Abstract
The threat of coronavirus disease (COVID-19) is increasing. Regarding the differences in the infection rate observed in each region, additionally to studies investigating the causes of differences in population density as a proxy for social distancing, an increasing trend of studies investigating the causes of differences in social capital has also been seen (ie, value sharing, acceptance of norms, unity, and trust through reciprocity). However, studies investigating whether social capital that controls the effects of population density also influences the infection rate are limited. Therefore, in this study, we analyzed the relationship between infection rate, population density, and social capital using statistical data of Japan’s every prefecture. Statistical analysis showed that social capital not only negatively correlates with infection rates and population densities, but also negatively correlates with infection rates controlling for the effects of population density. Additionally, controlling the relationship between the variables by mean age showed that social capital had a greater correlation with infection rate than population density. In other words, social capital mediates the relationship between population density and infection rates, indicating that social distancing alone is not enough to deter coronavirus disease; social capital needs to be recharged.
Keywords: coronavirus disease (COVID-19), population density, social distancing, social capital, Japan
What do we already know about this topic?
Regarding the differences in the infection rate of the coronavirus disease (COVID-19) observed in each region, in addition to studies investigating the causes of differences in population density as a proxy for social distancing, there is an increasing trend of studies investigating the causes of differences in social capital.
How does your research contribute to the field?
We found that social capital mediates the correlation between population density and infection rates, indicating that social distancing alone is not enough to deter coronavirus infection; social capital needs to be recharged.
What are your research’s implications towards theory, practice, or policy?
Our findings can be utilized not only as measures for the next wave of coronavirus that is expected shortly, but also as preventive measures for various infectious disease viruses in the future.
Introduction
The threat of coronavirus disease (COVID-19), discovered in Wuhan, China, in December 2019 that spread worldwide, is continuously affecting many lives. Japan is no exception, although it is reported that its death rate due to the virus is mysteriously low.1 The number of infected people, which had subsided in June 2020, began increasing again in July. Previous research showed that the infection rate tends to be high in large cities, such as Tokyo due to their high population density; research stated that population density can be used as a proxy variable for social distancing.2,3 Other studies conducted in different countries also confirmed a positive correlation between population density and infection rates.4-7
However, coronavirus infections cannot be prevented by low population density (or high social distancing) alone. Moreover, additionally to ensuring social distancing by refraining from going out, time lag, remote work, etc., the government is implementing anti-quarantine actions, such as wearing a mask, encouraging hand and finger disinfection, and refraining from having loud conversations as a basic policy for countermeasures against COVID-19, which has been strongly sought by the public.8 Among some possible options, many researchers are paying attention to social capital as a factor that promotes these quarantine actions.
Social capital, that is, value sharing, acceptance of norms, unity, and trust through reciprocity, is said to play an important role in solving problems through interaction and cooperation.9-11 Previous research has also shown that social capital is effective in solving public health challenges.12-14 For example, some studies show that a high level of social capital (trust and human connection with the government, mutual benefit, reciprocity, and solidarity) influenced the practice of preventive actions, such as vaccination, washing hands, and wearing a mask during the H1N1 outbreak in 2009.15-17 In connection with the COVID-19 pandemic, studies analyzing GPS information in the United States showed that residents in counties with high social capital were more cooperative in following regulations,18 reducing the increase in COVID-19 cases.19 A study in Italy also showed that areas with high social capital tended to have low outing rates and coronavirus mortality.20 In a related study, research in the field of human resource management based on a questionnaire survey showed that social capital (reciprocal support between a company and employee organizational commitment) enhanced employees’ willingness to cooperate in the workplace COVID-19 countermeasures.21
Why does social capital have this effect? This is because, social capital encourages information sharing and removes the uncertainty of choice,22-24 also encouraging collective action and deterring the occurrence of the free-rider problem.14,25-27 Regarding the former, Kawachi and Berkman28 argue that social capital helps promote the dissemination of health-related information and prevents unhealthy conduct. Regarding the latter, a recent empirical study conducted in China showed that social capital was successful in the prevention of COVID-19 by the facilitation of refraining from going out and wearing masks.29
The latter mechanism by which social capital restrains free riders has an affinity with collectivism, a cultural characteristic of Japan and Asian countries.30 Yamaguchi31 states that Japanese collectivistic behavior is based on the calculation of advantages and disadvantages. Receiving a reward from the group by suppressing one’s desires and serving them is an advantage; whereas, being punished by the group for interfering with its unity without suppressing one’s desires is a disadvantage. Therefore, to promote cooperative actions, it is necessary to have a mechanism in which a person who refuses cooperation receives a “Tit for Tat” treatment from another person.32 According to such a mechanism, Japan’s murahachibu (making people stand out of line if they do not follow the rules of the village) is wisdom.
As mentioned above, a growing number of studies tend to show that social capital has not only led to the prevention of epidemics but also has promoted quarantine action and deterrence of infection during the COVID-19 pandemic. However, to the best of our knowledge, no studies have shown a negative correlation between high social capital and coronavirus infection rates even after controlling the effects of population density. Therefore, in this study, we would like to address this issue using cross-sectional data at the local government level in Japan.
