Abstract
Objectives:
Examine the social influence of adult children on the cardiovascular-related health behaviors of older South Asian (SA) immigrants to inform lifestyle interventions.
Design:
This mixed-methods study used data from an ancillary study of social networks (2014–2018) in the Mediators of Atherosclerosis in South Asians Living in America cohort. Phase 1 was a quantitative analysis of self-reported diet and physical activity among SA adults (n=448, mean age=58 years, SD 8.4) who named at least one adult child to their social network. The Alternative Healthy Eating Index (AHEI) was used to measure parents’ diet; higher numbers indicate a healthier diet (range 0–110). Phase 2 was a thematic content analysis of in-depth qualitative interviews from a subsample of these parents (n=23, mean age=55, SD 7.6).
Results:
Parents with an adult child in their network who consumed uncooked vegetables daily had mean parental AHEI score 1.5 points higher (adjusted p-value=0.03) than those who had a child in the network who ate uncooked vegetables less often. When at least one adult child in their network ate fresh fruit daily compared to less frequently or when at least one child ate non-SA food daily compared to less frequently, mean parental AHEI scores were higher by 2.0 (adjusted p-value=0.01) and 1.6 (adjusted p-value=0.03) points respectively. Parents with an adult child in their network who exercised at least weekly were more likely to meet guideline-recommended physical activity levels than parents with children who exercised less often (76% v. 56%, adjusted p-value=0.02). Adult children provided social support and were seen as ‘role models’ for healthy behavior, especially when adopting Western health behaviors.
Conclusion:
Positive role modeling and support from adult children were important facilitators of healthy behavior change in older SA immigrants and can inform health behavior interventions for SA adults.
Keywords: social network, social influence, South Asian, MASALA, lifestyle intervention, intergenerational
Introduction
The benefits of social support on health have been widely acknowledged—higher levels of support have been linked with better physical and mental health (Falk et al. 1992; Berkman, Leo-Summers, and Horwitz 1992; Cohen 2004; Uchino 2004). Though a variety of relationship types and minority groups have been studied, very few studies have examined how social support influences the health of South Asians in the United States, an ethnic group with high levels of chronic diseases such as type 2 diabetes, hypertension, and heart disease (Talegawkar et al. 2017; Joshi et al. 2007; Palaniappan, Wang, and Fortmann 2004; Jose et al. 2014; A.M. Kanaya et al. 2010). Prior studies of social support in Asian Americans, which often aggregated all Asian Americans together, used both qualitative approaches and social network analyses to show that Asian Americans had family- and friend-centered social networks, relied on these networks for information about health, and had better physical and mental health if they had higher levels of support (Kim, Kreps, and Shin 2015; Jang, Yoon, and Park 2018; You et al. 2018; Rollock and Lui 2016). There have been few studies about social support and health in the South Asian subgroup of Asian Americans. The present study examined the role of adult children as an important source of social support and social influence on middle-age and older South Asian adults’ health behaviors and fills a critical gap in research on social support and minority health.
In 2017, there were 5.4 million South Asians in the United States and the ethnic group grew by 40% between 2010 and 2017 (SAALT 2019). South Asians face unique health challenges—a higher risk of cardiovascular disease, type 2 diabetes, and heart disease than non-Hispanic Whites and other Asian ethnic groups (Talegawkar et al. 2017; Joshi et al. 2007; A.M. Kanaya et al. 2010; Jose et al. 2014; Palaniappan, Wang, and Fortmann 2004). Prior data from the MASALA Study (Kandula et al. 2018) used egocentric social network analysis to show that South Asian social networks were highly family-centered, and that middle-aged and older South Asians with more family members in their network were more likely to have discussions about health with their network. Approximately 80% of participants said they could rely on adult children for social support, compared to 94% who said that about their spouses, and 66% who said they could rely on siblings, friends, or other relatives. These preliminary data suggested that adult children play a vital role in their parents’ lives, but almost no research has been done on the social influence of adult children on older South Asians.
In other ethnic groups, social network members influence health through provision of both social support and social influence. In the field of epidemiology, the relationship between social support and health has been extensively studied, and there are consistent finding that higher levels of social support improved mental and physical health, and decreased mortality (Falk et al. 1992; Berkman, Leo-Summers, and Horwitz 1992; Cohen 2004; Rosengren et al. 1993; Uchino 2004). In one meta-analysis of 122 studies, higher levels of social support and family cohesiveness were associated with increased adherence to medication regimens (DiMatteo 2004). Conversely, in a study using multivariate analysis, lower levels of social support negatively influenced chronic disease outcomes (Angerer et al. 2000).
In addition to social support, a separate but connected entity—social influence—must be considered when planning behavioral interventions. While social support is the actual support provided or the perception that one is receiving support, social influence is the effect of social relationships on behavior, thoughts, or emotions, and it operates via social support, role modeling or companionship. Thus, social support can lead to social influence on health-related behaviors (e.g. smoking, exercise or diet), but other forms of influence can also affect behavior even without direct provision of social support. For example, in a study of over 2,500 participants and a mean follow-up of 7.3 years, when members of a social network were less active and more sedentary, overall health worsened and mortality increased, an effect that may have been mediated through role modeling (Brummett et al. 2005).
Leveraging social networks in health behavior interventions requires identifying network members who have influence over specific behaviors (Latkin and Knowlton 2015). Familism, in which the needs of the family are more important than the needs of the individual, has been identified as a prominent cultural value in South Asian culture across both focus group and other qualitative fields of research, so family members may be especially salient for behavior change (Lamb 2009; Mukherjea et al. 2013). Despite this, little research has been done on social networks and health in this ethnic group. Further, as individuals in the U.S. live longer and the aging population grows, the role of adult children on their parents’ health merits in-depth study and clarification.
Looking specifically at the relationship between adult children and their parents, several quantitative studies have identified three main factors that influence the provision of support; 1) filial obligation, 2) reciprocity of social support, and 3) the ‘spill-over effect’ of healthy behaviors (Lorca and Ponce 2015; Thomas 2009; Yahirun, Sheehan, and Hayward 2017; Torssander 2013). Filial obligation was defined as the provision of support out of obligation or duty—often thought to be influenced by societal norms (Lorca and Ponce 2015; Thomas 2009). Reciprocity was defined as the give and take between two individuals in a relationship, such that adult children who received more support from their parents were more likely to return that support as well. The ‘spill-over effect’ posited that when adult children take part in healthy behaviors, their parents imitate or adopt those behaviors as well (Yahirun, Sheehan, and Hayward 2017; Torssander 2013).
Despite these theories of social influence, the effect of support from adult children on parental health has been indeterminate—some research has shown a negative effect on psychological well-being (Reczek and Zhang 2016), while other research has shown increased parental longevity and improved health (Torssander 2013; Friedman and Mare 2010). The form of social support offered and the reciprocity of support appeared to be essential in mediating adult children’s influence on their parents’ health. Studies showed that emotional support from adult children was more beneficial than informational support, and that providing support to adult children rather than receiving it improved subjective well-being (Lang and Schütze 2002; Reczek and Zhang 2016; Thomas 2009). Further, the ‘spill-over effect’ of healthy behaviors from adult children to parents mediated improved parental longevity and health through changes in exercise and smoking habits—especially in relationships where adult children had higher levels of education and more health-related knowledge than their parents (Yahirun, Sheehan, and Hayward 2017; Torssander 2013; Friedman and Mare 2010). Few have studied the role of adult children on the health of aging ethnic minorities, including South Asians, who have unique social and cultural contexts that influence the parent-child relationship.
