Abstract
Introduction. We systematically analyzed the most commonly used narrative note formats and content found in primary and specialty care visit notes to inform future research and electronic health record (EHR) development. Methods. We extracted data from the history of present illness (HPI) and impression and plan (IP) sections of 80 primary and specialty care visit notes. Two authors iteratively classified the format of the sections and compared the size of each section and the overall note size between primary and specialty care notes. We then annotated the content of these sections to develop a taxonomy of types of data communicated in the narrative note sections. Results. Both HPI and IP were significantly longer in primary care when compared to specialty care notes (HPI: n = 187 words, SD[130] vs. n = 119 words, SD [53]; p = 0.004 / IP: n = 270 words, SD [145] vs. n = 170 words, SD [101]; p < 0.001). Although we did not find a significant difference in the overall note size between the two groups, the proportion of HPI and IP content in relation to the total note size was significantly higher in primary care notes (40%, SD [13] vs. 28%, SD [11]; p < 0.001). We identified five combinations of format of HPI + IP sections respectively: (A) story + list with categories; (B) story + story; (C) list without categories + list with categories; (D) list with categories + list with categories; and (E) list with categories + story. HPI and IP content was significantly smaller in combination C compared to combination A (-172 words, [95% Conf. -326, -17.89]; p = 0.02). We identified seven taxa representing 45 different types of data: finding/condition documented (n = 14), intervention documented (n = 9), general descriptions and definitions (n = 7), temporal information (n = 6), reasons and justifications (n = 4), participants and settings (n = 4), and clinical documentation (n = 1).
Conclusion. We identified commonly used narrative note section formats and developed a taxonomy of narrative note content to help researchers to tailor their efforts and design more efficient clinical documentation systems.
Introduction
Primarily driven by financial incentives provided by the Meaning Use program, the U.S. health system has reached unprecedented electronic health record (EHR) adoption1, which was achieved through large-scale adoption of commercial EHRs2. These systems were adopted before facing a thorough redesign3 and before accumulation of compelling evidence of their full impact4. As a result, new unintended consequences have emerged at different levels of the U.S. health system5. Some notorious limitations of current systems include confusing interfaces6, excessive, overzealous alerts and reminders7, and bloated clinical notes8. The latter is particularly challenging because the clinical documentation that is essential in facilitating memory and recall and to enable understanding and care coordination9, has become an increasing source of frustration among clinicians10. Clinical notes play an important role in the so called EHR-associated documentation burden as they contribute to information overload11. In addition, notes created in the U.S. digital health system are significantly longer than similar documentation in other developed countries12, are not created to increase clinicians’ situational awareness13, often contain redundant information14, and in some cases may never be read despite containing information relevant to patient care15. To compensate for the need to enter narrative data manually, clinicians frequently create their notes by using the patient’s previous note, a remediable practice known as “copy-and-paste”16, which facilitates immediate data entry but further aggravates the documentation burden, and compromises note quality and patient safety17.
To address EHR limitations and their impact on clinical documentation, informatics leaders and researchers have proposed multiple solutions such as improving EHR design, interoperability, smarter clinical decision support (CDS) systems, transferring some data entry to patients18, and more recently, adoption of speech recognition and other computational methods3. We believe that these solutions, if implemented in isolation, may not be sufficient because they will be applied without a formal representation of relevant data about patients’ care context. We define patients’ care context as contextual information about the patient’s health and care (e.g., patient reports that his symptoms are getting worse), the underlying reasons behind a clinician’s decisions (e.g., a new imaging test is needed because the patient’s symptoms are worse), or a clinician’s interpretations (e.g., I believe the patient is not eligible for advanced therapy). By not being able to access relevant information considered by clinicians in their care decisions, irrelevant alerts continue to be fired7, data-entry consumes precious time that would otherwise be dedicated to direct patient care19, and EHR navigation forces clinicians to access isolated EHR components, which includes the tedious tasks of finding and reading long notes to search for data that are not always documented or cannot be found20.
We hypothesize that improving the EHR and particularly clinical documentation systems, will demand efforts in two important research areas: (1) creation of a formalism to represent patients care context data in computable form (modeled, structured, and coded); (2) a better understanding of the narrative content communicated in clinical notes. In previous studies we have developed a formalism to represent patients’ care context as a collection of subject-predicate-object or concept-relationship-concept tuples (e.g., patient-has_intervention-amoxicillin or amoxicillin-has_reason-allergic to ciprofloxacin). These tuples were formulated through a series of studies reporting clinical and contextual concepts and semantic relationships elicited from the literature21-22 and in annotations of clinical notes and patient-physician spoken communications during clinical visits23. In the latter, we have suggested several applications of the tuples to improve EHR navigation, CDS, learning health systems and data entry at the point of care.
Although several studies have assessed clinicians’ perceptions of clinical documentation systems from multiples perspectives such as the purposes of clinical notes, documentation of clinicians’ reasoning in their notes, preferred methods for note creation and preferred methods for note reading/retrieval24, current literature does not provide a systematic assessment of the content communicated in narrative note sections. Therefore, to augment our findings from previous studies21-23 and inform future research and EHR development, in the present study we explore the types of narrative data communicated in clinical notes and the most common formats used to create narrative note sections.