Review of Previous Studies and Presentation of Hypotheses
Population Density and Coronavirus Infection Rate
The relationship between population density and infection rate in Japan is shown in Kodera et al2 and Rashed et al.3 Studies in China,7 United States,5 Brazil,6 Turkey,4 and other countries also confirmed a positive correlation between population density and infection rates. These studies indicate increased opportunities for human contact (smaller social distances) associated with high population densities as a reason for the correlation. In support, some studies have directly investigated the effects of social distancing. For instance, results of a previous study’s independent online survey held in Japan showed that the number of infected people from January to March 2020 was smaller in prefectures with less face-to-face communication, less use of public transportation and fewer meals consumed outsides.33 Therefore, the following hypothesis is derived.
H1: There is a positive correlation between population density and infection rate.
Social Capital and Coronavirus Infection Rates
Previous studies have shown that social capital helps promote public health.12-17 Besides, increasing studies during the COVID-19 pandemic show that social capital encourages cooperation against coronavirus measures21,29 and controls infections.19,20 Therefore, the following hypothesis is derived.
H2: There is a negative correlation between social capital and the infection rate.
Population Density and Social Capital
Small cities are more likely to form social links than large cities.34 This is because the basic services provided by the government in large cities are not provided in small cities with a low population density, meaning maintenance of alternative services will require the unity and turnaround of residents.35 Several studies have found a supporting negative effect of population density on social interaction.36,37 Therefore, many studies have shown that densely populated large cities have lower social capital.38-41 Therefore, the following hypothesis is derived.
H3: There is a negative correlation between population density and social capital.
Partial Mediation Effect of Social Capital
Furthermore, we wanted to examine whether social capital correlates with infection rate if population density is included as a variable. An empirical study recently conducted in Japan showed that the higher the population density, the greater the impact of trust with the surrounding people on health.42 This suggests that population density alone is not enough to predict people’s health and that social capital acts as an intermediary between population density and health. Further, given that population density is not a variable that captures all social distancing, and that social capital is involved in the prevention of various types of epidemics, as shown above, population density and social capital are thought to affect the infection rate by complementing each other. Therefore, the following hypothesis is derived.
H4: Social capital partially mediates the relationship between population density and infection rates.
Full Mediation Effect of Social Capital
Population density (concentration of population in a certain area) used in this study is merely an indicator of one aspect of social distancing. Even in densely populated areas, people can reduce contact with each other. For example, a US study using mobile GPS location data showed that the normative element of social capital correlated with social distancing measured by the length of time at home.43 Further, infection risk depends, to a large extent, on each person’s social capital of following norms and disciplines, such as remote work, hand washing, and disinfection. Therefore, the following hypothesis is derived.
H5: Social capital fully mediates the relationship between population density and infection rates (Social capital has a greater correlation with infection rate than population density).
Data
For calculating the coronavirus infection rate, we used the cumulative number of infected people per 1 million population by July 3, 2020, as calculated by Sapporo Medical University.44 We used the data until July 3rd because it was just a delimiter. The increase in the number of people infected was not officially recognized as a threat until this date since the termination of the emergency declaration period from April 7th to May 25th. In other words, the data handled in this study is the cumulative total till July 4, when Tokyo Governor Yuriko Koike urged Tokyo residents to refrain from any nonessential and non-urgent trips to other prefectures in response to the confirmation of novel coronavirus disease in Tokyo exceeding 100 people for 3 consecutive days (The Japan Times News, 2020.7.4).45 For calculating population density, we used the “population density per 1 km2 of habitable area” for 2018 recorded in the Statistics Bureau.46 Both infection rate and population density were log-transformed and used for the analysis. For social capital, we used the “social capital comprehensive index” recorded in the Cabinet Office.47 This index was calculated from the responses of 3878 people to a questionnaire survey consisting of 10 questions about “friendship/interaction,” “trust,” and “social participation,” combining the figures in other 2 comprehensive statistics about “volunteer activity participation rate” and “community donation amount per person.” It is standardized using the formula “(prefecture value-average value)/standard deviation.” This index is one of the most comprehensive measures of social capital in Japan consisting of both subjective information (questionnaire survey) and objective information (external source), increasing objectivity and reducing the common method bias, making it different from other social capital measures that consist solely of subjective information. Furthermore, empirical studies have shown that this index correlates with lower unemployment and crime rates, higher fertility rates, higher life expectancy, and higher new start-up rates,47 a strength not found in other measures. Finally, the average age for 2015 obtained from the Statistics Bureau48 was used as a control variable.
