Abstract
Postnatal depression (PND) is common and predicts a range of adverse maternal and offspring outcomes. PND rates are highest among women with persistent mental health problems before pregnancy, and antenatal healthcare provides ideal opportunity to intervene. We examined antenatal perceived social support as a potential intervention target in preventing PND symptoms among women with prior mental health problems. A total of 398 Australian women (600 pregnancies) were assessed repeatedly for mental health problems before pregnancy (ages 14–29 years, 1992–2006), and again during pregnancy, two months postpartum and one year postpartum (2006–2014). Causal mediation analysis found that intervention on perceived antenatal social support has the potential to reduce rates of PND symptoms by up to 3% (from 15 to 12%) in women with persistent preconception symptoms. Supplementary analyses found that the role of low antenatal social support was independent of concurrent antenatal depressive symptoms. Combined, these two factors mediated up to more than half of the association between preconception mental health problems and PND symptoms. Trialling dual interventions on antenatal depressive symptoms and perceived social support represents one promising strategy to prevent PND in women with persistent preconception symptoms. Interventions promoting mental health before pregnancy may yield an even greater reduction in PND symptoms by disrupting a developmental cascade of risks via these and other pathways.
This article is part of the theme issue ‘Multidisciplinary perspectives on social support and maternal–child health’.
Keywords: postnatal depression, preconception, social support, maternal depression, antenatal, prospective
1. Introduction
Maternal postnatal depression (PND) is a global public health issue, with 1 in 10 women reporting clinically significant levels of depression at one year postpartum in high-income countries, and higher rates in developing countries [1–3]. The consequences for women and children are far-reaching [4]. For women, these can include reduced maternal capacity for sensitive and responsive caregiving [5], and symptom persistence or relapse beyond the postpartum [6]. Children exposed to maternal postpartum depression are at increased risk of emotional, behavioural and cognitive problems through childhood and into adulthood [4], even after accounting for genetic and other familial risks [7]. The economic costs of perinatal mental health problems are also substantial [8,9]. The prevention of PND is, therefore, a clinical and public health priority [10].
Social support is linked to depression across the life-course [11] and has received attention as a promising target for the prevention of PND [12–14]. For parents of infants, supportive relationships are likely to assume particular importance, given heightened risk for mental health problems, sleep disruption, loss of income, employment changes and relationship pressures [15]. In high-income countries, reduced connectedness of extended families, increasing work hours with both parents in the workforce and a cultural emphasis on autonomy and intensive mothering can also exacerbate challenges of parenthood [14,16,17]. Women's perceptions that sufficient perinatal social support is available appear particularly important [14,18]. Low perceived social support during pregnancy predicts PND symptoms even after accounting for other perinatal risks [6,14,19]. Conversely, perceived support from partners, family or friends appears protective against perinatal symptoms [14,20].
For these reasons, preventative interventions to promote maternal social support have been trialled, often commencing in pregnancy when many parents have greater health system contact [21]. These often show little reduction in rates of PND when applied generally, but there is some indication that targeted intervention in women at heightened risk may yield greater benefits [10,22]. One of the strongest and most reliable pre-existing risk factors for PND is a history of mental health problems [13]. For many women, perinatal depression is a continuation of pre-existing mental health problems with onset well before pregnancy [23,24]. Women with preconception mental health problems are not only disproportionately at risk of PND, but also may reap greater mental health benefits from antenatal intervention to promote social support. Persistent mental health problems may trigger social withdrawal, limiting opportunities to form and maintain supportive relationships in the transition to parenthood [25]. Women with long-term mental health problems may also have altered perception and capacity to accept available support, in turn exacerbating risk of symptom recurrence [25,26]. Further, lack of social support may also contribute to the onset and maintenance of mental health problems before and during pregnancy. Targeted intervention to improve social support in women with a prior history of mental health problems may thus prevent a developmental cascade of risk for PND symptoms in this vulnerable group.
For women with prior mental health problems, evaluating the potential benefit of intervention on antenatal social support remains an important priority. From a policy perspective, such evaluation is most valuable if it identifies potential gains relative to other feasible intervention targets, allowing strategic investment of limited funds. These include most notably antenatal depressive symptoms, a key focus of current intervention strategies [10], and other risks including financial difficulties and low maternal–fetal attachment [13,14,27]. Another consideration is the primary focus of prior trials on peer support (informally from friends or formally from trained supporters) [22,28], despite observational evidence for the importance of partner support [6,14]. The relative potential benefit of interventions by source of support in women with preconception mental health problems is unclear.
The purpose of this study is, therefore, to examine the extent to which low perceived antenatal social support mediates associations between preconception mental health problems and PND symptoms. We use data from the Victorian Intergenerational Health Cohort Study (VIHCS), a unique cohort with prospective assessment of women before pregnancy, during pregnancy and postnatally. Specifically, we examine the relative potential benefit of intervening on (i) perceived antenatal overall social support when compared with other potentially modifiable antenatal intervention targets; and (ii) perceived partner support, compared to friend/family support.
2. Methods
(a). Participants
The VIHCS is an ongoing prospective intergenerational study of preconception predictors of infant and child health, described elsewhere [29]. It arose from a cohort study commencing in 1992 in the state of Victoria, Australia (The Victorian Adolescent Health Cohort Study; VAHCS). Briefly, a close-to-representative sample of 1943 Victorian mid-secondary school students (1000 female) were selected via a two-stage cluster sampling design and assessed six-monthly during adolescence (VAHCS Waves 1–6: mean age 14.9–17.4 years), and three times in young adulthood (VAHCS Waves 7–9: 20.7, 24.1 and 29.1 years). VIHCS began in 2006 during the ninth wave of VAHCS. Between 2006 and 2013 (participant age 29–35 years, encompassing median maternal and paternal age for Australian births [30]), VAHCS participants were screened six-monthly for pregnancies via SMS, email and phone calls. Participants reporting a pregnancy or recently born infant were invited to participate in VIHCS, and asked to complete telephone interviews in trimester 3, two months postpartum and one year postpartum for each infant born during VIHCS screening. Participants' parents or guardians provided informed written consent at recruitment into VAHCS, and participants provided informed verbal consent at every subsequent wave. Protocols were approved by the human research ethics committee at the Royal Children's Hospital, Melbourne.
(b). Measures
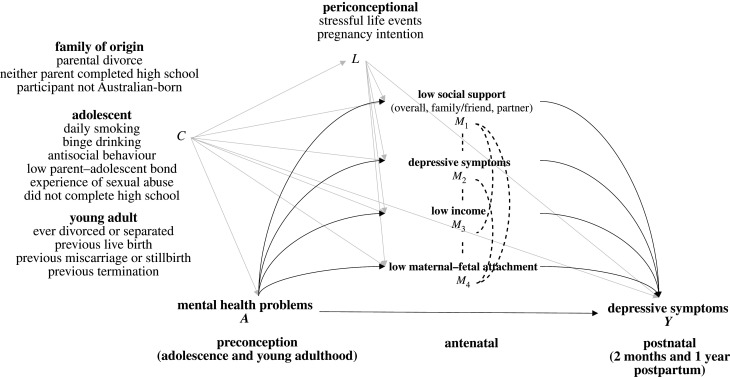
Figure 1 portrays our conceptual model.
