteristics of CAC that may be hypothesized to stimulate cardiovascular events and stroke are explained.
Direct damage and activation of endothelial cells by SARS-CoV-2 may initiate a procoagulant state, as it occurs during sepsis (73). Direct interaction with platelets and inflammatory cells, and secretion of pro-coagulant factors, such as tissue factor (TF) and von Willebrand factor (vWF), follows. Furthermore, activation of the coagulation cascade, inhibition of the anticoagulation system and fibrinolysis, and change in blood flow are associated with inflammation-induced coagulopathy (73) (Figure 2-E1, E2). Inflammatory cytokines may induce endothelial cells to secrete hyperactive ultra-large vWF multimers and prevent the cleavage of vWF to less active fragments (102). Furthermore, in patients with COVID-19, hyperactivation of the fibrinolysis system has been reported due to endothelial injury, elevated plasminogen activators, and elevated D-dimer levels (103). However, despite the elevated D-dimer levels, which usually suggest a hyperfibrinolytic state, a paradoxical fibrinolysis shutdown was shown in patients with COVID-19 (104). This hyperfibrinolytic state is not expected in sepsis-induced coagulopathy or DIC and is unique in COVID-19. The counter-balance of hyperfibrinolysis by elevated levels of fibrinolytic inhibitors, such as plasminogen activator inhibitor-1 (PAI-1), may in part explain the frequent thrombotic events in SARS-CoV-2 infection (105).
An abnormal elevation of plasma macromolecules such as immunoglobulins and fibrinogen in addition to cellular elements (erythrocytes, leukocytes, or platelets) increase the blood viscosity, impairs blood flow in the microvasculature, and damages endothelium (106, 107). Hyperviscosity is associated with hypercoagulability, blood stasis, and tissue ischemia complications (106, 107) (Figure 2-E4, Figure 3). COVID-19-associated hyperviscosity has been reported in patients with thrombotic complications which may be linked with hyper-fibrinogenemia or exaggerated cytokine release in SARS-CoV-2 infection (108).
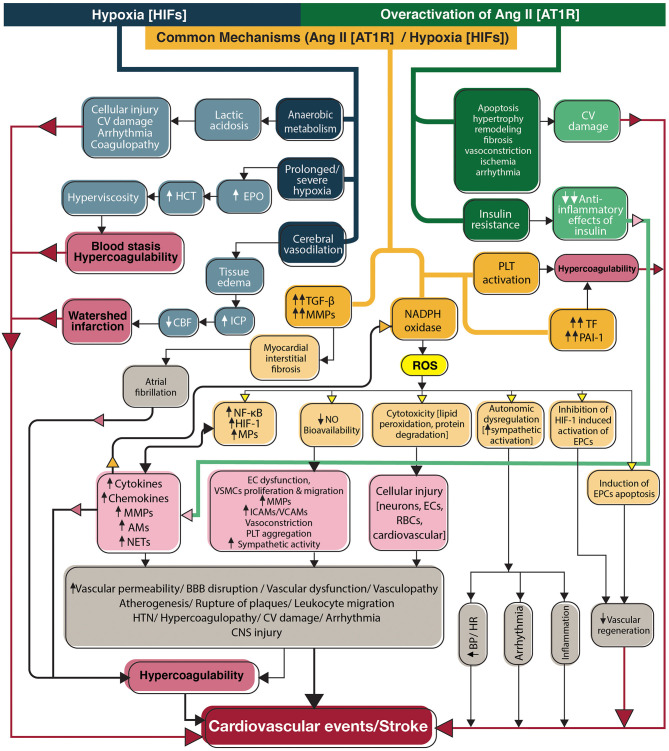
Figure 3.
Flowchart diagram shows the contribution of the renin-angiotensin system and hypoxia to stroke in SARS-CoV-2 infection. Overactivation of angiotensin II signaling pathways and hypoxia directly activate inflammation and coagulation systems, in addition to indirect activation through induction of NADPH, to produce reactive oxygen species (yellow box). Ang II acts through its main receptor, angiotensin type 1 receptor, and hypoxia mediates its effects through transcription factors, hypoxia-inducible factors. CV, Cardiovascular; EPO, Erythropoietin; HCT, Hematocrit; ICP, Intracranial pressure; CBF, Cerebral blood flow; TGF-β, Transforming growth factor-beta; MMPs, Matrix metallopeptidases; NADPH, Nicotinamide adenine dinucleotide phosphate; ROS, Reactive oxygen species; PLT, Platelet; TF, Tissue factor; PAI-1, Plasminogen activator inhibitor-1; HIFs, Hypoxia-inducible factors; NF-κB, Nuclear factor-kappa B; HIF-1, Hypoxia-inducible factor-1; MPs, Microparticles; AMs, Adhesion molecules; NETs, neutrophil extracellular traps; NO, Nitric oxide; EC, Endothelial cell; VSCM, Vascular smooth muscle cell; ICAMs, Intercellular adhesion molecules; VCAMs, Vascular cell adhesion molecules; BBB, Blood-brain barrier; HTN, Hypertension; CNS, Central nervous system; RBCs, Red blood cells; BP, Blood pressure; HR, Heart rate; EPCs, Endothelial progenitor cells; Ang II, Angiotensin II; AT1R, Angiotensin type 1 receptor; HIFs, Hypoxia-inducible factors.
Neutrophils secret an extracellular network consisting of proteolytic enzymes and chromatin (Figure 2-E5). The network, which attacks local pathogens, are called neutrophil extracellular traps (NETs). If uncontrolled, NETs cause cellular damage, endothelial injury, thrombosis, or vascular rupture and hemorrhage and they may have a pivotal role in the pathogenesis of severe COVID-19 (109). Plasma NETs are associated with disease severity in COVID-19 patients and micro-thrombosis through interaction with platelets (110). By forming intravascular clumps, NETs occlude the vessels, and accelerate thrombus formation leading to micro-vasculopathy in COVID-19 (111). The association between plasma NETs in patients with acute stroke and the severity of the stroke suggests the prominent role of neutrophils in arterial thrombosis (112). Neutrophils and NETs were detected in cerebral clots that were retrieved during endovascular reperfusion therapies from patients with large vessel occlusions. The specimens showed successful ex vivo thrombolysis after adding DNase-1 (to disrupt NETs) to tissue plasminogen activator (t-PA) (113).
Complement proteins are parts of the innate immunity that are implicated in coagulopathy and thrombosis (114) (Figure 2-E6). Pathologic examination of lung tissue and purpuric skin lesions of five patients with severe COVID-19 showed pauci-inflammatory thrombogenic vasculopathy with complement deposition (115). Based on data describing the co-localization of SARS-CoV-2 spike glycoproteins with complement products in these patients, direct activation of complement was hypothesized (115). Other evidences support that complement-induced endothelial injury is a chief contributor to the development of inflammation, thrombotic events, and organ failure in COVID-19 (116). SARS-CoV-2 spike protein subunits seem to directly activate the alternative complement pathway on the cellular surface (117). Attachment of SARS-CoV-2 spike protein to endothelial cells upregulates the expression of C3 (63). C3 reduction, due to overactivation and conversion to active components, was related to the poor prognosis of COVID-19 patients (118). Besides, elevated levels of activated complement products have been associated with the biomarkers of endothelial damage and the severity of COVID-19 (119).
Secondary antiphospholipid antibody syndrome (APS) may explain stroke in relatively young patients with COVID-19 (120). Elevation of antiphospholipid antibodies (APA) (Figure 2-E7) is associated with a higher incidence of thromboembolic events during viral infections (121). In a cohort of ICU-admitted COVID-19 patients with frequent thrombotic complications, positive APA was reported in 88% of patients (122). Multi-territory ischemic stroke was also reported in patients with COVID-19 and positive APA (123). Increased expression of adhesion molecules by endothelium, induction of TF, inhibition of endogenous anticoagulants in the protein C pathway, and activation of the complement system have been suggested as causes for APA-related thrombosis (124). Catastrophic APS is a rare entity and a severe form of APS with a high mortality rate. It causes microvascular thrombosis, rapid multi-organ dysfunction (125), and could be associated with the microvasculopathy observed in some severe COVID-19 infections.
Microparticles (MPs) are plasma membrane-derived vesicles blebbing during activation or apoptosis of different cell types, mainly including platelets, endothelial cells, and leukocytes. MPs present antigens similar to their cell of origin (126) (Figure 2-E8). In pathologic conditions such as sepsis and vascular diseases, the circulating levels of MPs elevate and participate in inflammation, coagulation, vascular dysfunction, and oxidative stress (126). Platelet-derived MPs are implicated in acute ischemic stroke (127). Their pro-coagulant activity is mainly associated with the presence of phosphatidylserine in the outer cell surface, providing a catalytic surface for the assembly of coagulation factors and thrombin generation and expression of TF (128). Higher levels of pro-coagulant MPs were detected in hospitalized COVID-19 patients compared to patients without the disease (129). Circulating MPs are correlated with the expression of pro-inflammatory cytokines in patients with COVID-19 and a possible predictor of the severity of COVID-19 (130).
Classic and Alternative Renin-Angiotensin System
The renin-angiotensin system (RAS) is primarily responsible for regulating blood pressure, water, and electrolytes (131) (Figure 3, green and orange pathways). Angiotensin II (Ang II) is produced from angiotensin I by the angiotensin-converting enzyme (ACE). Ang II is a potent vasoconstrictor and acts via its main receptor, angiotensin II receptor type 1 (AT1R), which is expressed in several tissues. Angiotensin II receptor type 2 (AT2R) with a lower affinity for Ang II counteracts with AT1R (131). On the other hand, ACE2, the homolog of ACE, is the main regulator of the classic RAS (132). ACE2 cleaves Ang II to Ang (1–7) and diverts the system to the alternative RAS with vasoprotective outcomes such as decreasing blood pressure, inflammation, and atherosclerosis. The main receptor of Ang (1–7) is Mas, but it also triggers AT2R. Ang (1–7) increases bradykinin levels by inhibiting ACE from its degradation and promotes vasodilation and fibrinolysis by bradykinin (132).
Consequences of ACE2 Reduction and Angiotensin II Overactivation
Receptor-mediated endocytosis of SARS-CoV-2 with ACE2 causes an elevation in the ACE/ACE2 ratio (133). Overactivation of the classic RAS may increase the risk of both hemorrhagic and ischemic stroke (134). The brain has an independent RAS that does not interact with peripheral RAS because of the BBB (135). However, blood-borne Ang II enters the CNS across the disrupted BBB or the circumventricular organs (136).
Ang II stimulates vascular events with activation of inflammation and coagulation. AT1R inhibition was shown to be a useful immunosuppressive therapy (137). It directly activates toll-like receptors on the leukocytes to stimulate “nuclear factor kappa B” (NF-κB) and produce cytokines, chemokines, adhesion molecules, and metalloproteinases. It also damages the endothelium resulting in atherosclerosis, destabilization of plaques, and thrombosis. Ang II decreases the anti-inflammatory effects of insulin by inhibiting its signal transduction, further increasing inflammation (138). Ang II promotes coagulation via stimulation of tissue factor expression and platelet aggregation. Conversely, by increasing PAI-1 and decreasing t-PA via breakdown of bradykinin, Ang II inhibits fibrinolysis (139).
Ang II and Oxidative Stress
Ang II downregulates the expression of nitric oxide (NO) by endothelium. NO is vasoprotective and prevents atherosclerosis by influencing endothelial cells, platelets, and vascular tone (140). NO is a potent endogenous vasodilator that counteracts with Ang II to increase regional blood flow and regulate BP. NO prevents coagulation and inflammation by inhibiting platelet aggregation and leukocyte adhesion (141). Ang II also decreases NO bioavailability by induction of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase to produce reactive oxygen species (ROS) (142). The significant role of NADPH oxidase activity in disease severity was shown in COVID-19 as its activity was higher in patients than controls and was observed to be markedly elevated in patients who required ICU admission. It was also higher in patients with thrombotic events than patients without thrombosis independent from other vascular risk factors suggesting the implication of oxidative stress in COVID-19-associated coagulopathy (143). The role of ROS in Ang II signaling has been specifically observed in CNS (144). Pathologic ROS levels are cytotoxic and cause vascular oxidative stress involved in the pathogenesis of stroke (145). ROS trigger NETs production which in turn promote vascular events (146). Through oxidative stress, Ang II increases endothelial progenitor cell apoptosis and decreases re-endothelialization and vascular regeneration after injury (147).
Cardiovascular Effects of Ang-II
The other well-established effect of Ang II is the enhancement of sympathetic activity, impacting cardiovascular responses such as heart rate and blood pressure (148). NO modulates this effect with anti-sympathetic activity (149). Ang II also promotes atherosclerosis and vascular dysfunction by creating oxidative stress. ROS stimulate vascular smooth muscle cell proliferation and migration (150) which elevate the risk for future cardiovascular and cerebrovascular events in SARS-CoV-2 infected survivors.
Cardiomyocytes undergo hypertrophy and remodeling with stimulation of AT1R (151). Through induction of transforming growth factor beta 1 and MMP-9 (associated with myocardial matrix remodeling) and induction of myocardial fibrosis, hypoxia-inducible factor 1α and Ang II are associated with pathogenesis and maintenance of atrial fibrillation (AF) (152).
Hypoxia
Hypoxia was an independent prognostic factor for severity in patients with COVID-19. Hypoxia was associated with elevated white blood cell counts, C-reactive protein, and D-dimer levels in patients with COVID-19, possibly indicating a relationship between hypoxia, inflammation, and coagulopathy in severe infection (153). Hypoxia causes cerebral vasodilation and tissue edema by increasing substances like NO and prostacyclin (154). Continued or severe hypoxia causes anaerobic metabolism and lactic acidosis, which additionally enhances vasodilation and tissue edema (154). These events may increase intracranial pressure, limit the cerebral blood flow, and cause cerebral ischemia (Figure 3- blue and orange pathways).
Role of Hypoxia-Inducible Factors
Hypoxia activates the expression of hypoxia-inducible factors (HIF1 and HIF2). These transcription factors have extensive crosstalk with the family of transcription factors NF-κB (155). Activation of inflammation requires nuclear translocation of NF-κB, which leads to the expression of the target genes. Enhanced activation of the NF-κB by HIFs is the key mechanism connecting hypoxia to inflammation (156). Hypoxia activates pro-coagulant factors such as TF by up-regulating the transcription factor early growth response-1 and restricts thrombolysis by increasing PAI-1 and reducing plasminogen activators (157). HIFs also increase NETs production that further promote thrombus formation (158). Platelets produce stabilized HIF-2α and PAI-1 and enhance thrombogenesis when stimulated by hypoxia (159). In addition, HIF-1-induced up-regulation of erythropoietin increases hematocrit, and blood viscosity and stimulates venous thrombosis (160).
Hypoxia and Oxidative Stress
Hypoxia also stimulates of NADPH oxidase to increase ROS. ROS cause lipid peroxidation, endothelial injury, increased vascular permeability, and disruption of BBB, which may further enhance the tissue edema (161). HIF-1 and ROS are involved in the pathogenesis, progression, and rupture of atherosclerotic plaques and arterial thrombosis (162).
Cardiovascular Effects of Hypoxia
Hypoxic cardiovascular injury results in lower cardiac output, which is further augmented by concomitant acidosis and elevated workload due to hypoxia-induced peripheral vasoconstriction (163). Hypoxia triggers cardiac arrhythmia, possibly due to the detrimental effects of anaerobic metabolism and ROS on the normal functions of ion channels. This association may highlight the role of antioxidants in preventing arrhythmia during hypoxic conditions (164).
Cardiovascular Complications
Risk factors for cardiovascular complications in SARS-CoV-2 infection that increase stroke risk are shown in Figures 1–6. The incidence of acute cardiac injury was reported 15% by a meta-analysis of patients with COVID-19 (165). Among 138 hospitalized patients with SARS-CoV-2 infection, cardiovascular complications such as acute cardiac injury (7%) and arrhythmia (16.7%) were more prevalent in patients who required ICU admission (166). Another study of 416 hospital-admitted patients with SARS-CoV-2 reported cardiac injury in 20% of cases. Similarly, this study reported a higher rate of complications, such as coagulation disorders and mortality among patients with cardiac injury than patients without cardiac injury (167). Cardiovascular complications can increase the risk of stroke. Cardioembolic stroke accounted for 22% of ischemic stroke among 32 patients with SARS-CoV-2 and 15.7% in patients included in a meta-analysis (11, 22). On the other hand, it should be noted that COVID-19 shares common risk factors with cardiovascular and cerebrovascular diseases. Consequently, the association between SARS-CoV-2 infection and cardiovascular/cerebrovascular complications may not be causative and may only represent potential comorbidities (168).
Myocardial injury, can be a direct or indirect consequence of ischemic and non-ischemic insults to the myocardium. Cardiac muscles and vessels are potential targets for direct SARS-CoV-2 infection since ACE2 receptors have been detected in cardiomyocytes, vascular endothelial cells, pericytes -important in sustaining endothelium function-, and smooth muscle cells (169, 170). Previously injured hearts are more susceptible to direct damage due to upregulated ACE2 (170, 171). Direct invasion is supported by endomyocardial biopsy of infected patients with detection of the SARS-CoV-2 genome in five patients and endomyocardial damage due to the infiltration of immune cells (172). Direct injury of coronary arteries could cause macrovascular dysfunction, acute coronary syndrome, and myocardial infarction (MI). The other possible mechanism for ischemic myocardial injury is coronary microvascular dysfunction (CMD). CMD has various pathogenic mechanisms and despite the significant prevalence has diagnostic and treatment pitfalls (173). Endothelial cells are implicated as key contributors to both macro- and microvascular dysfunction in COVID-19; therefore, evaluation of the endothelial biomarkers has been suggested for risk assessment of COVID-19 patients (174). In addition to endothelial cells, direct injury of pericytes has been associated with COVID-19 microvasculopathy (170, 175). Pericytes express ACE2 abundantly and are considered major targets for SARS-CoV-2 in the heart (176) which may cause non-obstructive MI (177). Histological study of human lung specimens proposed the pivotal role of pericyte loss in COVID-19-induced microvasculopathy (178). Endothelial barrier dysfunction (as seen in diabetes or hypertension) is necessary for the virus to reach the pericytes. Based on the COVID-19-pericyte hypothesis, SARS-CoV-2 infected pericytes induce adjacent endothelium to release vWF and result in a pro-coagulant state (179). This finding suggests pericytes as a new therapeutic target for SARS-CoV-2. Takutsubo syndrome, which has been reported in patients with SARS-CoV-2 infection (180), could be another consequence of CMD (181).
