Abstract
This review is intended to illuminate the emerging understanding of epigenetic modifications which regulate both adaptive and innate immunity in the skin. Host defense of the epidermis and dermis involves the interplay of many cell types to enable homeostasis, tolerance to the external environment and appropriate response to transient microbial, chemical and physical insults. To understand this process, the study of cutaneous immunology has focused on immune responses that reflect both adaptive learned and genetically programed innate defense systems. However, recent advances have begun to reveal that epigenetic modifications of chromatin structure also have a major influence on the skin immune system. This deeper understanding of how enzymatic changes in chromatin structure can modify the skin immune system and may explain how environmental exposures during life, and the microbiome, lead to both short-term and long-term changes in cutaneous allergic and other inflammatory processes. Understanding the mechanisms responsible for alterations in gene and chromatin structure within skin immunocytes could provide key insights into the pathogenesis of inflammatory skin diseases that have thus far evaded understanding by dermatologists.
Introduction
External structures of all organisms have evolved adaptions that permit tolerance to their normal environment while also permitting rapid immune defense to limit dangers such as microbial infections. Immunological adaptations in this system occurs throughout life. When functioning properly this leads to improved defense against dangerous antigens and better tolerance to molecules that do not pose a risk to health. The cell biology and genetics of this system have become increasingly well understood. However, changes in skin immune function are not entirely explained by inheritable genetic information. To better understand skin immunology and disease it is necessary to improve understanding of how an individual environment can alter expression of gene products that shape the immune system.
A major mechanism for control of any gene is its chromatin structure. Chromatin structure is influenced by several factors including modifications made to histones, a core component of chromatin (Zhang and Cao, 2019). A great deal of progress has been made into understanding how environmental stimuli can lead to changes in chromatin structure (Lio and Huang, 2020) (Feil and Fraga, 2012) (Bar-Sadeh et al., 2020). This process of alterations in gene expression by changing chromatin structure rather than intrinsic changes in the genetic code itself is known as epigenetics. Epigenetic changes influence chromatin structure by chemical modification, which has a striking impact on gene expression (Jaenisch and Bird, 2003). Many different environments have been shown to have epigenetic influence on gene function including high altitude (Julian, 2017), hypoxia (Brown and Rupert, 2014), psychological stress (Bartlett et al., 2017), and exercise (Landen et al., 2019).
Cutaneous biologists have made many important contributions to the fundamental understanding of epigenetics and human health in the context of cell development and tumor biology (Köhler and Rodríguez-Paredes, 2020) (Botchkarev, 2017). However, the effects of epigenetic modifications on skin immune function have not been as extensively investigated. Our goal in this review is to present an overview of current knowledge of epigenetic mechanisms that are relevant to skin immune responses. As the reader will note, conclusions regarding the role of epigenetics in immune function depend on various factors. The techniques used to assess the response and the cell type and type of epigenetic modification are important variables that can drive alternative interpretations. We hope that summarizing this information for skin immunologists will help to focus and speed research in this field and perhaps further advance therapeutics of inflammatory skin disorders.
Types of epigenetic modifications
There are several different mechanisms for epigenetic modification of chromatin structure that have been associated with immune reactions. These include histone acetylation, histone methylation, histone SUMOylation, histone phosphorylation, histone ubiquitination, histone citrullination, histone lactylation, and DNA methylation. We begin by first providing brief definitions of each class of epigenetic modification.
Histone acetylation
Positively charged histones contact and wrap negatively charged DNA into the nucleosome (Grunstein, 1997). The lysine-rich domains in the amino-terminal tails of histone are targets for acetylation. Once acetylation occurs, the positive charge in these domains are neutralized. This can result in less condensed chromatin and activation of gene expression (Hogg et al., 2020) (Zhang and Cao, 2019)).
Histone methylation
Histone H3 is the primary target of histone methylation and this modification, especially methylation of lysine, can cause both induction and repression of gene expression. Although there are many exceptions, typically gene activation is promoted by methylation at H3K4, H3K36, and H3K79, while gene-repression occurs by methylation at H3K9 and H3K27 (Jambhekar et al., 2019).
DNA methylation
DNA methylation targets DNA regions where a cytosine nucleotide is followed by a guanine nucleotide in a linear sequence from a 5’ to 3’ direction. This “CpG island” is often found in promoters sites of genes and DNA methylation typically results in gene silencing (Poli et al., 2020).
Histone SUMOylation
The small ubiquitin-related modifier (SUMO) is a ubiquitin-like protein involved in gene transcriptional modifications (Johnson and Gupta, 2001) (Melchior, 2000). SUMO can attach to other proteins, leading to the activation of an enzyme cascade. Histone SUMOylation is most often associated with transcriptional repression.
Histone phosphorylation
Histone phosphorylation takes place mainly at serine, threonine, and tyrosine residues (Qin et al., 2020). Phosphorylation disrupts the interaction between histones and DNA and contributes to the instability of chromatin structure.
Histone ubiquitination
Histone H2A and H2B are sites targeted by ubiquitination. Ubiquitination at H2A and H2B are located near the entry site of DNA into the nucleosome. Therefore, ubiquitination can change chromatin structure and access of other enzymes involved in gene transcription. This histone modification plays critical roles in both transcriptional activation or inhibition (Hofmann, 2009).
Histone citrullination
Histone citrullination regulates gene expression by antagonizing further methylation of DNA (Cuthbert et al., 2004). A methyl group in DNA can bind to an arginine site on histone, affecting binding DNA to histone, resulting in transcriptional activation. Citrullination enzyme PAD converts this arginine site to citrulline and inhibits further histone methylation to repress gene transcription.
Histone lactylation
Lactate regulates physiological and pathological functions of immune cells, and accelerates the lactylation of histone lysine residues, and directly affects transcription. This recently reported histone modification accelerates inflammatory gene transcription in macrophages (Zhang D. et al., 2019).
Functional consequences of epigenetic modifications are cell-type specific
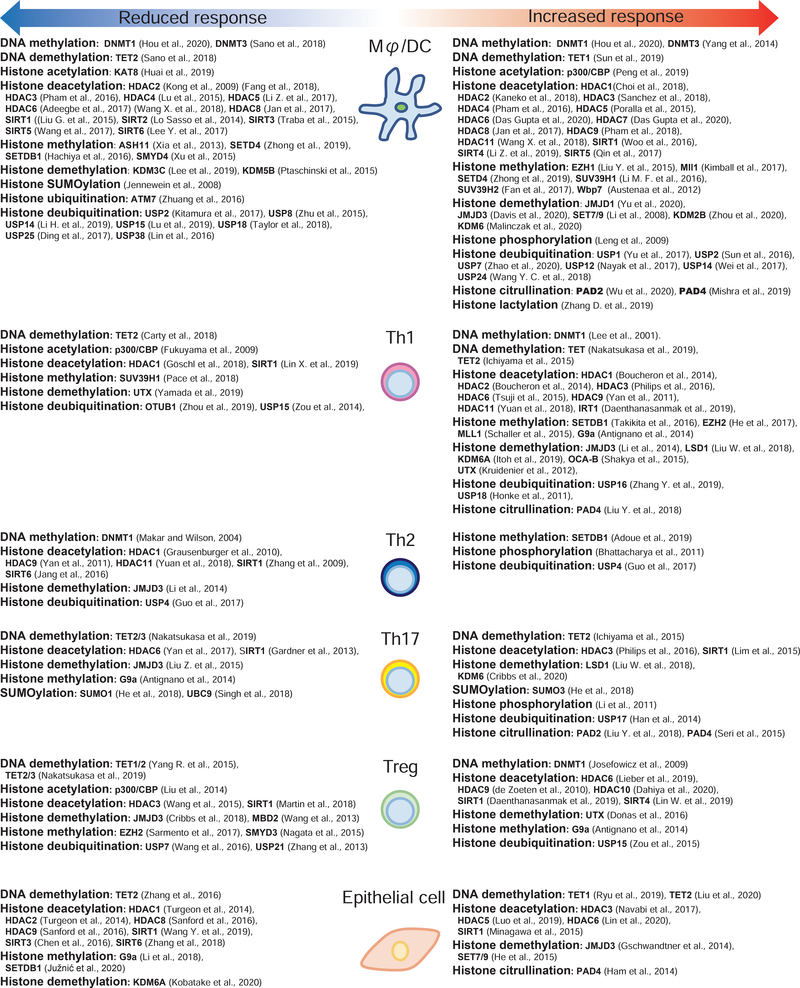
Adding to the complexity of the diverse epigenetic modifications that influence gene function is the observation that the functional consequence of these modifications cannot be universally applied to all cells of the immune system. Different cell types have been shown to respond very differently to similar epigenetic changes (Choi et al., 2018) (Turgeon et al., 2014) (Cao et al., 2014) (Pham et al., 2018) (Sanford et al., 2016) (Li X. et al., 2017) (Malinczak et al., 2020) (Kobatake et al., 2020). This results in increased expression of pro-inflammatory cytokines by some cells types and repression of the expression of inflammatory mediators by other cell types (Figure 1). For example, the effect of HDAC8 and HDAC9 is opposite in keratinocytes compared to macrophages. Inhibition of HDAC8 or HDAC9 will increase cytokine release in response to TLR activation of keratinocytes but will suppress cytokine responses from macrophages (Sanford et al., 2016). These alternative responses make sense when one considers the immunological context of the cell within the skin. For example, keratinocytes are in frequent contact with pathogen associated molecular patterns (PAMPs) or danger associated molecular patterns (DAMPs) and therefore may employ epigenetic mechanisms to tolerate frequent exposure. In contrast, cells deeper in the dermis such as macrophages may use the same epigenetic exposure to increase their capacity to promote inflammation. Other examples of this opposing response of epithelial cells and bone-marrow derived cells is seen with the histone demethylase KDM6A which positively regulates inflammatory cytokine production by macrophages but suppresses responses by epithelial cells from other organs (Choi et al., 2018) (Turgeon et al., 2014) (Cao et al., 2014) (Pham et al., 2018) (Li X. et al., 2017) (Malinczak et al., 2020). (Kobatake et al., 2020). In macrophages, KDM6A-knockdown reduces IL-6 and IFN-β (Li X. et al., 2017), and a KDM6 inhibitor reduces IL-6 in dendritic cells (Malinczak et al., 2020), but KDM6A-deficient urothelium has increased IL-6 (Kobatake et al., 2020). These different responses reflect the complexity of an incompletely understood system. One explanation for alternative responses that are cell type dependent is the presence of the corepressor and the nucleosome remodeling and deacetylase (NuRD) in macrophages. The NuRD complex negatively regulates inflammatory gene expression in macrophages (Ramirez-Carrozzi et al., 2006) (Musselman et al., 2009) but is not active in keratinocytes (Sanford et al., 2016). Epigenetic activation of genes that increase NuRD function will lead to repression of inflammation. In contrast, epigenetic activation of genes encoding inflammatory cytokines will increase inflammation. Thus, in this example, an epigenetic change that increases gene transcription can be either pro-inflammatory or anti-inflammatory. To best understand the potential influence of epigenetics on immunity we will next describe observations based on the cell type in which the experiments were performed.
