Abstract
We examined the association between dietary potassium intake and all-cause and cause-specific mortality among community-dwelling older adults. Potassium intake was assessed with a food frequency questionnaire administered to 1,363 older adults (mean age 71.0 ±10.6 years). Cox proportional hazard regressions estimated hazard ratios for sex-specific quintiles of calorie-adjusted potassium in relation to all-cause and cause-specific (cardiovascular disease, CVD, and stroke) mortality, adjusting for numerous covariates. There were 855 deaths (63% mortality) during the 20-year follow-up. Relative to the third quintile, potassium intake in the lowest quintile only was associated with increased risk of all-cause mortality (fully-adjusted hazard ratio 1.33; 95% CI 1.06, 1.67). Potassium intake was not significantly associated with CVD or stroke mortality. These results suggest that low potassium intake is associated with increased risk of mortality independent of overall health status. Ensuring adequate potassium in the diet may be an important strategy for reducing risk of earlier mortality among older adults.
Keywords: Nutrition, longevity, cardiovascular disease, stroke, aging
Introduction
Potassium is an essential nutrient required to maintain total body fluid volume, acid and electrolyte balance, and normal cell function.1 While potassium is abundant in many fresh fruits and vegetables, the manufacturing of processed foods reduces the amount of potassium in many commonly consumed foods. Consequently, diets with large amounts of processed foods and few fresh fruits and vegetables are often lacking in potassium. In the United States, processed foods represent nearly 70% of caloric intake.2 As a result, U.S. adults consume less than half the daily recommended potassium intake of 4,700 mg.3,4
Low potassium intake is associated with a number of chronic diseases including hypertension, cardiovascular disease, chronic kidney stone formation, and low bone-mineral density.1 High potassium intake, particularly among individuals with kidney disease, can lead to life-threatening arrhythmias and cardiac arrest.5 In the United States and Europe, chronic diseases are the leading cause of death, with diseases of the circulatory system (such as heart attack and stroke) being among the most important contributors to premature mortality.6,7 Understanding the association between potassium intake and mortality may enable simple interventions that could prevent or mitigate some of the most common and preventable health problems leading to early death.
Few studies have explored the association between dietary potassium and all-cause or cause-specific mortality.8–10 A recent systematic review, which concluded that there is insufficient evidence to identify associations between potassium intake and health or mortality outcomes, underscores the need for further research in this area.11 Here, we explored the association between dietary potassium intake and all-cause and cause-specific mortality in a well-characterized cohort of older men and women who completed a food frequency questionnaire in 1992–96, and were followed over 20 years. Our primary analyses were designed to investigate possible non-linear associations of potassium intake with mortality as many biological and dietary factors show harm for both deficiency and excess. We hypothesized that the lowest and highest levels of potassium intake would be associated with increased risk for all-cause, CVD, and stroke mortality.
Materials and Methods
Study Sample
Participants were 1,782 members of the Rancho Bernardo Study of Healthy Aging (RBS), who attended a research visit in 1992–96, when a food frequency questionnaire (FFQ) was administered. After excluding participants who were younger than 50 years old (n= 42), were missing dietary data (n=362), had 70 or more missing responses on the FFQ (n=7), or had implausible caloric intake (<700 or >4200 calories/day; n=812), there remained 1,363 individuals in the analytic sample. The study protocol was approved by the Institutional Review Board of the University of California, San Diego. All participants provided written informed consent.
Dietary Assessment
Participants completed the 153-item semiquantitative Willett FFQ, which asked them to indicate how often they consumed each of 153 foods in the past year.12,13 The Willett nutrient and database program was used to estimate daily nutrient intakes (HarvardSSFQ.5/93; Harvard TC Chan School of Public Health, Boston, Massachusetts). We examined daily intake of potassium, sodium, alcohol, calcium, fats, and total calories. We also included a measure of global dietary quality by determining degree of adherence to a Mediterranean-style diet.14,15 All measures were adjusted to a 2,000-calorie diet. The FFQ did not contain questions on the use of potassium chloride (KCl) salt substitutes. Our measure of dietary potassium does include potassium from vitamins and supplements. However, the amount of potassium in non-prescription supplements is limited to <100 mg by the Food and Drug Administration (FDA) and is not a significant source of daily potassium intake.16
Vital Status
Vital status was determined annually by mailed questionnaires through June 2016. Participants not known to be dead were censored at the date of last contact. Death certificates, available for 88% of decedents (n=750/855), were coded for underlying cause of death by a certified nosologist using the International Classification of Disease, Ninth Revision (ICD9). Outcome measures included all-cause mortality, cardiovascular disease (CVD) mortality, and stroke mortality. CVD mortality was defined as ICD9 codes 401 to 448; stroke mortality as ICD9 codes 430 to 438. Participants for whom we had a date of death, as determined from family report, obituaries, or the national death registry, but no death certificate, were included in analysis of all-cause mortality only.
