Abstract
Background
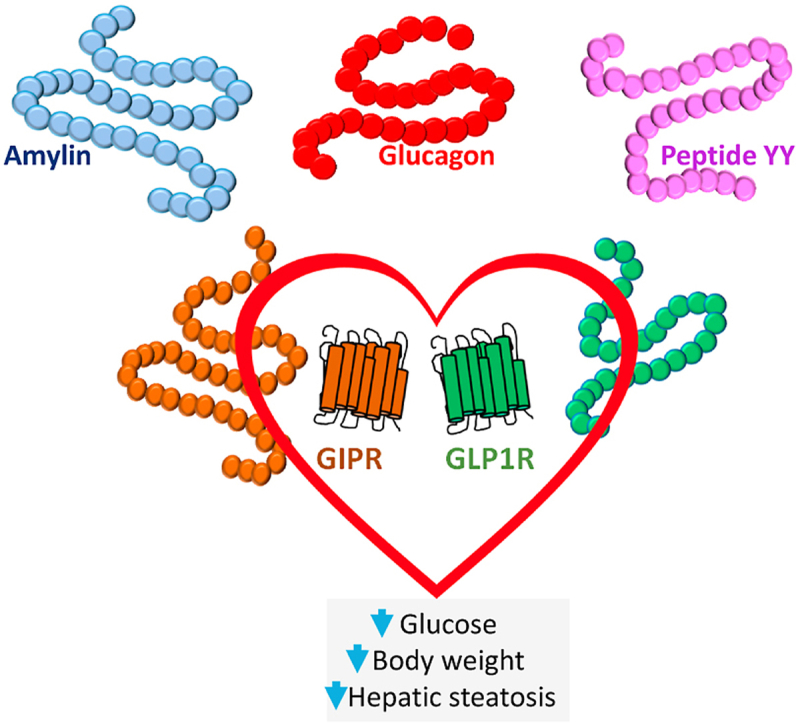
Glucagon-like peptide-1 receptor (GLP-1R) agonists are approved to treat type 2 diabetes and obesity. They elicit robust improvements in glycemic control and weight loss, combined with cardioprotection in individuals at risk of or with pre-existing cardiovascular disease. These attributes make GLP-1 a preferred partner for next-generation therapies exhibiting improved efficacy yet retaining safety to treat diabetes, obesity, non-alcoholic steatohepatitis, and related cardiometabolic disorders. The available clinical data demonstrate that the best GLP-1R agonists are not yet competitive with bariatric surgery, emphasizing the need to further improve the efficacy of current medical therapy.
Scope of review
In this article, we discuss data highlighting the physiological and pharmacological attributes of potential peptide and non-peptide partners, exemplified by amylin, glucose-dependent insulinotropic polypeptide (GIP), and steroid hormones. We review the progress, limitations, and future considerations for translating findings from preclinical experiments to competitive efficacy and safety in humans with type 2 diabetes and obesity.
Major conclusions
Multiple co-agonist combinations exhibit promising clinical efficacy, notably tirzepatide and investigational amylin combinations. Simultaneously, increasing doses of GLP-1R agonists such as semaglutide produces substantial weight loss, raising the bar for the development of new unimolecular co-agonists. Collectively, the available data suggest that new co-agonists with robust efficacy should prove superior to GLP-1R agonists alone to treat metabolic disorders.
Keywords: Diabetes, Obesity, Peptide, Receptor, Cardiovascular disease, Adipose tissue
Graphical abstract
Highlights
-
•
GLP-1 is a preferred partner for co-agonist development.
-
•
Co-agonist combinations must exhibit improved weight loss beyond GLP-1 alone.
-
•
Unimolecular coagonists must exhibit retained or improved cardioprotection.
-
•
Obesity represents an optimal condition for the development of new GLP-1 co-agonists.
1. Introduction
The development of glucagon-like peptide-1 receptor (GLP-1R) agonists to treat type 2 diabetes (T2D) and obesity [1] has sparked considerable efforts to develop next-generation therapies that are more effective than GLP-1R agonists alone. Although both T2D and obesity represent major therapeutic opportunities for new co-agonists, obesity is a disorder with a greater unmet need for safe and meaningfully effective therapies. Notably, bariatric surgery is the most effective current intervention for simultaneous reduction of body weight and resolution of T2D, setting a high bar for developing innovative new medicines. GLP-1-containing co-agonists are also being investigated to treat non-alcoholic steatohepatitis (NASH), a condition that is common in those with obesity and T2D and increasing in incidence [2], for which drug development is challenging and few effective therapies are available [3]. Given the extensive 15-year clinical experience with GLP-1R agonists, including an established safety profile in cardiovascular disease settings, this review will consider whether complementary mechanisms of action, when combined with GLP-1, might be effective yet safe new agents that are superior to GLP-1R agonists alone as therapy for metabolic disorders.
The rationale for developing peptide multi-agonists is supported by normal gut physiology, as the majority of peptide-secreting enteroendocrine cells are plurihormonal [4,5], and the gut secretes dozens of peptide hormones exerting glucoregulatory and/or anorectic activity [6]. The plurihormonal biology of gut endocrine cells is exemplified by L cells that express the proglucagon (GCG) gene, often together with neurotensin, cholecystokinin, and peptide YY [6]. Proglucagon-derived peptides (PGDPs) include GLP-1, glucagon, and oxyntomodulin, three peptides with unique metabolic activities suitable for treating diabetes or obesity [7]. The premise that combinatorial peptide therapy holds great therapeutic potential stems from multiple preclinical studies, emerging clinical data, and the remarkable results of bariatric surgery, an intervention associated with sustained increases in the circulating levels of multiple gut hormones [8,9]. Collectively, the current evidence suggests that simultaneous activation of peptidergic pathways may be useful for treating metabolic disorders. Nevertheless, the process of developing unimolecular agonists is challenging, entailing a precise understanding of the optimized ratios of each contributing molecular entity and potential complexity in interpreting unanticipated side effects. In this article, we review peptide candidates and their mechanisms being considered for co-agonist therapy with GLP-1 and highlight differences in rodent vs human biology and key unanswered considerations important for achieving clinical success.
2. Amylin
Amylin, also referred to as islet amyloid polypeptide (IAPP), is a 37 amino acid peptide that acts as both a neuropeptide and circulating endocrine hormone co-secreted with insulin from islet β cells. Amylin is also produced, at lower levels, in enteroendocrine cells. Amylin activates multiple amylin receptors comprised of calcitonin receptor (CTR) encoded by CALCR as well as different receptor activity-modifying proteins (RAMP) [10]. At least two different CTR splice variants may combine with 3 different RAMP proteins, potentially generating 6 distinct amylin receptors. Whether amylin acts to reduce food intake by primarily targeting neuronal and/or non-neuronal cell types in the hindbrain or other brain regions is not completely understood [10]. However, lesioning of the area postrema ablates the chronic satiating activity of amylin after a 7-day continuous intraperitoneal infusion in adult male rats fed a 17% fat diet [11]. Moreover, the anorectic actions of davalintide, a dual CTR/amylin receptor co-agonist, were markedly diminished in mice with genetic reduction of CTR expression in the nucleus of the solitary tract in mice [12]. These studies collectively illuminate the importance of the hindbrain for the pharmacological actions of amylin agonists.
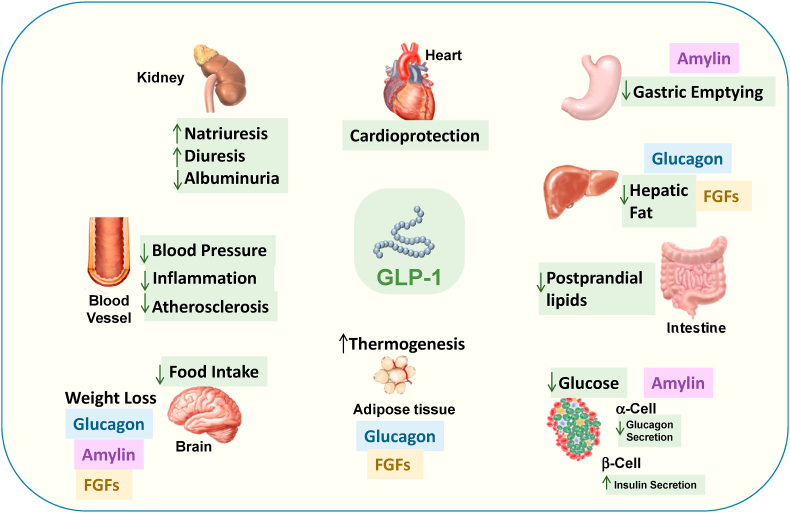
Studies in mice support physiological roles for both endogenous amylin action acting through the CTR on proopiomelanocortin (POMC) neurons and pharmacological amylin agonism in the control of energy homeostasis, encompassing locomotor activity, energy expenditure, and food intake [13]. Long-acting amylin analogs designed to avoid peptide aggregation as well as dual amylin and calcitonin receptor agonists (DACRA) produce robust weight loss in preclinical studies. A human amylin analog, pramlintide, was approved for therapy for type 1 diabetes and T2D in the US and lowers glucose by inhibiting gastric emptying and suppressing glucagon secretion (Figure 1), actions mediated by the activation of amylin receptors in the brain [10]. Nevertheless, the requirement for multiple daily injections and the comparatively modest effect on glycemic control and body weight result in limited clinical uptake of pramlintide.
Figure 1.
Actions of GLP-1, amylin, fibroblast growth factors (FGFs), leptin, and glucagon on key target organs relevant to metabolism.
The combined administration of amylin and leptin produces robust weight loss in preclinical studies of animals with diet-induced leptin resistance [14,15]. The mechanisms contributing to this combination's efficacy may include central potentiation of hypothalamic interleukin-6 (IL-6) activity enabling post-leptin receptor potentiation of leptin action, as genetic or pharmacological interruption of IL-6 action attenuates the weight loss activity of amylin in mice [16]. Notably, combination therapy with pramlintide (360 μg twice daily) and metreleptin (5 mg twice daily) produced considerable weight loss (mean 12.7 kg) over 20 weeks in overweight or obese human subjects [17]. Immunoneutralizing anti-leptin antibodies have been described in a small subset of subjects treated with metreleptin who also experienced transient weight gain or deterioration of metabolic control; however, the clinical significance of these findings remains uncertain [18]. Combinations of pramlintide (120 ug t.i.d.) and either phentermine or sibutramine produced greater efficacy (∼10% weight loss) than pramlintide alone in subjects with obesity studied over 24 weeks [19]. Long-acting amylin analogs continue to be investigated, alone or in combination with GLP-1R agonists, in clinical trials of subjects with obesity [19]. AM833, an investigational human amylin analog formulated for once weekly administration, has been assessed in short-term clinical studies in human subjects with obesity with or without co-administration of once-weekly semaglutide. AM833 at a dose of 4.5 mg achieved up to 10.8% weight loss as monotherapy over 26 weeks and weight loss of 17.1% in combination with semaglutide over 20 weeks [20]. Whether greater weight loss relative to semaglutide alone can be achieved with longer exposure to and different ratios of amylin-semaglutide combinations remains uncertain.
3. Cholecystokinin
Cholecystokinin (CCK) is a gut peptide that circulates in multiple molecular forms ranging from 8 to 58 amino acids. CCK inhibits food intake and reduces body weight in preclinical studies, actions predominantly mediated by the CCKAR gene encoding the cholecystokinin A receptor (CCK1R) [21]. Early human studies failed to show weight loss following a 24-week trial with GI181771X, a CCK1R agonist [22]. Nevertheless, CCK continues to be studied as a possible therapeutic candidate for weight loss. Combined administration of a CCK1R agonist together with amylin or a GLP-1R agonist over 14–28 days produced considerably greater weight loss relative to monotherapy in mice and rats [23]. Consistent with these findings, the administration of a long-acting CCK1R agonist for 13 weeks produced sustained reductions in food intake and weight loss in obese Gottingen mini-pigs [24]. A unimolecular CCK1R agonist AC170222-exenatide analog, designated C2816, was demonstrated to be a full agonist at both the GLP-1R and CCK1R receptors in vitro and produced ∼28% weight loss over 10 days in mice with diet-induced obesity [25]. Whether CCK agonism as a component of combination therapy is sufficient to produce long-term sustained weight loss in humans with obesity remains uncertain.
4. Fibroblast growth factors (FGFs)
FGFs encompass a large family of structurally related proteins that act locally as well as in an endocrine manner, producing metabolic actions in preclinical studies that include reduction of glycemia, body weight, and plasma lipid levels. FGFs generally enhance insulin action and might theoretically be complementary to classical incretin actions of GLP-1 focused on the islets (Figure 1). A single administration of FGF1 peripherally or into the brain produces remarkable sustained remission of experimental diabetes in preclinical studies [26,27], findings postulated to arise in part through increased hepatic glucose uptake [28]. Although the mechanisms transducing the sustained actions of FGF1 remain enigmatic, FGF1 administration together with pharmacological antagonism of the melanocortin-4 receptor in Lepob/ob mice highlights a key role of melanocortin signaling in transducing actions of FGF1 resulting in prolonged remission of experimental diabetes [29].
