Abstract
ABO blood types and their corresponding antigens have long been assumed to be related to different human diseases. So far, smaller studies on the relationship between mental disorders and blood types yielded contradicting results. In this study we analyzed the association between ABO blood types and lifetime major depressive disorder (MDD). We performed a pooled analysis with data from 26 cohorts that are part of the MDD working group of the Psychiatric Genomics Consortium (PGC). The dataset included 37,208 individuals of largely European ancestry of which 41.6% were diagnosed with lifetime MDD. ABO blood types were identified using three single nucleotide polymorphisms in the ABO gene: rs505922, rs8176746 and rs8176747. Regression analyses were performed to assess associations between the individual ABO blood types and MDD diagnosis as well as putative interaction effects with sex. The models were adjusted for sex, cohort and the first ten genetic principal components. The percentage of blood type A was slightly lower in cases than controls while blood type O was more prominent in cases. However, these differences were not statistically significant. Our analyses found no evidence of an association between ABO blood types and major depressive disorder.
Keywords: blood group, blood type, depression, MDD, association study, psychiatric disorders, PGC
1. Introduction
The ABO blood group system is the clinically most significant blood group system in transfusion and transplantation medicine. In addition to that, ABO blood types and their corresponding antigens have been shown to be associated with different human diseases (Ewald and Sumner, 2016; Groot et al., 2020). Studies indicate associations between ABO blood types and, for example, vascular disorders (higher risk for non-O blood groups), cancer (higher incidence for blood group A compared to O), metabolic diseases (lowest risk for type 2 diabetes mellitus in type O individuals) and cognitive impairment (increased risk in AB individuals) (Ewald and Sumner, 2016). Some smaller studies have also analyzed the relationship between ABO blood types and psychiatric disorders. A recent Croatian study on 156 psychiatric patients and 303 healthy blood donors indicates that psychiatric disorders occur almost three times more frequently in individuals with blood type AB compared to non-AB individuals. However, the authors found no statistically significant difference between the blood type distributions of individuals with mood disorders, psychotic disorders or addictions specifically (Pisk et al., 2019). An earlier U.S. study of the association between ABO blood types and depression severity, assessed with the Beck Depression Inventory (Beck and Steer, 1993), in a sample of 108 volunteers showed a significant difference between mean depression scores of individuals with blood types A, AB/B and O. Type O individuals exhibited a higher mean depression score (M=10.7, SD= 8.0) than both the type A (M=7.3, SD=5.8) and B/AB (M=5.8, SD=5.3) groups (Singg and Lewis, 2001).
However, there are no recent studies analyzing the relationship between ABO blood types and depression on a larger dataset with sufficient power. To address this, we combined data from 26 cohorts of the Major Depressive Disorder (MDD) working group of the Psychiatric Genomics Consortium (PGC). The pooled dataset included 37,208 individuals of which 41.6% were diagnosed with lifetime MDD. ABO blood types were identified using the three single nucleotide polymorphisms (SNPs) rs505922, rs8176746 and rs8176747 in the ABO gene on chromosome 9. We performed regression analyses to assess associations between the individual ABO blood types and MDD diagnosis. Given the higher prevalence of depression among women (Salk et al., 2017), we also analyzed interaction effects of blood types and sex on lifetime MDD risk to examine putative sex-specific associations.
2. Methods
2.1. Dataset
For our analyses we combined data from 26 case-control studies that are part of the MDD working group of the PGC. For a detailed description of the cohort sizes, inclusion/exclusion criteria, diagnostic tests as well as genotyping and imputation procedures, see (Wray et al., 2018) as well as supplementary tables S1 and S2. In summary, the cohorts include individuals of mainly European ancestry as study participants were recruited in Europe, the USA and Australia. All cases were required to have a lifetime diagnosis of MDD based on international consensus criteria (DSM-IV, ICD-9 or ICD-10) (World Health Organization, 1978; American Psychiatric Association, 1994). This was ascertained using structured diagnostic instruments from direct interview by trained interviewers or clinician administered checklists. The majority of studies excluded individuals with bipolar disorder, non-affective psychosis or MDD related to substance use disorders. The resulting dataset included 37,208 individuals (45.2% male) of which 41.6% were diagnosed with lifetime MDD.