Covariate Assessment
All covariates were assessed at the 1992–96 visit in which the FFQ was administered. A standardized, self-administered survey was used to assess smoking status (never, past, or current), exercise ≥ 3 times per week (yes or no), self-reported health rating (excellent, very good, good, fair or poor), medical history, and medication use. We categorized participants by number of common chronic diseases (0, 1, >1) including CVD, emphysema, cancer, osteoporosis, diabetes, arthritis, and hypertension. Educational attainment, ascertained at study entry, was classified as ≤12 years, 13–15 years, 16 years, and 17 or more years.
Trained nurses measured height, weight, and waist-hip ratio (WHR) with participants wearing light clothing and no shoes. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared and used as a measure of overall obesity. WHR was used as a measure of central obesity. Systolic (SBP) and diastolic blood pressure (DBP) was measured twice in rested, seated participants by nurses trained in the Hypertension Detection and Follow-up Program.17
Blood samples were obtained after a requested overnight fast. Fasting plasma glucose was measured by the glucose oxidase method by high performance liquid chromatography. Fasting plasma triglycerides, total cholesterol, high-density lipoprotein (HDL) and low-density lipoprotein (LDL) cholesterol were measured in a Centers for Disease Control and Prevention certified Lipid Research Clinic Laboratory. Enzymatic techniques using an ABA-200 biochromatic analyzer (Abbott Laboratories, Abbott Park, Illinois) measured total cholesterol and triglyceride levels. HDL cholesterol was measured according to the standardized procedures of the Lipid Research Clinic’s manual; LDL cholesterol was calculated using the Friedewald formula.18
Systolic (SBP) and diastolic blood pressure (DBP) was measured twice in seated participants. Hypertension was defined as SBP ≥ 140 mmHg, DBP≥90 mmHg, or use of anti-hypertensive medications. Diabetes was defined according to the 1999 World Health Organization Criteria: fasting plasma glucose ≥ 126 mg/dl, post-challenge plasma glucose ≥ 200 mg/dl, use of diabetes medications, or physician diagnosis. Kidney function was assessed by estimating the glomerular filtration rate (eGFR) using the abbreviated Modification of Diet in Renal Disease study equation.19 Prevalent CVD was defined as a self-reported history of coronary artery bypass surgery, angioplasty, myocardial infarction, angina, congestive heart failure, stroke or transient ischemic attack, carotid surgery, peripheral arterial surgery, or physician-diagnosed intermittent claudication.
Statistical Analysis
Because potassium intake was highly correlated with total caloric intake (r=0.78) we adjusted for total caloric intake using the nutrient residual method.20 Calorie-adjusted potassium intake was categorized into sex-specific quintiles to allow exploration of non-linear associations. Comparisons of demographic and health-related variables across potassium intake quintiles were performed using chi-square tests for categorical variables and analyses of variance (ANOVAs) for continuous variables. Cox proportional hazards regressions were used to examine associations of sex-specific quintiles of potassium intake with mortality using the third quintile as the reference category. Model 1 adjusted for age, sex, and total caloric intake. Model 2 additionally adjusted for exercise, education, daily alcohol intake, BMI, monounsaturated to saturated (mon/sat) fat ratio, total calcium, and calorie-adjusted sodium intake. Model 3 additionally included diabetes, hypertension, prevalent CVD, and eGFR. Possible linear associations of potassium intake with mortality was also assessed with potassium intake as a continuous variable.
Using potassium intake as a categorical variable, we tested for possible interactions of potassium intake by sex21,22 and kidney function (eGFR).23,24 To address bias that may result from including individuals in poor health at time of dietary assessment, we conducted three separate sensitivity analyses excluding participants who had prevalent CVD at baseline, diabetes at baseline, or who died within the first 2 years of follow-up. To address potential confounding due to overall dietary pattern, we included Mediterranean Diet score as a random effect to allow the association between potassium intake and mortality to vary by participants’ baseline diet.
Data were analyzed using R (R Foundation for Statistical Computing, Vienna, Austria). P-values <0.05 were considered significant.
