Abstract
Background
The Treatable ID App was created in 2012 as digital tool to improve early recognition and intervention for treatable inherited metabolic disorders (IMDs) presenting with global developmental delay and intellectual disability (collectively ‘treatable IDs’). Our aim is to update the 2012 review on treatable IDs and App to capture the advances made in the identification of new IMDs along with increased pathophysiological insights catalyzing therapeutic development and implementation.
Methods
Two independent reviewers queried PubMed, OMIM and Orphanet databases to reassess all previously included disorders and therapies and to identify all reports on Treatable IDs published between 2012 and 2021. These were included if listed in the International Classification of IMDs (ICIMD) and presenting with ID as a major feature, and if published evidence for a therapeutic intervention improving ID primary and/or secondary outcomes is available. Data on clinical symptoms, diagnostic testing, treatment strategies, effects on outcomes, and evidence levels were extracted and evaluated by the reviewers and external experts. The generated knowledge was translated into a diagnostic algorithm and updated version of the App with novel features.
Results
Our review identified 116 treatable IDs (139 genes), of which 44 newly identified, belonging to 17 ICIMD categories. The most frequent therapeutic interventions were nutritional, pharmacological and vitamin and trace element supplementation. Evidence level varied from 1 to 3 (trials, cohort studies, case–control studies) for 19% and 4–5 (case-report, expert opinion) for 81% of treatments. Reported effects included improvement of clinical deterioration in 62%, neurological manifestations in 47% and development in 37%.
Conclusion
The number of treatable IDs identified by our literature review increased by more than one-third in eight years. Although there has been much attention to gene-based and enzyme replacement therapy, the majority of effective treatments are nutritional, which are relatively affordable, widely available and (often) surprisingly effective. We present a diagnostic algorithm (adjustable to local resources and expertise) and the updated App to facilitate a swift and accurate workup, prioritizing treatable IDs. Our digital tool is freely available as Native and Web App (www.treatable-id.org) with several novel features. Our Treatable ID endeavor contributes to the Treatabolome and International Rare Diseases Research Consortium goals, enabling clinicians to deliver rapid evidence-based interventions to our rare disease patients.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13023-021-01727-2.
Keywords: Inborn error of metabolism, Metabolic disorders, Management, Therapy, Epilepsy, Intellectual developmental disorders, Diet, Pharmacological, Nutraceutical, Diagnostic, Outcomes, Evidence
Background
The past decade has seen revolutionary changes in the diagnosis and discovery of inherited metabolic disorders (IMDs), as well as development of new treatments [1]. Trials with small patient numbers remain challenging, but new methods for trial design, e.g., using natural history data as controls and crossover n-of-1 designs, have advanced our ability to determine whether treatments are effective or not [2]. What have these advances meant over the past decade for the treatment options of global developmental delay (DD according to the definition in Table 1A) and intellectual disability (ID), which is characterized by limitations starting before the age of 18 years in both intellectual functioning (IQ less than 70) and adaptive behavior. Our systematic literature review changed paradigms for this previously considered untreatable condition affecting 1–3% of the world’s population with substantial comorbidity, high lifetime costs, and emotional burden by identifying 81 treatable IDs in 2012, which increased to 89 in 2014 [3, 4]. With our review, we aimed to increase awareness and avoid the diagnostic and treatment delays so often suffered by rare diseases patients, with 25% of patients waiting 5 to 30 years for a diagnosis alone [5]. Now once again we address this medical gap and present an updated list of all Treatable IDs, which we define as IMDs which present with global developmental delay (DD) or ID yet are amenable to interventions targeting pathophysiology (e.g., nutraceutical, pharmacological, surgical, etc.) if initiated in a timely fashion.
Table 1.
A and B Definitions and search terms
| A. Definitions used in literature review |
|
Global developmental delay (DD): applied to age < 5 years; significant delay (= performance two standard deviations or more below the mean on age-appropriate, standardised norm-referenced testing) in two or more developmental domains including gross/fine motor skills, speech/language, cognition, social/personal, activities of daily living [53] Intellectual disability (ID): applied to age ≥ 5 years and manifesting before age 18 years, historically referred to as ‘mental retardation’; intellectual functioning level (IQ) less than 70 to 75 and significant limitations in two or more adaptive skills [54, 55] Inherited Metabolic Disorder (IMD): impairment of specific enzymes or biochemical pathways that is intrinsic to the pathomechanism. The presence of an abnormal metabolite is no longer a prerequisite [6]. This term excludes endocrine disorders such as hypothyroidism Causal of ID/DD: sufficient evidence in literature from bench and/or clinical research to make a pathophysiological relationship between IMD and ID/DD highly likely Treatable ID: if a particular therapeutic modality is capable of preventing or improving ID/DD phenotype, or halting/slowing neurocognitive decline (with acceptable adverse effects) in the IMD, i.e., positively influencing the ‘outcome measures’ Treatment strategies: Nutritional therapy, vitamin & trace element, enzyme replacement therapy, hematopoietic stem cell transplant, solid organ transplantation, pharmacological therapy, gene-based therapy, other (e.g., hemodialysis) Outcome measure/effect: A = improves psychomotor/cognitive development/IQ, B = improves behavioural/psychiatric disturbance(s), C = prevents acute metabolic decompensation, D = prevents, halts, or slows clinical deterioration, E = improves neurological manifestations (incl. neuro-imaging), F = improves seizure/epilepsy control, G = improves systemic manifestations Levels of evidence: Level of evidence: Level 1a = systematic review of RCT's, 1b = individual RCT, 1c = ‘All or None’ [= (prolongation of) survival with therapy]; Level 2a = systematic review of cohort studies, 2b = individual cohort study, 2c = ‘Outcomes Research’ [focused on end results of therapy for chronic conditions, including functioning and quality of life]; Level 3 = systematic review of case– control studies; Level 4 = individual case–control study or case-series/report; Level 5 = expert opinion without critical appraisal; based on physiology, bench research or first principles. If only one patient was reported, we assigned level ‘4–5′ as a way to nuance the treatment effects |
| B. Terms used for search strategy in PubMed [56] |
|
Developmental delay/intellectual disability: mental retardation, learning disorder(s), developmental disability/ disabilities, learning disability/disabilities, intellectual disability/disabilities, developmental delay, intelligence/classification, mentally disabled (persons), childhood/juvenile Alzheimer's, childhood/juvenile dementia, neurodegenerative disease Inherited Metabolic Disorder: metabolic disease(s), inborn error(s) of metabolism, metabolic disorder(s), metabolic condition(s), inherited metabolic disease(s), inherited metabolic disorder(s), biochemical disease(s) Treatment: treatment, management, therapy, cure, trial, (dietary) supplement, (dietary) restriction, diet, substrate inhibition, small molecule substrate reduction, enzyme replacement, vitamin(s), co-factor(s), bone marrow transplant, hematopoietic stem cell transplant, umbilical cord blood transplant(− ation), gene therapy |
There are several developments that should be considered to place the current overview of Treatable IDs in perspective. First, the new all-inclusive definition of an IMD, proposed in 2015 by Morava et al. [6] and recently endorsed by the international metabolic community in the International Classification of Inherited Metabolic Disorders (ICIMD): ‘Any condition in which the impairment of a biochemical pathway is intrinsic to the pathophysiology of the disease, regardless of whether there are abnormalities in currently available biochemical laboratory tests’(http://www.icimd.org) [7]. The number of IMDs now exceeds 1400 [8]. Second, the practice change our diagnostic algorithm has inspired, with international professional societies now prioritizing IMDs in the diagnostic evaluation of patients with ID in whom the cause is not evident after a thorough clinical exam [9–11] The digital tool ‘Treatable ID’ has certainly given this innovation a boost [12] as its digital accessibility proved useful both for educational as well as practical purposes (e.g., Continuum Child Neurology [13]), especially in remote areas where metabolic expertise might not be available onsite. The Treatable ID App was created in 2012, and is freely accessible as a Web App via http://www.treatable-id.org and since 2016 as a Native App via the App Store/Google Play. The App is designed for a target audience of various specialists evaluating children presenting with ID, both clinicians and laboratory scientists from student to expert level [12]. The Treatable ID App has a steady audience. Over the past 8 years there have been over 75,000 different users for the web App and over 10,000 downloads of the native App. The Treatable ID App is also part of the Treatable Intellectual Disability Endeavor (TIDE) diagnostic protocol [14]. In the second tier of the TIDE algorithm, the Treatable ID App is incorporated to optimize selection of targeted metabolic workup [14]. Also, numerous clinical and commercial labs have requested access to the Treatable ID gene lists for their quick turnaround phenotype-driven (virtual) gene panels. Third, as shown in a retrospective study by Sayson et al., using the Treatable ID algorithm can reduce costs and diagnostic delay for treatable IMDs underlying ID [15]. The same was shown in a prospective way, in our TIDE study which implemented the Treatable ID algorithm in 498 unexplained ID patients referred to a tertiary care centre (biochemical and clinical genetics as well as neurology departments) as add-on to clinical practice parameters at the time (2015). Indeed, this manuscript currently under review illustrates the presence of IMDs (6%) in this group of patients, even those without a classical multi-organ or degenerative phenotype (van Karnebeek et al. submitted) [16]. The fourth development is the remarkably large number of clinical trials with great promise, even pioneering gene-based therapy targeting the central nervous system, few of which however have made it to the real-world of reimbursed clinical care, and as such are not included here. Finally, despite the advances, the inequality in access to exome sequencing (ES) and other -omics technologies remains. Indeed, access determines the diagnostic approach; while for some countries and regions, metabolic testing is still the first tier, for others the exome-first approach has become standard of care [17]. Thus, algorithms must be tailored to local possibilities and expertise. Speed and accuracy are warranted as ‘time is brain’, i.e., early identification and intervention before irreversible damage is done [18]. Increasingly, therapy is center stage; even in the interpretation of genomic variants, response to therapy has been endorsed as a valuable criterion to determine pathogenicity [19]. The ultimate goal of creating a Treatabolome database comprising rare disease treatments at gene and variant levels was recently outlined [20]. Here, we contribute to this goal by presenting an updated state-of the-art overview of all treatable IDs along with a new version of the digital App freely accessible to professionals as well as patients, and suggest an updated diagnostic algorithm.
Material and methods
Our main goals were: (1) to identify all IMDs presenting with DD and/or ID (collectively termed ID in this paper) as a major feature, which are amenable to treatment targeting pathophysiology, supported by evidence in the literature reported up to January 2021, and (2) to translate this information into an updated version of the Treatable ID digital App, as well as (3) a diagnostic algorithm to facilitate early detection of treatable IMD in patients presenting with unexplained ID.
Literature review
For our literature review, we used a critical rather than a formal systematic literature review approach to answer the above stated question. We followed the Treatabolome approach as much as possible [20]. The systematic literature review in 2012 and its update in 2014 were used as a basis. Three independent reviewers (EH, CvK, SW) searched and critically appraised the literature, characterized the clinical and diagnostic recognition patterns as well as treatment modalities pertinent to the identified IMDs, and assessed the level of available evidence and effect of the various treatments on clinical outcome measures. The reviewers engaged in regular consensus meetings, and final decisions on any disagreements were reached by a majority vote of the reviewers plus an external expert (CRF).
Identification of treatable IMDs causing ID
Literature search
Definitions of terms relevant for the search strategy and keywords for terms DD, ID, IMD, and treatment are shown in Table 1A and B. We searched PubMed, restricted to English language and publication in peer-reviewed journals (http://www.ncbi.nlm.nih.gov/pubmed; 1960–January 2021) in a two-step approach. First, the 89 IMDs included in the 2012 and 2014 database were reassessed under consideration of the additional literature published; second, new treatable IDs were identified and reviewed. Additionally, the reference lists of identified articles, Orphanet [21] and Online Mendelian Inheritance in Man (OMIM) [22] were queried with the same search terms, and experts in the field were approached to identify new treatable IDs. To ensure comprehensiveness of treatment modalities, we identified all relevant references reporting outcome/effect for each of the selected treatments and IMDs. We searched bibliographies of included articles as well as PubMed (1960–January 2021) combining as keywords all known names for each IMD (including gene and enzyme) with the relevant therapeutic modalities (Table 1B).
Outcomes and levels of evidence
The ideal outcome of therapy for a treatable ID is the improvement of IQ and related developmental scores. As improvement of co-morbid features such as epilepsy, neurologic, behavioral or psychiatric problems is often a prerequisite for improved cognitive outcomes, these were included as ‘secondary outcomes’. Levels of evidence were defined and applied according to Table 1A.
Effect(s) of treatments on outcome measures
Effect(s) of treatment outcomes were defined as shown in Table 1A. We included treatments if they had a direct effect on ID (improvement or stabilization), or if there was a reasonable expectation that ID would be improved by significant improvement of other symptoms—such as seizures or severe movement disorders—thus making development possible. Supportive treatments and treatments with improvement only of systemic symptoms that were not reasonably related to ID were not included. If a treatment was not effective for all reported patients, we defined that at least a third of the patients needed to show improvement to ensure inclusion of potential beneficial treatments. All decisions on inclusion and exclusion of IMDs and treatments were mutually agreed upon during a final consensus meeting. In the previous review, a classification about standard of care versus individual basis was assigned to each treatment; given the growing attention to personalized medicine in IMD, we do not feel this distinction appropriate for our current review.
Inclusion/exclusion criteria
We included IMDs where ID was a major clinical feature (present in more than 50% of reported patients) and for which evidence supported amenability to the defined treatments with a positive effect on outcomes in at least one-third of patients.
Data extraction
For all IMDs meeting the criteria of a Treatable ID, the following information was captured:
Name of disease; gene and inheritance pattern; name of biochemical deficiency; group of disorder; screening and specific tests; neurological and non-neurological symptoms (only characteristic, specific and consistent symptoms were noted, see http://www.treatable-ID.org); treatment strategies (see Table 1A for categorization); specific therapies; level of evidence for each treatment and treatment effect (see Table 1A). Names and groups of disorders were based on the most recent ICIMD [7]. Disorders caused by pathogenic variants in multiple genes were reported as separate entries if there were meaningful differences in phenotype or treatment. For practical and user-friendliness purposes, if there were no meaningful differences, genes were grouped or ‘lumped’ and considered as one IMD.
Compliance to the FAIR guidelines for scientific data management and stewardship
We adhered as much as possible to the FAIR-compliant (findable, accessible, interoperable, reusable) template that will ultimately enable the building of a ‘Treatabolome’ database [20, 23]. We complied with the recommendations for a broad and inclusive literature search and the main elements of data extraction and data synthesis. The main deviation from the FAIR-compliant template in our review is that, due to the multitude of included IMDs, we did not perform a formal systematic review for each IMD. Furthermore, there are a few specific deviations from the template: we used OMIM gene/locus instead of phenotype OMIM numbers as we considered this approach more precise for the current review, and we did not specify all (contra)indications and marketing authorizations for each treatment due to of the multitude of included IMDs; this was outside the scope of this review.
Diagnostic tests and algorithm
We used our literature review results to update our diagnosed algorithm proposed in 2014. During the past years, ES has become accepted as first line tier testing in many countries around the world. However, metabolic screening is still applied given the specificity and sensitivity of tests, the short turnaround times and relative affordability and availability [24]. Metabolic profiles can also serve as functional readout, and “deep metabolic phenotyping” can help in the interpretation of genetic data. Therefore, we included both strategies in our algorithm to facilitate a practical guide for biochemical and genetic/genomic diagnosis. We first assessed which tests are necessary to identify each of the conditions. Accordingly, we grouped the IMDs into those diagnosed via ‘metabolic screening tests’ (1st Tier) versus IMDs diagnosed via ‘single test per single disease’ (2nd Tier) approach. First tier screening tests were defined as tests in blood and urine which are readily available in biochemical laboratories in most developed countries. Metabolic tests in the 2nd tier group evaluate Treatable IDs for which biochemical markers are difficult to interpret, and/or conventional diagnostic approach requires an invasive procedure or poorly accessible test (i.e., only performed in few centres worldwide). Furthermore, we analyzed which IMDs have no (reliable) biomarker profile and require primary molecular or (targeted) ES analysis. This approach with different strategies and tiers was then translated into a step-wise algorithm.
Treatable ID App design and development
The Treatable ID App was created in 2012 and later updated based on the 2012 and 2014 literature reviews [3, 4]. In 2021, the Treatable ID App has been updated and improved extensively both in content and design. The content is updated based on our 2021 literature search with updated and increased links to useful resources for each IMD. The design has been adapted to 2021 standards with a quick and solid interface. Both the Web App and the Native App use the same database which is an improvement over the previous version. As a result, new information can be added easily and this will ensure the content is always up to date. The database is built in Oracle.
The Web App can be used in all major browsers and the Native app can be downloaded from the App Store and Google Play. The creation of the Treatable ID App is supported and funded by the ‘Metakids Foundation’ in The Netherlands [25].
Results
Literature review
Treatable IDs
Our first systematic review identified 81 treatable IDs [3] and was updated with another 8 disorders in 2014 [4]. From these 89 disorders, our current literature search led to exclusion of 20 treatable IDs, because of insufficient evidence for effect of treatment on established outcome measures (n = 10), ID no longer considered a major clinical feature (n = 8), metabolic defect not causative of ID (n = 1) and duplicate disorder (n = 1). The disorders are listed in Additional File 1: Table 1.
Of the 69 remaining treatable IDs we grouped the following IMDs according to the method described: (1) Glycine encephalopathy due to aminomethyltransferase (AMT) or glycine decarboxylase (GLDC) deficiency; (2) Electron transfer flavoprotein subunit alpha (ETFA)/subunit beta (ETFB)/dehydrogenase deficiency (ETFDH); 3) Branched-chain ketoacid dehydrogenase E1 alpha (BCKDHA)/beta (BCKDHB)/E2 (DBT) deficiency; (4) Propionic acidemia due to propionyl-CoA carboxylase subunit alpha (PCCA)/beta (PCCB) deficiency; (5) Niemann-Pick disease type C1 (NPC1)/C2 (NPC2); (6) Pyruvate dehydrogenase E1 alpha (PDHA1)/beta (PDHB)/E2 (DLAT)/E3 (DLD)/E3BP (PDHX) deficiency; (7) ATP-sensitive potassium channel regulatory/pore-forming subunit superactivity (ABCC8/KCNJ11); (8) Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MTTL1/MTTQ/MTTH/MTTK/MTTC/MTTS1/MTND1/MTND5/MTND6/MTTS2).
