Summary
Objective
Describe the epidemiology of COVID-19 cases detected in the first four months of the pandemic in Ghana by person, place and time to provide an understanding of the local epidemiology of the disease.
Methods
We conducted an exploratory descriptive study of all confirmed COVID-19 cases in Ghana from March 12 to June 30, 2020. Data was merged from the country's electronic databases, cleaned and summarized using medians, proportions and geospatial analysis.
Design
A cross-sectional study design
Setting
Ghana
Participants
All confirmed COVID-19 cases in Ghana from March 12 to June 30, 2020
Interventions
None
Main Outcome measures
Epidemiological characterization of all confirmed COVID-19 cases recorded from March 12 – June 30, 2020 in Ghana by person, place and time.
Results
A total of 17,763 cases were recorded with median age (IQR) of 33years (One month to 85 years). Among the confirmed cases, 10,272 (57.8%) were males and 3,521 (19.8%) were symptomatic with cough recorded in 1,420 (40.3%) cases. The remaining 14,242 (80.2%) were asymptomatic. Greater Accra region recorded the highest number of confirmed cases 11,348 (63.9%). All 16 administrative regions had recorded cases of COVID-19 by June 30, 2020 due to internal migration between the hotspots and other regions. The epidemiological curve showed a propagated outbreak with 117 deaths (CFR= 0.67%) recorded.
Conclusion
A propagated outbreak of COVID – 19 was confirmed in Ghana on March 12, 2020. Internal migration from hotspots to other regions led to the spread of the virus across the nation. Majority of cases were asymptomatic.
Funding
The COVID-19 pandemic response and writing workshop by the Ghana Field Epidemiology and Laboratory Training Programme (GFELTP) was supported with funding from President Malaria Initiative – CDC, and Korea International Cooperation Agency (on CDC CoAg 6NU2GGH001876) through AFENET
Keywords: COVID-19, Epidemiology, pandemic, Ghana, geospatial
Introduction
Coronaviruses are RNA viruses that cause respiratory, hepatic and neurological diseases in domestic and wild animals, and humans.1,2 Among humans, six species of coronavirus have been identified to cause disease. 3 Among these, Severe Acute Respiratory Syndrome (SARS-CoV) and Middle East Respiratory Syndrome (MERS-CoV) are of zoonotic origin and have been known to cause severe acute respiratory syndrome outbreaks among humans. 4–7 With increasing human to animal contact and interfaces in recent times, an outbreak of novel zoonotic species of Coronavirus was reported in late 2019 in Wuhan, China.8–10 The causative pathogen for the outbreak was identified as SARS - Coronavirus - 2 which rapidly spread through China and other parts of the world.11–13The disease was thereafter named COVID-19.
Symptoms of COVID-19 include fever, dry cough, headache, sore throat, cold, difficulty in breathing, muscle pain and malaise. 14,15 From large cohorts of patients, it was found that the disease presents as self-limiting in approximately 80% of infected individuals with 15% developing severe pneumonia and mortality estimated at 3.5%.16–18 Individuals with underlying health conditions and the aged are more susceptible to the infection and have higher chances of severe outcomes. 15,19,20
The World Health Organization (WHO) declared COVID-19 as a Public Health Emergency of International Concern (PHEIC) on January 30, 2020 and later as the number of cases and territories reporting cases increased globally, COVID-19 was declared a pandemic on March 11, 2020. 21 As at July 1st, 2020, over 213 countries were affected with over 10 million cases and 515,000 deaths. 22 Currently most of the countries affected have reported both imported cases and local transmission. Heightened surveillance, tracing of case contacts, varying degrees of restrictions on movement, preventive measures including physical distancing, wearing of nose mask and personal hygiene are among the measures taken by countries to halt the spread of COVID-19. 23–26
Ghana recorded its first two cases on March 12, 2020. These were imported from Norway and Turkey. The country began its response with heightened surveillance for identification of cases and subsequent tracing of their contacts. Mandatory quarantine of travelers entering the country was imposed on March 17, 2020. The borders were subsequently closed on March 22, 2020. As the number of cases continued to increase to a little above 60, restrictions were placed on movement in the Greater Accra and Ashanti Regions on March 30, 2020 as response continued. Voluntary testing of people within 1–2 km radius of identified cases was also instituted. With these response strategies, the country was able to detect about 1000 additional cases of which about 90% were asymptomatic. As at June 30, 2020, over 300,000 tests have been conducted with over 17,000 confirmed cases, 117 deaths and 13,000 recoveries. 27
We describe here the epidemiology of the outbreak in Ghana as at June 30, 2020 to provide valuable insights into the development of this pandemic and to guide the response as the disease continues to spread.
Methods
Study Design
We conducted a cross sectional descriptive exploratory analysis of all diagnosed COVID-19 cases in Ghana from March 12 to June 30, 2020.