Analysis and Results
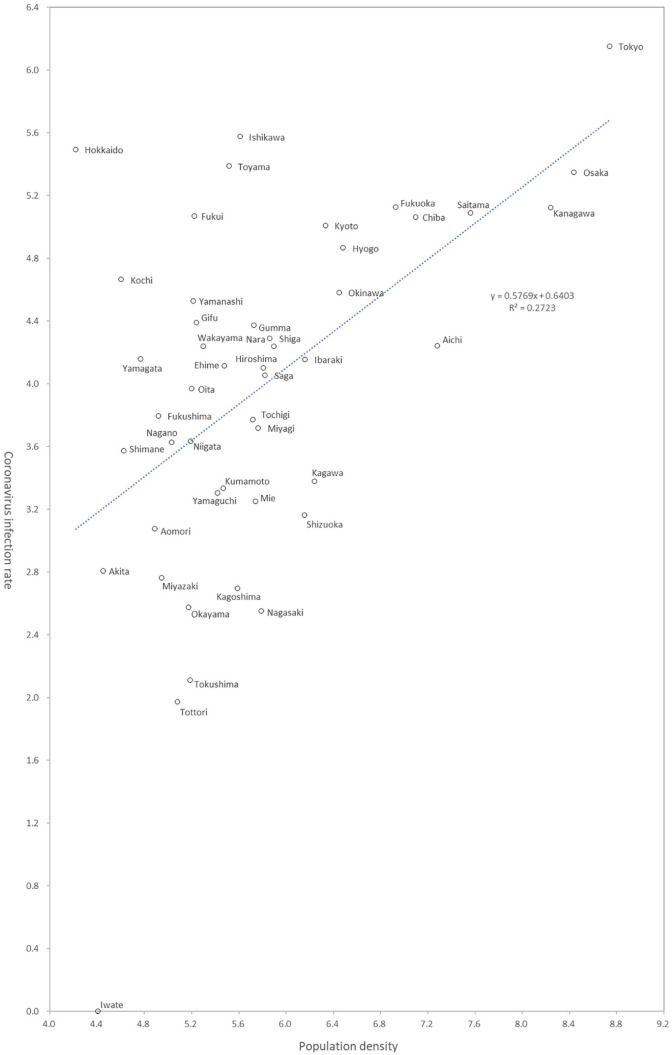
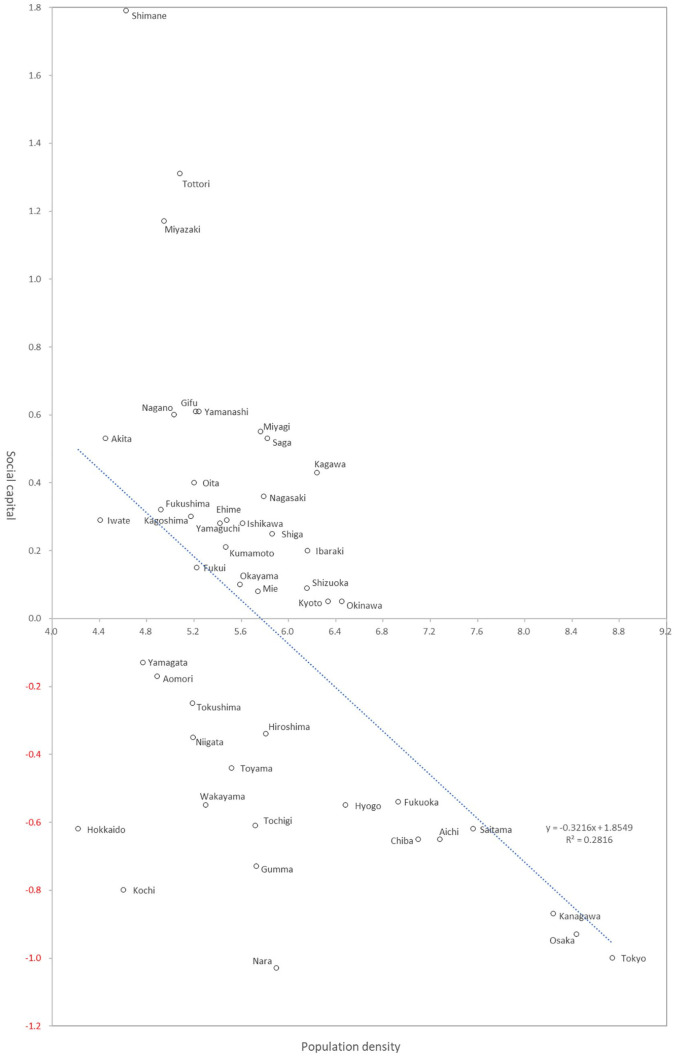
Table 1 is descriptive statistics. All skewness and kurtosis values computed to assess the normality of the scales were within the acceptable range (−2 and +2).49 Therefore, the following analysis was performed assuming that all 4 variables had a close to normal distribution. The lower part of the correlation coefficient table is the normal correlation coefficient, and the upper part is the partial correlation coefficient controlled by average age. In both cases, significant correlations are shown among the 3 variables. Figures 1 to 3 are scatter diagrams showing these relationships. These findings support H1-H3.
Table 1.
Descriptive Statistics.
| Mean | SD | Skewness | Kurtosis | 1 | 2 | 3 | ||
|---|---|---|---|---|---|---|---|---|
| 1 | Coronavirus infection rate | 3.967 | 1.132 | −0.886 | 1.987 | 0.310* | −0.416** | |
| 2 | Population density | 6.821 | 0.770 | 1.222 | 1.860 | 0.527** | −0.398** | |
| 3 | Social capital | 0.000 | 0.621 | 0.447 | 0.320 | −0.507** | −0.506** | |
| 4 | Average age | 47.300 | 1.667 | −0.554 | 1.187 | −0.475** | −0.697** | 0.342* |
Note. **Significant at 1% level.