We further ‘split’ two previously grouped (‘lumped’) disorders into five separate disease entities: 1) Coenzyme Q5 methyltransferase deficiency, 2) Coenzyme Q8A (ADCK3) deficiency, 3) Methylmalonic aciduria and homocystinuria, cblD type, 4) Homocystinuria, cblDv1 type, 5) Methylmalonic aciduria, cblDv2 type. This led to a final list of 72 treatable IDs that were already included in the 2014 database. Our literature search for “new” treatable IDs identified 44 disorders, combining to a total number of 116 treatable IDs included in this 2021 update and shown in Table 2 (new disorders are marked with an *).
Table 2.
Overview of 116 treatableIDs and diagnostic tests
| Group of disorder | Name of disorder | Gene(s) | Orphanet# | OMIM gene/locus# | HPO# | Diagnostic test |
|---|---|---|---|---|---|---|
| Congenital disorders of glycosylation | SLC35A2-CDG* | SLC35A2 (X-linked) | 356,961 | 314,375 | 7355 | Serum transferrin/N-glycan profiling |
| Congenital disorders of glycosylation | SLC35C1-CDG* | SLC35C1-CDG (AR) | 99,843 | 605,881 | 55,343 | Serum transferrin/N-glycan profiling |
| Congenital disorders of glycosylation | PMM2-CDG* | PMM2 (AR) | 79,318 | 601,785 | 5373 | Serum transferrin/N-glycan profiling |
| Congenital disorders of glycosylation | PIGA-CDG* | PIGA (X-linked) | – | 311,770 | – | Molecular testing |
| Congenital disorders of glycosylation | PIGM-CDG* | PIGM (AR) | 83,639 | 610,273 | 93,183 | Molecular testing |
| Congenital disorders of glycosylation | PIGO-CDG* | PIGO (AR) | 247,262 | 614,730 | 84,720 | Molecular testing |
| Disorders of amino acid metabolism | Arginase deficiency (synonym: argininemia) | ARG1 (AR) | 90 | 608,313 | 383 |
Plasma amino acids Plasma ammonia |
| Disorders of amino acid metabolism | Argininosuccinate lyase deficiency | ASL (AR) | 23 | 608,310 | 435 |
Plasma amino acids Plasma ammonia |
| Disorders of amino acid metabolism | Argininosuccinate synthetase deficiency (synonym: citrullinemia type 1) | ASS1 (AR) | 247,525 | 603,470 | 445 |
Plasma amino acids Plasma ammonia |
| Disorders of amino acid metabolism | Citrin deficiency | SLC25A13 (AR) | 247,582 | 603,859 | 10,165 | Plasma amino acids |
| Disorders of amino acid metabolism | Methionine synthase deficiency (synonym: homocystinuria-megaloblastic anemia, cblG type) | MTR (AR) | 2170 | 156,570 | 4548 | Plasma total homocysteine |
| Disorders of amino acid metabolism | Carbamoyl phosphate synthetase 1 deficiency | CPS1 (AR) | 147 | 608,307 | 1373 | Plasma amino acids |
| Disorders of amino acid metabolism | Mitochondrial sulfur dioxygenase deficiency (synonym: ethylmalonic encephalopathy) | ETHE1 (AR) | 51,188 | 608,451 | 23,474 |
Urine organic acids Plasma acylcarnitines Molecular testing |
| Disorders of amino acid metabolism | Glutaryl-CoA dehydrogenase deficiency (synonym: glutaric aciduria type 1) | GCDH (AR) | 25 | 608,801 | 2639 |
Plasma acylcarnitines Urine organic acids |
| Disorders of amino acid metabolism | Mitochondrial ornithine transporter deficiency (synonym: hyperornithinemia-hyperammonemia-homocitrullinuria syndrome) | SLC25A15 (AR) | 415 | 603,861 | 10,116 |
Plasma amino acids Plasma ammonia |
| Disorders of amino acid metabolism | Cystathionine beta-synthase deficiency (synonym: classic homocystinuria) | CBS (AR) | 394 | 613,381 | 875 |
Urine organic acids Plasma total homocysteine |
| Disorders of amino acid metabolism | Isovaleryl-CoA dehydrogenase deficiency (synonym: isovaleric acidemia) | IVD (AR) | 33 | 607,036 | 3712 |
Plasma acylcarnitines Urine organic acids |
| Disorders of amino acid metabolism | N-acetylglutamate synthase deficiency | NAGS (AR) | 927 | 608,300 | 162,417 |
Plasma amino acids Plasma ammonia |
| Disorders of amino acid metabolism | Glycine encephalopathy due to aminomethyltransferase (AMT) or glycine decarboxylase (GLDC) deficiency (synonym: nonketotic hyperglycinemia) | AMT/GLDC (AR) | 407 | 238,310 (AMT), 238,300 (GLDC) | 275 (AMT), 2731 (GLDC) |
Plasma amino acids CSF amino acids |
| Disorders of amino acid metabolism | Branched-chain ketoacid dehydrogenase E1 alpha (BCKDHA)/beta (BCKDHB)/E2 (DBT) deficiency (synonym: maple syrup urine disease type 1a (BCKDHA)/2 (DBT); Dihydrolipoyl transacylase deficiency (DBT)) | BCKDHA/BCKDHB/ DBT (AR) | 268,145, 268,162, 268,184 | 608,348 (BCKDHA), 248,611 (BCKDHB), 248,610 (DBT) | 593 (BCKDHA), 594 (BCKDHB), 1629 (DBT) | Plasma amino acids |
| Disorders of amino acid metabolism | Methylmalonic aciduria due to methylmalonyl-CoA mutase deficiency | MMUT (AR) | 289,916, 79,312 | 609,058 | 4594 |
Plasma acylcarnitines Urine organic acids Blood lactate Plasma ammonia |
| Disorders of amino acid metabolism | Ornithine transcarbamylase deficiency | OTC (X-linked) | 664 | 300,461 | 5009 |
Plasma amino acids Urine organic acids |
| Disorders of amino acid metabolism | Phenylalanine hydroxylase deficiency (synonym: phenylketonuria) | PAH (AR) | 79,254 | 612,349 | 5053 | Plasma amino acids |
| Disorders of amino acid metabolism | 3-phosphoglycerate dehydrogenase deficiency | PHGDH (AR) | 79,351 | 606,879 | 26,227 |
Plasma amino acids CSF amino acids |
| Disorders of amino acid metabolism | Phosphoserine aminotransferase deficiency | PSAT1 (AR) | 284,417 | 610,936 | 29,968 |
Plasma amino acids CSF amino acids |
| Disorders of amino acid metabolism | Propionic acidemia due to propionyl-CoA carboxylase subunit alpha (PCCA)/beta (PCCB) deficiency | PCCA/PCCB (AR) | 35 | 232,000 (PCCA), 232,050 (PCCB) | 5095 (PCAA), 5096 (PCCB) |
Plasma acylcarnitines Urine organic acids Blood lactate Plasma ammonia |
| Disorders of amino acid metabolism | Phosphoserine phosphatase deficiency | PSPH (AR) | 79,350 | 172,480 | 5723 |
Plasma amino acids CSF amino acids |
| Disorders of amino acid metabolism | Tyrosine aminotransferase deficiency (synonyms: tyrosinemia type 2; Richner-Hanhart syndrome) | TAT (AR) | 28,378 | 613,018 | 6898 |
Plasma amino acids Urine organic acids |
| Disorders of amino acid metabolism | Branched-chain ketoacid dehydrogenase kinase deficiency* | BCKDK (AR) | 308,410 | 614,901 | 10,295 | Plasma amino acids |
| Disorders of amino acid metabolism | Carbonic anhydrase VA deficiency | CA5A (AR) | 401,948 | 114,761 | 763 |
Plasma amino acids Plasma ammonia blood lactate molecular testing |
| Disorders of amino acid metabolism | 3-hydroxyisobutyryl-CoA hydrolase deficiency (synonym: beta-hydroxyisobutyryl-CoA deacylase deficiency)* | HIBCH (AR) | 88,639 | 250,620 | 26,275 |
Urine organic acids Molecular testing |
| Disorders of amino acid metabolism | Mitochondrial short-chain enoyl-CoA hydratase 1 deficiency* | ECHS1 (AR) | 255,241 | 616,277 | 1892 |
Urine organic acids Molecular testing |
| Disorders of amino acid metabolism | S-adenosylhomocysteine hydrolase deficiency* | AHCY (AR) | 88,618 | 613,752 | 191 |
Plasma amino acids Plasma total homocysteine |
| Disorders of amino acid metabolism | Glutamine synthetase deficiency* | GLUL (AR) | 71,278 | 610,015 | 2752 |
Plasma amino acids CSF amino acids |
| Disorders of carbohydrate metabolism | GLUT1 deficiency | SLC2A1 (AD) | 71,277 | 138,140 | 6513 | CSF other (CSF:blood glucose ratio) |
| Disorders of complex molecule degradation | Alpha-mannosidase deficiency | MAN2B1 (AR) | 309,282, 309,288 | 609,458 | 4125 | Urine oligosaccharides** |
| Disorders of complex molecule degradation | Aspartylglucosaminidase deficiency | AGA (AR) | 93 | 613,228 | 175 | Urine oligosaccharides** |
| Disorders of complex molecule degradation | Iduronate sulfatase deficiency (synonym: Hunter syndrome) | IDS (X-linked) | 217,085 | 300,823 | 3423 | Urine glycosaminoglycans** |
| Disorders of complex molecule degradation | Alpha-iduronidase deficiency (synonyms: Hurler syndrome [severe]; Scheie syndrome [attenuated]) | IDUA (AR) | 93,473 | 252,800 | 3425 | Urine glycosaminoglycans** |
| Disorders of complex molecule degradation | Arylsulfatase A deficiency | ARSA (AR) | 309,256, 309,263, 309,271 | 607,574 | 410 | Enzymatic testing (Arylsulfatase A) |
| Disorders of complex molecule degradation | Niemann-Pick disease type C1 (NPC1)/C2 (NPC2) | NPC1/NPC2 (AR) | 646 | 607,623 (NPC1), 601,015 (NPC2) | 4864 (NPC1), 10,577 (NPC2) | Plasma (oxy-)sterols |
| Disorders of complex molecule degradation | Beta-glucuronidase deficiency (synonym: Sly syndrome) | GUSB (AR) | 584 | 611,499 | 2990 | Urine glycosaminoglycans** |
| Disorders of complex molecule degradation | Tripeptidyl-peptidase 1 deficiency (synonym: CLN2 disease)* | TPP1 (AR) | 228,349 | 607,998 | 1200 | Enzymatic testing (Tripeptidyl-peptidase 1) |
| Disorders of complex molecule degradation | Alpha-fucosidase deficiency* | FUCA1 (AR) | 349 | 230,000 | 2517 | Urine glycosaminoglycans** |
| Disorders of complex molecule degradation | CLN7 disease* | MFSD8 (AR) | 228,366 | 611,124 | 256,471 | Molecular testing |
| Disorders of energy substrate metabolism | Arginine:glycine amidinotransferase (AGAT) deficiency | GATM (AR) | 35,704 | 602,360 | 2628 | (Plasma/) urine creatine & guanidinoacetate |
| Disorders of energy substrate metabolism | Creatine transporter deficiency | SLC6A8 (X-linked) | 52,503 | 300,036 | 6535 | Urine creatine & guanidinoacetate |
| Disorders of energy substrate metabolism | Guanidinoacetate methyltransferase deficiency | GAMT (AR) | 382 | 601,240 | 2593 | Urine creatine & guanidinoacetate |
| Disorders of energy substrate metabolism | Pyruvate dehydrogenase E1 alpha (PDHA1)/beta (PDHB)/E2 (DLAT)/E3 (DLD)/E3BP (PDHX) deficiency | PDHA1 (X-linked)/PDHB/DLAT/DLD/PDHX (AR) | 79,243 (PDHA1), 255,138 (PDHB), 79,244 (DLAT), 2394 (DLD), 255,182 (PDHX) | 300,502 (PDHA1), 179,060 (PDHB), 608,770 (DLAT), 238,331 (DLD), 608,769 (PDHX) | 5160 (PDHA1), 5162 (PDHB), 1737 (DLAT), 1738 (DLD), 8050 (PDHX) |
CSF other (lactate:pyruvate ratio) other (blood lactate:pyruvate ratio) |
| Disorders of energy substrate metabolism | Pyruvate dehydrogenase phosphatase deficiency* | PDP1 (AR) | 79,246 | 605,993 | 54,704 |
Plasma amino acids Urine organic acids |
| Disorders of fatty acid, carnitine, and ketone body metabolism | Mitochondrial acetoacetyl-CoA thiolase deficiency | ACAT1 (AR) | 134 | 607,809 | 38 | Urine organic acids |
| Disorders of fatty acid, carnitine, and ketone body metabolism | Electron transfer flavoprotein subunit alpha (ETFA)/subunit beta (ETFB)/dehydrogenase deficiency (ETFDH) (synonym: glutaric acidemia type 2A/2B/2C; multiple acyl-CoA dehydrogenase deficiency type 2A/2B/2C) | ETFA/ETFB/ETFDH (AR) | 26,791 | 608,053 (ETFA), 130,410 (ETFB), 231,675 (ETFDH) | 2108 (ETFA), 2109 (ETFB), 2110 (ETFDH) |
Plasma acylcarnitines Urine organic acids |
| Disorders of fatty acid, carnitine, and ketone body metabolism | 3-hydroxy-3-methylglutaryl-CoA lyase deficiency | HMGCL (AR) | 20 | 613,898 | 3115 | Urine organic acids |
| Disorders of fatty acid, carnitine, and ketone body metabolism | Mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase deficiency | HMGCS2 (AR) | 35,701 | 600,234 | 3158 | Urine organic acids |
| Disorders of fatty acid, carnitine, and ketone body metabolism | Epsilon-N-trimethyllysine hydroxylase deficiency* | TMLHE (X-linked) | 300,777 | 55,217 | Plasma acylcarnitines | |
| Disorders of lipid metabolism | X-linked adrenoleukodystrophy | ABCD1 (X-linked) | 139,396, 139,396 | 300,371 | 215 | Plasma very long chain fatty acids |
| Disorders of lipid metabolism | Sterol 27-hydroxylase deficiency (synonym: cerebrotendinous xanthomatosis) | CYP27A1 (AR) | 909 | 606,530 | 1593 | Other (plasma cholestanol) |
| Disorders of lipid metabolism | 7-dehydrocholesterol reductase deficiency | DHCR7 (AR) | 818 | 602,858 | 1717 | Plasma (oxy-)sterols |
| Disorders of mitochondrial cofactor biosynthesis | Coenzyme Q5 methyltransferase deficiency | COQ5 (AR) | 616,359 | 84,274 | Molecular testing*** | |
| Disorders of mitochondrial cofactor biosynthesis | Coenzyme Q8A (ADCK3) deficiency | COQ8A (AR) | 139,485 | 606,980 | 56,997 | Molecular testing |
| Disorders of nucleobase, nucleotide and nucleic acid metabolism | Isoleucyl-tRNA synthetase 1 deficiency* | IARS1 (AR) | 541,423 | 600,709 | 3376 | Molecular testing |
| Disorders of nucleobase, nucleotide and nucleic acid metabolism | Leucyl-tRNA synthetase 1 deficiency* | LARS1 (AR) | 370,088 | 151,350 | 51,520 | Molecular testing |
| Disorders of nucleobase, nucleotide and nucleic acid metabolism | Phenylalanyl-tRNA synthetase subunit beta deficiency* | FARSB (AR) | 178,506 | 609,690 | 10,056 | Molecular testing |
| Disorders of nucleobase, nucleotide and nucleic acid metabolism | Seryl-tRNA synthetase 1 deficiency* | SARS1 (AR) | 88,616 | 607,529 | 6301 | Molecular testing |
| Disorders of nucleobase, nucleotide and nucleic acid metabolism | Methionyl-tRNA synthetase 1 deficiency* | MARS1 (AR) | 397,735, 401,835, 440,427 | 156,560 | 4141 | Molecular testing |
| Disorders of nucleobase, nucleotide and nucleic acid metabolism | Phosphoribosylpyrophosphate synthetase deficiency* | PRPS1 (X-linked) | 1187 | 311,850 | 5631 | Urine purines & pyrimidines |
| Disorders of nucleobase, nucleotide and nucleic acid metabolism | CAD trifunctional protein deficiency* | CAD (AR) | 448,010 | 114,010 | 790 | Molecular testing |
| Disorders of peptide and amine metabolism | NRF2 superactivity (synonym: immunodeficiency, developmental delay, and hypohomocysteinemia)* | NFE2L2 (AD) | 600,492 | 4780 | Plasma total homocysteine | |
| Disorders of trace elements and metals | Hereditary ceruloplasmin deficiency | CP (AR) | 48,818 | 117,700 | 1356 | Copper & ceruloplasmin |
| Disorders of trace elements and metals | Copper-transporting ATPase subunit alpha deficiency (synonyms: Menkes disease [severe]; occipital horn syndrome [milder]) | ATP7A (AR) | 565 | 300,011 | 538 | copper & Ceruloplasmin |
| Disorders of trace elements and metals | Copper-transporting ATPase subunit beta deficiency (synonym: Wilson disease) | ATP7B (AR) | 905 | 606,882 | 540 | Copper & ceruloplasmin |
| Disorders of trace elements and metals | SLC39A8 deficiency* | SLC39A8 (AR) | 468,699 | 608,732 | 64,116 | Other (serum zinc, sialotransferrins, manganese, CSF lactate) |
| Disorders of trace elements and metals | MEDNIK syndrome | AP1S1 (AR) | 171,851 | 609,313 | 1174 |
Copper & ceruloplasmin Molecular testing |
| Disorders of vitamin and cofactor metabolism | Thiamine transporter 2 deficiency (synonym: biotin-thiamine-responsive basal ganglia disease) | SLC19A3 (AR) | 65,284, 199,348 | 606,152 | 80,704 | Molecular testing |
| Disorders of vitamin and cofactor metabolism | Biotinidase deficiency | BTD (AR) | 79,241 | 609,019 | 686 | Enzymatic testing (Biotinidase) |
| Disorders of vitamin and cofactor metabolism | Folate receptor alpha deficiency (synonym: neurodegeneration due to cerebral folate transport deficiency) | FOLR1 (AR) | 217,382 | 136,430 | 2348 | CSF other (methyltetrahydrofolate) |
| Disorders of vitamin and cofactor metabolism | Methylmalonic aciduria, cblA type | MMAA (AR) | 79,310 | 607,481 | 166,785 | Urine organic acids |
| Disorders of vitamin and cofactor metabolism | Methylmalonic aciduria, cblB type | MMAB (AR) | 79,311 | 607,568 | 326,625 | Urine organic acids |
| Disorders of vitamin and cofactor metabolism | Methylmalonic aciduria and homocystinuria, cblC type | MMACHC (AR) | 79,282 | 609,831 | 25,974 |
Urine organic acids Plasma total homocysteine |
| Disorders of vitamin and cofactor metabolism | Methylmalonic aciduria and homocystinuria, cblD type | MMADHC (AR) | 79,283 | 611,935 | 27,249 |
urine organic acids Plasma total homocysteine |
| Disorders of vitamin and cofactor metabolism | Homocystinuria, cblDv1 type | MMADHC (AR) | 308,380 | 611,935 | 27,249 | Plasma total homocysteine |
| Disorders of vitamin and cofactor metabolism | Methylmalonic aciduria, cblDv2 type | MMADHC (AR) | 308,442 | 611,935 | 27,249 | Urine organic acids |
| Disorders of vitamin and cofactor metabolism | Methionine synthase reductase deficiency (synonym: homocystinuria-megaloblastic anemia, cblE type) | MTRR (AR) | 2169 | 603,568 | 4552 | Plasma total homocysteine |
| Disorders of vitamin and cofactor metabolism | Methylmalonic aciduria and homocystinuria, cblF type | LMBRD1 (AR) | 79,284 | 612,625 | 55,788 |
Urine organic acids Plasma total homocysteine |
| Disorders of vitamin and cofactor metabolism | Methylmalonic aciduria and homocystinuria, cblJ type* | ABCD4 (AR) | 369,955 | 603,214 | 5826 |
