ABSTRACT
Background: Children and adolescents are affected in various ways by the lockdown measures due to the COVID-19 pandemic. Therefore, it is crucial to better understand the effects of the COVID-19 pandemic on mental health in this age-group.
Objective: The objective was to investigate and compare the effects of the COVID-19 pandemic on mental health in three age groups (1–6 years, 7–10 years, 11–19 years) and to examine the associations with psychological factors.
Methods: An anonymous online survey was conducted from 9 April to 11 May 2020 during the acute phase of major lockdown measures. In this cross-sectional study, children and adolescents aged between 1 and 19 years were recruited as a population-based sample. They were eligible if they were residents in Austria, Germany, Liechtenstein or Switzerland, were parents/caregivers of a child aged between 1 and 10 years or adolescents ≥11 years, had sufficient German language skills and provided informed consent.
Results: Among 5823 participants, between 2.2% and 9.9% reported emotional and behavioural problems above the clinical cut-off and between 15.3% and 43.0% reported an increase in these problems during the pandemic. Significant age-related effects were found regarding the type and frequency of problems (χ2(4)≥50.2, P ≤ 0.001). While preschoolers (1–6 years) had the largest increase in oppositional-defiant behaviours, adolescents reported the largest increase in emotional problems. Adolescents experienced a significantly larger decrease in emotional and behavioural problems than both preschoolers and school-children. Sociodemographic variables, exposure to and appraisal of COVID-19, psychotherapy before COVID-19 and parental mental health significantly predicted change in problem-scores (F ≥ 3.69, P ≤ 0.001).
Conclusion: A substantial proportion of children and adolescents experience age-related mental health problems during the COVID-19 pandemic. These problems should be monitored, and support should be offered to risk-groups to improve communication, emotion regulation and appraisal style.
KEYWORDS: Pandemic, COVID-19, mental health, development, adolescence, children, age
HIGHLIGHTS
Between 15.3% and 43.0% of the 1 to 19 years old children and adolescents reported an increase of problems during COVID-19.
Between 2.0% and 9.9% reported emotional and behavioural problems above the clinical cut-off.
Effects were associated with age, gender, exposure to and appraisal of COVID-19, attending psychotherapy before COVID-19 and parental mental health.
Short abstract
Antecedentes: Los niños y adolescentes se ven afectados de diversas maneras por las medidas de confinamiento debidas a la pandemia de COVID-19. Por lo tanto, es crucial comprender mejor los efectos de la pandemia de COVID-19 en la salud mental de este grupo de edad.
Objetivo: El objetivo fue investigar y comparar los efectos de la pandemia COVID-19 en la salud mental en tres grupos de edad (1-6 años, 7-10 años, 11-19 años) y examinar las asociaciones con factores psicológicos.
Métodos: Se realizó una encuesta anónima en línea del 9 de abril al 11 de mayo de 2020 durante la fase aguda de las principales medidas de confinamiento. Como una muestra basada en la población, en este estudio transversal, se reclutaron niños y adolescentes de entre 1 y 19 años. Eran seleccionables si residían en Austria, Alemania, Liechtenstein o Suiza, si eran padres/cuidadores de un niño de entre 1 y 10 años o adolescentes ≥11 años, si tenían suficientes conocimientos de alemán y proporcionaban el consentimiento informado
Resultados: Entre los 5823 participantes, entre el 2,2% y el 9,9% informaron de problemas emocionales y de comportamiento por encima del corte clínico y entre el 15,3% y el 43,0% informaron de un aumento de estos problemas durante la pandemia. Se encontraron efectos significativos relacionados con la edad en cuanto al tipo y la frecuencia de los problemas (χ2(4)≥50.2, P≤0.001). Mientras que los preescolares (1-6 años) tuvieron el mayor aumento en las conductas oposicionistas-desafiantes, los adolescentes reportaron el mayor aumento en los problemas emocionales. Los adolescentes experimentaron una disminución significativamente mayor de los problemas emocionales y de conducta que los preescolares y los escolares. Las variables sociodemográficas, la exposición y percepción del COVID-19, la psicoterapia antes del COVID-19 y la salud mental de los padres predijeron significativamente el cambio en las puntuaciones de los problemas (F≥3,69, P≤0,001).
Conclusión: Una proporción sustancial de niños y adolescentes experimentan problemas de salud mental relacionados con la edad durante la pandemia de COVID-19. Estos problemas deben ser vigilados y se debe ofrecer apoyo a los grupos de riesgo para mejorar la comunicación, la regulación de las emociones y el estilo de evaluación.
Palabras clave: Pandemia, COVID-19, salud mental, desarrollo, adolescencia, niños, edad
背景:因 COVID-19疫情采取的封锁措施以各种方式影响着儿童和青少年。因此,更好地了解此年龄群体中 COVID-19 疫情对心理健康的影响至关重要。
目的:旨在研究和比较三个年龄段(1-6 岁、7-10 岁、11-19 岁)群体中 COVID-19 疫情对心理健康的影响,并考查其与心理因素的关系。
方法:2020 年 4 月 9 日至 5 月11日,在重大封锁的紧急阶段进行了匿名在线调查。在这项横断面研究中,招募了 1 到 19 岁之间的儿童和青少年作为总体样本。如果他们是奥地利、德国、列支敦士登或瑞士的居民,是 1 至 10 岁之间儿童或 11 岁以上青少年的父母/监护人,具有足够的德语能力并提供知情同意,则符合资格。
结果:在 5823 名参与者中,有 2.2 %和 9.9 %的人分别报告了超过临床临界值的情绪和行为问题,15.3%和43.0%的人分别报告疫情期间这些问题有所增加。在问题的类型和频率上发现了显著的年龄相关影响(χ2(4)≥50.2, P≤0.001)。学龄前儿童(1-6岁)的对立违抗行为增加最多,而青少年报告的情绪问题增加最多。与学龄前儿童和学龄儿童相比,青少年的情绪和行为问题减少幅度显著更大。社会人口统计学变量、对COVID-19的暴露和评估、COVID-19之前有过心理治疗以及父母的心理健康状况可以显著预测问题得分的变化(F ≥ 3.69,P ≤ 0.001)。
结论:在 COVID-19 疫情期间,很大比例的儿童和青少年经历了年龄相关的心理健康问题。这些问题应得到监管,并应向风险群体提供支持,以改善沟通、情绪调节和评估方式。
关键词: 疫情, COVID-19, 心理健康, 发育, 青少年, 儿童, 年龄
1. Introduction
The COVID-19 pandemic has affected almost all countries in the world. To contain the spread of the virus lockdown measures were implemented that have severely affected daily life. Several studies have demonstrated that public health restrictions, such as quarantine, lead to increased distress and negative psychological effects in many individuals (Brooks et al., 2020). These effects have been consistently reported for the COVID-19 pandemic in adults (Qiu et al., 2020; Roger et al., 2020; Wang, Pan, et al., 2020). However, the effects on children and adolescents are largely unknown (Lee, 2020) although this age-group is affected in various ways.
First, the closure of child care and educational institutions, playgrounds, and leisure facilities has substantially disrupted the social networks of children and adolescents. Peer contacts are a major source of help when experiencing mental health problems and are especially relevant during adolescence. Therefore, young people might be particularly vulnerable to the effects caused by physical distancing measures and have shown high levels of loneliness, depression and anxiety during and after enforced social isolation (Loades et al., 2020; Sharma, Miguel, & Sharma, 2020).
Second, children and their parents have been challenged by the closure of schools and the need for home-based distance-learning models. These challenges are exacerbated for families with low income, confined living conditions, economic uncertainty, and the need to work remotely or being unable to work. This may have led to distress in child-parent interactions with a negative impact on their relationship or even increased rates of parental burnout and child maltreatment (Cluver et al., 2020; Griffith, 2020; Russell, Hutchison, Tambling, Tomkunas, & Horton, 2020). Furthermore, the closure of schools may have triggered or enhanced worries in students and their parents about their academic success and may have increased existing mental health problems due to loss of school routines, social stabilization and access to mental health services (Fegert & Schulze, 2020; Fegert, Vitiello, Plener, & Clemens, 2020; Lee, 2020).
Third, due to their limited cognitive and verbal capacity very young children might have difficulties in understanding changes in their daily routine (e.g. absence of regular caregivers) and in processing complex information about COVID-19. They also have to deal with their parents’ worries about the pandemic and its consequences (e.g. fear of death of relatives, financial loss), which is particularly challenging given their limited reasoning and coping skills. Further, studies suggest that very young children are a uniquely vulnerable group to experience adverse and traumatic events, to react to them in a particular distressing way and to suffer from detrimental long-term effects on their development. This is due to their rapid emotional and physiological development and their strong dependency on their caregivers as the primary source of their coping socialization and to protect them physically as well as emotionally (Dalton, Rapa, & Stein, 2020; De Young & Landolt, 2018; Russell et al., 2020). Taken together, these potential risks for children and adolescents make them a vulnerable group at each age, which should be given research priority (Golberstein, Wen, & Miller, 2020; Holmes et al., 2020). Yet, empirical studies on the effect of the COVID-19 pandemic on their mental health are sparse.
Studies (Liang et al., 2020; Wang, Zhang, Zhao, Zhang, & Jiang, 2020) with mixed age-groups between 12 and 50 years found no evidence for an age-related effect on mental health problems. A preliminary study (Jiao, Wang, & Liu, 2020) found that more than 30% of the children and adolescents in a Chinese general population sample aged 3–18 years experienced symptoms of clinginess, inattention and irritability. Notably, preschoolers had significantly more severe symptoms of clinging and fear about the health of relatives compared to children aged 6–18 years. The latter reported significantly more symptoms of inattention and obsessive requests for updates about the pandemic. A study (Liu et al., 2020) including a sample of preschoolers aged 4–6 years found evidence for sleep disturbances characterized by later bed- and wake-times as well as longer nocturnal and shorter nap sleep durations. Changes in eating behaviour, stress, reduced exposure to sunlight and more technology use during lockdown may have exerted such a negative effect on the sleeping patterns of children (Becker & Gregory, 2020).
Focusing on school-children only, a study (Xie et al., 2020) found high rates of depression (23%) and anxiety (19%). Additionally, 52% reported to worry at least to a moderate degree. Higher age, stricter COVID-19 measures, and more pronounced worry and optimism were significantly associated with depression but not anxiety. Gender had neither a significant effect on depression nor on anxiety.
With regard to adolescent-samples (Buzzi et al., 2020; Guessoum et al., 2020; Oosterhoff & Palmer, 2020; Saurabh & Ranjan, 2020; Zhou et al., 2020), participants also reported high rates of moderate to severe depression, anxiety, worry, helplessness, fear and dysfunctional attitudes towards the pandemic. On the contrary, a decrease in the usage of most substances was found during the lockdown. However, the frequency of both alcohol and cannabis use increased. Depression and fear of the infectivity of COVID-19 predicted solitary substance use (Dumas, Ellis, & Litt, 2020).
