Supplemental Digital Content is Available in the Text.
The trajectories identified show a long-term stability for chronic pain status for most individuals. Clinically relevant early risk factors for pain progression were identified.
Keywords: Chronic pain, Chronic widespread pain, CWP, Musculoskeletal pain, Trajectory
Abstract
Our knowledge of the prevalence, impact, and outcomes of chronic pain in the general population is predominantly based on studies over relatively short periods of time. The aim of this study was to identify and describe trajectories of the chronic pain status over a period of 21 years. Self-reported population data (n = 1858) from 5 timepoints were analyzed. Pain was categorized by: no chronic pain (NCP), chronic regional pain (CRP), and chronic widespread pain (CWP). Latent class growth analysis was performed for identification of trajectories and logistic regression analysis for identification of predictors for pain prognosis. Five trajectories were identified: (1) persistent NCP (57%), (2) migrating from NCP to CRP or CWP (5%), (3) persistent CRP or migration between CRP and NCP (22%), (4) migration from CRP to CWP (10%), and (5) persistent CWP (6%). Age, sleeping problems, poor vitality, and physical function at baseline were associated with pain progression from NCP. Female gender, seeking care for pain, lack of social support, poor physical function, vitality, and mental health predicted poor pain prognosis among those with CRP. In conclusion, chronic pain was common in the population including 6% reporting persistent CWP, although the majority persistently reported NCP. Most people had stable pain status, but some had ongoing change in pain status over time including people who improved from chronic pain. It was possible to identify clinically relevant factors, characterizing trajectories of chronic pain development, that can be useful for identifying individuals at risk and potential targets for intervention.
1. Introduction
Chronic pain, most often involving the musculoskeletal system, affects 40% to 50% of adult populations at any one time.9 Its impact on individuals is extensive in terms of physical restriction and psychological function and on society in terms of lost production and high health care use.13,16,37 Chronic pain in populations falls into 2 broad categories defined by the reported location and extent of pain in the body (regional and widespread). Chronic widespread pain (CWP) is reported to affect 10% of the adult population3,8,31–33 and is associated with greater impact and requires more complex care than chronic regional pain (CRP).6,11,14
Our knowledge and understanding of the prevalence, impact, and outcomes of chronic pain in populations, and its association with a range of markers of poor physical health, psychological distress, and socioeconomic status, is based predominantly on “snapshot” studies over relatively short periods of time. Yet for individuals and society, an important question is not simply the immediate burden of chronic pain, but the pattern of decline or recovery over long periods of time, and what preventable factors might determine these long-term outcomes. One way to investigate this course over time is to identify common trajectories (ie, clusters of individuals who share similar chronic pain symptom experiences over time). A strong body of evidence of long-term trajectory research now exists for specific regional musculoskeletal pain conditions (notably back pain), and this research consistently identifies distinct groups of individuals with different experience of their conditions over time.4,12,17,19,23,28 Such research is clinically informative and relevant for health policy because it highlights groups at high risk of poor long-term outcomes (eg, those with persistent high levels of pain intensity) and identifies factors associated with change (eg, predictive of long-term decline or improvement).27 Furthermore, trajectory research provides a platform to discuss novel or alternative treatment strategies and intervention targets based on likely long-term prognosis.18,25
There is less information on long-term patterns of broad categories of chronic musculoskeletal pain in populations. Specifically, the evolution and course of CWP over time and trajectories of regional and CWP. The pathogenesis of chronic pain is complex, with evidence of biological (regional pain, neuroplastic changes, abnormal muscle tissue, sensitisation, stress response, genetic and familial, comorbidity, sleep, and fatigue), psychological (self-esteem, coping, depression, and anxiety), and social (social isolation, social support, and health care policy) factors associated with onset and prognosis.1,5,10,14,22,35 A few prospective studies have indicated a developmental link between regional pain and CWP onset, suggesting progression from regional pain to CWP.2,8,24,32,33 However, to date, less is known of the developmental sequence and long-term course of CRP and CWP at a population level.
The aim of this study was to identify and describe different longitudinal pain status trajectories over a period of 21 years. The specific objectives were (1) to describe the common long-term trajectories of CRP and CWP and the characteristics of the individuals within those trajectories and (2) determine what factors at baseline are predictive of trajectory group membership.
2. Method
2.1. Study population
This was a 21-year longitudinal cohort study that recruited participants from 2 health care districts (mixed urban and rural population) in Halmstad and Laholm, Sweden (total population 70,704). In total, a representative sample of 3928 people aged 20 to 74 was selected by approaching every 18th woman and 18th man from an age-ordered computerised population register. Of the selected sample, 2425 (62%) responded to an initial baseline postal survey in 1995.7 This sample was followed up and sent a postal survey at 4 subsequent time points in 1998, 2003, 2007, and 2016. All study participants signed informed consent before entering the study. The study was approved by the Regional Ethical Review Board, Faculty of Medicine, University of Lund, Sweden (Dnr 2016/132).
All respondents who had data on pain location from at least 3 of the 5 time points (n = 1858) were included in this analysis (Fig. 1).
Figure 1.
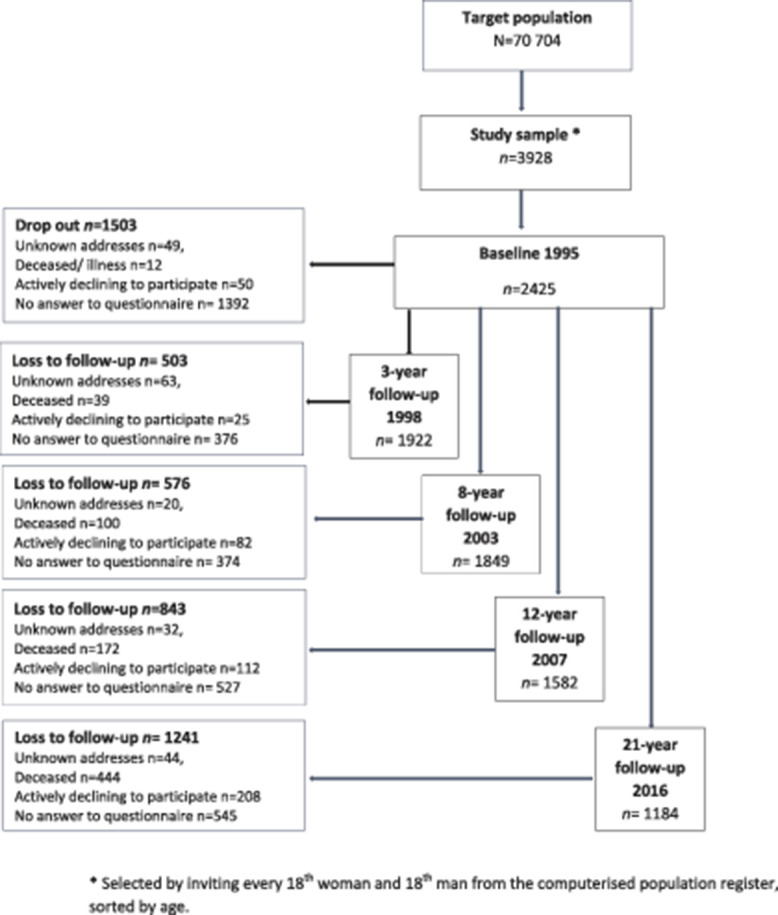
Flow diagram of surveys in the study cohort.
