Abstract
Mobility-related injuries associate with reduced quality of life, greater functional dependence, and quicker mortality in older adults - warranting prevention efforts. One factor elevating injury risk may be persistent low back pain, which can negatively affect cognitive and physical functions essential for safe mobility. Among older adults obtaining license renewal (n = 1,127), this study examined the association between persistent low back pain and incidence of falls and motor vehicle collisions (MVCs) for up to fifteen years. Overall, older adults with persistent low back pain were more likely to have a fall (OR = 1.54, 95%CI: 1.34–1.77) or MVC (OR = 1.38, 95%CI: 1.07–1.77) than those without back pain. Furthermore, the number of falls and MVCs was lower for people with better lower-limb and visuospatial function, respectively. Ameliorating pain and functioning in persistent lower back pain might contribute to improved mobility and a reduction of injury-related risk in later life.
Keywords: pain, cognition, injury, falls, motor vehicle collisions
1. Introduction
The two leading causes of injury-related death in adults ages 65 and older are falls and motor vehicle collisions (MVCs), making mobility-related injuries a prominent concern (Binder, 2002). Moreover, from 2002 to 2013, falls and MVCs accounted for approximately 69% of unintentional injury-related deaths in older adults (Kramarow et al., 2015). Thus, identifying older adults at risk represents a crucial endeavor.
Of particular interest to the current study is the effect of persistent low back pain, also commonly referred to as “chronic back pain”, which involves feelings of pain, muscle tension, and stiffness in the lower lumbar region that usually continues three or more months (Chou, 2011). Not only is persistent low back pain the most prevalent pain condition in adults aged 65 and older (>30%; Patel et al., 2013), but this enduring pain perception may interfere with crucial domains of cognitive (Anstey & Wood, 2011; Ball et al., 2002; Vance et al., 2006a; Chen, Peronto, & Edwards, 2012) and physical function (Sims et al., 2000; Vance et al., 2006a) imperative for safe mobility.
Specifically, according to the interruptive model of pain, pain disrupts normal cognitive processing and motor planning through resource competition and distraction (Eccleston & Crombez,1999). A plethora of studies now show that pain and attention share overlapping neural networks (e.g., salience detection system; Legrain et al., 2011); and because of its role in survival, pain easily overrides these networks – diverting attentional resources from other tasks. Furthermore, when pain persists, people eventually continue to complete other activities; however, they do so in the face of continuously distracting pain that increases task demands and chances of errors, even for simple behaviors. Although several seminal (e.g., Crombez et al., 1996) and recent studies (e.g., Vlaeyen et al., 2016) support these mechanisms, little work focuses on older adults and the consequences of pain for safe mobility.
Although scarce, studies support the negative impact of low back pain on cognitive-motor processing important for sate mobility in later life. Studies have found that older adults with persistent low back pain perform worse on several cognitive domains linked to injury risk including memory, executive function, and visuospatial ability (Weiner et al., 2006). Furthermore, older adults with severe back pain also report increased difficulty in activities of daily living such as housework, walking, climbing, and lifting (Leveille et al., 1999). Such diminished abilities might add to age-normative declines and increase the risk for both falls and MVCs in adults in late-middle and older adulthood.
Aims & Hypotheses
The purpose of the current study is to examine the relationship between persistent low back pain and subsequent falls and MVCs up to 15 years in a sample of community-dwelling adults aged 55 and older recruited during license renewal. Based on the interruptive model of pain (Eccleston & Crombez,1999), we hypothesized that over time those older adults reporting persistent low back pain after license renewal would have a greater risk of subsequent falls and MVCs due to pain’s interruptive effects on cognitive and physical functions important for mobility and driving (Leveille et al., 1999; Weiner et al., 2006).
As shown in general older adult samples, it was also expected that the probability of injuries in persons with persistent low back pain would be associated with initial cognitive and physical function at license renewal (i.e., baseline). Theoretically, people entering older adulthood with lower abilities would face greater disruption from pain and exhibit higher injury rates therefrom. Specifically, we hypothesized that lower performance on measures of divided attention, task-switching, and processing speed would be significantly associated with a higher likelihood of a subsequent fall or MVC due to their previously shown associations (Anstey & Wood, 2011; Ball et al., 2002; Chen, Peronto, & Edwards, 2012; Vance et al., 2006a, Vance et al., 2006b). Lastly, more difficulties in physical function tasks (lower limb ability) were hypothesized to predict greater odds of falls and/or MVCs over time, consistent with previous findings (Sims et al., 2000, Vance et al., 2006a). Interactions with baseline age were examined due to possible influences on functional assessments.
Methods
Procedure
The study design is illustrated in Figure 1. Between November 1998, and October 1999, adults (55+ years) were recruited from three Motor Vehicle Association [MVA] field sites in Maryland (Glen Burnie, Annapolis, Bel Air) as well as from local community sites. Procedures first received ethical approval by the supervising Intuitional Review Board at the University of Alabama at Birmingham (Approval Number: IRB-100907004). Then, under this approval, certified staff members of the MVAs or community centers approached adults ages 55 and older with current driving licenses and invited them to assist in a series of assessments. Other eligibility criteria included that older adults had to meet visual requirements for licensure in the state of Maryland, including a 20/70 or better visual acuity and a continuous field of vision of 110 degrees or better. Approximately, 2,391 of those identified and meeting eligibility (n = 3,970) agreed and provided written informed consent to participate in the evaluations, with those refusing participation mainly citing time constraints. Previous research with this data (Ball et al., 2006) noted no significant differences in demographics between individuals who declined and those who agreed to participate.
Figure 1.