One community-based dialogue showed that older South Asian immigrants were less independent, had lost part of their extended social network upon immigrating to America, relied on family members most when they were uncomfortable with English, and viewed their health in the context of family-based discussions (Puvar and Kalayil 2019). A small qualitative study utilizing semi-structured interviews (Sharma and Kemp 2012) examined 10 older South Asians and the role their adult children played in their health, focusing on filial piety, which they defined as the ‘long-term bonds of intergenerational reciprocity and affection, in which juniors provide care for their senior parents in old age. Sharma and Kemp studied the provision of emotional and instrumental (help with bathing, eating, and other activities of daily living) support; the traditional sense of filial piety was modified to accommodate for American values, but the underlying principle of filial piety persisted. They highlighted the reciprocity of support—parents helped their children with cooking or childcare and, in return, received financial support, emotional support, companionship or assistance with health issues. However, Sharma and Kemp did not study other forms of social support or evaluate social influence on concrete parental health behaviors such as diet and exercise.
We hypothesized that the role of adult children in their parents’ diet and exercise may be magnified by the unique position of adult children in the context of immigration (See Figure 1 for conceptual model). Upon immigration, older South Asians lose extended social networks and many face language barriers, resulting in an increased reliance on the nuclear family. In this context, children may be important sources of support and advice. Further, the adult children who were born in the U.S. or immigrated as children may be uniquely situated to provide new information about Western cultural attitudes and health norms in a way that social network members of the same age and acculturation level (spouses, siblings) cannot. This study aimed to understand the role and influence of adult children on the diet and exercise behaviors of older South Asian immigrants in the context of culture and immigration, specifically addressing 1) the ‘spill-over effect’ of healthy behaviors from adult children to their parents and 2) the reciprocity of social support between parent and child.
Figure 1.
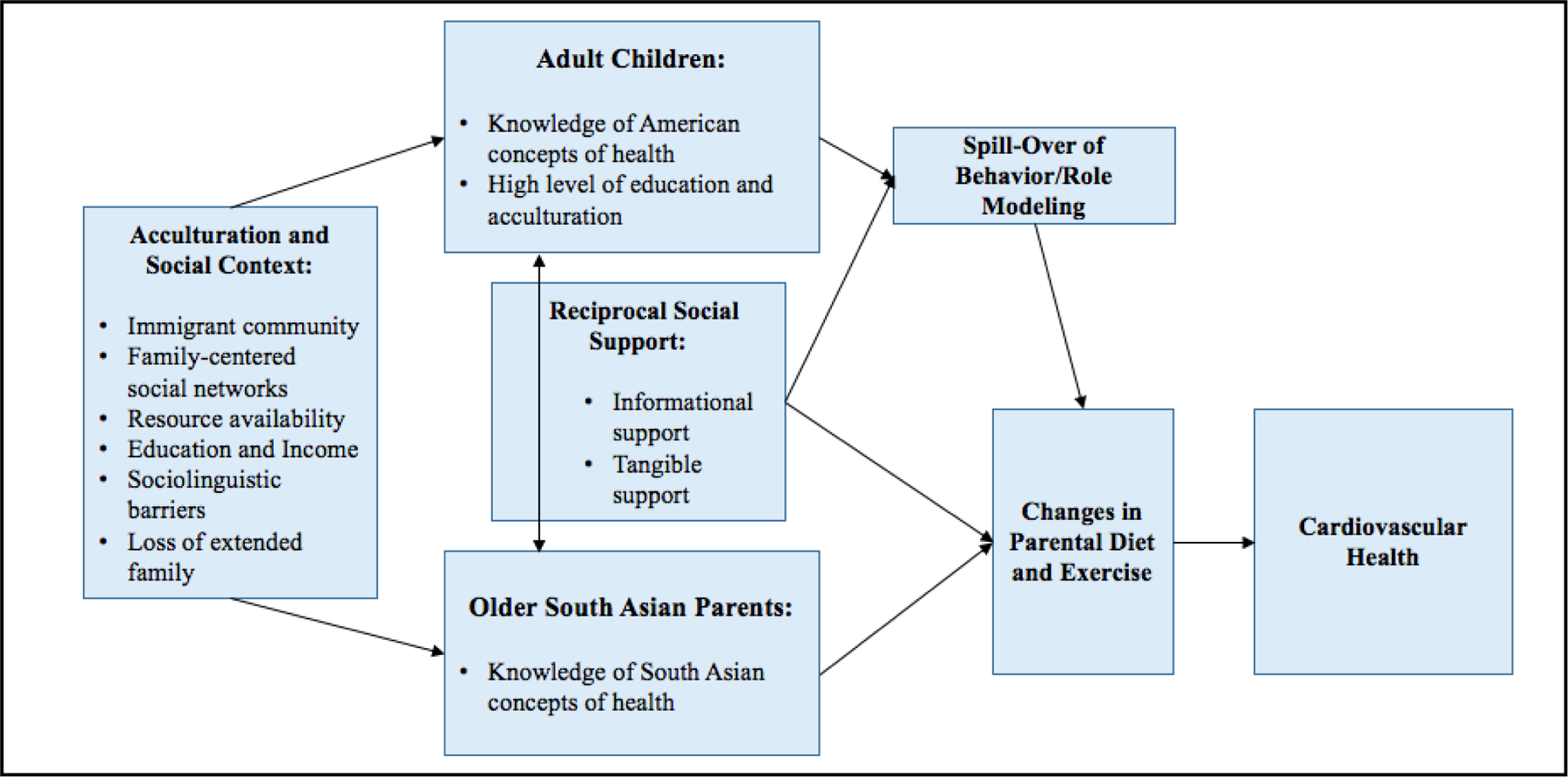
Conceptual Model of Impact of Adult Children on Diet and Exercise in South Asians.
Methods
Study Design
This mixed-methods study used a sequential explanatory design with two phases (Dominguez and Hollstein 2014). In Phase 1, a quantitative questionnaire elicited information about the MASALA participants’ (the parents’) social networks. In Phase 2, semi-structured interviews with a subset of parents obtained more detailed information about the social network and the parent-child relationship. Quantitative and qualitative data were then integrated, a key component of mixed-methods studies, which allowed for greater understanding and generalizability of findings from either type of data alone (Dominguez and Hollstein 2014).
Participants
The Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study is a community-based cohort of 906 South Asians (individuals from India, Pakistan, Bangladesh, Nepal, and Sri Lanka) living in the San Francisco Bay Area and seven census tracts close to Chicago, IL (age range 40–84 y, 46% women, 98% foreign-born). All participants were free of clinically-evident cardiovascular disease (e.g. heart attack, stroke, at baseline). Details regarding recruitment and baseline measurements such as education, income, age, marital status, birthplace, number of years living in the U.S., and religion were collected on all participants and have been described previously (Kanaya et al. 2013).
Phase 1—Quantitative
Participant Sample:
From 2014–2018, MASALA study participants were re-enrolled for an ancillary mixed-methods study of social networks. A total of 771 participants completed the quantitative egocentric network questionnaire. Phase 1 data were derived from the 448 participants who named an adult child to their social network in the quantitative questionnaire. The 448 participants who named adult children to their network were termed ‘parents’ for this study.
Data Collection:
Social network characteristics were obtained on parents using a standard egocentric approach in which the parent reported information on all their personal network members. A name generator that has been used by the General Social Survey (McPherson, Smith-Lovin, and Brashears 2006, years 1985 and 2004) as well as the National Social Life, Health, and Aging Project (Cornwell et al. 2009) was used to identify important network members. Parents were asked to name up to 10 people with whom they could discuss ‘important matters.’ This was followed by questions designed to collect detailed information about the first five network members who were listed. Specifically, parents were asked to characterize the type of relationship, the sociodemographic characteristics of network members (including age, education, number of years living in the U.S., and birthplace), the strength of the relationship (through emotional closeness and frequency of contact), the functions of network members, the discussion topics between participant and network member, and the frequency of communication between network members. The children were not contacted for participation in the study.
