This cohort study examines change in adolescents’ use of e-cigarettes, cannabis, and alcohol and in physical activity behaviors following the stay-at-home COVID-19 order in California.
Key Points
Question
How have adolescents’ substance use and physical activity behaviors changed under stay-at-home orders related to the COVID-19 pandemic?
Findings
In this cohort study of adolescents in Northern California, the overall prevalence of e-cigarette, cannabis, or alcohol use did not meaningfully change with a statewide stay-at-home order, but physical activity declined considerably.
Meaning
While youth substance use prevention and cessation support should continue, enhanced efforts to increase physical activity are needed.
Abstract
Importance
Stay-at-home policies related to the COVID-19 pandemic could disrupt adolescents’ substance use and physical activity.
Objective
To compare adolescents’ substance use and physical activity behaviors before and after stay-at-home restrictions.
Design, Setting, and Participants
Ongoing prospective cohort study of tobacco use behaviors among ninth- and tenth-grade students enrolled at 8 public high schools in Northern California from March 2019 to February 2020 and followed up from September 2019 to September 2020. Race/ethnicity was self-classified from investigator-provided categories and collected owing to racial/ethnic differences in tobacco and substance use.
Exposures
In California, a COVID-19 statewide stay-at-home order was imposed March 19, 2020. In this study, 521 six-month follow-up responses were completed before the order and 485 were completed after the order.
Main Outcomes and Measures
The prevalence of substance use (ie, past 30-day use of e-cigarettes, other tobacco, cannabis, and alcohol) and physical activity (active ≥5 days/week) was compared at baseline and follow-up. A difference-in-difference approach was used to assess whether changes from baseline to 6-month follow-up varied if follow-up occurred after the stay-at-home order, adjusting for baseline behaviors and characteristics. All models were weighted for losses to follow-up using the inverse probability method. Weights were derived from a logistic regression model for having a follow-up response (dependent variable), as predicted by baseline characteristics and behaviors.
Results
Of 1423 adolescents enrolled at baseline, 1006 completed 6-month follow-up (623 [62%] were female, and 492 [49%] were non-Hispanic White). e-Cigarette use declined from baseline to 6-month follow-up completed before the stay-at-home order (17.3% [89 of 515] to 11.3% [58 of 515]; McNemar χ2 = 13.54; exact P < .001) and 6-month follow-up completed after the stay-at-home order (19.9% [96 of 482] to 10.8% [52 of 482]; McNemar χ2 = 26.16; exact P < .001), but the extent of decline did not differ statistically between groups responding before vs after the stay-at-home order (difference-in-difference adjusted odds ratio, 0.84; 95% CI, 0.47-1.52; P = .58). In contrast, being physically active was unchanged from baseline if follow-up was before the order (53.7% [279 of 520] to 52.9% [275 of 520]; McNemar χ2 = 0.09; exact P = .82) but declined sharply from baseline if follow-up was after the order (54.0% [261 of 483] to 38.1% [184 of 483]; McNemar χ2 = 30.72; exact P < .001), indicating a pronounced difference in change from baseline after the stay-at-home order (difference-in-difference adjusted odds ratio, 0.49; 95% CI, 0.35-0.69; P < .001). Overall in the cohort, reported use of other tobacco, cannabis, and alcohol did not differ meaningfully before and after the order.
Conclusions and Relevance
In this cohort, a reduction in e-cigarette use occurred independently of COVID-19 stay-at-home restrictions, but persistent cannabis and alcohol use suggest continued need for youth substance use prevention and cessation support. Declining physical activity during the pandemic is a health concern.
Introduction
The effects of the COVID-19 pandemic have been dramatic and wide-reaching, affecting many more than those who become ill, including reports of increased substance use among adults.1 The pandemic and its associated school closures and restrictions on public gatherings could also disrupt adolescents’ engagement in various risk-taking and health-promoting behaviors, such as substance use and physical activity. Potential mechanisms include diminished peer interaction, greater proximity to parents, less participation in school-supported extracurricular activities, decreased availability of gathering spaces, less access to tobacco retailers, reduced exposure to substance use prevention programs, and heightened stress, anxiety, and boredom.
The extent to which adolescents’ health-related behaviors have changed during the pandemic carries implication for their short-term and long-term well-being. Declines in tobacco, alcohol, and cannabis use could serve as opportunities to accelerate prevention and cessation goals, whereas use increases would signal need for additional resources and support. More sedentary lifestyles under reduced access to recreational spaces and organized sports may deny youth physical and social benefits of exercise.2
At least 2 recent cross-sectional studies asked youth to compare their current (during the COVID-19 pandemic) substance use behaviors with their recalled behaviors prior to the pandemic. In an online survey of high school students in Ontario, Canada, use of e-cigarettes, cannabis, and binge drinking were all reported as less prevalent during the pandemic, although the prevalence of any alcohol use did not differ.3 In a national online survey of US adolescents and young adults, approximately two-thirds of those who had ever used e-cigarettes reported changing how much they use since the start the pandemic, with the majority of those who changed reporting quitting (36%) or reducing use (31%).4 Rather than rely on recalled behaviors, the present investigation provides individually linked prospective data collected before and after the implementation of a statewide stay-at-home order in California.