Study Setting
Ghana is a West African country occupying an area of 239,460 sq. km and lies between latitude 5° and 11° north. Ghana shares borders with Burkina Faso to the North, Togo to the east, Côte d'Ivoire to the west and the Atlantic Ocean to the south. The projected population from the 2010 national census as at May 2020 stands at 30,955,204. 28
The Ghana Health Service (GHS) is the largest public sector agency under the Ministry of Health that is responsible for provision of health service delivery to the Ghanaian population. Their mandate is to ensure that the health needs of Ghanaians are met. The country has five designated levels of health care starting from Community-based Health and Planning Services (level 1), health centers and clinics (level 2), district hospitals (level 3), regional hospitals (level 4) and tertiary hospitals (level 5). 29 Ghana has a well-structured health organogram with fairly adequate human resources and disease surveillance continues to improve across the country.
The two main epicenters of the country during the first four months of the COVID outbreak were Greater Accra and Ashanti Regions. Ashanti region is the third largest of the 16 administrative regions covering 10.2% of the total land area of Ghana. The region is the most densely populated in Ghana with an estimated 5,924,478 inhabitants according to the Ghana Statistical Service projected population for May 2020. 28 Greater Accra region occupies 1.4% of the total land area of the country. The region is the second most densely populated in the country and contains 15.4% of Ghana's population with 5,055,883 inhabitants. 28 The capital city of the country, Accra, is located in this region.
Data Sources and Data Cleaning
All data on COVID-19 cases recorded using three platforms sanctioned by the Ghana Health Service were used in this study. In the early stages of the outbreak, when the outbreak was limited to Greater Accra Region, data was entered into the Surveillance Outbreak Response Management & Analysis System (“SORMAS”, Helmholtz Centre for Infection Research. (2019). Braunschweig, Germany). However, as the outbreak continued to spread to other regions, additional platforms were introduced as a stopgap measure as the country expanded coverage of SORMAS beyond the epicenter. The Ghana Field Epidemiology and Laboratory Training Programme (GFELTP) together with the Geography department at the University of Ghana introduced the “ArcGIS” (Environmental Systems Research Institute (ESRI). (2014). ArcGIS online, Redlands, CA) and “Survey 123” (Environmental Systems Research Institute (ESRI) (2020), Survey 123, Redlands, CA) for collection of data on cases by epidemiologists and local health workers who were part of the response teams. Paper-based forms were also entered in REDCap. 30 This study pooled together the data from the three sources. The pooled data was cleaned using the unique identification numbers to remove duplicate entries. As part of the measure to protect patient identity, all personal identifying information were removed. The final cleaned dataset was used for this study.
Data Collection
At the point of sample collection, patient characteristics were collected from the patients and entered into the various databases including the Surveillance Outbreak Response and Management and Analysis System (SORMAS), ArcGIS Survey 123, and hard copy case-based forms. Data on the hard copy case-based forms were later entered into REDCap. Information collected from patients included their sex, age, Region, district, education status, occupation, date of diagnosis, travel history (either from outside the country or district of diagnosis) point of entry for cases with travel history, whether there was previous contact with a confirmed case and symptoms status (symptomatic or asymptomatic). For symptomatic cases, data on the date of symptom onset was also collected. Geographical location coordinates were plotted for all identified cases. In determining the epidemiological link of cases, a description of the index case in each district was reviewed.
Data Analysis
We conducted descriptive analysis by summarizing the data by person, place and time using median, frequencies, proportions, ratios, rates and maps. Categorical variables were expressed in frequencies and proportions. Continuous variables were summarized using measures of central tendency and their corresponding measures of dispersion. Age and sex distribution and ratios were reported. Case fatality rates were reported by region. Additionally, the geographical location of cases was used to build geospatial maps for the distribution of the cases using ArcGIS. We showed the epidemiological link between cases across the regions using index cases as points of movement. We reported local transmission and imported index cases from some regions to show the movement between and within the country.
An epidemiological curve was constructed for the outbreak. Further sub-group analysis was conducted showing the hotspots for COVID-19 infection at the initial two epicenters as at June 30, 2020 and the contact tracing outcomes for the first 30 cases recorded in the country. Denominators for some of the analysis varied due to missing data on some of the variables.
Ethical Consideration
The Ghana Health Service collected data used in this manuscript as part of response activities for COVID – 19 pandemics in Ghana. We however sought approval from the Ghana Health Service to use the data (GHS-ERC 006/05/20). The confidentiality of data was maintained throughout the study. Data was kept on password protected computers and was only accesses by authorized persons.
Results
Characteristics of Cases (Person)
Out of approximately 300,000 tests conducted, 17,763 cases were detected as at June 30, 2020 with median age (IQR) of 33 (one month to 85 years). Majority of cases were males 10,272 (57.8%) with the age group of 20–29 years having the highest number of cases 3,075 (17.3%) (Table 1).
