Abstract
Objectives:
To evaluate systematically the effectiveness of miniscrew-supported maxillary incisor intrusion compared with other nonsurgical intrusive mechanics for deep-bite correction.
Materials and Methods:
Unrestricted electronic searches in Embase, Web of Science, MEDLINE, LILACS, and Cochrane's CENTRAL as well as manual searches were conducted up to August 2019. Only randomized clinical trials (RCTs) were included. Study selection, data extraction, and bias assessment were done by two independent reviewers. The Cochrane risk-of-bias tool was used, and the quality of evidence was graded using the GRADE approach. A random-effects meta-analysis of continuous data, with its 95% confidence intervals (CIs), was used.
Results:
Seven RCTs were included in the quantitative synthesis, and the overall quality of evidence was very low to low. When compared with intrusion arches, miniscrews resulted in a more efficient deep-bite reduction with a standardized mean difference (SMD) of −0.48 (95% CI, −0.89 to −0.07). When miniscrews were used, a statistically significant difference was observed favoring less maxillary molar extrusion (SMD, −0.86; 95% CI, −1.46 to −0.27) and more incisor intrusion as measured from centroid to palatal plane (SMD, −0.95; 95% CI, −1.41 to −0.49). Results also showed a statistically nonsignificant difference regarding the amount of resultant root resorption between miniscrews and intrusion arches.
Conclusions:
There is weak evidence indicating efficient deep-bite correction using miniscrews. Root resorption seems to be an associated adverse effect that occurs regardless of the intrusive mechanics used. These conclusions should be viewed with great caution as further well-designed long-term research is recommended.
Keywords: Systematic review, Miniscrews, Mini-implants, Intrusion, Deep-bite malocclusion, Root resorption
INTRODUCTION
Deep overbites are considered a daunting challenge during orthodontic correction because of their various etiological backgrounds.1 Many associated factors could affect the mechanism chosen for correcting deep bites, such as the starting age of the patients, severity of deep bite, smile line, and any associated periodontal problems.2 Nonsurgical correction of deep bites could be accomplished by extruding the molars, intruding the incisors, proclination, or a combination of all of these methods.3,4 These movements are usually accomplished using a variety of treatment mechanics: anterior bite planes, functional appliances, J-hook headgear (J-HG), intrusion arches, reverse curve archwires, interarch elastics, clear aligners, and bonding the posterior molars.5
Extrusion of posterior teeth might be viewed as a good option in low-angle growing patients. However, in an adult population, these movements might be associated with greater tendencies for relapse as the masticatory muscles mature.6 Therefore, intruding the maxillary incisors may be a viable option in adults.7 The introduction of miniscrews has paved the way in dealing with deep-bite malocclusion. Their availability in different diameters and lengths permits their ease of insertion in different interradicular locations between the maxillary incisor teeth.8 Thus, effective incisor intrusion mechanics could be performed.9 In addition, miniscrews are well established in the literature as an excellent source for anchorage reinforcement with high rates of success and low frequencies of adverse effects.10
Consequently, identifying the plausible effects of miniscrews and other different intrusive mechanics would be of pronounced importance to clinicians. This systematic review was planned to critically evaluate the existing evidence with respect to the effectiveness of miniscrews in intruding the maxillary incisors and subsequently improving deep bites compared with other nonsurgical intrusive mechanics. Their effectiveness was explored through clinically relevant outcomes pertinent to the amount of deep-bite correction, root resorption, genuine incisor intrusion, vertical effect on the maxillary molars, as well as patient-reported outcomes.
MATERIALS AND METHODS
Protocol and Registration
This review was registered a priori in the International Prospective Register of Systematic Reviews (PROSPERO; CRD42018107906). It was conducted and reported according to the Cochrane Handbook of Systematic Reviews of Interventions11 and following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).12
Eligibility Criteria
The PICOS scheme was as follows:
Participants: Orthodontic patients with an increased overbite (≥4 mm), without age or gender predilection
Intervention: Intrusion of the maxillary incisors using orthodontic miniscrews
Comparison: Intrusion of the maxillary incisors using other active treatment mechanics
Outcomes: There were no restrictions on possible data acquisition sources for the primary and secondary outcomes as radiographs, clinical measurements, as well as measurements obtained through dental models were considered; data acquisition through questionnaires for patient-reported outcomes was also considered
Primary Outcome
Amount of overbite correction
Secondary Outcomes
Amount of root resorption
Amount of true incisor intrusion (centroid [Cr] to palatal plane [PP])
Vertical position of the maxillary molars
Patient-reported outcomes
Study Design
We evaluated only randomized controlled trials (RCTs) conducted in humans. Studies with nonrandomized designs, retrospective studies, case reports, and review articles were excluded. Studies with adjunctive surgical procedures and studies evaluating intrusive mechanics applied to the mandibular incisors were excluded.
Information Sources and Literature Search
The search was carried out by two review authors (RS and MR) in multiple electronic databases without any restrictions regarding the language or the publication date up to August 3, 2019. Free-text keywords and database-specific controlled text were used to search the Cochrane Central Register of Controlled Trials (CENTRAL), Embase, Web of Science, MEDLINE, and LILACS. In addition, ongoing and unpublished studies were sought by searching ClinicalTrials.gov, opengrey, the ISRCTN registry, and the ProQuest dissertations and theses database. A hand search was carried out to screen the reference lists of the included articles.
Study Selection
The eligibility of identified studies was initially checked by screening their titles and abstracts. Relevant articles were read in full text and judged against the inclusion/exclusion criteria for a final judgment. The process of study selection was performed by two independent review authors (HM and MR), and conflicts were resolved by contacting a third review author (RS).
Data Collection and Data Items
The process of data extraction was carried out independently by two review authors (RS and HM) using prepiloted data extraction forms. Disagreements were resolved through discussion with a third reviewer (AQ). Data items included the study identification, setting, miniscrew dimensions, applied force levels as well as methods of force delivery, age of participants, intervention and comparative groups, measurement methods, and outcomes. Attempts were made to contact the authors via email correspondence in case clarifications or missing data were required.