Results
Mean age of participants at baseline was 71.0 ±10.6 years. The average length of follow-up was 13.5 ± 6.2 years. Men comprised 39.8% of the sample (n=542). Men consumed significantly less potassium than women (average of 2,853 mg/day versus 3,096 mg/day, respectively). Unadjusted comparisons of baseline characteristics by sex-specific quintile of calorie-adjusted daily potassium intake indicated that there were significant differences between potassium quintiles for age, education, exercise, and diet variables (Table 1). Participants in Q1 and Q2 were younger than those in the higher quintiles. Education level and rate of exercise increased as dietary potassium quintile increased. No significant differences between potassium quintiles were observed for any of the health parameters. Increasing potassium intake was associated with increasing sodium and calcium intake, decreasing alcohol intake, and increasing adherence to a Mediterranean diet.
Table 1.
Baseline participant characteristics by sex-specific quintile of calorie-adjusted daily potassium intake (mg/day), Rancho Bernardo Study, 1992–96 (n=1,363).
| Daily Potassium Intake, Quintilea | ||||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | ||
| Characteristic | N (%) | N (%) | N (%) | N (%) | N (%) | p-value |
| Education (years) | 0.04 | |||||
| ≤12 | 86 (31.5) | 62 (22.8) | 70 (25.7) | 68 (25.0) | 50 (18.2) | |
| 13–15 | 97 (35.5) | 93 (34.2) | 85 (31.2) | 85 (31.2) | 96 (35.0) | |
| 16 | 57 (20.9) | 81 (29.8) | 77 (28.3) | 72 (26.5) | 77 (28.1) | |
| 17+ | 33 (12.1) | 36 (13.2) | 40 (14.7) | 47 (17.3) | 51 (18.6) | |
| Smoking | 0.16 | |||||
| Never | 120 (44.0) | 125 (46.0) | 127 (47.0) | 111 (40.8) | 112 (41.0) | |
| Past | 126 (46.2) | 128 (47.1) | 126 (46.7) | 146 (53.7) | 148 (54.2) | |
| Current | 27 (9.9) | 19 (7.0) | 17 (6.3) | 15 (5.5) | 13 (4.8) | |
| Exercise (≥3/wk) | 175 (64.6) | 186 (68.4) | 194 (71.6) | 207 (76.1) | 223 (81.4) | <0.001 |
| Diabetes | 32 (11.7) | 39 (14.3) | 33 (12.1) | 39 (14.3) | 33 (12.0) | 0.80 |
| Hypertension | 137 (50.4) | 137 (50.4) | 142 (52.4) | 150 (55.1) | 144 (52.7) | 0.79 |
| Prevalent CVD | 42 (15.4) | 48 (17.6) | 44 (16.2) | 38 (14.0) | 55 (20.1) | 0.37 |
| Cancer | 32 (15.2) | 45 (20.5) | 26 (11.4) | 40 (16.9) | 38 (16.7) | 0.12 |
| eGFRb <60 | 46 (16.9) | 33 (12.3) | 46 (17.0) | 62 (23.0) | 36 (13.2) | 0.01 |
| Health rating | 0.65 | |||||
| Excellent | 61 (22.3) | 65 (23.9) | 75 (27.6) | 64 (23.7) | 68 (24.9) | |
| Very Good | 112 (41.0) | 121 (44.5) | 108 (39.7) | 125 (46.3) | 118 (43.2) | |
| Good | 75 (27.5) | 69 (25.4) | 60 (22.1) | 58 (21.5) | 66 (24.2) | |
| Fair or Poor | 25 (9.2) | 17 (6.2) | 29 (10.7) | 23 (8.5) | 21 (7.7) | |
| Number of diseases | 0.54 | |||||
| 0 | 90 (33.0) | 87 (32.0) | 79 (29.0) | 76 (27.9) | 77 (28.1) | |
| 1 | 94 (34.4) | 85 (31.2) | 108 (39.7) | 98 (36.0) | 96 (35.0) | |
| 2 or more | 89 (32.6) | 100 (36.8) | 85 (31.2) | 98 (36.0) | 101 (36.9) | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p-value | |
