Abstract
Background: Burnout is common among physicians who care for critically ill patients and is known to contribute to worse patient outcomes. Fellows training in pulmonary and critical care medicine (PCCM) have risk factors that make them susceptible to burnout; for example, clinical environments that require increased intellectual and emotional demands with long hours. The Accreditation Council for Graduate Medical Education has recognized the increasing importance of trainee burnout and encourages training programs to address burnout.
Objective: To assess factors related to training and practice that posed a threat to the well-being among fellows training in PCCM and to obtain suggestions regarding how programs can improve fellow well-being.
Methods: We conducted a qualitative content analysis of data collected from a prior cross-sectional electronic survey with free-response questions of fellows enrolled in pulmonary, PCCM, and critical care medicine training programs in the United States. Fellows were asked what factors posed a threat to their well-being and what changes their training program could implement. Responses were qualitatively coded and categorized into themes using thematic analysis.
Results: A total of 427 fellows (44% of survey respondents) completed at least one free-response question. The majority of respondents (60%) identified as male and white/non-Hispanic (59%). The threats to well-being and burnout were grouped into five themes: clinical burden, individual factors, team culture, limited autonomy, and program resources. Clinical burden was the most common threat discussed by fellows. Fellows highlighted factors contributing to burnout that specifically pertained to trainees including challenging interpersonal relationships with attending physicians and limited protected educational time. Fellows proposed solutions addressing clinical care, changes at the program or institution level, and organizational culture changes to improve well-being.
Conclusion: This study provides insight into factors fellows report as contributors to burnout and decreased well-being in addition to investigating fellow-driven solutions toward improving well-being. These solutions may help pulmonary, PCCM, and critical care medicine program directors better address fellow well-being in the future.
Keywords: qualitative research, medical education, burnout
Burnout has been well described in healthcare professionals and is known to be common in physicians who care for critically ill patients (1). Burnout is a response to exposure to prolonged emotional and interpersonal workplace stressors, leading to exhaustion, depersonalization, and a reduced sense of personal efficacy (2). Physician burnout has been associated with worse patient safety, reduced quality of care, and decreased patient satisfaction (3–5). Furthermore, burnout may contribute to alcohol abuse, broken relationships, depression, and suicidal ideation among healthcare professionals (6, 7).
Healthcare professional trainees, including medical students and residents, have also been found to have high rates of burnout (8). Risk factors for burnout among residents and fellows includes high workload, lack of control over time management, challenging job situations, impaired interpersonal relationships, lack of a coverage system in the setting of an emergency, and lack of access to services to promote physician well-being (8–11).
Thus far, there has been limited research on burnout in fellows training in pulmonary and critical care medicine (PCCM). A nationwide survey of fellows training in PCCM found a burnout prevalence of 32% (11). Given the nature of their professional role with increased time spent in the intensive care unit (ICU) compared with noncritical care trainees, fellows training in PCCM may have unique factors that contribute to their burnout beyond those found to be significant in resident physicians.
In response to growing national concern about physician burnout, there has been an increased focus on the importance of promoting well-being among healthcare providers and in creating healthy work environments (1). The Accreditation Council for Graduate Medical Education (ACGME) recently revised its core program requirements recognizing the importance of burnout and depression in trainees (12). Although a variety of interventions have been trialed to reduce burnout in healthcare professionals and trainees (13, 14), there have been no multiinstitution studies asking trainee physicians what changes could be made to their training program to improve physician well-being.
This study aimed to 1) assess factors related to training and practice that posed a threat to physician well-being or increased burnout among fellows training in PCCM, and 2) describe suggestions from fellows regarding how training programs can improve physician well-being and reduce burnout.
Methods
Procedures
The study was reviewed by the Johns Hopkins University Institutional Review Board (IRB-X 00,163,987) and determined to be exempt. This was a qualitative content analysis of data collected in a prior cross-sectional study conducted by a survey from January to February 2019. The survey items were developed by a panel of fellows, program directors, and psychologists involved in medical education who are all listed as authors of this study and were iteratively revised through cognitive interviewing and pilot testing with trainees and pulmonary critical care fellows from the Association of Pulmonary and Critical Care Medicine Program Directors (APCCMPD) fellow workgroup. The survey was deployed through the Johns Hopkins Qualtrics survey software program to fellows enrolled in pulmonary, PCCM, and CCM fellowship training programs in the United States by using a member list available through the APCCMPD. Four weekly reminder emails were sent to individuals who had not completed the survey. A $10 Amazon voucher was provided on survey completion.