Indirect injury can occur due to severe lung infection, an imbalance between oxygen supply and consumption, hyperinflammation, endothelial damage, and coagulopathy. Subsequently, they can induce various cardiovascular complications involving arrhythmia, myocarditis, hypertension, vasculopathy, and inflammation-induced atherogenesis or plaque instability leading to thrombosis and MI (177, 182). Additionally, Ang II further exacerbates the inflammation and coagulation which may aggravate cardiovascular complications. Atherosclerosis, hypertension, myocardial fibrosis, impaired contractility, and increased risk of AF are among the possible complications induced by Ang II (183).
Arrhythmia may be a consequence of direct viral invasion and subsequent myocarditis, or other viral infection complications, such as anxiety, sympathetic overactivity, arrhythmogenic cytokines, hypoxia and acidosis, and electrolyte disturbance, and medications (184). New-onset AF has been reported even as the presenting manifestation of the COVID-19 without clinical or imaging findings indicating COVID-19 pneumonia (184, 185). It was previously reported that sepsis-induced AF occurs in 6–20% of patients, and it increases the risk for ischemic stroke and death during hospitalization (186). Although the sepsis-induced AF is often transient, there might be a higher risk for 5-year AF recurrence and in-hospital and long-term stroke occurrence (187).
Critical Illness
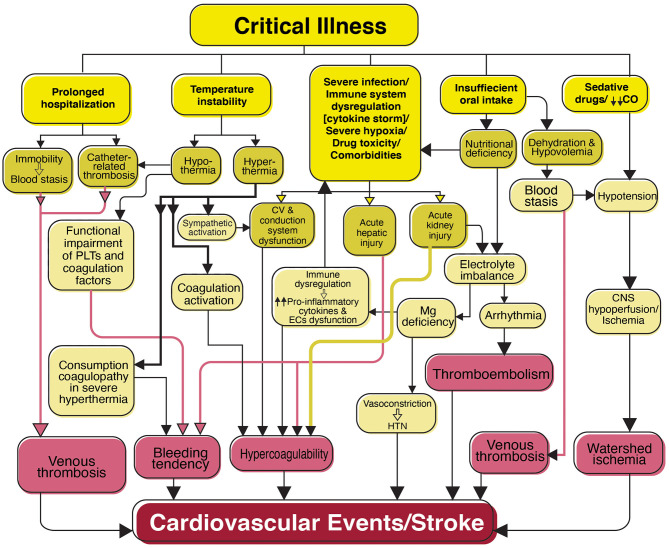
Critical illness and prolonged hospitalization raise the risk of strokes. Some of the factors associated with vascular events in patients with severe disease are presented in Figure 4.
Figure 4.
Flowchart diagram shows features of critical illness predisposing the patients with SARS-CoV-2 infection to cardiovascular events and stroke. Patients with a critical illness are mostly admitted to the intensive care unit (ICU) for prolonged periods. Clinical complications associated with critical illness including prolonged hospitalization, temperature instability, severe infection, and immune dysregulation, severe hypoxia, drug toxicity, comorbidities (e.g., diabetes mellitus, cardiovascular disease, and hypertension), insufficient oral intake, and sedative drugs are shown in association with their consequences that may result in cardiovascular events and stroke. PLTs, Platelets; CV, Cardiovascular; EC, Endothelial cells; Mg, Magnesium; HTN, Hypertension; CO, Cardiac output; CNS, Central nervous system.
Prolonged hospitalization causes immobility and increases the risk of venous thrombosis due to blood stasis and local hypoxia. Moreover, catheter-related thrombosis is a common complication of indwelling central venous catheters due to endothelial injury, blood stasis (188), and deep hypothermia (189).
Temperature instability in critical illness has been attributed to hemostatic disorders (190). Hyperthermia and decreased central blood volume have activated the sympathetic system and coagulation (showed by decreased activated partial thromboplastin time and elevated D-dimer) in the absence of concurrent sepsis, infection products, or evidence of endothelium injury (191). Although uncommon, there are reports of bleeding tendency due to consumption coagulopathy in severe hyperthermia (189). Despite the neuroprotective role of hypothermia in conditions such as brain ischemia (192), hypothermia-induced coagulopathy in ill patients may lead to hemorrhage by inhibiting platelet and coagulation factors (193).
Hepatic injury is one of the most common complications of COVID-19 and a predictor of disease severity and ICU admission (194). Hepatic injury was observed in the autopsy of COVID-19 patients (195). Pro-inflammatory cytokines, hypoxia, and drug-induced hepatotoxicity (194) in addition to direct viral invasion (196) are possible causes of liver injury in COVID-19. Considering the role of the liver in the coagulation system and drug metabolism, it is important to investigate the outcomes of COVID-19 liver injury, such as coagulation imbalance and risk for vascular events. As reported previously, other viruses such as cytomegalovirus, Epstein-Barr virus, and Hepatovirus A and B viruses have been related to thrombotic events in the setting of acute hepatitis (197). Although a causal relationship is not obvious, elevated liver tests are reported in patients who develop acute stroke in the course of SARS-CoV-2 infection (198, 199).
Up to 25% of critically ill patients with SARS-CoV-2 infection have been reported to develop acute kidney injury (AKI). Different mechanisms ranging from direct viral invasion to indirect effects such as RAS overactivation, hypovolemia, inflammation, hypercoagulability, and nephrotoxic drugs contribute to the development of AKI (7, 200). In addition to the risk of coagulation imbalance due to reduced medication excretion, AKI may also cause electrolyte disturbance and cardiac arrhythmia.
ICU patients with a critical illness are predisposed to nutritional deficiency due to insufficient oral intake and high metabolic demand. Electrolyte disturbance is one of the severe consequences of nutritional deficiency leading to arrhythmia and stroke. Magnesium has a significant role in immunomodulation via mediating many critical enzymatic reactions. By stimulating a pro-inflammatory state, increasing cytokine release, and endothelial dysfunction, hypomagnesemia may have an important role in COVID-19-associated coagulopathy (201). Magnesium supplementation has been used as an adjuvant treatment for COVID-19 patients and recommended for prevention and treatment, particularly in patients at risk for severe infection (202). Moreover, there is an association between hypomagnesemia and ischemic stroke due to vasoconstriction and hypertension (203).
Inadequate oral intake also leads to dehydration and hypovolemia that may predispose the CNS to hypoperfusion and ischemia, particularly in combination with cardiovascular dysfunction or administration of sedative medications that are frequently used among ICU patients. Hypovolemia also increases blood viscosity and stasis, predisposing patients to venous thrombosis.
Comorbidities/Risk Factors
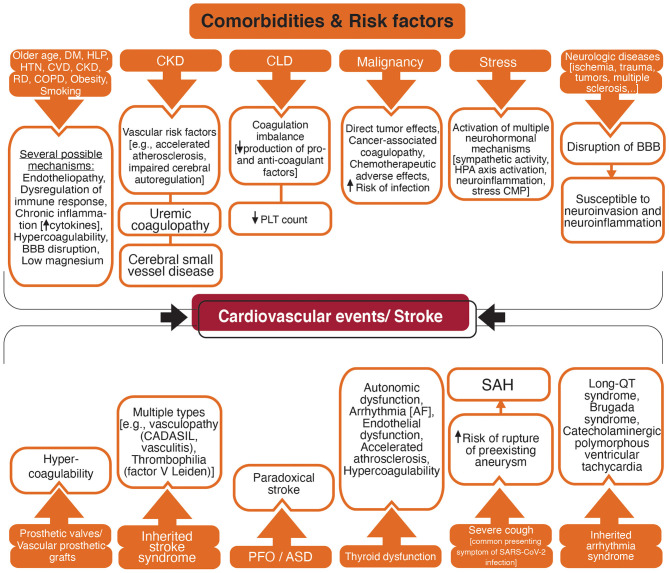
Figure 5 summarizes the possible comorbidities and risk factors associated with stroke in patients with COVID-19.
Figure 5.
Flowchart diagram shows acquired and inherited factors with a higher risk for vascular events and possible associated mechanisms. DM, Diabetes mellitus; HLP, Hyperlipidemia; HTN, Hypertension; CVD, Cardiovascular disease; CKD, Chronic Kidney disease; RD, Rheumatic disease; COPD, Chronic obstructive respiratory disease; BBB, blood-brain barrier; CLD, Chronic Liver Disease; PLT, Platelet; HPA, Hypothalamic-pituitary-adrenal; CMP, Cardiomyopathy; CADASIL, Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy; PFO, Patent foramen ovale; ASD, Atrial septal defect; AF, Atrial fibrillation; SAH, Subarachnoid hemorrhage; SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2.
Comorbidities With Proinflammatory and Procoagulant Phenotype
Pre-existing comorbidities such as older age, hyperlipidemia, diabetes, hypertension, cardiovascular disease, chronic kidney disease, chronic obstructive pulmonary disease (COPD), rheumatic diseases, malignancy, obesity, and smoking are related to the severe COVID-19 (204–206). These comorbidities are vascular risk factors with an increased risk for stroke in patients with SARS-CoV-2 infection (207). Endothelial dysfunction is a marker for atherosclerosis and is associated with vascular risk factors such as smoking, aging, hypercholesterolemia, hypertension, and hyperglycemia (208). Considering that endothelial cells are one of the main targets for SARS-CoV-2 (75), patients with pre-existing endothelial dysfunction are possibly more susceptible to endotheliopathy and vascular events. The chronic inflammatory state is a low-grade but long-term inflammation with elevated pro-inflammatory cytokines which occurs in conditions such as older age, stress, diabetes, hypertension, cardiovascular disease, rheumatic diseases, COPD, obesity, and smoking (209–211). A hypercoagulable state with elevated pro-inflammatory and pro-coagulant factors, impaired endogenous fibrinolytic system, and platelet hyperactivity is also related to these stroke risk factors such as older age (212), smoking (213), obesity (214), hypertension (215), and diabetes (216). Small vessel disease due to hypertension, diabetes, and hyperlipidemia may disrupt the BBB (217). In addition, comorbidities such as diabetes, hypertension, and hyperlipidemia are risk factors for hypomagnesemia (218, 219) which in turn elevates the risk of cardiovascular disease and stroke (203, 220–222).
Liver has an essential role in hemostasis by producing the coagulation and anti-coagulation factors, and the regulation of platelet synthesis by producing thrombopoietin (223, 224). Chronic liver disease can lead to coagulation imbalance and both thrombotic and bleeding disorders (223, 224).
Patients with chronic kidney disease (CKD) are at elevated risk for stroke, both hemorrhagic and ischemic, and poor outcome after stroke (225). Accelerated atherosclerosis, endothelial dysfunction, impaired cerebral autoregulation, anemia, uremic toxins, hyperhomocysteinemia, proteinuria, impaired calcium/phosphate metabolism have been suggested to increase the risk of stroke in patients with CKD (225–227). Cerebral small vessel disease that may be a marker of a multi-system endothelial disorder has been associated with the severity of renal impairment (228). CKD was suggested to have a predictive role in the presence and severity of cerebral small vessel disease (229).
Patients with different types of malignancy are vulnerable to both hemorrhagic and ischemic stroke (230). Stroke may result from direct effects of a primary or metastatic tumor in the CNS, or indirect effects of chemotherapeutic agents, higher susceptibility to infection, and cancer-associated coagulopathy (230, 231).
Patients with neurotrauma or pre-existing neurologic conditions such as multiple sclerosis and Alzheimer's disease may have BBB breakdown lasting for a longer time potentially increasing the risk for viral neuroinvasion and neuroinflammation (217, 232, 233).
Thyroid hormones influence the cardiovascular system and thyroid imbalance is associated with vascular diseases including stroke (234, 235). Supraventricular dysrhythmias including AF are associated with both overt and subclinical hyperthyroidism with elevated risk for cardioembolism (234). Hypothyroidism has a depressive effect on the cardiac conduction system that may be beneficial in patients who are at risk for cardiac ischemia and arrhythmia (236). However, hypothyroidism causes autonomic dysfunction with adverse cardiovascular effects (237) and increases the risk for QT prolongation and atrioventricular block (236). Hypothyroidism, even at subclinical levels, has been associated with vascular risk factors such as hypertension and hyperlipidemia that promote atherosclerosis (234, 238, 239). A hypercoagulable state, although has not been established, may occur in hyperthyroidism with elevated levels of fibrinogen and von Willebrand antigen (234, 239). Through various mechanisms, either elevation or reduction in thyroid hormone levels causes endothelial dysfunction, hypertension, impaired cardiac function (239). The significant prevalence of subclinical thyroid disease, 3–12% for subclinical hypothyroidism and 1–6% for subclinical hyperthyroidism (240), suggests assessing the thyroid function in patients with features of severe COVID-19.
Genetic Predisposition to Cardiovascular Disease and Stroke
Although SARS-CoV-2 infection makes patients with existing cardiometabolic diseases more vulnerable to have severe vascular consequences such as stroke, currently, there is no report of genome-wide association studies findings on stroke (ischemic stroke or hemorrhagic stroke) in COVID-19 patients. Whether individual genetic risk and polygenic theory for chronic cardiometabolic diseases and stroke play a role in the susceptibility to severe clinical manifestation in COVID-19 is still unknown.
The performance of polygenic risk scores (PRS) over the life course in several cardiometabolic diseases and neoplasms have been evaluated in a prospective setting and their value, when integrated with the known clinical risk factors and biomarkers, have been revealed (241). The cumulative risk for coronary artery disease, diabetes mellitus type 2, and AF was disproportionally increased after 40 years old when patients were stratified by categorical PRS from higher (>97.5%) to lower (<2.5%) scores. Genetic overlaps between stroke risk, early neurological changes, and some of the cardiovascular risk factors (diabetes and hypertension) have been identified (242). Because of the pleiotropy of genetic risk factors for both ischemic stroke and chronic diseases (243), we expect ischemic stroke will show a similar pattern. The cumulative disease rate for ischemic stroke will be disproportionally higher in the top PRS category. The polygenic contribution to early-onset was much higher than to late-onset in the same disease (241). Our retrospective study from the sensitivity analysis alternatively confirmed this disproportional increased PRS burden for ischemic stroke using younger cases vs. three tiers of older controls (from 59, 69 to 79) (243). Gene sets analyses highlighted the association of PRS with Gene Ontology terms (vascular endothelial growth factor, amyloid precursor protein, and atherosclerosis). All these pathways, as we reviewed here, could be potential targets of COVID-19. Future studies on this topic would help to lineate the potential capability of PRS in determining the genetic liability to the stroke or its subtypes as well as predicting the outcome in patients with COVID-19 infection. Whether patients having high PRS value for specific pathways may indicate the potential causal mechanism of ischemic stroke is still unknown and requires further investigation to validate. It is unclear to what extent PRS contributes to ischemic stroke in younger vs. older patient with COVID-19 infection.
Congenital Predisposition to Cardiovascular Disease and Stroke
Inherited stroke syndromes are among the disorders affecting the circulation and predisposing the patients to stroke. Cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is the most common hereditary stroke disorder. A patient with COVID-19 and CADASIL presented with multiple acute small vessel infarctions in subcortical areas that highlight the vulnerability of high-risk patients for stroke during COVID-19 infection (244). Inherited thrombophilias such as factor V Leiden and protein C deficiency increase vascular thrombosis risk (245). Also, patients with inherited arrhythmia syndrome such as congenital long QT syndrome, and Brugada syndrome might be at greater risk for COVID-19-related arrhythmia (246). In addition, the prevalence of patent foramen ovale is reported in about 25% of the general population and twice more in people with cryptogenic stroke (247). Patent foramen ovale associated stroke represents an important consideration when taking into account the high incidence of venous thrombosis among COVID-19 patients in the ICU ranging between 40% (248), and 69% (249).
Miscellaneous Risk Factors
Stress has been shown by a meta-analysis to be associated with a higher risk of cardiovascular mortality and stroke (250). This association is multifactorial and different neurohormonal mechanisms may be implicated. One mechanism might be the induction of toxic neuropeptides such as beta-amyloid that persists for a long time, activate the hypothalamic-pituitary-adrenal axis to produce a corticotropin-releasing hormone, increase neuroinflammation by activating mast cells (233, 250). Mast cells produce and respond to corticotropin-releasing hormone and can play a significant role in the cerebral pathologies in COVID-19 such as vascular dysfunction and BBB disruption (233). The incidence of stress cardiomyopathy (also known as Takotsubo syndrome) has been raised during the COVID-19 pandemic compared with the pre-pandemic period (251).
Cough is one of the most common presenting symptoms in COVID-19 (252). Though extremely rare, severe cough can suddenly increase intrathoracic pressure and cause a vascular rupture. A case of spontaneous spinal subarachnoid hemorrhage due to a severe cough that presented with a severe and sudden onset back pain and a headache was reported previously (253). A case of carotid artery dissection in a previously healthy adult patient was also reported during a course of severe cough due to pertussis (254).
Prosthetic valves and vascular prosthetic grafts are prone to thrombosis and subsequent vascular events. A patient with COVID-19 developed acute limb ischemia due to complete occlusion of the abdominal aortic prosthetic graft (255).
