Abstract
Background:
Hip arthroscopy is a viable treatment for femoroacetabular impingement syndrome (FAIS). Clinically relevant improvements in hip function and pain after surgery are often reported, but it is less clear how many patients achieve an acceptable symptom state (Patient Acceptable Symptom State [PASS]).
Purpose:
To investigate the proportion of patients who achieved a PASS 12 to 24 months after hip arthroscopy and to determine the cutoff scores of the 2 recommended and valid patient-reported outcome measures (the subscales of the Copenhagen Hip and Groin Outcome Score [HAGOS] and the International Hip Outcome Tool—33 [iHOT-33]) for which patients are most likely to achieve PASS.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Eligible study patients were identified in the Danish Hip Arthroscopy Registry. An electronic questionnaire was used to collect data on PASS, HAGOS, and iHOT-33 12 to 24 months after surgery. PASS was measured using an anchor question. Receiver operating characteristic curve analyses were applied to identify the PASS cutoff values of HAGOS and iHOT-33 scores.
Results:
A total of 137 individuals (mean age at surgery, 35.4 ± 9.4 years) were included in the study at a mean follow-up of 18.5 ± 3.2 months after surgery. At follow-up, 64 individuals (46.7%; 95% CI, 38.6-55.1) reported PASS. Higher HAGOS and iHOT-33 values were observed for participants who reported PASS compared with those who did not report PASS (Cohen d ≥ 1.06; P < .001). Cutoff scores for HAGOS subscales (42.5-82.5) and iHOT-33 (67.00) showed excellent to outstanding discriminative ability in predicting PASS (area under the curve, 0.82-0.92).
Conclusion:
In total, 46% of individuals having hip arthroscopy for FAIS achieved PASS at 12 to 24 months of follow-up. Patients who achieved PASS had statistically significant and substantially better self-reported hip function compared with those who did not achieve PASS. Cutoff values at HAGOS subscales and iHOT-33 showed excellent to outstanding discriminative ability in predicting patients with PASS.
Keywords: hip arthroscopy, Patient Acceptable Symptom State, PASS, patient-reported outcome measure, HAGOS, iHOT-33
Femoroacetabular impingement syndrome (FAIS) is a common cause of hip-related groin pain, mainly diagnosed in young and middle-aged physically active individuals.33 FAIS is defined as a motion-related disorder of the hip joint,11 predisposing to acetabular labral and cartilage injuries,10,19 and end-stage osteoarthritis.1
FAIS is often treated surgically using hip arthroscopy.8,34 A recent meta-analysis of 2 randomized controlled trials (RCTs) has found evidence for a small positive effect size (0.32; 95% CI, 0.07-0.57) of hip arthroscopy versus nonoperative treatment at 6 to 12 months of follow-up.12,22,32 Additionally, many cohort studies suggest that hip arthroscopy for FAIS is associated with large and clinically relevant improvements in pain and function pre- to post-operatively.17,23,24,30,39 Many patients, however, still present with persistent hip and groin pain and functional limitations after surgery,17,18,21,39 indicating that discrepancies may exist between “getting better” and “feeling good.”25 To better understand if patients consider their current state of health (eg, pain and function) to be at an acceptable level after hip arthroscopy for FAIS, the Patient Acceptable Symptom State (PASS) can be used.5,25 A 2015 study determined the cutoff scores of the modified Harris Hip Score (mHHS) and the Hip Outcome Score (HOS) for patients to be considered to have achieved PASS. Based on cutoff scores, approximately 65% achieved PASS.5 In addition, a recent systematic review showed that the majority of studies on hip arthroscopy did not achieve the PASS cutoff score for the HOS Sport subscale; however, this was measured across studies and not on an individual patient level.21 Furthermore, recent consensus statements and systematic reviews do not recommend the use of mHHS and HOS to evaluate patients with FAIS due to lack of content validity.11,15,40 The Copenhagen Hip and Groin Outcome Score (HAGOS)38 and the International Hip Outcome Tool-33 (iHOT-33)29 are recommended as the 2 preferred self-reported outcome measures to assess hip-related pain and function in young and middle-aged patients.11,15,40 Thus, combining PASS with HAGOS and/or iHOT-3315 could provide important information on the symptom state after hip arthroscopy for FAIS. This may help guide decision making before treatment,27 which is particularly relevant given the rapid rise in the number of patients diagnosed with FAIS.34
Therefore, the primary aim was to investigate the proportion of patients who achieved a PASS at 12 to 24 months after hip arthroscopy with a secondary aim to determine the cutoff values of the HAGOS subscales and iHOT-33 scores that indicate PASS after hip arthroscopy.
Methods
Study Design
This cross-sectional survey study investigated the proportion of individuals with PASS 12 to 24 months after hip arthroscopy for FAIS as the primary outcome measure, and the cutoff values of the HAGOS subscales38 and iHOT-33 scores29 for obtaining PASS as secondary outcomes. All eligible individuals and associated radiographic and operative data, were identified and extracted from the Danish Hip Arthroscopy Registry, initiated in 2012 with ongoing prospective registration of hip arthroscopies performed at 11 public and private hospitals in Denmark.31 The reporting adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.41 The study was deemed exempt from ethics review, as no intervention or testing of participants was conducted and all data were extracted from a registry approved by the Danish health authorities.31 The study was approved by the data agency of the capital region (ID: P-2019-277).
Study Setting
Demographic, radiological, and operative data, including preoperative HAGOS subscale scores, were extracted retrospectively on eligible participants from the Danish Hip Arthroscopy Registry undergoing hip arthroscopy between September 26, 2017, to September 26, 2018. Subsequently, we sent out questionnaires (PASS,5 HAGOS,38 and iHOT-3329) to patients.