2.2. Determining ABO blood types
The ABO gene is located on chromosome 9q34.2 and codes glycosyltransferase, which transfers nucleotide donor sugars to the H antigen to form ABO blood group antigens (Alkebsi et al., 2019). The four ABO blood types A, B, AB and O can be distinguished with three SNPs located in this gene: rs8176719 (c.261delG), rs8176746 (c.796C>A) and rs8176747 (c.803G>C) (Yamamoto et al., 1990; Daniels, 2013). The single base deletion 261delG marks the O allele and variants rs8176746 and rs8176747 discriminate between alleles A and B. Since genetic data for the deletion variant rs8176719 was not available in our dataset we instead utilized SNP rs505922 which is in high linkage disequilibrium with rs8176719 (D’=0.99, r′=0.87 in Europeans (Machiela and Chanock, 2015)). The ABO blood types were derived from these genetic variants as described in Table 1.
Table 1:
Determination of ABO blood types based on three SNPs from the ABO gene.
| rs505922 | rs8176746 | rs8176747 | Genotype | Phenotype |
|---|---|---|---|---|
| C/T | T/G | G/C | BO | B |
| C/T | T/T | G/G | BO | B |
| C/T | G/G | C/C | AO | A |
| C/C | T/G | G/C | AB | AB |
| C/C | T/T | G/G | BB | B |
| C/C | G/G | C/C | AA | A |
| T/T | T/G | G/C | OO | O |
| T/T | NA | NA | OO | O |
| T/T | G/G | C/C | OO | O |
| NA | C/C | G/G | NA | NA |
| C/T | NA | NA | NA | NA |
| NA | T/G | G/C | NA | NA |
| C/C | NA | NA | NA | NA |
NA: Allele not known / blood type cannot be determined
2.3. Association analyses
To assess the association between the MDD diagnosis and the individual ABO blood types A, B, AB and O we performed four separate logistic regressions using the software tool R version 3.4.3. For each analysis we adjusted for sex, cohort and the first ten genetic principal components. As secondary analyses we also studied the interaction effect of ABO blood types and sex on lifetime MDD risk adjusting for cohorts and the first ten genetic principal components.
3. Results
Table 2 displays the minimal, mean and maximal minor allele frequencies (MAFs) of rs505922, rs8176746 and rs8176747 across the 26 individual cohorts as well as the MAFs in the combined dataset. The MAFs in the combined dataset (rs505922: 34.49%, rs8176746/rs8176747: 7.42%) agree with the MAFs observed in the European populations of the 1000 Genomes Project (rs505922: 36.78%, rs8176746/rs8176747: 8.45%) (The 1000 Genomes Project Consortium, 2015; Alexander and Machiela, 2020). However, the MAFs of rs8176746 and rs8176747 are significantly higher (15.28%) when all populations of the 1000 Genomes Project are combined. A detailed account of the MAFs in the individual datasets is listed in supplementary tables S3 and S4.
Table 2:
Summary of minor allele frequencies in the individual PGC studies and selected populations of the 1000 Genomes Project. This table displays the minimal, mean and maximal minor allele frequencies (MAFs) of the individual studies as well as the MAFs in the combined dataset. For comparison, it also shows the MAFs in the combined European populations (EUR) of the 1000 Genomes Project (1000G, n=503) and in the dataset combining all populations (ALL) of the 1000 Genomes Project (n=2,504) (The 1000 Genomes Project Consortium, 2015; Alexander and Machiela, 2020).
