Abstract
A hospitalist-run medical short-stay unit (MSSU) was created at a university-affiliated teaching hospital in Montreal in 1989. Its primary aim was to provide efficient and high-quality care to patients requiring a brief stay in hospital for short-lived medical conditions. After evaluation in the emergency department (ED), patients judged to have acute conditions requiring a short hospital stay are admitted directly to the MSSU. Conversely, patients with more complex conditions requiring a longer stay in hospital are admitted to a clinical teaching unit (CTU). Care in the MSSU is provided by a rotating group of hospitalists. Ensuring the admission of appropriate patients during non-daytime hours was the main difficulty identified. Preliminary evaluation of the MSSU suggested that ED consultants were effective at selecting suitable patients for admission to the MSSU, because only 1 in 5 patients later required transfer to other hospital wards. The 5 most common MSSU discharge diagnoses were asthma and chronic obstructive lung disease, pneumonia, congestive heart failure, urinary tract infection and cellulitis. MSSU patients had a shorter length of stay, lower rates of in-hospital complications and lower rates of readmission within 30 days of discharge compared with CTU patients. Our hospitalist-run MSSU appears to offer a workable system of health care delivery for patients with acute, self-limited illness requiring a brief stay in hospital. The MSSU appeared to promote the efficient use of hospital beds without compromising patient outcomes, however, further research is required to compare the efficiency and outcomes of care directly with that provided by the traditional CTU system.
In the face of rising health care costs in Canada and the United States, effective means to reduce patients' length of stay in hospital while maintaining high- quality care have been sought.1,2 Advocates of the hospitalist movement suggest that the availability and expertise of on-site hospitalists (internists who primarily care for inpatients) lead to more efficient use of hospital resources and improved quality of care.3,4,5,6 In 1989, a hospitalist-run medical short-stay unit (MSSU) was opened at the Sir Mortimer B. Davis Jewish General Hospital, a university-affiliated tertiary care center. A key premise in instituting a designated MSSU was that admitting physicians would be able to identify accurately patients suitable for admission to a short-stay unit. It was also postulated that the efficiency and quality of patient care might be improved if patients with short-lived medical conditions thought to require a brief stay in hospital were admitted to a distinct inpatient unit rather than to one of the clinical teaching units (CTUs). Such patients would be cared for by a core group of hospitalists who would, over time, become increasingly expert in managing similar patients.
In this paper, we describe the evolution, structure, process and pitfalls of our hospitalist-run MSSU. We also report the results of a preliminary evaluation of the MSSU that assessed whether physicians are able to identify accurately patients suitable for admission to a short-stay unit and whether the care provided appears to be efficient without compromising patient outcomes.
Program description
In the late 1980s, our hospital experienced a severe problem with emergency department (ED) overcrowding predominantly by medical patients awaiting hospital admission. In part because of limitations in house staff numbers, it was not possible to expand the existing general medicine CTUs to accommodate these patients. It was proposed that the Department of Medicine open a staff-run short-stay medical unit, in the hope of taking the pressure off the ED and providing targeted care to patients requiring brief admission. When inaugurated in 1989, the MSSU was a 9-bed unit within a 637-bed university teaching hospital for adult patients. It expanded to 12 beds (3 rooms, each with 4 beds) in 1997 and 16 beds (4 rooms, each with 4 beds) in 1998 because of an increase in the number of ED patients requiring medical admission. During the first 2 years, MSSU patients were managed by their individual consulting subspecialists but, with the establishment of the Division of Internal Medicine in 1990, the MSSU evolved into a unit staffed exclusively by hospital-based internists.
The MSSU is now a geographically distinct 16-bed unit with its own regular nursing and physician staff. All attending staff physicians in the MSSU are internists–hospitalists from within a core group of 7 physicians who are members of the hospital's Division of Internal Medicine and also serve as Internal Medicine consultants to the ED.
