Abstract
Negative stereotypes about pre-exposure prophylaxis (PrEP) hinder PrEP uptake among young men who have sex with men (YMSM). Prior research suggests community homophobia may be linked to negative PrEP attitudes. Conversely, individuals with high gay community attachments (GCA) may have more access to credible PrEP information/resources. Among 285 YMSM recruited online, we estimated structural equation models to test competing conceptual models that inform pathways from perceived stigmas, GCA, and negative PrEP stereotype endorsements to PrEP uptake. In Model A, perceived stigma was directly associated with PrEP uptake, partially mediated by stereotype endorsement (β = − 0.05; 95% CI [− 0.09, − 0.01]) and GCA (β = − 0.06; 95% CI [− 0.11, 0.02]). In Model B, perceived stigma was associated with PrEP uptake (β = − 0.07; 95% CI [− 0.14, − 0.01]) through stereotype endorsement among high GCA YMSM. Complemented by anti-stigma initiatives, PrEP outreach for YMSM should utilize sex-positive messaging and disentangle negative PrEP stereotypes within gay-centric social spaces.
Keywords: Young gay and bisexual men, PrEP stigma, Gay community, Sexual health, HIV
Resumen
Los estereotipos negativos sobre la profilaxis pre-exposición (PrEP) dificultan su uso entre hombres jóvenes que tienen sexo con otros hombres (YMSM). Investigaciones anteriores sugieren que la homofobia comunitaria puede estar relacionada a las actitudes negativas sobre PrEP. En cambio, personas con alto apego a la comunidad gay (GCA) pueden tener más acceso a información y recursos creíbles sobre PrEP. Entre los 285 YMSM reclutados en línea, estimamos varios modelos de ecuaciones estructurales para contrastar las asociaciones entre los estigmas percibidos, la GCA, los estereotipos negativos sobre PrEP, y el uso de PrEP entre diversos modelos conceptuales. En el Modelo A, el estigma percibido se asoció directamente con el uso de PrEP, siendo parcialmente mediado por el endoso a estereotipos (β = − 0.05; IC del 95% [− 0.09, − 0.01]) y GCA (β = − 0.06; IC del 95% [− 0.11, 0.02]). En el Modelo B, el estigma percibido se asoció con el uso de PrEP (β = − 0.07; IC del 95% [− 0.14, − 0.01]) a través de los estereotipos entre YMSM con puntajes altos en GCA. Complementado con iniciativas contra el estigma, el alcance de la PrEP para YMSM debe utilizar mensajes de sexo positivo y desenredar los estereotipos negativos de PrEP dentro de los espacios sociales centrados en la comunidad gay.
Introduction
Pre-exposure prophylaxis (PrEP), a daily oral combination antiretroviral commercially offered as Truvada (emtricitabine and tenofovir disoproxil fumarate) or Descovy (emtricitabine and tenofovir alafenamide; not approved in the contexts of receptive vaginal intercourse), is a highly effective biomedical prevention strategy for populations disproportionately affected by the HIV epidemic [1–3]. Although high adherence to PrEP drastically reduces an individual’s risk of HIV seroconversion if exposed to the virus via sexual contact or drug use [4, 5], HIV prevention experts continue to be challenged by incremental increases in PrEP uptake by young men who have sex with men (YMSM) in the United States [6, 7]. Youth 13 to 24 years of age still account for 21% of new HIV cases, most of which are attributed to male-to-male sexual contact and more specifically, among those from racial/ethnic minority backgrounds [8, 9]. Annual infection rates have decreased by only six percent since 2010 among youth 13 to 24 years of age who were assigned male sex at birth. Recent surveillance efforts continue to exhibit increasing trends in the proportion of YMSM 18–24 years of age who report engaging in condomless anal intercourse (CAI) with conservative (i.e., lower-limit) estimates, suggesting that close to half of YMSM reported recent CAI (e.g., at last sexual intercourse; within the past year) [10–12]. Even more concerning, a recent study observed that among PrEP-eligible YMSM who are engaged in healthcare, just over half who discussed PrEP with a provider reported PrEP uptake. These data suggest that local strategies to improve PrEP uptake among YMSM are not being maximized and underscore the need for ongoing efforts to identify and intervene on YMSM’s barriers to PrEP access and adoption [13, 14].
HIV prevention experts and community leaders met the initial rollout of PrEP with mixed responses toward its use [15]. Prior to the approval of PrEP, messages around HIV prevention focused on YMSM limiting their sexual activity, number of sexual partners, and occasions of CAI [16]. Though considered a sexual health promotion strategy, resistance to PrEP uptake by high-profile HIV organizations has been well documented [17]. These organizations reported fears that PrEP uptake would motivate risk compensation in communities disproportionately affected by the HIV epidemic [18]. Specifically, some organizational leaders forecasted that PrEP uptake would facilitate less condom use and potentially result in perceptions of decreased susceptibility to HIV infection among men who have sex with men (MSM). Yet, in subsequent studies, researchers have observed limited evidence for adopting risk compensation behaviors among community samples of PrEP-using MSM compared to those without a prescription [19–22]. Nevertheless, PrEP stigmatization—that is, negative judgment cast on individuals who use PrEP [16]—persists among YMSM and those within the HIV prevention community [23]. Manifestations of PrEP stigma (e.g., perpetuating negative PrEP stereotypes and belief in subsequent risk compensation), especially among health care providers, can damage the uptake of PrEP among YMSM by minimizing opportunities to openly discuss HIV risk behaviors and limiting YMSM’s access to PrEP itself [24].
While researchers have observed substantial awareness of negative PrEP stereotypes among YMSM in prior studies, few have assessed the extent to which these youth endorse or ascribe to these beliefs [25, 26]. Negative PrEP stereotypes have arisen similarly to stereotypes that equated MSM with HIV with being sexually promiscuous and engaging in high-risk behaviors [25, 27, 28]. This parallel suggests that YMSM who have experienced or integrated negative community attitudes toward MSM or individuals living with HIV, may attribute similar beliefs to PrEP use. Despite awareness of negative PrEP stereotypes, MSM remain the predominant consumer base of the medication [29]; however, the extent to which negative PrEP stereotypes are linked to age-related inequity, particularly for those 25 and younger, in access and adoption warrant further investigation.
Urban-dwelling MSM may be integral to understanding how YMSM formulate attitudes, opinions, and motivations toward PrEP use [30, 31]. YMSM who have largely integrated themselves into, or have a greater attachment to, MSM networks are more likely to have friends who are PrEP consumers [32]. PrEP consumers may serve as ambassadors for PrEP by raising awareness, sharing personal reasons for use, relaying experiences they have had with using PrEP, and even providing recommendations for navigating PrEP medical care [33]. In fact, a prior study that assessed the social capital (i.e., access to social resources) contexts of HIV care found that among persons living with HIV, living in high social participation neighborhoods were associated with higher prevalence rates of HIV linkage-to-care [34]. However, the extent to which social participation, specifically via gay community attachment, is linked to PrEP uptake is poorly understood. In prior studies, researchers have frequently examined gay community attachment as predictors or mediators in assessments of social stressors and HIV-related outcomes [35–38]. While insightful, YMSM’s attachments and connectedness to their larger and local gay communities may contextualize how psychosocial factors (e.g., perceived stigma), sexual health-related experiences (e.g., exposure to PrEP), and their relationships manifest, suggesting gay community attachment as a moderator [30, 39]. Specifically, the social and psychosocial theoretical mechanisms that underlie access to PrEP may differ based on individual YMSM’s level of gay community attachment.
To address these gaps, we sought to characterize the extent to which YMSM in a high-HIV prevalence Mid-Atlantic urban corridor endorse negative stereotypes about MSM who use PrEP and reported lifetime PrEP uptake. The Mid-Atlantic corridor of Philadelphia, Baltimore, and Washington, DC reflects three priority jurisdictions identified in the Ending the HIV Epidemic by 2030 initiative for scaling up HIV prevention strategies, including PrEP rollout [40]. Additionally, we developed two competing conceptual models (Fig. 1) to test how YMSM’s PrEP stereotype endorsement levels are linked to PrEP uptake in the contexts of perceived community stigmas and that attend to potential differences in the role of gay community attachment. In Model A, we conceptualized YMSM’s perceived community stigmas to be associated with PrEP uptake through gay community attachment and subsequently through the endorsement of negative PrEP stereotypes. More specifically, we consider a potential direct link between gay community attachment and endorsement of negative PrEP stereotypes given prior findings that highlight positive peer networks’ role in sexual health promotion [41]. In Model B, we conceptualized gay community attachment as a moderator for the associations that perceived community stigmas have with PrEP uptake through PrEP stereotype endorsement. Specifically, the associations that perceived community stigmas and endorsements of negative PrEP stereotypes have with PrEP uptake may differ by gay community attachment levels. Gay communities serve as formal (e.g., functional support) and informal social support (e.g., appraisal support through community norms) resources that may thwart the contributions of negative factors on YMSM’s adoption of sexual health promotion strategies [30, 39]. The hypotheses for each model (Fig. 1) are listed as follows:
Fig. 1.