| Age (years) | 69.5 (11.4) | 70.8 (10.4) | 72.0 (10.6) | 72.7 (9.7) | 72.0 (10.7) | <0.01 |
| BMI (kg/m2) | 25.6 (4.3) | 25.4 (4.3) | 25.4 (3.7) | 25.3 (3.9) | 25.1 (3.7) | 0.62 |
| Waist hip ratio | 0.84 (0.09) | 0.84 (0.10) | 0.84 (0.09) | 0.84 (0.10) | 0.84 (0.09) | 0.81 |
| Systolic BP (mmHg) | 136.7 (22.0) | 136.0 (22.0) | 136.6 (21.7) | 137.0 (20.5) | 136.6 (23.4) | 0.99 |
| Diastolic BP (mmHg) | 76.3 (9.5) | 76.0 (9.8) | 76.2 (9.3) | 75.5 (8.8) | 74.8 (9.6) | 0.34 |
| Total cholesterol (mg/dL) | 211.0 (35.7) | 209.0 (35.5) | 210.0 (36.3) | 208.8 (38.8) | 208.2 (35.9) | 0.90 |
| HDL cholesterol (mg/dL) | 57.6 (17.4) | 58.5 (18.9) | 58.2 (18.0) | 58.3 (16.6) | 58.8 (16.2) | 0.96 |
| LDL cholesterol (mg/dL) | 128.5 (32.9) | 125.6 (31.8) | 127.3 (30.9) | 125.5 (33.2) | 126.2 (33.1) | 0.79 |
| Triglycerides (mg/dL) | 124.6 (71.2) | 126.7 (85.1) | 115.4 (67.0) | 125.2 (95.0) | 116.1 (60.1) | 0.25 |
| eGFR (mL/min/1.73m2) b | 77.2 (22.8) | 79.6 (18.8) | 76.6 (23.6) | 74.3 (19.0) | 77.0 (21.5) | 0.08 |
| Potassium (mg/day) | 2199 (345) | 2694 (136) | 2963 (135) | 3254 (151) | 3887 (592) | <0.001 |
| Sodium (mg/day) c | 1875 (461) | 1959 (338) | 2016 (332) | 2031 (346) | 2119 (547) | <0.001 |
| Total calories, (kcal) | 1987 (612) | 1693(512) | 1689 (497) | 1757(482) | 1965 (544) | <0.001 |
| Alcohol (g) | 10.5 (13.0) | 9.0 (10.8) | 7.9 (9.2) | 7.6 (9.7) | 6.7 (10.1) | <0.001 |
| Mon/sat fat ratio | 1.2 (0.2) | 1.2 (0.2) | 1.2 (0.2) | 1.2 (0.2) | 1.1 (0.2) | 0.01 |
| Calcium (mg/day) | 849 (459) | 909 (485) | 932 (515) | 1034 (552) | 1268 (634) | <0.001 |
| Mediterranean diet | 3.0 (1.4) | 3.9 (1.5) | 4.5 (1.6) | 4.9 (1.6) | 5.3 (1.6) | <0.001 |
Calorie-adjusted (to a 2000-calorie diet) potassium intake (mg) by sex-specific quintile:
Women: Q1≤ 2606, Q2=2607–2931, Q3=2932–3193, Q4=3194–3533, Q5≥3534;
Men: Q1≤ 2414, Q2=2415–2685, Q3=2686–2956, Q4=2957–3269, Q5≥3270;
eGFR, available on 1,347 participants
Sodium, available on 1,359 participants
CVD=cardiovascular disease; BP=blood pressure; HDL=high-density lipoprotein; LDL=low-density lipoprotein; eGFR=estimated glomerular filtration rate
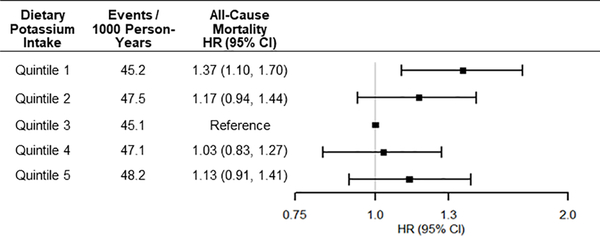
During the 20-year follow-up, there were 855 deaths (overall mortality rate 62.7%). In the subset of 750 participants with death certificates; 304 deaths were due to CVD and 76 to stroke. Hazard ratios (HR) for all-cause and cause-specific mortality by sex-specific quintile of calorie-adjusted daily potassium intake are shown in Table 2. Relative to Q3, participants in Q1 had 37% greater risk of all-cause mortality (95% CI 10%to 70%); an effect that was not materially changed by additional adjustment lifestyle, dietary, and health factors. HRs for all-cause mortality in the fully-adjusted model are shown in Figure 1. Potassium intake was not significantly related to CVD mortality or stroke mortality in fully adjusted models (Table 2).
Table 2:
Hazard ratios for all-cause and cause-specific mortality by sex-specific quintile of calorie-adjusted daily potassium intake (mg/day), Rancho Bernardo Study, 1992–96.