Participants
Data on 232 eligible patients who had undergone hip arthroscopy for FAIS during the preceding 12 to 24 months were extracted from the Danish Hip Arthroscopy Registry.31 Radiological and operative data were registered by the operating surgeons. Inclusion criteria were men/women aged 18 to 50 years at the time of surgery; treated for FAIS (minimal surgical procedures: cam resection and labral surgery) in the preceding 12 to 24 months; and preoperative evidence of cam morphology defined as an alpha angle ≥55º.11 Exclusion criteria were pure pincer morphology; a joint space width <3 mm; borderline hip dysplasia defined as a lateral center-edge angle <25º; pure extra-articular surgical procedure; a previous periacetabular osteotomy; revision hip arthroscopy; total hip arthroplasty; previous hip pathology such as Perthes disease, slipped capital femoral epiphysis and/or avascular necrosis of the femoral head; or any rheumatoid disease in the hip joint such as synovial chondromatosis.
Data Collection
Postoperative patient-reported outcome measures (PROMs: PASS,5 HAGOS,38 and iHOT-3329) were collected using a web-based survey distributed to eligible participants 12 to 24 months after the hip arthroscopy. The survey was delivered using the Research Electronic Data Capture (REDCap) tools (V 7.1.1; Vanderbilt University) hosted at the capital region of Denmark.13 Eligible individuals were contacted through a secure email system based on their civil registration number and provided with a unique password-secured link to the survey. Reminder emails were sent once a week for 3 consecutive weeks to all nonresponders.
Outcome Measures
The primary outcome measure was the proportion of patients who achieved a PASS at 12 to 24 months after hip arthroscopy for FAIS. This was measured using the following question (yes/no response): “Taking into account your hip and groin function and pain and how it affects your daily life including your ability to participate in sport and social activities, do you consider that your current state is acceptable if it remained like that for the rest of your life?”5,25 As secondary outcomes, we assessed the discriminative ability, measured as the area under the curve (AUC),14 and the cutoff scores, based on the Youden index,45 of the HAGOS subscales and iHOT-33 scores beyond which patients are more likely to achieve PASS.25 The HAGOS consists of 37 items divided into 6 subscales for symptoms, pain, physical function in activities of daily living (ADL), function in sport and recreation, participation in physical activities, and quality of life (QOL). Each question is assessed on a 5-point Likert scale with a corresponding score of 0 to 4. Subsequently, a score ranging from 0 (extreme symptoms) to 100 (no symptoms) is calculated for each subscale.38 The iHOT-33 consists of 33 items covering aspects of symptoms and functional limitation; sports and recreational activities; job-related concerns; and social, emotional, and lifestyle concerns. Each question is scored on a visual analog scale of 0 to 100 mm with higher values indicating better QOL. The overall score is calculated as the average score across items.29
Finally, we measured PASS in relation to sports function (PASSSport) and activities of daily living (PASSADL) separately, since patients with FAIS often seem be severely impaired in sports function, rather than daily activities.17,39 This was done using the following question for PASSSport: “Taking into account your hip and groin function and pain, and how it affects your ability to participate in sport, do you consider that your current state is acceptable if it remained like that for the rest of your life?” And for PASSADL: “Taking into account your hip and groin function and pain, and how it affects your ADL, do you consider that your current state is acceptable if it remained like that for the rest of your life?” In addition, we analyzed the associations, measured as odds ratio, between PASSSport and PASSADL with the overall PASS.
Bias
To reduce potential selection bias associated with only including patients from a single hip arthroscopy center and surgeon, we identified eligible patients in the Danish Hip Arthroscopy Registry.31 Additionally, we aimed for homogeneity of the study sample by including individuals who had been treated with both cam resection and acetabular labral surgery.26 Thus, pincer FAIS alone was not included, as this condition is less likely to result in intra-articular pathology.2,19 Furthermore, we used PROMs to evaluate the current state of health to avoid the potential that stakeholders, such as physiotherapists or surgeons, could bias the outcome.
Sample Size Considerations
The number of eligible individuals in the Danish Hip Arthroscopy Registry and responders determined the sample size of the study. With an expected proportion of patients who achieved PASS of approximately 50%,32 a precision of 10%, and a 95% CI, 96 patients were needed.42 This would also meet the minimum required sample size for detecting an AUC of ≥0.7 (acceptable discrimination) with an alpha and beta level of .05 and 0.2, respectively (V 19.2.1; MedCalc Software).
Statistical Analysis
Data derived from the PASS, PASSSport, and PASSADL were calculated using percentages with corresponding 95% CIs. Logistic regression analyses were conducted to assess the associations, measured as odds ratios, between both PASSSport and PASSADL (independent variables) with overall PASS (dependent variable). HAGOS subscale and iHOT-33 scores at follow-up were compared between participants with and without PASS using independent t tests, whereas differences in pre- and postoperative HAGOS subscales scores were analyzed using independent t tests, as missing preoperative data precluded paired t test analyses. No preoperative iHOT-33 scores were available from the Danish Hip Arthroscopy Registry precluding pre- to postoperative analysis.
Effect sizes for differences were calculated as Cohen d and assessed as trivial (<0.2), small (≥0.2), medium (≥0.5), and large (≥0.8).7 The discriminative ability of HAGOS subscale and iHOT-33 scores to predict PASS was analyzed by constructing receiver operating characteristic (ROC) curves for all HAGOS subscale and iHOT-33 scores using the PASS as the dependent variable. Discriminative ability was assessed as the AUC and classified according to Hosmer and Lemeshow14 as no discrimination (AUC = 0.5), poor discrimination (0.5 < AUC < 0.7), acceptable discrimination (0.7 ≤ AUC < 0.8), excellent discrimination (0.8 ≤ AUC < 0.9), and outstanding discrimination (AUC ≥ 0.9). The optimal HAGOS subscales and iHOT-33 cutoff scores to best predict the PASS with highest combined sensitivity and specificity, was derived using the Youden index (J = sensitivity + specificity –1), with a higher index score yielding a better combined sensitivity and specificity.45 The statistical analyses were performed in SPSS V 23 (SPSS Inc), with the significance level set at P < .05.
Results
Participants
A total of 140 out of 232 eligible individuals responded to the survey between October 15, 2019, and November 11, 2019 (response rate, 60.3%), of which 137 patients were included; 1 patient declined to participate whereas 2 patients were excluded due to not answering the overall PASS question. Of the 137 included patients, data were missing for the following outcomes due to not answering questions: PASSSport (n = 1); PASSADL (n = 2); HAGOS (n = 5); and iHOT-33 (n = 27). Detailed characteristics of the included patients and nonresponders are provided in Table 1. A significant difference in proportion was observed for sex between responders and nonresponders (P < .001). Significantly higher HAGOS Subscale scores were observed at follow-up compared with preoperatively (d = 0.51-0.94; P ≤ .001) (Appendix Table A1).
