Introduction
Although over the past 2 decades improvements in audiovisual communication technologies have led to an increased use of telemedicine across many health care disciplines [1,27], it had not been widely adopted in orthopedic surgery and other musculoskeletal specialties within the United States until the onset of the COVID-19 pandemic [19]. However, mandated social distancing measures and restrictions on in-person consultations have forced both clinicians and patients to become familiar with web-based videoconferencing platforms for care delivery. To continue providing musculoskeletal care during the pandemic, there has been a dramatic increase in telemedicine visits [2,20]. Previous studies on telemedicine have shown that these visits increase access to care while having lower overall costs and maintaining patient satisfaction [5,9]. With increased access to high-speed videoconferencing platforms, widely available personal computing devices, and patient demand for high-quality, convenient, efficient specialty care, telemedicine is an effective medium for musculoskeletal care that will endure beyond the COVID-19 pandemic [2,19,20,22,24,28]. One particular challenge to the long-term adoption of telemedicine in musculoskeletal specialties has been a widely held perception that remote visits are markedly limited by the inability to perform an in-person physical examination [3,12,13,29,30]. In particular, it has been thought that examination maneuvers requiring manual motor testing for strength, motion assessment, stability, and provocative testing for pain may be difficult to perform remotely [20]. However, in a randomized controlled trial of orthopedic visits in which telemedicine encounters were compared with in-person consultations, physicians rated their ability to examine patients as good or very good in 98% of telehealth visits, with no significant differences between groups and no adverse safety events [4]. When specifically considering the physical examination of the knee, closer review suggests that most of the examination can actually be successfully performed remotely with some modifications.
The purpose of this commentary is to describe a comprehensive knee physical examination for video telemedicine encounters, including (1) verbal instructions in layman’s terms of each examination maneuver, (2) annotated images of each examination maneuver that can be provided to patients via screen share options, and (3) checklists for documentation.
Preparation for Telemedicine Visit
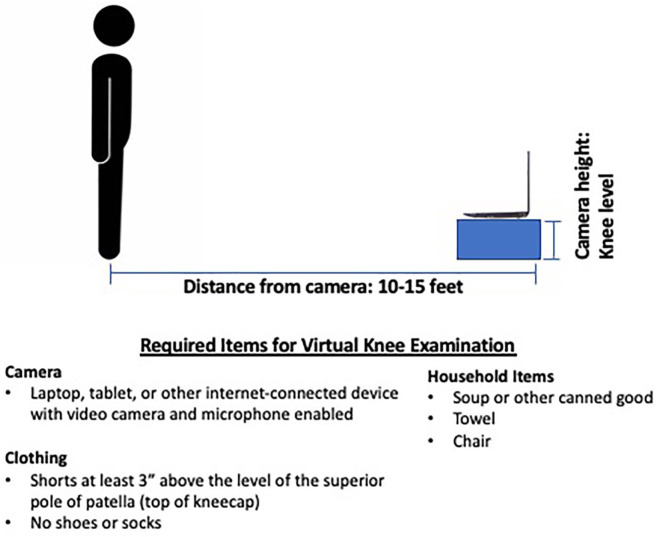
In our experience, before the scheduled encounter, the patient must be provided with information that allows them to become familiar with the specific Internet videoconferencing platform that is being used (eg, Zoom, Skype, and Teams) and should be encouraged to test and verify that their Internet connectivity, video quality, and audio systems are functional for the upcoming virtual visit. Most of these videoconferencing platforms allow for testing each of these parameters prior to a meeting, or in this case, a telemedicine encounter. In addition, prior to the virtual visit, we encourage the patient to complete an intake form containing questions about their chief complaint, history of present illness, past medical and surgical history, allergies, home medications, social history, and a complete review of systems. In addition to the virtual examination and medical decision-making, several of these aforementioned intake items must be collected and documented to appropriately bill for the visit. The patient should also review instructions on how to set up their camera to adequately visualize the knee. At the start of the visit, the patient should be seated with their camera centered at their eye level. During the physical examination, the patient will be asked to reposition themselves based on the specific examination maneuver being performed. The required distance and angle of the camera position will vary by the type of camera and the patient position. Finally, the patient should be dressed in appropriate clothing for the virtual visit. We provide the schematic shown in Fig. 1 to patients who are being seen for a knee complaint. This schematic contains guidelines for appropriate clothing, examination space, patient positioning, camera positioning, and any required common household items. In some cases, even when all the aforementioned information has been provided to the patient ahead of the visit, issues can arise with them connecting to the videoconferencing platform. First, we recommend that a member of the provider’s office staff calls the patient and attempts to guide them through these issues. However, it is essential that support from information technology is available for troubleshooting any technical difficulties that cannot be resolved by the provider’s office staff.