Table 1.
Baseline Characteristics of COVID-19 Cases in Ghana, 2020
| Baseline Characteristics | Confirmed Cases N (%) | |
| Sex | n=17,763 | |
| Male | 10,271 (57.8) | |
| Female | 7491 (42.2) | |
| Age | n=10,487 | |
| 0–9 | 250 (2.4) | |
| 10–19 | 708 (6.8) | |
| 20–29 | 3,073 (29.3) | |
| 30–39 | 3,209 (30.6) | |
| 40–49 | 1,652 (15.8) | |
| 50–59 | 1,003 (9.6) | |
| >60 | 592 (5.6) | |
| Occupation | n=4,184 | |
| Health worker | 683 (16.3) | |
| Formal employment | 1,700 (40.6) | |
| Artisan/ Self employed | 1,310 (31.4) | |
| Unemployed | 491 (11.7) | |
| Symptoms Status | n=17,763 | |
| Symptomatic | 3521 (19.8) | |
| Asymptomatic | 14,242 (80.2) | |
| Common Symptoms | n=3,521 | |
| Cough | 1,420 (40.3) | |
| Headache | 1,092 (31.0) | |
| Fever | 865 (24.5) | |
| General Weakness | 667 (18.9) | |
| Chest Pain | 300 (8.5) | |
| Joint/ Muscle Pain | 248 (7.0) | |
| Sore throat | 195 (5.5) | |
| Difficulty Breathing | 130 (3.6) | |
| Period of diagnosis | n=17,763 | |
| Month One | 1,648 (9.3) | |
| Month Two | 5,545 (31.2) | |
| Month Three | 7,380 (41.5) | |
| Month Four | 3,190 (17.9) | |
*Denominators are different due to missing data for some of the variables
Among 4,184 respondents out of total confirmed cases, 1700 (40.6%) worked in the formal sector and 683(16.3%) were healthcare workers.
Among the confirmed cases, 3,521 (19.8%) were symptomatic of which cough was the highest symptom recorded in 1,420 (40.3%) cases. The remaining 14,242 (80.2%) confirmed cases were asymptomatic. Majority of the confirmed cases (7,380, [41.5%]) were detected in between May 2020 (Table 1).
Location of Cases (Place)
The index cases for the country were detected on March 12, 2020 in Greater Accra region. Over 60% of the confirmed cases were reported in the Greater Accra Region (11,348 [63.9%]) followed by the Ashanti region (3,003 [16.9%]). By end of June, all 16 regions in the country had recorded cases of COVID-19. Out of 17,763 confirmed cases 13,190 (74.3%) had recovered as at June 30, 2020. Additionally, of the 4,573 active cases, Greater Accra Region had the highest number of active cases with 2,724. Overall case fatality rate for the country was 0.66% (Table 2)
Table 2.
Recoveries and Active cases by Regions, Ghana, June 30, 2020
| Date of recorded First Case |
Region | Number of Cases N (%) |
Recoveries/ Discharges N (%) |
Number of Active Cases |
Number of Deaths |
CFR |
| March 12, 2020 | Greater Accra | 11,348 (63.9) | 8624 (75.9) | 2,724 | 53 | 0.47 |
| March 13, 2020 | Ashanti | 3,003 (16.9) | 1814 (60.4) | 1,189 | 51 | 1.69 |
| March 14, 2020 | Western | 741 (4.2) | 691(93.3) | 50 | 1 | 0.13 |
| March 18, 2020 | Eastern | 773 (4.4) | 507 (65.6) | 266 | 2 | 0.26 |
| March 23, 2020 | Upper East | 312 (1.8) | 309 (99) | 12 | 1 | 0.32 |
| March 25, 2020 | Upper West | 38 (0.02) | 38 (100) | 0 | 0 | 0.00 |
| March 27, 2020 | Northern | 56 (0.31) | 26 (46.4) | 30 | 2 | 3.57 |
| April 5, 2020 | Central | 1,078 (6.1) | 851 (78.9) | 227 | 4 | 0.37 |
| April 5, 2020 | Volta | 221(1.2) | 199 (90) | 22 | 1 | 0.45 |
| April 6, 2020 | North East | 9 (0.05) | 3 (33.3) | 6 | 1 | 11.11 |
| April 17, 2020 | Oti | 62 (0.34) | 54 (87.1) | 8 | 0 | 0.00 |
| April 17, 2020 | Western North | 22 (0.12) | 18 (81.8) | 4 | 0 | 0.00 |
| May 15, 2020 | Savannah | 34 (0.19) | 31 (91.2) | 3 | 0 | 0.00 |
| May 20, 2020 | Bono East | 56 (0.31) | 18 (32.1) | 18 | 1 | 1.79 |
| May 25, 2020 | Ahafo | 8 (0.05) | 6 (75.0) | 2 | 0 | 0.00 |
| May 29, 2020 | Bono | 2 (0.01) | 1 (50.0) | 1 | 0 | 0.00 |
| Total | 17, 763 | 13, 190 (74.3) | 4,573 | 117 | 0.66 | |
Regional Index Cases
The first index cases were reported in the Greater Accra Region. Both cases were imported cases from Turkey and Norway. The next three regions to record cases were the Ashanti, Central and Western Regions before the disease was recorded progressively in other regions. Of the sixteen regions, the index cases for 8 regions (50%) were local index cases. (Table 3)
Table 3.