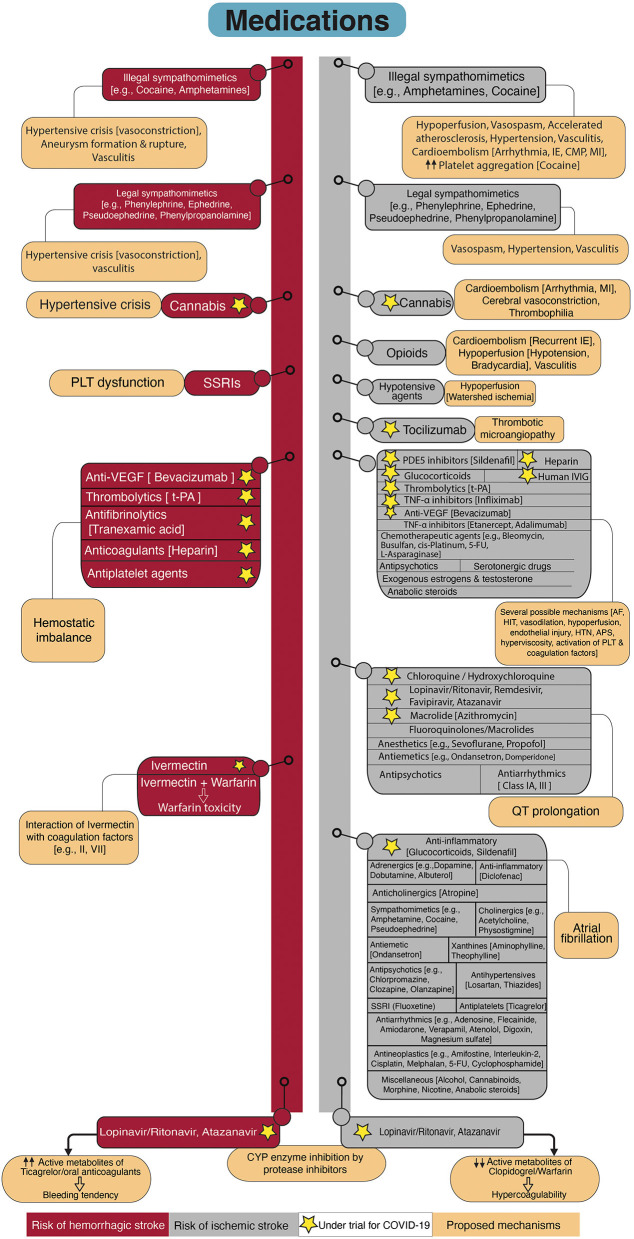
Medications
Figure 6 demonstrates the medications that have been associated with either ischemic or hemorrhagic stroke. Here, we briefly cover these medications by considering the presence (section Medications with Potential Benefit for COVID-19 Therapy) or absence (section Medications without Possible Effects on COVID-19) of potential benefit on COVID-19 therapy.
Figure 6.
Flowchart diagram shows drugs associated with stroke and possible underlying mechanisms. The left side of the diagram represents drugs with elevated risk for hemorrhagic stroke. The right side of the diagram shows drugs that increase the risk for ischemic stroke. Proposed mechanisms of stroke related to the drugs are provided attached to each drug. Some of the drugs are under investigation for COVID-19 which are marked by asterisks. SSRIs, Selective serotonin reuptake inhibitors; PLT, Platelet; VEGF, Vascular endothelial growth factor; t-PA, Tissue plasminogen activator; CYP, Cytochrome P450; MI, Myocardial infarction; IE, Infective endocarditis; CMP, Cardiomyopathy; PDE5, Phosphodiesterase type 5; IVIG, Intravenous immunoglobulin; TNF-α, tumor necrosis factor-alpha; 5-FU, 5-Fluorouracil; AF, Atrial Fibrillation; HIT, Heparin-induced thrombocytopenia; HTN, Hypertension; APS, Antiphospholipid antibody syndrome.
Medications With Potential Benefit for COVID-19 Therapy
Except for remdesivir, and a combination of baricitinib and remdesivir that have been recently approved for COVID-19 treatment (256, 257), the efficacy of other therapeutic agents in SARS-CoV-2 infected patients has not been approved. However, several medications are under investigation or being used off-label since the beginning of the pandemic (258). Some of these medications may be associated with serious complications such as stroke. Prolonged QT interval increases the risk of stroke independent of traditional risk factors (259). Administration of chloroquine and hydroxychloroquine (e.g., NCT04353336), favipiravir (e.g., NCT04359615, NCT04464408), lopinavir/ritonavir (e.g., NCT04372628, NCT04499677), atazanavir (e.g., NCT04468087, NCT04452565), remdesivir, and azithromycin (e.g., NCT04334382, NCT04359316), which are proposed as therapeutic options in SARS-CoV-2 infection, have the potential for QT interval prolongation and increasing the risk of arrhythmia (260–262). Some other medications from anesthetics, antipsychotics, antiemetics, and antiarrhythmics also have the QT prolongation potential. This complication is amplified by metabolism reduction (drug-induced, liver- and/or renal-induced), concomitant use of other medications with a potential for QT prolongation, electrolyte disturbance, and congenital long QT syndromes (263, 264).
Numerous drugs have the potential to inhibit the cytochrome P450 (CYP) system and increase the adverse effects of drugs that are inactivated by CYP enzymes. Azithromycin and antiviral agents such as lopinavir/ritonavir, atazanavir, remdesivir are inhibitors of CYP3A4 isoenzyme. The risk of QT prolongation is expected to be higher in combination use with other drugs that are metabolized by CYP3A4 such as chloroquine and hydroxychloroquine (265).
Antiretroviral protease inhibitors including lopinavir/ritonavir and atazanavir reduce viral replication and pro-inflammatory cytokines (266). Protease inhibitors are potent inhibitors of CYP, particularly CYP3A4, CYP2C9, and CYP2C19 (267). Protein inhibitors decrease the active metabolites of warfarin and increase the required warfarin maintenance dose (267), and change the active metabolites of antiplatelets (265, 268). For example, the antiplatelet function of clopidogrel was inadequate when administered in combination with antiretroviral agents (ritonavir and cobicistat, and atazanavir) (265, 268). Prasugrel remained effective despite a slight reduction in active metabolites (268). Thereby, when an antiplatelet is needed in combination with ritonavir, prasugrel is the best candidate. Conversely, ticagrelor is an activated medication and combined use with CYP inhibitors (such as ritonavir) increases its antiplatelet activity by 4-fold, which may induce bleeding (269). Combination therapy of ticagrelor with atazanavir is also restricted, atazanavir may increase the active metabolite of ticagrelor (265). The drug-drug interaction also exists between lopinavir/ritonavir and atazanavir, with direct oral anticoagulants such as rivaroxaban and apixaban (265). Patients infected with SARS-CoV-2 who were on direct oral anticoagulants showed a marked elevation in the plasma levels of anticoagulants after initiation of antiviral agents (270). Several antiarrhythmic drugs, such as amiodarone, lidocaine, and beta-blockers, are also metabolized by the hepatic CYP system. Close monitoring with measurement of serum drug concentration and electrocardiogram are recommended in a combinational regimen with antivirals (271).
Tumor necrosis factor alpha (TNF-α) inhibitors were proposed for the treatment of severe COVID-19 (272). From this family, Infliximab is being investigated for moderately or severely ill patients with COVID-19 (NCT04593940, NCT04425538). TNF-α inhibitors have been associated with the induction of antiphospholipid antibody syndrome and vasculitis (273, 274). These drugs are generally well-tolerated and the mentioned side effects are rare and reversible with drug cessation (274). However, arterial and venous thromboembolism have been reported in association with consumption of adalimumab, infliximab, and etanercept (275, 276). The observed thrombotic events with TNF-α inhibitors have been mainly related to the induction of antiphospholipid antibodies (277–279).
Tocilizumab is a monoclonal antibody that inhibits IL-6 receptors and is suggested as a therapeutic option for cytokine storm in COVID-19 pneumonia due to the prominent role of IL-6 in severe infection (280, 281) and is currently being investigated by several clinical trials (e.g., NCT04356937, NCT04445272). Although it may be beneficial in reducing the severity of stroke (282), there are rare cases of thrombotic microangiopathy involving multifocal cerebral lesions developed after administration of tocilizumab (283, 284). Tocilizumab was hypothesized as a trigger rather than a cause since patients had other risk factors for vascular events such as factor rheumatoid arthritis and factor V Leiden mutation.
Glucocorticoids are being used in the treatment of patients with severe COVID-19 (e.g., NCT04438980, NCT04395105, NCT04513184), whereas their use is associated with cardiovascular, cerebrovascular disease (285), and thromboembolic events with increased risk for AF (286).
Efficacy of high dose intravenous immunoglobulin (IVIG) has been observed in severe COVID-19 and has been suggested as a therapeutic option (287). IVIG is under evaluation by several clinical trials (e.g., NCT04432324, NCT04521309, NCT04480424). Previous evidence showed arterial and venous thrombosis after treatment with IVIG (288–291) even in young patients without risk factors for vascular diseases (290). Prothrombotic state in high dose IVIG therapy was attributed to hyperviscosity, vasospasm, platelet activation, and the presence of antiphospholipid antibodies and activated factor XI in some IVIG preparations (288–291).
Sildenafil, a cyclic guanosine monophosphate-specific phosphodiesterase type 5 inhibitor, is another candidate for the treatment of COVID-19 due to its role in inflammation reduction (NCT04489446, NCT04304313). Sildenafil was associated with a transient ischemic attack, ischemic stroke, and cerebral venous sinus thrombosis (292, 293). Endothelial dysfunction, hypoperfusion due to arterial dilation, and blood stasis due to vasodilation in patients with predisposing factors have been associated with vascular events in sildenafil users (292, 293). Rare cases of AF in patients with concomitant cardiac pathology have been related to sildenafil (294, 295).
Cannabis is used for its therapeutic effects in reducing chronic pain, nausea, and vomiting in patients under chemotherapy (296). Furthermore, it showed a beneficial role in animal models of ARDS by the reduction in pro-inflammatory cytokines, promotion of apoptosis in activated immune cells (297, 298), and upregulation of apelin (299), a peptide with protective role during ARDS (300). Due to the immunomodulatory effects of cannabis components, several clinical trials are registered to investigate its efficacy in the prevention and treatment of COVID-19 in addition to COVID-induced psychologic disorders such as anxiety and depression (NCT04467918, NCT03944447, NCT04731116, NCT04603781). On the other hand, several cases have been reported on the relationship between cannabis use and stroke and some of the cases were young and low risk for stroke (301, 302). However, the observed association may be related to concomitant smoking or the use of other unknown toxins in synthetic marijuana (302, 303). Cannabis exposure may be related to cerebral vasoconstriction, cardioembolism due to cardiac ischemia and arrhythmia, and thrombophilia (304, 305). Cannabis may rarely cause hemorrhagic stroke due to a sudden rise in blood pressure (305).
Heparin is the most widely used anticoagulant which can also be classified as an anti-inflammatory agent due to the inactivation of pro-inflammatory cytokines (306). In addition, the interaction of heparin with SARS-CoV-2 S1 spike protein supports the repurposing of heparin as an antiviral agent (307). Therefore, heparin has been added to the list of medications under investigation for COVID-19 (eg, NCT04530578, NCT04485429). Although heparin has a satisfactory safety profile and the risk of major bleeding events is low, there are some rare reports on severe and fatal bleeding such as intracranial hemorrhage in association with heparin administration (308, 309). Heparin-induced thrombocytopenia (HIT) is a relatively rare immune-mediated adverse reaction of heparin indicating by low platelet counts, as a result of anti-heparin-platelet factor 4 (PF4) antibodies, and arterial and venous thrombosis in almost 50–70% of patients with HIT (310). Thrombocytopenia and hypercoagulability are shared features betweenCOVID-19 coagulopathy and HIT. HIT is a life-threatening etiology for thrombocytopenia and hypercoagulability that appears to have a higher incidence during COVID-19. Among critically ill patients with COVID-19, the incidence of HIT was reported to be about 8%, which was 10-fold higher than control patients without COVID-19 (311). False-positive results of HIT during COVID-19 was also suggested by a study due to reasons such as the high prevalence of antiphospholipid syndrome and inaccurate laboratory assessment (312). There is a report of five patients with positive anti-heparin PF4 antibodies but confirmatory test for HIT returned positive for only one patient. The authors attributed the observation to the production of anti-heparin PF4 antibodies as a consequence of severe COVID-19 which was suggested by another study (313). To avoid overdiagnosis of HIT and unnecessary discontinuation of heparin, they recommended using the standard tests instead of antibody assessment alone (312).
Tissue plasminogen activator (t-PA) is under investigation for treating ARDS in COVID-19 (e.g., NCT04356833, NCT04357730). t-PA is the standard treatment for acute ischemic stroke that may adversely cause intracranial hemorrhage (314). Surprisingly, t-PA can cause a secondary hypercoagulability and increase the risk for thrombotic events (315).
Ivermectin is an anthelmintic agent with in vitro inhibition of SARS-CoV-2 replication (316). It is proposed as a treatment for COVID-19 and is under investigation (e.g., NCT04529525, NCT04425707). This medication was attributed to coagulopathy, possibly through interaction with coagulation factors (e.g., factors II and VII). This adverse reaction has been related to a case of warfarin toxicity after treatment with ivermectin (317).
Vascular endothelial growth factor (VEGF) antagonists are related to thrombotic and hemorrhagic side effects (318). VEGF-induced angiogenesis plays a significant role in acute lung injury of COVID-19 (319). For this reason, bevacizumab -an anti-VEGF agent- is under examination for the inhibition of angiogenesis in COVID-19 pneumonia (NCT04275414, NCT04344782, NCT04305106). Bevacizumab has been previously associated with venous and arterial thrombosis and hemorrhage, including stroke (320, 321).
Medications Without Possible Effects on COVID-19
In addition to medications under trials for SARS-CoV-2 infection, there are other medications with elevated risk for stroke. Prior routine consumption of these medications or use for acute conditions unrelated to COVID-19, such as trauma or surgery, might increase the risk of stroke which in addition to other stroke risk factors can lead to an attack in a patient with SARS-CoV-2 infection. Some of these medications, which are more widely used, are discussed here to remind the clinicians of other drugs with elevated risk of stroke particularly cryptogenic stroke.
AF can be stimulated by several mechanisms including medications. As discussed in earlier sections, patients with COVID-19 are prone to cardiovascular damage and new-onset arrhythmia as a consequence of comorbidities and infection. Drugs that have been associated with the induction of AF and the possible mechanisms are comprehensively reviewed by previous studies (322–324). Based on these studies, drug-induced AF is believed to have the following principal mechanisms: alterations in autonomic tone through either adrenergic or vagal stimulation, changing the atrial automaticity and conduction, direct cardiovascular toxicity such as coronary vasoconstriction/ischemia and electrolyte disturbances, local or systemic inflammation, oxidative stress, hyperthermia (322–324). A comprehensive discussion of all medications that are being associated with AF in addition to the possible mechanisms are not in the scope of this review; however, more commonly used medications are presented in Figure 6.
Some chemotherapeutic agents such as busulfan, bleomycin, cis-platinum, and fluorouracil increase the risk of thrombosis (325) and are also associated with cardiotoxicity (326). Angiogenesis inhibitors are also reported to be cardiotoxic with elevated risk for hypertension, arterial thromboembolism, and myocardial ischemia (327). L-asparaginase is an antineoplastic agent that causes a hypercoagulable state leading to thrombotic events. This drug causes reduced protein synthesis such as antithrombin III (328).
Exogenous estrogens, oral contraceptives, hormone replacement therapy, and estradiol produced from the conversion of exogenous testosterone are associated with the risk of venous and arterial thrombosis mainly through induction of hypercoagulability (329, 330). Tamoxifen has also an estrogenic effect and may be related to both venous thromboembolism and stroke (331).
Supraphysiologic doses of anabolic steroids are reported to cause ischemic stroke and myocardial infarction mostly in young patients with unremarkable vascular risk factors (332–334). A thrombogenic and an atherogenic state have been proposed as a result of AF, increased erythropoietin and hematocrit, increased thrombin and fibrin formation and platelet aggregation, vascular spasm, hypertension, insulin resistance, and dyslipidemia (332, 335, 336).
Antipsychotics are associated with increased risk for both stroke and MI possibly related to platelet aggregation, metabolic effects, and obesity (337). Serotonin is a vasoactive amine with both vasoconstrictive and vasodilative effects on cerebral arteries of different sizes (325). Selective serotonin reuptake inhibitor (SSRI) antidepressants and new antipsychotics such as clozapine and olanzapine have been reported to cause cardiodepression and arrhythmia (338). Based on a meta-analysis, patients with a one-time stroke under antidepressant therapy (including SSRI and tricyclic antidepressants) may be at elevated risk for stroke recurrence, particularly ischemic type. The risk was highest in patients under therapy with multiple antidepressants (339). SSRI use has also been shown to cause an elevated risk of ischemic stroke in patients 65 years and older (340). Platelets release serotonin at the site of endothelial injury to promote platelet aggregation (341). SSRI may decrease serotonin reuptake by platelets and cause platelet dysfunction and bleeding. Several studies have supported the increased risk of bleeding in patients with SSRI use (342, 343). According to a meta-analysis, SSRI is associated with a slightly increased risk of hemorrhagic cerebral events which is potentiated with concomitant use with oral anticoagulants (344).
Opioids, although rarely reported, are accused of being associated with ischemic stroke. Possible mechanisms might be cardioembolism due to recurrent infective endocarditis, hypotension, and bradycardia leading to global hypoperfusion and ischemia, and vasculitis (345).
Some of the illicit drugs including amphetamines and cocaine cause elevated incidence and mortality of stroke by sympathomimetic activity (346). Vascular spasm, an acute rise in blood pressure, aneurysm formation and rupture, and vasculitis are the reasons by which sympathomimetics may stimulate a stroke (346). Chronic use of these illegal sympathomimetics stimulates ischemic stroke. The proposed mechanisms are vasospasm and tissue hypoperfusion, accelerated atherosclerosis, increased platelet aggregation, vasculitis and cardioembolism due to infective endocarditis, arrhythmia, cardiomyopathy and myocardial infarction (305, 347). Sympathomimetic compounds in over-the-counter cold medications and appetite suppressants such as phenylpropanolamine and pseudoephedrine are also increase the risk of hemorrhagic and ischemic stroke and myocardial infarction (348, 349). Vascular events are more probable in chronic drug consumption or in higher doses than the recommended dose and the proposed mechanisms are related to sympathomimetic effects such as vasospasm and hypertension (348, 349).