As most of the aforementioned studies on the effects of the COVID-19 pandemic on the mental health of young people focused on either children or adolescents, a comparison of age-groups is not possible. Moreover, because most previous studies assessed current symptom levels, it remains unclear whether the reported symptoms had changed due to the COVID-19 pandemic. Therefore, the primary aim of this study was to assess the effects of the COVID-19 pandemic on emotional and behavioural problems of children and adolescents with a wide age-range from 1 to 19 years and to investigate how effects are related to age. Based on previous studies showing age-related stress reactions (McKinnon et al., 2016; Meiser-Stedman, Yule, Smith, Glucksman, & Dalgleish, 2005), we expected significant age-related effects on changes in emotional and behavioural problems experienced during the COVID-19 pandemic. Incorporating such a developmental psychopathology perspective seems promising as it might increase our understanding of symptom expression in the face of the COVID-19 pandemic by comparing responses across a broad age-range of children and adolescents. Such an understanding could also inform prevention- and intervention-strategies, ensuring that symptoms of special relevance for the respective age-group can be monitored carefully and targeted when necessary. We further hypothesized that sociodemographic variables, pre-existing risk factors present before the onset of the COVID-19 pandemic (i.e. attendance of psychotherapy, chronic physical disease(s), significant life events), exposure to and appraisal of COVID-19, and parental mental health would be significantly associated with changes in emotional and behavioural problems.
2. Methods
2.1. Study design and participants
In this cross-sectional study, an anonymous online survey with an expected duration of 20 minutes was developed. Participants were eligible if they (1) were residents in Austria, Germany, Liechtenstein or Switzerland; (2) were parents/caregivers of a child aged between 1 and 10 years or if they were adolescents ≥11 years; (3) had sufficient German language skills to understand the questions and (4) provided informed consent to study participation.
2.2. Procedures
The study was approved by the Institutional Review Boards of the universities of Zurich (#20.4.1) and Bern (#2020-04-00002). The survey was conducted from 9 April to 11 May 2020 as this was the period with major and mainly parallel lockdown measures in the respective countries, in particular closed day-care facilities and schools. Recruitment of participants was performed via email circulation, social media, websites and newspapers. Participants were provided with links for three different age-groups: (1) preschool-children (1–6 years), (2) school-children (7–10 years) and (3) adolescents aged 11 years or older. The survey including the informed consent was answered by parents or legal guardians for children younger than 11 years and by adolescents (11–19 years) themselves. No compensation was provided.
2.3. Outcomes
Emotional and behavioural problems were the primary outcome as assessed by specific items drawn from the respective age-adapted German versions of the Child Behaviour Checklist (CBCL): for ages 1–6 years (CBCL/1.5–5; Achenbach & Rescorla, 2000), for ages 7–10 years (CBCL/6-18R; Döpfner, Plück, & Kinnen, 2014), and for ages 11–19 years (Youth Self Report, YSR/11-18R; Döpfner et al., 2014). In children aged 1–6 years, affective problems (10 items), anxiety (10 items) and oppositional-defiant behaviours (6 items) were assessed by parent-report using the DSM-oriented subscales of the CBCL/1.5–5 (Achenbach & Rescorla, 2000). In children aged 7–10 years (CBCL/6-18R; Döpfner et al., 2014) and in adolescents aged 11–19 years (YSR/11-18R; Döpfner et al., 2014), problems corresponding to three established syndrome-scales were assessed: anxiety/depression (13 items), withdrawn/depression (8 items), aggressive behaviours (18 items CBCL/6-18R; 17 items YSR/11-18R) and three additional items (sleep, nightmares, and overtiredness). The CBCL/YSR are among the most widely used measures in children and adolescents with excellent psychometric properties (Nakamura, Ebesutani, Bernstein, & Chorpita, 2009). A specific behaviour in the CBCL/YSR is scored according to the manual on a three-point Likert scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true). Additionally, participants were asked in this study to indicate whether the respective behaviour occurred less (i.e. score of −1), equal (i.e. score of 0), or more since the COVID-19 pandemic (i.e. a score of +1). A raw summary change-score was calculated for each sub-/syndrome scale.
2.4. Covariates
The following covariates were assessed: sociodemographic variables (age, gender, living situation, parental education), pre-existing risk-factors (attendance of psychotherapy, chronic physical disease, life events), COVID-19 exposure, COVID-19 appraisals and parental mental health. Pre-existing risk-factors included questions (yes/no) whether the child/adolescent was in psychotherapy or had a chronic physical disease before COVID-19. Major family life events were assessed for the previous 6 months by the Life Event Scale (Landolt & Vollrath, 1998). This scale asks about the presence of 12 family life events resulting in a sum score between 0–12.
Exposure to COVID-19 was measured by self-generated questions on events related to COVID-19: closure of child-care/school, child is/was diagnosed with COVID-19, family member is/was diagnosed with COVID-19, family member is/was quarantined, family member is/was in hospital and death of a person related to the family. A summary score was formed assigning a score of ‘1’ per confirmed item and a score of ‘0’ if not (see supplementary eTable 1 for an overview of all self-generated items).
Appraisal was measured (1) by the degree of understanding of the child or adolescent about the COVID-19 pandemic used as a binary variable (yes/no) and (2) by three yes/no-questions about potential negative effects for the child/adolescent, family and parents resulting in a summary score between 0–3. Notably, appraisal questions captured the parental perception for children and the adolescents’ perception for the older age-group. Adolescent participants were additionally asked to answer three self-generated questions grounded in core concepts of stress-coping models (Groth et al., 2019; Lazarus & Folkman, 1984) on a three-point Likert-scale about the controllability of the situation (i.e. internal locus of control; Rotter, 1966), their confidence in being capable to deal with the situation efficiently (i.e. coping self-efficacy; Sandler, Kim-Bae, & MacKinnon, 2000), and the controllability of their emotions (i.e. emotion regulation; Gross, 1998).
Parental mental health was assessed in children <11 years via report of the caregiver using the Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001) and the Scale for General Anxiety Disorder (GAD-7; Spitzer, Kroenke, Williams, & Löwe, 2006) to measure the level of depressiveness and anxiety in the last 2 weeks. Both scales are well-validated screening instruments (Kroenke & Spitzer, 2002; Spitzer et al., 2006). The summary score of each measure was used. As a proxy for parental mental health, adolescents were asked to rate how worried their parents were about COVID-19 on a three-point Likert scale from ‘not at all worried’ to ‘very worried’.
2.5. Statistical analysis
Only full data-sets regarding outcome variables were analysed using SPSS 25 (IBM). We calculated means and standard deviations for continuous variables and frequencies for categorical variables. Statistical analyses were performed separately for the three age-groups: 1–6 (preschoolers), 7–10 (school-children) and 11–19 year olds (adolescents). Differences in frequencies of changes in emotional and behavioural problems between age-groups were tested on item-level by Chi2-tests with Cramer’s V as the effect size. Comparisons between all three age-groups were performed for 15 items of the CBCL/YSR, since these items are available in all age-versions (see eTable 2, supplementary data) (Achenbach & Rescorla, 2000; Döpfner et al., 2014). Standardized residuals and z-tests to compare column proportions were used to locate exact group-differences. Multivariable linear regressions were applied to assess associations between covariates and the summary change-scores of the sub-/syndrome-scales of the CBCL/YSR (Achenbach & Rescorla, 2000; Döpfner et al., 2014) as dependent variables. Statistical significance was defined by P-values <0.05 (two-sided).
3. Results
3.1. Sample characteristics
5823 children and adolescents (52.1% female) with a mean age of 7.6 (SD = 4.3) years participated in the study (see Table 1). Mothers answered the parent-reports in 89.1% (n = 4083) of all children. Among preschoolers (1–6y), 7.8% (n = 212) exceeded the clinical cut-off of T ≥ 70 (Achenbach & Rescorla, 2000; Döpfner et al., 2014) for affective problems, 4.7% (n = 128) for anxiety and 9.9% (n = 270) for oppositional-defiant problems. In school-children (7–10y), 9.7% (n = 179) scored above T ≥ 70 for anxiety/depression, 4.3% (n = 79) for withdrawn/depression and 9.9% (n = 184) for aggressive problems. In adolescents (11–19y), 9.0% (n = 112) scored above the clinical cut-off for anxiety/depression, 6.5% (n = 81) for withdrawn/depression and 2.0% (n = 25) for aggressive problems.
Table 1.