Urine organic acids Plasma total homocysteine |
| Disorders of vitamin and cofactor metabolism | Dihydropteridine reductase deficiency | QDPR (AR) | 226 | 612,676 | 5860 |
CSF neurotransmitters Other (biopterin loading test) |
| Disorders of vitamin and cofactor metabolism | Autosomal recessive GTP cyclohydrolase 1 deficiency | GCH1 (AR) | 2102 | 600,225 | 2643 | CSF neurotransmitters |
| Disorders of vitamin and cofactor metabolism | Holocarboxylase synthetase deficiency | HLCS (AR) | 79,242 | 609,018 | 3141 | Urine organic acids |
| Disorders of vitamin and cofactor metabolism | Cyclic pyranopterin monophosphate synthase deficiency (synonym: molybdenum cofactor deficiency type A) | MOCS1 (AR) | 308,386 | 603,707 | 4337 |
Urine purines & pyrimidines Urine sulfites/S-sulfocysteine, (serum uric acid) |
| Disorders of vitamin and cofactor metabolism | 5,10-methylenetetrahydrofolate reductase deficiency | MTHFR (AR) | 395 | 607,093 | 4524 |
Plasma amino acids Plasma total homocysteine |
| Disorders of vitamin and cofactor metabolism | 6-pyruvoyl-tetrahydropterin synthase deficiency | PTS (AR) | 13 | 612,719 | 5805 |
CSF neurotransmitters Other (biopterin loading test) |
| Disorders of vitamin and cofactor metabolism | Alpha-aminoadipic semialdehyde dehydrogenase deficiency (synonym: pyridoxine-dependent epilepsy) | ALDH7A1 (AR) | 3006 | 107,323 | 501 | Other (plasma P6C, urine alpha-aminoadipic semialdehyde) |
| Disorders of vitamin and cofactor metabolism | Sepiapterin reductase deficiency | SPR (AR) | 70,594 | 182,125 | 6697 |
CSF neurotransmitters Other (biopterin loading test) |
| Disorders of vitamin and cofactor metabolism | 5,10-methenyltetrahydrofolate synthetase deficiency (synonym: 5-formyltetrahydrofolate cycloligase deficiency)* | MTHFS (AR) | - | 604,197 | 10,588 |
CSF neurotransmitters CSF other (tetrahydrofolate & neopterin) |
| Disorders of vitamin and cofactor metabolism | Dihydrofolate reductase deficiency | DHFR (AR) | 319,651 | 126,060 | 1719 |
CSF neurotransmitters CSF other (tetrahydrofolate) |
| Disorders of vitamin and cofactor metabolism | Sodium-dependent multivitamin transporter deficiency* | SLC5A6 (AR) | – | 604,024 | 8884 | molecular testing |
| Disorders of vitamin and cofactor metabolism | Pyridoxamine 5′-phosphate oxidase deficiency* | PNPO (AR) | 79,096 | 603,287 | 55,163 |
CSF amino acids CSF other (vitamins) Molecular testing |
| Disorders of vitamin and cofactor metabolism | Thiamine pyrophosphokinase deficiency* | TPK1 (AR) | 293,955 | 614,458 | 27,010 |
CSF neurotransmitters Urine organic acids Blood lactate |
| Disorders of vitamin and cofactor metabolism | NAD(P)HX epimerase deficiency* | NAXE (AR) | 555,407 | 608,862 | 128,240 |
Molecular testing Blood lactate |
| Disorders of vitamin and cofactor metabolism | Mitochondrial thiamine pyrophosphate transporter deficiency* | SLC25A19 (AR) | 217,396 | 606,521 | 60,386 | Molecular testing |
| Disorders of vitamin and cofactor metabolism | Transcobalamin II deficiency* | TCN2 (AR) | 859 | 275,350 | 6948 |
Urine organic acids Plasma total homocysteine |
| Disorders of vitamin and cofactor metabolism | Proton-coupled folate transporter deficiency (synonym: hereditary folate malabsorption)* | SLC46A1 (AR) | 90,045 | 229,050 | 113,235 |
Serum/RBC folate CSF other (folate) CSF neurotransmitters |
| Endocrine metabolic disorders | ATP-sensitive potassium channel regulatory/pore-forming subunit superactivity* | ABCC8 (AD/AR)/KCNJ11 (AD) | 79,134 | 600,509 | 6833 | Molecular testing |
| mtDNA-related disorders | Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MTTL1/MTTQ/MTTH/MTTK/MTTC/MTTS1/MTND1/MTND5/MTND6/MTTS2) | MT-ND1/MT-ND4/MT-ND5/MT-ND6/MT-CO1/MT-CPO2/MT-CO3/ MT-TQ/MT-TH/MT-TL1/MT-TF/MT-TS1/MT-TS2/MT-TW (Mt) | 550 | 516,000 (MT-ND1), 516,003 (MT-ND4), 516,005 (MT-ND5), 516,006 (MT-ND6), 516,030 (MT-CO1), 516,040 (MT-CO2), 516,050 (MT-CO3), 590,030 (MT-TQ), 590,040 (MT-TH), 590,050 (MT-TL1), 590,070 (MT-TF), 590,080 (MT-TS1), 590,085 (MT-TS2), 590,095 (MT-TW) | 4535 (MT-ND1), 4536 (MT-ND4), 4540 (MT-ND5), 4541 (MT-ND6), 4512 (MT-CO1), 4513 (MT-CO2), 4514 (MT-CO3), 4572 (MT-TQ), 4574 (MT-TS1), 4578 (MT-TW) | Molecular testing blood lactate |
| Neurotransmitter disorders | Succinic semialdehyde dehydrogenase deficiency | ALDH5A1 (AR) | 22 | 610,045 | 7915 | Urine organic acids |
| Neurotransmitter disorders | Tyrosine hydroxylase deficiency | TH (AR) | 101,150 | 191,290 | 7054 | CSF neurotransmitters |
| Neurotransmitter disorders | Vesicular monoamine transporter 2 deficiency | SLC18A2 (AR) | 352,649 | 193,001 | 6571 | CSF neurotransmitters |
| Neurotransmitter disorders | Aromatic L-amino acid decarboxylase deficiency* | DDC (AR) | 35,708 | 107,930 | 1644 | CSF neurotransmitters |
| Neurotransmitter disorders | Ionotropic glutamate receptor NMDA type subunit 1 dysregulation* | GRIN1 (AD) | - | 138,249 | 2902 | Molecular testing |
| Neurotransmitter disorders | Ionotropic glutamate receptor NMDA type subunit 2A dysregulation* | GRIN2A (AD) | 289,266 | 138,253 | 2903 | Molecular testing |
| Neurotransmitter disorders | Ionotropic glutamate receptor NMDA type subunit 2B dysregulation* | GRIN2B (AD) | - | 138,252 | 2904 | Molecular testing |
| Neurotransmitter disorders | Ionotropic glutamate receptor NMDA type subunit 2D superactivity* | GRIN2D (AD) | 442,835 | 602,717 | 2906 | Molecular testing |
| Neurotransmitter disorders | DNAJC12 deficiency* | DNAJC12 (AR) | 508,523 | 617,384 | 56,521 |
Plasma amino acids CSF neurotransmitters |
| Nuclear-encoded disorders of oxidative phosphorylation | ACAD9 deficiency* | ACAD9 (AR) | 99,901 | 611,126 | 28,976 | other (muscle OXPHOS) |
| Other disorders of mitochondrial function | Mitochondrial aspartate-glutamate carrier isoform 1 deficiency (synonym: aralar deficiency)* | SLC25A12 (AR) | 353,217 | 612,949 | 8604 | Molecular testing |
| Other disorders of mitochondrial function | Mitochondrial aspartate aminotransferase deficiency* | GOT2 (AR) | - | 138,150 | 2806 |
Plasma amino acids Plasma ammonia Blood lactate |
Names and groups of disorders were based on the most recent International Conference on Inherited Metabolic Disorders (ICIMD) classification. OMIM = Online Mendelian Inheritance in Man®. HPO = Human Phenotype Ontology. Mode of inheritance for each gene is denoted as AD = autosomal dominant; AR = autosomal recessive; X-linked (dominant); Mt = mitochondrial. CSF = cerebrospinal fluid. * = new treatable ID (not included in previous database/review). ** = also identified by targeted enzyme testing. *** = consider white blood cells or muscle tissue CoQ10 analysis
Classification
Included treatable IDs belonged to the following 17 ICIMD categories: vitamin and cofactor metabolism 29 (25%), amino acid metabolism 28 (24%), complex molecule degradation 10 (9%), neurotransmitters 9 (8%), nucleobase, nucleotide and nucleic acid metabolism 7 (6%), disorders of glycosylation 6 (5%), energy substrate metabolism 5 (4%), trace elements and metals 5 (4%), fatty acid, carnitine, and ketone body metabolism 5 (4%), lipid metabolism 3 (3%), mitochondrial cofactor biosynthesis 2 (2%), other disorders of mitochondrial function 2 (2%), carbohydrate metabolism 1 (1%), peptide and amine metabolism 1 (1%), endocrine metabolic disorders 1 (1%), mtDNA-related disorders 1 (1%), and nuclear-encoded disorders of oxidative phosphorylation 1 (1%).
Types of treatment and levels of evidence
The different types of treatment as defined in Table 1A are shown per disorder in Table 3. Nutritional therapy was the most frequently used treatment strategy (32%), followed by pharmacological therapy 22%, vitamin and trace element substitution 22%, solid organ transplantation 8%, hematopoietic stem cell transplant 4%, enzyme replacement therapy 3%, gene-based therapy 2% and other therapy 7% (multiple treatments per disease entity were possible).
Table 3.
Overview of all causal therapies
| Name of disorder | Treatment strategy | Treatment | Level of evidence | Effect of treatment | ReferenceS |
|---|---|---|---|---|---|
| 3-hydroxy-3-methylglutaryl-CoA lyase deficiency | Nutritional therapy | Protein defined diet, avoid fasting, sick day management | 5 | C | [57] |
| 3-hydroxyisobutyryl-CoA hydrolase deficiency (synonym: beta-hydroxyisobutyryl-CoA deacylase deficiency) | Nutritional therapy | Valine restriction | 4 | A, E, G | [58] |
| 3-phosphoglycerate dehydrogenase deficiency | Nutritional therapy | L-Serine, glycine | 4 | D, E, F | [59] |
| 5,10-methenyltetrahydrofolate synthetase deficiency (synonym: 5-formyltetrahydrofolate cycloligase deficiency) | Vitamin & trace element | 5-methyltetrahydrofolate, methylcobalamin | 5 | E | [60] |
| 5,10-methylenetetrahydrofolate reductase deficiency | Nutritional therapy | Carnitine, methionine | 4 | C, D, G | [61] |
| Vitamin & trace element | Betaine, folate ± | 4 | C, D, G | [61] | |
| 6-pyruvoyl-tetrahydropterin synthase deficiency | Nutritional therapy | Phenylalanine-reduced diet ± | 4 | D, E | [62] |
| Vitamin & trace element | Folinic acid ± | 4 | A, E, F | [62] | |
| Pharmacological therapy | L-dopa + carbidopa, 5-Hydroxytryptophan, sapropterin dihydrochloride (synthetic BH4) co-factor therapy | 4 | A, B, E, F, G | [62] | |
| 7-dehydrocholesterol reductase deficiency | Nutritional therapy | Cholesterol | 4 | G | [63, 64] |
| Pharmacological therapy | Simvastatin | 1b | B | [63, 64] | |
| ACAD9 deficiency | Vitamin & trace element | Riboflavin | 4 | A, E | [65] |
| Alpha-aminoadipic semialdehyde dehydrogenase deficiency (synonym: pyridoxine-dependent epilepsy) | Nutritional therapy | Lysine restriction, arginine | 4 | A, D, E, F | [66] |
| Vitamin & trace element | Pyridoxine | 4 | A, D, E, F | [66] | |
| Alpha-fucosidase deficiency | Stem cell therapy | (Umbilical cord/bone marrow) hematopoietic stem cell transplantation | 4 | D, E, G | [67] |
| Alpha-iduronidase deficiency (synonyms: Hurler syndrome [severe]; Scheie syndrome [attenuated]) | Enzyme replacement therapy | Intrathecal iduronidase | 2b | A, D, G | [68, 69] |
| Stem cell therapy | Hematopoietic stem cell transplantation | 1c | D, G | [68, 69] | |
| Alpha-mannosidase deficiency | Enzyme replacement therapy | Velmanase alfa | 1c | D | [70, 71] |
| Stem cell therapy | Hematopoietic stem cell transplantation | 4 to 5 | D, E | [70, 71] | |
| Arginase deficiency (synonym: argininemia) | Nutritional therapy | Protein defined diet, arginine or citrulline | 2b, effect on growth 4 | B, C, D, E, G | [72] |
| Pharmacological therapy | Sodium phenylbutyrate, glycerol phenylbutyrate, sodium benzoate | 2b | B, C, D, E | [72] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [72] | |
| Solid organ transplant | Liver transplantation | 4 | A, B, D, E | [72] | |
| Arginine:glycine amidinotransferase (AGAT) deficiency | Nutritional therapy | Creatine | 4 | A, D, E | [73] |
| Argininosuccinate lyase deficiency | Nutritional therapy | Protein defined diet, arginine or citrulline | 2b, effect on growth 4 | B, C, D, E, G | [72] |
| Pharmacological therapy | Sodium phenylbutyrate, glycerol phenylbutyrate, sodium benzoate | 2b | B, C, D, E | [72] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [72] | |
| Solid organ transplant | Liver transplantation | 4 | A, B, D, E, systemic phenotype persists | [72] | |
| Argininosuccinate synthetase deficiency (synonym: citrullinemia type 1) | Nutritional therapy | Protein defined diet, arginine or citrulline | 2b, effect on growth 4 | B, C, D, E, G | [72] |
| Pharmacological therapy | Sodium phenylbutyrate, glycerol phenylbutyrate, sodium benzoate | 2b | B, C, D, E | [72] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [72] | |
| Solid organ transplant | Liver transplantation | 4 | A, B, D, E | [72] | |
| Aromatic L-amino acid decarboxylase deficiency | Pharmacological therapy | Dopamine agonist, monoamine oxidase (MAO) inhibitors, L-dopa + carbidopa (depending on mutation) | 4 | E, G | [74, 75] |
| Vitamin & trace element | Pyridoxine, folinic acid ± | 4 | E, G | [74, 75] | |
| Gene-based therapy | Gene therapy | 4 | A, B, E | [74, 75] | |
| Arylsulfatase A deficiency | Gene-based therapy | OTL-200 (stem cell-based gene therapy) | 2c | A, E | [76, 77] |
| Stem cell therapy | Hematopoietic stem cell transplantation | 4 to 5 | D | [76, 77] | |
| Aspartylglucosaminidase deficiency | Stem cell therapy | Hematopoietic stem cell transplantation | 4 to 5 | D | [78] |
| ATP-sensitive potassium channel regulatory/pore-forming subunit superactivity | Pharmacological therapy | Sulfonylurea | 4 | A, B, E, G | [79, 80] |
| Autosomal recessive GTP cyclohydrolase 1 deficiency | Nutritional therapy | Phenylalanine-reduced diet ± | 4 | D, E | [62] |
| Vitamin & trace element | Folinic acid ± | 4 | A, E, F | [62] | |
| Pharmacological therapy | L-dopa + carbidopa, 5-Hydroxytryptophan, sapropterin dihydrochloride (synthetic BH4) co-factor therapy | 4, 4 to 5 for 5-Hydroxytryptophan | A, B, E, F, G | [62] | |
| Beta-glucuronidase deficiency (synonym: Sly syndrome) | Enzyme replacement therapy | Vestronidase | 4 | A, G | [81] |
| Stem cell therapy | Hematopoietic stem cell transplantation | 4 | D, G | ||
| Biotinidase deficiency | Vitamin & trace element | Biotin | 2c | A, E, G | [82] |
| Branched-chain ketoacid dehydrogenase E1 alpha (BCKDHA)/beta (BCKDHB)/E2 (DBT) deficiency (synonym: maple syrup urine disease type 1a (BCKDHA)/2 (DBT); Dihydrolipoyl transacylase deficiency (DBT)) | Nutritional therapy | Restriction of branched chain amino acids, isoleucine, valine, avoid fasting, sick day management | 4 | A, C, D, G | [83, 84] |
| Vitamin & trace element | Thiamine ± | 4 | C, D, G | [83, 84] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [83, 84] | |
| Solid organ transplant | Liver transplantation | 4 | C, D, G | [83, 84] | |
| Branched-chain ketoacid dehydrogenase kinase deficiency | Nutritional therapy | Branched-chain amino acid supplementation | 5 | A, B, G | [85] |
| CAD trifunctional protein deficiency | Pharmacological therapy | Uridine | 4 | A, F | [30] |
| Carbamoyl phosphate synthetase 1 deficiency | Nutritional therapy | Protein defined diet, arginine or citrulline | 2b, effect on growth 4 | B, C, D, E, G | [72] |
| Pharmacological therapy | Sodium phenylbutyrate, glycerol phenylbutyrate, sodium benzoate, N-carbamyl-L-glutamate (carglumic acid) | 2b, 4 to 5 for carglumic acid | B, C, D, E, D for carglumic acid | [72] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [72] | |
| Solid organ transplant | Liver transplantation | 4 | A, B, D, E | [72] | |
| Carbonic anhydrase VA deficiency | Nutritional therapy | Sick day management | 4 | C, D | [86] |
| Pharmacological therapy | N-carbamyl-L-glutamate (carglumic acid) | 4 | C, D | [86] | |
| Citrin deficiency | Nutritional therapy | High-protein/high-fat/low-carbohydrate diet, avoid fasting, avoid glucose iv, lactose restriction, medium -chain triglycerides | 4 | B, C, D, E, F, G | [87] |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [87] | |
| Solid organ transplant | Liver Transplantation | 4 | C | [87] | |
| CLN7 disease | Gene based therapy | (Intrathecal) milasen | 4 to 5 | F | [36] |
| Coenzyme Q5 methyltransferase deficiency | Vitamin & trace element | CoQ10 | 4 to 5 | A, B, E | [88] |
| Coenzyme Q8A (ADCK3) deficiency | Vitamin & trace element | CoQ10 | 4 to 5 | E | [89] |
| Copper-transporting ATPase subunit alpha deficiency (synonyms: Menkes disease [severe]; occipital horn syndrome [milder]) | Pharmacological therapy | Copper histidine | 4 | D | [90] |
| Copper-transporting ATPase subunit beta deficiency (synonym: Wilson disease) | Vitamin & trace element | Zinc | 4 | A, E, G | [91, 92] |
| Pharmacological therapy | Copper chelators, tetrathiomolybdate | 4, 1b for tetrathiomolybdate | A, E, G | [91, 92] | |
| Creatine transporter deficiency | Nutritional therapy | Creatine, glycine, arginine | 4 | A, F | [93] |
| Cyclic pyranopterin monophosphate synthase deficiency (synonym: molybdenum cofactor deficiency type A) | Pharmacological therapy | Cyclic pyranopterin monophosphate | 2b | A, F | [94] |
| Cystathionine beta-synthase deficiency (synonym: classic homocystinuria) | Nutritional therapy | Protein defined diet, methionine restriction | 2c | C, D, G | [95] |
