Significance
This comprehensive life-course longitudinal study of body mass index (BMI) contributes knowledge about the temporal dynamics of BMI as individuals age and how social status defines disparities in lifetime obesity risk. Results show that adolescence and young adulthood are critical life stages when excess weight can rapidly accumulate and racial/ethnic or educational disparities emerge, most significantly among recent cohorts of young people. These cohort increases in the prevalence and rate of increase in obesity have alarming consequences for contemporary epidemiologic conditions such as the COVID-19 pandemic and US population health and life expectancy in years to come. Our study further contributes data analytic tools by linking and integrating multiple existing studies to advance science on social determinants of health.
Keywords: body mass index, obesity, life course, age trajectory, social disparities
Abstract
No research exists on how body mass index (BMI) changes with age over the full life span and social disparities therein. This study aims to fill the gap using an innovative life-course research design and analytic methods to model BMI trajectories from early adolescence to old age across 20th-century birth cohorts and test sociodemographic variation in such trajectories. We conducted the pooled integrative data analysis (IDA) to combine data from four national population-based NIH longitudinal cohort studies that collectively cover multiple stages of the life course (Add Health, MIDUS, ACL, and HRS) and estimate mixed-effects models of age trajectories of BMI for men and women. We examined associations of BMI trajectories with birth cohort, race/ethnicity, parental education, and adult educational attainment. We found higher mean levels of and larger increases in BMI with age across more recent birth cohorts as compared with earlier-born cohorts. Black and Hispanic excesses in BMI compared with Whites were present early in life and persisted at all ages, and, in the case of Black–White disparities, were of larger magnitude for more recent cohorts. Higher parental and adulthood educational attainment were associated with lower levels of BMI at all ages. Women with college-educated parents also experienced less cohort increase in mean BMI. Both race and education disparities in BMI trajectories were larger for women compared with men.
Overweight and obesity remain a persistent national public health concern. Obesity is linked to a range of adverse health outcomes, including greater risks of cardiovascular and metabolic diseases, multiple cancers, disability, death, and, most recently, vulnerabilities to COVID-19 infections and related morbidities (1–4). It is most commonly measured through body mass index (BMI), which captures a proportion of individuals’ weight and height (kilograms/meter2). BMI has been identified as a suitable proxy for distinguishing weight status in the population that strongly correlates with direct measures of body fat and chronic disease (5, 6). As of 2016, 70.9% of adults 20 y and over in the United States are considered overweight or obese (BMI = 25.0 to 29.9 or ≥30, respectively) (7). While the obesity epidemic has affected all age groups, the rapid rise in obesity among younger populations is particularly concerning (8). Among children and adolescents, the national rate of obesity has quadrupled over the past 40 y to 18.5% (9). Because youth who are overweight or obese tend to become overweight and obese adults, these shifts forecast increasing future burden of disease (10). The life-course pattern of BMI changes as one ages is critical for quantifying the magnitude of this burden but is understudied. In addition, obesity was considered a biomarker of health disparities with uneven distribution of prevalence across sociodemographic groups (4, 9), but it is not known whether these disparities grow or diminish over the life span. To better understand health risks facing the aging population, further research is needed to illuminate how life-course trajectories of BMI vary across population subgroups defined by gender, race, and educational attainment.
Age Patterns of and Cohort Variation in BMI
Previous research suggests a typically inverted-U-shaped age pattern of body weight and BMI, with weight rising steadily until middle age and stabilizing before an unintentional decline in later life linked to advanced age and treatments for comorbidities (11–13). Meanwhile, it was documented that the obesity epidemic of the past four decades has coincided with an earlier onset of obesity in life in more recent cohorts (14, 15). Given the BMI increase with age early in life (16), the accelerating trends across recent birth cohorts indicate that they will likely experience a greater duration of obesity over their lifetime, followed by poorer health outcomes linked with excess weight (14, 17). These consequences are already reflected among recent cohorts that exhibit higher rates of type-II diabetes, hypertension, and metabolic syndrome at younger ages compared with earlier cohorts (17–20). The extant literature, however, is rather limited in defining how BMI changes with age. The early life period of adolescence, for example, has not been sufficiently studied and yet it is the developmental stage when the social environment becomes increasingly important for obesity risks as young people gain more control over their behavioral choices (21). It is a sensitive period that presents unique opportunities for shaping adult BMI trajectories. The few longitudinal studies of age trajectories of BMI are confined to short time windows in life, such as from early to midlife, or midlife to late life (16, 22, 23). We have yet to understand how BMI development unfolds prospectively over the fuller life span from early to late life. Furthermore, the age change confounds with cohort variation in BMI but has not been properly addressed in studies focusing on age patterns only (24, 25).
Social Disparities in BMI
National estimates indicate that prevalence of overweight and obesity are socially patterned, disproportionately affecting Blacks, Hispanics, and those of lower socioeconomic status (SES) (26, 27) and particularly among women (15, 28–30). Research on SES disparities in BMI highlights the importance of educational status and suggests that both parental and adult educational attainment are strongly related to BMI (30–32). For instance, children whose parents had less than a high school degree were estimated to be three times more likely to be obese by age 6 y compared with peers with highly educated parents (33). Also, according to recent data ∼33% of adults without a high school degree were obese, whereas 21.5% who graduated from college or technical college were considered obese in the same time period (34). Several sociocultural and physiological pathways have been proposed to undergird these observed disparities in BMI, including socially disadvantaged groups having greater exposure to acute and chronic stressors (35, 36), fewer resources to mitigate these exposures such as healthier food choices or opportunities for exercise (37, 38), higher rates of obesogenic behaviors (e.g., sugar-sweetened beverage consumption and less physical activity) (39), possibly in response to elevated stress and less access to health-promoting resources (40), and social stress in the form of institutional and interpersonal discrimination which may accelerate physiological deterioration (41, 42) and disrupt metabolic functioning linked to increased BMI (43).
Although differences in BMI by gender, race/ethnicity, and SES are widely documented, their age patterns of change are not. Existing research is largely concerned with secular trends across population groups in early life but suggests social disparities in BMI may vary over the life course. For instance, the rise in adolescent obesity rates over the past decades has been particularly sharp for female and Black adolescents compared with their male and White counterparts (12, 44, 45). These disparities have been shown to widen between adolescence and midadulthood (46). Further, current national data reveal that the rate of growth has begun to level off among some groups. For example, adolescent obesity has significantly increased among non-Hispanic Blacks and Hispanics over the past two decades, but not among non-Hispanic Whites (47, 48). In adults, these trends also appear to vary by race/ethnicity: Obesity prevalence steadily rose among non-Hispanic White and Hispanic men but has remained stable among non-Hispanic Black men in recent years (48). Cohort analysis of national data also shows increasing Black and White gaps in obesity rates in successive female cohorts, peaking for those born after 1965 (33). In addition to the correlation between parental education and BMI change with age in early life (33), there is evidence that childhood disadvantage was predictive of obesity in adulthood for women (49, 50). Studies of BMI disparities share the data and analytic limitations of BMI studies in the overall population. It remains to be determined how these disparities change with age or how cohort processes shape the life-course trajectories of disparity patterns.
Life-Course Hypotheses of BMI Disparities
The central question this study aims to address is whether and when fundamental social statuses such as birth cohort membership, race/ethnicity, and educational attainment delineate different BMI trajectories across the life course. Do the BMI disparities in early life diminish, persist, or grow in middle age to late life? According to the “principle of cohort differences in aging” (51), cohorts are key contexts for shaping the individual aging process. Different birth cohorts experienced diverse early-life conditions and continuous accumulation of differential exposures to biological, social, and behavioral risk factors for health throughout the life course (52–54). Cohort effects are thus particularly relevant for our life-course investigation of obesity as a chronic metabolic status given the increasing exposures to obesogenic environments such as sedentary lifestyles, high-calorie diets, and technological innovations conducive to obesity in more recent cohorts increasingly earlier in life (55, 56).