Significant at 5% level. n = 47.
Coronavirus infection rate: Number of infected people per million (logarithmic display). For Iwate prefecture, where the number of infected people was 0 (that means logarithmic conversion not possible), we substituted 0 with 1, assuming that there was 1 infected person there.
Population density: Population density per 1 km2 of habitable area (logarithmic display). Social capital: A standardized index consisting of “communications and exchanges,” “trust,” “social participation,” “volunteer activity rate,” and “community solicitation amounts per capita.”
Figure 1.
Correlation between population density and coronavirus infection rate.
Figure 3.
Correlation between population density and social capital.
Furthermore, the results of the path analysis shown in Figure 4 indicate that the correlation between social capital and infection rate remains even when population density is controlled, that is, social capital partially mediates the relationship between population density and infection rate. This supports H4. Additionally, Figure 5 shows the results of a model, including age as a control. Here, population density makes the path of infection rates insignificant, indicating that social capital mediates the relationship between population density and infection rates perfectly. This indicates that social capital influences the infection rate more than population density does, supporting H5.
Figure 4.
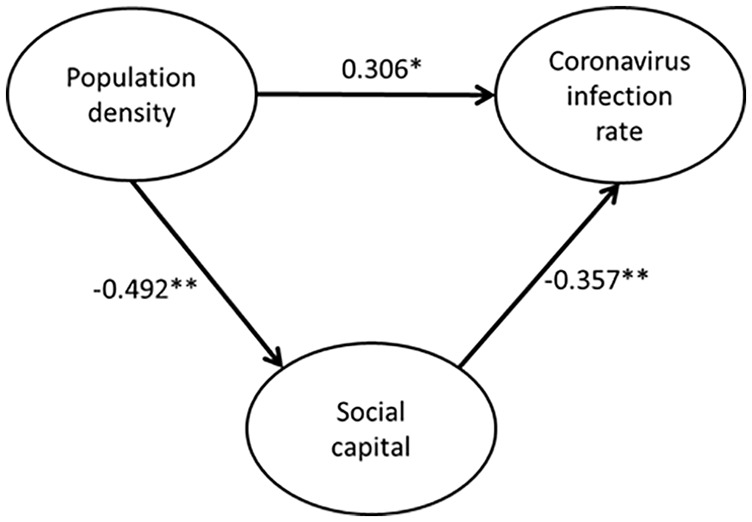
Result of path analysis.
Note. **Significant at 1% level.
*Significant at 5% level. n = 47.
Figure 5.
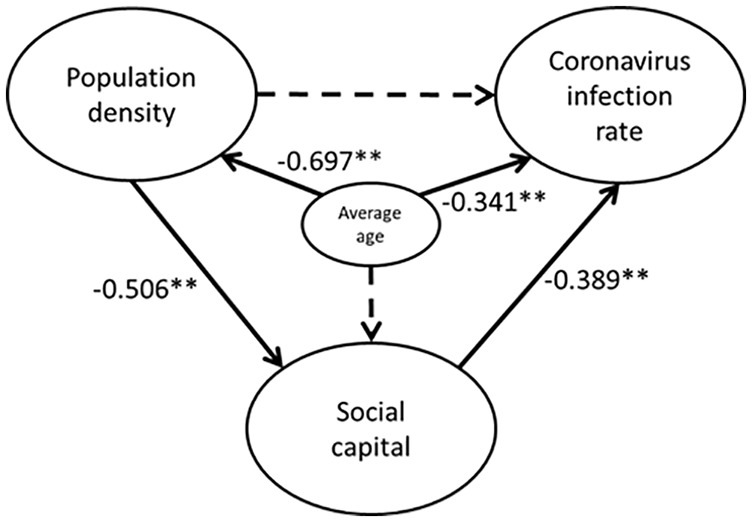
Result of path analysis (Controlled by average age).
Note. **Significant at 1% level.
*Significant at 5% level. n = 47.
Dashed arrow indicates not significant at 5% level.
Goodness-of-fit indices: χ2 = 2.150; df = 2; root mean square error of approximation (RMSEA) = 0.000; probability of close fit (PCLOSE) = 0.533; goodness of fit index (GFI) = 0.985; adjusted goodness of fit index (AGFI) = 0.926; normed fit index (NFI) = 0.979; comparative fit index (CFI) = 1.000.
Discussion
The results of this study based on the data from Japanese prefectures show that the negative correlation between social capital and infection rates is statistically significant in controlling population density. Social capital partially mediated the relationship between population density and infection rates. Low population density (or following social distancing) is not enough to prevent infection; it is essential to foster social capital based on solidarity, trust, and adherence to norms. Also, the result of the age-controlled model shows that social capital influences infection rates more than population density does. As seen in Figures 1 and 2, Hokkaido is a good example of this. Low population density should lead to low infection rates but a high infection rate is seen due to low social capital. This supports the argument by Kitayama et al50 which states that the culture of the pioneering spirit inherited in Hokkaido is based on individualism and empirical research by Yamawaki51 who verified it.