Figure 1. Opposing influence of epigenetic modifications on gene expression by different cell types that participate in the immune response of the skin.
Illustration to list epigenetic modifications that have been reported in each indicated cell type. References are organized to indicate if these modifications have been reported to result in evidence of cell activation or gene repression.
Macrophages/Dendritic Cells
Macrophages and dendritic cells (DCs) have central roles in immunity and often dictate the direction of responses for other immune cells. Expression of MHC class II and costimulatory factors CD80 and CD86 have an important role in antigen presentation and are positively regulated by histone demethylation (Malinczak et al., 2020). Histone deacetylation by HDAC2, HDAC6 inhibits expression of these genes (Adeegbe et al., 2017, Kong et al., 2009), whereas SIRT1 positively regulates antigen presentation (Woo et al., 2016). Histone phosphorylation and citrullination increases expression of inflammatory cytokines such as TNF-α, IL-1β, and IL-6, (Leng et al., 2009, Marwick et al., 2015, Yang et al., 2008) (Josefowicz et al., 2016), lactylation (Zhang D. et al., 2019) (Mishra et al., 2019, Sohn et al., 2015, Wu et al., 2020) (Mishra et al., 2019, Suzuki et al., 2016). On the contrary, SUMOylation contributes to the suppression of inflammatory cytokine production (Jennewein et al., 2008).
Observations of the immunological consequences from enzymes with opposite actions in DC or macrophages include histone acetylation, methylation, ubiquitination, and DNA methylation. This further complicates conclusions regarding the role of epigenetic modifications to alter function in these cell types. Some apparently contradictory observations may also reflect the specific sites or genes in the chromosome that are targeted by these enzymes. For example, positive regulation of inflammatory cytokine production is seen with histone acetylase; p300/CBP (Peng et al., 2019, van den Bosch et al., 2016)) and histone deacetylases; HDAC1 (Cantley et al., 2015, Choi et al., 2018), HDAC7 (Das Gupta et al., 2020, Shakespear et al., 2013), HDAC9 (Cao et al., 2014, Li et al., 2016, Pham et al., 2018), HDAC11 (Wang et al., 2018), and SIRT4 (Li et al., 2019)). Other histone acetylases negatively regulate inflammatory cytokine production (KAT8 (Huai et al., 2019)) (SIRT2 (Lo Sasso et al., 2014), SIRT3 (Traba et al., 2015), and SIRT6 (Lee et al., 2017)). Furthermore, inflammatory responses can differ depending on the method of targeting enzymes responsible for epigenetic modifications (Fang et al., 2018, Kaneko et al., 2018) (Sanchez et al., 2018) (Pham et al., 2016) (Lu et al., 2015) (Li Z. et al., 2017, Poralla et al., 2015) (Jan et al., 2017) (Lu et al., 2015, Moreno-Gonzalo et al., 2017, Zhang W. B. et al., 2019) (Das Gupta et al., 2020) (Wang et al., 2018) (Jan et al., 2017) (Sano et al., 2018) (Yang et al., 2014) (Qin et al., 2017) (Wang et al., 2017) (Sun et al., 2016) (Kitamura et al., 2017). These findings show specificity in targeting epigenetic modifications is important to understand therapeutic efficacy.
T cells
As classical immunocytes the many different T-cell subsets play a critical role in cutaneous immunity. Deubiquitination of histones and DNA methylation in T cells can promote their expansion (Dufner et al., 2015)) (Lee et al., 2001) (Manna et al., 2015). Histone acetylation and methylation have also been reported to positively regulate T cell development (Gao et al., 2017) (Göschl et al., 2018) (Boucheron et al., 2014) (Philips et al., 2016) (Takikita et al., 2016, Toubai et al., 2018) (Long et al., 2020). Th1 cells are positively driven by citrullination (Liu Y. et al., 2018), while negatively regulated by DNA demethylation (Carty et al., 2018). Depending on the methodology used, histone methylation can promote both directions in Th1 development with positive actions by EZH2 (He et al., 2017) and MLL1 (Schaller et al., 2015), and negative regulation of CD8+ T cell differentiation and long-term memory reprogramming capacity in CD8+ cells by SUV39H1 (Pace et al., 2018).
Th1 cytokines are positively regulated by DNA methylation (Nakatsukasa et al., 2019) (Ichiyama et al., 2015)). Histone demethylases (JMJD3 (Li et al., 2014), LSD1 (Liu W. et al., 2018), KDM6A (Itoh et al., 2019), UTX (Kruidenier et al., 2012), and OCA-B (Shakya et al., 2015)) and histone methyltransferases (G9a (Antignano et al., 2014), EZH2 (He et al., 2013) also positively regulate Th1 cytokine production.
HDACs and deubiquitinases exhibit opposite inflammatory actions depending on each enzyme in T cells. Th1 cytokines are positively regulated by HDAC6 (Tsuji et al., 2015), HDAC9 (Yan et al., 2011), and HDAC11 (Yuan et al., 2018)), whereas HDAC1 has the opposite effect (Göschl et al., 2018). Deubiquitination by USP16 (Zhang Y. et al., 2019) and USP18 (Honke et al., 2011) positively regulates inflammatory cytokine production, however, OTUB1 and USP15 show opposite effects (Zhou et al., 2019, Zou et al., 2014).
Th2 cells exacerbate allergic inflammation mediated by IL-4, IL-5, IL-12, and IL-13, and the importance of these cytokines in allergic cutaneous immunity is proven by the current treatment of targeted therapy for these cytokines (Beck et al., 2014). Th2 is positively driven by phosphorylation (Bhattacharya et al., 2011) (Blüml et al., 2009) and histone methylation (Adoue et al., 2019)). Histone deacetylation, histone deubiquitination, DNA methylation, histone demethylation basically suppress Th2 cytokine production (Jang et al., 2016, Yan et al., 2011) (Yuan et al., 2018) (Guo et al., 2017) (Makar and Wilson, 2004) (Li et al., 2014) (Grausenburger et al., 2010) (Zhang et al., 2009).