Limiting the responses to five network members is a typical approach to reduce burden and still elicit information about key individuals who influence parents’ health. Network measurements have been reported previously, and included size, composition, organizational affiliations, social support functions, and network members’ behaviors (Kandula et al. 2018).
Measures:
Social Network Exposure:
The social network exposure for the quantitative analysis was operationalized as having a child in the personal social network who a) exercised daily/weekly compared to having a child in the network who did not exercise at least daily/weekly and b) having a child in the network who ate certain foods daily compared to a child who did not eat those foods daily.
A conceptual model illustrating how adult children influence their parents’ health in the context of South Asian culture and the immigrant experience was used to drive the selection of outcomes and analyses (see Figure 1).
Outcomes—Parental Diet and Exercise:
The outcomes of interest included parental diet and parental exercise.
To measure diet, we used the Alternative Healthy Eating Index (AHEI), which includes 11 food components with scores ranging from 0 to 10 for each component, as a measure of diet quality. Dietary assessment was based on intake reported by parents on the validated Study of Health Assessment and Risk in Ethnic Groups (SHARE) Food Frequency Questionnaire, an instrument developed for South Asians in North America (Kelemen et al. 2003). AHEI scores were modeled on a continuous scale, and could range from 0 to 110, with higher AHEI scores indicating a higher quality diet (Chiuve et al. 2012).
Exercise was measured by self-report with the Cross-Cultural Activity Participation Study (Ainsworth et al. 1999). This study looked at self-reported exercise such as walking, dancing, sports, and swimming. Survey responses were used to calculate metabolic (MET)-minutes per week (with one MET defined as the energy consumed while sitting quietly). National guidelines in the U.S. recommend a minimum of 500 – 1000 MET-minutes per week of exercise (Nelson et al. 2007; “Appendix 1 – 2008 Physical Activity Guidelines - Health.Gov” 2008), and parents were further categorized as meeting or not meeting exercise recommendations (≥500 MET minutes per week).
Covariates:
Information on participant age, gender, study site, education level, income category and Traditional Cultural Beliefs Scale Score were collected at the baseline study visit (2010–2013) as previously described (Kanaya et al. 2013) and were included as covariates in regression analyses. Adjustments were made for age and gender because both affect exercise and diet independently from the parent-child dyad. The Chicago and San Francisco study sites also differ in health-related behaviors including diet and exercise. Education level and income category were included as covariates to control for the effect of socioeconomic status on exercise and diet. The Traditional Cultural Beliefs Scale is a previously validated scale ranging from 0 to 28 with lower scores reflecting stronger South Asian traditional cultural beliefs and higher scores reflecting weaker cultural beliefs. It was used as a covariate in this study to account for the effect of acculturation on diet and exercise.
Analyses:
Bivariate associations of lifestyle behaviors with network exposures were examined and descriptive statistics (means and proportions) were calculated for variables of interest, including parent characteristics, social network characteristics and child characteristics. We used multivariable linear regression to examine the association between having a child in the social network who ate certain foods at least daily (ie: uncooked vegetables, fresh fruit, non-South Asian food) with parental AHEI scores.
Similarly, we used multivariable logistic regression to examine whether having a child in the social network who exercised regularly (daily or daily/weekly) was associated with meeting exercise recommendations.
T-tests were used to compare continuous measures, and Chi-squared or Fisher’s exact tests were used to compare categorical variables. All statistical tests were performed using two-sided tests with α = 0.05 and were conducted using SAS, version 9.4 (SAS Institute; Cary, NC).
Phase 2—Qualitative
Participant Sample:
Of the original 771 participants who completed the quantitative egocentric network questionnaire, 43 participants completed additional, in-depth interviews to provide context and perspectives on their social networks and health. Participants were chosen to ensure adequate representation of men and women, various age groups, and small and large social networks. Phase 2 data were derived from the 23 participants who both named an adult child to their personal social network and completed an in-depth interview (see Figure 2). These 23 participants are a subset of the 448 parents analyzed in Phase 1, and are also termed ‘parents’ in this study.
Figure 2.
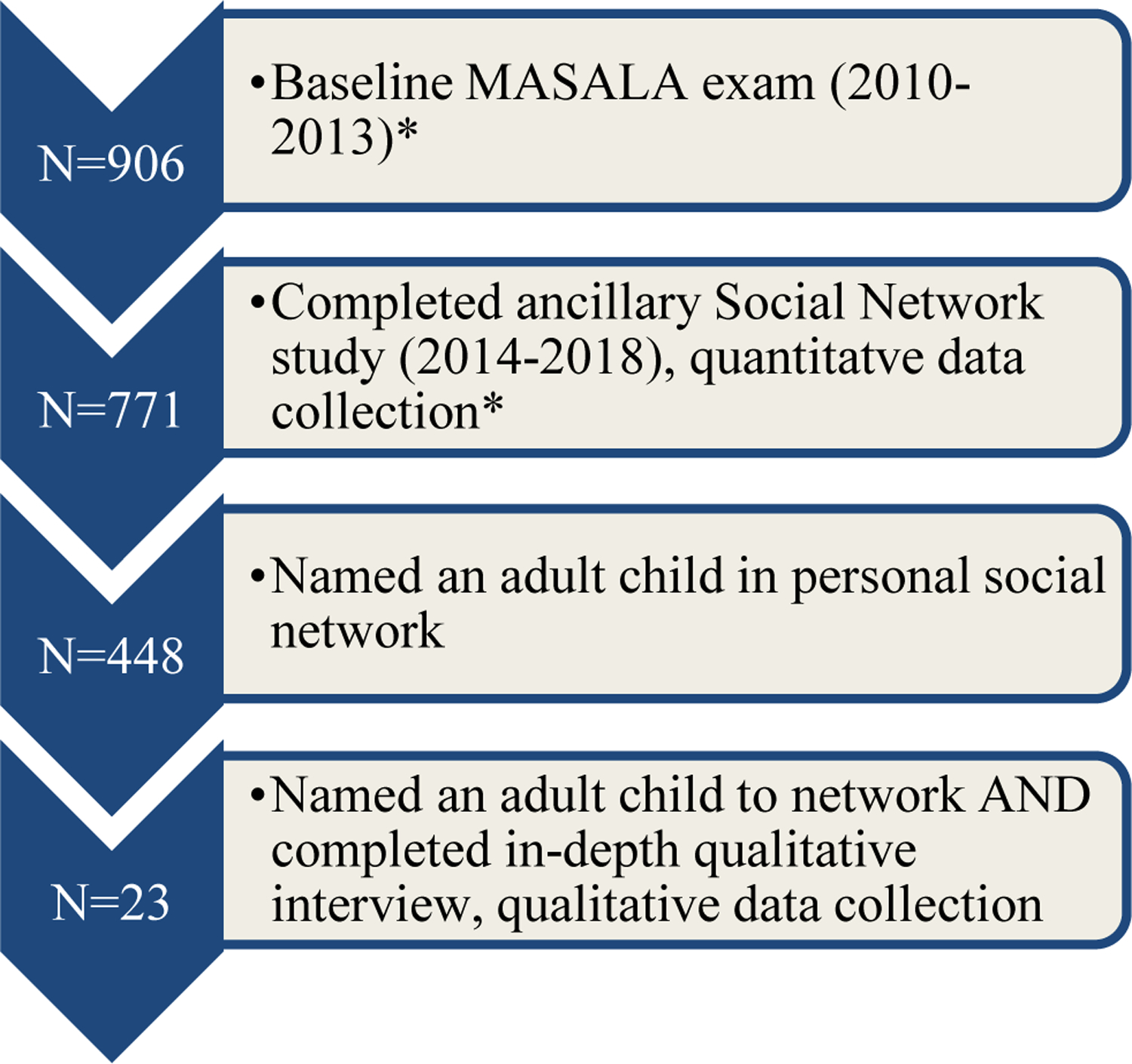
Diagram of Quantitative and Qualitative Data Collection
* This paper only included data on those who named and adult child to the network.
