Abstract
Background
Antipsychotic medications are used to address neuropsychiatric symptoms associated with dementia. Evidence suggests that among older adults with dementia, their harms outweigh their benefits. A quality improvement initiative was conducted to address inappropriate antipsychotic medication use in long-term care (LTC) in the province of Alberta.
Methods
We conducted a multimethod evaluation of the provincial implementation of the project in 170 LTC sites over a 3-year project period incorporating a quasi-experimental before–after design. Using a three-component intervention of education and audit and feedback delivered in a learning workshop innovation collaborative format, local LTC teams were supported to reduce the number of residents receiving antipsychotic medications in the absence of a documented indication. Project resources were preferentially allocated to supporting sites with the highest baseline antipsychotic medication use. Changes in antipsychotic medication use, associated clinical and economic outcomes, and the effects of the project on LTC staff, physicians, leaders and administrators, and family members of LTC residents were assessed at the conclusion of the implementation phase.
Results
The province-wide initiative was delivered with a 75% implementation fidelity. Inappropriate antipsychotic medication use declined from 26.8% to 21.1%. The decrease was achieved without unintended consequences in other outcomes including physical restraint use or aggressive behaviours. The project was more expensive but resulted in less inappropriate use of antipsychotics than the pre-project period (incremental cost per inappropriate antipsychotic avoided of $5 678.71). Accounts from family, organisational leaders, and LTC staff were supportive of the project activities and outcomes.
Conclusion
This quality improvement initiative was successfully delivered across an entire delivery arm of the continuing care sector. Quality of care in LTC was improved.
Keywords: quality improvement, collaborative, breakthrough groups, nursing homes, PDSA, performance measures
Introduction
Residential long-term care (LTC) serves approximately 15 500 older adults in the province of Alberta, of whom approximately 59% have been diagnosed with dementia or Alzheimer’s disease.1 2 Neuropsychiatric symptoms (NPS), such as agitation or aggression, are common.3 4 Antipsychotic medications are widely used to treat behaviours associated with NPS.5 6 Evidence shows that their associated risks may outweigh any potential benefits, such as the sedating effects for residents, worsened NPS and increased risk of falls, as well as the risk of serious adverse events including stroke and death.7–9
In this situation, antipsychotic medications can be withdrawn safely without detrimental outcomes.10 National and international efforts motivated by growing clinical consensus and public recognition that this is the right course of action have gained traction and align with resident-focused care.11 12 However, practice change requires support to be effective particularly in the resource-constrained environment of LTC.13 Ensuring a shared understanding of the risks associated with antipsychotic use and providing alternative strategies for managing responsive behaviours may facilitate non-pharmacological resident-focused dementia care. This paper describes the outcome of a provincial quality improvement initiative to decrease antipsychotic medication use among LTC residents in Alberta.
Methods
Context
We conducted a multimethod evaluation of the implementation of the Appropriate Use of Antipsychotics (AUA) quality improvement initiative. The initiative worked with local LTC teams to decrease antipsychotic medication use in the absence of a documented indication. A total of 170 LTC sites were included, with 11 early adopter sites taking part in a learning phase prior to spread to the remaining 159 sites in Alberta. The 3-year initiative began with a project planning and design phase to begin raising awareness of the potential risks associated with antipsychotic medication use among LTC leaders and organisational decision-makers, develop project resources, and identify and assess readiness of interested early adopter sites. The quality improvement intervention and implementation strategy are described in turn below.
Intervention
The three-component intervention consisted of staff education and audit and feedback of local data.14 15 Education aimed to increase knowledge and skills to reduce the number of residents receiving an antipsychotic medication. Change activity supported teams to conduct monthly medication reviews, complying with Alberta Health Continuing Care Health Service Standards.16 17 Education supported use of behaviour mapping, non-pharmacological strategies for the management of responsive behaviours and protecting sleep. Audit and feedback of medication reviews and number of residents receiving antipsychotic medications were tracked by a practice lead to support team progress. The practice lead also supported sites to manage challenges with resident behaviours without drugs.
Implementation strategy
The implementation strategy started with 11 early adopter sites to finalise process and materials prior to scaling up the intervention. Subsequent waves of 10–12 LTC teams were incorporated until the intervention had been delivered to 170 sites. Sites with the highest antipsychotic medication use (≥25%) were invited to participate in a collaborative learning model, as championed by the Institute for Healthcare Improvement to deliver large-scale quality improvement targeting a shared aim.18 The collaborative model consisted of three group learning workshops (LWs) spread over 9 months, with action periods between workshops in which frontline teams pursued plan–do–study–act quality improvement cycles to implement and test changes.19 20 Sites with antipsychotic medication use <25% received half-day education sessions and orientation to the available project resources.
