Abstract
Context:
Plantar fasciitis (PF) is a common condition in active individuals. The lack of agreement on PF etiology makes treatment challenging and highlights the importance of understanding risk factors for preventive efforts.
Objective:
The purpose of this systematic review and meta-analysis was to determine what factors may put physically active individuals at risk of developing PF.
Data Sources:
CENTRAL, CINAHL, EMBASE, Gray Lit, LILACS, MEDLINE (PubMed), ProQuest, Scopus, SPORTDiscus, and Web of Science were searched through April 2018 and updated in April 2020.
Study Selection:
Studies were included if they were original research investigating PF risk factors, compared physically active individuals with and without PF, were written in English, and were accessible as full-length, peer-reviewed articles.
Study Design:
Systematic review and meta-analysis.
Level of Evidence:
Level 3, because of inconsistent definitions and blinding used in the included observational studies.
Data Extraction:
Data on sample characteristics, study design and duration, groups, PF diagnosis, and risk factors were extracted. The methodological quality of the studies was assessed using the Strengthening the Reporting of Observational Studies in Epidemiology statement. When means and standard deviations of a particular risk factor were presented 2 or more times, that risk factor was included in the meta-analysis.
Results:
Sixteen studies were included in the systematic review and 11 risk factors in the meta-analysis. Increased plantarflexion range of motion (weighted mean difference [MD] = 7.04°; 95% CI, 5.88-8.19; P < 0.001), body mass index (MD = 2.13 kg/m2; 95% CI, 1.40-2.86; P < 0.001; I2 = 0.00%), and body mass (MD = 4.52 kg; 95% CI, 0.55-8.49; P = 0.026) were risk factors for PF.
Conclusion:
Interventions focused on addressing a greater degree of plantarflexion range of motion, body mass index, and body mass and their load on the force-absorbing plantar surface structures may be a good starting point in the prevention and treatment of active individuals with PF.
Keywords: plantar fasciosis, heel pain, physically active, athletic injuries, runners, military
The plantar fascia is a subcutaneous structure of dense connective tissue extending from the medial tubercle of the calcaneus to the metatarsal heads and supporting the medial longitudinal arch of the foot.6,17 It acts both as a beam for the metatarsals when they undergo bending forces such as in gait propulsion and as a truss when the foot absorbs forces such as during the loading phase of gait.17 Excessive load on the plantar fascia can result in plantar fasciitis (PF), which, despite its name, is considered a degenerative pathology versus an inflammatory condition.6,17 In fact, a more appropriate term for the condition is plantar fasciosis or plantar fasciopathy; these terms continue to gain traction.10,13
In active individuals, PF is common. Incidence ranges from 4.5% to 10.0% and prevalence is from 5.2% to 17.5% in runners.12 Individuals with PF often report a gradual onset of heel pain that is worse during their first few steps in the morning or after a period of inactivity.1 They also often report a localized area of maximal tenderness over the anteromedial aspect of the heel, particularly at the medial tubercle of the calcaneus where the plantar fascia originates.1,6 The pain may decline with a warm-up but then reappear at the end of training.17
Researchers cite intrinsic factors such as anatomy and extrinsic factors such as training errors as risk factors for PF,6,17 but few researchers have investigated risk factors specific to an active population. Furthermore, although the results of individual risk factor studies inform clinical practice, reported findings are often based on small samples with conflicting results. Studying the potential risk factors in a systematic fashion can strengthen preventive practices, reduce bias, and increase confidence through the analysis of pooled data. The purpose of this systematic review and meta-analysis was to assess what factors may put physically active individuals at risk of developing PF.
Methods
A detailed explanation of methods used to conduct this systematic review and meta-analysis are in Appendix 1 (available in the online version of this article) while an overview is provided below.
For inclusion in this systematic review, studies were original research that investigated risk factors associated with PF, compared physically active individuals with PF to physically active individuals without PF, were published in the English language, and were accessible as full manuscripts in peer-reviewed journals.