| Vitamin & trace element | Pyridoxine, betaine | 2c | D, E, G | [95] | |
| Dihydrofolate reductase deficiency | Vitamin & trace element | Folic acid | 4 | F, G | [96] |
| Dihydropteridine reductase deficiency | Nutritional therapy | Phenylalanine-reduced diet | 4 | D, E | [62] |
| Vitamin & trace element | Folinic acid | 4 | A, E, F | [62] | |
| Pharmacological therapy | L-dopa + carbidopa, 5-Hydroxytryptophan, sapropterin dihydrochloride (synthetic BH4) co-factor therapy ± | 4 | A, B, E, F, G | [62] | |
| DNAJC12 deficiency | Pharmacological therapy | BH4, L-dopa + carbidopa ± , 5-hydroxytryptophan ± | 4 | A, D, E | [97] |
| Electron transfer flavoprotein subunit alpha (ETFA)/subunit beta (ETFB)/dehydrogenase deficiency (ETFDH) (synonym: glutaric acidemia type 2A/2B/2C; multiple acyl-CoA dehydrogenase deficiency type 2A/2B/2C) | Nutritional therapy | Carnitine | 5 | C, D | [98] |
| Vitamin & trace element | Riboflavin | 5 | C, D | [98] | |
| Nutritional therapy | Beta-hydroxybutyrate | 2c | E, G | [98] | |
| Epsilon-N-trimethyllysine hydroxylase deficiency | Nutritional therapy | Carnitine | 4 to 5 | A, B, C | [99] |
| Folate receptor alpha deficiency (synonym: neurodegeneration due to cerebral folate transport deficiency) | Vitamin & trace element | Folinic acid | 4 | A, D, E, F | [100] |
| GLUT1 deficiency | Nutritional therapy | Ketogenic diet | 4 | F | [101] |
| Pharmacological therapy | Triheptanoin | 2b | A, E | [102] | |
| Glutamine synthetase deficiency | Nutritional therapy | Glutamine | 4 to 5 | A, E | [103] |
| Glutaryl-CoA dehydrogenase deficiency (synonym: glutaric aciduria type 1) | Nutritional therapy | Protein defined diet, lysine restriction, carnitine | 2c | C, D, E, G | [44] |
| Glycine encephalopathy due to aminomethyltransferase (AMT) or glycine decarboxylase (GLDC) deficiency (synonym: nonketotic hyperglycinemia) | Pharmacological therapy | Sodium benzoate, N-nitrosodimethylamine receptor antagonists | 4 | B, D, E, F | [104] |
| Guanidinoacetate methyltransferase deficiency | Nutritional therapy | Arginine restriction, creatine and ornithine | 4 | B, D, E, F | [105] |
| Hereditary ceruloplasmin deficiency | Other | Iron chelation | 4 | D, E | [106] |
| Holocarboxylase synthetase deficiency | Vitamin & trace element | Biotin | 4 | D | [107] |
| Homocystinuria, cblDv1 type | Vitamin & trace element | Hydroxycobalamin, betaine ± | 4 | C, D, G | [61] |
| Iduronate sulfatase deficiency (synonym: Hunter syndrome) | Stem cell therapy | Hematopoietic stem cell transplantation | 4 | D, E, G | [108] |
| Ionotropic glutamate receptor NMDA type subunit 1 dysregulation | Pharmacological therapy | Memantine | 4 to 5 | A, F | [109] |
| Ionotropic glutamate receptor NMDA type subunit 2A dysregulation | Pharmacological therapy | Memantine, IVIG | 4 | F | [110, 111] |
| Ionotropic glutamate receptor NMDA type subunit 2B dysregulation | Nutritional therapy | L-serine (for loss-of-function mutations) | 4 to 5 | A | [112] |
| Ionotropic glutamate receptor NMDA type subunit 2D superactivity | Pharmacological therapy | Memantine, IVIG | 4 | A, F | [111, 113] |
| Isoleucyl-tRNA synthetase 1 deficiency | Nutritional therapy | L-isoleucine, natural protein fortification | 4 to 5 | A, E, G | [114, 115] |
| Isovaleryl-CoA dehydrogenase deficiency (synonym: isovaleric acidemia) | Nutritional therapy | Protein defined diet, carnitine, avoid fasting, sick day management | 2c | C, G | [116] |
| Pharmacological therapy | N-carbamyl-L-glutamate (carglumic acid) | 4 | C, G | [116] | |
| Leucyl-tRNA synthetase 1 deficiency | Nutritional therapy | L-leucine, natural protein fortification | 4 to 5 | A, E, G | [114, 115] |
| MEDNIK syndrome | Vitamin & trace element | Zinc acetate | 4 to 5 | A, B, G | [117] |
| Methionine synthase deficiency (synonym: homocystinuria-megaloblastic anemia, cblG type) | Vitamin & trace element | Hydroxycobalamin, betaine ± | 4, 5 for betaine | C, D, G | [61] |
| Methionine synthase reductase deficiency (synonym: homocystinuria-megaloblastic anemia, cblE type) | Vitamin & trace element | Hydroxycobalamin, betaine ± | 4, 5 for betaine | C, D, G | [61] |
| Methionyl-tRNA synthetase 1 deficiency | Nutritional therapy | Methionine, increase protein intake | 5 | A, G | [118] |
| Methylmalonic aciduria and homocystinuria, cblC type | Nutritional therapy | Carnitine ± | 5 | C, D, G | [61] |
| Vitamin & trace element | Hydroxycobalamin, betaine | 4 | C, D, G | [61] | |
| Methylmalonic aciduria and homocystinuria, cblD type | Nutritional therapy | Carnitine ± | 5 | A, D, G | [61] |
| Vitamin & trace element | Hydroxycobalamin, betaine ± | 4 to 5, 5 for betaine | A, D, G | [61] | |
| Methylmalonic aciduria and homocystinuria, cblF type | Vitamin & trace element | Hydroxycobalamin, betaine | 4 | D, G | [61] |
| Methylmalonic aciduria and homocystinuria, cblJ type | Vitamin & trace element | Hydroxycobalamin, betaine ± | 4 to 5, 5 for betaine | D, G | [119] |
| Methylmalonic aciduria due to methylmalonyl-CoA mutase deficiency | Nutritional therapy | Protein defined diet, carnitine, avoid fasting, sick day management | 2c | C, D, G | [120] |
| Pharmacological therapy | N-carbamyl-L-glutamate (carglumic acid), sodium benzoate, antibiotics | 4 | C, D, G | [120] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [120] | |
| Solid organ transplant | Liver and/or kidney transplantation | 4 | C, D, G | [120] | |
| Methylmalonic aciduria, cblA type | Nutritional therapy | Protein defined diet, carnitine, avoid fasting, sick day management | 4 | C, D, G | [120] |
| Vitamin & trace element | Hydroxycobalamin | 4 | C, D, G | [120] | |
| Pharmacological therapy | N-carbamyl-L-glutamate (carglumic acid), sodium benzoate, antibiotics | 4 | D | [120] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [120] | |
| Solid organ transplant | Liver transplantation and/or kidney transplantation | 4 | C, D, G | [120] | |
| Methylmalonic aciduria, cblB type | Nutritional therapy | Protein defined diet, carnitine, avoid fasting, sick day management | 4 | C, D, G | [120] |
| Vitamin & trace element | Hydroxycobalamin | 4 | C, D, G | [120] | |
| Pharmacological therapy | N-carbamyl-L-glutamate (carglumic acid), sodium benzoate, antibiotics | 4 | D | [120] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [120] | |
| Solid organ transplant | Liver transplantation and/or kidney transplantation | 4 | C, D, G | [120] | |
| Methylmalonic aciduria, cblDv2 type | Nutritional therapy | Protein defined diet, carnitine, avoid fasting, sick day management | 4 | C, D, G | [120] |
| Vitamin & trace element | Hydroxycobalamin | 4 | C, D, G | [120] | |
| Pharmacological therapy | N-carbamyl-L-glutamate (carglumic acid), sodium benzoate, antibiotics | 4 | D | [120] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [120] | |
| Solid organ transplant | Liver transplantation and/or kidney transplantation | 4 | C, D, G | [120] | |
| Mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase deficiency | Nutritional therapy | Avoid Fasting, sick day management, dietary precursor restriction ± | 5 | C | [121] |
| Mitochondrial acetoacetyl-CoA thiolase deficiency | Nutritional therapy | Avoid fasting, sick day management, protein restriction, isoleucine restriction | 5 | C | [122] |
| Mitochondrial aspartate aminotransferase deficiency | Nutritional therapy | L-serine | 4 | A | [123] |
| Vitamin & trace element | Pyridoxine | 4 | A, F | [123] | |
| Mitochondrial aspartate-glutamate carrier isoform 1 deficiency (synonym: aralar deficiency) | Nutritional therapy | Ketogenic diet | 4 | A, E, F | [124] |
| Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MT-ND1/MT-ND4/MT-ND5/MT-ND6/MT-CO1/MT-CPO2/MT-CO3/ MT-TQ/MT-TH/MT-TL1/MT-TF/MT-TS1/MT-TS2/MT-TW) | Nutritional therapy | Arginine, citrulline, taurine | 4 to 5, 2b for Taurine | C, D, E, F | [125, 126] |
| Mitochondrial ornithine transporter deficiency (synonym: hyperornithinemia-hyperammonemia-homocitrullinuria syndrome) | Nutritional therapy | Protein defined diet, arginine or citrulline | 2b, effect on growth 4 | B, C, D, E, G | [72] |
| Pharmacological therapy | Sodium phenylbutyrate, glycerol phenylbutyrate, sodium benzoate | 2b | B, C, D, E | [72] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [72] | |
| Solid organ transplant | Liver transplantation | 4 to 5 | A, B, D, E, systemic phenotype persists | [72] | |
| Mitochondrial short-chain enoyl-CoA hydratase 1 deficiency | Nutritional therapy | Valine restriction | 4 | A, E, G | [58] |
| Mitochondrial sulfur dioxygenase deficiency (synonym: ethylmalonic encephalopathy) | Pharmacological therapy | N-acetylcysteine, antibiotics | 4 | E, G | [127] |
| Solid organ transplant | Liver transplantation | 4 | A | [127] | |
| Mitochondrial thiamine pyrophosphate transporter deficiency | Vitamin & trace element | Thiamine | 4 | C, D | [128] |
| N-acetylglutamate synthase deficiency | Nutritional therapy | Protein defined diet, arginine or citrulline | 2b, effect on growth 4 | B, C, D, E, G | [72] |
| Pharmacological therapy | Sodium phenylbutyrate, glycerol phenylbutyrate, sodium benzoate, N-carbamyl-L-glutamate (carglumic acid) | 2b, 4 for carglumic acid | B, C, D, E, D for carglumic acid | [72] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [72] | |
| Solid organ transplant | Liver transplantation | 4 | A, B, D, E | [72] | |
| NAD(P)HX epimerase deficiency | Vitamin & trace element | Niacin, CoQ10 | 4 to 5 | A, G | [129] |
| Niemann-Pick disease type C1 (NPC1)/C2 (NPC2) | Pharmacological therapy | Miglustat, intrathecal 2-hydroxypropyl-β-cyclodextrin | 1b, 2b for 2-hydroxypropyl-β-cyclodextrin | D, E | [130, 131] |
| NRF2 superactivity (synonym: immunodeficiency, developmental delay, and hypohomocysteinemia) | Vitamin & trace element | Ascorbic acid | 4 to 5 | A | [132] |
| Pharmacological therapy | Luteolin | 4 to 5 | A | [132] | |
| Ornithine transcarbamylase deficiency | Nutritional therapy | Protein defined diet, arginine or citrulline | 2b, effect on growth 4 | B, C, D, E, G | [72] |
| Pharmacological therapy | Sodium phenylbutyrate, glycerol phenylbutyrate, sodium benzoate | 2b | B, C, D, E | [72] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [72] | |
| Solid organ transplant | Liver transplantation | 4 | A, B, D, E | [72] | |
| Phenylalanine hydroxylase deficiency (synonym: phenylketonuria) | Nutritional therapy | Protein defined diet, phenylalanine-free L-amino acid suppletion/Glycomacropeptide (GMP), large neutral amino acid (LNAA), fatty acids | 2a, GMP 4 | B, D, E | [43] |
| Pharmacological therapy | Sapropterin dihydrochloride (synthetic BH4) co-factor therapy | 1b | B, D, E | [43] | |
| Enzyme replacement therapy | Pegvaliase | 1b | B, D, E | [43] | |
| Phenylalanyl-tRNA synthetase subunit beta deficiency | Nutritional therapy | L-phenylalanine | 4 to 5 | A, G | [115] |
| Phosphoribosylpyrophosphate synthetase deficiency | Pharmacological therapy | S-adenosylmethionine | 4 | D, G | [133] |
| Phosphoserine aminotransferase deficiency | Nutritional therapy | L-Serine, glycine | 4 | D, E, F | [59] |
| Phosphoserine phosphatase deficiency | Nutritional therapy | L-Serine, glycine | 4 | D, E, F | [59] |
| PIGA-CDG | Nutritional therapy | Ketogenic diet | 4 | A, F | [134] |
| PIGM-CDG | Pharmacological therapy | Sodium phenylbutyrate | 4 | A, F | [134] |
| PIGO-CDG | Vitamin & trace element | Pyridoxine | 4 to 5 | F | [134] |
| PMM2-CDG | Pharmacological therapy | Acetazolamide | 1b | E, G | [135] |
| Propionic acidemia due to propionyl-CoA carboxylase subunit alpha (PCCA)/beta (PCCB) deficiency | Nutritional therapy | Protein defined diet, carnitine, avoid fasting, sick day management | 2c | C, D, G | [120] |
| Pharmacological therapy | N-carbamyl-L-glutamate (carglumic acid), sodium benzoate, antibiotics | 4 | C, D, G | [120] | |
| Other | Hemodialysis, peritoneal dialysis | 4 | D | [120] | |
| Solid organ transplant | Liver and/or kidney transplantation | 4 | C, D, G | [120] | |
| Proton-coupled folate transporter deficiency (synonym: hereditary folate malabsorption) | Vitamin & trace element | (Levo-)folinic acid | 4 | A, E, F, G | [136] |
| Pyridoxamine 5′-phosphate oxidase deficiency | Vitamin & trace element | Pyridoxal phosphate | 4 | D, E, F | [137] |
| Pyruvate dehydrogenase E1 alpha (PDHA1)/beta (PDHB)/E2 (DLAT)/E3 (DLD)/E3BP (PDHX) deficiency | Nutritional therapy | Ketogenic diet | 4 for PDHA1 and PDHX, 5 for other genes | A, D, E, F | [138, 139] |
| Vitamin & trace element | Thiamine | 4 for some mutations | D, E, F | [138, 139] | |
| Pyruvate dehydrogenase phosphatase deficiency | Nutritional therapy | Ketogenic diet, thiamine ± | 4 | A, D, E | [140] |
| S-adenosylhomocysteine hydrolase deficiency | Nutritional therapy | Methionine restriction, creatinine, phosphatidylcholine | 4 | A, E, G | [141] |
| Solid organ transplant | Liver transplantation | 4 to 5 | A, E, G | [141] | |
| Sepiapterin reductase deficiency | Pharmacological therapy | L-dopa + carbidopa, 5-Hydroxytryptophan | 4 | A, B, E, F, G | [62] |
| Vitamin & trace element | Folinic acid ± | 5 | A, E, F | [62] | |
| Seryl-tRNA synthetase 1 deficiency | Nutritional therapy | L-serine | 4 to 5 | A, B, G | [114, 115] |
| SLC35A2-CDG | Nutritional therapy | Galactose | 4 | E, F, G | [142] |
| SLC35C1-CDG | Nutritional therapy | Fucose | 4 | A, G | [134] |
| SLC39A8 deficiency | Nutritional therapy | Galactose, manganese, uridine | 4 | F | [134] |
| Sodium-dependent multivitamin transporter deficiency | Vitamin & trace element | Biotin, alpha-lipoic acid, pantothenic acid | 4 | A, D, G | [143] |
| Sterol 27-hydroxylase deficiency (synonym: cerebrotendinous xanthomatosis) | Pharmacological therapy | Chenodeoxycholic Acid | 3a | B, D, E, G | [144] |
| Succinic semialdehyde dehydrogenase deficiency | Pharmacological therapy | Vigabatrin | 4 | B, F | [145] |
| Thiamine pyrophosphokinase deficiency | Vitamin & trace element | Thiamine | 4 | D | [146] |
| Thiamine transporter 2 deficiency (synonym: biotin-thiamine-responsive basal ganglia disease) | Vitamin & trace element | Thiamine, biotin | 2c for thiamine, 4 for biotin | D | [147] |
| Transcobalamin II deficiency | Vitamin & trace element | Cyanocobalamin, hydroxycobalamin | 4 | D, E, G | [148] |
| Tripeptidyl-peptidase 1 deficiency (synonym: CLN2 disease) | Enzyme replacement therapy | Cerliponase alfa | 2b | D | [149] |
| Tyrosine aminotransferase deficiency (synonyms: tyrosinemia type 2; Richner-Hanhart syndrome) | Nutritional therapy | Protein defined diet, phenylalanine and tyrosine restriction | 4 G, 5 for D | D, G | [150] |
| Tyrosine hydroxylase deficiency | Pharmacological therapy | L-dopa + carbidopa | 4 | A, E | [151] |
| Vesicular monoamine transporter 2 deficiency | Pharmacological therapy | Pramipexol (dopamine agonist) | 4 | A, E | [152] |
| X-linked adrenoleukodystrophy | Gene-based therapy | Gene therapy | 5 | D, E | [153] |
| Stem cell therapy | Hematopoietic stem cell transplantation | 1c | D, E | [154] |
Level of evidence: Level 1a = systematic review of RCT's, 1b = individual RCT, 1c = ‘All or None’ [= (prolongation of) survival with therapy]; Level 2a = systematic review of cohort studies, 2b = individual cohort study, 2c = ‘Outcomes Research’ [focused on end results of therapy for chronic conditions, including functioning and quality of life]; Level 3 = systematic review of case– control studies; Level 4 = individual case–control study or case-series/report; Level 5 = expert opinion without critical appraisal; based on physiology, bench research or first principles. If only one patient was reported, we assigned level ‘4 to 5′ as a way to nuance the treatment effects
Effect of treatment: A = improves psychomotor/cognitive development/IQ, B = improves behavioural/psychiatric disturbance(s), C = prevents acute metabolic decompensation, D = prevents, halts, or slows clinical deterioration, E = improves neurological manifestations (incl. neuro-imaging), F = improves seizure/epilepsy control, G = improves systemic manifestations
The level of evidence for each treatment as defined in Table 1A is shown in Table 3. Most often, case series or case reports with an evidence level of 4 (60%), 4–5 (12%) and 5 (8%) were reported; higher evidence levels accounted for a minority (level 1 for 4%, level 2 for 14%, level 3 for 0.5%) (Table 3).