| Daily Potassium Intake, Quintilea | |||||
|---|---|---|---|---|---|
| Mortality | Q1 HR (95% CI) | Q2 HR (95% CI) | Q3 Reference | Q4 HR (95% CI) | Q5 HR (95% CI) |
| All-Cause | |||||
| Number of deaths; person-years at risk | 164; 3627 | 177; 3724 | 165; 3659 | 175; 3719 | 174; 3606 |
| Model 1b | 1.37 (1.10,1.70) | 1.17 (0.94,1.44) | 1 | 1.03 (0.83,1.27) | 1.13 (0.91,1.41) |
| Model 2c | 1.36 (1.08,1.71) | 1.16 (0.94,1.44) | 1 | 1.01 (0.82,1.26) | 1.13 (0.90,1.41) |
| Model 3d | 1.33 (1.06,1.67) | 1.13 (0.91,1.40) | 1 | 1.01 (0.82,1.26) | 1.11 (0.88,1.38) |
| CVD | |||||
| Number of deaths; person-years at risk | 51; 3627 | 68; 3724 | 52; 3659 | 72; 3719 | 61; 3606 |
| Model 1b | 1.45 (0.98,2.15) | 1.45 (1.01,2.08) | 1 | 1.39 (0.97,1.99) | 1.31 (0.90,1.91) |
| Model 2c | 1.51 (1.00,2.26) | 1.46 (1.02,2.11) | 1 | 1.35 (0.94,1.94) | 1.28 (0.87,1.88) |
| Model 3d | 1.38 (0.92,2.08) | 1.34 (0.93,1.94) | 1 | 1.32 (0.92,1.89) | 1.18 (0.79,1.74) |
| Stroke | |||||
| Number of deaths; person-years at risk | 15; 3627 | 22; 3724 | 11; 3659 |
16; 3719 |
12; 3606 |
| Model 1b | 1.82 (0.82,4.03) | 2.21 (1.07,4.56) | 1 | 1.43 (0.66,3.08) | 1.12 (0.49,2.57) |
| Model 2c | 1.89 (0.83,4.28) | 2.21 (1.06,4.59) | 1 | 1.40 (0.64,3.02) | 1.07 (0.46,2.49) |
| Model 3d | 1.71 (0.75,3.91) | 1.92 (0.91,4.03) | 1 | 1.36 (0.63,2.96) | 1.02 (0.44,2.40) |
Calorie-adjusted (to a 2000-calorie diet) potassium intake (mg) by sex-specific quintile:
Women: Q1≤ 2606, Q2=2607–2931, Q3=2932–3193, Q4=3194–3533, Q5≥3534;
Men: Q1≤ 2414, Q2=2415–2685, Q3=2686–2956, Q4=2957–3269, Q5≥3270
Model 1: adjusted for sex, age, total caloric intake (n=1,363)
Model 2: Model 1 + exercise, education, alcohol intake, BMI, Mon/Sat Fat Ratio, calcium, and sodium intake (n=1,359)
Model 3: Model 2 + diabetes, hypertension, prevalent CVD, and eGFR (n=1,347)
Figure 1:
Events per 1000-person years and hazard ratios for all-cause mortality by sex-specific quintile of calorie-adjusted daily potassium intake, adjusted for age, sex and total caloric intake.
There were no significant interactions between potassium intake and sex, age, hypertension status or eGFR (p-value >0.05) for all-cause, CVD, or stroke mortality. Excluding participants with prevalent CVD, prevalent diabetes or who died within the first 2 years of follow-up did not materially change results. Inclusion of Mediterranean diet score did not change the results. No significant linear trends between potassium intake and all-cause mortality were observed.
Discussion
This study examined the association between potassium intake and all-cause and cause-specific mortality among older, community-dwelling adults followed for over 20 years. Diets in the lowest 20% of potassium intake (<1,900 mg/day for men; <1,800 mg/day for women, adjusted to a 2,000-calorie diet) were associated with a 33% increased risk of death compared to participants in the third quintile, independent of age, education, health behaviors, other dietary factors, and health status. Further increases in potassium intake were not associated with progressively lower risk. The highest quintile of potassium intake was not associated with increased risk. Although hazard ratios for cardiovascular and stroke mortality were larger for those in the lowest two quintiles of potassium intake, differences were not significant after adjustment for health parameters.
The finding that low potassium intake is associated with higher risk of all-cause mortality is generally consistent with results from the three studies that have examined dietary potassium intake and mortality. The Rotterdam study examined the association of potassium intake, assessed with a FFQ, in 1,205 adults aged 55 and older, followed for 5 years. Results showed that increased potassium intake was associated with reduced risk of all-cause mortality.8 Analysis of data from a nationally representative sample of 12,267 adults, aged 20 and over from the Third National Examination and Nutritional Health Survey (NHANES III), found that higher dietary potassium, assessed with a 24-hour food recall, was associated with lower risk of all-cause mortality over an average 15 years’ follow-up.9 Analysis of FFQ data from 90,137 participants of the Women’s Health Initiative, aged 50 to 79 at baseline and followed for an average of 11 years, found higher risk of all-cause mortality among women with the lowest quartile of potassium intake.10
Associations of potassium intake with CVD or stroke mortality have been less consistently observed. The lack of a significant association between CVD mortality and potassium intake observed here is consistent with results of the Rotterdam study.8 However, in NHANES III, higher potassium intake was associated with lower risk of CVD mortality.9 Relative to our sample, the NHANES III sample had greater ethnic diversity, greater prevalence of current smoking, and lower education levels than our sample, known risk factors for CVD mortality. Dietary potassium may show stronger protective associations among those at higher risk of CVD mortality.