| rs505922 | rs8176746 | rs8176747 | |
|---|---|---|---|
| Min. | 27.74% | 4.16% | 4.16% |
| Mean | 34.17% | 7.56% | 7.56% |
| Max. | 39.72% | 10.66% | 10.66% |
| combined | 34.49% | 7.42% | 7.42% |
| 1000G: EUR | 36.78% | 8.45% | 8.45% |
| 1000G: ALL | 35.40% | 15.28% | 15.28% |
The distribution of blood types in each cohort is displayed in Figure 1 A. In total, 42.49% of the 37,208 individuals had blood type A, 10.05% type B, 4.13% type AB and 43.34% had blood type O. This is in accordance with the expected distribution in a population of mainly European descent (Daniels, 2013). Figure 1 B shows the difference in blood type distribution between MDD cases and controls. The percentage of blood type A was slightly lower in cases than controls (41.84% vs. 42.94%) while blood type O was more prominent in cases (43.87% vs. 42.96%). The percentage of blood types B and AB displayed only minimal differences between MDD cases and controls (10.10% vs. 10.01% and 4.19% vs 4.09%).
Figure 1: Distribution of ABO blood types.
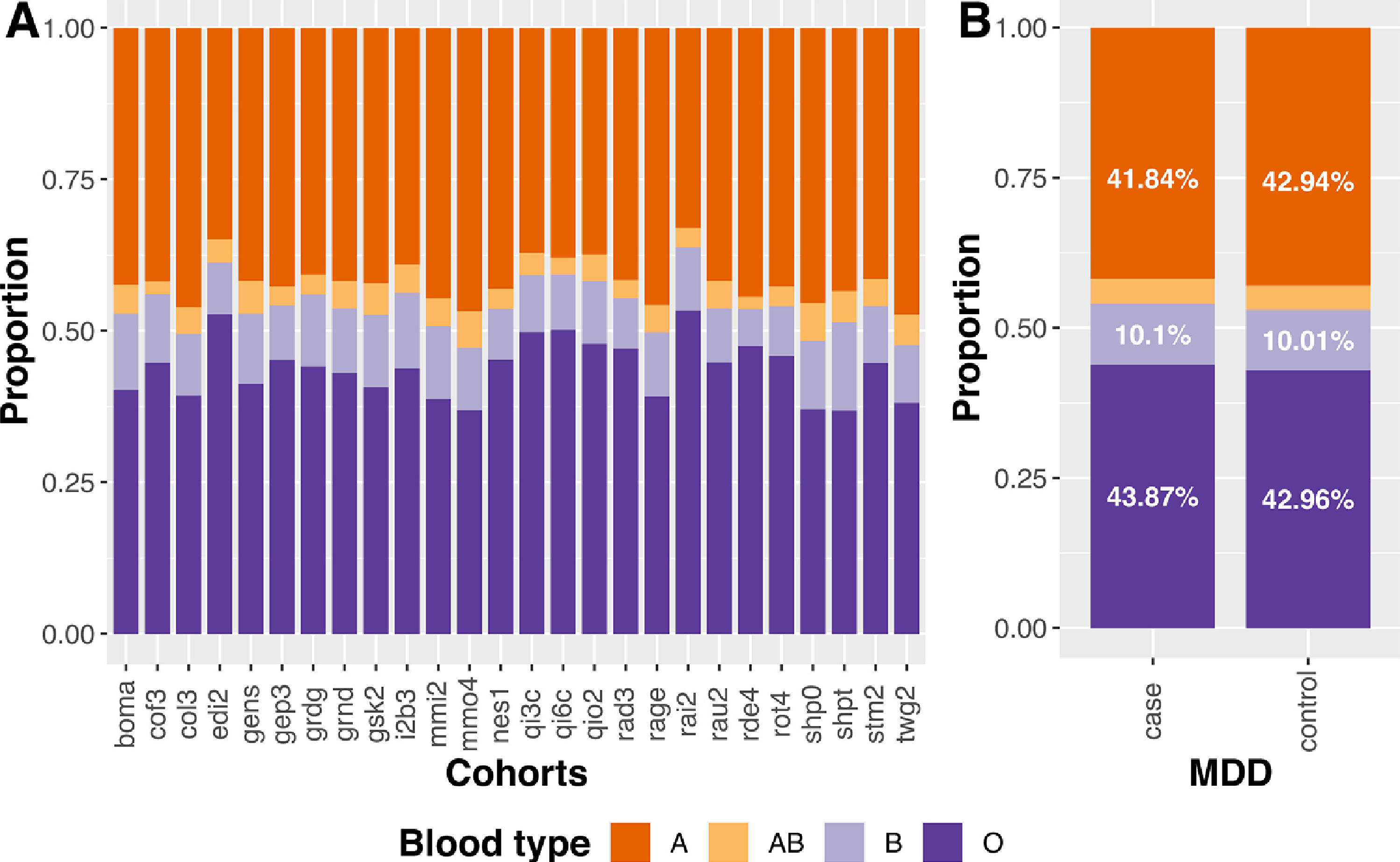
A Distribution of blood types in each cohort. B Distribution of blood types in MDD cases and controls.