Figure 1.
Directed acyclic graph portraying the assumed causal structure, showing the pathways from preconception mental health problems (A) to postpartum depressive symptoms (Y) via the four antenatal mediators (M1–4), after accounting for potential baseline (C) and post-exposure (L) confounding factors. In this conceptual model, we are agnostic about the directionality of causal influences between mediators, as indicated using dotted undirected arrows.
Preconception mental health problems (A) were assessed during VAHCS Waves 2–7 (participant ages 14–21 years) using the Revised Clinical Interview Schedule (CIS-R; range 0–56) [31], a structured psychiatric interview designed to assess symptoms of anxiety and depression in community samples. The CIS-R has been validated for use with adolescent populations [32]. At each wave, total score was dichotomized at ≥ 12 to identify mixed depression–anxiety symptoms at a level lower than major disorder, but that a general practitioner would view as clinically significant [31]. At Waves 8 and 9 (participant ages 24 and 29), symptoms were assessed with the General Health Questionnaire (GHQ-12; range 0–12), a screening measure widely used to assess psychiatric illness in the general population. Total scores were dichotomized at ≥ 3, a validated threshold that also corresponds to CIS-R ≥12 [31,33]. We constructed variables denoting the presence of preconception mental health problems at ≥ 1 adolescent wave (VAHCS Waves 2–6) and ≥ 1 young adult wave (VAHCS Waves 7–9). The continuity of preconception mental health problems was defined as ‘none’, ‘transient’ (present in adolescence or young adulthood, but not both) and ‘persistent’ (present in both adolescence and young adulthood).
Postnatal depressive (PND) symptoms (Y) were assessed at two months and one year postpartum, for each pregnancy, using the Edinburgh Postnatal Depression Scale (EPDS) [34]. The EPDS is a widely used 10-item scale that asks participants to rate the frequency of past-week depressive symptoms, validated for ante- and postnatal use [35]. Total scores (range 0–30) were calculated at each postnatal timepoint, and dichotomized at a threshold (≥ 10) recommended for use in screening for mild to severe PND [36].
We included four potential antenatal mediators (M) assessed during trimester three of pregnancy: low perceived social support, high depressive symptoms, low income and low maternal–fetal attachment. These were identified as associated with PND symptoms, screenable, potentially amenable to intervention and measured in this study [12,13]. Other periconceptional/pregnancy factors associated with PND symptoms but considered less amenable to intervention were included as covariates (L; see below). We dichotomized mediators for translatability to policy settings. To compare mediators at a level denoting relatively high vulnerability, we applied consistent thresholds of ≤ 10th percentile, except for low income where a policy-relevant threshold is predefined.
-
—
Maternal perceived social support was assessed using the six-item Maternity Social Support Scale [37]. Response options ranged from 0 (never) to 4 (always). We defined low overall social support as overall mean score ≤ 10th percentile, low partner support as mean score ≤ 10th percentile for the four partner items (‘My husband/partner helps me a lot’, ‘There is conflict with my husband/partner’, ‘I feel controlled by my husband/partner’ and ‘I feel loved by my husband/partner’), and low friend/family support as mean score ≤ 10th percentile for the two friend/family items (‘I have good friends who support me’ and ‘My family is always there for me’). These thresholds corresponded to mean score ≤ 2 (some of the time) in our sample. The scale has shown good reliability and predictive utility [37,38].
-
—
Depressive symptoms were assessed and dichotomized as per the postnatal waves, using the EPDS at ≥ 10 (corresponding to ≤ 10th percentile in our sample) [34].
-
—
Low income was reported as total household income and dichotomized at ≤ $50 000 per year, approximating Australian poverty line at the data-collection midpoint [39].
-
—
Maternal–fetal attachment was assessed using six items from the Maternal Fetal Attachment Scale [40]. Response options ranged from 0 (almost never) to 3 (almost always). Low maternal–fetal attachment was defined as ≤ 10th percentile. This scale has shown good reliability [41].
Our conceptual model included diverse potential preconception confounders (C), based on prior evidence, to maximize the plausibility of exchangeability assumptions [42,43]. We also considered potential periconceptional and pregnancy confounders (L) of the associations between antenatal factors and PND symptoms. Confounders are listed in figure 1, and described in detail in the electronic supplementary material, appendix.
(c). Statistical analysis
(i). Estimating the strength of the hypothesized pathways
We first investigated the strength of the hypothesized pathways from preconception mental health problems to PND symptoms via low social support by estimating the unadjusted and adjusted relative risk of (i) low antenatal overall, partner and friend/family support in women with persistent or transient versus no preconception mental health problems, and (ii) PND symptoms in women with versus without low antenatal social support. We used the Poisson regression with robust standard errors to account for within-family clustering.
In supplementary analyses, we evaluated correlations between low overall, partner and friend/family support and the other antenatal mediators in our conceptual model, estimated as the unadjusted relative risk of high antenatal depressive symptoms, low maternal–fetal attachment and low income, stratified by low antenatal social support. We also examined the strength of associations between low antenatal overall, partner and friend/family support and PND symptoms in women with persistent preconception mental health problems, with and without adjustment for the other antenatal factors.
(ii). Mediation analysis
We then estimated the potential reduction in PND symptoms in women with prior mental health problems achievable by intervention on antenatal overall social support versus other putative antenatal mediators, and on friend/family versus partner support. We extended a recent method for causal mediation with multiple interdependent mediators that extends previous approaches [44,45] to emulate the effects that would be obtained in a hypothetical randomized trial with interventions both on the exposure and each of a set of interdependent mediators [42]. For this question, we took two approaches. We first estimated (i) a ‘best case scenario’ intervention effect, estimating the potential reductions in PND symptoms in the exposed group if all risk due to the given mediators were eliminated. We then estimated (ii) a more ‘pragmatic scenario’, using a realistic benchmark estimable from the dataset, by estimating the potential reductions in PND symptoms in the exposed if the increased risk of the given mediators attributable to prior mental problems were eliminated. Models included the exposure, mediators, outcome, and all baseline and postexposure confounders. We did not additionally include interaction terms due to sample size and dimensionality of the problem.