Figure 2.
Correlation between social capital and coronavirus infection rate.
Compared to relatively individualistic prefectures, such as Hokkaido and Tokyo, other prefectures, supported by relatively high social capital, were able to successfully control the outbreak of COVID-19’s first wave. Most prefectures in Japan, like other Asian countries, have a strong culture of collectivism,30 with which social capital has a high conceptual affinity. Social capital was defined as value sharing, acceptance of norms, unity, and trust through reciprocity and is said to play an important role in solving problems through interaction and cooperation.9-11 Collectivism is defined as a set of feelings, beliefs, and behaviors related to solidarity and concern for others by respecting the group’s norms and duty rather than own pleasure.30,52,53 Previous empirical research suggests that sources of social capital at the individual level can be found in people’s immediate social surroundings, as well as their everyday social interactions.54 In line with this, a recent empirical study in China suggests that social capital affects COVID-19 response mainly through facilitating collective actions and promoting public acceptance of and compliance with control measures in the form of trust and norms at the individual level.55 These studies indicate how close and compatible social capital and collectivism are.
Looking back on the COVID-19 pandemic based on the results of this article, the high infection rate in large cities, such as Tokyo, can be explained not only by the narrow social distancing but also by the weakness of social capital. While the risks of COVID-19 are being exclaimed, the reason people go out to the so-called yoru no machi (entertainment district) where the risk of infection is high is that the norms for limiting their behaviors are weak. In a local city with a culture of traitor-tattooing, an immediate thought of “What is that person thinking?,” can be a strong weapon preventing his/her imprudent behavior. Especially in situations where the experience cannot be utilized like in the case of the COVID-19 pandemic, it is considered that the bonds and norms between citizens play a major role in making them take appropriate actions, especially in local cities.
From the perspective of preventing infectious diseases, it will be necessary to take various measures to restore social capital in each prefecture, especially in the heavily affected cities. Instead of pursuing the fulfillment of one’s desires, people should develop a culture where they respect cooperation and norms and are willing to control their actions for others around them. However, it is important to note the negative consequences of these cultures, such as the exclusion of strangers.56 Reportedly, bullying and targeting infected persons, especially in prefectures where the infection rate of COVID-19 is low, has occurred.57 This suggests that the strength of cohesion in areas with high social capital contributed to the prevention of infection and simultaneously had a disciplinary function for infected persons. Relatedly from a larger perspective, it has often been pointed out that such exclusivity hinders the internationalization of Japanese organizations especially in acquiring and motivating high-class or diverse human resources.58-60
Everything has its pros and cons. It may also be said that the reason the prevention of epidemics in Japan, especially in local cities, looks more successful than some other countries so far is that the good aspects of the Japanese as an inakamono (countryman) works. Cultivating a spirit that is open to others while at the same time strengthening unity is the right way to manage crises in a global society. The national and local governments, schools, and workplaces must work in tandem to achieve this goal.
Implication
In this study, cross-section analysis using prefecture-level data in Japan showed that social capital, in addition to low population density, plays an important role in preventing COVID-19. These findings can be utilized not only for the measures for the next wave of COVID-19 expected shortly but also for the preventive measures for various infectious viruses in the future. If social capital is more effective at controlling infection than low population density, it should be possible to prevent infections in a big city like Tokyo. For example, it may be effective to make friends who encourage people to stop doing things that are at high risk of infection, such as a dinner or entertainment with many people. Here, the community of familiar human bonds and morals that the countryside has should be referred to, although it is important to maintain a sense of balance as social capital has a negative side that encourages the exclusion of infected people.
Limitations
First, in this study, we used population density as a proxy variable for social distancing, following previous research.2,3 However, the real-world practices a social distancing that cannot be supplemented by population density, such as avoiding congestion due to staggered hours. Further, the magnitude of these efforts has been shown in previous studies to be influenced by social capital. Therefore, the difference in the definition of social distancing does not seem to significantly change the main conclusion of this study. Second, a huge limitation would be the small size of the sample. If the infection rate, social capital, and social distancing data with smaller units can be obtained, we can verify the reproducibility of the results of this study in future research.
Further, this study adopted a cross-section analysis indicating a correlation between population density, social capital, and infection rate. Future studies should examine the results of this study longitudinally to reveal more causal relationships. Comparison of the strength of the correlation by controlling age indicated that social capital showed a higher correlation with infection rate than population density. However, variables not covered in this study may have affected the relationship between these variables. In this sense, previous studies have shown that metrological factors,61,62 pollution,63,64 government policies,65 etc., correlate with infection rates. Studies in Japan have also shown that weather factors were associated with the spread of COVID-19.2,3,66 In the future, these variables should be included while verifying the analytical model presented in this study. Similarly, future studies should address the impact of governmental policies and guidelines on people’s behavior and infection rates, although they were not compulsory in Japan.
