B-cell receptor (BCR) signaling has emerged as a pivotal pathway in the pathogenesis and progression of chronic lymphocytic leukemia (CLL) and the introduction of small molecules targeting the BCR signalosome has dramatically changed the treatment landscape of CLL. Among such molecules, ibrutinib, a potent and selective inhibitor of the Bruton tyrosine kinase (BTK) protein, a central mediator of BCR signaling, has been associated with high efficacy and an acceptable toxicity profile in patients with CLL, including those with high-risk genetic features who respond poorly to chemoimmunotherapy.1
Ibrutinib, as well as other BCR inhibitors, produces an early redistribution of tissue-resident CLL cells into the blood, resulting in a transient, treatment-induced lymphocytosis. 2 Previous in vitro studies have shown that this phenomenon is correlated to the direct effect of the drug on B-cell adhesion and migration which leads to attenuated microenvironment retention and homing of CLL cells.3 A significant downmodulation in the gene expression and plasma concentration of tissue-homing chemokines has also been observed in vivo following combination therapies with ibrutinib and anti-CD20 monoclonal antibodies, currently being explored to improve patients’ clinical outcome.4 No data are, however, available on the modulation of CLL cell surface markers in this context. In the present study (ClinicalTrials.gov identifier NCT02232386), we analyzed the in vivo effects of ibrutinib on the expression of adhesion, migration and activation molecules in peripheral blood samples collected from 119 CLL patients enrolled in the GIMEMA LLC 1114 phase II front-line ibrutinib plus rituximab (IR) trial. In particular, the mean fluorescent intensity (MFI) of CD11a, CD18, CD38, CD40, CD43, CD44, CD49d, CD62L, CD69, CD80, CD81, CD86, CD154, CD184 and CD185 on leukemic B cells was evaluated on day 0 (D0) and day 14 (D14) of IR therapy. The CLL patients’ characteristics and experiments are detailed in Online Supplementary Table S1 and in the Online Supplementary Methods, respectively.
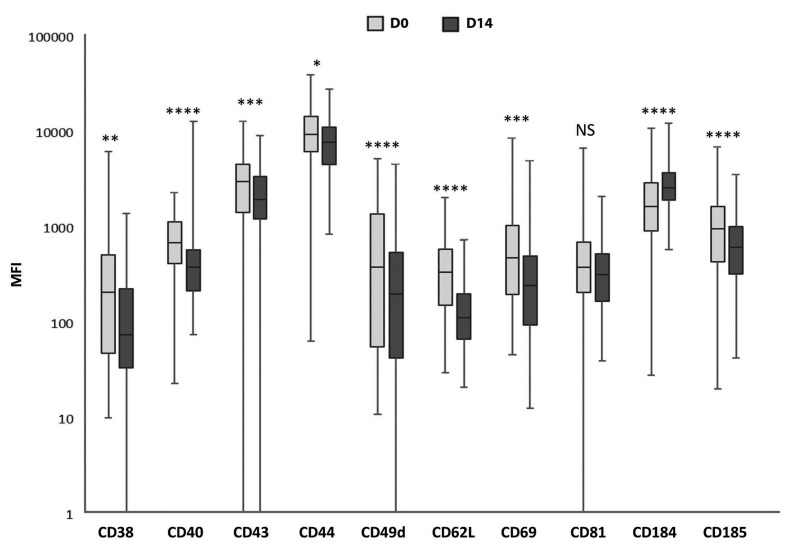
We found that 14 days of IR therapy were sufficient to induce a significant change in the levels of expression of the majority of the markers analyzed (10/15, 66.7%). As shown in Figure 1, among the antigens that were modulated, nine were downmodulated while only one was upmodulated after in vivo treatment. We observed a significant downmodulation of CD62L (467±437 vs. 162±134, P<0.00001), a key molecule in CLL cell migration, adhesion and transendothelial migration.5 The expression of the CXCL13 chemokine receptor CD185, another mediator of CLL tissue homing, also decreased significantly after in vivo treatment with IR (1396±1340 vs. 810±679, P<0.00001), while we unexpectedly observed upmodulation of the CXCL12 chemokine receptor CD184 (2309±1951 vs. 3127±1799, P<0.00001). These data are consistent with recent reports of both a greater dependency of CD184low CLL cells on microenvironmental stimuli for survival and a correlation between BCR-mediated CD184 downregulation and lymphadenopathy in CLL patients.6 In addition, ibrutinib, by inhibiting CD184-mediated signaling through blockade of CXCL12-mediated phosphorylation at CD184 Ser339, could reduce stromal tethering and further enhance CLL cell egress from lymph nodes in vivo.7
Figure 1.