Data are from an ongoing cohort of 1423 public high school students recruited from Northern California from March 2019 through February 2020, with follow-up as of September 2020. On March 19, 2020, California Governor Gavin Newsom ordered that all public schools immediately transition to remote education as part of a statewide stay-at-home order to slow COVID-19 spread.5 Here, we test the null hypotheses of no change in adolescents’ use of e-cigarettes, cannabis, or alcohol or in physical activity behaviors following the stay-at-home order.
Methods
This prospective analysis includes data from a cohort of students (N = 1423) attending 8 public high schools in Northern California. Cohort enrollment was staggered over time (Figure). Approximately half the sample completed the baseline survey from March through May 2019 (spring 2019 cohort); the remainder completed baseline from August 2019 through February 2020 (fall 2019 cohort). The spring 2019 cohort completed the 6-month follow-up survey prior to the California stay-at-home order, whereas the fall 2019 cohort primarily completed 6-month follow-up after the order (Figure). Superimposition of the stay-at-home order over the existing cohort design created an unanticipated opportunity to examine behavioral changes over time as a function of whether follow-up responses were made before or after the statewide stay-at-home order. An institutional review board at the University of California San Francisco reviewed and approved all study procedures.
Figure. Participant Recruitment and Retention.
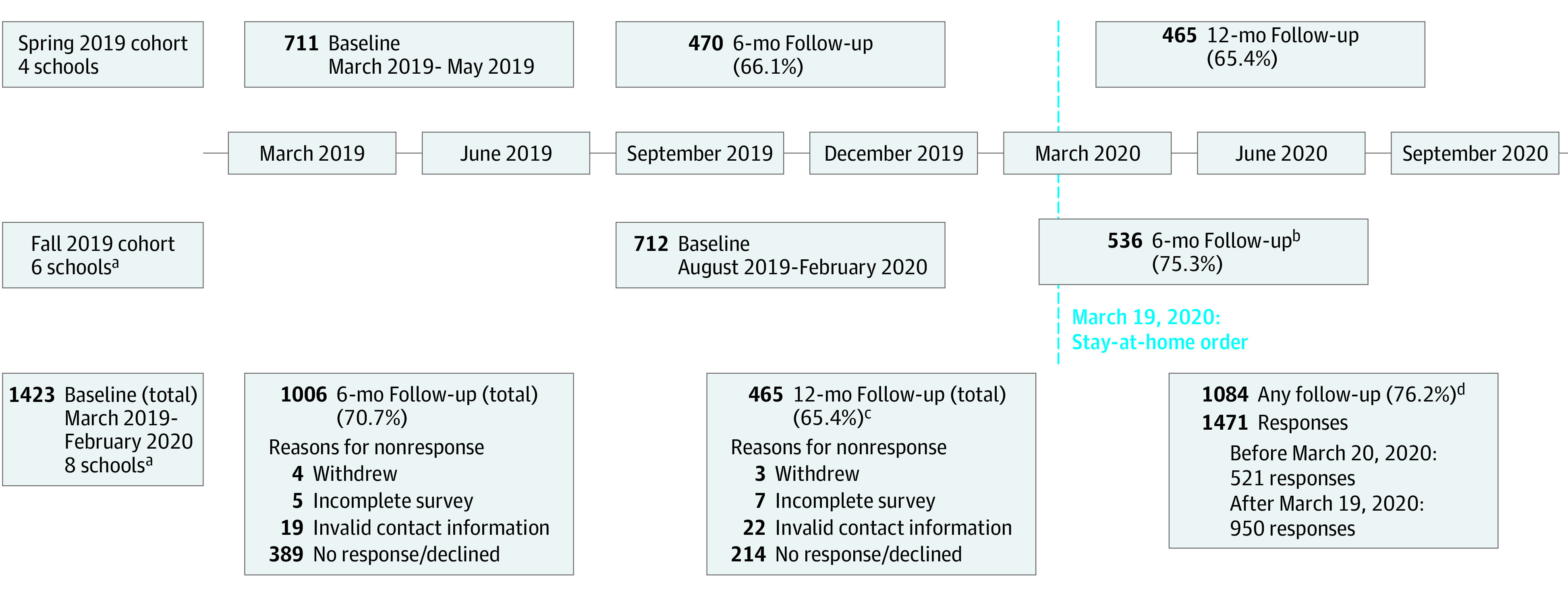
Baseline surveys (N = 1423) were completed from March 2019 through February 2020. Six- and 12-month follow-up surveys were administered electronically at the respective intervals from baseline. As of September 2020, all participants had been eligible for 6-month follow-up, and approximately half of the sample was eligible for 12-month follow-up.
aTwo schools enrolled in spring 2019 were revisited in fall 2019 to enroll new samples of ninth-grade students.
bOf these 536 follow-up responses, 51 were collected prior to March 20, 2020, and 485 were collected after the stay-at-home order. For this analysis, the 51 pre–stay-at-home responses were included with the spring 2019 cohort.
cThis retention percentage calculated among the 711 participants enrolled in spring 2019; the remaining 712 students enrolled in fall 2019 were not yet eligible for 12-month follow-up.
dThis retention percentage refers to participants in the entire cohort who completed at least one 6- or 12-month follow-up survey through September 2020. Some participants completed both a 6- and 12-month follow-up survey.