Risk of Bias in Individual Trials
Risk-of-bias assessment was performed independently by two review authors (RS and MR). Any disagreement was resolved through a discussion with another review author (HM). The recently modified Cochrane risk-of-bias tool (R.O.B 2.0)13 was used to assess the quality of the included RCTs. The Cochrane tool comprised five assessed domains: bias in the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in the measurement of the outcome, and bias in the selection of the results. A bias judgment of low, high, or presenting with some concerns was rendered based on the following: low risk of bias (all domains were judged as low risk of bias), high risk of bias (at least one domain was judged to be at a high risk of bias or most of the domains presented with some concerns), and some concerns (at least one domain was judged to have some concerns).
Summary Measures and Approach to Data Synthesis
It was considered appropriate to pool the studies if similar interventions and outcomes were presented. Otherwise, qualitative interpretation of the data would have been undertaken. As the amount of incisor intrusion was gauged to vary across populations, age groups, and applied mechanics, an a priori choice of a random-effects model seemed to be reasonable to account for between-study variance. For continuous data, the mean change scores and their standard deviations were pooled, and the standardized mean difference (SMD) was chosen as a summary effect measure along with its 95% confidence interval (CI). Based on recommendations in the Cochrane handbook,11 the SMD was chosen over the mean difference as it accounted for possible differences in scales or radiographic points the studies used for assessing the same respective outcome. The overlap in the 95% CIs was inspected graphically, and the 95% predictive intervals (PrIs) were subsequently calculated if three or more studies were pooled.14 Both absolute and relative between-study heterogeneity was quantified using the tau2 and I2 statistics. Clinical heterogeneity was inspected by looking into the populations, the different interventions, and outcomes. In all cases, the unit of analysis was the individual patient. The level of significance was established as a two-sided P < .05, except for tests of heterogeneity, where it was set at P < .1. Statistical synthesis was undertaken using Comprehensive Meta-Analysis Version 2.2.064 (Biostat Inc, Englewood, NJ).
Additional Analyses
Assessment of reporting biases, “small study” effects, and publication bias were planned to be inspected by Egger's linear regression15 and through contour-enhanced funnel plots if at least 10 RCTs were pooled. Sources of heterogeneity were prespecified to be inspected through mixed-effects subgroup analyses accounting for the following:
Types of intrusion arches
Location of inserted miniscrews
Patient-related characteristics of malocclusion (ie, incisor classification, skeletal pattern)
In addition, sensitivity analyses were prespecified to gauge the effects of individual studies on the overall effect estimate and to isolate the effects of studies judged with an overall low risk of bias. The quality of the resultant evidence was determined through the Grading of Recommendations Assessment, Development and Evaluation (GRADE).16
RESULTS
Study Selection
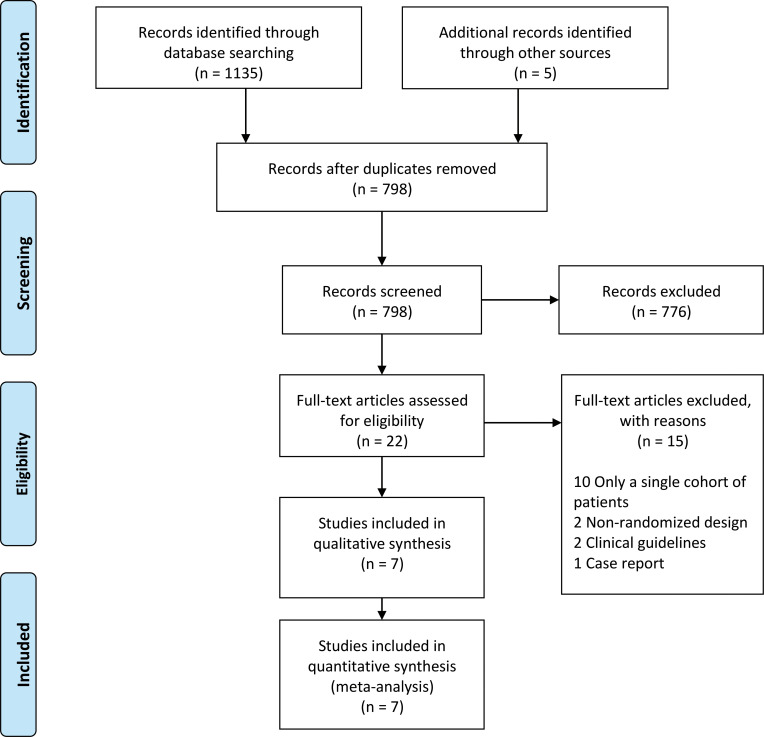
A total of 1140 citations were identified through searches. After removal of duplicates, 798 articles remained and were screened based on their titles and abstracts. A final sample of 22 articles were read in full text, and 7 RCTs subsequently met the inclusion criteria. Table 1 explains the results obtained from the search queries. Figure 1 illustrates the study selection and identification process. The full list of excluded studies and the communication list with authors are available upon request.
Table 1.
