Abstract
Introduction
A new emerging infectious disease caused by SARS-CoV-2 has caused a global pandemic. Early diagnosis is essential to prevent and halt the spread of the disease, patient management and isolation. In this study, we aimed to reveal correlations between clinical and laboratory findings with chest CT.
Methods
This in an observational case series single center study in a secondary hospital in Jakarta, Indonesia. Patients were included if they had typical symptoms and positive RT-PCR for SARS-CoV-2.
Results
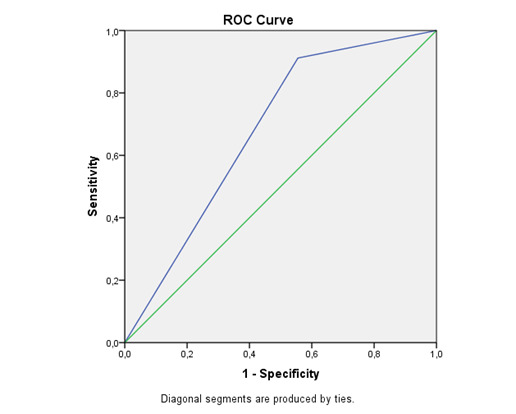
Forty-two patients with positive RT-PCR were included in this study. Typical CT findings were present in 33 (78.6%). We found a positive correlation between patients in whom the imaging was performed after the 4th day of symptoms and chest CT findings (r=0.365 p<0.05). In receiver operating characteristic analysis of this parameter, the area under curve (AUC) was 0.678, and the sensitivity and specificity were 0.96 and 0.44, respectively.
Conclusions
Early diagnosis of COVID-19 is essential to promptly isolate and treat suspected patients. Utilization of chest CT to help diagnosis in this pandemic era needs to be considered by healthcare facilities especially if RT-PCR is limited.
Keywords: Chest computed tomography, COVID-19, diagnosis
Introduction
A novel infectious disease has been reported in a cluster of hospitalized patients in Wuhan, Hubei province, China in late December, 2019. It was later found out that the organism was a novel coronavirus named as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the experts of the International Committee on Taxonomy of Viruses (ICTV), after being formerly called 2019 novel coronavirus (2019-nCoV). The World Health Organization (WHO) announced the disease name as coronavirus-disease-19 (COVID-19), spreading across nations and eventually announced as pandemic.1,2 Indonesia is currently experiencing a surge of cases of COVID-19, which emerged in the capital city Jakarta as the epicenter and spread widely all over the archipelago. Thousands of deaths rapidly caused by this disease have put the national health system under pressure. A recent study from Hafiz et al. describing clinical, laboratory and radiological features of COVID-19 in a secondary hospital in Jakarta showed that the majority of cases were moderate to severe. Early detection of cases is essential to halt the spread, to perform disease management, to reduce healthcare workers’ infection and to quarantine possible contacts from the person under investigation.3,4 Real time reverse transcriptase polymerase chain reaction (RT-PCR) is currently regarded as the gold standard for patients with respiratory symptoms like fever, shortness of breath and cough. Some known limitations for RT-PCR include false negative result, constrained supply-chain and yielding of results several days later; this has prompted us to consider other diagnostic tools. Chest CT imaging has been recognized as an essential tool and a complement to RT-PCR to diagnose COVID-19.5,6 In this study, we evaluated clinical, laboratory features and we aimed to find association with chest CT findings.
Methods
This in an observational case series single center study conducted in the Emergency Department (ED) of Budhi Asih Hospital, East Jakarta, Indonesia from 25 May 2020 to 31 July 2020. We examined 42 patients admitted to the ED with respiratory symptoms (cough, dyspnea), fever, fatigue, myalgia, chest pain, gastrointestinal symptoms (diarrhea, vomiting, abdominal pain or discomfort).7 Laboratory results were obtained immediately during admission. Subsequently all the patients confirmed with COVID-19 by RT-PCR from either nasal or oropharyngeal swab were included in this study. Chest CT was interpreted first by local radiologist then was reread by an outside thoracic radiologist who had experience for about 12 years. In our study, we used the British Society of Thoracic Imaging (BSTI) criteria to consider typical and atypical findings.8,9 Typical findings include ground-glass opacities (GGO), consolidation and crazy paving predominantly in the lower lung zones, bilateral and peripheral. Atypical features include nodules, lung cavitation, pleural effusion, tree in bud (TIB), parenchymal bands, atelectasis and isolated consolidation. This study has been approved by Budhi Asih Hospital ethics committee (No.211/KEP-ETIK/X/2020) with a waiver of informed consent.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) and categorical variables as percentages. Normality of data distribution was checked with the Kolmogorov-Smirnov test. Data which was distributed normally was analyzed with student’s t-test, while Mann-Whitney U test was applied for non-normally distributed data. Differences of percentages between groups were assessed with Chi-square or Fischer’s exact test. Pearson’s or Spearman’s correlation test were applied to conduct correlation analysis. Receiver operating curve (ROC) analysis was performed to determine the sensitivity and specificity of statistically significant variables. A p<0.05 was considered statistically significant.