Participants
As described elsewhere,6 we recruited schools located in municipalities with fewer than 50 000 residents and counties below 1000 persons per square mile.7 We focused on smaller communities where youth tobacco use historically is higher but representation in tobacco-related research has been low. All students in grades 9 or 10 at enrolled schools were eligible to participate. At each school, study staff visited to explain study objectives and distribute parental consent and student assent forms. Study staff returned 1 to 2 weeks later to assign individual identifiers and administer electronic baseline surveys. Participating students received a $10 gift card to an online retailer for each survey wave completed. Participating schools received $300.
Six-month follow-up surveys were administered remotely at their respective intervals from baseline via personalized survey links sent either by text message or email. By September 2020, all participants had been eligible for 6-month follow-up, and the spring 2019 cohort had been eligible for 12-month follow-up. In total, 1084 participants (76%) completed 1 or more follow-up survey. Five hundred twenty-one follow-up responses were collected prior to the California stay-at-home order, and 950 were collected after the order (Figure). No respondent had more than 1 response collected after the stay-at-home order.
Measurement
Substance Use and Physical Activity
The main outcomes of interest were substance use and physical activity behaviors. In all survey waves, participants were asked to indicate having ever used (yes/no) and number of days used (0-30) in the past 30 days for alcohol, cigarettes, cigars, e-cigarettes, hookah, cannabis, and conventional smokeless tobacco using items with product images and descriptions, including separate items for product subtypes (eg, pod or mod e-cigarettes, moist snuff or snus smokeless tobacco). Given low use prevalence, for this analysis, all tobacco products except e-cigarettes (ie, cigarettes, cigars, hookah, and smokeless tobacco) were combined as other tobacco. Physical activity was assessed by asking participants how many days (0-7) in the past 7 days “did you exercise or were physically active for at least 20 minutes that made you sweat or breathe hard?”8 To reduce information bias, all tobacco use items included photographs and product descriptions, and participants were reminded that responses were confidential.
Demographic, Socioeconomic, and Psychological Measures
Collected at baseline was sex, race/ethnicity, grade in school (ie, ninth or tenth), and self-reported scholastic performance (ie, mostly A’s, B’s, C’s, or below). Race/ethnicity was self-classified from investigator-provided categories and collected owing to racial/ethnic differences in tobacco and substance use.9 Measures of baseline socioeconomic position included participation in the federal school lunch program and 2 family affluence items (computer ownership and vacations taken in the past year).10 A screening instrument for symptoms of depression11 and a combined scale of sensation seeking and impulsivity12 (standardized to mean [SD] of 0 [1]) were also included as plausible confounding variables.
Tobacco Product Access
Shortly after the stay-at-home order, a new item was added to follow-up surveys asking, “How have social-distancing rules, school closures, and other developments related to COVID-19 and the novel corona virus affected your access to tobacco or nicotine products?” with response options of much more difficult, somewhat more difficult, no difference, somewhat easier, much easier to obtain tobacco now, or I don’t know.
Statistical Analysis
Participants’ baseline characteristics were summarized and compared between the spring 2019 and fall 2019 cohorts by χ2 test or 2-sample independent t test, as appropriate. In the main analysis, outcomes of interest were the prevalence of past 30-day use of e-cigarettes, other tobacco, cannabis, and alcohol and physical activity (5-7 days active in the past week) in the spring 2019 and fall 2019 cohorts at baseline 6-month follow-up and separately for the spring 2019 cohort at 12-month follow-up. To assess behavior changes within groups (ie, within the spring 2019 and fall 2019 cohorts) and to test whether changes in outcome prevalence from baseline to 6-month follow-up differed by cohort (ie, 6-month follow-up before or after the stay-at-home order), we used a difference-in-difference approach.13 Here, we fitted separate repeated measures logistic regression models for each behavioral outcome (eg, e-cigarette use), in which the main independent variables were cohort (spring 2019 or fall 2019) and survey wave (baseline or 6-month follow-up). A cohort-by-survey wave interaction term tested whether changes from baseline to 6-month follow-up differed by spring and fall cohorts. A statistically significant interaction would indicate different behavior trajectories after the stay-at-home order under certain assumptions, such as exchangeability of the cohorts (ie, no confounding) and that trends observed before the order would have continued in its absence.14 Separately, 12-month outcomes for the spring 2019 cohort were modeled to evaluate additional within-group changes. Models were estimated with generalized estimating equations (exchangeable correlation structure and robust variance) and adjusted for school and baseline covariables (Table 1), with missing covariable values (1% of values) multiply imputed by chained equations using the mi: command suite in Stata version 16 (StataCorp). All models were weighted for losses to follow-up using the inverse probability method. Weights were derived from a logistic regression model for having a follow-up response (dependent variable), as predicted by baseline characteristics and behaviors.