Peripheral administration of recombinant FGF1 in hyperglycemic mice produces robust glucose control and enhanced insulin sensitivity, actions dissociated from changes in cell proliferation, weight gain, or bone loss [27]. Moreover, peripheral administration of recombinant FGF1 also reduced hepatic fat accumulation and liver inflammation without induction of proliferation or fibrosis in mice with experimental liver injury [30]. FGF1 analogs engineered to exhibit diminished mitogenic potential continue to be explored to treat metabolic disorders such as diabetes and NASH.
FGF19, a human hormone that exhibits 51% amino acid identity with mouse FGF15, is produced predominantly in the gut, mimics a number of metabolic actions of FGF21, and levels of FGF19 increase in the circulation after bariatric surgery [31]. NGM282 (aldafermin), an analog of FGF19 that was engineered to exhibit reduced mitogenicity, reduced liver fat, but not blood glucose, after once daily administration for 28 days in human subjects with T2D [32]. Moreover, a 12-week course of NGM282 improved liver histology and reduced liver fat as well as biomarkers of inflammation and fibrosis in human subjects with biopsy-proven NASH [33].
FGF21 is a circulating hormone produced in multiple tissues, induced in the fasting state, and implicated in the metabolic response to fasting [34]. Multiple studies with FGF21 and FGF21 analogs demonstrate robust control of glucose and body weight reduction in preclinical studies. Gaich et al. examined the actions of the FGF21 analog LY2405319 in human subjects with obesity and T2D over 28 days [35]. Body weight was modestly reduced (−1.75 kg) but glycemia was not different; however, circulating levels of low-density lipoprotein cholesterol and triglycerides were reduced, whereas levels of high-density lipoprotein cholesterol were increased.
Considerable ongoing interest in FGF21 stems from its actions to reduce liver fat. Preclinical studies with a long-acting polyethylene glycosylated (PEGylated) FGF21 analog, B1344, in non-human primates with non-alcoholic liver disease demonstrated reduction of steatosis, attenuation of inflammation and fibrosis, and reduced hepatocyte injury after 11 weeks of therapy as assessed by analyzing liver biopsies [36]. B1344 also attenuated hepatic inflammation and liver injury in mice with experimental liver injury secondary to a methionine- and choline-deficient diet. A long-acting FGF21 analog, pegbelfermin, administered once a day at a dose of 10 or 20 mg for 16 weeks to overweight or obese human subjects with NASH reduced hepatic fat without changes in body weight or bone mineral density [33]. A 4-week trial of once-weekly administration of a long-acting FGF21 analog, PF-05231023, increased systolic and diastolic blood pressure and heart rate while reducing triglycerides without changing body weight in obese human subjects with hypertriglyceridemia with or without T2D [37]. Zhou et al. created a hybrid FGF molecule by combining FGF1 core sequences with the carboxy-terminal tail of FGF21 to create a FGF1HBS-FGF21C-tail hybrid. The chimeric FGF protein exhibited reduced mitogenic activity, prolonged circulating t1/2, and substantial glucose-lowering activity in mice and monkeys with experimental diabetes [38].
Gilroy et al. developed a unimolecular recombinant fusion protein encoding a long-acting GLP-1-FGF21 co-agonist using elastin-like polypeptide (ELP) linker technology to join the peptides, enabling continuous drug delivery via subcutaneous depots [39]. Remarkably, the EC50 of GLP1-ELP-FGF21 (23.9 ± 5.7 pM) for GLP-1R was similar to that of GLP1-ELP alone (29.5 ± 5.0 pM). The GLP1-ELP-FGF21 fusion protein produced more effective reduction of glycemia and body weight relative to the administration of the single agonists or an equimolar mixture of GLP1-ELP and ELP-FGF21 without evidence of fasting-associated hypoglycemia [39]. Whether FGF co-agonists can be developed for metabolic disorder therapy without risks of osteoporosis or unwanted cell proliferation remains unclear. Nevertheless, as both GLP-1R and FGF agonists are being investigated for NASH, it seems reasonable to consider a combinatorial approach given their distinct mechanisms of action.
5. Glucagon
Naturally occurring 37 amino acid oxyntomodulin contains the amino acid sequence of glucagon (GCG) and an 8 amino acid carboxyterminal extension and binds to the glucagon and GLP-1 receptors [7,40]. Classic physiology positions glucagon as a hormone with counter-regulatory activity that acutely increases glucose levels, raising concern about its use as a component of metabolic disease therapy. However, glucagon also inhibits food intake leading to weight loss, actions mediated through both the glucagon receptor (GCGR) and GLP-1R [41,42]. Indeed, a combination of peptide mutagenesis to eliminate the glucagon activity from oxyntomodulin, combined with studies in Glp1r−/− mice or WT mice using a GCGR antagonist, have highlighted the importance of both the GCGR and GLP-1R for the maximal weight loss effect ensuing from oxyntomodulin administration [43]. The actions through which GCG produces weight loss in preclinical studies are complex and include central effects and upregulation of FGF21 expression in the liver through mechanisms requiring the hepatic GCGR [44]. GCG increases FGF21 levels in mice and humans, implicating an indirect role for FGF21 in a subset of the metabolic actions of GCG converging on lipid metabolism and weight loss [45]. Glucagon also increases energy expenditure and brown adipose tissue (BAT) activity in mice [46], actions that are partially diminished in Fgf21−/− mice [46]; however, whether glucagon promotes meaningful BAT activity in humans is less clear [47]. Sustained GCG action has been associated with enhanced insulin-stimulated glucose disposal in lean and obese mice [44]. When used in combination with GLP-1, glucagon-containing co-agonists consistently reduce hyperglycemia in preclinical studies. As each GCGR-GLP-1R co-agonist contains a different set of affinities for the two receptors, it is not possible to make general conclusions about their mechanisms of action. Cotadutide, a dual GCGR-GLP1R investigational co-agonist under examination for treating NASH, reduced body weight in mice through mechanisms requiring the GLP-1R [42].
Preclinical studies demonstrated superior weight loss (by up to 30%) with cotadutide relative to liraglutide in mice with diet-induced obesity attributed to reductions in food intake and increased energy expenditure [41]. Daily cotadutide administration also reduced body weight by up to 11% in normal weight cynomolgus monkeys over 8 weeks [41]. Substantial reduction in glycemia, fat mass, and body weight was achieved following the administration of a DPP-4-resistant PEGylated GCGR-GLP-1R co-agonist in mice and rats with diet-induced obesity, actions attributed to substantial augmentation of energy expenditure [48]. The importance of GCG for co-agonist activity was demonstrated in studies of Glp1r−/− mice that lost substantial body weight yet also exhibited a deterioration of glucose tolerance after 4 weeks of co-agonist administration [48].
A dual GCGR-GLP-1R co-agonist formulated by introducing key GCG amino acid residues into the exendin-4 structure produced a robust inhibition of food intake and weight loss to a greater extent than similar doses of liraglutide in mice and monkeys with diet-induced obesity [49]. Consistent with the importance of GLP-1R for co-agonist activity, the dual agonist increased glycemic excursion in Glp1r−/− mice. Preclinical studies have also assessed the importance of glucagon action when incorporated together with sequences from GLP-1 (and exendin-4) and GIP into a unimolecular acylated DPP-4- resistant tri-agonist that augments cAMP accumulation through the GCGR, GIPR, and GLP-1R [50]. Administration of the tri-agonist produced ∼30% weight loss in mice with diet-induced obesity, actions arising through a combination of reduced food intake and increased energy expenditure. Studies of the tri-agonist in Gcgr−/−mice revealed the preservation of glucoregulatory action, yet substantial diminution of the weight loss effects, highlighting the important contribution of GCGR activation in the metabolic activity of the tri-agonist [50]. Notably, the administration of an acylated glucagon agonist alone produced ∼20% weight loss in high-fat diet-fed mice, and the extent of weight loss was enhanced when the glucagon agonist was combined with a GLP-1-GIP co-agonist. Hence, these findings highlight the contributions of GCGR activation to achieve weight loss in preclinical studies [50].
5.1. Glucagon-GLP-1 co-agonists and non-alcoholic steatohepatitis (NASH)
The actions of GCG on hepatic lipid metabolism combined with weight loss following GCG administration have prompted studies of GCGR-GLP-1R co-agonists in animal models of NASH. Indeed, hepatic GCGR signaling is essential for fatty acid oxidation as well as hepatic triglyceride synthesis and secretion in mice [51]. GCG reduces murine hepatic lipid content through multiple direct and indirect GCGR-dependent mechanisms [42]. De novo lipogenesis was markedly reduced in mice treated with either a selective GCG agonist, G1437, or cotadutide, associated with phosphorylation and inhibition of multiple enzymes in the hepatic lipid synthesis pathway [42]. Notably, both selective GCG agonism and cotadutide increased Ppargc1a expression and enhanced mitochondrial biogenesis in mouse and human hepatocytes and restored basal respiratory rates in hepatocytes isolated from mice with NASH. Cotadutide produced greater improvement in liver histology, including reductions in steatosis, inflammation, and fibrosis relative to cohorts treated with liraglutide, in mice with experimental NASH after similar degrees of weight loss [42]. Hence, GCG agonism may indirectly improve experimental components of NASH via weight loss and through direct actions to reduce hepatic lipogenesis and augment mitochondrial oxidative capacity [42].
5.2. Human studies with GCG co-agonists
Notwithstanding the robust weight loss effects of GCGR-GLP-1R co-agonists evident in preclinical studies, the available clinical data for these agents to date has engendered less enthusiasm. Glucagon-GLP-1 co-agonists designed for once weekly administration, such as efinopegdutide, LY2944876, SAR425899, and MEDI-0382 (cotadutide), have been assessed in short-term clinical trials in subjects with obesity and T2D. Although meaningful reductions in glycemia and body weight have been observed, it remains unclear whether these co-agonists produce superior reductions in body weight and HbA1c relative to optimized GLP-1R agonists alone in these patient populations [52,53].
Both native glucagon and GCGR-GLP-1R co-agonists acutely increase energy expenditure in short-term studies over hours to days in humans [[54], [55], [56], [57]]. However, there is little evidence that these actions are sustained with chronic administration. The dual glucagon-GLP-1 co-agonist SAR425899 was administered to overweight or obese human subjects for 28 days, improving glucose control and resulting in a maximal weight loss of 5 kg [52,58]. Despite these results, there are no ongoing clinical studies of SAR425899. Cotadutide was administered once daily for 49 days to overweight or obese subjects with T2D [59]. While cotadutide attenuated meal-related glycemic excursion and inhibited gastric emptying, body weight loss was ∼3.4%, substantially less than reported in preclinical studies. In a separate study, daily cotadutide administration for 41 days reduced fasting glucose and HbA1c and decreased liver fat and volume; however, placebo-subtracted weight loss was 2.14 kg [53]. Cotadutide was subsequently studied at doses ranging from 100 to 300 mg once daily in overweight or obese subjects with T2D. Study participants treated with 300 mg once daily exhibited weight loss of ∼4.4 kg at 54 weeks, greater than that observed with liraglutide (https://clinicaltrials.gov/ct2/show/results/NCT03235050) yet slightly less than the maximal weight loss achieved with semaglutide in similar patient populations [60]. The available human data for glucagon-GLP-1 co-agonists assessed in the context of T2D or obesity suggests that the best of these agents may currently be comparable but not superior to results obtained with GLP-1R agonists.
6. Glucose-dependent insulinotropic polypeptide (GIP)
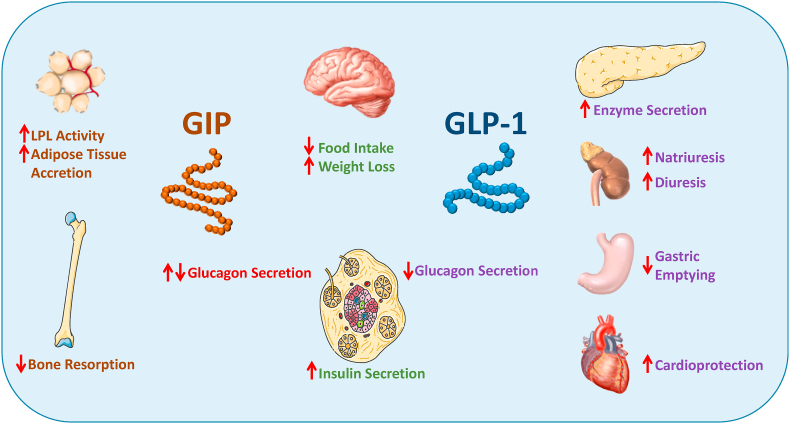
Combining GLP-1 with its incretin partner GIP is a promising strategy (Figure 2) under investigation for treating T2D and obesity. GIP is a 42 amino acid peptide that is produced within and released from intestinal K cells that are located primarily in the proximal small bowel. Similar to GLP-1, GIP is secreted in response to nutrient ingestion and enhances meal-stimulated insulin secretion in a glucose-dependent manner by activating its cognate GIP receptor (GIPR) in pancreatic beta cells [61]. GIP also exerts modest effects to increase glucagon secretion during hypoglycemia and suppress glucagon levels during hyperglycemia [62]. GIP also targets bone and adipose tissue, acutely inhibiting bone resorption [63] while exerting anabolic actions to promote lipid accretion in fat cells [64]. More recent preclinical studies have demonstrated that the central genetic activation of GIPR + neurons in the hypothalamus may also reduce food intake and promote weight loss [65], findings consistent with the peripheral administration of long-acting degradation-resistant GIPR agonists in mice with diet-induced obesity [66].