Effect(s) of treatments on outcome measures
Treatment prevented, halted, or slowed clinical deterioration in 62%, improved neurological manifestations (incl. neuro-imaging) in 47%, systemic manifestations in 44% and psychomotor/cognitive development/IQ in 37%; it prevented acute metabolic decompensation in 30%, improved seizure/epilepsy control in 22% and improved behavioural/psychiatric disturbance(s) in 21%.
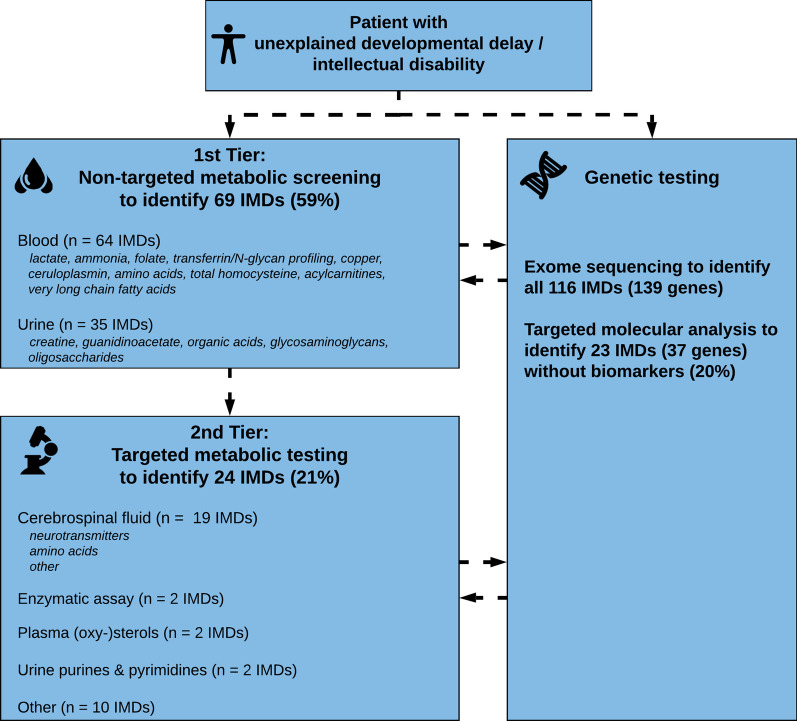
Diagnostic algorithm
The diagnostic algorithm in Fig. 1 is proposed for the evaluation of a patient of any age presenting with DD or ID in whom the cause is not apparent. It is based on the following results: 1st Tier or ‘basic’ metabolic screening (in blood: lactate, plasma ammonia, serum transferrin/N-glycan profiling, serum/red blood cell folate, serum copper and ceruloplasmin, plasma amino acids, plasma total homocysteine, plasma (or dried bloodspot) acylcarnitines, very long chain fatty acids; in urine: organic acids, creatine, guanidinoacetate, glycosaminoglycans and oligosaccharides) is available at most if not all diagnostic metabolic laboratories and can identify 69 (59%) of the 116 treatable IDs. Of course, further biochemical and genetic confirmation is warranted, but for the sake of prompt initiation of treatment, these first-tier results yield sufficient diagnostic information.
Fig. 1.
Diagnostic algorithm for treatable IDs. 1st Tier consists of non-targeted metabolic screening tests that are readily available in most developed countries. 2nd Tier consists of targeted metabolic tests, often more invasive and/or less available. Some IMDs are identified by multiple (screening) tests in the 1st and 2nd Tier. Genetic testing (targeted molecular analysis as well as exome sequencing) can be performed in parallel. (ID = Intellectual disability; IMD = Inherited Metabolic Disorder)
Importantly, for 23 of 116 IMDs (20%) no specific biomarker is currently available and thus molecular testing (targeted or via exome) is required (Fig. 1).
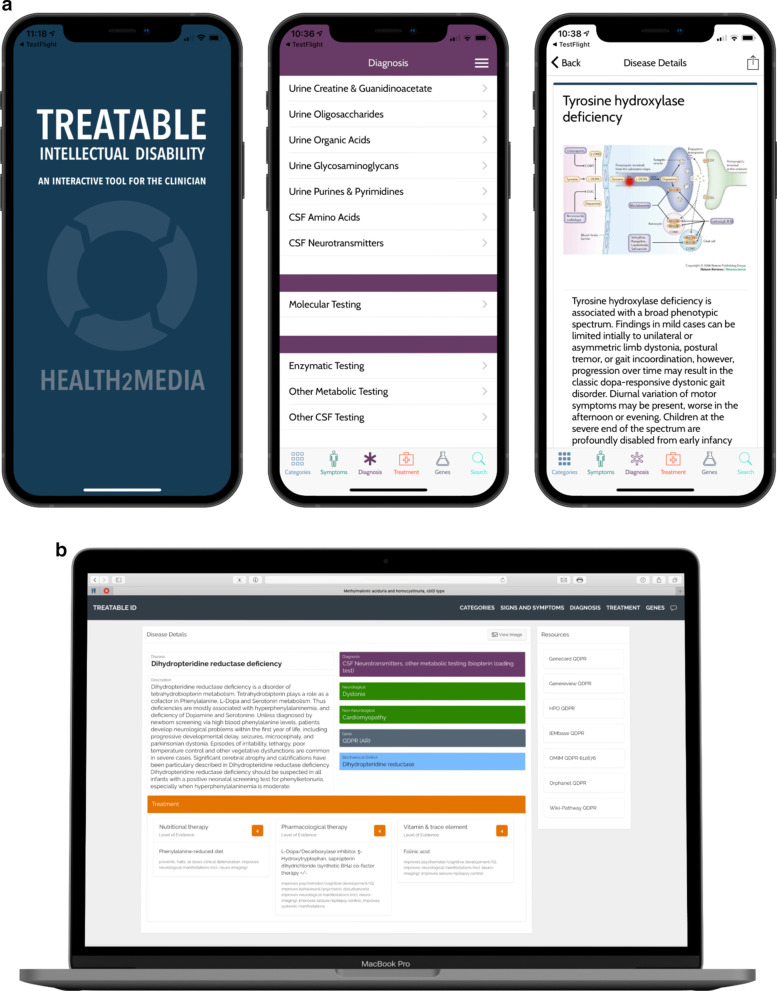
Fig. 2.
The updated Treatable ID App, an interactive digital tool for the clinician to a search for IMDs according to genes, signs and symptoms, diagnostic tests, and treatments, and b find information on specific IMDs along with links to other digital resources. (IMD = Inherited Metabolic Disorder)
Lumbar puncture for cerebrospinal fluid (CSF) neurotransmitter and amino-acid analysis is indicated in patients with neonatal or infantile seizures of unknown aetiology, dystonia or other movement disorders, progressive intellectual neurological deterioration (85 IMDs, 41% amenable to treatment [26]), severe psychiatric or behavioral phenotypes, and/or clinical findings suggestive of dopamine deficiency (hypersalivation, temperature dysregulation, oculogyric crises, or hypokinesia). An abnormal profile has important diagnostic as well as therapeutic implications, such as neurotransmitter supplementation, e.g., in GTCPH deficiency, or even in additional non-classic IMDs, e.g., in a PAK3 deficiency patient with severe automutilation and low CSF homovanillic acid (HVA) [27].
Treatable ID App
First, based on our 2021 literature search, the content has been updated in the Treatable ID App, including updated summaries, symptoms, diagnostic tests, treatments with levels of evidence and effects for each IMD. A disorder page has been designed of each IMD with links to Orphanet, OMIM, Human Phenotype Ontology (HPO), GeneReviews, GeneCards, IMDbase, Vademecum Metabolicum and WikiPathways. Second, based on user feedback, the design has been updated with a quick and solid interface. It is possible to search based on signs and symptoms for IMDs, the appropriate diagnostic tests and gene lists and panel designs, available treatments and evidence. Figure 2 illustrates the Treatable ID App features on mobile devices. The App is available via the App Store, Google Play and online (http://www.treatable-id.org) freely downloadable for all interested users including but not limited to general practitioners, medical and biochemical geneticists, neurologists, developmental and pediatricians, internists, metabolic diseases specialists, as well as laboratory specialists and patients and families.
Discussion
Targeted therapies for treatable IDs: strengthening the Treatabolome
Our systematic review from 2012 was the first to prioritize the treatability in the diagnostic evaluation of patients with DD and ID in whom the cause was not evident after a thorough clinical exam. As increasing numbers of patients are diagnosed through exome and genome sequencing in clinical practice or within research projects, it becomes ever more crucial to enable flagging of potentially treatable cases at a gene or variant level. However, this knowledge was (and still is) largely available only in ‘human-readable’ scientific publications or in expert practice, and our website and app were the first to capture this knowledge in a computer-accessible form that would allow automatic recognition and flagging in analysis and decision-support systems. The implementation of these web resources in national guidelines as well as treatment programs has successfully changed the clinical practice and inspired several reviews on other genetic diseases (e.g., neuromuscular disease [28], epilepsy [17] or movement disorders [29]). The final goal is a ‘treatabolome’ database accessible for all health care providers as well as patients.
Diagnostics advances
The field of IMDs is a moving target with 44 newly-defined IMDs included in our recent update, and still the IMDs are the largest group of monogenic conditions underlying ID amenable to treatment. The wide implementation of NGS techniques has led to the identification of new IMDs and the better understanding of the underlying pathophysiology has led to a substantial change in the definition of IMDs (‘Any condition in which the impairment of a biochemical pathway is intrinsic to the pathophysiology of the disease, regardless of whether there are abnormalities in currently available biochemical laboratory tests’). These changes led to an increasing number of individuals being diagnosed with IMDs for which no metabolic marker is available (e.g., CAD deficiency [30]), in turn leading to prioritization of exome sequencing (panels) in the diagnostic algorithm. However, these techniques are not always available or have significantly longer turnaround times than conventional metabolic screening in body fluids. Conversely, about 50% of all individuals undergoing genetic testing for ID remain without a diagnosis, which still makes metabolic screening an important part of the diagnostic workup. This is further underlined by a recent study on genomic newborn screening, showing that ES identifies only 9 out of 10 IMDs picked up reliably by tandem mass spectrometry. Thus picking up all patients eligible for early intervention urges a combined approach [31] The 1st and 2nd tier metabolic tests will also identify IDs not amenable to targeted therapy. Of course, any type of diagnosis is beneficial as it provides closure, end to a diagnostic odyssey, information to patients and families, as well as access to accurate genetic counseling, supportive care and reimbursement.
The exact order of diagnostic tests still depends on local resources and expertise and needs critical appraisal and personalization of the subsequent treatment itself. The diagnostic algorithm as shown in Fig. 1 is our recommendation, based on the yield of metabolic tests combined in the tiers, as well as availability at most if not all metabolic laboratories. The algorithm can be adapted according to the clinician’s insights and laboratory specialist’s expertise, as well as the patient’s clinical phenotype (red flags) along with local laboratory resources.
Increasingly, metabolomics or next generation metabolomic screening (NGMS) will replace the individual biochemical tests and assays, similar to ES replacing single gene tests or panels [32]. Already today, most genetic laboratories solely work with ES and use virtual panels or virtual single gene analysis when these tests are required. Hence, in most clinical situations, it seems reasonable to initiate metabolic screening and genetic testing in parallel. The metabolic screening results can validate the functional impact of genetic variants identified by ES (eg N-acetyl-mannosamine for NANS-CDG [33]), thus providing a functional read-out. In ES negative patients, metabolic aberrations can help to guide the genetic investigations to scrutinize genes in specific pathways and vice versa, the genetic results can direct the NGMS interpretation and/or require additional specific metabolic testing (e.g., enzyme assays). In life-threatening situations or Progressive Intellectual and Neurologic Deterioration (PIND), quick turn-around is indicated for both metabolic/NGMS screening (within hours) and ‘accelerated’/ ‘Turbo’ genome sequencing whenever available.
Treatment advances
In parallel, rare disease and (tailored) genetic therapies are gaining mainstream attention with the Food and Drug Administration (FDA) approval of the antisense oligonucleotide (Nusinersen) as well as the gene therapy (onasemnogene abeparvovec) for Spinal muscular atrophy (SMA) [34, 35] and the first personalized antisense oligonucleotide (Milasen) for CLN7-related neurodegeneration [36].
Our data show that although there has been much attention given to gene-based and enzyme replacement therapy, the majority of currently available, effective treatment strategies are nutritional, via dietary interventions and supplementation of vitamins and trace elements. These are relatively cheap, widely available, non-invasive and can be surprisingly effective.
Outcomes of disease and effect of treatment vary widely, depending on the IMD and therapy in question as well as the severity of the phenotype, the disease course and phase, the patient’s age and co-morbidity as well as yet unknown factors. For some IMDs, timely and continued treatment ensures patients live (almost) normal lives, with Phenylketonuria (PKU) being the most prominent example. PKU is not only a superb example for a treatable ID managed with a ‘classical’ nutritional intervention to restrict the toxic substrate, but also how further research can broaden the therapeutic opportunities (e.g., tetrahydrobiopterin, Pegvaliase) and how the genotype can help in treatment planning.
We decided to exclude certain disorders where ID is no longer considered one of the main clinical features (e.g., Succinyl-CoA:3-oxoacid-CoA transferase (SCOT) deficiency, Riboflavin transporter deficiency (RTD)), or where treatment was shown to be ineffective in larger studies (e.g., Sanfilippo syndrome A-D). However, with the increasing focus on personalized treatment we realize that some therapies will show positive effects in selected individuals, while not meeting the “evidence-based” definition for group as a whole.
As our literature review shows, new disorders have been added to this list at a high pace, with 44 new disorders added since 2014. Representative examples include CAD trifunctional protein deficiency in which oral supplementation of uridine (monophosphate) has shown to dramatically improve epilepsy and enable psychomotor development [30, 37]; or memantine repurposing for the treatment of Ionotropic glutamate receptor NMDA type subunit 2A (GRIN2A) dysregulation. For other IMDs, even with treatment, patients still have very severe symptoms, with improvement of IQ seldom reported, but often with improvement of communication skills and behavior. Also, improvement of seizure frequency and intensity can be achieved. While data are scarce to prove the assumption that early treatment will lead to better outcomes, this still seems logical and should prompt the earliest possible diagnosis.