Conclusion
The threat of the COVID-19 is increasing. Regarding the differences in the infection rate observed in each region, in addition to studies investigating the cause of differences in population density as a proxy for social distancing, there is an increasing trend toward studies investigating the cause of differences in social capital. However, studies have not yet investigated whether social capital that controls the effect of population density could influence the infection rate. Therefore, in this study, we analyzed the relationship between infection rate, population density, and social capital using statistical data of each prefecture in Japan. Statistical analysis showed that social capital not only correlates with infection rates and population densities but also has a negative correlation with infection rates controlling for the effects of population density. Besides, controlling the relationship between variables by mean age showed that social capital had a greater correlation with infection rate than population density. In other words, social capital mediates the correlation between population density and infection rates, meaning that social distancing alone is not enough to deter COVID-19, and social capital needs to be recharged.
Acknowledgments
The authors thank the members of Economic Research Institute for discussions about social capital and COVID-19 prevalence. The earlier version of this treatise is published on the following preprint server. https://arxiv.org/abs/2007.09939
Footnotes
Author Contributions: K.K. performed the data analysis, wrote the main manuscript text, and prepared the figures and tables. Y.Y. conducted the supervisory work and was responsible for funding acquisition and project administration. All authors reviewed and edited the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: This work did not require ethical approval because we use anonymous information that is open to the public.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by JSPS KAKENHI Grant Number JP17H06151.
ORCID iD: Keisuke Kokubun  https://orcid.org/0000-0002-7440-5049
https://orcid.org/0000-0002-7440-5049
References
- 1. Wingfield-Hayes R. Coronavirus: Japan’s mysteriously low virus death rate. BBC News. 2020. Updated July 4 2020. Accessed July 19, 2020. https://www.bbc.com/news/world-asia-53188847
- 2. Kodera S, Rashed EA, Hirata A. Correlation between COVID-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity. Int J Environ Res Public Health. 2020;17(15):5477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rashed EA, Kodera S, Gomez-Tames J, Hirata A. Influence of absolute humidity, temperature and population density on COVID-19 spread and decay durations: multi-prefecture study in Japan. Int J Environ Res Public Health. 2020;17(15):5354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coşkun H, Yıldırım N, Gündüz S. The spread of COVID-19 virus through population density and wind in Turkey cities. Sci Total Environ. 2020;751:141663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gupta A, Gharehgozli A. Developing a machine learning framework to determine the spread of COVID-19 (April 25, 2020). 2020. doi: 10.2139/ssrn.3635211 [DOI] [Google Scholar]
- 6. Pinto AS, Rodrigues CA, Sobrinho CL, et al. Covid-19 epidemic curve in Brazil: a sum of multiple epidemics, whose income inequality and population density in the states are correlated with growth rate and daily acceleration. Preprint. Posted onlineSeptember 14, 2020. medRxiv 20191353. doi: 10.1101/2020.09.09.20191353 [DOI] [Google Scholar]
- 7. Wang J, Tang K, Feng K, Lv W. High temperature and high humidity reduce the transmission of COVID-19. 2020. doi: 10.2139/ssrn.3551767 [DOI] [Google Scholar]
- 8. Cabinet Secretariat. Shingata coronavirus kansensyo taisakuno kihonteki taishohoshin (Basic countermeasure policy for new coronavirus infection control), 2020.3.28 (revised on 2020.5.25), Cabinet Secretariat New Coronavirus Infectious Diseases Control Promotion Office; 2020. Accessed July 17, 2020. https://corona.go.jp/news/ [Google Scholar]
- 9. Coleman JS. Social capital in the creation of human capital. Am J Sociol. 1988;94: S95-S120. [Google Scholar]
- 10. Fukuyama F. Trust: The Social Virtues and the Creation of Prosperity. Vol. 99. Free press; 1995. [Google Scholar]
- 11. Putnam RD. Bowling Alone: The Collapse and Revival of American Community. Simon & Schuster; 2000. [Google Scholar]
- 12. Asri KN, Wiliyanarti PF. Community social capital on fighting dengue fever in suburban Surabaya, Indonesia: a qualitative study. Int J Nurs Sci. 2017;4(4):374-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540-545. [DOI] [PubMed] [Google Scholar]
- 14. Pretty J. Social capital and the collective management of resources. Science. 2003;302(5652):1912-1914. [DOI] [PubMed] [Google Scholar]