Epidemiological link of Regional Index COVID-19 cases in Ghana, June 2020
| Date of Reported Index Case |
Region | District Reporting Index Case |
Places Visited Prior to detection (Region/ District/Country) |
Remarks |
| March 12, 2020 | Greater Accra | Ayawaso West | Norway, Turkey | Two imported cases were reported simultaneously. |
| March 13, 2020 | Ashanti | Obuasi | UK | Two index cases detected. One is an imported case while the other is a resident (community transmission) |
| Kumasi | Kumasi Resident | |||
| March 14, 2020 | Western | Shama | China | Imported |
| March 18, 2020 | Eastern | Lower Manya Krobo |
India | Imported |
| March 23, 2020 | Upper East | Bolgatanga | Nkawkaw (Eastern Region) | Travelled between the two towns in a space of three days |
| March 25, 2020 | Upper West | Wa | Greater Accra | Local transmission |
| March 27, 2020 | Northern | Tamale | Guinea Residents – Travelled through Burkina Faso and Togo |
Imported |
| April 5, 2020 | Central | Cape Coast | UK, returnee | Imported |
| April 5, 2020 | Volta | Aflao | Nigeria | Imported |
| Hohoe | Greater Accra Region | Two index Cases who moved from Accra to Hohoe in a bid to escape lockdown restrictions |
||
| April 6, 2020 | North East | West Mamprusi Municipal |
Cargo Mate moving from Market to Market in the northern zone |
Local Transmission. Posthumously confirmed. |
| April 17, 2020 | Oti | Nkwanta | Greater Accra Region | Travelers to the Northern region who moved from Accra in order to avoid the mandatory lockdown announced by Government |
| April 17, 2020 | Western North | Bibiani | Mines worker, No history of travel | Community Transmission |
| May 15, 2020 | Savannah | East Gonja | Works in Salaga, Resident in Tamale (Northern Region) during weekends |
Community transmission |
| May 20, 2020 | Bono East | Tano South Municipal | Obuasi | Local Transmission (Moved from Ashanti Region – one Epicenter) |
| May 25, 2020 | Ahafo | Asutifi South | Resident, No travel History | Community Transmission |
| May 29, 2020 | Bono | Jaman North | Ivory Coast | Imported Case (Togolese National) |
Geo-Spatial Distribution of COVID-19 Cases
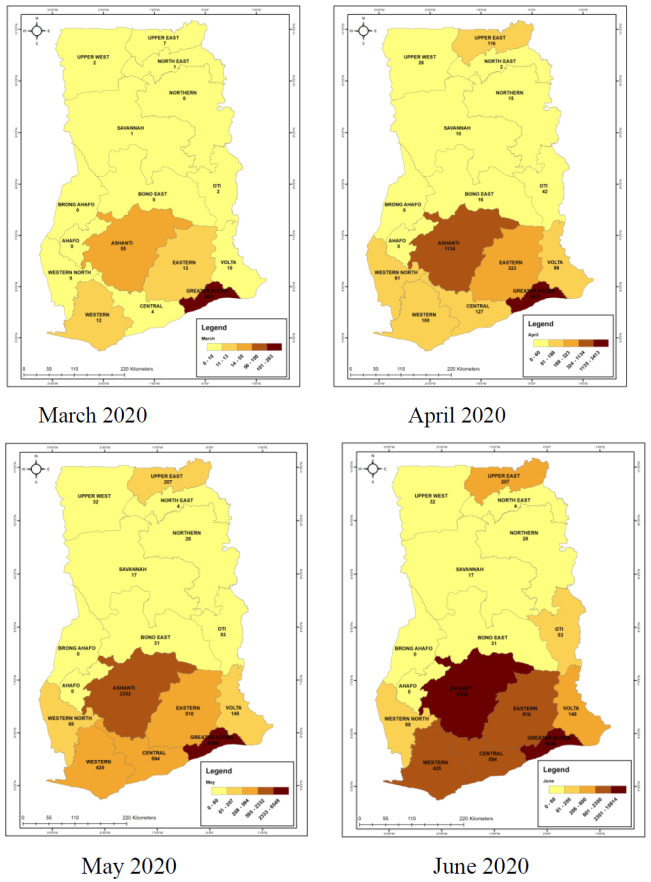
Over the past four months, the Geospatial maps of cumulative number of cases across the country showed that in March, few numbers of cases were reported in 4 regions in the country. From this initial four regions within month one, COVID-19 spread to fourteen out of the 16 administrative regions of the country by month two and by the third month, all sixteen regions had recorded cases with a general increasing cumulative trend (Figure 1A-D). The Greater Accra and Ashanti regions had the highest rate of increase in the number of cases with the number more than tripling in monthly intervals in Greater Accra Region.