Table 1.
Overview of Included Patients and Nonrespondentsa
| Included (N = 137) | Nonrespondents (n = 92) | |
|---|---|---|
| Male sex | 63 (46) | 68 (73.9)b |
| Mean age at surgery, y | 35.4 ± 9.4 | 33.3 ± 9.7 |
| Follow-up, mo | 18.5 ± 3.2 | |
| Radiological data | ||
| Alpha angle, deg | 72.3 ± 10.7 | 72.1 ± 10.2 |
| Lateral center-edge angle, deg | 31.1 ± 4.3 | 30.8 ± 4.6 |
| Joint space width >4.0 mm | 104 (75.9) | 71 (77.2) |
| Presence of crossover sign | 79 (57.7) | 43 (46.7) |
| Cartilage damage | (n = 131) | (n = 86) |
| Beck classification (acetabulum) | ||
| Normal cartilage | 1 (0.7) | 0 (0) |
| Fibrillation | 6 (4.6) | 10 (11.6) |
| Wave sign | 62 (47.3) | 32 (37.2) |
| Cleavage | 45 (34.4) | 38 (44.2) |
| Exposed bone | 17 (13.0) | 6 (7.0) |
| ICRS classification (caput femoris) | ||
| Normal cartilage | 103 (78.6) | 56 (65.1) |
| Almost normal | 10 (7.6) | 7 (8.1) |
| Abnormal | 10 (7.6) | 13 (15.1) |
| Severely abnormal | 7 (5.3) | 7 (8.1) |
| Exposed bone | 1 (0.7) | 3 (3.5) |
| Preoperative HAGOS score | (n = 102) | (n = 59) |
| Pain | 53.5 ± 19.0 | 50.8 ± 18.8 |
| Symptoms | 49.8 ± 18.2 | 44.9 ± 15.5 |
| Function in activities of daily living | 56.4 ± 25.4 | 50.0 ± 21.7 |
| Function in sport and recreation | 37.2 ± 23.9 | 33.6 ± 20.8 |
| Participation in physical activities | 22.7 ± 26.2 | 22.6 ± 20.2 |
| Quality of life | 30.5 ± 15.7 | 30.3 ± 16.5 |
aData are reported as n (%) or mean ± SD. HAGOS, Copenhagen Hip and Groin Outcome Score; ICRS, International Cartilage Regeneration & Joint Preservation Society.
bStatistically significant between-group difference in proportion (P < .001).
Patient Acceptable Symptom State
At follow-up, 64 participants (46.7%; 95% CI, 38.6-55.1) achieved an overall PASS.
Patient-Reported Outcome Measures Between Participants With and Without PASS
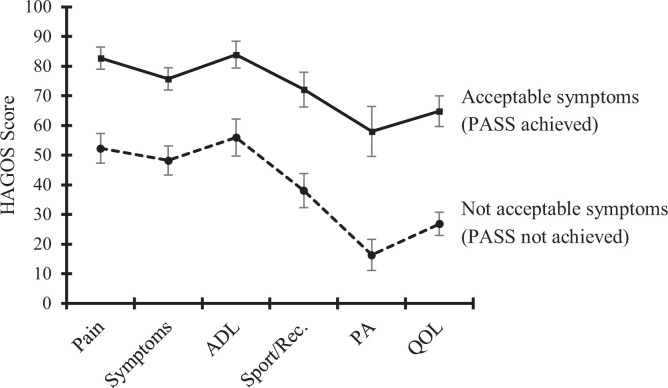
At follow-up, higher HAGOS values were observed for individuals with an acceptable symptom state compared with those without an acceptable symptom state for all subscales corresponding to large effect sizes (d ≥ 1.06; P < .001) (Figure 1 and Appendix Table A2).
Figure 1.
Self-reported hip and groin symptoms and function in individuals with (n = 64; solid line) and without (n = 68; dotted line) a Patient Acceptable Symptom State (PASS) at follow-up for subscales of the Copenhagen Hip and Groin Outcome Score (HAGOS). X-axis shows the 6 subscales of HAGOS. ADL, physical function in activities of daily living; PA, participation in physical activities; QOL, quality of life; Sport/Rec, function in sport and recreation. Error bars show 95% CIs.
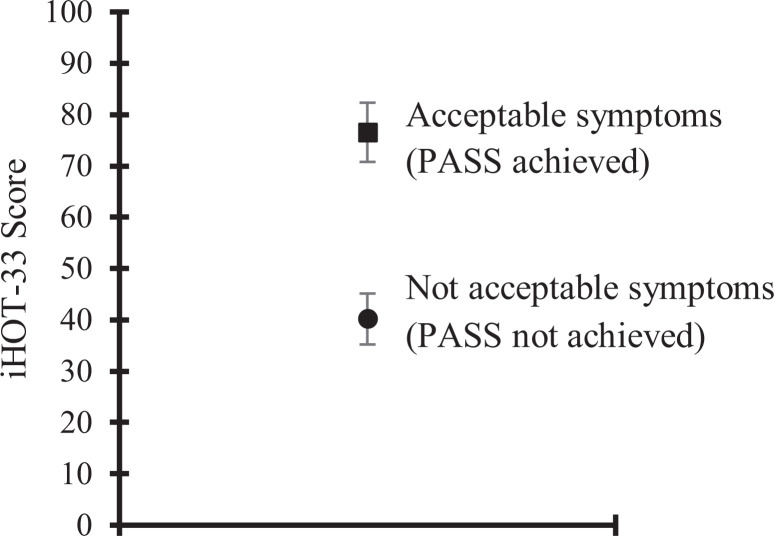
Likewise, higher iHOT-33 values were observed for participants with an acceptable symptom state compared with those without an acceptable symptom state corresponding to a large effect size (d = 1.35; P < .001) (Figure 2 and Appendix Table A3).
Figure 2.