Results
In our study, a total of 42 patients with confirmed RT-PCR test for COVID-19 were included. The mean age of the patients was 55.9±15.7 years (Table 1), 27 (62.8%) were male and 16 (27.2%) were female. Twenty-four patients (55.8%) had at least one comorbidity, most commonly diabetes n=21 (48.4%), hypertension n=13 (30.2%) and coronary artery disease n=1 (2.3%), respectively. Twenty-four patients (57.1%) had a history of smoking. Symptoms evaluation during admission included fever in n=20 cases (46.5%), shortness of breath n=32 (74.4%), cough n=25 (58.1%), vomiting n=35 (81.4%), fatigue n=9 (20.9%) and myalgia n=40 cases (93%). Basic laboratory findings revealed no statistically significant difference (p>0.05) regarding hemoglobin, leukocyte, thrombocyte, erythrocyte sedimentation rate (ESR), lactate dehydrogenase (LDH), blood sugar, alanine aminotransaminase (ALT), aspartate aminotransaminase (AST) and oxygen saturation. Only C-reactive protein (CRP) almost showed a statistically significant difference between groups (p=0.05). The duration of symptoms was 6.2±1.5 and 5.1±2.7 days for patients with typical and atypical chest CT respectively (p=0.012). A positive correlation was revealed between the presence of chest CT findings and symptoms duration in patients in whom the imaging was performed after the 4th day since symptom onset (r=0.365 p=0.010). Typical CT findings were present in 33 (78.6%) of the typical cases, and in only 9 (21.4%) of the atypical cases. A ROC analysis was performed to determine the correlation between duration of symptoms and diagnosis capability of chest CT. The area under the curve (AUC) was 0.678 (Figure 1), while sensitivity and specificity were 0.96 and 0.44 respectively. Sixteen patients had been admitted to the intensive care unit (ICU) in the follow up. Thirteen patients died (30.9%), while the rest had already been released from isolation.
Table 1. Clinical, laboratory and chest CT findings.
| Variable | Typical | Atypical | p value |
|---|---|---|---|
| Age (years), mean±SD | 54.7±16 | 60.1±14 | 0.373 |
| Gender, n (%) | |||
| Male | 22 (64.7) | 5 (55.6) | 0.446 |
| Female | 12 (35.3) | 4 (44.4) | |
| Number of comorbidities, n (%) | 0.055 | ||
| <2 | 18 (52.9) | 1 (11.1) | |
| ≥2 | 16 (52.9) | 8 (88.9) | |
| Diabetes mellitus, n (%) | 9 (69.2) | 4 (30.8) | 0.257 |
| Hypertension | 15 (71.4) | 6 (28.6) | 0.204 |
| Coronary artery disease, n (%) | 0 | 1(100) | 0.209 |
| Tuberculosis | 1 (20) | 4 (80) | 0.005 |
| Laboratory findings | |||
| Hemoglobin (g/dL) | 13.5±1.8 | 14±1.8 | 0.426 |
| Leucocyte count (m3/µL) | 9.1±4.1 | 7.6±3.1 | 0.309 |
| Thrombocyte count (m3/µL) | 271.9±106.8 | 255.8±75.6 | 0.675 |
| Lymphocytes (%), mean±SD | 13.5±1.8 | 18.2±9.5 | 0.699 |
| Neutrophil:lymphocyte ratio (NLR), mean±SD | 7.3±6.1 | 6.4±6.7 | 0.705 |
| Erythrocyte sedimentation rate (mm/h), median (range) | 52.5 (15-120) | 44 (7-109) | 0.354 |
| Lactate dehydrogenase (U/L), median (range) | 411 (88-2318) | 405 (100-770) | 0.332 |
| C-reactive protein (mg/L), mean±SD | 93±59.7 | 54.1±45.7 | 0.05 |
| Blood sugar level (mg/dL), mean±SD | 148±82.9 | 170.7±89.5 | 0.476 |
| Serum AST (mU/dL), median (range) | 49 (14-208) | 40 (17-53) | 0.245 |
| Serum ALT (mU/dL), median (range) | 29.5 (12-100) | 26 (5-41) | 0.211 |
| PaO2/FiO2, mean±SD | 365.3±183.3 | 272.1±161.1 | 0.173 |
| SaO2 (%), mean±SD | 93.2±6.1 | 93.2±9.5 | 0.995 |
SD – standard deviation.