A χ2-Test of independence did not show a significant association between MDD diagnosis and ABO blood type distribution (χ2(3)=4.59, p=0.205).
Moreover, none of the four regression analyses assessing the association between the individual blood types and MDD reached statistical significance (p<0.05, Figure 2). Figure 2 displays the effect estimates, p-values and confidence intervals of the four regression models. The effects in the individual cohorts are shown in Figures S1-S4.
Figure 2: Direct effects of ABO blood types on lifetime MDD risk.
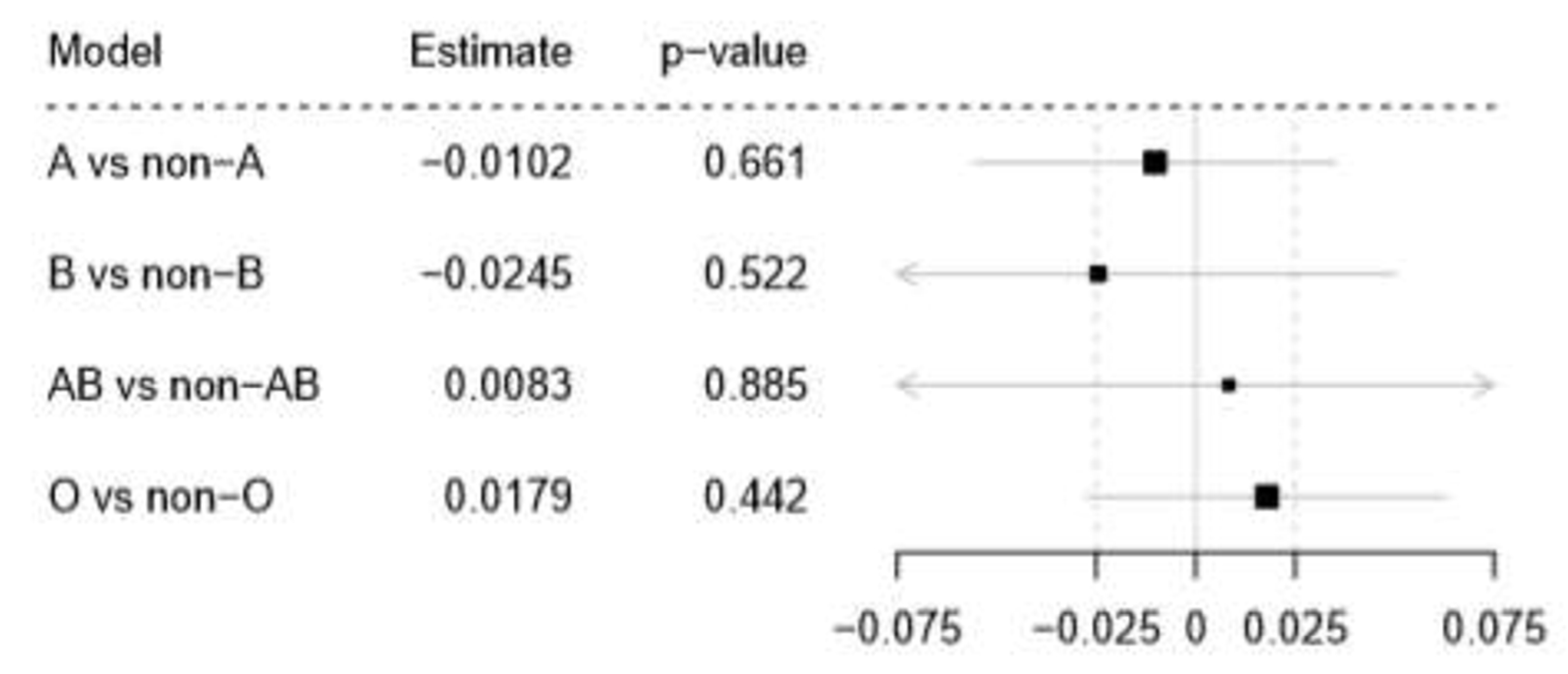
Forest plot displaying the estimates, p-values and confidence intervals of the four regression models adjusted for sex, cohort and the first ten genetic principal components. The boxes represent the estimates for the effects of the individual blood types on MDD risk. The horizontal lines represent the corresponding 95% confidence intervals.