Data sources and analysis
We assessed changes in antipsychotic medication use, associated clinical, economic and implementation outcomes, and the effects of the project on LTC staff, physicians, leaders and administrators, and resident’s family members. Residents, family, or the public were not involved in the design or conduct of the evaluation beyond their contribution as participants. Interviews with resident’s family members underwent a project ethics assessment and second-opinion review to consider and minimise ethical risks (https://albertainnovates.ca/programs/arecci/). Data were handled following best-practice standards.
Resident Assessment Instrument repository analytics
We investigated change in resident outcomes using data collected as part of the Resident Assessment Instrument-Minimum Data Set (RAI-MDS 2.0), (https://www.interrai.org) routinely collected for LTC residents in Alberta,21 in a quasi-experimental before–after design. The key performance indicator was the risk-adjusted quality indicator (QI) for the per cent of residents on antipsychotics without a documented indication (DRG01).22–24 The numerator of this QI included residents who received an antipsychotic medication in the 7 days prior to their assessment, and the denominator excluded residents with schizophrenia, Huntington’s chorea, delusions/hallucinations, or at end of life.25 The risk-adjustment process uses statistical methods to control for population differences, both at the resident level through covariate adjustment and at the facility level by stratification and reweighting of data, in order to support fair comparisons of quality of care across different facilities/organisations.26 Balancing measures were selected to ensure that the project did not result in unintended harm. These included the risk-adjusted QIs for residents with symptoms of delirium (DEL0X), falls in the past 30 days (FAL02) and pain (PAI0X). The indicators for physical restraint use excluding those who are quadriplegic (RES01) and the Aggressive Behaviour Scale (ABS), a summary score of the number and frequency of verbal and physical abuse, socially inappropriate or disruptive behaviour, and resistance to care, were also monitored. Other outcomes included hip and other fractures in the past 180 days and acute care health service utilisation (per cent of residents with 1+ hospital admission or emergency department (ED) visit in the past 90 days). Time points included the pre-project baseline (FY2011–2012 Q4) and the conclusion of implementation (FY2014–2015 Q4). The baseline time period was selected to reflect the pre-project state, prior to announcement of the provincial focus on reducing inappropriate antipsychotic medication use and associated awareness raising and readiness activities.
Economic evaluation
The economic evaluation assessed cost-effectiveness compared with pre-project usual care. A simple decision tree model compared: implementation of the AUA Project versus usual care for seniors with dementia and NPS at baseline and follow-up. The primary outcome measure was the incremental cost per episode of inappropriate antipsychotic use avoided. The healthcare system payer perspective was adopted. All resources and costs associated with implementation, borne by the provincial healthcare organisation (Alberta Health Services), were included. Costs borne by LTC facilities, residents and families were excluded.
Clinical events and costs considered in the analysis are listed in the supplemental file. Clinical events (online supplemental table S1) included the unadjusted probabilities of inappropriate antipsychotic use (DRG01; unadjusted to include the absolute number of residents inappropriately prescribed antipsychotics), improvement in NPS (defined as a minimum 1-point decrease in ABS score), and ED visits and hospitalisations. Due to data limitations, it was not possible to determine whether or not those who had ED visits or were hospitalised experienced improvement in NPS. Resources and costs considered in the economic evaluation included the costs of implementation, inappropriate antipsychotic use (estimated per resident, per day), ED visits and hospitalisations (online supplemental table S2). Overall budgetary impact was based on project costs and cost-savings from reductions in antipsychotic use and assumed that the total population of residents (n=14 474) was the same before and after the project, and equal to the total number of Alberta’s LTC residents.
bmjoq-2020-001211supp001.pdf (746.1KB, pdf)
Clinical event data for before and after implementation were in aggregate form for each LTC site, thus it was not possible to determine the number of residents with dementia and NPS, identify specific intervention exposed residents at the unit level, nor to track project-related resident-level changes in clinical outcomes. It was assumed that the total number of beds was equal to the total number of participants in the project and that the entire cohort had dementia and exhibited NPS.
Uncertainty in the model was addressed by deterministic and probabilistic sensitivity analyses. One-way sensitivity analyses were performed for the probability of inappropriate antipsychotic use, project costs and the cost per ED visit which were varied by ±50% of the average calculated estimate; the probabilities of ED visits and hospitalisations which were varied individually within their respective 95% CI; and the cost of hospitalisation which was varied based on minimum and maximum values provided by the Canadian Institute for Health Information (CIHI) patient cost estimator. Scenario analysis estimated cost-effectiveness of the AUA Project including estimated in-kind costs borne by LTC facilities to implement non-pharmacological interventions (eg, therapeutic garden at $212.25 per resident). Probabilistic sensitivity analysis was conducted to reflect the uncertainty surrounding the point values for the cost of inappropriate antipsychotic use and cost of ED visits and hospitalisations, where probabilities were simultaneously varied 10 000 times according to their distributions.