Figure 2.
Metabolic actions of GLP-1 and GIP on key target tissues.
Initial enthusiasm for the therapeutic use of GIP in humans with T2D was tempered by the demonstration that in contrast to GLP-1, the insulinotropic effects of acute GIP administration are diminished in patients with T2D [67,68]. Moreover, several preclinical studies demonstrated that loss of GIP secretion or genetic, immunologic, or pharmacological attenuation of GIP action promoted weight loss [[69], [70], [71], [72], [73]]. Thus, there appeared to be little incentive to pursue strategies that activated the GIPR to treat T2D. Consequently, the initial focus shifted to developing GLP-1R agonists to treat T2D [1]. However, renewed interest in the therapeutic potential of GIP emerged with studies showing that improving glucose control with antidiabetic therapies could restore the insulinotropic effect of GIP in patients with T2D [[74], [75], [76]]. The overlapping insulinotropic and subsequent body weight-lowering actions of both GLP-1 and GIP helped foster the notion that combining the actions of these two peptide hormones might have the potential to bolster their glucose-lowering and appetite-suppressing effects beyond what is observed with individual agents. An early indication that this combination could be superior to single GLP-1R agonist administration was provided by Finan et al. who demonstrated that two weeks of simultaneous administration of equimolar amounts of a GLP-1R and GIPR agonist reduced food intake, body weight, and fat mass in mice with diet-induced obesity (DIO) to a greater extent than either agent alone [77]. Additional preclinical proof of concept came from similar studies in rodent models of T2D and/or obesity wherein the combined activation of both GLP-1R and GIPR resulted in superior glucose-lowering and/or reduction in weight gain compared to the activation of either receptor alone [[78], [79], [80]]. The observed greater metabolic benefits with combined GLP-1R and GIPR activation spurred interest in developing unimolecular drugs that would unite the actions of GLP-1 and GIP (Figure 2) in a single molecule with a distinct pharmacokinetic profile and greater potential for regulatory approval.
6.1. Development of unimolecular GLP-1:GIP co-agonists
Finan et al. created a 40 amino acid single molecule peptide chimera on a glucagon backbone that exhibited balanced in vitro activity at both GLP-1 and GIP receptors, with minimal activity at the glucagon receptor and protracted action in vivo [77]. This unimolecular co-agonist was predicted to bind either GLP-1R or GIPR but not to both receptors simultaneously. Additional structural modifications included (i) substitution with aminoisobutyric acid at position 2 to increase resistance to DPP-4-mediated cleavage and inactivation, (ii) the addition of a C-terminal extension with 9 amino acids from exendin-4 to enhance structural stability, and (iii) acylation with a C16:0 fatty acid or PEGylation with 40 kDA PEG to extend in vivo activity, thus enabling daily or weekly administration, respectively [69]. The administration of unacylated, acylated, and PEGylated versions of this co-agonist dose-dependently reduced body weight, food intake, and fat mass and improved glycemic control and insulin sensitivity in rodent models of obesity and diabetes with greater efficacy than equimolar doses of GLP-1R agonist comparators exendin-4 and liraglutide [77]. Moreover, these superior effects could be achieved with less frequent dosing of long-acting co-agonists [77]. The acylated co-agonist also lowered blood glucose and increased insulin levels following graded glucose infusion in cynomulgus monkeys that had received a single subcutaneous injection of the co-agonist. In this study, the co-agonist exhibited greater metabolic potency relative to an equivalent dose of liraglutide, thus prompting clinical proof-of-concept studies in humans [77].
A single injection of 4, 8, or 16 mg of PEGylated GLP-1:GIP co-agonist in healthy humans increased insulin secretion and lowered blood glucose levels when administered 72 h prior to a graded glucose infusion challenge [77]. Subsequently, the clinical efficacy and safety of the PEGylated co-agonist was evaluated in a chronic ascending-dose study wherein 53 patients with T2D received once-weekly injections of 4, 12, 20, or 30 mg of the PEGylated co-agonist or placebo for 6 weeks. Co-agonist treatment was associated with significant dose-dependent reductions in HbA1c levels ranging from −0.53% to −1.11% for those patients receiving the 4 mg–30 mg doses, respectively, relative to a decrease of −0.16% in patients receiving placebo. Co-agonist treatment was well-tolerated, with reports of only mild to moderate side effects that included nausea and diarrhea [77]. The observation of limited GI side effects in this study contrasts with adverse events reported in studies of relatively high doses of long-acting GLP-1R agonists and was suggested to be indicative of a greater therapeutic index for GLP-1 receptor agonism when combined with a GIPR agonist. Although promising, the lack of a GLP-1R agonist comparator in this study makes it difficult to draw conclusions regarding the relative effectiveness of the co-agonist.
6.2. RG7697/NNC0090-2746
The acylated version of the GLP-1:GIP co-agonist originally developed by Finan et al. (as previously described) is synonymous with RG7697 and NNC0090-2746 [81]. The pharmacokinetics, pharmacodynamics, safety, and tolerability of RG7697/NNC0090-2746 were evaluated in 51 healthy volunteers in a double-blind, placebo-controlled trial wherein a single subcutaneous injection of doses ranging from 0.03 to 5 mg was administered [82]. The 19–25 h half-life of the drug confirmed its suitability for once-daily dosing. At doses ≥1.8 mg, RG7697/NNC0090-2746 reduced both glucose and insulin levels during a meal tolerance test. The drug was well-tolerated up to doses of 3.6 mg, with reports of mild adverse gastrointestinal events including nausea and vomiting. Increases in heart rate were observed at doses ≥1.8 mg, with the highest doses tested (3.6 and 5 mg) increasing the pulse rate by approximately 6–20 beats per minute (bpm) vs placebo. No treatment-emergent anti-RG7697/NNC0090-2746 antibodies were detectable in any of the participants [82]. Similar findings were reported in studies examining the pharmacokinetics, pharmacodynamics, and safety of RG7697/NNC0090-2746 in 56 patients with T2D who received once-daily subcutaneous injections of 0.25, 0.75, 1.1, 1.5, 2, or 2.5 mg of the co-agonist or placebo for 2 weeks in a randomized, double-blind, dose-escalation study [81]. Relative to placebo, doses ≥0.75 mg of RG7697/NNC0090-2746 were associated with dose-dependent reductions in fasting and postprandial glucose levels and increased insulin sensitivity, with no effect on gastric emptying. At the highest dose of 2.5 mg, significant reductions in HbA1c levels (−0.67% vs −0.21% for placebo) and body weight (−3.0 kg vs −0.9 kg for placebo) were observed with co-agonist treatment. The most frequent adverse events associated with co-agonist treatment in T2D patients were reported as mild in intensity and comprised nausea, diarrhea, and reduced appetite [81]. Dose-dependent increases in the heart rate (6–12 bpm) and lipase and amylase levels, which are typically observed with GLP-1R agonists, were also observed in co-agonist-treated subjects. To expand on these studies, the effects of RG7697/NNC0090-2746 on glycemic control, body weight, and other metabolic measurements were evaluated in a 12-week double-blind and placebo-controlled phase 2a clinical trial of 108 subjects with T2D inadequately controlled with metformin [83]. Subjects were randomized to receive once-daily subcutaneous injection of 1.8 mg of RG7697/NNC0090-2746 or placebo. Once-daily subcutaneous injections of liraglutide (1.8 mg starting with a 2-week dose escalation) were administered in an open-label reference arm. RG7697/NNC0090-2746 significantly reduced HbA1c levels and body weight relative to baseline values and compared to placebo, with reductions similar to those observed in patients treated with liraglutide in the open-label arm [83]. Reductions in body weight were observed at week 8 in co-agonist-treated patients but were no longer significant by week 12. Notably, post hoc analysis revealed that the greatest reductions in body weight with RG7697/NNC0090-2746 treatment were seen in those patients who had better glycemic control (HbA1c < 8.5%) at baseline. The authors suggested that this observation is in line with reports of greater sensitivity to GIP action upon amelioration of hyperglycemia. Reductions in total cholesterol levels were also evident in the RG7697/NNC0090-2746 treatment group. In contrast, no changes in cholesterol levels were seen in the open-label liraglutide group. Consistent with earlier clinical studies, the most frequently reported adverse events associated with RG7697/NNC0090-2746 use were nausea, vomiting, and diarrhea, and the co-agonist was deemed to be generally safe and well-tolerated [83]. Heart rate was elevated with RG7697/NNC0090-2746 (5.6 bpm relative to placebo), and 43% of individuals who received the co-agonist developed anti-drug antibodies, although these antibodies did not appear to alter drug efficacy.
6.3. Tirzepatide (LY3298176)
The leading molecule among unimolecular GLP-1:GIP co-agonists is tirzepatide (LY3298176), a 39 amino acid peptide whose basic structure stems from the GIP sequence but has been modified to include (i) substitution of the second amino acid with aminoisobutyric acid to avoid DPP-4 proteolysis and, (ii) addition of a C20 fatty di-acid acyl chain to enable non-covalent albumin binding and once-weekly subcutaneous dosing [84]. In vitro characterization using cell lines that recombinantly express either human GIP or GLP-1 receptors revealed that tirzepatide exhibits comparable binding affinity and potency at the human GIPR relative to that of the native GIP peptide. However, tirzepatide binds with 5-fold less affinity and is 13-fold less potent at the human GLP-1R than native GLP-1 [84], thus exhibiting bias for the GIPR. Preclinical studies demonstrated that tirzepatide reduced glucose levels during intraperitoneal glucose tolerance tests in wild-type and single incretin receptor-deficient mice to levels comparable to those observed for the GLP-1R agonist semaglutide in Gipr−/− mice and the DPP-4-resistant analog [d-Ala2]GIP in Glp1r−/− mice, indicating that the co-agonist is active at both receptors in vivo [84]. In mice with DIO, chronic treatment (every 3 days for 22 days) with 10 nmol/kg tirzepatide resulted in weight loss that was greater than that observed with similar treatment with 30 nmol/kg semaglutide. Interestingly, it was noted that, relative to semaglutide, tirzepatide treatment led to greater and more sustained reductions in food intake during the first 7–10 days of dosing associated with greater fat oxidation and increased energy expenditure after 7 days of drug treatment [84].
Early clinical evaluation of tirzepatide included a series of randomized, double-blind, placebo-controlled phase 1 trials designed to evaluate the safety, tolerability, pharmacokinetics, and pharmacodynamics of tirzepatide in humans [84]. The first of these was a single-ascending dose pharmacokinetic study of subcutaneous injections of tirzepatide at doses ranging between 0.25 and 8 mg vs placebo in 6 cohorts of healthy humans at a prespecified ratio of 3 tirzepatide-treated individuals to 1 placebo-treated individual. This study demonstrated that the mean half-life of tirzepatide in healthy humans was approximately 5 days, thus validating once-weekly administration of the co-agonist [84]. The second trial was a 4-week multiple ascending-dose study in healthy subjects wherein tirzepatide doses between 0.5 and 10 mg, 1.5 mg dulaglutide (GLP-1R agonist comparator control), or placebo were administered once a week at prespecified ratios of 6 tirzepatide:1 dulaglutide:1 placebo. Individuals receiving 10 mg tirzepatide did so via weekly up-titration with 5, 5, 8, and 10 mg. In healthy humans, dosing with 4.5 mg of tirzepatide resulted in significant reductions in fasting glucose vs placebo and improvements in glucose tolerance that were comparable to those of 1.5 mg dulaglutide. Relative to the baseline level, body weight was also reduced in individuals receiving tirzepatide at the 4.5 mg (−4.52 kg) or 10 mg doses (−4.05 kg) compared to 1.5 mg dulaglutide (−1.3 kg). The third trial was a 4-week multiple-dose phase 1b proof-of-concept study in subjects with T2D that tested fixed doses of 0.5 or 5 mg as well 10 and 15 mg doses that were delivered by 5/5/10/10 mg and 5/5/10/15 mg up-titration dosing schemes, respectively. Individuals were administered tirzepatide or placebo at a prespecified ratio of 4 tirzepatide:1 placebo. This study did not include a GLP-1R agonist comparator as a control group. Clear reductions in HbA1c, fasting glucose, and insulin levels were observed in the two groups receiving up-titrated tirzepatide dosing compared to placebo. Glucose tolerance was also improved with the three highest doses of tirzepatide, and plasma insulin levels during an oral glucose tolerance test were increased in subjects treated with 15 mg tirzepatide vs placebo. Dose- and time-dependent reductions in body weight were seen at all doses of tirzepatide relative to placebo, but statistical significance was only achieved at the two highest doses (−2.39 kg for 10 mg and −2.95 kg for 15 mg vs −0.32 kg for placebo). Moreover, reductions in body weight in subjects with T2D were less robust compared to the amount of weight loss observed with tirzepatide in healthy individuals in the second study [84].