Databases and Adopted Search Strategies
| Source (search Conducted up to August 3, 2019, Without Restrictions) |
Hits |
| EMBASE via Ovid (Overbite or deepbite or “deep bite” or Deep-bite or “increased overbite” or “reduced vertical proportions” or “decreased vertical proportions” or “low vertical proportions”) and (“deepbite correction” or “intrusion arch*” or intrusion or “burstone archwire” or “burstone intrusion arch*” or “ricketts utility arch*” or “ricketts intrusion arch*” or “connecticut intrusion arch*” or “intrusion incisors” or “intrusion maxillary incisors” or “maxillary incisors intrusion” or “intrusion upper anterior” or Miniscrew* or mini implant* or mini-implant* or mini-screw* or “orthodontic miniscrew implants” or headgear or “skeletal anchorage” or “temporary anchorage” or “bone anchorage” or “counteractive movements”) and orthodont*).af. | 300 |
| MEDLINE via EBSCOhost (“Overbite” (MESH) or deepbite or “deep bite” or Deep-bite or “increased overbite” or “reduced vertical proportions” or “decreased vertical proportions” or “maxillary incisor*”) and (“orthodontic anchorage procedures” (MESH) or “deepbite correction” or “intrusi*” or “intrusion arch*” or “burstone intrusion arch*” or “ricketts utility arch*” or “utility arch” or “connecticut intrusion arch*” or “J-hook headgear” or “headgear” or “maxillary incisors intrusion” or “extraoral traction appliances (MESH)” or Miniscrew* or mini implant* or mini-implant* or mini-screw* or “orthodontic miniscrew implant” or “skeletal anchorage” or “mini implant anchorage” or “bone anchorage” or “counteractive movements”) | 479 |
Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Library
|
86 |
| LILACS tw:( (tw:((overbite OR deepbite OR “deep bite” OR deep-bite OR “increased overbite” OR “reduced vertical proportions” OR “decreased vertical proportions” OR “low vertical proportions”))) AND (tw:((“deepbite correction” OR “intrusion arch*” OR intrusion OR “burstone archwire” OR “burstone intrusion arch*” OR “ricketts utility arch*” OR “ricketts intrusion arch*” OR “connecticut intrusion arch*” OR “intrusion incisors” OR “intrusion maxillary incisors” OR “maxillary incisors intrusion” OR “intrusion upper anterior” OR miniscrew* OR mini implant* OR mini-implant* OR mini-screw* OR “orthodontic miniscrew implants” OR headgear OR “skeletal anchorage” OR “temporary anchorage” OR “bone anchorage” OR “counteractive movements”))) AND (tw:(orthodont*))) AND (instance:“regional”) AND ( db:(“LILACS”)) | 66 |
| Web of Science TOPIC: ((Overbite OR deepbite OR “deep bite” OR Deep-bite OR “increased overbite” OR “reduced vertical proportions” OR “decreased vertical proportions” OR “low vertical proportions”)) AND TOPIC: ((“deepbite correction” OR “intrusion arch*” OR intrusion OR “burstone archwire” OR “burstone intrusion arch*” OR “ricketts utility arch*” OR “ricketts intrusion arch*” OR “connecticut intrusion arch*” OR “intrusion incisors” OR “intrusion maxillary incisors” OR “intrusion upper anterior” OR Miniscrew* OR mini implant* OR mini-implant* OR mini-screw* OR headgear OR “skeletal anchorage” OR “temporary anchorage” OR “bone anchorage” OR “counteractive movements”)) AND TOPIC: ((orthodont*)) Time span: All years. Indexes: SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, ESCI, CCR-EXPANDED, IC | 199 |
| Other bibliographic databases (ongoing and unpublished literature) ProQuest Dissertation and Thesis database Grey literature (opengrey) Clinical trial registry (ISRCTN registry) Clinicaltrials.gov | 5 |
| Manual searches Reference lists of included articles and relevant reviews | 5 |
| Total | 1140 |
Figure 1.
Diagram presenting the study identification process.
Study Characteristics
Table 2 summarizes the characteristics of the studies included. Seven parallel-group RCTs were included in this review.17–23 All included RCTs were conducted in university settings, with the exception of one study.22 Studies included a total of 202 treated patients with an age range mostly falling between 15 and 22 years. A total of 99 participants were allocated to the miniscrew group, and 95 participants were analyzed after being allocated to the intrusion arch group. Only eight participants were analyzed as part of the J-HG group in one study.19 All studies used a similar amount of applied force level in the intervention as well as the comparative groups. Applied forces ranged between 30–50 g per side. The miniscrews were inserted in two distinct locations: between the maxillary central and lateral incisors and between the maxillary lateral incisors and canines. All articles were published in English, with the exception of one doctoral thesis, which was published in Turkish and subsequently translated.21
Table 2.
Characteristics of the Included Studiesa
| Name |
Setting |
Intervention Group (No. of Participants) |
OMI Diameter/ Length, mm |
OMI Location |
OMI Force Level per Side/ Delivery Method |
Comparison Group (No. of Participants) |
Outcomes |
Measurement Methods |
Age Range, year |
| Gupta et al. (2017)17 | University setting, India | (Absoanchor Dentos, Daegu, Korea) OMIs (12) | 1.3/8 | Between maxillary laterals and canines | 30 g/NiTi coil | Connecticut intrusion arch (12) | Deep-bite correction Incisor position Molar vertical position | Lateral cephalograms | 15–25 |
| Gürlen and Aras (2016)18 | University setting, Turkey | (Ortholution, Seoul, South Korea) OMIs (16) | 1.4/7 | Between maxillary centrals and laterals | 30 g/power chain | Connecticut intrusion arch (16) | Deep-bite correction Root resorption Incisor position | Lateral cephalograms Periapicals | 12.5–16.5 |
| Jain et al. (2014)19 | University setting, India | (Absoanchor Dentos, Daegu, Korea) OMIs (10) | 1.4/6 | Between maxillary centrals and laterals | 40 g/NiTi coil | J-Hook headgear (8) Utility arch (9) | Deep-bite correction Incisor position Molar vertical position | Lateral cephalograms Periapicals Anterior occlusals | 16–22 |
| Kahraman et al. (2017)20 | University setting, Turkey | (Absoanchor Dentos, Daegu, Korea) OMIs (18) | 1.5/6 | Between maxillary laterals and canines | 40 g/NiTi coil | Connecticut intrusion arch (16) | Molar vertical position | 3D lateral cephalograms | NA |
| Karagöz et al. (2013)21 | University setting, Turkey | (DEWIMED) OMIs (13) | 1.4/8 | Between maxillary centrals and laterals | 50 g/ NiTi coil | Burstone Intrusion arch (12) | Deep-bite correction Root resorption Incisor position Molar vertical position | 3D lateral cephalograms 3D panoramic views | >15 |
| Kumar et al. (2017)22 | Dental center, India | (Absoanchor Dentos, Daegu, Korea) OMIs (15) | 1.3/7 | Between maxillary centrals and laterals | 30 g/power chain | Connecticut intrusion arch (15) | Incisor position Molar vertical position | Lateral cephalograms | 15–20 |
| Şenışık and Türkkahraman (2012)23 | University setting, Turkey | (Absoanchor Dentos, Daegu, Korea) OMIs (15) | 1.3/5 | Between maxillary laterals and canines | 35–50 g/NiTi coil | Connecticut intrusion arch (15) Control group (15) | Deep-bite correction Incisor position Molar vertical position | Lateral cephalograms Panoramic views | >15 |
OMI indicates orthodontic miniscrew implant; NiTi, nickel-titanium.