Family member interviews
Qualitative, structured telephone interviews allowed collection of perceptions of resident quality of life and experiences of having a loved one with dementia in LTC. The interview guide explored family member involvement in decision-making about the use of antipsychotic medications and observations of project outcomes.
Family members of residents with a dose reduction/discontinuation of antipsychotic medications were identified by site champions (whether or not the reduction/discontinuation was successful) and invited by recruitment letter. Interviews were audio recorded, transcribed and analysed by the team leads with an inductive approach using NVivo V.11 qualitative data analysis software27 following thematic analysis.28
LTC site and organisational leader survey
An online survey, using Select Survey29 gained feedback from organisational leaders/administrators on implementation and outcomes at their site(s). An invitation to participate was circulated to 122 sites and organisational leaders, with a reminder email sent mid-way through the 3-week data collection period. The invitation included a request to forward the survey invitation and link to other leaders in their organisation or area. Responses were analysed using SPSS V.23.0.30
LTC staff and physician survey
The survey collected feedback on perceived project resource requirements and associated outcomes and was conducted by both Select Survey and paper formats. Snowball sampling was used, with three AUA practice leads sending approximately 128 LTC site champions an email invitation to participate, with a follow-up email reminder sent approximately 1 week after the initial email invitation (early adopter sites or sites without a site champion were excluded). Champions were asked to forward or distribute the survey invitation to staff and physicians at their site. Recruitment remained open for 12 weeks.
Results
Implementation
Sites were intended to receive the LWs incorporating audit and feedback or education session based on their baseline antipsychotic medication use. Due to site, leader and organisational preferences, 26 sites designated to receive education sessions opted for the LWs, while 17 sites designated to receive LWs opted for education sessions, thus 127 sites (75%) received the intervention delivery type as planned. Additional project variation included intervention dose (length of LWs (6 hours), education sessions (2–4 hours), and number of LW attended by team members (range 1–3)), mode of delivery of the session (face-to-face or virtual), and timing of implementation (delayed in 46 sites due to leadership vacancies and local readiness to implement).
In total 119 (70%) sites took part in the LW approach, with 93 (78%) operating at the facility level while 26 (22%) undertook unit level implementation. Forty-six sites (27%) took part in the less resource-intensive education sessions. At least 554 unique LTC staff across the province participated in the LWs and education sessions. Five sites (3%) did not participate at all but were sent project information via email. All sites were notified of the project resources (available at: https://www.albertahealthservices.ca/scns/auatoolkit.aspx) through the LWs, education sessions or by email.
