This case series investigates ocular structural changes in 2 crew members who completed a 1-year–long mission as part of NASA’s One-Year Mission Study.
Key Points
Question
Are 6-month spaceflight missions sufficiently long to characterize the spaceflight-associated neuro-ocular syndrome risks of proposed longer-duration missions to the moon and Mars?
Findings
In a case series study of 2 crew members from a 1-year–long mission, 1 crew member developed mild optic disc edema after 270 days in spaceflight. In the other crew member, optic disc edema and choroid folds progressively worsened over the duration of the 1-year mission.
Meaning
Additional observations of crew members on missions longer than 6 months may be warranted to characterize spaceflight-associated neuro-ocular syndrome risks of extended duration spaceflight.
Abstract
Importance
While 6-month data are available regarding spaceflight-associated neuro-ocular syndrome, manned missions for 1 year and beyond are planned, warranting evaluation for spaceflight-associated neuro-ocular syndrome beyond 6 months.
Objective
To determine if the manifestation of spaceflight-associated neuro-ocular syndrome worsens during International Space Station missions exceeding the present 4- to 6-month duration.
Design, Setting, and Participants
The One-Year Mission Study used quantitative imaging modalities to investigate changes in ocular structure in 2 crew members who completed a 1-year–long spaceflight mission. This study investigated the ocular structure of crew members before, during, and after their mission on the International Space Station. Two crew members participated in this study from March 2015 to September 2016. Analysis began in March 2015 and ended in May 2020.
Exposures
Crew members were tested before, during, and up to 1 year after spaceflight.
Main Outcomes and Measures
This study compares ocular changes (peripapillary retinal edema, axial length, anterior chamber depth, and refraction) in two 1-year spaceflight mission crew members with cohort crew members from a 6-month mission (n = 11). Minimum rim width (the shortest distance between Bruch membrane opening and the internal limiting membrane) and peripapillary total retinal thickness were measured using optical coherence tomography.
Results
Both crew members were men. Minimum rim width and total retinal thickness increased in both participants throughout the duration of spaceflight exposure to the maximal observed change from preflight (minimum rim width: participant 1, 561 [+149 from preflight] μm at flight day 270; participant 2, 539 [+56 from preflight] μm at flight day 270; total retinal thickness: participant 1, 547 [+135 from preflight] μm at flight day 90; participant 2, 528 [+45 from preflight] μm at flight day 210). Changes in peripapillary choroid engorgement, axial length, and anterior chamber depth appeared similar between the 1-year mission participants and a 6-month mission cohort.
Conclusions and Relevance
This report documents the late development of mild optic disc edema in 1 crew member and the progressive development of choroidal folds and optic disc edema in another crew member over the duration of 1 year in low Earth orbit aboard the International Space Station. Previous reports characterized the ocular risk associated with 4 to 6 months of spaceflight. As future spaceflight missions are planned to increase in duration and extend beyond low Earth orbit, further observation of astronaut ocular health on spaceflight missions longer than 6 months in duration may be warranted.
Introduction
Spaceflight-associated neuro-ocular syndrome (SANS) develops in crew members during long-duration missions (>1 month of spaceflight)1,2 and is defined by the presentation of 1 or more of the following findings during or immediately following spaceflight: optic disc edema, chorioretinal folds, globe flattening, and hyperopic refractive error shift. Ophthalmic imaging demonstrates that Frisén grade optic disc edema develops in approximately 16% to 19% of crew members during and after long-duration spaceflight.3 More recently, optic disc edema as quantified by optical coherence tomography (OCT) has been documented in approximately 70% of crew members.4 Six-month spaceflights in low Earth orbit have resulted in peripapillary optic disc edema and choroid thickening that presented bilaterally and in male and female individuals.4 The incidence of SANS in crew members is concerning to the aerospace medicine community given that future spaceflight missions, for example to Mars, will exceed 6 months in duration.