Methods
Settings and Study Design. We conducted a descriptive study to identify the most commonly used note section formats and types of data communicated in narrative note sections. We extracted data from the note sections history of present illness (HPI) and impression and plan (IP) from a random sample of 80 primary and specialty care visit notes written between 03/01/2019 and 06/30/2019 at the University of Alabama-Birmingham (UAB) primary and specialty care clinics. Forty primary care notes were selected from the specialty internal medicine and 40 specialty care notes were selected from the specialties ear, nose, and throat (ENT) (20 notes) and urology (20 notes). We choose the note sections HPI and IP because they are more likely to contain the expressivity of patients’ care context, which is not typically found in more structured note sections such as “medication list” or “laboratory results.” We chose the specialties internal medicine, ENT and urology because they provide a wide range of concepts ranging from common infections and chronic diseases to complex surgeries, thereby increasing their generalizability. The UAB Institutional Review Board approved the study.
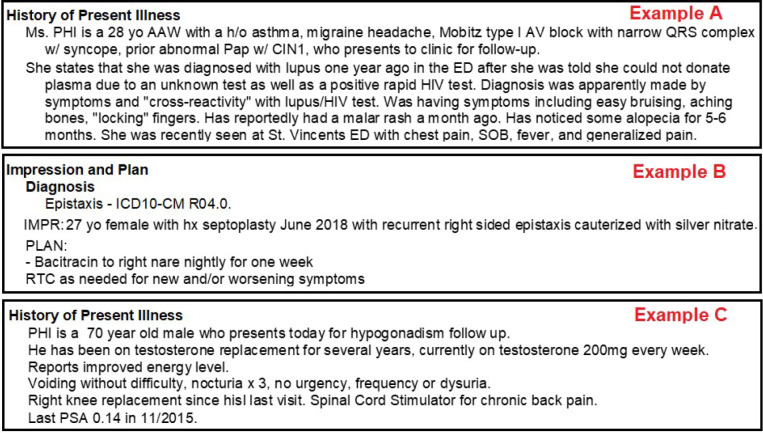
Identification of note section format and size. One of the authors (TKC) extracted the content from HPI and IP sections of the selected notes and replaced any identifiable information with the acronym PHI (protected health information). Two authors (TKC and PID) iteratively classified the content of the sections of each note as story (i.e., two or more coherent sentences that form a paragraph - Figure 1 -A), list with categories (i.e., list of sentences that do not form a coherent paragraph, but are organized by category - Figure 1-B) and list without categories (i.e., list of sentences that neither form a coherent paragraph nor are organized by category - Figure 1-C). When two formats were found in the same note section (e.g., story and list with categories), we classified the section using the predominant format (i.e., the larger one by number of words). We calculated the total number of words for each note (the entire note), and the total number of words in each narrative note section (HPI and IP). Next, we identified the most common combinations of note formats used. We then performed the following comparisons: (1) the size of each note section (HPI and IP) between primary and specialty care notes; (2) the combined size of HPI and IP between primary and specialty care notes; (3) the total note size between primary and specialty care notes; (4) the proportion of content in HPI and IP in relation to the total note size between primary care and specialty care notes; and (5) the size of the different combinations of format for HPI and IP across the whole sample.
Classification of note content. We were unable to find a publicly available classification of narrative note content, and therefore, we developed a coding scheme with types of data that are likely to be communicated in narrative note sections (e.g., history of a finding or intervention) based on concepts represented in our collection of note content tuples previously reported23. This initial scheme was used by two authors (TKC and PID) who independently annotated the de-identified content of HPI and IP sections of a random sample of five notes, and then met in person to modify the initial coding scheme by adding, eliminating, or merging codes via consensus. These authors then used the updated coding scheme to annotate a random sample of 15 notes (five from each specialty - internal medicine, ENT, and Urology). We calculated inter-rater agreement and upon satisfactory agreement (> 80% agreement and K >.80) we split the remaining sample between the two authors. If no satisfactory agreement was achieved, another sample of 15 notes was annotated. This process was repeated until a satisfactory agreement was achieved or the whole sample was annotated. The coding scheme was modified as needed via consensus after each round. Annotations were performed at the sentence level with concepts (e.g., findings, procedures, orders) annotated individually, except when similar concepts were mentioned as a sequence in a sentence. For example, in the sentence “Patient has history of orbital cellulitis and bilateral nasal congestion,” the entire sentence was annotated as “history of finding/condition reported.” After annotating the 80 notes in our sample, the coding authors met in person to iteratively formulate categories of types of data communicated in clinical notes by merging similar codes from our final annotation scheme. These categories formed the taxa of a taxonomy of narrative note content. Note: at this preliminary stage, we avoided the use of generic types of data or taxa (e.g., other) and attempted to classify each annotated sentence in at least one type of data/taxon to avoid ambiguity.