Figure 1. Receiver operating characteristic curve revealing the relationship between days of symptoms duration and typical CT findings.
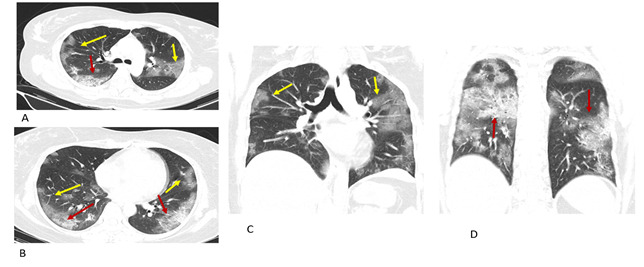
Thirty-three patients (78.6%) had chest CT findings consistent with typical COVID-19 pneumonia (Table 2). The most common typical findings on CT were ground glass opacity (GGO) (Figure 2) in 18 cases (42.9%), consolidation in 13 cases (30.9%) and crazy paving in 5 cases (11.9%), respectively (Table 2). Atypical findings were found in only 9 cases (21.4%). Amongst patients with atypical imaging features we found discrete pulmonary nodules which included both centrilobular and TIB nodular patterns in 7 cases (16.6%), 5 cases (11.9%) with lung cavitation, only 1 case (2.4%) had pleural effusion and parenchymal band was noted in 4 cases (9.5%).
Table 2. Chest CT findings.
| Radiologic pattern | Categories | N=42 (% of total) |
|---|---|---|
| Typical findings | Ground glass opacity | 18 (42.85) |
| Consolidation | 13 (30.9) | |
| Crazy paving | 5 (11.9) | |
| Focality | Unifocal | 18 (42.85) |
| Multifocal | 24 (57.14) | |
| Location | Unilateral | 9 (21.42) |
| Bilateral | 33 (78.57) | |
| Peripheral | 29 (69) | |
| Central | 10 (23.8) | |
| Other findings | Cavitation | 5 (11.9) |
| Tree in bud | 4 (9.52) | |
| Nodules | 3 (7.14) | |
| Pleural effusion | 1 (2.38) | |
| Parenchymal bands | 4 (9.52) | |
| Cardiomegaly | 12 (28.57) | |
| Type of abnormality | Typical | 33 (78.57) |
| Atypical | 9 (21.42) | |
| Severity | Mild | 6 (14.28) |
| Moderate | 24 (57.14) | |
| Severe | 12 (28.57) |
Figure 2. Typical COVID 19. Transverse CT images shows multiple ground-glass opacities (A, B yellow arrow) and mixed ground glass opacities and consolidation in both of the lower lung lobes (A, B, red arrow). Coronal reconstruction CT shows peripheral multifocal GGO (C, D yellow arrow) and consolidation (D red arrow) in both upper and lower lung lobes.