Th17 are involved in various inflammatory skin diseases and the downstream pathway promotes neutrophil function. Psoriasis is a representative Th17-mediated skin disease and IL-17-targeted biologics are efficient therapies (Langley et al., 2014). Th17 development and its cytokine production are positively driven by citrullination (Liu Y. et al., 2018, Seri et al., 2015)), phosphorylation (Li et al., 2011), and deubiquitination (Han et al., 2014) (Liu X. et al., 2013). DNA demethylation promotes Th17 development by TET2 (Ichiyama et al., 2015), however, negatively regulates these function by TET2/3 (Nakatsukasa et al., 2019). DNA demethylation, histone deacetylation, and SUMOylation show different effects depending on targeted epigenetic enzymes (Nakatsukasa et al., 2019)(Ichiyama et al., 2015)(Lim et al., 2015) (Gardner et al., 2013) (Yan et al., 2017) (He et al., 2018, Singh et al., 2018). Histone methylation negatively regulates IL-17 production (Antignano et al., 2014), while histone demethylation also showed both positive/negative regulation of Th17 development (Itoh et al., 2019) (Cribbs et al., 2020) (Li et al., 2014) (Liu W. et al., 2018) (Liu et al., 2015).
Tregs have potent capacity to regulate many inflammatory responses (Wing et al., 2019). Treg development and function are positively regulated by DNA demethylation (Nakatsukasa et al., 2019, Yang et al., 2015) (Kim and Leonard, 2007) and histone acetylation (Liu Y. et al., 2013) (>Liu et al., 2014). HDAC3 has shown positive regulation of Treg development (Wang et al., 2015)). The contribution of SIRT1 on Treg function is still controversial and depends on the treatment approach (Daenthanasanmak et al., 2019) (Martin et al., 2018). Histone methylases/demethylases and deubiquitinase show different effects on Tregs depending on each enzyme (Antignano et al., 2014, Nagata et al., 2015, Wang et al., 2016)) (Zou et al., 2015) (Cribbs et al., 2018) (Sarmento et al., 2017, Wang et al., 2013) (Doñas et al., 2016).
Epithelial cells
Epithelial cells are not considered classical immunocytes but have become increasingly appreciated as a critical cell type for regulation of immunity (Honda et al., 2013) (Zhang et al., 2016) (Luger and Schwarz, 1990). Keratinocytes, as the primary epithelial cell in the skin, influences immune responses by both direct expression of cytokines and antimicrobial peptides and by indirect functions as a barrier between the environment and classical immunocytes. As limited information is available that has specifically looked at epigenetic regulation of keratinocyte immune function, this section will also highlight observations from epithelial cells in other organs.
Different HDACs have been reported to negatively regulate inflammatory cytokine expression by epithelia (HDAC1 in intestinal epithelial cells (Turgeon et al., 2014), HDAC2 in intestinal epithelial cells (Turgeon et al., 2014), HDAC8 in keratinocytes (Sanford et al., 2016), HDAC9 in keratinocytes (Sanford et al., 2016), SIRT3 in bronchial epithelial cells (Chen et al., 2016), and SIRT6 in keratinocytes (Zhang et al., 2018) and kidney tubule epithelial cells (Gao et al., 2020)). Histone demethylase KDM6A has shown activity in urothelium (Kobatake et al., 2020), histone methyltransferase G9a in keratinocytes (Li et al., 2018) and SETDB1 in intestinal epithelial cells (Južnić et al., 2020). Inflammatory cytokines have been also shown to be positively regulated by HDAC3 in intestinal epithelial cells (Navabi et al., 2017), HDAC5 in bronchial epithelial cells (Luo et al., 2019), and HDAC6 in bronchial epithelial cells (Lin et al., 2020). Histone demethylation enzymes, JMJD3 and SET7/9, positively regulate the production of antimicrobial peptides by keratinocytes (Gschwandtner et al., 2014) and inflammatory cytokines by bronchial epithelial cells (He et al., 2015), respectively. Citrullination increases inflammatory cytokine and chemokine production by renal tubule cells (Ham et al., 2014). A DNA demethylase, TET1, enhances inflammatory cytokine production by keratinocytes (Ryu et al., 2019). The role of SIRT1 on inflammatory cytokine production is controversial when studied by silencing in bronchial epithelial cells (Tang et al., 2017), gingival epithelial cells (Minagawa et al., 2015), and retina epithelial cells (Xiao and Liu, 2019). Overexpression of SIRT1 reduces inflammatory responses by keratinocytes (Wang et al., 2019).
Epigenetic modulation of inflammatory skin diseases
Some reports have focused on the impact of epigenetic changes in inflammatory skin disease, but much more research is needed to understand how modifications of chromatin structure in multiple cell types translates into disease. The following briefly summarizes some key conclusions by the disease in which the observations were made.
Contact dermatitis is a Th1-mediated inflammatory skin disease and DC-T cell interactions influence the development of skin inflammation in this disorder. Little is known about the contribution of epigenetic modifications in contact dermatitis. Topical butyrate has been reported to reduce contact hypersensitivity responses through increased number of Foxp3-positive cells in the sodium butyrate-treated skin (Schwarz et al., 2017).
Atopic dermatitis is a representative of a Th2-mediated chronic allergic inflammatory disease. Pan-HDAC inhibition by trichostatin A negatively regulates atopic inflamed skin in mice (Kim et al., 2010). On the other hand, SIRT1 preserved skin barrier function in atopic dermatitis (Ming et al., 2015).
Psoriasis is a representative of a Th17 mediated inflammatory skin disease. SIRT1 is decreased in psoriatic skin, while SIRT6 is increased. This has a positive correlation with detection of inflammatory cytokines (Rasheed et al., 2016). There are several reports to evaluate the actual impact of epigenetic modifications on psoriatic skin lesions. SIRT1 and SIRT2 negatively regulate psoriatic skin inflammation, and psoriasiform skin inflammation was aggravated by SIRT1 inhibition (Xie et al., 2015) and Sirt2-deficiency (Hao et al., 2020). As an overall impact of HDAC inhibition, topically applied sodium butyrate reduced imiquimod-induced inflammation and downregulated IL-17 and induced IL-10 and FOXP3 transcripts (Schwarz et al., 2020).
A constitutive source of inhibitors for HDACs is the presence of short-chain fatty acids such as butyrate produced by C. acnes when growing under fermentation conditions in hair follicles (Shu et al., 2013). Short-chain fatty acids produced by C. acnes inhibits HDACs in keratinocytes. Inhibition of HDAC8 and HDAC9 in keratinocytes and sebocytes greatly increases the release of inflammatory cytokines after exposure to TLR ligands (Sanford et al., 2019, Sanford et al., 2016). These observations may be a clue to the pathogenesis of acne vulgaris and provides a mechanism for the microbiome to regulate immune functions through an epigenetic mechanism.
Future directions
The role of epigenetics in cutaneous immunity still remain largely unknown. As this brief review has summarized, there are abundant existing observations suggesting that control of gene expression by epigenetic events can influence immune functions. It is tempting to speculate that by understanding the role of epigenetics in skin immunity it may be possible to explain and/or reverse the development of chronic inflammatory disorders that have not shown major associations with whole genome DNA sequence analysis. However, the current state of this field requires much more work to accurately interpret the significance of past observations. Epigenetic enzymes can have opposite inflammatory responses that depend on the treatment, and this leads to the difficulty to understand the real function of these enzymes. Elucidation of immune cell function by specific cell-targeted assessment of specific enzymes is desired to get a better understanding of the mechanisms of epigenetic regulation important to skin immunity. Such studies can lead to validation of the role of these systems in vivo and successful interventional trials to treat inflammatory skin disorders.
Funding:
RLG is supported by R37AI052453 R01AR069653, R01AR074302, R01AI53185, R01AR076082 and U01AI52038
Y.S is supported by a JSPS Overseas Research Fellowship.