We estimated each of the following mediation effects on the risk difference scale, expressed as a marginally adjusted difference in the risk of PND symptoms, adjusted for pre- and periconceptional confounders via a g-computation procedure:
-
—
Interventional indirect effect via mediator k (IIEk): The reduction in the risk of PND symptoms in those with persistent preconception mental health problems achievable by intervention to (i) set mediator k under exposure to be absent, effectively eliminating all risk due to mediator k; or (ii) shift their mediator distribution to the levels in those without persistent preconception problems, in both cases leaving other interdependent mediator distributions unchanged. The latter amounts to setting the mediator under exposure to a random draw from the distribution under no exposure.
-
—
Interventional direct effect (IDE). The remaining risk difference under intervention to (i) set all mediators jointly to be absent, effectively eliminating all risk due to included mediators; or (ii) make the joint distribution of mediators in the exposed (i.e. levels of all the putative mediators and their correlations) to be as in the unexposed.
-
—
Total causal effect (TCE): The overall difference in the risk of PND symptoms if all participants were set to be exposed (persistent preconception mental health problems) versus unexposed (no persistent preconception mental health problems). The TCE can be expressed as the sum of IIEk, the IDE and an effect that compares joint mediator intervention with the sum of individual interventions on each mediator (IIEint).
All analyses included participants who responded in at least one preconception wave and at least one perinatal wave. Incomplete data were handled using multiple imputation under a fully conditional specification framework [46]. We imputed 35 complete datasets based on the proportion of records with any missing data. Parameter estimates were obtained by pooling results across imputed datasets using Rubin's rules. To assess potential for participation bias, we compared VIHCS participant characteristics with those in VAHCS who were either not screened for pregnancies due to prior study withdrawal or were screened and eligible but did not participate. We used Stata 16 [47]. Code for analysis from this paper may be accessed at https://osf.io/4h2xm/?view_only=868a559a861b466caaf50cdd4bdd1606.
3. Results
The flow of participants through the study is in electronic supplementary material, figure S1. The initial sample of adolescents recruited to VAHCS in 1992 included 1000 females. Fourteen years and nine waves later, at the start of VIHCS screening and perinatal data collection, 885 (88%) women were available for screening. During VIHCS screening, 465 women reported pregnancies and were thus eligible to participate in VIHCS. Of these, 398 women participated with 600 pregnancies. Women who were screened, identified as eligible and participated in VIHCS were broadly representative of the original VAHCS cohort on measured baseline demographic, mental health and health risks [29].
Electronic supplementary material, table S1 summarizes participant characteristics using observed data, and proportions of missing data. Preconception mental health problems were reported in 27% of pregnancies, corresponding to 24% of women. Low perceived overall, family/friend and partner support were reported in 11%, 9% and 8% of pregnancies, respectively. Of those women who participated with more than one pregnancy, few (13–14%) had discordant support ratings across pregnancy (normative/high in one pregnancy, and low in another). Rates of PND symptoms were similar at two months (7%) and one year (8%) postpartum. The cumulative rate of PND symptoms across timepoints was 13%, with 5% reporting symptoms at two months postpartum only, 6% reporting symptoms at one year postpartum only and 2% reporting symptoms at both timepoints.
Table 1 shows estimated associations of women's preconception mental health problems with low antenatal overall, partner and friend/family support. Rates of each type of support were higher among those with preconception mental health problems, and highest among those with persistent symptoms (electronic supplementary material, table S2). After adjustment, persistent preconception mental health problems were associated with increased risk of low overall (adjusted risk ratio (aRR) 3.8, 95% CI 1.6, 9.2) and partner support (aRR 3.6, 95% CI 1.2, 11.0). Associations with low friend/family support were smaller, and attenuated after adjustment (aRR 1.6, 95% CI 0.7, 3.9).
Table 1.
Relative risk of low social support during pregnancy, by preconception mental health problems (N = 600 pregnancies).
| low antenatal social support |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| low overall support |
low friend/family support |
low partner support |
|||||||
| preconception mental health problems | RRa | 95% CIa | p-value | RRa | 95% CIa | p-value | RRa | 95% CIa | p-value |
| unadjusted | |||||||||
| none (reference category) | — | — | — | ||||||
| transient | 3.4 | 1.4, 8.2 | 0.006 | 2.2 | 1.0, 4.9 | 0.060 | 2.9 | 1.1, 8.1 | 0.036 |
| persistent | 4.3 | 1.8, 10.2 | 0.001 | 2.6 | 1.2, 5.9 | 0.018 | 3.5 | 1.2, 10.3 | 0.021 |
| adjusted for preconception characteristicsb | |||||||||
| none (reference category) | — | — | — | ||||||
| transient | 2.7 | 1.1, 6.7 | 0.033 | 1.5 | 0.7, 3.5 | 0.332 | 2.8 | 1.0, 7.9 | 0.052 |
| persistent | 3.8 | 1.6, 9.2 | 0.004 | 1.6 | 0.7, 3.9 | 0.262 | 3.6 | 1.2, 11.0 | 0.022 |
aRR, relative risk; 95% CI, 95% confidence intervals.
bAdjusted for mother's family of origin, adolescent and young adult preconception characteristics.
Table 2 shows estimated associations of low antenatal overall, partner and friend/family support with PND symptoms at two months and one year postpartum. The risk of PND symptoms was consistently higher among those with low overall support; associations were most pronounced at two months postpartum with an almost fourfold increase in risk, and remained after adjustment. Low partner support was associated with a threefold increase in the risk of PND symptoms at both two months and one year postpartum after adjustment. Associations between family/friend support and PND symptoms were evident at one year postpartum only, and attenuated somewhat after adjustment.
Table 2.
Relative risk of PND symptoms, by low social support during pregnancy (N = 600 pregnancies).
| PNDa symptoms |
||||||
|---|---|---|---|---|---|---|
| two months postpartum |
one year postpartum |
|||||
| low antenatal social support | RRa | 95% CIa | p-value | RRa | 95% CIa | p-value |
| unadjusted | ||||||
| low overall support | 3.8 | 2.0, 7.2 | <0.000 | 2.9 | 1.4, 6.1 | 0.005 |
| low friend/family support | 1.6 | 0.6, 4.0 | 0.325 | 2.7 | 1.3, 5.7 | 0.007 |
| low partner support | 3.6 | 1.7, 7.4 | 0.001 | 2.9 | 1.2, 7.1 | 0.017 |
| adjusted for pre- and periconceptional characteristicsb | ||||||
| low overall support | 4.3 | 1.8, 10.4 | 0.001 | 2.8 | 1.2, 6.6 | 0.020 |
| low friend/family support | 1.1 | 0.4, 3.0 | 0.795 | 1.8 | 0.8, 4.0 | 0.132 |
| low partner support | 3.4 | 1.4, 8.5 | 0.008 | 3.5 | 1.4, 8.6 | 0.008 |
| further adjusted for preconception mental health problemsc | ||||||
| low overall support | 3.7 | 1.6, 8.6 | 0.003 | 2.4 | 1.0, 5.4 | 0.042 |
| low friend/family support | 1.1 | 0.4, 2.9 | 0.822 | 1.8 | 0.8, 4.0 | 0.157 |
| low partner support | 2.9 | 1.2, 7.0 | 0.017 | 3.0 | 1.2, 7.2 | 0.015 |
aPND, postnatal depression; RR, relative risk, 95% CI, 95% confidence intervals.
bAdjusted for mother's family of origin, adolescent and young adult pre- and periconception characteristics.
cAdjusted for mother's family of origin, adolescent and young adult pre- and periconception characteristics and preconception mental health problems.