Within the survey, three free response questions asked fellows about threats to well-being and for suggestions regarding how training programs can improve well-being. These questions were:
-
1)
What factors of your training/practice, if any, do you feel pose a threat to your physician wellness and/or increase your burnout?
-
2)
Of these factors, which do you feel affects your physician wellness and/or burnout risk the most?
-
3)
What are things your training program can do to improve your physician wellness and/or reduce burnout?
Responses to free response questions were not required for survey completion. There was no limit placed on the number of threats or length of responses fellows could provide. During cognitive interviewing and pilot testing, pulmonary and critical care fellows expressed understanding that survey questions referred to their wellness and burnout as related to being PCCM fellows.
Individual Characteristics
Demographic data including age, sex, and race/ethnicity were collected. Participants were also asked to provide information regarding relationship status, caregiver responsibilities, type of fellowship, and geographic location of their fellowship.
Analysis
The responses to the three free response questions were analyzed via inductive qualitative content analysis. A subgroup of investigators (M.S., M.N.E., J.O’T., and S.Z.) worked together to inductively create a codebook based on participant responses. Using this codebook, author J.O.’T. coded responses to the free response questions (15). Given the short length of responses to free response questions, Microsoft Excel (Microsoft) was used to code qualitative data. Modifications to the codebook were then discussed and agreed on by the subgroup of investigators. Two independent coders (J.O.’T. and S.Z.) then recoded the data on the basis of the modified codebook. Any threats to reliability and validity were addressed by triangulation among the investigators (16). Any discrepancies between the two coders were discussed with senior investigators (M.N.E. and M.S.) with the final coding decided based on group consensus. A coding comparison among J.O.’T. and S.Z. was calculated using Cohen’s κ coefficient. The codes were then organized into themes using thematic analysis informed by prior studies about physician burnout (17). Given the similarity in responses to Question 1 and 2, we have chosen to focus on the responses to Question 1 in our presentation of results. By nature of this free response survey, formal evaluation of saturation could not be assessed but a recurrence of themes was documented, with most themes being reported by at least three people.
Results
The survey was sent to 976 pulmonary, PCCM, and CCM fellows, and 427 fellows (44%) completed at least one free response question. Over 90% of the 427 fellows who completed at least one free response question were PCCM fellows (Table 1). The responding fellows were divided among their first (37%), second (33%), or third and above (30%) fellowship years. The majority of respondents (60%) identified as men and 59% of fellows identified as non-Hispanic white. A total of 326 fellows (76%) reported that they were married, with 176 (41%) reporting caregiver responsibilities (defined as caring for children, disabled or ill family members, or elders). Of the 427 fellows who completed a free response question, 143 fellows (33%) screened positive for burnout and 175 (41%) screened positive for depressive symptoms.
Table 1.
Characteristics of sample population responding to any open-ended question (N = 427)
| Characteristic | n (%) |
|---|---|
| Fellowship type | |
| Critical care medicine | 33 (8) |
| Pulmonary medicine | 5 (1) |
| Pulmonary and critical care medicine | 388 (91) |
| Missing | 1 (<1) |
| Fellowship year | |
| First-year | 156 (37) |
| Second-year | 141 (33) |
| Third-year or beyond | 128 (30) |
| Missing | 2 (<1) |
| AAMC geographic region | |
| Central | 113 (26) |
| Northeast | 175 (41) |
| South | 54 (13) |
| West | 63 (15) |
| Missing | 22 (5) |
| Age* | 32.6 ± 2.79 |
| Gender | |
| Identifies as male | 255 (60) |
| Identifies as female | 169 (39) |
| Missing | 3 (1) |
| Married | 326 (76) |
| Has caregiver responsibilities† | 176 (41) |
| Race/ethnicity | |
| White/non-Hispanic | 252 (59) |
| Black/non-Hispanic | 12 (3) |
| Asian or Pacific Islander | 103 (25) |
| Hispanic | 15 (4) |
| Native American/Alaskan | 1 (<1) |
| More than one option | 34 (8) |
| Missing | 10 (2) |
| Screened positive for burnout | 143 (33) |
| Screened positive for depressive symptoms | 175 (41) |
Definition of abbreviation: AAMC = Association of American Medical Colleges.
Note that the percentages do not equal 100 because of rounding.
Reported as mean ± standard deviation.
Caregiver responsibilities include children, disabled or ill family member, or elders.