Data analysis. We compared the size of each note section, of the combined note sections, of the total note, and of the proportion of narrative note sections between primary and specialty care notes using an independent t-test. To compare the size of the different combinations of note format we used the one-way analysis of variance (ANOVA), with statistical significance defined as p value < 0.05. If a significant difference between the combinations of formats was observed, we used the post hoc Tukey test for pairwise comparison of means with equal variance to identify which of the combinations differed. Inter-rater agreement for the annotations of narrative note content was calculated using Cohen’s Kappa. The statistical analysis was performed using Stata version 16 statistical software [StataCorp LP, College Station, TX]. The annotation of narrative note content was performed using NVivo version 12.
Results
Overall, HPI sections in primary care notes were significantly longer than HPI sections in specialty care notes (mean = 187 words, SD[130] vs. mean = 119 words, SD [53]; p = 0.004). IP sections in primary care notes were also significantly longer than IP sections in specialty care notes (mean = 270 words, SD [145] vs. mean = 170 words, SD [101]; p < 0.001). When combined, the size of HPI and IP sections was also significantly longer in primary care when compared to specialty care notes (mean = 457 words, SD [203] vs. mean = 290 words, SD [187]; p < 0.001). Although the total size of the notes was not significantly different between primary and specialty care notes (mean = 1128 words, SD [49] vs. mean = 1081 words, SD [57]; p = 0.53), the proportion of HPI and IP content in relation to the total note size was significantly higher in primary care notes when compared to specialty care notes (40%, SD [13] vs. 28%, SD [11]; p < 0.001). Table 1 summarizes the comparisons of size between primary and specialty care notes.
The most common formats of HPI in primary care notes were story (notes = 36; mean size = 198 words, SD [131]), followed by list with categories (notes = 3; mean size = 99 words, SD [56]) and list without categories (notes = 1; mean size = 22 words, SD [0]). The most common formats of IP in primary care notes were list with categories (notes = 32; mean size = 288 words, SD [155]), followed by story (notes = 8; mean size = 197 words, SD [59]). The most common formats of HPI in specialty care notes were story (notes = 21; mean size = 130 words, SD [52]), followed by list without categories (notes = 14; mean size = 113 words, SD [55]) and list with categories (notes = 5; mean size = 92 words, SD [47]). The most common formats of IP in specialty care notes were list with categories (notes = 23; mean size = 123 words, SD [54]), followed by story (notes = 17; mean size = 233 words, SD [116]). None of the notes had the IP section classified as list without categories. Table 2 summarizes the average size of each note section per note format and specialty.
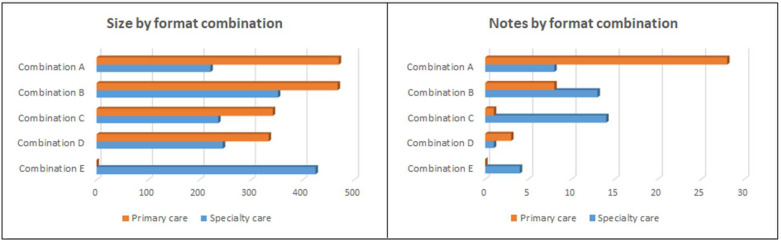
We identified five combinations of format of HPI and IP sections respectively: (A) story + list with categories (notes = 36; mean size = 415 words, SD [222]); (B) story + story (notes = 21; mean size = 396 words, SD [156]); (C) list without categories + list with categories (notes = 15; mean size = 243 words, SD [81]); (D) list with categories + list with categories (notes = 4; mean size = 312 words, SD [110]); and (E) list with categories + story (notes = 4; mean size = 425 words, SD [115]). There was a statistically significant difference between the combinations of formats as determined by one-way ANOVA (F(4,75) = 2.75, p = 0.03). A Tukey post-hoc test revealed that HPI and IP content was significantly smaller in combination C compared to combination A (-172 words, [95% Conf. -326, -17.89]; p = 0.02). Table 3 summarizes the size of each combination of narrative note format and Figure 2 illustrates the size and the number of notes by combination of formats.
After the definition of an initial coding scheme and an initial round with independent annotation of 15 notes, inter-rater agreement was 83%, K .83, we therefore split the remaining sample between the two coding authors.