Effects of ibrutinib plus rituximab in vivo treatment on the expression of chronic lymphocytic leukemia cell adhesion molecules, chemokine receptors and activation markers. Box plots show the comparison between the expression levels for each of the antigens analyzed on primary leukemic B cells before and after 14 days of in vivo treatment with ibrutinib plus rituximab. Data are presented as mean fluorescent intensity values obtained with specific monoclonal antibodies compared with values given by isotype controls. Significant differences are indicated as ****P<0.00001, ***P<0.0001, **P<0.001, *P<0.01; NS: not significant (paired Student t-test). D0: before treatment, D14: after 14 days of treatment; MFI: mean fluorescent intensity.
CLL cells also showed significantly reduced expression of CD38 and CD49d (n=48/119 CD38+ cases: 874±941 vs. 353±289, P=0.0002 and n=62/119 CD49d+ cases: 1449±1087 vs. 811±790, P<0.00001; respectively), which are associated with a worse prognosis as mediators of leukemic B-cell localization in tissue protective niches, promoting rapid growth and longer cell survival. Furthermore, among cell activation and co-stimulatory molecules, IR treatment induced significant downmodulation of CD44 (10999±6845 vs. 8844±5858, P=0.0011), a surface glycoprotein receptor for hyaluronic acid, CD40 (820±493 vs. 445±309, P<0.00001) and CD69 (825±1069 vs. 464±699, P<0.0001). Since the expression of these markers is characteristic of tissue-resident CLL cells, these results, in line with previous in vitro8 and in vivo9 observations, suggest that ibrutinib may reduce leukemic cell activation, interfering with B-cell survival and proliferation. We also recorded a significant downmodulation in the expression of CD43 (3503±2535 vs. 2714±1813, P=0.00005); contrariwise, CD81 expression resulted unchanged after 14 days of treatment (527±661 vs. 423±353, P=0.085). As both antigens are employed in CLL for the flow cytometric detection of minimal residual disease,10 our data suggest that CD43 is not a reliable marker under ibrutinib therapy and that the identification of different fluorimetric panels excluding CD43 should be considered in this context.
In agreement with the changes in MFI levels, ibrutinib treatment also induced significant decreases in the percentages of CLL cells expressing CD38 (P<0.00001), CD40 (P<0.0001), CD44 (P<0.0001), CD49d (P=0.004), CD62L (P<0.0001), CD69 (P<0.00001) and CD185 (P<0.00001). In contrast, no differences in either MFI or percentage values were observed for CD11a, CD18a, CD80, CD86 and CD154, as these antigens were barely expressed on leukemic B cells (data not shown).
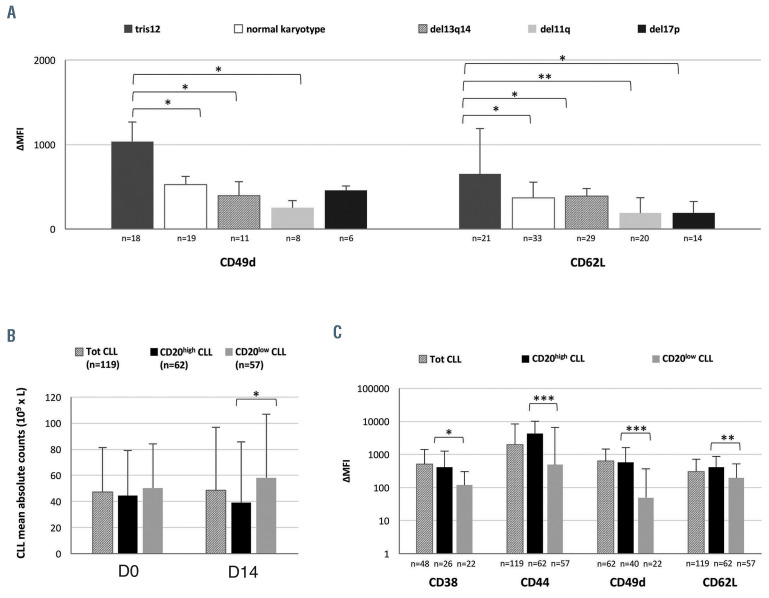
Figure 2.