Descriptive sample characteristics for separate age-groups (N = 5823)
| Age group | 1–6 years N = 2726 |
7–10 years N = 1854 |
11–19 years N = 1243 |
|---|---|---|---|
| Age groups, No. (%) | 1y: 133 (4.9) | 7y: 427 (23.0) | 11y: 164 (13.2) |
| 2y: 310 (11.4) | 8y: 528 (28.5) | 12y: 152 (12.2) | |
| 3y: 600 (22.0) | 9y: 492 (26.5) | 13y: 162 (13.0) | |
| 4y: 763 (28.0) | 10y: 407 (22.0) | 14y: 177 (14.2) | |
| 5y: 569 (20.9) | 15y: 165 (13.3) | ||
| 6y: 351 (12.9) | 16y: 200 (16.1) | ||
| 17y: 111 (8.9) | |||
| 18y: 78 (6.3)19y: 34 (2.7) | |||
| Country, No. (%) | |||
| Switzerland/Liechtenstein | 1064 (39.0) | 790 (42.6) | 619 (49.8) |
| Germany | 1075 (39.4) | 447 (24.1) | 295 (23.7) |
| Austria | 580 (21.3) | 617 (33.3) | 329 (26.5) |
| Other | 7 (0.3) | ·· | ·· |
| Child gender, No. (%) | |||
| Female | 1355 (49.7) | 878 (47.4) | 802 (64.5) |
| Male | 1371 (50.3) | 975 (52.6) | 434 (34.9) |
| Diversea | ·· | 1 (0.1) | 7 (0.6) |
| Pre-COVID education, No. (%) | |||
| Attending daycare | 1143 (41.9) | ·· | ·· |
| Attending kindergarden | 1528 (56.1) | ·· | ·· |
| Attending school | ·· | ·· | 1146 (92.2) |
| Apprenticeship | ·· | ·· | 82 (6.6) |
| Dropped school/apprenticeship | ·· | ·· | 15 (1.2) |
| Living with both parents, No. (%) | 2552 (93.6) | 1650 (89.0) | 1000 (80.5) |
| Maternal education, No. (%) | |||
| Mandatory school not completed | 2 (0.1) | 2 (0.1) | ·· |
| Completed mandatory school | 18 (0.7) | 13 (0.7) | ·· |
| Completed apprenticeship (1–2 years) | 39 (1.4) | 37 (2.0) | ·· |
| Completed apprenticeship (3–4 years) | 480 (17.6) | 441 (23.8) | ·· |
| A-level equivalent or college of higher education | 835 (30.6) | 617 (33.3) | ·· |
| University | 1352 (49.6) | 743 (40.1) | ·· |
| Not applicable | 0 (0.0) | 1 (0.1) | ·· |
| Paternal education, No. (%) | |||
| Mandatory school not completed | 7 (0.3) | 4 (0.2) | ·· |
| Completed mandatory school | 36 (1.3) | 29 (1.6) | ·· |
| Completed apprenticeship (1–2 years) | 41 (1.5) | 37 (2.0) | ·· |
| Completed apprenticeship (3–4 years) | 632 (23.2) | 531 (28.6) | ·· |
| A-level equivalent or college of higher education | 835 (30.6) | 592 (31.9) | ·· |
| University | 1175 (43.1) | 653 (35.2) | ·· |
| Not applicable | 0 (0.0) | 8 (0.4) | ·· |
| Parental mental health | |||
| Depressiveness, PHQ-9, mean (SD) | 5.12 (4.09) | 4.44 (3.74) | ·· |
| Anxiety, GAD-7, mean (SD) | 4.41 (3.68) | 3.96 (3.41) | ·· |
| Parental worries about COVID-19, No. (%) | |||
| Not at all worried | ·· | ·· | 233 (18.7) |
| Little worried | ·· | ·· | 803 (64.6) |
| Very worried | ·· | ·· | 205 (16.5) |
| Not applicable | ·· | ·· | 2 (0.2) |
| Pre-COVID psychological treatment, No. (%) | 24 (0.9) | 95 (5.1) | 120 (9.7) |
| Missing | ·· | ·· | 3 (0.2) |
| Pre-existing child chronic physical disease, No. (%) | 88 (3.2) | 110 (5.9) | 97 (7.8) |
| Number of pre-COVID significant life events, LES | |||
| Mean (SD) | 0.77 (1.03) | 0.66 (1.04) | 0.93 (1.18) |
| None | 1413 (51.8) | 1094 (59.0) | 592 (47.6) |
| One | 775 (28.4) | 470 (25.4) | 359 (28.9) |
| Two | 374 (13.7) | 178 (9.6) | 159 (12.8) |
| ≥3 | 164 (6.1) | 112 (6.0) | 132 (10.7) |
| Missing | 0 (0.0) | 0 (0.0) | 1 (0.1) |
| Exposure to COVID-19, mean (SD) | 0.65 (0.61) | 1.08 (0.49) | 1.24 (0.62) |
| Appraisal | |||
| Understand yes, No. (%) | 1392 (51.1) | 1779 (96.0) | 1159 (93.2) |
| Negative consequences, Cronbach’s alpha, No. (%) | α = 0.72 | α = 0.64 | α = 0.63 |
| Summary score: 0 | 1699 (62.3) | 1054 (56.9) | 467 (37.6) |
| Summary score: 1 | 550 (20.2) | 486 (26.2) | 336 (27.0) |
| Summary score: 2 | 230 (8.4) | 174 (9.4) | 246 (19.8) |
| Summary score: 3 | 247 (9.1) | 140 (7.6) | 194 (15.6) |
| Internal Control, No. (%) | |||
| Not at all control | ·· | ·· | 94 (7.6) |
| Little control | ·· | ·· | 641 (51.6) |
| Very much control | ·· | ·· | 508 (40.9) |
| Coping self-efficacy, No. (%) | |||
| Not at all confident | ·· | ·· | 34 (2.7) |
| Little confident | ·· | ·· | 406 (32.7) |
| Very confident | ·· | ·· | 803 (64.6) |
| Emotionally overwhelmed, No. (%) | |||
| Not at all | ·· | ·· | 543 (43.7) |
| Little overwhelmed | ·· | ·· | 558 (44.9) |
| Very overwhelmed | ·· | ·· | 142 (11.4) |
| Changes in emotional and behavioural problemsc, CBCL/YSR | |||
| Changes in affective problems, mean (SD), range, Cronbach’s alpha | 1.00 (2.27), –10.00 to 10.00, α = 0.73 |
·· | ·· |
| Changes in anxiety problems, mean (SD), range, Cronbach’s alpha |
1.15 (2.29), –10.00 to 10.00, α = 0.79 |
·· | ·· |
| Changes in oppositional-def. problems, mean (SD), range, Cronbach’s alpha |
1.73 (2.47), –6.00 to 6.00, α = 0.89 |
·· | ·· |
| Changes in anxiety/depression, mean (SD), range, Cronbach’s alpha |
·· | 0.46 (3.14), –13.00 to 13.00, α = 0.87 |
0.14 (3.72), –13.00 to 13.00, α = 0.87 |
| Changes in withdrawn/depression, mean (SD), range, Cronbach’s alpha |
·· | 0.24 (2.02), –8.00 to 8.00, α = 0.84 |
−0.05 (2.48), –8.00 to 8.00, α = 0.81 |
| Changes in aggressive problems, mean (SD), range, Cronbach’s alpha |
·· | 1.27 (4.83), –18.00 to 18.00, α = 0.92 |
−0.71 (4.89), –17.00 to 17.00, α = 0.93 |
Note. ‘··’ indicates this item was not assessed in this study; a for calculation of T-scores mean score of the respective T-score for males and female was formed; binary gender (male/female) was used in regression analysis; b summary score comprised 7 items in the child-versions and 6 items in the adolescent-version; c raw summary-scores were calculated for each sub-/syndrome scale by summing the change-score of each corresponding item rated as decrease (score: −1), equal (score: 0), or increase (score: 1). Abbreviations: CBCL, Child Behaviour Checklist (Achenbach & Rescorla, 2000; Döpfner et al., 2014); GAD-7 (Spitzer et al., 2006), Scale for General Anxiety Disorder; LES (Landolt & Vollrath, 1998), Life Event Scale; NA, not applicable to this age-group; PHQ-9 (Kroenke et al., 2001), Patient Health Questionnaire-9; YSR (Döpfner et al., 2014), Youth Self-Report.
3.2. Changes in emotional and behavioural problems
Figure 1 depicts the frequencies of changes in the sub-/syndrome-scales of the CBCL/YSR (Achenbach & Rescorla, 2000; Döpfner et al., 2014). Between 15.3% and 43.0% of the participants reported an increase in problems during the COVID-19 pandemic. A detailed overview of changes on item-level for seven age groups is provided in eTable 2, supplementary data. Across all age-groups, being defiant and arguing was most consistently reported to have increased. In preschoolers, all oppositional symptoms (except: being uncooperative in 1–3y), crying, sleeping problems, clinging, sadness (4–6y), not sleeping alone (4–6y), and being upset by separation (1–3y) have consistently increased in more than 20% of the sample. In school-children (7–10y), an increase in being stubborn, mood changes, sulking, demanding attention, being nervous, and crying (7–8y) was most frequently reported (>20% of the sample). Adolescents consistently experienced an increase in nervousness (>20%). Those aged between 14–19 years also reported heightened levels of worries, overtiredness, underactivity, sadness and mood changes (>20%). Only adolescents aged 17–19 years, frequently (>20%) experienced an increase of fears about school and crying.
Figure 1.
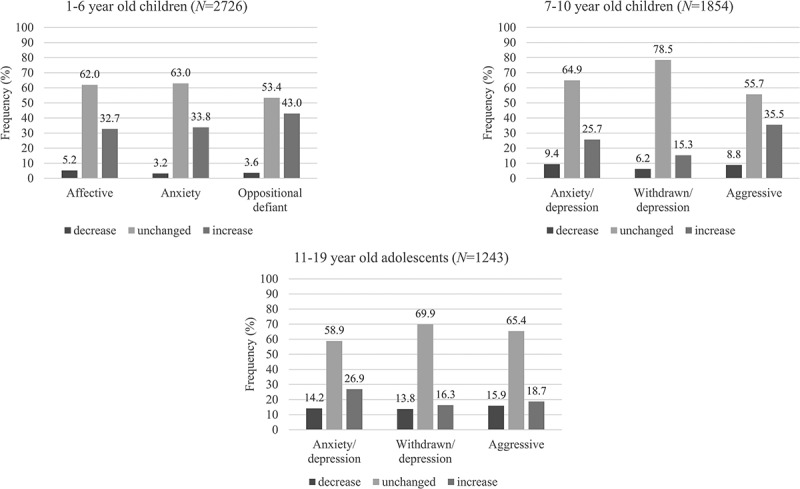
Changes in summary scores in emotional and behavioral problems for separate age-groups
An unchanged status is defined as summary change score between –1 and 1, an increase as a summary-change score >1, and a decrease as a summary-change score <–1.
3.3. Age-related effects on changes in emotional and behavioural problems
Significant differences between the three age-groups (1–6y, 7–10y, 11–19y) were found for changes in all 15 emotional and behavioural problems with small effect-sizes and a moderate effect-size (Cohen, 1988) for being disobedient (see Table 2). The increase of crying, sleeping problems/nightmares and all oppositional-defiant behaviours was significantly largest in preschoolers compared to school-children and adolescents. School-children were significantly more fearful than preschoolers and adolescents but showed a moderate increase in several emotional and behavioural problems. Up to 26.9% of adolescents reported an increase of problems (see Figure 1) that was highest in worries, being overtired, underactive and nervous compared to younger age-groups (see Table 2). Up to 15.9% of adolescents showed a decrease in problems and reported this significantly more frequently than preschool- and school-children in all but one of the 15 emotional and behavioural problems.
Table 2.