Electronic supplementary material, tables S3 and S4 show estimated unadjusted associations between low overall, partner and friend/family support and the other concurrently assessed antenatal mediators in our conceptual model, and estimated associations between low antenatal social support and PND symptoms after adjustment for the other antenatal mediators in women with preconception mental health problems. The risk of antenatal depressive symptoms was higher in those with each type of low antenatal support compared to those with normal/high social support. There was weak evidence of an association between low social support and low income, and little evidence of an association with low maternal–fetal attachment. Despite the correlations between mediators, observed associations between low antenatal overall or partner support and PND symptoms remained after adjustment for other potential antenatal mediators, albeit with wider confidence intervals (two months postpartum: aRR 3.5, 95% CI 1.0, 12.4; one year postpartum: aRR 2.2, 95% CI 0.7, 6.6).
Table 3 displays the results from the first mediation analysis, examining the reduction in PND symptoms that might be achieved by intervening on low antenatal overall support, relative to other potential antenatal mediators. Estimated risks of PND symptoms were higher in women with persistent preconception symptoms than those without at both two months (15.0% versus 3.2%; TCE 11.8%) and one year (16.2 versus 2.7%; TCE 13.5%) postpartum.
Table 3.
Estimated reduction in rates of PND symptoms achieved by intervention on the preconception exposure (TCE) and antenatal mediators (IIE), in women with persistent preconception symptoms (N = 600 pregnancies).
| PNDa symptoms two months postpartum |
PNDa symptoms one year postpartum |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| risk reduction (%) | 95% CI | p-value | proportion of TCE (%) | risk remaining in exposed (%) | risk reduction (%) | 95% CI | p-value | proportion of TCE (%) | risk remaining in exposed (%) | |
| risk of PND symptoms under exposure (no intervention) | — | — | — | — | 15.0 | — | — | — | — | 16.2 |
| total causal effect of the preconception exposure (TCE)b | 11.8 | 4.5, 19.0 | 0.002 | 100 | 3.2 | 13.5 | 5.9, 21.1 | 0.000 | 100 | 2.7 |
| estimated effects of hypothetical intervention on the mediators | ||||||||||
| Scenario 1: best-case intervention eliminating all mediator risk | ||||||||||
| interventional indirect effects via mediators (IIE)c | ||||||||||
| IIE1 (antenatal low social support) | 3.0 | −0.3, 6.3 | 0.073 | 26 | 12.0 | 1.5 | −1.8, 4.7 | 0.376 | 11 | 14.7 |
| IIE2 (antenatal depressive symptoms) | 4.9 | 1.0, 8.8 | 0.015 | 42 | 10.1 | 6.3 | 2.2, 10.4 | 0.003 | 47 | 9.9 |
| IIE3 (antenatal low maternal–fetal attachment) | 1.3 | −1.2, 3.9 | 0.304 | 11 | 13.7 | <1 | −3.0, 1.7 | 0.601 | −5 | 16.8 |
| IIE4 (antenatal low income) | 1.9 | −0.6, 4.3 | 0.130 | 16 | 13.1 | <1 | −1.1, 2.9 | 0.380 | 7 | 15.3 |
| IIEint (mediators' interdependence) | −2.1 | −4.4, 0.2 | 0.073 | −18 | — | <1 | −2.7, 1.6 | 0.625 | −4 | — |
| interventional direct effect not via mediators (IDE)d | 2.7 | −2.9, 8.4 | 0.341 | 23 | — | 6.0 | −1.2, 13.3 | 0.104 | 45 | — |
| Scenario 2: pragmatic intervention lowering mediator levels to those in the unexposed | ||||||||||
| interventional indirect effects via mediators (IIE)e | ||||||||||
| IIE1 (antenatal low social support) | 2.3 | −0.4, 5.0 | 0.094 | 20 | 12.7 | 1.1 | −1.5, 3.8 | 0.394 | 8 | 15.1 |
| IIE2 (antenatal depressive symptoms) | 3.9 | 0.5, 7.3 | 0.025 | 33 | 11.1 | 4.7 | 1.2, 8.3 | 0.009 | 35 | 11.5 |
| IIE3 (antenatal low maternal–fetal attachment) | <1 | −1.2, 1.3 | 0.934 | <1 | 14.9 | <1 | −1, 0.8 | 0.883 | <1 | 16.3 |
| IIE4 (antenatal low income) | <1 | −1.3, 2.1 | 0.638 | 4 | 14.6 | <1 | −0.9, 1.2 | 0.805 | 1 | 16.1 |
| IIEint (mediators' interdependence) | −1.0 | −2.6, 0.6 | 0.217 | –9 | — | <1 | −2, 1.2 | 0.653 | −3 | — |
| interventional direct effect not via mediators (IDE)f | 6.1 | 0.2, 19.0 | 0.002 | 52 | — | 7.9 | 1.1, 14.7 | 0.023 | 59 | — |
aPND, postnatal depression. All models adjusted for mother's family of origin, adolescent and young adult preconception and periconceptional characteristics.
bRisk difference comparing exposed versus unexposed.
cSet given mediator under exposure to zero (no risk).
dRisk difference comparing exposed versus unexposed under intervention setting all mediators to zero (no risk).
eSet given mediator under exposure to a random draw from its distribution under no exposure.
fRisk difference comparing exposed versus unexposed under intervention jointly lowering all mediators to those in unexposed.
At two months postpartum, the estimated reduction in PND rates achievable by intervention on low overall social support was 2.3% (20% of TCE) under a pragmatic intervention scenario, and 3.0% (26% of TCE) under a best-case intervention scenario. At one year postpartum, the estimated reduction by intervention on low overall social support was 1.1% (8% of TCE; pragmatic scenario) and 1.5% (11% of TCE; best-case scenario).
Considering the other potential intervention targets, the estimated reduction in PND rates achievable by intervention on antenatal depressive symptoms was 3.9% (33% of TCE) under a pragmatic intervention scenario, and 4.9% (42% of TCE) under a best-case intervention scenario, at two months postpartum. At one year postpartum, the estimated reduction was 4.7% (35% of TCE; pragmatic scenario) and 6.3% (47% of TCE; best-case scenario). By contrast, aside from small risk reductions under a best-case scenario at two months postpartum, the roles of income and maternal–fetal attachment were negligible (less than 0.5% combined). The proportion of TCE via the mediators' interdependence (IIEint) was negative, as expected, because summing the effects overestimates what is achievable due to between-mediator correlations.