The secondary analyses examining the interaction effects of ABO blood types and sex on MDD risk also did not reach statistical significance. The effect estimates and p-values of the interaction effects as well as the effect estimates and confidence intervals of the sex stratified analyses are displayed in Figure 3.
Figure 3: Interaction effect of ABO blood types and sex on lifetime MDD risk.
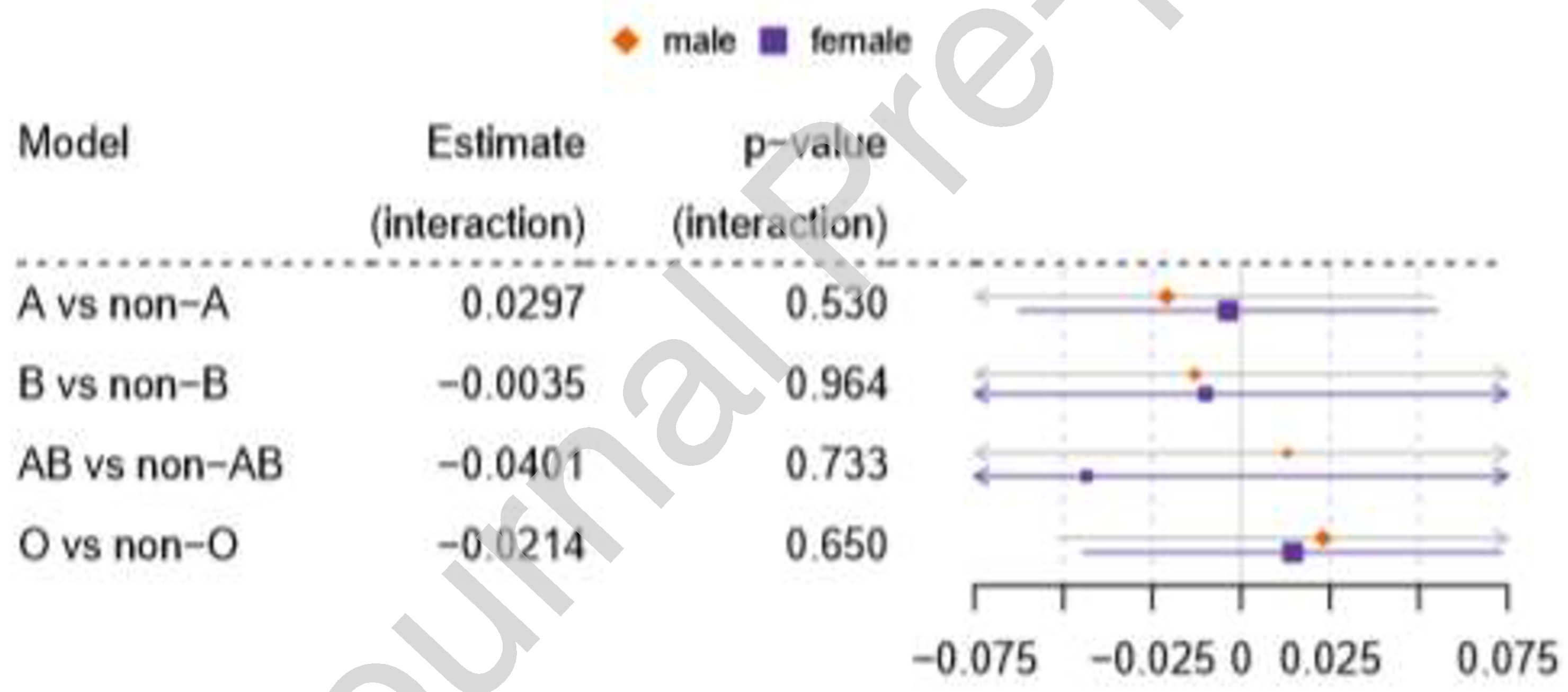
The columns display the effect estimates and the corresponding p-values for the interaction effect of blood types A, B, AB, O and sex on MDD risk. The boxes represent the individual estimates for the effect of the specific blood type on MDD risk in males and females, respectively. The horizontal lines represent the corresponding 95% confidence intervals.