Modulation of the expression of adhesion molecules, chemokine receptors and activation markers in patients with chronic lymphocytic leukemia after 14 days of ibrutinib plus rituximab in vivo treatment, according to cytogenetic aberrations and CD20 expression. (A) Comparison of the changes of expression of adhesion molecules, chemokine receptors and activation markers among the different cytogenetic categories (i.e., tris12, normal karyotype, del13q14, del11q and del17p). Data are presented as the difference between mean fluorescent intensity (MFI) of surface marker expression after 14 days (D14) of ibrutinib plus rituximab (IR) treatment compared to baseline (D0) (DMFI: D14MFI-D0MFI). Significant differences are indicated as **P<0.01, *P<0.05 (unpaired Student t-test). (B) Correlation between CD20 MFI and chronic lymphocytic leukemia (CLL) median absolute cell counts on D0 and D14 of IR in vivo treatment. CLL patients were subdivided according to a higher (CD20high MFI≥1000) or lower (CD20low MFI<1000) CD20 expression on the basis of the median value of the geometric MFI of the antigen at baseline (*P<0.05, unpaired Student t-test). D0 and D14 CLL median absolute cell counts observed in the totality of samples included in the study are added for comparison. (C) Comparison of changes of expression of adhesion molecules, chemokine receptors and activation markers between CD20high and CD20low CLL patients after 14 days of IR treatment (ΔMFI: D14MFI-D0MFI; ***P<0.001, **P<0.01, *P<0.05, unpaired Student t-test). Data of antigen expression changes observed in the totality of samples analyzed for each antigen are added for comparison.
With regard to the main biological prognostic factors in CLL, no significant differences in antigen modulation were observed according to the IGHV status. This finding is in agreement with the evidence that CLL patients with unmutated or mutated IGHV genes respond equally well to treatment with ibrutinib1 and supports the hypothesis that peripheral lymphocytosis is more related to the role of BTK in cell adhesion and migration, and less to its function in BCR signaling.11 On the contrary, the presence of TP53 mutations was associated with a lower downmodulation of CD62L MFI (21/119 TP53 mutated vs. 98/119 TP53 wild-type cases, DMFI: 202±172 vs. 479±424, P=0.039). Taking into account a lesser dependency of TP53-mutated CLL cells on the BCR pathway for survival and proliferation,12 these data may help to elucidate the biological basis for the suboptimal response of TP53-disrupted patients to ibrutinib alone or in combination with anti-CD20 monoclonal antibodies.13,14
A differential response was also observed with regard to cytogenetic aberrations. On D14, CLL samples harboring an isolated trisomy 12 (tris12+ CLL, n=21/119) showed a significantly greater downmodulation of CD49d and CD62L when compared to CLL cases with other fluorescence in situ hybridization patterns, with the exception of CD49d in del17p+ cases (Figure 2A). These results reflected the increased expression of integrins on tris12+ CLL cells. A higher baseline MFI was indeed observed for CD49d (tris12+ vs. normal karyotype, P=0.016; tris12+ vs. del13q14+, P=0.002; tris12+ vs. del11q+, P=0.0003; tris12+ vs. del17p+, P=0.029) and CD62L (tris12+ vs. del11q+, P=0.003; tris12+ vs. del17p+, P=0.026) compared to tris12– samples, which may clarify the specific tropism of tris12+ cells towards lymph nodes and the shortened lymphocytosis observed during ibrutinib monotherapy.15
Lymphocytosis was observed in 36 of the 119 CLL patients (30.3%), with D0 vs. D14 absolute lymphocyte counts being 42.6±26.4x109/L vs. 92.8±57.3x109/L, respectively (P<0.00001). The lymphocytosis appeared associated with the downmodulation of at least four antigens (P=0.050), independently of the type of antigens involved. No significant differences in antigen modulation were recorded according to the presence (36/119 cases) or absence (83/119 cases) of lymphocytosis, suggesting that ibrutinib-mediated inhibition of microenvironmental interactions could not always turn into an increase in absolute lymphocyte count, probably because of the cytotoxic effect on both tissue-resident and mobilized CLL cells. Accordingly, when CLL patients were subdivided on the basis of level of CD20 expression into those with higher (CD20high MFI ≥1000, n=62/119) or lower (CD20low MFI <1000, n=57/119) expression, CD20high cases showed both a greater clearance of CLL cells (CLL median absolute cell counts on D14 in CD20high vs. CD20low cases: 38.9±46.7x109/L vs. 58.3±48.6x109/L, P=0.030) (Figure 2B) and a lower incidence of lymphocytosis (15/62 [24.6%] vs. 21/57 [36.8%], P=0.083) on D14. In addition, CD20high CLL samples were characterized by a significantly greater downmodulation of CD38, CD44, CD49d and CD62L antigens (Figure 2C), suggesting that these cells may be more prone to mobilize into the periphery and be exposed to monoclonal antibody-mediated killing.