Data Collection:
Interviewers used a semi-structured interview guide that was developed by the research team using literature on the social and interpersonal processes that shape diet, exercise and health. Questions were designed to elicit information about health-related social support and social influence from network members and how those factors related to participants’ health behaviors. All interviews were conducted in English, Hindi or Urdu by trained interviewers. First, participants were asked to discuss their general relationship with each member of the network and how these individuals influenced their health and behaviors. Next, they were asked about the types of social support they received from each network member. Finally, they were asked about network members’ health behaviors and who they considered to be most important in maintaining their family’s health.
Data Analysis:
Qualitative interviews were conducted, recorded, translated and transcribed. Codes were created following the thematic analysis framework, with at least two co-authors (AR, SD, MM, AP-T, SM, or NK) coding each interview in NVivo (QSR International). Discrepancies were resolved by discussion and consensus among members of the research team. Codes were cross-referenced using the matrix feature in NVivo to identify major themes in the context of a conceptual model illustrating how adult children influence their parents’ health within the South Asian immigrant experience (see Figure 1). Themes were then confirmed in the full context of each interview, and finalized through discussion among the research team (primarily AR, SD and NK).
Results
Sample Characteristics
Parents (n=448) averaged 58 years old (SD 8.43), 48% were women, 89% were married, and 88% obtained a bachelor’s degree or higher. The majority (91%) were born in South Asia, and 62% had lived in the US for greater than 25 years. Social networks had a high proportion of family (81%) and South Asians (92%). Compared to parents who named adult children to their social networks but did not complete in depth interviews (n=425), those who did complete in depth interviews (n=23) had similar demographic characteristics (See Table 1).
Table 1.
Demographic characteristics of South Asian parents (participants who named at least one adult child to their social network), MASALA Study 2014–2018
| Characteristic | All parents (N=448) | Parents who did not complete the qualitative interview (N=425) | Parents who completed in-depth interview (N=23) | P-value | |
|---|---|---|---|---|---|
| N (%) or Mean (SD) | N (%) or Mean (SD) | N (%) or Mean (SD) | |||
| Age, years; Mean (SD) | 58.22 (8.43) | 58.39 (8.45) | 55.22 (SD 7.66) | 0.08 | |
| Women, N (%) | 215 (48%) | 202 (48%) | 13 (57%) | 0.40 | |
| Education | < Bachelor’s Degree | 55 (12%) | 51 (12%) | 4 (17%) | 0.65 |
| Bachelor’s Degree | 125 (28%) | 120 (28%) | 5 (22%) | ||
| > Bachelor’s Degree | 268 (60%) | 254 (60%) | 14 (61%) | ||
| Family Income | < $75k | 118 (26%) | 112 (26%) | 6 (26%) | 0.45 |
| $75–100k | 42 (9%) | 42 (10%) | 0 (0%) | ||
| > 100k | 273 (61%) | 257 (61%) | 16 (70%) | ||
| Unknown | 15 (3%) | 14 (3%) | 1 (4%) | ||
| Married, N (%) | 398 (89%) | 375 (88%) | 23 (100%) | 0.08 | |
| Years lived in the US* | <15 years | 62 (14%) | 58 (14%) | 4 (17%) | 0.84 |
| 15–25 years | 110 (25%) | 104 (25%) | 6 (26%) | ||
| >25 years | 276 (62%) | 263 (62%) | 13 (57%) | ||
| Percent of life in US, N (%)* | <50% | 251 (56%) | 238 (56%) | 13 (57%) | 0.96 |
| >=50% | 197 (44%) | 187 (44%) | 10 (43%) | ||
| Birthplace, N (%) | India | 394 (88%) | 372 (87.5%) | 22 (96%) | 0.85 |
| Pakistan | 12 (3%) | 11 (2.6%) | 1 (4%) | ||
| Bangladesh | 1 (0.2%) | 1 (0.2%) | 0 | ||
| Nepal | 1 (0.2%) | 1 (0.2%) | 0 | ||
| Sri Lanka | 3 (0.7%) | 3 (0.7%) | 0 | ||
| Other | 34 (8%) | 34 (7.6%) | 0 | ||
| United States | 3 (0.7%) | 3 (0.7%) | 0 | ||
| Network Parameters** | Network size; Mean (SD) | 5.81 (2.48) | 5.81 (2.50) | 5.91 (SD 2.17) | 0.33 |
| Proportion relatives; Mean (SD) | 0.81 (0.21) | 0.81 (0.21) | 0.78 (SD 0.22) | 0.50 | |
| Proportion South Asian; Mean (SD) | 0.92 (0.19) | 0.92 (0.19) | 0.92 (SD 0.15) | 0.89 | |
| Proportion female; Mean (SD) | 0.57 (0.23) | 0.57 (0.23) | 0.52 (SD 0.30) | 0.30 | |
| Closeness to alters; Mean (SD) | 4.53 (0.45) | 4.52 (0.46) | 4.58 (0.42) | 0.54 | |
For those born outside of US in total cohort
Network parameters included: size; proportion of network made up of related individuals, South Asians, and women; and closeness to alters (parents rated closeness to each network member on scale 1–5).
Children (n=720) averaged 32 years old (SD 9), 48% were women, 91% spent more than half their life in the U.S., and 85% obtained a bachelor’s degree or higher. The proportion of children who were female was significantly higher for the group of parents who completed qualitative interviews (n=34, 65%) compared to those that did not (n=686, 47%), but otherwise were demographically similar (See Table 2).
Table 2.