We hypothesize SANS findings increase in magnitude during International Space Station missions longer than traditional missions of 4- to 6-months’ duration. In this study, we investigated ocular structural changes in 2 individuals who completed a 1-year–long mission as a part of NASA’s One-Year Mission Study.5,6
Methods
This study was approved by the NASA Johnson Space Center’s Institutional Review and Human Research Multilateral Review Boards and adhered to the Declaration of Helsinki.7 Informed written consent was obtained. Both 1-year–long mission crew members (participants 1 and 2) had similar prior spaceflight experience of 180 and 176 days, respectively, and cumulative total time in spaceflight of 520 and 516 days on conclusion of the 1-year–long mission, respectively. The 2 crew members participated in this study from March 2015 to September 2016. Methods used in this 1-year–long mission study have been previously described for 6-month spaceflight missions.4 In this study, ophthalmic imaging (before/after flight: CR-2 Plus AF; Cannon; inflight: OIS EyeScan; Ophthalmic Imaging Systems), optical biometry (before/after flight only: IOLMaster 500; Zeiss), and OCT (Spectralis; Heidelberg Engineering) data were collected 21 to 3 months before flight and in-flight within a 10-day window of flight days 10, 30, 90, 150, 210, 270, and 320. Postflight testing occurred within 7 days after landing, a 10-day window of the 30th and 90th day after returning, and 30-day window of the 180th and 365th day after returning. Because this study was limited to two 1-year–long mission crew members, statistical analyses were not conducted; however, figures presented here include both 1-year–long mission data and 6-month mission data from the larger Ocular Health study cohort4 (n = 11) for visual comparison. Bruch membrane folds were segmented by a single expert grader and verified by a second expert. Fold metrics were quantified based on deviation from a nondeformed Bruch membrane layer using MATLAB software (MathWorks).
Both participants underwent comprehensive eye examinations at the NASA Johnson Space Center Flight Medicine clinic, including ophthalmic imaging, OCT, cycloplegic refraction, and intraocular pressure and were cleared to participate in their assigned mission. Neither participant had a history of systemic disease (eg, hypertension, connective tissue disorders, iron deficiency, diabetes, or kidney disease) or reported use of medication (eg, vitamin A, tetracycline, corticosteroids, or nalidixic acid) that could produce elevated intracranial pressure. Analysis began in March 2015 and ended in May 2020.
Results
Preflight OCT images demonstrated preexisting bilateral macular choroidal folds in participant 1, likely associated with previous spaceflight. This study was not specifically designed to evaluate orbital edema, and abnormalities were not documented during routine examination. Quantitative OCT analysis of choroidal folds in both eyes of participant 1 highlights progressive development of macular choroidal folds with flight duration, characterized by development of new folds and deformation of existing folds (Figure 1; eFigure 1 in the Supplement). Reported values correspond with the B scan on which the maximum value occurred. Before spaceflight, there were 15 folds documented in the left eye and 18 folds documented in the right eye. Maximum fold height was 32 μm in the left eye and 29 μm in the right eye. Maximum fold width was 1240 μm in the left eye and 1289 μm in the right eye. Fold count (left eye, 18; right eye, 21) and maximum height (left eye, 50 μm; right eye, 36 μm) increased from before flight to flight day 150, while maximum width (left eye, 1229 μm; right eye, 1051 μm) decreased. From flight day 150 to 270, fold count (left eye, 21; right eye, 23) increased in both eyes, maximum height remained at 50 μm in the left eye and increased to 42 μm in the right eye, and maximum width decreased in both eyes (left eye, 816 μm; right eye, 941 μm). Maximum height decreased postflight but did not return to preflight values by 180 days postflight (fold count: left eye, 16; right eye, 17; maximum height: left eye, 43 μm; right eye, 41 μm; maximum width: left eye, 1172 μm; right eye, 1289 μm) or the 365-day postflight examination (fold count: left eye, 14; right eye, 17; maximum height: left eye, 45 μm; right eye, 38 μm; maximum width: left eye, 1086 μm; right eye, 1400 μm).
Figure 1. Optical Coherence Tomography Images of the Left Eye Show the Development of Macular Choroidal Folds in Flight.