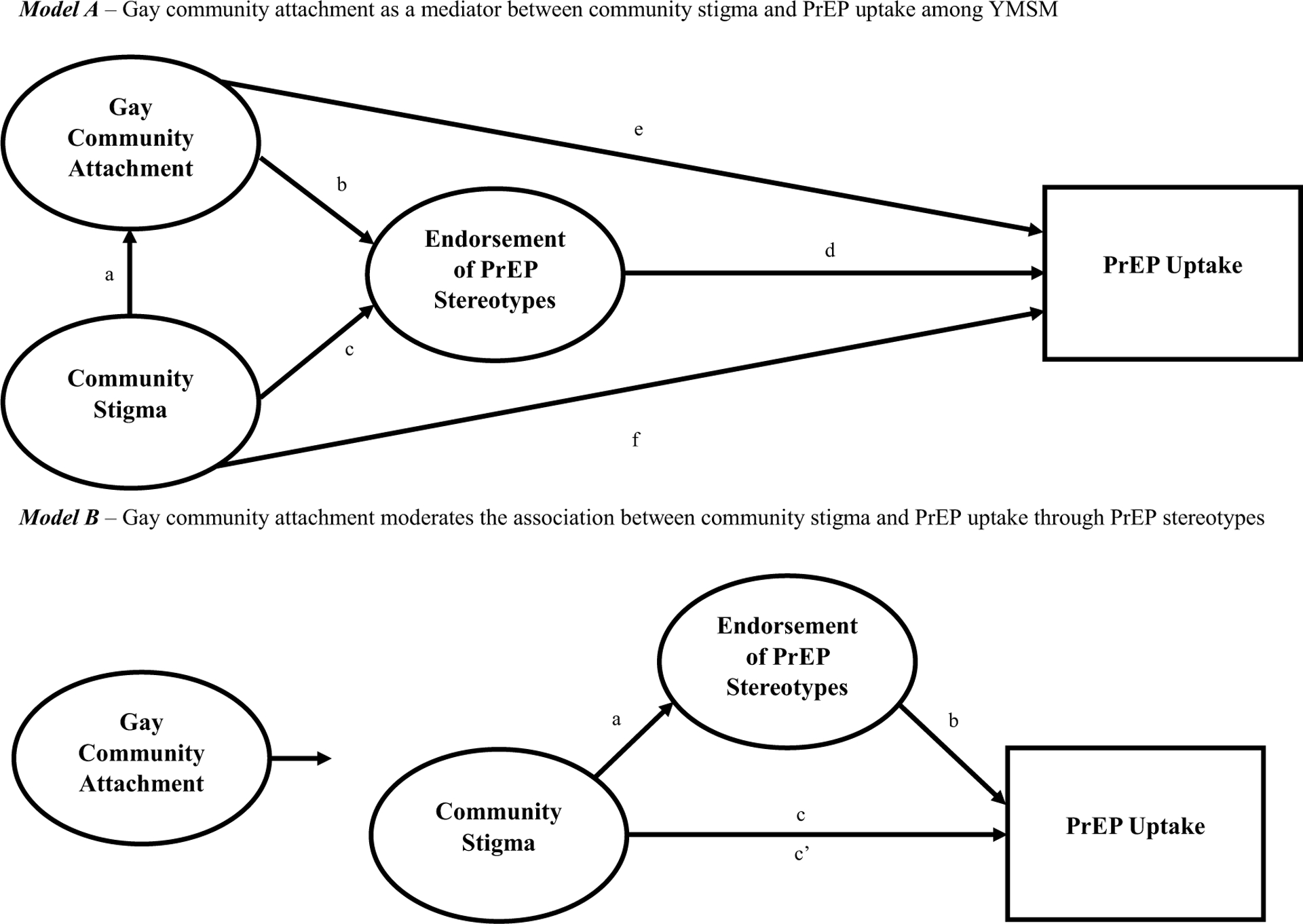
Competing conceptual models. Model A gay community attachment as a mediator between community stigma and PrEP uptake among YMSM. Model B gay community attachment moderates the association between community stigma and PrEP uptake through PrEP stereotypes
Model A
Hypothesis [H]1: Gay community attachment will exhibit a direct, positive association (path e), whereas endorsement of negative PrEP stereotypes (path d) and perceived community stigmas (HIV and homophobia; path f) will have a direct, negative association with YMSM’s PrEP uptake.
H2: Gay community attachment (path b) and perceived community stigmas (path c) will have an inverse and positive association with endorsement levels of negative PrEP stereotypes, respectively.
H3: Perceived community stigmas will have a positive association with negative PrEP stereotype endorsement through gay community attachment (path a * b).
H4: Perceived community stigmas will be negatively associated with gay community attachment, which in turn will be negatively associated with endorsement of negative PrEP stereotypes (path a * e).
H5: Perceived stigmas will be negatively associated with PrEP uptake through endorsement levels of negative PrEP stereotypes (path c * d).
H6: Endorsement of negative PrEP stereotypes will mediate the associations that gay community attachment and perceived stigmas have with YMSM’s PrEP uptake (path a * b * d).
Model B
H7: Gay community attachment would moderate the association between perceived stigmas and PrEP uptake through PrEP stereotype endorsement (path a * b), with the association being weaker for YMSM with high gay community attachment compared to YMSM with low levels of gay community attachment.
Methods
Procedures
This study’s data come from a cross-sectional, observational study examining YMSM’s PrEP uptake, social and community networks, and risk behaviors in a disproportionately HIV-affected region in the Mid-Atlantic. Participants were recruited from Grindr and Facebook between October 2018 and February 2019. Participants were eligible if they identified as a cisgender male, were 18–25 years old, self-reported as HIV-negative or HIV status unaware, had sex with a man in the past 6 months, and reported a residential zip code along the Philadelphia (PA), Baltimore (MD), or Washington (DC) metropolitan corridor. Those who completed an electronic informed consent were directed to complete a confidential web-survey, which lasted between 20 and 30 min. Participants were compensated with a $10 Amazon e-gift card for their time. Participants’ responses were protected within a University of Pennsylvania firewalled server. Study procedures were reviewed and approved by the University of Pennsylvania Institutional Review Board.
To prevent duplicate and falsified entries, we monitored the duplication of email and I.P. addresses and crosschecked I.P. addresses with the zip codes and residential addresses/cross-streets provided by participants [42]. Of the 1287 attempted web-survey entries, we removed cases in which prospective participants did not complete the screener survey (n = 585, 45.5%), were ineligible (n = 207, 16.1%), consented, but did not complete the survey (n = 112, 8.7%), and provided duplicate/falsified entries (n = 93, 7.2%). These exclusions yielded an analytic sample of N = 290 YMSM (72.1% completion rate) in the Mid-Atlantic United States. We then conducted a missing-cases analysis and found that only five participants, which included those who had never heard of PrEP, provided incomplete responses to our variables of interest. Given this small number, we employed listwise deletion and removed these cases from our analysis, yielding a final analytic sample of N = 285 YMSM.
Measures
PrEP Uptake
Participants were asked a single item of whether they had ever taken PrEP before a sexual or drug use exposure to reduce the risk of getting HIV. Responses included: (1) Yes, I am on PrEP right now; (2) Yes, I have in the past, but I’m not on PrEP anymore; and (3) No, I have never taken PrEP. Those who reported being on PrEP or having taken PrEP in the past were collapsed to create a dichotomous variable for lifetime PrEP uptake (0 = No lifetime PrEP uptake; 1 = Any lifetime PrEP uptake).
Endorsement of Negative PrEP Stereotypes
We adopted a seven-item scale on community support for PrEP (e.g., “Men who have sex with men taking PrEP are being reckless”) to examine participants’ endorsement of negative PrEP stereotypes [43]. Items were assessed on a 4-point scale (0 = Strongly disagree, 3 = Strongly agree); positively worded items were reverse-coded (e.g., “Men who have sex with men taking PrEP are being responsible”). The seven items yielded high internal consistency (Cronbach’s alpha = 0.79). We developed a mean score of the items with higher scores reflecting greater endorsement levels and lower scores reflecting lower endorsement levels.
Gay Community Attachment
We included four items assessing gay community attachment (“I feel that I am part of my area’s LGBT community,” “Participating in my area’s LGBT community is a positive thing for me,” “I feel a bond with the LGBT community,” and “I am proud of my area’s LGBT community”). These items were presented on a 4-point scale (0 = Strongly disagree, 3 = Strongly agree) and exhibited high internal consistency (Cronbach’s alpha = 0.86). The four items were averaged together, with higher scores indicating greater gay community attachment.
Community Stigma
We included measures of perceived community stigmas given prior research that argues a parallel development between stigma toward MSM, persons living with HIV, and those who use PrEP. For Perceived Sexual Prejudice and Perceived HIV Stigma, we adapted the seven items of the Perceptions of Local Stigma scale to each construct (e.g., “Most people in my area think poorly of a(n) [man who has sex with men/HIV-positive person]”) [44]. These items were offered on a 4-point scale (0 = Strongly disagree, 3 = Strongly agree) and positively-worded items were reverse-coded. The seven items demonstrated high internal consistency for perceived community homophobia (Cronbach’s alpha = 0.91) and perceived HIV stigma (Cronbach’s alpha = 0.87). Items for each construct were averaged together with high scores indicating high perceived stigma.
Sociodemographic Characteristics and Other Covariates
Participants self-reported their age, race/ethnicity (0 = Non-Hispanic White; 1 = Racial/Ethnic Minority [inclusive of Non-Hispanic Black, Hispanic/Latino—All Races, and Other or Multiple Races/Ethnicities due to low variance]), sexual identity (0 = Gay, queer, same-gender loving, or homosexual; 1 = Other MSM identity [inclusive of bisexual and pansexual due to low variance]), HIV status (0 = Negative, 1 = Unknown or Unaware), Relationship status (0 = Single, 1 = In a Monogamous Relationship, 2 = In a Non-monogamous Relationship), Education level (0 = Less than college degree; 1 = College degree or higher), and employment status (0 = Full-Time, 1 = Part-Time, 2 = Unemployed). Participants’ self-reported residential zip codes were recoded to reflect their home metropolitan area (0 = Baltimore, 1 = Philadelphia, 2 = Washington, DC). Lastly, participants were asked to report the number of sexual partners they had in which they did not use condoms as the insertive (i.e., top) and receptive (i.e., bottom) partner, respectively. We summed these values and then dichotomized the variable given its Poisson distribution to reflect participants who engaged in no condomless anal intercourse (0) and those who engaged in any (1) condomless anal intercourse (CAI) in the past 3 months.