In light of these theoretical propositions, we test three hypotheses of BMI change within the life-course theoretical and analytic framework for health disparities (57). First, the intercohort change hypothesis predicts that there are substantial intercohort variations in BMI trajectories over the life course, with more recent cohorts having higher levels and/or rates of increase in BMI. Second, we further test the intracohort inequality hypothesis that racial and educational disparities in BMI change significantly over the life course, independent of cohort differences. Previous studies suggest two alternative directions of change: 1) increasing disparities or widening gaps with age that reflect the cumulative advantage/disadvantage process whereby exposures associated with advantaged or disadvantaged backgrounds accumulate over time to increase the BMI differentials across the life course (58, 59) and 2) decreasing disparities or narrowing gaps with age that reflect the age-as-leveler process due to early mortality of socially disadvantaged adults (60, 61) and/or equalization of work-related resources following the exit of labor force (62). Third, we test the intercohort difference in intracohort inequality hypothesis that the life-course patterns of change in racial and educational disparities in BMI trajectories vary by cohort. That is, we further examine the extent to which cohort-specific social, historical, and epidemiologic contexts may moderate the racial or educational disparities in BMI such that the cumulative advantage/disadvantage or leveling process with aging strengthens or weakens in more recently born cohorts.
Testing these life-course hypotheses using cohort analysis is important for research and policy for three reasons. First, it ensures appropriate inferences are attributed to etiology and/or social causation. Age effects of BMI represent aging-related developmental changes internal to individuals, whereas cohort variation reflects exogenous contextual changes in broader social epidemiologic conditions. Second, it informs the generalizability of findings. In the absence of cohort effects, the rates at which BMI changes with age are equally applicable across all cohorts. However, differences across cohorts indicate the existence of social forces and exposures affecting age changes that are cohort-specific. Third, to the extent that cohort effects serve as aggregate proxies for structural correlates, the distinction of BMI variation by age and cohort is especially valuable for identifying the underlying social and environmental factors that are amenable to modifications. Prior studies of obesity are limited by inadequate research designs that do not allow for the test of these hypotheses. Data are often cross-sectional or short-term longitudinal follow-ups of nonpopulation-based samples of single birth cohorts during one particular life stage. Ignoring cohort effects simplifies the analysis but assumes equal patterns of age change in BMI across individuals born and coming of age in vastly different historical times. This assumption has been shown untenable by increasing evidence to the contrary (24) and needs to be empirically tested. Previous studies also report inconsistent directions of change in health disparities and contradictory findings regarding the cumulative dis/advantage and age-as-leveler theories, partly due to the confounding of aging and cohort differences (57). Furthermore, divergence and convergence in BMI disparities may emerge in different stages of life and for different birth cohorts (63). As a result, previous research cannot adjudicate among competing hypotheses about the intercohort and intracohort heterogeneities. Adequately addressing this problem would require extensive longitudinal data that follow diverse and representative populations from birth to death and analytic designs that make efficient use of such data which have never been implemented to our knowledge.
This study aims to fill persistent gaps in the current body of research on social disparities in BMI over the life course. Given the known biological differences in body composition by sex and the complexity of including multiple interactions (e.g., sex, age, and cohort), we examine three key questions separately for women and men to address our three hypotheses:
-
1)
Intercohort variation – What are the age trajectories of BMI change from adolescence to old age and how do patterns in these trajectories differ by birth cohort?
-
2)
Intracohort heterogeneity – independent of/within birth cohorts,
-
a)
How do BMI trajectories differ by race/ethnicity across the life span?
-
b)
How do BMI trajectories differ by life-course education as measured by both parental and adult educational attainment across the life span?
-
a)
-
3)
Intercohort variation in intracohort heterogeneity – Do patterns of racial and/or educational differences in BMI trajectories further vary by birth cohort? While we focus on the independent racial and educational gradients in BMI change, we also test for interaction effects between cohort and race/ethnicity and cohort and education in longitudinal models of age change to capture potential moderation of these gradients by cohort-related contexts.
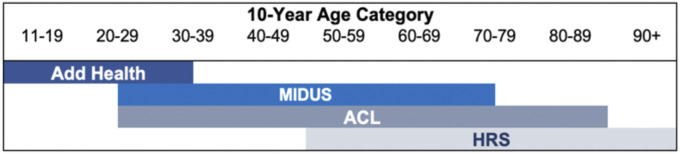
We contend that our study answers these questions of obesity changes with age that no prior study has for three reasons. First, large national datasets such as the National Health and Nutrition Examination Survey (NHANES) tracking the prevalence of obesity across population subgroups are cross-sectional and cannot inform us of how risk changes with age because age effects are confounded with cohort effects in such data. Second, lifetime longitudinal studies that follow diverse and representative populations from birth to death in the United States do not exist. Third, even if they did, their coverage of birth cohorts is limited. That is, they can only provide information about the cohorts who have already aged into later life when what we need is information about the cohorts that are now young and middle-aged adults who will enter old age in the future, or vice versa. Thus, it is impossible to accurately gauge the future disease burden based on conventional data. Our study fills these gaps using a life-course design to integrate multiple diverse population-based longitudinal studies that leverages a more heterogeneous aggregate sample of a wider age range than any existing study to date. Extending prior life-course studies using the coordinated integrative data analysis (IDA) (64–66), we combine four population-based prospective cohort studies into one sample with augmented age ranges using a pooled IDA (Analytic Methods). Fig. 1 illustrates how this research design integrates studies that collectively cover multiple stages of the life course from early adolescence to late adulthood (ages 11 to 90 y and older). The use of innovative design and IDA enables us to test new hypotheses about life-course variations in BMI trajectories not possible before. Our investigations are uniquely capable of revealing specific life periods when BMI increases and social disparities in BMI emerge and enlarge. Identifying time windows within which alterations of facets of social disadvantage would provide maximum benefits can inform more targeted disease prevention and intervention.
Fig. 1.
Integrative life-course research design: age coverage by study membership. This innovative research design uses pooled IDA to combine four large cohort studies: National Longitudinal Study of Adolescent to Adult Health (Add Health), Midlife in the US Study (MIDUS), Americans’ Changing Lives Study (ACL), and the Health and Retirement Study (HRS). These studies collectively cover multiple stages of the life course from adolescence to late adulthood from age 11 through 90 y and older. Data from Add Health, MIDUS, ACL, and HRS included respondents aged 11 to 34 y, 25 to 75 y, 25 to 90 y, and 50 to 107 y, respectively.
Results
Intercohort Change.
Results show evidence supporting hypothesis 1 of intercohort variation in BMI trajectories. The summary statistics presented in Table 1 document the mean BMI values indicating overweight or obese for most age groups except for the adolescents and very old and continuous increases across cohorts born before 1975. Middle-aged adults in recent cohorts born between 1955 and 1984 on average reached the threshold of obesity.
Table 1.
Summary statistics of BMI by age and birth cohort: Pooled data 1986 to 2012
 |
Yellow shading = overweight (BMI 25 to 29.99); red shading = obese (BMI >30).
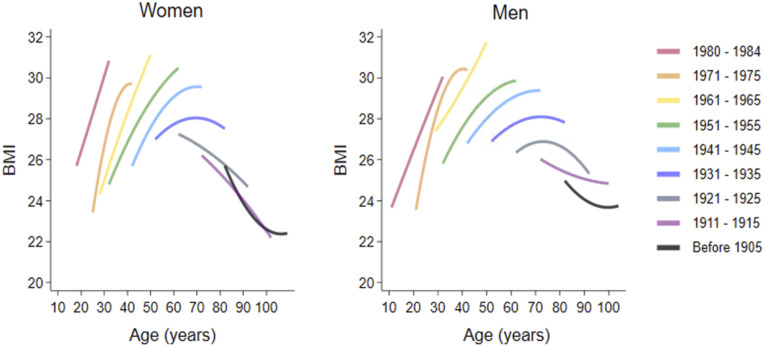
The independent age and cohort effects estimated from the linear mixed-effects growth-curve models are presented in model 1 (SI Appendix, Tables S3 and S4) for women and men. The significant linear and quadratic growth rates of BMI for both genders indicate concave patterns of age change in BMI where BMI increases from adolescence to middle age, peaks between age 50 to 69 y, and begins to decline after the age of 70 y. Consistent with the descriptive analysis in Table 1, there were significant cohort variations in the age trajectories of BMI. Successive birth cohorts had increasing mean levels of BMI [women: β(SE) = 0.62(0.02), P < 0.001; men: β(SE) = 0.51(0.15), P < 0.001] and significant differences in the growth rates (linear and quadratic for women; quadratic for men). As illustrated in Fig. 2 of the model-predicted BMI trajectories, for every other 5-y cohort each successive cohort had higher average BMI and steeper slopes of increase in BMI at the same ages as their predecessors.