Table 1. Participant Characteristics by Enrollment Cohort: Adolescents in Northern California, US (2019-2020).
| Baseline characteristic | No. (%) | P valued | |
|---|---|---|---|
| Spring 2019 cohort (n = 521)a,b | Fall 2019 cohort (n = 485)b,c | ||
| Grade in school | |||
| Ninth | 247 (48.4) | 328 (68.6) | <.001 |
| Tenth | 263 (51.6) | 150 (31.4) | |
| Sex | |||
| Female | 311 (59.7) | 312 (64.3) | .10 |
| Male | 206 (39.5) | 165 (34.0) | |
| Other | 4 (0.8) | 8 (1.6) | |
| Race/ethnicity | |||
| Hispanic/Latinx | 185 (34.6) | 173 (35.7) | .98 |
| Non-Hispanic White | 256 (49.9) | 236 (48.7) | |
| Othere | 80 (15.5) | 76 (15.7) | |
| Computers at home, No. | |||
| 0 | 46 (9.0) | 58 (12.1) | .04 |
| 1 | 136 (26.7) | 113 (23.6) | |
| 2 | 112 (22.0) | 133 (27.8) | |
| >2 | 215 (42.24) | 175 (36.5) | |
| Family vacations in past year, No. | |||
| 0 | 107 (21.1) | 92 (19.1) | .09 |
| 1 | 115 (22.7) | 142 (29.5) | |
| 2 | 111 (21.9) | 105 (21.8) | |
| >2 | 174 (34.3) | 143 (29.7) | |
| School lunch program | |||
| Free or reduced | 253 (51.7) | 312 (64.3) | <.001 |
| Full price | 183 (37.4) | 86 (17.7) | |
| Do not know | 53 (10.8) | 87 (17.9) | |
| Scholastic performance | |||
| Mostly A’s | 210 (40.4) | 227 (46.9) | .21 |
| Mostly B’s | 202 (38.8) | 166 (34.3) | |
| Mostly C’s or below | 83 (16.0) | 72 (14.9) | |
| Do not know | 25 (4.8) | 19 (3.9) | |
| Depression symptoms | |||
| Positive screen | 167 (32.2) | 153 (31.8) | .90 |
| Negative screen | 352 (67.8) | 328 (68.2) | |
| e-Cigarette use in past 30 d | |||
| Never | 327 (62.8) | 301 (62.1) | .79 |
| Ever (0 d) | 101 (19.4) | 87 (17.9) | |
| 1-5 d | 55 (10.6) | 55 (11.3) | |
| 6-30 d | 38 (7.3) | 42 (8.7) | |
| Other tobacco use in past 30 dd | |||
| 0 d | 487 (93.5) | 467 (96.3) | .04 |
| 1-30 d | 34 (6.5) | 18 (3.7) | |
| Cannabis use in past 30 d | |||
| Never | 351 (67.4) | 303 (62.5) | .20 |
| Ever (0 d) | 77 (14.8) | 87 (17.9) | |
| 1-5 d | 53 (10.2) | 63 (13.0) | |
| 6-30 d | 40 (7.7) | 32 (6.6) | |
| Alcohol use in past 30 d | |||
| 0 d | 428 (82.1) | 386 (79.8) | .33 |
| 1-30 d | 93 (17.9) | 98 (20.2) | |
| Physically active in past week | |||
| 0-1 d | 51 (9.8) | 42 (8.7) | .83 |
| 2-4 d | 190 (36.5) | 180 (37.3) | |
| 5-7 d | 279 (53.7) | 261 (54.0) | |
| Sensation-seeking score, standardized mean (SD) | −0.05 (0.98) | −0.07 (1.01) | .75 |
| Has a follow-up responsef | |||
| Before March 20, 2020 | 521 (100) | 0 (0) | NA |
| After March 19, 2020 | 387 (74.3) | 485 (100) | NA |
Abbreviation: NA, not applicable.
Includes participants from schools recruited March 2019 to May 2019 and whose 6-month follow-up was completed before the March 19, 2020, California stay-at-home order. This also includes 51 participants recruited in August 2019 and whose 6-month follow-up responses were collected from February 27, 2020, to March 7, 2020.
This Table includes only individuals with a 6-month follow-up observation. For a comparison of the full baseline sample to the follow-up analytic sample, including 12-month follow-up, see eTable 1 in the Supplement. Number of participants may be smaller for some variables owing to missing data.
Includes participants from schools recruited August 2019 to February 2020 and whose 6-month follow-up was completed after the March 19, 2020, California stay-at-home order.
χ2 Test to compare the spring and fall cohorts; exception: sensation-seeking score tested with t test.
Other race/ethnicity included American Indian or Alaska Native, Asian, Black, Native Hawaiian or Pacific Islander, more than 1 race, prefer not to respond, and missing data.
Follow-up completed after March 19, 2020, in the spring 2019 cohort refers to 12-month follow-up.
To examine post–stay-at-home behavior in the total study, we additionally combined 6-month follow-up responses from the fall 2019 cohort with 12-month follow-up responses from the spring 2019 cohort (ie, all post–stay-at-home responses) and compared with matched behaviors from the most recent pre–stay-at-home response using the Wilcoxon signed-rank test. All substance use items asked about behaviors in the past 30 days; therefore, responses collected within 30 days of the stay-at-home order could conceivably reflect behaviors that preceded the order. For this reason, we repeated analyses considering only individuals whose follow-up occurred 30 days or more after the stay-at-home order (ie, after April 18, 2020).
In supplemental analyses (eTable 2 in the Supplement), we modeled all follow-up behaviors with the main independent variable being whether data were collected after the stay-at-home order, controlling for baseline behaviors and characteristics. We also examined initiation and stopping of behaviors between baseline and follow-up.
Results
The spring 2019 and fall 2019 participants who completed 6-month follow-up were similar in their aggregate characteristics and behaviors, with some exceptions (Table 1). Fall 2019 participants were statistically significantly more likely to be in ninth grade and report participation in federal school lunch programs (Table 1). Likewise, follow-up participants were largely similar to the enrolled cohort (eTable 1 in the Supplement).