After evaluation in the ED by the Internal Medicine consultant, patients who are judged to have acute conditions that require a brief (1–3 days) stay in hospital and who are likely to be discharged as soon as their medical problems no longer require a stay in hospital are selected by the consultant for direct admission to the MSSU. The consultant writes a detailed admission note and admitting orders. Once admitted to the MSSU, patients are assessed and managed by a hospitalist physician who rotates through the unit on a weekly to biweekly basis. The physician does rounds in the MSSU twice daily and is available on-site all day to confer with nurses, consultants, ancillary staff and family members, to check test results and to address problems that arise throughout the day. A hospitalist from within the same core group provides coverage on weekend days. At night, the unit is signed out to and covered by the ED-based Internal Medicine overnight resident, with backup from the attending hospitalist as needed. In order to keep the flow of patients moving, the physician and the discharge planning nurse initiate discharge planning on the first hospital day. After hospital discharge, MSSU patients are seen within 1–2 weeks in the Division of Internal Medicine's daily clinic to follow up on their clinical status and review the results of any outstanding tests. Thereafter, they are followed by their usual physician, who receives a copy of the summary of their admission to and their stay in hospital.
Conversely, patients who are judged by the ED-based internist to have complex medical conditions that require extensive investigation or longer duration of treatment, or both, are admitted to 1 of 2 general medicine CTUs where they are cared for by a ward team made up of residents and medical students who are directly supervised by the CTU attending physician. The flow of patients to and from these areas is depicted in Fig. 1.
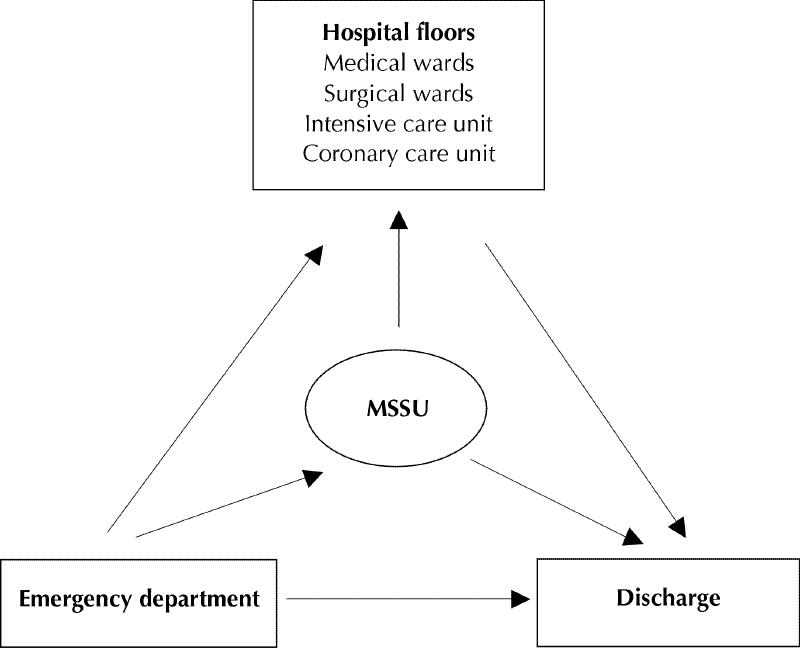
Fig. 1: Flow of patients. MSSU = medical short-stay unit.
During the daytime, the attending hospitalist is able to “protect” MSSU beds for exclusive use by short-stay patients. During off-hours, however, if beds are available in the MSSU but not on the CTUs, medical patients awaiting CTU admission are occasionally admitted to the MSSU by the ED-based overnight resident. Although these patients can be transferred to the CTUs the next day, the use of the MSSU as a holding area with subsequent transfer to another unit is inefficient for patients, nurses and doctors alike. Nevertheless, during periods of increased pressure on medical beds, we have found it difficult to enforce strictly a policy preventing these admissions. Clearly, each hospital would have to determine the optimal number of short-stay beds appropriate for the volume and case mix of its medical patients, because the more this optimal number is exceeded, the greater the risk of misuse of these beds.
Because our MSSU is situated in a university-affiliated teaching hospital, an issue that merits exploration is whether the removal of those patients admitted to the MSSU from the pool of patients available to medical trainees on the CTUs has a measurable adverse impact on their training because of lack of exposure to “short-stay” types of medical problems.