Risk of Bias Within Individual Studies
All included studies were judged to have an overall high risk of bias (Table 3). Several shortcomings were observed because of the lack of adequate randomization methods, absence of outcome assessment blinding, and suspicion of selective reporting due to lack of reporting on adverse effects and important outcomes expected from such trials.
Table 3.
Risk of Bias in Included Studies
| Gupta et al. (2017)17 |
Gürlen and Aras (2016)18 |
Jain et al. (2014)19 |
Kahraman et al. (2017)20 |
Karagöz et al. (2013)21 |
Kumar et al. (2017)22 |
Şenışık and Türkkahraman (2012)23 |
|
| Bias in randomization | High | Some concerns | Some concerns | High | High | Some concerns | High |
| Bias due to deviations from intended intervention | Low | Low | Some concerns | Low | High | Low | Low |
| Bias due to missing data | Low | Low | Low | Some concerns | Low | Low | Low |
| Measurement of outcome | Some Concerns | Low | High | High | High | Some concerns | High |
| Selection of result | High | High | High | High | Some concerns | High | High |
| Overall bias | High | High | High | High | High | High | High |
Results of Individual Studies and Data Synthesis
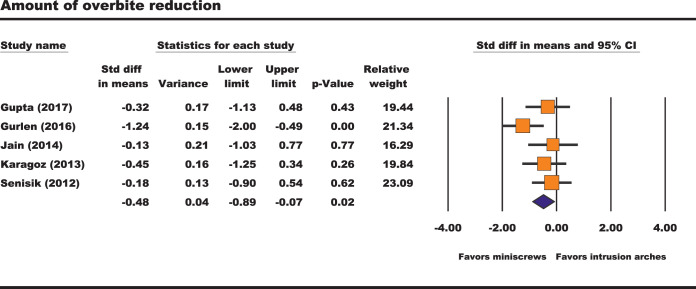
Amount of deep-bite correction.
The amount of deep-bite correction was statistically pooled from five RCTs. A statistically significant SMD was noted favoring a higher amount of deep-bite reduction in the miniscrew group when compared with the intrusion arch group (SMD, −0.48; 95% CI, −0.89 to −0.07; 95% PrI, −1.45 to 0.49; I2, 24%; tau2, 0.05; 5 RCTs; Figure 2). One small study19 compared the amount of deep-bite correction between the miniscrews and J-HG. A statistically significant mean difference of −1.5 mm (P = .025) was deduced favoring improved reduction in the deep bite for the miniscrew group.
Figure 2.
Forest plot of the amount of deep-bite correction.
Root resorption (amount of root length changes).
Changes in root length were assessed in only two of the included RCTs analyzing data derived from 57 participants.18,21 Exploratory quantitative synthesis of linear root length changes observed from two-dimensional radiographs indicated no statistically significant differences in the amount of root resorption between the miniscrew group and the intrusion arch group as seen in the UR1 (SMD, −0.53; 95% CI, −1.09 to 0.04; I2, 11%; tau2, 0.02; 2 RCTs), UL1 (SMD, −0.41; 95% CI, −1.13 to 0.32; I2, 46%; tau2, 0.13; 2 RCTs), UR2 (SMD, −0.42; 95% CI, −1.02 to 0.19; I2, 23%; tau2, 0.04; 2 RCTs), and UL2 (SMD, −0.41; 95% CI, −1.04 to 0.23; I2, 30%; tau2, 0.06; 2 RCTs).
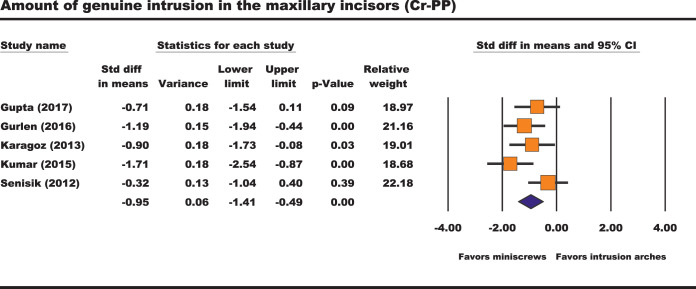
Amount of true incisor intrusion (Cr-PP).
Five RCTs were pooled to assess the amount of true incisor intrusion between the miniscrew and the intrusion arch groups. A statistically significant difference favored more true incisor intrusion in the miniscrew group (SMD, −0.95; 95% CI, −1.41 to −0.49; 95% PrI, −2.2 to 0.3; I2, 41%; tau2, 0.11; 5 RCTs; Figure 3).
Figure 3.
Forest plot of the amount of incisor intrusion (Cr-PP).