Fig. 1.
Schematic of virtual knee examination.
Virtual Knee Examination
We have divided the knee examination into a basic examination (core knee examination) and pathology-specific special testing [17]. The basic examination includes inspection, palpation, range of motion testing, motor testing, sensory testing, and a peripheral vascular examination [3]. Patients with undifferentiated lower extremity pain with or without low back pain should be assessed for a neurologic etiology. (The lumbar spine examination is covered in a separate article in this special issue of the HSS Journal.) Hip or peripheral vascular pathology should also be considered when the pain is difficult for the patient to localize. An assessment for hip pain and restricted motion should be performed on nearly every patient with a complaint of knee pain. (The hip examination is covered in a separate article in this issue.) Special testing can be performed as needed based on the patient’s history and findings on the core knee examination. A PowerPoint document that contains annotated illustrated examples of each knee physical examination maneuver is available as Supplemental Presentation 1. The clinician may choose to demonstrate the examination maneuver to the patient or can share the annotated illustrated examples via screen share options.
Core knee examination
The patient should be asked to position themselves so that their camera will be able to visualize the front, sides, and back of the knee as they turn their body toward the camera during a thorough inspection. This inspection of the bilateral lower extremities should evaluate for coronal and sagittal alignment, muscle atrophy, deformity, prior incisions, scars, effusion, soft tissue swelling, ecchymosis, erythema, skin lesions, or rashes. Gait should be assessed. The patient may be asked to identify the location of maximal pain by pointing to that area and self-palpating. Bilateral range of motion testing should be performed. A virtual goniometer may be used for the evaluation of both alignment and range of motion [7,28]. While bilateral sensory testing and a peripheral vascular examination can be performed by the patient, strength testing requires a remote examiner, such as a family member (Supplemental Table 1 [available online]).
Special testing
Pathology-specific special testing can be categorized into ligament tests, meniscal tests, and patellofemoral joint tests.
Ligament testing
Previous studies have shown that, when performed by an experienced examiner, the lever test is actually more sensitive than other tests, including the Lachman test, for the diagnosis of anterior cruciate ligament (ACL) injury [3,18]. As originally described, the examiner presses down on the distal third of the patient’s quadriceps with 1 hand, while the other hand is positioned as a fist beneath the proximal third of the patient’s calf [14]. A positive test results in an objective and visual finding—the patient’s heel will not raise off the table; it does not rely on subjective determination like the Lachman and anterior drawer tests. We have modified this examination to be performed by the patient independently, with a soup or vegetable can placed beneath the calf, and the patient pressing down on their distal quadriceps muscle. To evaluate for posterior cruciate ligament injury, the posterior sag test [25] and the quadriceps active test [3,6,25] can be performed by the patient independently. Both of these tests should be performed while the patient is supine and the camera is pointed toward the side of the knee (Supplemental Table 2).
Meniscus testing
We have modified the common tests used to assess for meniscal pathology to be performed by the patient independently, including the bounce test and the hyperflexion test [3,21]. As it was originally described, the Thessaly test can be performed by the patient independently while directly facing the camera (Supplemental Table 3) [3,8,10].
Patellofemoral joint testing
The “J-sign” indicates patellar maltracking and may be observed with the patient facing the camera in a seated position and actively moving their knee back and forth through a range of motion from flexion into extension [3,21,23,26]. Patellofemoral crepitus can similarly be detected by the patient by placing 1 of their hands over the patella while actively moving the affected knee back and forth from flexion into extension. Crepitus may be enhanced by knee extension against resistance, and the patient can be encouraged to do this with the help of a family member. We have modified the patellar apprehension test to be performed entirely by the patient in a seated position with the ankle of the affected extremity crossed over the unaffected leg and a laterally directed force placed on the patella using both thumbs [3,21]. A single-leg squat performed with the patient directly facing the camera can demonstrate valgus and internal rotation collapse that may suggest a correctible neuromuscular imbalance or hip pathology which can contribute to anterior knee pain (Supplemental Table 4) [11].