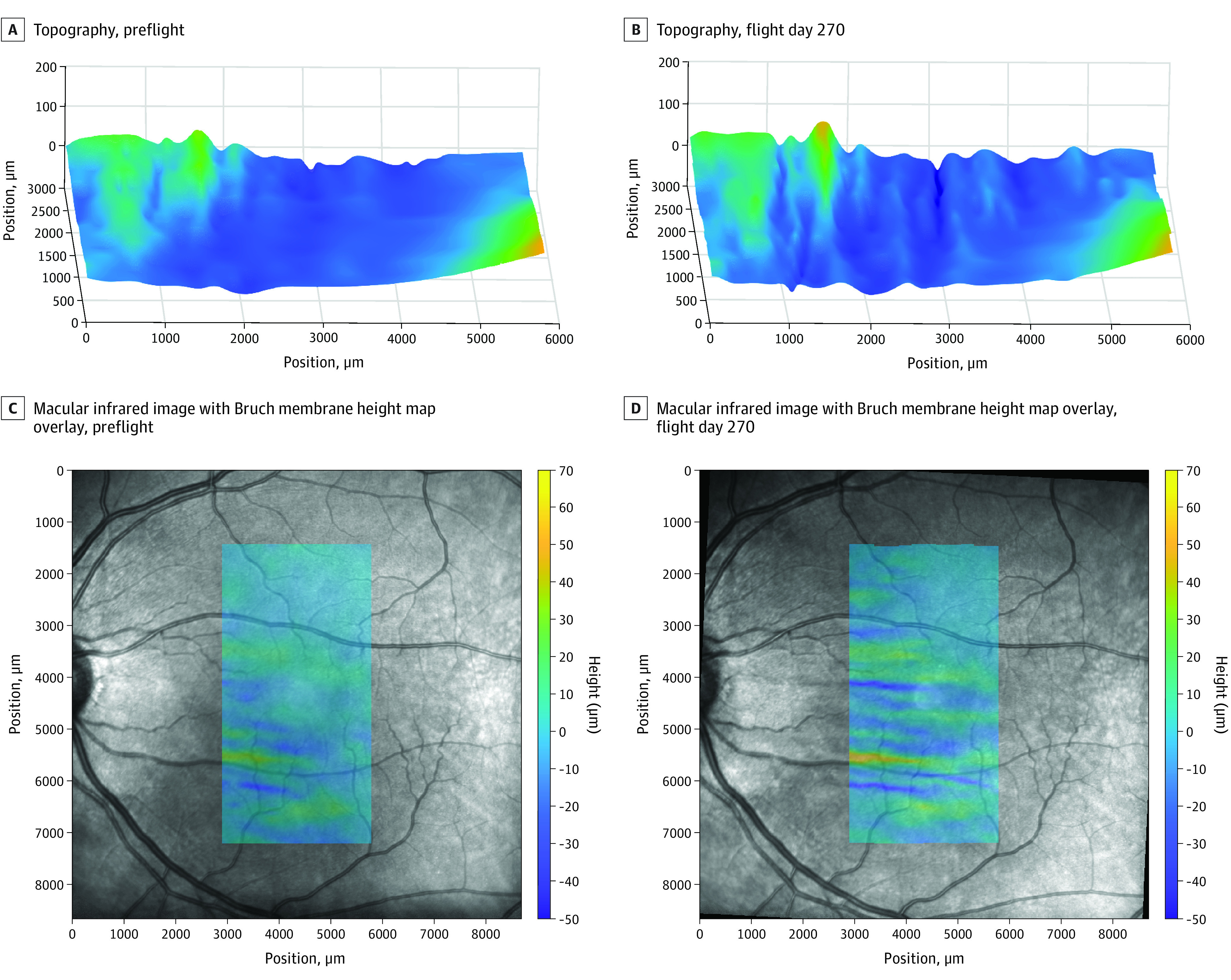
Macular choroidal folds progressively worsened in participant 1 throughout the 1-year–long mission. Bruch membrane was segmented by a single expert grader and verified by a second expert. Fold metrics were quantified based on deviation from a nondeformed Bruch membrane layer using MATLAB software (MathWorks). A and B, Bruch membrane topography (left side corresponds with the inferior side of images in C and D). C and D, Macular infrared image with Bruch membrane heightmap overlay. See eFigure 1 in the Supplement for an example of Bruch membrane segmentation.