Across all three studies, the most frequently reported adverse events were gastrointestinal in nature and included nausea, vomiting, diarrhea, reduced appetite, and abdominal distension, which were dose-dependent and considered to be mild to moderate in severity [84]. In general, individuals with T2D reported fewer GI adverse events and were able to tolerate higher doses of tirzepatide than healthy individuals. Increases in the pulse rate were detected at the two highest tirzepatide doses in the T2D trial (+8.82 bpm for 10 mg and +9.8 bpm for 15 mg vs −3.81 bpm for placebo), comparable to the increase in the pulse rate (+11.2 bpm) seen with dulaglutide in healthy subjects.
The efficacy and safety of tirzepatide were next evaluated in a 26-week, double-blind, placebo-controlled trial in subjects with T2D inadequately controlled with diet and exercise alone or treated with stable metformin therapy [85]. In this phase 2b study, individuals were randomized to receive once-weekly subcutaneous injection of 1, 5, 10, or 15 mg of tirzepatide, 1.5 mg of the GLP-1R agonist dulaglutide (active comparator), or placebo for 26 weeks. To improve gastrointestinal tolerability, the patients assigned to the 10 or 15 mg doses of tirzepatide were up-titrated to final doses, with those in the 10 mg group receiving a 5 mg dose for the first two weeks and then a 10 mg dose for the remainder of the study, whereas the subjects in the 15 mg group were given a 5 mg dose for the first two weeks, a 10 mg dose for the next four weeks, and a 15 mg dose for the remaining study duration. Tirzepatide treatment was associated with dose-dependent reductions in HbA1c (−1.06% at 1 mg to −1.94% at 15 mg vs −0.06% for placebo) from baseline that were greater at all doses relative to placebo and non-inferior to dulaglutide. At 26 weeks, 33–90% of the subjects treated with tirzepatide achieved an HbA1c target of <7% (vs 12% with placebo and 52% with dulaglutide) and 15–82% of the subjects reached an HbA1c target of ≤6.5% (vs 2% with placebo and 39% with dulaglutide), with a greater proportion of the patients in the 5, 10, or 15 mg tirzepatide dose groups achieving these HbA1c targets compared to those treated with dulaglutide. Approximately 18% of the patients receiving the 10 mg dose and 30% of the subjects receiving the 15 mg dose of tirzepatide achieved normoglycemia (HbA1c < 5.7%) compared with 2% of the patients treated with dulaglutide. Dose-dependent reductions in fasting plasma glucose levels from baseline to week 26, relative to placebo, were observed for all tirzepatide doses, with reductions at the 5, 10, and 15 mg doses being significantly greater than what was achieved with dulaglutide (−0.4 mmol/L at 1 mg to −3.4 mmol/L at 15 mg for tirzepatide vs 0.9 mmol/L for placebo and −1.2 mmol/L for dulaglutide). Significant improvements in HOMA2-B (beta cell function) and HOMA2-IR (insulin sensitivity) and greater reductions in plasma levels of fasting insulin and glucagon (adjusted by fasting glucose) were seen with the higher 5–15 mg doses of tirzepatide relative to dulaglutide [85]. All of the tirzepatide doses reduced body weight compared to placebo in a dose-dependent manner. Reductions in mean body weight from baseline to week 26 ranged from −0.9 kg at 1 mg of tirzepatide to −11.3 kg at 15 mg of tirzepatide (vs −0.4 kg for placebo and −2.7 kg for dulaglutide) and were greater at the 5, 10, and 15 mg doses than dulaglutide. Additionally, more individuals in the 5, 10, and 15 mg tirzepatide dose groups achieved body weight targets (≥5%, ≥10%, and ≥15% weight loss from baseline) than those in the dulaglutide group. By week 26, tirzepatide treatment at 5, 10, and 15 mg doses was also associated with greater reductions in waste circumference than both placebo and dulaglutide. This study's authors suggest that these reductions in waist circumference could be indicative of decreased visceral fat that could explain, at least in part, the improvements in insulin sensitivity observed in patients receiving tirzepatide in this study. Reductions in total cholesterol (relative to placebo only) and triglyceride (relative to placebo and dulaglutide) levels were also evident by week 26 in the subjects treated with the higher doses of tirzepatide. Interestingly, in a recent post hoc study, further analysis of plasma samples from this trial revealed that tirzepatide dose-dependently lowered triglyceride, apoC-III, and apoB levels over time and reduced the number of large triglyceride-rich lipoprotein particles and small low-density lipoprotein particles compared to dulaglutide and/or placebo [86]. Only a small portion of these changes could be attributed to tirzepatide-induced weight loss. These findings indicate a net improvement in insulin sensitivity and a shift toward a less atherogenic lipoprotein profile in subjects with T2D treated with tirzepatide, with potential implications for cardiovascular safety [86]. A related post hoc analysis from the same trial [85] analyzed levels of liver enzymes, keratin-18, procollagen III, and adiponectin in tirzepatide-treated subjects after 26 weeks [87]. Liver enzymes and NASH biomarkers were reduced and adiponectin levels were increased after 26 weeks in the subjects treated with 15 mg of tirzepatide once weekly [87].
The available information suggests that adverse events experienced with tirzepatide were similar to those reported for dulaglutide. The one noteworthy exception was the higher percentage of patients in the 15 mg tirzepatide group who discontinued study treatment prematurely due to adverse events. The most common treatment-emergent adverse events were gastrointestinal symptoms that included nausea, vomiting, and diarrhea. These were reported to be dose-dependent, mild to moderate in severity, and transient. Reduced appetite was the second most common treatment-associated adverse event. A range of dose-escalation regimens has been explored to optimize the tolerability of tirzepatide in human subjects with T2D [88]. Starting doses were 2.5, 4, or 5 mg once weekly for 4 weeks, followed by progressive dose escalation to 12 or 15 mg by week 8. Rates of nausea were generally lower than 40%, with a very low rate of drug discontinuation, findings consistent with currently utilized GLP-1R agonists such as dulaglutide and semaglutide [88]. The cardiovascular safety of once-weekly tirzepatide is currently being compared to that of dulaglutide in the SURPASS cardiovascular outcome trial. This study has a primary endpoint of 3-point major adverse cardiovascular events (MACE; myocardial infarction, stroke, and cardiovascular death), is expected to randomize 12,500 subjects with T2D, and concludes in the third quarter of 2024.
6.4. Potential mechanisms for effectiveness of GLP-1:GIP co-agonism
As resistance to GIP action in T2D can be overcome by restoring glucose levels to near normal, it has been postulated that the glucose-lowering effects of simultaneous GLP-1R agonism could rapidly restore GIP sensitivity, thus enabling superior glucose-lowering action when combined. Moreover, GLP-1 and GIP appear to activate distinct subsets of hypothalamic neurons coupled to reduction of food intake [65], providing a greater degree of weight loss than that achieved with activation of a single CNS receptor alone. Support for this possibility comes from the observed greater reductions in body weight seen in T2D subjects with lower baseline HbA1c in clinical studies with RG7697/NNC0090-2746 [83]. It remains uncertain whether starting co-agonist therapy at less advanced stages of diabetes or treating patients with co-agonists for longer periods to allow GIP to manifest its full potential will be useful clinical approaches.
6.5. Outstanding questions for dual GLP-1:GIP therapy
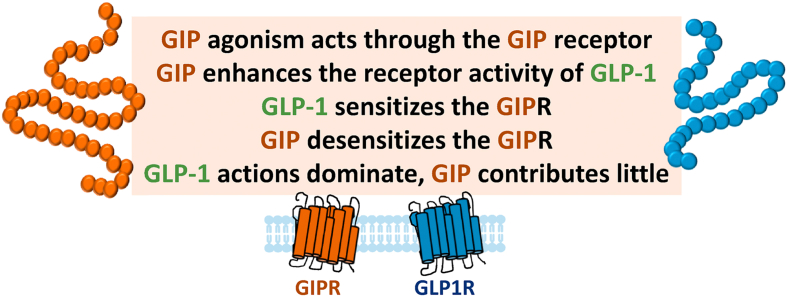
The magnitude of weight loss and reduction in HbA1c observed with tirzepatide raises a number of mechanistic questions (Figure 3). Is it actually the combination of GLP-1R agonism with GIPR agonism that is important? Does the unique ratio of peptides and unimolecular nature of the co-agonist impart a greater benefit through as-yet-unknown mechanisms? Do these unimolecular drugs target GLP-1 and GIP receptors on the same cell, different cells in different tissues, or both? As the β cell actions of GIPR agonism appear susceptible to tachyphylaxis reflecting receptor desensitization, will this be overcome in a unimolecular GLP-1:GIP co-agonist? Moreover, will co-agonists retain their efficacy and benefits with sustained use? As GLP-1R agonists have been approved for T2D and obesity [1], appear potentially efficacious in NASH [89], and exhibit cardioprotection in humans with T2D at risk of or with established cardiovascular disease [90], will a GLP-1:GIP co-agonist fully recapitulate all of the benefits ascribed to GLP-1R agonism (Figure 2)? Conversely, short-term studies have demonstrated that GIP may inhibit bone resorption; will this potentially translate into a clinically meaningful added benefit of GLP-1:GIP co-agonism in older subjects at risk of osteoporosis?
Figure 3.
Possible mechanisms of the interaction of GIP and GLP-1 for treatment of metabolic disorders.
An additional layer of complexity underlying the rational development of GLP-1:GIP co-agonists stems from multiple studies demonstrating that GIPR antagonism may also be metabolically beneficial [91]. Notably, GIPR agonists and antagonists exhibit similar efficacy in preventing weight gain or promoting weight loss when combined with a GLP-1R agonist, providing support for developing GIPR antagonist:GLP-1R agonist combinations [91]. Agonist-induced GIPR desensitization has been proposed as a potential unifying mechanism to explain this paradoxical observation [91,92], raising the fascinating possibility that we may witness the development of competing therapeutic strategies based on either GIPR agonism or antagonism, together with GLP-1R agonism, to treat T2D or obesity.
7. Insulin
Insulin is a logical partner for GLP-1, with entirely complementary mechanisms of action contributing to additive glucose reduction in subjects with T2D. Two insulin:GLP-1 co-formulated combinations have been approved to treat T2D: lixisenatide-insulin glargine and liraglutide-insulin degludec. Both formulations produce robust glucose control often without weight gain and with less hypoglycemia than observed with insulin alone. Indeed, these combinations provide a preferable alternative than simply increasing the insulin dose in subjects already exhibiting suboptimal glycemic responses to insulin [93,94] or those exhibiting insufficient responses to GLP-1R agonist therapy [95,96]. Remarkably however, the clinical adoption of insulin-GLP-1 therapies has been slow, much lower than that observed for newer GLP-1R agonists. The clinical development of a once weekly basal insulin icodec raises the possibility of developing a more convenient yet highly effective once weekly insulin-GLP-1 formulation.
8. Leptin
While clinical trials of leptin monotherapy did not produce sufficiently meaningful weight loss to merit regulatory approval for obesity, considerable interest remains in using leptin alone or in combination with other agents as a weight loss therapy. Moreover, progress continues in studies designed to overcome leptin resistance, as exemplified by the concomitant administration of the pentacyclic triterpene celastrol, which enhances leptin sensitivity through mechanisms requiring interleukin 1 receptor 1 [97]. Preclinical studies with amylin, GLP-1R agonists, or FGF21 demonstrate that these peptides, either as single agents or glucagon-GLP-1 co-agonists, can partially re-sensitize leptin weight loss responses (to a greater extent than that achieved with caloric restriction) in animals with diet-induced obesity or experimental diabetes [14,[98], [99], [100]]. Indeed, in clinical studies, the combination of leptin and pramlintide produced greater weight loss than that achieved with each agent alone [14,17]. Analysis of human responses to leptin administration suggests that individuals with lower leptin levels may exhibit greater leptin sensitivity and enhanced weight loss with leptin administration [101]. Indeed, preclinical studies reducing leptin levels or partially blocking leptin action demonstrate enhanced and/or restored leptin sensitivity in the context of obesity and pre-existing hyperleptinemia [102]. Moreover, as previously noted, complementary efforts are focused on identifying downstream components of leptin receptor signaling amenable to modulation by small molecule enhancers of leptin sensitization [97], collectively suggesting multiple future avenues for enhancing leptin action in obesity therapy.
9. Peptide YY (PYY)
PYY is a 36 amino acid peptide that is cleaved by DPP-4 to generate PYY(3–36), a peptide that inhibits food intake by activating the Y2 receptor (Y2R). PYY levels are elevated after bariatric surgery and have been proposed to contribute to reduced food intake and weight loss observed after metabolic surgery. Preclinical studies of metabolic surgery in mice with inactivation of PYY or its receptor yield conflicting results, with some supporting an important role for PYY in weight loss [103], yet others demonstrating that signaling through Y2R is dispensable for bariatric surgery-induced weight loss [104]. PYY administration has been explored alone, or in combination, for treating obesity. Cyclization of PYY(3–36) followed by antibody conjugation or PEGylation generated a long-acting PYY analog that produced a sustained anorectic response, weight loss, and attenuated emesis when administered for 21 days to obese rhesus macaques [105]. Adding liraglutide for the last 5 days of the treatment regimen produced additional reductions in food intake and weight loss. Potent long-acting acylated and PEGylated degradation-resistant PYY analogs produce impressive sustained reduction of food intake and weight loss when administered alone and in combination with concomitantly administered GLP-1R agonists over several weeks in high-fat diet-fed mice [106]; however, similarly potent unimolecular PYY-GLP-1 co-agonists have not yet been developed for clinical investigation.