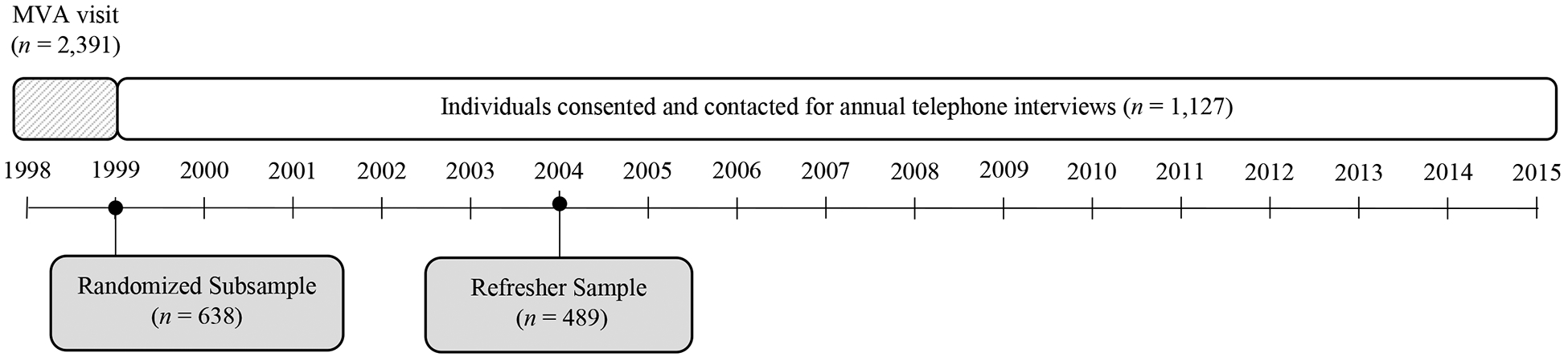
Study design.
Evaluations were done after license renewal, and participants were informed that performance would have no bearing on their driving privileges. The license renewal process in Maryland conducts assessments of visual acuity and visual fields, which helped to exclude participants with visual impairments. Participants who agreed to participate were escorted to a room where written informed consent was obtained. Next, a battery of assessments was given described below. These evaluations were done before asking about health conditions and injuries (conducted through a phone interview within 2-weeks of their MVA appointment) which kept testers blinded to their health status during assessment.
After these evaluations, a subsample of participants was invited and 1,127 provided written consent to be contacted to complete long-term phone interviews and provide demographics. Initially, a random sample of 638 people was contacted three weeks after the MVA appointment and annually for fifteen years to provide longitudinal data. This design was implemented due to budgetary limitations restricting the number of interviews to be conducted each year but still allowed us to collect a moderate-sized randomized sample. To refresh our initial participant pool, however, we planned to add in attrition replacements in a later wave (n = 489) to preserve the representative validity of our longitudinal data, which was done at the sixth year. After the initial MVA appointment and for annual follow-ups, a trained research assistant conducted a telephone interview including participant reports on a various range of behaviors and conditions including the presence of persistent low back pain (yes or no), how many days per week they drove, as well as if they had a fall or MVC that year. Answering these questions over time, participants provided an average of six years of follow-up data. Regarding retention, 80.5% of the sample participated up to the twelfth year. After this point, an average of 43.8% of the sample remained up to the fifteenth year. Reasons for non-participation in any of the follow-ups included being deceased as reported from secondary contact (19%), unable to participate at a single time point due to time or another constraint (21%), and participant dropout (20%). Individuals with missing values tended to be older (Pope et al., 2020).
Measures
Self-reported persistent low back pain
As part of annual telephone interviews, participants reported on several health issues. Participants were queried, “Since the last time we called you, have you been diagnosed and/or treated (includes being prescribed medication) by a physician for any of the following conditions:” and then a list of conditions were read to them. Specific to this study, participants reported if they were diagnosed or treated for “persistent back pain” answering either “Yes,” “No,” or “Do Not Know.” Such status questions are common indicators of low back pain in epidemiological studies and align well with verified diagnosis (Schuh-Renner et al., 2019).
Self-reported falls
Each year, participants were asked, “How many times have you fallen in the last 12 months?” Participants responded yes to one of the six answer choices: 0, 1, 2, 3, 4, or more than 4. This retrospective count method has been used in previous studies while showing strong agreement with observed fall histories (Bergland ey al., 2002).
Self-reported motor vehicle collisions
Each year, participants were asked, “How many crashes have you been involved in over the last year when you were the driver?” Participants responded by providing a number from 0 or more. Retrospective reports are preferred over state-reported MVCs in older adults, as most events never end up in state records (Anstey et al., 2009).
Driving exposure
When assessing older adult crash risk, it remains important to adjust for how often they drive through days driven per week (Blanchard et al., 2010). At each wave, participants were asked one specific question, “In an average week, how many days out of seven do you normally drive?” Participants could respond anywhere from 0 to 7.
Divided attention.
The second subtest of the Useful Field of View (UFOV®2; Ball & Owsley, 1993) was used to measure abilities to identify a central target and locate a simultaneously presented peripheral target, i.e., divided attention capacity. Display duration was manipulated using a double staircase method until a 75% correction detection threshold was identified. This threshold is reported in milliseconds (ms) and provides a measure of divided attention capacity. Higher scores represent worse divided attention capacity. This measure shows strong stability over time (r = .88; Edwards et al., 2005). The UFOV also shows strong convergent validity with real world measures of inattention in everyday environments such as the roadway (Wood et al., 2012).
Processing speed and task-switching.