4. Discussion
Previous studies indicated an association between ABO blood types and psychiatric disorders (Singg and Lewis, 2001; Pisk et al., 2019), although the specific risk-conferring blood type has differed. The most recent study found a higher risk of psychiatric disorders (mood disorder, psychotic disorder, addiction and personality disorder) in AB-individuals (Pisk et al., 2019) whereas other studies indicate a higher risk for depressive symptoms in individuals with blood type O compared to non-O individuals (Singg and Lewis, 2001). One critical limitation of these studies is their low power as they included only up to ~500 individuals. With our sample size of 37,208 we had a power of 80% to detect a significant (p<0.05) association with effect size 0.017 between blood type distribution and MDD diagnosis performing a χ2-test. However, we found no evidence to support such an association. This is in accordance with results from a recent study on the association between genetically determined ABO blood groups and different health and disease outcomes in the UK Biobank cohort that also did not find a significant association with a broader phenotype of depression classified by self-report and ICD 10 codes (supplement of (Groot et al., 2020)).
Since the probability of lifetime MDD increases with age, we performed secondary analyses on a subset of 24,917 individuals for which information on age at interview was available to examine whether adjustment for age affects the results. Again, no association was found in these analyses and additionally adjusting for age at interview did not affect the results on this dataset (Figures S5-S7).
Overall, our analyses do not replicate significant findings of previous studies. However, we acknowledge several limitations of our study. Notably, the 26 cohorts included in our analysis were heterogeneous with respect to genotyping platforms (Table S2) and inclusion/exclusion criteria for cases and controls (Table S1). Moreover, some of the cohorts were ascertained from population-based studies while others focused on clinically-ascertained cases; to the extent that these differences reflect varying etiologic factors, they may have obscured an association between blood type and depression.
Furthermore, detailed data on individual depression symptoms or depression severity were not available for this study. Therefore, we are incapable of evaluating to what extent these factors are influenced by blood types. However, considering the previously mentioned significant findings in smaller studies (Singg and Lewis, 2001) the association between ABO blood types and depression severity or symptoms presents an interesting research question for further analyses in suitable datasets.
Additionally, the individual cohorts combined in this study are largely of European ancestry. Further analyses on datasets with different ancestries are required to assess the generalizability of the results.
For future analyses, the inclusion of additional blood parameters such as rhesus (Rh) factor and secretor status could yield a more detailed understanding of the role of blood cell markers and depression.
Supplementary Material
Highlights.
Blood type A slightly more prominent in controls than cases
Blood type O slightly more prominent in cases than controls
Blood types show no significant association with major depressive disorder (MDD)
No evidence for an interaction effect of sex and ABO blood types on MDD
Acknowledgment
The Study of Health in Pomerania (SHIP) is part of the Community Medicine Research net (CMR) (http://www.medizin.uni-greifswald.de/icm) of the University Medicine Greifswald, which is supported by the German Federal State of Mecklenburg- West Pomerania. MRI scans in SHIP and SHIP-TREND have been supported by a joint grant from Siemens Healthineers, Erlangen, Germany and the Federal State of Mecklenburg-West Pomerania.