2.2. Outcome
Chronic musculoskeletal pain was defined using the same key item at all 5 time points: have you experienced pain lasting more than 3 months during the last 12 months? The location of the pain was reported using a manikin with 18 predefined bodily regions in the musculoskeletal system; head and abdomen were not included.7,8
Chronic widespread pain was defined according to the American College of Rheumatology 1990 criteria for fibromyalgia39 (pain present in both the left and right side of the body, above and below the waist, and in the axial skeleton lasting for 3 months or more). When chronic pain was present but criteria for a widespread condition were not met, the participant was classified as having CRP. Participants who did not report any chronic pain were categorized as no chronic pain (NCP).
2.3. Baseline covariates
Sleep problems were assessed using the Uppsala Sleep Inventory (USI)29,30: How much of a problem do you have with: (1) falling asleep at night? (2) Waking up during the night? (3) Waking up too early in the morning? (4) Not feeling rested after sleep?
The problems were recorded on a 5-point scale: (1) = no problems, (2) = minor problems, (3) = moderate problems, (4) = severe problems, and (5) = very severe problems. Those who had responded “moderate problems,” “severe problems,” or “very severe problems” were considered to have sleep problems. The cut-off has been used previously by members of the group developing the inventory29 and is in line with our previous study of this cohort.1 The sleeping problems were further categorized by the number of reported sleeping problems (0-4) according the definition above. Three categories of sleeping problems were used for analyses: 0 sleeping problems, 1 sleeping problem, and 2 or more sleeping problems.
The health status was assessed by SF-36 health survey in its Swedish standard version36 including 8 subscales ranging from 0 to 100, where a higher score indicates better health. The subscales assessing physical function, vitality, and mental health were included in this study. Because of skewed distributions, the variables were dichotomized at the lower tertile score. This resulted in “poor physical function” (score 0-89) and “good physical function” (score 90-100), “poor vitality” (score 0-60) and “good vitality” (score 61-100), and “poor mental health” (score 0-79) and “good mental health” (score 80-100).
The socioeconomic status was classified based on self-reported occupation in 1995, of which 3 groups were formed: manual workers, nonmanual employees (lower/intermediate/higher nonmanual employees and upper-level executives), and others (including self-employed, housewives, and students).34
Care seeking was assessed by the item: how many times have you sought care for pain or ache during the last year? Followed by a list of examples of different care givers (including specialist doctors, physiotherapist, and chiropractor). This was dichotomized into “yes” (have sought care at least once at any of the suggested care givers) or “no” (have not sought care).
Lifestyle factors of smoking (never or previous smoker/smoker), alcohol consumption (never or seldom drinking/once a month/1-2 times per week/daily), and physical activity (do you exercise regularly? -no/yes, 1-2 times per week/more than 2 times per week) were assessed.
The immigrant status, was assessed by the item: have you or your parents moved to Sweden from another country? yes/no.
Social support was assessed by the item do you feel you have one or a few persons who can give you proper personal support to handle stress and problems in life?—yes, for sure/yes, probably/not for sure/no. The variable was categorized into yes (definitely/probably) and no (not sure/no).
2.4. Descriptive
Additional characteristics of the members of the clusters identified were assessed and presented for descriptive purposes, including the SF-36 subscales physical and emotional role function, bodily pain (assessing severity and impact of acute or chronic pain), general health, and social function.
2.5. Statistical analysis
To establish trajectories, participants were included if they had completed information on pain on at least 3 of the 5 time points. Differences between included and excluded (because of missing data from more than 2 time points) participants were assessed using descriptive analysis.
At each time point, participants were categorised based on their pain status: NCP, CRP, and CWP. Latent class growth analysis (LCGA) was performed to identify common patterns (trajectories) of pain over the 21 years. Latent class growth analysis uses the reported pain status over all of the time points to group participants into clusters. Each cluster represents a distinct pattern of pain over time which should reflect that of each participant allocated to that cluster. Participants were assigned to the cluster where their posterior probability of membership was highest (ie, the cluster to which they had the highest probability of belonging based on their individual pattern of pain over time). The optimal number of clusters was determined by considering (1) statistical goodness of fit measures (the smallest Akaike's information criterion or Bayes' information criteria [BIC]) and the Lo-Mendell-Rubin adjusted likelihood test, (2) average posterior probabilities for participants belonging to each cluster (ideally exceeding 0.7), (3) smallest cluster size with a targeted minimum of 10% of participants in a cluster, and (4) interpretation and assessment of the clinical nature of the clusters by the research team. Quadratic growth curves were applied for all clusters identified within the LCGA models.
Clusters were then described across baseline covariates. Differences in covariates between clusters were analysed by analysis of variance for means, Kruskal–Wallis for medians, and χ2 tests for proportions.
Baseline predictors of trajectory clusters were determined by comparing pairs of clusters using binary logistic regression. We compared clusters which were characterised by NCP at baseline (between those with poor prognosis defined by movement to CRP and/or CWP over time and those with good prognosis defined by remaining in NCP over time). We also compared clusters characterised by CRP at baseline to those with poor prognosis defined by progression to CWP and a good prognosis defined by remaining as CRP or improving to NCP. Associations with baseline predictors were adjusted for age and gender.
To establish the impact of missing data, sensitivity analyses were conducted. Differences in baseline characteristics between included with missing data from 0, 1, or 2 time points were investigated, and a LCGA was conducted including only those with complete information at all 5 time points.
M-plus version 8 and SPSS version 24 software programs were used to perform the analyses.
3. Results
The number of respondents at each time point was: baseline n = 2425, 3-year follow-up n = 1992, 8-year follow-up n = 1849, 12-year follow-up n = 1582, and 21-year follow-up n = 1184 (Fig. 1). The analyses in this study included 1858 (77%) individuals who provided data on pain location for at least 3 of the 5 study time points. From the 1858 individuals included in the LCGA analysis, n = 33 had missing data on chronic pain at baseline in 1995, n = 192 had missing data on chronic pain at the 3-year follow-up, n = 135 had missing data on chronic pain at the 8-year follow-up, n = 377 had missing data at the 12-year follow-up, and n = 708 had missing data at the 21-year follow-up.