Interrater reliability analysis was performed for coding. Cohen’s κ coefficient was calculated among coders J.O.’T. and S.Z. and resulted in substantial agreement, κ = 0.80.
Threats to Physician Well-Being and Burnout
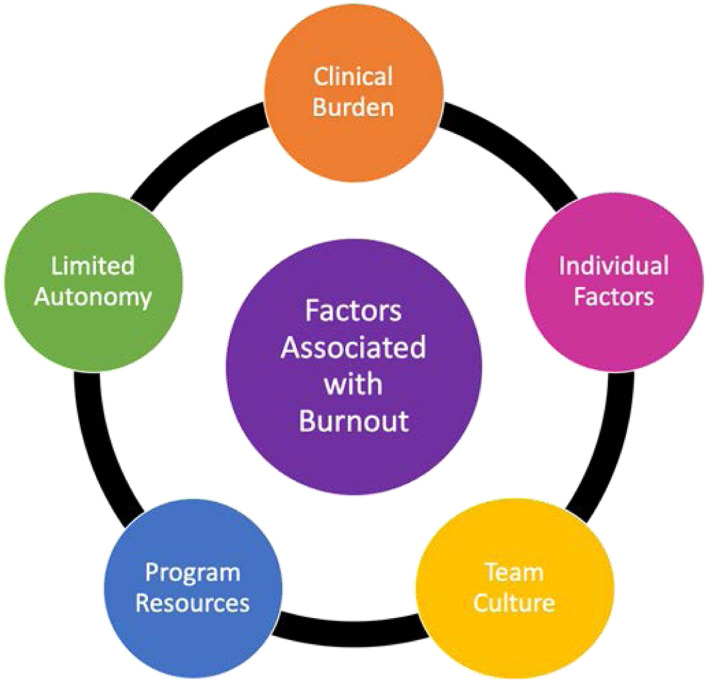
A free response answer to an inquiry about threats to physician well-being and burnout was provided by 423 fellows. Among the respondents, 26 (6%) indicated they had no sources of burnout or were unsure about sources of burnout. Five themes were found to pose a threat to physician wellness and/or increase burnout: clinical burden, individual factors, team culture, program resources, and limited autonomy (Figure 1).
Figure 1.
Common fellow reported themes from written responses to the following question: “What factors of your training/practice, if any, do you feel pose a threat to your physician wellness and/or increase your burnout?”
Clinical burden
A commonly reported threat to fellow well-being was a clinical burden, reported by 301 fellows (71%). The most commonly referenced code within clinical burden was workload (N = 207, 49%) (Table 2). One fellow described workload as, “Working long hours, taking home call, not getting enough sleep, and then working a 12+ hours shift the next day during which I know I am making mistakes and working less efficiently than normal” (Fellow 201).
Table 2.
Themes identified from written responses to the question, “What factors of your training/practice, if any, do you feel pose a threat to your physician wellness and/or increase your burnout?”*
| Theme and Code | n (%)† | Exemplar Quote |
|---|---|---|
| Clinical burden | ||
| Workload | 207 (49) | “Combination of frequency of overnight call with length of harder clinical rotations.” 78 |
| “12 continuous days of 12 h a day ICU.” 220 | ||
| Administrative burden | 82 (19) | “Billing and EMR, documentation.” 262 |
| “Amount of documentation in electronic medical record.” 26 | ||
| Patient responsibility | 63 (15) | “High pressure environment without room for errors.” 427 |
| “Ratio of patients to provider.” 1 | ||
| Emotional toll | 54 (13) | “Taking care of dying patients without an emotional outlet to address this.” 104 |
| “Futile care in the ICU.” 5 | ||
| Clinical resources | 49 (12) | “Clinic-related issues such as outside records, follow-up, phone calls.” 310 |
| “Limited clinic nursing support.” 185 | ||
| Individual factors | ||
| Work–life | 52 (12) | “Not having enough truly free time away from the hospital.” 139 |
| “Having to take lots of work home.” 323 | ||
| Personal health concerns | 34 (8) | “Lack of time for self-maintenance.” 365 |
| “Chronic sleep deprivation.” 384 | ||
| Finances | 27 (6) | “The debt the debt the debt.” 14 |
| “Financial insecurity.” 426 | ||
| Resources for child health | 8 (2) | “Lack of any structured maternity leave.” 119 |
| “Lack of childcare.” 264 | ||
| Team culture | ||
| Leadership issues | 85 (20) | “Emphasis on hospital and institutional priorities over individual learning.” 87 |
| “Reporting same problems to the program leadership without changes.” 290 | ||
| Interpersonal relationships | 54 (13) | “Poor interpersonal/professional interactions (hostile environment).” 132 |
| “Feeling like a scribe for attendings, midlevels being given more priority than trainees.” 297 | ||
| Lack of appreciation | 44 (10) | “Being made to feel like a workhorse instead of someone who is respected.” 497 |
| “Lack of recognition by attendings and staff.” 236 | ||
| Communication | 17 (4) | “Unclear expectations.” 463 |
| “Challenges in responding to feedback.” 68 | ||
| Program resources | ||
| Protected time | 47 (11) | “Simultaneous “protected” time that doesn’t really exist in which to produce other research work in an academic setting.” 379 |
| “Pressure to complete research/academic production to get an academic job while balancing clinical responsibilities.” 4 | ||
| Educational inefficiency | 38 (9) | “Rotations with poor education: Service ratio.” 373 |
| “Lack of program leadership emphasis on importance of clinical care, education, QI efforts (as opposed to significant emphasis on research accomplishments).” 229 | ||