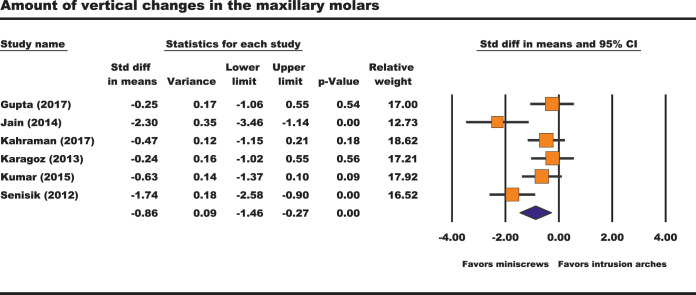
Amount of vertical changes in the maxillary molars.
Six RCTs addressed the amount of extrusion in the maxillary molars in the miniscrew group compared with the intrusion arch. Less extrusive molar movement was noted in the miniscrew group (SMD, −0.86; 95% CI, −1.46 to −0.27; 95% PrI, −3.2 to 1.5; I2, 68%; tau2, 0.61; 6 RCTs; Figure 4). In one small RCT,19 the amount of extrusion of the maxillary molars was not statistically significant between the J-HG group and the miniscrew group, with a mean difference of 0.2 mm (P = .5).
Figure 4.
Forest plot of the amount of molar extrusion.
Patient-Reported Outcomes
Patient-reported outcome is not a specific outcome but a category of many outcomes. However, under this wide domain, none of the included RCTs reported on patients' perception of their treatment, satisfaction, or preference regarding the intrusive mechanics used.
Additional Analyses
Assessment of reporting biases, “small study” effects, and publication bias were not accomplished as the number of included studies was limited. In addition, sensitivity analyses gauging the effect of low risk-of-bias studies could not be performed because of the absence of high-quality RCTs. However, sensitivity analyses exploring the impact of individual studies on the overall effect estimates did not seem to significantly influence the effect size estimates (Figures 5 and 6). A detailed presentation of the performed primary and subgroup analyses is presented (Table 4).
Figure 5.
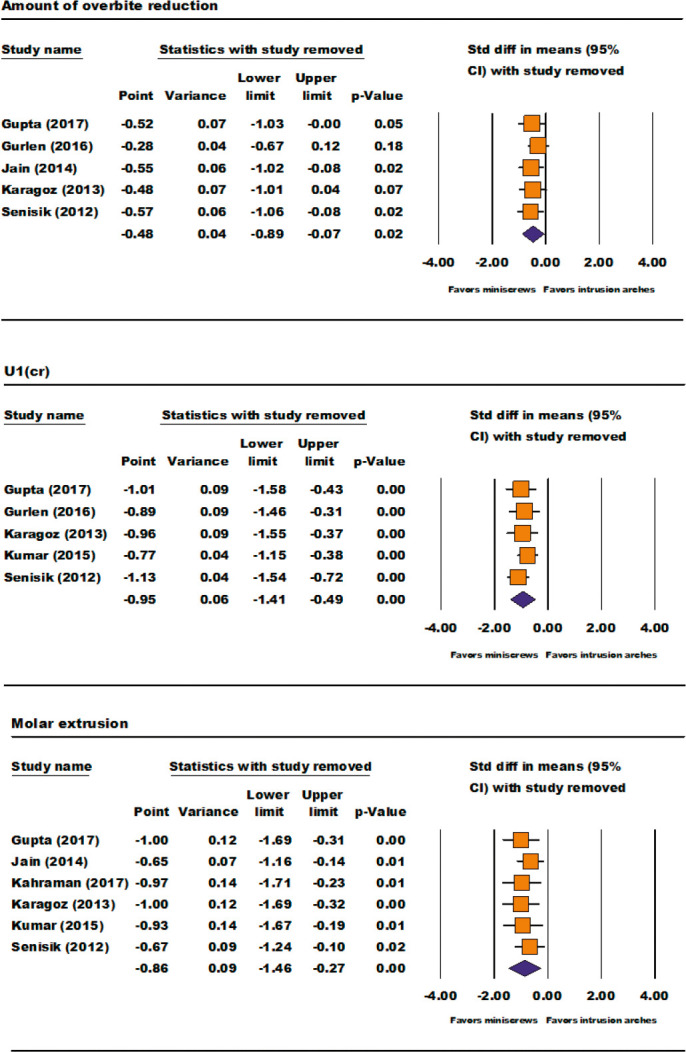
Sensitivity analyses.
Figure 6.
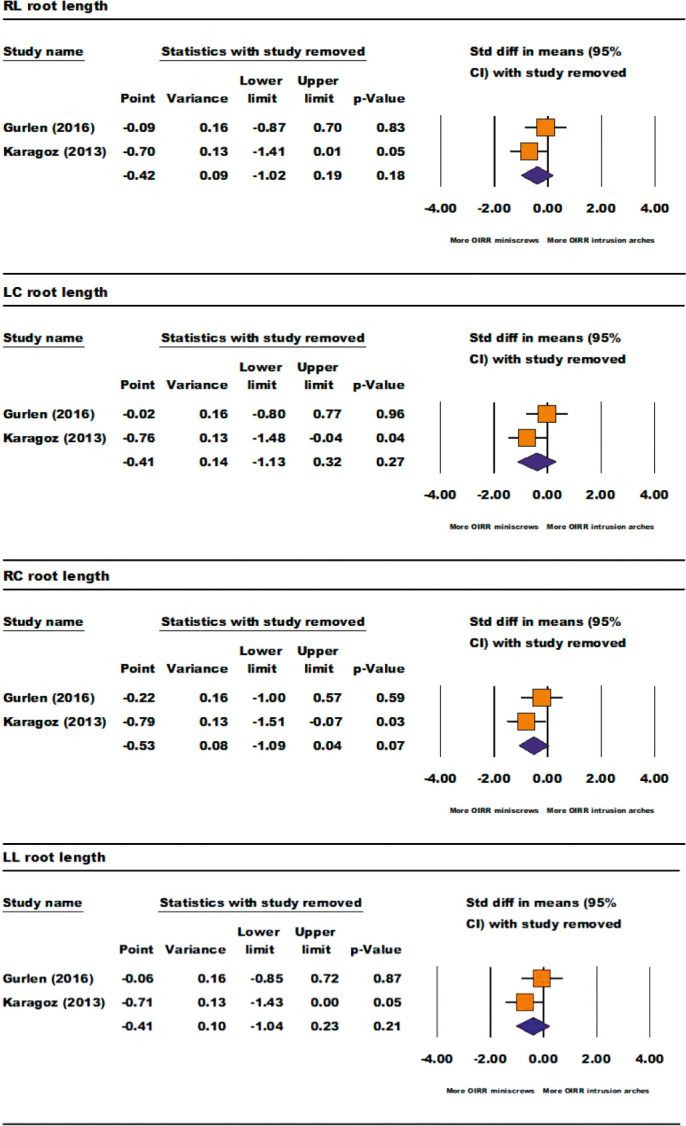
Sensitivity analyses of the amount of root length loss (OIRR: Orthodontically induced root resorption).