The maneuvers that comprise the Beighton score (knee and elbow recurvatum, thumb to forearm apposition, and lumbar flexion) can be performed independently by the patient to evaluate for generalized joint hypermobility (Supplemental Table 5) [15].
Implementation of Virtual Knee Examination
The tools provided here offer a comprehensive, standardized approach to the virtual knee examination including office workflow, previsit setup, and physical examination testing. Similar to an in-person new patient consultation, we recommend that the virtual knee physical examination starts with the core knee examination followed by additional pathology-specific special testing as clinically appropriate. The specific special tests performed should be directed by the patient’s history of present illness and findings on the core knee examination. The time required to perform an examination can vary based on a variety of factors, but in our experience, the core knee examination as listed requires approximately 5 minutes and a problem-focused examination generally approximately 5 to 10 minutes to complete. Efficiency can be optimized by choosing a sequence of examination maneuvers that minimizes the number of times the patient is asked to move between standing, sitting, and supine positions. Improved standardization of these modified virtual examination tests will result in improved reliability and validity of the virtual examination.
Limitations
An in-office examination performed by an experienced clinician undoubtedly offers a more comprehensive musculoskeletal evaluation compared with a virtual examination including focused palpation in areas consistent with patient’s history, tactile recognition of crepitus, accurate strength assessment, and assessment of ligament integrity. At this point, it is impossible to replace the ability of an experienced clinician to perform certain physical examination maneuvers such as the Lachman and pivot shift examinations for ACL injury. In addition to knee ligament assessment, we have found that remote assessment of patellar instability also generally provides more limited diagnostic information compared with an in-person examination. When patients present with a history suggestive of these conditions, we typically perform a virtual physical examination during the initial consultation but have a low threshold to obtain advanced imaging (typically in the form of a magnetic resonance imaging) which may be followed by a subsequent in-person visit for examination. However, by including alternatives such as the lever test for ACL integrity [3,18] and our modification of patellar apprehension testing, we can still obtain useful data that allow for reasonable clinical decision-making. Although we provide our best recommendations regarding optimal positioning of the patient and camera for each examination maneuver, videoconferencing may prevent clinicians from interpreting certain tests with the same accuracy as an in-person examination. A specific example of this is a subtle knee flexion contracture or effusion that is more easily appreciated in person than via videoconferencing. While we attempted to modify as many tests as possible to be performed independently by the patient, certain tests do require a remote examiner. Such tests are often performed by someone who is not trained in performing the musculoskeletal examination, and it is possible that findings may be incorrectly interpreted or reported by the examiner or patient, despite uniform instructions. The sensitivity, specificity, and diagnostic accuracy of the tests that we have included when performed by a patient or by an untrained remote examiner and interpreted by a clinician have yet to be defined but are likely lower than published values for the same tests when they are performed by an experienced examiner in person. It is critical that treatment plans only be formulated when findings of the virtual physical examination corroborate the patient’s history and imaging studies. Conflicting findings must prompt an in-person evaluation prior to clinical decision-making [16].
The COVID-19 crisis has forced our society to become increasingly facile with video-based communication platforms. Orthopedists and other providers of musculoskeletal care have found that virtual physical examinations can be performed in a similar manner to in-office visits, albeit with some inherent limitations [22]. Various modifications of physical examination maneuvers, including for evaluation of the knee, have helped to overcome some of these limitations and allow for a more comprehensive virtual examination. Due in part to high patient and clinician satisfaction, health care savings, improved access to care, and improved time efficiency, we believe that telemedicine in orthopedics will endure beyond the resolution of the current COVID-19 crisis. Future studies will seek to validate the virtual knee examination maneuvers presented here.