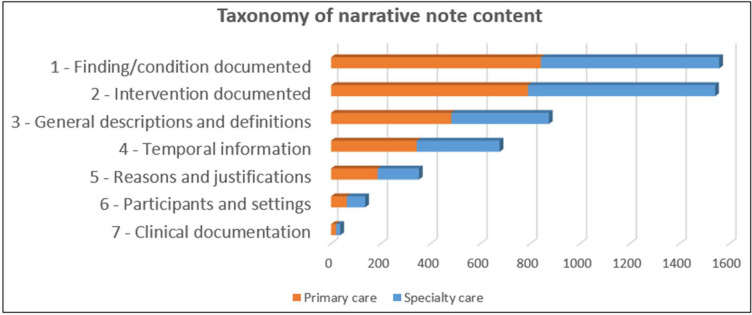
We identified 45 types of data communicated in narrative note sections. The most common types of data in HPI in primary care notes were “history of intervention reported” (n = 106) and “history of finding/condition” reported (n = 106), followed by “description or value of a finding/condition” (n = 87). The most common types of data in IP in primary care notes were “intervention planned or recommended” (n = 299), followed by “date of an intervention” (n = 220), and “finding/condition present/presumed” (n = 114). The most common types of data in HPI in specialty care notes were “history of intervention reported” (n = 98), followed by “history of finding/condition reported” (n = 73), and “date of an intervention” (n = 65). The most common types of data in IP in specialty care notes were “intervention planned or recommended” (n = 110), followed by “intervention performed during the visit” (n = 64), and “reason for ordering or performing an intervention” (n = 43). We classified the types of data into seven taxa: 1 - finding/condition documented (n = 14), 2 - intervention documented (n = 9), 3 - general descriptions and definitions (n = 7), 4 - temporal information (n = 6), 5 - reasons and justifications (n = 4), 6 - participants and settings (n = 4), and 7 - clinical documentation (n = 1). Figure 3 illustrates the taxonomy of narrative note content and Table 4 lists the 45 types of data communicated in narrative note sections.
Discussion
We systematically assessed and classified the most commonly used narrative note section formats and narrative content reported in primary and specialty care notes. Although assessments of clinicians’ preferences about note formats and about the expressivity of clinicians’ reasoning found in narrative note sections have been previously reported24, to our knowledge, no systematic assessment of the most common formats used in narrative note sections is available in the literature. The quantitative assessment of note content redundancy and the deleterious effects of “copy-and-paste” have been also reported14, but an assessment of the most common types of data communicated in narrative note sections has not. Our findings will empower the broader medical and informatics communities by facilitating the identification of note content that is more commonly found in narrative note sections, and the most commonly used narrative note section formats to help informatics researchers to tailor their efforts and design clinical documentation systems that can accommodate common structures for documenting patients’ care context data.
Primary care notes were found to have significantly longer narrative note sections when compared to specialty care notes. This is likely explained by the fact that primary care physicians tend to have a holistic view of the patient and usually treat or at least follow up on most patient’s present or presumed conditions, whereas specialty care clinicians tend to focus on specific findings and conditions that require immediate or long-term specialized care25. Although the overall note size was not significantly different between the two groups, primary care notes had significantly higher proportion of content in HPI and IP sections than specialty care notes. This is also consistent with a larger number of findings and conditions treated by primary care physicians. Our annotations demonstrate that the note section HPI was more frequently documented as a story in both groups, and the most common types of data in this section include “history of intervention reported” and “history of finding/condition reported,” but these are more frequent in primary care notes (106 instances vs. 98 instances and 106 instances vs. 73 instances, respectively), indicating a greater variety of concepts documented in primary care documents. A similar pattern was observed in the IP section with the most common format being list with categories in both groups, and the most commonly reported type of data in both groups being “intervention planned or recommended,” but with nearly triple the frequency of interventions found in primary care notes (299 instances) when compared specialty care notes (110 instances).
Not surprisingly, our annotations revealed that narrative note sections frequently contain contextual information about the patient’s health and care and clinicians’ decisions. The top five types of data in HPI in both groups represent 40% of the overall HPI annotations, and include documentation of past or present findings, conditions, and interventions, as well as the description or value of findings or conditions (e.g., hemoglobin/hematocrit: 8/26). The top five types of data in IP represent 45% of the overall IP annotations and include interventions planned or recommended by the clinician as well as contextual data about intervention such as their date (e.g., return to clinic in three months) and the reasons or justifications for ordering them (e.g., return to clinic if symptoms reoccur). However, another important element of patients’ care context data, the clinician’s interpretations, which we annotated as “clinical interpretation of findings/conditions or interventions,” was not found as frequently as the other components of patients’ care context.
Overall, clinicians’ interpretations were only the 16th most common type of data found in our annotations. In HPI, it was found in only six instances in primary care notes and only once in specialty care notes, and most instances referred to interpretations likely expected to be found in the IP section (e.g., patient demonstrates good inhaler technique). In IP, it was slightly more frequent but ranked moderately low compared to other types of data (9th in primary care notes and 10th in specialty care notes). We found 57 instances of clinician’s interpretations in the IP section in primary care notes and 22 instances in specialty care notes.
We believe that several factors contribute to the relatively low frequency of documentation of clinicians’ reasoning. First, the steady implementation of pay-for-performance payment models increased the demand for capturing accurate, structured data26, which could force clinicians to more frequently document (or import) billing-associated data into their notes. This is reinforced by the fact that the need to document non-clinically relevant data in clinical notes is an increasing source of frustration among clinicians11. In our annotations, coded diagnoses were more frequent than clinical interpretations in IP in specialty care notes (24 instances vs. 22 instances). Second, the coupling of EHR limitations and strict coding/billing requirements are also considered a contributing factor for the longer notes found in the U.S.12, and could as well contribute to the documentation of non-clinically relevant information at the expense of patients’ care context data. Third, previous studies suggest that clinicians tend to make conscious decisions about what to document in their clinical notes27, and documentation or the lack thereof of interpretations could be one of these conscious decisions. Finally, previous studies suggest that current EHRs provide virtually no automation for documentation of clinicians’ reasoning in their clinical notes24, which provides opportunities for developing clinical documentation systems that can help clinicians’ more frequently document and access their own interpretations, as well as other clinicians’ interpretations about patients’ health and care.