Fig. 2.
Predicted BMI trajectories by birth cohort for women and men. Results are based on model 1 in SI Appendix, Tables S3 and S4 for women and men, respectively. Only every other birth cohort is included for purpose of illustration. The overall pattern of BMI change by age was similar for both men and women, with an increase in BMI from adolescence to middle age, peaking around ages 50 to 60 y, and then a decline after the age of 70. The pattern of cohort variation for both genders show that each successive cohort displayed a higher average BMI and steeper slopes of increase in BMI at the same ages than their predecessors.
Intracohort Inequality.
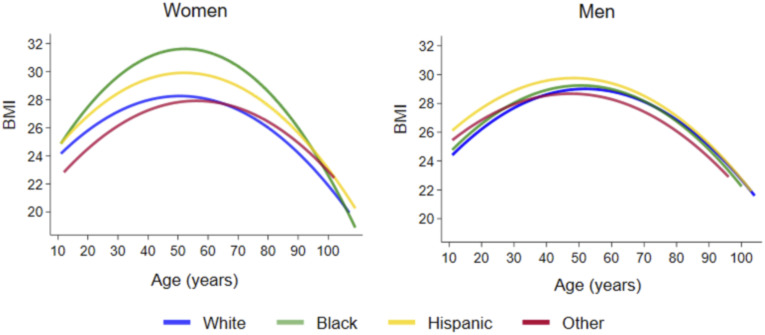
Results shown in models 2 and 3 (SI Appendix, Tables S3 and S4) largely support hypothesis 2: There are significant intracohort racial and educational inequalities in BMI trajectories, net of cohort effects. Model 2 includes fixed effects of race/ethnicity and shows substantial racial differences in the age trajectories of BMI for both genders. Compared with White women, Black and Hispanic women exhibited substantially higher BMI on average [β(SE) = 3.23(0.11), P < 0.001 and β(SE) = 1.98(0.16), P < 0.001, respectively], whereas women in the “Other” race category had lower mean BMI [β(SE) = −0.62(0.25), P < 0.05]. Black women also show significant differences in linear and quadratic rates of change in BMI compared with Whites. Fig. 3 illustrates the racial gradient in BMI trajectories estimated from the model for both women and men. Higher BMI among Blacks relative to Whites and other racial groups is prominent at all ages for women, with the Black–White gap increasing until midlife and then decreasing in late life. The BMI trajectory for Hispanic women lies between those of Blacks and Whites. The results for men show different racial patterns. While both Black and Hispanic men show significantly higher BMI on average than Whites, Hispanic men had higher mean BMI [β(SE) = 1.17(0.14), P < 0.001) than Blacks [β (SE) = 0.21(0.11), P < 0.05], whereas men in the “Other” race category do not differ significantly from Whites. Fig. 3 further shows that the Hispanic–White gap in age trajectories is more prominent in young and middle adulthood and wider than the Black–White gap. Similar to the results for women, racial differences in men increased in early to midlife but gradually disappeared in old age. This suggests that cumulative disadvantage describes racial disparities in BMI during young and middle adulthood, followed by a leveling process of racial gaps in old age.
Fig. 3.
Predicted BMI trajectories by race and ethnicity for women and men. Results are based on model 2 in SI Appendix, Tables S3 and S4, respectively. Black and Hispanic women displayed higher BMI trajectories than White or other race women across the lifespan. Black women had the highest BMI trajectory across all groups, with BMI rising precipitously in early adulthood. For men, the racial/ethnic gradient in BMI trajectory is smaller, with Hispanic men having significantly higher average BMI than White men, particularly in young and midadulthood. Racial gaps generally diminish in old age.
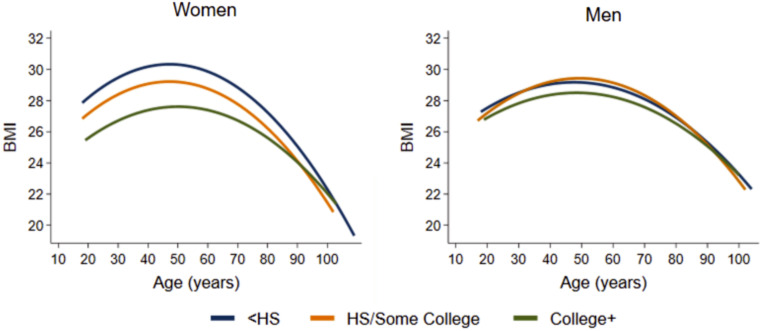
Model 3 includes fixed effects of life-course education variables which show expected negative associations between parental and adult educational attainment with BMI, adjusting for age, cohort, and race/ethnicity. For women, there is a clear educational gradient in the BMI trajectories, as exemplified in Fig. 4. Adults who have or adults with parents who have high school and college degrees show increasingly lower mean BMI compared with those without a high school degree. The associations appear stronger for adult education than parental education when both are included in the model. The gap between the lowest- and highest-educated women remains substantial across the life course until old age, when it starts to diminish due to a significant slowdown of BMI declines with age in college-educated women. The corresponding results for men show similar patterns of the educational gradient that are smaller in magnitude and more modest in statistical significance. For men, it seems only college-level parental and adult education have significant negative associations with mean BMI, and the gaps between all adult educational groups narrowed in old age. In contrast to the directional change in racial gaps in BMI with age, the educational gaps are largely constant in young and middle adulthood and diminished only in late life as predicted by the age-as-leveler model. Adding the life-course education variables slightly attenuated the racial differences in mean BMI, but the racial gaps in women and the Hispanic BMI excess in men remain statistically significant, suggesting important differential racial processes operating independently of educational stratification in BMI trajectories.
Fig. 4.
Predicted BMI trajectories by adult educational status. Results are based on model 3 in SI Appendix, Tables S3 and S4 for women and men, respectively. For women, there is a clear educational gradient in the BMI trajectories, such that those with less than a high school degree have the highest average BMI trajectory, followed by those with a high school degree, and then those with a college degree or more that show the lowest BMI trajectory. This pattern holds across most of the lifespan but then decreases around 100 y of age. The trajectories for men are similar to those of women but smaller in magnitude.
Intercohort Variation in Intracohort Inequality.
We tested interaction effects between cohort and race/ethnicity and cohort and life-course education in all of the intercept, linear, and quadratic growth rate models and included only those that remain statistically significant (at P < 0.05 level, two-tailed test) in the final model 4. The results show evidence in support of hypothesis 3 that there were cohort variations in both racial and educational gradients in BMI trajectories. For women, Hispanic and other race groups had smaller cohort increases in the mean BMI levels than Whites. Black women had a cohort increase in the average BMI level similar to that of White women but different cohort patterns in the age growth trajectories, as indicated by the significant birth-cohort-by-Black interactions in the linear and quadratic growth rate models. The cohort-specific patterns of racial differences are more clearly seen in Fig. 5 where the Black–White gaps in predicted BMI trajectories decreased with age for the earliest cohorts born 1915 to 1924, stayed constant for the subsequent 1935-to-1944 cohorts, diverged for the baby boomers born between 1955 and 1964 with the largest Black excess across all cohorts by midlife, and narrowed for the latest 1975-to-1984 cohorts with similarly high BMI for both groups. For men, the addition of race and cohort interaction terms changed the racial patterning of the mean BMI levels such that the Hispanics no longer differed from Whites in the mean BMI or cohort increase therein. The Black excess compared with Whites, on the other hand, remained significant and enlarged. Like women, men differ in racial patterning of BMI trajectories by birth cohort. Fig. 5 shows that earlier cohorts of Black and White men crossed over in their BMI trajectories in older ages, while more recent cohorts had more parallel age trajectories as Blacks had consistently steeper increases in BMI over all observed ages than Whites.
Fig. 5.
Black–White differences in predicted BMI trajectories by birth cohort. Results are based on model 4 in SI Appendix, Tables S3 and S4 for women and men, respectively. Only every other 10-y birth cohort is included for purpose of illustration. Black women exhibited steeper increases in BMI than White women over all ages and cohorts. Though cohort variations in the Black and White gaps in BMI trajectories are evident for both genders, they are more substantial for women compared with men. More recent cohorts show more consistently greater increases in BMI in Blacks than in Whites.