Self-reported hip symptoms in individuals with (n = 53; square) and without (n = 57; circle) a Patient Acceptable Symptom State (PASS) at follow-up for the International Hip Outcome Tool--33 (iHOT-33). Error bars show 95% CIs.
ROC Curve Analyses
For all HAGOS subscales and iHOT-33, the AUC showed excellent to outstanding discriminative ability (AUC, 0.815-0.916) in predicting individuals with PASS (Table 2 and Appendix Figures A1 and A2). The cutoff values, including sensitivity and specificity, for each subscale of HAGOS and iHOT-33, are presented in Table 2.
Table 2.
AUC Values Derived From ROC Curve Analyses and PASS Cutoff Values, and Their Respective Sensitivity and Specificity, for HAGOS Subscales and iHOT-33 Scoresa
| PROM | AUC (95% CI) | Cutoff Valueb,c | Sensitivity | Specificity |
|---|---|---|---|---|
| HAGOS subscale | ||||
| Pain | 0.89 (0.84-0.95) | 68.75 | 0.84 | 0.79 |
| Symptoms | 0.86 (0.80-0.92) | 62.50 | 0.84 | 0.74 |
| ADL | 0.82 (0.74-0.89) | 82.50 | 0.66 | 0.85 |
| Sport/Rec | 0.84 (0.78-0.91) | 60.94 | 0.75 | 0.81 |
| Physical activity | 0.83 (0.75-0.90) | 43.75 | 0.69 | 0.90 |
| Quality of life | 0.92 (0.87-0.97) | 42.50 | 0.84 | 0.90 |
| iHOT-33 | 0.88 (0.82-0.95) | 67.00 | 0.74 | 0.95 |
aADL, physical function in daily living; AUC, area under the ROC curve; HAGOS, Copenhagen Hip and Groin Outcome Score; iHOT-33, International Hip Outcome Tool--33; PASS, Patient Acceptable Symptom State; PROM, patient-reported outcome measure; ROC, receiver operating characteristic; Sport/Rec, function in sport and recreation.
bThe cutoff values were derived using the Youden index (J = sensitivity + specificity -1), which is based on the best combined sensitivity and specificity; a higher index score yields a better combined sensitivity and specificity.45
cThe cutoff score represents the score beyond which an individual is more likely to have an acceptable symptom state.
PASS in Relation to Sport and ADL
At follow-up, 55 individuals (40.4%; 95% CI, 32.6-48.8) and 72 individuals (53.3%; 95% CI, 44.9-61.9) reported an acceptable symptom state in relation to PASSSport and PASSADL, respectively. Having achieved PASSSport or PASSADL was associated with overall PASS corresponding to an odds ratio of 168.6 (95% CI, 35.9-793.2) and 30.4 (95% CI, 11.5-80.2), respectively.
Discussion
We found that less than half of patients (46.7%) who had undergone hip arthroscopy for FAIS in the previous 12 to 24 months reported an acceptable symptom state. Additionally, 40.4% and 53.3% had an acceptable symptom state related to PASSSport and PASSADL, respectively. The cutoff scores, beyond which patients are more likely to achieve PASS,25 ranged from 42.5 (HAGOS QOL subscale) to 82.5 (HAGOS ADL subscale), whereas the iHOT-33 score was 67. These findings can easily be applied in previous studies where HAGOS and/or iHOT-33 scores have been obtained, to retrospectively quantify the proportion of patients with PASS.
The proportion of patients with a PASS in the present study (46.7%) is similar to a recent multicenter RCT showing that 48% allocated to hip arthroscopy achieved the PASS cutoff score of HOS ADL (≥87 points) at the 8-month follow-up.32 Similar to the study from Palmer et al,32 our study included a general population with FAIS from multiple hip arthroscopy centers, indicating that the percentage of patients achieving PASS in a general population is likely about 50%. Of note, cohort studies from single high-volume hip arthroscopy centers and a single surgeon have reported that 60% to 73% of patients seem to achieve PASS based on cutoff scores from HOS Sport (≥72.1 points35 and ≥75 points5), HOS ADL (≥87 points),5 mHHS (≥74 points),5,43 and iHOT-33 (≥58 points).28 Such discrepancy may be explained by surgeon experience, criteria for surgery, and selection bias of patients undergoing surgery. Surprisingly, none of the above studies reported the proportion of patients that achieved PASS based on the question itself,25 despite having obtained this information for calculation of the cutoff score.5,28,35 Thus, we argue that the present study is the first to clearly report PASS in a general population after hip arthroscopy for FAIS.