Short-term (150 min) infusions of PYY alone reduce food ingestion in overweight human subjects, and further reductions are observed when PYY is co-infused with GLP-1 or oxyntomodulin [107,108]. A combined subcutaneous infusion (over 12 h each day) of native GLP-1, oxyntomodulin, and PYY for 28 days to overweight human subjects with prediabetes or diabetes produced a weight loss of 4 kg, together with a reduction in the mean amplitude of glycemic excursion [109]. Intranasal administration of 200 or 600 μg PYY(3–36) three times daily before each meal for 12 weeks in human subjects with obesity failed to exhibit either a dose-dependent or meaningful reduction in body weight [110]. Hence, the available human evidence is insufficient to support the use of PYY alone or in combination with other peptides as an important pharmacological regulator of weight loss in humans.
10. GLP-1-directed pharmacology for glucocorticoid, estrogen, or thyroid hormones
Peptide hormones such as GLP-1 and glucagon have also been used to selectively target G protein-coupled receptors and deliver steroid hormones as cargo to specific cell types in preclinical studies. Conjugation of GLP-1 and the glucocorticoid hormone dexamethasone produced striking weight loss through a combination of reduced food intake and increased energy expenditure in obese mice, while reducing inflammation in the brain and peripheral organs, findings associated with improvement in insulin sensitivity [111]. Notably, the GLP-1-dexamethasone conjugate improved glucose metabolism via the β cell GLP-1R without suppressing the hypothalamic pituitary axis or impairing bone turnover and density [111]. A GLP-1R-estrogen conjugate designed to deliver estrogen to GLP-1R + cells produced robust weight loss in mice without evidence of systemic estrogen action as assessed through analysis of uterine weight and the growth of estrogen-dependent breast cancer xenografts [112]. Genetic analyses in mice suggested that these actions were mediated through central nervous system GLP-1Rs and associated with the induction of POMC and leptin receptor expression in the arcuate nucleus [112]. β cell-selective delivery of estrogen achieved via a GLP-1-estrogen conjugate improved the viability of mouse and human β cells [113] without evidence of systemic actions of estrogen in vivo. Metabolic benefits encompassing weight loss, resolution of hepatic fat and inflammation, correction of experimental dyslipidemia, and attenuation of atherosclerosis in Western diet-fed and Ldlr−/− mice have also been observed following the administration of a glucagon-3,3′,5-triiodothyronine (T3) conjugate [114]. These actions were associated with increased energy expenditure, required the GCGR and hepatic expression of the thyroid hormone receptor beta gene, were evident in mouse models of NASH, and were not associated with evidence of systemic hyperthyroidism [114]. Whether one or more of these steroid-peptide hormone conjugates will enter clinical development remains uncertain.
11. Pitfalls and data limitations
The available evidence provides strong support, based on preclinical studies, for developing GLP-1-based co-agonists, yet the clinical progress for producing these compounds remains limited. The leading co-agonist, tirzepatide, is being examined in phase 3 clinical trials for diabetes and obesity, rekindling interest in how GIPR signaling interacts favorably with GLP-1R agonism. A number of issues merit consideration in understanding the preclinical-clinical gaps. First, it is likely that some compounds are administered in preclinical studies at doses that may be much higher on a relative basis than those tolerated in human studies. Most GLP-1-based peptide therapies produce nausea and vomiting in humans, adverse events that may not be evident in preclinical experiments. The impressive weight loss observed with several peptides in mice often reflects contributions from sympathetic nervous system engagement, BAT activation, and induction of energy expenditure, metabolic events that have rarely been recapitulated in sustained human studies. For example, GLP-1 increases sympathetic nervous system activity [115] and energy expenditure in animal experiments [116,117], but not in humans with T2D or obesity [[118], [119], [120], [121], [122]]. Similar findings relate to glucagon-containing agonists that robustly activate BAT and energy expenditure in mice [46,48,50], yet these mechanisms have not made appreciable contributions to weight loss in human studies. Consistent with the lack of effect of gut peptides on the metabolic rate in humans, energy expenditure was not different in human subjects experiencing weight loss after Roux-en-Y gastric bypass (RYGB) [123], a condition known to be associated with elevated circulating levels of multiple gut peptides.
Although GLP-1R agonists increase heart rate, long-acting GLP-1R agonists have been shown to be cardioprotective in those with T2D. Little is known about the cardiovascular actions of most candidate peptides being investigated as partners for GLP-1. Preclinical studies in mice demonstrate little impact of GIPR agonism on outcomes in mice with experimental myocardial infarction, whereas genetic disruption of the Gipr in all tissues, or selectively in cardiomyocytes, was associated with reduced infarct size and improved survival [124]. Observational studies in 8,044 subjects linked higher fasting levels of GIP with an increased risk of cardiovascular disease and all-cause mortality [125]. Similarly, GIP levels were higher in subjects with peripheral artery disease; however, adenoviral GIP expression exerted anti-inflammatory actions and reduced atherosclerosis in Western diet-fed ApoE-/- mice [126]. The available data are insufficient to predict the outcomes of modifying GIPR signaling in human subjects with diabetes or obesity exposed chronically to GIPR-based co-agonists.
Little information informs the potential actions of amylin in the human cardiovascular system. Cardiovascular outcome studies were not required for the approval of pramlintide, and the available preclinical data are insufficient to predict whether amylin agonism will impact cardiovascular pathophysiology in susceptible individuals. Glucagon is known to exhibit acute chronotropic and inotropic actions in animals and humans [127]; however, these actions do not appear to be sustained in human subjects. Although acute GCG administration is deleterious in a mouse model of myocardial infarction, findings dependent on the cardiomyocyte GCGR [128], adult human ventricles do not exhibit meaningful expression of GCGR mRNA transcripts [129]. Hence, additional analysis of the cardiovascular safety of putative clinically approved GCG-containing co-agonists is warranted. The available information suggests that the benefits of weight loss, blood pressure reduction, and improved glycemic control with new GLP-1-based co-agonists are unlikely to pose additional risks for cardiovascular safety in humans.
12. Summary
The preceding overview represents a partial summary of combinatorial mechanisms with efficacy in preclinical studies. Numerous additional GLP-1 co-administration strategies have demonstrated benefits in animals, including neurotensin-GLP-1 combinations for obesity and NASH [130], melanocortin-4 and GLP-1R co-administration for obesity and diabetes [131], and unimolecular combinations of a proprotein convertase subtilisin/kexin type 9 inhibitor and a GLP-1R agonist for subjects at high risk of diabetes, obesity, and cardiovascular disease [132]. While unimolecular co-agonists present unique advantages in regard to manufacturing, simplicity of dosing, and clinical development, it can be difficult to predict the optimal ratio of each peptide agonist to maximize the benefits of the combination in humans, and interpreting unanticipated adverse events ensuing from the administration of a novel multi-agonist can be difficult.
While preclinical studies of many co-agonists often generate exciting findings with robust weight loss coupled with excellent glycemic control, clinical progress has been slow and more difficult [133]. Notably, while recent progress with co-agonists such as tirzepatide has been impressive, higher doses of semaglutide achieved greater than 15% weight loss in investigational studies of human subjects with obesity, raising the bar for co-agonist efficacy. Nevertheless, the substantial proven benefits of GLP-1 action coupled with emerging preclinical and clinical data strongly suggest that multiple highly efficacious GLP-1-based co-agonists are likely to be approved for the treatment of metabolic diseases such as diabetes, obesity and NASH.
Acknowledgments
D.J.D. is supported by CIHR grant 154321, investigator-initiated studies of peptide hormone action sponsored by Novo Nordisk, a Banting and Best Diabetes Center-Novo Nordisk Chair in Incretin Biology, and the Novo Nordisk Foundation-Mt. Sinai Hospital fund for the study of gut peptides.
Conflict of interest
D.J.D. has been a consultant or speaker for Forkhead Therapeutics, Intarcia, Kallyope, Merck, and Novo Nordisk in the last 12 months. Mt. Sinai Hospital has received grants from Merck, Novo Nordisk, and Takeda for investigator-initiated preclinical studies of glucagon-like peptide action in the Drucker lab. D.J.D. does not hold stock or equity in any of these companies.
References
- 1.Drucker D.J., Habener J.F., Holst J.J. Discovery, characterization, and clinical development of the glucagon-like peptides. Journal of Clinical Investigation. 2017;127(12):4217–4227. doi: 10.1172/JCI97233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schauer P.R., Bhatt D.L., Kirwan J.P., Wolski K., Aminian A., Brethauer S.A. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. New England Journal of Medicine. 2017;376(7):641–651. doi: 10.1056/NEJMoa1600869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman S.L., Neuschwander-Tetri B.A., Rinella M., Sanyal A.J. Mechanisms of NAFLD development and therapeutic strategies. Nature Medicine. 2018;24(7):908–922. doi: 10.1038/s41591-018-0104-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts G.P., Larraufie P., Richards P., Kay R.G., Galvin S.G., Miedzybrodzka E.L. Comparison of human and murine enteroendocrine cells by transcriptomic and peptidomic profiling. Diabetes. 2019;68(5):1062–1072. doi: 10.2337/db18-0883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beumer J., Puschhof J., Bauza-Martinez J., Martinez-Silgado A., Elmentaite R., James K.R. High-resolution mRNA and secretome atlas of human enteroendocrine cells. Cell. 2020;181(6):1291–1306. doi: 10.1016/j.cell.2020.04.036. e1219. [DOI] [PubMed] [Google Scholar]
- 6.Drucker D.J. Evolving concepts and translational relevance of enteroendocrine cell biology. Journal of Clinical Endocrinology & Metabolism. 2016;101(3):778–786. doi: 10.1210/jc.2015-3449. [DOI] [PubMed] [Google Scholar]
- 7.Sandoval D.A., D'Alessio D.A. Physiology of proglucagon peptides: role of glucagon and GLP-1 in health and disease. Physiological Reviews. 2015;95(2):513–548. doi: 10.1152/physrev.00013.2014. [DOI] [PubMed] [Google Scholar]
- 8.le Roux C.W., Aylwin S.J., Batterham R.L., Borg C.M., Coyle F., Prasad V. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Annals of Surgery. 2006;243(1):108–114. doi: 10.1097/01.sla.0000183349.16877.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Madsbad S., Dirksen C., Holst J.J. Mechanisms of changes in glucose metabolism and bodyweight after bariatric surgery. Lancet Diabetes Endocrinol. 2014;2(2):152–164. doi: 10.1016/S2213-8587(13)70218-3. [DOI] [PubMed] [Google Scholar]
- 10.Boyle C.N., Lutz T.A., Le Foll C. Amylin - its role in the homeostatic and hedonic control of eating and recent developments of amylin analogs to treat obesity. Molecular Metabolism. 2018:8203–8210. doi: 10.1016/j.molmet.2017.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lutz T.A., Mollet A., Rushing P.A., Riediger T., Scharrer E. The anorectic effect of a chronic peripheral infusion of amylin is abolished in area postrema/nucleus of the solitary tract (AP/NTS) lesioned rats. International Journal of Obesity and Related Metabolic Disorders. 2001;25(7):1005–1011. doi: 10.1038/sj.ijo.0801664. [DOI] [PubMed] [Google Scholar]