When considered together, under a best-case intervention scenario eliminating all risk of PND symptoms due to all mediators, the remaining risk difference was 23% at two months postpartum and 45% at one year postpartum. Under a more pragmatic intervention scenario lowering the distribution of all mediators to those in the unexposed, the remaining risk difference was 52% at two months postpartum and 59% at one year postpartum.
In the second mediation analysis (electronic supplementary material, table S5), we compared the potential effects of intervention on low antenatal friend/family support versus low antenatal partner support. We estimated that, aside from a small risk reduction evident under a best-case intervention scenario at one year postpartum (1.2%; 9% of TCE), intervention to reduce low family/friend support yielded negligible reductions in PND symptoms. The estimated potential impact of intervention on antenatal partner support was greater, reducing rates of PND symptoms among women with preconception mental health problems by 1.6% (14% of TCE) under a pragmatic scenario and 2.0% (17% of TCE) under a best-case scenario at two months postpartum and by 1.8 (13% of TCE) under a pragmatic scenario and 2.3% (17% of TCE) under a best-case scenario at one year postpartum.
4. Discussion
Women with a long-term history of mental health problems before pregnancy were at substantially increased risk of PND symptoms, with estimated rates of 15–16% in this group compared to 3% in women without a prior history. The overall proportion of preconception associations mediated by included antenatal factors was 41–77%, driven almost entirely by antenatal social support and depressive symptoms. Interventions on antenatal social support in women with persistent pre-pregnancy mental health problems have the potential to reduce rates of PND symptoms by up to 3% (from 15 to 12%), in a best-case scenario where all mediator risk is eliminated. Importantly, a more conservative target of raising levels of social support to those seen in women without prior mental health problems could also yield comparable gains (up to 2.3%, from 15% to 12.7%). Interventions on antenatal depressive symptoms directly also had the potential to reduce PND symptoms by up to 6.3%. Nonetheless, associations between antenatal social support and PND were robust to adjustment for antenatal depressive symptoms, suggesting an independent role of social support. Findings support a role of antenatal social support, as well as highlighting the likelihood of multiple, complex pathways from preconception to postpartum mental health problems.
Prospectively, women with persistent preconception mental health problems were more than three times more likely to report low antenatal support, a finding consistent with prior retrospective reports [26]. Our findings suggest a role of low antenatal overall and partner-specific social support in mediating associations between preconception mental health problems and PND symptoms. This may reflect both greater support needs and difficulties in eliciting and maximizing support [25,26], increasing risk of symptom recurrence. Negative attribution style is a further potential explanation. Global perceived support may reflect a stable view of the social environment, shaped by lifelong experience [48]. Attachment and trauma models emphasize family of origin legacies in increasing risk of depression, social difficulties and perceived unavailability of a reliable attachment figure [49]. Nonetheless, partner-specific perceived support is likely to reflect not only general interpersonal disposition but also qualities of the couple's relationship [48]. Partner support is a broad construct, and our measure may also capture general partner dissatisfaction and intimate partner violence and abuse, both also risk factors for PND [13,50].
Our finding of a negligible role of family/friend support aligns with prior evidence that associations between women's peer networks during pregnancy and PND symptoms may reflect underlying risks, and partially explain the limited efficacy of peer support interventions [14,51]. Aggregation of friend/family support may also mask more specific roles, such as the maternal grandmother. Evidence on family support is mixed, with suggestion that increases to retirement age and distances between extended family members impact grandparental availability [52].
(a). Strengths and limitations
VIHCS is a unique, population-based prospective study of adolescent health with rich developmental data on diverse mental health and behavioural outcomes, spanning two generations. Our use of recent causal mediation methods represents an advance over prior methods, by quantifying the potential relative benefit of interventions at a population level considering multiple interdependent mediators, and by providing best-case versus more realistic estimates of potential intervention effects. However, limitations common to mature cohorts should be considered. Attrition was low in VAHCS, with little evidence that those participating in VIHCS differed from the eligible or baseline VAHCS sample. However, there remains potential for selection bias due to differences on unmeasured characteristics.
Options for data linkage in Australia preclude prospective identification of new pregnancies to an existing longitudinal cohort. Therefore, participants were contacted every six months and invited to join the study if they were pregnant. This makes our study one of very few internationally with antenatal survey data on a long-term preconception cohort. The higher levels of missingness at this wave reflects the logistical challenge of detecting all pregnancies in this way before the birth of the child. When the study detected a new pregnancy after the child was born, we included that child in the VIHCS sample from the postnatal waves onwards, to minimize bias due to selective recruitment. We then used multiple imputation data with a rich imputation variable set to minimize potential for biases due to missing data as far as possible. Nonetheless, as with all cohort studies, potential for bias due to missing data remains. We note that rates of adolescent and young adult mental health problems in our sample were similar to those reported in other prospective cohorts [53]. Rates of ante- and postnatal depressive symptoms were at the lower end of previously reported meta-analytic bounds [54].
This study included Australian women aged 29–36 years, maximizing recruitment within a discrete window around peak maternal age at birth in Australia [30]. Future research should explore associations in younger and older parents given different risk profiles. The role of social support is also influenced by culture, community and policy [14]; for example, Australia's paid parental leave scheme provides financial context for our findings, suggesting a need to explore these questions across political, socio-economic and cultural settings.
Measures were self-reported, which opens the possibility of shared method variance. However, perceived sufficiency of support with respect to felt need has intrinsic value, strong predictive validity and is easily screened [14,18]. Further, associations of low antenatal social support with PND were not explained by concurrent low mood. Our social support measure was brief to reduce participant burden, so that we were able to investigate the high-level categories of partner versus family/friend support. Our findings were consistent with prior observational evidence of the relatively small role of family/friend when compared with partner support during pregnancy. However, future research may investigate the role of more specific sources and types of support (including emotional, practical, informational or other types of support) [55,56]. The breadth of the VIHCS dataset and use of new methods enabled adjustment for many potential preconception and periconceptional confounders. Potential for unmeasured confounding remains. Future directions include the preventive role of antenatal social support in women with additional vulnerabilities, such as intimate partner violence.
5. Conclusion
Even though women with preconception mental health problems are at substantially increased risk of perinatal depression, evidence of effective strategies to prevent symptom recurrence has been limited. Our findings highlight two avenues for research and practice. First, we observed a role of low perceived social support over and above antenatal depressive symptoms, with these two factors accounting for most of the mediated effect. Thus, our findings support a focus on trialling dual intervention on these two factors specifically for women with a background of persistent problems [57]. Prior trials have predominantly focused on peer support [21,28]. Our findings suggest potential promise of intervention on perceived overall and partner support in women with prior mental health problems. These may include efforts to address underlying attributional and interpersonal processes [58], and greater emphasis on family-focused, partner-inclusive care and consideration of the social context in perinatal mental health strategies [59–61].