Participant 1 first demonstrated Frisén grade 1 edema (modified Frisén Scale)8 in the right eye at flight day 30 that persisted until 90 days after return to Earth. On flight day 319, participant 2 displayed mild disc edema (Figure 2; eFigure 2 in the Supplement) that did not reach the threshold for Frisén grade 1 classification. This edema resolved within 30 days after return to Earth and was consistent with OCT measures of optic nerve head rim tissue thickness. Preflight minimum rim width in the right eye was 412 μm and 483 μm and increased by 149 μm and 56 μm on flight day 270 in participants 1 and 2, respectively. In the 6-month cohort, minimum rim width increased by a mean (SD) of 53 (24) μm to 395 (82) μm at flight day 150 (Figure 3A).
Figure 2. Fundus Images of Participant 2 Show Signs of Optic Disc Edema Late in Flight.
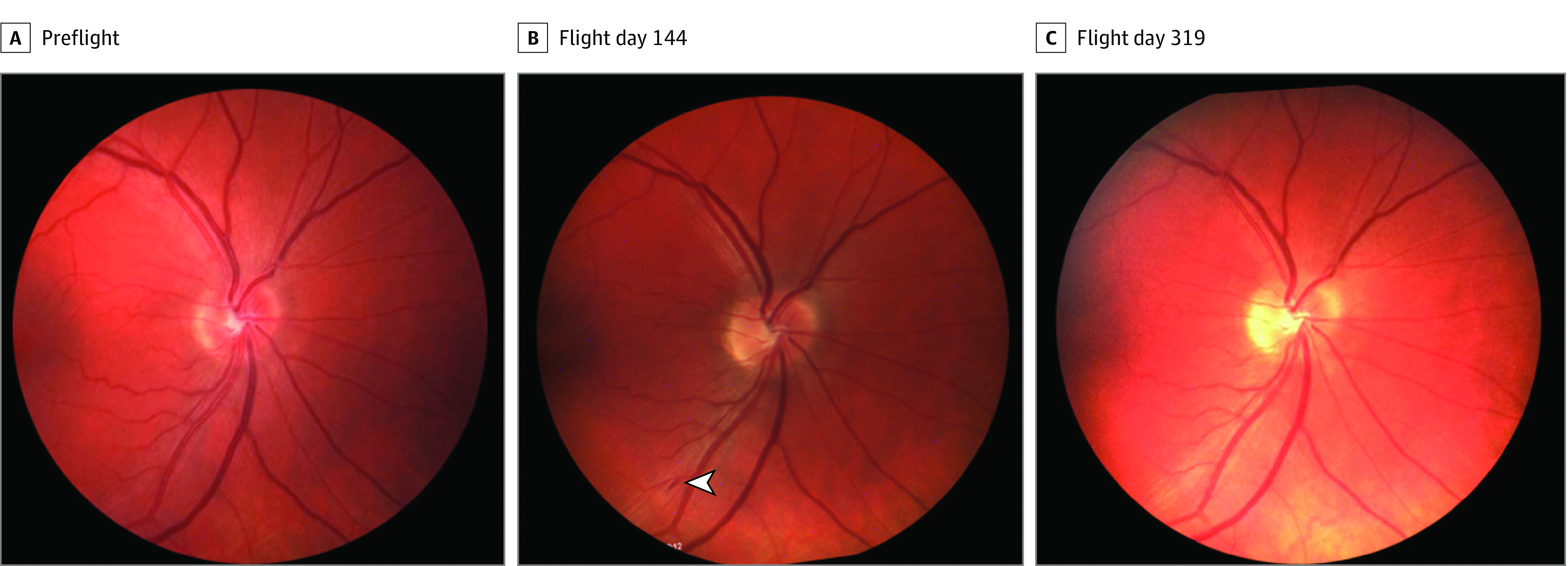
Ophthalmic images were acquired preflight and postflight (CR-2 Plus AF digital nonmydriatric retinal camera; Canon) and during flight (OIS EyeScan; Ophthalmic Imaging Systems). Participant 2 demonstrated mild disc edema and increased blurring of the superior and nasal disc margin in the right eye after 319 days of spaceflight. Optic disc edema in this participant resolved within 30 days of return to earth. In addition, participant 2 demonstrated evidence of an intraretinal flame hemorrhage along the inferotemporal arcade that presented after 83 days of spaceflight and resolved between spaceflight days 144 (arrowhead) and 208. See eFigure 2 in the Supplement for fundus images of participant 1 during flight.
Figure 3. Change in Minimum Rim Width and Total Retinal Thickness .