Data Analytic Strategies
To characterize participants’ endorsement of negative PrEP stereotypes and PrEP uptake, we first generated a descriptive account of YMSM’s sociodemographic characteristics, PrEP behaviors, parallel community stigmas, and gay community attachment. We tested bivariate associations (chi-square, t-tests, Pearson’s correlation) comparing differences in the endorsement of negative PrEP stereotypes and PrEP uptake by indicators of social participation (e.g., gay community attachment), parallel community stigmas (e.g., perceived sexual prejudice and HIV stigma), sociodemographic characteristics, and recent CAI.
To test our first conceptual model (Model A: Hypotheses 1–6), we developed structural equation models (SEM) using Mplus 8.0 [45] to test the direct and indirect pathways connecting PrEP stereotype endorsement, stigma, and gay community attachment to YMSM’s lifetime PrEP use. SEM permits simultaneous examination of pathways with endogenous latent variables (e.g., perceived community stigma, gay community attachment, and endorsement of negative PrEP stereotypes) [46]. Moreover, parceling, a technique to reduce the structural parameter bias by summing several items together, was used to explain stigma. We used parceling methods to produce fewer parameters, which produce stable parameter estimates and better model fit [47]. The parallel stigma factor is explained by two sub-factors: perceived community homophobia and HIV stigma. The seven items in each sub-factor were randomly categorized into two parcels: a 3-item parcel and a 4-item parcel. Therefore, four parcels served as indicators under stigma instead of using two sub-factors.
In addition, we included theoretically accepted modifications in the final model by allowing correlations and used robust weighted least squares (WLSMV) due to binary outcome [48]. With WLSMV, the probit regression was employed on the path with a binary outcome, and linear regression was utilized on the path with a latent continuous outcome. Indirect effects including a path with a binary outcome were interpreted as probit regression coefficients. The size of the indirect effect was estimated by the product of the effect of the independent variable on the mediator and the effect of the mediator on the dependent variable. The direct effect is the effect of the independent variable on the dependent variable controlling for the effect of the mediator [49]. We present our findings based on four goodness of fit indices: comparative fit index (CFI), Tucker-Lewis Index (TLI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA). Hu and Bentler suggested values of 0.90 or higher for CFI and TLI, a value of 0.08 or lower for SRMR, and a value of 0.06 or lower for RMSEA represents acceptable fit [50].
To test the second conceptual model (Model B: Hypothesis 7), we repeated these steps for a stratified sub-analysis, assessing the indirect effects of parallel community stigmas on lifetime PrEP use through endorsement levels of negative PrEP stereotypes by separating the sample into sub-groups based on participants’ levels of gay community attachment (low versus high). Stratified models provide an opportunity to assess effect modification when theoretical frameworks include hypotheses that specify how social circumstances (e.g., gay community attachment) may contribute to all or multiple pathways in the model [51, 52]. Given the range of the gay community attachment variable (mean scores between 1 and 4), we conducted a median split to classify participants as having low gay community attachment if they had a mean score between 1 and 2.49 (n = 111; 38.9%) and classify participants as having high gay community attachment if they had a mean score between 2.50 and 4 (n = 174, 61.1%).
Results
Participants
A summary of participant characteristics is provided in detail in Table 1. The mean age of participants was 22.18 years (standard deviation, sd = 2.15). Participants were predominantly Non-Hispanic White (n = 185, 64.9%) with smaller numbers of Non-Hispanic Black (n = 23, 8.1%), Hispanic/Latino (All races; n = 40, 14.0%), and Other and Multiple Races/Ethnicities (n = 37, 13.0%). Most participants identified as gay, queer, same-gender loving, or homosexual (n = 230, 80.7%).
Table 1.
Participant characteristics, N = 285
| Variable | n (%) | m (sd) |
|---|---|---|
| Age, range 18–25 | 22.20 (2.13) | |
| Race/ethnicity | ||
| Non-Hispanic White | 185 (64.9) | |
| Non-Hispanic Black | 23 (8.1) | |
| Hispanic/Latino all races | 40 (14.0) | |
| Other race or multiracial | 37 (13.0) | |
| Sexual identity | ||
| Gay, queer, same-gender loving, or homosexual | 230 (80.7) | |
| Other MSM identity | 55 (19.3) | |
| HIV status | ||
| Negative | 255 (89.5) | |
| Unknown or unaware | 30 (10.5) | |
| Relationship status | ||
| Single | 185 (64.9) | |
| In a relationship, monogamous | 51 (17.9) | |
| In a relationship, non-monogamous | 49 (17.2) | |
| Education level | ||
| Less than college degree | 119 (41.8) | |
| A college degree or higher | 166 (58.2) | |
| Employment status | ||
| Unemployed | 74 (26.0) | |
| Part-time | 78 (27.4) | |
| Full-time | 133 (46.6) | |
| Metropolitan area | ||
| Baltimore | 51 (17.9) | |
| Philadelphia | 110 (38.6) | |
| Washington, DC | 124 (43.5) | |
| Recent condomless anal intercourse | ||
| None | 76 (26.7) | |
| Any | 209 (73.3) | |
| Gay community attachment, range 1–4 | 2.76 (0.73) | |
| Stigma: perceived community homophobia, range 1–4 | 1.90 (0.58) | |
| Stigma: perceived community HIV stigma, range 1–4 | 2.44 (0.55) | |
| Endorsement of PrEP stereotypes, range 1–4 | 1.93 (0.60) | |
| Lifetime PrEP use | ||
| None | 182 (63.9) | |
| Any | 103 (36.1) |
Most YMSM self-reported an HIV-negative status (n = 255, 89.5%), Over half of the sample identified as single (n = 185, 64.9%) and reported engaging in any CAI in the past 3 months (n = 209; 73.3%). On average, participants reported moderate to high gay community attachment (m = 2.76, sd = 0.73, range 1–4), and moderate levels of perceived stigma (community homophobia m = 1.90, sd = 0.58, range 1–4; community HIV stigma m = 2.44, sd = 0.55, range 1–4).
Endorsement of Negative PrEP Stereotypes
Our sample exhibited, on average, a moderate level of PrEP stereotype endorsement (m = 1.93, sd = 0.60, range 1–4). Bivariate tests (Table 2) demonstrated that racial/ethnic minority participants had higher endorsements of negative PrEP stereotypes compared to Non-Hispanic White participants (t = − 2.11, p = 0.036). YMSM who reported any lifetime PrEP use on average, had less endorsement of negative PrEP stereotypes than those with no prior PrEP use (t = 2.38, p = 0.018). Participants who reported any recent CAI on average, reported less endorsement of PrEP stigma, compared to those who reported no recent CAI (t = 2.72, p = 0.007). Age (r = − 0.16, p = 0.006) was negatively correlated with endorsement of negative PrEP stereotypes. Of the two stigma variables, only perceived community homophobia was positively correlated with the endorsement of negative PrEP stereotypes (r = 0.19, p = 0.002). We observed no bivariate differences in stereotype endorsement by sexual identity, HIV status, relationship status, education level, employment status, metro area, gay community attachment, or perceived community HIV stigma.
Table 2.
Endorsement of PrEP stereotypes and PrEP uptake by sample characteristics among YMSM, N = 285
| Endorsement of negative PrEP stereotypes | PrEP uptake (0: Never [n = 182, 63.9%], 1: Any [n= 103, 36.1%]) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uptake = 0 | Uptake = 1 | Uptake = 0 | Uptake = 1 | χ2 | t | p | ||||||
| Variable | m (sd) | t | F | r | p | n (%) | n (%) | m (sd) | m (sd) | |||
| Age | −0.16 | 0.008 | 21.69 (2.09) | 23.10 (1.91) | −5.63 | < 0.001 | ||||||
| Race/ethnicity | ||||||||||||
| Non-Hispanic White | 1.87 (0.61) | −2.11 | 0.036 | 110 (59.5) | 75 (40.5) | 4.42 | 0.035 | |||||
| Racial minority | 2.03 (0.59) | 72 (72.0) | 28 (28.0) | |||||||||
| Sexual identity | ||||||||||||
| Gay, queer or homosexual | 1.90 (0.60) | −1.66 | 0.098 | 138 (60.0) | 92 (40.0) | 7.69 | 0.006 | |||||
| Other MSM identity | 2.05 (0.62) | 44 (80.0) | 11 (20.0) | |||||||||
| HIV status | ||||||||||||
| Negative | 1.92 (0.60) | −0.98 | 0.327 | 154 (60.4) | 101 (39.6) | 12.62 | < 0.001 | |||||
| Unknown or unaware | 2.03 (0.65) | 28 (93.3) | 28 (93.3) | |||||||||
| Relationship status | ||||||||||||
| Single | 1.91 (0.61) | 0.48 | 0.621 | 118 (63.8) | 67 (36.2) | 12.12 | 0.002 | |||||
| In a relationship, monogamous | 2.01 (0.53) | 41 (80.4) | 10 (19.6) | |||||||||
| In a relationship, non-monogamous | 1.92 (0.67) | 23 (46.9) | 26 (53.1) | |||||||||
| Education level | ||||||||||||
| Less than college degree | 1.99 (0.62) | 1.47 | 0.143 | 93 (78.2) | 26 (21.8) | 18.08 | <0.001 | |||||
| A college degree or higher | 1.89 (0.59) | 89 (53.6) | 77 (46.4) | |||||||||
| Employment status | ||||||||||||
| Unemployed | 1.97 (0.70) | 1.61 | 0.202 | 52 (70.3) | 22 (29.7) | 24.18 | < 0.001 | |||||
| Part-time | 2.01 (0.54) | 64 (82.1) | 14 (17.9) | |||||||||
| Full-time | 1.86 (0.58) | 66 (49.6) | 67 (50.4) | |||||||||
| Metropolitan area | ||||||||||||
| Baltimore | 2.01 (0.66) | 0.68 | 0.508 | 68 (54.8) | 56 (45.2) | 8.94 | 0.011 | |||||
| Philadelphia | 1.90 (0.60) | 81 (73.6) | 29 (26.4) | |||||||||
| Washington, DC | 1.92 (0.59) | 33 (64.7) | 18 (35.3) | |||||||||
| Recent condomless anal intercourse | ||||||||||||
| None | 2.10 (0.65) | 2.72 | 0.007 | 61 (80.3) | 15 (19.7) | 12.08 | 0.001 | |||||
| Any | 1.88 (0.58) | 121 (57.9) | 88 (42.1) | |||||||||
| Gay community attachment | −0.08 | 0.175 | 2.63 (0.69) | 2.99 (0.75) | −4.09 | < 0.001 | ||||||
| Stigma: perceived comm. homophobia | 0.19 | 0.002 | 2.00 (0.59) | 1.72 (0.51) | 4.08 | < 0.001 | ||||||
| Stigma: perceived comm. HIV stigma | 0.09 | 0.129 | 2.49 (0.57) | 2.36 (0.52) | 1.94 | 0.053 | ||||||
| Endorsement of PrEP stereotypes | 1.99 (0.61) | 1.82 (0.58) | 2.38 | 0.018 | ||||||||
| Lifetime PrEP uptake | ||||||||||||
| None | 1.99 (0.61) | 2.38 | 0.018 | |||||||||
| Any | 1.82 (0.58) | |||||||||||
PrEP Uptake
Over one-third (n = 103; 36.1%) of participants reported lifetime PrEP uptake. Bivariate tests (Table 2) indicated that PrEP uptake was associated with older age (t = − 5.63, p < 0.001), being Non-Hispanic White compared to racial/ethnic minority YMSM (χ2 = 4.42, p = 0.035), identifying as gay compared to another MSM identity (χ2 = 7.69, p = 0.006), higher education (χ2 = 18.08, p < 0.001), and being full-time employed (χ2 = 24.18, p < 0.001). A greater proportion of participants who had ever taken PrEP reported being in non-monogamous relationships or identified as single compared to those who were currently in monogamous relationships (χ2 = 12.12, p = 0.002). Similarly, a greater proportion of participants who reported any recent CAI also reported any lifetime PrEP uptake compared to participants who reported no recent CAI (χ2 = 12.08, p = 0.001). PrEP uptake was associated with higher levels of gay community attachment (t = − 4.09, p < 0.001), lower perceived community homophobia (t = 4.08, p < 0.001), and lower endorsement of negative PrEP stereotypes (t = 2.38, p = 0.018). Perceived community HIV stigma approached, but did not achieve statistical significance in its association with PrEP uptake (t = 1.94, p = 0.053).