Second, our findings support calls to evaluate the potential benefit of preventive efforts before pregnancy [62,63]. We found that a substantial proportion of the associations between preconception and postnatal symptoms were not mediated by low social support or the other included antenatal factors, highlighting the likelihood of multiple, complex pathways. Preconception care is increasingly recognized as a critical element of healthcare for women of reproductive age, benefitting women across the life-course and into future pregnancies, should they occur [64]. Such strategies may include focused preconception care for women with long-term mental health problems, given the complexity and treatment lag times of intervention on socio-emotional health and partner relationships. Prevention strategies from adolescence may have broader benefits in limiting symptom persistence and intergenerational impacts. Adolescence is a critical window of socio-emotional development, commonly marked by the shift from parent to peer as primary support as well as first romantic or sexual relationships [65]. Strengthening investment in adolescent mental health, including healthy and supportive relationship patterns, may thus yield multiple cascading benefits for women that also extend into future pregnancies [66].
Acknowledgements
We thank participants, collaborators and study teams of the Victorian Adolescent and Intergenerational Health Cohort Studies.
Data accessibility
Code for analysis from this paper may be accessed at https://osf.io/4h2xm/?view_only=868a559a861b466caaf50cdd4bdd1606. Ethics approvals for this study do not permit the data to be made publicly available, due to limitations of participant consent and concerns regarding potential re-identifiability. If required and upon request, the dataset subset can be made available to a named individual for the purpose of replication of research findings.
Authors' contributions
E.A.S., G.C.P. and E.M. conceived the paper. E.A.S., M.M.-B., M.M., E.M., C.A.O. and G.C.P. devised the analysis plan and all authors approved it. E.A.S., M.M.-B., M.M. and C.J.G. conducted the analysis. E.A.S. drafted the manuscript. M.M.-B. and M.M. contributed to drafting of the Methods section. C.A.O. contributed to drafting of the Discussion section. All authors critically revised the manuscript. All authors approved the final version of the manuscript.
Competing interests
The authors declare no competing interests.
Funding
This work was supported by the ARC (DP180102447), NHMRC, Australian Rotary Health, Colonial Foundation, Perpetual Trustees, Financial Markets Foundation for Children (Australia), Royal Children's Hospital Foundation and the Murdoch Children's Research Institute. G.C.P. is supported by NHMRC (APP1117873), S.B. by NHMRC (APP1103976), C.A.O. by NHMRC (APP1175086), M.M.-B. by ARC (DE190101326), K.C.T. by the Canadian Institutes of Health Research (MFE158141), and L.M.H. by the South London and Maudsley NHS Foundation Trust and King's College London NIHR (National Institute for Health Research) Biomedical Research Centre. Research and NIHR South London Applied Research Collaboration at the Murdoch Children's Research Institute is supported by the Victorian Government's Operational Infrastructure Program.
References
- 1.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. 2005. Perinatal depression: a systematic review of prevalence and incidence. Obstet. Gynecol. 106, 1071-1083. ( 10.1097/01.AOG.0000183597.31630.db) [DOI] [PubMed] [Google Scholar]
- 2.Almond P. 2009. Postnatal depression: a global public health perspective. Perspect. Public Health 129, 221-227. ( 10.1177/1757913909343882) [DOI] [PubMed] [Google Scholar]
- 3.Roshaidai Mohd Arifin S, Cheyne H, Maxwell M. 2018. Review of the prevalence of postnatal depression across cultures. AIMS Public Health 5, 260-295. ( 10.3934/publichealth.2018.3.260) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, Pariante CM. 2014. Effects of perinatal mental disorders on the fetus and child. Lancet 384, 1800-1819. ( 10.1016/s0140-6736(14)61277-0) [DOI] [PubMed] [Google Scholar]
- 5.Pearson RM, Melotti R, Heron J, Joinson C, Stein A, Ramchandani PG, Evans J. 2012. Disruption to the development of maternal responsiveness? The impact of prenatal depression on mother–infant interactions. Infant Behav. Dev. 35, 613-626. ( 10.1016/j.infbeh.2012.07.020) [DOI] [PubMed] [Google Scholar]
- 6.Howard LM, Molyneaux E, Dennis C-L, Rochat T, Stein A, Milgrom J. 2014. Non-psychotic mental disorders in the perinatal period. Lancet 384, 1775-1788. ( 10.1016/s0140-6736(14)61276-9) [DOI] [PubMed] [Google Scholar]
- 7.Gjerde LC, Eilertsen EM, Hannigan LJ, Eley T, Røysamb E, Reichborn-Kjennerud T, Rijsdijk FV, McAdams TA, Ystrom E. 2019. Associations between maternal depressive symptoms and risk for offspring early-life psychopathology: the role of genetic and non-genetic mechanisms. Psychol. Med. 51, 441-449. ( 10.1017/S0033291719003301) [DOI] [PubMed] [Google Scholar]
- 8.Bauer A, Parsonage M, Knapp M, Iemmi V, Adelaja B. 2014. Costs of perinatal mental health problems. London, UK: Centre for Mental Health and London School of Economics. Retrieved from https://www.centreformentalhealth.org.uk/publications/costs-perinatal-mental-health-problems , 07/09/2020.
- 9.PricewaterhouseCoopers Consulting Australia. 2019. The cost of perinatal depression and anxiety in Australia. Sydney, NSW: Gidget Foundation Australia. Retrieved from https://www.perinatalwellbeingcentre.org.au/news/cost-of-perinatal-depression-and-anxietyin-australia, 07/09/2020.