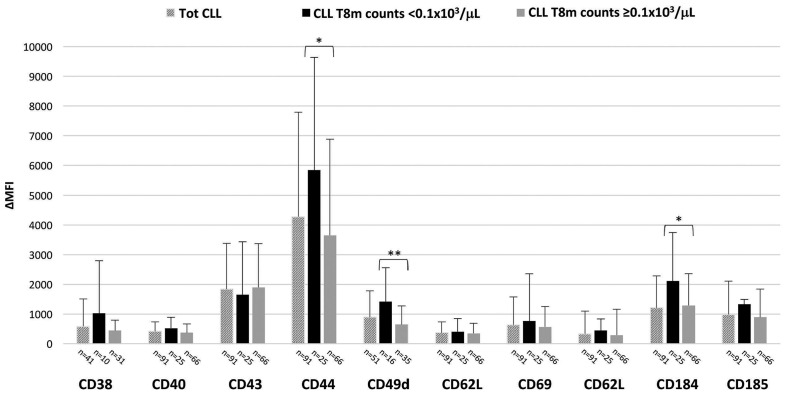
Finally, in order to assess a possible relationship between antigen expression changes and response to treatment, the MFI modulation on D14 was correlated to the amount of residual CLL cells detected in the peripheral blood 8 months after the start of IR treatment. Among 91 of 119 cases with available data, three of the 91 (3.3%) were negative for minimal residual disease while 88 (96.7%) were positive with a median minimal residual disease 8 months after starting IR treatment of 18.7%±23.7 (range, 0.01%-94%). Interestingly, an overall higher MFI modulation of all antigens analyzed, except for CD43, was observed in cases with more profound reduction of the CLL absolute cell count to values below 0.1x103/mL (n=25/91), corresponding to a percentage of pathological cells within the total leukocyte population of less than 1.5%, except for two cases with values of 2.2% and 3.0% (mean 0.64%±0.80). These differences became statistically significant for CD44 and CD49d downmodulation (CLL <0.1x103/mL vs. CLL ≥0.1x103/mL: DMFI 5839±3800 vs. 3655±3226, P=0.025 and 1415±1146 vs. 648±626, P=0.009; respectively), as well as for CD184 upmodulation (CLL <0.1x103/mL CLL ≥0.1x103/mL: DMFI 2111±1635 vs. 1291±1070, P=0.016) (Figure 3), suggesting a potential role for ibrutinibmediated early modulation of CLL surface antigen expression in predicting the degree of response to IR therapy.
Figure 3.
Correlation between the changes of expression of adhesion molecules, chemokine receptors and activation markers on day 14 compared to baseline and chronic lymphocytic leukemia absolute cell counts observed at 8 months after the start of ibrutinib plus rituximab treatment. Chronic lymphocytic leukemia absolute cell counts were calculated from flow cytometric minimal residual disease values available for 91 of the 119 patients included in the study. Data are presented as mean fluorescent intensity (MFI) of surface marker expression obtained after 14 days (D14) of ibrutinib plus rituximab treatment with respect to baseline (D0) (ΔMFI: D14MFI-D0MFI; **P<0.01, *P<0.05, unpaired Student t-test). The antigen expression changes observed in the totality of samples analyzed for each antigen are added for comparison.
Taken together, the present data demonstrate the profound immunophenotypic changes induced in vivo on primary CLL cells by 14 days of IR therapy. Since most of the molecules involved mediate the interaction of leukemic B cells with the microenvironment, our results may help to elucidate the mobilization process of CLL cells observed during ibrutinib treatment and the relationship between antigen modulation and peripheral lymphocytosis in the context of treatment approaches combining ibrutinib with anti-CD20 antibodies. The ongoing extended follow-up will further clarify the influence of the early antigen modulation on long-term therapeutic efficacy in vivo, in order to better understand the biological basis of the effect of ibrutinib over time and eventually to provide further specific antigen targets for CLL treatment.