Structural Equation Models
The final SEM results are presented in Table 3 and Figs. 2 (Model A) and 3 (Model B).
Table 3.
Parameter estimates for final mediation model
| Path | Estimates | 95% CI |
|---|---|---|
| Model with gay community attachment as a mediatora | ||
| Perceived community stigma → stereotype endorsement | ||
| Direct effect (c) | 0.21* | 0.08, 0.34 |
| Indirect effect (a * b) | 0.02 | −0.02,0.05 |
| Gay community attachment →PrEP uptake | ||
| Direct effect (e) | 0.25* | 0.11,0.40 |
| Indirect effect (b * d) | 0.02 | −0.01,0.04 |
| Perceived community stigma →PrEP uptake | ||
| Direct effect (f) | −0.19* | −0.36,−0.02 |
| Total indirect effect | −0.11* | −0.17,−0.05 |
| Indirect effect (c * d) | −0.05* | −0.09,−0.01 |
| Indirect effect (a * e) | −0.06* | −0.11,−0.02 |
| Indirect effect (a * b * d) | −0.004 | −0.01,0.004 |
| Model with gay community attachment as a moderatorb—low gay community attachment | ||
| Perceived community stigma →stereotype endorsement | ||
| Direct effect (c) | −0.11 | −0.38,0.16 |
| Total indirect effect (a * b) | −0.03 | −0.09,0.02 |
| Model with gay community attachment as a moderatorb—high gay community attachment | ||
| Perceived community stigma → stereotype endorsement | ||
| Direct effect (c) | −0.26* | −0.47,−0.06 |
| Total indirect effect (a * b) | −0.07* | −0.13,−0.01 |
Fig. 2.
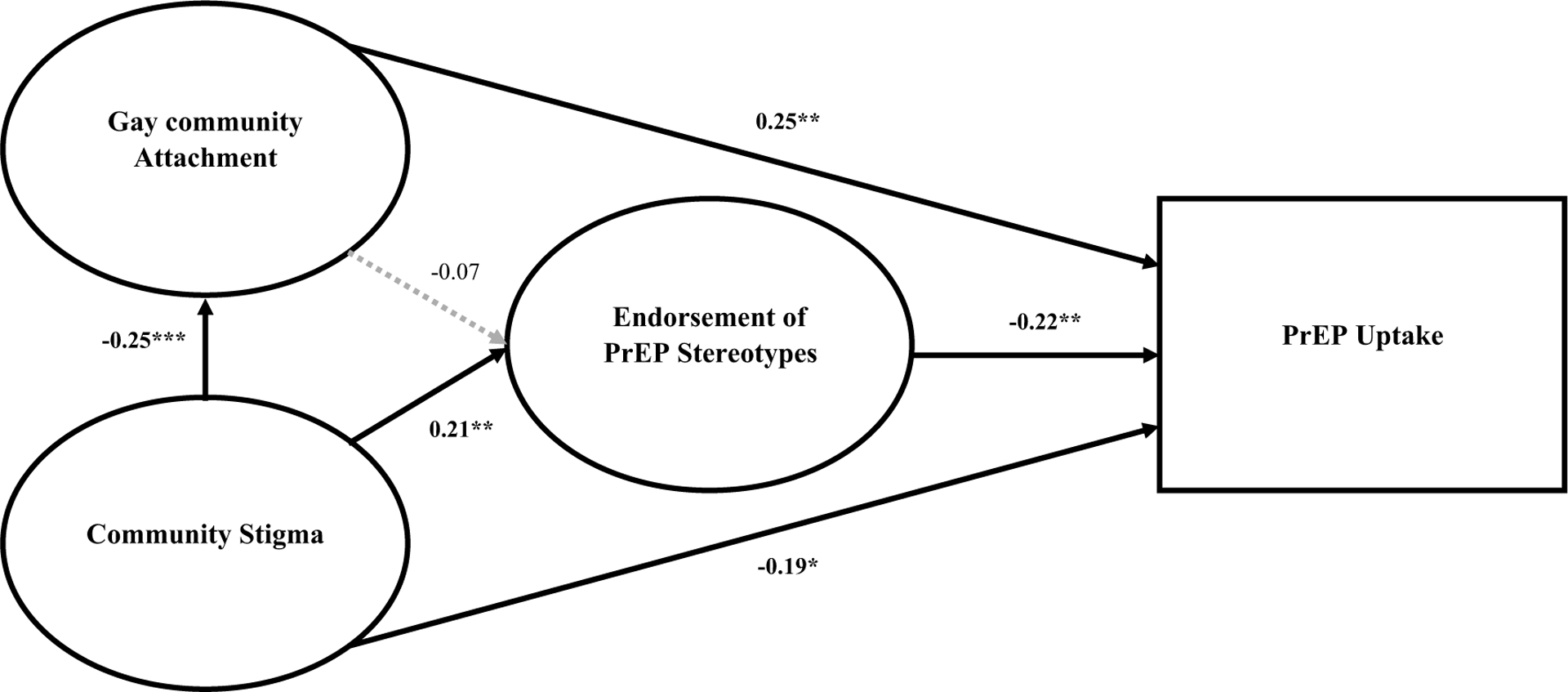
Structural equation model with gay community attachment as a mediator adjusted for age, race/ethnicity, sexual identity, employment status, relationship status, and condomless anal intercourse
Fig. 3.
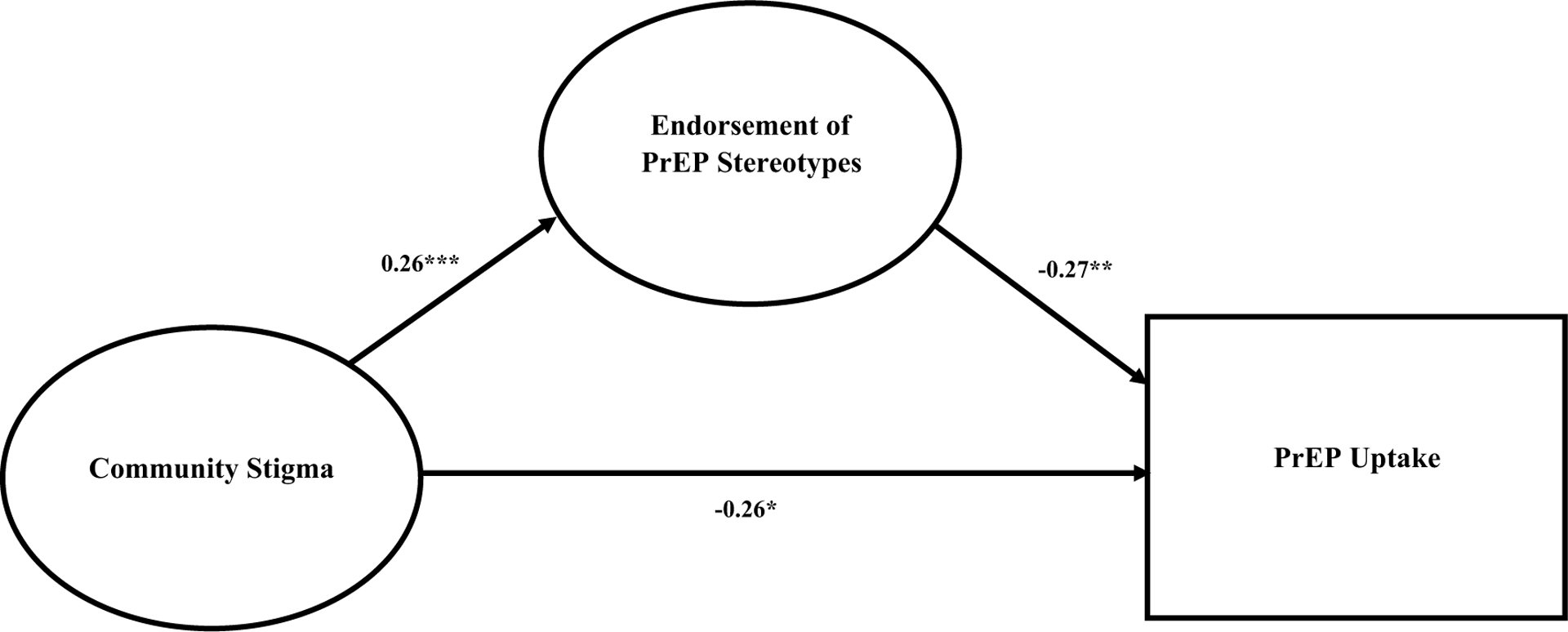
Structural equation model for YMSM with high gay community attachment adjusted for age, race/ethnicity, sexual identity, employment status, relationship status, and condomless anal intercourse
Model A
The final SEM model was adjusted for age, race/ethnicity, sexual identity, employment status, relationship status, and recent CAI (CFI = 0.94; TLI = 0.93; SRMR = 0.08; RMSEA = 0.06 [CI = 0.05, 0.07]). As shown in Fig. 2, greater perceived community stigmas were associated with greater endorsement of negative PrEP stereotype (path c: β = 0.21; 95% CI [0.08, 0.34]; p = 0.002) and less attachment to gay community (path a: β = − 0.25; 95% CI [− 0.37, − 0.13]; p < 0.001). However, there was no significant associations between gay community attachment and endorsement of negative PrEP stereotype (path b: β = − 0.07; 95% CI [− 0.19, 0.06]; p = 0.30). In addition, greater attachment to the gay community was associated with lifetime PrEP use (path e: β = 0.25; 95% CI [0.11, 0.40]; p = 0.001), while greater endorsement to negative PrEP stereotypes (path d: β = − 0.22; 95% CI [− 0.37, − 0.08]; p = 0.002) and greater perceived community stigma (path f: β = − 0.19; 95% CI [− 0.36, − 0.02]; p = 0.03) were associated with no life time PrEP use.