RAI repository analytics
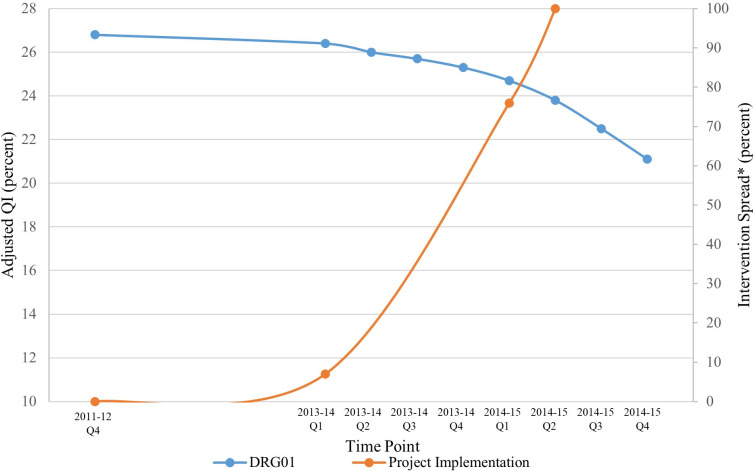
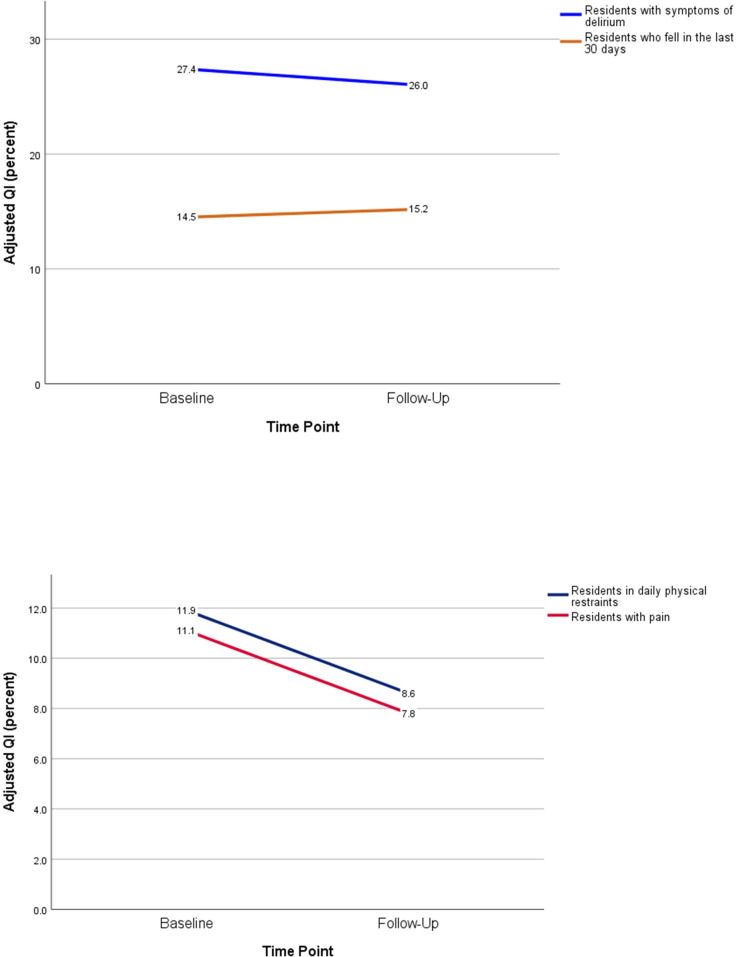
Over the course of the project, there was a decrease in the proportion of residents inappropriately receiving antipsychotic medications (figure 1), from 26.8% at baseline to 21.1% at follow-up. The per cent of residents with symptoms of delirium declined from 27.4% at baseline to 26.0% at follow-up, and the QI for falls increased from 14.5% to 15.2% (figure 2A). Pain among LTC residents declined from baseline (11.1%) to follow-up (7.8%, figure 2B). Daily physical restraint use declined from 11.9% to 8.6% (figure 2B). ABS scores remained unchanged, with a mean (SD) score of 1.7 (2.4) at baseline and 1.6 (2.3) at follow-up.
Figure 1.
The risk-adjusted quality indicator (QI) for the per cent of LTC residents on antipsychotics without a diagnosis of psychosis (DRG01) at the project baseline (FY2011–2012 Q4) and follow-up (FY2014–2015 Q4) time points and the associated per cent of spread of the intervention to LTC sites during project implementation. *For sites participating in the learning workshop series, the intervention spread reflects the quarter in which the first learning workshop was delivered. LTC, long-term care.
Figure 2.
LTC resident outcomes at baseline and follow-up, reported as the per cent of residents experiencing the outcome. (A) The risk-adjusted quality indicator (QI) for LTC residents with symptoms of delirium and who fell in the last 30 days. (B) The risk-adjusted QI for LTC residents with pain and in daily physical restraints. LTC, long-term care.
Resident fractures and acute care health service utilisation are shown in table 1, with no change between baseline and follow-up. There was an increase in hospital admissions, from 8.2% at baseline to 8.6% at follow-up, an absolute increase of 79 more admissions. However, ED visits decreased from 4.3% at baseline to 3.6% at follow-up, equal to 87 fewer visits.
Table 1.
Unadjusted outcomes for fractures, hospitalisations and emergency visits for LTC residents in Alberta
| Outcome | FY2011–2012 Q4 Count (%) |
FY2014–2015 Q4 Count (%) |
| Hip fractures (in the past 180 days) | 210 (1.5) | 224 (1.5) |
| Fractures, other than hip (in the past 180 days) | 223 (1.6) | 244 (1.7) |
| Hospital admissions (1 or more times in the past 90 days) | 1170 (8.2) | 1249 (8.6) |
| Emergency department visits (1 or more times in the past 90 days) | 612 (4.3) | 525 (3.6) |
LTC, long-term care.
Economic evaluation
The clinical events estimated probabilities of the unadjusted inappropriate antipsychotic use as 28.1% before the project and 21.9% afterwards, a 6.2% reduction in inappropriate antipsychotic use. Residents taking antipsychotics, either before or after the AUA Project, had a lower probability of improvement in NPS compared with residents not on antipsychotics (online supplemental table S1). Individuals who were on antipsychotics after the AUA Project had the highest probability of hospitalisations and ED visits (online supplemental table S1).