Supplementary Material
Funding Statement
Funding: this work was supported by funds from Associazione Italiana Ricerca sul Cancro (AIRC), Special 5x1000 Program Metastases (21198), Milan (Italy) to RF. SI and MLM were supported by ROMAIL ONLUS, PM was supported by GIMEMA ONLUS.
References
- 1.Byrd JC, Furman RR, Coutre SE, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369(1):32-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Herman SE, Niemann CU, Farooqui M, et al. Ibrutinib-induced lymphocytosis in patients with chronic lymphocytic leukemia: correlative analyses from a phase II study. Leukemia. 2014;28(11):2188-2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Rooij MF, Kuil A, Geest CR, et al. The clinically active BTK inhibitor PCI-32765 targets B-cell receptor- and chemokine-controlled adhesion and migration in chronic lymphocytic leukemia. Blood. 2012;119(11):2590-2594. [DOI] [PubMed] [Google Scholar]
- 4.Burger JA, Keating MJ, Wierda WG, et al. Safety and activity of ibrutinib plus rituximab for patients with high-risk chronic lymphocytic leukaemia: a single-arm, phase 2 study. Lancet Oncol. 2014;15(10):1090-1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beke Debreceni I, Szász R, Kónya Z, Erdődi F, Kiss F, Kappelmayer J. Lselectin expression is influenced by phosphatase activity in chronic lymphocytic leukemia. Cytometry B Clin Cytom. 2019;96(2):149-157. [DOI] [PubMed] [Google Scholar]
- 6.Kriston C, Plander M, Márk Á, et al. In contrast to high CD49d, low CXCR4 expression indicates the dependency of chronic lymphocytic leukemia (CLL) cells on the microenvironment. Ann Hematol. 2018;97(11):2145-2152. [DOI] [PubMed] [Google Scholar]
- 7.Chen S-S, Chang BY, Chang S, et al. BTK inhibition results in impaired CXCR4 chemokine receptor surface expression, signaling and function in chronic lymphocytic leukemia. Leukemia. 2016;30(4):833-843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen Y, Best OG, Mulligan SP, Christopherson RI. Ibrutinib and idelalisib block immunophenotypic changes associated with the adhesion and activation of CLL cells in the tumor microenvironment. Leuk Lymphoma. 2018;59(8):1927-1937. [DOI] [PubMed] [Google Scholar]
- 9.Herman SE, Sun X, McAuley EM, et al. Modeling tumor–host interactions of chronic lymphocytic leukemia in xenografted mice to study tumor biology and evaluate targeted therapy. Leukemia. 2013;27(12):2311-2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rawstron AC, Böttcher S, Letestu R, et al. Improving efficiency and sensitivity: European Research Initiative in CLL (ERIC) update on the international harmonised approach for flow cytometric residual disease monitoring in CLL. Leukemia. 2013;27(1):142-149. [DOI] [PubMed] [Google Scholar]
- 11.Maffei R, Fiorcari S, Martinelli S, Potenza L, Luppi M, Marasca R. Targeting neoplastic B cells and harnessing microenvironment: the "double face" of ibrutinib and idelalisib. J Hematol Oncol. 2015;8:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guarini A, Peragine N, Messina M, et al. Unravelling the suboptimal response of TP53-mutated chronic lymphocytic leukaemia to ibrutinib. Br J Haematol. 2019;184(3):392-396. [DOI] [PubMed] [Google Scholar]
- 13.O'Brien S, Furman RR, Coutre S, et al. Single-agent ibrutinib in treatment- naïve and relapsed/refractory chronic lymphocytic leukemia: a 5- year experience. Blood. 2018;131(17):1910-1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burger JA, Sivina M, Jain N, et al. Randomized trial of ibrutinib versus ibrutinib plus rituximab in patients with chronic lymphocytic leukemia (CLL). Blood. 2019;133(10):1011-1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thompson PA, Ferrajoli A, O'Brien S, Wierda WG, Keating MJ, Burger JA. Trisomy 12 is associated with an abbreviated redistribution lymphocytosis during treatment with the BTK inhibitor ibrutinib in patients with chronic lymphocytic leukaemia. Br J Haematol. 2015;170(1):125-128. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.