Ease of accessing tobacco and nicotine products was asked of participants contacted after the stay-at-home order, including tobacco users and nonusers. Overall, 82% participants (738 of 899) responded, “I don’t know,” and 92% (676 of 738) of these participants were past 30-day tobacco nonusers. Among responses other than “I don’t know,” endorsing much (25% [41 of 161]) or somewhat (21% [34 of 161]) more difficult to access tobacco was together slightly more common than no difference (43% [69 of 161]) and much more common than somewhat (4% [6 of 161]) or much (7% [11 of 161]) easier.
Past 30-day use of e-cigarettes decreased meaningfully prior to the stay-at-home order, from 17% (89 of 515) at baseline to 11% (58 of 515) at 6-month follow-up in the spring 2019 cohort and also declined (from 20% [96 of 482] before to 11% [52 of 482]) in the fall 2019 cohort (Table 2). Difference-in-difference analysis suggested no meaningful difference in e-cigarette use trajectory between the spring and fall cohorts (Table 2). Similarly, difference-in-difference analyses did not identify statistically significant cohort difference in the trajectories of use of other tobacco products, cannabis, or alcohol (Table 2). While cannabis use prevalence declined at 6-month follow-up in the fall 2019 cohort, cannabis use was not different at 12-month follow-up (ie, after the stay-at-home order) in the spring 2019 cohort (Table 2).
Table 2. Behaviors at Baseline and Follow-up: Spring 2019 and Fall 2019 Cohorts.
| Cohort | Observed behaviors, No./total No. (%) | Within-group difference, 6 mo vs baseline, adjusted OR (95% CI)b | P value, between-group difference-in-difference (6 mo)c | Within-group difference, 12 mo vs baseline, adjusted OR (95% CI)b,d | ||
|---|---|---|---|---|---|---|
| Baselinea | Follow-up | |||||
| 6 mo | 12 mo | |||||
| Spring 2019e,f | ||||||
| e-Cigarettesg | 89/515 (17.3) | 58/515 (11.3) | 50/464 (10.8) | 0.38 (0.25-0.58) | .58 | 0.38 (0.24-0.60) |
| Other tobaccog,h | 34/521 (6.5) | 20/521 (3.8) | 19/465 (4.1) | 0.49 (0.26-0.90) | .81 | 0.67 (0.32-1.42) |
| Cannabisg | 91/518 (17.6) | 83/518 (16.0) | 85/464 (18.3) | 0.73 (0.50-1.05) | .31 | 0.90 (0.62-1.30) |
| Alcoholg | 89/513 (17.3) | 94/513 (18.3) | 85/462 (18.4) | 0.91 (0.65-1.28) | .93 | 0.85 (0.59-1.23) |
| Physical activityi | 279/520 (53.7) | 275/520 (52.9) | 184/462 (39.8) | 0.94 (0.75-1.19) | <.001 | 0.55 (0.42-0.71) |
| Fall 2019j,k | ||||||
| e-Cigarettesg | 96/482 (19.9) | 52/482 (10.8) | NA | 0.32 (0.24-0.60) | NA | NA |
| Other tobaccog,h | 18/485 (3.7) | 11/485 (2.3) | NA | 0.55 (0.26-1.18) | NA | NA |
| Cannabisg | 95/485 (19.6) | 71/485 (14.6) | NA | 0.56 (0.39-0.79) | NA | NA |
| Alcoholg | 94/477 (19.7) | 91/477 (19.1) | NA | 0.90 (0.63-1.28) | NA | NA |
| Physical activityi | 261/483 (54.0) | 184/483 (38.1) | NA | 0.46 (0.36-0.60) | NA | NA |
Abbreviations: NA, not applicable; OR, odds ratio.
Baseline values restricted to those with 6-month follow-up (n = 521 in spring 2019 cohort and n = 485 in fall 2019 cohort). Number of participants may be smaller for some behaviors owing to missing outcome data.
Adjusted model covariables (all measured at baseline): sex, race/ethnicity, year in school, home computer ownership, family vacations, school lunch program participation, academic performance, depression screen, sensation seeking, school, and other behaviors (ie, use of e-cigarettes, cannabis, alcohol, and other tobacco and physical activity, excluding the outcome behavior). Missing covariable values multiply imputed.
Difference-in-difference comparisons test whether within-group differences in behaviors from baseline to 6-month follow-up differ by cohort. P value is from cohort × survey wave interaction term, estimated using generalized estimating equation logistic regression models weighted for losses to follow-up and including within-participant correlation (exchangeable) and robust variance estimation.
Twelve-month and 6-month outcomes modeled separately.
Participants from schools recruited March 2019 to May 2019 whose 6-month follow-up was completed before the March 19, 2020, California stay-at-home order.
From the fall 2019 cohort schools, 51 six-month follow-up responses were collected prior to the March 19, 2020, California stay-at-home order (collected from February 27, 2020, to March 7, 2020). For this analysis, those responses are included with the spring 2019 cohort.
Use ≥1 day in the past 30 days.
Any tobacco product (ie, cigarettes, cigars, hookah, or smokeless tobacco), e-cigarettes excluded.
Physical activity ≥5 days in the past week.