The Trail Making Task (TMT) parts A and B (Reitan, 1958) were used to measure processing speed and task-switching ability (an aspect of executive function), respectively. In TMT-A, participants use a pencil to sequentially connect integers in ascending order as quickly as possible (1, 2, 3, 4, 5, etc.). In TMT-B, participants connect a mix of integers and letters in alternating and ascending order (1, A, 2, B, etc.). Scores represent total completion time with higher scores indicating slower processing speed for TMT-A and worse set-shifting for TMT-B. Both measures show strong stability over time (both rs >.78; Dikmen et al., 1999; Feinkohl et al., 2020) and convergent validity with other measures of processing speed (TMT-A with Digit Symbol Substitution, r = .63) and task switching (TMT-B and Wisconsin Card Sorting Task, r = .33; Sánchez-Cubillo et al., 2009).
Visuospatial construction.
The Motor-free Visual Perception Task (MVPT) (Colarusso & Hammill, 1972) was used to measure spatial abilities and visuospatial construction. In the task, participants select one of three incomplete figures, which would match the target figure if all lines were connected. A higher total number of incorrect answers (errors, max score = 11) represents worse visuospatial perception. This measure shows convergent validity with other tasks quantifying visuospatial cognition (MVPT and Developmental Test of Visual Perceptual Skills, r = .39; Test of Visual Perceptual Skills, r = .48; Brown et al., 2009). The scale showed acceptable internal consistency (r = .69) and moderate test-retest stability (r = .62; Brown et al., 2009).
Physical (lower-limb) function.
Walk time from the Rapid Walk task (Marottoli et al., 1994) was used to measure lower-limb function. During this task, participants are asked to walk 10 feet, turn, and return to the starting position. Elapsed time (seconds) for completion of the task is recorded. Higher scores represent worse lower limb mobility. This measure shows high convergent validity with other lower-limb measures like treadmill performance (r = .71 to .82), gait speed (r = .73), and self-reported physical endurance (r = .63) (Rikli et al., 1998; Harada et al., 1999). The test also shows high test-retest reliability (r = .95; Harada et al., 1999).
Statistical analyses
Likelihood of having an injury
To model the likelihood of a fall or MVC, general estimating equations fitted the probability on a binomial distribution using SAS software. Participants were categorized as having a fall in the last 12 months (coded as 1) or not having a fall in the previous 12 months (coded as 0) for each year assessed. The same coding scheme was used for MVCs, having at least one MVC in the last 12 months (coded as 1) or not having an MVC in the previous 12 months (coded as 0) for each year assessed. In two separate models, the likelihood of having a fall or MVC (reported annually as a dichotomous outcome) was regressed on the presence of persistent low back pain at each year (Yes coded as 1 and No coded as 0) while controlling for demographic factors of race, sex, and age. We additionally controlled for roadway exposure (days driven per week each year) for the MVC analysis. General estimating equations for these analyses fitted the probability on a binary distribution in the SAS software to obtain odds ratios (OR).
Predictors of falls and MVCs within persistent low back pain
Next, we sought to determine the physical and cognitive factors that explain the number of injuries amongst older adults with persistent low back pain. To do so, we tested if variables of cognitive (divided attention, task-switching, processing speed, and visuospatial perception) and physical function (walk time) collected at license renewal related to the likelihood of falls and MVCs (two separate models on the raw count outcomes). General estimating equations for these analyses fitted the probability on a Poisson distribution in the SAS software to obtain incidence rate ratios (IRR).
For all models, we used an exchangeable working correlation matrix that assumed consistent associations between falls and MVCs across years; this was supported by the lack of autoregressive φ coefficients upon observation. All available data from participants were used in order to allow for the most accurate working correlation matrix, using the all-available-pairs method. All cognitive and physical performance measures were mean-centered for clearer interpretation: model estimates describe effects for one-unit increases above the sample average.
Results
Participants
The mean age of this total sample evaluated (n = 1,127) was 68.77 years at enrollment (SD = 7.57), with slightly higher percentage of males (54.2%) than females (45.8%). Most of the sample was white (94.2%). On average across all timepoints, participants drove approximately 5 days a week (M = 5.40, SD = 1.87). Table 1 shows demographic information and mean reaction times on measures of UFOV®2, TMT-A, TMT-B, and mean number of errors on the MVPT task stratified by whether they reported persistent back pain ever in the study (n = 308) or not (n = 813). Demographically, groups appeared comparable at license renewal minus two exceptions: Participants reporting persistent low back pain had a quicker average performance on UFOV®2 than unaffected peers (b = −.002, SE = .001, p = .001) and slower walking speed than peers (b = .08, SE = .04, p = .033).
Table 1.
Descriptive statistics on overall sample and those with persistent low back pain
| No Back-Pain Sample (n = 813) | Low Back Pain Sample (n = 308) | p | |||
|---|---|---|---|---|---|
| Variables | Mean/% | SD/n | Mean/% | SD/n | |
| Age | 69.00 | 7.73 | 68.13 | 7.11 | .811 |
| Sex | .004 | ||||
| Female | |||||
| Male | 57.07 | 813 | 46.75 | 144 | |
| Race | .955 | ||||
| White | 94.09 | 764 | 94.48 | 291 | |
| Black | |||||
| Days per week driven | 5.16 | 1.68 | 4.94 | 1.58 | .169 |
| Walk time (s) | 6.44 | 2.09 | 6.62 | 2.04 | .033 |
| UFOV Subtest 2 (divided attention, ms) | 172.96 | 152.34 | 137.30 | 132.46 | .017 |
| TMT-A (processing speed) | 13.01 | 36.79 | 13.07 | 34.26 | .883 |
| TMT-B (task switching, s) | 103.30 | 46.44 | 95.72 | 37.55 | .526 |
| MVPT (visuo-spatial perception, errors) | 1.63 | 1.75 | 1.34 | 1.53 | .302 |
Note. A general linear model tested for group differences simultaneously. MVPT = Motor Visual Perception Test; TMT= Trail Making Task; UFOV = Useful Field of View.