Footnotes
Conflict of Interest:
R.L.G. is a co-founder, scientific advisor, consultant and has equity in MatriSys Biosciences and is a consultant, receives income and has equity in Sente Inc.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adeegbe DO, Liu Y, Lizotte PH, Kamihara Y, Aref AR, Almonte C, et al. Synergistic Immunostimulatory Effects and Therapeutic Benefit of Combined Histone Deacetylase and Bromodomain Inhibition in Non-Small Cell Lung Cancer. Cancer Discov 2017;7(8):852–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adoue V, Binet B, Malbec A, Fourquet J, Romagnoli P, van Meerwijk JPM, et al. The Histone Methyltransferase SETDB1 Controls T Helper Cell Lineage Integrity by Repressing Endogenous Retroviruses. Immunity 2019;50(3):629–44.e8. [DOI] [PubMed] [Google Scholar]
- Antignano F, Burrows K, Hughes MR, Han JM, Kron KJ, Penrod NM, et al. Methyltransferase G9A regulates T cell differentiation during murine intestinal inflammation. J Clin Invest 2014;124(5):1945–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar-Sadeh B, Rudnizky S, Pnueli L, Bentley GR, Stöger R, Kaplan A, et al. Unravelling the role of epigenetics in reproductive adaptations to early-life environment. Nat Rev Endocrinol 2020;16(9):519–33. [DOI] [PubMed] [Google Scholar]
- Bartlett AA, Singh R, Hunter RG. Anxiety and Epigenetics. Adv Exp Med Biol 2017;978:145–66. [DOI] [PubMed] [Google Scholar]
- Beck LA, Thaçi D, Hamilton JD, Graham NM, Bieber T, Rocklin R, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med 2014;371(2):130–9. [DOI] [PubMed] [Google Scholar]
- Bhattacharya P, Gupta G, Majumder S, Adhikari A, Banerjee S, Halder K, et al. Arabinosylated lipoarabinomannan skews Th2 phenotype towards Th1 during Leishmania infection by chromatin modification: involvement of MAPK signaling. PloS one 2011;6(9):e24141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blüml S, Zupkovitz G, Kirchberger S, Seyerl M, Bochkov VN, Stuhlmeier K, et al. Epigenetic regulation of dendritic cell differentiation and function by oxidized phospholipids. Blood 2009;114(27):5481–9. [DOI] [PubMed] [Google Scholar]
- Botchkarev VA. The Molecular Revolution in Cutaneous Biology: Chromosomal Territories, Higher-Order Chromatin Remodeling, and the Control of Gene Expression in Keratinocytes. J Invest Dermatol 2017;137(5):e93–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boucheron N, Tschismarov R, Goeschl L, Moser MA, Lagger S, Sakaguchi S, et al. CD4(+) T cell lineage integrity is controlled by the histone deacetylases HDAC1 and HDAC2. Nat Immunol 2014;15(5):439–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CJ, Rupert JL. Hypoxia and environmental epigenetics. High Alt Med Biol 2014;15(3):323–30. [DOI] [PubMed] [Google Scholar]
- Cantley MD, Fairlie DP, Bartold PM, Marino V, Gupta PK, Haynes DR. Inhibiting histone deacetylase 1 suppresses both inflammation and bone loss in arthritis. Rheumatology (Oxford) 2015;54(9):1713–23. [DOI] [PubMed] [Google Scholar]
- Cao Q, Rong S, Repa JJ, St Clair R, Parks JS, Mishra N. Histone deacetylase 9 represses cholesterol efflux and alternatively activated macrophages in atherosclerosis development. Arterioscler Thromb Vasc Biol 2014;34(9):1871–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carty SA, Gohil M, Banks LB, Cotton RM, Johnson ME, Stelekati E, et al. The Loss of TET2 Promotes CD8(+) T Cell Memory Differentiation. J Immunol 2018;200(1):82–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen IC, Huang HH, Chen PF, Chiang HC. Sirtuin 3 Protects against Urban Particulate Matter-Induced Autophagy in Human Bronchial Epithelial Cells. Toxicol Sci 2016;152(1):113–27. [DOI] [PubMed] [Google Scholar]
- Choi HW, Shin PG, Lee JH, Choi WS, Kang MJ, Kong WS, et al. Anti-inflammatory effect of lovastatin is mediated via the modulation of NF-κB and inhibition of HDAC1 and the PI3K/Akt/mTOR pathway in RAW264.7 macrophages. Int J Mol Med 2018;41(2):1103–9. [DOI] [PubMed] [Google Scholar]
- Cribbs AP, Terlecki-Zaniewicz S, Philpott M, Baardman J, Ahern D, Lindow M, et al. Histone H3K27me3 demethylases regulate human Th17 cell development and effector functions by impacting on metabolism. Proc Natl Acad Sci U S A 2020;117(11):6056–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbert GL, Daujat S, Snowden AW, Erdjument-Bromage H, Hagiwara T, Yamada M, et al. Histone deimination antagonizes arginine methylation. Cell 2004;118(5):545–53. [DOI] [PubMed] [Google Scholar]
- Daenthanasanmak A, Iamsawat S, Chakraborty P, Nguyen HD, Bastian D, Liu C, et al. Targeting Sirt-1 controls GVHD by inhibiting T-cell allo-response and promoting Treg stability in mice. Blood 2019;133(3):266–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahiya S, Beier UH, Wang L, Han R, Jiao J, Akimova T, et al. HDAC10 deletion promotes Foxp3(+) T-regulatory cell function. Sci Rep 2020;10(1):424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das Gupta K, Shakespear MR, Curson JEB, Murthy AMV, Iyer A, Hodson MP, et al. Class IIa Histone Deacetylases Drive Toll-like Receptor-Inducible Glycolysis and Macrophage Inflammatory Responses via Pyruvate Kinase M2. Cell Rep 2020;30(8):2712–28.e8. [DOI] [PubMed] [Google Scholar]
- de Zoeten EF, Wang L, Sai H, Dillmann WH, Hancock WW. Inhibition of HDAC9 increases T regulatory cell function and prevents colitis in mice. Gastroenterology 2010;138(2):583–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doñas C, Carrasco M, Fritz M, Prado C, Tejón G, Osorio-Barrios F, et al. The histone demethylase inhibitor GSK-J4 limits inflammation through the induction of a tolerogenic phenotype on DCs. J Autoimmun 2016;75:105–17. [DOI] [PubMed] [Google Scholar]
- Dufner A, Kisser A, Niendorf S, Basters A, Reissig S, Schönle A, et al. The ubiquitin-specific protease USP8 is critical for the development and homeostasis of T cells. Nat Immunol 2015;16(9):950–60. [DOI] [PubMed] [Google Scholar]
- Fang WF, Chen YM, Lin CY, Huang HL, Yeh H, Chang YT, et al. Histone deacetylase 2 (HDAC2) attenuates lipopolysaccharide (LPS)-induced inflammation by regulating PAI-1 expression. J Inflamm (Lond) 2018;15:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feil R, Fraga MF. Epigenetics and the environment: emerging patterns and implications. Nat Rev Genet 2012;13(2):97–109. [DOI] [PubMed] [Google Scholar]
- Gao B, Kong Q, Zhang Y, Yun C, Dent SYR, Song J, et al. The Histone Acetyltransferase Gcn5 Positively Regulates T Cell Activation. J Immunol 2017;198(10):3927–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Z, Chen X, Fan Y, Zhu K, Shi M, Ding G. Sirt6 attenuates hypoxia-induced tubular epithelial cell injury via targeting G2/M phase arrest. J Cell Physiol 2020;235(4):3463–73. [DOI] [PubMed] [Google Scholar]
- Gardner PJ, Joshi L, Lee RW, Dick AD, Adamson P, Calder VL. SIRT1 activation protects against autoimmune T cell-driven retinal disease in mice via inhibition of IL-2/Stat5 signaling. J Autoimmun 2013;42:117–29. [DOI] [PubMed] [Google Scholar]
- Göschl L, Preglej T, Hamminger P, Bonelli M, Andersen L, Boucheron N, et al. A T cell-specific deletion of HDAC1 protects against experimental autoimmune encephalomyelitis. J Autoimmun 2018;86:51–61. [DOI] [PubMed] [Google Scholar]
- Grunstein M Histone acetylation in chromatin structure and transcription. Nature 1997;389(6649):349–52. [DOI] [PubMed] [Google Scholar]
- Gschwandtner M, Zhong S, Tschachler A, Mlitz V, Karner S, Elbe-Bürger A, et al. Fetal human keratinocytes produce large amounts of antimicrobial peptides: involvement of histone-methylation processes. J Invest Dermatol 2014;134(8):2192–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Z, Xu P, Ge S, Zhang C, Zheng X, Xu J, et al. Ubiquitin specific peptidase 4 stabilizes interferon regulatory factor protein and promotes its function to facilitate interleukin-4 expression in T helper type 2 cells. Int J Mol Med 2017;40(4):979–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha SD, Reid C, Meshkibaf S, Kim SO. Inhibition of Interleukin 1β (IL-1β) Expression by Anthrax Lethal Toxin (LeTx) Is Reversed by Histone Deacetylase 8 (HDAC8) Inhibition in Murine Macrophages. J Biol Chem 2016;291(16):8745–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham A, Rabadi M, Kim M, Brown KM, Ma Z, D’Agati V, et al. Peptidyl arginine deiminase-4 activation exacerbates kidney ischemia-reperfusion injury. Am J Physiol Renal Physiol 2014;307(9):F1052–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han L, Yang J, Wang X, Wu Q, Yin S, Li Z, et al. The E3 deubiquitinase USP17 is a positive regulator of retinoic acid-related orphan nuclear receptor γt (RORγt) in Th17 cells. J Biol Chem 2014;289(37):25546–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao L, Park J, Jang HY, Bae EJ, Park BH. Inhibiting protein kinase activity of pyruvate kinase M2 by sirtuin 2 deacetylase attenuates psoriasis. J Invest Dermatol 2020. [DOI] [PubMed] [Google Scholar]