We thank all participants who were part of the studies and enabled the work of the MDD working Group of the PGC.
Funding and Disclosure
L.G. was supported by the German Research Foundation (DFG, grant no. 403694598). S.V. was supported by the German Federal Ministry of Education and Research (BMBF) within the framework of the e:Med research and funding concept (Integrament; grant no. 01ZX1614E). H.J.G. has received travel grants and speakers honoraria from Fresenius Medical Care and Janssen Cilag. He has received research funding from the German Research Foundation, the German Federal Ministry of Education and Research (BMBF), the DAMP Foundation, Fresenius Medical Care, the EU “Joint Programme Neurodegenerative Disorders” (JPND: 01ED1615) and the European Social Fund (ESF). The PGC has received major funding from the US National Institute of Mental Health (5 U01MH109528–03).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All other authors state that they have nothing to disclose.
Names and affiliations of all members of the MDD working group of the PGC can be found in the supplement.
References
- Alexander TA, Machiela MJ, 2020. LDpop: an interactive online tool to calculate and visualize geographic LD patterns. BMC bioinformatics 21 (1). 10.1186/s12859-020-3340-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkebsi L, Ohnishi H, Nakajima-Shimada J, Onizuka Y, Ideno Y, Sato Y, Hayashi K, 2019. Validation of the Accuracy of Self-Reported ABO Blood Types in the Japan Nurses’ Health Study. Asian Pacific journal of cancer prevention: APJCP 20 (3), 789–793. 10.31557/APJCP.2019.20.3.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, 1994. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. JAMA 272 (10), 828–829. 10.1001/jama.1994.03520100096046. [DOI] [Google Scholar]
- Beck AT, Steer RA, 1993. Beck Depression Inventory: manual. Harcourt Brace, San Antonio (Tx). [Google Scholar]
- Daniels G, 2013. Human blood groups, 3rd ed. Wiley-Blackwell, Chichester. [Google Scholar]
- Ewald DR, Sumner SCJ, 2016. Blood type biochemistry and human disease. Wiley interdisciplinary reviews. Systems biology and medicine 8 (6), 517–535. 10.1002/wsbm.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groot HE, Villegas Sierra LE, Said MA, Lipsic E, Karper JC, van der Harst P, 2020. Genetically Determined ABO Blood Group and its Associations With Health and Disease. Arteriosclerosis, thrombosis, and vascular biology 40 (3), 830–838. 10.1161/ATVBAHA.119.313658. [DOI] [PubMed] [Google Scholar]
- Machiela MJ, Chanock SJ, 2015. LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics 31 (21), 3555–3557. 10.1093/bioinformatics/btv402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisk SV, Vuk T, Ivezić E, Jukić I, Bingulac-Popović J, Filipčić I, 2019. ABO blood groups and psychiatric disorders: a Croatian study. Blood transfusion = Trasfusione del sangue 17 (1), 66–71. 10.2450/2018.0266-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk RH, Hyde JS, Abramson LY, 2017. Gender Differences in Depression in Representative National Samples: Meta-Analyses of Diagnoses and Symptoms. Psychological bulletin 143 (8), 783–822. 10.1037/bul0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singg S, Lewis JL, 2001. Depression and Blood Types. Psychological Reports (88), 725–726. [DOI] [PubMed] [Google Scholar]