Likelihood of having an injury
Odds of having a fall (Table 2)
Table 2.
Likelihood of a fall in total sample (n = 1,127).
| Variable | OR | 95%CI | p |
|---|---|---|---|
| Baseline Variables | |||
| Age*** | 1.02 | 1.01 to 1.03 | <.001 |
| Female** | 1.29 | 1.12 to 1.48 | .001 |
| White* | 1.49 | 1.04 to 2.16 | .031 |
| Time-varying effects | |||
| Year*** | 1.08 | 1.06 to 1.10 | <.001 |
| Low back pain*** | 1.54 | 1.34 to 1.77 | <.001 |
Note. Continuous variable centered around the sample average.
p < .001,
p < .01,
p < .05.
Fifty-one percent of the sample (51.5%, n = 580) reported a fall over time. Within the total sample, when an older adult reported persistent low back pain in the last year, there was 54% higher odds of having a fall (OR = 1.54, 95%CI: 1.34, 1.77, p < .001). Female sex (OR = 1.29, 95%CI: 1.12, 1.48) and being white (OR = 1.49, 95%CI: 1.04, 2.16) were associated with higher odds of a fall (p < .05). Older age at baseline was associated with a small increased likelihood of having a fall (OR = 1.02, 95% CI: 1.01, 1.03, p <.001), and years elapsed after license renewal was also associated with increased odds of having a fall over time (OR = 1.08, 95%CI: 1.06, 1.10, p < .001).
Odds of having an MVC (Table 3)
Table 3.
Likelihood of an MVC in total sample (n = 1,127).
| Variable | OR | 95%CI | p |
|---|---|---|---|
| Baseline Variables | |||
| Age | 1.01 | .99 to 1.03 | .177 |
| Female | 1.17 | .96 to 1.43 | .122 |
| Black** | 1.66 | 1.19 to 2.30 | .003 |
| Time-varying effects | |||
| Year** | 1.04 | 1.02 to 1.07 | .001 |
| Days driven per week* | 1.06 | 1.01 to 1.12 | .025 |
| Low back pain* | 1.38 | 1.07 to 1.77 | .012 |
Note. Continuous variable centered around the sample average.
p < .001,
p < .01,
p < .05.
Thirty-three percent (32.7%, n = 369) of the participants were involved in being in an MVC over time. When older adults reported persistent low back pain in the last year, they exhibited higher odds of an MVC (OR = 1.38; 95% CI: 1.07, 1.77, p = .012). Furthermore, days driven per week for each year (OR = 1.06; 95% CI: 1.01, 1.12) was significantly associated with higher odds of an MVC (ps < .05). There were no significant effects for age at baseline or sex (ps > .10). In terms of race, Black older adults were 66% more likely to incur an MVC (OR = 1.66, 95%CI: 1.19, 2.30). There was also a significant effect of time: For each year after baseline, there was an increased 4% odds of an MVC (95%CI: 1.02, 1.07, p = .001).
Predictors of falls within persistent low back pain (Table 4)
Table 4.
Likelihood of falls in those with persistent low back pain (n = 308).
| Variable | IRR | 95% CI | p |
|---|---|---|---|
| Overall odds | |||
| Year | .98 | .94 to 1.04 | .542 |
| Age | 1.01 | .99 to 1.04 | .415 |
| Female* | 2.64 | 1.01 to 6.93 | .048 |
| White | 2.44 | .64 to 9.39 | .194 |
| Walk time (s)** | 1.35 | 1.11 to 1.64 | .003 |
| UFOV- (divided attention, ms) | .99 | .99 to 1.01 | .590 |
| TMT-A (processing speed, s) | 1.02 | .96 to 1.08 | .584 |
| TMT-B (set-shifting, s) | 1.00 | .99 to 1.01 | .775 |
| MVPT (visuo-spatial perception, errors) | .88 | .52 to 1.51 | .647 |
Note. MVPT = Motor Visual Perception Task, TMT-A = Trails Making Task Part A, TMT-B = Trail Making Task Part B, UFOV = Useful Field of View. Continuous variable centered around the sample average.
p < .001,
p < .01,
p < .05.
Of the older adults who ever reported persistent low back pain, 71.1 % (n = 219) reported falls (M = 4.39, SD = 9.75). Looking at Table 4, there were no significant effects of age or race (ps > .10), but female sex (IRR = 2.64, 95%CI: 1.01, 6.93) was associated with an increased likelihood of falls over time (p = .048). Looking at the other between-subject effects, physical function (walk time) significantly related to a higher likelihood of having a fall: For every second longer a participant took on walk time task, their likelihood of a fall increased (IRR = 1.35; 95% CI: 1.11, 1.64, p = .003). No significant effects emerged for cognitive tasks (ps > .10). Looking at time-varying effects, there was no significant effect of the number of years after license renewal on the likelihood of having a fall (p = .542).
Predictors of MVCs within persistent low back pain (Table 5)
Table 5.
Likelihood of MVCs in those with persistent low back pain (n = 308)
| Variable | IRR | 95%CI |
|---|---|---|
| Main Effects | ||
| Year*** | 1.09 | 1.05 to 1.14 |
| Age | 1.02 | .99 to 1.04 |
| Female | 1.11 | .75 to 1.62 |
| Black | 1.22 | .63 to 2.37 |
| Days per week driven at each year | 1.05 | .94 to 1.16 |
| Walk time (s) | .97 | .89 to 1.06 |
| UFOV- (divided attention, ms) | .99 | .99 to 1.001 |
| TMT-A (processing speed, s) | .99 | .99 to 1.004 |
| TMT-B (task switching, s) | 1.001 | .99 to 1.01 |
| MVPT (visuo-spatial perception, errors) | 1.08 | .96 to 1.22 |
| Age interaction | ||
| MVPT (visuo-spatial perception, errors)** | .98 | .97 to .99 |
Note. MVPT = Motor Visual Perception Task, TMT-A = Trails Making Task Part A, TMT-B = Trail Making Task Part B, UFOV = Useful Field of View. Continuous variable centered around the sample average.
p < .001,
p < .01,
p < .05.