Age-related changes in emotional and behavioural problems since Corona-pandemic
| Age-group |
||||
|---|---|---|---|---|
| CBCL/YSR item (footnote: item number of CBCL1.5–5, CBCL6-18 R, YSR11-18 R); |
1–6 years (N = 2726) |
7–10 years (N = 1854) |
11–19 years (N = 1243) |
χ2(df), P-value (95% CI), Cramer’s V |
| Cries a lot13, 14, 14 | ||||
| Less, No. (%) Standardized residual, Z-value |
134a (4.9%) –2.7 |
92a (5.0%) –2.1 |
134b (10.8%) 6.5 |
χ2(4) = 87.78, P < 0.001 (0.000; 0.000), V = 0.09 |
| Equal, No. (%) Standardized residual, Z-value |
1913a (70.2%) –1.1 |
1363b (73.5%) 0.8 |
911a,b (73.3%) 0.6 |
|
| More, No. (%) Standardized residual, Z-value |
679a (24.9%) 3.3 |
399b (21.5%) –0.4 |
198c (15.9%) –4.5 |
|
| Trouble sleeping38,100,100 | ||||
| Less, No. (%) Standardized residual, Z-value |
114a (4.2%) –2.9 |
102a (5.5%) 0.1 |
102b (8.2%) 4.1 |
χ2(4) = 89.10, P < 0.001 (0.000; 0.000), V = 0.09 |
| Equal, No. (%) Standardized residual, Z-value |
1900a (69.7%) –1.9 |
1453b (78.4%) 2.8 |
887a (71.4%) -0.6 |
|
| More, No. (%) Standardized residual, Z-value |
712a (26.1%) 4.9 |
299b (16.1%) –5.2 |
254c (20.4%) –1.0 |
|
| Overtired50,54,54 | ||||
| Less, No. (%) Standardized residual, Z-value |
171a (6.3%) –1.6 |
96a (5.2%) –3.1 |
147b (11.8%) 6.2 |
χ2(4) = 321.90, P < 0.001 (0.000; 0.000), V = 0.17 |
| Equal, No. (%) Standardized residual, Z-value |
2254a (82.7%) 0.2 |
1699b (91.6%) 4.4 |
838c (67.4%) –5.8 |
|
| More, No. (%) Standardized residual, Z-value |
301a (11.0%) 0.7 |
59b (3.2%) –9.8 |
258c (20.8%) 11.0 |
|
| Little interest71, enjoys little5,5 | ||||
| Less, No. (%) Standardized residual, Z-value |
108a (4.0%) –4.1 |
100a (5.4%) –0.8 |
132b (10.6%) 7 · 0 |
χ2(4) = 97.80, P < 0.001 (0.000; 0.000), V = 0.09 |
| Equal, No. (%) Standardized residual, Z-value |
2397a (87.9%) 2.0 |
1564b (84.4%) 0.0 |
957c (77.0%) –2.9 |
|
| More, No. (%) Standardized residual, Z-value |
221a (8.1%) –2.7 |
190b (10.2%) 0.8 |
154b (12.4%) 3.0 |
|
| Underactive89,102,102 | ||||
| Less, No. (%) Standardized residual, Z-value |
126a (4.6%) –3.6 |
90a (4.9%) –2.6 |
155b (12.5%) 8.5 |
χ2(4) = 163.02, P < 0.001 (0.000; 0.000), V = 0.12 |
| Equal, No. (%) Standardized residual, Z-value |
2300a (84.4%) 2.8 |
1487b (80.2%) 0.3 |
849c (68.3%) –4.5 |
|
| More, No. (%) Standardized residual, Z -value |
300a (11.0%) –4.2 |
277b (14.9%) 1.1 |
239c (19.2%) 4.9 |
|
| Sad90,103,103 | ||||
| Less, No. (%) Standardized residual, Z-value |
98a (3.6%) –3.9 |
100b (5.4%) 0.1 |
112c (9.0%) 5.6 |
χ2(4) = 50.23, P < 0.001 (0.000; 0.000), V = 0.07 |
| Equal, No. (%) Standardized residual, Z-value |
2059a (75.5%) 0.6 |
1390a, b (75.0%) 0.2 |
888b (71.4%) –1.2 |
|
| More, No. (%) Standardized residual, Z-value |
569a (20.9%) 0.8 |
364a (19.6%) –0.5 |
243a (19.5%) –0.5 |
|
| Fears32,29,29 | ||||
| Less, No. (%) Standardized residual, Z-value |
73a (2.7%) –5.1 |
81b (4.4%) –0.9 |
128c (10.3%) 8.7 |
χ2(4) = 123.39, P < 0.001 (0.000; 0.000), V = 0.10 |
| Equal, No. (%) Standardized residual, Z-value |
2485a (91.2%) 1.7 |
1640b (88.5%) 0.2 |
1004 c (80.8%) –2.7 |
|
| More, No. (%) Standardized residual, Z-value |
168a (6.2%) –1.8 |
133a, b (7.2%) 0.2 |
111b (8.9%) 2.5 |
|
| Nervous47,45,45 | ||||
| Less, No. (%) Standardized residual, Z-value |
79a (2.9%) –6.3 |
137b (7.4%) 2.8 |
122b (9.8%) 5.9 |
χ2(4) = 294.46, P < 0.001 (0.000; 0.000), V = 0.16 |
| Equal, No. (%) Standardized residual, Z-value |
2252a (82.6%) 5.9 |
1273b (68.7%) –2.1 |
721c (58.0%) –6.2 |
|
| More, No. (%) Standardized residual, Z-value |
395a (14.5%) –7.7 |
444b (23.9%) 2.5 |
400c (32.2%) 8.3 |
|
| Nightmares48,47,47 | ||||
| Less, No. (%) Standardized residual, Z-value |
71a (2.6%) –5.4 |
91b (4.9%) 0.1 |
122c (9.8%) 7.9 |
χ2(4) = 118.94, P < 0.001 (0.000; 0.000), V = 0.10 |
| Equal, No. (%) Standardized residual, Z-value |
2273a, b (83.4%) –0.1 |
1586b (85.5%) 0.9 |
1005a (80.9%) –1.0 |
|
| More, No. (%) Standardized residual, Z-value |
382a (14.0%) 3.7 |
177b (9.5%) –2.6 |
116b (9.3%) –2.3 |
|
| Fearful87,50,50 | ||||
| Less, No. (%) Standardized residual, Z-value |
70a (2.6%) –5.8 |
104b (5.6%) 1.1 |
120c (9.7%) 7.2 |
χ2(4) = 109.22, P < 0.001 (0.000; 0.000), V = 0.10 |
| Equal, No. (%) Standardized residual, Z-value |
2452a (89.9%) 1.7 |
1560b (84.1%) –1.2 |
1045b (84.1%) –1.0 |
|
| More, No. (%) Standardized residual, Z -value |
204a (7.5%) –1.1 |
190b (10.2%) 3.2 |
78a (6.3%) –2.3 |
|
| Worries99,112,112 | ||||
| Less, No. (%) Standardized residual, Z-value |
57a (2.1%) –5.4 |
89b (4.8%) 1.3 |
98c (7.9%) 6.4 |
χ2(4) = 163.59, P < 0.001 (0.000; 0.000), V = 0.12 |
| Equal, No. (%) Standardized residual, Z-value |
2290a (84.0%) 3.1 |
1464b (79.0%) 0.1 |
835c (67.2%) –4.6 |
|
| More, No. (%) Standardized residual, Z-value |
379a (13.9%) –3.9 |
301a (16.2%) –0.8 |
310b (24.9%) 6.8 |
|
| Defiant15, argues3,3 | ||||
| Less, No. (%) Standardized residual, Z-value |
82a (3.0%) –4.3 |
98b (5.3%) 0.9 |
101c (8.1%) 5.3 |
χ2(4) = 142.74, P < 0.001 (0.000; 0.000), V = 0.11 |
| Equal, No. (%) Standardized residual, Z-value |
1592a (58.4%) –2.8 |
1182b (63.8%) 0.6 |
871c (70.1%) 3.3 |
|
| More, No. (%) Standardized residual, Z-value |
1052a (38.6%) 5.5 |
574b (31.0%) –1.2 |
271c (21.8%) –6.7 |
|
| Disobedient20, disob. at home22,22 | ||||
| Less, No. (%) Standardized residual, Z-value |
65a (2.4%) –5.7 |
87b (4.7%) –0.1 |
125c (10.1%) 8.6 |
χ2(4) = 500.37, P < 0.001 (0.000; 0.000), V = 0.21 |
| Equal, No. (%) Standardized residual, Z-value |
1729a (63.4%) –5.7 |
1472b (79.4%) 3.4 |
1031c (82.9%) 4.2 |
|
| More, No. (%) Standardized residual, Z-value |
932a (34.2%) 12.8 |
295b (15.9%) –6.0 |
87c (7.0%) –11.6 |
|
| Stubborn81,86,86 | ||||
| Less, No. (%) Standardized residual, Z-value |
82a (3.0%) –4.2 |
91b (4.9%) 0.3 |
104c (8.4%) 5.8 |
χ2(4) = 305.30, P < 0.001 (0.000; 0.000), V = 0.16 |
| Equal, No. (%) Standardized residual, Z-value |
1771a (65.0%) –3.3 |
1271b (68.6%) –0.8 |
1046c (84.2%) 5.9 |
|
| More, No. (%) Standardized residual, Z-value |
873a (32.0%) 7.3 |
492b (26 · 5%) 1 · 3 |
93c (7.5%) –12.4 |
|
| Temper tantrums85,95,95 | ||||
| Less, No. (%) Standardized residual, Z-value |
92a (3.4%) -4.7 |
99b (5.3%) –0.2 |
127c (10.2%) 7.2 |
χ2(4) = 244.79, P < 0.001 (0.000; 0.000), V = 0.15 |
| Equal, No. (%) Standardized residual, Z-value |
1776a (65.2%) –3.6 |
1411b (76.1%) 2.6 |
949b (76.3%) 2.2 |
|
| More, No. (%) Standardized residual, Z-value |
858a (31.5%) 8.6 |
344b (18.6%) –4.4 |
167c (13.4%) –7.3 |
|
Note. Standardized residuals are the difference between the expected and the observed frequencies divided by the square root of the expected frequencies. Standardized residuals are significant at P < 0.05 for Z>|1.96|, at P < 0.01 for Z>|2.58|, at P < 0.001 for Z>|3.29|; different subscripts a, b, and c indicate significant differences at P < 0.05 for comparison of column frequencies between age-groups; Cramer’s V (df* = 2) is small for V = 0.07 and moderate for V = 0.21 (Cohen, 1988)29. Abbreviations: CBCL (Achenbach & Rescorla, 2000; Döpfner et al., 2014), Child Behaviour Checklist; YSR (Döpfner et al., 2014), Youth Self-Report.
3.4. Predictors of changes in emotional and behavioural problems
Results of multivariable regression analysis are shown in Table 3. All regression models were significant with the explained variance between 3.0% in adolescents and 19.0% in preschoolers. Regarding socio-demographic variables, being older was significantly associated with an increase in affective and oppositional-defiant behaviours in preschoolers and in withdrawn/depression problems in school-children. Males were significantly more likely to experience an increase in oppositional-defiant/aggressive problems in both preschool- and school-children than females. Living together with both parents was associated with higher levels of all types of problems in preschoolers and more depression/anxiety in school-children. Higher parental education assessed in children only was significantly related to an increase in anxiety in preschoolers and anxiety/depression as well as withdrawn/depression in school-children. Socio-demographic variables were not significantly associated with any outcome-domain in adolescents.
Table 3.