We found significant cohort variations in the life-course educational gradients in mean levels of but not rate of change in BMI for both genders. Fig. 6 illustrates the mean BMI predicted across cohorts by parental education levels. Women with college-educated parents experienced significantly less cohort increase in the average BMI than their peers with less parental education. For men, high-school-level parental and adult education both show significantly greater cohort increases than college-level education in mean BMI, albeit with smaller differences among the educational groups as well as across cohorts compared with women.
Fig. 6.
Predicted average BMI (with 95% CIs) by birth cohort and parent educational status. Results are based on model 4 in SI Appendix, Tables S3 and S4 for women and men, respectively. Only every other 5-y birth cohort is included for purpose of illustration. While average BMI is similar for all educational groups for the earliest cohorts, gaps between those with more highly educated parents and those with the least-educated parents emerged for cohorts born after 1940 and widened for each consecutive cohort. For both genders there were larger cohort increases in mean BMI in the lower parental educational status groups compared with those with college-educated parents.
Discussion
Excessive weight gain over the life course is known to be associated with various adverse health and well-being outcomes, and sociodemographic subgroups vary widely in prevalence of obesity as well as related health problems (1–4, 7–10). What is not known, however, is how BMI changes during the aging process and how population subgroups differ in such changes. No current research has modeled patterns of change in BMI and social disparities therein over the full life span to definitively answer these questions. In this comprehensive life-course longitudinal study, we fill this gap by characterizing BMI trajectories that spanned from early adolescence to old age for 20th-century birth cohorts ranging from the 1890s to the early 1980s. This paper uses a longitudinal research design combining multiple national cohort studies and conducts a pooled IDA to quantify life-course processes of BMI change at the population level. Our study contributes greater knowledge about the temporal dynamics by which complex interactive effects of race and intergenerational educational attainment are related to BMI at different life-course stages and how these associations vary by birth cohort.
Previous research on the temporal sources of the obesity epidemic in the United States has attributed the surge in obesity rates in recent decades to mainly period effects affecting individuals of all ages as opposed to cohort effects (24, 55). The data on which prior research was based, such as the NHANES or National Health Interview Survey (NHIS), is notably cross-sectional, which makes it impossible to make valid inference about within-individual change over time. The longitudinal data included in our study design allowed us to estimate true within-individual age-related change and distinguish such change from cohort effects for a robust test of the intercohort change hypothesis. Consistent with mounting evidence of cohort heterogeneity in aging experiences across countries (67, 68), our study adds evidence for substantial cohort increases in the mean and growth rates of BMI with age, a finding not possible to discern from an analysis of age trajectories of change alone. This finding is largely consistent with prior work using other national datasets and advanced cohort analysis and modeling that showed the obesity epidemic, while being a period-based phenomenon, had cohort- and age-specific impacts such that younger individuals from most recent cohorts were more affected and had higher BMIs (24, 25). Similar findings of recent cohort increases in BMI trajectories in both the overall population and specific race/ethnic groups such as Black women were also found in studies of single datasets included in our pooled IDA such as ACL (24), MIDUS (69), and HRS (70).
The finding of increasingly earlier onset of obesity suggests increasingly longer durations of its physiological, cognitive, and behavioral impacts over the life span across successive birth cohorts coming of age and entering old age. Moreover, our findings support the demographic forecasts made in previous research about the stagnating decline in heart disease mortality for the 1950s cohorts and mortality increase for the 1970s cohorts (56). The present results also complement established studies that have revealed stronger associations between BMI and certain chronic health conditions (e.g., diabetes and hypertension) for racial and ethnic minorities compared with the general population (71, 72), as well as increasing disability among younger adults and later birth cohorts, possibly due to earlier onset of obesity (73–75).
Recent work suggests that the experience of obesity early in childhood and adolescence positively predicts later obesity in middle age (76). Thus, it is possibly that disparities in obesity emerge even earlier than adolescence (77) and likely contribute to the BMI trajectories observed here. Childhood obesity is beyond the scope of our study due to lack of data for integration, but future investigations into life-course patterns of BMI would benefit from extending analyses to include individuals at earlier ages and those from contemporary birth cohorts. Regardless, our study provides strong evidence that adolescence and young adulthood are particularly important windows in the life course during which excessive weight and its morbidity consequences can rapidly accumulate and are thus critical to reducing future disease burden and death toll in the US population.
Previous research has often found that race/ethnicity and SES are strongly associated with the way health changes over the life course, but the patterns of these changes are much less clear. Because leading theoretical perspectives such as the cumulative advantage/disadvantage and age-as-leveler hypotheses emphasize intracohort differentiation, we appropriately tested these hypotheses by distinguishing age- and cohort-related BMI changes that may otherwise be confounded in previous research. Our analyses explicitly accounting for cohort effects revealed intracohort inequality patterns by race/ethnicity and education across life stages as well as intercohort variation in intracohort heterogeneities not before shown. We note persistent racial and educational disparities of BMI trajectories within cohorts that further change in magnitude across the life span and cohorts. Such patterning is particularly salient for women. We found that on average Black females begin with the highest BMI in adolescence, and this elevated trajectory tracks significantly throughout life, despite slower growth compared with White females in older age. This finding is consistent with previous longitudinal studies (22) and extends our understanding of how racial/ethnic BMI disparities seem to be set early in life (21). The Black–White gaps in the age trajectories show stronger trends of divergence among the baby boomer cohorts than their predecessors, indicating that the cumulative advantage/disadvantage process drove the racial disparities in these cohorts more than the others. The racial patterns of BMI trajectories for men show more complicated patterns of differences among the minorities. We found higher overall BMI levels in Hispanic men compared with the other racial groups. Previous studies showed higher obesity prevalence for Mexican American boys than Whites and Blacks (78) and a similar pattern for Hispanic men (79), although this was limited to ages in adolescence to young adulthood. There may be gender-specific behavioral factors and attitudes toward weight that might help explain the difference between the patterns for Hispanic men and women (80) that are beyond the scope of our investigation and warrant further research.
We found that the life-course process linking parental and adult educational attainment with BMI trajectories produces largely constant gaps between the high and low levels of education for most of adult life. As opposed to cumulative dis/advantages which increase the BMI gap over time, the stability of educational gradients in BMI across age suggests the persistence of early inequality throughout life, reflecting a lasting impact of early-life conditions that set individuals on a stable trajectory with constant dis/advantages that are not altered by adult conditions later in life. We further found larger educational gaps in mean BMI in more recent cohorts. While the average BMI levels increased across cohorts for all groups, individuals from college-educated families or with college education themselves show less increase in recent cohorts. Notably, the protective effects of life-course education are stronger for women than men at most periods of the life span, suggesting a higher return for metabolic health of higher education for women. The gender-specific life-course patterning of education-related BMI change thus indicates the necessity of future research to stratify analyses by gender and the potential benefits for health policy to continuously invest in education for young women.
We further note that racial and ethnic health disparities are often attributed to group differences in socioeconomic resources, owing to the well-established SES–health gradient and large racial/ethnic inequalities in SES (81, 82). Yet, our results reveal that socioeconomic inequality does not fully account for racial/ethnic disparities in BMI, especially when further stratified by gender. A hypothesized mechanism for the racial/ethnic disparity in BMI trajectory is that burdens of discrimination and differential access to health-promoting resources may accelerate biological processes of aging or trigger less health-promoting coping behaviors in minority individuals relative to Whites (83). Indeed, racial and ethnic minorities are more likely than their White counterparts to experience interpersonal discrimination (84), which is linked to greater stress and in turn contributes to health disparities (85). Evidence of structural discrimination in the form of residential segregation and environmental racism may also compound these stressors (86) and contribute to ongoing disparities in overweight and obesity, above and beyond the secular trend. The findings here underscore the need to consider the roles of unequal and cumulative exposure to stressors and discrimination in generating racial health disparities in both women and men. This study also reinforces the growing recognition that multiple social identities overlap and may present different dimensions of disadvantage (e.g., gender discrimination, racial discrimination, and school dropout) that contribute to observed obesity disparities across population subgroups.