Overall, 42.9% (n = 132) of older adults who ever reported persistent low back pain had MVCs (M = .52, SD = .88). Looking at demographic variables, no significant differences emerged for having an MVC over time (ps > .10). Moreover, cognitive function appeared related to MVCs over time: greater errors on the MVPT task (visuospatial perception) was associated with an increased likelihood of MVCs over time (IRR = 1.08) but this was dependent on the age at license renewal (IRR = .98, 95%CI: .96, .99). No other cognitive task was significantly associated with the likelihood of an MVC (ps >.10). Walk time performance was not associated with MVCs over time (p = .515).
Discussion
This study is among the first to investigate persistent low back pain in older adults (over the age of 55) and how it relates to the two leading causes of mobility-related injuries in the aging population: fall and MVCs. Overall, some associations align with the general theory that pain interferes with recruiting resources for cognitive-motor processes that permit safe mobility (Eccleston & Crombez, 1999) as those with persistent lower back pain were more likely to experience a fall and MVC. Furthermore, in subgroup analyses, we examined which measures of cognition and motor function predicted fall and MVC rates in people with persistent low back pain with notable findings.
First, for MVCs, poorer visuospatial abilities indexed by the MVPT task predicted a higher number of crashes over time. This finding aligns with previous works highlighting a disruptive role of pain on visuospatial perception when persistent, including worse visuospatial motor skills (Weiner et al., 2006), visual memory (Berryman et al., 2013) and spatial orientation (Legrain & Torta, 2015). In addition to showing possibly worse distraction from pain occurrence, perhaps persons with persistent low back are at a disadvantage when responding to everyday, typical cognitive errors. For example, pain’s role in increasing attentional demands might delay the deployment of simple recovery strategies when visuospatial errors occur commonly on the road, i.e., strategic planning when misjudging gaps between cars. Additional work with driving simulation could observe realistic reactions to everyday visuospatial problems in a secure setting for this population. As a caveat, older age at assessment diminishes the association between visuospatial function and crash risk, likely because older adults become more mindful of their lower driving ability when declines occur and reduce driving (West et al., 2003).
In terms of physical function, participants with slower walk times at relicensure had higher fall rates over time. This positive association is likely because slower lower limb movement implicates poor balance or gait that makes older adults more susceptible to bumping into hazards or impeded recovery when tripping. Indeed, other tasks measuring gait and walking ability (e.g., Time-Up-and-Go Task) show positive associations with fall risk (Beauchet et al., 2011); such measures might additionally help screen for fall risk in this population. Musculoskeletal pain can also coincide with problems like dizziness that might produce trips (Kendall et al., 2015). However, if physical function is a predominant mechanism, it might be advantageous to consider the role of related abilities such as spinal lumbar flexion, sitting-to-standing movement, and load carrying in future studies, since these are commonly disrupted in older adults with back pain (Shum et al., 2005).
Our results suggest that problems in cognitive processing and motor abilities in persons with persistent low back pain may increase rates of MVCs and falls, respectively. However, this work emphasizes improved efforts to more precisely identify modifiable mechanisms in order to inform preventative efforts such as early risk assessment and targeted rehabilitation. Two considerations would benefit such work: First, the context in which skills are measured seems essential. For example, driving is a largely visuospatial task, which might explain why cognitive tests assessing visuospatial processing might be more predictive of MVCs than standard verbally based cognitive screening tests. Also, walking appeared to be a better predictor of falls than other tasks, possibly because it directly assessed cognitive-motor planning in the proximate context of falls, i.e., lower-limb movement across surface. Another consideration is the timing of testing. Although our selected measures capture general cognitive differences predicting injuries across extensive periods (Clay et al., 2005; Edwards et al., 2005, Goode et al., 1998), their predictive utility might be enhanced with shorter time gaps, especially as older adults undergo accelerated changes in cognition into their sixties (Schaie et al., 1989).
Concerning clinical implications, our study shines a light on new possibilities to enhance mobility safety in older adults. One, we show that assessing lower back pain appears advantageous to clinical decisions about injury risk, especially in people deemed fit to drive or performing above impairment on standard functional assessments. Secondly, our study may support a clinical paradigm shift from considering pain as a sole injury symptom into a possible vital sign for long term injury risk. Accounting for bidirectional links between pain, cognition, and physical function might enhance future safety research. Also, targeted observational studies might identify possible positive feedback cycles in clinical populations where pain resulting from a disease or injury increases the odds of recurrent injuries independent of other risk factors. Lastly, this study highlights many opportunities for clinicians to improve safety as pain goes largely unscreened and undermanaged in older adults (Denny et al., 2012). For example, prescriptions of nonpharmacological approaches, like exercise, can effectively reduce pain (Tse et al., 2011). Such interventions can simultaneously strengthen risk-lowering skills such as higher visuospatial problem-solving and gait stability (Cadore et al., 2013; Landrigan et al., 2019) – which might be essential in patients with treatment-resistant pain. Furthermore, patients see even minute physical activity from interventions as worthwhile (Janevic et al., 2019). Applicable to the interruptive model of pain, such approaches may improve analgesia and daily function by training individuals to redirect attentional resources away from pain processing back to other daily tasks (Ring et al., 2008). Intervention work on pain and injury risk is limited and likely to run into barriers common in prevention programs, such as cognitive impairment, frailty, and lack of motivation (Malik et al., 2019). Nonetheless, continued investigations are worthwhile to prevent avoidable accidents in our aging population.
