Abstract
Background
Oral 5‐aminosalicylic acid (5‐ASA; also known as mesalazine or mesalamine) preparations were intended to avoid the adverse effects of sulfasalazine (SASP) while maintaining its therapeutic benefits. In an earlier version of this review, we found that 5‐ASA drugs were more effective than placebo for maintenance of remission of ulcerative colitis (UC), but had a significant therapeutic inferiority relative to SASP. In this version, we have rerun the search to bring the review up to date.
Objectives
To assess the efficacy, dose‐responsiveness, and safety of oral 5‐ASA compared to placebo, SASP, or 5‐ASA comparators for maintenance of remission in quiescent UC and to compare the efficacy and safety of once‐daily dosing of oral 5‐ASA with conventional (two or three times daily) dosing regimens.
Search methods
We performed a literature search for studies on 11 June 2019 using MEDLINE, Embase, and the Cochrane Library. In addition, we searched review articles and conference proceedings.
Selection criteria
We included randomized controlled trials with a minimum treatment duration of six months. We considered studies of oral 5‐ASA therapy for treatment of participants with quiescent UC compared with placebo, SASP, or other 5‐ASA formulations. We also included studies that compared once‐daily 5‐ASA treatment with conventional dosing of 5‐ASA and 5‐ASA dose‐ranging studies.
Data collection and analysis
We used standard methodological procedures expected by Cochrane. The primary outcome was the failure to maintain clinical or endoscopic remission. Secondary outcomes were adherence, adverse events (AE), serious adverse events (SAE), withdrawals due to AEs, and withdrawals or exclusions after entry. Trials were separated into five comparison groups: 5‐ASA versus placebo, 5‐ASA versus SASP, once‐daily dosing versus conventional dosing, 5‐ASA (balsalazide, Pentasa, and olsalazine) versus comparator 5‐ASA formulation (Asacol and Salofalk), and 5‐ASA dose‐ranging. We calculated the risk ratio (RR) and 95% confidence interval (CI) for each outcome. We analyzed data on an intention‐to‐treat basis, and used GRADE to assess the overall certainty of the evidence.
Main results
The search identified 44 studies (9967 participants). Most studies were at low risk of bias. Ten studies were at high risk of bias. Seven of these studies were single‐blind and three were open‐label.
5‐ASA is more effective than placebo for maintenance of clinical or endoscopic remission. About 37% (335/907) of 5‐ASA participants relapsed at six to 12 months compared to 55% (355/648) of placebo participants (RR 0.68, 95% CI 0.61 to 0.76; 8 studies, 1555 participants; high‐certainty evidence). Adherence to study medication was not reported for this comparison. SAEs were reported in 1% (6/550) of participants in the 5‐ASA group compared to 2% (5/276) of participants in the placebo group at six to 12 months (RR 0.60, 95% CI 0.19 to 1.84; 3 studies, 826 participants; low‐certainty evidence). There is probably little or no difference in AEs at six to 12 months' follow‐up (RR 0.93, 95% CI 0.73 to 1.18; 5 studies, 1132 participants; moderate‐certainty evidence).
SASP is more effective than 5‐ASA for maintenance of remission. About 48% (416/871) of 5‐ASA participants relapsed at six to 18 months compared to 43% (336/784) of SASP participants (RR 1.14, 95% CI 1.03 to 1.27; 12 studies, 1655 participants; high‐certainty evidence). Adherence to study medication and SAEs were not reported for this comparison. There is probably little or no difference in AEs at six to 12 months' follow‐up (RR 1.07, 95% CI 0.82 to 1.40; 7 studies, 1138 participants; moderate‐certainty evidence).