- He S, Liu Y, Meng L, Sun H, Wang Y, Ji Y, et al. Ezh2 phosphorylation state determines its capacity to maintain CD8(+) T memory precursors for antitumor immunity. Nat Commun 2017;8(1):2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S, Owen DR, Jelinsky SA, Lin LL. Lysine Methyltransferase SETD7 (SET7/9) Regulates ROS Signaling through mitochondria and NFE2L2/ARE pathway. Sci Rep 2015;5:14368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S, Xie F, Liu Y, Tong Q, Mochizuki K, Lapinski PE, et al. The histone methyltransferase Ezh2 is a crucial epigenetic regulator of allogeneic T-cell responses mediating graft-versus-host disease. Blood 2013;122(25):4119–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He Z, Zhang J, Huang Z, Du Q, Li N, Zhang Q, et al. Sumoylation of RORγt regulates T(H)17 differentiation and thymocyte development. Nat Commun 2018;9(1):4870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann K Ubiquitin-binding domains and their role in the DNA damage response. DNA Repair (Amst) 2009;8(4):544–56. [DOI] [PubMed] [Google Scholar]
- Hogg SJ, Beavis PA, Dawson MA, Johnstone RW. Targeting the epigenetic regulation of antitumour immunity. Nat Rev Drug Discov 2020. [DOI] [PubMed] [Google Scholar]
- Honda T, Egawa G, Grabbe S, Kabashima K. Update of immune events in the murine contact hypersensitivity model: toward the understanding of allergic contact dermatitis. J Invest Dermatol 2013;133(2):303–15. [DOI] [PubMed] [Google Scholar]
- Honke N, Shaabani N, Cadeddu G, Sorg UR, Zhang DE, Trilling M, et al. Enforced viral replication activates adaptive immunity and is essential for the control of a cytopathic virus. Nat Immunol 2011;13(1):51–7. [DOI] [PubMed] [Google Scholar]
- Huai W, Liu X, Wang C, Zhang Y, Chen X, Chen X, et al. KAT8 selectively inhibits antiviral immunity by acetylating IRF3. J Exp Med 2019;216(4):772–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang I, Lee E, Jeon SA, Yu JW. Histone deacetylase 6 negatively regulates NLRP3 inflammasome activation. Biochem Biophys Res Commun 2015;467(4):973–8. [DOI] [PubMed] [Google Scholar]
- Ichiyama K, Chen T, Wang X, Yan X, Kim BS, Tanaka S, et al. The methylcytosine dioxygenase Tet2 promotes DNA demethylation and activation of cytokine gene expression in T cells. Immunity 2015;42(4):613–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Into T, Inomata M, Niida S, Murakami Y, Shibata K. Regulation of MyD88 aggregation and the MyD88-dependent signaling pathway by sequestosome 1 and histone deacetylase 6. J Biol Chem 2010;285(46):35759–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itoh Y, Golden LC, Itoh N, Matsukawa MA, Ren E, Tse V, et al. The X-linked histone demethylase Kdm6a in CD4+ T lymphocytes modulates autoimmunity. J Clin Invest 2019;129(9):3852–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaenisch R, Bird A. Epigenetic regulation of gene expression: how the genome integrates intrinsic and environmental signals. Nat Genet 2003;33 Suppl:245–54. [DOI] [PubMed] [Google Scholar]
- Jambhekar A, Dhall A, Shi Y. Roles and regulation of histone methylation in animal development. Nat Rev Mol Cell Biol 2019;20(10):625–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jan JS, Chou YC, Cheng YW, Chen CK, Huang WJ, Hsiao G. The Novel HDAC8 Inhibitor WK2–16 Attenuates Lipopolysaccharide-Activated Matrix Metalloproteinase-9 Expression in Human Monocytic Cells and Improves Hypercytokinemia In Vivo. Int J Mol Sci 2017;18(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang HY, Gu S, Lee SM, Park BH. Overexpression of sirtuin 6 suppresses allergic airway inflammation through deacetylation of GATA3. J Allergy Clin Immunol 2016;138(5):1452–5.e13. [DOI] [PubMed] [Google Scholar]
- Jennewein C, Kuhn AM, Schmidt MV, Meilladec-Jullig V, von Knethen A, Gonzalez FJ, et al. Sumoylation of peroxisome proliferator-activated receptor gamma by apoptotic cells prevents lipopolysaccharide-induced NCoR removal from kappaB binding sites mediating transrepression of proinflammatory cytokines. J Immunol 2008;181(8):5646–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson ES, Gupta AA. An E3-like factor that promotes SUMO conjugation to the yeast septins. Cell 2001;106(6):735–44. [DOI] [PubMed] [Google Scholar]
- Josefowicz SZ, Shimada M, Armache A, Li CH, Miller RM, Lin S, et al. Chromatin Kinases Act on Transcription Factors and Histone Tails in Regulation of Inducible Transcription. Molecular cell 2016;64(2):347–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julian CG. Epigenomics and human adaptation to high altitude. J Appl Physiol (1985) 2017;123(5):1362–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Južnić L, Peuker K, Strigli A, Brosch M, Herrmann A, Häsler R, et al. SETDB1 is required for intestinal epithelial differentiation and the prevention of intestinal inflammation. Gut 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalin JH, Butler KV, Akimova T, Hancock WW, Kozikowski AP. Second-generation histone deacetylase 6 inhibitors enhance the immunosuppressive effects of Foxp3+ T-regulatory cells. J Med Chem 2012;55(2):639–51. [DOI] [PubMed] [Google Scholar]
- Kaneko J, Okinaga T, Ariyoshi W, Hikiji H, Fujii S, Iwanaga K, et al. Ky-2, a hybrid compound histone deacetylase inhibitor, regulated inflammatory response in LPS-driven human macrophages. Cell Biol Int 2018;42(12):1622–31. [DOI] [PubMed] [Google Scholar]
- Kim HP, Leonard WJ. CREB/ATF-dependent T cell receptor-induced FoxP3 gene expression: a role for DNA methylation. J Exp Med 2007;204(7):1543–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim TH, Jung JA, Kim GD, Jang AH, Cho JJ, Park YS, et al. The histone deacetylase inhibitor, trichostatin A, inhibits the development of 2,4-dinitrofluorobenzene-induced dermatitis in NC/Nga mice. Int Immunopharmacol 2010;10(10):1310–5. [DOI] [PubMed] [Google Scholar]
- Kitamura H, Ishino T, Shimamoto Y, Okabe J, Miyamoto T, Takahashi E, et al. Ubiquitin-Specific Protease 2 Modulates the Lipopolysaccharide-Elicited Expression of Proinflammatory Cytokines in Macrophage-like HL-60 Cells. Mediators Inflamm 2017;2017:6909415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobatake K, Ikeda KI, Nakata Y, Yamasaki N, Ueda T, Kanai A, et al. Kdm6a Deficiency Activates Inflammatory Pathways, Promotes M2 Macrophage Polarization, and Causes Bladder Cancer in Cooperation with p53 Dysfunction. Clin Cancer Res 2020;26(8):2065–79. [DOI] [PubMed] [Google Scholar]
- Köhler F, Rodríguez-Paredes M. DNA Methylation in Epidermal Differentiation, Aging, and Cancer. J Invest Dermatol 2020;140(1):38–47. [DOI] [PubMed] [Google Scholar]
- Kong X, Fang M, Li P, Fang F, Xu Y. HDAC2 deacetylates class II transactivator and suppresses its activity in macrophages and smooth muscle cells. J Mol Cell Cardiol 2009;46(3):292–9. [DOI] [PubMed] [Google Scholar]
- Kruidenier L, Chung CW, Cheng Z, Liddle J, Che K, Joberty G, et al. A selective jumonji H3K27 demethylase inhibitor modulates the proinflammatory macrophage response. Nature 2012;488(7411):404–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landen S, Voisin S, Craig JM, McGee SL, Lamon S, Eynon N. Genetic and epigenetic sex-specific adaptations to endurance exercise. Epigenetics 2019;14(6):523–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langley RG, Elewski BE, Lebwohl M, Reich K, Griffiths CE, Papp K, et al. Secukinumab in plaque psoriasis--results of two phase 3 trials. N Engl J Med 2014;371(4):326–38. [DOI] [PubMed] [Google Scholar]