Table 4.
Detailed Results From Primary and Subgroup Analysesa
| Analysisb |
Ncomp |
SMD |
95% CI |
P |
| Deep-bite correction | ||||
| All studies (REM) | 5 | −0.48 | −0.89 to −0.07 | |
| Subgroup analyses (MEA) | ||||
| Location of miniscrews | .36 | |||
| Maxillary lateral and canine | 2 | −0.24 | −0.78 to 0.30 | |
| Maxillary central and lateral | 3 | −0.64 | −1.3 to 0.01 | |
| Type of intrusion arch | .73 | |||
| CIA | 3 | −0.58 | −1.24 to 0.08 | |
| BIA | 1 | −0.45 | −1.25 to 0.34 | |
| UA | 1 | −0.13 | −1.03 to 0.77 | |
| Root resorption (REM) | ||||
| Maxillary right central incisor | 2 | −0.53 | −1.09 to 0.04 | |
| Maxillary left central incisor | 2 | −0.41 | −1.13 to 0.32 | |
| Maxillary right lateral incisor | 2 | −0.42 | −1.02 to 0.19 | |
| Maxillary left lateral incisor | 2 | −0.41 | −1.04 to 0.23 | |
| True incisor intrusion | ||||
| All studies (REM) | 5 | −0.95 | −1.41 to −0.49 | |
| Subgroup analyses (MEA) | ||||
| Location of miniscrews | .035* | |||
| Maxillary lateral and canine | 2 | −0.49 | −1.03 to 0.06 | |
| Maxillary central and lateral | 3 | −1.26 | −1.72 to −0.8 | |
| Type of intrusion arch | .9 | |||
| CIA | 4 | −0.96 | −1.55 to −0.37 | |
| BIA | 1 | −0.9 | −1.73 to − 0.08 | |
| Vertical movement in maxillary molar | ||||
| All studies (REM) | 6 | −0.86 | −1.46 to −0.27 | |
| Subgroup analyses (MEA) | ||||
| Location of miniscrews | .8 | |||
| Maxillary lateral and canine | 3 | −0.8 | −1.67 to 0.06 | |
| Maxillary central and lateral | 3 | −0.97 | −2.02 to 0.08 | |
| Type of intrusion arch | .015* | |||
| CIA | 4 | −0.75 | −1.36 to −0.15 | |
| BIA | 1 | −0.24 | −1.02 to 0.55 | |
| UA | 1 | −2.3 | −3.46 to −1.14 | |
BIA indicates Burstone intrusion arch; CI, confidence interval; CIA, Connecticut intrusion arch; MEA, mixed-effects subgroup analyses; P, test for between-subgroup heterogeneity; REM, random-effects meta-analysis; SMD, standardized mean difference; UA, utility arch.
Subgroup analyses for specific malocclusion characteristics could not be performed as individual studies did not adequately report on these aspects.
Significant at P < .05.
Quality of Evidence
According to the GRADE approach, very low to low quality of evidence for the explored outcomes is expected. Evidence was mainly downgraded because of shortcomings in the methodological quality of included RCTs. A detailed explanation is presented in Table 5.
Table 5.
GRADE Approach: Miniscrews vs Intrusion Arches
| Certainty Assessment |
Summary of Findings |
||||||||||
| No. of Participants (Studies) and Follow-up |
Risk of Bias |
Inconsistency |
Indirectness |
Imprecision |
Publication Bias |
Overall Certainty of Evidence |
Study Event Rates |
Relative Effect (95% CI) |
Anticipated Absolute Effects |
||
| With Intrusion Arches |
With Miniscrews |
Risk with Intrusion Arches |
Risk Difference With Miniscrews |
||||||||
| Deep-bite correction (assessed with: mm) | |||||||||||
| 130 (5 RCTs) | Very seriousa | Not serious | Not serious | Not serious | None | ⊕⊕○○ LOW | 64 | 66 | — | — | SMD 0.48 SD lower (0.89 lower to 0.07 lower) |
| Root length loss (follow-up: median 4 mo; assessed with: mm) | |||||||||||
| 57 (2 RCTs) | Very seriousa | Not serious | Not serious | Seriousb | None | ⊕○○○ VERY LOW | 28 | 29 | — | — | SMDc ranges from 0.41 to 0.53 SD lower |
| Genuine incisor intrusion (assessed with: mm [Cr to PP]) | |||||||||||
| 141 (5 RCTs) | Very seriousa | Not serious | Not serious | Not serious | None | ⊕⊕○○ LOW | 70 | 71 | — | — | SMD 0.95 SD lower (1.41 lower to 0.49 lower) |
| Amount of vertical movements in the maxillary molars (assessed with: mm) | |||||||||||
| 162 (6 RCTs) | Very seriousa | Seriousd | Not serious | Not serious | None | ⊕○○○ VERY LOW | 80 | 82 | — | — | SMD 0.86 SD lower (1.46 lower to 0.27 lower) |
Downgraded two levels for risk of bias within all included RCTs.