Implications for future research and EHR development. The importance of communicating what clinicians are thinking about the patients and their problems has already been reported by Weed in 196828, however, a half-century later we still lack key information about patients’ care context in their health records, which coupled with bloated digital notes, introduces data obfuscation and facilitates medical errors5. Further research is needed to explore clinicians’ perceptions about preferred narrative note section formats and relevant narrative content, since frequency of use does not necessarily assure usefulness of content. Our work can guide research focused on the development of clinical documentation systems that facilitate creation and retrieval of concise notes, especially for the creation and synthesis of narrative content relevant to patient care. This may require a combination of a formal representation of narrative note content23 to augment prominent computational methods such as conversational speech recognition and natural language processing3. These methods could be used to automatically capture clinical and contextual data often verbalized during clinical visits23,27 and, when combined with other modern language understanding methods29 improve data entry at the point of care, by facilitating automatic creation of narrative note content that adheres to the preferred narrative formats and relevant content.
Limitations. Although our taxonomy was created with a robust sample of notes and annotations, its taxa include data from only one institution; notes from other institutions may reveal other types of data. We included only three clinical specialties; notes from other specialties may contain additional formats and data types. However, our methods are reproducible and can be relatively easily applied to other institutions and specialties. We did not assess other note sections such as “review of systems” or “health maintenance,” which in some cases may contain context data not captured by our annotations. However, we believe that these instances are rare and, in most cases, include information already documented in HPI and IP, therefore, our annotations may have covered most patients’ care context data documented by clinicians. Known influences to note creation such as copy-and-paste or the use of templates were out of the scope, but we believe they may influence creation of narrative content and warrant future studies.
Conclusions
We assessed and classified the most commonly used narrative note section formats and narrative content reported in primary and specialty care notes. Narrative note sections tend to be significantly longer in primary care than in specialty care notes, despite a similar overall note size between these groups. We identified commonly used narrative note section formats and developed a taxonomy of narrative note content to help researchers to tailor their efforts and design more efficient clinical documentation systems.
Acknowledgements
This work was supported by funds from the Informatics Institute of the University of Alabama at Birmingham.
Figures & Table
Figure 1. Examples of the note formats story (A), list with categories (B), and list without categories (C).
Figure 2. HPI+IP size by format combination (left) and number of notes by format combination (right).
Figure 3. Taxonomy of narrative note content with total annotations by taxa and specialty.
Table 1. Comparisons of size (in words) between primary and specialty care notes.
| Category | Primary care, n (SD) | Specialty care, n (SD) | p value |
| HPI | 187 (130) | 119 (53) | 0.004 |
| IP | 270 (145) | 170 (101) | < 0.001 |
| HPI+IP | 457 (203) | 290 (187) | < 0.001 |
| Total | 1128 (49) | 1081 (57) | 0.53 |
| Proportion ((HPI+IP)/Total) | 40% (13%) | 28% (11%) | < 0.001 |
Abbreviations: HPI: history of present illness; IP: impression and plan; SD: standard deviation.
Table 2. Average size (in words) of each note section per note format and specialty.
| Format | HPI, mean (SD) | Notes | IP, mean (SD) | Notes |
| Primary care | ||||
| List with categories | 99 (56) | 3 | 288 (155) | 32 |
| List without categories | 22 (0) | 1 | - | - |
| Story | 198 (131) | 36 | 197 (59) | 8 |
| Specialty care | ||||
| List with categories | 92 (47) | 5 | 123 (54) | 23 |
| List without categories | 113 (55) | 14 | - | - |
| Story | 130 (52) | 21 | 233 (116) | 17 |
| Combined | ||||
| List with categories | 94 (47) | 8 | 219 (147) | 55 |
| List without categories | 107 (55) | 15 | - | - |
| Story | 173 (113) | 57 | 221 (101) | 25 |
Abbreviations: HPI: history of present illness; IP: impression and plan; SD: standard deviation.
Table 3. Average size (in words) of each combination of narrative note format.
| Primary care | Specialty care | Combined | ||||
| Combination (HPI + IP) | Mean (SD) | Notes | Mean (SD) | Notes | Mean (SD) | Notes |
| A - Story + list with categories | 470 (216) | 28 | 221 (105) | 8 | 415 (222) | 36 |
| B - Story + story | 468 (191) | 8 | 352 (118) | 13 | 396 (156) | 21 |
| C - List without categories + list with categories | 342 (0) | 1 | 236 (80) | 14 | 243 (81) | 15 |
| D - List with categories + list with categories | 334 (123) | 3 | 245 (0) | 1 | 312 (110) | 4 |
| E - List with categories + story | - | 0 | 425 (155) | 4 | 425 (115) | 4 |
Abbreviations: HPI: history of present illness; IP: impression and plan; SD: standard deviation.