There is little or no difference in clinical or endoscopic remission rates between once‐daily and conventionally dosed 5‐ASA. About 37% (717/1939) of once‐daily participants relapsed over 12 months compared to 39% (770/1971) of conventional‐dosing participants (RR 0.94, 95% CI 0.88 to 1.01; 10 studies, 3910 participants; high‐certainty evidence). There is probably little or no difference in medication adherence rates. About 10% (106/1152) of participants in the once‐daily group failed to adhere to their medication regimen compared to 8% (84/1154) of participants in the conventional‐dosing group (RR 1.18, 95% CI 0.72 to 1.93; 9 studies, 2306 participants; moderate‐certainty evidence). About 3% (41/1587) of participants in the once‐daily group experienced a SAE compared to 2% (35/1609) of participants in the conventional‐dose group at six to 12 months (RR 1.20, 95% CI 0.77 to 1.87; moderate‐certainty evidence). There is little or no difference in the incidence of AEs at six to 13 months' follow‐up (RR 0.98, 95% CI 0.92 to 1.04; 8 studies, 3497 participants; high‐certainty evidence).
There may be little or no difference in the efficacy of different 5‐ASA formulations. About 44% (158/358) of participants in the 5‐ASA group relapsed at six to 18 months compared to 41% (142/349) of participants in the 5‐ASA comparator group (RR 1.08, 95% CI 0.91 to 1.28; 6 studies, 707 participants; low‐certainty evidence).
Authors' conclusions
There is high‐certainty evidence that 5‐ASA is superior to placebo for maintenance therapy in UC. There is high‐certainty evidence that 5‐ASA is inferior compared to SASP. There is probably little or no difference between 5‐ASA and placebo, and 5‐ASA and SASP in commonly reported AEs such as flatulence, abdominal pain, nausea, diarrhea, headache, and dyspepsia. Oral 5‐ASA administered once daily has a similar benefit and harm profile as conventional dosing for maintenance of remission in quiescent UC.
Plain language summary
Oral 5‐aminosalicylic acid compounds for maintaining remission in ulcerative colitis
What was the aim of this review?
The aim of this Cochrane Review was to find out if oral 5‐aminosalicylic acid (also known as mesalazine or mesalamine) helps maintain remission and prevent relapse in people with ulcerative colitis. Ulcerative colitis is an inflammatory bowel disease that results in long‐lasting inflammation of the colon. Some common symptoms include bloody diarrhea, abdominal and rectal pain, weight loss, fatigue and fever. The review authors collected and analyzed all relevant studies to answer this question and found 44 studies.
How up‐to‐date is this review?
The review authors searched for studies that had been published up to June 2019.
What was studied in the review?
The researchers examined whether oral 5‐aminosalicylic acid was better than a placebo (a fake medication), other comparator 5‐aminosalicylic acid formulations, sulfasalazine, different dose levels of oral 5‐aminosalicylic acid, and once‐daily dosing compared to conventional dosing in people with ulcerative colitis. The outcomes included clinical or endoscopic (where a long, thin tube is directly entered into the bowel) remission, adherence to medication regimen, and side effects from the medication.
What were the main results of the review?
The review authors found 44 relevant studies (9967 participants). These studies compared oral 5‐aminosalicylic medications to placebo, comparator 5‐aminosalicylic acid formulations, sulfasalazine, different dose levels of oral 5‐aminosalicylic acid, and once‐daily dosing compared to conventional dosing.
Eight studies (1555 participants) assessed the effectiveness of oral 5‐aminosalicylic acid compared to placebo. The studies found oral 5‐aminosalicylic acid was more effective than placebo for maintaining clinical or endoscopic remission (high‐certainty evidence). Twelve studies (1655 participants) assessed the effectiveness of sulfasalazine compared to 5‐aminosalicylic acid. The studies found sulfasalazine to be slightly more effective compared to 5‐aminosalicylic acid (high‐certainty evidence). Ten studies (3910 participants) assessed the effectiveness of once‐daily compared to conventional dosing (twice daily). The studies found there was probably no difference between the groups for maintaining clinical or endoscopic remission (moderate‐certainty evidence). An additional analysis of adherence to study medication was also done on once‐daily versus conventional dosing. The results showed there was probably no difference in adherence to taking medication between the two dosing groups (moderate‐certainty evidence). Six studies (1781 participants) assessed oral 5‐aminosalicylic acid (e.g. balsalazide, Pentasa, and olsalazine) compared to other 5‐aminosalicylic acid formulations (e.g. Asacol and Salofalk). The studies found there was probably no difference in clinical or endoscopic remission between the 5‐aminosalicylic acid and the 5‐aminosalicylic acid comparator groups (low‐certainty evidence).