- 12.Cheng W., Gonzalez I., Pan W., Tsang A.H., Adams J., Ndoka E. Calcitonin receptor neurons in the mouse nucleus tractus solitarius control energy balance via the non-aversive suppression of feeding. Cell Metabolism. 2020;31(2):301–312. doi: 10.1016/j.cmet.2019.12.012. e305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coester B., Koester-Hegmann C., Lutz T.A., Le Foll C. Amylin/calcitonin receptor-mediated signaling in POMC neurons influences energy balance and locomotor activity in chow-fed male mice. Diabetes. 2020;69(6):1110–1125. doi: 10.2337/db19-0849. [DOI] [PubMed] [Google Scholar]
- 14.Roth J.D., Roland B.L., Cole R.L., Trevaskis J.L., Weyer C., Koda J.E. Leptin responsiveness restored by amylin agonism in diet-induced obesity: evidence from nonclinical and clinical studies. Proceedings of the National Academy of Sciences of the U S A. 2008;105(20):7257–7262. doi: 10.1073/pnas.0706473105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trevaskis J.L., Coffey T., Cole R., Lei C., Wittmer C., Walsh B. Amylin-mediated restoration of leptin responsiveness in diet-induced obesity: magnitude and mechanisms. Endocrinology. 2008;149(11):5679–5687. doi: 10.1210/en.2008-0770. [DOI] [PubMed] [Google Scholar]
- 16.Le Foll C., Johnson M.D., Dunn-Meynell A.A., Boyle C.N., Lutz T.A., Levin B.E. Amylin-induced central IL-6 production enhances ventromedial hypothalamic leptin signaling. Diabetes. 2015;64(5):1621–1631. doi: 10.2337/db14-0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ravussin E., Smith S.R., Mitchell J.A., Shringarpure R., Shan K., Maier H. Enhanced weight loss with pramlintide/metreleptin: an integrated neurohormonal approach to obesity pharmacotherapy. Obesity (Silver Spring) 2009;17(9):1736–1743. doi: 10.1038/oby.2009.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chan J.L., Koda J., Heilig J.S., Cochran E.K., Gorden P., Oral E.A. Immunogenicity associated with metreleptin treatment in patients with obesity or lipodystrophy. Clinical Endocrinology. 2016;85(1):137–149. doi: 10.1111/cen.12980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aronne L.J., Halseth A.E., Burns C.M., Miller S., Shen L.Z. Enhanced weight loss following coadministration of pramlintide with sibutramine or phentermine in a multicenter trial. Obesity (Silver Spring) 2010;18(9):1739–1746. doi: 10.1038/oby.2009.478. [DOI] [PubMed] [Google Scholar]
- 20.Novo Nordisk Inc successfully completes AM833 phase 2 trial and phase 1 combination trial with AM833 and semaglutide in obesity. 2020. https://www.novonordisk.com/content/nncorp/global/en/news-and-media/news-and-ir-materials/news-details.html?id=274 Press Release June 18 2020. [Google Scholar]
- 21.Kopin A.S., Mathes W.F., McBride E.W., Nguyen M., Al-Haider W., Schmitz F. The cholecystokinin-A receptor mediates inhibition of food intake yet is not essential for the maintenance of body weight. Journal of Clinical Investigation. 1999;103(3):383–391. doi: 10.1172/JCI4901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jordan J., Greenway F.L., Leiter L.A., Li Z., Jacobson P., Murphy K. Stimulation of cholecystokinin-A receptors with GI181771X does not cause weight loss in overweight or obese patients. Clinical Pharmacology & Therapeutics. 2008;83(2):281–287. doi: 10.1038/sj.clpt.6100272. [DOI] [PubMed] [Google Scholar]
- 23.Trevaskis J.L., Sun C., Athanacio J., D'Souza L., Samant M., Tatarkiewicz K. Synergistic metabolic benefits of an exenatide analogue and cholecystokinin in diet-induced obese and leptin-deficient rodents. Diabetes, Obesity and Metabolism. 2015;17(1):61–73. doi: 10.1111/dom.12390. [DOI] [PubMed] [Google Scholar]
- 24.Christoffersen B.O., Skyggebjerg R.B., Bugge A., Kirk R.K., Vestergaard B., Uldam H.K. Long-acting CCK analogue NN9056 lowers food intake and body weight in obese Gottingen Minipigs. International Journal of Obesity. 2020;44(2):447–456. doi: 10.1038/s41366-019-0386-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hornigold D.C., Roth E., Howard V., Will S., Oldham S., Coghlan M.P. A GLP-1:CCK fusion peptide harnesses the synergistic effects on metabolism of CCK-1 and GLP-1 receptor agonism in mice. Appetite. 2018:127334–127340. doi: 10.1016/j.appet.2018.05.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scarlett J.M., Rojas J.M., Matsen M.E., Kaiyala K.J., Stefanovski D., Bergman R.N. Central injection of fibroblast growth factor 1 induces sustained remission of diabetic hyperglycemia in rodents. Nature Medicine. 2016;22(7):800–806. doi: 10.1038/nm.4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suh J.M., Jonker J.W., Ahmadian M., Goetz R., Lackey D., Osborn O. Endocrinization of FGF1 produces a neomorphic and potent insulin sensitizer. Nature. 2014;513(7518):436–439. doi: 10.1038/nature13540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scarlett J.M., Muta K., Brown J.M., Rojas J.M., Matsen M.E., Acharya N.K. Peripheral mechanisms mediating the sustained antidiabetic action of FGF1 in the brain. Diabetes. 2019;68(3):654–664. doi: 10.2337/db18-0498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bentsen M.A., Rausch D.M., Mirzadeh Z., Muta K., Scarlett J.M., Brown J.M. Transcriptomic analysis links diverse hypothalamic cell types to fibroblast growth factor 1-induced sustained diabetes remission. Nature Communications. 2020;11(1):4458. doi: 10.1038/s41467-020-17720-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu W., Struik D., Nies V.J., Jurdzinski A., Harkema L., de Bruin A. Effective treatment of steatosis and steatohepatitis by fibroblast growth factor 1 in mouse models of nonalcoholic fatty liver disease. Proceedings of the National Academy of Sciences of the U S A. 2016;113(8):2288–2293. doi: 10.1073/pnas.1525093113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Somm E., Jornayvaz F.R. Fibroblast growth factor 15/19: from basic functions to therapeutic perspectives. Endocrine Reviews. 2018;39(6):960–989. doi: 10.1210/er.2018-00134. [DOI] [PubMed] [Google Scholar]
- 32.DePaoli A.M., Zhou M., Kaplan D.D., Hunt S.C., Adams T.D., Learned R.M. FGF19 analog as a surgical factor mimetic that contributes to metabolic effects beyond glucose homeostasis. Diabetes. 2019;68(6):1315–1328. doi: 10.2337/db18-1305. [DOI] [PubMed] [Google Scholar]
- 33.Harrison S.A., Rinella M.E., Abdelmalek M.F., Trotter J.F., Paredes A.H., Arnold H.L. NGM282 for treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2018;391(10126):1174–1185. doi: 10.1016/S0140-6736(18)30474-4. [DOI] [PubMed] [Google Scholar]
- 34.Fazeli P.K., Lun M., Kim S.M., Bredella M.A., Wright S., Zhang Y. FGF21 and the late adaptive response to starvation in humans. Journal of Clinical Investigation. 2015;125(12):4601–4611. doi: 10.1172/JCI83349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gaich G., Chien J.Y., Fu H., Glass L.C., Deeg M.A., Holland W.L. The effects of LY2405319, an FGF21 analog, in obese human subjects with type 2 diabetes. Cell Metabolism. 2013;18(3):333–340. doi: 10.1016/j.cmet.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 36.Cui A., Li J., Ji S., Ma F., Wang G., Xue Y. The effects of B1344, a novel fibroblast growth factor 21 analog, on nonalcoholic steatohepatitis in nonhuman primates. Diabetes. 2020;69(8):1611–1623. doi: 10.2337/db20-0209. [DOI] [PubMed] [Google Scholar]
- 37.Kim A.M., Somayaji V.R., Dong J.Q., Rolph T.P., Weng Y., Chabot J.R. Once-weekly administration of a long-acting fibroblast growth factor 21 analogue modulates lipids, bone turnover markers, blood pressure and body weight differently in obese people with hypertriglyceridaemia and in non-human primates. Diabetes, Obesity and Metabolism. 2017;19(12):1762–1772. doi: 10.1111/dom.13023. [DOI] [PubMed] [Google Scholar]
- 38.Zhao L., Niu J., Lin H., Zhao J., Liu Y., Song Z. Paracrine-endocrine FGF chimeras as potent therapeutics for metabolic diseases. EBioMedicine. 2019:48462–48477. doi: 10.1016/j.ebiom.2019.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gilroy C.A., Capozzi M.E., Varanko A.K., Tong J., D'Alessio D.A., Campbell J.E. Sustained release of a GLP-1 and FGF21 dual agonist from an injectable depot protects mice from obesity and hyperglycemia. Science Advances. 2020;6(35) doi: 10.1126/sciadv.aaz9890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Du X., Kosinski J.R., Lao J., Shen X., Petrov A., Chicchi G.G. Differential effects of oxyntomodulin and GLP-1 on glucose metabolism. American Journal of Physiology. Endocrinology and Metabolism. 2012;303(2):E265–E271. doi: 10.1152/ajpendo.00142.2012. [DOI] [PubMed] [Google Scholar]
- 41.Henderson S.J., Konkar A., Hornigold D.C., Trevaskis J.L., Jackson R., Fritsch Fredin M. Robust anti-obesity and metabolic effects of a dual GLP-1/glucagon receptor peptide agonist in rodents and non-human primates. Diabetes, Obesity and Metabolism. 2016;18(12):1176–1190. doi: 10.1111/dom.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boland M.L., Laker R.C., Mather K., Nawrocki A., Oldham S., Boland B.B. Resolution of NASH and hepatic fibrosis by the GLP-1R/GcgR dual-agonist Cotadutide via modulating mitochondrial function and lipogenesis. Nat Metab. 2020;2(5):413–431. doi: 10.1038/s42255-020-0209-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kosinski J.R., Hubert J., Carrington P.E., Chicchi G.G., Mu J., Miller C. The glucagon receptor is involved in mediating the body weight-lowering effects of oxyntomodulin. Obesity (Silver Spring) 2012;20(8):1566–1571. doi: 10.1038/oby.2012.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim T., Holleman C.L., Nason S., Arble D.M., Ottaway N., Chabenne J. Hepatic glucagon receptor signaling enhances insulin-stimulated glucose disposal in rodents. Diabetes. 2018;67(11):2157–2166. doi: 10.2337/db18-0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Habegger K.M., Stemmer K., Cheng C., Muller T.D., Heppner K.M., Ottaway N. Fibroblast growth factor 21 mediates specific glucagon actions. Diabetes. 2013;62(5):1453–1463. doi: 10.2337/db12-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beaudry J.L., Kaur K.D., Varin E.M., Baggio L.L., Cao X., Mulvihill E.E. The brown adipose tissue glucagon receptor is functional but not essential for control of energy homeostasis in mice. Molecular Metabolism. 2019:2237–2248. doi: 10.1016/j.molmet.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salem V., Izzi-Engbeaya C., Coello C., Thomas D.B., Chambers E.S., Comninos A.N. Glucagon increases energy expenditure independently of brown adipose tissue activation in humans. Diabetes, Obesity and Metabolism. 2016;18(1):72–81. doi: 10.1111/dom.12585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Day J.W., Ottaway N., Patterson J.T., Gelfanov V., Smiley D., Gidda J. A new glucagon and GLP-1 co-agonist eliminates obesity in rodents. Nature Chemical Biology. 2009;5(10):749–757. doi: 10.1038/nchembio.209. [DOI] [PubMed] [Google Scholar]
- 49.Elvert R., Bossart M., Herling A.W., Weiss T., Zhang B., Kannt A. Team players or opponents: coadministration of selective glucagon and GLP-1 receptor agonists in obese diabetic monkeys. Endocrinology. 2018;159(8):3105–3119. doi: 10.1210/en.2018-00399. [DOI] [PubMed] [Google Scholar]
- 50.Finan B., Yang B., Ottaway N., Smiley D.L., Ma T., Clemmensen C. A rationally designed monomeric peptide triagonist corrects obesity and diabetes in rodents. Nature Medicine. 2015;21(1):27–36. doi: 10.1038/nm.3761. [DOI] [PubMed] [Google Scholar]
- 51.Longuet C., Sinclair E.M., Maida A., Baggio L.L., Maziarz M., Charron M.J. The glucagon receptor is required for the adaptive metabolic response to fasting. Cell Metabolism. 2008;8(5):359–371. doi: 10.1016/j.cmet.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tillner J., Posch M.G., Wagner F., Teichert L., Hijazi Y., Einig C. A novel dual glucagon-like peptide and glucagon receptor agonist SAR425899: results of randomized, placebo-controlled first-in-human and first-in-patient trials. Diabetes, Obesity and Metabolism. 2019;21(1):120–128. doi: 10.1111/dom.13494. [DOI] [PubMed] [Google Scholar]