Table 4. List of types of data identified in the annotations of HPI and IP note sections.
| Primary care | Specialty care | ||||||
| Taxa | Type of data | Description | Example | HPI | IP | HPI | IP |
| 2 | Intervention planned or recommended | Documentation of the intention to start an intervention, or intervention recommended | We will get him set up to see the interventional radiologists to discuss sclerotherapy | 7 | 299 | 9 | 110 |
| 2 | History of intervention reported | History of an intervention documented in the note | Dilated eye exam in 2019 | 106 | 88 | 98 | 36 |
| 1 | Finding/condition present/presumed | A finding/condition that is currently affecting the patient | Diagnosis: Acute upper respiratory infection | 54 | 220 | 22 | 11 |
| 3 | Description or value of a finding/condition | Description or quantitative value of a finding/condition | Dizziness feels like spinning or lightheaded sensation | 87 | 106 | 55 | 14 |
| 4 | Date of an intervention | One-time event, specific time or onset of an intervention informed | On February 7 he underwent a scrotal ultrasound | 42 | 114 | 65 | 38 |
| 1 | History of finding/condition reported | History of a finding/condition documented in the note | Past medical history of thyroid cancer | 106 | 54 | 73 | 23 |
| 5 | Reason for ordering or performing an intervention | Reason for an intervention including diagnostic process | If not improved, would obtain sleep study | 43 | 99 | 25 | 48 |
| 1 | Finding/condition absent or denied | Statement indicating that a finding/condition is not reported, is denied or is absent | No evidence of inflammatory arthritis | 69 | 21 | 53 | 8 |
| 2 | Intervention performed during the visit | Any intervention performed/discussed during the visit | Right cerumen impaction removed | 6 | 60 | 5 | 64 |
| 3 | Patient demographic information | Patient demographic information described in the note | Patient is a 41-year-old Hispanic female | 41 | 26 | 31 | 21 |
| 4 | Frequency of an intervention | Statement indicating the frequency of an intervention | Continue daily allopurinol | 28 | 50 | 9 | 10 |
| 1 | Anatomical site of a finding condition | Indication of the anatomical site of a finding or condition | Reports great improvement in left foot redness and swelling | 39 | 9 | 33 | 14 |
| 1 | Finding condition suggested by intervention or clinician | A specific finding/condition suggested by an intervention or by a clinician | Comprehensive review of systems is completely negative | 19 | 60 | 4 | 10 |
| 2 | Intervention present/presumed | Statement indicating that patient has an active intervention | Chronic lower back pain is currently managed by pain clinic | 37 | 34 | 17 | 2 |
| 2 | Intervention absent or denied | Statement indicating that an intervention is not reported, is denied or is absent | They are not using any form of birth control | 23 | 33 | 29 | 2 |
| 3 | Clinical interpretation about a finding/condition or intervention | Explicit interpretation of a finding/condition or intervention documented | No history of depression and I think her symptoms are consistent with normal grief | 6 | 57 | 1 | 22 |
| 3 | Description of patient education | Statement about patient education/counselling or comprehension | Education topics: Nutrition and exercise education | 1 | 38 | 1 | 43 |
| 2 | Effectiveness or the lack thereof of an intervention | Inference about the effectiveness or the lack thereof of an intervention | Symptoms improved with steroid | 22 | 19 | 20 | 13 |
| 1 | Progress of a finding/condition | The progress of a finding/condition | She states this has continued unchanged over the last 2 months | 30 | 12 | 20 | 6 |
| 2 | Intervention as the reason for a visit | An intervention documented as the reason for the visit | Presents today for packing and splint removal | 30 | 19 | 15 | 4 |
| 3 | Social habits, lifestyle or environment | Description of social habits, lifestyle or environmental factors that affect patients health | Patient states she is eating smaller, healthier meals | 35 | 21 | 8 | 3 |
| 4 | Date of a finding/condition | One-time event, specific time or onset of a finding/condition informed | His blood pressure is elevated today | 24 | 21 | 20 | 2 |
| 3 | Description or value of an intervention | Description or quantitative value of an intervention | Patient was able to control the bleeding at home by using rinses to expel initial clot | 19 | 12 | 7 | 28 |
| 1 | Finding/condition as reason for the visit | A finding/condition documented as the reason for the visit | Presents today for evaluation of head congestion | 13 | 11 | 28 | 13 |