Downgraded one level for low number of included trials.
SMD values denote only the highest and lowest observations. Detailed results are presented in Table 4.
Downgraded one level for statistical heterogeneity.
DISCUSSION
This review provided an insight into the effectiveness of miniscrews in correcting deep bites. No previous systematic reviews addressed the plausible effects of miniscrews or intrusion arches in participants with deep overbites. Hence, the qualitative and quantitative interpretation of the results pertinent to this review would be of great clinical value.
According to quantitative synthesis, miniscrews had a greater overall effect on reducing overbites than did the intrusion arches. Similarly, Aydoğdu and Özsoy24 found that miniscrews resulted in a similar amount of deep-bite correction compared with conventional utility arches during intrusion of mandibular incisors. However, they had to place their miniscrews in a strictly narrower interradicular space between the mandibular incisors; thus, some difficulties might have been expressed in sustaining the miniscrews.25
The amount of true intrusion of the maxillary incisors assessed by the distance between the Cr and the PP was found to be statistically significant favoring miniscrews. In this context, Deguchi and colleagues4 explained that miniscrews produce more true intrusion as the force is applied closer to the center of resistance, and this might be attributed to the location of the inserted miniscrews as well as the direction and magnitude of the intrusion forces, since light-controlled forces result in more efficient intrusion. This hypothesis was further tested in this review, as the exploratory subgroup analyses denoted more genuine incisor intrusion when the miniscrews were placed bilaterally between the maxillary central and lateral incisors.
It was not surprising that the pooled results showed less extrusive effects on the maxillary molars in the miniscrew group. This proved that the modes of action of the two intrusive mechanics were dissimilar. The mode of action of miniscrews mainly targeted dentoalveolar effects on the incisors, while the mode of action of the intrusion arches involved both intruding the incisors and extruding the posterior molars.26,27 In a clinical situation, a combination of dentoalveolar effects on both the molars and the incisors could be beneficial in young subjects without excessive gingival show. However, in adult subjects with gummy smiles, miniscrews might be a more appropriate method of nonsurgical deep-bite correction. However, transpalatal arches were recommended to minimize the plausible extrusive effects on the maxillary molars.28
In addition, two studies18,21 reported on changes in root length. Both studies reported an average linear loss of root length of about 1 mm. The pooled results did not indicate a statistically significant difference between the miniscrew and intrusion arch groups. These results presented the expected values of root length loss during a 4-month period18 and up until the end of the intrusion phase.21 Thus, these results should be interpreted with caution, as the progression of these adverse root length changes through a full course of orthodontic treatment involving the intrusion of the maxillary incisors is yet unknown. Intruded teeth showed no signs of loss of tooth vitality. As a consequence, loss of tooth vitality did not seem to be related to the method of intrusion but may be more directly associated with the force magnitude, as uncontrolled forces may be the main reason in occluding the capillary blood flow. Taking this into account, it is emphasized that potential anatomical restrictions restrict the use of miniplates in the anterior maxillary region,29 thus promoting miniscrews as the primary source of skeletal anchorage for intruding the maxillary incisors.
Only one small RCT compared miniscrew anchorage to the J-HG.19 According to that trial, miniscrews resulted in a favorable effect on deep-bite reduction when compared with the J-HG. Those results were not in agreement with a prospective nonrandomized trial that concluded that there were no significant differences between the two intrusion methods.4 This might be explained by differences in the magnitude and direction of forces between those two studies. In addition, no significant differences were noted between both groups with regard to the amount of extrusive effects on the maxillary molars, which could possibly be attributed to the lack of study power and methods of J-HG adjustment.
Recommendations for Future Research
Future RCTs should be powered to detect differences between the intervention groups through a priori sample size calculation. Authors are encouraged to comprehensively report on all possible outcomes and associated side effects. Prospective RCTs should be designed to address the full course of orthodontic treatment and to include a follow-up period to determine the stability of overbite correction. Future reviews are encouraged to explore intrusion effects on the mandibular incisors and to focus on the possible inclination changes in the maxillary incisors, as well as the possible effects of extruding the molars on vertical skeletal dimensions. Also, it would be important to assess whether a relationship exists between overbite reduction and molar extrusion, as well as to determine whether the amount of overjet reduction and overall length of treatment correlate with the amount of root length change recorded.
Strengths and Limitations
This review attempted to analyze systematically the contemporary literature regarding a clinically relevant topic in orthodontic practice. Wide and unrestricted searches for all eligible studies were undertaken with comprehensive qualitative and quantitative reporting on the review outcomes. It is acknowledged that there were methodological shortcomings observed within the RCTs included. In turn, this reduced the level of confidence in the conclusions and resulted in an overall very low to low quality of evidence, clouding the conclusions with a degree of uncertainty. Thus, definitive recommendations for clinical practice could not be provided. In addition, patient-reported outcomes could not be addressed, since the included studies did not adequately explore this area. Results related to the long-term stability of deep-bite correction and expected root resorption throughout a full course of treatment were not investigated in the included studies.
CONCLUSIONS
Very low to low quality of evidence indicated that miniscrews were more effective in intruding the maxillary incisors and correcting deep bites.
The effectiveness of miniscrews in correcting deep bites seems to be associated with a greater degree of genuine maxillary incisor intrusion and less extrusive effects on the maxillary molars.
Regardless of the intrusive mechanics used, the maxillary incisors seem to exhibit some degree of root resorption during their intrusion phase.
Future long-term and well-designed RCTs are still required to elaborate on this important clinical subject.