Because of recent interest expressed in the medical literature in assessing the impact of hospitalists on inpatient care,2,3,6 we conducted a preliminary assessment of the effectiveness of the MSSU. We used computerized administrative discharge data to assess whether ED-based Internal Medicine consultants could accurately identify suitable patients for MSSU admission and to examine indicators of the efficiency of bed use for MSSU patients compared with CTU patients. In our evaluation, CTU data were used simply as benchmarks of “usual” care because the 2 patient populations are clearly different with regard to case mix, case severity, comorbidity and social conditions.
Methods
We retrospectively identified all patients discharged from the MSSU and the CTUs from Apr. 1, 1995, to Mar. 31, 1996, which was a stable, 1-year window prior to the expansion of the MSSU to 12 beds in 1997 and then to 16 beds in 1998. Data on age, sex, discharge diagnosis, complication rate, death rate, hospital readmission during the month post discharge, number of subspecialty consultations, length of stay and patient–bed ratio were obtained from our hospital's administrative database. Comparisons were made between patients discharged from the MSSU and those discharged from the CTUs.
Results
During the study period, there were 9 beds in the MSSU compared with 72 beds on the 2 CTUs combined (Table 1). The database provided discharge information only, where discharge refers to release from hospital or death. Over the 1-year study period, 865 patients were discharged from the MSSU. A review by hand of the MSSU admission logbook showed that 1094 patients were admitted to the MSSU during this same period. Thus, 4 of 5 patients admitted to the MSSU remained there until discharge, whereas 1 of 5 patients required transfer to other units (e.g., CTUs, surgical or intensive care units).
Table 1
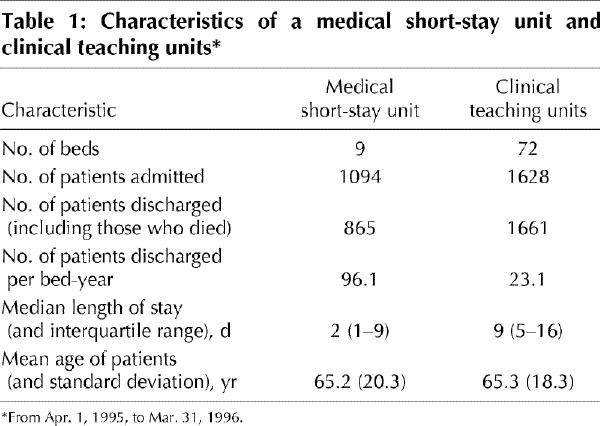
Bed occupancy in the MSSU was 96.1 patients/bed per year (compared with 23.1 patients/bed per year on the CTUs). The median length of stay in the MSSU was 2 days (interquartile range [IQR] 1–9 days) compared with 9 days (IQR 5–16 days) for the CTUs. The distribution of days spent in the MSSU and CTUs is illustrated in Fig. 2.
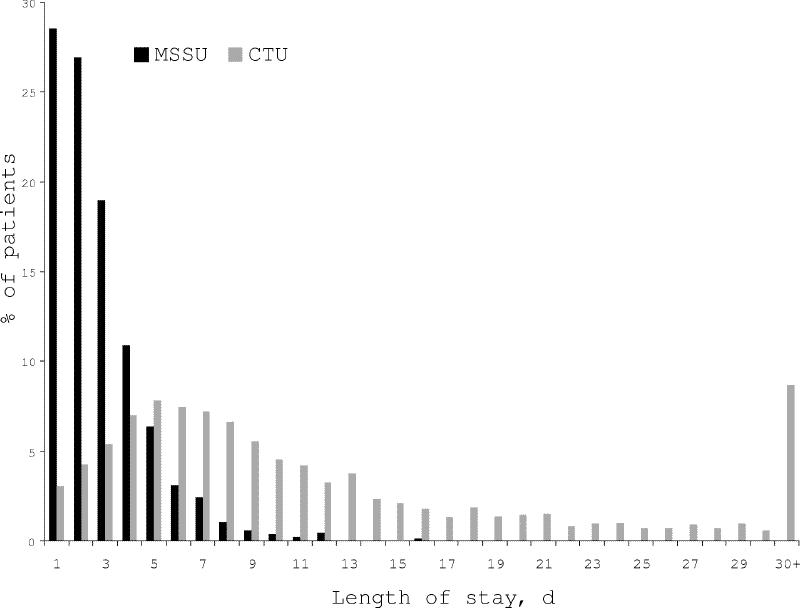
Fig. 2: Distribution of days spent in the MSSU and the CTUs. CTU = clinical teaching unit.