Despite these advances, we acknowledge a few study limitations. First, while our measures of early-life SES using the Add Health wave I data reported by the parents provide prospective measures which are an improvement over retrospective reports from respondents used in most prior research, the same early-life measures are not available in the other datasets. In preliminary analyses using individual datasets, we did not observe any substantive differences in the results regarding the associations between BMI trajectories and parental education measured prospectively or retrospectively. We deem it reasonable to combine studies based on this observation. Future research should utilize prospective SES measures wherever possible to better test their associations with BMI outcomes. The substantial evidence of strong educational patterning of BMI outcomes also calls for future research expanding the measurement of SES to other indicators, such as income or wealth, which also exhibit life-course variations. Second, in some waves of data collection, such as Add Health wave I and the ACL, height and weight are self-reported. Although respondents tend to systematically underestimate their weight and overestimate their height (87), self-reported BMI has been found to be an overall reasonable proxy for measured BMI. For example, research comparing self-reported and measured height and weight in Add Health show high correlations (e.g., r = 0.99) and differences are mainly found in the tails of the distributions (88). In addition, report bias producing smaller BMI values, if true, tend to result in conservative estimates regarding the associations between age, gender, race/ethnicity, and education with BMI.
Third, prior studies show that selective mortality may impact the estimation of the life-course duration of severe obesity and its health consequence (89, 90). We consider two ways selective mortality could affect our analysis of the older adults, mostly from the HRS study. First, selective mortality of obese individuals could contribute to an overestimation of cohort effects on obesity. We observe lower mean BMIs for the earliest-born cohorts in our sample. It is possible that members of these birth cohorts who were obese died prior to being surveyed. However, cohort effects on BMI levels similar to those reported here have been observed in other data such as the NHIS and NHANES that are less subject to this limitation (24, 55).
Therefore, we expect any bias this contributes to our analysis is small. Second, selective mortality could render underestimation of disparities in late-life BMI trajectories because those most deprived of social and economic resources earlier in life, who are also often racial and ethnic minorities (91), are less likely to have survived to be observed at older ages. We probed this possibility by testing the mortality related attrition effect using the HRS sample. In a sensitivity analysis, we added the attrition status variables (died during follow-up; nonresponse during follow-up) to the growth curve models and compared the coefficients with those in the models without attrition status in the HRS sample as well as the pooled IDA sample. The conclusions remained the same after accounting for those who died with fewer follow-up observations relative to their peers and higher baseline BMIs and steeper rates of increase with age. Future research should further examine with additional samples whether the selective survival of more robust individuals in late life alone or other homogenizing mechanisms operate to reduce the subgroup differences in old age.
Fourth, we focused our analyses on modeling the temporal dynamics of BMI change with age and did not examine potential mediating roles of health behavioral or psychosocial factors previously linked to metabolic health outcomes in explaining the cohort, race, or SES–BMI associations. Prior studies using other national datasets such as the NHANES and NHIS show that adjusting for obesity-prone behaviors such as physical inactivity and consumption of savory snacks or sugar-sweetened beverages explained some period increases but not recent cohort increases in obesity risks (24). Other studies of individual datasets included in our integrated study showed varying influences of behavioral risk factors as potential mediating mechanisms across life stages. For instance, the Add Health data show that fast-food consumption mediated some race/ethnic and parental SES associations with BMI in young adulthood, but physical inactivity, cigarette smoking, alcohol abuse, and social isolation were not associated with BMI in the same model including all covariates (30). Coordinated IDA studies including the MIDUS and HRS showed that behavioral covariates such as social isolation, depressive symptoms, physical activity, and cigarette smoking did not individually or jointly mediate the adult SES–BMI associations in middle to older adulthood (64, 65). It is possible that other SES-related factors such as health care access, neighborhood exposures, and cognitive or noncognitive skills are at play. It is also possible that racial minority status and SES disadvantage may act as direct stressors to induce adverse physical conditions rather than indirectly through behavioral and psychosocial pathways (92). Addressing this question requires additional covariates standardized across datasets which were not available in our analysis and is a topic for future research.
In light of the above considerations, our study has made significant contributions to the literature. It provides an extensive life-course and cohort analysis of BMI change and its social patterning across multiple developmental periods, including adolescence and young, mid, and late adulthood. This study informs improved approaches to obesity prevention and reducing health disparities by identifying adolescence and young adulthood as critical time windows when excess weight can rapidly accumulate and racial/ethnic or educational disparities emerge and become set throughout adulthood, most significantly among recent cohorts of young people. These cohort increases in the prevalence and rate of increase in obesity has alarming consequences for contemporary epidemiologic conditions such as the COVID-19 pandemic and US population health and life expectancy in years to come. Our study further contributes innovative data analytic tools in response to an increased demand for linking and integrating multiple existing studies to advance science on the social determinants of health in the era of big data.
Materials and Methods
Data.
We used data combined from four national longitudinal surveys summarized in SI Appendix, Table S1. These combined data yielded a total of 64,999 respondents at baselines and 272,472 person-years of observations from 1986 to 2012, after excluding those missing information on height and weight or with biologically implausible BMI values (BMI <12 or >70 kg/m2; n = 370) following guidelines in previous studies (93, 94). Data for adolescence to young adulthood came from participants in the National Longitudinal Study of Adolescent to Adult Health (Add Health) ages 11 to 19 y in wave I (1994 to 1995), followed up in wave III (2001 to 2002) at ages 18 to 26 y and in wave IV (2008) at ages 24 to 34 y (95). Data for young to midadulthood are from two other studies, including respondents aged 25 to 90 y in the Americans’ Changing Lives Study (ACL) (96) surveyed at wave I (1986), with survivors followed up at wave II (1989), wave III (1994), wave IV (2001 to 2002), and wave V (2011); respondents aged 25 to 75 y from the Midlife in the US Study (MIDUS) (97) were surveyed in wave I (1995) and wave II (2005). Data for mid to late adulthood are from three studies, including the ACL and MIDUS, and participants were aged 50 y and older in the Health and Retirement Study (HRS) (98) at baseline in 1992 and 1998 and followed every 2 y through 2012.
Baseline sample characteristics by data source are reported in SI Appendix, Table S2, which presents the weighted descriptive statistics of all variables used in the analysis. We used the study-specific sampling weights to account for the sampling designs within studies and normed these weights for the pooled sample. The average baseline BMI across all studies is 27.8 (SD = 5.9), which falls within the overweight category. The pooled sample has a mean age of 58 y (SD = 18.9; range = 11 to 107) and is 52.2% female and 78.9% non-Hispanic White. Nearly half of respondents’ parents (45.1%) did not graduate high school. Most respondents had a high school degree or higher (80.6%). A small percentage of the sample (8.7%) was born outside of the United States.
Measures.
BMI.
BMI was calculated from participants’ weight and height using the standard formula adapted for US customary units (weight in pounds*703)/height in inches squared (99). Height and weight were measured in all study waves except for the ACL and wave I of Add Health, where height and weight were self-reported. Previous research has indicated that self-reported data are highly correlated with measured height and weight and is a valid indicator for BMI (100).
Race/ethnicity.
We grouped participants into four categories based on self-reported race/ethnicity: non-Hispanic White, non-Hispanic Black, Hispanic, and other.
Life-course education.
Life-course education was measured as parental and adult education status. Parental education was reported by participant’s parents in Add Health and by participants in HRS, MIDUS, and ACL. It was measured as the maximum of mother and father educational attainment as either highest degree earned or total number of years of schooling in two-parent households. We converted the variable to three categories consistent across datasets: <12 y or less than high school, 12 to 15 y or high school/some college, and 16 or more years or college degree or more. Adult education was reported by respondents as the years of schooling completed and coded into the same categories as the parental education. For Add Health respondents who were young at baseline, we combined data from all waves to get the highest level of education completed.
Age and birth cohort.
Age was recorded at each wave in single years. Respondents were grouped into 17 distinct 5-y birth cohorts ranging from before 1905 to 1980 to 1984.
Study membership.
A group of binary indicator variables of the source of data or membership in specific study, including Add Health, MIDUS, HRS, and ACL.
Immigrant status.
A binary indicator of immigrant status (foreign born vs. not) was also included as a covariate.
Analytic Methods.
IDA.