In the base case analysis, implementation of the AUA Project resulted in an incremental cost per inappropriate antipsychotic use avoided of $5678.71 compared with no AUA Project (table 2). The results of the uncertainty analyses are in the online supplemental table S3 and figure S1. The cost-effectiveness results were sensitive to changes in the probability of inappropriate antipsychotic use. If the pre-project probability of inappropriate antipsychotic use is less than 21.08%, the AUA Project becomes less effective and more expensive (dominated) compared with no AUA Project. The AUA Project is thus never cost-saving, regardless of its effectiveness. The cost-effectiveness results are robust to reasonable changes in project costs, cost per ED visit and cost per hospitalisation. The addition of in-kind implementation costs increased the incremental cost per inappropriate antipsychotic avoided to $9102.09. Probabilistic sensitivity analysis revealed that, compared with no AUA Project, the AUA Project will be more effective and more expensive 30.2% of the time, more expensive and less effective 37.9% of the time, more effective and less expensive 22.0% of the time, and less expensive and less effective 9.9% of the time.
Table 2.
Results of the cost-effectiveness comparing AUA Project with no AUA Project
| Outcome of interest | Strategy | Cost ($) | Incremental cost ($) | Effectiveness | Incremental effectiveness | Incremental cost-effectiveness ratio |
| Cost per inappropriate antipsychotic use avoided | No AUA Project | 1191.06 | — | 0.719 | — | — |
| AUA Project | 1543.13 | 352.08 | 0.781 | 0.062 | $5678.71 per inappropriate antipsychotic use avoided |
Applying the observed 6.2% reduction in appropriate antipsychotic use to the total population of residents in LTC, there would be 897 fewer residents inappropriately prescribed antipsychotics after the project (table 3). This gives a cost-saving of approximately $111 318 from the pre-project period year. Deducting this amount from the upfront project cost ($623 796) and the additional estimated ED visit and hospitalisation costs ($1 656 119), the additional investment for the AUA Project was estimated as $2 168 597.
Table 3.
Budget and clinical impact analysis of the AUA Project
| No AUA Project | AUA Project | Bottom line | |
| Inappropriate antipsychotic use (# of residents) |
4067 | 3170 | 897 fewer residents |
| Annual cost of inappropriate antipsychotic use | $504 715 | $393 397 | −$111 318 |
| Number of ED visits | 612 | 525 | −87 ED visits |
| Number of hospitalisations | 1170 | 1249 | +79 hospitalisations |
| Cost of ED visits and hospitalisations | $25 478 009 | $27 134 128 | +$1 656 119 |
| Total cost of AUA Project | — | $623 796 | +$623 796 |
| Overall cost | $25 982 723 | $28 151 320 | +$2 168 597 |
ED, emergency department.
Family member interviews
Thirty-five family members from 19 LTC sites were invited to participate, and 26 family members of 27 residents did so (74% response rate; one participant provided experiences of both parents in LTC). Ten participants (38%) provided experiences as a spouse and 16 (62%) from the perspective of an adult child of a parent(s) in LTC. According to family members, unverified by medical records, 12 residents had a reduction in antipsychotic medications and 15 residents had their medications discontinued. The vast majority of residents (93%) did not have their antipsychotic medication restarted or dose increased by the date of the interview. Family member interviewees commented on the changes they observed after medication reduction/removal and their satisfaction with care.
Family members provided an abundance of rich data on the changes observed in their spouse/parent. The number of comments on positive changes (n=119, 85.6%) far outnumbered the negatives (n=20, 14.3%), despite being asked to comment on both. Family members cited increased alertness, decreased sleepiness, and increased engagement and participation.
Although the majority of respondents reported positive outcomes, family members did report some drawbacks associated with the dose reduction or discontinuation of antipsychotics. For some, the downside of change was somewhat minor, including increased restlessness and vocalisations. Family members also cited a few instances of minor altercations with staff or other residents.
Family members were asked about their satisfaction with resident care. Increased satisfaction was described by interviewees who perceived an improved sense of partnership with staff or an increase in personalised care. Predominantly, dissatisfaction was related to concerns regarding staffing levels at the site or staff turnover.
LTC site and organisational leader survey
Ninety-nine surveys were completed. A response rate cannot be calculated due to the sampling method. Leaders provided their perspectives on changes necessary at their site, satisfaction with the project and effect on residents.
Approximately two-thirds of leaders (n=62, 62.6%) reported that staff work pattern changes were not necessary to accommodate the use of non-pharmacological approaches to NPS. Among those responding that work pattern changes were necessary, 22 (22.2%) cited changes including providing temporary one-on-one care, using different staff (eg, recreation, occupational or physiotherapists), and adjusting recreation and pastoral care hours to allow more evening programming.
The majority of leaders were satisfied or very satisfied (n=79, 79.8%) with the project. Although positive comments included the quality of the resources, LWs and support from the project team, the most frequent criticism was that the project was staff resource and time intensive, and more resources were required for implementation. The majority of respondents agreed or strongly agreed (n=77, 77.7%) that the benefits they saw over the course of the project were worth the effort of involvement. A small number of leaders (n=5) noted that they were already focused on the AUA aside from their participation in the project. When asked for their opinion of the effects of the AUA Project on residents, the majority agreed or strongly agreed that participation contributed to improved resident experience (n=79, 79.8%), health (n=70, 70.7%) and quality of life (n=78, 78.8%).