Demographic characteristics of adult children (named to social networks by parents), MASALA Study 2014–2018
| Characteristic | All adult children named to social network (N=720) | Adult children named to social network who did not complete the qualitative interview (N=686) | Adult children named to social network and discussed during in-depth interviews (N=34) | P-value | |
|---|---|---|---|---|---|
| N (%) or Mean (SD) | N (%) or Mean (SD) | N (%) or Mean (SD) | |||
| Age, years; Mean (SD) | 32 (SD 9) | 33 (SD 9) | 30 (SD 7) | 0.20 | |
| Female, N (%) | 345 (48%) | 323 (47%) | 22 (65%) | 0.04 | |
| Education* | < Bachelor’s Degree | 97 (14) | 103 (14%) | 6 (17%) | 0.29 |
| Bachelor’s Degree | 249 (37) | 257 (36%) | 8 (24%) | ||
| > Bachelor’s Degree | 332 (49) | 352 (49%) | 20 (59%) | ||
| U.S. born | 398 (58) | 417 (58%) | 19 (56%) | 0.81 | |
| Years Living in US | <15 years | 49 (7) | 51 (7%) | 2 (6%) | 0.96 |
| 15–25 years | 254 (37) | 267 (37%) | 13 (38%) | ||
| >25 years | 383 (56) | 402 (56%) | 19 (56%) | ||
| Percent of life in the U.S. | >=50% | 618 (90%) | 652 (91%) | 34 (100%) | 0.05 |
| <50% | 68 (10%) | 68 (9%) | 0 (0%) | ||
| Current Location | U.S. | 662 (97%) | 696 (97%) | 34 (100%) | 0.54 |
| South Asia | 4 (1%) | 4 (1%) | 0 (0%) | ||
| Other country | 20 (3%) | 20 (3%) | 0 (0%) | ||
Missing for 8 children in total cohort
Phase 1 Findings—Quantitative Data
Among MASALA participants who named children to their network, the mean AHEI score was 74.3 (SD 7.0). Quantitative data is summarized in Table 3. Parents with at least one adult child in the network who ate non-South Asian food daily had higher AHEI scores compared to parents whose children did not eat non-SA food daily (mean AHEI score 75.3 versus 73.4, 95% CI 0.2–2.9). Similarly, parents with at least one adult child in the network who ate uncooked vegetables daily had higher AHEI scores than parents whose children did not eat uncooked vegetables daily (mean AHEI score 75.2 versus 73.4, 95% CI 0.2–2.8). Finally, parents with at least one adult child in the network who ate fresh fruits daily had higher AHEI scores than parents whose children did not eat fresh fruits daily (mean AHEI score 74.8 versus 73.0, 95% CI 0.5–3.5). There were no significant differences between parental AHEI scores based on whether their children ate South Asian food or cooked vegetables daily. The data also did not demonstrate differences in parental AHEI scores based on adult children’s daily consumption of unhealthy foods, , including processed foods, sugar-sweetened beverages and diet drinks, though the prevalence of these behaviors was low among the children.
Table 3.
Mean parental AHEI and children’s dietary and exercise behaviors
| Raw Scores by Group | Unadjusted Model | Adjusted ModelƗ | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Network member who eats… | Number of parents whose adult child meets behavior, N (%) | Mean AHEI score for parents whose child meets behavior (SD) | Mean AHEI Score for parents whose child does not meet behavior (SD) |
Linear Regression Modeling AHEI Score
|
||||
| Beta | 95% CI | Beta | 95% CI | |||||
| South Asian Food Daily | 183 (41%) | 73.6 (6.2) | 74.7 (7.4) | −1.1 | (−2.4, 0.3) | −0.7 | (−2.2, 0.8) | |
| Non-South Asian Food Daily | 205 (46%) | 75.3 (7.0) | 73.4 (6.8) | 1.9 | (0.6, 3.2)** | 1.6 | (0.2, 2.9) * | |
| Raw Vegetables Daily | 222 (50%) | 75.1 (6.5) | 73.4 (7.3) | 1.7 | (0.4, 3.0)* | 1.5 | (0.2, 2.8) * | |
| Cooked Vegetables Daily | 331 (74%) | 74.6 (6.7) | 73.5 (7.7) | 1.1 | (−0.4, 2.6) | 0.9 | (−0.6, 2.5) | |
| Fresh Fruit Daily | 314 (70%) | 74.8 (6.4) | 72.9 (8.1) | 1.9 | (0.5, 3.3)** | 2.0 | (0.5, 3.5) ** | |
| Diet Drinks Daily | 58 (13%) | 72.8 (7.2) | 74.5 (6.9) | −0.9 | (−4.2, 2.4) | −0.1 | (−3.4, 3.2) | |
| Sugar Sweetened Beverages Daily | 18 (4%) | 73.4 (9.1) | 74.3 (6.9) | −1.7 | (−3.7, 0.2) | −1.2 | (−3.2, 0.8) | |
| Processed or Packaged Food Daily | 9 (2%) | 74.1 (7.3) | 74.3 (7.0) | −0.2 | (−4.8, 4.5) | −1.4 | (−6.0, 3.2) | |
| Network member who… | Number of parents whose child meets behavior, N (%) | Parent meets exercise recommendations and has child who meets behavior N (%) |
Parent meets exercise recommendations but their child does not meet behavior N (%) |
Logistic Regression Modeling Probability of Ego Meeting Exercise Requirements
|
||||
| Odds ratio | 95% CI | Odds ratio | 95% CI | |||||
| Exercises Daily or Weekly | 395 (88) | 301 (76) | 30 (58) | 2.4 | (1.3, 4.3)*** | 2.1 | (1.1, 4.0) * | |
Adjusted for parental age, gender, study site, education level, income, Traditional Cultural Beliefs Scale Score
p<0.05
p<0.01
p<0.001
Among parents with any adult child in the network who exercised daily or weekly, 76% of parents met exercise recommendations of ≥ 500 MET-minutes/week, compared to 58% who had an adult child in the network who did not exercise at least weekly (OR 2.1, 95% CI 1.1–4.0).
Phase 2 Findings—Qualitative Data
Three major themes were identified from interview data: 1) adult children provided various forms of social support to parents, 2) social influence manifested as the ‘spill-over effect,’ and 3) social support was reciprocal between parent and child. These major themes, as well as number of parents to voice each theme, are listed in Table 4.
Table 4.
Major themes related to social support and influence in the South Asian parent-adult child relationship, MASALA Study 2014–2018
| Major Theme | Number of Parents Voicing Theme (% of total) | Illustrative Quote |
|---|---|---|
| Forms of Social Support | ||
| Emotional Support | 14 (61%) | ‘Even when she was younger [she] was always wise, but kind of gives me matter of fact, good advice.’ –SA, a 56 year old woman. |
| Informational Support | 13 (57%) | ‘My son tells me, in the morning to eat a big breakfast and not to [eat] any snacks in between and just if you’re eating, eat some vegetable snack or fruit snack because cookies also have lots of carbs and things, lot of sugar.’ –EA, a 56 year old woman. |
| Companionship and Accountability | 13 (57%) | ‘Back when I was in a better routine of going for a jog and I used to go with [my daughter] we used to do it a lot more frequently because we would kind of encourage each other to go. And you know sometimes I would be in the mood to go or sometimes she would be in the mood to go…it’s easier you know, because then you have company.’ –TS, a 44 year old woman. |
| Instrumental Support | 12 (52%) | ‘If I have a headache or, like right now I have shoulder pain and so, I told her and she will suggest ‘Go to this doctor,’ or she will do some research and tell me ‘You just call this number,’ and sometimes she takes appointment for me, also.’ –MS, a 59 year old man. |
| Social Influence | ||
| Children as Role Models | 17 (74%) | ‘He’s so much that he will not eat carb because body building, you know, so no naans**, no puris*** in our house now…my sons inspire me towards good health’ – HR, a 49 year old woman. |
| Introduction to Western Behaviors | 13 (57%) | ‘My wife and I, we are very much Indian food based. From her we learned…we had salad, and soup and one baked dish. It was fine and we enjoyed it very much. So that way she is helping us to keep that option.’ – JA, a 68 year old man. |
| Reciprocity of Support | ||
| Children Receive Instrumental Support | 18 (78%) | ‘Even though they both have full-time nannies sometimes in the evening [my daughter] needs more help so the reason I’m not looking for a new job, at least not until February, is that I just want to help her.’ –SA, a 56 year old woman. |
| Parent Role Models Health | 11 (48%) | ‘He’s put on some weight, right, so now I, you know, he started with three miles and I want him to go up…so I kind of work with him’ –NV, a 46 year old man. |
| Parents Provide Health Information | 9 (39%) | ‘With my kids, I do push them, I do tell them, you know, eat healthy or take your meds if you need to, work out if possible.’ –RR, a 55 year old woman. |
South Asian baked flatbread
South Asian deep-fried flatbread
Social Support
Parents identified four major forms of social support that their adult children provided for them: emotional, informational, companionship, and instrumental support (see Table 4). Social support was defined as the actual support provided or the perception that one received support.