Originated from psychometrics and developmental sciences, IDA has the distinct advantage of permitting examination of an extended developmental period beyond any one study. Prior applications of the extensive life-course design used a form of the IDA, i.e., coordinated analysis consisting of coordinated parallel modeling within each individual dataset to examine the same associations between harmonized measures of social factors and biomarkers across the datasets (64–66). The inference drawn about the life-course variation in the associations of interest is qualitative and indirect. In this study, we extend prior coordinated analysis to a pooled analysis of the combined data from multiple studies using a synthesized multicohort or cohort-sequential design to model the age patterns of BMI change. This method is particularly well-suited for our approach given the large sample sizes and extensive overlap in ages across studies that allow for the creation of a pooled dataset with an augmented age range for the rigorous test of our life-course hypotheses. Table 1 depicts the accelerated longitudinal data structure that consists of adjacent birth cohorts that have substantial age overlaps that range from 20 to 40 y. Such extensive overlap in ages across studies of multiple birth cohorts provides greater statistical power for longitudinal analyses of age and cohort differences than any previous single cohort studies.
In combining independent studies, we followed the principled and well-validated methods for cohort-sequential IDA developed by Curran and colleagues (101, 102) Importantly, between-sample heterogeneity is a distinct strength of IDA given enhanced participant demographic representation, broader age, period, and cohort assessments, and enhanced psychometric assessment of core theoretical constructs. To capitalize on these strengths, we build on the established methodological guidelines for synthesizing large longitudinal datasets (101, 102) to enhance study comparability by directly modeling heterogeneity across studies to strengthen both internal and external validity about resulting population inferences. We explicitly accounted for heterogeneity across studies due to measurement, sampling design, and historical time. First, all measures of our research interest are available across datasets, which greatly facilitated the creation of commensurate variables of key exposures used in the pooled analysis. The harmonization of these variables across studies was conducted in the same fashion as the original study of the life-course design by Yang and Land (24). Second, we directly model study membership as a fixed effect in all analysis to account for study-related differences. Third, we further adjust for time period and birth cohort effects using methods for longitudinal cohort analysis as described below.
Linear mixed-effects growth-curve models.
Linear mixed-effects (generalized linear mixed model) growth-curve models were employed for the IDA of age trajectories of change in BMI across the life course. These models have the advantage of allowing data unbalanced in time by incorporating all individuals regardless of the number of waves they contribute to the person-year dataset, thereby reducing the number of cases lost to follow-up (103, 104). In these models, age trajectories of BMI change are defined by two growth parameters, including the intercept and slope, which are allowed to vary from individual to individual (as random effects) and to vary by respondent characteristics (as fixed effects). A basic model specification for estimating the associations of birth cohort, race, and education with the BMI growth trajectories is the following.
Level-1 repeated observation model.
where BMIti is the BMI score for respondent i at time t, for i = 1,…,n and t =1,…,Ti (Ti is the number of measurements and ranges from 1 to the maximum number of waves) and is modeled as a function of age (centered around cohort median), with the random within-person error of assumed to be normally distributed.
Level-2 model.
where growth parameters, including , , and , depend on person-level characteristics, birth cohort, race/ethnicity and life-course education variables. The level-2 model thus specifies a distinct average trajectory for each racial and educational group, adjusting for birth cohort variation. The residual random effects, are assumed to have a multivariate normal distribution. In all models we adjust for study membership to account for study design effects as well as other control variables. In the growth parameters models above, the cohort effect coefficients (, , and represent the test for the intercohort change hypothesis, and the race (, , and and education (, , and effect coefficients represent the tests for the intracohort inequality hypothesis. We further tested the intercohort change in intracohort inequality hypothesis by including the interaction effects of birth cohort with race and education variables in models for all growth parameters specified above. We estimated these models separately for men and women given the known sex differences in the biology of obesity. We further tested the sex differences by including interaction effects of sex with covariates in growth models. The presence of statistical significance for most of these interactions supports the stratified analyses and meaningful comparisons of findings for men and women.
Distinguishing aging from cohort effects within a single longitudinal study is complicated by two key issues identified before (24). The first key issue is that the observed age ranges differ by birth cohort, so age and cohort variables are highly correlated for nonoverlapping segments of the life course. We used two analytic strategies to resolve this problem. First, we used cohort-median-centered age variables to prevent the bias in the estimate arising from systematic variation in age across the cohorts (57, 86). Second, the use of IDA based on the enhanced longitudinal design further strengthens the tests of significance given the combination of more birth cohorts with augmented age coverages (increased overlapping ages) across studies.
The second key issue concerns period effects. The simultaneous estimation of age, period, and cohort effects creates the model identification problem. We adopted two alternatives. First, within each study that spans short time periods, period effects can be assumed to be trivial and omitted from the models, or otherwise detected through the age-by-cohort interaction effects (68). Further, pooling multiple datasets that span different periods, we also estimated additional fixed effects of study membership and birth-cohort-by-study interaction. Because the additional analyses including the cohort-by-study interaction showed no statistical significance for the interaction term or improved model fit, we estimated the models without the interaction term in the final analyses presented below. Statistical analyses were conducted using Stata 16.1 (StataCorp).
Supplementary Material
Acknowledgments
This research is supported by NIH grants to Y.C.Y. (R01 AG057800) and K.M.H. (P01 HD31921) and to the Carolina Population Center for training (T32 HD007168 and T32 HD091058) and research support (R24 HD050924) and is also supported by University Cancer Research Funds to Y.C.Y. at the Lineberger Cancer Center. This research uses data from Add Health, a program project directed by K.M.H. and designed by J. Richard Udry, Peter S. Bearman, and K.M.H. at the University of North Carolina at Chapel Hill and funded by Grant P01 HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Information on how to obtain the Add Health data files is available on the Add Health website (https://addhealth.cpc.unc.edu). We thank the reviewers for their insightful comments and suggested revisions of earlier versions of this paper.
Footnotes
Competing interest statement: Y.C.Y. and B.L. are coauthors on a 2017 article.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2020167118/-/DCSupplemental.
Data Availability
All study data are included in the article and/or SI Appendix.