PASS Cutoff Scores for HAGOS and iHOT-33
Our study showed a large difference in all HAGOS subscale and iHOT-33 scores between individuals who achieved PASS versus those who did not achieve PASS, indicating that the PASS question was effective in dichotomizing patients into good and poor outcomes. Consequently, ROC analyses showed excellent to outstanding discriminative ability in predicting PASS with sensitivity and specificity ranging from 0.66 to 0.84 (HAGOS subscales) and 0.74 to 0.95 (iHOT-33). This corresponds well with previous studies of HOS-Sport (cutoff score ≥72.1 points; AUC, 0.88635 and ≥75 points; sensitivity, 79.6; specificity, 96.9),5 HOS ADL (cutoff score ≥87 points; sensitivity, 82.7; specificity, 84.4),5 mHHS (cutoff score ≥74 points; sensitivity, 89.7; specificity, 87.5),5 and iHOT-33 (cutoff score ≥58 points; AUC, 0.870).28 However, HOS and mHHS are not recommended as PROMs for patients with FAIS.15
To our knowledge, our study is the first to report PASS cutoff values for HAGOS, which is a recommended PROM in young and middle-aged individuals with FAIS.11,15 The cutoff score for iHOT-33 in the present study is slightly higher than what has previously been reported by Maxwell et al,28 with a cutoff score of ≥58 points compared with our cutoff score of ≥67 points. This may be due to a different setting (single surgeon vs national registry) or study population in Maxwell et al, which included different diagnoses in their study, with only 36% presenting with cam morphology versus 100% in the present study. Nonetheless, by using these cutoff scores for HAGOS and/or iHOT-33, it is possible to obtain a more detailed profile of the symptomatic state after hip arthroscopy for FAIS, not only relying on pre- to postsurgical improvements and/or achievement of a healthy reference score.39 As an example, the UK FASHIoN trial, an RCT comparing the effect of hip arthroscopy with nonoperative treatment for FAIS, reported mean iHOT-33 values of 58.8 (hip arthroscopy group) and 49.7 points (nonoperative group) at 12-month follow-up.12 Thus, based on the iHOT-33 cutoff scores for achieving PASS (approximately 58-67 points),28 it is likely that approximately half of the patients allocated to hip arthroscopy in the UK FASHIoN trial did not achieve PASS12; findings that are similar to the present study, and the Femoroacetabular Impingement Treatment trial where 48% (hip arthroscopy group) achieved the PASS cutoff scores based on HOS ADL.32
Sport Function and ADL
To our knowledge, our study is the first to categorize PASS into different domains: PASSSport and PASSADL. While the PASS is normally employed to investigate the acceptable state of health considering pain and symptoms in all aspects of life,5,25 achieving or not achieving PASS may be driven by pain and/or symptoms in specific situations and contexts. This is further highlighted by the logistic regression analyses, showing that patients who achieved PASSSport had the highest odds versus PASSADL (168 vs 30) of achieving overall PASS. Our results suggest that an acceptable symptom state may be more difficult to achieve in relation to sport compared with ADL (40.4% vs 53.3%). The fact that 60% did not achieve PASS in relation to sport is in line with a recent systematic review reporting that 64% of studies failed to achieve the PASS cutoff score for the HOS Sport subscale.21 Thus, in a general population, achieving PASS in relation to sports function seems less likely than achieving PASS in relation to ADL. Such information should be included as part of the shared decision-making process before surgery. The discrepancy between PASSADL and PASSSport in the present study corresponds well with the notion that the HAGOS ADL subscale has a higher ceiling effect compared with the HAGOS Sport/Rec subscale.36,38 Therefore, a larger proportion of participants are more likely to report no problems in ADL compared with sport activities. We speculate that problems in sports activities may be the reason for not achieving overall PASS while still having acceptable symptoms during ADL in some patients.17,18,39 This highlights that including sports function in the PASS question seems crucial to truly capture patient satisfaction.
Different Concepts of PROMs: Getting Better (Minimal Important Change), Feeling Good (PASS), or Getting Back to Normal (Normal Reference Values)
Previous hip arthroscopy studies have mainly used PROMs to deal with the concept of “change scores” over a specific time period.12,23 While such information is important for establishing the effect of a treatment, a change score may be difficult to interpret for the patient who is about to decide whether to undergo hip arthroscopy (ie, “What does a 15-point improvement on iHOT-33 or HAGOS Sport/Rec actually mean?”). Such information can be obtained using the minimal important change score,20,25 with data suggesting that most patients (>66%) exceed this and get better from before to 1-year after surgery.39 While this is useful for the patient to know before treatment, “getting better” is not equivalent to “feeling good,”39 which is normally measured with PASS.25 While “feeling good” after hip arthroscopy is often considered a successful treatment outcome, achieving PASS may not reflect a normal state of function. Reference values for HAGOS subscales have previously been defined based on mixed healthy individuals39 and hip and groin injury-free male soccer players.37 These scores are generally higher (range, 64.3-100 points)37,39 compared with the HAGOS subscale PASS cutoff values in the present study (range, 42.5-82.5 points).39 This discrepancy highlights that patients with FAIS do not need to reach values comparable with healthy individuals in order to “feel good” after hip arthroscopy. We can only speculate why this seems to be the case; one reason may be that patients often have long periods of pain and functional limitations before receiving appropriate treatement.4,6 Thus, it may be that improvements in pain and function after hip arthroscopy, although not reaching a pain-free level, are regarded as acceptable for many patients also considering their state before treatment. This is further highlighted by the large proportion of patients being satisfied with the treatment, without this necessarily reflecting pain-free function.3
Clinical Implications
We believe information based on these different concepts of PROMs (ie, “getting better,” “feeling good,” and “getting back to normal”) is paramount to convey to surgical candidates as part of the shared treatment decision-making process. Such information may also help align preoperative expectations with actual postoperative outcomes.27 This seems important, as patients with FAIS tend to be overly optimistic regarding the effect of hip arthroscopy, with 53% and 61% of patients not meeting their preoperative expectations for general and sport function, respectively, at the 12-month follow-up.27 The current literature of postoperative FAIS patients suggests that 60% to 70% exceed the minimal important change and thus get better,39 around 50% achieve PASS and thus feel good,32 and 20% to 30% achieve healthy reference values and thus get back to normal function.39
Limitations
The present study is not without limitations. First, the response rate of 60% may result in selection bias; however, the responders and nonresponders are comparable in terms of demographic, radiographic, and surgical parameters, whereas our PASS results resemble those from a recent RCT.32 Second, there are different methods to measure a patient’s acceptable symptom state25: by using either a dichotomized yes-no question, as in the present study, or by using continuous scales9 or Likert scales16 with predefined cutoffs. In addition, the anchor question may be formulated differently, with no consensus on the most appropriate way.25 Inspired by previous studies,16,25 we used an anchor question related to acceptable symptoms and function, whereas other studies have used anchor questions related to treatment satisfaction.9 It is, however, likely that satisfaction with the treatment measures a different construct than postoperative symptoms and function3; thus, our PASS question concerned symptoms and function, rather than treatment satisfaction. Additionally, we categorized the overall PASS question into PASSSport and PASSADL; however, we appreciate that no psychometric properties have been established, and thus these results should be interpreted with caution.
A third limitation is that several ways exist to derive the PASS cutoff values: the Youden index45; the 80% specificity method; and the 75th percentile approach. In a study applying all methods, comparable cutoff values of the Harris Hip Score were found after hip arthroplasty.45 Thus, we used the Youden index45 in line with previous hip arthroscopy studies.5,28,35 Fourth, the large dropout of patients not answering the full iHOT-33 questionnaire may have implications for the cutoff score. Finally, it should be acknowledged that PASS cutoff scores may be influenced by cross-cultural differences, age, the patient’s own context of what constitutes an acceptable symptom state or not,44 and the follow-up time point.9 However, self-reported pain and function in patients with FAIS seems to plateau at 12 to 24 months after surgery.23 Future studies with large sample sizes should seek to investigate whether PASS cutoff scores after hip arthroscopy are affected by age and sex.