- The 1000 Genomes Project Consortium, 2015. A global reference for human genetic variation. Nature 526 (7571), 68–74. 10.1038/nature15393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 1978. The International Classification of Diseases: ninth revision (ICD-9). Annals of internal medicine 88 (3). 10.7326/0003-4819-88-3-424. [DOI] [PubMed] [Google Scholar]
- Wray NR, Ripke S, Mattheisen M, Trzaskowski M, Byrne EM, Abdellaoui A, Adams MJ, Agerbo E, Air TM, Andlauer TMF, Bacanu S-A, Bækvad-Hansen M, Beekman AFT, Bigdeli TB, Binder EB, Blackwood DRH, Bryois J, Buttenschøn HN, Bybjerg-Grauholm J, Cai N, Castelao E, Christensen JH, Clarke T-K, Coleman JIR, Colodro-Conde L, Couvy-Duchesne B, Craddock N, Crawford GE, Crowley CA, Dashti HS, Davies G, Deary IJ, Degenhardt F, Derks EM, Direk N, Dolan CV, Dunn EC, Eley TC, Eriksson N, Escott-Price V, Kiadeh FHF, Finucane HK, Forstner AJ, Frank J, Gaspar HA, Gill M, Giusti-Rodríguez P, Goes FS, Gordon SD, Grove J, Hall LS, Hannon E, Hansen CS, Hansen TF, Herms S, Hickie IB, Hoffmann P, Homuth G, Horn C, Hottenga J-J, Hougaard DM, Hu M, Hyde CL, Ising M, Jansen R, Jin F, Jorgenson E, Knowles JA, Kohane IS, Kraft J, Kretzschmar WW, Krogh J, Kutalik Z, Lane JM, Li Y, Li Y, Lind PA, Liu X, Lu L, MacIntyre DJ, MacKinnon DF, Maier RM, Maier W, Marchini J, Mbarek H, McGrath P, McGuffin P, Medland SE, Mehta D, Middeldorp CM, Mihailov E, Milaneschi Y, Milani L, Mill J, Mondimore FM, Montgomery GW, Mostafavi S, Mullins N, Nauck M, Ng B, Nivard MG, Nyholt DR, O’Reilly PF, Oskarsson H, Owen MJ, Painter JN, Pedersen CB, Pedersen MG, Peterson RE, Pettersson E, Peyrot WJ, Pistis G, Posthuma D, Purcell SM, Quiroz JA, Qvist P, Rice JP, Riley BP, Rivera M, Saeed Mirza S, Saxena R, Schoevers R, Schulte EC, Shen L, Shi J, Shyn SI, Sigurdsson E, Sinnamon GBC, Smit JH, Smith DJ, Stefansson H, Steinberg S, Stockmeier CA, Streit F, Strohmaier J, Tansey KE, Teismann H, Teumer A, Thompson W, Thomson PA, Thorgeirsson TE, Tian C, Traylor M, Treutlein J, Trubetskoy V, Uitterlinden AG, Umbricht D, van der Auwera S, van Hemert AM, Viktorin A, Visscher PM, Wang Y, Webb BT, Weinsheimer SM, Wellmann J, Willemsen G, Witt SH, Wu Y, Xi HS, Yang J, Zhang F, Arolt V, Baune BT, Berger K, Boomsma DI, Cichon S, Dannlowski U, Geus E.C.J. de, DePaulo JR, Domenici E, Domschke K, Esko T, Grabe HJ, Hamilton SP, Hayward C, Heath AC, Hinds DA, Kendler KS, Kloiber S, Lewis G, Li QS, Lucae S, Madden PFA, Magnusson PK, Martin NG, McIntosh AM, Metspalu A, Mors O, Mortensen PB, Müller-Myhsok B, Nordentoft M, Nöthen MM, O’Donovan MC, Paciga SA, Pedersen NL, Penninx BWJH, Perlis RH, Porteous DJ, Potash JB, Preisig M, Rietschel M, Schaefer C, Schulze TG, Smoller JW, Stefansson K, Tiemeier H, Uher R, Völzke H, Weissman MM, Werge T, Winslow AR, Lewis CM, Levinson DF, Breen G, Børglum AD, Sullivan PF, 2018. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nature genetics 50 (5), 668–681. 10.1038/s41588-018-0090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto F. i., Clausen H, White T, Marken J, Hakomori S. i., 1990. Molecular genetic basis of the histo-blood group ABO system. Nature (345), 229–233. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