- 15. Chuang YC, Huang Y, Tseng KC, Yen CH, Yang LH. Social capital and health-protective behavior intentions in an influenza pandemic. PLoS One. 2015;10(4):e0122970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ronnerstrand B. Social capital and immunization against the 2009 A(H1N1)V pandemic in Sweden. Scand J Public Health. 2013;41(8):853-859. [DOI] [PubMed] [Google Scholar]
- 17. Pitas N, Ehmer C. Social capital in the response to COVID-19. Am J Health Promot. 2020;34(8):942-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Borgonovi F, Andrieu E. Bowling together by bowling alone: social capital and Covid-19. Covid Econ. 2020;17:73-96. [DOI] [PubMed] [Google Scholar]
- 19. Varshney LR, Socher R. COVID-19 growth rate decreases with social capital. Preprint. Posted online April 29, 2020. medRxiv 20077321. doi: 10.1101/2020.04.23.20077321 [DOI] [Google Scholar]
- 20. Bartscher AK, Seitz S, Slotwinski M, Siegloch S, Wehrhöfer N. Social capital and the spread of Covid-19: insights from European countries. CESifo working paper 8346. 2020. [DOI] [PMC free article] [PubMed]
- 21. Kokubun K, Ino Y, Ishimura K. Social capital and resilience make an employee cooperate for coronavirus measures and lower his/her turnover intention. Preprint. Posted online July 23 2020. arXiv:2007.07963 [econ.GN]. https://arxiv.org/abs/2007.07963
- 22. Chung N, Nam K, Koo C. Examining information sharing in social networking communities: applying theories of social capital and attachment. Telemat Inform. 2016;33(1):77-91. [Google Scholar]
- 23. Li Y, Ye F, Sheu C. Social capital, information sharing and performance. Int J Oper Prod Manag. 2014;34(11):1440-1462. [Google Scholar]
- 24. Six B, Zimmeren E, Popa F, Frison C. Trust and social capital in the design and evolution of institutions for collective action. Int J Commons. 2015;9(1):151-176. [Google Scholar]
- 25. Koutsou S, Partalidou M, Ragkos A. Young farmers’ social capital in Greece: trust levels and collective actions. J Rural Stud. 2014;34:204-211. [Google Scholar]
- 26. Mosse D. Collective action, common property, and social capital in South India: an anthropological commentary. Econ Dev Cult Change. 2006;54(3):695-724. [Google Scholar]
- 27. Ostrom E. Collective action and the evolution of social norms. J Econ Perspect. 2003;14(3):137-158. [Google Scholar]
- 28. Kawachi I, Berkman L. Social cohesion, social capital and health. In: Berkman L, Kawachi I, eds. Social Epidemiology. Oxford University Press; 2000:174-190. [Google Scholar]
- 29. Yang L, Ren Y. Moral obligation, public leadership, and collective action for epidemic prevention and control: evidence from the corona virus disease 2019 (COVID-19) emergency. Int J Environ Res Public Health. 2020;17(8):2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hofstede G. Culture’s Consequence. Sage Publications; 1980. [Google Scholar]
- 31. Yamaguchi S. Empirical evidence on collectivism among the Japanese. In Kim U, Triandis HC, Kagitcibasi C, Choi S-C, Yoon G, eds. Individualism and Collectivism: Theory, Method, and Applications. Sage; 1994: 175-188. [Google Scholar]
- 32. Axelrod R. The Evolution of Cooperation. Basic Books Inc; 1984. [Google Scholar]
- 33. Shoji M, Cato S, Iida T, Ishida K, Ito A, McElwain K. COVID-19 and social distancing in the absence of legal enforcement: survey evidence from Japan. MPRA paper 100723. 2020. [Google Scholar]
- 34. Putnam RD. Tuning in, tuning out: the strange disappearance of social capital in America. PS Polit Sci Polit. 1995;28(4):664-683. [Google Scholar]
- 35. Browne W. The Failure of National Rural Policy. Georgetown University Press; 2001. [Google Scholar]
- 36. Brueckner JK, Largey AG. Social interaction and urban sprawl. J Urban Econ. 2008;64(1):18-34. [Google Scholar]
- 37. Dempsey N, Bramley G, Power S, Brown C. The social dimension of sustainable development: defining urban social sustainability. Sustain Dev. 2011;19(5):289-300. [Google Scholar]
- 38. Andrews R. Civic engagement, ethnic heterogeneity, and social capital in urban areas: evidence from England. Urban Aff Rev. 2009;44(3):428-440. [Google Scholar]
- 39. Eriksson R, Rataj M. The geography of starts-ups in Sweden. The role of human capital, social capital and agglomeration. Entrepreneurship Reg Dev. 2019;31(9-10):735-754. [Google Scholar]
- 40. Rupasingha A, Goetz SJ, Freshwater D. The production of social capital in US counties. J Socio Econ. 2006;35(1):83-101. [Google Scholar]
- 41. Veenstra G. Social capital and health (plus wealth, income inequality and regional health governance). Soc Sci Med. 2002;54(6):849-868. [DOI] [PubMed] [Google Scholar]
- 42. Sato Y, Aida J, Tsuboya T, et al. Generalized and particularized trust for health between urban and rural residents in Japan: a cohort study from the JAGES project. Soc Sci Med. 2018;202:43-53. [DOI] [PubMed] [Google Scholar]