3.1. Baseline characteristics
Baseline characteristics of those included (n = 1858) and excluded (n = 567 with missing data on pain location from at least 3 of the 5 time points) are presented in Table 1. At baseline, 12.7% of the participants included in the analysis reported CWP and 25.3% had CRP. There were no differences in age and baseline pain status between the 1858 individuals included in the analysis and the 567 individuals excluded. However, those included were more likely to be women (55% vs 47%), Table 1.
Table 1.
Baseline characteristics of those included and excluded.
| Baseline characteristics | Included, N = 1858 | Not included (<3 of 5 time points), N = 567 |
|---|---|---|
| Age; mean (SD) | 46.3 (14.6) | 46.8 (17.7) |
| Female gender; n (%) | 1027 (55.3) | 266 (46.9) |
| Number of pain regions; mean (SD) | 1.9 (3.3) | 2.1 (3.6) |
| Pain group*; n (%) | ||
| NCP | 1133 (62.1) | 333 (62.6) |
| CRP | 461 (25.3) | 127 (23.9) |
| CWP | 231 (12.7) | 72 (13.5) |
| No of sleep problems | ||
| 0 | 934 (52.9) | 248 (47.9) |
| 1 | 308 (17.4) | 79 (15.3) |
| ≥2 | 525 (29.7) | 191 (36.9) |
| Socioeconomic status by work; n (%) | ||
| Nonmanual | 761 (41.0) | 162 (28.6) |
| Manual | 866 (46.6) | 301 (53.1) |
| Others† | 231 (12.4) | 104 (18.3) |
| Physical function; n (%) | ||
| Good | 1270 (70.1) | 305 (57.9) |
| Poor | 541 (29.9) | 222 (42.1) |
| Vitality; n (%) | ||
| Good | 1206 (65.9) | 308 (56.4) |
| Poor | 623 (34.1) | 238 (43.6) |
| Mental health; n (%) | ||
| Good | 1246 (68.1) | 307 (56.2) |
| Poor | 583 (31.9) | 239 (43.8) |
| Care seek pain; n (%) | ||
| Yes | 687 (43.5) | 206 (45.2) |
| No | 893 (56.5) | 250 (54.8) |
| Social support; n (%) | ||
| Yes/yes probably | 1611 (87.1) | 456 (82.3) |
| No/not sure | 238 (12.9) | 98 (17.7) |
Based on full pain report at baseline for those included (n1825) and not included (n532).
† Others include self-employed, housewives, and students.
CRP, chronic regional pain; CWP, chronic widespread pain; NCP, no chronic pain.
Among those included, n 835 responded at all 5 time points. In general, they were younger and rated over all better health, regarding baseline characteristics (table S1, in appendix, available at http://links.lww.com/PAIN/B224). Those with missing data at the 21-year follow-up (time point 4) were in general older and rated overall poorer health than those who did not have missing data at time point 4 (table S2, in appendix, available at http://links.lww.com/PAIN/B224).
3.2. Identified trajectories
Results from the LCGA showed that the optimal number of clusters was either 4 or 5. Both the 4-cluster and 5-cluster models identified a “persistent NCP” and a “persistent CWP” cluster. The 5-cluster model was optimal based on the BIC test (Table 2). The smallest cluster size of the 5-cluster model was 5% vs 6% in the four-cluster model, and it had 1 cluster with average posterior probability less than 0.7 (lowest value in the 4-cluster model was 0.714). However, the 5 cluster model was determined as more clinically meaningful than the 4-cluster solution because it reflected 4 different but typical clinical patterns (persistent NCP, persistent CWP, persistent CRP, and migration from CRP to CWP) and an important change trajectory (eg, NCP to CRP or CWP).
Table 2.
Statistical goodness of fit for the optimal number of clusters from latent class growth analysis models.
| No. of clusters | Log likelihood | BIC | AIC | LMR, P |
|---|---|---|---|---|
| 2 | −6543.774 | 13,147.766 | 13,103.548 | <0.001 |
| 3 | −6398.835 | 12,887.998 | 12,821.671 | <0.001 |
| 4 | −6367.397 | 12,855.231 | 12,766.795 | <0.001 |
| 5 | −6349.154 | 12,848.852 | 12,738.307 | 0.1381 |
| 6 | −6341.450 | 12,863.555 | 12,730.901 | 0.0384 |
AIC, Akaike's information criterion; BIC, Bayes' information criteria; LMR, Lo-Mendel Rubin adjusted likelihood test.
The average posterior probabilities for participation in the 5 identified clusters were 0.617 to 0.898 (the 4-cluster model had average posterior probabilities between 0.714 and 0.927). The cluster identified as including those who typically migrated from NCP to CRP or CWP was the smallest (5% of the sample) and had the lowest average posterior probability for belonging in a trajectory (0.617).
The mean probabilities for each pain categorisation related to cluster membership in the 5-cluster model are shown in Table 3, and their clinical characterisations were as follows:
(1) Persistent NCP (N = 1052; 57%): typically reporting NCP throughout the 21 years of follow-up. Probability of NCP from 0.88 (baseline) to 0.73 (timepoint 4). 499 (47%) of participants allocated to this cluster reported NCP at all (3-5) included timepoints.
(2) Migrating from NCP to CRP/CWP (N = 92; 5%): high probability of reporting NCP at baseline (0.97) and at timepoint 1 (0.85). The probability of reporting CRP and CWP then increased (from 0.16 at time point 1-0.90 at time point 4), indicating a migration from NCP to CRP or CWP over time.
(3) Persistent CRP or Migration between CRP and NCP (N = 411; 22%): highest mean probability of reporting CRP at baseline and subsequent timepoints. At timepoint 4 however, the probability of reporting NCP within the cluster increased (from 0.29 at baseline to 0.42), suggesting that the cluster is describing both persistent CRP over time and migration between CRP and NCP over time.
(4) Migration from CRP to CWP (N = 184; 10%): high probability of reporting CRP at baseline (0.59) and at timepoint one (0.56), but the probability of reporting CWP increased from timepoint 2 onward (0.48-0.78), indicating that members of this cluster generally migrated from CRP to CWP over time.
(5) Persistent CWP (N = 119; 6%): highest probability of reporting CWP throughout the entire 21-year study period (range 0.82-0.99). 86 participants (72%) allocated to this cluster reported CWP at all (3-5) included timepoints.
Table 3.