The lack of significant association between dietary potassium and stroke mortality observed here is also consistent with findings from the Rotterdam study.8 This is in contrast to earlier findings on a subset (n=859) of the Rancho Bernardo Study cohort who completed a 24 hour dietary recall in the 1972–1974 visit.25 Results from that study showed that higher potassium intake was associated with reduced risk for stroke death among women.25 However, there were few stroke deaths during the 12-year follow-up (9 for men, 15 for women). Analyses of data from the NHANES I study (n=9,866) suggests that associations of dietary potassium with stroke mortality may differ by sex, race/ethnicity and health status: Dietary potassium intake was associated with reduced stroke mortality among black men, who consumed lower levels of potassium than white men, but not among white men or among women. Hypertensive men, but not hypertensive women or non-hypertensive men, also showed an association between higher potassium intake and reduced stroke mortality.26
The function of potassium in the body is closely linked with sodium.1 Both high and low levels of sodium intake are associated with high blood pressure27–29 and increased mortality risk.8,9,30–32 We did not examine mortality in relation to the sodium:potassium ratio because FFQs have substantial potential for systematic error in dietary sodium assessment33, thus FFQ are not recommended for use in assessing associations of sodium intake with health outcomes.34 There is less risk of bias in estimation of potassium intake from FFQs.35 We adjusted for sodium intake, assuming that any inaccuracies in the measurement of sodium would be randomly distributed across potassium intake quintiles. Our observation of a significant association between potassium intake and mortality persisted after adjustment for sodium intake, suggesting an independent association between potassium intake and mortality beyond potassium’s relationship with sodium.
It is possible that our results may be due to a healthier diet overall among those who consume higher levels of potassium. However, results were unchanged after including a Mediterranean diet score as a random effect, suggesting that the observed potassium association was independent of the overall effect of a healthier diet. It is also possible that the association of low potassium intake with increased risk of mortality arises because people who are less healthy, and thus at higher risk of early death, may eat a more limited diet. However, results were unchanged in sensitivity analyses excluding those with prevalent CVD or diabetes at baseline, or participants who died within the first 2 years of follow-up, suggesting that neither known or occult disease accounts for our findings
Limitations of this study include the relatively homogenous sample, comprising mostly white, well-educated, middle-class individuals, which may limit generalizability. However, this decreases confounding due to race/ethnicity, access to health care, and the ability to access nutritious foods. In addition, we were unable to identify cause-specific mortality among 12% of decedents in our study due to the absence of death certificates. Key strengths of our study are the long follow-up of up to 20 years and the ability to adjust for numerous carefully assessed health-related covariates.
Conclusion
Older adults with the lowest levels of potassium intake were at significantly greater risk of death over the 20 year follow up period. Although caution is warranted in drawing causal inferences from observational data, these findings suggest that monitoring potassium intake among older adults may be important for reducing risk of early mortality. Since many fruits, vegetables and oily fish are high in potassium, adherence to a Mediterranean style diet, as recommended by current dietary guidelines, would ensure potassium intake in excess of the amount found to be associated with increased mortality risk in this study.
Take Away Points.
Older adults with very low levels of dietary potassium showed increased risk of mortality.
This association was not explained by overall health status.
Ensuring adequate potassium intake by consuming potassium-rich foods such as fruits, vegetables, and oily fish, may enhance longevity in older age.
Acknowledgements
The authors would like to thank A. Z. LaCroix, PhD in the Joint Doctoral Program Practicum for helpful comments on the study. Jaclyn Bergstrom, MS and Richele Bettencourt, MS provided the Rancho Bernardo Study data.
This work was supported by the National Institutes of Health (NIH) under grant numbers R01AA021187 and R01AG062483. Data acquisition for the Rancho Bernardo Study was funded by the National Institutes of Health under grant numbers DK31801, AG07181, and AG028507.
Footnotes
Disclosure statement
None of the authors have any conflicts of interest to report.