Parents strongly relied on their adult children for emotional support, and specifically for advice. HR, a 49 year-old woman, described that she went to her son, who was into ‘positivity and emotional health’ for advice when she was having a hard time relating to her sisters-in-law: ‘He taught me some good ways of socially interacting, like the American ways … and these things from him helped me really become a good person.’ She described how her son’s perspective helped her deal with relationship problems more effectively. More than half of parents felt that their children were able to provide them with emotional support when they were faced with other difficult relationship issues or health problems.
In addition to relying on their adult children for emotional support, parents also identified adult children as a significant source of information about health. Among other things, their adult children taught them about the nutritional content of different foods, label reading, portion control, and techniques to reduce or replace unhealthy snacks. Parents often identified children as a primary source of information about health (see Table 4).
Parents noted that their children would not only teach them about healthy behaviors, but also engaged in these behaviors alongside them, providing companionship that parents felt helped them practice healthier habits (see Table 4). Others felt their adult children would even hold them accountable if they wanted to change their behavior. SS, a 42 year-old woman, explained: ‘I know that [if] I were to say I was going to do something… [my son would] remind me every day, I know he would do it.’
Finally, parents described receiving instrumental support from adult children, which was defined as physical assistance or any other forms of tangible support. Most often, children helped their parents navigate the health system or provided financial support, but they also helped parents keep track of medications, make screening appointments, and research medical issues (see Table 4). Less commonly, children did household chores for their parents.
Of note, parents identified few negative influences on health behaviors from their children. Most negative influences described were in regard to worry about children’s relationships or success, conflict between traditionally South Asian and Western values, children living away from home, or issues with in-laws.
Social Influence manifested as the ‘spill-over effect’
The ‘spill-over effect’ was confirmed in these South Asian parent-child relationships, but it was also magnified by parental acceptance of informational support from their adult children. Parents valued the informational support from their adult children, which appeared to promote healthy changes in parental behavior. Parents attributed this to acculturation and education, which increased exposure to ideas about health and wellness that were very different from traditional SA norms.
Nearly 75% of parents saw their children as role models for healthy behavior (see Table 4). They observed their children living in healthier ways, and often identified their children as sources of inspiration when they were trying to change their behavior, especially for dietary changes. SS, a 42 year-old woman, describes how she views her son as a role model: ‘He has given up sugar for the past, I would say, four years. I think “He’s a kid, so much younger than me, and he’s able to do it.”‘ Because children were seen as role models for healthy behaviors, parents were willing to accept health-related information and to imitate or adopt the behaviors they saw their children participating in.
Parental acceptance of adult children’s informational support was strengthened by parental belief that some of the Western health behaviors their children had adopted were healthier than traditional South Asian behaviors. Nearly sixty percent of parents said their children had adopted Western health behaviors and consequently introduced those ideas to their parents (see Table 4). NR, a 51 year old woman, described how she was unfamiliar with healthy Western dietary options, but once her son joined the track team in high school, he would come home with information from his coach about healthy foods that the whole family would then adopt. A 66 year old woman, LR, described how the process of acculturation led to new health information: ‘I was not aware I was overweight and I was not familiar with the American culture, so she was the one and my son who made us familiar with all the foods.’ In fact, NR, whose son influenced the family diet through his track coach, also described the children of South Asian immigrants as more ‘health conscious.’ She contrasted this with her own parents, saying ‘it’s a cultural difference… and I think a combination of attitude and plus the plentifulness of moving to this country was not good for that [older] generation.’ She described her own generation as culturally ‘in between’ her parents’ and her children’s generations.
Reciprocity of Support
In addition to the unique role of adult children in the South Asian immigrant community, the support provided by children to their parents was accepted due to the reciprocity of social support in the child-parent dyad.
Parents provided many forms of support for their children, including instrumental and informational support (see Table 4). NK, a 58 year old woman, noted that she enjoyed preparing food for her son, commenting ‘If I don’t do it, I’ll be unhappy.’
Parents also identified themselves as role models for healthy behaviors for their children in addition to seeing their children as role models (see Table 4). MS, a 59 year old man, echoed a common theme among parents that he worked hard to keep his children from eating processed, packaged foods and to promote healthy fresh foods. This concept was referred to in the context of Western culture’s reliance on packaged foods, and he implied that by promoting fresh food consumption, he was also reinforcing South Asian concepts of healthy eating. The reciprocity of support and the perception of both themselves and their children as role models indicated a give-and-take relationship in which parents were more able to accept health related information from their children because they too could provide valuable information about health, rooted in South Asian culture, to their children.
Discussion and Integration of Findings
This is one of the few studies that examined the role of specific social network members on health in South Asian immigrants in the U.S. Our mixed-methods data suggested that adult children are an important influence on parental health behaviors and that underlying mechanisms include social support and ‘spill-over’ of healthy behavior.
In Phase 1, the quantitative data suggested that parents with adult children who consumed specific foods and exercised regularly had higher diet quality and were more likely to meet exercise recommendations those whose children did not. Although these finding are consistent with findings in other populations (Higgs and Thomas 2016), the reasons for these differences have not been elucidated, and the specific ways adult children influenced these behaviors merited further exploration. Interview data illuminated the possible reasons for these associations with three main findings: first, adult children provided various forms of health-related social support; second, healthy behaviors from adult children were found to ‘spill-over’ to their parents; and third, social support between parents and children was reciprocal. Integration of the findings supported the hypothesis that adult children of older South Asian immigrants are in a unique situation to influence their parents due to their position within immigrant families in the U.S., where they serve as credible sources of informational support and role models of certain healthy behaviors adopted as part of the acculturation process.
We found that parents with an adult child in the network who consumed non-South Asian food, raw vegetables, or fresh fruit daily had higher diet quality than parents who had a child in the network that did not consume these foods as frequently. When children consumed South Asian food or cooked vegetables daily, there was no association with healthier parental diet. Parental diet was also unaffected by children’s consumption of sugary beverages, diet drinks or processed foods, which was also supported by qualitative data; packaged and processed foods were likely not accepted by parents due to parental emphasis and role modeling of South Asian norms about healthy food, such as eating fresh foods rather than processed foods. The combined effects of ‘spill-over,’ children’s and parents’ education, and acculturation may explain why children’s consumption of healthy non-South Asian food (raw vegetables and fresh fruit) was associated with improved parental diet when other aspects of non-South Asian diet (packaged foods) were not.
Children introduced their parents to Western concepts of health and then provided companionship and accountability in changing what both parent and child thought were unhealthy dietary behaviors. These acculturative processes and reciprocal role modeling may explain how South Asian immigrant parents used new health information, brought to them by their adult children, and integrated it with their own concepts of a healthy lifestyle that were based in South Asian cultural norms.
Another important finding that can be explained by the combined processes of acculturation and role modeling was older South Asians’ acceptance of children’s informational support. Prior findings from non-immigrant populations suggested that informational support from adult children had negative effects on parental health and well-being (Thomas 2009; Reczek and Zhang 2016; Lang and Schütze 2002), but we found the opposite to be true. The adult children’s unique ability to introduce Western ideas of health and wellness to their parents may have made it easier for parents to accept information from children. This is especially true in the setting of immigration, in which children are exposed to more Western health concepts than their parents through higher education and in which parents rely heavily on the nuclear family and actively take up Western cultural behaviors. However, another major factor in this acceptance was reciprocity of support—parents provided support to their adult children and also influenced their health, suggesting a give-and-take relationship in which information from adult children may have been more readily accepted and incorporated.