Indirect effects of perceived community stigma on the endorsement of negative PrEP stereotypes through gay community attachments were not statistically significant (path a * b: β = 0.02; 95% CI [− 0.02, 0.05]; p = 0.32). In addition, the indirect effect of gay community attachment on lifetime PrEP use through the endorsement of negative PrEP stereotype was not statistically significant (path b * d: β = 0.02; 95% CI [− 0.01, 0.04]; p = 0.32). However, the total indirect effect of perceived community stigma on PrEP uptake was statistically significant (β = − 0.11; 95% CI [− 0.17, − 0.05]; p < 0.001). The relationship between stigma and PrEP uptake was partially mediated by endorsement of negative PrEP stereotype and gay community attachment. Specifically, YMSM who perceived greater community stigma were more likely to endorse negative PrEP stereotype which in turn was negatively associated with PrEP uptake (path c * d: β = − 0.05; 95% CI [− 0.09, − 0.01]; p = 0.03). Additionally, YMSM who reported greater stigma reported less gay community attachment, which was inversely associated with lifetime PrEP use (path a * e: β = − 0.06; 95% CI [− 0.11, − 0.02]; p = 0.01). Among covariates, age (β = 0.41; 95% CI [0.28, 0.53]; p < 0.001), being in a non-monogamous relationship as opposed to being single (β = 0.19; 95% CI [0.06, 0.33]; p = 0.005), and reporting any recent CAI (β = 0.27; 95% CI [0.13, 0.41]; p < 0.001) were positively associated with PrEP uptake. Racial/ethnic minority identity (β = − 0.16; 95% CI [− 0.31, − 0.02]; p = 0.03), identifying as Other sexual identity as opposed to gay or homosexual (β = − 0.23; 95% CI [− 0.38, − 0.08]; p = 0.003), part-time (β = − 0.41; 95% CI [− 0.57, − 0.24]; p < 0.001) and unemployment/student (β = − 0.25; 95% CI [− 0.42, − 0.08]; p = 0.004) compared to full-time, and being a non-monogamous relationship compared to those who identified as single (β = − 0.22; 95% CI [− 0.37, − 0.08]; p = 0.003) remained negatively associated with PrEP uptake.
Model B
We observed no statistically significant pathways linking perceived community stigmas and endorsement of negative PrEP stereotypes among participants who reported low levels of gay community attachment (n = 111, 38.9%). However, among these men, age (β = 0.31; 95% CI [0.09, 0.52]; p = 0.01) and any recent CAI (β = 0.52; 95% CI [0.28, 0.77]; p < 0.001) were positively associated, and being in a monogamous relationship compared to being single (β = − 0.30; 95% CI [− 0.57, − 0.03]; p = 0.03) was negatively associated with PrEP uptake (CFI = 0.95; TLI = 0.94; SRMR = 0.09; RMSEA = 0.05 [CI = 0.02, 0.07]). Among YMSM who reported high levels of gay community attachment (n = 174, 61.1%), the association between perceived community stigmas and lifetime PrEP uptake was partially mediated by endorsement levels of negative PrEP stereotypes (path a * b: β = − 0.07; 95% CI [− 0.13, − 0.01]; p = 0.03) after adjusting for age, race/ethnicity, sexual identity, relationship status, employment status, and recent CAI (CFI = 0.90; TLI = 0.87; SRMR = 0.10; RMSEA = 0.08 [CI = 0.06, 0.09]). In this model, greater stigma was positively associated endorsement of negative PrEP stereotype (path a: β = 0.26; 95% CI [0.10, 0.41]; p = 0.001), which was inversely associated with PrEP uptake (path b: β = − 0.27; 95% CI [− 0.44, − 0.09]; p = 0.003). There was a statistically significant, negative direct effect between perceived community stigmas and PrEP uptake (path c: β = − 0.26; 95% CI [− 0.47, − 0.06]; p = 0.01). Among covariates, age (β = 0.43; 95% CI [0.28, 0.59]; p < 0.0001), being in a non-monogamous relationship as opposed to being single (β = 0.18; 95% CI [0.01, 0.34]; p = 0.04), and reporting any recent CAI (β = 0.20; 95% CI [0.02, 0.37]; p = 0.03) were positively associated with PrEP uptake. Racial/ethnic minority identity (β = − 0.20; 95% CI [− 0.38, − 0.01]; p = 0.04), identifying as Other sexual identity as opposed to gay or homosexual (β = − 0.25; 95% CI [− 0.44, − 0.06]; p = 0.01), being a monogamous relationship compared to those who identified as single (β = − 0.18; 95% CI [− 0.36, − 0.004]; p = 0.05), and part-time employment (β = − 0.53; 95% CI [− 0.72, − 0.34]; p < 0.001), and unemployment/student (β = − 0.27; 95% CI [− 0.50, − 0.05]; p = 0.02) compared to full-time employment remained negatively associated with PrEP uptake.
Discussion
Our study’s goal was to characterize YMSM’s endorsement of negative stereotypes about PrEP and how these attitudes are linked to lifetime PrEP use. We found moderate levels of endorsement of negative PrEP stereotypes among the study cohort and a connection between negative PrEP stereotype endorsement and lower uptake with PrEP. Consistent with prior studies, our results highlight how negative stereotypes attributed to PrEP use remain an ongoing barrier to YMSM’s PrEP uptake [16, 26]. These findings pose negative PrEP stereotypes as potential challenges to PrEP rollout efforts in the Mid-Atlantic region where local initiatives have increased the availability and accessibility of PrEP (e.g., financial/co-pay assistance programs, PrEP clinic locators). Despite these initiatives, negative PrEP stereotypes may inhibit many YMSM, especially those who would benefit the most from the medication, from seeking and initiating PrEP. However, the extent to which negative stereotypes interact with awareness and consumption of PrEP-related initiatives warrant further exploration.
We observed support for our hypothesis that stigma was directly and positively associated with endorsing negative PrEP stereotypes. These findings suggest that continued and scaled-up anti-homophobic and HIV-related stigma interventions may be critical to disentangling negative PrEP-related stereotypes and improving PrEP uptake. Many YMSM who have never used PrEP, however, reported no or low endorsement of negative stereotypes, underscoring that there remain alternative and multilevel barriers to PrEP linkage-to-care and uptake that must be addressed to increase PrEP adoption [53, 54]. Given that youth reflect only 11% of current PrEP users [13], our findings advocate for multilevel interventions to improve PrEP initiation among YMSM.
We found support for our hypothesis that higher scores on gay community attachment would be directly associated with lifetime PrEP use. Participants were recruited predominantly from urban metropolitan areas known for having queer-centric and lesbian, gay, bisexual, transgender, and queer (LGBTQ)-friendly spaces (e.g., “gayborhoods”) [55–57]. YMSM in these areas are not only more likely to have encountered many MSM who are currently on PrEP compared to those living in areas with limited queer communities, but these youth may also have access and exposure to a greater variety (i.e., in-person) sexual health or PrEP-affirming messages [58, 59]. However, our hypothesis that PrEP stereotype endorsements would mediate the association between gay community attachment and PrEP use was not supported by the data. In fact, our analysis suggests that gay community attachment operated as a moderator in the model. In our stratified analysis (Fig. 1 Model B), we observed negative associations between PrEP use and stigma and PrEP stereotype endorsement, respectively, among YMSM who reported high gay community attachment levels. We did not observe this relationship among YMSM with low levels of gay community attachment. These findings align with prior studies pointing to the complex role of gay community attachment and connectedness as sources of both risk and resilience with regard to sexual health [37, 59]. One possible interpretation of this finding may be that highly-attached/connected YMSM who perceive more stigma may have less evolved conceptualizations of sexual risk, particularly in light of newer biomedical HIV prevention modalities. These YMSM may be more critical of their peers’ self-expressions of sexuality and sexual behaviors with greater attention to how their networks’ behaviors align with negative PrEP stereotypes. YMSM may forego linkage-to-PrEP to distance themselves from negative PrEP-related stereotypes, similar to how many individuals from other marginalized backgrounds (e.g., racial/ethnic minorities) minimize threats of stigmatization by behaving in a way that distances themselves from pervasive stereotypes [60]. Studies that aim to explore the mechanisms by which YMSM tap into social network resources to overcome negative attitudes and beliefs about PrEP are needed to inform PrEP interventions in queer-centric spaces and neighborhoods.