Limitations and strengths.
Study findings should be considered in light of limitations. First, this study only examined the impact of persistent lower back pain. Persistent pain can be present in many other locations in older adulthood and overall pain might have a more general effect on injury risk. Furthermore, some specific pains like that in the neck can relate to dizziness, which might elevate injury risk uniquely (Kendall et al., 2015). Secondly, it is important to note that while these findings show increased likelihood for injury-related outcomes, the estimates may be conservative due to the expanded age range of our older adult sample (over 55 rather than 65 years old), the overall health of the sample (e.g., the fact they were able to renew their license), and possible underreporting of injury outcomes. While older adults were told during the consenting process that involvement in the study would not impact their license renewal, reporting still may have been affected. Third, although previous research supports that persistent low back pain precedes injuries (Leveille et al., 2009), a reverse direction is possible such that pain derived from these injuries. More closely spaced follow-ups with lagged indicators might help clarify directionality issues in future studies. Next, some cases of driving cessation occurred over time (approximately 5% of individuals total), which may have weakened the relations between our variables and the risk of MVCs. Thus, as mentioned in a previous paper from the parent study (Ball et al., 2006), persons with lower performance may present a higher likelihood of an MVC. Still, this association diminishes over time due to driving restriction. Also, the MVCs included at-fault and not-at-fault crashes and were self-reported, which may have additionally obscured relationships.
Regarding the sample with persistent low back pain, the sample size was modest, requiring caution when interpreting exact estimates; therefore, the confidence intervals must strongly be considered. Next, cognitive and physical variables were only measured at the MVA appointment before telephone interviewing, which prevented authors from assessing the time-varying effects of these measures on the likelihood of an injury. For example, the presence of cognitive decline preceding impairment strongly predicts crash involvement and falls (Huisingh et al., 2018). Another potential contributing factor might be conventional pain medication like opioids and, sometimes, benzodiazepines, which could have increased injury risk. Comorbid psychiatric disorders might lead to driving under the influence and affect crash risk as well (Choi et al., 2017). Furthermore, participants were mostly white (94%), which may limit the generalizability of findings. However, the study controlled for many demographic differences in a moderate sample size and screened out visual impairments, which aids confidence in our findings.
Conclusion.
Across 15 years, older drivers with persistent low back pain incurred more falls and MVCs. Fortunately, despite being sudden and unexpected events, these negative mobility-related outcomes are not chance events but thought to be products of accumulated, and hopefully, modifiable risk factors. Within this potential at-risk group of people with persistent low back pain, our results implicated diminished cognitive and physical function as possible determinants of adverse mobility-related outcomes to be explored further with repeated assessments across shorter term time intervals. Additional research to disentangle mechanisms may improve interventions to reduce potentially deadly MVCs and falls in adults living with persistent pain.
Acknowledgements:
A special thank you to the UAB Department of Psychology and the Edward R. Roybal Center for Translational Research on Aging and Mobility. K. Ball owns stock in the Visual Awareness Research Group (formerly Visual Awareness, Inc.), and Posit Science, Inc., the companies that market the Useful Field of View Test and speed of processing training software. Posit Science acquired Visual Awareness, and K. Ball continues to collaborate on the design and testing of these assessments and training programs as a member of the Posit Science Scientific Advisory Board.
Funding: This work was supported by the National Institute on Aging [5R01AG021958-10, 1 P30 AG022838 (Edward R. Roybal Center for Translational Research on Aging and Mobility)] and U.S. Department of Transportation/National Highway Traffic Safety Administration (DOT/NHTSA) Contract DTNH22-96-C-05140, “Model Driver Screening and Evaluation Program.
Footnotes
Ethical Approval: All procedures were approved from the University of Alabama at Birmingham Institutional Review Board (Approval Number: IRB-100907004).
Conflict of Interest Declaration: The authors declare the absence of known competing financial or personal relationships that could have influenced the work reported in this paper.