Prioritizing treatable IMDs in the ID workup
The systematic review of 2012 and its update in 2014 were the first evidence-based approach to demonstrate the significance of IMDs in the diagnostic work up of ID/DD. Whilst most recommendations for the diagnostic workup of DD/ID prioritize frequency of conditions and yield of diagnostic tests, our approach prioritized treatability over frequency and strategizes metabolic/biochemical evaluation in a two-tiered fashion. The utility of this approach was recently shown in the 7-year TIDE-BC study, where we used the two-tiered TIDE diagnostic algorithm for treatable IMD detection superimposed onto current guidelines for the evaluation of unexplained ID. A total of 498 patients (63% male) patients were enrolled; etiologic diagnoses were established in 260 patients (52%), including treatable IMDs in 5%, a third of whom presented with nonspecific symptoms not primarily suggestive of an IMD. Another 15 individuals were diagnosed with a non-treatable IEM [16]. This study represents the first comprehensive metabolic evaluation of a large cohort of patients with ID that is broadly representative of the population seen in a tertiary centre with a biochemical and genetic focus, and therefore possible bias towards IMD. The 29 treatable IMD cases identified and the high overall etiologic diagnosis rate demonstrate the clinical utility of overlaying the TIDE protocol onto current guidelines [16]. The results emphasize the importance of testing for treatable IEMs in all patients with unexplained ID, as earlier diagnosis provides the opportunity to mitigate or possibly prevent irreversible brain damage. Even IMDs for which the typical phenotype comprises complex neurologic abnormalities, PIND or multi-organ disease rather than isolated or stable ID, the earliest or presenting symptom is often developmental delay only (e.g. mucopolysaccharidoses) and thus applying the proposed algorithm and App broadly will enhance early pick-up and treatment of IMDs.
Treatable ID App
The updated Treatable ID App is designed to serve as an up-to-date, easily accessible and freely available digital tool for all clinicians and laboratory specialists evaluating children presenting with ID. Given the challenge of keeping up with clinical and scientific developments, possibly even more so for rare disorders, this app is meant to facilitate this process and translate the vast knowledgebase into a handy resource for early diagnosis and timely treatment. Searching based on signs and symptoms to generate a differential diagnosis and overviews of tests and treatments is a new feature. Also, a gene list for targeted exome analysis can be generated. The App is kept succinct in order to facilitate quick and easy use. Links are provided to more extensive databases, such as IEMbase [8], that provide more details on diagnostics and symptoms. This way, clinicians can easily access more information as needed. Obviously, the Treatable ID App will need to be updated regularly to reflect advances in the field. The current implementation is designed to facilitate this updating process, every 12 months.
Limitations and improvements
Treatobolome database
The development of the ‘treatabolome’ database poses many challenges, especially with regard to curation, and will require expert input from both the clinical domain and the computational and data stewardship domain.
Multi-omics to improve metabolic and genetic (newborn) screening
Another ongoing challenge is the improvement of metabolic screening towards comprehensive tests (next generation metabolic screening, combining metabolomics, glycomics and lipidomics, etc.) [32]. This is in line with the needs to improve and extend genetic screening methods by adding mitochondrial DNA analysis from exome data, genome sequencing and RNA sequencing to the ‘first tier’ genetic toolbox [38] [39] [40]. The implementation of genetic screening into newborn screening programs together with metabolic screening is one of the ongoing challenges.
Standardizing therapies and creating higher evidence levels
Our literature search revealed several shortcomings (for a general review on this topic, the evidence creation in IMD, see Stockler-Ipsiroglu et al. [2]) that need to be addressed in the future. The evidence of the investigated literature is low. Guidelines, following methodologies established by Scottish Intercollegiate Guideline Network (SIGN) [41] and Grading of Recommendations, Assessment, Development and Evaluations (GRADE) [42] based on rigorous evidence rating and transparent grading of recommendations have become an important tool for the standardization of clinical management of IMDs. These are, however, only available for 13 of the > 1400 known IMDs (e.g., for PKU [43], Glutaric aciduria I [44] or Cobalamin deficiencies [45]). This is reflected by our literature review identifying most often non-analytic case series or case reports with an evidence level of 4 (60%), 4–5 (12%) and 5 (8%).
Because of the nature of rare disorders itself and the current trend to simultaneously develop (or better explore) different treatment modalities for single IMDs, alternative clinical trial designs with the ability to evaluate treatments in small populations within a short time are needed more than ever [46].
With the emergence of drug repurposing for personalized therapies, N-of-1 trials will be increasingly used for proof of principle studies in single patients. Such trial designs will address clinical heterogeneity [47], and incorporate personally meaningful outcomes reflecting patients’ preferences and real world daily experience of the rare disease. In cases where clinical trials cannot be performed, registries with well-defined clinical endpoints can elevate the evidence created by registry-based trials. Adopting common data elements with standardized ontologies [48] as well as the agreement on core outcome sets, [49] is now considered a prerequisite for comparability of data collected across the medical systems caring for rare diseases patients.
Access of patients to new technologies and treatments
Our Treatable ID App and algorithm aligns with the vision of the International Rare Diseases Research Consortium to enable all people living with a rare disease to receive an accurate diagnosis and personalized care plan. However access to therapy is still a considerable hurdle in many parts of the world. European Reference Networks and designated centres of expertise address this medical gap. To ‘leave no one behind’, we encourage timely refer all diagnosed patients (at least once) to a such centre to enable access to therapeutic interventions as well as participation in clinical trials and other research studies. Expertise in compounding drugs and magistral preparations is essential for equitable access, as well as a voice in health policy on reimbursement of and access to (orphan) drug and nutritional therapy reimbursement [50] [51] [52].
Conclusions
Treatable IMDs are a moving target. The broad implementation of next-generation genomic and metabolomic testing in daily clinical practice has accelerated the diagnostics for many individuals with ID. In parallel, the increasing knowledge about the genetic basis of disease, insights into pathophysiology, and advances in therapeutic and targeting strategies catalyze the Treatabolome as a whole; this is true as well for IMDs causing ID. At the same time, methods for evidence generation with small patient numbers as well as more extensive and longer-term follow-up studies will reveal that some therapeutic interventions initially deemed effective do not alter primary or secondary outcomes. These exciting developments require continuous updates of the Treatable ID App, the Treatabolome database, as well as other digital resources. In parallel, diagnostic protocols—whether metabolic or genomic—should also be adjusted to prioritize treatable conditions in the diagnostic workup of suspected IMDs and ensure the earliest possible intervention. We encourage clinicians to use our App to facilitate diagnosis and intervention for treatable IDs, and welcome all feedback including treatable IDs we may have missed.
Supplementary Information
Additional File 1. Inherited metabolic disorders (IMDs) included in our 2012 (PMID 22212131) and 2014 (PMID 24518794) reviews and currently excluded.
Acknowledgments
The authors are grateful to the patients and families for daily teaching and inspiration, to the clinical and scientific colleagues for all their efforts to advance diagnosis and treatment of IMDs and finally to Mr Jeff Joa (Vancouver) for his technical contribution to the App.
Abbreviations
- ES
Exome sequencing
- DD
Global developmental delay
- IMD
Inherited metabolic disorder
- ICIMD
International classification of inherited metabolic disorders
- ID
Intellectual disability
- CSF
Cerebrospinal fluid
- HVA
Homovanillic acid
- NGS
Next generation sequencing
- NGMS
Next generation metabolomic screening
- PIND
Progressive intellectual and neurologic deterioration
- SMA
Spinal muscular atrophy
- PKU
Phenylketonuria
- COS
Core outcome measure set
Authors’ contributions
EHvK performed the literature review, critical assessment and data extraction, participated in consensus meetings, drafted and edited the manuscript. SW performed the literature review, critical assessment and data extraction, participated in consensus meetings, drafted and edited the manuscript. MK contributed to the literature review and critical assessment, performed data extraction, participated in consensus meetings and edited the manuscript. LT contributed to the literature review and critical assessment, and revised the manuscript. RH contributed to review data translation and Treatable ID App design with feature updates, and contributed to the App sections of the manuscript. SS performed the initial systematic review on treatable IDs and the initial version of the App, critical assessment of data, and edited the current version of the manuscript. CF contributed to the literature review, performed data extraction and critical assessment, participated in consensus meetings and revised the manuscript. CvK designed study, supervised the literature review, critical assessment and data extraction, participated in consensus meetings, translated and prepared data for the App, drafted and edited the manuscript. All authors approved the final version of the manuscript.
Funding
CvK is supported by a salary award from ‘Stichting Metakids’ in The Netherlands. SW is supported by ERAPERMED2019-310—Personalized Mitochondrial Medicine (PerMiM) and FWF Jubiläumsfondprojekt Nr. 18023.
Availability of data and materials
All data generated and analyzed during this study are included in this published article, the supplementary information files and the Treatable ID app (www. Treatable-id.org). The literature search and data are available upon request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Eva M. M. Hoytema van Konijnenburg and Saskia B. Wortmann have contributed equally to this work
References
- 1.van Karnebeek CDM, Wortmann SB, Tarailo-Graovac M, Langeveld M, Ferreira CR, van de Kamp JM, et al. The role of the clinician in the multi-omics era: are you ready? J Inherit Metab Dis. 2018;41:571–582. doi: 10.1007/s10545-017-0128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stockler‐Ipsiroglu S, Potter BK, Yuskiv N, Tingley K, Patterson M, Karnebeek C. Developments in evidence creation for treatments of inborn errors of metabolism. J Inherit Metab Dis. 2020;jimd.12315. [DOI] [PMC free article] [PubMed]
- 3.van Karnebeek CDM, Stockler S. Treatable inborn errors of metabolism causing intellectual disability: A systematic literature review. 2012;105:368–381. doi: 10.1016/j.ymgme.2011.11.191. [DOI] [PubMed] [Google Scholar]
- 4.van Karnebeek CDM, Shevell M, Zschocke J, Moeschler JB, Stockler S. The metabolic evaluation of the child with an intellectual developmental disorder: diagnostic algorithm for identification of treatable causes and new digital resource. Mol Genet Metab. 2014;111:428–438. doi: 10.1016/j.ymgme.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 5.International joint recommendations to address specific needs of undiagnosed rare disease patients. SWAN UK (the support group run by Genetic Alliance UK), the Wilhelm Foundation, EURORDIS (Rare Diseases Europe), Rare Voices Australia (RVA), the Canadian Organization for Rare Disorders (CORD), the Advocacy Service for Rare and Intractable Diseases’ stakeholders in Japan (ASrid) and the National Organization for Rare Disorders (NORD). http://download2.eurordis.org.s3.amazonaws.com/documents/pdf/Undiagnosed-International-Joint-Recommendations.pdf. Accessed 23 Dec 2020.
- 6.Morava E, Rahman S, Peters V, Baumgartner MR, Patterson M, Zschocke J. Quo vadis: the re-definition of “inborn metabolic diseases”. J Inherit Metab Dis. 2015;38:1003–1006. doi: 10.1007/s10545-015-9893-x. [DOI] [PubMed] [Google Scholar]
- 7.International Classification of Inherited Metabolic Disorders (ICIMD). http://www.icimd.org. Accessed 10 Dec 2020. [DOI] [PMC free article] [PubMed]
- 8.Inborn Errors of Metabolism Knowledgebase (IEMbase). www.IEMbase.org. Accessed 10 Dec 2020.
- 9.Moeschler JB, Shevell M. Comprehensive evaluation of the child with intellectual disability or global developmental delays. Pediatrics. 2014;134:e903–e918. doi: 10.1542/peds.2014-1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bélanger SA, Caron J. Evaluation of the child with global developmental delay and intellectual disability. Paediatr Child Health. 2018;23:403–410. doi: 10.1093/pch/pxy093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van den Elzen A. NVK richtlijn Ontwikkelingsachterstand/verstandelijke beperking. 2018. https://www.nvk.nl/themas/kwaliteit/richtlijnen/richtlijn?componentid=7667712&tagtitles=Erfelijke%2Ben%2Baangeboren%2Baandoeningen,Metabole%2BZiekten,Keel-Neus-Oog%2B(KNO),Neurologie. Accessed 10 Dec 2020.
- 12.van Karnebeek CDM, Houben RFA, Lafek M, Giannasi W, Stockler S. The treatable intellectual disability APP www.treatable-id.org: A digital tool to enhance diagnosis & care for rare diseases. Orphanet J Rare Dis. 2012;7:47. [DOI] [PMC free article] [PubMed]
- 13.Van Karnebeek CDM. Evaluation of the child with developmental impairments. Contin Lifelong Learn. Neurol. 2018. [DOI] [PubMed]
- 14.van Karnebeek CD, Stockler-Ipsiroglu S. Early identification of treatable inborn errors of metabolism in children with intellectual disability: The Treatable Intellectual Disability Endeavor protocol in British Columbia. Paediatr Child Health. 2014;19:469–471. doi: 10.1093/pch/19.9.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sayson B, Popurs MAM, Lafek M, Berkow R, Stockler-Ipsiroglu S, van Karnebeek CDM. Retrospective analysis supports algorithm as efficient diagnostic approach to treatable intellectual developmental disabilities. Mol Genet Metab. 2015;115:1–9. doi: 10.1016/j.ymgme.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 16.van Karnebeek, Clara D.M. ; Dragojlovic, Nick; Sinclair, Graham; Salvarinova, Ramona; Horvath, Gabriella; Selby, Katherine; Ghani A et al. The TIDE study: treatable inherited metabolic disorders identified in a cohort of 498 children with unexplained intellectual developmental disorder. Submitted.
- 17.van Karnebeek CDM, Sayson B, Lee JJY, Tseng LA, Blau N, Horvath GA, et al. Metabolic evaluation of epilepsy: a diagnostic algorithm with focus on treatable conditions. Front Neurol. 2018;9:1016. doi: 10.3389/fneur.2018.01016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hillert A, Anikster Y, Belanger-Quintana A, Burlina A, Burton BK, Carducci C, et al. The genetic landscape and epidemiology of phenylketonuria. Am J Hum Genet. 2020;107:234–250. doi: 10.1016/j.ajhg.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shen JJ, Wortmann SB, de Boer L, Kluijtmans LAJ, Huigen MCDG, Koch J, et al. The role of clinical response to treatment in determining pathogenicity of genomic variants. Genet Med. 2020. [DOI] [PubMed]
- 20.Atalaia A, Thompson R, Corvo A, Carmody L, Piscia D, Matalonga L, et al. A guide to writing systematic reviews of rare disease treatments to generate FAIR-compliant datasets: Building a Treatabolome. Orphanet J Rare Dis. 2020. [DOI] [PMC free article] [PubMed]
- 21.Orphanet. http://www.orpha.net/consor/cgi-bin/index.php?lng=EN. Accessed 10 Dec 2020.
- 22.Online Mendelian Inheritance in Man (OMIM). http://www.omim.org. Accessed 10 Dec 2020.
- 23.Wilkinson MD, Dumontier M, Aalbersberg IjJ, Appleton G, Axton M, Baak A, et al. The FAIR Guiding Principles for scientific data management and stewardship. Sci Data. 2016;3:160018. doi: 10.1038/sdata.2016.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wanders RJA, Vaz FM, Ferdinandusse S, van Kuilenburg ABP, Kemp S, van Karnebeek CD, et al. Translational Metabolism: A multidisciplinary approach towards precision diagnosis of inborn errors of metabolism in the omics era. J. Inherit. Metab. Dis. 2019. [DOI] [PubMed]
- 25.Metakids. http://www.metakids.nl. Accessed 10 Dec 2020.