Select databases were searched to identify studies that met the inclusion criteria. Reference lists of included or other relevant articles (eg, recent reviews) were also searched for additional references. The initial search was carried out from the earliest date to April 2018 using keywords (Medical Subject Headings and text words) within 3 groups: group 1 terms pertained to the population, group 2 terms pertained to the injury, and group 3 terms pertained to risk factors. The search strategy was updated using the same keywords in April 2020. Two reviewers divided the articles and screened titles and/or abstracts of studies identified in the search.
Two reviewers independently abstracted relevant data from all included studies into a spreadsheet and conducted the quality assessment; a third reviewer checked their abstraction for accuracy and completeness. As the 2 reviewers abstracted the data, they used the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement to assess what was planned, completed, and found in the studies, all of which were observational in nature (cross-sectional, cohort, case-control).27
After data abstraction, the reviewers evaluated common continuous variables grouped by the following risk factor categories: ankle plantarflexion range of motion (ROM), body mass index (BMI), body mass, dynamic pronation, arch height, height, static pronation, training volume, ankle dorsiflexion ROM, standing calcaneal angle, years running, leg-length discrepancy, total rearfoot movement, and quadriceps angle (Q-angle). If the outcome means and standard deviations for a risk factor were reported for 2 or more groups/studies, a meta-analysis was conducted to estimate a pooled effect size. Weighted mean differences (MDs) and 95% CIs were calculated using random-effects models. Heterogeneity was assessed using I2, which measures the degree of inconsistency across studies.9 A value of 25%, 50%, and 75% indicates low, moderate, and high levels, respectively, of heterogeneity in a sample.9 OpenMeta[Analyst] was used to estimate pooled effect sizes, 95% CIs, and heterogeneity.29
Results
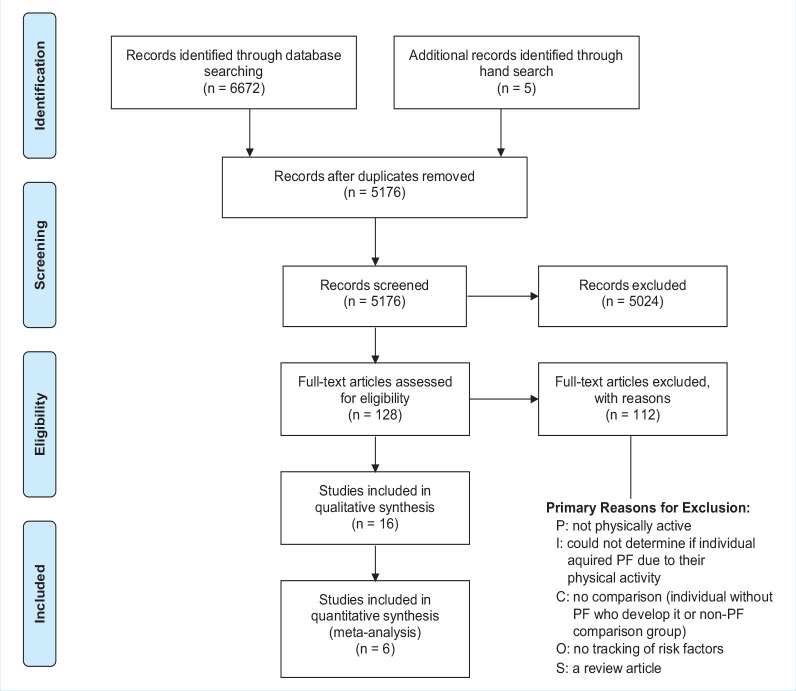
A total of 6672 studies were found using the search strategy. After removing duplicates, eliminating studies that did not fit the PICOS (patient, intervention, comparison, outcome, study design) question, and hand searching reference lists, a total of 16 original research studies were included in the systematic review and underwent risk assessment and data extraction (Figure 1). When examining extracted data from the 16 original research studies to identify common risk factors across studies for the meta-analysis, 6 studies were eligible for the meta-analysis.2,8,14,18,21,30 Summary of findings and characteristics of the 16 studies included in this systematic review are presented in Appendix 2 (available online). The 6 cross-sectional studies included in the meta-analysis were published between 1984 and 2019, involved 801 participants (181 PF, 620 control), and provided sufficient data to assess 11 risk factors (Table 1).
Figure 1.
Search process flowchart. PF, plantar fasciitis.
Table 1.