- Lee PP, Fitzpatrick DR, Beard C, Jessup HK, Lehar S, Makar KW, et al. A critical role for Dnmt1 and DNA methylation in T cell development, function, and survival. Immunity 2001;15(5):763–74. [DOI] [PubMed] [Google Scholar]
- Lee Y, Ka SO, Cha HN, Chae YN, Kim MK, Park SY, et al. Myeloid Sirtuin 6 Deficiency Causes Insulin Resistance in High-Fat Diet-Fed Mice by Eliciting Macrophage Polarization Toward an M1 Phenotype. Diabetes 2017;66(10):2659–68. [DOI] [PubMed] [Google Scholar]
- Leng J, Butcher BA, Egan CE, Abi Abdallah DS, Denkers EY. Toxoplasma gondii prevents chromatin remodeling initiated by TLR-triggered macrophage activation. J Immunol 2009;182(1):489–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Yao Q, Mariscal AG, Wu X, Hülse J, Pedersen E, et al. Epigenetic control of IL-23 expression in keratinocytes is important for chronic skin inflammation. Nat Commun 2018;9(1):1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Ruan Q, Hilliard B, Devirgiliis J, Karin M, Chen YH. Transcriptional regulation of the Th17 immune response by IKK(alpha). J Exp Med 2011;208(4):787–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Zou J, Wang M, Ding X, Chepelev I, Zhou X, et al. Critical role of histone demethylase Jmjd3 in the regulation of CD4+ T-cell differentiation. Nat Commun 2014;5:5780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Zhang Q, Ding Y, Liu Y, Zhao D, Zhao K, et al. Methyltransferase Dnmt3a upregulates HDAC9 to deacetylate the kinase TBK1 for activation of antiviral innate immunity. Nat Immunol 2016;17(7):806–15. [DOI] [PubMed] [Google Scholar]
- Li X, Zhang Q, Shi Q, Liu Y, Zhao K, Shen Q, et al. Demethylase Kdm6a epigenetically promotes IL-6 and IFN-β production in macrophages. J Autoimmun 2017;80:85–94. [DOI] [PubMed] [Google Scholar]
- Li Z, Li H, Zhao ZB, Zhu W, Feng PP, Zhu XW, et al. SIRT4 silencing in tumor-associated macrophages promotes HCC development via PPARδ signalling-mediated alternative activation of macrophages. J Exp Clin Cancer Res 2019;38(1):469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Qin H, Li J, Yu L, Yang Y, Xu Y. HADC5 deacetylates MKL1 to dampen TNF-α induced pro-inflammatory gene transcription in macrophages. Oncotarget 2017;8(55):94235–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieber AD, Beier UH, Xiao H, Wilkins BJ, Jiao J, Li XS, et al. Loss of HDAC6 alters gut microbiota and worsens obesity. FASEB J 2019;33(1):1098–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim HW, Kang SG, Ryu JK, Schilling B, Fei M, Lee IS, et al. SIRT1 deacetylates RORγt and enhances Th17 cell generation. J Exp Med 2015;212(5):607–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H, Fu G, Yu Q, Wang Z, Zuo Y, Shi Y, et al. Carbon black nanoparticle induces HDAC6-mediated inflammatory responses in 16HBE cells. Toxicol Ind Health 2020:748233720947214. [DOI] [PubMed] [Google Scholar]
- Lin W, Chen W, Liu W, Xu Z, Zhang L. Sirtuin4 suppresses the anti-neuroinflammatory activity of infiltrating regulatory T cells in the traumatically injured spinal cord. Immunology 2019;158(4):362–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lio CJ, Huang SC. Circles of Life: linking metabolic and epigenetic cycles to immunity. Immunology 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W, Fan JB, Xu DW, Zhu XH, Yi H, Cui SY, et al. Knockdown of LSD1 ameliorates the severity of rheumatoid arthritis and decreases the function of CD4 T cells in mouse models. Int J Clin Exp Pathol 2018;11(1):333–41. [PMC free article] [PubMed] [Google Scholar]
- Liu X, Li H, Zhong B, Blonska M, Gorjestani S, Yan M, et al. USP18 inhibits NF-κB and NFAT activation during Th17 differentiation by deubiquitinating the TAK1-TAB1 complex. J Exp Med 2013;210(8):1575–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Lightfoot YL, Seto N, Carmona-Rivera C, Moore E, Goel R, et al. Peptidylarginine deiminases 2 and 4 modulate innate and adaptive immune responses in TLR-7-dependent lupus. JCI insight 2018;3(23). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Wang L, Predina J, Han R, Beier UH, Wang LC, et al. Inhibition of p300 impairs Foxp3⁺ T regulatory cell function and promotes antitumor immunity. Nat Med 2013;19(9):1173–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, Cao W, Xu L, Chen X, Zhan Y, Yang Q, et al. The histone H3 lysine-27 demethylase Jmjd3 plays a critical role in specific regulation of Th17 cell differentiation. J Mol Cell Biol 2015;7(6):505–16. [DOI] [PubMed] [Google Scholar]
- Lo Sasso G, Menzies KJ, Mottis A, Piersigilli A, Perino A, Yamamoto H, et al. SIRT2 deficiency modulates macrophage polarization and susceptibility to experimental colitis. PloS one 2014;9(7):e103573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long X, Zhang L, Zhang Y, Min M, Lin B, Chen J, et al. Histone methyltransferase Nsd2 is required for follicular helper T cell differentiation. J Exp Med 2020;217(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W, You R, Yuan X, Yang T, Samuel EL, Marcano DC, et al. The microRNA miR-22 inhibits the histone deacetylase HDAC4 to promote T(H)17 cell-dependent emphysema. Nat Immunol 2015;16(11):1185–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luger TA, Schwarz T. Evidence for an epidermal cytokine network. J Invest Dermatol 1990;95(6 Suppl):100s–4s. [DOI] [PubMed] [Google Scholar]
- Luo J, An X, Yao Y, Erb C, Ferguson A, Kolls JK, et al. Epigenetic Regulation of IL-17-Induced Chemokines in Lung Epithelial Cells. Mediators Inflamm 2019;2019:9050965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makar KW, Wilson CB. DNA methylation is a nonredundant repressor of the Th2 effector program. J Immunol 2004;173(7):4402–6. [DOI] [PubMed] [Google Scholar]
- Malinczak CA, Rasky AJ, Fonseca W, Schaller MA, Allen RM, Ptaschinski C, et al. Upregulation of H3K27 Demethylase KDM6 During Respiratory Syncytial Virus Infection Enhances Proinflammatory Responses and Immunopathology. J Immunol 2020;204(1):159–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manna S, Kim JK, Baugé C, Cam M, Zhao Y, Shetty J, et al. Histone H3 Lysine 27 demethylases Jmjd3 and Utx are required for T-cell differentiation. Nat Commun 2015;6:8152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin AN, Alexander-Miller M, Yoza BK, Vachharajani V, McCall CE. Sirtuin1 Targeting Reverses Innate and Adaptive Immune Tolerance in Septic Mice. J Immunol Res 2018;2018:2402593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marwick JA, Tudor C, Khorasani N, Michaeloudes C, Bhavsar PK, Chung KF. Oxidants induce a corticosteroid-insensitive phosphorylation of histone 3 at serine 10 in monocytes. PloS one 2015;10(4):e0124961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior F SUMO--nonclassical ubiquitin. Annu Rev Cell Dev Biol 2000;16:591–626. [DOI] [PubMed] [Google Scholar]
- Minagawa T, Okui T, Takahashi N, Nakajima T, Tabeta K, Murakami S, et al. Resveratrol suppresses the inflammatory responses of human gingival epithelial cells in a SIRT1 independent manner. J Periodontal Res 2015;50(5):586–93. [DOI] [PubMed] [Google Scholar]
- Ming M, Zhao B, Shea CR, Shah P, Qiang L, White SR, et al. Loss of sirtuin 1 (SIRT1) disrupts skin barrier integrity and sensitizes mice to epicutaneous allergen challenge. J Allergy Clin Immunol 2015;135(4):936–45.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra N, Schwerdtner L, Sams K, Mondal S, Ahmad F, Schmidt RE, et al. Cutting Edge: Protein Arginine Deiminase 2 and 4 Regulate NLRP3 Inflammasome-Dependent IL-1β Maturation and ASC Speck Formation in Macrophages. J Immunol 2019;203(4):795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno-Gonzalo O, Ramírez-Huesca M, Blas-Rus N, Cibrián D, Saiz ML, Jorge I, et al. HDAC6 controls innate immune and autophagy responses to TLR-mediated signalling by the intracellular bacteria Listeria monocytogenes. PLoS Pathog 2017;13(12):e1006799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musselman CA, Mansfield RE, Garske AL, Davrazou F, Kwan AH, Oliver SS, et al. Binding of the CHD4 PHD2 finger to histone H3 is modulated by covalent modifications. Biochem J 2009;423(2):179–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata DE, Ting HA, Cavassani KA, Schaller MA, Mukherjee S, Ptaschinski C, et al. Epigenetic control of Foxp3 by SMYD3 H3K4 histone methyltransferase controls iTreg development and regulates pathogenic T-cell responses during pulmonary viral infection. Mucosal Immunol 2015;8(5):1131–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakatsukasa H, Oda M, Yin J, Chikuma S, Ito M, Koga-Iizuka M, et al. Loss of TET proteins in regulatory T cells promotes abnormal proliferation, Foxp3 destabilization and IL-17 expression. Int Immunol 2019;31(5):335–47. [DOI] [PubMed] [Google Scholar]
