As COVID-19 continues to strain public health systems and vaccination programmes race against new variants that might be more transmissible or capable of evading immune responses, the urgent need for simple, accessible, and frequent testing remains. Inexpensive, scalable, and sustainable strategies that allow easily repeatable testing over time need to be made widely available. This is possible by testing saliva.
The gold-standard sample for SARS-CoV-2 detection defaulted to the nasopharyngeal swab because of its role in detection of other upper respiratory tract pathogens. Demand for swabs drove a cascading collapse of supply chains and worsened shortages of personal protective equipment (PPE) required by health-care workers for sample collection. As the need for mass testing and frequent, repeated sampling surged, the urgency for alternative sample types became apparent.
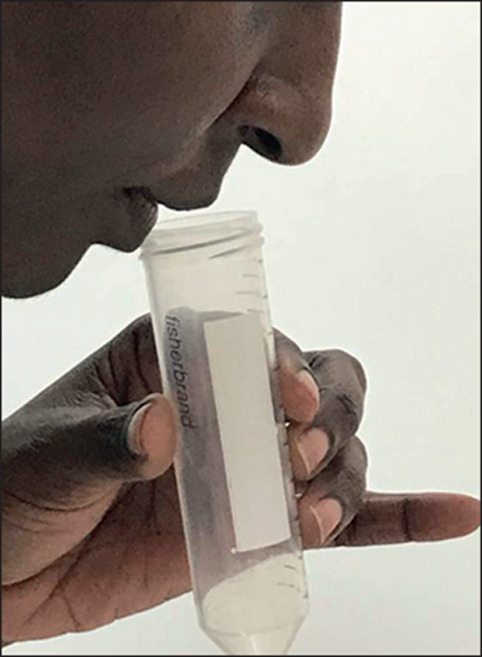
Although not a traditional diagnostic sample type, reports on the use of saliva for SARS-CoV-2 detection emerged within months. Compared with swab-based methods, saliva collection is minimally invasive, can be reliably self-collected without trained personnel,1, 2 and alleviates supply demands on swabs and PPE. As a result, saliva permits more affordable, frequent testing that causes less testing aversion and presents fewer risks to health-care personnel compared with swab-based methods.
Despite enthusiasm for saliva testing, controversy remains surrounding its sensitivity for SARS-CoV-2 detection compared with other tests. Unlike sampling with swabs, collection and processing methods for saliva are largely unstandardised. Therefore, studies evaluating the efficacy of saliva-based SARS-CoV-2 testing have been conflicting and incommensurate, and often unclear or inconsistent about testing procedures and analyses. Much of this variation among studies probably stems from early evaluations of inpatient saliva, which is generally more viscous with higher mucus content, rendering it more difficult to process than general population samples.3 Contradictory reports have hindered regulatory authorisation and widespread adoption of saliva testing.
As successful approaches were replicated, additional evidence for saliva testing emerged. By November, 2020, 58 studies had evaluated SARS-CoV-2 detection in saliva, 54 using RT-PCR, four using reverse transcription loop-mediated isothermal amplification, and three using both (appendix). However, methodological discrepancies between studies led to highly variable detection rates. Most (69%) RT-PCR studies found greater or similar (≤10% difference) sensitivities for saliva compared with nasopharyngeal and other swab-based methods, whereas 7% showed mixed results, with sensitivity differing by population group, stage of infection, or method. Only 24% found saliva to be less sensitive than nasopharyngeal swabs, which suggests that if adequate methods are applied, the effectiveness of saliva-based PCR tests is at least similar to that of swab-based approaches. By contrast, using less robust methods can skew the sensitivities reported across studies. Importantly, saliva detected an additional 10% of positive individuals for whom swabs produced false negative results.
Saliva testing was successfully adopted for SARS-CoV-2 detection in numerous countries, including South Korea, Germany, and Japan.4 In the USA, saliva testing gained traction to facilitate the reopening of educational institutions,5 with its potential for pooling samples for processing,6 enabling sustainable testing programmes.7 As a preferable method for frequent, repeat testing, saliva could be particularly well suited for detecting SARS-CoV-2 during the prodromal phase,8 decreasing risk of further transmission.