Risk factors included in the meta-analysis
| Risk Factor | Participants and Groups | Mean ± SD | Studies/Data Sets Excluded From Meta-analysis and Reasons |
|---|---|---|---|
| Significant risk factorsa | |||
| Ankle plantarflexion ROM, deg | Total: 100 recreational and competitive runners14,30
39 PF (right: 12,30 left: 12,30 affected: 1514) 61 Control (right: 21,30 left: 21,30 unaffected: 1914) |
PF: 62.8 ± 1.4 Control: 56.2 ± 1.0 |
|
| Body mass index, kg/m2 | Total: 90 recreational runners21 and 113 military recruits8
101 PF (male: 90, female: 11) 102 control (male: 82, female: 20) |
PF: 24.1 ± 2.6 Control: 22.0 ± 2.3 |
No control group data reported19,26
Data were significant outliers22 |
| Body mass, kg | Total: 90 recreational runners21
30 PF (male: 19, female: 11) 60 control (male: 40, female: 20) |
PF: 67.9 ± 14.3 Control: 63.9 ± 11.4 |
No control group data reported20,26
Data were significant outliers22 |
| Nonsignificant risk factorsa | |||
| Arch height index | Total: 124 recreational and competitive runners14,21
45 PF, 79 control |
PF: 0.25 ± 0.07 Control: 0.26 ± 0.08 |
No control group data reported19
Different measurement approach18 |
| Height, m | Total: 90 recreational runners21
30 PF (male: 19, female: 11) 60 control (male: 40, female: 20) |
PF: 1.7 ± 0.1 Control: 1.8 ± 0.1 |
No control group data reported4,19,25 |
| Static pronation, deg | Total: 448 runners2
16 PF (right: 8, left: 8) 432 control (right: 216, left: 216) |
PF: 7.1 ± 0.4 Control: 7.8 ± 1.8 |
|
| Training volume, km/wk | Total: 123 recreational and competitive runners21,30
42 PF, 81 control |
PF: 40.6 ± 6.3 Control: 36.3 ± 12.3 |
Insufficient control group data reported4,14,19 |
| Ankle dorsiflexion ROM, deg | Recreational and competitive runners14
15 PF, 19 control Female runners18 25 PF, 25 control Runners30 12 PF, 21 control Military recruits8 71 PF, 42 control |
PF: 10.7 ± 5.1, control: 10.2 ± 4.8 Knee extended: PF: 4.3 ± 5.8, control: 2.1 ± 4.4 Knee flexed: PF: 15.8 ± 6.9, control: 14.3 ± 7.3 Right: PF: 7.4 ± 4.9, control: 9.5 ± 4.5 Left: PF: 8.1 ± 4.3, control: 9.8 ± 4.2 |
|
| Q-angle, deg | Recreational and competitive runners14
15 PF, 19 control Military recruits8 71 PF, 42 control |
PF: 13.0 ± 5.7 Control: 13.6 ± 6.4 PF: 16.5 ± 6.8 Control: 16.5 ± 5.9 |
|
| Studies with high heterogeneityb | |||
| Dynamic pronation, deg | Total: 532 recreational and competitive runners2,14,18
56 PF (right: 8,2 left: 8,2 affected: 4014,18) 476 control (right: 216,2 left: 216,2 unaffected: 4414,18) |
PF: −3.0 ± 4.4 Control: −1.4 ± 4.9 |
|
| Standing calcaneal angle, deg | Female runners18
25 PF, 25 control Long-distance runners19 30 PF, 60 control Runners30 12 PF, 21 control |
PF: 4.1 ± 3.3, Control: 3.2 ± 3.3 PF: 6.9 ± 3.2, Control: 7.2 ± 5.5 Right: PF: 5.7 ± 4.3, Control: 8.3 ± 3.5 Left: PF: 4.0 ± 3.9, Control: 6.2 ± 3.9 |
No control group data reported21 |
PF, plantar fasciitis; Q-angle, quadriceps angle; ROM, range of motion.
Data in this category are reported as pooled means ± SDs.
Data in this category are reported as group means ± SDs by study.