Contributor Information
Tyler Reed Bell, University of California San Diego, Department of Psychiatry, San Diego, CA
Caitlin Northcutt Pope, University of Kentucky, Department of Gerontology, Lexington, KY
Pariya Fazeli, University of Alabama at Birmingham, School of Nursing, Birmingham, AL
Michael Crowe, University of Alabama at Birmingham, Department of Psychology, Birmingham, AL
Karlene Ball, University of Alabama at Birmingham, Department of Psychology, Birmingham, AL
References
- Anstey KJ, & Wood J (2011). Chronological age and age-related cognitive deficits are associated with an increase in multiple types of driving errors in late life. Neuropsychology, 25(5), 613–621. [DOI] [PubMed] [Google Scholar]
- Anstey KJ, Wood J, Caldwell H, Kerr G, & Lord SR (2009). Comparison of self-reported crashes, state crash records, and an on-road driving assessment in a population-based sample of drivers aged 69–95 years. Traffic Injury Prevention, 10(1), 84–90 [DOI] [PubMed] [Google Scholar]
- Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, Marsiske M, … Tennstedt SL (2002). Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA, 288(18), 2271–2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball K, & Owsley C (1993). The useful field of view test: a new technique for evaluating age-related declines in visual function. Journal of the American Optometric Association, 64(1), 71–79. [PubMed] [Google Scholar]
- Ball KK, Roenker DL, Wadley VG, Edwards JD, Roth DL, McGwin G Jr, … & Dube T (2006). Can high-risk older drivers be identified through performance-based measures in a Department of Motor Vehicles setting? Journal of the American Geriatrics Society, 54(1), 77–84. [DOI] [PubMed] [Google Scholar]
- Beauchet O, Fantino B, Allali G, Muir SW, Montero-Odasso M, & Annweiler C (2011). Timed Up and Go test and risk of falls in older adults: A systematic review. The Journal of Nutrition, Health & Aging, 15(10), 933–938. [DOI] [PubMed] [Google Scholar]
- Bergland A, Jarnlo GB, & Laake K (2002). Validity of an index of self-reported walking for balance and falls in elderly women. Advances in Physiotherapy, 4(2), 65–73. [Google Scholar]
- Berryman C, Stanton TR, Bowering KJ, Tabor A, McFarlane A, & Moseley GL (2013). Evidence for working memory deficits in chronic pain: A systematic review and meta-analysis. PAIN®, 154(8), 1181–1196. [DOI] [PubMed] [Google Scholar]
- Binder S (2002). Injuries among older adults: the challenge of optimizing safety and minimizing unintended consequences. Injury Prevention, 8(suppl 4), iv2–iv4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard RA, Myers AM, & Porter MM (2010). Correspondence between self-reported and objective measures of driving exposure and patterns in older drivers. Accident Analysis & Prevention, 42(2), 523–529. [DOI] [PubMed] [Google Scholar]
- Brown T, Mullins E, & Stagnitti K (2009). The concurrent validity of three visual perception tests used with adults. Occupational Therapy in Health Care, 23(2), 99–118. [DOI] [PubMed] [Google Scholar]
- Cadore EL, Rodríguez-Mañas L, Sinclair A, & Izquierdo M (2013). Effects of different exercise interventions on risk of falls, gait ability, and balance in physically frail older adults: A systematic review. Rejuvenation Research, 16(2), 105–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen TY, Peronto CL, & Edwards JD (2012). Cognitive function as a prospective predictor of falls. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 67(6), 720–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi NG, DiNitto DM, & Marti CN (2019). Older adults driving under the influence: Associations with marijuana use, marijuana use disorder, and risk perceptions. Journal of Applied Gerontology, 38(12), 1687–1707. [DOI] [PubMed] [Google Scholar]
- Chou, Robert. “Low back pain (chronic).” American Family Physician, 15 August. 2011, www.aafp.org/afp/2011/0815/p437.html. [Google Scholar]
- Clay OJ, Wadley VG, Edwards JD, Roth DL, Roenker DL, & Ball KK (2005). Cumulative meta-analysis of the relationship between Useful Field of View and driving performance in older adults: Current and future implications. Optometry and Vision Science, 82(8), 724–731. [DOI] [PubMed] [Google Scholar]
- Crombez G, Eccleston C, Baeyens F, & Eelen P (1996). The disruptive nature of pain: An experimental investigation. Behaviour Research and Therapy, 34(11–12), 911–918. [DOI] [PubMed] [Google Scholar]
- Denny DL, & Guido GW (2012). Undertreatment of pain in older adults: An application of beneficence. Nursing Ethics, 19(6), 800–809. [DOI] [PubMed] [Google Scholar]
- Dikmen SS, Heaton RK, Grant I, & Temkin NR (1999). Test–retest reliability and practice effects of expanded Halstead–Reitan Neuropsychological Test Battery. Journal of the International Neuropsychological Society, 5(4), 346–356 [PubMed] [Google Scholar]
- Eccleston C, & Crombez G (1999). Pain demands attention: A cognitive–affective model of the interruptive function of pain. Psychological bulletin, 125(3), 356–366. [DOI] [PubMed] [Google Scholar]
- Edwards JD, Vance DE, Wadley VG, Cissell GM, Roenker DL, & Ball KK (2005). Reliability and validity of useful field of view test scores as administered by personal computer. Journal of clinical and Experimental Neuropsychology, 27(5), 529–543. [DOI] [PubMed] [Google Scholar]
- Feinkohl I, Borchers F, Burkhardt S, Krampe H, Kraft A, Speidel S, … & Slooter A (2020). Stability of neuropsychological test performance in older adults serving as normative controls for a study on postoperative cognitive dysfunction. BMC Research Notes, 13(1), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goode KT, Ball KK, Sloane M, Roenker DL, Roth DL, Myers RS, & Owsley C (1998). Useful field of view and other neurocognitive indicators of crash risk in older adults. Journal of Clinical Psychology in Medical Settings, 5(4), 425–440. [Google Scholar]
- Harada ND, Chiu V, & Stewart AL (1999). Mobility-related function in older adults: assessment with a 6-minute walk test. Archives of Physical Medicine and Rehabilitation, 80(7), 837–841. [DOI] [PubMed] [Google Scholar]