References
- 1.World Health Organization. “Potassium intake for adults and children: Guideline”. (2012). [PubMed] [Google Scholar]
- 2.Martinez Steele E, Baraldi LG, Louzada ML, Moubarac JC, Mozaffarian D, Monteiro CA. “Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study”. BMJ Open. 6, no. 3 (2016): e009892, doi: 10.1136/bmjopen-2015-009892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services and U.S. Department of Agriculture. “2015–2020 Dietary Guidelines for Americans” 8th Edition (2015). [Google Scholar]
- 4.Cogswell EM, Loria LC, Terry MA, Zhao SL, Chen ST-C, Wang SC-Y, Wright SJ, Pfeiffer SC, Merritt SR, Moy SC, et al. “Nationally-representative 24-h Urine Specimens Indicate Most U.S. Adults Consume Excess Dietary Sodium and Not Enough Potassium, National Health and Nutrition Examination Survey (NHANES), 2014”. Circulation. 134, Suppl_1 (2016): A16878–A16878. [Google Scholar]
- 5.Phillips BM, Milner S, Zouwail S, Roberts G, Cowan M, Riley SG, Phillips AO. “Severe hyperkalaemia: demographics and outcome”. Clin Kidney J. 7, no. 2 (2014): 127–33, doi: 10.1093/ckj/sft158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. “Leading causes of death and numbers of deaths, by sex, race, and Hispanic origin: United States, 1980 and 2014” (2015).
- 7.England PH. Health Profile for England, 2017 2017. Available from: https://www.gov.uk/government/publications/health-profile-for-england.
- 8.Geleijnse JM, Witteman JC, Stijnen T, Kloos MW, Hofman A, Grobbee DE. “Sodium and potassium intake and risk of cardiovascular events and all-cause mortality: the Rotterdam Study”. Eur J Epidemiol. 22, no. 11 (2007): 763–70, doi: 10.1007/s10654-007-9186-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, Chang MH, Gwinn M, Dowling N, Khoury MJ, et al. “Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey”. Arch Intern Med. 171, no. 13 (2011): 1183–91, doi: 10.1001/archinternmed.2011.257. [DOI] [PubMed] [Google Scholar]
- 10.Seth A, Mossavar-Rahmani Y, Kamensky V, Silver B, Lakshminarayan K, Prentice R, Van Horn L, Wassertheil-Smoller S. “Potassium intake and risk of stroke in women with hypertension and nonhypertension in the Women’s Health Initiative”. Stroke. 45, no. 10 (2014): 2874–80, doi: 10.1161/STROKEAHA.114.006046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newberry SJ, Chung M, Anderson CAM, Chen C, Fu Z, Tang A, Zhao N, Booth M, Marks J, Hollands S, et al. “Sodium and Potassium Intake: Effects on Chronic Disease Outcomes and Risks”. AHRQ Comparative Effectiveness Reviews. Rockville, MD, (2018). [PubMed] [Google Scholar]
- 12.Willett W Nutritional Epidemiology. New York: Oxford University Press; (1998). [Google Scholar]
- 13.Willett WC, Sampson L, Browne ML, Stampfer MJ, Rosner B, Hennekens CH, Speizer FE. “The use of a self-administered questionnaire to assess diet four years in the past”. Am J Epidemiol. 127, no. 1 (1988): 188–99. [DOI] [PubMed] [Google Scholar]
- 14.Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB. “Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women”. Circulation. 119, no. 8 (2009): 1093–100, doi: 10.1161/CIRCULATIONAHA.108.816736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richard EL, Laughlin GA, Kritz-Silverstein D, Reas ET, Barrett-Connor E, McEvoy LK. “Dietary patterns and cognitive function among older community-dwelling adults”. Nutrients. 10, no. 8 (2018), doi: 10.3390/nu10081088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hendler SS, Rorvik DR. PDR for Nutritional Supplements. Montvale: Thomson Reuters; 2008. [Google Scholar]
- 17.“The hypertension detection and follow-up program: Hypertension detection and follow-up program cooperative group”. Prev Med. 5, no. 2 (1976): 207–15. [DOI] [PubMed] [Google Scholar]
- 18.Friedewald WT, Levy RI, Fredrickson DS. “Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge”. Clin Chem. 18, no. 6 (1972): 499–502. [PubMed] [Google Scholar]
- 19.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F, Chronic Kidney Disease Epidemiology C. “Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate”. Ann Intern Med. 145, no. 4 (2006): 247–54. [DOI] [PubMed] [Google Scholar]
- 20.Willett W, Stampfer MJ. “Total energy intake: implications for epidemiologic analyses”. Am J Epidemiol. 124, no. 1 (1986): 17–27. [DOI] [PubMed] [Google Scholar]