As the pandemic evolves, the positive predictive value (PPV) and negative predictive value (NPV) expected from a given sensitivity and specificity in real-world settings vary with infection prevalence. As prevalence declines in a population, NPV increases whereas PPV decreases. However, robust estimates of sensitivity and specificity underpin accurate predictive values for any prevalence. Methodological differences that influence reported sensitivities directly affect predictive values in clinical and community settings. Inconsistent and insufficiently reported methods contribute to incommensurate PPV and NPV estimates.
Saliva-based SARS-CoV-2 testing methods could influence detection rates relative to nasopharyngeal methods for multiple reasons, which include methodological flaws, such as simply substituting saliva in nasopharyngeal-specific extraction methods. Saliva requires different handling to swabs; it is insufficient to merely apply swab-based techniques.
Saliva collection procedures could also affect sample integrity, which influences detection. Studies using methods involving clear saliva (rather than sputum) and processing to reduce viscosity (eg, homogenisation) showed greater sensitivities relative to swabs. Methods requiring forceful production of saliva, such as by spitting or coughing instead of drooling, reduced sensitivity (appendix). Oropharyngeal spitting, in particular, should be discouraged, because the resulting samples are generally thicker and more difficult to process, and the additional steps that are required to reduce viscosity increase risk of cross-contamination. Less-controlled expulsion of saliva (spitting) also increases transmission risk. Furthermore, procedures that involve interfering substances, such as collection devices with cotton or components that inhibit nucleic acid amplification9 and storage tubes that might degrade RNA,10 reduced test sensitivity.
Standardisation of salivary testing methods is necessary to improve detection rates and resolve discrepancies between studies. To facilitate this change, authors should present methodology that is sufficiently detailed to enable replication. Authors should clearly describe both the sample collection and RNA extraction method, including the sample volume from which RNA is extracted and the volume to which RNA is eluted. Such volumes can inform RNA concentration and generate evidence regarding whether this affects detection. Although recent systematic reviews11, 12 found saliva to be an effective sample type, differences in sample preparation and RNA extraction were not assessed; however, these differences are likely to contribute to sensitivity differences.
The stage of infection during sample collection could also contribute to test sensitivity differences. Data suggest that nasopharyngeal swabs can detect historical cases (positive results from the detection of remnant viral material following COVID-19 recovery13), with discordance between paired saliva and nasopharyngeal data more than 21 days from onset, in which nasopharyngeal specimens produced 20–30% more positives than did saliva.14 Early in the pandemic, when there was less testing, studies might have therefore misinterpreted the sensitivity of nasopharyngeal samples relative to saliva. In actuality, the lower tendency of saliva samples to detect long-term shedding relative to nasopharyngeal swabs14 is beneficial; saliva might be preferable for gauging active rather than historical infection. An increasingly accurate indication of infectiousness can avert unnecessarily prolonged isolation periods, which threaten mental health and economic wellbeing. Testing saliva throughout infection could permit shorter isolation, allowing essential workers to return to their duties sooner. Nonetheless, neither saliva nor nasopharyngeal testing should be used alone to determine infectiousness. Testing should contribute to a holistic review of health status, which includes symptom presentation and recovery trajectory.
Just as for SARS-CoV-2 RNA detection, saliva testing is a scalable alternative to blood-based antibody testing, with anti-SARS-CoV-2 antibodies in saliva found to reflect concentrations in serum.15 Thus, a single, non-invasive saliva sample can simultaneously enable the identification of active cases, previous cases, and vaccine-induced immune responses. Although detection of current infection informs isolation measures, antibody testing can elucidate the extent of previous outbreaks and improve understanding of asymptomatic transmission. Combined, these data could facilitate monitoring of both outbreaks and population immune statuses, guiding policy decisions including risk prioritisation for limited doses of vaccine. Importantly, salivary antibody testing provides a scalable means for monitoring herd immunity in a postvaccination world.
Highly sensitive saliva-based SARS-CoV-2 testing methods permit frequent and convenient testing, challenging the nasopharyngeal swab for designation as a gold-standard sample type. Unlike other sample types, saliva is simple to self-collect, and supply chains for mass testing strategies are easier to establish and sustain. Replication of the most successful saliva methods is of paramount importance both to resolving controversy surrounding saliva as a sample type and to facilitating its uptake. Standardised, inexpensive, and broadly implementable saliva-based methods could make frequent, comfortable testing for SARS-CoV-2 a reality for communities globally.