Participants from schools recruited August 2019 to February 2020 whose 6-month follow-up was completed after the March 19, 2020, California stay-at-home order.
The fall 2019 cohort was not yet eligible for 12-month follow-up as of September 2020.
Decreasing physical activity was the most evident behavior change associated with the stay-at-home order. The prevalence of being physically active 5 or more days per week was nearly identical at baseline in both cohorts (spring 2019 cohort: 54% [279 of 520]; fall 2019 cohort: 54% [261 of 483]) and in 6-month follow-up responses collected prior to the stay-at-home order (Table 2). However, adolescents were less likely to report being physically active after the stay-at-home order (38% [184 of 483] in the fall 2019 cohort), with difference-in-difference estimates indicating half the odds of being physically active at 6-month follow-up in the fall 2019 cohort than had the same trajectory as the spring 2019 cohort applied (Table 2).
Considering all follow-up responses collected after the stay-at-home order, the prevalence of other tobacco, cannabis, and alcohol use after the order was not statistically significantly different from values reported in the most recent surveys before the stay-at-home order, but e-cigarette use and physical activity were lower (Table 3). Patterns were highly similar in follow-up responses collected after April 18, 2020 (Table 3).
Table 3. Behaviors Before and After Stay-at-Home Order, Combined Cohort.
| Variable | Behavior at follow-up vs most recent previous survey, No./total No. (%)a | |||||
|---|---|---|---|---|---|---|
| Follow-up after March 19, 2020 (n = 950)b | Follow-up after April 18, 2020 (n = 643)b,c | |||||
| Previous | Follow-up | P valued | Previous | Follow-up | P valued | |
| e-Cigarettese | 152/944 (16.1) | 101/944 (10.7) | <.001 | 114/638 (17.9) | 65/638 (10.2) | <.001 |
| Other tobaccoe,f | 33/950 (3.5) | 30/950 (3.2) | .75 | 22/643 (3.4) | 20/643 (3.1) | .85 |
| Cannabise | 170/949 (17.9) | 156/949 (16.4) | .24 | 121/642 (18.8) | 105/642 (16.4) | .10 |
| Alcohole | 184/936 (19.7) | 175/936 (18.7) | .57 | 129/632 (20.4) | 122/632 (19.3) | .60 |
| Physical activityg | 507/948 (53.5) | 370/948 (39.0) | <.001 | 333/641 (52.0) | 252/641 (39.3) | <.001 |
The combined cohort includes all follow-up responses (6-month or 12-month follow-up survey) that were collected after the date of interest. The previous response of interest was either the baseline or 6-month follow-up survey, whichever was most recent and preceded the stay-at-home order.
Number of participants may be smaller for some behaviors owing to missing data.
As a robustness check, excludes responses collected within 30 days of the California stay-at-home order because product use questionnaire items asked about use in the past 30 days.
Wilcoxon signed rank test for paired responses (exact).
Use ≥1 day in the past 30 days.
Any tobacco product (ie, cigarettes, cigars, hookah, or smokeless tobacco), e-cigarettes excluded.
Physical activity ≥5 days in the past week.
In supplemental analyses of all 6-month and 12-month follow-up observations, adjusted models suggested no meaningful or statistically significant difference in use of e-cigarettes, other tobacco, cannabis, or alcohol in follow-up before or after the stay-at-home order (eTable 2 in the Supplement). However, achieving 5 or more days of physical activity per week was less common after the stay-at-home order (odds ratio, 0.57; 95% CI, 0.45-0.73; eTable 2 in the Supplement). Of participants reporting being physically active before the stay-at-home order, 52% (135 of 261) no longer reached 5 or more active days per week after the order (eTable 3 in the Supplement).
Discussion
In this prospective cohort of adolescents in Northern California, the overall reported use of tobacco, cannabis, and alcohol use did not change substantially following the implementation of school closures and other social distancing measures associated with the COVID-19 pandemic. Unlike substance use, achieving at least 5 days of vigorous physical activity a week was notably less common following the California stay-at-home order. These findings suggest a need for parents and schools to continue substance use prevention efforts and to dedicate additional attention to physical activity promotion.
Enhancing physical activity during a pandemic may require novel and creative strategies, especially given suspended interscholastic sports seasons, potentially restricted access to exercise venues, such as gyms, recreation centers, parks and trails, and restrictions on nonessential travel to exercise spaces. Physical activity is an important element of adolescent health, promoting cardiovascular fitness and muscle strength, reducing body fat accumulation, and potentially offering cognitive and social benefits.2,15 The COVID-19 pandemic potentially adds further barriers for children already facing challenges to being physically active, especially among those who are socioeconomically disadvantaged.16 Recently, some parents have encouraged socially distanced group fitness activities to keep children moving.17 Whether pandemic-related declines in physical activity prove long-lasting or reverse after school athletic programs resume may dictate long-term health implications.
In an unexpected finding, the prevalence of e-cigarette use declined from baseline both in groups that were followed up prior to and after the stay-at-home order. One plausible explanation for reduced e-cigarette use before the pandemic could be growing e-cigarette safety fears among adolescents following the outbreak of e-cigarette or vaping product use–associated lung injury (EVALI) beginning in late summer 2019.18 Soon after the EVALI outbreak, perceptions of the harmfulness of e-cigarettes were found to increase among adults in the US19 and UK.20 Media reports often emphasized the young age of many patients with EVALI, as did public communication in California,21 information likely of particular salience for adolescents. The decline in e-cigarette use in our cohort aligns with National Youth Tobacco Survey results showing a drop in past 30-day e-cigarette use among US high school students from 27.5% in 2019 to 19.6% in 2020.22 National Youth Tobacco Survey data were collected from January to March 2020 but truncated owing to pandemic-related school closures.22 A pending question is whether declines in e-cigarette use will persist after media attention to EVALI fades.