Figure 1A-1D.
Cumulative Spatial maps showing geo-spatial distribution of COVID-19 Cases over the four-month period.
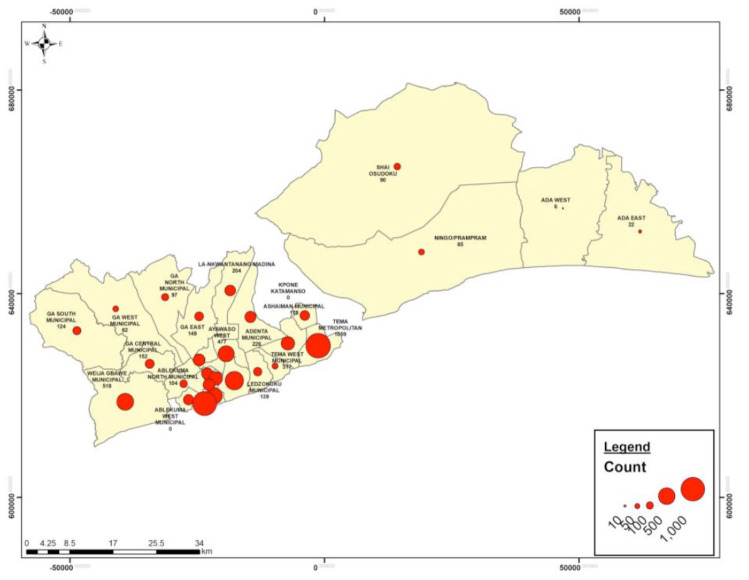
Hotspots for COVID-19 Infection at the two initial Epicenters
Dots analysis showed that the hotspots for COVID-19 infection in Accra included the Accra Metropolis, Tema metropolis and Weija Gbawe municipal (Figure 2).
Figure 2.
Dots Map showing the hotspots for COVID-19 in Greater Accra Region as at June 30th, 2020
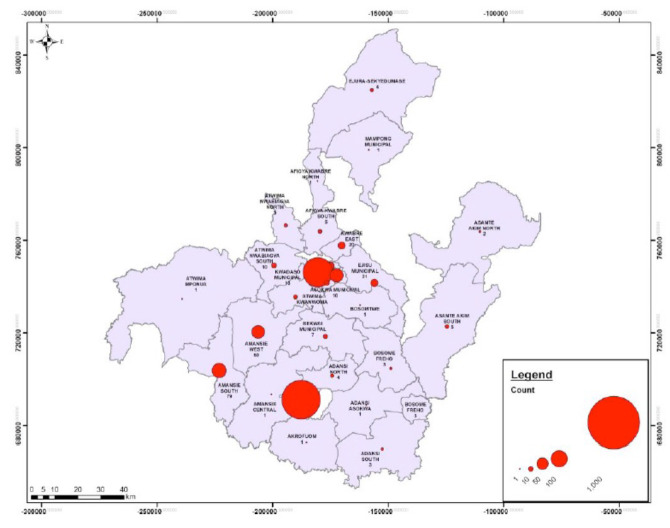
In Ashanti region, Obuasi municipal and Kumasi metropolitan were identified as hotspots with over 500 cumulative cases reported from these districts (Figure 3).
Figure 3.
A dots map showing hotspots for COVID-19 infection in the Ashanti Region as at June 30th, 2020.
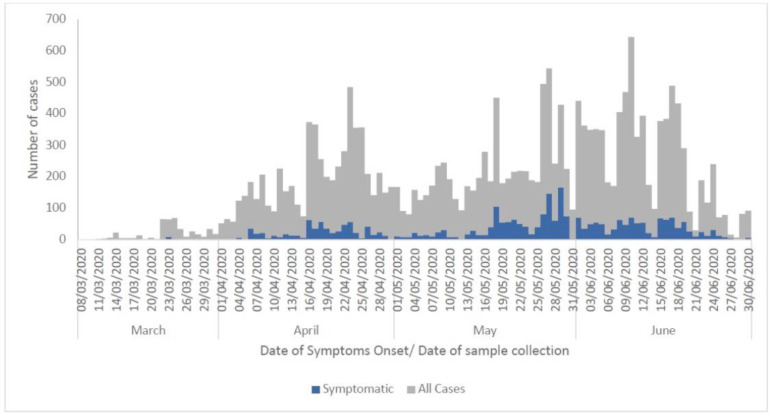
Epidemiological Curve of COVID-19 Cases, March-June 2020
The distribution of cases showed a propagated outbreak with multiple peaks of about one-month interval. The highest peak of confirmed cases as at June 30, 2020 was observed at June 10, 2020. (Figure 4). The index cases were confirmed on March 12, 2020. Among symptomatic patients, cases were distributed over the four months with multiple peaks with the highest peak on April 29, 2020 (Figure 4).