- 53.Ambery P., Parker V.E., Stumvoll M., Posch M.G., Heise T., Plum-Moerschel L. MEDI0382, a GLP-1 and glucagon receptor dual agonist, in obese or overweight patients with type 2 diabetes: a randomised, controlled, double-blind, ascending dose and phase 2a study. Lancet. 2018;391(10140):2607–2618. doi: 10.1016/S0140-6736(18)30726-8. [DOI] [PubMed] [Google Scholar]
- 54.Nair K.S. Hyperglucagonemia increases resting metabolic rate in man during insulin deficiency. Journal of Clinical Endocrinology & Metabolism. 1987;64(5):896–901. doi: 10.1210/jcem-64-5-896. [DOI] [PubMed] [Google Scholar]
- 55.Tan T., Behary P., Tharakan G., Minnion J., Al-Najim W., Albrechtsen N.J.W. The effect of a subcutaneous infusion of GLP-1, OXM, and PYY on energy intake and expenditure in obese volunteers. Journal of Clinical Endocrinology & Metabolism. 2017;102(7):2364–2372. doi: 10.1210/jc.2017-00469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cegla J., Troke R.C., Jones B., Tharakan G., Kenkre J., McCullough K.A. Coinfusion of low-dose GLP-1 and glucagon in man results in a reduction in food intake. Diabetes. 2014;63(11):3711–3720. doi: 10.2337/db14-0242. [DOI] [PubMed] [Google Scholar]
- 57.Tan T.M., Field B.C., McCullough K.A., Troke R.C., Chambers E.S., Salem V. Coadministration of glucagon-like peptide-1 during glucagon infusion in man results in increased energy expenditure and amelioration of hyperglycemia. Diabetes. 2013;62(4):1131–1138. doi: 10.2337/db12-0797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Visentin R., Schiavon M., Gobel B., Riz M., Cobelli C., Klabunde T. Dual glucagon-like peptide-1 receptor/glucagon receptor agonist SAR425899 improves beta-cell function in type 2 diabetes. Diabetes, Obesity and Metabolism. 2020;22(4):640–647. doi: 10.1111/dom.13939. [DOI] [PubMed] [Google Scholar]
- 59.Parker V.E.R., Robertson D., Wang T., Hornigold D.C., Petrone M., Cooper A.T. Efficacy, safety, and mechanistic insights of cotadutide, a dual receptor glucagon-like peptide-1 and glucagon agonist. Journal of Clinical Endocrinology & Metabolism. 2020;105(3) doi: 10.1210/clinem/dgz047. [DOI] [PubMed] [Google Scholar]
- 60.Drucker D.J. Advances in oral peptide therapeutics. Nature Reviews Drug Discovery. 2020;19(4):277–289. doi: 10.1038/s41573-019-0053-0. [DOI] [PubMed] [Google Scholar]
- 61.Campbell J.E., Drucker D.J. Pharmacology physiology and mechanisms of incretin hormone action. Cell Metabolism. 2013;17(4):819–837. doi: 10.1016/j.cmet.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 62.Christensen M.B., Calanna S., Holst J.J., Vilsboll T., Knop F.K. Glucose-dependent insulinotropic polypeptide: blood glucose stabilizing effects in patients with type 2 diabetes. Journal of Clinical Endocrinology & Metabolism. 2014;99(3):E418–E426. doi: 10.1210/jc.2013-3644. [DOI] [PubMed] [Google Scholar]
- 63.Nissen A., Christensen M., Knop F.K., Vilsboll T., Holst J.J., Hartmann B. Glucose-dependent insulinotropic polypeptide inhibits bone resorption in humans. Journal of Clinical Endocrinology & Metabolism. 2014;99(11):E2325–E2329. doi: 10.1210/jc.2014-2547. [DOI] [PubMed] [Google Scholar]
- 64.Asmar M., Simonsen L., Madsbad S., Stallknecht B., Holst J.J., Bulow J. Glucose-dependent insulinotropic polypeptide may enhance fatty acid re-esterification in subcutaneous abdominal adipose tissue in lean humans. Diabetes. 2010;59(9):2160–2163. doi: 10.2337/db10-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Adriaenssens A.E., Biggs E.K., Darwish T., Tadross J., Sukthankar T., Girish M. Glucose-dependent insulinotropic polypeptide receptor-expressing cells in the hypothalamus regulate food intake. Cell Metabolism. 2019;30(5):987–996. doi: 10.1016/j.cmet.2019.07.013. e986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mroz P.A., Finan B., Gelfanov V., Yang B., Tschop M.H., DiMarchi R.D. Optimized GIP analogs promote body weight lowering in mice through GIPR agonism not antagonism. Molecular Metabolism. 2019:2051–2062. doi: 10.1016/j.molmet.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nauck M.A., Heimesaat M.M., Orskov C., Holst J.J., Ebert R., Creutzfeldt W. Preserved incretin activity of glucagon-like peptide 1 [7-36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. Journal of Clinical Investigation. 1993:91301–91307. doi: 10.1172/JCI116186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vilsboll T., Krarup T., Madsbad S., Holst J.J. Defective amplification of the late phase insulin response to glucose by GIP in obese Type II diabetic patients. Diabetologia. 2002;45(8):1111–1119. doi: 10.1007/s00125-002-0878-6. [DOI] [PubMed] [Google Scholar]
- 69.Nasteska D., Harada N., Suzuki K., Yamane S., Hamasaki A., Joo E. Chronic reduction of GIP secretion alleviates obesity and insulin resistance under high-fat diet conditions. Diabetes. 2014;63(7):2332–2343. doi: 10.2337/db13-1563. [DOI] [PubMed] [Google Scholar]
- 70.Miyawaki K., Yamada Y., Ban N., Ihara Y., Tsukiyama K., Zhou H. Inhibition of gastric inhibitory polypeptide signaling prevents obesity. Nature Medicine. 2002;8(7):738–742. doi: 10.1038/nm727. [DOI] [PubMed] [Google Scholar]
- 71.Althage M.C., Ford E.L., Wang S., Tso P., Polonsky K.S., Wice B.M. Targeted ablation of glucose-dependent insulinotropic polypeptide-producing cells in transgenic mice reduces obesity and insulin resistance induced by a high fat diet. Journal of Biological Chemistry. 2008;283(26):18365–18376. doi: 10.1074/jbc.M710466200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fulurija A., Lutz T.A., Sladko K., Osto M., Wielinga P.Y., Bachmann M.F. Vaccination against GIP for the treatment of obesity. PloS One. 2008;3(9):e3163. doi: 10.1371/journal.pone.0003163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Killion E.A., Wang J., Yie J., Shi S.D., Bates D., Min X. Anti-obesity effects of GIPR antagonists alone and in combination with GLP-1R agonists in preclinical models. Science Translational Medicine. 2018;10(472) doi: 10.1126/scitranslmed.aat3392. [DOI] [PubMed] [Google Scholar]
- 74.Hojberg P.V., Vilsboll T., Rabol R., Knop F.K., Bache M., Krarup T. Four weeks of near-normalisation of blood glucose improves the insulin response to glucagon-like peptide-1 and glucose-dependent insulinotropic polypeptide in patients with type 2 diabetes. Diabetologia. 2009;52(2):199–207. doi: 10.1007/s00125-008-1195-5. [DOI] [PubMed] [Google Scholar]
- 75.Aaboe K., Knop F.K., Vilsboll T., Volund A., Simonsen U., Deacon C.F. KATP channel closure ameliorates the impaired insulinotropic effect of glucose-dependent insulinotropic polypeptide in patients with type 2 diabetes. Journal of Clinical Endocrinology & Metabolism. 2009;94(2):603–608. doi: 10.1210/jc.2008-1731. [DOI] [PubMed] [Google Scholar]
- 76.Aaboe K., Akram S., Deacon C.F., Holst J.J., Madsbad S., Krarup T. Restoration of the insulinotropic effect of glucose-dependent insulinotropic polypeptide contributes to the antidiabetic effect of dipeptidyl peptidase-4 inhibitors. Diabetes, Obesity and Metabolism. 2015;17(1):74–81. doi: 10.1111/dom.12395. [DOI] [PubMed] [Google Scholar]
- 77.Finan B., Ma T., Ottaway N., Muller T.D., Habegger K.M., Heppner K.M. Unimolecular dual incretins maximize metabolic benefits in rodents, monkeys, and humans. Science Translational Medicine. 2013;5(209) doi: 10.1126/scitranslmed.3007218. 209ra151. [DOI] [PubMed] [Google Scholar]
- 78.Irwin N., Hunter K., Frizzell N., Flatt P.R. Antidiabetic effects of sub-chronic activation of the GIP receptor alone and in combination with background exendin-4 therapy in high fat fed mice. Regulatory Peptides. 2009;153(1–3):70–76. doi: 10.1016/j.regpep.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 79.Gault V.A., Kerr B.D., Harriott P., Flatt P.R. Administration of an acylated GLP-1 and GIP preparation provides added beneficial glucose-lowering and insulinotropic actions over single incretins in mice with Type 2 diabetes and obesity. Clinical Science. 2011;121(3):107–117. doi: 10.1042/CS20110006. [DOI] [PubMed] [Google Scholar]
- 80.Norregaard P.K., Deryabina M.A., Tofteng Shelton P., Fog J.U., Daugaard J.R., Eriksson P.O. A novel GIP analogue, ZP4165, enhances glucagon-like peptide-1-induced body weight loss and improves glycaemic control in rodents. Diabetes, Obesity and Metabolism. 2018;20(1):60–68. doi: 10.1111/dom.13034. [DOI] [PubMed] [Google Scholar]
- 81.Schmitt C., Portron A., Jadidi S., Sarkar N., DiMarchi R. Pharmacodynamics, pharmacokinetics and safety of multiple ascending doses of the novel dual glucose-dependent insulinotropic polypeptide/glucagon-like peptide-1 agonist RG7697 in people with type 2 diabetes mellitus. Diabetes, Obesity and Metabolism. 2017;19(10):1436–1445. doi: 10.1111/dom.13024. [DOI] [PubMed] [Google Scholar]
- 82.Portron A., Jadidi S., Sarkar N., DiMarchi R., Schmitt C. Pharmacodynamics, pharmacokinetics, safety and tolerability of the novel dual glucose-dependent insulinotropic polypeptide/glucagon-like peptide-1 agonist RG7697 after single subcutaneous administration in healthy subjects. Diabetes, Obesity and Metabolism. 2017;19(10):1446–1453. doi: 10.1111/dom.13025. [DOI] [PubMed] [Google Scholar]
- 83.Frias J.P., Bastyr E.J., 3rd Vignati L., Tschop M.H., Schmitt C., Owen K. The sustained effects of a dual GIP/GLP-1 receptor agonist, NNC0090-2746, in patients with type 2 diabetes. Cell Metabolism. 2017;26(2):343–352. doi: 10.1016/j.cmet.2017.07.011. e342. [DOI] [PubMed] [Google Scholar]
- 84.Coskun T., Sloop K.W., Loghin C., Alsina-Fernandez J., Urva S., Bokvist K.B. LY3298176, a novel dual GIP and GLP-1 receptor agonist for the treatment of type 2 diabetes mellitus: from discovery to clinical proof of concept. Mol Metab. 2018;18:3–14. doi: 10.1016/j.molmet.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Frias J.P., Nauck M.A., Van J., Kutner M.E., Cui X., Benson C. Efficacy and safety of LY3298176, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial. Lancet. 2018;392(10160):2180–2193. doi: 10.1016/S0140-6736(18)32260-8. [DOI] [PubMed] [Google Scholar]
- 86.Wilson J.M., Nikooienejad A., Robins D.A., Roell W.C., Riesmeyer J.S., Haupt A. Dual GIP and GLP-1 receptor agonist, tirzepatide, improves lipoprotein biomarkers associated with insulin resistance and cardiovascular risk in patients with type 2 diabetes. Diabetes, Obesity and Metabolism. 2020 doi: 10.1111/dom.14174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hartman M.L., Sanyal A.J., Loomba R., Wilson J.M., Nikooienejad A., Bray R. Effects of novel dual GIP and GLP-1 receptor agonist tirzepatide on biomarkers of nonalcoholic steatohepatitis in patients with type 2 diabetes. Diabetes Care. 2020;43(6):1352–1355. doi: 10.2337/dc19-1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Frias J.P., Nauck M.A., Van J., Benson C., Bray R., Cui X. Efficacy and tolerability of tirzepatide, a dual glucose-dependent insulinotropic peptide and glucagon-like peptide-1 receptor agonist in patients with type 2 diabetes: a 12-week, randomized, double-blind, placebo-controlled study to evaluate different dose-escalation regimens. Diabetes, Obesity and Metabolism. 2020;22(6):938–946. doi: 10.1111/dom.13979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Armstrong M.J., Gaunt P., Aithal G.P., Barton D., Hull D., Parker R. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387(10019):679–690. doi: 10.1016/S0140-6736(15)00803-X. [DOI] [PubMed] [Google Scholar]
- 90.Drucker D.J. The cardiovascular biology of glucagon-like peptide-1. Cell Metabolism. 2016;24(1):15–30. doi: 10.1016/j.cmet.2016.06.009. [DOI] [PubMed] [Google Scholar]
- 91.Killion E.A., Lu S.C., Fort M., Yamada Y., Veniant M.M., Lloyd D.J. Glucose-dependent insulinotropic polypeptide receptor therapies for the treatment of obesity, do agonists = antagonists? Endocrine Reviews. 2020;41(1) doi: 10.1210/endrev/bnz002. [DOI] [PubMed] [Google Scholar]
- 92.Holst J.J., Rosenkilde M.M. GIP as a therapeutic target in diabetes and obesity: insight from incretin Co-agonists. Journal of Clinical Endocrinology & Metabolism. 2020;105(8) doi: 10.1210/clinem/dgaa327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Aroda V.R., Rosenstock J., Wysham C., Unger J., Bellido D., Gonzalez-Galvez G. Efficacy and safety of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide in type 2 diabetes inadequately controlled on basal insulin and metformin: the LixiLan-L randomized trial. Diabetes Care. 2016;39(11):1972–1980. doi: 10.2337/dc16-1495. [DOI] [PubMed] [Google Scholar]