The findings of the present study partly align with previously reported cross-sectional results in which youth or young adults surveyed during the COVID-19 pandemic reported less substance use than they recalled using prior to the pandemic.3,4 We found less e-cigarette use (but not other substance use) compared with baseline but no association with the onset of pandemic-related restrictions. The availability of prospective data may be a reason for divergent results. It is possible that, as in the present cohort, young people may have reduced their e-cigarette use before the pandemic, and their recalled behaviors did not fully capture the temporal sequence of events. Age and geographic differences between study populations should also be considered.
Engagement in at least some level of social distancing has been reported as very high among US youth in the weeks following the California stay-at-home order (and other similar state and city measures).23,24 We found that some adolescents reported diminished access to tobacco products, plausibly owing to less contact with peers, retail store closures, or other reasons. Despite possible challenges in accessing tobacco products, overall use prevalence of tobacco, cannabis, and alcohol did not decline, suggesting continued access, possibly via alternative access channels,4 such as online purchases or from parents or other adults. While persistent use levels are concerning, substance use did not appear to increase in our cohort, unlike as reported for adults.1 It should be noted that while the overall prevalence of substance use behaviors were similar before and after the stay-at-home order, individuals’ behaviors were not necessarily constant. For each behavior, use initiation was balanced by other adolescents who ceased use. Further investigation is needed to understand individual behavioral motivations.
Strengths and Limitations
A key strength of the present investigation is the ability to test changes over time using prospective data with good cohort retention (76%), especially under pandemic conditions that precluded in-school follow-up visits. Attrition merits consideration as a limitation, although matched-pairs analysis and model weighting for losses to follow-up help address this concern. It is possible that shifting from in-school data collection at baseline to remote survey administration at follow-up impaired baseline to follow-up comparisons, for instance, if youth were more likely to exaggerate their substance use behavior in the presence of peers but downplay their use when taking a survey at home. However, we did not see systematic changes in physical activity or in cannabis or alcohol use between baseline and pre–stay-at-home follow-up surveys, despite moving to online methods. An unanticipated strength was follow-up falling partly before and after a disruptive event.
Results drawn from this regional population may not generalize to adolescents nationally or in other geographic contexts. Rural counties in Northern California were not isolated from the COVID-19 pandemic, with 36% of California Health Interview Survey participants in this region reporting they had lost a job or experienced reduced worked hours or income owing to the pandemic.25 Baseline tobacco use prevalence was lower in this cohort of ninth- and tenth-grade students than reported for all high school students nationally26 but higher than recent statewide estimates for California,27 as expected for these rural communities. Notably, post–stay-at-home follow-up took place over a 6-month period from March to September 2020. While the onset of the COVID-19 pandemic was the most notable and drastic disruption to the cohort, not captured in this analysis would be any subtler secular trends, potentially as social-distancing measures (and willingness to adhere to them) relaxed in the months after the initial stay-at-home order.
Conclusions
In conclusion, the current findings underscore the need to continue strong tobacco and cannabis control efforts during the COVID-19 pandemic, restricting youth access and supporting prevention and cessation. A marked decline in physical activity suggests a need for alternative strategies to promote physical fitness in this more challenging context.
eTable 1. Participant Characteristics, Full and Follow-up Samples: Adolescents in Northern California, USA (2019-2020)
eTable 2. Behaviors at Follow-up: Associations with Stay-at-Home Order
eTable 3. Changes in Behaviors: Spring 2019 and Fall 2019 Cohorts
References
- 1.Czeisler MÉ, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049-1057. doi: 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landry BW, Driscoll SW. Physical activity in children and adolescents. PM R. 2012;4(11):826-832. doi: 10.1016/j.pmrj.2012.09.585 [DOI] [PubMed] [Google Scholar]
- 3.Dumas TM, Ellis W, Litt DM. What does adolescent substance use look like during the COVID-19 pandemic? examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health. 2020;67(3):354-361. doi: 10.1016/j.jadohealth.2020.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaiha SM, Lempert LK, Halpern-Felsher B. Underage youth and young adult e-cigarette use and access before and during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(12):e2027572. doi: 10.1001/jamanetworkopen.2020.27572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Office of Governor Gavin Newsom . Governor Gavin Newsom issues stay at home order. Press release. Published March 19, 2020. Accessed October 12, 2020. https://www.gov.ca.gov/2020/03/19/governor-gavin-newsom-issues-stay-at-home-order/