| Career development | 37 (9) | “The lack of care by mentors/superiors.” 328 |
| “Limited opportunity for creative work or growth.” 414 | ||
| Lack of perks‡ | 8 (2) | “Not enough free food.” 63 |
| “No place to rest at work.” 175 | ||
| Limited autonomy | ||
| Schedule | 39 (9) | “Lack of control/planning for our schedule and work hours.” 383 |
| Flexibility | “Lack of control over one’s schedule.” 120 | |
| Autonomy | 36 (9) | “The lack of autonomy in my program has significantly decreased the amount of satisfaction that I get from work.” 72 |
| “Essentially, a lack of control over medical decision despite bearing the burdens of malpractice risk.” 310 |
Definition of abbreviations: EMR = electronic medical record; ICU = intensive care unit.
Italicized numbers with quotes represent fellow identification numbers.
Fellow responses reported as the frequency of theme mention (n) as a percentage of total responses (N = 423). The total exceeds 100% because of multiple themes referenced per response.
Perks included free food, coffee, parking, and activities.
The theme clinical burden additionally encompassed codes for administrative burden, patient responsibilities, the emotional toll of patient care, and resource access for clinical care (Table 2). As one fellow wrote about documentation, coded as an administrative burden: “There is little opportunity to take joy in being a physician and specialist given the time constraints of having too many patients as well as having to document for hours on end. I feel like I am not really taking care of the patient” (Fellow 288).
Another fellow described the emotional toll: “The expectations during one shift are so high, pulled in so many directions, that it leaves little room to do a good job. This leads to loss of meaningfulness in my work and I feel unhappy about the work I am doing. This also leads to a loss of humanity as I rarely find time for a simple break or to eat when hungry” (Fellow 198).
Individual factors
A total of 68 fellows (16%) described individual factors that posed a threat to physician wellness and/or increased burnout, which comprised the second theme. The most common code within individual factors was the work–life balance. Within this code, fellows described having inadequate time with family and friends, or work encroaching on personal time. One fellow wrote: “Outpatients having access to me 24/7. They are ruining my life” (Fellow 403).
The individual factors theme includes codes about concerns about personal health, finances, and resources for child health (Table 2). As one fellow wrote, “Cost of living increases exceeds salary, particularly when factoring in childcare in a high cost of living area, requiring moonlighting or excessively long commutes to avoid going further into debt” (Fellow 92).
Team culture
Within the third theme, over one-third of fellows (35%) described elements of team culture that threatened their well-being and/or increased burnout; codes include leadership issues, interpersonal relationships, lack of appreciation, and difficulties with communication (Table 2). On the subject of the fellowship program leadership issues, fellows reported programs making changes without soliciting feedback from them. A fellow suggested for leadership to “make an attempt (even if it is not wholehearted) to listen to our issues and try to fix them” (Fellow 184).
Interpersonal relationships with attending physicians and “contentious relationships with nurse practitioners and physician assistants about distribution of work” (Fellow 192) were also seen as a threat to well-being.
One fellow described “the pettiness and aggressiveness of attendings. We’re treated like children” (Fellow 286).
Fellows also described a lack of appreciation as a factor threatening wellness:
“The fellowship program relies heavily on the clinical service provided by fellows but in the event of any issues is very unlikely to solicit the fellow’s perspective or ensure that the fellows have adequate support, rather the result is punitive, leading to a sense of unease and unappreciation” (Fellow 217).