| 6 | Executor of an intervention | Indication of the executor of an intervention | Hypothyroidism: managed by Dr. PHI | 6 | 15 | 28 | 7 |
| 4 | Duration of a finding/condition | Statement about the length of time of a finding/condition | Shortness of breath over the past 2 weeks | 23 | 5 | 18 | 4 |
| 6 | Setting/location of an intervention | Setting/location where an intervention was performed (including diagnostic process) | She was recently seen at St. Vincents | 16 | 22 | 9 | 3 |
| 3 | Description of a goal or preference | Description of a specific goal or preference by the patient or the clinician | Patient is interested in pharmacotherapy for her anxiety | 12 | 22 | 7 | 8 |
| 1 | Finding/condition identified during the visit | Finding/condition identified by the clinician during the visit | Blood pressure mildly elevated today | 4 | 20 | 1 | 22 |
| 4 | Frequency of a finding/condition | Statement indicating the frequency of a finding/condition | She has frequent falls, >10 in the past year | 17 | 3 | 19 | 3 |
| 5 | Reason for not ordering or performing an intervention | Reason or justification for not performing a procedure or intervention | Based on his anatomy surgery would significantly improve his airway | 5 | 17 | 8 | 9 |
| 1 | Patients overall state reported | Statement about the overall state of the patient | She notes that she is overall doing well | 23 | 2 | 8 | 4 |
| 1 | Cause of a finding/condition | Inference about the presumed cause of a finding/condition | He was struggling with insomnia due to environmental factors | 15 | 16 | 6 | 0 |
| 7 | Clinical documentation or the lack thereof | Documents mentioned in a clinical note or mentioned as missing | Patient had another thyroid US in June | 11 | 9 | 8 | 2 |
| 4 | Duration of an intervention | Statement about the length of time of an intervention | Has been on Ritalin since 2018. | 11 | 6 | 3 | 9 |
| 5 | Reason for discontinuing an intervention | The reason for discontinuing an active or past intervention | Patient no longer taking gabapentin as pain has resolved | 9 | 10 | 3 | 4 |
| 1 | Suspected finding/condition | A finding/condition described as suspected or as a current concern (not confirmed) | Suspect chronic venous stasis changes plus volume overload | 3 | 13 | 8 | 1 |
| 1 | Finding/condition as coded diagnosis | Coded diagnosis documented in the note | Tonsillar mass - ICD10-CM R22.0. | 0 | 0 | 0 | 24 |
| 1 | Complicating factor of a finding/condition | Inference about a factor that further aggravates a finding/condition | Patient seen by ENT who diagnosed GERD as a contributor to allergic rhinitis | 6 | 11 | 3 | 0 |
| 1 | Family history of finding/condition reported | Family history of a finding/condition documented in the note | Family history of premature cardiovascular disease | 8 | 5 3 | 1 | |
| 2 | Suspected intervention | An intervention described as suspected or not confirmed | Patient had one additional unknown test performed in Miami | 2 | 2 3 | 0 | |
| 2 | Side effect of an intervention | Documentation of the side effect of an intervention | Patient states drying side effects of hydrochlorothiazide | 4 | 0 2 | 0 | |
| 6 | Visit participants | Participants of the visit other than the patient | Today she returns with her daughter | 3 | 0 0 | 1 | |
| 5 | Reason for ruling out a finding/condition | Reason for not considering (ruling out) a finding/condition | Because it is a mild complaint, this less likely to be malignant | 0 | 4 0 | 0 | |
| 6 | Historian | Indication of the person reporting a finding/condition or intervention | Husband says she has been sleeping about 20 hours per day | 1 | 0 0 | 1 | |
Note: Types of data are sorted by descending order of occurrences in all sources. Example sentences are shortened in some cases for the interest of space. Sentences may be classified in more than one type of data/taxon. Abbreviations: HPI: history of present illness; IP: impression and plan; PHI: protected health information; ICD-CM: International Classification of Diseases-Clinical Modification; GERD: Gastroesophageal reflux disease.
References
- 1.The Office of the National Coordinator for Health Information Technology – Health IT Dashboard [cited 2018 July 27]. Available from: https://dashboard.healthit.gov/quickstats/quickstats.php .
- 2.KLAS Research. Hospital EMR Market Share URL: https://klasresearch.com/report/us-hospital-emr-market-share- 2018/1279 . [accessed 2019-05-10]
- 3.Wachter R, Goldsmith J. To combat physician burnout and improve care, fix the electronic health record. J. Harv Bus Rev. March 30, 2018.