Supplemental Material
Supplemental material, sj-pdf-2-hss-10.1177_1556331620975039 for The Knee Examination for Video Telemedicine Encounters by Samuel A. Taylor, Joseph D. Lamplot, Joseph D. Lamplot, Sridhar Pinnamaneni, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Danyal H. Nawabi, Warren K. Young, Scott A. Rodeo and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-pptx-3-hss-10.1177_1556331620975039 for The Knee Examination for Video Telemedicine Encounters by Samuel A. Taylor, Joseph D. Lamplot, Joseph D. Lamplot, Sridhar Pinnamaneni, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Danyal H. Nawabi, Warren K. Young, Scott A. Rodeo and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-zip-1-hss-10.1177_1556331620975039 for The Knee Examination for Video Telemedicine Encounters by Samuel A. Taylor, Joseph D. Lamplot, Joseph D. Lamplot, Sridhar Pinnamaneni, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Danyal H. Nawabi, Warren K. Young, Scott A. Rodeo and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Joshua S. Dines, MD, reports relationships with Arthrex Inc, Thieme Inc, Linvatec, Wolters Kluwer Health, American Shoulder and Elbow Surgeons, and the Journal of Shoulder and Elbow Surgery, outside the submitted work. Scott A. Rodeo, MD, reports relationships with Advance Medical and Ortho RTI, outside the submitted work. Samuel A. Taylor, MD, reports relationships with DJO Orthopedics and Mitek, outside the submitted work. The other authors declare they have no conflicts of interest.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
Supplemental Material: Supplemental material for this article is available online.
CME Credit: Please go to HSS eAcademy at https://bit.ly/HSSJCME to find all journal-related CME, complete the online post-test, and claim CME credit.
References
- 1. Baker J, Stanley A. Telemedicine technology: a review of services, equipment, and other aspects. Curr Allergy Asthma Rep. 2018;18(11):60. [DOI] [PubMed] [Google Scholar]
- 2. Bernstein DN, Baumhauer JF, Kang JD, Makhni MC. Transforming the orthopaedic patient experience through telemedicine. J Patient Exp. 2020;7(3):302–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bronstein RD, Schaffer JC. Physical examination of the knee: meniscus, cartilage, and patellofemoral conditions. J Am Acad Orthop Surg. 2017;25(5):365–374. [DOI] [PubMed] [Google Scholar]
- 4. Buvik A, Bugge E, Knutsen G, Smabrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Craig J, Patterson V. Introduction to the practice of telemedicine. J Telemed Telecare. 2005;11(1):3–9. [DOI] [PubMed] [Google Scholar]
- 6. Daniel DM, Stone ML, Barnett P, Sachs R. Use of the quadriceps active test to diagnose posterior cruciate-ligament disruption and measure posterior laxity of the knee. J Bone Joint Surg Am. 1988;70(3):386–391. [PubMed] [Google Scholar]
- 7. Ferriero G, Vercelli S, Sartorio F, et al. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36(2):146–151. [DOI] [PubMed] [Google Scholar]
- 8. Goossens P, Keijsers E, van Geenen RJC, et al. Validity of the Thessaly test in evaluating meniscal tears compared with arthroscopy: a diagnostic accuracy study. J Orthop Sports Phys Ther. 2015;45(1):18–24, B1. [DOI] [PubMed] [Google Scholar]
- 9. Granja C, Janssen W, Johansen MA. Factors determining the success and failure of eHealth interventions: systematic review of the literature. J Med Internet Res. 2018;20(5):e10235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Harrison BK, Abell BE, Gibson TW. The Thessaly test for detection of meniscal tears: validation of a new physical examination technique for primary care medicine. Clin J Sport Med. 2009;19(1):9–12. [DOI] [PubMed] [Google Scholar]
- 11. Herrington L. Knee valgus angle during single leg squat and landing in patellofemoral pain patients and controls. Knee. 2014;21(2):514–517. [DOI] [PubMed] [Google Scholar]
- 12. Hippensteel KJ, Brophy R, Smith MV, Wright RW. A comprehensive review of physical examination tests of the cervical spine, scapula, and rotator cuff. J Am Acad Orthop Surg. 2019;27(11):385–394. [DOI] [PubMed] [Google Scholar]
- 13. Hippensteel KJ, Brophy R, Smith MV, Wright RW. Comprehensive review of provocative and instability physical examination tests of the shoulder. J Am Acad Orthop Surg. 2019;27(11):395–404. [DOI] [PubMed] [Google Scholar]