Beyond our hypotheses, our findings provide insight into sociodemographic and behavioral differences in endorsement of negative PrEP stereotypes and PrEP uptake. Though researchers have described PrEP-related stigma and stereotyping experiences among racial/ethnic minority MSM, few have informed the extent to which MSM from communities of color hold stereotyped beliefs [21, 61, 62]. Our findings indicate that endorsement levels of negative PrEP stereotypes were higher among racial/ethnic minority participants than their Non-Hispanic counterparts. These data are particularly concerning as racial/ethnic minority YMSM, particularly Black and Latino YMSM, are disproportionately affected by the HIV epidemic in the region [63]. Furthermore, our findings support prior research that has exhibited limited PrEP uptake in younger age groups, racial and ethnic minority men who have sex with men (MSM) compared to Non-Hispanic White MSM, and in socio-economic disadvantaged communities [3, 64, 65]. We also found that participants’ relationship statuses were associated with PrEP uptake indicating YMSM who were single or in non-monogamous relationships were more likely to report ever using PrEP. However, relationship status was a self-reported measure that does not imply behavior (e.g., YMSM who have consensually agreed to non-monogamy but have not engaged in sexual intercourse with a non-main partner), and prior studies have argued that relationship monogamy statuses are not static among MSM populations [66, 67]. Participants who reported recent CAI were more likely to report PrEP uptake than those who did not, which suggests that PrEP efforts in the region, despite low uptake, are reaching those who are likely to benefit from the medicine. Our measure of CAI, however, was limited to the past three months; therefore, we advocate for ongoing surveillance to assess how YMSM navigate sexual risk and sexual health promotion over time.
Our study’s findings underscore the need to support future research in this area. Prevention experts seeking to unpack the role of negative PrEP stereotypes on PrEP adoption should aim to explore who within high-risk YMSM’s social networks have the strongest influence, both positively and negatively, to elicit effective sexual health promotion. Identifying network members with whom YMSM consider trustworthy informational resources about PrEP may be integral to capitalizing on these resources to minimize PrEP misinformation [68]. Furthermore, our measurement of gay community attachment reflects YMSM’s psychological affiliations to the gay community, thereby providing limited insight into their social integration within physical gay spaces and the interactions or conversations that occur between one another related to sexual health (e.g., general positivity, advocating, and altruistic motivations). While gay communities often serve as a sexuality-affirming resource for many YMSM [69, 70], personal attachments do not necessarily convey community trustworthiness or the idiosyncratic norms that arise from one’s active, social involvement [71, 72]. This disconnect limits how we understand ingroup communication pathways for stigmatizing attitudes, beliefs, and stereotypes, warranting further investigation.
Furthermore, psychological attachments to the gay community fail to capture whether YMSM know who in their network, if any, are taking or have ever taken PrEP. On the one hand, knowing the extent to which individuals in one’s network have taken PrEP may elicit descriptive norms in YMSM that promote positive beliefs about or motivations to seek PrEP. Similarly, intergroup contact theory suggests that increased contact with members of stigmatized statuses reduces intergroup prejudice [73]; therefore, linking positive attributions to PrEP use may be facilitated more easily among YMSM who are connected to PrEP-consuming peers. Qualitative accounts may be informative to understanding how individual and network attitudes toward PrEP emerge and whether MSM networks provide various types of PrEP-related social support (e.g., raising awareness, information on with whom to talk to about PrEP).
Another potential factor that may inform the theoretical pathways that community stigmas, gay community attachment, and PrEP stereotypes have with PrEP uptake in future studies is internalized homonegativity. In a recent study, internalized homonegativity was associated with being in earlier stages along the PrEP continuum among YMSM [74]. Elevated levels of internalized homonegativity may exacerbate the direct association that perceived community stigmas have with PrEP uptake. Internalized homonegativity may also inform the extent to which YMSM create psychological and physical attachments to the gay community, thereby limiting potential and critical resources for sexual health-related social support [75]. Necessary support may include informational support from peers who facilitate acquiring facts that dispel myths and misinformation about PrEP.
Additional studies may also shed light on how YMSM perceive their PrEP-using peers and whether these perceptions inform their PrEP beliefs. Alternatively, our participants may also be more involved in discussing PrEP with network members outside of the gay community that they have identified as credible health resources (e.g., family members, community leaders, medical providers, and HIV prevention organizations) [76]. Identifying trusted resources for health information, especially in queer-centric neighborhoods, may inform the development of interventions that foster more open, honest, and productive conversations about sexual health and biomedical HIV prevention.
Our study’s findings provide implications for interventions that aim to reduce PrEP stigma and motivate PrEP uptake in YMSM. Several PrEP interventions and strategies continue to emerge to facilitate PrEP uptake, including peer-navigation services and locator tools to help interested individuals identify local PrEP providers [77, 78]; however, these initiatives must be complemented by strategies that counter against social barriers like PrEP stigma and negative stereotypes. Interventions aiming to reduce negative PrEP stereotypes must lean on strategies that promote encouraging or favorable PrEP discussions within MSM social networks and within other networks through which MSM navigate their sexual health (e.g., health providers and familial networks). Mass media campaigns have historically been integral to eliciting productive community conversations in HIV prevention and treatment [79]. Though local health campaigns have facilitated the production of positive PrEP norms (e.g., #PrEP4Love campaign), HIV implementation experts must scale up PrEP messages to be sex-positive, combat negative stereotypes, link PrEP use to altruistic motivations (i.e., keeping those in one’s sexual networks safe), and culturally resonate with local YMSM [80, 81]. Capitalizing on resources like social media and partner-seeking mobile applications may be critical for disseminating credible information and building skills to discuss PrEP within YMSM’s social networks. However, these interventions must also address sexuality (and perhaps HIV) stigmas, given their parallel attributions to negative PrEP stereotypes.
Lastly, while our findings provided important insight into the role of PrEP stereotypes and PrEP use among YMSM, our study had several limitations. First, our results are unlikely generalizable given that our sample’s catchment area was the Mid-Atlantic Corridor of the US, which despite high HIV prevalence also exhibits greater PrEP uptake than regions in the nation like the Deep South [13]. Therefore, participants’ responses may differ from other YMSM living in other areas across the country. Second, we recruited using Grindr and Facebook advertisements. It remains unclear whether YMSM who do not use these two social media platforms have different perspectives about PrEP. Third, our study’s recruitment materials explicitly referenced sexual health, which may have led to selection bias of young men who are already highly educated about PrEP, resulting in limited variability regarding participants’ perceptions of their peers’ PrEP attitudes and discussions. Fourth, our sample had limited variation in race/ethnicity, education level, and HIV status (negative versus unaware/unknown). This limited our capacity to perform within-group differences beyond two categories and yielding potential Type II errors [82]. Similar analyses should be conducted in samples from other communities of YMSM to explore the dynamics of negative PrEP stereotypes in other settings and populations. Additionally, we were unable to ascertain reasons or motivations for taking PrEP, particularly among participants who reported being in a monogamous relationship as circumstances such as being in a relationship with a partner living with HIV may provide greater insight into contributing factors of YMSM’s PrEP beliefs and behaviors. By addressing these limitations, future research should aim to capture a broader sample of YMSM in regions with less access to PrEP, including those with little knowledge of PrEP and those with negative attitudes towards PrEP. These strategies may better identify demographic characteristics that distinguish those who possess negative attitudes toward PrEP from those who do not. Finally, our ability to make causal inferences is limited due to the cross-sectional nature of this study. PrEP stereotypes, stigma, gay community attachment, and PrEP use were measured at a single point in time, making it difficult to assess the directionality of the effects seen in our results. Future studies should employ time-series analyses to assess how changing attitudes and network characteristics might be related to engagement across the PrEP continuum, spanning awareness, intention, and willingness to seek PrEP, accessing PrEP-related medical care, initiating PrEP medications, and sustained PrEP adherence.
Conclusions
The successful rollout of PrEP to communities at high risk for HIV like YMSM remains a high priority HIV prevention strategy for ending the HIV epidemic in the United States. As structural interventions to facilitate the availability and accessibility of PrEP continue to emerge, these efforts must be paired with strategies that minimize intra-individual and interpersonal barriers to adopting PrEP. The development of negative attitudes about PrEP among YMSM is a persisting barrier associated with less progression along the PrEP continuum. To our knowledge, our study is one of the first to explore how gay community attachment contextualized with parallel community stigmas (e.g., community homophobia and HIV stigma) were associated with the endorsement of negative PrEP stereotypes and lifetime PrEP use. We conclude that the capacity for HIV prevention programs to leverage positive qualities of social networks and undermine negative PrEP stereotypes demands ongoing and additional support to reduce incident cases of HIV among YMSM.
Funding
This publication resulted (in part) from research supported by the Centers for AIDS Research at the University of Pennsylvania (P30 AI 045008; PI Ronald Collman), Johns Hopkins University (P30 AI 094189; PI: Richard Chaisson), and the District of Columbia (P30 AI 117970; PI: Alan E. Greenberg). This collaboration is supported by the following NIH Co-Funding and Participating Institutes and Centers: NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, FIC, NIGMS, NIDDK, and OAR. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of interest All authors have no potential or actual conflicts of interest to declare.
Ethical Approval Ethics approval for the current study was obtained by the University of Pennsylvania Institutional Review Board.