Conclusion
In total, 46% of individuals having hip arthroscopy for FAIS achieved PASS at 12 to 24 months of follow-up. Patients who achieved PASS had statistically significant and substantially better self-reported hip function compared with those who did not achieve PASS. Cutoff values at HAGOS subscales and iHOT-33 showed excellent to outstanding discriminative ability in predicting individuals with an acceptable symptom state.
Acknowledgment
The authors thank the steering committee of the Danish Hip Arthroscopy Registry for allowing access to registry data.
APPENDIX
Table A1.
Differences in Self-reported Hip and Groin Function Measured With the HAGOS Preoperatively to Postoperativelya
| HAGOS | Preoperative (n = 102) | Postoperative (n = 132) | Between-Group Difference (95% CI); Cohen d |
|---|---|---|---|
| Symptoms | 49.8 ± 18.2 | 61.6 ± 22.6 | 11.7 (6.3-17.1); 0.64b |
| Pain | 53.5 ± 19.0 | 67.1 ± 23.7 | 13.6 (8.0-19.3); 0.72b |
| ADL | 56.6 ± 25.4 | 69.5 ± 26.3 | 12.9 (6.2-19.7); 0.51b |
| Sport/Rec | 37.2 ± 23.9 | 54.6 ± 29.1 | 17.3 (10.3-24.3); 0.72b |
| PA | 22.7 ± 26.2 | 36.6 ± 35.0 | 13.9 (5.7-22.1); 0.53b |
| QOL | 30.5 ± 15.7 | 45.3 ± 26.5 | 14.7 (8.9-20.6); 0.94b |
aData are presented as mean ± SD. ADL, physical function in daily living; HAGOS, Copenhagen Hip and Groin Outcome Score; PA, participation in physical activities; QOL, quality of life; Sport/Rec, function in sport and recreation.
bStatistically significant difference between groups (P < .05).
Table A2.
Differences in Self-reported Hip and Groin Function Measured With the HAGOS in Patients With and Without an Acceptable Symptom State at Follow-Upa
| HAGOS | Postoperative (n = 132) | Acceptable Symptom State (n = 64) | Not Acceptable Symptom State (n = 68) | Between-Group Difference (95% CI); Cohen d |
|---|---|---|---|---|
| Symptoms | 61.6 ± 22.6 | 75.7 ± 15.1 | 48.2 ± 20.3 | 27.5 (21.3-33.7); 1.22b |
| Pain | 67.1 ± 23.7 | 82.7 ± 15.0 | 52.3 ± 20.7 | 30.4 (24.2-36.7); 1.28b |
| ADL | 69.5 ± 26.3 | 83.9 ± 18.1 | 56.0 ± 25.7 | 28.0 (20.2-35.7); 1.06b |
| Sport/Rec | 54.6 ± 29.1 | 72.1 ± 23.5 | 38.1 ± 23.8 | 34.1 (25.9-42.2); 1.17b |
| PA | 36.6 ± 35.0 | 58.0 ± 33.7 | 16.4 ± 21.7 | 41.6 (31.9-51.4); 1.19b |
| QOL | 45.3 ± 26.5 | 64.8 ± 20.7 | 26.8 ± 16.2 | 38.0 (31.6-44.4); 1.43b |
aData are presented as mean ± SD. ADL, function in activities of daily living; HAGOS, Copenhagen Hip and Groin Outcome Score; PA, function in physical activities; QOL, quality of life; Sport/Rec, function in sport and recreation.
bStatistically significant difference between groups (P < .05).
Table A3.
Differences in Self-reported Hip and Groin Function Measured With the iHOT-33 in Patients With and Without an Acceptable Symptom State at Follow-upa
| Postoperative (n = 110) | Acceptable Symptom State (n = 53) | Not Acceptable Symptom State (n = 57) | Between-Group Difference (95% CI); Cohen d | |
|---|---|---|---|---|
| iHOT-33 | 57.6 ± 26.8 | 76.5 ± 20.9 | 40.2 ± 16.6 | 36.2 (28.7-43.7); 1.35b |
aData are presented as mean ± SD. iHOT-33, International Hip Outcome Tool--33.
bStatistically significant difference between groups (P < .05).
Figure A1.
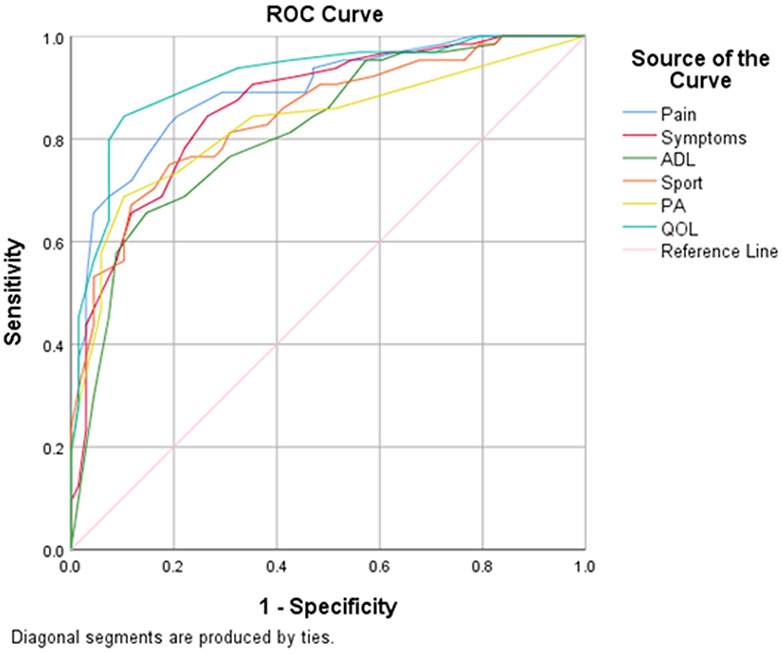
Receiver operating characteristic (ROC) curves for the subscales of the Copenhagen Hip and Groin Outcome Score. ADL, physical function in activities of daily living; PA, participation in physical activities; QOL, quality of life; Sport, function in sport and recreation.