References
- 1.Halfon N., Larson K., Slusser W., Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad. Pediatr. 13, 6–13 (2013). [DOI] [PubMed] [Google Scholar]
- 2.Kearns K., Dee A., Fitzgerald A. P., Doherty E., Perry I. J., Chronic disease burden associated with overweight and obesity in Ireland: The effects of a small BMI reduction at population level. BMC Public Health 14, 143 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garvey W. T.et al.; Reviewers of the AACE/ACE Obesity Clinical Practice Guidelines , American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr. Pract. 22, 1–203 (2016). [DOI] [PubMed] [Google Scholar]
- 4.Belanger M. J., et al., Covid-19 and disparities in nutrition and obesity. N. Engl. J. Med. 383, e69 (2020). [DOI] [PubMed] [Google Scholar]
- 5.Sun Q., et al., Comparison of dual-energy x-ray absorptiometric and anthropometric measures of adiposity in relation to adiposity-related biologic factors. Am. J. Epidemiol. 172, 1442–1454 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huxley R., Mendis S., Zheleznyakov E., Reddy S., Chan J., Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk–A review of the literature. Eur. J. Clin. Nutr. 64, 16–22 (2010). [DOI] [PubMed] [Google Scholar]
- 7.National Center for Health Statistics (US) , “Health, United States, 2018” (National Center for Health Statistics, Hyattsville, MD, 2019). [PubMed]
- 8.Ogden C. L., Carroll M. D., Fryar C. D., Flegal K. M., Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS Data Brief, 1–8 (2015). [PubMed] [Google Scholar]
- 9.Skinner A. C., Ravanbakht S. N., Skelton J. A., Perrin E. M., Armstrong S. C., Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 141, e20173459 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Pergola G., Silvestris F., Obesity as a major risk factor for cancer. J. Obes. 2013, 291546 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheehan T. J., DuBrava S., DeChello L. M., Fang Z., Rates of weight change for Black and White Americans over a twenty year period. Int. J. Obes. Relat. Metab. Disord. 27, 498–504 (2003). [DOI] [PubMed] [Google Scholar]
- 12.Clarke P., O’Malley P. M., Johnston L. D., Schulenberg J. E., Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986-2004. Int. J. Epidemiol. 38, 499–509 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagin D. S., Odgers C. L., Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 6, 109–138 (2010). [DOI] [PubMed] [Google Scholar]
- 14.Lee J. M., et al., Getting heavier, younger: Trajectories of obesity over the life course. Int. J. Obes. 34, 614–623 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson W., Li L., Kuh D., Hardy R., How has the age-related process of overweight or obesity development changed over time? Co-ordinated analyses of individual participant data from five United Kingdom birth cohorts. PLoS Med. 12, e1001828, discussion e1001828 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zajacova A., Burgard S. A., Body weight and health from early to mid-adulthood: A longitudinal analysis. J. Health Soc. Behav. 51, 92–107 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reinehr T., Metabolic syndrome in children and adolescents: A critical approach considering the interaction between pubertal stage and insulin resistance. Curr. Diab. Rep. 16, 8 (2016). [DOI] [PubMed] [Google Scholar]
- 18.Pinhas-Hamiel O., Zeitler P., The global spread of type 2 diabetes mellitus in children and adolescents. J. Pediatr. 146, 693–700 (2005). [DOI] [PubMed] [Google Scholar]
- 19.Nguyen Q. C., et al., Blood spot-based measures of glucose homeostasis and diabetes prevalence in a nationally representative population of young US adults. Ann. Epidemiol. 24, 903–9.e1 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nguyen Q. C., et al., Discordance in national estimates of hypertension among young adults. Epidemiology 22, 532–541 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris K. M., An integrative approach to health. Demography 47, 1–22 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hargrove T. W., BMI trajectories in adulthood: The intersection of skin color, gender, and age among African Americans. J. Health Soc. Behav. 59, 501–519 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gordon-Larsen P., The N. S., Adair L. S., Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity (Silver Spring) 18, 1801–1804 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang Y., Land K. C., Age-Period-Cohort Analysis: New Models, Methods, and Empirical Applications (Chapman and Hall/CRC, 2013). [Google Scholar]
- 25.Masters R. K., Powers D. A., Link B. G., Obesity and US mortality risk over the adult life course. Am. J. Epidemiol. 177, 431–442 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hales C. M., Carroll M. D., Fryar C. D., Ogden C. L., Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief, 1–8 (2017). [PubMed] [Google Scholar]
- 27.Ailshire J. A., House J. S., The unequal burden of weight gain: An intersectional approach to understanding social disparities in BMI trajectories from 1986 to 2001/2002. Soc. Forces 90, 397–423 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Center for Health Statistics (US) , “Health, United States, 2015: With special feature on racial and ethnic health disparities” (Report No. 2016-1232, National Center for Health Statistics, Hyattsville, MD, 2016), p. 26. [PubMed]
- 29.Flegal K. M., Kruszon-Moran D., Carroll M. D., Fryar C. D., Ogden C. L., Trends in obesity among adults in the United States, 2005 to 2014. JAMA 315, 2284–2291 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yang Y. C., Johnson M. P., Schorpp K. M., Boen C. E., Harris K. M., Young adult risk factors for cancer: Obesity, inflammation, and sociobehavioral mechanisms. Am. J. Prev. Med. 53, S21–S29 (2017a). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McLaren L., Socioeconomic status and obesity. Epidemiol. Rev. 29, 29–48 (2007). [DOI] [PubMed] [Google Scholar]
- 32.Bae D., Wickrama K. A. S., O’Neal C. W., Social consequences of early socioeconomic adversity and youth BMI trajectories: Gender and race/ethnicity differences. J. Adolesc. 37, 883–892 (2014). [DOI] [PubMed] [Google Scholar]
- 33.Lamerz A., et al., Social class, parental education, and obesity prevalence in a study of six-year-old children in Germany. Int. J. Obes. 29, 373–380 (2005). [DOI] [PubMed] [Google Scholar]
- 34.Robert Wood Johnson Foundation and Trust for America’s Health , F as in Fat: How Obesity Threatens America’s Future (Trust for America’s Health, Washington, DC, 2011). [Google Scholar]
- 35.Link B. G., Phelan J., Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995, 80–94 (1995). [PubMed] [Google Scholar]
- 36.Phelan J. C., Link B. G., Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 41, 311–330 (2015). [Google Scholar]
- 37.Morland K., Wing S., Diez Roux A., The contextual effect of the local food environment on residents’ diets: The atherosclerosis risk in communities study. Am. J. Public Health 92, 1761–1767 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Powell L. M., Slater S., Chaloupka F. J., The relationship between community physical activity settings and race, ethnicity and socioeconomic status. Evidence-based preventive. Medicine (Baltimore) 1, 135–144 (2004). [Google Scholar]
- 39.Gordon-Larsen P., Nelson M. C., Popkin B. M., Longitudinal physical activity and sedentary behavior trends: Adolescence to adulthood. Am. J. Prev. Med. 27, 277–283 (2004). [DOI] [PubMed] [Google Scholar]
- 40.Kant A. K., Graubard B. I., 40-year trends in meal and snack eating behaviors of American adults. J. Acad. Nutr. Diet. 115, 50–63 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Colen C. G., Addressing racial disparities in health using life course perspectives: Toward a constructive criticism. Du Bois Rev. 8, 79–94 (2011). [Google Scholar]
- 42.Gee G. C., Ford C. L., Structural racism and health inequities: Old issues, new directions. Du Bois Rev. 8, 115–132 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mattei G., Bursi S., Ferrari S., 598–The sixth criterion of the metabolic syndrome. Eur. Psychiatry 28, 1 (2013).21920709 [Google Scholar]
- 44.Ogden C. L., Carroll M. D., Kit B. K., Flegal K. M., Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 311, 806–814 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee H., Lee D., Guo G., Harris K. M., Trends in body mass index in adolescence and young adulthood in the United States: 1959-2002. J. Adolesc. Health 49, 601–608 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McTigue K. M., Garrett J. M., Popkin B. M., The natural history of the development of obesity in a cohort of young U.S. adults between 1981 and 1998. Ann. Intern. Med. 136, 857–864 (2002). [DOI] [PubMed] [Google Scholar]
- 47.Ogden C. L., et al., Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA 315, 2292–2299 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ogden C. L., et al., Trends in obesity prevalence by race and hispanic origin—1999-2000 to 2017-2018. JAMA 324, 1208–1210 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khlat M., Jusot F., Ville I., Social origins, early hardship and obesity: A strong association in women, but not in men? Soc. Sci. Med. 68, 1692–1699 (2009). [DOI] [PubMed] [Google Scholar]
- 50.Lee H., Harris K. M., Gordon-Larsen P., Life course perspectives on the links between poverty and obesity during the transition to young adulthood. Popul. Res. Policy Rev. 28, 505–532 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Riley M. W., On the significance of age in sociology. Soc. Change Life Course 1, 24–45 (1988). [Google Scholar]
- 52.Ryder N. B., The cohort as a concept in the study of social change. Am. Sociol. Rev. 30, 843–861 (1965). [PubMed] [Google Scholar]
- 53.Ben-Shlomo Y., Kuh D., A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. Int. J. Epidemiol. 31, 285–293 (2002). [PubMed] [Google Scholar]