Program resources
The fourth theme listed as posing a threat to wellness and/or increased burnout by 101 fellows (24%) was program resources, which included the codes of protected time, educational inefficiency, career development, and lack of perks (i.e., free food, coffee, and parking) (Table 2). A fellow described insufficient protected time: “Clinical care always bleeds into ‘protected time’ supposedly dedicated to research/scholarship” (Fellow 211).
Educational inefficiency was described as work obligations that did not benefit education. As a fellow wrote, “being used as a workhorse to make money for the hospital and pick up attending workload when it doesn’t benefit learning” (Fellow 47).
Within the code of career development, fellows described insufficient mentorship and dissatisfaction with their career trajectory:
“The feeling that attendings, program leadership, and/or mentors are not interested in your learning and career development. They are more interested in preserving the status quo of career trajectories” (Fellow 409).
Limited autonomy
Finally, within the fifth theme of limited autonomy, 65 fellows (15%) described factors limiting clinical autonomy and schedule flexibility as threats to well-being (Table 2). Per one fellow, “Faculty do not allow fellows to lead rounds, independently perform procedures, or make primary decisions with their feedback and guidance. Usually my experience has been that the attending takes the lead, while I take care of logistics, note writing, and orders” (Fellow 481).
Suggestions for Improving Fellowship Well-Being
A free response answer regarding how training programs could improve well-being or reduce burnout was provided by 375 fellows. Of these, 57 fellows (15%) suggested no changes be made, as their programs were doing a good job, whereas others believed some of the difficulties, such as long hours, sick patients, and challenging outcomes, were inherent to training in PCCM.
“Now I actually make a point of this and inform new applicants to make sure they understand the pitfalls of this subspecialty” (Fellow 470).
There were three themes of recommendations from fellows regarding changes to improve well-being and reduce burnout: changes at the program or institution level, changes related to clinical practice, and changes related to the organizational culture.
Program or institution
Fifty percent of fellows recommended changes be made at the program or institutional level to promote well-being (Table 3). Codes within this theme include protected academic development, more perks (including free food, coffee, and access to gym memberships), program leadership changes, providing more mental health/emotional support, supporting financial needs, providing resources related to children and family, and ensuring a backup provider system was organized. Fellows asked program directors to “Listen, listen, listen. Treat us like adults” (Fellow 409).
Table 3.
Themes identified from written responses to the question, “What are things your training program can do to improve your physician wellness and/or reduce burnout?”*
| Theme and Code | n (%)† | Exemplar Quote |
|---|---|---|
| Program or institution | ||
| Protected academic development | 87 (23) | “Set up guidelines for what responsibilities should NOT be assigned to the fellow, as they have little educational value and simply take advantage of the fellow to do busy work.” 449 |
| “Fewer mandatory educational conferences or protected time to attend them.” 333 | ||
| Perks (free food, coffee, parking, and activities) | 71 (19) | “Free food and counseling sessions to deal with stress at workplace.” 228 |
| “Improve or additional on-site gym access, financial support for childcare, some kind of activity for spouses, free and nutritious food.” 69 | ||
| Program leadership | 44 (12) | “Increase microaggressions awareness.” 478 |
| “Meet with the fellows and actually change aspects of the program, which has not been done to a large degree. All of the programs decisions seem designed to maximize attendings work satisfaction.” 352 | ||
| Mental health/emotional support | 24 (6) | “Offer assistance with wellness. Allowing easy access to mental health services, including coverage for shift. More resources for wellness.” 103 |
| “Hearing attendings experience with burnout.” 116 | ||
| Physical activity | 23 (6) | “Having an on-site gym would be hugely beneficial.” 258 |
| “Free yoga sessions.” 35 | ||
| Financial | 22 (6) | “Do anything to actually reduce the burdens of training and raising a family (for many of us, anyway) on a salary that compels us to moonlight to make ends meet. Negotiate for meals at every hospital.” 114 |
| “Provide additional financial support for educational costs (study aids, board examination costs, publication fees).” 207 | ||
| Resources related to children/family | 19 (5) | “Help fellows obtain spots in the on-site daycare program. There is a 1-yr waitlist. Residents and fellows should have preferred access given the hours worked and pay received.” 134 |
| “Improve parental and maternity leave to at least the standard of the rest of the University.” 343 | ||