The STROBE assessment of what was planned, completed, and found in the 16 individual studies are presented in Appendix 3 (available online). Items with the highest conformity across studies included the introduction/rationale (81%), definition of variables in the methods (75%), and reported results of outcome data (75%). Items with the lowest conformity across studies included results on participants (19%) and descriptive data (13%), reduction of bias in methods (6%), description of statistical methods (7%), and funding sources (6%).
Risk Factors for PF Included in the Meta-Analysis
Continuous data for the following risk factors were reported 2 or more times and included in the meta-analysis: ankle plantarflexion ROM, BMI, body mass, dynamic pronation, arch height, height, static pronation, training volume, ankle dorsiflexion ROM, standing calcaneal angle, and Q-angle. More than 120 other risk factors were reported in the 16 studies; however, none other were measured consistently in more than 2 studies (Appendix 2, available online). Because of the heterogeneity of the risk factors not included in the meta-analysis, no moderate-to-strong evidence exists supporting their role as risk factors for PF.
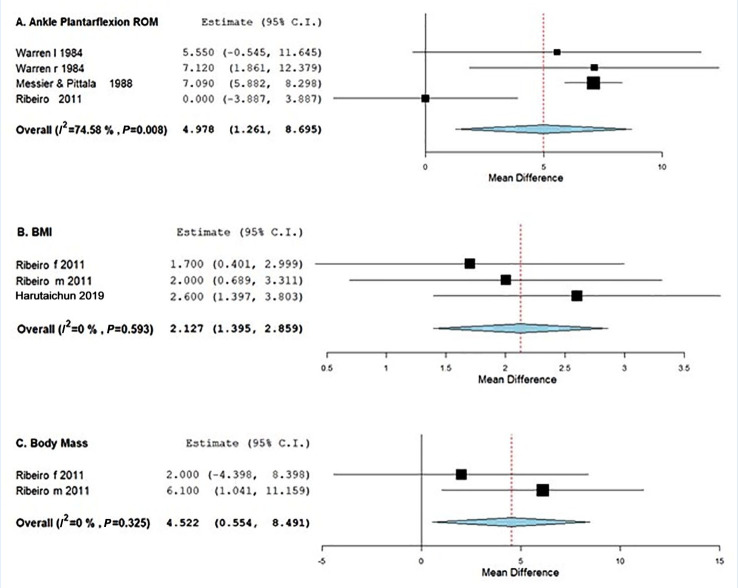
There were significant differences between individuals with PF compared with control groups for the following risk factors in the meta-analysis: ankle plantarflexion ROM, BMI, and body mass (Figure 2, Table 1). Specifically, individuals with PF had significantly greater plantarflexion ROM compared with control groups (PF: 62.8° ± 1.4°; control: 56.2° ± 0.55°; MD = 7.04°; 95% CI, 5.88-8.19; P < 0.001; I2 = 0.00%) (Figure 2a, Table 1). Individuals with PF had significantly higher BMI compared with control groups (PF: 24.1 ± 2.6 kg/m2; control: 22.0 ± 2.3 kg/m2; MD = 2.13 kg/m2; 95% CI, 1.40-2.86; P < 0.001; I2 = 0.00%) (Figure 2b, Table 1). And individuals with PF had significantly more body mass compared with control groups (PF: 67.9 ± 14.3 kg; control: 63.9 ± 11.4 kg; MD = 4.52 kg; 95% CI, 0.55-8.49; P = 0.026; I2 = 0.00%) (Figure 2c, Table 1).
Figure 2.
Effects of ankle plantarflexion ROM, BMI, and body mass, on PF. BMI, body mass index; PF, plantar fasciitis; ROM, range of motion.
No significant differences between individuals with PF and control groups were found for the following risk factors in the meta-analysis: arch height index (MD = −0.01; 95% CI, −0.03 to 0.01; P = 0.48; I2 = 0.00%) (Appendix 4a, available online; Table 1), height (MD = −0.02 m; 95% CI, −2.43 to 2.39; P = 0.99; I2 = 0.00%) (Appendix 4b, Table 1), static pronation (MD = −0.64°; 95% CI, −3.71 to 2.43; P = 0.68; I2 = 0.00%) (Appendix 4c, Table 1), training volume (MD = 1.66 km/wk; 95% CI, −4.95 to 8.27; P = 0.62; I2 = 28.2%) (Appendix 4d, Table 1), ankle dorsiflexion ROM (MD = 0.47°; 95% CI, 1.14-2.08; P = 0.57; I2 = 68.3%) (Appendix 4e, Table 1), and Q-angle (MD = −0.90°; 95% CI, −2.14 to 1.96; P = 0.93; I2 = 0.00%) (Appendix 4f, Table 1).