Predictors of changes in emotional and behavioural problems in separate age-groups (multivariate linear regression analyses)
| B | SEB | β | CI (95%) | P | B | SEB | β | CI (95%) | P | B | SEB | β | CI (95%) | P | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Age-group preschoolers: 1–6 years (N = 2726) | |||||||||||||||
| |
Increase in affective problems |
Increase in anxiety problems |
Increase in oppositional-defiant problems |
||||||||||||
| Sociodemo-graphics | |||||||||||||||
| Child age | 0.09 | 0.04 | 0.05 | 0.02; 0.16 | 0.010 | 0.03 | 0.04 | 0.02 | −0.04; 0.10 | 0.359 | 0.14 | 0.04 | 0.08 | 0.07; 0.21 | <0.001 |
| Child female gender | −0.07 | 0.08 | −0.02 | −0.23; 0.09 | 0.380 | −0.11 | 0.08 | −0.02 | −0.26; 0.05 | 0.184 | −0.39 | 0.09 | −0.08 | −0.56; −0.22 | <0.001 |
| Living with both parents | 0.41 | 0.16 | 0.05 | 0.09; 0.74 | 0.012 | 0.43 | 0.17 | 0.05 | 0.10; 0.75 | 0.011 | 0.36 | 0.18 | 0.04 | 0.02; 0.71 | 0.040 |
| Parental education | 0.02 | 0.03 | 0.01 | −0.04; 0.07 | 0.562 | 0.08 | 0.03 | 0.06 | 0.03; 0.14 | 0.002 | 0.00 | 0.03 | 0.00 | −0.05; 0.06 | 0.954 |
| Pre-existing variables | |||||||||||||||
| Child in psychotherapy | 0.25 | 0.43 | 0.01 | −0.59; 1.08 | 0.566 | −0.07 | 0.43 | −0.00 | −0.91; 0.77 | 0.870 | 0.35 | 0.46 | 0.01 | −0.54; 1.25 | 0.443 |
| Chronic physical disease | −0.25 | 0.23 | −0.02 | −0.69; 0.19 | 0.261 | −0.32 | 0.23 | −0.03 | −0.76; 0.13 | 0.163 | 0.08 | 0.24 | 0.01 | −0.40; 0.55 | 0.747 |
| Family life events, LES sum score | −0.06 | 0.04 | −0.03 | −0.13; 0.02 | 0.145 | −0.01 | 0.04 | −0.00 | −0.09; 0.07 | 0.820 | −0.03 | 0.04 | −0.01 | −0.11; 0.05 | 0.511 |
| COVID-19 exposure | 0.11 | 0.07 | 0.03 | −0.03; 0.24 | 0.114 | −0.03 | 0.07 | −0.01 | −0.16; 0.11 | 0.717 | 0.08 | 0.07 | 0.02 | −0.07; 0.22 | 0.296 |
| Appraisal | |||||||||||||||
| Understanding | 0.01 | 0.09 | 0.00 | −.17; 0.19 | 0.937 | 0.07 | 0.09 | 0.02 | −0.12; 0.25 | 0.469 | −0.02 | 0.10 | −0.00 | −0.21; 0.18 | 0.860 |
| Negative consequences | 0.46 | 0.05 | 0.20 | 0.37; 0.55 | <0.001 | 0.41 | 0.05 | 0.17 | 0.32; 0.50 | <0.001 | 0.53 | 0.05 | 0.21 | 0.44; 0.63 | <0.001 |
| Parental mental health | |||||||||||||||
| PHQ-9 sum score | 0.13 | 0.02 | 0.23 | 0.10; 0.16 | <0.001 | 0.10 | 0.02 | 0.18 | 0.07; 0.13 | <0.001 | 0.12 | 0.02 | 0.19 | 0.08; 0.15 | <0.001 |
| GAD-7 sum score | 0.05 | 0.02 | 0.08 | 0.02; 0.08 | 0.003 | 0.10 | 0.02 | 0.16 | 0.07; 0.13 | <0.001 | 0.08 | 0.02 | 0.12 | 0.05; 0.12 | <0.001 |
| F (df) | 49.70 (12) | 49.11 (12) | 55.65 (12) | ||||||||||||
| R2 adj. | 0.18 | 0.18 | 0.19 | ||||||||||||
|
P |
<0.001 |
|
|
|
|
<0.001 |
|
|
|
|
<0.001 |
|
|
|
|
|
Age-group school-children: 7–10 years (N = 1854) | |||||||||||||||
| |
Increase of anxiety/depression |
Increase of withdrawn/depression |
Increase of aggressive problems |
||||||||||||
| Sociodemo-graphics | |||||||||||||||
| Child age | 0.12 | 0.07 | 0.04 | −0.01; 0.24 | 0.078 | 0.11 | 0.04 | 0.06 | 0.03; 0.19 | 0.010 | 0.05 | 0.10 | 0.01 | −0.14; 0.25 | 0.594 |
| Child female gender | −0.14 | 0.14 | −0.02 | −0.42; 0.13 | 0.311 | −0.07 | 0.09 | −0.02 | −0.25; 0.11 | 0.426 | −0.49 | 0.21 | −0.05 | −0.91; −0.07 | 0.022 |
| Living with both parents | 0.51 | 0.23 | 0.05 | 0.06; 0.96 | 0.025 | 0.18 | 0.15 | 0.03 | −0.11; 0.47 | 0.228 | 0.68 | 0.35 | 0.04 | −0.01; 1.36 | 0.054 |
| Parental education | 0.11 | 0.05 | 0.06 | 0.02; 0.20 | 0.014 | 0.08 | 0.03 | 0.06 | 0.02; 0.13 | 0.009 | 0.11 | 0.07 | 0.04 | −0.03; 0.24 | 0.122 |
| Pre-existing variables | |||||||||||||||
| Child in psychotherapy | −0.82 | 0.32 | −0.06 | −1.46; −0.19 | 0.011 | −0.71 | 0.21 | −0.08 | −1.12; −0.29 | 0.001 | −0.74 | 0.50 | −0.03 | −1.72; 0.23 | 0.133 |
| Chronic physical disease | −0.13 | 0.30 | −0.01 | −0.71; 0.46 | 0.668 | −0.10 | 0.19 | −0.01 | −0.48; 0.29 | 0.624 | −0.52 | 0.46 | −0.03 | −1.41; 0.38 | 0.258 |
| Family life events, LES sum score | −0.01 | 0.07 | 0.00 | −0.15; 0.12 | 0.845 | 0.01 | 0.04 | 0.01 | −0.07; 0.10 | 0.776 | 0.05 | 0.10 | 0.01 | −0.15; 0.26 | 0.629 |
| COVID-19 exposure | 0.08 | 0.14 | 0.01 | −0.20; 0.37 | 0.561 | 0.08 | 0.09 | 0.02 | −0.11; 0.26 | 0.424 | −0.03 | 0.22 | −0.00 | −0.47; 0.40 | 0.882 |
| Appraisal | |||||||||||||||
| Understanding | −0.50 | 0.35 | −0.03 | −1.19; 0.20 | 0.161 | 0.08 | 0.23 | 0.01 | −0.37; 0.54 | 0.718 | −0.84 | 0.54 | −0.03 | −1.90; 0.23 | 0.123 |
| Negative consequences | 0.51 | 0.08 | 0.15 | 0.35; 0.67 | <0.001 | 0.25 | 0.05 | 0.11 | 0.14; 0.35 | <0.001 | 0.62 | 0.13 | 0.12 | 0.37; 0.87 | <0.001 |
| Parental mental health | |||||||||||||||
| PHQ-9 sum score | 0.09 | 0.03 | 0.11 | 0.03; 0.15 | 0.002 | 0.07 | 0.02 | 0.14 | 0.04; 0.11 | <0.001 | 0.21 | 0.04 | 0.16 | 0.12; 0.30 | <0.001 |
| GAD-7 sum score | 0.12 | 0.03 | 0.13 | 0.06; 0.19 | <0.001 | 0.05 | 0.02 | 0.08 | 0.01; 0.09 | 0.028 | 0.17 | 0.05 | 0.12 | 0.07; 0.26 | 0.001 |
| F (df) | 18.03 (12) | 12.95 (12) | 19.40 (12) | ||||||||||||
| R2 adj. | 0.10 | 0.07 | 0.11 | ||||||||||||
| P | <0.001 | <0.001 | <0.001 | ||||||||||||
| |
Age-group adolescents: 11–19 years (N = 1243) |
||||||||||||||
| |
Increase of anxiety/depression |
Increase of withdrawn/depression |
Increase of aggressive problems |
||||||||||||
| Sociodemo-graphics | |||||||||||||||
| Child age | 0.04 | 0.05 | 0.03 | −0.05; 0.14 | 0.365 | 0.04 | 0.03 | 0.04 | −0.02; 0.10 | 0.216 | 0.03 | 0.06 | 0.01 | −0.10; 0.16 | 0.635 |
| Child female gender | 0.25 | 0.22 | 0.03 | −0.18; 0.67 | 0.251 | 0.06 | 0.15 | 0.01 | −0.22; 0.35 | 0.657 | 0.19 | 0.30 | 0.02 | −0.39; 0.77 | 0.524 |
| Living with both parents | −0.20 | 0.26 | −0.02 | −0.71; 0.31 | 0.437 | −0.20 | 0.17 | −0.03 | −0.54; 0.14 | 0.257 | −0.53 | 0.36 | −0.04 | −1.23–0.17 | 0.135 |
| Pre-existing variables | |||||||||||||||
| Adolescent in psychotherapy | 1.01 | 0.36 | 0.08 | 0.27; 1.68 | 0.005 | 0.46 | 0.24 | 0.06 | −0.01; 0.94 | 0.054 | −0.38 | 0.49 | −0.02 | −1.34; 0.58 | 0.438 |
| Chronic physical disease | 0.53 | 0.38 | 0.04 | −0.22; 1.28 | 0.166 | −0.15 | 0.26 | −0.02 | −0.65; 0.35 | 0.557 | 0.73 | 0.52 | 0.04 | −0.29; 1.76 | 0.161 |
| Family life events, LES sum score | −0.11 | 0.09 | −0.03 | −0.29; 0.07 | 0.236 | −0.08 | 0.06 | −0.04 | −0.19; 0.04 | 0.207 | −0.18 | 0.12 | −0.04 | −0.42; 0.06 | 0.138 |
| COVID-19 exposure | −0.30 | 0.17 | −0.05 | −0.63; 0.03 | 0.070 | −0.25 | 0.11 | −0.06 | −0.47; −0.03 | 0.027 | −0.60 | 0.23 | −0.08 | −1.05; −0.15 | 0.009 |
| Appraisal | |||||||||||||||
| Understanding | 0.11 | 0.41 | 0.01 | −0.70; 0.93 | 0.783 | 0.32 | 0.28 | 0.03 | −0.22; 0.864 | 0.245 | 0.55 | 0.57 | 0.03 | −0.56; 1.67 | 0.334 |
| Internal control | 0.12 | 0.18 | 0.02 | −0.23; 0.47 | 0.492 | 0.02 | 0.12 | 0.01 | −0.21; 0.26 | 0.840 | 0.13 | 0.24 | 0.02 | −0.34; 0.61 | 0.581 |
| Coping self-efficacy | −0.51 | 0.22 | −0.07 | 0.94; −0.09 | 0.018 | −0.45 | 0.15 | −0.10 | −0.74; −0.17 | 0.002 | −0.38 | 0.30 | −0.04 | −0.96; 0.21 | 0.205 |
| Emotional overwhelmment | 0.86 | 0.17 | 0.16 | 0.52; 1.20 | <0.001 | 0.42 | 0.12 | 0.12 | 0.20; 0.65 | <0.001 | 0.14 | 0.24 | 0.02 | −0.32; 0.61 | 0.546 |
| Negative consequences | 0.58 | 0.10 | 0.17 | 0.38; 0.77 | <0.001 | 0.44 | 0.07 | 0.19 | 0.30; 0.57 | <0.001 | 0.69 | 0.14 | 0.16 | 0.42; 0.97 | <0.001 |
| Parental mental health | |||||||||||||||
| Worry of parents | 0.05 | 0.18 | 0.01 | −0.30; 0.41 | 0.776 | −0.12 | 0.12 | −0.03 | −0.35; 0.12 | 0.336 | −0.41 | 0.25 | −0.05 | −0.89; 0.08 | 0.104 |
| F (df) | 11.98 (13) | 10.66 (13) | 3.69 (13) | ||||||||||||
| R2 adj. | 0.10 | 0.09 | 0.03 | ||||||||||||
| P | <0.001 | <0.001 | <0.001 | ||||||||||||
In terms of pre-existing characteristics, attending psychotherapy before COVID-19 was associated with a decrease in anxiety/depression and withdrawn/depression problems in school-children but had no significant association in preschoolers. In adolescence, the opposite effect was found with regard to anxiety/depression. Exposure to COVID-19 was significantly associated with a decrease in withdrawn/depression and aggressive behaviours in adolescents but not in children. The presence of chronic physical disease and the number of life events in the previous 6 months were not significantly associated with any outcome-domain and in any age-group.