Figure 4.
Epidemiological Curve of confirmed COVID-19 cases in Ghana, March 12, 2020 – June 30, 2020.
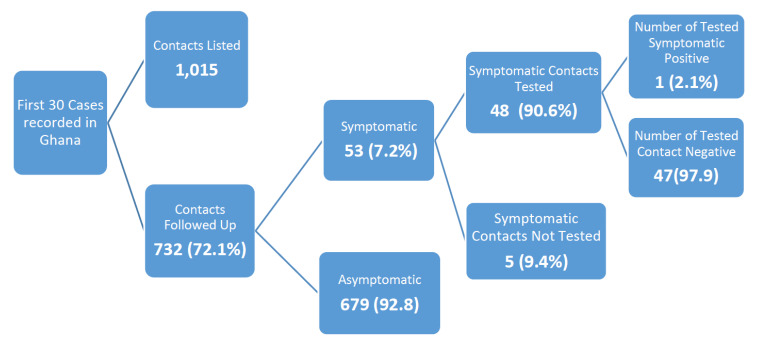
Contact Tracing for First Thirty Cases, Ghana
From the first thirty cases recorded by the country, 1,015 contacts were listed of which 732 (72.1%) were successfully followed up. The number of contacts who developed symptoms and were tested were 53 with one contact testing positive for COVID – 19 as shown in Figure 5.
Figure 5.
Contact Tracing for First 30 Cases of COVID-19 Outbreak, Ghana, 2020
Discussion
This study set out to determine the epidemiological characterization of the first 17,763 confirmed cases of COVID-19 that were recorded in Ghana from March 12 to June 30, 2020. Majority of the cases were males. This is in line with other epidemiological descriptive studies of COVID-19 where most cases were males as recorded in china and East Indonesia. 31,32 In a study conducted in Iceland, researchers were unsure if males being more affected may be due to more exposure or biologic tendencies.33 In similar epidemiological studies in China and Italy, findings showed that infected males were more likely to have severe disease though we could not establish or refute this finding in our setting due to unavailability of data on severity of cases. 34,35 However, this is an indication that gender is a risk factor for severity of COVID-19 and has a bearing on the gender specific mortality rate. In addition, this goes to support the global demographic statistics that men have a lower life expectancy than women. Although these findings were not established in Ghana, it gives an insight as to where we need to prioritize our gender specific interventions and risk communication. 36
In the first four months of the COVID-19 pandemic in Ghana, approximately 75% of recorded cases were asymptomatic. Having a large proportion of cases showing no symptoms has implications for control of the disease as cases who are unaware of their status will continue interacting with people thereby propagating the outbreak. Research has shown that large proportions of cases exhibit no symptoms especially in countries where screening is done amongst populations without symptoms.37–40 Ghana instituted an enhanced screening around radius of confirmed cases from March 31st, 2020 to April 27, 2020. Enhanced contact tracing is an advanced form of contact tracing which deals with the testing of samples from residents within certain specified area of an already confirmed case, with a goal of early case finding, isolation and control of the disease. A 1–2 km radius was used in Ghana's enhanced contact tracing basing on population density, social interaction within the localities and setting. Institution of enhanced contact tracing was a huge contributory factor to the high proportion of asymptomatic cases detected in the country as enhanced screening contributed over 63% of cases detected as at April, 2020 with 93% of cases detected through enhanced surveillance in the country being asymptomatic 41. In the USA, of 600 sailors aboard an aircraft that tested positive for COVID-19, over 60% had no symptoms and in homeless shelter in Boston, 100% of the 167 people who tested positive for COVID-19 were equally asymptomatic.42,43 These findings have been the driving force for advocation of masks wearing by the general population as a control measure.
Mandatory wearing of masks regardless of COVID-19 status is being implemented heavily in Ghana with support from the Government and all other institutions together with other preventive measures including regular hand washing. 41
The data shows that as demonstrated in other countries, COVID-19 is highly infectious and has spread into all 16 administrative regions of the country within the first 100 days of onset of the outbreak in the country. The epidemiological curves of all confirmed cases and symptomatic cases both show propagated outbreak with several peaks. The downward trends are not sustained long enough before another spike of cases is recorded. Although, the spread of the disease and numbers affected is slow in contrast to developed countries, the consistent increase in the peaks as the outbreak continues is a cause for concern. In the two main epicenters of the COVID-19 outbreak, identified hotspots were the Tema Metropolis and Weija Gbawe municipal in Accra. Tema metropolis is home to several industrial institutions and has recorded localized COVID-19 outbreaks in institutions including one in an inner food processing factory where over 600 cases were recorded. It is therefore not surprising that Tema metro is identified as a hotspot for COVID-19. Additionally, Accra metro is the central part of the capital where major trading activities take place. Looking at the prevalent practices that are associated with the metropolis including overcrowding, it is in line that the metro is identified as a hotspot as well. Kumasi Metropolis is also the central trading point in the Ashanti region. The identifications of these hotspots support the known epidemiological findings and underscores the need for heightened observation of preventive measures at social activities.