REFERENCES
- 1.Nielsen IL. Vertical malocclusions: etiology, development, diagnosis and some aspects of treatment. Angle Orthod. 1991;61:247–260. doi: 10.1043/0003-3219(1991)061<0247:VMEDDA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Kaushik A, Sidhu M, Grover S, Kumar S. Comparative evaluation of intrusive effects of miniscrew, Connecticut intrusion arch, and utility intrusion arch—an in vivo study. Journal of Pierre Fauchard Academy (India Section) 2015;29:69–76. [Google Scholar]
- 3.Raj A, Acharya SS, Mohanty P, et al. Comparison of intrusive effects of mini screws and Burrstone intrusive arch: a radiographic study. Adv Hum Biol. 2015;5:49–55. [Google Scholar]
- 4.Deguchi T, Murakami T, Kuroda S, Yabuuchi T, Kamioka H, Takano-Yamamoto T. Comparison of the intrusion effects on the maxillary incisors between implant anchorage and J-hook headgear. Am J Orthod Dentofacial Orthop. 2008;133:654–660. doi: 10.1016/j.ajodo.2006.04.047. [DOI] [PubMed] [Google Scholar]
- 5.Proffit WR, Fields HW, Sarver DM. Contemporary orthodontics e-book. Philadelphia, Penn: Elsevier Health Sciences; 2018. [Google Scholar]
- 6.Nanda R. Esthetics and Biomechanics in Orthodontics. Philadelphia, Penn: Elsevier Health Sciences; 2015. [Google Scholar]
- 7.Burstone CR. Deep overbite correction by intrusion. Am J Orthod Dentofacial Orthop. 1977;72:1–22. doi: 10.1016/0002-9416(77)90121-x. [DOI] [PubMed] [Google Scholar]
- 8.Mohammed H, Wafaie K, Rizk MZ, Almuzian M, Sosly R, Bearn DR. Role of anatomical sites and correlated risk factors on the survival of orthodontic miniscrew implants: a systematic review and meta-analysis. Prog Orthod. 2018;19:36. doi: 10.1186/s40510-018-0225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goel P, Tandon R, Agrawal KK. A comparative study of different intrusion methods and their effect on maxillary incisors. J Oral Biol Craniofac Res. 2014;4:186–191. doi: 10.1016/j.jobcr.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Papageorgiou SN, Zogakis IP, Papadopoulos MA. Failure rates and associated risk factors of orthodontic miniscrew implants: a meta-analysis. Am J Orthod Dentofacial Orthop. 2012;142:577–595. doi: 10.1016/j.ajodo.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 11.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0. London, UK: The Cochrane Collaboration; 2011. [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 13.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 14.IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6:e010247. doi: 10.1136/bmjopen-2015-010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta N, Tripathi T, Rai P, Kanase A. A comparative evaluation of bite opening by temporary anchorage devices and Connecticut intrusion arch: an in vivo study. Int J Orthod Rehabil. 2017;8:129–135. [Google Scholar]
- 18.Gürlen SÖ, Aras I. Comparison of the treatment effects of two intrusive mechanics: Connecticut intrusion arch and mini-implant. Turkiye Klinikleri. Dishekimligi Bilimleri Dergisi. 2016;22:195–201. [Google Scholar]
- 19.Jain RK, Kumar SP, Manjula WS. Comparison of intrusion effects on maxillary incisors among mini implant anchorage, J-hook headgear and utility arch. J Clin Diagn Res. 2014;8:21–24. doi: 10.7860/JCDR/2014/8339.4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kahraman F, Kilic N, Dagsuyu İM. Farklı Kesici İntrüzyon Mekaniklerinin Daimi Üst Birinci Molar Dişlere Etkilerinin Üç Boyutlu Olarak Değerlendirilmesi. Cumhuriyet Dental Journal. 2017;20:113–121. [Google Scholar]
- 21.Karagöz A. Derin Örtülü Kapanışlı Olgularda Üst Keser Intrüzyonunun Konik Işınlı Bilgisayarlı Tomografi ile İncelenmesi. 2013 Available at: openaccess.hacettepe.edu.tr Accessed August 1, 2019.
- 22.Kumar P, Datana S, Londhe SM, Kadu A. Rate of intrusion of maxillary incisors in Class II Div 1 malocclusion using skeletal anchorage device and Connecticut intrusion arch. Med J Armed Forces India. 2017;73:65–73. doi: 10.1016/j.mjafi.2015.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Şenışık NE, Türkkahraman H. Treatment effects of intrusion arches and mini-implant systems in deepbite patients. Am J Orthod Dentofacial Orthop. 2012;141:723–733. doi: 10.1016/j.ajodo.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 24.Aydoğdu E, Özsoy Ö. Effects of mandibular incisor intrusion obtained using a conventional utility arch vs bone anchorage. Angle Orthod. 2011;81:767–775. doi: 10.2319/120610-703.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ludwig B, Glasl B, Kinzinger GS, Lietz T, Lisson JA. Anatomical guidelines for miniscrew insertion: vestibular interradicular sites. J Clin Orthod. 2011;45:165–173. [PubMed] [Google Scholar]
- 26.Tripathi T, Gupta N, Rai P, Kanase Neha A. A comparative evaluation of bite opening by temporary anchorage devices and Connecticut intrusion arch: an in vivo study. Int J Orthod Rehabil. 2017;8:129–135. [Google Scholar]
- 27.Kim T, Kim H, Lee S. Correction of deep overbite and gummy smile by using a miniimplant with a segmented wire in a growing Class II Division 2 patient. Am J Orthod Dentofacial Orthop. 2006;130:676–685. doi: 10.1016/j.ajodo.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 28.Nayak U, Goyal V, Godhrawala F, Saxena R. Comparison of skeletodental changes occurring during deep overbite correction with mini-implant anchorage system and the utility arches reinforced by a transpalatal arch. Journal of Indian Orthodontic Society. 2011;46:9–14. [Google Scholar]
- 29.Cornelis MA, Scheffler NR, Nyssen-Behets C, De Clerck HJ, Tulloch JC. Patients' and orthodontists' perceptions of miniplates used for temporary skeletal anchorage: a prospective study. Am J Orthod Dentofacial Orthop. 2008;133:18–24. doi: 10.1016/j.ajodo.2006.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]