- 94.Billings L.K., Doshi A., Gouet D., Oviedo A., Rodbard H.W., Tentolouris N. Efficacy and safety of IDegLira versus basal-bolus insulin therapy in patients with type 2 diabetes uncontrolled on metformin and basal insulin: the DUAL VII randomized clinical trial. Diabetes Care. 2018;41(5):1009–1016. doi: 10.2337/dc17-1114. [DOI] [PubMed] [Google Scholar]
- 95.Blonde L., Rosenstock J., Del Prato S., Henry R., Shehadeh N., Frias J. Switching to iGlarLixi versus continuing daily or weekly GLP-1 RA in type 2 diabetes inadequately controlled by GLP-1 RA and oral antihyperglycemic therapy: the LixiLan-G randomized clinical trial. Diabetes Care. 2019;42(11):2108–2116. doi: 10.2337/dc19-1357. [DOI] [PubMed] [Google Scholar]
- 96.Linjawi S., Bode B.W., Chaykin L.B., Courreges J.P., Handelsman Y., Lehmann L.M. The efficacy of IDegLira (insulin degludec/liraglutide combination) in adults with type 2 diabetes inadequately controlled with a GLP-1 receptor agonist and oral therapy: DUAL III randomized clinical trial. Diabetes Therapy. 2017;8(1):101–114. doi: 10.1007/s13300-016-0218-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Feng X., Guan D., Auen T., Choi J.W., Salazar Hernandez M.A., Lee J. IL1R1 is required for celastrol's leptin-sensitization and antiobesity effects. Nature Medicine. 2019;25(4):575–582. doi: 10.1038/s41591-019-0358-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Muller T.D., Sullivan L.M., Habegger K., Yi C.X., Kabra D., Grant E. Restoration of leptin responsiveness in diet-induced obese mice using an optimized leptin analog in combination with exendin-4 or FGF21. Journal of Peptide Science. 2012;18(6):383–393. doi: 10.1002/psc.2408. [DOI] [PubMed] [Google Scholar]
- 99.Sakai T., Kusakabe T., Ebihara K., Aotani D., Yamamoto-Kataoka S., Zhao M. Leptin restores the insulinotropic effect of exenatide in a mouse model of type 2 diabetes with increased adiposity induced by streptozotocin and high-fat diet. American Journal of Physiology. Endocrinology and Metabolism. 2014;307(8):E712–E719. doi: 10.1152/ajpendo.00272.2014. [DOI] [PubMed] [Google Scholar]
- 100.Clemmensen C., Chabenne J., Finan B., Sullivan L., Fischer K., Kuchler D. GLP-1/glucagon coagonism restores leptin responsiveness in obese mice chronically maintained on an obesogenic diet. Diabetes. 2014;63(4):1422–1427. doi: 10.2337/db13-1609. [DOI] [PubMed] [Google Scholar]
- 101.Friedman J.M. Leptin and the endocrine control of energy balance. Nature Metabolism. 2019;1(8):754–764. doi: 10.1038/s42255-019-0095-y. [DOI] [PubMed] [Google Scholar]
- 102.Zhao S., Kusminski C.M., Elmquist J.K., Scherer P.E. Leptin: less is more. Diabetes. 2020;69(5):823–829. doi: 10.2337/dbi19-0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chandarana K., Gelegen C., Karra E., Choudhury A.I., Drew M.E., Fauveau V. Diet and gastrointestinal bypass-induced weight loss: the roles of ghrelin and peptide YY. Diabetes. 2011;60(3):810–818. doi: 10.2337/db10-0566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Boland B.B., Mumphrey M.B., Hao Z., Townsend R.L., Gill B., Oldham S. Combined loss of GLP-1R and Y2R does not alter progression of high-fat diet-induced obesity or response to RYGB surgery in mice. Molecular Metabolism. 2019:2564–2572. doi: 10.1016/j.molmet.2019.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rangwala S.M., D'Aquino K., Zhang Y.M., Bader L., Edwards W., Zheng S. A long-acting PYY3-36 analog mediates robust anorectic efficacy with minimal emesis in nonhuman primates. Cell Metabolism. 2019;29(4):837–843. doi: 10.1016/j.cmet.2019.01.017. e835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lear S., Pflimlin E., Zhou Z., Huang D., Weng S., Nguyen-Tran V. Engineering of a potent, long-acting NPY2R agonist for combination with a GLP-1R agonist as a multi-hormonal treatment for obesity. Journal of Medicinal Chemistry. 2020 doi: 10.1021/acs.jmedchem.0c00740. [DOI] [PubMed] [Google Scholar]
- 107.Schmidt J.B., Gregersen N.T., Pedersen S.D., Arentoft J.L., Ritz C., Schwartz T.W. Effects of PYY3-36 and GLP-1 on energy intake, energy expenditure, and appetite in overweight men. American Journal of Physiology. Endocrinology and Metabolism. 2014;306(11):E1248–E1256. doi: 10.1152/ajpendo.00569.2013. [DOI] [PubMed] [Google Scholar]
- 108.Field B.C., Wren A.M., Peters V., Baynes K.C., Martin N.M., Patterson M. PYY3-36 and oxyntomodulin can be additive in their effect on food intake in overweight and obese humans. Diabetes. 2010;59(7):1635–1639. doi: 10.2337/db09-1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Behary P., Tharakan G., Alexiadou K., Johnson N., Wewer Albrechtsen N.J., Kenkre J. Combined GLP-1, oxyntomodulin, and peptide YY improves body weight and glycemia in obesity and prediabetes/type 2 diabetes: a randomized, single-blinded, placebo-controlled study. Diabetes Care. 2019;42(8):1446–1453. doi: 10.2337/dc19-0449. [DOI] [PubMed] [Google Scholar]
- 110.Gantz I., Erondu N., Mallick M., Musser B., Krishna R., Tanaka W.K. Efficacy and safety of intranasal peptide YY3-36 for weight reduction in obese adults. Journal of Clinical Endocrinology & Metabolism. 2007;92(5):1754–1757. doi: 10.1210/jc.2006-1806. [DOI] [PubMed] [Google Scholar]
- 111.Quarta C., Clemmensen C., Zhu Z., Yang B., Joseph S.S., Lutter D. Molecular integration of incretin and glucocorticoid action reverses immunometabolic dysfunction and obesity. Cell Metabolism. 2017;26(4):620–632. doi: 10.1016/j.cmet.2017.08.023. e626. [DOI] [PubMed] [Google Scholar]
- 112.Finan B., Yang B., Ottaway N., Stemmer K., Muller T.D., Yi C.X. Targeted estrogen delivery reverses the metabolic syndrome. Nature Medicine. 2012;18(12):1847–1856. doi: 10.1038/nm.3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sachs S., Bastidas-Ponce A., Tritschler S., Bakhti M., Bottcher A., Sanchez-Garrido M.A. Targeted pharmacological therapy restores beta-cell function for diabetes remission. Nat Metab. 2020;2(2):192–209. doi: 10.1038/s42255-020-0171-3. [DOI] [PubMed] [Google Scholar]
- 114.Finan B., Clemmensen C., Zhu Z., Stemmer K., Gauthier K., Muller L. Chemical hybridization of glucagon and thyroid hormone optimizes therapeutic impact for metabolic disease. Cell. 2016;167(3):843–857. doi: 10.1016/j.cell.2016.09.014. e814. [DOI] [PubMed] [Google Scholar]
- 115.Yamamoto H., Lee C.E., Marcus J.N., Williams T.D., Overton J.M., Lopez M.E. Glucagon-like peptide-1 receptor stimulation increases blood pressure and heart rate and activates autonomic regulatory neurons. Journal of Clinical Investigation. 2002;110(1):43–52. doi: 10.1172/JCI15595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Osaka T., Endo M., Yamakawa M., Inoue S. Energy expenditure by intravenous administration of glucagon-like peptide-1 mediated by the lower brainstem and sympathoadrenal system. Peptides. 2005;26(9):1623–1631. doi: 10.1016/j.peptides.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 117.Lockie S.H., Heppner K.M., Chaudhary N., Chabenne J.R., Morgan D.A., Veyrat-Durebex C. Direct control of brown adipose tissue thermogenesis by central nervous system glucagon-like Peptide-1 receptor signaling. Diabetes. 2012;61(11):2753–2762. doi: 10.2337/db11-1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Janssen L.G.M., Nahon K.J., Bracke K.F.M., van den Broek D., Smit R., Sardjoe Mishre A.S.D. Twelve weeks of exenatide treatment increases [(18)F]fluorodeoxyglucose uptake by brown adipose tissue without affecting oxidative resting energy expenditure in nondiabetic males. Metabolism. 2020:106154167. doi: 10.1016/j.metabol.2020.154167. [DOI] [PubMed] [Google Scholar]
- 119.Bergmann N.C., Lund A., Gasbjerg L.S., Meessen E.C.E., Andersen M.M., Bergmann S. Effects of combined GIP and GLP-1 infusion on energy intake, appetite and energy expenditure in overweight/obese individuals: a randomised, crossover study. Diabetologia. 2019;62(4):665–675. doi: 10.1007/s00125-018-4810-0. [DOI] [PubMed] [Google Scholar]
- 120.Basolo A., Burkholder J., Osgood K., Graham A., Bundrick S., Frankl J. Exenatide has a pronounced effect on energy intake but not energy expenditure in non-diabetic subjects with obesity: a randomized, double-blind, placebo-controlled trial. Metabolism. 2018:85116–85125. doi: 10.1016/j.metabol.2018.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Blundell J., Finlayson G., Axelsen M., Flint A., Gibbons C., Kvist T. Effects of once-weekly semaglutide on appetite, energy intake, control of eating, food preference and body weight in subjects with obesity. Diabetes, Obesity and Metabolism. 2017;19(9):1242–1251. doi: 10.1111/dom.12932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.van Can J., Sloth B., Jensen C.B., Flint A., Blaak E.E., Saris W.H. Effects of the once-daily GLP-1 analog liraglutide on gastric emptying, glycemic parameters, appetite and energy metabolism in obese, non-diabetic adults. International Journal of Obesity. 2014;38(6):784–793. doi: 10.1038/ijo.2013.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schmidt J.B., Pedersen S.D., Gregersen N.T., Vestergaard L., Nielsen M.S., Ritz C. Effects of RYGB on energy expenditure, appetite and glycaemic control: a randomized controlled clinical trial. International Journal of Obesity. 2016;40(2):281–290. doi: 10.1038/ijo.2015.162. [DOI] [PubMed] [Google Scholar]
- 124.Ussher J.R., Campbell J.E., Mulvihill E.E., Baggio L.L., Bates H.E., McLean B.A. Inactivation of the glucose-dependent insulinotropic polypeptide receptor improves outcomes following experimental myocardial infarction. Cell Metabolism. 2018;27(2):450–460. doi: 10.1016/j.cmet.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 125.Jujic A., Atabaki-Pasdar N., Nilsson P.M., Almgren P., Hakaste L., Tuomi T. Glucose-dependent insulinotropic peptide and risk of cardiovascular events and mortality: a prospective study. Diabetologia. 2020;63(5):1043–1054. doi: 10.1007/s00125-020-05093-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kahles F., Liberman A., Halim C., Rau M., Mollmann J., Mertens R.W. The incretin hormone GIP is upregulated in patients with atherosclerosis and stabilizes plaques in ApoE(-/-) mice by blocking monocyte/macrophage activation. Mol Metab. 2018:14150–14157. doi: 10.1016/j.molmet.2018.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ali S., Drucker D.J. Benefits and limitations of reducing glucagon action for the treatment of type 2 diabetes. American Journal of Physiology. Endocrinology and Metabolism. 2009;296(3):E415–E421. doi: 10.1152/ajpendo.90887.2008. [DOI] [PubMed] [Google Scholar]
- 128.Ali S., Ussher J.R., Baggio L.L., Kabir M.G., Charron M.J., Ilkayeva O. Cardiomyocyte glucagon receptor signaling modulates outcomes in mice with experimental myocardial infarction. Molecular Metabolism. 2014;4(2):132–143. doi: 10.1016/j.molmet.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Baggio L.L., Yusta B., Mulvihill E.E., Cao X., Streutker C.J., Butany J. GLP-1 receptor expression within the human heart. Endocrinology. 2018;159(4):1570–1584. doi: 10.1210/en.2018-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ratner C., He Z., Grunddal K.V., Skov L.J., Hartmann B., Zhang F. Long-acting neurotensin synergizes with liraglutide to reverse obesity through a melanocortin-dependent pathway. Diabetes. 2019;68(6):1329–1340. doi: 10.2337/db18-1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Clemmensen C., Finan B., Fischer K., Tom R.Z., Legutko B., Sehrer L. Dual melanocortin-4 receptor and GLP-1 receptor agonism amplifies metabolic benefits in diet-induced obese mice. EMBO Molecular Medicine. 2015;7(3):288–298. doi: 10.15252/emmm.201404508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Jain M., Carlson G., Cook W., Morrow L., Petrone M., White N.E. Randomised, phase 1, dose-finding study of MEDI4166, a PCSK9 antibody and GLP-1 analogue fusion molecule, in overweight or obese patients with type 2 diabetes mellitus. Diabetologia. 2019;62(3):373–386. doi: 10.1007/s00125-018-4789-6. [DOI] [PubMed] [Google Scholar]
- 133.Sadry S.A., Drucker D.J. Emerging combinatorial hormone therapies for the treatment of obesity and T2DM. Nature Reviews Endocrinology. 2013;9(7):425–433. doi: 10.1038/nrendo.2013.47. [DOI] [PubMed] [Google Scholar]