The epidemiological links between index cases also show that the disease spread to other regions through imported cases and some cases who moved out of the two epi-centers in a bid to avoid the lockdown that was instituted by the Government on March 30, 2020. 41 Our findings reiterate the need for timely response in the times of outbreaks of infectious diseases. Delays in implementing control measure bring about dire consequences and with the changing landscape of the COVID-19 outbreak in Ghana, there is a need for response efforts to be sustained in order to ensure control of the outbreak. As Ghana has begun to ease restrictions in the country with large numbers of students returning to school, and social events including churches, funerals and weddings opening up, we need to be mindful of a possible rebound of numbers of infected individuals and plan for it.
Details of Contact tracing that was conducted for the first thirty recorded cases showed that – only one contact tested positive amongst the 53 symptomatic contacts recorded. In the beginning of the outbreak, only symptomatic contacts were tested. This means that the country probably missed out on asymptomatic contacts who could have developed the infection as well. Several countries have recorded infections amongst asymptomatic contacts including china, USA and the United Kingdom (UK). 17,38–40 However, as the number of cases without travel history and having no epidemiological link to previous cases increased in Ghana, it became apparent that community level transmission was ongoing. This data was the basis for Ghana coming up with other strategies in case finding and response leading to the enhanced contact tracing strategy deployed in Ghana and this strategy led to a surge in the number of confirmed cases and with majority of them being asymptomatic.
As this study was purely based on routine data collected from detected cases, our study is limited by missing data. We compensated for this by using all available data sources in the country and cross validated the data retrieved from the sources. Additionally, we reported the exact number of verified data for each variable. Additionally, we were also limited by unavailability of data on important covariates such as comorbidities of the cases and the severity of the disease affecting our ability to draw conclusions on this.
Conclusion
The epidemiological characteristics of the first 17, 763 COVID-19 cases in Ghana showed propagated spread of COVID – 19 detection in all 16 regions of the nation. More than a third of all cases detected nationwide were asymptomatic. Greater Accra and Ashanti regions have the highest number of recorded cases and active cases as of June 30th, 2020. Identified hotspot districts in Accra as Accra metropolis, Tema Metropolis and Weija-Gbawe municipal. In Ashanti Region, identified hotspots were the Obuasi municipal and Kumasi metropolitan areas. Continuous movement within the country at critical points after detection of the outbreak including days before lockdown fuelled the spread of the outbreak to other administrative regions.
Acknowledgement
We acknowledge the Ghana Health Service for granting permission for the data. We also acknowledge the regions for verification of data used for this study. Special thanks go to the following for supporting with the manuscript writing process, Ms. Delia Akosua Bandoh, Mr. Ben Aikins, Dr. Mary Amoako-Coleman, Dr. Seth Afagbedzi, Dr. Alex Barimah Owusu, and Ms. Benedicta Atsu.