There is probably little or no evidence of a difference in commonly reported side effects between 5‐aminosalicylic acid and any of the comparators. Commonly reported side effects included flatulence, abdominal pain, nausea, diarrhea, headache, dyspepsia (indigestion), and nasopharyngitis (inflammation of the nasal passages).
Summary of findings
Background
Description of the condition
Ulcerative colitis (UC) is an inflammatory bowel condition that results in long‐lasting inflammation of the colon. Some common symptoms of UC include diarrhea, abdominal and rectal pain, weight loss and fatigue. In addition to these symptoms, approximately 6% to 47% of patients also experience extraintestinal manifestations affecting the eyes, joints, liver, and skin. These manifestations may include arthritis, uveitis, oral ulcers, and primary sclerosing cholangitis (Rothfuss 2006). The pathogenesis of UC is unknown; however, there are genetic and environmental factors that have been correlated with the increased risk. UC is more common in the industrialized world, especially in North America and Western Europe. The overall worldwide incidence is 1.2 to 20.3 cases per 100,000 people per year, with a prevalence of 7.6 to 245 cases per 100,000 people per year (Danese 2011; Loftus 2004). In North America, the prevalence of UC ranges from 120 to 250 cases per 100,000 people and the incidence ranges from 8 to 20 cases per 100,000 people (Loftus 2004).
Treatments for UC may include biological therapies (adalimumab, infliximab, vedolizumab, golimumab, ustekinumab), corticosteroids, azathioprine or 6‐mercaptopurine, and 5‐aminosalicylic acids (5‐ASA; also known as mesalazine or mesalamine). For people with mild‐to‐moderate UC, 5‐ASAs and corticosteroids are the standard treatment for induction of remission. This is followed by thiopurines, anti‐tumor necrosis factor (anti‐TNF) drugs, or adhesion molecule inhibitors for moderate‐to‐severe UC (Feuerstein 2014).
Description of the intervention
The successful management of UC was greatly facilitated after the introduction of sulfasalazine (SASP) by Svartz (Svartz 1942). SASP is composed of 5‐ASA linked to sulfapyridine via a diazo bond. This bond is readily cleaved by bacterial azoreductases in the colon to yield the two components (Peppercorn 1972). Of these, 5‐ASA is the therapeutically active component, while sulfapyridine, which is primarily absorbed into systemic circulation, is assumed to function solely as a carrier molecule (Azad Khan 1977; Klotz 1980; Van Hees 1980).
How the intervention might work
Administration of unbound or uncoated 5‐ASA revealed that it was readily absorbed in the upper jejunum and was unable to reach the colon in therapeutic concentrations (Myers 1987; Nielsen 1983; Schroeder 1972). Ingested SASP largely resists such premature absorption and thus is able to serve as a delivery system that transports 5‐ASA to the affected regions of the lower intestinal tract (Schroeder 1972). While corticosteroid therapy is more effective in the treatment of severe UC (Truelove 1955; Truelove 1959), the use of SASP in maintaining remission has been well established (Misiewitz 1965).
Despite its benefits, up to 30% of people receiving SASP have reported adverse effects (AE) (Nielsen 1982). It was concluded that many were due to the sulfapyridine moiety, especially those effects found to be dose‐dependent (Das 1973; Myers 1987). This discovery spawned more than a decade of research aimed at finding alternative 5‐ASA delivery systems.