Figure A2.
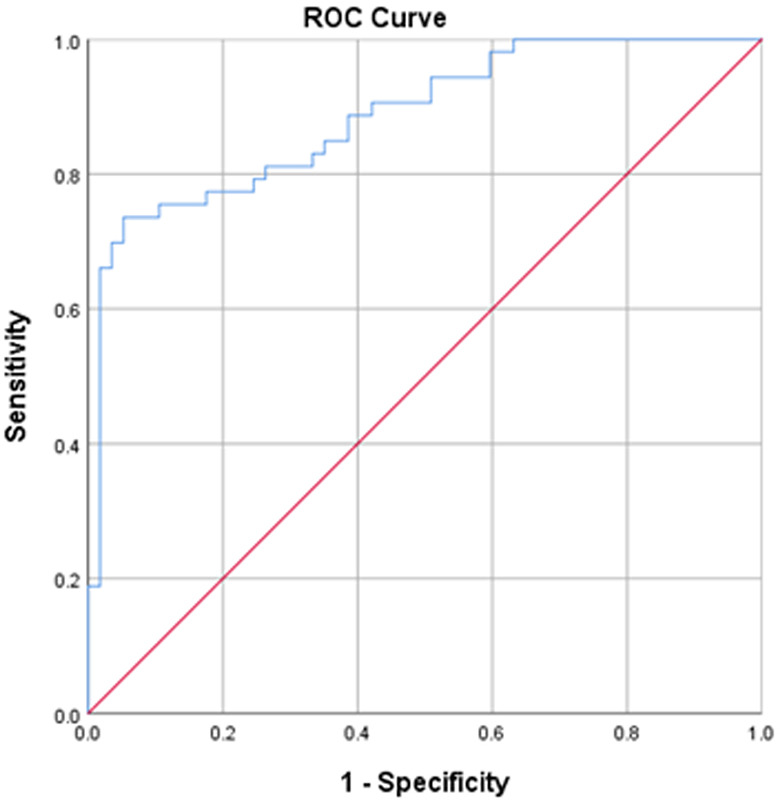
Receiver operating characteristic (ROC) curves for the International Hip Outcome Tool--33. Red line indicates reference line.
Footnotes
Final revision submitted October 18, 2020; accepted November 23, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the Danish Ethics Committee of the Capital Region.
References
- 1. Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72(6):918–923. [DOI] [PubMed] [Google Scholar]
- 2. Agricola R, Heijboer MP, Roze RH, et al. Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthritis Cartilage. 2013;21(10):1514–1521. [DOI] [PubMed] [Google Scholar]
- 3. Aprato A, Jayasekera N, Villar RN. Does the modified Harris hip score reflect patient satisfaction after hip arthroscopy? Am J Sports Med. 2012;40(11):2557–2560. [DOI] [PubMed] [Google Scholar]
- 4. Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88(7):1448–1457. [DOI] [PubMed] [Google Scholar]
- 5. Chahal J, Van Thiel GS, Mather RC, 3rd, et al. The Patient Acceptable Symptomatic State for the Modified Harris Hip Score and Hip Outcome Score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med. 2015;43(8):1844–1849. [DOI] [PubMed] [Google Scholar]
- 6. Clohisy JC, Baca G, Beaule PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–1356. [DOI] [PubMed] [Google Scholar]
- 7. Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159. [DOI] [PubMed] [Google Scholar]
- 8. de Sa D, Hölmich P, Phillips M, et al. Athletic groin pain: a systematic review of surgical diagnoses, investigations and treatment. Br J Sports Med. 2016;50(19):1181–1186. [DOI] [PubMed] [Google Scholar]
- 9. Galea VP, Florissi I, Rojanasopondist P, et al. The Patient Acceptable Symptom State for the Harris Hip Score following total hip arthroplasty: validated thresholds at 3-month, 1-, 3-, 5-, and 7-year follow-up. J Arthroplasty. 2020;35(1):145–152. [DOI] [PubMed] [Google Scholar]
- 10. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 11. Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169–1176. [DOI] [PubMed] [Google Scholar]
- 12. Griffin DR, Dickenson EJ, Wall PDH, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet. 2018;391(10136):2225–2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)---a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. John Wiley & Sons; 2000. [Google Scholar]
- 15. Impellizzeri FM, Jones DM, Griffin D, et al. Patient-reported outcome measures for hip-related pain: a review of the available evidence and a consensus statement from the International Hip-related Pain Research Network, Zurich 2018. Br J Sports Med. 2020;54(14):848–857. [DOI] [PubMed] [Google Scholar]
- 16. Impellizzeri FM, Mannion AF, Naal FD, Hersche O, Leunig M. The early outcome of surgical treatment for femoroacetabular impingement: success depends on how you measure it. Osteoarthritis Cartilage. 2012;20(7):638–645. [DOI] [PubMed] [Google Scholar]
- 17. Ishøi L, Thorborg K, Kraemer O, Hölmich P. Return to sport and performance after hip arthroscopy for femoroacetabular impingement in 18- to 30-year-old athletes: a cross-sectional cohort study of 189 athletes. Am J Sports Med. 2018;46(11):2578–2587. [DOI] [PubMed] [Google Scholar]
- 18. Ishøi L, Thorborg K, Kraemer O, Hölmich P. The association between specific sports activities and sport performance following hip arthroscopy for femoroacetabular impingement syndrome: a secondary analysis of a cross-sectional cohort study including 184 athletes. J Hip Preserv Surg. 2019;6(2):124–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ishøi L, Thorborg K, Kraemer O, Lund B, Mygind-Klavsen B, Hölmich P. Demographic and radiographic factors associated with intra-articular hip cartilage injury: a cross-sectional study of 1511 hip arthroscopy procedures. Am J Sports Med. 2019;47(11):2617–2625. [DOI] [PubMed] [Google Scholar]
- 20. Jevsevar DS, Sanders J, Bozic KJ, Brown GA. An introduction to clinical significance in orthopaedic outcomes research. JBJS Rev. 2015;3(5):01874474-201503050-00002. [DOI] [PubMed] [Google Scholar]
- 21. Jones DM, Crossley KM, Ackerman IN, et al. Physical activity following hip arthroscopy in young and middle-aged adults: a systematic review. Sports Med Open. 2020;6(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kemp JL, Mosler AB, Hart H, et al. Improving function in people with hip-related pain: a systematic review and meta-analysis of physiotherapist-led interventions for hip-related pain. Br J Sports Med. 2020;54(23):1382–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kierkegaard S, Langeskov-Christensen M, Lund B, et al. Pain, activities of daily living and sport function at different time points after hip arthroscopy in patients with femoroacetabular impingement: a systematic review with meta-analysis. Br J Sports Med. 2017;51(7):572–579. [DOI] [PubMed] [Google Scholar]