| Back up provider | 10 (3) | “No real organization. If you want to go to a conference or have a family emergency, you are left begging other fellows for coverage and always must make it up.” 222 |
| “Establish a sick call system.” 348 | ||
| Clinical | ||
| Reduce physician workload | 86 (23) | “Divide tasks more equitably, have the fellows more integrated into the team, rather than triaging the ICU 24/7.” 71 |
| “Cap length of a particular rotation at 4 wk. Reduce frequency of overnight call.” 78 | ||
| More flexibility in work | 58 (16) | “Standardizing time off and schedule so that sleep/wake cycles can regulate for longer periods of time. For example, I do not need a reduction in the amount of call but if it was more patterned and predictable, I could likely help plan better.” 275 |
| “Limit bleed of work in home life.” 204 | ||
| Involve more care providers | 38 (10) | “Increase clinical staff support or limit (cap) number of patients/procedures/etc. for academic teams.” 198 |
| “Hire more fellows and institute a night float system.” 131 | ||
| Assistance with administrative burden | 31 (8) | “Decreased the number of patients required to be seen (especially in clinic). Simplify the billing system.” 318 |
| “Provide ancillary resources like people that can set up our patients with sleep studies, pulmonary rehab, etc.” 29 | ||
| Make attending physicians more available to provide care | 9 (2) | “Prioritize physician wellness among the faculty. It’s hard to imagine improving fellow burnout when the faculty appear burned out.” 474 |
| “Have dedicated attendings to each service that are not responsible for nonclinical duties at the same time, allowing us to be more efficient and get the day done in a reasonable time.” 15 | ||
| Organizational culture | ||
| Professional interpersonal interactions/team building | 33 (9) | “Community building, listen to feedback on how to improve.” 157 |
| “Improve relations between fellowships.” 97 | ||
| Appreciation | 32 (9) | “Frequent recognition of fellow contributions to division/department objectives and patient care.” 204 |
| “Anything that makes me feel valued will probably reduce my sense of burnout.” 485 | ||
| Clear communication | 20 (5) | “Clear delineation of fellows’ clinical role.” 319 |
| “More clearly defined roles for fellows and APP’s.” 192 | ||
| More autonomy | 6 (2) | “Support fellows in decisions if justification is found reasonable.” 310 |
| “More autonomy.” 34 |
Definition of abbreviation: APP = advance practice provider; ICU = intensive care unit.
Italicized numbers with quotes represent fellow identification numbers.
Fellow responses reported as the frequency of theme mention (n) as a percentage of total responses (N = 375). The total exceeds 100% because of multiple themes referenced per response.
One fellow highlighted the importance of addressing financial concerns and providing resources related to children and family: “At the institutional level, there is zero recognition of the cost of living and childcare. For reference, average childcare in my city is $2,500/month and annual salary is $72,000. Subsidized childcare would be a miracle cure for my own stress and burnout. I would trade every other ‘wellness’ initiative for tangible help dealing with the financial burden” (Fellow 53).
Fellows also recommended loan forgiveness and funding sources other than the postgraduate year scale. As one fellow said, “There needs to be alternative funding sources for supporting senior fellows/junior faculty as they transition to assistant professor roles. Staying on the postgraduate year (PGY) scale is not tenable and will select for fellows who are 1) without kids, or 2) have a high-earning spouse” (Fellow 43).
Clinical practice
There were 172 fellows (46%) who suggested changes to clinical practice to reduce burnout, which comprised the second theme (Table 3). Reduction of physician workload was the most common code in this theme with recommended initiatives such as reduced number of hours worked, reduction in the overnight call, a protected weekend day off during all ICU rotations, and “better coordination of clinic days while on inpatient services” (Fellow 159).
Other codes within the changes to clinical practice theme include increasing flexibility in work, involving more care providers to decrease the clinical burden per provider, providing assistance with the administrative burden of clinical care with decreased documentation burden, and making attending physicians more available to provide clinical care.
Organizational culture
Finally, 73 fellows (19%) recommended making organizational culture changes, which were categorized as the third theme. The codes within this theme included improving professional interpersonal interactions with attending physicians and other team members, improving appreciation for fellows, setting clear communication efforts about expectations for the fellow’s role on the team, and more autonomy for fellows (Table 3).
A fellow highlighted the importance of supporting younger fellows on the team: “I think that most burnout interventions that provide an escape hatch from work are not helpful. People have to get joy from the job… I’m helping younger docs learn the ropes, helping patients, and doing procedures that bring me joy” (Fellow 14).