LTC staff and physician survey
A total of 217 surveys were completed by LTC staff and physicians. Staff (n=196) and physician (n=21) responses were analysed separately. The top three respondent groups included registered nurses (14.3%), unit managers (11.5%) and care aides (10.1%).
Staff were asked about their use of non-pharmacological strategies to manage resident behaviours. More than three-quarters reported using individualised care and conversational approaches to manage resident behaviours, while more than half reported using visiting/socialising, physical activity, music/art/gardening therapy, or personal environment modifications. Reasons for not using these strategies included lack of budget for supplies/staff and being too time-consuming. Respondents reported increased use of such strategies over the duration of the project (75.9% of staff and 26.7% of physician respondents). Staff reported higher perceptions of effectiveness of non-pharmacological strategies than did physicians for reducing both the frequency (30.4% vs 14.3%) and severity (23.4% vs 14.3%) of residents’ behaviours. The majority of staff (n=125, 71.8%) and one-quarter of physician respondents (n=5, 27.8%) agreed or strongly agreed that the AUA Project resulted in them, personally, feeling better prepared to manage residents’ behaviours. The majority of staff respondents (n=154, 84.6%) and seven physician respondents (41.2%) agreed or strongly agreed that the AUA Project resulted in better resident quality of life.
Discussion
This paper describes the implementation of a quality improvement initiative across the entire LTC sector of continuing care in Alberta. LTC teams were engaged in efforts to reduce antipsychotic medication use at their local site. Over the project period, the per cent of residents on antipsychotic medications without a documented indication decreased by 5.7%–21.1% suggesting that the provincial target of 20% may be achievable, particularly as project activities spread to other units within facilities.
The decline in antipsychotic medication use was achieved without serious unintended consequences, such as increases in aggressive behaviours or physical restraint use. The perception of LTC leader respondents was that staff increased the use of non-pharmacological approaches to managing resident behaviours. LTC leader participants were satisfied with their site’s involvement with the project, with the perceived benefits of being involved in the project outweighing the required resource and time requirements. Family members, leaders, and LTC staff and physician respondents all commented on their perception of improvement in resident(s)’ quality of life. Parallel findings regarding nursing staff perceptions of the benefits of reducing antipsychotic medications of LTC residents were reported by Simmons et al.31
Success of this initiative was enabled by providing teams with a structure fitting in with other performance-monitoring requirements. Continuing Care Health Service Standards require monthly medication reviews where medications used are a chemical restraint.17 As such, this project supported what was already being asked of sites, rather than adding new activities or care processes to site workflow.
The results of this project should be interpreted recognising contextual factors that might have influenced outcomes. For example, a site with a concurrent initiative to address physical restraint use likely saw change in their QI attributable to both initiatives. At the same time as this project, there was increasing recognition of the need to address inappropriate antipsychotic medication use, prompted by national public reporting and other regional efforts.12 32–34 This attention may have contributed to efforts among sites not participating in the more resource-intensive LWs. Examination of CIHI indicators over the same period as this project shows a decrease in the inappropriate use of antipsychotics across a number of provinces,35 with improvements in British Columbia and Ontario exceeding that of Alberta. It is impossible to know the degree of change that would have been achieved in Alberta without the AUA Project, nor on what timeline. Future efforts to understand the local context may help to better match project resources to meet site or team needs.
The AUA Project did not result in a cost-saving outcome, although originally projected to produce such. Within the implementation period, high-cost medications became generic and the funding model for generic drugs changed. This resulted in lower drug costs avoided than were originally forecasted, but these would have been insufficient to produce cost-saving. As sustainability of the project outcomes is achieved and monitored, it is likely that additional project resources will reduce and actions transitioned into regular operations. Despite lack of cost-saving, improvement in resident care is the right action to take when a practice is associated with more risk than benefit. There is recognition that some investment may be needed to jumpstart practice change. Provincially, sufficient gains were made in reducing inappropriate antipsychotic medication use, and in recognition of and support for the project, as to produce a culture shift regarding non-pharmacological resident-focused dementia care. As such, this project paved the way for other de-prescribing initiatives.
There are a number of limitations of this work. First, we acknowledge that the costs to the LTC site/organisation for project implementation were not included, such as those associated with delivering non-pharmacological interventions to residents who would have received an antipsychotic. Further information from the LTC site perspective would be an asset to future activities. Second, the resident outcomes monitored over the course of the project used facility-level reporting, and aggregation at the zone or provincial level. By focusing at the facility level, we may have missed potentially important unit-level information that might have informed our understanding of implementation success and/or challenges.36 Likewise, and third, we cannot definitively ascribe causation, due to the lack of non-intervention comparator sites and acknowledgement of a national shift in attitude to prescribing of antipsychotics for behavioural symptoms associated with dementia. However, despite these limitations, this work demonstrates that large-scale quality improvement initiatives can deliver provincial change in quality outcomes within a defined implementation period.