Informed Consent Informed consent was obtained electronically from all participants prior to completing the web-based survey.
References
- 1.Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-Tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):151ra125. 10.1126/scitranslmed.3004006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gray ME, Shenoi SV, Dillingham R. Pre-exposure prophylaxis as HIV prevention in high-risk adolescents. J Pediatr Pediatr Med. 2018;2(1):5–10. [PMC free article] [PubMed] [Google Scholar]
- 3.Hoots BE, Finlayson T, Nerlander L, et al. Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men—20 US cities, 2014. Clin Infect Dis. 2016;63(5):672–7. 10.1093/cid/ciw367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martin M, Vanichseni S, Suntharasamai P, et al. The impact of adherence to preexposure prophylaxis on the risk of HIV infection among people who inject drugs. AIDS. 2015;29(7):819–24. 10.1097/QAD.000000000000613. [DOI] [PubMed] [Google Scholar]
- 5.Spinner CD, Boesecke C, Zink A, et al. HIV pre-exposure prophylaxis (PrEP): a review of current knowledge of oral systemic HIV PrEP in humans. Infection. 2016;44(2):151–8. 10.1007/s15010-015-0850-2. [DOI] [PubMed] [Google Scholar]
- 6.Holloway I, Dougherty R, Gildner J, et al. PrEP uptake, adherence, and discontinuation among California YMSM using geosocial networking applications. J Acquir Immune Defic Syndr. 2017;74(1):15–20. 10.1097/QAI.0000000000001164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuhns LM, Hotton AL, Schneider J, et al. Young men who have sex with men is associated with race, sexual risk behavior and peer network size. AIDS Behav. 2017;21(5):1376–82. 10.1007/s10461-017-1739-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. HIV and gay and bisexual men. Centers for Disease Control and Prevention; 2017. https://www.cdc.gov/hiv/pdf/group/msm/cdc-hiv-msm.pdf. Accessed 1 July 2020 [Google Scholar]
- 9.Centers for Disease Control and Prevention. HIV and youth. Centers for Disease Control and Prevention; 2018. https://www.cdc.gov/hiv/pdf/group/age/youth/cdc-hiv-youth.pdf. Accessed 1 July 2020 [Google Scholar]
- 10.Kudon HZ, Mulatu MS, Song W, Heitgerd J, Rao S. Trends in condomless sex among MSM who participated in CDC-funded HIV risk-reduction interventions in the United States, 2012–2017. J Public Health Manag Pract. 2020. 10.1097/phh.0000000000001143. [DOI] [PubMed] [Google Scholar]
- 11.Paz-Bailey G, Mendoza MC, Finlayson T, Wejnert C, Le B, Rose C, Raymond HF, Prejean J, for the NHBS Study Group. Trends in condom use among MSM in the United States: the role of antiretroviral therapy and seroadaptive strategies. AIDS. 2016;30(12):1985–90. 10.1097/QAD.0000000000001139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanchez TH, Zlotorzynska M, Sineath RC, Kahle E, Tregear S, Sullivan PS. National trends in sexual behavior, substance use and HIV testing among United States men who have sex with men recruited online, 2013 through 2017. AIDS Behav. 2018;22:2413–25. 10.1007/s10461-018-2168-4. [DOI] [PubMed] [Google Scholar]
- 13.AIDSVu. Mapping PrEP: first ever data on PrEP users across the U.S. AIDSVu; 2018. https://aidsvu.org/prep/.
- 14.Kanny D, Jeffries WL IV, Chapin-Bardales J, Denning P, Cha S, Finlayson T, Wejnert C, the National HIV Behavioral Surveillance Study Group. Racial/ethnic disparities in HIV preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. Cent Dis Control Prev Morb Mortal Wkly Rep. 2019;68(37):801–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammack PL, Meyer IH, Krueger EA, et al. HIV testing and preexposure prophylaxis (PrEP) use, familiarity, and attitudes among gay and bisexual men in the United States: a national probability sample of three birth cohorts. PLoS ONE. 2018;13(9):e0202806. 10.1371/journal.pone.0202806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Golub SA. PrEP stigma: implicit and explicit drivers of disparity. Curr HIV AIDS Rep 15(2): 190–197. 10.1007/s11904-018-0385-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tuller D HIV prevention drug’s slow uptake undercuts its early promise. Health Aff. 2018;37(2):178–80. 10.1377/hlthaff.2017.1650. [DOI] [PubMed] [Google Scholar]
- 18.Calabrese SK, Magnus M, Mayer KH, et al. “Support Your Client at the Space That They’re in”: HIV pre-exposure prophylaxis (PrEP) prescribers’ perspectives on PrEP-related risk compensation. AIDS Patient Care STDs. 2017;31(4):196–204. 10.1089/apc.2017.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grov C, Whitfield TH, Rendina HJ, et al. Willingness to take PrEP and potential for risk compensation among highly sexually active gay and bisexual men. AIDS Behav. 2015;19:2234–44. 10.1007/s10461-015-1030-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marcus JL, Glidden DV, Mayer KH, et al. No evidence of sexual risk compensation in the iPrEx trial of daily oral HIV preexposure prophylaxis. PLoS ONE. 2013;8(12):e81997. 10.1371/journal.pone.0081997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Milam J, Jain S, Dubé M, et al. Sexual risk compensation in preexposure prophylaxis demonstration study among individuals at risk of HIV. J Acquir Immune Defic Syndr. 2019;80(1):e9–13. 10.1097/QAI.00000000000001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Newcomb ME, Moran K, Feinstein BA, et al. Pre-exposure prophylaxis (PrEP) use and condomless anal sex: evidence of risk compensation in a cohort of young men who have sex with men. J Acquir Immune Defic Syndr. 2018;77(4):358–64. 10.1097/QAI0000000000001604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dubov A, Galbo P, Altice FL, Fraenkel L. Stigma and shame experiences by MSM who take PrEP for HIV prevention: a qualitative study. Am J Mens Health. 2018;12(6):1832–43. 10.1177/1557988318797437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calabrese SK, Krakower DS, Mayer KH. Integrating HIV preexposure prophylaxis (PrEP) into routine preventive health care to avoid exacerbating disparities. Am J Public Health. 2017;107(12):1883–9. 10.2105/AJPH.2017.304061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Golub SA, Gamarel KE, Surace A. Demographic differences in PrEP-related stereotypes: implications for implementation. AIDS Behav. 2017;21(5):1229–35. 10.1007/s10461-015-1129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knight R, Small W, Carson A, Shoveller J. Complex and conflicting social norms: implications for future HIV pre-exposure prophylaxis (PrEP) interventions in Vancouver, Canada. PLoS ONE. 2016;11(1):e0146513. 10.1371/journal.pone.0146513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calabrese SK, Underhill K. How stigma surrounding the use of HIV preexposure prophylaxis undermines prevention and pleasure: a call to destigmatize “Truvada Whores.” Am J Public Health. 2015;105(10):1960–4. 10.2105/AJPH.2015.302816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kite ME, Bryant-Lees KB. Historical and contemporary attitudes toward homosexuality. Teach Psychol. 2016;43(2):164–70. 10.1177/0098628316636297. [DOI] [Google Scholar]
- 29.AIDSMap. PrEP use is rising fast in US, but large racial disparities remain. http://www.aidsmap.com/PrEP-use-is-rising-fast-in-US-but-large-racial-disparities-remain/page/3065545/. Accessed 1 July 2020
- 30.Phillips G, Neray B, Birkett M, et al. Role of social and sexual network factors in PrEP utilization among YMSM and transgender women in Chicago. Prev Sci. 2019;20(7):1089–97. 10.1007/s11121-019-00995-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schneider JA, Zhou AN, Laumann EO. A new HIV prevention network approach: sociometric peer change agent selection. Soc Sci Med. 2015;125:192–202. 10.1016/j.socscimed.2013.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wood S, Dowshen N, Bauermeister JA, et al. Social support networks among young men and transgender women of color receiving HIV pre-exposure prophylaxis. J Adolesc Health. 2020;66(3):268–74. 10.1016/j.jadolhealth.2019.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walsh JL. Applying the information-motivation-behavioral skills model to understand PrEP intentions and use among men who have sex with men. AIDS Behav. 2019;23:1904–16. 10.1007/s10461-018-2371-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ransome Y, Kawachi I, Dean LT. Neighborhood social capital in relation to late HIV diagnosis, linkage to HIV care, and HIV care engagement. AIDS Behav. 2017;21:891–904. 10.1007/s10461-016-1581-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moody RL, Starks TJ, Grov C, Parsons JT. Internalized homophobia and drug use in a national cohort of gay and bisexual men: examining depression, sexual anxiety, and gay community attachment as mediating factors. Arch Sex Behav. 2018;47:1133–44. 10.1007/s10508-017-1009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Painter TM, Song EY, Mullins MM, et al. Social support and other factors associated with HIV testing by Hispanic/Latino gay, bisexual, and other men who have sex with men in the U.S. South. AIDS Behav. 2019;23:S251–65. 10.1007/s10461-019-02540-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Petruzella A, Feinstein BA, Davila J, Lavner JA. Moderators of the association between community connectedness and internalizing symptoms among gay men. Arch Sex Behav. 2019;48(5):1519–28. 10.1007/s10508-018-1355-8. [DOI] [PubMed] [Google Scholar]
- 38.Shuper PA, MacLachlan DJ, Joharchi N, et al. HIV risk and protective factors in the context of alcohol and substance use during pride. AIDS Behav. 2018;22:2797–806. 10.1007/s10461-018-2117-2. [DOI] [PubMed] [Google Scholar]
- 39.Hotton AL, Keene L, Corbin DE, et al. The relationship between Black and gay community involvement and HIV-related risk behaviors among Black men who have sex with men. J Gay Lesbian Soc Serv. 2018;30(1):64–81. 10.1080/10538720.2017.1408518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.HIV.gov. What is ‘Ending the HIV Epidemic: A Plan for America’?. 2019. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. Accessed 25 Jan 2020.