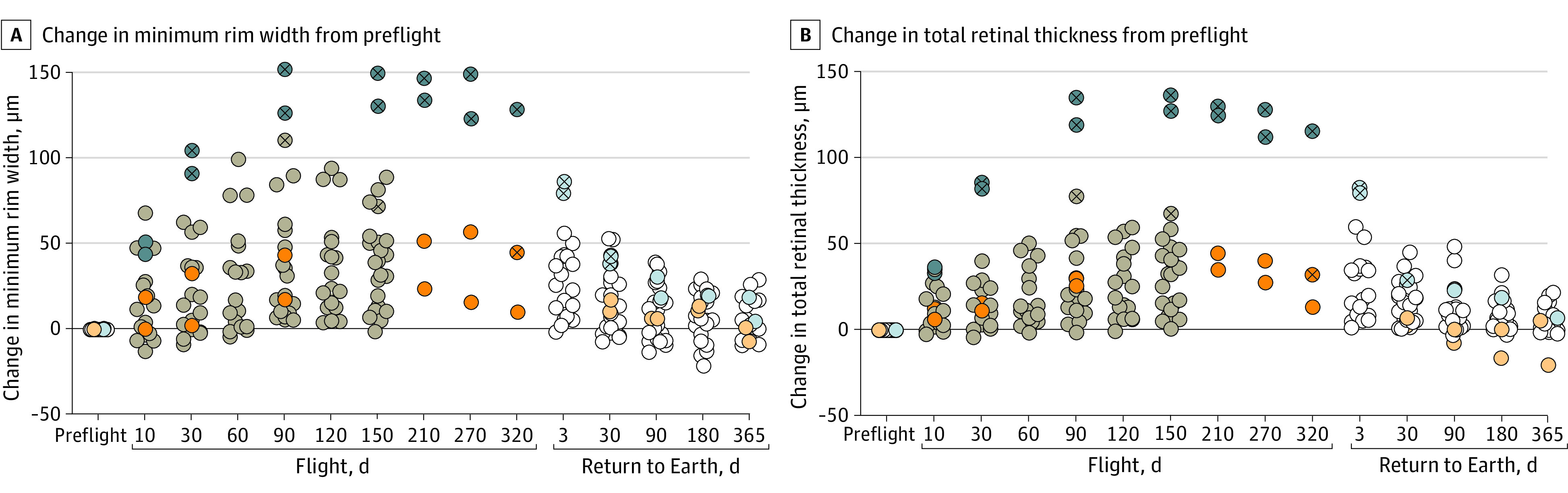
The change in minimum rim width (A) and global total retinal thickness (B) is compared with before spaceflight (preflight) for both eyes of each participant (circles). The open circles represent data collected before and after spaceflight in the 6-month cohort; gray circles, data collected during spaceflight in the 6-month cohort; blue circles, data collected from participant 1; orange circles, data collected from participant 2; and circles with a superimposed cross, an eye that had optic disc edema findings.
Both 1-year–long mission crew members demonstrated progressively greater global total retinal thickness (TRT) at the optic nerve head (Bruch membrane opening to 250 μm) with flight duration. In participant 1, TRT progressively increased to a maximum thickness of 547 μm (+135 μm from preflight) in the right eye by flight day 90 and remained elevated for the remainder of the mission. In participant 2, TRT increased to a maximum thickness of 528 μm (+45 μm from preflight) in the right eye on flight day 210 and remained elevated for the remainder of the mission. This TRT change exceeds our physiological variability and measurement error threshold.9 In 6-month crew members, TRT increased by a mean (SD) of 34 (19) μm to 415 (50) μm at flight day 150.4 TRT decreased in crew members after return to Earth but was still elevated in the right eye of participant 1 compared with before flight at 365 days after return to Earth (Figure 3B).