Conclusion
Local teams can be engaged and supported to make improvements to care practices. If antipsychotic medications are a proxy indicator for good dementia care, the AUA Project has demonstrated that awareness and education may be solid first steps toward this. Addressing antipsychotic medication use was an entry point to initiating a culture change within LTC sites to move toward a more person-centred philosophy of care. The positive interaction with and engagement of sites is likely to bode well for future quality improvement initiatives addressing quality of care and resident outcomes in LTC.
Acknowledgments
Quality improvement initiative was made possible with funding from the Alberta Health Services (AHS). We thank the Outcomes Evaluation Subcommittee members for their contributions to shape the evaluation framework and their guidance conducting the evaluation components. We recognise the assistance from AHS Primary Data Support and Clinical Analytics, and Deborah Katz for expertise on the RAI quality indicators and data access. We thank Jennifer Herrick, Jeff Burnell, Jackie Liu and Gilles Lamerton for assistance with modelling antipsychotic drug costs using Calgary Zone pharmacy information. We acknowledge the leadership of the Seniors Health Strategic Clinical Network and the Addiction & Mental Health Strategic Clinical Network for sponsoring this project. Finally, we thank the participants who contributed their experiences and perspectives during data collection.
Footnotes
Contributors: HMH and TL planned the evaluation and led the evaluative activities, with the contributions of a subcommittee, including MC and FC. FC and LS conducted the economic analysis. AW and JS provided leadership within the project and its development for publication. All authors reviewed the final version of this manuscript and approved its submission to BMJ Open Quality.
Funding: Funding for this quality improvement initiative was provided by the Alberta Health Services (no grant number).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This project was not subject to institutional research ethics review board oversight; consultation with the AHS Legal and Privacy department determined a privacy impact assessment was not required.
References
- 1.Alberta Health Services . 2019-20 AHS annual report. Edmonton, Alberta; 2020. [Google Scholar]
- 2.Government of Alberta . Alberta long-term care resident profile 2016/2017. Edmonton, Alberta: Alberta Health, Continuing Care, 2018. [Google Scholar]
- 3.Steinberg M, Shao H, Zandi P, et al. Point and 5-year period prevalence of neuropsychiatric symptoms in dementia: the Cache County study. Int J Geriatr Psychiatry 2008;23:170–7. 10.1002/gps.1858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lyketsos CG. Neuropsychiatric symptoms in dementia: overview and measurement challenges. J Prev Alzheimers Dis 2015;2:155–6. 10.14283/jpad.2015.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liperoti R, Pedone C, Corsonello A. Antipsychotics for the treatment of behavioral and psychological symptoms of dementia (BPSD). Curr Neuropharmacol 2008;6:117–24. 10.2174/157015908784533860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yunusa I, Alsumali A, Garba AE, et al. Assessment of reported comparative effectiveness and safety of atypical antipsychotics in the treatment of behavioral and psychological symptoms of dementia: a network meta-analysis. JAMA Netw Open 2019;2:e190828. 10.1001/jamanetworkopen.2019.0828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma H, Huang Y, Cong Z, et al. The efficacy and safety of atypical antipsychotics for the treatment of dementia: a meta-analysis of randomized placebo-controlled trials. J Alzheimers Dis 2014;42:915–37. 10.3233/JAD-140579 [DOI] [PubMed] [Google Scholar]
- 8.Bjerre LM, Farrell B, Hogel M, et al. Deprescribing antipsychotics for behavioural and psychological symptoms of dementia and insomnia: evidence-based clinical practice guideline. Can Fam Physician 2018;64:17–27. [PMC free article] [PubMed] [Google Scholar]
- 9.Sturm AS, Trinkley KE, Porter K, et al. Efficacy and safety of atypical antipsychotics for behavioral symptoms of dementia among patients residing in long-term care. Int J Clin Pharm 2018;40:135–42. 10.1007/s11096-017-0555-y [DOI] [PubMed] [Google Scholar]
- 10.Declercq T, Petrovic M, Azermai M, et al. Withdrawal versus continuation of chronic antipsychotic drugs for behavioural and psychological symptoms in older people with dementia. Cochrane Database Syst Rev 2013:CD007726. 10.1002/14651858.CD007726.pub2 [DOI] [PubMed] [Google Scholar]
- 11.Zuidema SU, Johansson A, Selbaek G, et al. A consensus guideline for antipsychotic drug use for dementia in care homes. bridging the gap between scientific evidence and clinical practice. Int Psychogeriatr 2015;27:1849–59. 10.1017/S1041610215000745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elmi A, Yiu V, Tierney M. Healthy debate: improving appropriateness of antipsychotic use in long-term care. Available: http://healthydebate.ca/2015/06/topic/community-long-term-care/antipsychotics
- 13.Varkey P, Antonio K. Change management for effective quality improvement: a primer. Am J Med Qual 2010;25:268–73. 10.1177/1062860610361625 [DOI] [PubMed] [Google Scholar]
- 14.Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;2012:CD000259. 10.1002/14651858.CD000259.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grimshaw JM, Eccles MP, Lavis JN, et al. Knowledge translation of research findings. Implementation Science 2012;7. 10.1186/1748-5908-7-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Birney A, Charland P, Cole M, et al. Evaluation of the antipsychotic medication review process at four long-term facilities in Alberta. J Multidiscip Healthc 2016;9:499–509. 10.2147/JMDH.S116008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alberta Health . Continuing care health service standards. Edmonton, AB: Government of Alberta; 2016. [Google Scholar]
- 18.Institute for Healthcare Improvement . The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. Cambridge, MA 2003.