Results of the meta-analysis for dynamic pronation and standing calcaneal angle were inconclusive due to high heterogeneity (≥75%). Four data sets across 3 studies measured dynamic pronation as a potential risk factor for PF (Table 1).2,14,18 While participants were recreational and competitive runners (n = 532; 56 PF, 476 control), the high heterogeneity (I2 = 85.62%) suggests other factors, such as PF definition used or measurement method, were different between studies and could not be controlled, indicating data should not be pooled. Therefore, the role of dynamic pronation as a PF risk factor remains unknown.
Four studies measured standing calcaneal angle as a potential risk factor for PF (Table 1).18,19,21,30 While participants were recreational and competitive runners (n = 206; 79 PF, 127 control), the high heterogeneity (I2 = 75.1%) suggests other factors, such as PF definition used or measurement method, were too varied among studies and could not be controlled, indicating data should not be pooled. All 4 studies defined the standing calcaneal angle, a measure of calcaneal valgus or rearfoot pronation, as the angle of the posterior heel (calcaneus) bisected by a vertical line; however, the method to obtain the measurement varied between studies. Therefore, the role of standing calcaneal angle as a stress fracture risk factor remains unknown.
Summary of Findings for Studies Not Included in the Meta-analysis
Findings from studies that reported continuous data on leg-length discrepancy (n = 2),14,30 total rearfoot movement (n = 1),14 and years running (n = 5),4,14,21,26 but did not meet the minimum criteria for meta-analysis, are presented in Appendix 2 (available online). The evidence for the role of leg-length discrepancy as a risk factor of PF is conflicting. Warren30 measured leg-length inequality (cm) and found no difference between PF and control groups, whereas Messier and Pittala14 measured true and apparent leg length and reported that 53% of the PF group and 21% of the control group presented with abnormal (>0.64 cm) leg-length discrepancies. However, small sample sizes and inconsistent reporting of leg-length discrepancy contribute to uncertainty about this risk factor. Messier and Pittala14 found total rearfoot movement (degrees) did not discriminate between PF and control groups. While years running, or running experience, was reported in 5 studies,4,14,19,21,26 it was not included in the meta-analysis because of lack of reporting a standardized definition, control group data, and measures of dispersion. Of the 3 studies that statistically analyzed years running, 1 study4 found participants with PF reported significantly more years running than control participants, while 2 studies14,19 found no difference between the PF group and control groups. The remaining 2 studies21,26 descriptively reported similar time for years running between PF and control groups.
Four studies reported noncontinuous data on medial longitudinal arch/foot type (n = 3),4,24,26 knee alignment (n = 2),4,26 and sex (n = 3)4,16,26 but were sufficiently heterogeneous that pooling was ill-advised. Medial longitudinal arch, or foot type, was determined through static measurements (n = 2),4,26 gait analysis (n = 1),26 or unknown methods (n = 1)24 and categorized as normal, pes cavus, pes planus, and excessive overpronation. In 2 studies, 55% (146/267)26 and 70% (28/40)24 of participants with PF displayed excessive pronation compared with the other foot types.24,26 Conversely, 1 study4 reported that participants with PF more often displayed pes cavus (57%, 24/42) than normal (23%, 26/112) or pes planus (17%, 2/12) foot types. Knee alignment was assessed in 2 studies4,26 by investigators during a static evaluation and categorized as neutral, genu valgum, or genu varum with conflicting results. Di Caprio et al4 reported 48% (22/46) of participants with PF displayed genu varum knee alignment compared with 26% (26/102) neutral and 22% (4/18) genu valgum, whereas Taunton et al26 reported similar percentages of genu valgum and genu varum in participants with PF. Of the 3 studies examining sex as a risk factor, Owens et al16 reported an adjusted odds ratio of 1.85 (95% CI 1.62-2.12), suggesting that female patients were 85% more likely to present with PF than their male counterparts (1.0 adjusted odds ratio). Conversely, Di Caprio et al and Taunton et al24 reported male patients (37%-75%) were affected with PF more than their female counterparts (25%) in their study populations.