© 2021 Orchid Allicock
We declare no competing interests. MA-H and ALW contributed equally as senior authors.
Supplementary Material
References
- 1.Petrone ME, Yolda-Carr D, Breban M, et al. Usability of saliva collection devices for SARS-CoV-2 diagnostics. medRxiv. 2021 doi: 10.1101/2021.02.01.21250946. published online Feb 4. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wyllie AL, Fournier J, Casanovas-Massana A, et al. Saliva or nasopharyngeal swab specimens for detection of SARS-CoV-2. N Engl J Med. 2020;383:1283–1286. doi: 10.1056/NEJMc2016359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landry ML, Criscuolo J, Peaper DR. Challenges in use of saliva for detection of SARS CoV-2 RNA in symptomatic outpatients. J Clin Virol. 2020;130 doi: 10.1016/j.jcv.2020.104567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oba J, Taniguchi H, Sato M, et al. RT-PCR screening tests for SARS-CoV-2 with saliva samples in asymptomatic people: strategy to maintain social and economic activities while reducing the risk of spreading the virus. Keio J Med. 2021 doi: 10.2302/kjm.2021-0003-OA. published online March 19. [DOI] [PubMed] [Google Scholar]
- 5.Bi C, Mendoza R, Cheng H-T, et al. Pooled surveillance testing program for asymptomatic SARS-CoV-2 infections in K-12 schools and universities. medRxiv. 2021 doi: 10.1016/j.eclinm.2021.101028. https://www.medrxiv.org/content/10.1101/2021.02.09.21251464v1 published online Feb 12. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watkins AE, Fenichel EP, Weinberger DM, et al. Pooling saliva to increase SARS-CoV-2 testing capacity. medRxiv. 2020 doi: 10.1101/2020.09.02.20183830. published online Sept 3. (preprint). [DOI] [Google Scholar]
- 7.Fogarty A, Joseph A, Shaw D. Pooled saliva samples for COVID-19 surveillance programme. Lancet Respir Med. 2020;8:1078–1080. doi: 10.1016/S2213-2600(20)30444-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson AJ, Zhou S, Hoops SL, et al. Saliva testing is accurate for early-stage and presymptomatic COVID-19. medRxiv. 2021 doi: 10.1101/2021.03.03.21252830. published online March 5. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matic N, Stefanovic A, Leung V, et al. Practical challenges to the clinical implementation of saliva for SARS-CoV-2 detection. Eur J Clin Microbiol Infect Dis. 2021;40:447–450. doi: 10.1007/s10096-020-04090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becker D, Sandoval E, Amin A, et al. Saliva is less sensitive than nasopharyngeal swabs for COVID-19 detection in the community setting. medRxiv. 2020 doi: 10.1101/2020.05.11.20092338. published online May 17. (preprint). [DOI] [Google Scholar]
- 11.Butler-Laporte G, Lawandi A, Schiller I, et al. Comparison of saliva and nasopharyngeal swab nucleic acid amplification testing for detection of SARS-CoV-2: a systematic review and meta-analysis. JAMA Intern Med. 2021 doi: 10.1001/jamainternmed.2020.8876. published online Jan 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bastos ML, Perlman-Arrow S, Menzies D, Campbell JR. The sensitivity and costs of testing for SARS-CoV-2 infection with saliva versus nasopharyngeal swabs: a systematic review and meta-analysis. Ann Intern Med. 2021 doi: 10.7326/M20-6569. published online Jan 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li N, Wang X, Lv T. Prolonged SARS-CoV-2 RNA shedding: not a rare phenomenon. J Med Virol. 2020;92:2286–2287. doi: 10.1002/jmv.25952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turner F, Vandenberg A, Slepnev VI, et al. Post-disease divergence in SARS-CoV-2 RNA detection between nasopharyngeal, anterior Nares and saliva/oral fluid specimens—significant implications for policy & public health. bioRxiv. 2021 doi: 10.1101/2021.01.26.21250523. published online Jan 26. [DOI] [Google Scholar]
- 15.Randad PR, Pisanic N, Kruczynski K, et al. COVID-19 serology at population scale: SARS-CoV-2-specific antibody responses in saliva. medRxiv. 2020 doi: 10.1101/2020.05.24.20112300. published online May 26. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