Another fellow highlighted the importance of improved appreciation to reduce burnout and wrote, “Show at least a modicum of appreciation for the clinical service being provided by fellows and provide adequate support from a divisional and institutional perspective” (Fellow 217).
Discussion
In this nationwide survey of fellows training in PCCM, fellows suggested a number of factors contributing to burnout which were qualitatively grouped into five themes: clinical burden, individual factors, team culture, lack of program resources, and limited autonomy. Fellows offered suggestions on how to enhance well-being that was grouped into three themes: changes to the program or institution (i.e., improving training environment), clinical care (i.e., reducing physician workload), and changing the organizational culture (i.e., improving communication with team members).
Factors contributing to burnout within this study were similar to previously described research within different subspecialties in medicine, with threats including clinical workload, lack of autonomy, lack of time for personal/family life, and poor support (3, 6, 8, 18–20). Some threats to well-being described by fellows, such as those categorized within clinical burden and individual factors, may pertain to all physicians. Other threats described are factors that may impact fellows more because of the academic hierarchy. For example, within team culture, fellows described challenges with interpersonal relationships with attending physicians and difficulty with effective communication. Fellows often serve as a go-between for attending physicians and residents, nursing staff, and patients. Clear communication and expectations in addition to professional and productive relationships with attending physicians are important for effective patient care. Within program resources, threats such as educational inefficiency and inadequate career development opportunities are also relevant for fellows, who pursued a fellowship in an effort to further their education and skillset development to further their career opportunities.
There has been limited research on interventions to reduce burnout at the program and division level (21). In a nationwide survey of PCCM division directors, many directors indicated they have not tried to address burnout and do not know of effective solutions to promote well-being (21). Research emphasizes the importance of acknowledging and assessing the problem of burnout, harnessing the power of effective leadership, and building targeted interventions to address burnout (6). To inform the creation of burnout interventions, it is important to incorporate suggestions from fellows and consider including fellows on well-being committees (1). Although some recommendations from fellows highlighted big picture issues in medicine that will take time to address, including overall physician workload, financial compensation, and documentation requirements, fellows also provided recommendations for changes that can be made at the program level and within the culture of the organization.
At the training program level, fellows recommended protected academic development time to support career development. This includes initiatives such as dedicated research time for individuals looking to pursue physician–scientist careers, ensuring fellows have time free of clinical obligations to attend educational conferences, and protecting clinical elective time to allow fellows to take full advantage of learning opportunities on the elective. Fellows also asked for improved program leadership efforts to involve fellows before making fellowship changes and advocate for fellows within the department and institution. Finally, fellows endorsed the importance of developing mental health resources within fellowship programs. Access to mental health services has been shown to be associated with lower odds of burnout (11) and has been highlighted to be essential by the ACGME (12).
From an organizational culture level, fellows reported activities targeting improved interpersonal relationships with attending physicians and other team members would help to improve well-being such as community-building activities. Promoting community at work has been acknowledged as a critical mechanism to help physicians navigate the professional challenges of medicine (6). Fellows advocated for recognition of their efforts within the division through mechanisms such as public recognition at both the division and institutional level and treatment with more respect from program and division leadership. Studies have shown that the recognition of employees boosts productivity, increases job satisfaction, and improves communication and cooperation within the workplace (14).
Strengths and Limitations
This study is one of the first to investigate threats to the well-being of fellows training in PCCM and to seek recommendations from fellows on strategies and suggestions to improve burnout. Its strengths include a nationwide representation of pulmonary, PCCM, and CCM fellowships. The characteristics of respondents are similar to reported characteristics of pulmonary and critical care fellows documented by the ACGME and represent 31 of 42 states with fellowship programs, supporting a representative sample (22). There were also several limitations to this study. We cannot comment on the experiences of nonresponders as being positive or negative surrounding burnout. In inquiring about “physician wellness and/or burnout” at the same time, the survey questions may have led participants to describe factors that led to lack of wellness that did not necessarily contribute to burnout. Within our pilot testing sessions, participants expressed understanding that survey questions referred to physician wellness and burnout related to being a PCCM fellow and answered questions in this way. Given the nature of our data collection via an anonymous survey, we were unable to clarify or further investigate free response statements made by fellows. Maintaining anonymity was important to allow for open discussion of fellow concerns. Inherently in qualitative analysis, all bias cannot be removed. Although coders were involved in PCCM fellowship training, neither was involved in administrative roles within their PCCM fellowships and consensus of coding with senior investigators was sought for disagreements.