- Janevic MR, Shute V, Connell CM, Piette JD, Goesling J, & Fynke J (2019). The role of pets in supporting cognitive-behavioral chronic pain self-management: Perspectives of older adults. Journal of Applied Gerontology, 0733464819856270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall JC, Hartvigsen J, French SD, & Azari MF (2015). Is there a role for neck manipulation in elderly falls prevention?–An overview. The Journal of the Canadian Chiropractic Association, 59(1), 53. [PMC free article] [PubMed] [Google Scholar]
- Kramarow E, Chen L-H, Hedegaard H, & Warner M (2015). Deaths from unintentional injury among adults aged 65 and over: United States, 2000–2013. NCHS Data Brief (199), 1–8. [PubMed] [Google Scholar]
- Landrigan JF, Bell T, Crowe M, Clay OJ, & Mirman D (2019). Lifting cognition: A meta-analysis of effects of resistance exercise on cognition. Psychological Research, 1–17. [DOI] [PubMed] [Google Scholar]
- Legrain V, Iannetti GD, Plaghki L, & Mouraux A (2011). The pain matrix reloaded: A salience detection system for the body. Progress in Neurobiology, 93(1), 111–124. [DOI] [PubMed] [Google Scholar]
- Leveille SG, Bean J, Bandeen-Roche K, Jones R, Hochberg M, & Guralnik JM (2002). Musculoskeletal pain and risk for falls in older disabled women living in the community. Journal of the American Geriatrics Society, 50(4), 671–678. [DOI] [PubMed] [Google Scholar]
- Leveille SG, Guralnik JM, Hochberg M, Hirsch R, Ferrucci L, Langlois J, … Ling S (1999). Low back pain and disability in older women: independent association with difficulty but not inability to perform daily activities. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 54(10), M487–M493. [DOI] [PubMed] [Google Scholar]
- Leveille S,G, Jones RN, Kiely DK, Hausdorff JM, Smerling RH, Guralnik JM, … & Bean JF (2009). Chronic musculoskeletal pain and the occurrence of falls in an older populaiton. JAMA, 302(20), 2214–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik H, Virag B, Fick F, Hunter PV, Kaasalainen S, & Dal Bello-Haas V (2019). Fall prevention program characteristics and experiences of older adults and program providers in Canada: A thematic content analysis. Journal of Applied Gerontology, 0733464819874600. [DOI] [PubMed] [Google Scholar]
- Marottoli RA, Cooney LM, Wagner DR, Doucette J, & Tinetti ME (1994). Predictors of automobile crashes and moving violations among elderly drivers. Annals of internal medicine, 121(11), 842–846. [DOI] [PubMed] [Google Scholar]
- Patel KV, Guralnik JM, Dansie EJ, & Turk DC (2013). Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain, 154(12), 2649–2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope CN, Fazeli PL, Bell TR, Gaini MS, Mrug S, Vance DE, & Ball KK (2020). A longitudinal investigation of falls and motor vehicle crashes in older drivers. Journal of Aging and Health, 0898264320915111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitan R (1958). Trail making manual for administration, scoring, and interpretation. Department of Neurology, Section of Neuropsychology, Indiana University Medical Center, Indianapolis. [Google Scholar]
- Rikli RE, & Jones CJ (1998). The reliability and validity of a 6-minute walk test as a measure of physical endurance in older adults. Journal of Aging and Physical Activity, 6(4), 363–375 [Google Scholar]
- Ring C, Edwards L, & Kavussanu M (2008). Effects of isometric exercise on pain are mediated by blood pressure. Biological Psychology, 78(1), 123–128. [DOI] [PubMed] [Google Scholar]
- Sánchez-Cubillo I1, Periáñez JA, Adrover-Roig D, Rodríguez-Sánchez JM, Rios-Lago M, Tirapu JEEA, & Barcelo F (2009). Construct validity of the Trail Making Test: role of task-switching, working memory, inhibition/interference control, and visuomotor abilities. Journal of the International Neuropsychological Society: JINS, 15(3), 438. [DOI] [PubMed] [Google Scholar]
- Schaie KW (1989) Individual differences in rate of cognitive change in adulthood. Bengston VL, Schaie KW (Eds.), The Course of Later Life: Research and Reflections, 65–85, Springer, New York. [Google Scholar]
- Schuh-Renner A, Canham-Chervak M, Grier TL, & Jones BH (2019). Accuracy of self-reported injuries compared to medical record data. Musculoskeletal science and practice, 39, 39–44. [DOI] [PubMed] [Google Scholar]
- Shum GL, Crosbie J, & Lee RY (2005). Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit. Spine, 30(17), 1998–2004. [DOI] [PubMed] [Google Scholar]
- Sims RV, McGwin G Jr, Allman RM, Ball K, & Owsley C (2000). Exploratory study of incident vehicle crashes among older drivers. Journals of Gerontology-Biological Sciences and Medical Sciences, 55(1), M22–7. [DOI] [PubMed] [Google Scholar]
- Tse MM, Wan VT, & Ho SS (2011). Physical exercise: Does it help in relieving pain and increasing mobility among older adults with chronic pain? Journal of Clinical Nursing, 20(5‐6), 635–644. [DOI] [PubMed] [Google Scholar]
- Vance DE, Ball KK, Roenker DL, Wadley VG, Edwards JD, & Cissell GM (2006a). Predictors of falling in older Maryland drivers: A structural-equation model. Journal of Aging and Physical Activity, 14(3), 254–269. [DOI] [PubMed] [Google Scholar]
- Vance DE, Roenker DL, Cissell GM, Edwards JD, Wadley VG, & Ball KK (2006b). Predictors of driving exposure and avoidance in a field study of older drivers from the state of Maryland. Accident Analysis & Prevention, 38(4), 823–831. [DOI] [PubMed] [Google Scholar]
- Vlaeyen JW, Morley S, & Crombez G (2016). The experimental analysis of the interruptive, interfering, and identity-distorting effects of chronic pain. Behaviour Research and Therapy, 86, 23–34. [DOI] [PubMed] [Google Scholar]
- Weiner DK, Rudy TE, Morrow L, Slaboda J, & Lieber S (2006). The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Medicine, 7(1), 60–70. [DOI] [PubMed] [Google Scholar]
- West CG, Gildengorin G, Haegerstrom-Portnoy G, Lott LA, Schneck ME, & Brabyn JA (2003). Vision and driving self-restriction in older adults. Journal of the American Geriatrics Society, 51(10), 1348–1355. [DOI] [PubMed] [Google Scholar]
- Wood JM, Chaparro A, Lacherez P, & Hickson L (2012). Useful Field of View predicts driving in the presence of distracters. Optometry and Vision Science, 89(4), 373–381. [DOI] [PubMed] [Google Scholar]