Asacol® (Proctor and Gamble) consists of a pellet of 5‐ASA destined for release in the terminal ileum or colon due to a coating known as Eudragit‐S, a resin that dissolves at a pH greater than 7 (Dew 1982a). Claversal® or Mesasal® (GlaxoSmithKline), Salofalk® (Axcan Pharma, Falk Foundation), and Rowasa® (Reid‐Rowell) are similar delayed‐release preparations of 5‐ASA pellets coated with Eudragit L, a resin that dissolves at a pH greater than 6 (the approximate pH of the ileum/colon) (Hardy 1987; Myers 1987). Pentasa® (Marion‐Merrell‐Dow) is a microsphere formulation that consists of 5‐ASA microgranules enclosed within a semi‐permeable membrane of ethylcellulose. It is designed for controlled release that begins in the duodenum and continues into the affected regions of the lower bowel (Rasmussen 1982). Olsalazine or Dipentum® (Pharmacia & Upjohn) consists of two 5‐ASA molecules linked by a diazo bond (Staerk Laursen 1990; Willoughby 1982). Other formulations, such as benzalazine and balsalazide, are composed of 5‐ASA molecules azo‐bonded to various benzoic acid derivatives (Chan 1983; Fleig 1988). Like SASP, these compounds are poorly absorbed in the upper digestive tract but are readily metabolized by the intestinal flora in the lower bowel. MMX mesalamine (Lialdaa® or Mezavanta®) uses Multi Matrix System (MMX) technology to delay and extend delivery of active drug throughout the colon (Kamm 2008).
The newer 5‐ASA preparations were intended to avoid the AEs of SASP while maintaining its therapeutic benefits. These drugs are more costly, however, and still cause AEs in some patients (Rao 1987). The efficacy and safety of the 5‐ASA preparations have been evaluated in numerous clinical trials that have often lacked sufficient statistical power to arrive at definitive conclusions. In an earlier meta‐analysis, Sutherland 1993 found that the newer 5‐ASA drugs were no more effective than SASP for maintenance of remission in UC. This systematic review is an update of the Cochrane Review published in 2012 (Feagan 2012). We proceeded with this updated review, in accordance with the format of Cochrane, to include the more recent studies as well as to evaluate the effectiveness, dose‐responsiveness, and safety of the 5‐ASA preparations in terms of more precise outcome measures.
Many patients are non‐adherent with conventional multi‐dose (two or three times daily) treatment regimens, which may result in reduced efficacy and can lead to an increased risk of relapse in people with quiescent disease (Kane 2001; Kane 2003a), poor long‐term prognosis (Kane 2008a), and increased costs of care (Beaulieu 2009; Kane 2008a). Poor adherence may be particularly problematic in quiescent disease (Kane 2001; Kane 2003a), since patients lack continuing symptoms that incentivize them to take medication. Although multiple factors influence medication adherence in people with UC, it is commonly believed that a high pill burden and multi‐dose regimens are major determinants (Ediger 2007; Kane 2008a). Accordingly, it is reasonable to hypothesize that once‐daily dosing of 5‐ASA might improve both adherence with maintenance therapy and outcomes.
Why it is important to do this review
This review was performed to assess the evidence supporting the use of oral 5‐ASA for the maintenance of remission in people with UC. The efficacy and safety of oral 5‐ASA compared to placebo, oral 5‐ASA compared to different formulations, and once‐daily compared to conventional dosing for the treatment of UC. Many of these trials were small and lacked sufficient statistical power to arrive at definitive conclusions. This systematic review is an update of a previously published Cochrane Review and includes three new studies (Gordon 2016; Park 2019; Suzuki 2017).
Objectives
To assess the efficacy, dose‐responsiveness, and safety of oral 5‐ASA compared to placebo, SASP, or 5‐ASA comparators for maintenance of remission in quiescent UC and to compare the efficacy and safety of once‐daily dosing of oral 5‐ASA with conventional (two or three times daily) dosing regimens.
Methods
Criteria for considering studies for this review
Types of studies
Prospective, randomized controlled trials of parallel design, with a minimum treatment duration of six months.
Types of participants
Participants of any age with mild‐to‐moderate UC in remission as defined by Truelove and Witts (Truelove 1955).
Types of interventions
We included trials of oral 5‐ASA therapy for treatment of participants with UC in remission compared with placebo, SASP, or other formulations of 5‐ASA. We also considered studies that compared once‐daily 5‐ASA treatment with conventional dosing of 5‐ASA (two or three times daily) and 5‐ASA dose‐ranging studies.
Types of outcome measures
Outcome measures included endoscopic or clinical relapse, or early withdrawal, as defined by the authors of each study.
Primary outcomes
Endoscopic or clinical relapse as defined by the authors of each study.
Secondary outcomes
Adherence with medication regimen.
Adverse events (AE).
Serious adverse events (SAE).