The mean age of MSSU patients was 65.2 years (standard deviation 20.3), and 48.7% were male (Table 1). The 5 most frequent principal discharge diagnoses were asthma and chronic obstructive lung disease (n = 126, 15%), pneumonia (n = 95, 11%), congestive heart failure (n = 57, 7%), urinary tract infection, including pyelonephritis (n = 52, 6%), and cellulitis (n = 40, 5%).
MSSU patients were less ill than CTU patients, as shown by lower rates of coded in-hospital complications such as urinary tract infection, drug rash, nosocomial pneumonia or diarrhea, and delirium (5% v. 31%), higher rates of discharge to their own homes (82% v. 74%) rather than to other settings and lower in-hospital mortality (1% v. 13%). One or more subspecialty consultations were requested by the treating physician for 39% of MSSU patients compared with 67% of CTU patients. The rate of readmission to hospital within 30 days of discharge was 9.6% in MSSU patients (compared with 13.9% in CTU patients). During the first 3 days post discharge, 2.2% of MSSU patients were readmitted, 1.2% were readmitted from 4 days to 1 week post discharge and 6.1% from 1 week to 1 month post discharge.
Discussion
In this paper, we have described the MSSU, a self-contained short-stay unit within a university teaching hospital staffed by a core group of internists–hospitalists. The MSSU is clearly viable, because it has been in operation for 11 years, with 2 expansions in bed capacity during this time. Our preliminary evaluation of its effectiveness suggests that consultant internists in our ED were able to identify appropriately patients suitable for admission to a short-stay unit, because 80% of patients admitted to the MSSU remained there until discharged from hospital and because patients selected for MSSU admission appeared to be less ill than CTU patients. This was indicated by their lower rates of complication, subspecialty consultations, in-hospital mortality, readmission within 30 days of discharge and by their higher rates of discharge to their own homes. Furthermore, compared with CTU patients, patients discharged from the MSSU had a shorter length of stay with a consequent higher turnover of beds. Patients' age or sex did not appear to influence the decision to admit to the MSSU as opposed to the CTUs, because these characteristics were similarly distributed in the 2 patient groups.
Although this preliminary evaluation did not permit direct comparison of patients with similar severity of illness admitted to the MSSU with those admitted to the CTUs, it is conceivable that selecting patients who are less ill for management in a dedicated unit may be more efficient than sending them to a CTU where patients with more complex problems occupy more of the ward team's time. The provision of care to MSSU patients by a core group of hospitalists and nurses who develop expertise in dealing with a narrower range of diagnoses than that found on the CTUs may also lead to more efficient care and better patient outcomes. However, these assumptions need to be formally tested by adjusting comparisons for important confounders such as case mix, case severity, comorbidity and social situation, by specifying process and outcome measures, and by distinguishing outcomes attributable to hospitalist-delivered care from those attributable to other changes in health care delivery.7 Examining in detail the characteristics of the 20% of patients initially admitted to the MSSU who required transfer to another unit is a matter of importance, because admission of these patients to the MSSU was probably inappropriate. Unfortunately, because we used computerized discharge data, we were unable to consider this in our preliminary evaluation, but we intend to address this issue in a more definitive comparative evaluation that is currently being developed. Another issue that merits study is whether the lack of exposure of medical trainees to “short-stay” patients leads to deficiencies in their training.