- 43. Bai JJ, Jin W, Wan C. The impact of social capital on individual responses to COVID-19 pandemic: evidence from social distancing (June 14, 2020). 2020. doi: 10.2139/ssrn.3609001. [DOI] [Google Scholar]
- 44. Sapporo Medical University. Todohukenbetsu Jinkoatarino Shingata coronavirus Kansenshasuno Suii (Changes in the number of new coronavirus infections per population by prefecture). Department of Genome Medical Science, Frontier Medical Research Institute, Sapporo Medical University; 2020. Accessed July 6, 2020. https://web.sapmed.ac.jp/canmol/coronavirus/japan.html? [Google Scholar]
- 45. The Japan Times News. Tokyo reports 131 COVID-19 cases, topping 100 for third day in a row. 2020. Accessed July 6, 2020. https://www.japantimes.co.jp/news/2020/07/04/national/tokyo-130-coronavirus/
- 46. Statistics Bureau. Shakaiseikatsu tokeisihyo: Todofukenno sihyo, 2020 (Social Life Statistics Index-Prefecture Index-2020). Statistics Bureau, Ministry of Internal Affairs and Communications, Tokyo; 2020. Accessed July 6, 2020. https://www.stat.go.jp/data/k-sugata/naiyou.html [Google Scholar]
- 47. Cabinet Office. Heisei 14 nendo social capital: Yutakana ningenkankeito siminkatsudono kojunkanwo motomete (2002 social capital: in search of rich human relations and a virtuous cycle of civic activities), Civil Affairs Division, National Living Bureau, Cabinet Office; 2003. Accessed July 6, 2020. https://www.npo-homepage.go.jp/toukei/2009izen-chousa/2009izen-sonota/2002social-capital [Google Scholar]
- 48. Statistics Bureau. Heisei 27nen Kokuzeichosa: Todofuken Shichosonbetsu Tokeihyo (2015 Census Statistics Table by Prefecture/City). Statistics Bureau, Ministry of Internal Affairs and Communications; 2017. [Google Scholar]
- 49. Bachman L. Statistical Analyses for Language Assessment. Cambridge University Press; 2004. [Google Scholar]
- 50. Kitayama S, Ishii K, Imada T, Takemura K, Ramaswamy J. Voluntary settlement and the spirit of independence: evidence from Japan’s northern frontier. J Pers Soc Psychol. 2006;91(3):369-384. [DOI] [PubMed] [Google Scholar]
- 51. Yamawaki N. Within-culture variations of collectivism in Japan. J Cross Cult Psychol. 2012;43(8):1191-1204. [Google Scholar]
- 52. Hui CH. Measurement of individualism-collectivism. J Res Pers. 1988;22(1):17-36. [Google Scholar]
- 53. Triandis HC. Individualism-collectivism and personality. J Pers. 2001;69(6):907-924. [DOI] [PubMed] [Google Scholar]
- 54. Beilmann M, Kööts-Ausmees L, Realo A. The relationship between social capital and individualism–collectivism in Europe. Soc Indic Res. 2018;137(2):641-664. [Google Scholar]
- 55. Wu C. Social capital and COVID-19: a multidimensional and multilevel approach. Chin Sociol Rev. 2021;53:27-54. doi: 10.1080/21620555.2020.1814139 [DOI] [Google Scholar]
- 56. Portes A. Social capital: its origins and applications in modern sociology. Annu Rev Sociol. 1998:24(1);1-24. doi: 10.1146/annurev.soc.24.1.1 [DOI] [Google Scholar]
- 57. The Japan Times News. Japan sees rise in harassment, bullying and discrimination linked to COVID-19. 2020. Accessed July 6, 2020. https://www.japantimes.co.jp/news/2020/03/02/national/japan-sees-rise-harassment-bullying-cases-linked-coronavirus-outbreak/
- 58. Keeley TD. International Human Resource Management in Japanese Firms: Their Greatest Challenge. Palgrave; 2001. [Google Scholar]
- 59. Kokubun K. Education, organizational commitment, and rewards within Japanese manufacturing companies in China. Empl Relat. 2018;40(3):458-485. [Google Scholar]
- 60. Kokubun K, Yasui M. The difference and similarity of the organizational commitment–rewards relationship among ethnic groups within Japanese manufacturing companies in Malaysia. Int J Sociol Soc Policy. 2020;40(11/12):1391-1421. [Google Scholar]
- 61. Islam ARMT, Hasanuzzaman M, Azad MAK, et al. Effect of meteorological factors on COVID-19 cases in Bangladesh. Environ Dev Sustain. Published online October 8. 2020. doi: 10.1007/s10668-020-01016-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sarkodie SA, Owusu PA. Impact of meteorological factors on COVID-19 pandemic: evidence from top 20 countries with confirmed cases. Environ Res. 2020;191:110101. doi: 10.1016/j.envres.2020.110101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Cole MA, Ozgen C, Strobl E. Air pollution exposure and Covid-19 in Dutch municipalities. Environ Resour Econ. 2020;76(4):581-610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Zhang Z, Xue T, Jin X. Effects of meteorological conditions and air pollution on COVID-19 transmission: evidence from 219 Chinese cities. Sci Total Environ. 2020;741:140244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020;584(7820):262-267. [DOI] [PubMed] [Google Scholar]
- 66. Azuma K, Kagi N, Kim H, Hayashi M. Impact of climate and ambient air pollution on the epidemic growth during COVID-19 outbreak in Japan. Environ Res. 2020;190:110042. [DOI] [PMC free article] [PubMed] [Google Scholar]