- 10.US Preventive Services Task Force et al. 2019. Interventions to prevent perinatal depression: US Preventive Services Task Force Recommendation Statement. JAMA 321, 580-587. ( 10.1001/jama.2019.0007) [DOI] [PubMed] [Google Scholar]
- 11.Gariepy G, Honkaniemi H, Quesnel-Vallee A. 2016. Social support and protection from depression: systematic review of current findings in Western countries. Br. J. Psychiatry 209, 284-293. ( 10.1192/bjp.bp.115.169094) [DOI] [PubMed] [Google Scholar]
- 12.Beck CT. 2001. Predictors of postpartum depression: an update. Nurs. Res. Pract. 50, 275-285. ( 10.1097/00006199-200109000-00004) [DOI] [PubMed] [Google Scholar]
- 13.Biaggi A, Pariante CM. 2020. Risk factors for depression and anxiety during the perinatal period. In Handbook of perinatal clinical psychology: from theory to practice (eds RM Quatraro, P Grussu), p. 21. New York, NY: Routledge. [Google Scholar]
- 14.Yim IS, Tanner Stapleton LR, Guardino CM, Hahn-Holbrook J, Dunkel Schetter C. 2015. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu. Rev. Clin. Psychol. 11, 99-137. ( 10.1146/annurev-clinpsy-101414-020426) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saxbe D, Rossin-Slater M, Goldenberg D. 2018. The transition to parenthood as a critical window for adult health. Am. Psychol. 73, 1190. ( 10.1037/amp0000376) [DOI] [PubMed] [Google Scholar]
- 16.Budds K. 2021. Validating social support and prioritizing maternal wellbeing: beyond intensive mothering and maternal responsibility. Phil. Trans. R. Soc. B 376, 20200029. ( 10.1098/rstb.2020.0029) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sear R. 2021. The male breadwinner nuclear family is not the ‘traditional’ human family, and promotion of this myth may have adverse health consequences. Phil. Trans. R. Soc. B 376, 20200020. ( 10.1098/rstb.2020.0020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thoits PA. 2011. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 52, 145-161. ( 10.1177/0022146510395592) [DOI] [PubMed] [Google Scholar]
- 19.Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, Ericksen J, Ellwood D, Buist A. 2008. Antenatal risk factors for postnatal depression: a large prospective study. J. Affect. Disord. 108, 147-157. ( 10.1016/j.jad.2007.10.014) [DOI] [PubMed] [Google Scholar]
- 20.Goodman SH, Tully EC. 2009. Recurrence of depression during pregnancy: psychosocial and personal functioning correlates. Depress Anxiety 26, 557-567. ( 10.1002/da.20421) [DOI] [PubMed] [Google Scholar]
- 21.Fontein-Kuipers YJ, Nieuwenhuijze MJ, Ausems M, Bude L, de Vries R.. 2014. Antenatal interventions to reduce maternal distress: a systematic review and meta-analysis of randomised trials. BJOG 121, 389-397. ( 10.1111/1471-0528.12500) [DOI] [PubMed] [Google Scholar]
- 22.Dennis C-L. 2005. Psychosocial and psychological interventions for prevention of postnatal depression: systematic review. BMJ 331, 15. ( 10.1136/bmj.331.7507.15) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patton GC, et al. 2015. Prediction of perinatal depression from adolescence and before conception (VIHCS): 20-year prospective cohort study. Lancet 386, 875-883. ( 10.1016/s0140-6736(14)62248-0) [DOI] [PubMed] [Google Scholar]
- 24.Thomson KC, et al. 2020. Adolescent antecedents of maternal and paternal perinatal depression: a 36-year prospective cohort. Psychol. Med. 1-8. ( 10.1017/S0033291720000902) [DOI] [PubMed] [Google Scholar]
- 25.Hammen C. 1991. Generation of stress in the course of unipolar depression. J. Abnorm. Psychol. 100, 555. ( 10.1037/0021-843X.100.4.555) [DOI] [PubMed] [Google Scholar]
- 26.Asselmann E, Wittchen HU, Erler L, Martini J. 2016. Peripartum changes in social support among women with and without anxiety and depressive disorders prior to pregnancy: a prospective-longitudinal study. Arch. Women's Ment. Health. 19, 943-952. ( 10.1007/s00737-016-0608-6) [DOI] [PubMed] [Google Scholar]
- 27.Rollè L, Giordano M, Santoniccolo F, Trombetta T. 2020. Prenatal attachment and perinatal depression: a systematic review. Int. J. Environ. Res. Public Health 17, 2644. ( 10.3390/ijerph17082644) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fancourt D, Perkins R. 2018. Effect of singing interventions on symptoms of postnatal depression: three-arm randomised controlled trial. Br. J. Psychiatry 212, 119-121. ( 10.1192/bjp.2017.29) [DOI] [PubMed] [Google Scholar]
- 29.Spry E, et al. 2020. The Victorian Intergenerational Health Cohort Study (VIHCS): study design of a preconception cohort from parent adolescence to offspring childhood. Paediatr. Perinat. Epidemiol. 34, 86-98. ( 10.1111/ppe.12602) [DOI] [PubMed] [Google Scholar]
- 30.Australian Bureau of Statistics. 2013. Births, Australia, 2012, Table 1.2 Births, Summary statistics for Victoria—2002 to 2012, data cube: Excel spreadsheet, cat. no. 33010DO001_2012, viewed 18 August 2015. See http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3301.02012?OpenDocument.
- 31.Lewis G, Pelosi AJ, Araya R, Dunn G. 1992. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol. Med. 22, 465-486. ( 10.1017/s0033291700030415) [DOI] [PubMed] [Google Scholar]
- 32.Patton GC, Coffey C, Posterino M, Carlin JB, Wolfe R, Bowes G. 1999. A computerised screening instrument for adolescent depression: population-based validation and application. Soc. Psychiatry Psychiatr. Epidemiol. 34, 166-172. ( 10.1007/s001270050129) [DOI] [PubMed] [Google Scholar]
- 33.Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C. 1997. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 27, 191-197. ( 10.1017/s0033291796004242) [DOI] [PubMed] [Google Scholar]
- 34.Cox JL, Holden JM, Sagovsky R. 1987. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150, 782-786. ( 10.1192/bjp.150.6.782) [DOI] [PubMed] [Google Scholar]
- 35.Murray D, Cox JL. 1990. Screening for depression during pregnancy with the Edinburgh depression scale (EDDS). J. Reprod. Infant Psychol. 8, 99-107. ( 10.1080/02646839008403615) [DOI] [Google Scholar]
- 36.National Collaborating Centre for Mental Health. 2018. Antenatal and postnatal mental health: the NICE guideline on clinical management and service guidance. London, UK: The British Psychological Society and The Royal College of Psychiatrists. [PubMed] [Google Scholar]
- 37.Webster J, Linnane JWJ, Dibley LM, Hinson JK, Starrenburg SE, Roberts JA. 2000. Measuring social support in pregnancy: can it be simple and meaningful? Birth-Issues Perinat. Care 27, 97-101. ( 10.1046/j.1523-536x.2000.00097.x) [DOI] [PubMed] [Google Scholar]
- 38.Webster J, Pritchard MA, Creedy D, East C. 2003. A simplified predictive index for the detection of women at risk for postnatal depression. Birth 30, 101-108. ( 10.1046/j.1523-536X.2003.00228.x) [DOI] [PubMed] [Google Scholar]
- 39.Social Policy Research Centre. 2016. Poverty in Australia. Strawberry Hills, NSW: Australian Council of Social Service. Retrieved from https://www.acoss.org.au/wp-content/uploads/2016/10/Poverty-in-Australia-2016.pdf. on 07/09/2020.