References
- 1.Weiss SR, Leibowitz JL. Advances in Virus Research. Vol. 81. Academic Press Inc.; 2011. Coronavirus pathogenesis; pp. 85–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Monchatre-Leroy E, Boué F, Boucher JM, et al. Identification of alpha and beta coronavirus in wildlife species in france: bats, rodents, rabbits, and hedgehogs. Viruses. 2017;9(12) doi: 10.3390/v9120364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Su S, Wong G, Shi W, et al. Epidemiology, Genetic Recombination, and Pathogenesis of Coronaviruses. Trends in Microbiology. 2016;24(6):490–502. doi: 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zaki AM, Van Boheemen S, Bestebroer TM, Osterhaus ADME, Fouchier RAM. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. New England Journal of Medicine. 2012;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 5.Gao H, Yao H, Yang S, Li L. From SARS to MERS: evidence and speculation. Frontiers of Medicine. 2016;10(4):377–382. doi: 10.1007/s11684-016-0466-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peiris JS, Lai ST, Poon LL, Guan Y, Yam LY, Lim W, Nicholls J, Yee WK, Yan WW, Cheung MT, Cheng VC, Chan KH, Tsang DN, Yung RW, Ng TK, Yuen KY, SARS study group Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003 Apr 19;361(9366):1319–1325. doi: 10.1016/s0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019 Mar;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu P, Hao X, Lau EHY, et al. Real-time tentative assessment of the epidemiological characteristics of novel coronavirus infections in Wuhan, China, as at 22 January 2020. Eurosurveillance. 2020;25(3):2000044. doi: 10.2807/1560-7917.ES.2020.25.3.2000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. New England Journal of Medicine. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. Journal of Autoimmunity. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? The Lancet Infectious Diseases. doi: 10.1016/S1473-3099(20)30129-8. Published online March 5, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? The Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chinazzi M, Davis JT, Ajelli M, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):eaba9757. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, Evaluation and Treatment Coronavirus (COVID-19) StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 15.Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Military Medical Research. 2020;7(1):11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuen KS, Ye ZW, Fung SY, Chan CP, Jin DY. SARS-CoV-2 and COVID-19: The most important research questions. Cell and Bioscience. 2020;10(1) doi: 10.1186/s13578-020-00404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Medicine and Infectious Disease. 2020;34:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du Y, Tu L, Zhu P, et al. Clinical Features of 85 Fatal Cases of COVID-19 from Wuhan. A Retrospective Observational Study. American journal of respiratory and critical care medicine. 2020;201(11):1372–1379. doi: 10.1164/rccm.202003-0543OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomedica. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Worldometer, author. Coronavirus Cases. Worldometer; [DOI] [Google Scholar]
- 23.Ecdc, author. Novel Coronavirus Disease 2019 (COVID-19) Pandemic: Increased Transmission in the EU/EEA and the UK – Sixth Update. [Google Scholar]
- 24.Khanna R, Cicinelli M, Gilbert S, Honavar S, Murthy G V. COVID-19 pandemic: Lessons learned and future directions. Indian Journal of Ophthalmology. 2020;68(5):703. doi: 10.4103/ijo.IJO_843_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thompson J, Mcmurray S. (No Title) [DOI]
- 26.Cowling BJ, Leung GM. (No Title). :1. [DOI]
- 27.Makinen M, Sealy S, Bitran RA, Adjei S, Munoz R. Private health sector assessment in Ghana. (World Bank Working Paper No. 210) Private health sector assessment in Ghana. 2011;125 doi: 10.1596/978-0-8213-8624-8. [DOI] [Google Scholar]
- 28.Service GS-G, author. Projected Population for Ghana, 2020. 2020. [July 20, 2020]. Published 2020. https://statsghana.gov.gh/nationalaccount_macros.php?Stats=MTA1NTY1NjgxLjUwNg==/webstats/s679n2sn87. [Google Scholar]
- 29.Pharmacess, author. [September 11, 2020]. (No Title). https://www.pharmaccess.org/wp-content/uploads/2018/01/The-healthcare-system-in-Ghana.pdf.
- 30.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paramita S, Isnuwardana R, Rahmadi A, Rafshodia O. Epidemiological characteristics of COVID-19 patients in Samarinda, East Kalimantan, Indonesia. [DOI] [Google Scholar]
- 32.CDC C, author. Method Study Design. 2020. [Google Scholar]
- 33.Gudbjartsson DF, Helgason A, Jonsson H, et al. Spread of SARS-CoV-2 in the Icelandic Population. New England Journal of Medicine. 2020;382(24):2302–2315. doi: 10.1056/NEJMoa2006100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guan W, Ni Z, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New England Journal of Medicine. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Onder G, Rezza G, Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA - Journal of the American Medical Association. 2020;323(18):1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 36.Jin J-M, Bai P, He W, et al. Gender Differences in Patients With COVID-19: Focus on Severity and Mortality. Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang L, Zhang X, Zhang X, et al. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16-23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. Journal of Infection. 2020;80(6):e1–e13. doi: 10.1016/j.jinf.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rivett L, Sridhar S, Sparkes D, et al. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. eLife. 2020;9 doi: 10.7554/eLife.58728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. New England Journal of Medicine. 2020;382(22):2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gandhi M, Yokoe DS, Havlir D V. Asymptomatic transmission, the achilles' heel of current strategies to control Covid-19. New England Journal of Medicine. 2020;382(22):2158–2160. doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kenu E, Frimpong J, Kworam K. Responding to the COVID-19 pandemic in Ghana. Ghana Medical Journal. 2020;54(2):72–73. doi: 10.4314/gmj.v54i2.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.CDC reviewing ‘stunning’ universal testing results from Boston homeless shelter. [July 17, 2020]. https://www.boston25news.com/news/cdc-reviewing-stunning-universal-testing-results-bostonhomeless-shelter/Z253TFBO6RG4HCUAARBO4YWO64/
- 43.Coronavirus clue? Most cases aboard U.S. aircraft carrier are symptom-free - Reuters. [July 17, 2020]. https://www.reuters.com/article/us-healthcoronavirus-usa-military-sympt-idUSKCN21Y2GB.