With regard to appraisal, perceived negative consequences were significantly associated with higher problem-levels in all age-groups and outcomes while the degree of understanding had no significant association in any age-group. In adolescents, being confident to be able to efficiently cope with the pandemic was associated with less anxiety/depression and withdrawn/depression while feeling emotionally overwhelmed due to COVID-19 had the opposite effect. In preschoolers and school-children, poor mental health of the parent was associated with an increase in all outcomes while the degree of parental worrying had no significant effect on adolescents.
4. Discussion
This is the first international study that investigates the effects of the COVID-19 pandemic on emotional and behavioural problems in a large sample of children and adolescents aged between 1 and 19 years. Between 15.3% and 43.0% of the participants reported an increase in problems during COVID-19. Effects differed related to age, gender, exposure to and appraisal of COVID-19, having attended psychotherapy before COVID-19 and parental mental health. Between 2.0% and 9.9% of the 1–19 year olds reported emotional and behavioural problems above the clinical cut-off. Preschoolers aged 1–6 years had clinically relevant mental health problems in 4.7% (anxiety), 7.8% (affective problems) and 9.9% (oppositional-defiant problems) of the sample; school-children aged 7–10 years in 4.3% (withdrawn/depression), 9.7% (anxiety/depression) and 9.9% (aggressive problems); adolescents aged 11–19 years in 4.3% (withdrawn/depression), 9.7% (anxiety/depression), and 2.0% (aggressive problems). With the exception of aggressive behaviours in adolescents, these frequencies are around 2 to 5 times higher than the expected prevalence of 2.0% (T > 70) in the general population (Achenbach & Rescorla, 2000; Döpfner et al., 2014). This suggests that in a substantial proportion of children and adolescents the COVID-19 pandemic leads to mental health problems. This conclusion is supported by previous studies (Buzzi et al., 2020; Jiao et al., 2020; Saurabh & Ranjan, 2020; Xie et al., 2020; Zhou et al., 2020) and our finding that between 15.3% and 43.0% of all participants reported an increase in problems during the major COVID-19 lockdown measures. However, the comparability to our study is limited as in German-speaking countries only partial lockdown measures have been applied at the time of baseline-recruitment (e.g. it was always possible to leave home) which is known to have less detrimental effects (Saurabh & Ranjan, 2020; Xie et al., 2020). This may also explain why in contrast to some other studies (Xie et al., 2020; Zhou et al., 2020) we did not find an effect of exposure to COVID-19 in preschoolers and school-children.
Importantly, the reaction to the COVID-19 pandemic in terms of the type of problem and frequency differed significantly between age-groups. Parents of preschoolers reported the largest increase in oppositional-defiant behaviours while adolescents showed the largest increase in emotional problems. School-children had a profile with only moderate increase in both behavioural and emotional problems. The reason for this difference between age-groups may be that the reaction to a stressor, such as the COVID-19 pandemic, is developmentally determined. Several emotional problems require cognitive skills that may not be (fully) acquired in (younger) children. For example, worrying is based on the capacity to anticipate, mentally represent, and reason about future catastrophic events, which typically improves during childhood and gets most influential on functioning at age 13 (Grist & Field, 2012). Accordingly, the frequency of worrying increased from preschoolers to school-children to adolescents in our study. Moreover, several characteristic features of adolescence (e.g. high rates of negative affectivity and reactivity, low self-esteem) are known to confer specific risk at this age for the development of emotional problems as part of anxiety and depression (Rapee et al., 2019). In line with this, emotional problems had the largest increase among adolescents in our study.
Notably, these results need to be interpreted in the light of potential reporter-effects (i.e. we used parent-reports for children and self-reports for adolescents) as there is robust evidence for cross-informant discrepancies between parent- and adolescent self-reported mental health problems (De Los Reyes et al., 2015; Rescorla et al., 2013). Parents are supposed to report less internalizing problems due to their limited insight into their child’s feelings while they may report at least as many externalizing problems as their child because such behaviours are directly observable (Achenbach, McConaughy, & Howell, 1987; De Los Reyes et al., 2015). This may explain why we detected more externalizing problems in children and more internalizing problems in adolescents. However, there is evidence that parent- and self-reports of adolescents tend to rate the same items as low, medium or high, which contradicts substantial disagreement about the problem-type (Hamblin et al., 2016; Rescorla et al., 2013). Given that problem-scores are generally higher in self- than in parent-reports (Rescorla et al., 2013), parents might have under-reported their children’s mental health problems in this study, in particular internalizing problems. Nevertheless, in line with our results very young children tend to react to adverse and traumatic events predominantly with dysregulated, externalizing behaviours rather than with internalizing problems due to their limited cognitive abilities (Kertz & Woodruff-Borden, 2011; Scheeringa, Zeanah, Myers, & Putnam, 2003; Straussner & Calnan, 2014). Accordingly, similar age-effects on the type of mental health problems of children aged 1–19 years during COVID-19 were also found in a study using parental reports only for qualitative thematic analyses (Fitzpatrick, Carson, & Weisz, 2020), thus supporting our results.
Interestingly, adolescents reported on average a significantly larger decrease in both emotional and behavioural problems than preschool- and school-children using parental report. This may be due to the higher prevalence of mental disorders in adolescence compared to childhood (Dalsgaard, Thorsteinsson, & Trabjerg, 2020), which leaves more room for improvement. Given that adolescents are more salient to peer-rejection than any other age-group (Rapee et al., 2019), some may have experienced the physical distancing measures as relieving because of less negative peer-interactions and social comparisons. Alternatively, while younger children strongly rely on their parents’ reaction to the crisis, adolescents may have dealt with the challenges during the pandemic successfully with a positive impact on their self-efficacy and mental health (Fegert et al., 2020).
Several risk and protective factors could be identified. Increasing age was significantly associated with an increase in oppositional-defiant behaviours in preschoolers and with withdrawn/depression in school-children. Being male was associated with a higher risk of oppositional-defiant and aggressive problems in preschool- and school-children. This further supports our finding of age-related reactions to COVID-19 and is in line with evidence that the incidence of oppositional-defiant and conduct disorders is higher in boys and peaks at 8 years of age while depressive symptoms begin to increase during late childhood (Dalsgaard et al., 2020). Reporter-differences should be kept in mind when interpreting these results as there is some evidence that parents tend to report higher problem scores for boys than for girls despite the absence of such gender-differences in self-reports (Van Roy, Groholt, Heyerdahl, & Clench-Aas, 2010).
Living together with both parents was significantly associated with an increase in anxiety and depression in preschoolers and school-children but not in adolescents. This may be due to new or enhanced partnership problems and confinement-related distress, as it has been found after other life-events, with a negative impact on mental health in the whole family system (Prime, Wade, & Browne, 2020; Weijers, Steensel, & Bögels, 2018). This is supported by recent findings that during the COVID-19 pandemic parent-reported mental health problems in children were positively associated with the number of family members in the home (Fitzpatrick et al., 2020).
The relevance of parental behaviour on the child`s mental health is also reflected by our result that negative parental appraisal of the pandemic and poor parental mental health had the most consistent effect in preschoolers and school-children across all outcomes. The lack of an effect of all parental variables in adolescents suggests that younger children may be especially prone to the negative reaction of their parents, possibly due to their limited understanding of the pandemic, which was most pronounced in preschoolers in our study. Alternatively, results might have been affected by reporter-differences because parents’ own distress and symptoms are known to influence their perception of their child’s distress and symptoms (Kassam-Adams, García-España, Miller, & Winston, 2006; Russell et al., 2020). One explanation for this effect may be that parents with high levels of distress or mental health problems recall more negative information about their child`s mental health from their memory than other informants. Additionally, they have a lower threshold by which they gauge whether their child’s behaviour is problematic (De Los Reyes & Kazdin, 2004). This may lead to an increased association of child and parental mental health problems. Nevertheless, most studies could demonstrate that parental reports on child behaviours are still quite accurate and valid despite being influenced by parental psychopathology (Querido, Eyberg, & Boggs, 2001).
Higher parental education was associated with more emotional problems in children. One reason may be that higher parental education was found to be related to more parental distress, possibly because of greater perceived difficulties in combining responsibility for paid work and child-care during COVID-19 (Craig, 2006; Qiu et al., 2020). This may have exerted a negative impact on the child’s mental health (Russell et al., 2020). Alternatively, some studies reported that higher parental education was linked to less open communication about a life event with the affected child and subsequently to more mental health problems (Dalton et al., 2020, 2019). Another explanation may be that during the early stage of the pandemic families with lower parental education, who are more likely economically at risk, might have had other worries in addition to their child’s mental health.
Having received psychotherapy, an indicator of existing mental health problems before COVID-19, was associated with a decrease in emotional problems in school-children but with an increase in adolescents. The result for adolescents is well in line with the literature (Fegert et al., 2020): Individuals with existing mental health problems are known to have limited coping skills and tend to overly use maladaptive emotions-regulation strategies (Compas et al., 2017). Therefore, exposure to stressors (e.g. home-schooling, loss of direct contact to friends, political news) triggers excessive worries and existing mental health problems (Caporino, Exley, & Latzman, 2020; Hartman, Rommelse, van der Klugt, Wanders, & Timmerman, 2019). In contrast to childhood, adolescence is a time-period with increasing relevance of peers relative to the family (Rapee et al., 2019). Therefore, reduction of peer interactions and social support may have led to a loss of protection against social-emotional distress and thereby to an exacerbation of previous mental health problems. Interestingly, the opposite direction of this effect was found in school-children. This suggests that children might have perceived and appraised changes in their everyday life due to COVID-19 measures, such as limited peer contact and home-schooling, as not stressful and/or as manageable. Spending time with the family and mastering challenges together may have led to increased family cohesion, self-efficacy and social support, which are protective factors in the face of stressors and positively related to mental health (Groth et al., 2019; Schultze-Lutter, Schimmelmann, & Schmidt, 2016).
The severity of exposure to COVID-19 was associated with lower levels of withdrawn/depression and aggressive behaviour in adolescents. Such a beneficial effect of increased exposure to COVID-19 was also found in other studies including adolescent samples (Buzzi et al., 2020), probably due to the relief of stressful situations related to school closure, which was the most frequent exposure-experience in our study. Dealing with the virus directly may have reduced uncertainty in terms of fear of the unknown and may have enabled mastery-experiences leading to better mental health (Janssen et al., 2020; Schultze-Lutter et al., 2016).
4.1. Limitations
Limitations of this study include the cross-sectional design, which impedes any causal conclusions. However, we did not only assess current problem-levels but also changes experienced during the COVID-19 pandemic. Further, since our survey was conducted during the period with major lockdown measures, the risk of a recall-bias was minimized.
With regard to recruitment, our sample is a non-probability sample. This increases the risk for a self-selection bias. Our sample may thereby underrepresent the most vulnerable groups (e.g. deprived children or migrants, families with low socio-economic status and education level), which limits the generalizability of findings.
Another limitation is the rather small amount of explained variance in the regression models, in particular in the older age-groups. This may be due to the fact that several covariates were parent-variables, which might be most influential in the younger age-groups. Therefore, additional variables of special relevance for school-children and adolescents should be integrated in future prediction-models. On an individual level, these may include peer relationships, self-concept/self-efficacy, coping and emotion regulation skills, healthy living style, temperament and personality; on an environmental level, social and peer support, neighbourhood cohesion and socio-economic status (Fritz, de Graaff, Caisley, van Harmelen, & Wilkinson, 2018; Schultze-Lutter et al., 2016).