Discussion
COVID-19 is a new emerging infectious disease caused by a novel identified coronavirus SARS-CoV-2 and has an incubation period between 2-14 days. This virus is highly transmissible from person to person mainly via respiratory droplets (cough, sneeze), contaminated surface (fomite) and it was recently revealed that airborne and fecal transmission may be possible. Therefore, early diagnosis is very important to slow the spread of the disease. Early identification of transmissible and infected persons has become mandatory to halt its transmission. Virus nucleic acid real-time RT-PCR testing has been regarded as the current standard diagnostic method but in most health facilities in limited resources settings the turnover time before receiving the results could take several days. Hence, the infected individual has already transmitted the infection to others when the results are disclosed. False negative results of RT-PCR have been detected in some studies despite patients having relevant clinical, laboratory and radiological features typical for SARS-CoV-2 infection.10 The positivity of RT-PCR might be dependent on several factors such as the phase of the disease when the virus may be present in the lower respiratory tract rather than the upper respiratory tract, the collection technique and the transport chain until it is processed, also the possibility of contamination during laboratory diagnosis. The diagnostic dilemma in symptomatic patients with COVID-19 has become a real challenge in this pandemic era. Considering that RT-PCR has several limitations such as delayed result, false negative results and constrained supply chain, it is reasonable to evaluate other diagnostic tool to help identify, treat and isolate patients.
The sensitivity of chest X-ray (CXR) is low in the early phase and mild disease.11 Normal CXR does not rule out COVID-19 and approximately one third of patients presented without abnormality of CXR. The greater sensitivity of CT for early pneumonic changes is more relevant in the setting where healthcare facilities can perform chest CT for suspected symptomatic patients without compromising the safety of medical workers and non-COVID-19 patients. This includes ensuring the personal protective equipment, decontamination of the diagnostic room and appropriate rotation of the patients in a timely manner.12 Chest CT can detect early changes in pulmonary parenchyma, hence the infected individual may be isolated and treat accordingly. Close contacts of the patients might be notified early and commence the self-isolation and monitoring process thereby stopping them from possibility transmitting the infection to other people.13 In this study, we aimed to determine the timing to use chest CT and the relation between typical clinical, laboratory findings and chest CT. For this purpose, we included only RT-PCR positive patients and found positive correlation between the patient’s duration of symptoms and CT findings.
The most common CT findings were GGO with or without consolidation, mostly in lower lung zones. In our study, GGO was found in 18 (42.9%) patients. The appearance of crazy-paving sign on CT is characterized by thickening of the interlobular septa and intralobular lines on the background of the GGO and is not as common as the GGO and consolidations.14 This condition, as in other SARS viruses, is caused by alveolar edema and interstitial inflammation in acute lung tissue impairment and occurs in 5-36% of CT scans.15 In our study, crazy-paving pattern was found in 4 (9.5%) cases. Observation of this sign together with diffuse GGO and consolidations indicates the peak period of the disease. Six patients (14.3%) showed atypical findings on CT. In a study by Sudhir Bhandari et al. on 80 COVID patients revealed that about 2.5% of patients had atypical imaging features on high-resolution CT.16 In another retrospective study on 96 suspected COVID patients by de Jaegere et al. found that amongst 45 RT-PCR positive patients, 2.5-5.3% showed atypical imaging features on high-resolution CT.17 In our study, typical CT findings were present in 33 patients (78.6%), in whom the imaging was performed after the 4th day of symptoms. When this parameter was evaluated by ROC analysis (Figure 2), the AUC, sensitivity, specificity were found to be 0.678, 0.96 and 0.44, respectively (Table 3). Several studies have revealed the relationship between chest CT and duration of symptoms. Kant et al. reported that typical CT findings can be found as early as more than two days from initial symptoms, while an earlier and larger sample study by Bernheim et al. demonstrated that CT findings of early COVID-19 could be found in 0-4 days of symptoms.6,18 Limitations of our study included a small sample size in a single center of a secondary hospital, and the observational design. Nevertheless, our study is the first study in Indonesia to reveal importance of chest CT in early diagnosis of COVID-19.
Table 3. Receiver operating characteristic analysis data obtained to reveal importance of chest CT.
| Parameter | Cut-off | AUC | AUC 95% CI | Sensitivity | Specificity | p value |
|---|---|---|---|---|---|---|
| Duration of symptoms | 4 | 0.678 | 0.457-0.899 | 0,96 | 0.44 | 0.026 |
| Comorbidities | 2 | 0.709 | 0.536-0.883 | 0,47 | 0.11 | 0.055 |
| CRP | 82 | 0.717 | 0.537-0.898 | 0,58 | 0.44 | 0.050 |
CI – confidence interval; CRP = C-reactive protein.