- Navabi N, Whitt J, Wu SE, Woo V, Moncivaiz J, Jordan MB, et al. Epithelial Histone Deacetylase 3 Instructs Intestinal Immunity by Coordinating Local Lymphocyte Activation. Cell Rep 2017;19(6):1165–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace L, Goudot C, Zueva E, Gueguen P, Burgdorf N, Waterfall JJ, et al. The epigenetic control of stemness in CD8(+) T cell fate commitment. Science 2018;359(6372):177–86. [DOI] [PubMed] [Google Scholar]
- Peng J, Li J, Huang J, Xu P, Huang H, Liu Y, et al. p300/CBP inhibitor A-485 alleviates acute liver injury by regulating macrophage activation and polarization. Theranostics 2019;9(26):8344–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham TX, Bae M, Lee Y, Park YK, Lee JY. Transcriptional and posttranscriptional repression of histone deacetylases by docosahexaenoic acid in macrophages. J Nutr Biochem 2018;57:162–9. [DOI] [PubMed] [Google Scholar]
- Pham TX, Park YK, Lee JY. Anti-Inflammatory Effects of Spirulina platensis Extract via the Modulation of Histone Deacetylases. Nutrients 2016;8(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philips RL, Chen MW, McWilliams DC, Belmonte PJ, Constans MM, Shapiro VS. HDAC3 Is Required for the Downregulation of RORγt during Thymocyte Positive Selection. J Immunol 2016;197(2):541–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poli G, Fabi C, Bellet MM, Costantini C, Nunziangeli L, Romani L, et al. Epigenetic Mechanisms of Inflammasome Regulation. Int J Mol Sci 2020;21(16). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poralla L, Stroh T, Erben U, Sittig M, Liebig S, Siegmund B, et al. Histone deacetylase 5 regulates the inflammatory response of macrophages. J Cell Mol Med 2015;19(9):2162–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin J, Wen B, Liang Y, Yu W, Li H. Histone Modifications and their Role in Colorectal Cancer (Review). Pathol Oncol Res 2020;26(4):2023–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin K, Han C, Zhang H, Li T, Li N, Cao X. NAD(+) dependent deacetylase Sirtuin 5 rescues the innate inflammatory response of endotoxin tolerant macrophages by promoting acetylation of p65. J Autoimmun 2017;81:120–9. [DOI] [PubMed] [Google Scholar]
- Ramirez-Carrozzi VR, Nazarian AA, Li CC, Gore SL, Sridharan R, Imbalzano AN, et al. Selective and antagonistic functions of SWI/SNF and Mi-2beta nucleosome remodeling complexes during an inflammatory response. Genes Dev 2006;20(3):282–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasheed H, El-Komy M, Hegazy RA, Gawdat HI, AlOrbani AM, Shaker OG. Expression of sirtuins 1, 6, tumor necrosis factor, and interferon-γ in psoriatic patients. Int J Immunopathol Pharmacol 2016;29(4):764–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryu YS, Kang KA, Piao MJ, Ahn MJ, Yi JM, Hyun YM, et al. Particulate matter induces inflammatory cytokine production via activation of NFκB by TLR5-NOX4-ROS signaling in human skin keratinocyte and mouse skin. Redox Biol 2019;21:101080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez S, Lemmens S, Baeten P, Sommer D, Dooley D, Hendrix S, et al. HDAC3 Inhibition Promotes Alternative Activation of Macrophages but Does Not Affect Functional Recovery after Spinal Cord Injury. Exp Neurobiol 2018;27(5):437–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanford JA, O’Neill AM, Zouboulis CC, Gallo RL. Short-Chain Fatty Acids from Cutibacterium acnes Activate Both a Canonical and Epigenetic Inflammatory Response in Human Sebocytes. J Immunol 2019;202(6):1767–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanford JA, Zhang LJ, Williams MR, Gangoiti JA, Huang CM, Gallo RL. Inhibition of HDAC8 and HDAC9 by microbial short-chain fatty acids breaks immune tolerance of the epidermis to TLR ligands. Sci Immunol 2016;1(4). [DOI] [PubMed] [Google Scholar]
- Sano S, Oshima K, Wang Y, Katanasaka Y, Sano M, Walsh K. CRISPR-Mediated Gene Editing to Assess the Roles of Tet2 and Dnmt3a in Clonal Hematopoiesis and Cardiovascular Disease. Circ Res 2018;123(3):335–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmento OF, Svingen PA, Xiong Y, Sun Z, Bamidele AO, Mathison AJ, et al. The Role of the Histone Methyltransferase Enhancer of Zeste Homolog 2 (EZH2) in the Pathobiological Mechanisms Underlying Inflammatory Bowel Disease (IBD). J Biol Chem 2017;292(2):706–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller M, Ito T, Allen RM, Kroetz D, Kittan N, Ptaschinski C, et al. Epigenetic regulation of IL-12-dependent T cell proliferation. J Leukoc Biol 2015;98(4):601–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz A, Bruhs A, Schwarz T. The Short-Chain Fatty Acid Sodium Butyrate Functions as a Regulator of the Skin Immune System. J Invest Dermatol 2017;137(4):855–64. [DOI] [PubMed] [Google Scholar]
- Schwarz A, Philippsen R, Schwarz T. Induction of Regulatory T Cells and Correction of Cytokine Disbalance by Short-Chain Fatty Acids: Implications for Psoriasis Therapy. J Invest Dermatol 2020. [DOI] [PubMed] [Google Scholar]
- Seri Y, Shoda H, Suzuki A, Matsumoto I, Sumida T, Fujio K, et al. Peptidylarginine deiminase type 4 deficiency reduced arthritis severity in a glucose-6-phosphate isomerase-induced arthritis model. Sci Rep 2015;5:13041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakespear MR, Hohenhaus DM, Kelly GM, Kamal NA, Gupta P, Labzin LI, et al. Histone deacetylase 7 promotes Toll-like receptor 4-dependent proinflammatory gene expression in macrophages. J Biol Chem 2013;288(35):25362–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakya A, Goren A, Shalek A, German CN, Snook J, Kuchroo VK, et al. Oct1 and OCA-B are selectively required for CD4 memory T cell function. J Exp Med 2015;212(12):2115–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu M, Wang Y, Yu J, Kuo S, Coda A, Jiang Y, et al. Fermentation of Propionibacterium acnes, a commensal bacterium in the human skin microbiome, as skin probiotics against methicillin-resistant Staphylococcus aureus. PloS one 2013;8(2):e55380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AK, Khare P, Obaid A, Conlon KP, Basrur V, DePinho RA, et al. SUMOylation of ROR-γt inhibits IL-17 expression and inflammation via HDAC2. Nat Commun 2018;9(1):4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn DH, Rhodes C, Onuma K, Zhao X, Sharpe O, Gazitt T, et al. Local Joint inflammation and histone citrullination in a murine model of the transition from preclinical autoimmunity to inflammatory arthritis. Arthritis Rheumatol 2015;67(11):2877–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Qin Z, Li Q, Wan JJ, Cheng MH, Wang PY, et al. MicroRNA-124 negatively regulates LPS-induced TNF-α production in mouse macrophages by decreasing protein stability. Acta Pharmacol Sin 2016;37(7):889–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki A, Kochi Y, Shoda H, Seri Y, Fujio K, Sawada T, et al. Decreased severity of experimental autoimmune arthritis in peptidylarginine deiminase type 4 knockout mice. BMC Musculoskelet Disord 2016;17:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takikita S, Muro R, Takai T, Otsubo T, Kawamura YI, Dohi T, et al. A Histone Methyltransferase ESET Is Critical for T Cell Development. J Immunol 2016;197(6):2269–79. [DOI] [PubMed] [Google Scholar]
- Tang L, Chen Q, Meng Z, Sun L, Zhu L, Liu J, et al. Suppression of Sirtuin-1 Increases IL-6 Expression by Activation of the Akt Pathway During Allergic Asthma. Cell Physiol Biochem 2017;43(5):1950–60. [DOI] [PubMed] [Google Scholar]