Discussion and Future Perspective
Patients with SARS-CoV-2 infection need prevention for vascular events, especially during hospitalization. According to the International Society of Thrombosis and Hemostasis, all hospitalized patients infected with SARS-CoV-2 benefit from coagulation monitoring with D-dimer level, prothrombin time, platelet count, and fibrinogen. Prophylactic low molecular weight heparin therapy is also beneficial (350). Considering the hypercoagulability in COVID-19, higher doses of anticoagulants with extended duration of anticoagulation may be needed, and laboratory and clinical follow-ups should occur in shorter intervals. Notably, a high incidence of arterial and venous thrombosis occurs despite thromboprophylaxis (89, 249). Among a cohort of infected patients who were discharged without anticoagulants, 2.5% presented with a thrombotic event post-discharge (mean of 30 days), including one ischemic stroke at day 40 post-discharge (351). However, therapeutic or prophylactic doses of anticoagulation may result in severe and fatal intracranial hemorrhage in SARS-CoV-2 infected patients (89, 352), possibly due to endotheliopathy and vascular fragility. Based on the current literature, it cannot be anticipated for how long COVID-19 survivors would be prone to the elevated risk of stroke. Previous experiences with other pathologies may provide an insight into the duration of the preventive strategies. Follow up of hospitalized pneumonia patients revealed an increased risk of cerebro- and cardiovascular diseases, even up to 10 years. After adjustment for cardiovascular risk factors, the risk was highest in the first month, had been progressively declined in the first year, and remained as high as 1.5-fold of the risk in the controls in the following years (353). Similarly, hospitalization for sepsis increased the 1-year risk of stroke, particularly in younger patients (354). In the influenza-like illnesses, the higher odds of ischemic stroke was significant up to 60 days (355). Study on twenty-five SARS-CoV-1 survivors after 12 years showed a significant disruption in the lipid metabolism, cardiovascular abnormalities, and altered glucose metabolism, compared to healthy controls (356).
Finally, the role of antiplatelet agents in the secondary prevention of stroke is clear (357). Patients with SARS-CoV-2 infection may further benefit from antiplatelets due to the role of platelets in the coagulopathy related to severe COVID-19. On the other hand, platelets are essential components of defense against viruses and antiplatelets may inhibit the immune system in the early stages of viral infection complicating antiplatelet therapy. In this respect, previous studies have shown the lack of cytotoxic T cell-mediated response and inhibition of viral clearance in platelet-depleted animals (358) and also in animals treated with dual aspirin/clopidogrel (359). Due to the lack of clear evidence, it is most reasonable to personalize patient care. While waiting for the results of standard trials for COVID-19 treatment, uncontrolled administration of several drugs may increase the risk for adverse reactions such as stroke.
In summary, the present narrative review highlighted the potential pathways that may be associated with CNS invasion by SARS-CoV-2. We pictured the potential etiopathogenic mechanisms that may account for the causative association between COVID-19 and stroke. Further research is required to assist us in understanding the full spectrum of SARS-CoV-2 infection in triggering acute cardio- and cerebrovascular events.
Author Contributions
SASN, SS, VA, and RZ contributed to the conception and design of the study. SASN, SS, EK, IF, FKh, MS, FKo, and SA performed the literature review, wrote the first draft of the manuscript, and prepared the figures. GT, JL, VA, DW, and RZ wrote sections of the manuscript and performed the initial revision. All authors contributed to the final revision of the manuscript and figures and read and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Jafarzadeh A, Chauhan P, Saha B, Jafarzadeh S, Nemati M. Contribution of monocytes and macrophages to the local tissue inflammation and cytokine storm in COVID-19: lessons from SARS and MERS, and potential therapeutic interventions. Life Sci. (2020) 257:118102. 10.1016/j.lfs.2020.118102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McFee RB. SARS 2 human coronavirus (COVID−19, SARS CoV2). Dis Mon. (2020) 66:101063. 10.1016/j.disamonth.2020.101063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. (2020) 77:1–9. 10.1001/jamaneurol.2020.1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nepal G, Rehrig JH, Shrestha GS, Shing YK, Yadav JK, Ojha R, et al. Neurological manifestations of COVID-19: a systematic review. Crit Care. (2020) 24:421. 10.1186/s13054-020-03121-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. (2020) 94:55–8. 10.1016/j.ijid.2020.03.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paniz-Mondolfi A, Bryce C, Grimes Z, Gordon RE, Reidy J, Lednicky J, et al. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol. (2020) 92:699–702. 10.1002/jmv.25915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Puelles VG, Lütgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, et al. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. (2020) 383:590–2. 10.1056/NEJMc2011400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Solomon IH, Normandin E, Bhattacharyya S, Mukerji SS, Keller K, Ali AS, et al. Neuropathological features of Covid-19. N Engl J Med. (2020) 383:989–92. 10.1056/NEJMc2019373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Belani P, Schefflein J, Kihira S, Rigney B, Delman B, Mahmoudi K, et al. COVID-19 is an independent risk factor for acute ischemic stroke. Am J Neuroradiol. (2020) 41:1361–4. 10.3174/ajnr.A6650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shahjouei S, Naderi S, Li J, Khan A, Chaudhary D, Farahmand G, et al. Risk of stroke in hospitalized SARS-CoV-2 infected patients: a multinational study. EBioMedicine. (2020) 59:102939. 10.1016/j.ebiom.2020.102939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee KW, Yusof Khan AHK, Ching SM, Chia PK, Loh WC, Abdul Rashid AM, et al. Stroke and novel coronavirus infection in humans: a systematic review and meta-analysis. Front Neurol. (2020) 11:1196. 10.3389/fneur.2020.579070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamakawa M, Kuno T, Mikami T, Takagi H, Gronseth G. Clinical characteristics of stroke with COVID-19: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. (2020) 29:105288. 10.1016/j.jstrokecerebrovasdis.2020.105288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsivgoulis G, Katsanos AH, Ornello R, Sacco S. Ischemic stroke epidemiology during the COVID-19 pandemic: navigating uncharted waters with changing tides. Stroke. (2020) 51:1924–6. 10.1161/STROKEAHA.120.030791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katsanos AH, Palaiodimou L, Zand R, Yaghi S, Kamel H, Navi BB, et al. The impact of SARS-CoV-2 on stroke epidemiology and care: a meta-analysis. Ann Neurol. (2020) 89:380–8. 10.1002/ana.25967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. (2017) 135:e146–603. 10.1161/CIR.0000000000000491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dula AN, Gealogo Brown G, Aggarwal A, Clark KL. Decrease in stroke diagnoses during the COVID-19 pandemic: where did all our stroke patients go? JMIR Aging. (2020) 3:e21608. 10.2196/21608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, et al. Risk of ischemic stroke in patients with Covid-19 versus patients with influenza. JAMA Neurol. (2020) 77:1–7. 10.1101/2020.05.18.20105494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu J, Xiao W, Liang X, Zhang P, Shi L, Wang Y, et al. The association of cerebrovascular disease with adverse outcomes in COVID-19 patients: a meta-analysis based on adjusted effect estimates. J Stroke Cerebrovasc Dis. (2020) 29:105283. 10.1016/j.jstrokecerebrovasdis.2020.105283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashrafi F, Zali A, Ommi D, Salari M, Fatemi A, Arab-Ahmadi M, et al. COVID-19-related strokes in adults below 55 years of age: a case series. Neurol Sci. (2020) 41:1985–9. 10.1007/s10072-020-04521-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. (2020) 382:e60. 10.1056/NEJMc2009787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.John S, Kesav P, Mifsud VA, Piechowski-Jozwiak B, Dibu J, Bayrlee A, et al. Characteristics of large-vessel occlusion associated with COVID-19 and ischemic stroke. Am J Neuroradiol. (2020) 41:2263–8. 10.3174/ajnr.A6799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, et al. SARS2-CoV-2 and stroke in a New York healthcare system. Stroke. (2020) 51:2002–11. 10.1161/STROKEAHA.120.030335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beyrouti R, Adams ME, Benjamin L, Cohen H, Farmer SF, Goh YY, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatr. (2020) 91:889–91. 10.1136/jnnp-2020-323586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Majidi S, Fifi J, Ladner T, Lara-Reyna J, Yaeger K, Yim B, et al. Emergent large vessel occlusion stroke during New York City's COVID-19 outbreak: clinical characteristics and paraclinical findings. Stroke. (2020) 51:2656–63. 10.1161/STROKEAHA.120.030397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fara MG, Stein LK, Skliut M, Morgello S, Fifi JT, Dhamoon MS. Macrothrombosis and stroke in patients with mild Covid-19 infection. J Thromb Haemost. (2020) 18:2031–3. 10.1111/jth.14938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, et al. Air, surface environmental, and personal protective equipment contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. (2020) 323:1610–2. 10.1001/jama.2020.3227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, et al. Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. (2020) 69:1010–8. 10.1136/gutjnl-2020-320953 [DOI] [Google Scholar]
- 28.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. (2020) 181:271–80.e8. 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang K, Chen W, Zhou Y-S, Lian J-Q, Zhang Z, Du P, et al. SARS-CoV-2 invades host cells via a novel route: CD147-spike protein. bioRxiv [Internet]. (2020) 2020.03.14.988345. Available online at: https://www.biorxiv.org/content/10.1101/2020.03.14.988345v1
- 30.Walls AC, Park Y-J, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. (2020) 181:281–92.e6. 10.1016/j.cell.2020.02.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coutard B, Valle C, de Lamballerie X, Canard B, Seidah NG, Decroly E. The spike glycoprotein of the new coronavirus 2019-nCoV contains a furin-like cleavage site absent in CoV of the same clade. Antiviral Res. (2020) 176:104742. 10.1016/j.antiviral.2020.104742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Millet JK, Whittaker GR. Host cell proteases: critical determinants of coronavirus tropism and pathogenesis. Virus Res. (2015) 202:120–34. 10.1016/j.virusres.2014.11.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matusiak M, Schürch CM. Expression of SARS-CoV-2 entry receptors in the respiratory tract of healthy individuals, smokers and asthmatics. Respir Res. (2020) 21:252. 10.1186/s12931-020-01521-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cantuti-Castelvetri L, Ojha R, Pedro LD, Djannatian M, Franz J, Kuivanen S, et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. (2020) 370:856–60. 10.1126/science.abd2985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daly JL, Simonetti B, Antón-Plágaro C, Kavanagh Williamson M, Shoemark DK, Simón-Gracia L, et al. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science. (2020) 370:861–5. 10.1126/science.abd3072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Louveau A, Harris TH, Kipnis J. Revisiting the mechanisms of CNS immune privilege. Trends Immunol. (2015) 36:569–77. 10.1016/j.it.2015.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kennedy RH, Silver R. Neuroimmune signaling: cytokines and the CNS. In: Pfaff DW, Volkow ND, editors. Neuroscience in the 21st Century. New York, NY: Springer New York; (2016). p. 1–41. 10.1007/978-1-4614-6434-1_174-1 [DOI] [Google Scholar]
- 38.Qiao J, Li W, Bao J, Peng Q, Wen D, Wang J, et al. The expression of SARS-CoV-2 receptor ACE2 and CD147, and protease TMPRSS2 in human and mouse brain cells and mouse brain tissues. Biochem Biophys Res Commun. (2020) 533:867–71. 10.1016/j.bbrc.2020.09.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davies J, Randeva HS, Chatha K, Hall M, Spandidos DA, Karteris E, et al. Neuropilin-1 as a new potential SARS-CoV-2 infection mediator implicated in the neurologic features and central nervous system involvement of COVID-19. Mol Med Rep. (2020) 22:4221–6. 10.3892/mmr.2020.11510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kumar A, Pareek V, Prasoon P, Faiq MA, Kumar P, Kumari C, et al. Possible routes of SARS-CoV-2 invasion in brain: in context of neurological symptoms in COVID-19 patients. J Neurosci Res. (2020) 98:2376–83. 10.1002/jnr.24717 [DOI] [PubMed] [Google Scholar]
- 41.Li Y-C, Bai W-Z, Hirano N, Hayashida T, Taniguchi T, Sugita Y, et al. Neurotropic virus tracing suggests a membranous-coating-mediated mechanism for transsynaptic communication. J Comp Neurol. (2013) 521:203–12. 10.1002/cne.23171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Diefenbach RJ, Miranda-Saksena M, Douglas MW, Cunningham AL. Transport and egress of herpes simplex virus in neurons. Rev Med Virol. (2008) 18:35–51. 10.1002/rmv.560 [DOI] [PubMed] [Google Scholar]
- 43.Brann DH, Tsukahara T, Weinreb C, Lipovsek M, Van den Berge K, Gong B, et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying COVID-19-associated anosmia. Sci Adv. (2020) 6:eabc5801. 10.1126/sciadv.abc5801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ueha R, Kondo K, Kagoya R, Shichino S, Ueha S, Yamasoba T. Background mechanisms of olfactory dysfunction in COVID-19: expression of ACE2, TMPRSS2, and Furin in the nose and olfactory bulb in human and mice. bioRxiv [Internet]. (2020) 2020.05.15.097352. Available online at: https://www.biorxiv.org/content/10.1101/2020.05.15.097352v1
- 45.Butowt R, von Bartheld CS. Anosmia in COVID-19: Underlying Mechanisms and Assessment of an Olfactory Route to Brain Infection. Neuroscientist [Internet]. (2020). 10.1177/1073858420956905. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. (2008) 82:7264–75. 10.1128/JVI.00737-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bulfamante G, Chiumello D, Canevini MP, Priori A, Mazzanti M, Centanni S, et al. First ultrastructural autoptic findings of SARS-Cov-2 in olfactory pathways and brainstem. Minerva Anestesiol. (2020) 86:678–9. 10.23736/S0375-9393.20.14772-2 [DOI] [PubMed] [Google Scholar]
- 48.Coolen T, Lolli V, Sadeghi N, Rovaï A, Trotta N, Taccone FS, et al. Early postmortem brain MRI findings in COVID-19 non-survivors. Neurology. (2020) 95:e2016–27. 10.1212/WNL.0000000000010116 [DOI] [PubMed] [Google Scholar]
- 49.Tsivgoulis G, Fragkou PC, Lachanis S, Palaiodimou L, Lambadiari V, Papathanasiou M, et al. Olfactory bulb and mucosa abnormalities in persistent COVID-19-induced anosmia: a magnetic resonance imaging study. Eur J Neurol. (2021) 28:e6–8. 10.1111/ene.14537 [DOI] [PubMed] [Google Scholar]
- 50.Perlman S, Jacobsen G, Afifi A. Spread of a neurotropic murine coronavirus into the CNS via the trigeminal and olfactory nerves. Virology. (1989) 170:556–60. 10.1016/0042-6822(89)90446-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bolay H, Gül A, Baykan B. COVID-19 is a real headache! Headache. (2020) 60:1415–21. 10.1111/head.13856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ma D, Chen C-B, Jhanji V, Xu C, Yuan X-L, Liang J-J, et al. Expression of SARS-CoV-2 receptor ACE2 and TMPRSS2 in human primary conjunctival and pterygium cell lines and in mouse cornea. Eye. (2020) 34:1212–9. 10.1038/s41433-020-0939-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019. (COVID-19) in Hubei Province, China. JAMA Ophthalmol. (2020) 138:575–8. 10.1001/jamaophthalmol.2020.1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. (2020) 92:589–94. 10.1002/jmv.25725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. (2020) 277:2251–61. 10.1007/s00405-020-06024-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cooper KW, Brann DH, Farruggia MC, Bhutani S, Pellegrino R, Tsukahara T, et al. COVID-19 and the chemical senses: supporting players take center stage. Neuron. (2020) 107:219–33. 10.1016/j.neuron.2020.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Matsuda K, Park CH, Sunden Y, Kimura T, Ochiai K, Kida H, et al. The vagus nerve is one route of transneural invasion for intranasally inoculated influenza a virus in mice. Vet Pathol. (2004) 41:101–7. 10.1354/vp.41-2-101 [DOI] [PubMed] [Google Scholar]