- 21.Hedayati SS, Minhajuddin AT, Ijaz A, Moe OW, Elsayed EF, Reilly RF, Huang CL. “Association of urinary sodium/potassium ratio with blood pressure: sex and racial differences”. Clin J Am Soc Nephrol. 7, no. 2 (2012): 315–22, doi: 10.2215/CJN.02060311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mente A, O’Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, Morrison H, Li W, Wang X, Di C, et al. “Association of urinary sodium and potassium excretion with blood pressure”. N Engl J Med. 371, no. 7 (2014): 601–11, doi: 10.1056/NEJMoa1311989. [DOI] [PubMed] [Google Scholar]
- 23.Kovesdy CP, Matsushita K, Sang Y, Brunskill NJ, Carrero JJ, Chodick G, Hasegawa T, Heerspink HL, Hirayama A, Landman GWD, et al. “Serum potassium and adverse outcomes across the range of kidney function: a CKD Prognosis Consortium meta-analysis”. Eur Heart J. 39, no. 17 (2018): 1535–1542, doi: 10.1093/eurheartj/ehy100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Noori N, Kalantar-Zadeh K, Kovesdy CP, Murali SB, Bross R, Nissenson AR, Kopple JD. “Dietary potassium intake and mortality in long-term hemodialysis patients”. Am J Kidney Dis. 56, no. 2 (2010): 338–47, doi: 10.1053/j.ajkd.2010.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khaw KT, Barrett-Connor E. “Dietary potassium and stroke-associated mortality. A 12-year prospective population study”. N Engl J Med. 316, no. 5 (1987): 235–40, doi: 10.1056/NEJM198701293160502. [DOI] [PubMed] [Google Scholar]
- 26.Fang J, Madhavan S, Alderman MH. “Dietary potassium intake and stroke mortality”. Stroke. 31, no. 7 (2000): 1532–7. [DOI] [PubMed] [Google Scholar]
- 27.Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. “Effect of lower sodium intake on health: systematic review and meta-analyses”. BMJ. 346 (2013): f1326, doi: 10.1136/bmj.f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.He FJ, Li J, Macgregor GA. “Effect of longer-term modest salt reduction on blood pressure”. Cochrane Database Syst Rev. 4 (2013): CD004937, doi: 10.1002/14651858.CD004937.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jackson SL, Cogswell ME, Zhao L, Terry AL, Wang CY, Wright J, Coleman King SM, Bowman B, Chen TC, Merritt RK, et al. “Association between urinary sodium and potassium excretion and blood pressure among adults in the United States: National Health and Nutrition Examination Survey, 2014”. Circulation. 137 (2017) 237–246, doi: 10.1161/CIRCULATIONAHA.117.029193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cook NR, Appel LJ, Whelton PK. “Sodium intake and all-cause mortality over 20 years in the Trials of Hypertension Prevention”. J Am Coll Cardiol. 68, no. 15 (2016): 1609–1617, doi: 10.1016/j.jacc.2016.07.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Judd SE, Aaron KJ, Letter AJ, Muntner P, Jenny NS, Campbell RC, Kabagambe EK, Levitan EB, Levine DA, Shikany JM, et al. “High sodium:potassium intake ratio increases the risk for all-cause mortality: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study”. J Nutr Sci. 2 (2013): e13, doi: 10.1017/jns.2013.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yamori Y, Liu L, Mizushima S, Ikeda K, Nara Y, Group CS. “Male cardiovascular mortality and dietary markers in 25 population samples of 16 countries”. J Hypertens. 24, no. 8 (2006): 1499–505, doi: 10.1097/01.hjh.0000239284.12691.2e. [DOI] [PubMed] [Google Scholar]
- 33.Cobb LK, Anderson CA, Elliott P, Hu FB, Liu K, Neaton JD, Whelton PK, Woodward M, Appel LJ, American Heart Association Council on L, et al. “Methodological issues in cohort studies that relate sodium intake to cardiovascular disease outcomes: a science advisory from the American Heart Association”. Circulation. 129, no. 10 (2014): 1173–86, doi: 10.1161/CIR.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 34.McLean RM, Farmer VL, Nettleton A, Cameron CM, Cook NR, Campbell NRC, Consortium T. “Assessment of dietary sodium intake using a food frequency questionnaire and 24-hour urinary sodium excretion: a systematic literature review”. J Clin Hypertens (Greenwich). 19, no. 12 (2017): 1214–1230, doi: 10.1111/jch.13148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Freedman LS, Commins JM, Moler JE, Willett W, Tinker LF, Subar AF, Spiegelman D, Rhodes D, Potischman N, Neuhouser ML, et al. “Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for potassium and sodium intake”. Am J Epidemiol. 181, no. 7 (2015): 473–87, doi: 10.1093/aje/kwu325. [DOI] [PMC free article] [PubMed] [Google Scholar]