- Tao R, de Zoeten EF, Ozkaynak E, Chen C, Wang L, Porrett PM, et al. Deacetylase inhibition promotes the generation and function of regulatory T cells. Nat Med 2007;13(11):1299–307. [DOI] [PubMed] [Google Scholar]
- Toubai T, Tamaki H, Peltier DC, Rossi C, Oravecz-Wilson K, Liu C, et al. Mitochondrial Deacetylase SIRT3 Plays an Important Role in Donor T Cell Responses after Experimental Allogeneic Hematopoietic Transplantation. J Immunol 2018;201(11):3443–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traba J, Kwarteng-Siaw M, Okoli TC, Li J, Huffstutler RD, Bray A, et al. Fasting and refeeding differentially regulate NLRP3 inflammasome activation in human subjects. J Clin Invest 2015;125(12):4592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuji G, Okiyama N, Villarroel VA, Katz SI. Histone deacetylase 6 inhibition impairs effector CD8 T-cell functions during skin inflammation. J Allergy Clin Immunol 2015;135(5):1228–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turgeon N, Gagné JM, Blais M, Gendron FP, Boudreau F, Asselin C. The acetylome regulators Hdac1 and Hdac2 differently modulate intestinal epithelial cell dependent homeostatic responses in experimental colitis. Am J Physiol Gastrointest Liver Physiol 2014;306(7):G594–605. [DOI] [PubMed] [Google Scholar]
- van den Bosch T, Boichenko A, Leus NGJ, Ourailidou ME, Wapenaar H, Rotili D, et al. The histone acetyltransferase p300 inhibitor C646 reduces pro-inflammatory gene expression and inhibits histone deacetylases. Biochem Pharmacol 2016;102:130–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Liu TY, Lai CH, Rao YH, Choi MC, Chi JT, et al. Glycolysis-dependent histone deacetylase 4 degradation regulates inflammatory cytokine production. Mol Biol Cell 2014;25(21):3300–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F, Wang K, Xu W, Zhao S, Ye D, Wang Y, et al. SIRT5 Desuccinylates and Activates Pyruvate Kinase M2 to Block Macrophage IL-1β Production and to Prevent DSS-Induced Colitis in Mice. Cell Rep 2017;19(11):2331–44. [DOI] [PubMed] [Google Scholar]
- Wang L, Kumar S, Dahiya S, Wang F, Wu J, Newick K, et al. Ubiquitin-specific Protease-7 Inhibition Impairs Tip60-dependent Foxp3+ T-regulatory Cell Function and Promotes Antitumor Immunity. EBioMedicine 2016;13:99–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Liu Y, Han R, Beier UH, Bhatti TR, Akimova T, et al. FOXP3+ regulatory T cell development and function require histone/protein deacetylase 3. J Clin Invest 2015;125(3):1111–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Liu Y, Han R, Beier UH, Thomas RM, Wells AD, et al. Mbd2 promotes foxp3 demethylation and T-regulatory-cell function. Mol Cell Biol 2013;33(20):4106–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Wu Y, Jiao J, Huang Q. Mycobacterium tuberculosis infection induces IL-10 gene expression by disturbing histone deacetylase 6 and histonedeacetylase 11 equilibrium in macrophages. Tuberculosis (Edinb) 2018;108:118–23. [DOI] [PubMed] [Google Scholar]
- Wang Y, Huo J, Zhang D, Hu G, Zhang Y. Chemerin/ChemR23 axis triggers an inflammatory response in keratinocytes through ROS-sirt1-NF-κB signaling. J Cell Biochem 2019;120(4):6459–70. [DOI] [PubMed] [Google Scholar]
- Wing JB, Tanaka A, Sakaguchi S. Human FOXP3(+) Regulatory T Cell Heterogeneity and Function in Autoimmunity and Cancer. Immunity 2019;50(2):302–16. [DOI] [PubMed] [Google Scholar]
- Woo SJ, Lee SM, Lim HS, Hah YS, Jung ID, Park YM, et al. Myeloid deletion of SIRT1 suppresses collagen-induced arthritis in mice by modulating dendritic cell maturation. Exp Mol Med 2016;48(3):e221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z, Tian Y, Alam HB, Li P, Duan X, Williams AM, et al. PAD2 Mediates Caspase-1 Associated Lethality in Pseudomonas Aeruginosa Pneumonia Induced Sepsis. J Infect Dis 2020. [DOI] [PubMed] [Google Scholar]
- Xiao H, Liu Z. Effects of microRNA‑217 on high glucose‑induced inflammation and apoptosis of human retinal pigment epithelial cells (ARPE‑19) and its underlying mechanism. Mol Med Rep 2019;20(6):5125–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie S, Su Z, Zhang B, Ge J, Song S, Sun G, et al. SIRT1 Activation Ameliorates Aldara-Induced Psoriasiform Phenotype and Histology in Mice. J Invest Dermatol 2015;135(7):1915–8. [DOI] [PubMed] [Google Scholar]
- Yamada T, Nabe S, Toriyama K, Suzuki J, Inoue K, Imai Y, et al. Histone H3K27 Demethylase Negatively Controls the Memory Formation of Antigen-Stimulated CD8(+) T Cells. J Immunol 2019;202(4):1088–98. [DOI] [PubMed] [Google Scholar]
- Yan B, Liu Y, Bai H, Chen M, Xie S, Li D, et al. HDAC6 regulates IL-17 expression in T lymphocytes: implications for HDAC6-targeted therapies. Theranostics 2017;7(4):1002–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan K, Cao Q, Reilly CM, Young NL, Garcia BA, Mishra N. Histone deacetylase 9 deficiency protects against effector T cell-mediated systemic autoimmunity. J Biol Chem 2011;286(33):28833–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang R, Qu C, Zhou Y, Konkel JE, Shi S, Liu Y, et al. Hydrogen Sulfide Promotes Tet1- and Tet2-Mediated Foxp3 Demethylation to Drive Regulatory T Cell Differentiation and Maintain Immune Homeostasis. Immunity 2015;43(2):251–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang SR, Valvo S, Yao H, Kode A, Rajendrasozhan S, Edirisinghe I, et al. IKK alpha causes chromatin modification on pro-inflammatory genes by cigarette smoke in mouse lung. Am J Respir Cell Mol Biol 2008;38(6):689–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X, Wang X, Liu D, Yu L, Xue B, Shi H. Epigenetic regulation of macrophage polarization by DNA methyltransferase 3b. Mol Endocrinol 2014;28(4):565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan L, Chen X, Cheng L, Rao M, Chen K, Zhang N, et al. HDAC11 regulates interleukin-13 expression in CD4+ T cells in the heart. J Mol Cell Cardiol 2018;122:1–10. [DOI] [PubMed] [Google Scholar]
- Zhang D, Tang Z, Huang H, Zhou G, Cui C, Weng Y, et al. Metabolic regulation of gene expression by histone lactylation. Nature 2019;574(7779):575–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang LJ, Sen GL, Ward NL, Johnston A, Chun K, Chen Y, et al. Antimicrobial Peptide LL37 and MAVS Signaling Drive Interferon-β Production by Epidermal Keratinocytes during Skin Injury. Immunity 2016;45(1):119–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q, Cao X. Epigenetic regulation of the innate immune response to infection. Nat Rev Immunol 2019;19(7):417–32. [DOI] [PubMed] [Google Scholar]
- Zhang R, Li H, Guo Q, Zhang L, Zhu J, Ji J. Sirtuin6 inhibits c-triggered inflammation through TLR4 abrogation regulated by ROS and TRPV1/CGRP. J Cell Biochem 2018;119(11):9141–53. [DOI] [PubMed] [Google Scholar]
- Zhang WB, Yang F, Wang Y, Jiao FZ, Zhang HY, Wang LW, et al. Inhibition of HDAC6 attenuates LPS-induced inflammation in macrophages by regulating oxidative stress and suppressing the TLR4-MAPK/NF-κB pathways. Biomed Pharmacother 2019;117:109166. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Liu RB, Cao Q, Fan KQ, Huang LJ, Yu JS, et al. USP16-mediated deubiquitination of calcineurin A controls peripheral T cell maintenance. J Clin Invest 2019;129(7):2856–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X, Yu J, Cheng X, Zhao B, Manyam GC, Zhang L, et al. The deubiquitinase Otub1 controls the activation of CD8(+) T cells and NK cells by regulating IL-15-mediated priming. Nat Immunol 2019;20(7):879–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou Q, Jin J, Hu H, Li HS, Romano S, Xiao Y, et al. USP15 stabilizes MDM2 to mediate cancer-cell survival and inhibit antitumor T cell responses. Nat Immunol 2014;15(6):562–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou Q, Jin J, Xiao Y, Zhou X, Hu H, Cheng X, et al. T Cell Intrinsic USP15 Deficiency Promotes Excessive IFN-γ Production and an Immunosuppressive Tumor Microenvironment in MCA-Induced Fibrosarcoma. Cell Rep 2015;13(11):2470–9. [DOI] [PMC free article] [PubMed] [Google Scholar]