Discussion
Of the 11 risk factors analyzed, individuals with increased ankle plantarflexion ROM, BMI, and body mass compared with their noninjured counterparts were more likely to incur PF. Arch height, height, static pronation, training volume, ankle dorsiflexion ROM, and Q-angle were not risk factors for PF. Because of high heterogeneity, it is unclear if dynamic pronation and standing calcaneal angle are risk factors for PF.
Increased plantarflexion ROM was a risk factor for PF. Perhaps a tight triceps surae increases the degree of plantarflexion during the running gait cycle due to the positive correlation between plantar fascia tension and Achilles tendon load.3 Additionally, a positive relationship exists between plantar fascia thickness and Achilles tendon paratenon thickness suggesting that the Achilles tendon could be involved with PF pathology.23 The connection between the plantar fascia and Achilles tendon explains the common focus on the relieving triceps surae tension during plantar fascia treatment.3
In addition to plantarflexion ROM, increased BMI and body mass are both risk factors for PF. Because BMI is a poor indication of body fat in populations such as athletes and military personnel,11,28 these results suggest athletes and military personnel with increased mass relative to their squared height are at greater risk for PF; however, the increased mass could be due to lean mass or fat mass. Interestingly, BMI appears to also be a risk factor for medial tibial stress syndrome in physically active individuals.7 The association of 2 overuse injuries with BMI suggests that individuals with increased BMI and body mass may need slow, steady, and progressive increases in exercise allowing for appropriate adaptation of tissue to loading.
Arch height, height, static pronation, training volume, ankle dorsiflexion ROM, and Q-angle were not risk factors for PF in the meta-analysis. Of these nonrisk factors, the heterogeneity for arch height, height, static pronation, and Q-angle was low, the heterogeneity for training volume low-moderate, and the heterogeneity for ankle dorsiflexion ROM moderate-high. For all these non–risk factors, the mean difference between groups was negligible. In regard to training volume, the risk for PF among individuals who train at various levels is a clinical question often discussed among health care professionals and active individuals alike because of its hypothesized role in overuse injury. Based on the low-moderate heterogeneity of the studies in the meta-analysis, and the inconsistent findings within the individual studies measuring training volume as a risk, the role of training volume on PF risk is uncertain. However, given its practical relevance, studies on how training volume affects PF represents an area of research with strong potential for clinical impact.
Notably, the role of dynamic pronation in PF could not be determined because of high heterogeneity. It is often speculated that overpronation contributes to PF because pronation places greater tension on the plantar fascia.2,24,30 Three articles2,14,18 in the meta-analysis used rearfoot motion during running as indicators of pronation. Pronation is really a triplanar movement composed of subtalar eversion, forefoot abduction, and talocrural dorsiflexion.5 Therefore, the meta-analysis results suggest it is actually increased subtalar, or rearfoot, eversion versus triplanar pronation that remains unknown as a risk factor for PF.
It may be that limited ankle dorsiflexion ROM in individuals with PF is related to a compensatory increase in rearfoot eversion; however, given that the PF participants in the meta-analysis had similar ankle dorsiflexion ROM than non-PF participants, this may help explain why rearfoot motion was not a risk factor for PF.15 Interestingly, in 2 of the systematically reviewed studies not included in the meta-analysis, pronation was measured via qualitative versus quantitative analysis and authors found PF participants were more pronated compared with non-PF participants.24,26 Qualitative analyses may allow observation of the foot in a multisegmented fashion (rearfoot, midfoot, forefoot) versus as 1 rigid segment such as the quantitative measures included in the meta-analysis (rearfoot alone). Research incorporating quantitative measures of the multiple segments of the foot is needed to determine if dynamic pronation is a risk factor or not for PF.15
Limitations of this systematic review and meta-analysis include the lack of consistency in the >100 risk factors reported in the 16 studies, which did not allow for all PF risk factors to be analyzed. The loss of data for the meta-analysis due to disparate methods and reporting of means, measures of variability, and heterogeneity prevented a thorough analysis of many risk factors, which highlights the importance consistent methodology and reporting in original research articles. The quality of reporting, as assessed via the STROBE statement, was quite varied among the 16 observational studies. Last, although the original intent of this article was to capture physically active individuals from various sports and activities, in 5 of the 6 studies included in the meta-analysis, the participants were runners and in 1 study, military personnel, limiting the generalizability of the findings.