Mean probabilities of each pain type at each time point, by cluster.
| Persistent NCP | Migration from NCP to CRP/CWP | Persistent CRP or migration between CRP and NCP | Migration from CRP to CWP | Persistent CWP | |
|---|---|---|---|---|---|
| No. (%) | 1052 (57) | 92 (5) | 411 (22) | 184 (10) | 119 (6) |
| BL (1995) | |||||
| NCP | 0.888 | 0.973 | 0.287 | 0.188 | 0.001 |
| CRP | 0.103 | 0.025 | 0.571 | 0.589 | 0.008 |
| CWP | 0.008 | 0.002 | 0.141 | 0.223 | 0.991 |
| T1 (1998) | |||||
| NCP | 0.882 | 0.845 | 0.272 | 0.127 | 0.002 |
| CRP | 0.109 | 0.143 | 0.577 | 0.559 | 0.026 |
| CWP | 0.009 | 0.012 | 0.151 | 0.314 | 0.972 |
| T2 (2003) | |||||
| NCP | 0.863 | 0.338 | 0.271 | 0.067 | 0.008 |
| CRP | 0.126 | 0.547 | 0.578 | 0.454 | 0.098 |
| CWP | 0.010 | 0.115 | 0.152 | 0.479 | 0.894 |
| T3 (2007) | |||||
| NCP | 0.838 | 0.135 | 0.290 | 0.043 | 0.015 |
| CRP | 0.149 | 0.567 | 0.570 | 0.358 | 0.170 |
| CWP | 0.013 | 0.298 | 0.140 | 0.599 | 0.815 |
| T4 (2016) | |||||
| NCP | 0.728 | 0.101 | 0.415 | 0.018 | 0.013 |
| CRP | 0.248 | 0.527 | 0.500 | 0.202 | 0.153 |
| CWP | 0.024 | 0.372 | 0.086 | 0.779 | 0.834 |
CRP, chronic regional pain; CWP, chronic widespread pain; NCP, no chronic pain.
The patterns of mean number of pain sites reported on the manikin over the 21-year follow-up in the different clusters, presented in Figure 2, support the pain trajectories identified by the LCGA and the interpretation of the mean probabilities for the pain groups related to the identified clusters.
Figure 2.
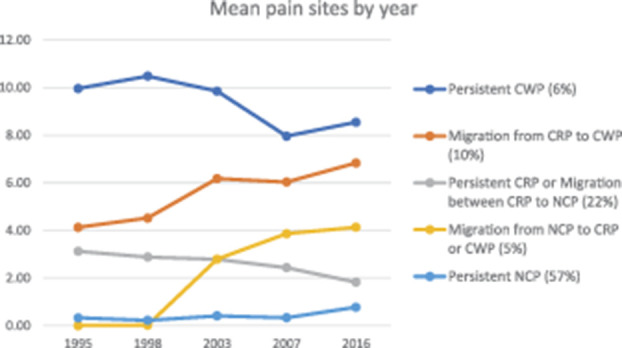
Mean number of pain sites for each cluster over the 5 time points. CRP, chronic regional pain; CWP, chronic widespread pain; NCP, no chronic pain.
3.3. Characteristics of the participants of the clusters
The identified clusters differed in most baseline characteristics investigated, including age, gender, sleep, socioeconomic status (by work), alcohol habits, migrant status, all dimensions of the SF-36, mean number of pain regions, care seeking behaviour, and social support. There was less difference between the clusters regarding smoking and regular exercise. Among the women, 8.6% belonged to the persistent CWP cluster, as compared with 3.7% of men (Table 4).
Table 4.
Baseline characteristics of the study participants grouped by cluster membership.
| Persistent NCP | Migration from NCP to CRP/CWP | Persistent CRP or migration between CRP and NCP | Migration from CRP to CWP | Persistent CWP | P* | |
|---|---|---|---|---|---|---|
| N | 1052 | 92 | 411 | 184 | 119 | |
| Age group n (%) | ||||||
| 20-29 | 233 (22) | 10 (11) | 41 (10) | 18 (10) | 6 (5) | <0.001 |
| 30-39 | 201 (19) | 20 (22) | 60 (15) | 35 (19) | 11 (9) | |
| 40-49 | 229 (22) | 31 (34) | 90 (22) | 43 (23) | 24 (20) | |
| 50-59 | 215 (20) | 17 (19) | 101 (25) | 44 (24) | 33 (28) | |
| 60-74 | 174 (17) | 14 (15) | 119 (29) | 44 (24) | 45 (38) | |
| Gender n (%) | ||||||
| Female | 543 (52) | 50 (54) | 227 (55) | 119 (65) | 88 (74) | <0.001 |
| Male | 509 (48) | 42 (46) | 184 (45) | 65 (35) | 31 (26) | |
| Problem with sleep: n (%) | ||||||
| Initiating sleep | 138 (14) | 15 (17) | 121 (30) | 60 (33) | 56 (48) | <0.001 |
| Maintaining sleep | 173 (17) | 22 (24) | 186 (47) | 87 (48) | 84 (72) | <0.001 |
| Non-restorative sleep | 183 (18) | 26 (29) | 159 (41) | 98 (55) | 87 (74) | <0.001 |
| Early awakening | 118 (12) | 19 (21) | 128 (33) | 62 (35) | 62 (54) | <0.001 |
| No of sleep problems n (%) | ||||||
| 0 | 678 (67) | 49 (54) | 139 (36) | 53 (30) | 15 (13) | <0.001 |
| 1 | 168 (17) | 18 (20) | 74 (19) | 37 (21) | 11 (10) | |
| ≥2 | 158 (16) | 23 (26) | 172 (45) | 86 (49) | 86 (77) | |
| Socioeconomic status by work n (%) | ||||||
| Nonmanual | 474 (45) | 42 (46) | 155 (38) | 59 (32) | 31 (26) | <0.001 |
| Manual | 431 (41) | 42 (46) | 208 (51) | 110 (60) | 75 (63) | |
| Others† | 147 (14) | 8 (9) | 48 (12) | 15 (8) | 13 (11) | |
| Alcohol n (%) | ||||||
| Never or seldom | 301 (29) | 26 (28) | 152 (37) | 79 (43) | 66 (55) | <0.001 |
| Once a month | 469 (45) | 40 (44) | 162 (40) | 69 (38) | 32 (27) | |
| 1-2 times per week or daily | 278 (26) | 26 (28) | 96 (23) | 35 (19) | 18 (15) | |
| Smoking n (%) | ||||||
| Never/previous smoker | 849 (81) | 74 (80) | 323 (79) | 136 (74) | 90 (76) | 0.197 |
| Smoker | 198 (19) | 18 (20) | 86 (21) | 48 (26) | 28 (24) | |
| Immigrant n (%) | <0.001 | |||||
| Yes | 85 (8) | 13 (14) | 41 (10) | 27 (15) | 27 (23) | |
| No | 961 (92) | 79 (86) | 366 (90) | 157 (85) | 90 (77) | |
| Regular exercise n (%) | ||||||
| No | 425 (41) | 36 (40) | 182 (45) | 85 (46) | 41 (35) | 0.631 |
| Yes, 1-2 times/week | 373 (36) | 32 (36) | 133 (33) | 59 (32) | 48 (41) | |
| Yes, >2 times/week | 243 (23) | 22 (24) | 94 (23) | 39 (21) | 27 (23) | |
| SF36 mean (sd) | ||||||
| Physical function | 93.9 (11.2) | 91.0 (13.9) | 81.8 (18.9) | 77.5 (20.0) | 58.0 (24.1) | <0.001 |
| Role function, physical | 91.8 (23.0) | 85.7 (31.7) | 70.2 (39.1) | 58.4 (40.5) | 37.9 (41.6) | <0.001 |
| Bodily pain | 84.9 (19.8) | 81.1 (23.1) | 57.3 (21.6) | 51.1 (21.2) | 36.1 (17.7) | <0.001 |
| General health | 83.9 (16.3) | 78.5 (18.6) | 67.1 (22.1) | 58.9 (22.5) | 44.5 (20.8) | <0.001 |
| Vitality | 76.4 (19.0) | 69.6 (21.9) | 62.6 (22.1) | 52.9 (24.1) | 39.9 (21.3) | <0.001 |
| Social function | 93.9 (14.1) | 89.5 (19.5) | 86.8 (21.1) | 78.9 (24.9) | 67.5 (26.8) | <0.001 |
| Role function, emotional | 91.7 (23.0) | 83.9 (31.0) | 79.2 (35.1) | 69.5 (40.4) | 60.2 (40.7) | <0.001 |
| Mental health | 86.0 (15.2) | 80.6 (18.3) | 78.2 (19.4) | 70.1 (21.9) | 64.8 (21.7) | <0.001 |
| No. of pain regions (0-18) | ||||||
| Mean (SD) | 0.3 (1.2) | 0.0 (0.0) | 3.1 (2.8) | 4.1 (3.0) | 10.0 (3.7) | <0.001 |
| Median (IQR) | 0 (0) | 0 (0) | 3 (4) | 4 (4) | 9 (5) | |
| Care seek pain n (%) | ||||||
| Yes | 305 (32) | 31 (37) | 188 (59) | 98 (69) | 65 (82) | <0.001 |
| No | 650 (68) | 53 (63) | 131 (41) | 45 (32) | 14 (18) | <0.001 |
| Social support n (%) | ||||||
| Yes/yes probably | 952 (91) | 79 (88) | 348 (85) | 140 (77) | 92 (78) | <0.001 |
| No/not sure | 97 (9) | 11 (12) | 62 (15) | 42 (23) | 26 (22) |
Differences in covariates between clusters were analysed by ANOVA for means, Kruskal–Wallis for medians, and chi-square tests for proportions.
Others include self-employed, housewives, and students.
ANOVA, analysis of variance; CRP, chronic regional pain; CWP, chronic widespread pain; NCP, no chronic pain.
3.4. Predictors for pain prognosis
3.4.1. Predictors associated with prognostic path: no chronic pain to chronic regional pain or CWP
In a crude unadjusted model, entering each predictor separately, being 30 to 39 or 40 to 49 year old, reporting at least 2 of the sleeping problems, poor physical function, and poor vitality were significantly associated with membership of the trajectory “migrating from NCP to CRP or CWP” compared with “persistent NCP.” Being an immigrant had a borderline association with membership of the trajectory. In an age and gender adjusted model, these predictors remained significant. Regarding the other predictors investigated, the trend was similar in both the crude and the age/gender adjusted model. Poor mental health was close to significant, and gender, care seeking, consuming alcohol at least weakly, smoking, social support, and manual work showed a tendency of association (ORs above 1) with poor prognosis, although nonsignificant (Table 5).
Table 5.
Associations with migrating from NCP to CRP or CWP compared with belonging to cluster Persistent NCP.
| N | Crude | Age and gender adjusted | |||
|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||
| Age | 1144 | ||||
| 20-29 | 1 | 1 | |||
| 30-39 | 2.32 | 1.06-5.07* | 2.33 | 1.06-5.09* | |
| 40-49 | 3.15 | 1.51-6.58* | 3.16 | 1.51-6.59* | |
| 50-59 | 1.84 | 0.83-4.11 | 1.86 | 0.83-4.16 | |
| 60-74 | 1.88 | 0.81-4.32 | 1.88 | 0.82-4.33 | |
| Gender | 1144 | ||||
| Male | 1 | 1 | |||
| Female | 1.12 | 0.73-1.71 | 1.16 | 0.73-1.72 | |
| Sleep problems | 1094 | ||||
| 0 | 1 | 1 | |||
| 1 problem | 1.48 | 0.84-2.61 | 1.53 | 0.86-2.70 | |
| ≥2 problems | 2.01 | 1.19-3.40* | 1.94 | 1.13-3.31* | |
| Care seeking | 1039 | ||||
| No | 1 | 1 | |||
| yes | 1.25 | 0.78-1.98 | 1.29 | 0.81-2.05 | |
| Alcohol | 1140 | ||||
| Never/seldom | 1 | 1 | |||
| Once a month | 0.99 | 0.59-1.65 | 0.99 | 0.58-1.69 | |
| 1-2 times/week or daily | 1.08 | 0.61-1.91 | 1.07 | 0.59-1.95 | |
| Smoking | 1139 | ||||
| No | 1 | 1 | |||
| Previously | 1.33 | 0.81-2.19 | 1.19 | 0.71-1.99 | |
| Yes | 1.14 | 0.65-2.01 | 1.07 | 0.60-1.89 | |
| Immigrant | 1138 | ||||
| No | 1 | 1 | |||
| Yes | 1.86 | 0.99-3.48 | 1.89 | 1.00-3.58* | |
| Exercise | 1131 | ||||
| >2 times/week | 1 | 1 | |||
| 1-2 times/week | 0.95 | 0.54-1.67 | 0.87 | 0.49-1.54 | |
| No | 0.94 | 0.54-1.63 | 0.91 | 0.51-1.62 | |
| Social support | 1139 | ||||
| Yes/probably | 1 | 1 | |||
| No/not sure | 1.37 | 0.70-2.66 | 1.23 | 0.63-2.40 | |
| Socioeconomic status | 1144 | ||||
| Nonmanual work | 1 | 1 | |||
| Manual work | 1.10 | 0.70-1.72 | 1.21 | 0.77-1.91 | |
| Others† | 0.61 | 0.28-1.34 | 0.77 | 0.35-1.71 | |
| Physical function | 1122 | ||||
| Good | 1 | 1 | |||
| Poor | 1.75 | 1.04-2.94* | 1.85 | 1.06-3.22* | |
| Vitality | 1133 | ||||
| Good | 1 | 1 | |||
| Poor | 1.84 | 1.15-2.94* | 1.75 | 1.09-2.83* | |
| Mental health | 1133 | ||||
| Good | 1 | 1 | |||
| Poor | 1.57 | 0.98-2.52 | 1.53 | 0.95-2.48 | |
P < 0.05.
† Others include self-employed, housewives, and students.
CRP, chronic regional pain.
3.4.2. Predictors associated with prognostic path: chronic regional pain to CWP
In a crude unadjusted model, entering each predictor separately, female gender, seeking care for pain during the last 12 months, lack of social support, poor physical function, poor vitality, and poor mental health predicted membership of the trajectory “migration from CRP to CWP” compared with “persistent CRP or migration between CRP and NCP.” Being a manual worker was close to significant. In an age and gender adjusted model, these predictors remained significant, but also being a manual worker was significantly associated with migration to CWP. Age 30 to 49 years of age, having sleep problems, smoking, and being an immigrant showed a tendency of association with poor prognosis in both the crude and the age/gender adjusted model, although nonsignificant (Table 6).
Table 6.
Associations with “migration from CRP to CWP” compared with “persistent CRP or migration between CRP and NCP.”
| N | Crude | Age and gender adjusted | |||
|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | ||
| Age | 595 | ||||
| 20-29 | 1 | 1 | |||
| 30-39 | 1.33 | 0.66-2.66 | 1.32 | 0.66-2.66 | |
| 40-49 | 1.09 | 0.56-2.11 | 1.10 | 0.57-2.14 | |
| 50-59 | 0.99 | 0.51-1.92 | 1.02 | 0.53-1.98 | |
| 60-75 | 0.84 | 0.44-1.62 | 0.87 | 0.45-1.67 | |
| Gender | 595 | ||||
| Male | 1 | 1 | |||
| Female | 1.48 | 1.04-2.13* | 1.46 | 1.02-2.10* | |
| Sleep problems | 561 | ||||
| 0 | 1 | 1 | |||
| 1 problem | 1.31 | 0.79-2.18 | 1.39 | 0.83-2.32 | |
| ≥2 problems | 1.31 | 0.87-1.97 | 1.38 | 0.91-2.10 | |
| Care seeking | 462 | ||||
| No | 1 | 1 | |||
| yes | 1.52 | 1.00-2.30* | 1.55 | 1.02-2.37* | |
| Alcohol | 593 | ||||
| Never/seldom | 1 | 1 | |||
| Once a month | 0.82 | 0.55-1.21 | 0.81 | 0.54-1.22 | |
| 1-2 times/week or daily | 0.70 | 0.44-1.13 | 0.75 | 0.46-1.22 | |
| Smoking | 593 | ||||
| No | 1 | 1 | |||
| Previously | 0.71 | 0.47-1.08 | 0.74 | 0.48-1.13 | |
| Yes | 1.17 | 0.76-1.80 | 1.15 | 0.74-1.79 | |
| Immigrant | 591 | ||||
| No | 1 | 1 | |||
| Yes | 1.54 | 0.91-2.58 | 1.52 | 0.90-2.58 | |
| Exercise | 592 | ||||
| >2 times/week | 1 | 1 | |||
| 1-2 times/week | 1.07 | 0.66-1.73 | 1.07 | 0.67-1.71 | |
| No | 1.13 | 0.72-1.77 | 1.00 | 0.61-1.63 | |
| Social support | 592 | ||||
| Yes/probably | 1 | 1 | |||
| No/not sure | 1.68 | 1.09-2.61* | 1.79 | 1.15-2.80* | |
| Socioeconomic status | 592 | ||||
| Nonmanual work | 1 | 1 | |||
| Manual work | 1.39 | 0.95-2.03 | 1.49 | 1.01-2.20* | |
| Others† | 0.82 | 0.43-1.58 | 0.86 | 0.44-1.67 | |
| Physical function | 575 | ||||
| Good | 1 | 1 | |||
| Poor | 1.85 | 1.29-2.66* | 2.16 | 1.46-3.21* | |
| Vitality | 583 | ||||
| Good | 1 | 1 | |||
| Poor | 2.03 | 1.42-2.91* | 2.06 | 1.43-2.97* | |
| Mental health | 583 | ||||
| Good | 1 | 1 | |||
| Poor | 1.90 | 1.34-2.72* | 1.90 | 1.33-2.72* | |
P < 0.05.
† Others include self-employed, housewives, and students.
CRP, chronic regional pain; NCP, no chronic pain.
3.5. Sensitivity analyses
The sensitivity analysis indicates that the 4-cluster or 5-cluster model was optimal as suggested by BIC and Lo-Mendell-Rubin -p-value (table S3, in appendix, available at http://links.lww.com/PAIN/B224) when analysis was restricted to respondents with data at all time points. The 5 cluster model yielded clusters of a similar nature to the main analysis, with comparable prevalence, although as expected the proportion of those with CWP at all time points is lower in those who have fully completed follow-up in line with the findings shown elsewhere that those lost to follow-up tend to have poorer overall health (Table 1) at baseline (table S4, available at http://links.lww.com/PAIN/B224).
Given the broadly similar pattern of results between this analysis of those with complete follow-up and our main analysis, the latter was retained for the main analysis as reflecting more precise cluster separation.
4. Discussion
We have identified trajectories that describe differing chronic pain status over a long period of time in a general population sample of Swedish adults. A key finding is that just over half of the individuals belonged to a cluster that reported NCP (persistent NCP) over the entire study period. Although a substantial proportion reported persisting chronic regional or widespread pain (28%), those with NCP who migrated to chronic pain status (CRP or CWP) represented only a small proportion (5%), suggesting a relative stability in trajectories over this long period of time. Factors predictive of the migration from NCP to CRP or CWP showed that there were modifiable factors that predicted long-term pain development. These included sleeping problems, poor physical and mental health, poor vitality, care seeking, and lack of social support, all of which may indicate potential targets for intervention.
Overall, the proportions of people with chronic pain status at baseline and within trajectory groups are in line with previous estimates of all chronic pain (∼40%,9) and CWP (∼10%,3). The distribution of chronic pain status also reflected previously reported trends by age. The prevalence estimates previously reported are based on point prevalence or shorter time periods. Our study adds insights into how individuals change in the chronic pain status over a period of 21 years. Furthermore, this study shows that 85% of the population can be expected to be rather stable in their chronic pain status over a long period of time.
More than half of the studied population belonged to a trajectory that in general did not report chronic pain over the entire study period. This was more pronounced in the youngest age groups, which is not surprising given previous studies report an increasing prevalence of chronic pain in middle age.26,31 However, even at older ages between 60 and 74 years, the trajectory with NCP was the most common, representing more than 40% of the participants in this group. This pattern reflects previous findings that the prevalence of chronic pain reaches a plateau at older ages.7,26 It was slightly less common for women to persistently report NCP, a finding supported by previous research reporting a higher prevalence of chronic pain in women.3,21,26,31
Participants migrating from NCP to CRP or CWP were fewer than expected. The interpretation is that this trajectory represents a smaller group of individuals that has a distinct development of chronic pain from an NCP status. Furthermore, because this cohort recruited from (baseline) age groups between 20 and 74, a high proportion already had chronic pain by the time of entry into the study. The highest risk of belonging to the group developing CRP or CWP is seen in age groups below 50 years. Previously published figures from baseline data in this study show a prevalence of over 20% of chronic pain already among 20 to 29 year old.7 The overall image is that long-term patterns of pain are already becoming established by the time adulthood is reached,15,20 and rising age in adulthood increases the likelihood of stable patterns over time.
Both men and women were equally represented in the NCP to CRP/CWP trajectory, which suggests that men and women have equal risks of developing chronic pain. Taking into account the higher prevalence of chronic pain among women reported in population studies,3,21,26,31 this suggests that the higher prevalence is because women are less likely than men to improve from chronic pain conditions over time. Other factors associated with development of CRP or CWP from NCP were sleep problems, being an immigrant, poor physical function, and poor vitality in SF-36 health status. In this trajectory, the migration from NCP to CRP or CWP occurs more than 3 years after baseline, which indicates a window of opportunity for intervention.
Among those reporting CRP at baseline, 2 trajectories were identified—1 including those typically developing CWP, and 1 group who in general reported persistent CRP or migration between CRP and NCP, where belonging to the latter group was more than twice as common. Belonging to the trajectory, developing CWP was less common in the younger age group, but equally common in the age groups of 30 years or older and almost 2 times more common among women than men. This is in line with previous studies reporting higher prevalence of CWP in older age groups and in women.3,21,26,31 Baseline covariates that predicted a poor prognosis were female gender, being care seeking, not having social support, being a manual worker, poor physical function, poor vitality, and poor mental health. The identified predictors are in line with previously reported factors associated with poor prognosis24,27 and CWP,1,2,5,8,10,22,24,26,32 and our study provides novel insights into the associations with long-term chronic pain status and that the risk factors of importance are identifiable early in the pain progression.
This study showed that only 6.4% of the studied population belonged to a cluster with persistent CWP over the entire study period. The prevalence of CWP in the population has previously been consistently estimated at between 10% to 13%.3,8,31–33 However, our analysis introduces a fresh and more detailed perspective on this estimate. We have shown that about half of this group with CWP continue to report CWP over a long time-period of more than 20 years, which indicates a distinct CWP group who appear to have impactful CWP set earlier in life. This persistent CWP trajectory was twice as common among women than men, a finding in line with previous research.3,21,26,31 These results further support the theory that once chronic pain has developed, women have higher risk for poor pain prognosis, including persistence of CWP. Other factors characterizing this trajectory were older age at baseline, sleep problems, being manual workers, drinking alcohol less often, being an immigrant, shorter education, poor health status, care seeking, and low social support. This variety of factors, present already at baseline, further supports the complex aetiology of CWP and the impact CWP has on individuals.5,10,14,35 Further research that considers chronic pain from a life course approach is required to fully understand the factors that lead to the development and persistence of this trajectory.
A major strength of this study is the ability to analyse trajectories of chronic pain status over a longer time-period (21 years) compared with most other studies of trajectories of pain. A review by Kongsted25 considered 10 studies of trajectories for those with back pain, with the maximum timescale for any of these studies being 12 months, although one study did compare time periods separated by 7 years. The much longer timescale in our study gives insight into a life course perspective on the understanding of chronic pain, a perspective that has a growing interest within the pain literature.18,38 Another key strength is the use of a representative general population sample with a reasonable baseline response rate (62%), a reasonable loss to follow-up (50%) given the length of follow-up of 21 years, and no major difference in the pain status at baseline between those included in the analysis and those with missing data who were excluded. We cannot rule out that non-response could have affected the proportion of the population within each of the 5 clusters, but, as identified by the sensitivity analysis, this is unlikely to impact on the nature of the identified clusters. Further strengths are the use of validated measures of chronic pain status including CWP, and the use of a wide range of psychosocial factors examined for their association with chronic pain status trajectories. In addition, this study used a robust analysis approach to determine long-term trajectories of chronic pain and interpreted the results with respect to their clinical applicability and meaningfulness. Limitations include a lack of knowledge of the chronic pain status of participants in the time periods between follow-up points (5 years on average), although the weight of evidence from other pain trajectory studies suggest relative stability over time.25 The low cluster size of the NCP to CRP/CWP cluster and its low average posterior probability suggests this cluster needs further verification in future research. We were able to identify distinct trajectories of chronic pain and the clusters had different baseline characteristics.
5. Conclusion
Although chronic pain is common, the larger proportion in a population is characterized by those persistently reporting NCP over a long period of time. Furthermore, most people with CRP do not develop CWP. This long-term study also shows that there is an ongoing change in pain status over time where people also improve from chronic pain. It is possible to identify factors early on that characterize trajectories of chronic pain development, that are clinically relevant, can be used to identify individuals at risk, and are potential targets for intervention. The fact that 6% of the adult population have CWP that persists over a period of more than 20 years, however, serves as a reminder of the scale of the public health problem and the individual suffering represented by this unchanging group.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Appendix A. Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/B224.
Acknowledgements
This work was supported by a researcher grand from Swedish AFA insurance.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painjournalonline.com).
Contributor Information
Paul Campbell, Email: p.campbell@keele.ac.uk.
Zoe A. Michaleff, Email: zmichale@bond.edu.au.
Vicky Y. Strauss, Email: victoria.strauss@csm.ox.ac.uk.
Kelvin P. Jordan, Email: k.p.jordan@keele.ac.uk.
Ann Bremander, Email: ann.bremander@fou-spenshult.se.
Peter Croft, Email: p.r.croft@keele.ac.uk.
Stefan Bergman, Email: stefan.bergman@fou-spenshult.se.