- 54.Finch C. E., Crimmins E. M., Inflammatory exposure and historical changes in human life-spans. Science 305, 1736–1739 (2004). [DOI] [PubMed] [Google Scholar]
- 55.Reither E. N., Hauser R. M., Yang Y., Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc. Sci. Med. 69, 1439–1448 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Reither E. N., Olshansky S. J., Yang Y., New forecasting methodology indicates more disease and earlier mortality ahead for today’s younger Americans. Health Aff. (Millwood) 30, 1562–1568 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang Y., Lee L. C., Sex and race disparities in health: Cohort variations in life course patterns. Soc. Forces 87, 2093–2124 (2009). [Google Scholar]
- 58.O’Rand A. M., “Cumulative processes in the life course” in The Craft of Life Course Research, Elder G. H., Giele J. Z., Eds. (Guilford Press, New York, 2009), pp. 121–140. [Google Scholar]
- 59.Willson A. E., Shuey K. M., Elder G. H. Jr, Cumulative advantage processes as mechanisms of inequality in life course health. Am. J. Sociol. 112, 1886–1924 (2007). [Google Scholar]
- 60.Dupre M. E., Educational differences in age-related patterns of disease: Reconsidering the cumulative disadvantage and age-as-leveler hypotheses. J. Health Soc. Behav. 48, 1–15 (2007). [DOI] [PubMed] [Google Scholar]
- 61.Kim J., Miech R., The Black-White difference in age trajectories of functional health over the life course. Soc. Sci. Med. 68, 717–725 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.O’Rand A. M., Henretta J. C., Age and Inequality: Diverse Pathways through Later Life (Westview Press, Boulder, CO, 1999). [Google Scholar]
- 63.Brown T. H., O’Rand A. M., Adkins D. E., Race-ethnicity and health trajectories: Tests of three hypotheses across multiple groups and health outcomes. J. Health Soc. Behav. 53, 359–377 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yang Y. C., Gerken K., Schorpp K., Boen C., Harris K. M., Early-life socioeconomic status and adult physiological functioning: A life course examination of biosocial mechanisms. Biodemogr. Soc. Biol. 63, 87–103 (2017b). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yang Y. C., Schorpp K., Boen C., Johnson M., Harris K. M., Socioeconomic status and biological risks for health and illness across the life course. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 613–624 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang Y. C., et al., Social relationships and physiological determinants of longevity across the human life span. Proc. Natl. Acad. Sci. U.S.A. 113, 578–583 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yang Y., Lee L. C., Dynamics and heterogeneity in the process of human frailty and aging: Evidence from the U.S. older adult population. J. Gerontol. B Psychol. Sci. Soc. Sci. 65B, 246–255 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chen F., Yang Y., Liu G., Social change and socioeconomic disparities in health over the life course in China: A cohort analysis. Am. Sociol. Rev. 75, 126–150 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee C., Park S., Examining cumulative inequality in the association between childhood socioeconomic status and body mass index from midlife to old age. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 1264–1274 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pavela G., Is childhood socioeconomic status independently associated with adult BMI after accounting for adult and neighborhood socioeconomic status? PLoS One 12, e0168481 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Taylor H. A. Jr, et al., Relationships of BMI to cardiovascular risk factors differ by ethnicity. Obesity (Silver Spring) 18, 1638–1645 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Colin Bell A., Adair L. S., Popkin B. M., Ethnic differences in the association between body mass index and hypertension. Am. J. Epidemiol. 155, 346–353 (2002). [DOI] [PubMed] [Google Scholar]
- 73.Mehta N. K., Chang V. W., Secular declines in the association between obesity and mortality in the United States. Popul. Dev. Rev. 37, 435–451 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alley D. E., Chang V. W., The changing relationship of obesity and disability, 1988-2004. JAMA 298, 2020–2027 (2007). [DOI] [PubMed] [Google Scholar]
- 75.Al Snih S., et al., The effect of obesity on disability vs mortality in older Americans. Arch. Intern. Med. 167, 774–780 (2007). [DOI] [PubMed] [Google Scholar]
- 76.Rundle A. G., et al., Tracking of obesity in childhood into adulthood: Effects on body mass index and fat mass index at age 50. Child. Obes. 16, 226–233 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dixon B., Peña M. M., Taveras E. M., Lifecourse approach to racial/ethnic disparities in childhood obesity. Adv. Nutr. 3, 73–82 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.MacKay A. P., Fingerhut L. A., Duran C. R., “Health, United States, 2000: Adolescent Health Chartbook” (National Center for Health Statistics, Hyattsville, MD, 2000).
- 79.Albrecht S. S., Gordon-Larsen P., Ethnic differences in body mass index trajectories from adolescence to adulthood: A focus on Hispanic and Asian subgroups in the United States. PLoS One 8, e72983 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Williams J. E., Kabukuru A., Mayo R., Griffin S. F., Commentary: A social-ecological perspective on obesity among Latinos. Ethn. Dis. 21, 467–472 (2011). [PubMed] [Google Scholar]
- 81.Wang Y., Zhang Q., Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am. J. Clin. Nutr. 84, 707–716 (2006). [DOI] [PubMed] [Google Scholar]
- 82.Farmer M. M., Ferraro K. F., Are racial disparities in health conditional on socioeconomic status? Soc. Sci. Med. 60, 191–204 (2005). [DOI] [PubMed] [Google Scholar]
- 83.Jackson P. B., Health inequalities among minority populations. J. Gerontol. B Psychol. Sci. Soc. Sci., 60, S63–S67 (2005). [DOI] [PubMed] [Google Scholar]
- 84.Forman T. A., Williams D. R., Jackson J. S., Gardner C., “Race, place, and discrimination” in Perspectives on Social Problems, Gardner C., Ed. (JAI Press, 1997), pp. 231–261. [Google Scholar]
- 85.Williams D. R., Mohammed S. A., Discrimination and racial disparities in health: Evidence and needed research. J. Behav. Med. 32, 20–47 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yao L., Robert S. A., The contributions of race, individual socioeconomic status, and neighborhood socioeconomic context on the self-rated health trajectories and mortality of older adults. Res. Aging 30, 251–273 (2008). [Google Scholar]
- 87.Spencer E. A., Appleby P. N., Davey G. K., Key T. J., Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr. 5, 561–565 (2002). [DOI] [PubMed] [Google Scholar]
- 88.Kuczmarski M. F., Kuczmarski R. J., Najjar M., Effects of age on validity of self-reported height, weight, and body mass index: Findings from the third national health and nutrition examination survey, 1988-1994. J. Am. Diet. Assoc. 101, 28–34, quiz 35–36 (2001). [DOI] [PubMed] [Google Scholar]
- 89.Ferraro K. F., Thorpe R. J. Jr, Wilkinson J. A., The life course of severe obesity: Does childhood overweight matter? J. Gerontol. B Psychol. Sci. Soc. Sci. 58, S110–S119 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ferraro K. F., Kelley-Moore J. A., Cumulative disadvantage and health: Long-term consequences of obesity? Am. Sociol. Rev. 68, 707–729 (2003). [PMC free article] [PubMed] [Google Scholar]
- 91.Hayward M. D., Miles T. P., Crimmins E. M., Yang Y., The significance of socioeconomic status in explaining the racial gap in chronic health conditions. Am. Sociol. Rev. 65, 910–930 (2000). [Google Scholar]
- 92.Boen C., Yang Y. C., The physiological impacts of wealth shocks in late life: Evidence from the Great Recession. Soc. Sci. Med. 150, 221–230 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Li W., et al., Small-area estimation and prioritizing communities for obesity control in Massachusetts. Am. J. Public Health 99, 511–519 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cheng F. W., et al., Body mass index and all-cause mortality among older adults. Obesity (Silver Spring) 24, 2232–2239 (2016). [DOI] [PubMed] [Google Scholar]
- 95.Harris K. M., et al., Cohort profile: The national longitudinal study of adolescent to adult health (Add Health). Int. J. Epidemiol. 48, 1415–1415k (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.University of Michigan , Institute for Social Research, Americans’ Changing Lives (ACL). https://acl.isr.umich.edu/. Accessed 12 December 2019.
- 97.University of Wisconsin-Madison , Institute on Aging, Midlife in the United States (MIDUS). http://midus.wisc.edu/. Accessed 22 January 2020.
- 98.University of Michigan , Institute for Social Research, The Health and Retirement Study (HRS). https://hrs.isr.umich.edu/. Accessed 22 January 2020.
- 99.Oria H. E., et al. , Guidelines for weight calculations and follow-up in bariatric surgery. Surg. Obes. Relat. Dis. 1, 67–68 (2005). [DOI] [PubMed] [Google Scholar]
- 100.Goodman E., Hinden B. R., Khandelwal S., Accuracy of teen and parental reports of obesity and body mass index. Pediatrics 106, 52–58 (2000). [DOI] [PubMed] [Google Scholar]
- 101.Curran P. J., Hussong A. M., Integrative data analysis: The simultaneous analysis of multiple data sets. Psychol. Methods 14, 81–100 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bainter S. A., Curran P. J., Advantages of integrative data analysis for developmental research. J. Cogn. Dev. 16, 1–10 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Miyazaki Y., Raudenbush S. W., Tests for linkage of multiple cohorts in an accelerated longitudinal design. Psychol. Methods 5, 44–63 (2000). [DOI] [PubMed] [Google Scholar]
- 104.Raudenbush S. W., Bryk A. S., Hierarchical Linear Models: Applications and Data Analysis Methods (Sage, 2002), vol. 1. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All study data are included in the article and/or SI Appendix.