- 4.Colicchio TK, Del Fiol G, Cimino JJ. Health information technology as a learning health system: Call for a national monitoring system. Learn Health Syst. 2019 Nov 20;4(1):e10207. doi: 10.1002/lrh2.10207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colicchio TK, Cimino JJ, Del Fiol G. Unintended Consequences of Nationwide Electronic Health Record Adoption: Challenges and Opportunities in the Post-Meaningful Use Era. J Med Internet Res. 2019;21(6):e13313. doi: 10.2196/13313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howe JL, Adams KT, Hettinger AZ, Ratwani RM. Electronic Health Record Usability Issues and Potential Contribution to Patient Harm. JAMA. 2018 Mar 27;319(12):1276–1278. doi: 10.1001/jama.2018.1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryant AD, Fletcher GS, Payne TH. Drug interaction alert override rates in the Meaningful Use era: no evidence of progress. Appl Clin Inform. 2014;5(3):802–813. doi: 10.4338/ACI-2013-12-RA-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siegler EL, Adelman R. Copy and paste: a remediable hazard of electronic health records. Am. J. Med. 2009;122(6):495–496. doi: 10.1016/j.amjmed.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 9.Strauss Anselm L., Fagerhaugh Shizuko Y., Suczek Barbara, Wiener Carolyn L. Social Organization of Medical Work. Chicago and London: University of Chicago Press; 1985. [Google Scholar]
- 10.Ho Y-X, Gadd CS, Kohorst KL, Rosenbloom ST. A Qualitative Analysis Evaluating The Purposes And Practices Of Clinical Documentation. Appl Clin Inform. 2014;5(1):153–68. doi: 10.4338/ACI-2013-10-RA-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koopman RJ, Steege LMB, Moore JL, et al. Physician Information Needs and Electronic Health Records (EHRs): Time to Reengineer the Clinic Note. J Am Board Fam Med. 2015 May 1;28(3):316–23. doi: 10.3122/jabfm.2015.03.140244. [DOI] [PubMed] [Google Scholar]
- 12.Downing NL, Bates DW, Longhurst CA. Physician Burnout in the Electronic Health Record Era: Are We Ignoring the Real Cause? Ann Intern Med. 2019 Feb 5;170(3):216–217. doi: 10.7326/L18-0604. [DOI] [PubMed] [Google Scholar]
- 13.Lenert LA. Toward Medical Documentation That Enhances Situational Awareness Learning. AMIA Annu Symp Proc. 2017 Feb;10(2016):763–71. [PMC free article] [PubMed] [Google Scholar]
- 14.Wrenn JO, Stein DM, Bakken S, Stetson PD. Quantifying clinical narrative redundancy in an electronic health record. J Am Med Inform Assoc. 2010;17(1):49–53. doi: 10.1197/jamia.M3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB. Use of electronic clinical documentation: time spent and team interactions. Journal of the American Medical Informatics Association. 2011;18(2):112–7. doi: 10.1136/jamia.2010.008441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siegler EL, Adelman R. Copy and paste: a remediable hazard of electronic health records. Am J Med. 2009. [DOI] [PubMed]
- 17.Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T. Safe Practices for Copy and Paste in the EHR. Appl Clin Inform. 2017 Jan 11;8(1):12–34. doi: 10.4338/ACI-2016-09-R-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Payne TH, Corley S, Cullen TA, Gandhi TK, Harrington L, Kuperman GJ, et al. Report of the AMIA EHR 2020 Task Force on the Status and Future Direction of EHRs. J Am Med Inform Assoc. 2015 May 28;ocv066 doi: 10.1093/jamia/ocv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, Goeders L, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med. 2016 Dec 06;165(11):753–760. doi: 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 20.Bowman S. Impact of electronic health record systems on information integrity: quality and safety implications. Perspect Health Inf Manag. 2013;10:1c. [PMC free article] [PubMed] [Google Scholar]
- 21.Cimino JJ, Li Z, Weng C. Dykes P, editor. An Exploration of the Terminology of Clinical Cognition and Reasoning. 2018 AMIA Fall Symposium, San Francisco. 2018 Dec 5;2018:321–329. [PMC free article] [PubMed] [Google Scholar]
- 22.Dissanayake PI, Colicchio TK, Cimino JJ. Using clinical reasoning ontologies to make smarter clinical decision support systems: a systematic review and data synthesis. J Am Med Inform Assoc. 2020 Jan 1;27(1):159–74. doi: 10.1093/jamia/ocz169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Colicchio TK, Dissanayake PI, Cimino JJ. Formal Representation of Patients’ Care Context Data: the Path to Improving the Electronic Health Record. J Am Med Inform Assoc. 2020. (in press) [DOI] [PMC free article] [PubMed]
- 24.Colicchio TK, Cimini J. Clinicians’ Reasoning as Reflected in Electronic Clinical Note-Entry and Reading/Retrieval: A Systematic Review and Qualitative Synthesis. J Am Med Inform Assoc. 2019 Feb 1;26(2):172–184. doi: 10.1093/jamia/ocy155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ackerman S, Gleason N. Transitioning Patients From Specialty Care to Primary Care: What We Know and What We Can Do. J Ambul Care Manage. 2018 Dec;41(4):314–22. doi: 10.1097/JAC.0000000000000253. [DOI] [PubMed] [Google Scholar]
- 26.Sittig DF, Wright A, Ash J, Singh H. New unintended adverse consequences of electronic health records. Yearb Med Inform. 2016 Nov;10(1):7–12. doi: 10.15265/IY-2016-023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tuepker A, Zickmund SL, Nicolajski CE, et al. Providers’ note-writing practices for post-traumatic stress disorder at five United States Veterans Affairs facilities. J Behav Health Serv Res. 2016;43(3):428–42. doi: 10.1007/s11414-015-9472-9. [DOI] [PubMed] [Google Scholar]
- 28.Weed LL. Medical records that guide and teach. N Engl J Med. 1968;278(11):593–600. doi: 10.1056/NEJM196803142781105. [DOI] [PubMed] [Google Scholar]
- 29.Devlin J, Chang M-W, Lee K, Toutanova K., Devlin J., et al. Bert: pre-training of deep bidirectional transformers for language understanding. Association for Computational Linguistics; 2019. pp. 4171–4186. 2019. [Google Scholar]