- 19.Langley GJ, Moen RD, Nolan KM. Improvement guide: a practical approach to enhancing organizational performance. 2nd edn. San Francisco, CA: Jossey-Bass, 2009. [Google Scholar]
- 20.Deming WE. Out of the crisis. Cambridge, MA: Massachusetts Institute of Technology; 1986. [Google Scholar]
- 21.Hirdes JP, Fries BE, Morris JN, et al. Integrated health information systems based on the RAI/MDS series of instruments. Healthc Manage Forum 1999;12:30–40. 10.1016/S0840-4704(10)60164-0 [DOI] [PubMed] [Google Scholar]
- 22.Canadian Institute for Health Information . Continuing care reporting system RAI-MDS 2.0 output specifications, 2015–2016. Ottawa, ON; 2015. [Google Scholar]
- 23.Zimmerman DR, Karon SL, Arling G, et al. Development and testing of nursing home quality indicators. Health Care Financ Rev 1995;16:107–27. [PMC free article] [PubMed] [Google Scholar]
- 24.Karon SL, Zimmerman DR. Using indicators to structure quality improvement initiatives in long-term care. Qual Manag Health Care 1996;4:54–76. 10.1097/00019514-199604030-00008 [DOI] [PubMed] [Google Scholar]
- 25.Canadian Institute for Health Information . Indicator library: general methodology notes — clinical indicators, February 2019. Ottawa, ON; 2019. [Google Scholar]
- 26.Canadian Institute for Health Information . CCRS quality indicators risk adjustment methodology. Ottawa, ON; 2013. [Google Scholar]
- 27.QSR International . NVivo, version 11. Burlington, MA; 2012. [Google Scholar]
- 28.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 29.ClassApps Inc . Select survey. Kansas City, MO: NET ClassApps Inc; 2015. [Google Scholar]
- 30.IBM Corp . IBM SPSS statistics for windows, version 23.0. Armonk, NY: IBM Corp; 2015. [Google Scholar]
- 31.Simmons SF, Bonnett KR, Hollingsworth E, et al. Reducing antipsychotic medication use in nursing homes: a qualitative study of nursing staff perceptions. Gerontologist 2018;58:e239–50. 10.1093/geront/gnx083 [DOI] [PubMed] [Google Scholar]
- 32.Morris N. CFHI Welcomes CIHI indicators for long term care sector. Available: https://www.cfhi-fcass.ca/SearchResultsNews/2015/06/10/cfhi-welcomes-cihi-indicators-for-long-term-care-sector
- 33.Malagaris I, Mehta HB, Li S, et al. Decrease of anticholinergic drug use in nursing home residents in the United States, 2009 to 2017. J Am Geriatr Soc 2020;68:2797–804. 10.1111/jgs.16776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hirdes JP, Major J, Didic S, et al. A Canadian cohort study to evaluate the outcomes associated with a multicenter initiative to reduce antipsychotic use in long-term care homes. J Am Med Dir Assoc 2020;21:817–22. 10.1016/j.jamda.2020.04.004 [DOI] [PubMed] [Google Scholar]
- 35.Canadian Institute for Health Information . Your health system: potentially inappropriate use of antipsychotics in long-term care (percentage). Ottawa, ON; 2020. [Google Scholar]
- 36.Norton PG, Murray M, Doupe MB, et al. Facility versus unit level reporting of quality indicators in nursing homes when performance monitoring is the goal. BMJ Open 2014;4:e004488. 10.1136/bmjopen-2013-004488 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2020-001211supp001.pdf (746.1KB, pdf)
Data Availability Statement
Data are available upon request.