- 6.Chaffee BW, Couch ET, Urata J, Cash D, Werts M, Halpern-Felsher B. Electronic cigarette and moist snuff product characteristics independently associated with youth tobacco product perceptions. Tob Induc Dis. 2020;18:71. doi: 10.18332/tid/125513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hewitt M. Defining “rural” areas: impact on health care policy and research. Health Program, Office of Technology Assessment, Congress of the United States; 1989. [Google Scholar]
- 8.US Centers for Disease Control and Prevention . National Health and Nutrition Examination Survey: NHANES 2011-2012. Accessed March 26, 2021. https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2011
- 9.Keyes KM, Vo T, Wall MM, et al. Racial/ethnic differences in use of alcohol, tobacco, and marijuana: is there a cross-over from adolescence to adulthood? Soc Sci Med. 2015;124:132-141. doi: 10.1016/j.socscimed.2014.11.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chzhen Y, Moor I, Pickett W, Toczydlowska E, Stevens G. Family Affluence and Inequality in Adolescent Health and Life Satisfaction: Evidence From the HBSC Study 2002-2014. UNICEF Office of Research-Innocenti. Published April 2016. https://www.unicef-irc.org/publications/pdf/IWP_2016_10.pdf [Google Scholar]
- 11.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959-976. doi: 10.1017/S0033291702006074 [DOI] [PubMed] [Google Scholar]
- 12.Stephenson MT, Hoyle RH, Palmgreen P, Slater MD. Brief measures of sensation seeking for screening and large-scale surveys. Drug Alcohol Depend. 2003;72(3):279-286. doi: 10.1016/j.drugalcdep.2003.08.003 [DOI] [PubMed] [Google Scholar]
- 13.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312(22):2401-2402. doi: 10.1001/jama.2014.16153 [DOI] [PubMed] [Google Scholar]
- 14.French B, Stuart EA. Study designs and statistical methods for studies of child and adolescent health policies. JAMA Pediatr. 2020;174(10):925-927. doi: 10.1001/jamapediatrics.2020.3408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. 2011;45(11):886-895. doi: 10.1136/bjsports-2011-090185 [DOI] [PubMed] [Google Scholar]
- 16.Armstrong S, Wong CA, Perrin E, Page S, Sibley L, Skinner A. Association of physical activity with income, race/ethnicity, and sex among adolescents and young adults in the United States: findings from the National Health and Nutrition Examination Survey, 2007-2016. JAMA Pediatr. 2018;172(8):732-740. doi: 10.1001/jamapediatrics.2018.1273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levin R. Shut down your computers, kids, and lace up. New York Times. Published November 28, 2020. Accessed December 1, 2020. https://www.nytimes.com/2020/11/28/at-home/exercise-for-kids.html
- 18.Perrine CG, Pickens CM, Boehmer TK, et al. ; Lung Injury Response Epidemiology/Surveillance Group . Characteristics of a multistate outbreak of lung injury associated with e-cigarette use, or vaping: United States, 2019. MMWR Morb Mortal Wkly Rep. 2019;68(39):860-864. doi: 10.15585/mmwr.mm6839e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dave D, Dench D, Kenkel D, Mathios A, Wang H. News that takes your breath away: risk perceptions during an outbreak of vaping-related lung injuries. J Risk Uncertain. 2020;60(3):281-307. doi: 10.1007/s11166-020-09329-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tattan-Birch H, Brown J, Shahab L, Jackson SE. Association of the US outbreak of vaping-associated lung injury with perceived harm of e-cigarettes compared with cigarettes. JAMA Netw Open. 2020;3(6):e206981. doi: 10.1001/jamanetworkopen.2020.6981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.California Department of Public Health . New public education campaign targets deadly outbreak of vaping-related illness. Press release. Published October 24, 2019. Accessed October 12, 2020. https://www.cdph.ca.gov/Programs/OPA/Pages/NR19-028.aspx
- 22.Wang TW, Neff LJ, Park-Lee E, Ren C, Cullen KA, King BA. E-cigarette use among middle and high school students: United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(37):1310-1312. doi: 10.15585/mmwr.mm6937e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oosterhoff B, Palmer CA, Wilson J, Shook N. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J Adolesc Health. 2020;67(2):179-185. doi: 10.1016/j.jadohealth.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gaiha SM, Cheng J, Halpern-Felsher B. Association between youth smoking, electronic cigarette use, and COVID-19. J Adolesc Health. 2020;67(4):519-523. doi: 10.1016/j.jadohealth.2020.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.UCLA Center for Health Policy Research . 2020 California health interview survey preliminary COVID-19 estimates provided by the UCLA Center for Health Policy Research. Published May 2020. Accessed September 29, 2020. https://healthpolicy.ucla.edu/health-profiles/Pages/COVID-19-Preliminary-Estimates.aspx
- 26.Gentzke AS, Creamer M, Cullen KA, et al. Vital Signs: Tobacco product use among middle and high school students: United States, 2011-2018. MMWR Morb Mortal Wkly Rep. 2019;68(6):157-164. doi: 10.15585/mmwr.mm6806e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu S-H, Zhuang Y-L, Braden K, et al. Results of the statewide 2017-18 California Student Tobacco Survey. Accessed October 12, 2020. https://www.cdph.ca.gov/Programs/CCDPHP/DCDIC/CTCB/CDPH%20Document%20Library/ResearchandEvaluation/Reports/2017-18CaliforniaStudentTobaccoSurveyBiennialReport.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Participant Characteristics, Full and Follow-up Samples: Adolescents in Northern California, USA (2019-2020)
eTable 2. Behaviors at Follow-up: Associations with Stay-at-Home Order
eTable 3. Changes in Behaviors: Spring 2019 and Fall 2019 Cohorts