Conclusions
Early diagnosis is essential to promptly isolate and treat suspected patients. RT-PCR is currently regarded as the gold standard but still has some limitations. The literature strongly suggested that chest CT can be beneficial to help diagnose and monitor disease progression. In our study, patients presenting with symptoms duration longer than 4 days in whom clinical and laboratory findings were consistent with COVID-19 had a positive correlation with chest CT. The utilization of chest CT to help diagnosis in this pandemic era needs to be strongly considered by healthcare facilities especially if RT-PCR is limited or showed false negative results. This will help in specific management, besides helping the society at large.
Acknowledgement
We really acknowledge the kindness from Budhi Asih Hospital administration to facilitate and provide our study. We thanked for all the authors with all the hard work physically and physiologically during this pandemic.
Footnotes
Authors’ contributions statement: MH, AZ, AD designed the study and drafted the manuscript. MH, AD, ME collected the data and performed background literature review. AZ interpreted the images. MH, AD, ME carried out the statistical analysis. SA, FS meticulously supervised the results and discussion. All authors reviewed and approved the final version of the manuscript.
Conflicts of interest: All authors – none to declare.
Funding: None to declare.
References
- 1.Xu B, Xing Y, Peng J, et al. Chest CT for detecting COVID-19: a systematic review and meta-analysis of diagnostic accuracy. Eur Radiol. 2020;30:5720–7. doi: 10.21203/rs.3.rs-20481/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;296:E32–40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hafiz M, Icksan AG, Harlivasari AD, Aulia R, Susanti F, Eldinia L. Clinical, radiological features and outcome of COVID-19 patients in a secondary hospital in Jakarta, Indonesia. J Infect Dev Ctries. 2020;14:750–7. doi: 10.3855/jidc.12911. [DOI] [PubMed] [Google Scholar]
- 4.Feng Y, Ling Y, Bai T, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med. 2020;201:1380–8. doi: 10.1164/rccm.202002-0445OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao AT, Tong YX, Zhang S. False-negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: rather than recurrence. J Med Virol. 2020;92:1755–6. doi: 10.1002/jmv.25855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernheim A, Mei X, Huang M, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L, Gao Y, Lou LL, Zhang GJ. The clinical dynamics of 18 cases of COVID-19 outside of Wuhan, China. Eur Respir J. 2020;55:2000398. doi: 10.1183/13993003.00398-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH. Radiographic and CT features of viral pneumonia. Radiographics. 2018;38:719–39. doi: 10.1148/rg.2018170048. [DOI] [PubMed] [Google Scholar]
- 9.Kanne JP. Chest CT findings in 2019 novel coronavirus (2019-nCoV) infections from Wuhan, China: key points for the radiologist. Radiology. 2020;295:16–17. doi: 10.1148/radiol.2020200241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020;295:715–21. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Chest. 2020;158:106–16. doi: 10.1016/j.chest.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li B, Li X, Wang Y, et al. Diagnostic value and key features of computed tomography in coronavirus disease 2019. Emerg Microbes Infect. 2020;9:787–93. doi: 10.1080/22221751.2020.1750307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song F, Shi N, et al. Emerging coronavirus 2019-nCoV pneumonia. Radiology. 2020;295:210–7. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur Radiol. 2020;30:4381–9. doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from coronavirus disease 2019 (COVID-19) Radiology. 2020;295:715–21. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhandari S, Rankawat G, Bagarhatta M, et al. Clinico-radiological evaluation and correlation of CT chest images with progress of disease in COVID-19 patients. J Assoc Physicians India. 2020;68:34–42. [PubMed] [Google Scholar]
- 17.de Jaegere TMH, Krdzalic J, Fasen BACM, Kwee RM. COVID-19 CT Investigators South-East Netherlands (CISEN) study group Radiological Society of North America chest CT classification system for reporting COVID-19 pneumonia: interobserver variability and correlation with RT-PCR. Radiol Cardiothorac Imaging. 2020;2:e200213. doi: 10.1148/ryct.2020200213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Atkinson B. Petersen E. SARS-CoV-2 shedding and infectivity. Lancet. 2020;395:1339–40. doi: 10.1016/S0140-6736(20)30868-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