- 58.Li Z, Liu T, Yang N, Han D, Mi X, Li Y, et al. Neurological manifestations of patients with COVID-19: potential routes of SARS-CoV-2 neuroinvasion from the periphery to the brain. Front Med. (2020) 14:533–41. 10.1007/s11684-020-0786-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Varga Z, Flammer A, Steiger P, Haberecker M, Andermatt R, Zinkernagel A, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. (2020) 395:1417–8. 10.1016/S0140-6736(20)30937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Desforges M, Le Coupanec A, Stodola JK, Meessen-Pinard M, Talbot PJ. Human coronaviruses: viral and cellular factors involved in neuroinvasiveness and neuropathogenesis. Virus Res. (2014) 194:145–58. 10.1016/j.virusres.2014.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, Peske JD, et al. Structural and functional features of central nervous system lymphatic vessels. Nature. (2015) 523:337–41. 10.1038/nature14432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li F, Wang Y, Yu L, Cao S, Wang K, Yuan J, et al. Viral infection of the central nervous system and neuroinflammation precede blood-brain barrier disruption during japanese encephalitis virus infection. J Virol. (2015) 89:5602–14. 10.1128/JVI.00143-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Naoki K, Sandro S, Yutaro K, Deepthi MS, Visesha K, Lea G, et al. Flow-mediated susceptibility and molecular response of cerebral endothelia to SARS-CoV-2 infection. Stroke. (2021) 52:260–70. 10.1161/STROKEAHA.120.032764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Buzhdygan TP, DeOre BJ, Baldwin-Leclair A, Bullock TA, McGary HM, Khan JA, et al. The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in-vitro models of the human blood–brain barrier. Neurobiol Dis. (2020) 146:105131. 10.1016/j.nbd.2020.105131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J Infect. 2020/04/10. (2020) 80:607–13. 10.1016/j.jinf.2020.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jose RJ, Manuel A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. (2020) 8:e46–7. 10.1016/S2213-2600(20)30216-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kritas SK, Ronconi G, Caraffa A, Gallenga CE, Ross R, Conti P. Mast cells contribute to coronavirus-induced inflammation: new anti-inflammatory strategy. J Biol Regul Homeost Agents. (2020) 34:9–14. 10.23812/20-Editorial-Kritas [DOI] [PubMed] [Google Scholar]
- 68.Afrin LB, Weinstock LB, Molderings GJ. Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome. Int J Infect Dis. (2020) 100:327–32. 10.1016/j.ijid.2020.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gu J, Gong E, Zhang B, Zheng J, Gao Z, Zhong Y, et al. Multiple organ infection and the pathogenesis of SARS. J Exp Med. (2005) 202:415–24. 10.1084/jem.20050828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kim W-K, Corey S, Alvarez X, Williams K. Monocyte/macrophage traffic in HIV and SIV encephalitis. J Leukoc Biol. (2003) 74:650–6. 10.1189/jlb.0503207 [DOI] [PubMed] [Google Scholar]
- 71.Fry M, Ferguson AV. The sensory circumventricular organs: brain targets for circulating signals controlling ingestive behavior. Physiol Behav. (2007) 91:413–23. 10.1016/j.physbeh.2007.04.003 [DOI] [PubMed] [Google Scholar]
- 72.Bentivoglio M, Kristensson K, Rottenberg ME. Circumventricular organs and parasite neurotropism: neglected gates to the brain? Front Immunol. (2018) 9:2877. 10.3389/fimmu.2018.02877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schouten M, Wiersinga WJ, Levi M, van der Poll T. Inflammation, endothelium, and coagulation in sepsis. J Leukoc Biol. (2008) 83:536–45. 10.1189/jlb.0607373 [DOI] [PubMed] [Google Scholar]
- 74.McCuskey RS, Urbaschek R, Urbaschek B. The microcirculation during endotoxemia. Cardiovasc Res. (1996) 32:752–63. 10.1016/S0008-6363(96)00113-7 [DOI] [PubMed] [Google Scholar]
- 75.Goshua G, Pine A, Meizlish M, Chang CH, Zhang H, Bahel P, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. (2020) 7:e575–82. 10.1016/S2352-3026(20)30216-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nagel MA. Varicella zoster virus vasculopathy: clinical features and pathogenesis. J Neurovirol. (2014) 20:157–63. 10.1007/s13365-013-0183-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ding Y, Wang H, Shen H, Li Z, Geng J, Han H, et al. The clinical pathology of severe acute respiratory syndrome (SARS): a report from China. J Pathol. (2003) 200:282–9. 10.1002/path.1440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vaschetto R, Cena T, Sainaghi PP, Meneghetti G, Bazzano S, Vecchio D, et al. Cerebral nervous system vasculitis in a Covid-19 patient with pneumonia. J Clin Neurosci. (2020) 79:71–3. 10.1016/j.jocn.2020.07.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Oliveira R, de MC, de Santos DH, Olivetti BC, Takahashi JT. Bilateral trochlear nerve palsy due to cerebral vasculitis related to COVID-19 infection. Arq Neuropsiquiatr. (2020) 78:385–6. 10.1590/0004-282x20200052 [DOI] [PubMed] [Google Scholar]
- 80.Hanafi R, Roger P-A, Perin B, Kuchcinski G, Deleval N, Dallery F, et al. COVID-19 neurologic complication with CNS vasculitis-like pattern. Am J Neuroradiol. (2020) 41:1384–7. 10.3174/ajnr.A6651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Assinger A. Platelets and infection - an emerging role of platelets in viral infection. Front Immunol. (2014) 5:649. 10.3389/fimmu.2014.00649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Xu P, Zhou Q, Xu J. Mechanism of thrombocytopenia in COVID-19 patients. Ann Hematol. (2020) 99:1205–8. 10.1007/s00277-020-04019-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Qu R, Ling Y, Zhang Y, Wei L, Chen X, Li X, et al. Platelet-to-lymphocyte ratio is associated with prognosis in patients with coronavirus disease-19. J Med Virol. (2020) 92:1533–41. 10.1002/jmv.25767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019. (COVID-19) infections: a meta-analysis. Clin Chim Acta. (2020) 506:145–8. 10.1016/j.cca.2020.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kaushansky K. The molecular mechanisms that control thrombopoiesis. J Clin Invest. (2005) 115:3339–47. 10.1172/JCI26674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yin S, Huang M, Li D, Tang N. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolysis [Internet]. (2020) 1–4. 10.1007/s11239-020-02105-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Crowley Jj, Hannigan M, Daly K. Reactive thrombocytosis and stroke following cardiopulmonary bypass surgery: case report on three patients. Eur Heart J. (1994) 15:1144–6. 10.1093/oxfordjournals.eurheartj.a060642 [DOI] [PubMed] [Google Scholar]
- 88.Ho KM, Yip CB, Duff O. Reactive thrombocytosis and risk of subsequent venous thromboembolism: a cohort study. J Thromb Haemost. (2012). 10:1768–74. 10.1111/j.1538-7836.2012.04846.x [DOI] [PubMed] [Google Scholar]
- 89.Al-Samkari H, Karp Leaf RS, Dzik WH, Carlson JCT, Fogerty AE, Waheed A, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. (2020) 136:489–500. 10.1182/blood.2020006520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dong H, Zhang X, Qian Y. Mast cells and neuroinflammation. Med Sci Monit Basic Res. (2014) 20:200–6. 10.12659/MSMBR.893093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tran H, Mittal A, Sagi V, Luk K, Nguyen A, Gupta M, et al. Mast cells induce blood brain barrier damage in SCD by causing endoplasmic reticulum stress in the endothelium. Front Cell Neurosci. (2019) 13:56. 10.3389/fncel.2019.00056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Parrella E, Porrini V, Benarese M, Pizzi M. The role of mast cells in stroke. Cells. (2019) 8:437. 10.3390/cells8050437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Strbian D, Kovanen PT, Karjalainen-Lindsberg M-L, Tatlisumak T, Lindsberg PJ. An emerging role of mast cells in cerebral ischemia and hemorrhage. Ann Med. (2009) 41:438–50. 10.1080/07853890902887303 [DOI] [PubMed] [Google Scholar]
- 94.Roncati L, Ligabue G, Fabbiani L, Malagoli C, Gallo G, Lusenti B, et al. Type 3 hypersensitivity in COVID-19 vasculitis. Clin Immunol. (2020) 217:108487. 10.1016/j.clim.2020.108487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ishibashi R, Aoki T, Nishimura M, Hashimoto N, Miyamoto S. Contribution of mast cells to cerebral aneurysm formation. Curr Neurovasc Res. (2010) 7:113–24. 10.2174/156720210791184916 [DOI] [PubMed] [Google Scholar]
- 96.Hasan D, Chalouhi N, Jabbour P, Hashimoto T. Macrophage imbalance (M1 vs. M2) and upregulation of mast cells in wall of ruptured human cerebral aneurysms: preliminary results. J Neuroinflammation. (2012) 9:222. 10.1186/1742-2094-9-222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Signorelli F, Sela S, Gesualdo L, Chevrel S, Tollet F, Pailler-Mattei C, et al. Hemodynamic stress, inflammation, and intracranial aneurysm development and rupture: a systematic review. World Neurosurg. (2018) 115:234–44. 10.1016/j.wneu.2018.04.143 [DOI] [PubMed] [Google Scholar]
- 98.Musher DM, Abers MS, Corrales-Medina VF. Acute infection and myocardial infarction. N Engl J Med. (2019) 380:171–6. 10.1056/NEJMra1808137 [DOI] [PubMed] [Google Scholar]
- 99.Hansson GK, Libby P, Tabas I. Inflammation and plaque vulnerability. J Intern Med. (2015) 278:483–93. 10.1111/joim.12406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sheth AR, Grewal US, Patel HP, Thakkar S, Garikipati S, Gaddam J, et al. Possible mechanisms responsible for acute coronary events in COVID-19. Med Hypotheses. (2020) 143:110125. 10.1016/j.mehy.2020.110125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Iba T, Levy JH, Connors JM, Warkentin TE, Thachil J, Levi M. The unique characteristics of COVID-19 coagulopathy. Crit Care. (2020) 24:360. 10.1186/s13054-020-03077-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bernardo A, Ball C, Nolasco L, Moake J, Dong J. Effects of inflammatory cytokines on the release and cleavage of the endothelial cell-derived ultralarge von Willebrand factor multimers under flow. Blood. (2004) 104:100–6. 10.1182/blood-2004-01-0107 [DOI] [PubMed] [Google Scholar]
- 103.Levi M, Thachil J, Iba T, Levy J. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. (2020) 7:e438–40. 10.1016/S2352-3026(20)30145-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wright FL, Vogler TO, Moore EE, Moore HB, Wohlauer MV, Urban S, et al. Fibrinolysis shutdown correlation with thromboembolic events in severe COVID-19 infection. J Am Coll Surg. (2020) 231:193–203.e1. 10.1016/j.jamcollsurg.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Seheult JN, Seshadri A, Neal MD. Fibrinolysis shutdown and thrombosis in severe COVID-19. J Am Coll Surg. (2020) 231:203–4. 10.1016/j.jamcollsurg.2020.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kwaan HC. Role of plasma proteins in whole blood viscosity: a brief clinical review. Clin Hemorheol Microcirc. (2010) 44:167–76. 10.3233/CH-2010-1271 [DOI] [PubMed] [Google Scholar]
- 107.Rogers AP, Estes M. Hyperviscosity syndrome [Internet]. In: StatPearls. Treasure Island, FL: StatPearls Publishing; (2020). Available online at: www.ncbi.nlm.nih.gov/books/NBK518963/ (accessed December 15, 2020). [Google Scholar]
- 108.Maier CL, Truong AD, Auld SC, Polly DM, Tanksley C-L, Duncan A. COVID-19-associated hyperviscosity: a link between inflammation and thrombophilia? Lancet. (2020) 395:1758–9. 10.1016/S0140-6736(20)31209-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Narasaraju T, Tang BM, Herrmann M, Muller S, Chow VTK, Radic M. Neutrophilia and NETopathy as key pathologic drivers of progressive lung impairment in patients with COVID-19. Front Pharmacol. (2020) 11:870. 10.3389/fphar.2020.00870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Middleton EA, He X-Y, Denorme F, Campbell RA, Ng D, Salvatore SP, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. (2020) 136:1169–79. 10.1182/blood.2020007008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Leppkes M, Knopf J, Naschberger E, Lindemann A, Singh J, Herrmann I, et al. Vascular occlusion by neutrophil extracellular traps in COVID-19. EBioMedicine. (2020) 58:102925. 10.1016/j.ebiom.2020.102925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Vallés J, Lago A, Santos MT, Latorre AM, Tembl JI, Salom JB, et al. Neutrophil extracellular traps are increased in patients with acute ischemic stroke: prognostic significance. Thromb Haemost. (2017) 117:1919–29. 10.1160/TH17-02-0130 [DOI] [PubMed] [Google Scholar]
- 113.Laridan E, Denorme F, Desender L, François O, Andersson T, Deckmyn H, et al. Neutrophil extracellular traps in ischemic stroke thrombi. Ann Neurol. (2017) 82:223–2. 10.1002/ana.24993 [DOI] [PubMed] [Google Scholar]
- 114.Fletcher-Sandersjöö A, Bellander B-M. Is COVID-19 associated thrombosis caused by overactivation of the complement cascade? A literature review. Thromb Res. (2020) 194:36–41. 10.1016/j.thromres.2020.06.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. (2020) 220:1–13. 10.1016/j.trsl.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Noris M, Benigni A, Remuzzi G. The case of complement activation in COVID-19 multiorgan impact. Kidney Int. (2020) 98:314–22. 10.1016/j.kint.2020.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yu J, Yuan X, Chen H, Chaturvedi S, Braunstein EM, Brodsky RA. Direct activation of the alternative complement pathway by SARS-CoV-2 spike proteins is blocked by factor D inhibition. Blood. (2020) 136:2080–9. 10.1182/blood.2020008248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fang S, Wang H, Lu L, Jia Y, Xia Z. Decreased complement C3 levels are associated with poor prognosis in patients with COVID-19: a retrospective cohort study. Int Immunopharmacol. (2020) 89:107070. 10.1016/j.intimp.2020.107070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cugno M, Meroni PL, Gualtierotti R, Griffini S, Grovetti E, Torri A, et al. Complement activation and endothelial perturbation parallel COVID-19 severity and activity. J Autoimmun. (2021) 116:102560. 10.1016/j.jaut.2020.102560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ehrenfeld M, Tincani A, Andreoli L, Cattalini M, Greenbaum A, Kanduc D, et al. Covid-19 and autoimmunity. Autoimmun Rev. (2020) 19:102597. 10.1016/j.autrev.2020.102597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Abdel-Wahab N, Talathi S, Lopez-Olivo MA, Suarez-Almazor ME. Risk of developing antiphospholipid antibodies following viral infection: a systematic review and meta-analysis. Lupus. (2018) 27:572–83. 10.1177/0961203317731532 [DOI] [PubMed] [Google Scholar]
- 122.Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. (2020) 46:1089–98. 10.1007/s00134-020-06062-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. (2020) 382:e38. 10.1056/NEJMc2007575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Brighton TA, Chesterman CN. Antiphospholipid antibodies and thrombosis. Baillieres Clin Haematol. (1994) 7:541–57. 10.1016/S0950-3536(05)80098-8 [DOI] [PubMed] [Google Scholar]
- 125.Espinosa G, Rodriguez-Pinto I, Cervera R. Catastrophic antiphospholipid syndrome: an update. Panminerva Med. (2017) 59:254–68. 10.23736/S0031-0808.17.03324-9 [DOI] [PubMed] [Google Scholar]
- 126.Reid V, Webster NR. Role of microparticles in sepsis. Br J Anaesth. (2012) 109:503–13. 10.1093/bja/aes321 [DOI] [PubMed] [Google Scholar]
- 127.Chen Y, Xiao Y, Lin Z, Xiao X, He C, Bihl JC, et al. The role of circulating platelets microparticles and platelet parameters in acute ischemic stroke patients. J Stroke Cerebrovasc Dis. (2015) 24:2313–20. 10.1016/j.jstrokecerebrovasdis.2015.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Owens AP, III, Mackman N. Microparticles in hemostasis and thrombosis. Circ Res. (2011) 108:1284–97. 10.1161/CIRCRESAHA.110.233056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Marchandot B, Sattler L, Jesel L, Matsushita K, Schini-Kerth V, Grunebaum L, et al. COVID-19 related coagulopathy: a distinct entity? J Clin Med. (2020) 9:1651. 10.3390/jcm9061651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.GUO D-Z, Lv Y, Qi Y, Pan S. Increased circulating microparticles and inflammatory factors aggravate coronavirus disease 2019 (COVID-19). Res Sq. (2020). Available online at: https://www.researchsquare.com/article/rs-19182/v1
- 131.Herichova I, Szantoova K. Renin-angiotensin system: upgrade of recent knowledge and perspectives. Endocr Regul. (2013) 47:39–52. 10.4149/endo_2013_01_39 [DOI] [PubMed] [Google Scholar]
- 132.Xia H, Lazartigues E. Angiotensin-converting enzyme 2: central regulator for cardiovascular function. Curr Hypertens Rep. (2010) 12:170–5. 10.1007/s11906-010-0105-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong J-C, Turner AJ, et al. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2. Circ Res. (2020) 126:1456–74. 10.1161/CIRCRESAHA.120.317015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Abboud H, Abboud FZ, Kharbouch H, Arkha Y, El Abbadi N, El Ouahabi A. COVID-19 and SARS-Cov-2 infection: pathophysiology and clinical effects on the nervous system. World Neurosurg. (2020) 140:49–53. 10.1016/j.wneu.2020.05.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Moulik S, Speth RC, Turner BB, Rowe BP. Angiotensin II receptor subtype distribution in the rabbit brain. Exp brain Res. (2002) 142:275–83. 10.1007/s00221-001-0940-5 [DOI] [PubMed] [Google Scholar]
- 136.Schulz M, Engelhardt B. The circumventricular organs participate in the immunopathogenesis of experimental autoimmune encephalomyelitis. Cerebrospinal Fluid Res. (2005) 2:8. 10.1186/1743-8454-2-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Nataraj C, Oliverio MI, Mannon RB, Mannon PJ, Audoly LP, Amuchastegui CS, et al. Angiotensin II regulates cellular immune responses through a calcineurin-dependent pathway. J Clin Invest. (1999) 104:1693–701. 10.1172/JCI7451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Dandona P, Dhindsa S, Ghanim H, Chaudhuri A. Angiotensin II and inflammation: the effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockade. J Hum Hypertens. (2007) 21:20–7. 10.1038/sj.jhh.1002101 [DOI] [PubMed] [Google Scholar]
- 139.Brown NJ, Vaughan DE. Role of Angiotensin II in Coagulation and Fibrinolysis. Heart Fail Rev. (1999) 3:193–8. 10.1023/A:1009757416302 [DOI] [Google Scholar]