Moreover, the use of caregiver-reports for children and self-reports for adolescents may have exerted an effect on the type and frequency of reported problems (Rescorla et al., 2013). Therefore, the usage of a multi-informant approach (De Los Reyes et al., 2015) and more age-adapted self-reports would be promising to better capture the child`s perspective. However, by now these well-established proxy measures are the only alternative for a mental health assessment at large scales in young children due to their lack of cognitive capacity to understand the response categories, to recall specific examples and to self-reflect on their own behaviours (Cleridou, Patalay, & Martin, 2017; Poulain et al., 2020). Future studies would also benefit from the validation of the self-generated exposure- and appraisal-items as well as the usage of change-scores of the CBCL-scales. Although the self-generated items were developed thoughtfully based on the conceptual definitions of the underlying core constructs, their psychometric quality might be in need of improvement. Therefore, the results of the regression analyses need to be interpreted cautiously and provide only some first insights into psychological factors that might be relevant to deal with the COVID-19 pandemic.
Because of the significant developmental differences within each age-groups (e.g. between 1 and 6 years) and in our total sample, we cannot exclude that the detected differences in emotional and behavioural symptoms are strongly influenced by developmental differences in cognitive, emotional and social skills. Therefore, future studies should apply more fine-grained analyses with smaller subgroups using a longitudinal design to disentangle age and developmental effects.
4.2. Strengths and implications
Despite these limitations, our study has important strengths (e.g. large international sample, broad age-range to investigate developmental peculiarities, negative and beneficial effects) and implications. Given that children and adolescents react differently related to their developmental stage, age-specific problems should be carefully monitored as it remains unclear if they are just a temporal phenomenon or the starting point or deterioration of a mental disorder. Special support should be offered to the identified risk groups, in particular those adolescents who have been in psychotherapy before and with a negative appraisal style.
As adolescents mainly suffer from emotional, that is internalizing problems, their needs may be easily overlooked from the outside. They may especially benefit from interventions to promote coping self-efficacy and emotion regulation skills. In very young children, most emphasis should be put on monitoring and treating dysregulated behaviours (e.g. crying, sleeping problems) and oppositional-defiant problems as early as possible as they are well known to be risk factors for a parent-child spiral of verbal and physical aggression, abuse and stable dysregulated behaviour trajectories across childhood (Barr, Trent, & Cross, 2006; Derella, Burke, Stepp, & Hipwell, 2020; Winsper & Wolke, 2014). To this aim, it seems of utmost importance to decrease parental stress and mental health problems and to enhance positive appraisal and an open communication style about the pandemic. Consequently, public health authorities should provide prevention programmes remotely focusing on parental stress (Ehrensaft, Knous-Westfall, & Alonso, 2016; Richards et al., 2006) and offering information for caregivers how to improve parent-child communication about COVID-19 and its consequences by taking the child’s age and comprehension of illness and causality into account.
5. Conclusions
In summary, a substantial proportion of children and adolescents experience an exacerbated stress response due to COVID-19 measures. The resulting emotional and behavioural problems should be monitored in a developmentally sensitive way, and support should be offered to specific risk groups. Thereby, the sole focus on physical health should be overcome by including mental health in prevention measures to successfully cope with the short- and long-term effects of the pandemic.
Supplementary Material
Acknowledgments
The authors would like to thank all children, adolescents, parents, and caregivers for their participation in the study. Further, the authors would like to thank all institutions and research partners for sharing information about this study.
Funding Statement
This study had no external funding. The authors had full access to all the data in the study and the corresponding author had final responsibility for the decision to submit the publication.
Authors’ contributions
MAL and SJS performed the literature search, designed the study, monitored the data collection, and did the statistical analyses. IL and LB performed the literature search and created the figure and tables for the manuscript. IL, LB, MAL, and SJS contributed to the interpretation of the data. SJS drafted the first version of the manuscript. IL, LB, MAL, and SJS critically reviewed and revised the manuscript for intellectual content and approved the final version.
Disclosure statement
No potential conflict of interest was reported by the authors.
Ethics committee approval
The study was approved by the Institutional Review Boards of the universities of Zurich (#20.4.1) and Bern (#2020-04-00002).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, SJS. The data are not publicly available due to containing information that could compromise the privacy of research participants.
Supplemental Material
Supplemental data for this article can be accessed here.
References
- Achenbach, T. M., McConaughy, S. H., & Howell, C. T. (1987). Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin, 101(2), 213–17. doi: 10.1037/0033-2909.101.2.213 [DOI] [PubMed] [Google Scholar]
- Achenbach, T. M., & Rescorla, I. (2000). Manual for the ASEBA preschool forms and profiles. Child behavior checklist for ages 1 1/2-5. Burlington: University of Vermont, Research Centre for Children, Youth, and Families. [Google Scholar]
- Barr, R. G., Trent, R. B., & Cross, J. (2006). Age-related incidence-curve of hospitalized shaken baby syndrome cases: Convergent evidence for crying as a trigger to shaking. Child Abuse & Neglect, 30(1), 7–16. doi: 10.1016/j.chiabu.2005.06.009 [DOI] [PubMed] [Google Scholar]
- Becker, S. P., & Gregory, A. M. (2020). Editorial perspective: Perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. Journal of Child Psychology and Psychiatry, 61(7), 757–759. doi: 10.1111/jcpp.13278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzzi, C., Tucci, M., Ciprandi, R., Brambilla, I., Caimmi, S., Ciprandi, G., & Marseglia, G. L. (2020). The psycho-social effects of COVID-19 on Italian adolescents’ attitudes and behaviors. Italian Journal of Pediatrics, 46(1), 69. doi: 10.1186/s13052-020-00833-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caporino, N. E., Exley, S., & Latzman, R. D. (2020). Youth anxiety about political news. Child Psychiatry and Human Development, 51(5), 683–698. doi: 10.1007/s10578-020-00972-z [DOI] [PubMed] [Google Scholar]
- Cleridou, K., Patalay, P., & Martin, P. (2017). Does parent-child agreement vary based on presenting problems? Results from a UK clinical sample. Child and Adolescent Psychiatry and Mental Health, 11(1), 22. doi: 10.1186/s13034-017-0159-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluver, L., Lachman, J. M., Sherr, L., Wessels, I., Krug, E., Rakotomalala, S., … McDonald, K. (2020). Parenting in a time of COVID-19. The Lancet, 395(10231), e64. doi: 10.1016/S0140-6736(20)30736-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Compas, B. E., Jaser, S. S., Bettis, A. H., Watson, K. H., Gruhn, M. A., Dunbar, J. P., … Thigpen, J. C. (2017). Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychological Bulletin, 143(9), 939–991. doi: 10.1037/bul0000110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig, L. (2006). Does father care mean fathers share? A comparison of how mothers and fathers in intact families spend time with children. Gender and Society, 20(2), 259–281. doi: 10.1177/0891243205285212 [DOI] [Google Scholar]
- Dalsgaard, S., Thorsteinsson, E., & Trabjerg, B. B. (2020). Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiatry, 77(2), 155–164. doi: 10.1001/jamapsychiatry.2019.3523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton, L., Rapa, E., & Stein, A. (2020). Protecting the psychological health of children through effective communication about COVID-19. Lancet, 4, 346–347. doi: 10.1016/S2352-4642(20)30097-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton, L., Rapa, E., Ziebland, S., Rochat, T., Kelly, B., Hanington, L., … Stein, A. (2019). Communication with children and adolescents about the diagnosis of a life-threatening condition in their parent. The Lancet, 393(10176), 1164–1176. doi: 10.1016/S0140-6736(18)33202-1 [DOI] [PubMed] [Google Scholar]
- De Los Reyes, A., Augenstein, T. M., Wang, M., Thomas, S. A., Drabick, D., Burgers, D. E., & Rabinowitz, J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141(4), 858–900. doi: 10.1037/a0038498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes, A., & Kazdin, A. E. (2004). Measuring informant discrepancies in clinical child research. Psychological Assessment, 16(3), 330–334. doi: 10.1037/1040-3590.16.3.330 [DOI] [PubMed] [Google Scholar]
- De Young, A. C., & Landolt, M. A. (2018). PTSD in children below the age of 6 years. Current Psychiatry Reports, 20(11), 97. doi: 10.1007/s11920-018-0966-z [DOI] [PubMed] [Google Scholar]
- Derella, O. J., Burke, J. D., Stepp, S. D., & Hipwell, A. E. (2020). Reciprocity in undesirable parent-child behavior? Verbal aggression, corporal punishment, and girls’ oppositional defiant symptoms. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 49(3), 420–433. doi: 10.1080/15374416.2019.1603109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Döpfner, M., Plück, J., & Kinnen, C. (2014). für die Arbeitsgruppe Deutsche Child Behavior Checklist. Manual deutsche Schulalter-Formen der Child Behavior Checklist von Thomas M. Achenbach. Elternfragebogen über das Verhalten von Kindern und Jugendlichen, (CBCL/6-18R), Lehrerfragebogen über das Verhalten von Kindern und Jugendlichen (TRF/6-18R), Fragebogen für Jugendliche (YSR/11-18R). Göttingen: Hogrefe. [Google Scholar]
- Dumas, T. M., Ellis, W., & Litt, D. M. (2020). What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. Journal of Adolescent Health, 1–8. In press. doi: 10.1016/j.jadohealth.2020.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrensaft, M. K., Knous-Westfall, H. M., & Alonso, T. L. (2016). Web-based prevention of parenting difficulties in young, urban mothers enrolled in post-secondary education. The Journal of Primary Prevention, 37(6), 527–542. doi: 10.1007/s10935-016-0448-1 [DOI] [PubMed] [Google Scholar]
- Fegert, J. M., & Schulze, M. E. (2020). COVID-19 and ist impact on child and adolescent psychiatry – A German and personal perspective. Irish Journal of Psychological Medicine, 1–3. doi: 10.1017/ipm.2020.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert, J. M., Vitiello, B., Plener, P. L., & Clemens, V. (2020). Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health, 14(1), 20. doi: 10.1186/s13034-020-00329-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick, O., Carson, A., & Weisz, J. R. (2020). Using mixed methods to identify the primary mental health problems and needs of children, adolescents, and their caregivers during the Coronavirus (COVID-19) pandemic. Child Psychiatry and Human Development, (1), 1–12. doi: 10.1007/s10578-020-01089-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz, J., de Graaff, A. M., Caisley, H., van Harmelen, A. L., & Wilkinson, P. O. (2018). A systematic review of amenable resilience factors that moderate and/or mediate the relationship between childhood adversity and mental health in young people. Frontiers in Psychiatry, 9, 230. doi: 10.3389/fpsyt.2018.00230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein, E., Wen, H., & Miller, B. F. (2020). Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics, 174(9), 819. doi: 10.1001/jamapediatrics.2020.1456 [DOI] [PubMed] [Google Scholar]