Conclusion
In a physically active population, the primary risk factors for PF are increased plantarflexion ROM, BMI, and body mass. A greater degree of plantarflexion ROM, BMI, and body mass appear to place increased tensile load on the force-absorbing structures of the plantar surface of the foot, making them important considerations when creating prevention and treatment programs for PF. Many other potential risk factors for PF exist but were unable to be comprehensively evaluated in this systematic review and meta-analysis because of the heterogeneity of research methods and reporting.
Supplemental Material
Supplemental material, sj-docx-2-sph-10.1177_1941738120970976 for Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis by Karrie L. Hamstra-Wright, Kellie C. Huxel Bliven, R. Curtis Bay and Burcu Aydemir in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-3-sph-10.1177_1941738120970976 for Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis by Karrie L. Hamstra-Wright, Kellie C. Huxel Bliven, R. Curtis Bay and Burcu Aydemir in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-4-sph-10.1177_1941738120970976 for Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis by Karrie L. Hamstra-Wright, Kellie C. Huxel Bliven, R. Curtis Bay and Burcu Aydemir in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-tiff-1-sph-10.1177_1941738120970976 for Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis by Karrie L. Hamstra-Wright, Kellie C. Huxel Bliven, R. Curtis Bay and Burcu Aydemir in Sports Health: A Multidisciplinary Approach
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350:2159-2166. [DOI] [PubMed] [Google Scholar]
- 2. Busseuil C, Freychat P, Guedj EB, Lacour JR. Rearfoot-forefoot orientation and traumatic risk for runners. Foot Ankle Int. 1998;19:32-37. [DOI] [PubMed] [Google Scholar]
- 3. Cheung JT-M, Zhang M, An K-N. Effect of Achilles tendon loading on plantar fascia tension in the standing foot. Clin Biomech (Bristol, Avon). 2006;21:194-203. [DOI] [PubMed] [Google Scholar]
- 4. Di Caprio F, Buda R, Mosca M, Calabro A, Giannini S. Foot and lower limb diseases in runners: assessment of risk factors. J Sports Sci Med. 2010;9:587-596. [PMC free article] [PubMed] [Google Scholar]
- 5. Dugan SA, Bhat KP. Biomechanics and analysis of running gait. Phys Med Rehabil Clin N Am. 2005;16:603-621. [DOI] [PubMed] [Google Scholar]
- 6. Dyck DD, Boyajian-O’Neill LA. Plantar fasciitis. Clin J Sport Med. 2004;14:305-309. [DOI] [PubMed] [Google Scholar]
- 7. Hamstra-Wright KL, Bliven KCH, Bay C. Risk factors for medial tibial stress syndrome in physically active individuals such as runners and military personnel: a systematic review and meta-analysis. Br J Sports Med. 2015;49:362-369. [DOI] [PubMed] [Google Scholar]
- 8. Harutaichun P, Boonyong S, Pensri P. Predictors of plantar fasciitis in Thai novice conscripts after 10-week military training: a prospective study. Phys Ther Sport. 2019;35:29-35. [DOI] [PubMed] [Google Scholar]
- 9. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hossain M, Alexander P, Burls A, Jobanputra P. Foot orthoses for patellofemoral pain in adults. Cochrane Database of Systematic Reviews. 2011;1:CD008402. [DOI] [PubMed] [Google Scholar]
- 11. Kruschitz R, Wallner-Liebmann SJ, Hamlin MJ, et al. Detecting body fat—a weighty problem BMI versus subcutaneous fat patterns in athletes and non-athletes. PLoS One. 2013;8:e72002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lopes AD, Hespanhol Júnior LC, Yeung SS, Costa LOP. What are the main running-related musculoskeletal injuries? A systematic review. Sports Med. 2012;42:891-905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McNeill W, Silvester M. Plantar heel pain. J Bodyw Mov Ther. 2017;21:205-211. [DOI] [PubMed] [Google Scholar]
- 14. Messier SP, Pittala KA. Etiologic factors associated with selected running injuries. Med Sci Sports Exerc. 1988;20:501-505. [PubMed] [Google Scholar]
- 15. Mousavi SH, Hijmans JM, Rajabi R, Diercks R, Zwerver J, van der Worp H. Kinematic risk factors for lower limb tendinopathy in distance runners: a systematic review and meta-analysis. Gait Posture. 2019;69:13-24. [DOI] [PubMed] [Google Scholar]
- 16. Owens BD, Wolf JM, Seelig AD, et al. ; Millennium Cohort Study Team. Risk factors for lower extremity tendinopathies in military personnel. Orthop J Sports Med. 2013;1:2325967113492707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Petraglia F, Ramazzina I, Costantino C. Plantar fasciitis in athletes: diagnostic and treatment strategies. A systematic review. Muscles Ligaments Tendons J. 2017;7:107-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pohl MB, Hamill J, Davis IS. Biomechanical and anatomic factors associated with a history of plantar fasciitis in female runners. Clin J Sport Med. 2009;19:372-376. [DOI] [PubMed] [Google Scholar]
- 19. Ribeiro AP, Sacco ICN, Dinato RC, João SMA. Relationships between static foot alignment and dynamic plantar loads in runners with acute and chronic stages of plantar fasciitis: a cross-sectional study. Braz J Phys Ther. 2016;20:87-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ribeiro AP, Sacco ICN, Dinato RC, João SMA. Relationships between static foot alignment and dynamic plantar loads in runners with acute and chronic stages of plantar fasciitis: a cross-sectional study. Braz J Phys Ther. 2016;20:87-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ribeiro AP, Trombini-Souza F, Tessutti V, Rodrigues Lima F, Sacco I de CN, João SMA. Rearfoot alignment and medial longitudinal arch configurations of runners with symptoms and histories of plantar fasciitis. Clinics (Sao Paulo). 2011;66:1027-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sadat-Ali M. Plantar fasciitis/calcaneal spur among security forces personnel. Mil Med. 1998;163:56-57. [PubMed] [Google Scholar]
- 23. Stecco C, Corradin M, Macchi V, et al. Plantar fascia anatomy and its relationship with Achilles tendon and paratenon. J Anat. 2013;223:665-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Taunton JE, Clement DB, McNicol K. Plantar fasciitis in runners. Can J Appl Sport Sci. 1982;7:41-44. [PubMed] [Google Scholar]
- 25. Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR. Plantar fasciitis: a retrospective analysis of 267 cases. Phys Ther Sport. 2002;3:57-65. [Google Scholar]
- 26. Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500-1524. [DOI] [PubMed] [Google Scholar]
- 28. Venkateshaiah M. Body mass index and its adequacy in capturing body fat. Thai J Physiol Sci. 2007;20:97-100. [Google Scholar]
- 29. Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end.J Stat Softw. 2012;49:1-15. [Google Scholar]
- 30. Warren BL. Anatomical factors associated with predicting plantar fasciitis in long-distance runners. Med Sci Sports Exerc. 1984;16:60-63. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-2-sph-10.1177_1941738120970976 for Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis by Karrie L. Hamstra-Wright, Kellie C. Huxel Bliven, R. Curtis Bay and Burcu Aydemir in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-3-sph-10.1177_1941738120970976 for Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis by Karrie L. Hamstra-Wright, Kellie C. Huxel Bliven, R. Curtis Bay and Burcu Aydemir in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-4-sph-10.1177_1941738120970976 for Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis by Karrie L. Hamstra-Wright, Kellie C. Huxel Bliven, R. Curtis Bay and Burcu Aydemir in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-tiff-1-sph-10.1177_1941738120970976 for Risk Factors for Plantar Fasciitis in Physically Active Individuals: A Systematic Review and Meta-analysis by Karrie L. Hamstra-Wright, Kellie C. Huxel Bliven, R. Curtis Bay and Burcu Aydemir in Sports Health: A Multidisciplinary Approach