- 140.Holtz J, Goetz RM. The endothelium and the renin-angiotensin system. Arzneimittelforschung. (1994) 44:397–402. [PubMed] [Google Scholar]
- 141.Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, et al. Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature. (1995) 377:239–42. 10.1038/377239a0 [DOI] [PubMed] [Google Scholar]
- 142.Lassegue B, Clempus RE. Vascular NAD (P) H oxidases: specific features, expression, and regulation. Am J Physiol Integr Comp Physiol. (2003) 285:R277–97. 10.1152/ajpregu.00758.2002 [DOI] [PubMed] [Google Scholar]
- 143.Violi F, Oliva A, Cangemi R, Ceccarelli G, Pignatelli P, Carnevale R, et al. Nox2 activation in Covid-19. Redox Biol. (2020) 36:101655. 10.1016/j.redox.2020.101655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zimmerman MC, Lazartigues E, Lang JA, Sinnayah P, Ahmad IM, Spitz DR, et al. Superoxide mediates the actions of angiotensin II in the central nervous system. Circ Res. (2002) 91:1038–45. 10.1161/01.RES.0000043501.47934.FA [DOI] [PubMed] [Google Scholar]
- 145.Menon B, Ramalingam K, Kumar R. Evaluating the role of oxidative stress in acute ischemic stroke. J Neurosci Rural Pract. (2020) 11:156–9. 10.1055/s-0039-3402675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Stoiber W, Obermayer A, Steinbacher P, Krautgartner W-D. The role of reactive oxygen species (ROS) in the formation of extracellular traps (ETs) in humans. Biomolecules. (2015) 5:702–23. 10.3390/biom5020702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Endtmann C, Ebrahimian T, Czech T, Arfa O, Laufs U, Fritz M, et al. Angiotensin II impairs endothelial progenitor cell number and function in vitro and in vivo: implications for vascular regeneration. Hypertension. (2011) 58:394–403. 10.1161/HYPERTENSIONAHA.110.169193 [DOI] [PubMed] [Google Scholar]
- 148.Reid IA. Interactions between ANG II, sympathetic nervous system, and baroreceptor reflexes in regulation of blood pressure. Am J Physiol Metab. (1992) 262:E763–78. 10.1152/ajpendo.1992.262.6.E763 [DOI] [PubMed] [Google Scholar]
- 149.Zucker IH, Liu J-L. Angiotensin II—nitric oxide interactions in the control of sympathetic outflow in heart failure. Heart Fail Rev. (2000) 5:27–43. [DOI] [PubMed] [Google Scholar]
- 150.Owens GK. Role of contractile agonists in growth regulation of vascular smooth muscle cells. In: Cox RH, editor. Cellular and Molecular Mechanisms in Hypertension. Boston, MA: Springer; (1991). p. 71–9. 10.1007/978-1-4684-6015-5 [DOI] [PubMed] [Google Scholar]
- 151.Greindling KK, Lassegue B, Alexander RW. Angiotensin receptors and their therapeutic implications. Annu Rev Pharmacol Toxicol. (1996) 36:281–306. 10.1146/annurev.pa.36.040196.001433 [DOI] [PubMed] [Google Scholar]
- 152.Su F, Zhang W, Chen Y, Ma L, Zhang H, Wang F. Significance of hypoxia-inducible factor-1α expression with atrial fibrosis in rats induced with isoproterenol. Exp Ther Med. (2014) 8:1677–82. 10.3892/etm.2014.1989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Xie J, Covassin N, Fan Z, Singh P, Gao W, Li G, et al. Association between hypoxemia and mortality in patients with COVID-19. Mayo Clin Proc. (2020) 95:1138–47. 10.1016/j.mayocp.2020.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pearce WJ. Mechanisms of hypoxic cerebral vasodilatation. Pharmacol Ther. (1995) 65:75–91. 10.1016/0163-7258(94)00058-B [DOI] [PubMed] [Google Scholar]
- 155.D'Ignazio L, Bandarra D, Rocha S. NF-κB and HIF crosstalk in immune responses. FEBS J. (2016) 283:413–24. 10.1111/febs.13578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Eltzschig HK, Carmeliet P. Hypoxia and inflammation. N Engl J Med. (2011) 364:656–65. 10.1056/NEJMra0910283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yan S-F, Mackman N, Kisiel W, Stern DM, Pinsky DJ. Hypoxia/hypoxemia-induced activation of the procoagulant pathways and the pathogenesis of ischemia-associated thrombosis. Arterioscler Thromb Vasc Biol. (1999) 19:2029–35. 10.1161/01.ATV.19.9.2029 [DOI] [PubMed] [Google Scholar]
- 158.Evans CE. Hypoxia and HIF activation as a possible link between sepsis and thrombosis. Thromb J. (2019) 17:1–4. 10.1186/s12959-019-0205-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Chaurasia SN, Kushwaha G, Kulkarni PP, Mallick RL, Latheef NA, Mishra JK, et al. Platelet HIF-2α promotes thrombogenicity through PAI-1 synthesis and extracellular vesicle release. Haematologica. (2019) 104:2482–92. 10.3324/haematol.2019.217463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Stockmann C, Fandrey J. Hypoxia-induced erythropoietin production: a paradigm for oxygen-regulated gene expression. Clin Exp Pharmacol Physiol. (2006) 33:968–79. 10.1111/j.1440-1681.2006.04474.x [DOI] [PubMed] [Google Scholar]
- 161.Lehner C, Gehwolf R, Tempfer H, Krizbai I, Hennig B, Bauer H-C, et al. Oxidative stress and blood–brain barrier dysfunction under particular consideration of matrix metalloproteinases. Antioxid Redox Signal. (2011) 15:1305–23. 10.1089/ars.2011.3923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Gupta N, Ashraf MZ. Hypoxia Signaling in Cardiovascular Diseases, editors Hypoxia and Anoxia. London, UK: IntechOpen; (2018). Available online at: https://www.intechopen.com/books/hypoxia-and-anoxia/hypoxia-signaling-in-cardiovascular-diseases [Google Scholar]
- 163.van Beek JHGM. Effects of hypoxia and hypercapnia on cardiac contractility and energetics. In: Dahan A, Teppema L, van Beek JHGM, editors. Physiology And Pharmacology of Cardio-Respiratory Control. Dordrecht: Springer; (1998). 10.1007/978-94-011-5129-0_3 [DOI] [Google Scholar]
- 164.Macdonald WA, Hool LC. The effect of acute hypoxia on excitability in the heart and the L-type calcium channel as a therapeutic target. Curr Drug Discov Technol. (2008) 5:302–11. 10.2174/157016308786733546 [DOI] [PubMed] [Google Scholar]
- 165.Vakhshoori M, Heidarpour M, Shafie D, Taheri M, Rezaei N, Sarrafzadegan N. Acute cardiac injury in COVID-19: a systematic review and meta-analysis. Arch Iran Med. (2020) 23:801–12. 10.34172/aim.2020.107 [DOI] [PubMed] [Google Scholar]
- 166.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. (2020) 5:802–10. 10.1001/jamacardio.2020.0950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Tsivgoulis G, Palaiodimou L, Katsanos AH, Caso V, Köhrmann M, Molina C, et al. Neurological manifestations and implications of COVID-19 pandemic. Ther Adv Neurol Disord. (2020) 13:1756286420932036. 10.1177/1756286420932036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Hamming I, Timens W, Bulthuis MLC, Lely AT, Navis GJ, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. a first step in understanding SARS pathogenesis. J Pathol. (2004) 203:631–7. 10.1002/path.1570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res. (2020) 116:1097–100. 10.1093/cvr/cvaa078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Ghafouri-Fard S, Noroozi R, Omrani MD, Branicki W, Pośpiech E, Sayad A, et al. Angiotensin converting enzyme: a review on expression profile and its association with human disorders with special focus on SARS-CoV-2 infection. Vascul Pharmacol. (2020) 130:106680. 10.1016/j.vph.2020.106680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Escher F, Pietsch H, Aleshcheva G, Bock T, Baumeier C, Elsaesser A, et al. Detection of viral SARS-CoV-2 genomes and histopathological changes in endomyocardial biopsies. ESC Hear Fail. (2020) 7:2440–7. 10.1002/ehf2.12805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Camici PG, d'Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. (2015) 12:48–62. 10.1038/nrcardio.2014.160 [DOI] [PubMed] [Google Scholar]
- 174.Evans PC, Rainger GE, Mason JC, Guzik TJ, Osto E, Stamataki Z, et al. Endothelial dysfunction in COVID-19: a position paper of the ESC Working Group for Atherosclerosis and Vascular Biology, and the ESC Council of Basic Cardiovascular Science. Cardiovasc Res. (2020) 116:2177–84. 10.1093/cvr/cvaa230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Peretto G, Sala S, Caforio ALP. Acute myocardial injury, MINOCA, or myocarditis? Improving characterization of coronavirus-associated myocardial involvement. Eur Heart J. (2020) 41:2124–5. 10.1093/eurheartj/ehaa396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Robinson FA, Mihealsick RP, Wagener BM, Hanna P, Poston MD, Efimov IR, et al. Role of angiotensin-converting enzyme 2 and pericytes in cardiac complications of COVID-19 infection. Am J Physiol Circ Physiol. (2020) 319:H1059–68. 10.1152/ajpheart.00681.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. (2020) 116:1666–87. 10.1093/cvr/cvaa106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Cardot-Leccia N, Hubiche T, Dellamonica J, Burel-Vandenbos F, Passeron T. Pericyte alteration sheds light on micro-vasculopathy in COVID-19 infection. Intensive Care Med. (2020) 46:1777–8. 10.1007/s00134-020-06147-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.He L, Mäe MA, Muhl L, Sun Y, Pietilä R, Nahar K, et al. Pericyte-specific vascular expression of SARS-CoV-2 receptor ACE2 – implications for microvascular inflammation and hypercoagulopathy in COVID-19. bioRxiv [Internet]. (2020). 10.1101/2020.05.11.088500v2 [DOI] [Google Scholar]
- 180.Singh S, Desai R, Gandhi Z, Fong HK, Doreswamy S, Desai V, et al. Takotsubo syndrome in patients with COVID-19: a systematic review of published cases. SN Compr Clin Med. (2020) 1–7. 10.1007/s42399-020-00557-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Vitale C, Rosano GMC, Kaski JC. Role of coronary microvascular dysfunction in takotsubo cardiomyopathy. Circ J. (2016) 80:299–305. 10.1253/circj.CJ-15-1364 [DOI] [PubMed] [Google Scholar]
- 182.Geng Y-J, Wei Z-Y, Qian H-Y, Huang J, Lodato R, Schultz RJ. Pathophysiological characteristics and therapeutic approaches for pulmonary injury and cardiovascular complications of coronavirus disease 2019. Cardiovasc Pathol. (2020) 47:107228. 10.1016/j.carpath.2020.107228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Patel KP, Schultz HD. Angiotensin peptides and nitric oxide in cardiovascular disease. Antioxid Redox Signal. (2013) 19:1121–32. 10.1089/ars.2012.4614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Seecheran R, Narayansingh R, Giddings S, Rampaul M, Furlonge K, Abdool K, et al. Atrial arrhythmias in a patient presenting with Coronavirus Disease-2019 (COVID-19) infection. J Investig Med High Impact Case Rep. (2020) 8:2324709620925571. 10.1177/2324709620925571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Taha ME, Alsafi W, Taha M, Eljack A, Ibrahim H. Coronavirus disease and new-onset atrial fibrillation: two cases. Cureus. (2020) 12:e8066. 10.7759/cureus.8066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Walkey AJ, Wiener RS, Ghobrial JM, Curtis LH, Benjamin EJ. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA. (2011) 306:2248–54. 10.1001/jama.2011.1615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Walkey AJ, Hammill BG, Curtis LH, Benjamin EJ. Long-term outcomes following development of new-onset atrial fibrillation during sepsis. Chest. (2014) 146:1187–95. 10.1378/chest.14-0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Wall C, Moore J, Thachil J. Catheter-related thrombosis: a practical approach. J Intensive Care Soc. (2016) 17:160–7. 10.1177/1751143715618683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Levi M. Hemostasis and thrombosis in extreme temperatures (hypo-and hyperthermia). Semin Thromb Hemost. (2018) 44:651–5. 10.1055/s-0038-1648231 [DOI] [PubMed] [Google Scholar]
- 190.Niven DJ, Léger C, Stelfox HT, Laupland KB. Fever in the critically ill: a review of epidemiology, immunology, and management. J Intensive Care Med. (2012) 27:290–7. 10.1177/0885066611402463 [DOI] [PubMed] [Google Scholar]
- 191.Meyer MAS, Ostrowski SR, Overgaard A, Ganio MS, Secher NH, Crandall CG, et al. Hypercoagulability in response to elevated body temperature and central hypovolemia. J Surg Res. (2013) 185:e93–100. 10.1016/j.jss.2013.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Yenari MA, Hemmen TM. Therapeutic hypothermia for brain ischemia. Stroke. (2010). 41:S72–4. 10.1161/STROKEAHA.110.595371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Polderman KH. Hypothermia and coagulation. Crit Care. (2012). 16:A20 (2012). 10.1186/cc11278 [DOI] [Google Scholar]
- 194.Tian D, Ye Q. Hepatic complications of COVID-19 and its treatment. J Med Virol. (2020) 92:1818–24. 10.1002/jmv.26036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. (2020) 8:420–2. 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Chai X, Hu L, Zhang Y, Han W, Lu Z, Ke A, et al. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. biorxiv [Internet]. (2020). 10.1101/2020.02.03.931766 [DOI] [Google Scholar]
- 197.Galli L, Gerdes VEA, Guasti L, Squizzato A. Thrombosis associated with viral hepatitis. J Clin Transl Hepatol. (2014) 2:234–9. 10.14218/JCTH.2014.00031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Morassi M, Bagatto D, Cobelli M, D'Agostini S, Gigli GL, Bnà C, et al. Stroke in patients with SARS-CoV-2 infection: case series. J Neurol. (2020) 267:2185–92. 10.1007/s00415-020-09885-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Aghayari Sheikh Neshin S, Basirjafari S, Saberi A, Shahhosseini B, Zarei M. Liver abnormality may develop cerebral vein thrombosis in COVID-19. J Neurol Sci. (2020) 417:117076. 10.1016/j.jns.2020.117076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Gabarre P, Dumas G, Dupont T, Darmon M, Azoulay E, Zafrani L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. (2020) 46:1339–48. 10.1007/s00134-020-06153-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Iotti S, Wolf F, Mazur A, Maier J. The COVID-19 pandemic: is there a role for magnesium? Hypotheses and perspectives. Magnes Res. (2020) 33:21–7. 10.1684/mrh.2020.0465 [DOI] [PubMed] [Google Scholar]
- 202.Tang C-F, Ding H, Jiao R-Q, Wu X-X, Kong L-D. Possibility of magnesium supplementation for supportive treatment in patients with COVID-19. Eur J Pharmacol. (2020) 886:173546. 10.1016/j.ejphar.2020.173546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Ohira T, Peacock JM, Iso H, Chambless LE, Rosamond WD, Folsom AR. Serum and dietary magnesium and risk of ischemic stroke: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. (2009) 169:1437–44. 10.1093/aje/kwp071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Gülsen A, Yigitbas BA, Uslu B, Drömann D, Kilinc O. The effect of smoking on COVID-19 symptom severity: systematic review and meta-analysis. Pulm Med. (2020) 2020:7590207. 10.1101/2020.08.15.20102699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wang X, Fang X, Cai Z, Wu X, Gao X, Min J, et al. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 patients: a systemic review and meta-analysis. Research. (2020) 2020:2402961. 10.34133/2020/2402961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Zhao Q, Meng M, Kumar R, Wu Y, Huang J, Lian N, et al. The impact of COPD and smoking history on the severity of COVID-19: a systemic review and meta-analysis. J Med Virol. (2020) 92:1915–21. 10.1002/jmv.25889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Bhatia R, Srivastava MVP. COVID-19 and stroke: incidental, triggered or causative. Ann Indian Acad Neurol. (2020) 23:318–24. 10.4103/aian.AIAN_380_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Hadi HAR, Carr CS, Al Suwaidi J. Endothelial dysfunction: cardiovascular risk factors, therapy, and outcome. Vasc Health Risk Manag. (2005) 1:183–98. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1993955 [PMC free article] [PubMed] [Google Scholar]
- 209.Bautista LE, Vera LM, Arenas IA, Gamarra G. Independent association between inflammatory markers (C-reactive protein, interleukin-6, and TNF-alpha) and essential hypertension. J Hum Hypertens. (2005) 19:149–54. 10.1038/sj.jhh.1001785 [DOI] [PubMed] [Google Scholar]
- 210.Pahwa R, Jialal I. Chronic Inflammation. Treasure Island, FL: StatPearls Publishing; (2020). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK493173/ (accessed December 10, 2020). [Google Scholar]
- 211.Piché M-E, Lemieux S, Weisnagel SJ, Corneau L, Nadeau A, Bergeron J. Relation of high-sensitivity C-reactive protein, interleukin-6, tumor necrosis factor-alpha, and fibrinogen to abdominal adipose tissue, blood pressure, and cholesterol and triglyceride levels in healthy postmenopausal women. Am J Cardiol. (2005) 96:92–7. 10.1016/j.amjcard.2005.02.051 [DOI] [PubMed] [Google Scholar]
- 212.Gharacholou SM, Becker RC. Hemostasis and thrombosis in older adults. J Thromb Thrombolysis. (2009) 27:249. 10.1007/s11239-009-0308-4 [DOI] [PubMed] [Google Scholar]
- 213.Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. (2010) 8:917–32. 10.1586/erc.10.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Blokhin IO, Lentz SR. Mechanisms of thrombosis in obesity. Curr Opin Hematol. (2013) 20:437–44. 10.1097/MOH.0b013e3283634443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Nadar S, Lip GYH. The prothrombotic state in hypertension and the effects of antihypertensive treatment. Curr Pharm Des. (2003) 9:1715–32. 10.2174/1381612033454559 [DOI] [PubMed] [Google Scholar]
- 216.Carr ME. Diabetes mellitus: a hypercoagulable state. J Diabetes Complicat. (2001) 15:44–54. 10.1016/S1056-8727(00)00132-X [DOI] [PubMed] [Google Scholar]