- Griffith, A. K. (2020). Parental burnout and child maltreatment during the COVID-19 pandemic. Journal of Family Violence. doi: 10.1007/s10896-020-00172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grist, R. M., & Field, A. P. (2012). The mediating effect of cognitive development on children’s worry elaboration. Journal Behavior Therapy and Experimental Psychiatry, 43(2), 801–807. doi: 10.1016/j.jbtep.2011.11.002 [DOI] [PubMed] [Google Scholar]
- Gross, J. J. (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. doi: 10.1037/1089-2680.2.3.271 [DOI] [Google Scholar]
- Groth, N., Schnyder, N., Kaess, M., Markovic, A., Rietschel, L., Moser, S., … Schmidt, S. J. (2019). Coping as a mediator between locus of control, competence beliefs, and mental health: A systematic review and structural equation modelling meta-analysis. Behaviour Research and Therapy, 121, 103442. doi: 10.1016/j.brat.2019.103442 [DOI] [PubMed] [Google Scholar]
- Guessoum, S. B., Lachal, J., Radjack, R., Carretier, E., Minassian, S., Benoit, L., & Moro, M. R. (2020). Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Research, 291, 113264. doi: 10.1016/j.psychres.2020.113264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamblin, R. J., Salloum, A., Andel, R., Nadeau, J. M., McBride, N. M., Lewin, A. B., & Storch, E. A. (2016). Predictors of parent-child agreement on child anxiety diagnoses on the ADIS-IV-C/P. Psychiatry Research, 245, 303–310. doi: 10.1016/j.psychres.2016.07.041 [DOI] [PubMed] [Google Scholar]
- Hartman, C. A., Rommelse, N., van der Klugt, C. L., Wanders, R. B. K., & Timmerman, M. E. (2019). Stress exposure and the course of ADHD from childhood to young adulthood: Comorbid severe emotion dysregulation or mood and anxiety problems. Journal of Clinical Medicine, 8(11), 1824. doi: 10.3390/jcm8111824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. doi: 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen, L., Kullberg, M. J., Verkuil, B., van Zwieten, N., Wever, M., van Houtum, L., … Elzinga, B. M. (2020). Does the COVID-19 pandemic impact parents’ and adolescents’ well-being? An EMA-study on daily affect and parenting. PloS One, 15(10), e0240962. doi: 10.1371/journal.pone.0240962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao, W. Y., Wang, L. N., & Liu, J. (2020). Behavioral and emotional disorders in children during the COVID-19 epidemic. Journal of Pediatrics, 221, 264–266.e1. (in press). doi: 10.1016/j.jpeds.2020.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams, N., García-España, J. F., Miller, V. A., & Winston, F. (2006). Parent-child agreement regarding children’s acute stress: The role of parent acute stress reactions. Journal of the American Academy of Child and Adolescent Psychiatry, 45(12), 1485–1493. doi: 10.1097/01.chi.0000237703.97518.12 [DOI] [PubMed] [Google Scholar]
- Kertz, S. J., & Woodruff-Borden, J. (2011). The developmental psychopathology of worry. Clinical Child and Family Psychology Review, 14(2), 174–197. doi: 10.1007/s10567-011-0086-3 [DOI] [PubMed] [Google Scholar]
- Kroenke, K., & Spitzer, R. L. (2002). The PHQ: A new depression diagnostic and severity measure. Psychiatrics Annals, 32(9), 509–515. doi: 10.3928/0048-5713-20020901 [DOI] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landolt, M. A., & Vollrath, M. (1998). Life event scale (Unpublished manuscript). Zurich, Switzerland: University Children’s Hospital Zurich. [Google Scholar]
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer. [Google Scholar]
- Lee, J. (2020). Mental health effects of school closures during COVID-19. The Lancet Child & Adolescent Health, 4(6), 421. doi: 10.1016/S2352-4642(20)30109-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, L., Ren, H., Cao, R., Hu, Y., Qin, Z., Li, C., & Mei, S. (2020). The effect of COVID-19 on youth mental health. Psychiatric Quarterly, 1–12. doi: 10.1007/s11126-020-09744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Z., Tang, H., Jin, Q., Wang, G., Yang, Z., Chen, H., … Owens, J. (2020). Sleep of preschoolers during the coronavirus disease 2019 (COVID-19) outbreak. Journal of Sleep Research, e13142. doi: 10.1111/jsr.13142 [DOI] [PubMed] [Google Scholar]
- Loades, M. E., Chatburn, E., Higson-Sweeney, N., Reynolds, S., Shafran, R., Brigden, A., … Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. Journal of the American Academy of Child and Adolescent Psychiatry, 59(11), 1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinnon, A., Meiser-Stedman, R., Watson, P., Dixon, C., Kassam-Adams, N., Ehlers, A., … Dalgleish, T. (2016). The latent structure of acute stress disorder symptoms in trauma-exposed children and adolescents. Journal of Child Psychology and Psychiatry, 57(11), 1799–1809. doi: 10.1111/jcpp.12597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meiser-Stedman, R., Yule, W., Smith, P., Glucksman, E., & Dalgleish, T. (2005). Acute stress disorder and posttraumatic stress disorder in children and adolescents involved in assaults or motor vehicle accidents. American Journal of Psychiatry, 162(7), 1381–1383. doi: 10.1176/appi.ajp.162.7.1381 [DOI] [PubMed] [Google Scholar]
- Nakamura, B. J., Ebesutani, C., Bernstein, A., & Chorpita, B. F. (2009). A psychometric analysis of the child behavior checklist DSM-oriented scales. Journal of Psychopathology and Behavioral Assessment, 31(3), 178–189. doi: 10.1007/s10862-008-9119-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosterhoff, B., & Palmer, C. (2020). Attitudes and psychological factors associated with news monitoring, social distancing, disinfecting, and hoarding behaviors among US adolescents during the Coronavirus disease 2019 pandemic. JAMA Pediatrics, 174(12), 1184. doi: 10.1001/jamapediatrics.2020.1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulain, T., Vogel, M., Meigen, C., Spielau, U., Hiemisch, A., & Kiess, W. (2020). Parent-child agreement in different domains of child behavior and health. PloS One, 15(4), e0231462. doi: 10.1371/journal.pone.0231462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime, H., Wade, M., & Browne, D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 1–13. doi: 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), e100213. doi: 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Querido, J. G., Eyberg, S. M., & Boggs, S. R. (2001). Revisiting the accuracy hypothesis in families of young children with conduct problems. Journal of Clinical Child & Adolescent Psychology, 30(2), 253–261. doi: 10.1207/S15374424JCCP3002_12 [DOI] [PubMed] [Google Scholar]
- Rapee, R. M., Oar, E. L., Johnco, C. J., Forbes, M. K., Fardouly, J., Magson, N. R., & Richardson, C. E. (2019). Adolescent development and risk for the onset of social-emotional disorders: A review and conceptual model. Behaviour Research and Therapy, 123, 103501. doi: 10.1016/j.brat.2019.103501 [DOI] [PubMed] [Google Scholar]
- Rescorla, L. A., Ginzburg, S., Achenbach, T. M., Ivanova, M. Y., Almqvist, F., Begovac, I., … Verhulst, F. C. (2013). Cross-informant agreement between parent-reported and adolescent self-reported problems in 25 societies. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division, 53(2), 262–273. doi: 10.1080/15374416.2012.717870 [DOI] [PubMed] [Google Scholar]
- Richards, P. G., Bertocci, G. E., Bonshek, R. E., Giangrande, P. L., Gregson, R. M., Jaspan, T., … Wade, A. (2006). Shaken baby syndrome. Archives of Disease in Childhood, 91(3), 205–206. doi: 10.1136/adc.2005.090761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roger, J. P., Chesney, E., Oliver, D., Pollak, T. A., McGuire, P., Fusar-Poli, P., … David, A. S. (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry, 7(1), 1–17. doi: 10.1016/S2215-0366(20)30203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotter, J. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs, 80(1), 1–28. doi: 10.1037/h0092976 [DOI] [PubMed] [Google Scholar]
- Russell, B. S., Hutchison, M., Tambling, R., Tomkunas, A. J., & Horton, A. L. (2020). Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent-child relationship. Child Psychiatry and Human Development, 51(5), 671–682. doi: 10.1007/s10578-020-01037-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler, I. N., Kim-Bae, L. S., & MacKinnon, D. (2000). Coping and negative appraisal as mediators between control beliefs and psychological symptoms in children of divorce. Journal of Clinical Child Psychology, 29(3), 336–347. doi: 10.1207/S15374424JCCP2903_5 [DOI] [PubMed] [Google Scholar]
- Saurabh, K., & Ranjan, S. (2020). Compliance and psychological impact of quarantine in children and adolescents due to Covid-19 pandemic. Indian Journal of Pediatrics, 87(7), 532–536. doi: 10.1007/s12098-020-03347-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa, M. S., Zeanah, C. H., Myers, L., & Putnam, F. W. (2003). New findings on alternative criteria for PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry, 42(5), 561–570. doi: 10.1097/01.CHI.0000046822.95464.14 [DOI] [PubMed] [Google Scholar]
- Schultze-Lutter, F., Schimmelmann, B. G., & Schmidt, S. J. (2016). Resilience, risk, mental health and well-being: Associations and conceptual differences. European Child & Adolescent Psychiatry, 25(5), 459–466. doi: 10.1007/s00787-016-0851-4 [DOI] [PubMed] [Google Scholar]
- Sharma, V., Miguel, R. O., & Sharma, N. (2020). Risk and protective factors for adolescent and young adults mental health within the context of COVID-19 a perspective from Nepal. Journal of Adolescent Health, 67(135–137). doi: 10.1016/j.jadohealth.2020.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder. The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Straussner, S. A. L., & Calnan, A. J. (2014). Trauma through the life cycle: A review of current literature. Clinical Social Work Journal, 42(4), 323–335. doi: 10.1007/s10615-014-0496-z [DOI] [Google Scholar]
- Van Roy, B., Groholt, B., Heyerdahl, S., & Clench-Aas, J. (2010). Understanding discrepancies in parent-child reporting of emotional and behavioural problems: Effects of relational and socio-demographic factors. BMC Psychiatry, 10(1), 56. doi: 10.1186/1471-244X-10-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729–1754. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, G., Zhang, Y., Zhao, J., Zhang, J., & Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID-19 outbreak. The Lancet, 395(10228), 945–947. doi: 10.1016/S0140-6736(20)30547-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weijers, D., Steensel, F. J. A., & Bögels, S. M. (2018). Associations between psychopathology in mothers, fathers and their children: A structural modeling approach. Journal of Child and Family Studies, 27(6), 1992–2003. doi: 10.1007/s10826-018-1024-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winsper, C., & Wolke, D. (2014). Infant and toddler crying, sleeping and feeding problems and trajectories of dysregulated behavior across childhood. Journal of Abnormal Child Psychology, 42(5), 831–843. doi: 10.1007/s10802-013-9813-1 [DOI] [PubMed] [Google Scholar]
- Xie, X., Xue, Q., Zhou, Y., Zhu, K., Liu, Q., Zhang, J., & Song, R. (2020). Mental health status among children in home confinement during the Coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatrics, 174(9), 898. doi: 10.1001/jamapediatrics.2020.1619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, S.-J., Zhang, L.-G., Wang, -L.-L., Guo, Z.-C., Wang, J.-Q., Chen, J.-C., … Chen, J.-X. (2020). Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry, 29(6), 749–758. doi: 10.1007/s00787-020-01541-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, SJS. The data are not publicly available due to containing information that could compromise the privacy of research participants.