We found only one other report in English of a medical short-stay unit for adult patients admitted to hospital on the medical service. Bazarian and colleagues described a 16-bed, internist-run short-stay unit at a university teaching hospital whose case mix and mean length of stay (2.4 days) was similar to ours and whose initiation led to a reduction in the number of hours spent in the ED for patients with chest pain or asthma.8 A Spanish group9 reported the initiation of a short-stay medical unit at their institution that resulted in reductions in both mean length of stay among all medical patients (by 3.4 days) and in the number of medical patients admitted to a nonmedical ward because of a lack of beds in the medical ward. Other reports in the literature on designated short-stay units pertain to pediatric units,10 units attached to accident and emergency departments for patient observation after head trauma or intoxication11,12 or units to rule out acute coronary syndromes in low-risk patients.13
We conclude from our preliminary evaluation that our hospitalist-run MSSU appears to offer a feasible system of health care delivery to patients with acute, self-limited illness requiring a brief stay in hospital. Consultant internists in the ED were able to identify effectively suitable patients for admission to a medical short-stay unit. At first sight, the MSSU appears to promote the efficient use of hospital beds without compromising patient outcomes, however, further research is clearly needed to compare definitively the efficiency and outcomes of care delivered to similar patients in the MSSU with that in the traditional CTUs and to assess the impact of a staff-run MSSU on the training experience of medical students and residents. If the cost-effectiveness of our MSSU model can be demonstrated, implementation of similar hospitalist-run units should be considered by other hospitals.
Footnotes
This article has been peer reviewed.
Acknowledgements: We acknowledge the assistance of Sylvie Mayer from the Medical Records Department of the Sir Mortimer B. Davis Jewish General Hospital in assembling our patient database. We also wish to acknowledge the role of Dr. Harold Frank in the founding of our MSSU and thank him for helpful information concerning its early history.
Dr. Kahn is a Clinical Research Scholar supported by the Fonds de la Recherche en Santé du Québec.
Competing interests: None declared.
Reprint requests to: Dr. Susan R. Kahn, Center for Clinical Epidemiology and Community Studies, Sir Mortimer B. Davis Jewish General Hospital, Rm. A-130, 3755 Cote Ste Catherine Rd., Montreal QC H3T 1E2; fax 514 340-7564; susank@epid.jgh.mcgill.ca
References
- 1.Slataper R. Quality of care and the hospitalist. The hospitalist: newsletter of the National Association of Inpatient Physicians 1997;1:5-6.
- 2.Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA 1998;279:1560-5. [DOI] [PubMed]
- 3.Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med 1996;335:514-7. [DOI] [PubMed]
- 4.Freese RB. The Park Nicollet experience in establishing a hospitalist system. Ann Intern Med 1999;130:350-4. [DOI] [PubMed]
- 5.Wachter R. Hospitalists: their role in the American health care system. J Med Pract Manage 1997;Nov–Dec:123-6.
- 6.Sox HC. The hospitalist model: perspectives of the patient, the internist, and internal medicine. Ann Intern Med 1999;130:368-72. [DOI] [PubMed]
- 7.Showstack J, Katz PP, Weber E. Evaluating the impact of hospitalists. Ann Intern Med 1999;130:376-81 [DOI] [PubMed]
- 8.Bazarian JJ, Schneider SM, Newman VJ, Chodosh J. Do admitted patients held in the emergency department impact the throughput of treat-and-release patients? Acad Emerg Med 1996;3:1113-8. [DOI] [PubMed]
- 9.De la Iglesia Martinez F, Pellicer Vazquez C, Ramos Polledo V, Castro Romero B, Rodriguez Sotillo A, Diz-Lois Martinez F. [The short-stay medical unit of La Coruna: our experience.] [Spanish] An Med Interna 1997;14:125-7. [PubMed]
- 10.McConnochie KM, Russo MJ, McBride T, Szilagyi PG, Brooks AM, Roghmann KJ. How commonly are children hospitalized for asthma eligible for care in alternative settings? Arch Pediatr Adolesc Med 1999;153:49-55. [DOI] [PubMed]
- 11.Goodacre SW. Role of the short stay observation ward in accident and emergency department in the United Kingdom. J Accid Emerg Med 1998;15:26-30. [DOI] [PMC free article] [PubMed]
- 12.Hadden DS, Dearden CH, Rocke LG. Short stay observation patients: general wards are inappropriate. J Accid Emerg Med 1996;13:163-5. [DOI] [PMC free article] [PubMed]
- 13.Gaspoz JM, Lee TH, Weinstein MC, Cook EF, Goldman P, Komaroff AL, et al. Cost-effectiveness of a new short-stay unit to “rule out” acute myocardial infarction in low risk patients. J Am Coll Cardiol 1994;24:1249-59. [DOI] [PubMed]