- 217.Rosenberg GA. Neurological diseases in relation to the blood-brain barrier. J Cereb Blood Flow Metab. (2012) 32:1139–51. 10.1038/jcbfm.2011.197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Hyassat D, Al Sitri E, Batieha A, El-Khateeb M, Ajlouni K. Prevalence of hypomagnesaemia among obese Type 2 diabetic patients attending the National Center for Diabetes, Endocrinology and Genetics (NCDEG). Int J Endocrinol Metab. (2014) 12:e17796. 10.5812/ijem.17796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Chrysant SG, Chrysant GS. Association of hypomagnesemia with cardiovascular diseases and hypertension. Int J Cardiol Hypertens. (2019) 1:100005. 10.1016/j.ijchy.2019.100005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Del Gobbo LC, Imamura F, Wu JHY, de Oliveira Otto MC, Chiuve SE, Mozaffarian D. Circulating and dietary magnesium and risk of cardiovascular disease: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. (2013) 98:160–73. 10.3945/ajcn.112.053132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Amighi J, Sabeti S, Schlager O, Mlekusch W, Exner M, Lalouschek W, et al. Low serum magnesium predicts neurological events in patients with advanced atherosclerosis. Stroke. (2004) 35:22–7. 10.1161/01.STR.0000105928.95124.1F [DOI] [PubMed] [Google Scholar]
- 222.Fang X, Wang K, Han D, He X, Wei J, Zhao L, et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. BMC Med. (2016) 14:210. 10.1186/s12916-016-0742-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Flores B, Trivedi HD, Robson SC, Bonder A. Hemostasis, bleeding and thrombosis in liver disease. J Transl Sci. (2017) 3:10.15761/JTS.1000182. 10.15761/JTS.1000182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Tripodi A, Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med. (2011) 365:147–56. 10.1056/NEJMra1011170 [DOI] [PubMed] [Google Scholar]
- 225.Ghoshal S, Freedman BI. Mechanisms of stroke in patients with chronic kidney disease. Am J Nephrol. (2019) 50:229–39. 10.1159/000502446 [DOI] [PubMed] [Google Scholar]
- 226.Dad T, Weiner DE. Stroke and chronic kidney disease: epidemiology, pathogenesis, and management across kidney disease stages. Semin Nephrol. (2015) 35:311–22. 10.1016/j.semnephrol.2015.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Nayak-Rao S, Shenoy MP. Stroke in patients with chronic kidney disease…: how do we approach and manage it? Indian J Nephrol. (2017) 27:167–71. 10.4103/0971-4065.202405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Makin SDJ, Cook FAB, Dennis MS, Wardlaw JM. Cerebral small vessel disease and renal function: systematic review and meta-analysis. Cerebrovasc Dis. (2015) 39:39–52. 10.1159/000369777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Toyoda K. Cerebral small vessel disease and chronic kidney disease. J Stroke. (2015) 17:31–7. 10.5853/jos.2015.17.1.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Dardiotis E, Aloizou A-M, Markoula S, Siokas V, Tsarouhas K, Tzanakakis G, et al. Cancer-associated stroke: pathophysiology, detection and management (Review). Int J Oncol. (2019) 54:779–96. 10.3892/ijo.2019.4669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Graus F, Rogers LR, Posner JB. Cerebrovascular complications in patients with cancer. Medicine. (1985) 64:16–35. 10.1097/00005792-198501000-00002 [DOI] [PubMed] [Google Scholar]
- 232.Blixt J, Svensson M, Gunnarson E, Wanecek M. Aquaporins and blood-brain barrier permeability in early edema development after traumatic brain injury. Brain Res. (2015) 1611:18–28. 10.1016/j.brainres.2015.03.004 [DOI] [PubMed] [Google Scholar]
- 233.Kempuraj D, GP S, Ahmed ME, Raikwar S, Thangavel R, Khan A, et al. COVID-19, mast cells, cytokine storm, psychological stress, and neuroinflammation. Neurosci. (2020) 26:402–14. 10.1177/1073858420941476 [DOI] [PubMed] [Google Scholar]
- 234.Squizzato A, Gerdes V, Brandjes D, Büller H, Stam J. Thyroid diseases and cerebrovascular disease. Stroke. (2005) 36:2302–10. 10.1161/01.STR.0000181772.78492.07 [DOI] [PubMed] [Google Scholar]
- 235.Meng-Han Y, Yang F-Y, Lee D-D. Thyroid disease as a risk factor for cerebrovascular disease. J Stroke Cerebrovasc Dis. (2015) 24:912–20. 10.1016/j.jstrokecerebrovasdis.2014.11.032 [DOI] [PubMed] [Google Scholar]
- 236.Udovcic M, Pena RH, Patham B, Tabatabai L, Kansara A. Hypothyroidism and the heart. Methodist Debakey Cardiovasc J. (2017) 13:55–9. 10.14797/mdcj-13-2-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Mahajan AS, Lal R, Dhanwal DK, Jain AK, Chowdhury V. Evaluation of autonomic functions in subclinical hypothyroid and hypothyroid patients. Indian J Endocrinol Metab. (2013) 17:460–4. 10.4103/2230-8210.111642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Hak AE, Pols HA, Visser TJ, Drexhage HA, Hofman A, Witteman JC. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam study. Ann Intern Med. (2000) 132:270–8. 10.7326/0003-4819-132-4-200002150-00004 [DOI] [PubMed] [Google Scholar]
- 239.Razvi S, Jabbar A, Pingitore A, Danzi S, Biondi B, Klein I, et al. Thyroid hormones and cardiovascular function and diseases. J Am Coll Cardiol. (2018) 71:1781–96. 10.1016/j.jacc.2018.02.045 [DOI] [PubMed] [Google Scholar]
- 240.Kim YA, Park YJ. Prevalence and risk factors of subclinical thyroid disease. Endocrinol Metab. (2014) 29:20–9. 10.3803/EnM.2014.29.1.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Mars N, Koskela JT, Ripatti P, Kiiskinen TTJ, Havulinna AS, Lindbohm JV, et al. Polygenic and clinical risk scores and their impact on age at onset and prediction of cardiometabolic diseases and common cancers. Nat Med. (2020) 26:549–57. 10.1038/s41591-020-0800-0 [DOI] [PubMed] [Google Scholar]
- 242.Ibanez L, Heitsch L, Dube U, Farias FHG, Budde J, Bergmann K, et al. Overlap in the genetic architecture of stroke risk, early neurological changes, and cardiovascular risk factors. Stroke. (2019) 50:1339–45. 10.1161/STROKEAHA.118.023097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Li J, Chaudhary DP, Khan A, Griessenauer C, Carey DJ, Zand R, Abedi V. Polygenic risk scores augment stroke subtyping. Neurol Genet. (2021) 7:e560. 10.1212/NXG.0000000000000560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Williams OH, Mohideen S, Sen A, Martinovic O, Hart J, Brex PA, et al. Multiple internal border zone infarcts in a patient with COVID-19 and CADASIL. J Neurol Sci. (2020) 416:116980. 10.1016/j.jns.2020.116980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Green D. Thrombophilia and stroke. Top Stroke Rehabil. (2003) 10:21–33. 10.1310/L9KD-N5N8-69X0-08QK [DOI] [PubMed] [Google Scholar]
- 246.Wu C-I, Postema PG, Arbelo E, Behr ER, Bezzina CR, Napolitano C, et al. SARS-CoV-2, COVID-19, and inherited arrhythmia syndromes. Hear Rhythm. (2020) 17:1456–62. 10.1016/j.hrthm.2020.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Atianzar K, Casterella P, Zhang M, Sharma R, Gafoor S. Update on the management of patent foramen ovale in 2017: indication for closure and literature review. US Cardiol Rev. (2017) 11:75. 10.15420/usc.2017:18:1 [DOI] [Google Scholar]
- 248.Cook D, Douketis J, Crowther MA, Anderson DR. The diagnosis of deep venous thrombosis and pulmonary embolism in medical-surgical intensive care unit patients. J Crit Care. (2005) 4:314–9. 10.1016/j.jcrc.2005.09.003 [DOI] [PubMed] [Google Scholar]
- 249.Llitjos J, Leclerc M, Chochois C, Monsallier J, Ramakers M, Auvray M, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. (2020) 18:1743–6. 10.1111/jth.14869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Emdin CA, Odutayo A, Wong CX, Tran J, Hsiao AJ, Hunn BHM. Meta-analysis of anxiety as a risk factor for cardiovascular disease. Am J Cardiol. (2016) 118:511–9. 10.1016/j.amjcard.2016.05.041 [DOI] [PubMed] [Google Scholar]
- 251.Jabri A, Kalra A, Kumar A, Alameh A, Adroja S, Bashir H, et al. Incidence of stress cardiomyopathy during the coronavirus disease 2019. pandemic. JAMA Netw Open. (2020) 3:e2014780. 10.1001/jamanetworkopen.2020.14780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. (2020) 368:m1091. 10.1136/bmj.m1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Oji Y, Noda K, Tokugawa J, Yamashiro K, Hattori N, Okuma Y. Spontaneous spinal subarachnoid hemorrhage after severe coughing: a case report. J Med Case Rep. (2013) 7:274. 10.1186/1752-1947-7-274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Danuta MS, Buxton JA, Hestrin M, Keyes RD, Lynch K, Halperin SA. Carotid artery dissection as a possible severe complication of pertussis in an adult: clinical case report and review. Clin Infect Dis. (2003) 36:e1–4. 10.1086/344776 [DOI] [PubMed] [Google Scholar]
- 255.Giacomelli E, Dorigo W, Fargion A, Calugi G, Cianchi G, Pratesi C. Acute thrombosis of an aortic prosthetic graft in a patient with severe COVID-19-Related pneumonia. Ann Vasc Surg. (2020) 66:8–10. 10.1016/j.avsg.2020.04.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of Covid-19 - final report. N Engl J Med. (2020) 383:1813–26. 10.1056/NEJMc2022236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Kalil AC, Patterson TF, Mehta AK, Tomashek KM, Wolfe CR, Ghazaryan V, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. (2020) 384:795–807. 10.1056/NEJMoa2031994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Sarkar C, Mondal M, Torequl Islam M, Martorell M, Docea AO, Maroyi A, et al. Potential therapeutic options for COVID-19: Current status, challenges, and future perspectives. Front Pharmacol. (2020) 11:1428. 10.3389/fphar.2020.572870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Soliman EZ, Howard G, Cushman M, Kissela B, Kleindorfer D, Le A, et al. Prolongation of QTc and risk of stroke: the REGARDS (REasons for Geographic and Racial Differences in Stroke) study. J Am Coll Cardiol. (2012) 59:1460–7. 10.1016/j.jacc.2012.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Michaud V, Dow P, Al Rihani SB, Deodhar M, Arwood M, Cicali B, et al. Risk assessment of drug-induced Long QT Syndrome for some COVID-19 repurposed drugs. Clin Transl Sci. (2020) 14:20–8. 10.1111/cts.12882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Poluzzi E, Raschi E, Godman B, Koci A, Moretti U, Kalaba M, et al. Pro-arrhythmic potential of oral antihistamines (H1): combining adverse event reports with drug utilization data across Europe. PLoS ONE. (2015) 10:e0119551. 10.1371/journal.pone.0119551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Ly T, Ruiz ME. Prolonged QT interval and torsades de pointes associated with atazanavir therapy. Clin Infect Dis. (2007) 44:e67–8. 10.1086/511875 [DOI] [PubMed] [Google Scholar]
- 263.Crotti L, Arbelo E. COVID-19 treatments, QT interval and arrhythmic risk: the need for an international Registry on Arrhythmias. Hear Rhythm. (2020) 17:1423–4. 10.1016/j.hrthm.2020.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Nachimuthu S, Assar MD, Schussler JM. Drug-induced QT interval prolongation: mechanisms and clinical management. Ther Adv drug Saf. (2012) 3:241–53. 10.1177/2042098612454283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Ghasemiyeh P, Borhani-Haghighi A, Karimzadeh I, Mohammadi-Samani S, Vazin A, Safari A, et al. Major neurologic adverse drug reactions, potential drug-drug interactions and pharmacokinetic aspects of drugs used in COVID-19 patients with stroke: a narrative review. Ther Clin Risk Manag. (2020) 16:595–605. 10.2147/TCRM.S259152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Yu WL, Toh HS, Liao CT, Chang WT. A double-edged sword-cardiovascular concerns of potential anti-COVID-19 drugs. Cardiovasc Drugs Ther. (2020). 10.1007/s10557-020-07024-7. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Esterly JS, Darin KM, Gerzenshtein L, Othman F, Postelnick MJ, Scarsi KK. Clinical implications of antiretroviral drug interactions with warfarin: a case–control study. J Antimicrob Chemother. (2013) 68:1360–3. 10.1093/jac/dkt043 [DOI] [PubMed] [Google Scholar]
- 268.Marsousi N, Daali Y, Fontana P, Reny J-L, Ancrenaz-Sirot V, Calmy A, et al. Impact of boosted antiretroviral therapy on the pharmacokinetics and efficacy of clopidogrel and prasugrel active metabolites. Clin Pharmacokinet. (2018) 57:1347–54. 10.1007/s40262-018-0637-6 [DOI] [PubMed] [Google Scholar]
- 269.Marsousi N, Samer CF, Fontana P, Reny JL, Rudaz S, Desmeules JA, et al. Coadministration of ticagrelor and ritonavir: toward prospective dose adjustment to maintain an optimal platelet inhibition using the PBPK approach. Clin Pharmacol Ther. (2016) 100:295–304. 10.1002/cpt.407 [DOI] [PubMed] [Google Scholar]
- 270.Testa S, Prandoni P, Paoletti O, Morandini R, Tala M, Dellanoce C, et al. Direct oral anticoagulant plasma levels' striking increase in severe COVID-19 respiratory syndrome patients treated with antiviral agents: the Cremona experience. J Thromb Haemost. (2020) 18:1320–3. 10.1111/jth.14871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Agarwal S, Agarwal SK. Lopinavir-ritonavir in SARS-CoV-2 infection and drug-drug interactions with cardioactive medications. Cardiovasc Drugs Ther. (2020) 1–14. Available online at: https://link.springer.com/article/10.1007%2Fs10557-020-07070-1#citeas. 10.1007/s10557-020-07070-1 [DOI] [PMC free article] [PubMed]
- 272.Robinson PC, Richards D, Tanner HL, Feldmann M. Accumulating evidence suggests anti-TNF therapy needs to be given trial priority in COVID-19 treatment. Lancet Rheumatol. (2020) 2:e653–5. 10.1016/S2665-9913(20)30309-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Vereckei E, Kriván G, Réti M, Szodoray P, Poór G, Kiss E. Anti-TNF-alpha-induced anti-phospholipid syndrome manifested as necrotizing vasculitis. Scand J Rheumatol. (2010) 39:175–7. 10.3109/03009740902832753 [DOI] [PubMed] [Google Scholar]
- 274.Guillevin L, Mouthon L. Tumor necrosis factor-alpha blockade and the risk of vasculitis. J Rheumatol. (2004) 31:1885–7. Available online at: https://www.jrheum.org/content/31/10/1885.long [PubMed] [Google Scholar]
- 275.Korswagen LA, Bartelds GM, Krieckaert CLM, Turkstra F, Nurmohamed MT, van Schaardenburg D, et al. Venous and arterial thromboembolic events in adalimumab-treated patients with antiadalimumab antibodies: a case series and cohort study. Arthritis Rheum. (2011) 63:877–83. 10.1002/art.30209 [DOI] [PubMed] [Google Scholar]
- 276.Petitpain N, Gambier N, Wahl D, Chary-Valckenaere I, Loeuille D, Gillet P. Arterial and venous thromboembolic events during anti-TNF therapy: a study of 85 spontaneous reports in the period 2000-2006. Biomed Mater Eng. (2009) 19:355–64. 10.3233/BME-2009-0600 [DOI] [PubMed] [Google Scholar]
- 277.Nosbaum A, Goujon C, Fleury B, Guillot I, Nicolas J-F, Bérard F. Arterial thrombosis with anti-phospholipid antibodies induced by infliximab. Eur J Dermatology. (2007) 17:546–7. 10.1684/ejd.2007.0280 [DOI] [PubMed] [Google Scholar]
- 278.Grange L, Nissen MJ, Garambois K, Dumolard A, Duc C, Gaudin P, et al. Infliximab-induced cerebral thrombophlebitis. Rheumatology. (2005) 44:260–1. 10.1093/rheumatology/keh451 [DOI] [PubMed] [Google Scholar]
- 279.Virupannavar S, Brandau A, Guggenheim C, Laird-Fick H. Possible association of etanercept, venous thrombosis, and induction of antiphospholipid syndrome. Case Rep Rheumatol. (2014) 2014:801072. 10.1155/2014/801072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Dastan F, Saffaei A, Haseli S, Marjani M, Moniri A, Abtahian Z, et al. Promising effects of tocilizumab in COVID-19: a non-controlled, prospective clinical trial. Int Immunopharmacol. (2020) 88:106869. 10.1016/j.intimp.2020.106869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Zhang C, Wu Z, Li J-W, Zhao H, Wang G-Q. Cytokine release syndrome in severe COVID-19: interleukin-6 receptor antagonist tocilizumab may be the key to reduce mortality. Int J Antimicrob Agents. (2020) 55:105954. 10.1016/j.ijantimicag.2020.105954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Jacob H, Rajkumar V, Louise M. Abstract TP270: Interleukin-6 receptor inhibition with tocilizumab ameliorates ischemic stroke damage in mice. Stroke. (2017) 48(suppl_1):ATP270. 10.1161/str.48.suppl_1.tp270 [DOI] [Google Scholar]
- 283.Jewell P, Ansorge O, Kuker W, Irani SR, Zamboni G. Tocilizumab-associated multifocal cerebral thrombotic microangiopathy. Neurol Clin Pract. (2016) 6:e24–6. 10.1212/CPJ.0000000000000220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Ito S, Tsutsumi Y, Kikuchi R, Matsuoka S, Shimoyama N. [Thrombotic microangiopathy developing subsequent to tocilizumab therapy in a patient with TAFRO syndrome]. Rinsho Ketsueki. (2018) 59:2432–7. 10.11406/rinketsu.59.2432 [DOI] [PubMed] [Google Scholar]
- 285.Souverein PC, Berard A, Van Staa TP, Cooper C, Egberts ACG, Leufkens HGM, et al. Use of oral glucocorticoids and risk of cardiovascular and cerebrovascular disease in a population based case–control study. Heart. (2004) 90:859–65. 10.1136/hrt.2003.020180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Christiansen CF, Christensen S, Mehnert F, Cummings SR, Chapurlat RD, Sørensen HT. Glucocorticoid use and risk of atrial fibrillation or flutter: a population-based, case-control study. Arch Intern Med. (2009) 169:1677–83. 10.1001/archinternmed.2009.297 [DOI] [PubMed] [Google Scholar]
- 287.Cao W, Liu X, Bai T, Fan H, Hong K, Song H, et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with Coronavirus Disease 2019. Open Forum Infect Dis. (2020) 7:ofaa102. 10.1093/ofid/ofaa102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Emerson GG, Herndon CN, Sreih AG. Thrombotic complications after intravenous immunoglobulin therapy in two patients. Pharmacother J Hum Pharmacol Drug Ther. (2002) 22:1638–41. 10.1592/phco.22.17.1638.34125 [DOI] [PubMed] [Google Scholar]