Withdrawal due to AEs.
Exclusion of withdrawal after entry.
Search methods for identification of studies
Electronic searches
We searched MEDLINE, Embase, the Cochrane library (CENTRAL), the Cochrane IBD Specialized Register, and clinicaltrials.gov from inception to 11 June 2019. We applied no language or document type restrictions. The search strategy is listed in Appendix 1.
Searching other resources
We searched review articles and conference abstracts to identify additional studies.
Data collection and analysis
Selection of studies
Two review authors (AM and TN) independently selected relevant studies for analysis based on the prespecified inclusion criteria. We discussed disagreements between review authors and reached agreement by consensus. When necessary, we contacted the original authors to clarify outcomes and trial methodology.
Data extraction and management
Two review authors (AM and TN) independently extracted data using a standard data extraction form. We recorded results using an intention‐to‐treat (ITT) basis and settled any discrepancies between review authors by consensus. We extracted baseline characteristics (sex, age, disease location, disease duration), intervention type (dose, administration), comparator (no intervention, placebo, active comparator), and prespecified primary and secondary outcomes.
Assessment of risk of bias in included studies
Two review authors (AM and TN) independently assessed the risk of bias in the included studies using the Cochrane 'Risk of bias' tool (Higgins 2011a). Factors assessed included:
sequence generation (i.e. was the allocation sequence adequately generated?);
allocation sequence concealment (i.e. was allocation adequately concealed?);
blinding (i.e. was knowledge of the allocated intervention adequately prevented during the study?);
incomplete outcome data (i.e. were incomplete outcome data adequately addressed?);
selective outcome reporting (i.e. are reports of the study free of suggestion of selective outcome reporting?); and
other potential sources of bias (i.e. was the study apparently free of other problems that could put it at a high risk of bias?).
A judgement of 'yes' indicated low risk of bias, 'no' indicated high risk of bias, and 'unclear' indicated unclear or unknown risk of bias. We resolved disagreements by consensus. We contacted study authors when there was insufficient information to determine risk of bias.
Measures of treatment effect
For dichotomous outcomes, we calculated the risk ratio (RR) and corresponding 95% confidence interval (CI). We pooled the results for each comparison group to determine the RR and 95% CI for each outcome resulting from 5‐ASA therapy relative to placebo, SASP, or 5‐ASA comparator; and once‐daily 5‐ASA therapy relative to conventional dosing. We used a fixed‐effect model. We pooled studies for analysis if participants, outcomes, and interventions were similar (determined by consensus among authors). We pooled studies comparing 5‐ASA formulations for analysis if they compared equimolar doses of oral 5‐ASA. For continuous outcomes, we planned to calculate the mean difference (MD) if studies used the same scale, or standardized mean difference (SMD) if studies used different scales, both with 95% CI.
Unit of analysis issues
For trials with multiple arms (e.g. different dose groups), we divided the placebo group across subgroups so that independent comparisons could be performed between each subgroup and the split placebo group (Higgins 2011b). To avoid potential carry‐over effects, we only used data from before the first cross‐over for any included cross‐over studies. For outcomes that were measured at different time points, we determined the appropriate fixed intervals for follow‐up (Higgins 2011b). For recurring events (i.e. AEs), we used the proportion of participants who had at least one event for analysis. There were no cluster randomized trials.
Dealing with missing data
We analyzed missing dichotomous outcomes according to the ITT principle. Participants with missing data were assumed to be treatment failures. Alternatively, for continuous outcomes, we used the number of participants who completed the trial and did not impute any missing variables.
Assessment of heterogeneity
We assessed the presence of heterogeneity among studies using the Chi² test (a P value of 0.10 was statistically significant) and the I² statistic (Higgins 2003). If there was statistically significant heterogeneity, we calculated the RR and 95% CI using a random‐effects model. We did not pool data in a meta‐analysis if there was a high degree of heterogeneity (e.g. I² greater than 75%).
Assessment of reporting biases
We compared the outcomes listed in the study protocols to the outcomes listed in the final manuscripts. However, if we could not locate the protocol, we compared the outcomes listed in the methods section to the outcomes in the results section. If there was a sufficient number of studies included (i.e. more than 10) in the pooled analyses, we planned to use a funnel plot to investigate a potential publication bias.