- 26.Warmerdam HAG, Termeulen-Ferreira EA, Tseng LA, Lee JY, van Eeghen AM, Ferreira CR, et al. A scoping review of inborn errors of metabolism causing progressive intellectual and neurologic deterioration (PIND). Front Neurol. 2020. [DOI] [PMC free article] [PubMed]
- 27.Horvath GA, Tarailo-Graovac M, Bartel T, Race S, Van Allen MI, Blydt-Hansen I, et al. Improvement of self-injury with dopamine and serotonin replacement therapy in a patient with a hemizygous PAK3 mutation: a new therapeutic strategy for neuropsychiatric features of an intellectual disability syndrome. J Child Neurol. 2018;33:106–113. doi: 10.1177/0883073817740443. [DOI] [PubMed] [Google Scholar]
- 28.Thompson R, Bonne G, Missier P, Lochmüller H. Targeted therapies for congenital myasthenic syndromes: Systematic review and steps towards a treatabolome. Emerg Top Life Sci. 2019;3:19–37. doi: 10.1042/ETLS20180100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ebrahimi-Fakhari D, Van Karnebeek C, Münchau A. Movement disorders in treatable inborn errors of metabolism. Mov Disord. 2019;34:598–613. doi: 10.1002/mds.27568. [DOI] [PubMed] [Google Scholar]
- 30.Koch J, Mayr JA, Alhaddad B, Rauscher C, Bierau J, Kovacs-Nagy R, et al. CAD mutations and uridine-responsive epileptic encephalopathy. Brain [Internet] 2017;140:279–286. doi: 10.1093/brain/aww300. [DOI] [PubMed] [Google Scholar]
- 31.Adhikari AN, Gallagher RC, Wang Y, Currier RJ, Amatuni G, Bassaganyas L, et al. The role of exome sequencing in newborn screening for inborn errors of metabolism. Nat Med. 2020;26:1392–1397. doi: 10.1038/s41591-020-0966-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Coene KLM, Kluijtmans LAJ, van der Heeft E, Engelke UFH, de Boer S, Hoegen B, et al. Next-generation metabolic screening: targeted and untargeted metabolomics for the diagnosis of inborn errors of metabolism in individual patients. J Inherit Metab Dis. 2018;41:337–353. doi: 10.1007/s10545-017-0131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van Karnebeek CDM, Bonafé L, Wen XY, Tarailo-Graovac M, Balzano S, Royer-Bertrand B, et al. NANS-mediated synthesis of sialic acid is required for brain and skeletal development. Nat Genet. 2016;48:777–784. doi: 10.1038/ng.3578. [DOI] [PubMed] [Google Scholar]
- 34.Hoy SM. Nusinersen: first global approval. Drugs. 2017;77:473–479. doi: 10.1007/s40265-017-0711-7. [DOI] [PubMed] [Google Scholar]
- 35.Hoy SM. Onasemnogene Abeparvovec: first global approval. Drugs. 2019;79:1255–1262. doi: 10.1007/s40265-019-01162-5. [DOI] [PubMed] [Google Scholar]
- 36.Kim J, Hu C, Moufawad E, Achkar C, Black LE, Douville J, Larson A, et al. Patient-customized oligonucleotide therapy for a rare genetic disease. N Engl J Med. 2019;381:1644–1652. doi: 10.1056/NEJMoa1813279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rymen D, Lindhout M, Spanou M, Ashrafzadeh F, Benkel I, Betzler C, et al. Expanding the clinical and genetic spectrum of CAD deficiency: an epileptic encephalopathy treatable with uridine supplementation. Genet Med. 2020;22:1589–1597. doi: 10.1038/s41436-020-0933-z. [DOI] [PubMed] [Google Scholar]
- 38.Kremer LS, Wortmann SB, Prokisch H. “Transcriptomics”: molecular diagnosis of inborn errors of metabolism via RNA-sequencing. J Inherit Metab Dis. 2018;41:525–532. doi: 10.1007/s10545-017-0133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wagner M, Berutti R, Lorenz-Depiereux B, Graf E, Eckstein G, Mayr JA, et al. Mitochondrial DNA mutation analysis from exome sequencing—A more holistic approach in diagnostics of suspected mitochondrial disease. J Inherit Metab Dis. 2019;42:909–917. doi: 10.1002/jimd.12109. [DOI] [PubMed] [Google Scholar]
- 40.Riley LG, Cowley MJ, Gayevskiy V, Minoche AE, Puttick C, Thorburn DR, et al. The diagnostic utility of genome sequencing in a pediatric cohort with suspected mitochondrial disease. Genet Med. 2020;22:1254–1261. doi: 10.1038/s41436-020-0793-6. [DOI] [PubMed] [Google Scholar]
- 41.Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. Br Med J. 2001;323:334–336. doi: 10.1136/bmj.323.7308.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van Wegberg AMJ, MacDonald A, Ahring K, Bélanger-Quintana A, Blau N, Bosch AM, et al. The complete European guidelines on phenylketonuria: diagnosis and treatment. Orphanet J Rare Dis. 2017;12:162. doi: 10.1186/s13023-017-0685-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boy N, Mühlhausen C, Maier EM, Heringer J, Assmann B, Burgard P, et al. Proposed recommendations for diagnosing and managing individuals with glutaric aciduria type I: second revision. J Inherit Metab Dis. 2017;40:75–101. doi: 10.1007/s10545-016-9999-9. [DOI] [PubMed] [Google Scholar]
- 45.Huemer M, Diodato D, Schwahn B, Schiff M, Bandeira A, Benoist JF, et al. Guidelines for diagnosis and management of the cobalamin-related remethylation disorders cblC, cblD, cblE, cblF, cblG, cblJ and MTHFR deficiency. J Inherit Metab Dis. 2017;40:21–48. doi: 10.1007/s10545-016-9991-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tingley K, Coyle D, Graham ID, Sikora L, Chakraborty P, Wilson K, et al. Using a meta-narrative literature review and focus groups with key stakeholders to identify perceived challenges and solutions for generating robust evidence on the effectiveness of treatments for rare diseases. Orphanet J Rare Dis. 2018;13:104. doi: 10.1186/s13023-018-0851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shamseer L, Sampson M, Bukutu C, Schmid CH, Nikles J, Tate R, et al. CONSORT extension for reporting N-of-1 trials (CENT) 2015: explanation and elaboration. J Clin Epidemiol. 2016;76:18–46. doi: 10.1016/j.jclinepi.2015.05.018. [DOI] [PubMed] [Google Scholar]
- 48.Köhler S, Vasilevsky NA, Engelstad M, Foster E, McMurry J, Aymé S, et al. The human phenotype ontology in 2017. Nucleic Acids Res. 2017;45:D865–D876. doi: 10.1093/nar/gkw1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rubinstein YR, McInnes P. NIH/NCATS/GRDR® Common Data Elements: a leading force for standardized data collection. Contemp Clin Trials. 2015;42:78–80. doi: 10.1016/j.cct.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stawowczyk E, Malinowski KP, Kawalec P, Bobiński R, Siwiec J, Panteli D, et al. Reimbursement status and recommendations related to orphan drugs in European Countries. Front Pharmacol. 2019;10. [DOI] [PMC free article] [PubMed]
- 51.Dooms M, Carvalho M. Compounded medication for patients with rare diseases. Orphanet J Rare Dis. 2018;13:1. doi: 10.1186/s13023-017-0741-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dooms M, Killick J. Off-label use of medicines: the need for good practice guidelines. Int J Risk Saf Med. 2017;29:17–23. doi: 10.3233/JRS-170737. [DOI] [PubMed] [Google Scholar]
- 53.Shevell MI. Present conceptualization of early childhood neurodevelopmental disabilities. J Child Neurol. 2010;25:120–126. doi: 10.1177/0883073809336122. [DOI] [PubMed] [Google Scholar]
- 54.Luckasson R, Reeve A. Naming, defining, and classifying in mental retardation. Ment Retard. 2001;39:47–52. doi: 10.1352/0047-6765(2001)039<0047:NDACIM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 55.Shevell M. Global developmental delay and mental retardation or intellectual disability: conceptualization, evaluation, and etiology. Pediatr Clin North Am. 2008;55:1071–1084. doi: 10.1016/j.pcl.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 56.Pubmed. https://pubmed.ncbi.nlm.nih.gov. Accessed 10 Dec 2020.
- 57.Grünert SC, Schlatter SM, Schmitt RN, Gemperle-Britschgi C, Mrázová L, Balcı MC, et al. 3-Hydroxy-3-methylglutaryl-coenzyme A lyase deficiency: clinical presentation and outcome in a series of 37 patients. Mol Genet Metab. 2017;121:206–215. doi: 10.1016/j.ymgme.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 58.Abdenur JE, Sowa M, Simon M, Steenari M, Skaar J, Eftekharian S, et al. Medical nutrition therapy in patients with HIBCH and ECHS1 defects: clinical and biochemical response to low valine diet. Mol Genet Metab Reports. 2020;24:100617. doi: 10.1016/j.ymgmr.2020.100617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van der Crabben SN, Verhoeven-Duif NM, Brilstra EH, Van Maldergem L, Coskun T, Rubio-Gozalbo E, et al. An update on serine deficiency disorders. J Inherit Metab Dis. 2013;36:613–619. doi: 10.1007/s10545-013-9592-4. [DOI] [PubMed] [Google Scholar]
- 60.Rodan LH, Qi W, Ducker GS, Demirbas D, Laine R, Yang E, et al. 5,10-methenyltetrahydrofolate synthetase deficiency causes a neurometabolic disorder associated with microcephaly, epilepsy, and cerebral hypomyelination. Mol Genet Metab. 2018;125:118–126. doi: 10.1016/j.ymgme.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Huemer M, Baumgartner MR. The clinical presentation of cobalamin-related disorders: from acquired deficiencies to inborn errors of absorption and intracellular pathways. J Inherit Metab Dis. 2019;42:686–705. doi: 10.1002/jimd.12012. [DOI] [PubMed] [Google Scholar]
- 62.Opladen T, López-Laso E, Cortès-Saladelafont E, Pearson TS, Sivri HS, Yildiz Y, et al. Consensus guideline for the diagnosis and treatment of tetrahydrobiopterin (BH4) deficiencies. Orphanet J Rare Dis. 2020;15:126. doi: 10.1186/s13023-020-01379-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wassif CA, Kratz L, Sparks SE, Wheeler C, Bianconi S, Gropman A, et al. A placebo-controlled trial of simvastatin therapy in Smith-Lemli-Opitz syndrome. Genet Med. 2017;19:297–305. doi: 10.1038/gim.2016.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bianconi SE, Cross JL, Wassif CA, Porter FD. Pathogenesis, epidemiology, diagnosis and clinical aspects of Smith–Lemli–Opitz syndrome. Expert Opin Orphan Drugs. 2015;3:267–280. doi: 10.1517/21678707.2015.1014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Repp BM, Mastantuono E, Alston CL, Schiff M, Haack TB, Rötig A, et al. Clinical, biochemical and genetic spectrum of 70 patients with ACAD9 deficiency: is riboflavin supplementation effective? Orphanet J Rare Dis. 2018;13:120. doi: 10.1186/s13023-018-0784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Coughlin CR, van Karnebeek CDM, Al-Hertani W, Shuen AY, Jaggumantri S, Jack RM, et al. Triple therapy with pyridoxine, arginine supplementation and dietary lysine restriction in pyridoxine-dependent epilepsy: Neurodevelopmental outcome. Mol Genet Metab. 2015;116:35–43. doi: 10.1016/j.ymgme.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 67.Jiang M, Liu S, Jiang H, Lin Y, Shao Y, Hu H, et al. Brain abnormalities in fucosidosis: transplantation or supportive therapy? Metab Brain Dis. 2017;32:317–320. doi: 10.1007/s11011-017-9968-5. [DOI] [PubMed] [Google Scholar]
- 68.Eisengart JB, Pierpont EI, Kaizer AM, Rudser KD, King KE, Pasquali M, et al. Intrathecal enzyme replacement for Hurler syndrome: biomarker association with neurocognitive outcomes. Genet Med. 2019;21:2552–2560. doi: 10.1038/s41436-019-0522-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aldenhoven M, Wynn RF, Orchard PJ, O’Meara A, Veys P, Fischer A, et al. Long-term outcome of Hurler syndrome patients after hematopoietic cell transplantation: an international multicenter study. Blood. 2015;125:2164–2172. doi: 10.1182/blood-2014-11-608075. [DOI] [PubMed] [Google Scholar]
- 70.Harmatz P, Cattaneo F, Ardigò D, Geraci S, Hennermann JB, Guffon N, et al. Enzyme replacement therapy with velmanase alfa (human recombinant alpha-mannosidase): Novel global treatment response model and outcomes in patients with alpha-mannosidosis. Mol Genet Metab. 2018;124:152–160. doi: 10.1016/j.ymgme.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 71.Ceccarini M, Codini M, Conte C, Patria F, Cataldi S, Bertelli M, et al. Alpha-mannosidosis: therapeutic strategies. Int J Mol Sci. 2018;19:1500. doi: 10.3390/ijms19051500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Häberle J, Burlina A, Chakrapani A, Dixon M, Karall D, Lindner M, et al. Suggested guidelines for the diagnosis and management of urea cycle disorders: first revision. J Inherit Metab Dis. 2019;42:1192–1230. doi: 10.1002/jimd.12100. [DOI] [PubMed] [Google Scholar]
- 73.Stockler-Ipsiroglu S, Apatean D, Battini R, DeBrosse S, Dessoffy K, Edvardson S, et al. Arginine:glycine amidinotransferase (AGAT) deficiency: clinical features and long term outcomes in 16 patients diagnosed worldwide. Mol Genet Metab. 2015;116:252–259. doi: 10.1016/j.ymgme.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 74.Wassenberg T, Molero-Luis M, Jeltsch K, Hoffmann GF, Assmann B, Blau N, et al. Consensus guideline for the diagnosis and treatment of aromatic l-amino acid decarboxylase (AADC) deficiency. Orphanet J Rare Dis. 2017;12:12. doi: 10.1186/s13023-016-0522-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kojima K, Nakajima T, Taga N, Miyauchi A, Kato M, Matsumoto A, et al. Gene therapy improves motor and mental function of aromatic l-amino acid decarboxylase deficiency. Brain. 2019;142:322–333. doi: 10.1093/brain/awy331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Groeschel S, Kühl J-S, Bley AE, Kehrer C, Weschke B, Döring M, et al. Long-term outcome of allogeneic hematopoietic stem cell transplantation in patients with juvenile metachromatic leukodystrophy compared with nontransplanted control patients. JAMA Neurol. 2016;73:1133. doi: 10.1001/jamaneurol.2016.2067. [DOI] [PubMed] [Google Scholar]
- 77.Sessa M, Lorioli L, Fumagalli F, Acquati S, Redaelli D, Baldoli C, et al. Lentiviral haemopoietic stem-cell gene therapy in early-onset metachromatic leukodystrophy: an ad-hoc analysis of a non-randomised, open-label, phase 1/2 trial. Lancet. 2016;388:476–487. doi: 10.1016/S0140-6736(16)30374-9. [DOI] [PubMed] [Google Scholar]
- 78.Malm G, Mansson J-E, Winiarski J, Mosskin M, Ringden O. Five-year follow-up of two siblings with aspartylglucosaminuria undergoing allogeneic stem-cell transplantation from unrelated donors. Transplantation. 2004;78:415–419. doi: 10.1097/00007890-200408150-00015. [DOI] [PubMed] [Google Scholar]
- 79.Rafiq M, Flanagan SE, Patch A-M, Shields BM, Ellard S, Hattersley AT. Effective treatment with oral sulfonylureas in patients with diabetes due to sulfonylurea receptor 1 (SUR1) mutations. Diabetes Care. 2008;31:204–209. doi: 10.2337/dc07-1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vaxillaire M, Dechaume A, Busiah K, Cave H, Pereira S, Scharfmann R, et al. New ABCC8 mutations in relapsing neonatal diabetes and clinical features. Diabetes. 2007;56:1737–1741. doi: 10.2337/db06-1540. [DOI] [PubMed] [Google Scholar]
- 81.Parini R, Deodato F. Intravenous enzyme replacement therapy in mucopolysaccharidoses: clinical effectiveness and limitations. Int J Mol Sci. 2020;21:2975. doi: 10.3390/ijms21082975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jay AM, Conway RL, Feldman GL, Nahhas F, Spencer L, Wolf B. Outcomes of individuals with profound and partial biotinidase deficiency ascertained by newborn screening in Michigan over 25 years. Genet Med. 2015;17:205–209. doi: 10.1038/gim.2014.104. [DOI] [PubMed] [Google Scholar]
- 83.Frazier DM, Allgeier C, Homer C, Marriage BJ, Ogata B, Rohr F, et al. Nutrition management guideline for maple syrup urine disease: An evidence- and consensus-based approach. Mol Genet Metab. 2014;112:210–217. doi: 10.1016/j.ymgme.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 84.Molema F, Martinelli D, Hörster F, Kölker S, Tangeraas T, Koning B, et al. Liver and/or kidney transplantation in amino and organic acid‐related inborn errors of metabolism: An overview on European data. J Inherit Metab Dis. 2020. [DOI] [PMC free article] [PubMed]
- 85.García-Cazorla A, Oyarzabal A, Fort J, Robles C, Castejón E, Ruiz-Sala P, et al. Two novel mutations in the BCKDK (Branched-Chain Keto-Acid Dehydrogenase Kinase) gene are responsible for a neurobehavioral deficit in two pediatric unrelated patients. Hum Mutat. 2014;35:470–477. doi: 10.1002/humu.22513. [DOI] [PubMed] [Google Scholar]
- 86.van Karnebeek CD, Sly WS, Ross CJ, Salvarinova R, Yaplito-Lee J, Santra S, et al. Mitochondrial carbonic anhydrase VA deficiency resulting from CA5A alterations presents with hyperammonemia in early childhood. Am J Hum Genet. 2014;94:453–461. doi: 10.1016/j.ajhg.2014.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Okano Y, Ohura T, Sakamoto O, Inui A. Current treatment for citrin deficiency during NICCD and adaptation/compensation stages: Strategy to prevent CTLN2. Mol Genet Metab. 2019;127:175–183. doi: 10.1016/j.ymgme.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 88.Malicdan MCV, Vilboux T, Ben-Zeev B, Guo J, Eliyahu A, Pode-Shakked B, et al. A novel inborn error of the coenzyme Q10 biosynthesis pathway: cerebellar ataxia and static encephalomyopathy due to COQ5 C-methyltransferase deficiency. Hum Mutat. 2018;39:69–79. doi: 10.1002/humu.23345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Traschütz A, Schirinzi T, Laugwitz L, Murray NH, Bingman CA, Reich S, et al. Clinico-genetic, imaging and molecular delineation of COQ8A-Ataxia: a multicenter study of 59 patients. Ann Neurol. 2020;88:251–263. doi: 10.1002/ana.25751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vairo FP, Chwal BC, Perini S, Ferreira MAP, de Freitas Lopes AC, Saute JAM. A systematic review and evidence-based guideline for diagnosis and treatment of Menkes disease. Mol Genet Metab. 2019;126:6–13. doi: 10.1016/j.ymgme.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 91.Brewer GJ, Askari F, Lorincz MT, Carlson M, Schilsky M, Kluin KJ, et al. Treatment of Wilson disease with ammonium tetrathiomolybdate. Arch Neurol. 2006;63:521. doi: 10.1001/archneur.63.4.521. [DOI] [PubMed] [Google Scholar]