- 41.Reid RJ, Lardier DT Jr, Garcia-Reid P, Yu D. HIV testing among racial and ethnic minority adolescents living in an urban community. J HIV/AIDS Soc Serv. 2017;16(3):228–49. 10.1080/15381501.2016.1244653. [DOI] [Google Scholar]
- 42.Bauermeister JA, Pingel E, Zimmerman M, et al. Data quality in HIV/AIDS web-based surveys: handling invalid and suspicious data. Field Methods. 2012;24:272–91. 10.1177/1525822X12443097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Holt M, Schmidt HM, Kolstee J, et al. Willingness to use and have sex with men taking HIV pre-exposure prophylaxis (PrEP): results of online surveys of Australian gay and bisexual men, 2011–2015. Sex Transm Infect. 2017;93(6):438–44. 10.1136/sextrans-2016-052774. [DOI] [PubMed] [Google Scholar]
- 44.Martin JL, Dean L. Summary of measures: mental health effects of AIDS on at-risk homosexual men. Reference type: Unpublished work; 1987. [Google Scholar]
- 45.Muthén LK, Muthén B. Mplus. The comprehensive modelling program for applied researchers: user’s guide. 2016; 5. [Google Scholar]
- 46.Klem L Structural equation modeling. In: Grimm LG, Yarnolds PR, editors. Reading and understanding MORE multivariate statistics. Washington, DC: American Psychological Association; 2000. [Google Scholar]
- 47.Matsunaga M Item parceling in structural equation modeling: a primer. Commun Methods Meas. 2008;2(4):260–93. 10.1080/19312450802458935. [DOI] [Google Scholar]
- 48.Muthén BO, Muthé LK, Asparouhov T. Regression and mediation analysis using Mplus. Los Angeles: Muthén and Muthén; 2017. [Google Scholar]
- 49.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–91. 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- 50.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–155. 10.1080/10705519909540118. [DOI] [Google Scholar]
- 51.Arrington-Sanders R, Rosenberger JG, Matson P, et al. Factors associated with emotional satisfaction during first anal intercourse in a sample of YMSM. J Homosex. 2016;63(7):989–984. 10.1080/00918369.2015.1113836. [DOI] [PubMed] [Google Scholar]
- 52.Corraini P, Olsen M, Pedersen L, et al. Effect modification, interaction and mediation: an overview of theoretical insights for clinical investigators. Clin Epidemiol. 2017;9:331–8. 10.2147/CLEP.S129728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holloway IW, Tan D, Gildner JL, et al. Facilitators and barriers to pre-exposure prophylaxis willingness among young men who have sex with men who use geosocial networking applications in California. AIDS Patient Care STDs. 2017;31(12):517–27. 10.1089/apc.2017.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Flash CA, Adegboyega OO, Yu X, et al. Correlates of linkage to HIV preexposure prophylaxis among HIV-testing clients. J Acquir Immune Defic Syndr. 2018;77(4):365–72. 10.1097/QAI.0000000000001605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grov C, Cain D, Whitfield TH, et al. Recruiting a US national sample of HIV-negative gay and bisexual men to complete at-home self-administered HIV/STI testing and surveys: challenges and opportunities. Sex Res Soc Policy. 2016;13:1–21. 10.1007/s13178-015-0212-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Whitehead J, Shaver J, Stephenson R. Outness, stigma, and primary health care utilization among rural LGBT populations. PLoS ONE. 2016;11(1):e0146139. 10.1371/journal.pone.0146139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dehlin JM, Stillwagon R, Pickett J, et al. #PrEP4Love: an evaluation of a sex-positive HIV prevention campaign. J Med Internet Res. 2019;5(2):e12822. 10.2196/12822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pettigrew TF, Tropp LR, Wagner U, Christ O. Recent advances in intergroup contact theory. Int J Intercult Relat. 2011;35:271–80. 10.1016/j.ijintrel.2011.03.001. [DOI] [Google Scholar]
- 59.Carpiano RM, Kelly BC, Easterbrook A, Parsons JT. Community and drug use among gay men: the role of neighborhoods and networks. J Health Soc Behav. 2011;52(1):74–90. 10.1177/0022146510395026. [DOI] [PubMed] [Google Scholar]
- 60.Eaton AA, Rios D. Social challenges faced by queer Latino college men: navigating negative responses to coming out in a double minority sample of emerging adults. Cult Divers Ethn Minor Psychol. 2017;23(4):457–67. 10.1037/cdp0000134. [DOI] [PubMed] [Google Scholar]
- 61.Brooks RA, Nieto O, Landrian A, et al. Experiences of preexposure prophylaxis (PrEP)-related stigma among Black MSM PrEP users in Los Angeles. J Urban Health. 2019. 10.1007/s11524-019-00371-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Brooks RA, Landrian A, Nieto O, Fehrenbacher A. Experiences of anticipated and enacted pre-exposure prophylaxis (PrEP) stigma among Latino MSM in Los Angeles. AIDS Behav. 2019;23:1964–73. 10.1007/s10461-019-02397-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hergenrather KC, Emmanuel D, Durant S, Rhodes SD. Enhancing HIV prevention among young men who have sex with men: a systematic review of HIV behavioral interventions for young gay and bisexual men. AIDS Educ Prev. 2016;28(3):252–71. 10.1521/aeap.2016.28.3.252. [DOI] [PubMed] [Google Scholar]
- 64.García M, Harris AL. PrEP awareness and decision-making for Latino MSM in San Antonio, Texas. PLoS ONE. 2017;12(9):e0184014. 10.1371/journal.pone.0184014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rolle CP, Rosenberg ES, Siegler AJ, et al. Challenges in translating PrEP interest into uptake in an observational study of young Black MSM. J Acquir Immune Defic Syndr. 2017;76(3):250–8. 10.1097/QAI.0000000000001497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Van Eeden-Moorefield B, Malloy K, Benson K. Gay men’s (non) monogamy ideals and lived experience. Sex Roles. 2016;75:43–55. 10.1007/s11199-015-0566-x. [DOI] [Google Scholar]
- 67.Philpot SP, Duncan D, Ellard J, et al. Negotiating gay men’s relationships: how are monogamy and non-monogamy experienced and practised over time? Cult Health Sex. 2018;20(8):915–28. 10.1080/13691058.2017.1392614. [DOI] [PubMed] [Google Scholar]
- 68.Kelly JA, Amirkhanian YA, Walsh JL, et al. Social network intervention to increase pre-exposure prophylaxis (PrEP) awareness, interest, and use among African American men who have sex with men. AIDS Care. 2020;32(Sup2):40–6. 10.1080/09540121.2020.1739207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grosskopf NA, LeVasseur MT, Glaser DB. Use of the internet and mobile-based “apps” for sex-seeking among men who have sex with men in New York City. Am J Mens Health. 2014;8:510–20. 10.1177/1557988314527311. [DOI] [PubMed] [Google Scholar]
- 70.Macapagal K, Moskowitz DA, Li DH, et al. Hookup app use, sexual behavior, and sexual health among adolescent men who have sex with men in the United States. J Adolesc Health. 2018;62(6):708–15. 10.1016/j.jadohealth.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Samuel LJ, Commodore-Mensah Y, Himmelfarb CR. Developing behavioral theory with the systematic integration of community social capital concepts. Health Educ Behav. 2014;41(4):359–75. 10.1177/1090198113504412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zarwell M, Robinson WT. Development of a social capital scale for constructed families of gay, bisexual, and other men who have sex with men. PLoS ONE. 2018;13(2):e0208781. 10.1371/journal.pone.0208781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Paluck EL, Green SA, Green DP. The contact hypothesis re-evaluated. Behav Public Policy. 2019;3(2):129–58. 10.1017/bpp.2018.25. [DOI] [Google Scholar]
- 74.Meanley S, Chandler C, Jaiswal J, et al. Are sexual minority stressors associated with young men who have sex with men’s (YMSM) level of engagement in PrEP? Behav Med. 2020. 10.1080/08964289.2020.1731675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kapadia F, Halkitis P, Barton S, et al. Associations between social support network characteristics and receipt of emotional and material support among a sample of male sexual minority youths. J Gay Lesbian Soc Serv. 2014;26:279–302. 10.1080/10538720.2014.924458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Grimm J, Schwartz J. “It’s like birth control for HIV”: communication and stigma for gay men on PrEP. J Homosex. 2018. 10.1080/00918369.2018.1495978. [DOI] [PubMed] [Google Scholar]
- 77.Reback CJ, Clark KA, Rünger D, Fehrenbacher AE. A promising PrEP navigation intervention for transgender women and men who have sex with men experiencing multiple syndemic health disparities. J Community Health. 2019;44:1193–203. 10.1007/s10900-019-00705-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Siegler AJ, Wirtz S, Weber S, Sullivan PS. Developing a web-based geolocated directory of HIV pre-exposure prophylaxis-providing clinics: the PrEP locator protocol and operating procedures. JMIR Public Health Surveill. 2017;3(3):e58. 10.2196/publichealth.7902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.French RS, Bonell C, Wellings K, Weatherburn P. An exploratory review of HIV prevention mass media campaigns targeting men who have sex with men. BMC Public Health. 2014;14:616. http://www.biomedcentral.com/1471-2458/14/616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Keene LC, Dehlin JM, Pickett J, et al. #PrEP4Love: success and stigma following release of the sex-positive PrEP public health campaign. Cult Health Sex. 2020. 10.1080/13691058.2020.1715482. [DOI] [PubMed] [Google Scholar]
- 81.Wilson N Altruism in preventive health behavior: at-scale evidence from the HIV/AIDS pandemic. Econ Hum Biol. 2018;30:119–29. 10.1016/j.ehb.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 82.Bartlett JE, Kotrlik JW, Higgins CC. Organizational research: determining appropriate sample size in survey research. Inf Technol Learn Perform J. 2001;19(1):43–50. [Google Scholar]