Data synthesis
Trials made five comparisons: 5‐ASA versus placebo, 5‐ASA versus SASP, once‐daily dosing versus conventional dosing, 5‐ASA versus comparator 5‐ASA, and 5‐ASA dose‐ranging. We pooled data from studies where the intervention, participant groups, and outcomes were similar. We pooled the RR and 95% CI for dichotomous outcomes and the MD or SMD and corresponding 95% CI for continuous outcomes.
Subgroup analysis and investigation of heterogeneity
We performed the following subgroup analyses.
Once‐daily versus conventional dosing studies subgrouped by formulation.
5‐ASA‐controlled trials subgrouped by common 5‐ASA comparators (e.g. Asacol, Claversal, Salofalk, and Pentasa).
Dose‐ranging studies subgrouped by 5‐ASA formulation.
Subgrouped according to the specific 5‐ASA preparation for those outcomes for which there were two or more studies that used a similar drug.
Sensitivity analysis
We conducted sensitivity analyses as appropriate to investigate heterogeneity. We also conducted sensitivity analyses excluding studies with a high risk of bias. All statistical analyses were performed using the Cochrane Review Manager 5 software package (Review Manager 2014).
'Summary of findings' tables
We used the GRADE approach for rating the overall certainty of the evidence for the primary outcomes and selected secondary outcomes of interest. Randomized trials start as high‐certainty evidence, but may be downgraded due to:
limitations in design and implementation (risk of bias);
indirectness of evidence;
inconsistency (unexplained heterogeneity);
imprecision (sparse data); and
reporting bias (publication bias).
The overall certainty of the evidence for each outcome was determined after considering each of these elements, and categorized as high certainty (i.e. further research is very unlikely to change our confidence in the estimate of effect); moderate certainty (i.e. further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate); low certainty (i.e. further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate); and very‐low certainty (i.e. we are very uncertain about the estimate) (Guyatt 2008; Schünemann 2011).
For the 'Summary of findings' tables, we included the following outcomes: endoscopic or clinical relapse, failure to adhere with study medication, at least one AEs, at least one SAEs, withdrawal due to AEs and exclusion/withdrawal after entry.
Results
Description of studies
Results of the search
The literature search conducted on 11 June 2019 identified 3331 studies. We identified 20 additional studies through searching of references. After removal of duplicates, 2321 reports remained for review of titles and abstracts. After reviewing the titles and abstracts of these studies, we selected 132 reports of oral 5‐ASA maintenance treatment for quiescent UC for full‐text review (Figure 1).
1.
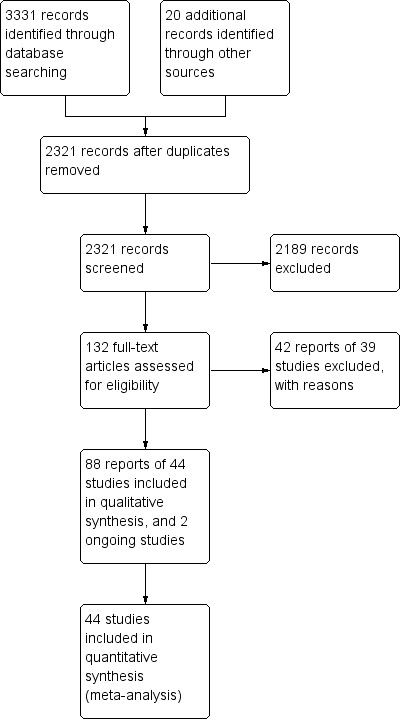
Study flow diagram.