References
- [1].Aili K, Andersson M, Bremander A, Haglund E, Larsson I, Bergman S. Sleep problems and fatigue as predictors for the onset of chronic widespread pain over a 5- and 18-year perspective. BMC Musculoskelet Disord 2018;19:390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Andersson HI. The course of non-malignant chronic pain: a 12-year follow-up of a cohort from the general population. Eur J Pain 2004;8:47–53. [DOI] [PubMed] [Google Scholar]
- [3].Andrews P, Steultjens M, Riskowski J. Chronic widespread pain prevalence in the general population: a systematic review. Eur J Pain 2018;22:5–18. [DOI] [PubMed] [Google Scholar]
- [4].Axen I, Bodin L, Bergstrom G, Halasz L, Lange F, Lovgren PW, Rosenbaum A, Leboeuf-Yde C, Jensen I. Clustering patients on the basis of their individual course of low back pain over a six month period. BMC Musculoskelet Disord 2011;12:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bergman S. Psychosocial aspects of chronic widespread pain and fibromyalgia. Disabil Rehabil 2005;27:675–83. [DOI] [PubMed] [Google Scholar]
- [6].Bergman S. Management of musculoskeletal pain. Best Pract Res Clin Rheumatol 2007;21:153–66. [DOI] [PubMed] [Google Scholar]
- [7].Bergman S, Herrstrom P, Hogstrom K, Petersson IF, Svensson B, Jacobsson LT. Chronic musculoskeletal pain, prevalence rates, and sociodemographic associations in a Swedish population study. J Rheumatol 2001;28:1369–77. [PubMed] [Google Scholar]
- [8].Bergman S, Herrstrom P, Jacobsson LT, Petersson IF. Chronic widespread pain: a three year followup of pain distribution and risk factors. J Rheumatol 2002;29:818–25. [PubMed] [Google Scholar]
- [9].Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287–333. [DOI] [PubMed] [Google Scholar]
- [10].Burri A, Ogata S, Vehof J, Williams F. Chronic widespread pain: clinical comorbidities and psychological correlates. PAIN 2015;156:1458–64. [DOI] [PubMed] [Google Scholar]
- [11].Carnes D. Patterns of chronic pain in the population. Int J Osteopathic Med 2011;14:81–5. [Google Scholar]
- [12].Chen Y, Campbell P, Strauss VY, Foster NE, Jordan KP, Dunn KM. Trajectories and predictors of the long-term course of low back pain: cohort study with 5-year follow-up. PAIN 2018;159:252–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cieza A, Stucki G, Weigl M, Kullmann L, Stoll T, Kamen L, Kostanjsek N, Walsh N. ICF Core Sets for chronic widespread pain. J Rehabil Med 2004(44 suppl):63–8. [DOI] [PubMed] [Google Scholar]
- [14].Clauw DJ, Crofford LJ. Chronic widespread pain and fibromyalgia: what we know, and what we need to know. Best Pract Res Clin Rheumatol 2003;17:685–701. [DOI] [PubMed] [Google Scholar]
- [15].Coenen P, Smith A, Paananen M, O'Sullivan P, Beales D, Straker L. Trajectories of low back pain from adolescence to young adulthood. Arthritis Care Res 2017;69:403–12. [DOI] [PubMed] [Google Scholar]
- [16].Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, Kerns R, Von Korff M, Porter L, Helmick C. Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep 2018;67:1001–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Dunn KM, Campbell P, Jordan KP. Long-term trajectories of back pain: cohort study with 7-year follow-up. BMJ Open 2013;3:e003838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Dunn KM, Hestbaek L, Cassidy JD. Low back pain across the life course. Best Pract Res Clin Rheumatol 2013;27:591–600. [DOI] [PubMed] [Google Scholar]
- [19].Dunn KM, Jordan K, Croft PR. Characterizing the course of low back pain: a latent class analysis. Am J Epidemiol 2006;163:754–61. [DOI] [PubMed] [Google Scholar]
- [20].Dunn KM, Jordan KP, Mancl L, Drangsholt MT, Le Resche L. Trajectories of pain in adolescents: a prospective cohort study. PAIN 2011;152:66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gran JT. The epidemiology of chronic generalized musculoskeletal pain. Best Pract Res Clin Rheumatol 2003;17:547–61. [DOI] [PubMed] [Google Scholar]
- [22].Gupta A, Silman AJ, Ray D, Morriss R, Dickens C, MacFarlane GJ, Chiu YH, Nicholl B, McBeth J. The role of psychosocial factors in predicting the onset of chronic widespread pain: results from a prospective population-based study. Rheumatology 2007;46:666–71. [DOI] [PubMed] [Google Scholar]
- [23].Kent P, Kongsted A. Identifying clinical course patterns in SMS data using cluster analysis. Chiropractic Man Therap 2012;20:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kindler LL, Jones KD, Perrin N, Bennett RM. Risk factors predicting the development of widespread pain from chronic back or neck pain. J Pain 2010;11:1320–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kongsted A, Kent P, Axen I, Downie AS, Dunn KM. What have we learned from ten years of trajectory research in low back pain? BMC Musculoskelet Disord 2016;17:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Landmark T, Romundstad P, Butler S, Kaasa S, Borchgrevink P. Development and course of chronic widespread pain: the role of time and pain characteristics (the HUNT pain study). PAIN 2019;160:1976–81. [DOI] [PubMed] [Google Scholar]
- [27].Larsson B, Björk J, Börsbo B, Gerdle B. A systematic review of risk factors associated with transitioning from regional musculoskeletal pain to chronic widespread pain. Eur J Pain 2012;16:1084–93. [DOI] [PubMed] [Google Scholar]
- [28].Leino-Arjas P, Rajaleid K, Mekuria G, Nummi T, Virtanen P, Hammarstrom A. Trajectories of musculoskeletal pain from adolescence to middle age: the role of early depressive symptoms, a 27-year follow-up of the Northern Swedish Cohort. PAIN 2018;159:67–74. [DOI] [PubMed] [Google Scholar]
- [29].Mallon L, Broman JE, Hetta J. Relationship between insomnia, depression, and mortality: a 12-year follow-up of older adults in the community. Int Psychog 2000;12:295–306. [DOI] [PubMed] [Google Scholar]
- [30].Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med 2002;251:207–16. [DOI] [PubMed] [Google Scholar]
- [31].Mansfield KE, Sim J, Jordan JL, Jordan KP. A systematic review and meta-analysis of the prevalence of chronic widespread pain in the general population. PAIN 2016;157:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].McBeth J, Macfarlane GJ, Hunt IM, Silman AJ. Risk factors for persistent chronic widespread pain: a community-based study. Rheumatology 2001;40:95–101. [DOI] [PubMed] [Google Scholar]
- [33].Papageorgiou AC, Silman AJ, Macfarlane GJ. Chronic widespread pain in the population: a seven year follow up study. Ann Rheum Dis 2002;61:1071–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Statistics Sweden (SCB). Socio-economic classification MIS 1982:4. Available at: https://www.scb.se/en/finding-statistics/statistics-by-subject-area/other/other/other-publications-non-statistical/pong/publications/mis-19824.-socio-economic-classification/. Accessed July 1, 2020. [Google Scholar]
- [35].Smith BH, Macfarlane GJ, Torrance N. Epidemiology of chronic pain, from the laboratory to the bus stop: time to add understanding of biological mechanisms to the study of risk factors in population-based research? PAIN 2007;127:5–10. [DOI] [PubMed] [Google Scholar]
- [36].Sullivan M, Karlsson J, Ware JE, Jr. The Swedish SF-36 Health Survey—I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med 1995;41:1349–58. [DOI] [PubMed] [Google Scholar]
- [37].Turk DC, Fillingim RB, Ohrbach R, Patel KV. Assessment of psychosocial and functional impact of chronic pain. J Pain 2016;17(9 suppl):T21–49. [DOI] [PubMed] [Google Scholar]
- [38].Walco GA. Toward an integrated model of pain over the life course. PAIN 2004;108:207–8. [DOI] [PubMed] [Google Scholar]
- [39].Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P. The American college of rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheum 1990;33:160–72. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/B224.