- 40.Cranley MS. 1981. Development of a tool for the measurement of maternal attachment during pregnancy. Nurs. Res. 30, 281-284. ( 10.1097/00006199-198109000-00008) [DOI] [PubMed] [Google Scholar]
- 41.McMahon CA, Boivin J, Gibson FL, Hammarberg K, Wynter K, Saunders D, Fisher J. 2011. Age at first birth, mode of conception and psychological wellbeing in pregnancy: findings from the parental age and transition to parenthood Australia (PATPA) study. Hum. Reprod. 26, 1389-1398. ( 10.1093/humrep/der076) [DOI] [PubMed] [Google Scholar]
- 42.Moreno-Betancur M, Moran P, Becker D, Patton GC, Carlin JB. 2021. Mediation effects that emulate a target randomised trial: simulation-based evaluation of ill-defined interventions on multiple mediators. Stat. Methods Med. Res. ( 10.1177/0962280221998409). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.VanderWeele TJ. 2019. Principles of confounder selection. Eur. J. Epidemiol. 34, 211-219. ( 10.1007/s10654-019-00494-6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moreno-Betancur M, Carlin JB. 2018. Understanding interventional effects: a more natural approach to mediation analysis? Epidemiology 29, 614-617. ( 10.1097/ede.0000000000000866) [DOI] [PubMed] [Google Scholar]
- 45.Vansteelandt S, Daniel RM. 2017. Interventional effects for mediation analysis with multiple mediators. Epidemiology 28, 258-265. ( 10.1097/EDE.0000000000000596) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.White IR, Royston P, Wood AM. 2011. Multiple imputation using chained equations: issues and guidance for practice. Stat. Med. 30, 377-399. ( 10.1002/sim.4067) [DOI] [PubMed] [Google Scholar]
- 47.StataCorp. 2019. Stata Statistical Software: Release 16.
- 48.Pierce GR, Sarason IG, Sarason BR. 1991. General and relationship-based perceptions of social support: are two constructs better than one? J. Pers. Soc. Psychol. 61, 1028. ( 10.1037/0022-3514.61.6.1028) [DOI] [PubMed] [Google Scholar]
- 49.Ainsworth MDS, Eichberg CG.. 1991. Effects on infant–mother attachment of mother's unresolved loss of an attachment figure, or other traumatic experience. In Attachment across the life cycle (eds CM Parkes, J Stevenson-Hinde, P Marris). New York, NY: Routledge. [Google Scholar]
- 50.Webster J, Holt V. 2004. Screening for partner violence: direct questioning or self-report? Obstet. Gynecol. 103, 299-303. ( 10.1097/01.AOG.0000110245.83404.3d) [DOI] [PubMed] [Google Scholar]
- 51.Henrichs KL, McCauley HL, Miller E, Styne DM, Saito N, Breslau J. 2014. Early menarche and childhood adversities in a nationally representative sample. Int. J. Pediatr. Endocrinol. 2014, 14. ( 10.1186/1687-9856-2014-14) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hamilton M, Jenkins B. 2015. Grandparent childcare and labour market participation in Australia (SPRC Report 14/2015). Retrieved from https://nationalseniors.com.au/research/socialconnectedness-communities/grandparent-childcare-and-labour-market-participation-in-australia on 07/09/2020. [Google Scholar]
- 53.Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. 2010. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol. Med. 40, 899-909. ( 10.1017/S0033291709991036) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG. 2017. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 219, 86-92. ( 10.1016/j.jad.2017.05.003) [DOI] [PubMed] [Google Scholar]
- 55.Myers S, Page AE, Emmott EH. 2021. The differential role of practical and emotional support in infant feeding experience in the UK. Phil. Trans. R. Soc. B 376, 20200034. ( 10.1098/rstb.2020.0034) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McLeish J, Redshaw M. 2021. ‘She come like a sister to me’: a qualitative study of volunteer social support for disadvantaged women in the transition to motherhood in England. Phil. Trans. R. Soc. B 376, 20200023. ( 10.1098/rstb.2020.0023) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Milgrom J, Schembri C, Ericksen J, Ross J, Gemmill AW. 2011. Towards parenthood: an antenatal intervention to reduce depression, anxiety and parenting difficulties. J. Affect. Disord. 130, 385-394. ( 10.1016/j.jad.2010.10.045) [DOI] [PubMed] [Google Scholar]
- 58.Milgrom J, Hirshler Y, Reece J, Holt C, Gemmill AW. 2019. Social support—a protective factor for depressed perinatal women? Int. J. Environ. Res. Public Health 16, 1426. ( 10.3390/ijerph16081426) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Barker B, Iles JE, Ramchandani PG. 2017. Fathers, fathering and child psychopathology. Curr. Opin. Psychol. 15, 87-92. ( 10.1016/j.copsyc.2017.02.015) [DOI] [PubMed] [Google Scholar]
- 60.Pilkington PD, Whelan TA, Milne LC. 2015. A review of partner-inclusive interventions for preventing postnatal depression and anxiety. Clin. Psychol. 19, 63-75. ( 10.1111/cp.12054) [DOI] [Google Scholar]
- 61.Daniele MAS. 2021. Male partner participation in maternity care and social support for childbearing women: a discussion paper. Phil. Trans. R. Soc. B 376, 20200021. ( 10.1098/rstb.2020.0021) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Catalao R, Mann S, Wilson C, Howard LM. 2020. Preconception care in mental health services: planning for a better future. Br. J. Psychiatry 216, 180-181. ( 10.1192/bjp.2019.209) [DOI] [PubMed] [Google Scholar]
- 63.Wilson C, Howard LM, Reynolds RM, Simonoff E, Ismail K. 2018. Preconception health. Lancet 392, 2266-2267. ( 10.1016/S0140-6736(18)32199-8) [DOI] [PubMed] [Google Scholar]
- 64.Barker M, et al. 2018. Intervention strategies to improve nutrition and health behaviours before conception. Lancet 391, 1853-1864. ( 10.1016/s0140-6736(18)30313-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Adeyemi-Fowode OA, Gerancher KR. 2018. Promoting healthy relationships in adolescents. Obstet. Gynecol. 132, E213-E220. ( 10.1097/AOG.0000000000002945) [DOI] [PubMed] [Google Scholar]
- 66.Sawyer SM, Afifi RA, Bearinger LH, Blakemore S-J, Dick B, Ezeh AC, Patton GC. 2012. Adolescence: a foundation for future health. Lancet 379, 1630-1640. ( 10.1016/s0140-6736(12)60072-5) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Code for analysis from this paper may be accessed at https://osf.io/4h2xm/?view_only=868a559a861b466caaf50cdd4bdd1606. Ethics approvals for this study do not permit the data to be made publicly available, due to limitations of participant consent and concerns regarding potential re-identifiability. If required and upon request, the dataset subset can be made available to a named individual for the purpose of replication of research findings.