Burnout impacts physician trainees and the quality of care they are able to provide. This study provides insight for program and division directors on threats to well-being that influence fellows training in PCCM and contributes to the dialogue of how burnout can be better addressed in the future.
Supplementary Material
Footnotes
Supported by the Association of Pulmonary and Critical Care Medicine Program Directors and by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number T32HL007534. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Contributions: M.N.E. and M.S. designed the work and contributed to the acquisition of data. All authors participated in the analysis or interpretation of data. J.O’T., S.Z., M.N.E., and M.S. drafted the manuscript, with M.H.A., R.W.A., L.D.B., G.T.B., K.M.B., S.T.D., M.M.K.S.K., P.H.L., J.W.M., C.S.R., K.A.R., M.I.S., and G.R.W. revising the manuscript for important intellectual content. All authors provided final approval of the manuscript for publication and agree to be accountable for all aspects of this work.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals. A call for action. Am J Respir Crit Care Med. 2016;194:106–113. doi: 10.1164/rccm.201604-0708ST. [DOI] [PubMed] [Google Scholar]
- 2.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 3.Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 4.Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open. 2017;7:e015141. doi: 10.1136/bmjopen-2016-015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anagnostopoulos F, Liolios E, Persefonis G, Slater J, Kafetsios K, Niakas D. Physician burnout and patient satisfaction with consultation in primary health care settings: evidence of relationships from a one-with-many design. J Clin Psychol Med Settings. 2012;19:401–410. doi: 10.1007/s10880-011-9278-8. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149:334–341. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 8.Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1:236–242. doi: 10.4300/JGME-D-09-00054.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen JS, Patten S. Well-being in residency training: a survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Med Educ. 2005;5:21. doi: 10.1186/1472-6920-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nyssen AS, Hansez I, Baele P, Lamy M, De Keyser V. Occupational stress and burnout in anaesthesia. Br J Anaesth. 2003;90:333–337. doi: 10.1093/bja/aeg058. [DOI] [PubMed] [Google Scholar]
- 11.Sharp M, Bukart KM, Adelman MH, Ashton RW, Biddison LD, Bosslet G, et al. A national survey of burnout and depression among fellows training in pulmonary and critical care medicine: a special report by the Association of Pulmonary and Critical Care Medicine program directors Chest[online ahead of print] 2020 Sep 18; DOI: 10.1016/j.chest.2020.08.2117. PubMed [DOI] [PMC free article] [PubMed]
- 12.Accredited Council for Graduated Medical Education Summary of changes to ACGME common program requirements section VI Chicago, IL: Accredited Council for Graduated Medical Education; [accessed 2019 Sep 18]. Available from: https://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements/Summary-of-Proposed-Changes-to-ACGME-Common-Program-Requirements-Section-VI [Google Scholar]
- 13.Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 14.Walsh AL, Lehmann S, Zabinski J, Truskey M, Purvis T, Gould NF, et al. Interventions to prevent and reduce burnout among undergraduate and graduate medical education trainees: a systematic review. Acad Psychiatry. 2019;43:386–395. doi: 10.1007/s40596-019-01023-z. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 16.Archibald MM. Investigator triangulation: a collaborative strategy with potential for mixed methods research. J Mixed Methods Res. 2016;10:228–250. [Google Scholar]
- 17.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 18.Embriaco N, Azoulay E, Barrau K, Kentish N, Pochard F, Loundou A, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175:686–692. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- 19.Upton D, Mason V, Doran B, Solowiej K, Shiralkar U, Shiralkar S. The experience of burnout across different surgical specialties in the United Kingdom: a cross-sectional survey. Surgery. 2012;151:493–501. doi: 10.1016/j.surg.2011.09.035. [DOI] [PubMed] [Google Scholar]
- 20.Escribà‐Agüir V, Pérez‐Hoyos S. Psychological well-being and psychosocial work environment characteristics among emergency medical and nursing staff. Stress Health. 2007;23:153–160. [Google Scholar]
- 21.Rinne ST, Swamy L, Anderson E, Shah T, Dixon AE, Kaminski N, et al. Perspectives on burnout from pulmonary, critical care, and sleep medicine division directors. Am J Respir Crit Care Med. 2020;201:111–114. doi: 10.1164/rccm.201906-1262LE. [DOI] [PubMed] [Google Scholar]
- 22.Accreditation Council for Graduate Medical Education. ACGME data resource book 2017–2018. Chicago, IL: Accreditation Council for Graduated Medical Education: 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.