Similar to the 6-month cohort, spaceflight resulted in peripapillary choroidal engorgement (12° circle scan, without enhanced depth imaging) in both participants. Axial length magnitude of change (participant 1, −0.06 mm in the right eye and −0.08 mm in the left eye; participant 2, −0.02 mm in the right eye and −0.03 mm in the left eye) and anterior chamber depth (participant 1, −0.14 mm in the right eye and −0.20 mm in the left eye; participant 2, −0.19 mm in the right eye and −0.12 mm in the left eye) measured by optical biometry (IOL Master 500; Zeiss) in 1-year–long mission crew were similar to the 6-month spaceflight cohort,4 and both axial length and anterior chamber depth similarly remained lower than preflight values for up to 1 year after landing. Immediate postflight testing of participant 1 indicated a spherical equivalent shift of +0.25 diopters (D) in the right eye and +0.50 D in the left eye compared with preflight (right eye, +1.50 D; left eye, +1.75 D). Spherical equivalent returned to preflight values by 90 days after returning to Earth and 180 days after returning to Earth in the right and left eye, respectively. There was no measured change in spherical equivalent from preflight to postflight in participant 2.
Discussion
In support of our hypothesis, this study documents the late development of optic disc edema in 1 crew member and progressive development of choroidal folds and optic disc edema in another crew member throughout the duration of 1 year in low Earth orbit aboard the International Space Station. As spaceflight missions increase in duration, quantitative analyses of ocular structural and functional changes are important to monitor astronaut health and the efficacy of potential SANS countermeasures.
Limitations
Given the variability of ocular changes observed in 6-month mission participants, the ocular changes reported here in 2 participants may not be generalizable to other 1-year mission participants. Here we quantify choroidal folds; however, other types of folds have been documented during spaceflight.
Conclusions
These data suggest ocular structural changes may be dependent on spaceflight duration. However, there is still a need to identify factors contributing to the variable presentation of ocular findings. Investigations with more participants in 1-year–long missions are needed to confirm the localized findings presented here.
eFigure 1. Example Bruch membrane layer segmentation for macular choroidal fold analysis
eFigure 2. Fundus images of S1 during the one-year mission
References
- 1.Mader TH, Gibson CR, Pass AF, et al. Optic disc edema, globe flattening, choroidal folds, and hyperopic shifts observed in astronauts after long-duration space flight. Ophthalmology. 2011;118(10):2058-2069. doi: 10.1016/j.ophtha.2011.06.021 [DOI] [PubMed] [Google Scholar]
- 2.Patel N, Pass A, Mason S, Gibson CR, Otto C. Optical coherence tomography analysis of the optic nerve head and surrounding structures in long-duration international space station astronauts. JAMA Ophthalmol. 2018;136(2):193-200. doi: 10.1001/jamaophthalmol.2017.6226 [DOI] [PubMed] [Google Scholar]
- 3.Stenger MB, Tarver WJ, Brunstetter T, et al. Risk of spaceflight associated neuro-ocular syndrome (SANS). National Aeronautics and Space Administration. Published November 30, 2017. Accessed February 15, 2018. https://humanresearchroadmap.nasa.gov/evidence/reports/SANS.pdf?rnd=0.434276635495143
- 4.Macias BR, Patel NB, Gibson CR, et al. Association of long-duration spaceflight with anterior and posterior ocular structure changes in astronauts and their recovery. JAMA Ophthalmol. 2020;138(5):553-559. doi: 10.1001/jamaophthalmol.2020.0673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Charles JB, Pietrzyk RA. A year on the international space station: implementing a long-duration biomedical research mission. Aerosp Med Hum Perform. 2019;90(1):4-11. doi: 10.3357/AMHP.5178.2019 [DOI] [PubMed] [Google Scholar]
- 6.NASA . The one year mission. Accessed March 25, 2021. https://www.nasa.gov/content/one-year-crew
- 7.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 8.Scott CJ, Kardon RH, Lee AG, Frisén L, Wall M. Diagnosis and grading of papilledema in patients with raised intracranial pressure using optical coherence tomography vs clinical expert assessment using a clinical staging scale. Arch Ophthalmol. 2010;128(6):705-711. doi: 10.1001/archophthalmol.2010.94 [DOI] [PubMed] [Google Scholar]
- 9.Laurie SS, Lee SMC, Macias BR, et al. Optic disc edema and choroidal engorgement in astronauts during spaceflight and individuals exposed to bed rest. JAMA Ophthalmol. 2020;138(2):165-172. doi: 10.1001/jamaophthalmol.2019.5261 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Example Bruch membrane layer segmentation for macular choroidal fold analysis
eFigure 2. Fundus images of S1 during the one-year mission