- 14. Jarbo KA, Hartigan DE, Scott KL, Patel KA, Chhabra A. Accuracy of the lever sign test in the diagnosis of anterior cruciate ligament injuries. Orthop J Sports Med. 2017;5(10). 10.1177/2325967117729809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Juul-Kristensen B, Røgind H, Jensen DV, Remvig L. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology (Oxford). 2007;46(12):1835–1841. [DOI] [PubMed] [Google Scholar]
- 16. Kane LT, Thakar O, Jamgochian G, et al. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29(4):775–783. [DOI] [PubMed] [Google Scholar]
- 17. Lamplot JP, Pinnamaneni S, Swensen-Buza S, et al. The virtual shoulder and knee physical examination. Orthop J Sports Med. 2020;8. 10.1177/2325967120962869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lelli A, Di Turi RP, Spenciner DB, Dòmini M. The “Lever Sign”: a new clinical test for the diagnosis of anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2794–2797. [DOI] [PubMed] [Google Scholar]
- 19. Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469–e476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Makhni MC, Riew GJ, Sumathipala MG. Telemedicine in orthopaedic surgery: challenges and opportunities. J Bone Joint Surg Am. 2020;102(13):1109–1115. [DOI] [PubMed] [Google Scholar]
- 21. Malanga GA, Andrus S, Nadler SF, McLean J. Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil. 2003;84(4):592–603. [DOI] [PubMed] [Google Scholar]
- 22. Massey PA, McClary K, Zhang AS, Savoie FH, Barton RS. Orthopaedic surgical selection and inpatient paradigms during the coronavirus (COVID-19) pandemic. J Am Acad Orthop Surg. 2020;28(11):436–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Post WR. Clinical evaluation of patients with patellofemoral disorders. Arthroscopy. 1999;15(8):841–851. [DOI] [PubMed] [Google Scholar]
- 24. Rao SS, Loeb AE, Amin RM, Golladay GJ, Levin AS, Thakkar SC. Establishing telemedicine in an academic total joint arthroplasty practice: needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today. 2020;6:617–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rubinstein RA, Jr, Shelbourne KD, McCarroll JR, VanMeter CD, Rettig AC. The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries. Am J Sports Med. 1994;22(4):550–557. [DOI] [PubMed] [Google Scholar]
- 26. Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter KE. Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res. 2010;468(1):266–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tachakra S, Wang XH, Istepanian RSH, Song YH. Mobile e-health: the unwired evolution of telemedicine. Telemed J E Health. 2003;9(3):247–257. [DOI] [PubMed] [Google Scholar]
- 28. Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102(12):e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination. Part I: the rotator cuff tests. Am J Sports Med. 2003;31(1):154–160. [DOI] [PubMed] [Google Scholar]
- 30. Tennent TD, Beach WR, Meyers JF. A review of the special tests associated with shoulder examination. Part II: laxity, instability, and superior labral anterior and posterior (SLAP) lesions. Am J Sports Med. 2003;31(2):301–307. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-2-hss-10.1177_1556331620975039 for The Knee Examination for Video Telemedicine Encounters by Samuel A. Taylor, Joseph D. Lamplot, Joseph D. Lamplot, Sridhar Pinnamaneni, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Danyal H. Nawabi, Warren K. Young, Scott A. Rodeo and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-pptx-3-hss-10.1177_1556331620975039 for The Knee Examination for Video Telemedicine Encounters by Samuel A. Taylor, Joseph D. Lamplot, Joseph D. Lamplot, Sridhar Pinnamaneni, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Danyal H. Nawabi, Warren K. Young, Scott A. Rodeo and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery
Supplemental material, sj-zip-1-hss-10.1177_1556331620975039 for The Knee Examination for Video Telemedicine Encounters by Samuel A. Taylor, Joseph D. Lamplot, Joseph D. Lamplot, Sridhar Pinnamaneni, Stephanie Swensen-Buza, Cort D. Lawton, Joshua S. Dines, Danyal H. Nawabi, Warren K. Young, Scott A. Rodeo and Samuel A. Taylor in HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery