Abstract
Context:
Awareness of important injury risk factors associated with excessive pitching volume has been highlighted in the literature, but injury rates remain high. Shoulder pain in baseball players is associated with various changes in musculoskeletal movements, which presents as measurable impairments throughout the kinetic chain. Baseball coaches and rehabilitation professionals have utilized exercise programs targeting strength and flexibility of the throwing arm to prevent injuries. The purpose of this review is to summarize the current evidence regarding the effectiveness of arm care exercise programs in reducing upper extremity injury rates in adolescent baseball players.
Evidence Acquisition:
A search of electronic databases, including CINAHL with full text, MEDLINE, and SPORTDiscus was conducted to retrieve available articles in English from the years 2010 through 2020. The search terms injury prevention, exercise, and adolescent baseball were used.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
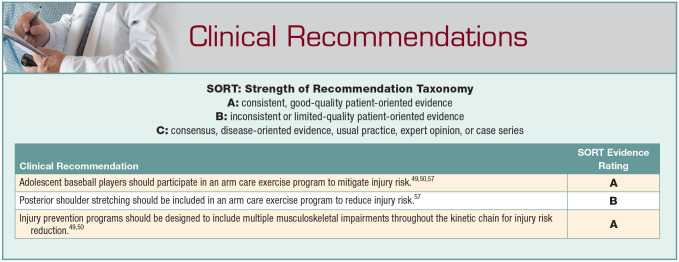
Improving shoulder internal rotation range of motion by stretching the posterior shoulder muscles daily was associated with a 36% risk reduction of shoulder and elbow injuries. Group-based arm care exercise programs that target multiple musculoskeletal impairments demonstrated an approximately 50% reduced risk of elbow injury.
Conclusion:
For adolescent baseball players, arm care injury prevention programs focusing on important musculoskeletal impairments are effective at reducing injury incidence rates. Multimodal injury prevention programs that improve multiple musculoskeletal impairments are more comprehensive and may result in better injury reduction than programs focusing on a singular impairment.
Keywords: arm care, injury prevention program, baseball
The relationship between overhead throwing and upper extremity injury in adolescent baseball players continues to be a concern for health care providers.19,29,32 Nearly 50% of adolescent baseball pitchers report pain in the shoulder or elbow while throwing during the season31 and the frequency of ulnar collateral ligament reconstructions has disproportionately increased in adolescents compared with collegiate or professional level pitchers.21,30 After substantial efforts from researchers, pitching volume has been shown to be a fundamental risk factor for throwing-related injuries.1,28,40,42,51 Despite injury prevention efforts, such as pitching volume reduction, the overall upper extremity injury rate in adolescent baseball players has not been substantially reduced over the past decade. Although, between the 2004-2005 and 2014-2015 seasons, the annual incidence of shoulder injuries declined from 2.07 to 1.39 per 10,000 athletic exposures (AEs) and elbow injuries increased from 0.84 to 1.06 per 10,000 AEs, these trends are not statistically different.52
Although the awareness of important injury risk factors associated with excessive pitching volume has been highlighted, injury rates remain high.15,18 Volume-related risk factors include high pitch counts,14,28,29,37 pitching greater than 8 months per year,40,43 playing on multiple teams,8,37 showcases,8,67 pitching with arm pain or fatigue,29,37,40,64 and throwing greater than 100 innings per season.18 Pitching volume guidelines such as Pitch Smart exist to protect pitchers from overuse and excessive arm fatigue.34 However, compliance rates with these guidelines are typically underwhelming17,24,41,66 and pitch counts have demonstrated inconsistent results in achieving injury risk reduction.2 Thus, solely focusing on pitch volume management is likely not sufficient for effective injury prevention.33
Baseball coaches and sports medicine professionals have recommended and utilized exercise programs targeting strength and flexibility of the throwing arm in an attempt to prevent injuries.12,33,45,58 These arm care exercise programs vary considerably but they follow 4 principles: (1) identify risk factors, (2) define cutoff values for the risk factors based on normative data, (3) assessment and reassessment procedures that are reliable and valid, and (4) preventative exercise programs should be implemented.12
More recently, researchers have begun to investigate if proper management of specific physical impairments could result in injury risk reduction.19,49,50,57,58 Theoretically, managing risk factors could result in decreased injury rates and associated time lost from sport. However, we are not aware of any literature reviews that analyze whether injury prevention programs affect injury rates in adolescent baseball players. Therefore, the purpose of this clinical review is to summarize the current evidence regarding the value of arm care exercise programs at reducing injury incidence in adolescent baseball players.
Arm Care Injury Prevention Programs
Musculoskeletal limitations or inefficiencies throughout the kinetic chain can result in excessive physiological stress in the throwing arm.3,9,53 To address these deficiencies, arm care exercise programs have been developed49,50,57,63 to improve strength, dynamic stability, and range of motion (ROM) of the muscles and joints important to the throwing motion and related to shoulder and elbow health in overhead athletes.63 Historically, arm care exercise programs began as generalized upper body strengthening or targeted stretching to a particular muscle group. More recently, these programs have evolved to target multiple physical impairments throughout the kinetic chain and used screening to individualize program design. However, to date there are a limited number of prospective clinical trials that have explored the effectiveness of arm care exercise programs at reducing injury risk in overhead athletes.49,50,57
Upper Extremity Strengthening
The benefit of including shoulder strengthening exercises in arm care programs for injury risk reduction is unclear in the literature among high level of evidence (LOE) studies.39 In a prospective cohort (LOE 2), Shitara et al56 identified that external rotator weakness, measured as a ratio between dominant and nondominant arms, was associated with up to 7.3 increased odds for injury in high school baseball players. However, other high-quality evidence, 2 LOE 220,48 and 1 LOE 3,59 have not supported decreased absolute shoulder strength or external rotator strength ratio as injury risk factors in adolescent baseball players. According to Sakata et al,48 deficits in external rotation (ER), serratus anterior, or lower trapezius strength ratios were related to elbow injury in youth baseball players. Likewise, Tyler et al59 reported that preseason deficits in shoulder ER, internal rotation (IR), or supraspinatus weakness were unrelated to upper extremity injury in high school baseball players. However, inconsistencies in testing setup position may have contributed to the variation seen in these results. Specifically, Tyler et al measured shoulder ER in a supine position and reported the absolute strength deficit whereas Sakata et al48 and Shitara et al56 measured ER weakness in prone and reported the ratio of ER and IR weakness.
The Thrower’s Ten exercise program is a commonly used shoulder and elbow strengthening program,60,62 which has been recommended as an injury prevention program.13,44,45 The program is based on electromyographic data that implicate specific exercises to best achieve meaningful muscle activation and strengthening of the shoulder girdle and elbow musculature.44,46 The Thrower’s Ten program and more recently the updated Advanced Thrower’s Ten exercise program63 has been found to improve key performance metrics important to baseball pitchers, such as shoulder strength and endurance36 and pitching velocity.16 However, the ability of the Thrower’s Ten to reduce injury risk appears to be unknown. To date, no published studies have investigated injury risk reduction outcomes associated with the Thrower’s Ten or Advanced Thrower’s Ten exercise programs in baseball players. Further research is needed to quantify the degree to which shoulder strength deficits contribute to injury risk and explore if the Thrower’s Ten program can decrease injury incidence in baseball pitchers.
Shoulder Stretching
As one of the most commonly studied areas, shoulder mobility deficits or adaptations to throwing are commonly observed and may be risk factors for injury. Restricted shoulder IR mobility limits energy transfer to the throwing arm during the pitching motion and requires greater effort to maintain throwing velocity, which could increase stress on the upper extremity.10 The presence of glenohumeral internal rotation deficit (GIRD) has been associated with biomechanical faults in high school pitchers, such as larger trunk tilt and less trunk rotation.10 A dominant-side GIRD has been proposed as an injury risk factor in overhead throwers.4,5,23 Shanley et al55 (LOE 2), found that high school baseball players who had GIRD of greater than 25° in their dominant shoulder were at nearly 5 times (risk ratio [RR] 4.8; 95% CI, 2.1-11.3) greater risk for injury. It appears that GIRD may be an important musculoskeletal adaptation in baseball pitchers and proper management with posterior shoulder stretching can reduce upper extremity injury risk.
In a prospective cohort (LOE 2), Shitara et al57 examined the outcome of an injury prevention program in reducing shoulder and elbow injury risk over the course of a competitive baseball season (150 days) in 92 high school baseball pitchers. This study compared the difference in incidences of upper extremity injury defined as ≥8 days of disability between shoulder self-stretching for GIRD and external rotator strengthening for rotator cuff weakness. Stretching the posterior shoulder muscles daily by performing the “sleeper stretch” to improve shoulder IR ROM was associated with a 36% (hazard ratio [HR], 0.355; 95% CI, 0.133-0.947) shoulder and elbow injury risk reduction.57 The overall incidence of shoulder and/or elbow injury for pitchers who performed posterior shoulder stretching compared with pitchers who did not was 25% (n = 8/32) and 57% (n = 8/14), respectively. Additionally, time-to-event analysis showed that pitchers who performed daily sleeper stretching were able to pitch 3 times longer throughout the season compared with those who did not perform daily preventive stretching.57 Although rotator cuff weakness has been suggested as an injury factor for high school pitchers,56,59 Shitara et al57 found that posterior shoulder stretching alone was more effective than the addition of external rotator strengthening at reducing incidence of injury.
Multimodal Group Arm Care Program
More recently, arm care programming has expanded beyond the narrow focus of 1 or 2 injury risk factors by evolving into comprehensive programs that target multiple impairments throughout the entire body. Throwing a baseball is a full-body movement pattern and requires appropriate linkage between the upper and lower body.3 Several studies have evaluated the overhead thrower from a biomechanical perspective and determined that appropriate kinetic linking is necessary for optimal performance and decreased injury risk.3,9,11,35,53 Important musculoskeletal deficits that have been identified as potential injury risk factors for adolescent baseball players include GIRD,55,56 total range of motion (TROM),49 decreased hip IR ROM,49,50 poor thoracic posture,48,49 and deficits in single-leg balance.65 Arm care programs focusing on full body strength and ROM maintenance are likely more advantageous for injury prevention because they address multiple risk factors or impairments.8,40,61
Preventative programs which target multiple known risk factors have shown promise in improving physical impairments and reducing injury rates in youth baseball players.49,50 Two high-quality prospective studies have been published delineating the effectiveness of an injury prevention program in youth baseball players.49,50 In a 2018 nonrandomized controlled trial (LOE 2), Sakata et al49 reported a 49.2% (HR, 50.8%; 95% CI, 0.29-0.88) reduction in the incidence of medial elbow pain in 305 youth baseball players after a preventative program targeting strength and ROM of the shoulders, hips, and spine. The injury prevention program, called the Yokohama Baseball-9 (YKB-9), was performed 2 times per week and consisted of a total of 18 exercises (9 strengthening and 9 stretching) designed to improve multiple risk factors throughout the kinetic chain. Improvement of physical injury risk factors resulted in an incidence of 0.8 per 1000 AEs in the athletes who performed the prevention training compared with 1.7 per 1000 AEs in those who did not participate. Multivariate logistical regression identified improvement in shoulder TROM, decreased thoracic kyphosis angle, and increased lead hip IR ROM as the most important musculoskeletal impairments associated with predicting success in preventing elbow injuries.49 These findings are consistent with other research that has implicated decreased TROM, poor thoracic spine ROM, and limited hip IR ROM as important impairments that could increase risk for injury. In a 2018 systematic review and meta-analysis, Bullock et al4 reported that shoulder TROM less than 160° and asymmetries greater than 10° were both associated with increased injury risk. In an LOE 2 study, an increased thoracic kyphosis angle of greater than 30° was associated with a 2-fold increased risk for injury in youth baseball players.48 Limited hip IR ROM, which seems remote to the throwing shoulder, has also been associated with increased risk for development of medial elbow pain.47,48
In 2019, the original YKB-9 program was modified to be less complex and time intensive. The modified YKB-9 (mYKB-9) program reduced the number of exercises from 18 to 9, but still consisted of (1) stretching for the elbow, shoulder, and hip; (2) dynamic mobility for the scapula and thorax; and (3) lower body balance.50 The effectiveness of the mYKB-9 program was evaluated in a clustered randomized controlled trial (LOE 2) at reducing elbow and shoulder injuries in a cohort of 237 youth baseball players.50 At 12-month follow-up, the incidence of shoulder/elbow injuries was significantly lower in the athletes who completed the mYKB-9 program compared with those who did not participate (HR, 1.94; 95% CI, 1.17-3.2). Specifically, those who did not participate in the mYKB-9 program were nearly 2 times more likely to experience an upper extremity injury. Furthermore, there was a 48.5% reduction in risk for shoulder or elbow injury associated with participating in the mYKB-9 program compared with the control group. This reduction in overuse elbow injury is consistent with the results found by Sakata et al50 in 2019.
Compared with the original YKB-9, the mYKB-9 program, which included half as many exercises, resulted in an overall adherence rate improvement from 57.4% (n = 78/136) to 73.4% (n = 89/109). Additionally, athletes who demonstrated high adherence with the injury prevention program had 0.5 per 1000 AEs incidence of elbow injury compared with 1.2 per 1000 AEs in those who had low adherence.50 The simplification of mYKB-9 program greatly improved adherence while not compromising effectiveness, suggesting that fewer but more targeted exercises can still achieve similar reductions in injury incidence.
Screening for Musculoskeletal Impairments
The arm care exercise programs in this clinical review show promise at reducing injury risk in adolescent baseball players, but the independent risk factors are also important when designing these preventative programs. Researchers have previously studied preseason movement-based screens in high school and collegiate baseball players as a way to predict injury risk.6,7,25 Poor performance on the Functional Movement Screen (FMS) shoulder mobility test was associated with an adjusted odds ratio of 5.14 (95% CI, 1.14-22.9) of having an overuse injury during the preseason.7 Additionally, poor performance on the Selective Functional Movement Assessment upper extremity pattern tests were associated with increased odds of overuse symptoms. Specifically, identified dysfunction in either the unilateral shoulder extension/IR pattern or the unilateral shoulder flexion/ER pattern was associated with an adjusted odds ratio of 6.10 (95% CI, 1.22-30.5) and 17.07 (95% CI, 13.9-210.2) during both the preseason and the competitive season, respectively.7 However, these screening procedures are limited to only the shoulder and do not consider other important musculoskeletal impairments, specifically the thorax, hips, and dynamic balance.
Individualized-Group Arm Care Programs
Injury risk is multifactorial48,49,56 and since each individual baseball player could possess unique impairments, it seems logical to individualize arm care programs to maximize benefit. Shoulder pain in overhead athletes is commonly associated with various musculoskeletal movement changes, which can present as measurable impairments in the upper and lower quarter, but may manifest differently in each player.3,27,54 In general, group-based programs are limited in depth by only focusing on single risk factors or specific injuries.38 The 48.5% injury incidence reduction as seen in mYKB-9 is encouraging, but there still remains room for improvement, as a large proportion of baseball players still sustained an overuse injury.50 Individualized arm care programs could address multiple musculoskeletal impairments such as shoulder strength and ROM, thoracic spine mobility, hip ROM, and balance. Appropriate distribution of exercises based on the need of the player could potentially create a better avenue for greater injury risk reduction.
In an LOE 2 study, Huebner et al22 found that 50% of high school soccer players were able to advance from “high” to “low” risk based on the Move2Perform injury risk categorization algorithm26 after an 8-week individualized injury prevention program. Lehr et al26 validated the Move2Perform software as an injury risk algorithm that takes into consideration current pain, previous injury history, FMS performance, and Y Balance Test–Lower Quarter asymmetries and composite score relative to an individual’s age, gender, and sport. Individuals who were classified into the “high-risk” category were at a 3.4 (RR, 3.4; 95% CI, 2.0-6.0) times increased risk for future injury.26 Using preseason screening, Huebner et al assigned a combination of 3 strengthening and stretching exercises that were performed during the warm-up and cooldown based on the individual’s FMS score. The remaining components of the program consisted of a group-based plyometric, agility, and core training program that was similar for all athletes.22 Interestingly, individuals who reported pain during screening were unlikely to make a categorical improvement. This suggests that when screening produces pain, a group-based program is not individualized enough to reduce injury risk and appropriate referral to a health care provider for a detailed assessment should be considered.
Limitations
This literature review is not without limitations. First, the conclusions of this review are based on the results of the limited number of prospective arm care exercise studies that have evaluated injury incidence reduction as an outcome measure. Although limited in quantity, the studies reviewed demonstrate a high level of evidence and are representative of the current scientific knowledge base in adolescent baseball. Second, individualized group programming has only preliminary evidence on effectiveness and has not been explored in baseball players. Finally, this review focused exclusively on adolescent baseball players. Therefore, the conclusions of this review may not be generalizable to other baseball players at the collegiate or professional level.
Conclusion
For adolescent baseball players, performing arm care exercises for injury prevention that focus on important musculoskeletal impairments are effective at reducing injury incidence rates. Injury prevention programs that focus on a singular musculoskeletal risk factor, such as posterior shoulder stretching, are effective but may not be comprehensive enough to obtain ideal injury reduction because they fail to consider throwing injuries as multifactorial. Adolescent baseball players, especially pitchers, should be encouraged to perform a multimodal arm care exercise program that incorporates localized posterior shoulder stretching and normalizing shoulder TROM, thoracic spine mobility, and hip IR ROM to best prevent throwing-related injury.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Agresta CE, Krieg K, Freehill MT. Risk factors for baseball-related arm injuries: a systematic review. Orthop J Sports Med. 2019;7:2325967119825557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bakshi NK, Inclan PM, Kirsch JM, Bedi A, Agresta C, Freehill MT. Current workload recommendations in baseball pitchers: a systematic review. Am J Sports Med. 2020;48:229-241. [DOI] [PubMed] [Google Scholar]
- 3. Ben Kibler W, Sciascia A. Kinetic chain contributions to elbow function and dysfunction in sports. Clin Sports Med. 2004;23:545-552. [DOI] [PubMed] [Google Scholar]
- 4. Bullock GS, Faherty MS, Ledbetter L, Thigpen CA, Sell TC. Shoulder range of motion and baseball arm injuries: a systematic review and meta-analysis. J Athl Train. 2018;53:1190-1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The “dead arm” revisited. Clin Sports Med. 2000;19:125-158. [DOI] [PubMed] [Google Scholar]
- 6. Busch AM, Clifton DR, Onate JA. Relationship of movement screens with past shoulder or elbow surgeries in collegiate baseball players. Int J Sports Phys Ther. 2018;13:1008-1014. [PMC free article] [PubMed] [Google Scholar]
- 7. Busch AM, Clifton DR, Onate JA, Ramsey VK, Cromartie F. Relationship of preseason movement screens with overuse symptoms in collegiate baseball players. Int J Sports Phys Ther. 2017;12:960-966. [PMC free article] [PubMed] [Google Scholar]
- 8. Chalmers PN, Sgroi T, Riff AJ, et al. Correlates with injury in youth and adolescent pitchers. Orthop J Sports Med. 2015;3(3suppl):2325967115S2325900005. [Google Scholar]
- 9. Chalmers PN, Wimmer MA, Verma NN, et al. The relationship between pitching mechanics and injury: a review of current concepts. Sports Health. 2017;9:216-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chou PP, Chou YL, Wang YS, Wang RT, Lin HT. Effects of glenohumeral internal rotation deficit on baseball pitching among pitchers of different ages. J Shoulder Elbow Surg. 2018;27:599-605. [DOI] [PubMed] [Google Scholar]
- 11. Chu SK, Jayabalan P, Kibler WB, Press J. The kinetic chain revisited: new concepts on throwing mechanics and injury. PM R. 2016;8(3suppl):S69-S77. [DOI] [PubMed] [Google Scholar]
- 12. Cools AM, Johansson FR, Borms D, Maenhout A. Prevention of shoulder injuries in overhead athletes: a science-based approach. Braz J Physi Ther. 2015;19:331-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Erbaugh Franz C, Hall-Bibb D, Stockdale M, Thompson A, Biggs B. Elbow injury prevention in youth Dominican baseball players: a training intervention pilot study. Int J Allied Health Sci Pract. 2019;17:Article 6. [Google Scholar]
- 14. Erickson BJ, Chalmers PN, Axe MJ, Romeo AA. Exceeding pitch count recommendations in Little League Baseball increases the chance of requiring Tommy John surgery as a professional baseball pitcher. Orthop J Sports Med. 2017;5:2325967117695085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Erickson BJ, Nwachukwu BU, Rosas S, et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43:1770-1774. [DOI] [PubMed] [Google Scholar]
- 16. Escamilla RF, Ionno M, deMahy MS, et al. Comparison of three baseball-specific 6-week training programs on throwing velocity in high school baseball players.J Strength Cond Res. 2012;26:1767-1781. [DOI] [PubMed] [Google Scholar]
- 17. Fazarale JJ, Magnussen RA, Pedroza AD, Kaeding CC, Best TM, Classie J. Knowledge of and compliance with pitch count recommendations: a survey of youth baseball coaches. Sports Health. 2012;4:202-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Fleisig GS, Andrews JR, Cutter GR, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. Am J Sports Med. 2011;39:253-257. [DOI] [PubMed] [Google Scholar]
- 19. Greenberg EM, Lawrence JTR, Fernandez-Fernandez A, et al. Physical and functional differences in youth baseball players with and without throwing-related pain. Orthop J Sports Med. 2017;5:2325967117737731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Harada M, Takahara M, Mura N, Sasaki J, Ito T, Ogino T. Risk factors for elbow injuries among young baseball players. J Shoulder Elbow Surg. 2010;19:502-507. [DOI] [PubMed] [Google Scholar]
- 21. Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of medial ulnar collateral ligament reconstruction: a 10-year study in New York State. Am J Sports Med. 2016;44:729-734. [DOI] [PubMed] [Google Scholar]
- 22. Huebner BJ, Plisky PJ, Kiesel KB, Schwartzkopf-Phifer K. Can injury risk category be changed in athletes? An analysis of an injury prevention system. Int J Sports Phys Ther. 2019;14:127-134. [PMC free article] [PubMed] [Google Scholar]
- 23. Keller RA, De Giacomo AF, Neumann JA, Limpisvasti O, Tibone JE. Glenohumeral internal rotation deficit and risk of upper extremity injury in overhead athletes: a meta-analysis and systematic review. Sports Health. 2018;10:125-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Knapik DM, Continenza SM, Hoffman K, Gilmore A. Youth baseball coach awareness of pitch count guidelines and overuse throwing injuries remains deficient. J Pediatr Orthop. 2018;38:e623-e628. [DOI] [PubMed] [Google Scholar]
- 25. Lee CL, Hsu MC, Chang WD, et al. Functional movement screen comparison between the preparative period and competitive period in high school baseball players. J Exerc Sci Fitness. 2018;16:68-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lehr ME, Plisky PJ, Butler RJ, Fink ML, Kiesel KB, Underwood FB. Field-expedient screening and injury risk algorithm categories as predictors of noncontact lower extremity injury. Scand J Med Sci Sports. 2013;23:e225-e232. [DOI] [PubMed] [Google Scholar]
- 27. Lintner D, Noonan TJ, Kibler WB. Injury patterns and biomechanics of the athlete’s shoulder. Clin Sports Med. 2008;27:527-551. [DOI] [PubMed] [Google Scholar]
- 28. Lyman S, Fleisig GS, Andrews JR, Osinski ED. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463-468. [DOI] [PubMed] [Google Scholar]
- 29. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33:1803-1810. [DOI] [PubMed] [Google Scholar]
- 30. Mahure SA, Mollon B, Shamah SD, Kwon YW, Rokito AS. Disproportionate trends in ulnar collateral ligament reconstruction: projections through 2025 and a literature review. J Shoulder Elbow Surg. 2016;25:1005-1012. [DOI] [PubMed] [Google Scholar]
- 31. Makhni EC, Morrow ZS, Luchetti TJ, et al. Arm pain in youth baseball players: a survey of healthy players. Am J Sports Med. 2014;43:41-46. [DOI] [PubMed] [Google Scholar]
- 32. McFarland EG, Ireland ML. Rehabilitation programs and prevention strategies in adolescent throwing athletes. Instr Course Lect. 2003;52:37-42. [PubMed] [Google Scholar]
- 33. Melugin HP, Leafblad ND, Camp CL, Conte S. Injury prevention in baseball: from youth to the pros. Curr Rev Musculoskelet Med. 2018;11:26-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. MLB. Major League Baseball. Pitch Smart. Published 2014. Accessed October 6, 2019. https://www.mlb.com/pitch-smart/pitching-guidelines
- 35. Mlynarek RA, Lee S, Bedi A. Shoulder injuries in the overhead throwing athlete. Hand Clin. 2017;33:19-34. [DOI] [PubMed] [Google Scholar]
- 36. Myers NL, Toonstra JL, Smith JS, Padgett CA, Uhl TL. Sustained isometric shoulder contraction on muscular strength and endurance: a randomized clinical trial. Int J Sports Phys Ther. 2015;10:1015-1025. [PMC free article] [PubMed] [Google Scholar]
- 37. Norton R, Honstad C, Joshi R, Silvis M, Chinchilli V, Dhawan A. Risk factors for elbow and shoulder injuries in adolescent baseball players: a systematic review. Am J Sports Med. 2019;47:982-990. [DOI] [PubMed] [Google Scholar]
- 38. Noyes FR, Barber Westin SD. Anterior cruciate ligament injury prevention training in female athletes: a systematic review of injury reduction and results of athletic performance tests. Sports Health. 2012;4:36-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. Published 2011. Accessed May 15, 2020. http://www.cebm.net/index.aspx?o=5653 [Google Scholar]
- 40. Olsen SJ, 2nd, Fleisig GS, Dun S, Loftice J, Andrews JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905-912. [DOI] [PubMed] [Google Scholar]
- 41. Pamias-Velázquez KJ, Figueroa-Negrón MM, Tirado-Crespo J, Mulero-Portela AL. Compliance with injury prevention measures in youth pitchers: survey of coaches in Little League of Puerto Rico. Sports Health. 2016;8:274-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Popchak A, Burnett T, Weber N, Boninger M. Factors related to injury in youth and adolescent baseball pitching, with an eye toward prevention. Am J Phys Med Rehabil. 2015;94:395-409. [DOI] [PubMed] [Google Scholar]
- 43. Pytiak AV, Stearns P, Bastrom TP, et al. Are the current Little League pitching guidelines adequate? A single-season prospective MRI study. Orthop J Sports Med. 2017;5:2325967117704851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Reinold MM, Escamilla RF, Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39:105-117. [DOI] [PubMed] [Google Scholar]
- 45. Reinold MM, Gill TJ, Wilk KE, Andrews JR. Current concepts in the evaluation and treatment of the shoulder in overhead throwing athletes, part 2: injury prevention and treatment. Sports Health. 2010;2:101-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Reinold MM, Macrina LC, Wilk KE, et al. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. J Athl Train. 2007;42:464-469. [PMC free article] [PubMed] [Google Scholar]
- 47. Saito M, Kenmoku T, Kameyama K, et al. Relationship between tightness of the hip joint and elbow pain in adolescent baseball players. Orthop J Sports Med. 2014;2:2325967114532424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sakata J, Nakamura E, Suzukawa M, Akaike A, Shimizu K. Physical risk factors for a medial elbow injury in junior baseball players: a prospective cohort study of 353 players. Am J Sports Med. 2017;45:135-143. [DOI] [PubMed] [Google Scholar]
- 49. Sakata J, Nakamura E, Suzuki T, et al. Efficacy of a prevention program for medial elbow injuries in youth baseball players. Am J Sports Med. 2018;46:460-469. [DOI] [PubMed] [Google Scholar]
- 50. Sakata J, Nakamura E, Suzuki T, et al. Throwing injuries in youth baseball players: can a prevention program help? A randomized controlled trial. Am J Sports Med. 2019;47:2709-2716. [DOI] [PubMed] [Google Scholar]
- 51. Salamh P, Jones E, Bashore M, Liu X, Hegedus EJ. Injuries and associated risk factors of the shoulder and elbow among adolescent baseball pitchers: a systematic review and meta-analysis. Phys Ther Sport. 2020;43:108-119. [DOI] [PubMed] [Google Scholar]
- 52. Saper MG, Pierpoint LA, Liu W, Comstock RD, Polousky JD, Andrews JR. Epidemiology of shoulder and elbow injuries among United States high school baseball players: school years 2005-2006 through 2014-2015. Am J Sports Med. 2018;46:37-43. [DOI] [PubMed] [Google Scholar]
- 53. Scarborough DM, Bassett AJ, Mayer LW, Berkson EM. Kinematic sequence patterns in the overhead baseball pitch. Sports Biomech. 2020;19:569-586. [DOI] [PubMed] [Google Scholar]
- 54. Sciascia A, Kibler WB. The pediatric overhead athlete: what is the real problem? Clin J Sport Med. 2006;16:471-477. [DOI] [PubMed] [Google Scholar]
- 55. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med. 2011;39:1997-2006. [DOI] [PubMed] [Google Scholar]
- 56. Shitara H, Kobayashi T, Yamamoto A, et al. Prospective multifactorial analysis of preseason risk factors for shoulder and elbow injuries in high school baseball pitchers. Knee Surg Sports Traumatol Arthroscopy. 2017;25:3303-3310. [DOI] [PubMed] [Google Scholar]
- 57. Shitara H, Yamamoto A, Shimoyama D, et al. Shoulder stretching intervention reduces the incidence of shoulder and elbow injuries in high school baseball players: a time-to-event analysis. Sci Rep. 2017;7:45304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Trakis JE, McHugh MP, Caracciolo PA, Busciacco L, Mullaney M, Nicholas SJ. Muscle strength and range of motion in adolescent pitchers with throwing-related pain: implications for injury prevention. Am J Sports Med. 2008;36:2173-2178. [DOI] [PubMed] [Google Scholar]
- 59. Tyler TF, Mullaney MJ, Mirabella MR, Nicholas SJ, McHugh MP. Risk factors for shoulder and elbow injuries in high school baseball pitchers: the role of preseason strength and range of motion. Am J Sports Med. 2014;42:1993-1999. [DOI] [PubMed] [Google Scholar]
- 60. Wilk KE, Andrews JR, Arriigo CA. Preventive and Rehabilitative Exercises for the Shoulder and Elbow. 5th ed. American Sports Medicine Institute; 1997. [Google Scholar]
- 61. Wilk KE, Arrigo CA, Hooks TR, Andrews JR. Rehabilitation of the overhead throwing athlete: there is more to it than just external rotation/internal rotation strengthening. PM R. 2016;8(3suppl):S78-S90. [DOI] [PubMed] [Google Scholar]
- 62. Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30:136-151. [DOI] [PubMed] [Google Scholar]
- 63. Wilk KE, Yenchak AJ, Arrigo CA, Andrews JR. The Advanced Throwers Ten Exercise Program: a new exercise series for enhanced dynamic shoulder control in the overhead throwing athlete. Phys Sportsmed. 2011;39(4):90-97. [DOI] [PubMed] [Google Scholar]
- 64. Yang J, Mann BJ, Guettler JH, et al. Risk-prone pitching activities and injuries in youth baseball: findings from a national sample. Am J Sports Med. 2014;42:1456-1463. [DOI] [PubMed] [Google Scholar]
- 65. Yukutake T, Nagai K, Yamada M, Aoyama T. Risk factors for elbow pain in Little League baseball players: a cross-sectional study focusing on developmental factors. J Sports Med Phys Fitness. 2015;55:962-968. [PubMed] [Google Scholar]
- 66. Yukutake T, Yamada M, Aoyama T. A survey examining the correlations between Japanese Little League baseball coaches’ knowledge of and compliance with pitch count recommendations and player elbow pain. Sports Health. 2013;5:239-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Zabawa L, Alland JA. Association between parental understanding of Pitch Smart guidelines and youth baseball player injuries. Orthop J Sports Med. 2019;7:2325967119846314. [DOI] [PMC free article] [PubMed] [Google Scholar]