Limitations and Strengths
Limitations of this study included the cross-sectional quantitative design, which limited causal inference and focused on data collected only from the parents without data collected directly from the children, which could have altered Phase 1 findings. We also evaluated several different network exposures, which raises the issue of multiple exposures (Patel and Ioannidis 2014). Although our choice of exposures was based on an a priori conceptual model and hypotheses, it is possible that significant associations were due to chance, and there is a need to replicate these findings. Further, only data on adult children, not children less than 18 years of age, was included, which may have altered the impact of children on their parents’ health behaviors in Phase 2. Finally, the MASALA Study population was from only two geographic areas in the U.S., participants had a high socioeconomic status, and were largely of Indian origin, which does not represent the heterogeneity of the South Asian community in the U.S.
Despite these limitations, this study used a theoretically-informed mixed-methods design in a relatively large sample, with established measures of diet and physical activity and in-depth semi-structured interviews. We also selected covariates that were potential confounders, including those variables that were potential causes of the exposure or outcome or both, and those that may have captured unmeasured common causes of the exposure and the outcome. Though the findings may not be generalizable to all South Asians, our findings reflect the general demographics of South Asian immigrants in the U.S., where Indians comprise the largest subset of the South Asian community (over 80%), followed by Pakistanis, Bangladeshis, Nepali, and Sri Lankans (SAALT 2019). Our findings provide rich, empiric evidence of how adult children influence the health of middle- and older-aged South Asians in the U.S., and can inform health promotion strategies in this population.
Conclusion
Integration of the quantitative and qualitative data from this study showed that adult children in South Asian families influenced their parents’ diet and exercise by providing social support, introducing Western concepts of health, holding their parents accountable for behavioral change, and by acting as role models for healthy behavior. Our data support the idea that for older South Asian immigrants, adult children provide trustworthy and acceptable sources of health information that influences parental exercise and diet. Given that the South Asian immigrant community is at high risk of morbidity and mortality from cardiovascular risk factors and diseases that can be prevented and partially treated by lifestyle modification, future prevention efforts in this community should consider incorporating adult children to help implement and sustain healthy behaviour change.
Acknowledgements
The authors thank the MASALA Study staff and participants, especially Akansha Batra and Darlena David. The authors are supported by National Heart, Lung and Blood Institute grants 5R01HL093009 (PI: Kanaya) and 1R01HL120725 (PI: Kandula).
Funding Details: National Heart, Lung and Blood Institute 2R01HL093009 (PI: Kanaya) and 1R01HL120725 (PI: Kandula)
Footnotes
Declaration of Interest Statement
The authors do not have any conflicts of interest.
References
- Ainsworth Barbara E., Irwin Melinda L., Addy Cheryl L., Whitt Melicia C., and Stolarczyk Lisa M.. 1999. “Moderate Physical Activity Patterns of Minority Women: The Cross-Cultural Activity Participation Study Maternal Serum Screening View Project.” Article in Journal of Women’s Health & Gender-Based Medicine 8. 10.1089/152460999319129. [DOI] [PubMed] [Google Scholar]
- Angerer Peter, Siebert Uwe, Kothny Wolfgang, Mühlbauer Dagmar, Mudra Harald, and Schacky Clemens von. 2000. “Impact of Social Support, Cynical Hostility and Anger Expression on Progression of Coronary Atherosclerosis.” Journal of the American College of Cardiology 36 (6): 1781–88. 10.1016/S0735-1097(00)00944-X. [DOI] [PubMed] [Google Scholar]
- “Appendix 1 – 2008 Physical Activity Guidelines - Health.Gov.” 2008. Physical Activity Guidelines. 2008 https://health.gov/paguidelines/2008/appendix1.aspx.
- Berkman Lisa F., Leo-Summers Linda, and Horwitz Ralph I.. 1992. “Emotional Support and Survival after Myocardial Infarction. A Prospective, Population-Based Study of the Elderly.” Annals of Internal Medicine 117 (12): 1003–9. 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- Brummett Beverly H., Mark Daniel B., Siegler Ilene C., Williams Redford B., Babyak Michael A., Clapp-Channing Nancy E., and Barefoot John C.. 2005. “Perceived Social Support as a Predictor of Mortality in Coronary Patients: Effects of Smoking, Sedentary Behavior, and Depressive Symptoms.” Psychosomatic Medicine 10.1097/01.psy.0000149257.74854.b7. [DOI] [PubMed] [Google Scholar]
- Chiuve Stephanie E, Fung Teresa T, Rimm Eric B, Hu Frank B, McCullough Marjorie L, Wang Molin, Stampfer Meir J, and Willett Walter C. 2012. “Alternative Dietary Indices Both Strongly Predict Risk of Chronic Disease.” The Journal of Nutrition 142 (6): 1009–18. 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen Sheldon. 2004. “Social Relationships and Health.” American Psychologist 59 (8): 676–84. 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cornwell Benjamin, Schumm L Philip, Laumann Edward O, and Graber Jessica. 2009. “Social Networks in the NSHAP Study: Rationale, Measurement, and Preliminary Findings.” The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 64 Suppl 1 (Suppl 1): i47–55. 10.1093/geronb/gbp042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo M Robin. 2004. “Social Support and Patient Adherence to Medical Treatment: A Meta-Analysis.” Health Psychology 23 (2): 207–18. 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Dominguez Silvia, and Hollstein Betina. 2014. Mixed Methods Social Networks Research Design and Applications [Google Scholar]
- Falk A, Hanson BS, Isacsson SO, and Ostergren PO. 1992. “Job Strain and Mortality in Elderly Men: Social Network, Support, and Influence as Buffers.” American Journal of Public Health 82 (8): 1136–39. 10.2105/AJPH.82.8.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman Esther, and Mare Robert. 2010. “Education of Children and Differential Mortality of Parents : Do Parents Benefit from Their Children ‘ s Attainments ?” CCPR Population Working Papers, no. September. [Google Scholar]
- Higgs Suzanne, and Thomas Jason. 2016. “Social Influences on Eating.” Current Opinion in Behavioral Sciences 9: 1–6. 10.1016/j.cobeha.2015.10.005. [DOI] [Google Scholar]