- 24. Kierkegaard S, Mechlenburg I, Lund B, Rømer L, Soballe K, Dalgas U. Is hip muscle strength normalised in patients with femoroacetabular impingement syndrome one year after surgery? Results from the HAFAI cohort. J Sci Med Sport. 2019;22(4):413–419. [DOI] [PubMed] [Google Scholar]
- 25. Kvien TK, Heiberg T, Hagen KB. Minimal clinically important improvement/difference (MCII/MCID) and Patient Acceptable Symptom State (PASS): what do these concepts mean? Ann Rheum Dis. 2007;66(Suppl 3): iii40–iii41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lund B, Mygind-Klavsen B, Nielsen TG, et al. Danish Hip Arthroscopy Registry (DHAR): the outcome of patients with femoroacetabular impingement (FAI). J Hip Preserv Surg. 2017;4(2):170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mannion AF, Impellizzeri FM, Naal FD, Leunig M. Fulfilment of patient-rated expectations predicts the outcome of surgery for femoroacetabular impingement. Osteoarthritis Cartilage. 2013;21(1):44–50. [DOI] [PubMed] [Google Scholar]
- 28. Maxwell S, Pergaminelis N, Renouf J, Tirosh O, Tran P. Identification of a Patient Acceptable Symptomatic State score for the International Hip Outcome Tool in people undergoing hip arthroscopy. Arthroscopy. 2018;34(11):3024–3029. [DOI] [PubMed] [Google Scholar]
- 29. Mohtadi NG, Griffin DR, Pedersen ME, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33). Arthroscopy. 2012;28(5):595–605. [DOI] [PubMed] [Google Scholar]
- 30. Mullins K, Hanlon M, Carton P. Arthroscopic correction of femoroacetabular impingement improves athletic performance in male athletes. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2285–2294. [DOI] [PubMed] [Google Scholar]
- 31. Mygind-Klavsen B, Gronbech Nielsen T, Maagaard N, et al. Danish Hip Arthroscopy Registry: an epidemiologic and perioperative description of the first 2000 procedures. J Hip Preserv Surg. 2016;3(2):138–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Palmer AJR, Ayyar Gupta V, Fernquest S, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. BMJ. 2019;364:l185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Reiman MP, Agricola R, Kemp JL, et al. Consensus recommendations on the classification, definition and diagnostic criteria of hip-related pain in young and middle-aged active adults from the International Hip-related Pain Research Network, Zurich 2018. Br J Sports Med. 2020;54(11):631–641. [DOI] [PubMed] [Google Scholar]
- 34. Reiman MP, Thorborg K, Hölmich P. Femoroacetabular impingement surgery is on the rise---but what is the next step? J Orthop Sports Phys Ther. 2016;46(6):406–408. [DOI] [PubMed] [Google Scholar]
- 35. Stone AV, Beck EC, Malloy P, et al. Preoperative predictors of achieving clinically significant athletic functional status after hip arthroscopy for femoroacetabular impingement at minimum 2-year follow-up. Arthroscopy. 2019;35(11):3049–3056. [DOI] [PubMed] [Google Scholar]
- 36. Thomeé R, Jonasson P, Thorborg K, et al. Cross-cultural adaptation to Swedish and validation of the Copenhagen Hip and Groin Outcome Score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):835–842. [DOI] [PubMed] [Google Scholar]
- 37. Thorborg K, Branci S, Stensbirk F, Jensen J, Hölmich P. Copenhagen Hip and Groin Outcome Score (HAGOS) in male soccer: reference values for hip and groin injury-free players. Br J Sports Med. 2014;48(7):557–559. [DOI] [PubMed] [Google Scholar]
- 38. Thorborg K, Hölmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med. 2011;45(6):478–491. [DOI] [PubMed] [Google Scholar]
- 39. Thorborg K, Kraemer O, Madsen AD, Hölmich P. Patient-reported outcomes within the first year after hip arthroscopy and rehabilitation for femoroacetabular impingement and/or labral injury: the difference between getting better and getting back to normal. Am J Sports Med. 2018;46(11):2607–2614. [DOI] [PubMed] [Google Scholar]
- 40. Thorborg K, Tijssen M, Habets B, et al. Patient-reported outcome (PRO) questionnaires for young to middle-aged adults with hip and groin disability: a systematic review of the clinimetric evidence. Br J Sports Med. 2015;49(12):812. [DOI] [PubMed] [Google Scholar]
- 41. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–835. [DOI] [PubMed] [Google Scholar]
- 42. Wayne WD. Biostatistics: A Foundation for Analysis in the Health Sciences. 7th ed. Wiley and Sons; 1999. [Google Scholar]
- 43. Wolfson TS, Ryan MK, Begly JP, Youm T. Outcome trends after hip arthroscopy for femoroacetabular impingement: when do patients improve? Arthroscopy. 2019;35(12):3261–3270. [DOI] [PubMed] [Google Scholar]
- 44. Wright AA, Hensley CP, Gilbertson J, Leland JM, 3rd, Jackson S. Defining Patient Acceptable Symptom State thresholds for commonly used patient reported outcomes measures in general orthopedic practice. Man Ther. 2015;20(6):814–819. [DOI] [PubMed] [Google Scholar]
- 45. Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. [DOI] [PubMed] [Google Scholar]