- 289.Basta M. Intravenous immunoglobulin-related thromboembolic events–an accusation that proves the opposite. Clin Exp Immunol. (2014) 178 (Suppl 1):153–5. 10.1111/cei.12551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Wani J. Stroke in a young adult receiving intravenous immunoglobulin therapy for immune thrombocytopenic purpura. J Appl Hematol. (2016) 7:35–7. 10.4103/1658-5127.181112 [DOI] [Google Scholar]
- 291.Vucic S, Chong PST, Dawson KT, Cudkowicz M, Cros D. Thromboembolic complications of intravenous immunoglobulin treatment. Eur Neurol. (2004) 52:141–4. 10.1159/000081465 [DOI] [PubMed] [Google Scholar]
- 292.Morgan JC, Alhatou M, Oberlies J, Johnston KC. Transient ischemic attack and stroke associated with sildenafil (Viagra) use. Neurology. (2001) 57:1730–1. 10.1212/WNL.57.9.1730 [DOI] [PubMed] [Google Scholar]
- 293.Rufa A, Cerase A, Monti L, Dotti MT, Giorgio A, Sicurelli F, et al. Recurrent venous thrombosis including cerebral venous sinus thrombosis in a patient taking sildenafil for erectile dysfunction. J Neurol Sci. (2007) 260:293–5. 10.1016/j.jns.2007.05.011 [DOI] [PubMed] [Google Scholar]
- 294.Ruhela M, Bagarhatta R. Atrial fibrillation: a rare but probable adverse effect of sildenafil. Int J Basic Clin Pharmacol. (2018) 7:813. 10.18203/2319-2003.ijbcp20181192 [DOI] [Google Scholar]
- 295.Hahn I-H, Hoffman RS. Aroused to atrial fibrillation? Am J Emerg Med. (2000) 18:642. 10.1016/S0735-6757(00)90302-4 [DOI] [PubMed] [Google Scholar]
- 296.National Academies of Sciences, Engineering, and Medicine Health and Medicine, Division Board on Population Health and Public Health Practice, Committee on the Health Effects of Marijuana . Therapeutic effects of Cannabis and Cannabinoids. In: The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: National Academies Press; (2017). p. 85–93. [PubMed] [Google Scholar]
- 297.Khodadadi H, Salles ÉL, Jarrahi A, Chibane F, Costigliola V, Yu JC, et al. Cannabidiol modulates cytokine storm in acute respiratory distress syndrome induced by simulated viral infection using synthetic RNA. Cannabis Cannabinoid Res. (2020) 5:197–201. 10.1089/can.2020.0043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Mohammed A, FK Alghetaa H, Miranda K, Wilson K, P Singh N, Cai G, et al. Δ9-tetrahydrocannabinol prevents mortality from acute respiratory distress syndrome through the induction of apoptosis in immune cells, leading to cytokine storm suppression. Int J Mol Sci. (2020) 21:6244. 10.3390/ijms21176244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Salles ÉL, Khodadadi H, Jarrahi A, Ahluwalia M, Paffaro VA, Jr, Costigliola V, et al. Cannabidiol (CBD) modulation of apelin in acute respiratory distress syndrome. J Cell Mol Med. (2020) 24:12869–72. 10.1111/jcmm.15883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Fan X-F, Xue F, Zhang Y-Q, Xing X-P, Liu H, Mao S-Z, et al. The Apelin-APJ axis is an endogenous counterinjury mechanism in experimental acute lung injury. Chest. (2015) 147:969–78. 10.1378/chest.14-1426 [DOI] [PubMed] [Google Scholar]
- 301.Hackam DG. Cannabis and stroke: systematic appraisal of case reports. Stroke. (2015) 46:852–6. 10.1161/STROKEAHA.115.008680 [DOI] [PubMed] [Google Scholar]
- 302.Freeman MJ, Rose DZ, Myers MA, Gooch CL, Bozeman AC, Burgin WS. Ischemic stroke after use of the synthetic marijuana “spice.” Neurology. (2013) 81:2090–3. 10.1212/01.wnl.0000437297.05570.a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Barber PA, Pridmore HM, Krishnamurthy V, Roberts S, Spriggs DA, Carter KN, et al. Cannabis, ischemic stroke, and transient ischemic attack a case-control study. Stroke. (2013) 44:2327–9. 10.1161/STROKEAHA.113.001562 [DOI] [PubMed] [Google Scholar]
- 304.Desai R, Singh S, Patel K, Goyal H, Shah M, Mansuri Z, et al. Stroke in young cannabis users (18-49 years): National trends in hospitalizations and outcomes. Int J Stroke. (2020) 15:535–9. 10.1177/1747493019895651 [DOI] [PubMed] [Google Scholar]
- 305.Esse K, Fossati-Bellani M, Traylor A, Martin-Schild S. Epidemic of illicit drug use, mechanisms of action/addiction and stroke as a health hazard. Brain Behav. (2011) 1:44–54. 10.1002/brb3.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Mousavi S, Moradi M, Khorshidahmad T, Motamedi M. Anti-inflammatory effects of heparin and its derivatives: a systematic review. Adv Pharmacol Sci. (2015) 2015:507151. 10.1155/2015/507151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Mycroft-West C, Su D, Elli S, Guimond S, Miller G, Turnbull J, et al. The 2019 coronavirus (SARS-CoV-2) surface protein (Spike) S1 Receptor Binding Domain undergoes conformational change upon heparin binding. bioRxiv. (2020) 2020.02.29.971093. Available online at: https://www.biorxiv.org/content/10.1101/2020.02.29.971093v2
- 308.Zidane M, Schram MT, Planken EW, Molendijk WH, Rosendaal FR, van der Meer FJM, et al. Frequency of major hemorrhage in patients treated with unfractionated intravenous heparin for deep venous thrombosis or pulmonary embolism: a study in routine clinical practice. Arch Intern Med. (2000) 160:2369–73. 10.1001/archinte.160.15.2369 [DOI] [PubMed] [Google Scholar]
- 309.Cossette B, Pelletier M-E, Carrier N, Turgeon M, Leclair C, Charron P, et al. Evaluation of bleeding risk in patients exposed to therapeutic unfractionated or low-molecular-weight heparin: a cohort study in the context of a quality improvement initiative. Ann Pharmacother. (2010) 44:994–1002. 10.1345/aph.1M615 [DOI] [PubMed] [Google Scholar]
- 310.Warkentin TE. Heparin-induced thrombocytopenia in critically ill patients. Semin Thromb Hemost. (2015) 41:49–60. 10.1055/s-0034-1398381 [DOI] [PubMed] [Google Scholar]
- 311.Daviet F, Guervilly C, Baldesi O, Bernard-Guervilly F, Pilarczyk E, Genin A, et al. Heparin-induced thrombocytopenia in severe COVID-19. Circulation. (2020) 142:1875–7. 10.1161/CIRCULATIONAHA.120.049015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Lingamaneni P, Gonakoti S, Moturi K, Vohra I, Zia M. Heparin-Induced Thrombocytopenia in COVID-19. J Investig Med High Impact Case Rep. (2020) 8:2324709620944091. 10.1177/2324709620944091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Liu X, Zhang X, Xiao Y, Gao T, Wang G, Wang Z, et al. Heparin-induced thrombocytopenia is associated with a high risk of mortality in critical COVID-19 patients receiving heparin-involved treatment. medRxiv. (2020) 2020.04.23.20076851. Available online at: https://www.medrxiv.org/content/10.1101/2020.04.23.20076851v1
- 314.Fugate JE, Rabinstein AA. Update on Intravenous Recombinant Tissue Plasminogen Activator for Acute Ischemic Stroke. Mayo Clin Proc. (2014) 89:960–72. 10.1016/j.mayocp.2014.03.001 [DOI] [PubMed] [Google Scholar]
- 315.Doepp F, Sanad W, Schreiber S, Baumann G, Borges A. Left ventricular apical thrombus after systemic thrombolysis with recombinant tissue plasminogen activator in a patient with acute ischemic stroke. Cardiovasc Ultrasound. (2005) 3:14. 10.1186/1476-7120-3-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Caly L, Druce JD, Catton MG, Jans DA, Wagstaff KM. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. (2020) 178:104787. 10.1016/j.antiviral.2020.104787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Gilbert BW, Slechta J. A case of ivermectin-induced warfarin toxicity: first published report. Hosp Pharm. (2018) 53:393–4. 10.1177/0018578718758972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.van Heeckeren WJ, Sanborn SL, Narayan A, Cooney MM, McCrae KR, Schmaier AH, et al. Complications from vascular disrupting agents and angiogenesis inhibitors: aberrant control of hemostasis and thrombosis. Curr Opin Hematol. (2007) 14:468–80. 10.1097/MOH.0b013e3282a6457f [DOI] [PubMed] [Google Scholar]
- 319.Scavone C, Brusco S, Bertini M, Sportiello L, Rafaniello C, Zoccoli A, et al. Current pharmacological treatments for COVID-19: what's next? Br J Pharmacol. (2020) 177:4813–24. 10.1111/bph.15072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Zakarija A, Kwaan HC. Adverse effects on hemostatic function of drugs used in hematologic malignancies. Semin Thromb Hemost. (2007) 33:355–64. 10.1055/s-2007-976171 [DOI] [PubMed] [Google Scholar]
- 321.Zuo P-Y, Chen X-L, Liu Y-W, Xiao C-L, Liu C-Y. Increased risk of cerebrovascular events in patients with cancer treated with bevacizumab: a meta-analysis. PLoS ONE. (2014) 9:e102484. 10.1371/journal.pone.0102484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.van der Hooft CS, Heeringa J, van Herpen G, Kors JA, Kingma JH, Stricker BHC. Drug-induced atrial fibrillation. J Am Coll Cardiol. (2004) 44:2117–24. 10.1016/j.jacc.2004.08.053 [DOI] [PubMed] [Google Scholar]
- 323.Kaakeh Y, Overholser BR, Lopshire JC, Tisdale JE. Drug-induced atrial fibrillation. Drugs. (2012) 72:1617–30. 10.2165/11633140-000000000-00000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Tisdale JE, Chung MK, Campbell KB, Hammadah M, Joglar JA, Leclerc J, et al. Drug-induced arrhythmias: a scientific statement from the american heart association. Circulation. (2020) 142:e214–33. 10.1161/CIR.0000000000000905 [DOI] [PubMed] [Google Scholar]
- 325.Ramot Y, Nyska A, Spectre G. Drug-induced thrombosis: an update. Drug Saf. (2013) 36:585–603. 10.1007/s40264-013-0054-6 [DOI] [PubMed] [Google Scholar]
- 326.Hassan SA, Palaskas N, Kim P, Iliescu C, Lopez-Mattei J, Mouhayar E, et al. Chemotherapeutic agents and the risk of ischemia and arterial thrombosis. Curr Atheroscler Rep. (2018) 20:10. 10.1007/s11883-018-0702-5 [DOI] [PubMed] [Google Scholar]
- 327.Abdel-Qadir H, Ethier J-L, Lee DS, Thavendiranathan P, Amir E. Cardiovascular toxicity of angiogenesis inhibitors in treatment of malignancy: a systematic review and meta-analysis. Cancer Treat Rev. (2017) 53:120–7. 10.1016/j.ctrv.2016.12.002 [DOI] [PubMed] [Google Scholar]
- 328.Beinart G, Damon L. Thrombosis associated with L-asparaginase therapy and low fibrinogen levels in adult acute lymphoblastic leukemia. Am J Hematol. (2004) 77:331–5. 10.1002/ajh.20230 [DOI] [PubMed] [Google Scholar]
- 329.Lowe GDO. Hormone replacement therapy and cardiovascular disease: increased risks of venous thromboembolism and stroke, and no protection from coronary heart disease. J Intern Med. (2004) 256:361–74. 10.1111/j.1365-2796.2004.01400.x [DOI] [PubMed] [Google Scholar]
- 330.Martinelli I, Battaglioli T, Mannucci PM. Pharmacogenetic aspects of the use of oral contraceptives and the risk of thrombosis. Pharmacogenetics. (2003) 13:589–94. 10.1097/00008571-200310000-00002 [DOI] [PubMed] [Google Scholar]
- 331.Bushnell CD, Goldstein LB. Risk of ischemic stroke with tamoxifen treatment for breast cancer: a meta-analysis. Neurology. (2004) 63:1230–3. 10.1212/01.WNL.0000140491.54664.50 [DOI] [PubMed] [Google Scholar]
- 332.Santamarina RD, Besocke AG, Romano LM, Ioli PL, Gonorazky SE. Ischemic stroke related to anabolic abuse. Clin Neuropharmacol. (2008) 31:80–5. 10.1097/WNF.0b013e3180ed4485 [DOI] [PubMed] [Google Scholar]
- 333.Frankle MA, Eichberg R, Zachariah SB. Anabolic androgenic steroids and a stroke in an athlete: case report. Arch Phys Med Rehabil. (1988) 69:632–3. [PubMed] [Google Scholar]
- 334.Christou GA, Christou KA, Nikas DN, Goudevenos JA. Acute myocardial infarction in a young bodybuilder taking anabolic androgenic steroids: a case report and critical review of the literature. Eur J Prev Cardiol. (2016) 23:1785–96. 10.1177/2047487316651341 [DOI] [PubMed] [Google Scholar]
- 335.Akçakoyun M, Alizade E, Gündogdu R, Bulut M, Tabakci MM, Açar G, et al. Long-term anabolic androgenic steroid use is associated with increased atrial electromechanical delay in male bodybuilders. Biomed Res Int. (2014) 2014:451520. 10.1155/2014/451520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Esperón CG, López-Cancio ME, Bermejo PG, Dávalos EA. Chapter 89 - anabolic androgenic steroids and stroke. In: Preedy VRBT-N of DA and SM , editor. Neuropathology of Drug Addictions and Substance Misuse. San Diego, CA: Academic Press; (2016). p. 981–90. 10.1016/B978-0-12-800212-4.00089-3 [DOI] [Google Scholar]
- 337.Zivkovic S, Koh CH, Kaza N, Jackson CA. Antipsychotic drug use and risk of stroke and myocardial infarction: a systematic review and meta-analysis. BMC Psychiatry. (2019) 19:189. 10.1186/s12888-019-2177-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Pacher P, Kecskemeti V. Cardiovascular side effects of new antidepressants and antipsychotics: new drugs, old concerns? Curr Pharm Des. (2004) 10:2463–75. 10.2174/1381612043383872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Juang H-T, Chen P-C, Chien K-L. Using antidepressants and the risk of stroke recurrence: report from a national representative cohort study. BMC Neurol. (2015) 15:86. 10.1186/s12883-015-0345-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Trifirò G, Dieleman J, Sen EF, Gambassi G, Sturkenboom MCJM. Risk of ischemic stroke associated with antidepressant drug use in elderly persons. J Clin Psychopharmacol. (2010) 30:252–8. 10.1097/JCP.0b013e3181dca10a [DOI] [PubMed] [Google Scholar]
- 341.De FC. The role of serotonin in thrombogenesis. Clin Physiol Biochem. (1990) 8:40–9. [PubMed] [Google Scholar]
- 342.Laporte S, Chapelle C, Caillet P, Beyens M-N, Bellet F, Delavenne X, et al. Bleeding risk under selective serotonin reuptake inhibitor (SSRI) antidepressants: a meta-analysis of observational studies. Pharmacol Res. (2017) 118:19–32. 10.1016/j.phrs.2016.08.017 [DOI] [PubMed] [Google Scholar]
- 343.Meijer WEE, Heerdink ER, Nolen WA, Herings RMC, Leufkens HGM, Egberts ACG. Association of risk of abnormal bleeding with degree of serotonin reuptake inhibition by antidepressants. Arch Intern Med. (2004) 164:2367–70. 10.1001/archinte.164.21.2367 [DOI] [PubMed] [Google Scholar]
- 344.Hackam DG, Mrkobrada M. Selective serotonin reuptake inhibitors and brain hemorrhage: a meta-analysis. Neurology. (2012) 79:1862–5. 10.1212/WNL.0b013e318271f848 [DOI] [PubMed] [Google Scholar]
- 345.Fonseca AC, Ferro JM. Drug abuse and stroke. Curr Neurol Neurosci Rep. (2013) 13:325. 10.1007/s11910-012-0325-0 [DOI] [PubMed] [Google Scholar]
- 346.Westover AN, McBride S, Haley RW. Stroke in young adults who abuse amphetamines or cocaine: a population-based study of hospitalized patients. Arch Gen Psychiatry. (2007) 64:495–502. 10.1001/archpsyc.64.4.495 [DOI] [PubMed] [Google Scholar]
- 347.Tsatsakis A, Docea AO, Calina D, Tsarouhas K, Zamfira L-M, Mitrut R, et al. A mechanistic and pathophysiological approach for stroke associated with drugs of abuse. J Clin Med. (2019) 8:1295. 10.3390/jcm8091295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Cantu C, Arauz A, Murillo-Bonilla LM, López M, Barinagarrementeria F. Stroke associated with sympathomimetics contained in over-the-counter cough and cold drugs. Stroke. (2003) 34:1667–72. 10.1161/01.STR.0000075293.45936.FA [DOI] [PubMed] [Google Scholar]
- 349.Lafaurie M, Olivier P, Khouri C, Atzenhoffer M, Bihan K, Durrieu G, et al. Myocardial infarction and ischemic stroke with vasoconstrictors used as nasal decongestant for common cold: a French pharmacovigilance survey. Eur J Clin Pharmacol. (2020) 76:603–4. 10.1007/s00228-019-02807-w [DOI] [PubMed] [Google Scholar]
- 350.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. (2020) 18:1023–6. 10.1111/jth.14810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Patell R, Bogue T, Koshy A, Bindal P, Merrill M, Aird WC, et al. Postdischarge thrombosis and hemorrhage in patients with COVID-19. Blood. (2020) 136:1342–6. 10.1182/blood.2020007938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Musoke N, Lo KB, Albano J, Peterson E, Bhargav R, Gul F, et al. Anticoagulation and bleeding risk in patients with COVID-19. Thromb Res. (2020) 196:227–30. 10.1016/j.thromres.2020.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Corrales-Medina VF, Alvarez KN, Weissfeld LA, Angus DC, Chirinos JA, Chang C-CH, et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. (2015) 313:264–74. 10.1001/jama.2014.18229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Boehme AK, Ranawat P, Luna J, Kamel H, Elkind MSV. Risk of acute stroke after hospitalization for sepsis: a case-crossover study. Stroke. (2017) 48:574–80. 10.1161/STROKEAHA.116.016162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Boehme AK, Luna J, Kulick ER, Kamel H, Elkind MSV. Influenza-like illness as a trigger for ischemic stroke. Ann Clin Transl Neurol. (2018) 5:456–63. 10.1002/acn3.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Wu Q, Zhou L, Sun X, Yan Z, Hu C, Wu J, et al. Altered lipid metabolism in recovered SARS patients twelve years after infection. Sci Rep. (2017) 7:9110. 10.1038/s41598-017-09536-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Rothlisberger JM, Ovbiagele B. Antiplatelet therapies for secondary stroke prevention: an update on clinical and cost-effectiveness. J Comp Eff Res. (2015) 4:377–84. 10.2217/cer.15.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Iannacone M, Sitia G, Isogawa M, Whitmire JK, Marchese P, Chisari FV, et al. Platelets prevent IFN-alpha/beta-induced lethal hemorrhage promoting CTL-dependent clearance of lymphocytic choriomeningitis virus. Proc Natl Acad Sci USA. (2008) 105:629–34. 10.1073/pnas.0711200105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Iannacone M, Sitia G, Narvaiza I, Ruggeri ZM, Guidotti LG. Antiplatelet drug therapy moderates immune-mediated liver disease and inhibits viral clearance in mice infected with a replication-deficient adenovirus. Clin Vaccine Immunol. (2007) 14:1532–5. 10.1128/CVI.00298-07 [DOI] [PMC free article] [PubMed] [Google Scholar]