- Jang Yuri, Yoon Jungwon, and Park Nan Sook. 2018. “Source of Health Information and Unmet Healthcare Needs in Asian Americans.” Journal of Health Communication 23 (7): 652–60. 10.1080/10810730.2018.1500660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jose Powell O, Frank Ariel T H, Kapphahn Kristopher I, Goldstein Benjamin A, Eggleston Karen, Hastings Katherine G, Cullen Mark R, and Palaniappan Latha P. 2014. “Cardiovascular Disease Mortality in Asian Americans.” Journal of the American College of Cardiology Vol. 64. 10.1016/j.jacc.2014.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi Prashant, Islam Shofiqul, Pais Prem, Reddy Srinath, Dorairaj Prabhakaran, Kazmi Khawar, Pandey Mrigendra Raj, et al. 2007. “Risk Factors for Early Myocardial Infarction in South Asians Compared With Individuals in Other Countries.” Journal of the American Medical Association 297 (3): 286. 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- Kanaya AM, Wassel CL, D Mathur A Stewart D Herrington, Budoff MJ, Ranpura V, and Liu K. 2010. “Prevalence and Correlates of Diabetes in South Asian Indians in the United States: Findings From the Metabolic Syndrome and Atherosclerosis in South Asians Living in America Study and the Multi-Ethnic Study of Atherosclerosis.” Metabolic Syndrome and Related Disorders 8 (2): 157–64. 10.1089/met.2009.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanaya Alka M, Kandula Namratha, Herrington David, Budoff Matthew J, Hulley Stephen, Vittinghoff Eric, and Liu Kiang. 2013. “Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study: Objectives, Methods, and Cohort Description.” Clinical Cardiology 36 (12): 713–20. 10.1002/clc.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandula Namratha R, Cooper Andrew J, Schneider John A, Fujimoto Kayo, Kanaya Alka M, Horn Linda Van, Dekoning Lawrence, and Siddique Juned. 2018. “Personal Social Networks and Organizational Affiliation of South Asians in the United States.” BMC Public Health 18 (1). 10.1186/s12889-018-5128-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelemen Linda E., Anand Sonia S., Vuksan Vladimir, Yi Qilong, Teo Koon K., Devanesen Sudarshan, and Yusuf Salim. 2003. “Development and Evaluation of Cultural Food Frequency Questionnaires for South Asians, Chinese, and Europeans in North America.” Journal of the American Dietetic Association 103 (9): 1178–84. 10.1016/S0002-8223(03)00985-4. [DOI] [PubMed] [Google Scholar]
- Kim Wonsun, Kreps Gary L, and Shin Cha-Nam. 2015. “The Role of Social Support and Social Networks in Health Information–Seeking Behavior among Korean Americans: A Qualitative Study.” International Journal for Equity in Health 14 (April): 40. 10.1186/s12939-015-0169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb S 2009. Aging and the Indian Diaspora: Cosmopolitan Families in India and Abroad. Aging and The Indian Diaspora: Cosmopolitan Families in India and Abroad Brandeis University. https://www.scopus.com/inward/record.uri?eid=2-s2.0-84897256941&partnerID=40&md5=cc18eaa21b6f956a2b3ccbda1f23c483. [Google Scholar]
- Lang Frieder R, and Schütze Yvonne. 2002. “Adult Children’s Supportive Behaviors and Older Parents’ Subjective Well–Being—A Developmental Perspective on Intergenerational Relationships.” Journal of Social Issues 58 (4): 661–80. 10.1111/1540-4560.00283. [DOI] [Google Scholar]
- Latkin Carl A, and Knowlton Amy R. 2015. “Social Network Assessments and Interventions for Health Behavior Change: A Critical Review.” Behavioral Medicine (Washington, D.C.) 41 (3): 90–97. 10.1080/08964289.2015.1034645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorca Maria Beatriz Fernandez, and Herrera Ponce Maria Soledad. 2015. “Normative, Structural, and Individual Factors That Predispose Adult Children to Provide Social Support to Their Elderly Parents.” Journal of Comparative Family Studies 46 (4): 517–40. https://search-proquest-com.ezproxy.galter.northwestern.edu/docview/1785001695?rfr_id=info%3Axri%2Fsid%3Aprimo/ip?accountid=12861/ip?accountid=147023. [Google Scholar]
- McPherson Miller, Lynn Smith-Lovin, and Brashears Matthew E.. 2006. “Social Isolation in America: Changes in Core Discussion Networks over Two Decades.” American Sociological Review 71 (June): 353–75. http://www2.asanet.org/journals/asr/2006/. [Google Scholar]
- Mukherjea Arnab, Underwood Kelsey Clark, Stewart Anita L, Ivey Susan L, and Kanaya Alka M. 2013. “Asian Indian Views on Diet and Health in the United States: Importance of Understanding Cultural and Social Factors to Address Disparities.” Fam Community Health 36 (4): 311–23. 10.1097/FCH.0b013e31829d2549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson Miriam E., Rejeski W. Jack, Blair Steven N., Duncan Pamela W., Judge James O., King Abby C., Macera Carol A., and Castaneda-Sceppa Carmen. 2007. “Physical Activity and Public Health in Older Adults.” Medicine & Science in Sports & Exercise 39 (8): 1435–45. 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- Palaniappan Latha, Wang Yun, and Fortmann Stephen P. 2004. “Coronary Heart Disease Mortality for Six Ethnic Groups in California, 1990–2000.” Annals of Epidemiology 14 (7): 499–506. 10.1016/j.annepidem.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Patel Chirag J., and Ioannidis John P.A.. 2014. “Placing Epidemiological Results in the Context of Multiplicity and Typical Correlations of Exposures.” Journal of Epidemiology and Community Health 10.1136/jech-2014-204195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puvar Dhara, and Kalayil Ann P. 2019. “Key Findings from South Asians Aging in America” South Asian American Policy and Research Institute. 2019. https://mailchi.mp/f68d864ff7ad/youre-invited-1501449?e=891b85eef3. [Google Scholar]
- Reczek Corinne, and Zhang Zhe. 2016. “Parent-Child Relationships and Parent Psychological Distress: How Do Social Support, Strain, Dissatisfaction, and Equity Matter?” Research on Aging 38 (7): 742–66. 10.1177/0164027515602315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollock David, and Lui P. Priscilla. 2016. “Do Spouses Matter? Discrimination, Social Support, and Psychological Distress among Asian Americans.” Cultural Diversity and Ethnic Minority Psychology 22 (1): 47–57. 10.1037/cdp0000045. [DOI] [PubMed] [Google Scholar]
- Rosengren A, Orth-Gomér K, Wedel H, and Wilhelmsen L. 1993. “Stressful Life Events, Social Support, and Mortality in Men Born in 1933.” British Medical Journal 307 (6912): 1102 LP–1105. 10.1136/bmj.307.6912.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAALT. 2019. “A Demographic Snapshot of South Asians in the United States” 2019. https://bit.ly/2EFumF1.
- Sharma Karuna, and Kemp Candace L. 2012. “‘One Should Follow the Wind’: Individualized Filial Piety and Support Exchanges in Indian Immigrant Families in the United States.” Journal of Aging Studies 26 (2): 129–39. 10.1016/j.jaging.2011.10.003. [DOI] [Google Scholar]
- Talegawkar SA, Jin Yichen, Kandula NR, and Kanaya AM. 2017. “Cardiovascular Health Metrics among South Asian Adults in the United States: Prevalence and Associations with Subclinical Atherosclerosis.” Preventive Medicine 96: 79–84. 10.1016/j.ypmed.2016.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas Patricia A. 2009. “Is It Better to Give or to Receive? Social Support and the Well-Being of Older Adults.” The Journals of Gerontology: Series B 65B (3): 351–57. 10.1093/geronb/gbp113. [DOI] [PubMed] [Google Scholar]
- Torssander Jenny. 2013. “From Child to Parent? The Significance of Children’s Education for Their Parents’ Longevity.” Demography 50 (2): 637–59. 10.1007/s13524-012-0155-3. [DOI] [PubMed] [Google Scholar]
- Uchino Bert N. 2004. “Social Support and All-Cause Mortality.” In Social Support and Physical Health Yale University Press. 10.12987/yale/9780300102185.003.0004. [DOI] [Google Scholar]
- Yahirun Jenjira J, Sheehan Connor M, and Hayward Mark D. 2017. “Adult Children’s Education and Changes to Parents’ Physical Health in Mexico.” Social Science & Medicine 181: 93–101. 10.1016/j.socscimed.2017.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- You Jin, Wang Carol, Yiu Yeung Nelson Chun, and Lu Qian. 2018. “Socioeconomic Status and Quality of Life among Chinese American Breast Cancer Survivors: The Mediating Roles of Social Support and Social Constraints.” Psycho-Oncology 27 (7): 1742–49. 10.1002/pon.4719. [DOI] [PubMed] [Google Scholar]