- 92.Schilsky ML. Wilson disease. Clin Liver Dis. 2017;21:755–767. doi: 10.1016/j.cld.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 93.Dunbar M, Jaggumantri S, Sargent M, Stockler-Ipsiroglu S, van Karnebeek CDM. Treatment of X-linked creatine transporter (SLC6A8) deficiency: systematic review of the literature and three new cases. Mol Genet Metab. 2014;112:259–274. doi: 10.1016/j.ymgme.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 94.Schwahn BC, Van Spronsen FJ, Belaidi AA, Bowhay S, Christodoulou J, Derks TG, et al. Efficacy and safety of cyclic pyranopterin monophosphate substitution in severe molybdenum cofactor deficiency type A: a prospective cohort study. Lancet. 2015;386:1955–1963. doi: 10.1016/S0140-6736(15)00124-5. [DOI] [PubMed] [Google Scholar]
- 95.Morris AAM, Kožich V, Santra S, Andria G, Ben-Omran TIM, Chakrapani AB, et al. Guidelines for the diagnosis and management of cystathionine beta-synthase deficiency. J Inherit Metab Dis. 2017;40:49–74. doi: 10.1007/s10545-016-9979-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Banka S, Blom HJ, Walter J, Aziz M, Urquhart J, Clouthier CM, et al. Identification and characterization of an inborn error of metabolism caused by dihydrofolate reductase deficiency. Am J Hum Genet. 2011;88:216–225. doi: 10.1016/j.ajhg.2011.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Anikster Y, Haack TB, Vilboux T, Pode-Shakked B, Thöny B, Shen N, et al. Biallelic mutations in DNAJC12 cause hyperphenylalaninemia, dystonia, and intellectual disability. Am J Hum Genet. 2017;100:257–266. doi: 10.1016/j.ajhg.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.van Rijt WJ, Jager EA, Allersma DP, Aktuğlu Zeybek AÇ, Bhattacharya K, Debray F-G, et al. Efficacy and safety of D, L-3-hydroxybutyrate (D, L-3-HB) treatment in multiple acyl-CoA dehydrogenase deficiency. Genet Med. 2020;22:908–916. doi: 10.1038/s41436-019-0739-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ziats MN, Comeaux MS, Yang Y, Scaglia F, Elsea SH, Sun Q, et al. Improvement of regressive autism symptoms in a child with TMLHE deficiency following carnitine supplementation. Am J Med Genet Part A. 2015;167:2162–2167. doi: 10.1002/ajmg.a.37144. [DOI] [PubMed] [Google Scholar]
- 100.Al-Baradie RS, Chaudhary MW. Diagnosis and management of cerebral folate deficiency A form of folinic acid-responsive seizures. Neurosciences. 2014;19:312–316. [PMC free article] [PubMed] [Google Scholar]
- 101.Alter AS, Engelstad K, Hinton VJ, Montes J, Pearson TS, Akman CI, et al. Long-term clinical course of Glut1 deficiency syndrome. J Child Neurol. 2015;30:160–169. doi: 10.1177/0883073814531822. [DOI] [PubMed] [Google Scholar]
- 102.Hainque E, Gras D, Meneret A, Atencio M, Luton M-P, Barbier M, et al. Long-term follow-up in an open-label trial of triheptanoin in GLUT1 deficiency syndrome: a sustained dramatic effect. J Neurol Neurosurg Psychiatry. 2019;90:1291–1293. doi: 10.1136/jnnp-2018-320283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Häberle J, Shahbeck N, Ibrahim K, Schmitt B, Scheer I, O’Gorman R, et al. Glutamine supplementation in a child with inherited GS deficiency improves the clinical status and partially corrects the peripheral and central amino acid imbalance. Orphanet J Rare Dis. 2012;7:48. doi: 10.1186/1750-1172-7-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bjoraker KJ, Swanson MA, Coughlin CR, Christodoulou J, Tan ES, Fergeson M, et al. Neurodevelopmental outcome and treatment efficacy of benzoate and dextromethorphan in siblings with attenuated nonketotic hyperglycinemia. J Pediatr. 2016;170:234–239. doi: 10.1016/j.jpeds.2015.12.027. [DOI] [PubMed] [Google Scholar]
- 105.Khaikin Y, Sidky S, Abdenur J, Anastasi A, Ballhausen D, Buoni S, et al. Treatment outcome of twenty-two patients with guanidinoacetate methyltransferase deficiency: An international retrospective cohort study. Eur J Paediatr Neurol. 2018;22:369–379. doi: 10.1016/j.ejpn.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 106.Miyake Z, Nakamagoe K, Yoshida K, Kondo T, Tamaoka A. Deferasirox might be effective for microcytic anemia and neurological symptoms associated with aceruloplasminemia: a case report and review of the literature. Intern Med. 2020;59:1755–1761. doi: 10.2169/internalmedicine.4178-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Donti TR, Blackburn PR, Atwal PS. Holocarboxylase synthetase deficiency pre and post newborn screening. Mol Genet Metab Reports. 2016;7:40–44. doi: 10.1016/j.ymgmr.2016.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kubaski F, Yabe H, Suzuki Y, Seto T, Hamazaki T, Mason RW, et al. Hematopoietic stem cell transplantation for patients with mucopolysaccharidosis II. Biol Blood Marrow Transplant. 2017;23:1795–1803. doi: 10.1016/j.bbmt.2017.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Papa FT, Mancardi MM, Frullanti E, Fallerini C, Della Chiara V, Zalba-Jadraque L, et al. Personalized therapy in a GRIN1 mutated girl with intellectual disability and epilepsy. Clin Dysmorphol. 2018;27:18–20. doi: 10.1097/MCD.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 110.Pierson TM, Yuan H, Marsh ED, Fuentes-Fajardo K, Adams DR, Markello T, et al. GRIN2A mutation and early-onset epileptic encephalopathy: personalized therapy with memantine. Ann Clin Transl Neurol. 2014;1:190–198. doi: 10.1002/acn3.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hausman-Kedem M, Menascu S, Greenstein Y, Fattal-Valevski A. Immunotherapy for GRIN2A and GRIN2D-related epileptic encephalopathy. Epilepsy Res. 2020;163:106325. doi: 10.1016/j.eplepsyres.2020.106325. [DOI] [PubMed] [Google Scholar]
- 112.Soto D, Olivella M, Grau C, Armstrong J, Alcon C, Gasull X, et al. l-Serine dietary supplementation is associated with clinical improvement of loss-of-function GRIN2B -related pediatric encephalopathy. Sci Signal. 2019;12:eaaw0936. [DOI] [PubMed]
- 113.Li D, Yuan H, Ortiz-Gonzalez XR, Marsh ED, Tian L, McCormick EM, et al. GRIN2D recurrent de novo dominant mutation causes a severe epileptic encephalopathy treatable with NMDA receptor channel blockers. Am J Hum Genet. 2016;99:802–816. doi: 10.1016/j.ajhg.2016.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Fuchs SA, Schene IF, Kok G, Jansen JM, Nikkels PGJ, van Gassen KLI, et al. Aminoacyl-tRNA synthetase deficiencies in search of common themes. Genet Med. 2019;21:319–330. doi: 10.1038/s41436-018-0048-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kok G, Tseng L, Schene IF, Dijsselhof ME, Salomons G et al. Treatment of ARS-deficiencies with specific amino acids. Under Review. [DOI] [PMC free article] [PubMed]
- 116.Grünert SC, Wendel U, Lindner M, Leichsenring M, Schwab KO, Vockley J, et al. Clinical and neurocognitive outcome in symptomatic isovaleric acidemia. Orphanet J Rare Dis. 2012;7:9. doi: 10.1186/1750-1172-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Incecik F, Bisgin A, Yılmaz M. MEDNIK syndrome with a frame shift causing mutation in AP1S1 gene and literature review of the clinical features. Metab Brain Dis. 2018;33:2065–2068. doi: 10.1007/s11011-018-0313-4. [DOI] [PubMed] [Google Scholar]
- 118.Lenz D, Stahl M, Seidl E, Schöndorf D, Brennenstuhl H, Gesenhues F, et al. Rescue of respiratory failure in pulmonary alveolar proteinosis due to pathogenic MARS1 variants. Pediatr Pulmonol. 2020;55:3057–3066. doi: 10.1002/ppul.25031. [DOI] [PubMed] [Google Scholar]
- 119.Coelho D, Kim JC, Miousse IR, Fung S, du Moulin M, Buers I, et al. Mutations in ABCD4 cause a new inborn error of vitamin B12 metabolism. Nat Genet. 2012;44:1152–1155. doi: 10.1038/ng.2386. [DOI] [PubMed] [Google Scholar]
- 120.Baumgartner MR, Hörster F, Dionisi-Vici C, Haliloglu G, Karall D, Chapman KA, et al. Proposed guidelines for the diagnosis and management of methylmalonic and propionic acidemia. Orphanet J Rare Dis. 2014;9:130. doi: 10.1186/s13023-014-0130-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lee T, Takami Y, Yamada K, Kobayashi H, Hasegawa Y, Sasai H, et al. A Japanese case of mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase deficiency who presented with severe metabolic acidosis and fatty liver without hypoglycemia. JIMD Rep. 2019;48:19–25. doi: 10.1002/jmd2.12051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Grünert SC, Sass JO. 2-methylacetoacetyl-coenzyme A thiolase (beta-ketothiolase) deficiency: one disease - two pathways. Orphanet J Rare Dis. 2020;15:106. doi: 10.1186/s13023-020-01357-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.van Karnebeek CDM, Ramos RJ, Wen X-Y, Tarailo-Graovac M, Gleeson JG, Skrypnyk C, et al. Bi-allelic GOT2 mutations cause a treatable malate-aspartate shuttle-related encephalopathy. Am J Hum Genet. 2019;105:534–548. doi: 10.1016/j.ajhg.2019.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Dahlin M, Martin DA, Hedlund Z, Jonsson M, Döbeln U, Wedell A. The ketogenic diet compensates for AGC1 deficiency and improves myelination. Epilepsia. 2015;56:e176–e181. doi: 10.1111/epi.13193. [DOI] [PubMed] [Google Scholar]
- 125.El-Hattab AW, Adesina AM, Jones J, Scaglia F. MELAS syndrome: clinical manifestations, pathogenesis, and treatment options. Mol Genet Metab. 2015;116:4–12. doi: 10.1016/j.ymgme.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 126.Ohsawa Y, Hagiwara H, Nishimatsu SI, Hirakawa A, Kamimura N, Ohtsubo H, et al. Taurine supplementation for prevention of stroke-like episodes in MELAS: a multicentre, open-label, 52-week phase III trial. J Neurol Neurosurg Psychiatry. 2019;90:529–536. doi: 10.1136/jnnp-2018-317964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Tam A, AlDhaheri NS, Mysore K, Tessier ME, Goss J, Fernandez LA, et al. Improved clinical outcome following liver transplant in patients with ethylmalonic encephalopathy. Am J Med Genet A. 2019;179:1015–1019. doi: 10.1002/ajmg.a.61104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ortigoza-Escobar JD, Alfadhel M, Molero-Luis M, Darin N, Spiegel R, de Coo IF, et al. Thiamine deficiency in childhood with attention to genetic causes: Survival and outcome predictors. Ann Neurol. 2017;82:317–330. doi: 10.1002/ana.24998. [DOI] [PubMed] [Google Scholar]
- 129.Trinh J, Imhoff S, Dulovic-Mahlow M, Kandaswamy KK, Tadic V, Schäfer J, et al. Novel NAXE variants as a cause for neurometabolic disorder: implications for treatment. J Neurol. 2020;267:770–782. doi: 10.1007/s00415-019-09640-2. [DOI] [PubMed] [Google Scholar]
- 130.Patterson MC, Vecchio D, Prady H, Abel L, Wraith JE. Miglustat for treatment of Niemann-Pick C disease: a randomised controlled study. Lancet Neurol. 2007;6:765–772. doi: 10.1016/S1474-4422(07)70194-1. [DOI] [PubMed] [Google Scholar]
- 131.Ory DS, Ottinger EA, Farhat NY, King KA, Jiang X, Weissfeld L, et al. Intrathecal 2-hydroxypropyl-β-cyclodextrin decreases neurological disease progression in Niemann-Pick disease, type C1: a non-randomised, open-label, phase 1–2 trial. Lancet. 2017;390:1758–1768. doi: 10.1016/S0140-6736(17)31465-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Huppke P, Weissbach S, Church JA, Schnur R, Krusen M, Dreha-Kulaczewski S, et al. Activating de novo mutations in NFE2L2 encoding NRF2 cause a multisystem disorder. Nat Commun. 2017;8:818. doi: 10.1038/s41467-017-00932-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.de Brouwer APM, van Bokhoven H, Nabuurs SB, Arts WF, Christodoulou J, Duley J. PRPS1 mutations: four distinct syndromes and potential treatment. Am J Hum Genet. 2010;86:506–518. doi: 10.1016/j.ajhg.2010.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Brasil S, Pascoal C, Francisco R, Marques-da-Silva D, Andreotti G, Videira P, et al. CDG therapies: from bench to bedside. Int J Mol Sci. 2018;19:1304. doi: 10.3390/ijms19051304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Martínez-Monseny AF, Bolasell M, Callejón-Póo L, Cuadras D, Freniche V, Itzep DC, et al. AZATAX: acetazolamide safety and efficacy in cerebellar syndrome in PMM2 congenital disorder of glycosylation (PMM2-CDG) Ann Neurol. 2019;85:740–751. doi: 10.1002/ana.25457. [DOI] [PubMed] [Google Scholar]
- 136.Lubout CMA, Goorden SMI, van den Hurk K, Jaeger B, Jager NGL, van Koningsbruggen S, et al. Successful treatment of hereditary folate malabsorption with intramuscular folinic acid. Pediatr Neurol. 2020;102:62–66. doi: 10.1016/j.pediatrneurol.2019.06.009. [DOI] [PubMed] [Google Scholar]
- 137.Hatch J, Coman D, Clayton P, Mills P, Calvert S, Webster RI, et al. Normal neurodevelopmental outcomes in PNPO deficiency: a case series and literature Review. JIMD Rep. 2015;91–7. [DOI] [PMC free article] [PubMed]
- 138.Sofou K, Dahlin M, Hallböök T, Lindefeldt M, Viggedal G, Darin N. Ketogenic diet in pyruvate dehydrogenase complex deficiency: short- and long-term outcomes. J Inherit Metab Dis. 2017;40:237–245. doi: 10.1007/s10545-016-0011-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Jauhari P, Sankhyan N, Vyas S, Singhi P. Thiamine responsive pyruvate dehydrogenase complex deficiency: a potentially treatable cause of Leigh’s disease. J Pediatr Neurosci. 2017;12:265. doi: 10.4103/jpn.JPN_191_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bedoyan JK, Hecht L, Zhang S, Tarrant S, Bergin A, Demirbas D, et al. A novel null mutation in the pyruvate dehydrogenase phosphatase catalytic subunit gene (PDP1) causing pyruvate dehydrogenase complex deficiency. JIMD Rep. 2019;48:26–35. doi: 10.1002/jmd2.12054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Barić I, Staufner C, Augoustides-Savvopoulou P, Chien Y-H, Dobbelaere D, Grünert SC, et al. Consensus recommendations for the diagnosis, treatment and follow-up of inherited methylation disorders. J Inherit Metab Dis. 2017;40:5–20. doi: 10.1007/s10545-016-9972-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Witters P, Tahata S, Barone R, Õunap K, Salvarinova R, Grønborg S, et al. Clinical and biochemical improvement with galactose supplementation in SLC35A2-CDG. Genet Med. 2020;22:1102–1107. doi: 10.1038/s41436-020-0767-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Byrne AB, Arts P, Polyak SW, Feng J, Schreiber AW, Kassahn KS, et al. Identification and targeted management of a neurodegenerative disorder caused by biallelic mutations in SLC5A6. NPJ Genomic Med. 2019;4:28. doi: 10.1038/s41525-019-0103-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Verrips A, Dotti MT, Mignarri A, Stelten BML, Verma S, Federico A. The safety and effectiveness of chenodeoxycholic acid treatment in patients with cerebrotendinous xanthomatosis: two retrospective cohort studies. Neurol Sci. 2020;41:943–949. doi: 10.1007/s10072-019-04169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Vogel KR, Ainslie GR, Walters DC, McConnell A, Dhamne SC, Rotenberg A, et al. Succinic semialdehyde dehydrogenase deficiency, a disorder of GABA metabolism: an update on pharmacological and enzyme-replacement therapeutic strategies. J Inherit Metab Dis. 2018;41:699–708. doi: 10.1007/s10545-018-0153-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhu B, Wu J, Chen G, Chen L, Yao Y. Whole exome sequencing identifies a novel mutation of TPK1 in a Chinese Family with Recurrent Ataxia. J Mol Neurosci. 2020;70:1237–1243. doi: 10.1007/s12031-020-01568-x. [DOI] [PubMed] [Google Scholar]
- 147.Tabarki B, Alfadhel M, AlShahwan S, Hundallah K, AlShafi S, AlHashem A. Treatment of biotin-responsive basal ganglia disease: Open comparative study between the combination of biotin plus thiamine versus thiamine alone. Eur J Paediatr Neurol. 2015;19:547–552. doi: 10.1016/j.ejpn.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 148.Trakadis YJ, Alfares A, Bodamer OA, Buyukavci M, Christodoulou J, Connor P, et al. Update on transcobalamin deficiency: clinical presentation, treatment and outcome. J Inherit Metab Dis. 2014;37:461–473. doi: 10.1007/s10545-013-9664-5. [DOI] [PubMed] [Google Scholar]
- 149.Schulz A, Ajayi T, Specchio N, de Los RE, Gissen P, Ballon D, et al. Study of intraventricular cerliponase Alfa for CLN2 disease. N Engl J Med. 2018;378:1898–1907. doi: 10.1056/NEJMoa1712649. [DOI] [PubMed] [Google Scholar]
- 150.Peña-Quintana L, Scherer G, Curbelo-Estévez ML, Jiménez-Acosta F, Hartmann B, La Roche F, et al. Tyrosinemia type II: mutation update, 11 novel mutations and description of 5 independent subjects with a novel founder mutation. Clin Genet. 2017;92:306–317. doi: 10.1111/cge.13003. [DOI] [PubMed] [Google Scholar]
- 151.Willemsen MA, Verbeek MM, Kamsteeg E-J, de Rijk-van Andel JF, Aeby A, Blau N, et al. Tyrosine hydroxylase deficiency: a treatable disorder of brain catecholamine biosynthesis. Brain. 2010;133:1810–1822. doi: 10.1093/brain/awq087. [DOI] [PubMed] [Google Scholar]
- 152.Rilstone JJ, Alkhater RA, Minassian BA. Brain dopamine-serotonin vesicular transport disease and its treatment. N Engl J Med. 2013;368:543–550. doi: 10.1056/NEJMoa1207281. [DOI] [PubMed] [Google Scholar]
- 153.Eichler F, Duncan C, Musolino PL, Orchard PJ, De Oliveira S, Thrasher AJ, et al. Hematopoietic stem-cell gene therapy for cerebral adrenoleukodystrophy. N Engl J Med. 2017;377:1630–1638. doi: 10.1056/NEJMoa1700554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Engelen M, Kemp S, de Visser M, van Geel BM, Wanders RJA, Aubourg P, et al. X-linked adrenoleukodystrophy (X-ALD): clinical presentation and guidelines for diagnosis, follow-up and management. Orphanet J Rare Dis. 2012;7:51. doi: 10.1186/1750-1172-7-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional File 1. Inherited metabolic disorders (IMDs) included in our 2012 (PMID 22212131) and 2014 (PMID 24518794) reviews and currently excluded.
Data Availability Statement
All data generated and analyzed during this study are included in this published article, the supplementary information files and the Treatable ID app (www. Treatable-id.org). The literature search and data are available upon request.