Included studies
We included 88 reports of 44 studies involving 9967 participants (Andreoli 1987; Ardizzone 1995; Ardizzone 1999; Courtney 1992; D'Haens 2012; Deventer 2001; Dew 1983; Dignass 2009a; Fockens 1995; Giaffer 1992a; Gordon 2016; Green 1992; Green 1998; Hanauer 1996; Hawkey 1997; Hawthorne 2012; Ireland 1988a; Ito 2010; Kamm 2008; Kane 2003b; Kane 2008b; Kiilerich 1992; Kruis 1995; Kruis 2001; Kruis 2011; Lichtenstein 2010; Mahmud 2002; McIntyre 1988; Miner 1995; Mulder 1988; Nilsson 1995; Paoluzi 2005; Park 2019; Pica 2012; Prantera 2009; Rijk 1992; Riley 1988; Rutgeerts 1989; Sandberg‐Gertzen 1986; Sandborn 2010; Suzuki 2017; Travis 1994; Watanabe 2013; Wright 1993) (see Characteristics of included studies table).
Eight studies were placebo‐controlled (Ardizzone 1999; Gordon 2016; Hanauer 1996; Hawkey 1997; Lichtenstein 2010; Miner 1995; Sandberg‐Gertzen 1986; Wright 1993). Twelve studies compared 5‐ASA to SASP (Andreoli 1987; Ardizzone 1995; Dew 1983; Ireland 1988a; Kiilerich 1992; Kruis 1995; McIntyre 1988; Mulder 1988; Nilsson 1995; Rijk 1992; Riley 1988; Rutgeerts 1989). Twelve studies were maintenance of remission studies comparing once‐daily dosing of 5‐ASA with conventional dosing (D'Haens 2012; Dignass 2009a; Hawthorne 2012; Kamm 2008; Kane 2003b; Kane 2008b; Kruis 2011; Park 2019; Prantera 2009; Sandborn 2010; Suzuki 2017; Watanabe 2013). Six studies compared the efficacy and safety of various formulations of oral 5‐ASA to other formulations of oral 5‐ASA for maintenance treatment (Courtney 1992; Deventer 2001; Green 1998; Ito 2010; Kruis 2001; Mahmud 2002). Ten trials were dose‐ranging studies of oral 5‐ASA (Deventer 2001; Fockens 1995; Giaffer 1992a; Green 1992; Hanauer 1996; Kruis 2001; Kruis 2011; Paoluzi 2005; Pica 2012; Travis 1994). Six studies were formal non‐inferiority studies (D'Haens 2012; Dignass 2009a; Hawthorne 2012; Ito 2010; Sandborn 2010; Watanabe 2013).
Excluded studies
We excluded 39 reports with reasons (see Characteristics of excluded studies table).
Risk of bias in included studies
A summary of the risk of bias assessment is provided in Figure 2. Most of the included studies were of high methodological quality. Ten studies were at high risk of bias.
2.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Allocation
Nineteen studies did not describe methods used for allocation concealment and were rated as unclear for this item (Andreoli 1987; Ardizzone 1999; Ardizzone 1995; Courtney 1992; Deventer 2001; Dew 1983; Fockens 1995; Giaffer 1992a; Gordon 2016; Green 1992; Green 1998; Hawthorne 2012; Kruis 2001; Lichtenstein 2010; Mahmud 2002; Paoluzi 2005; Pica 2012; Travis 1994; Watanabe 2013). The remaining studies were at low risk of allocation bias.
Thirty of 43 included studies did not describe the method used for randomization and were rated as unclear for this item (Ardizzone 1995; Ardizzone 1999; D'Haens 2012; Deventer 2001; Dew 1983; Dignass 2009a; Giaffer 1992a; Gordon 2016; Green 1992; Green 1998; Hawkey 1997; Hawthorne 2012; Ireland 1988a; Kamm 2008; Kruis 2011; Lichtenstein 2010; McIntyre 1988; Miner 1995; Mulder 1988; Nilsson 1995; Paoluzi 2005; Pica 2012; Rijk 1992; Riley 1988; Rutgeerts 1989; Sandberg‐Gertzen 1986; Sandborn 2010; Travis 1994; Watanabe 2013; Wright 1993). The remaining studies were at low risk of randomization bias.
Blinding
Seven studies were single‐blind with a blinded investigator assessing outcomes (Courtney 1992; Deventer 2001; Dignass 2009a; Hawthorne 2012; Kane 2003b; Kane 2008b; Sandborn 2010). Three studies were open‐label and investigators and participants were not blinded to treatment assignment (Kamm 2008; Mahmud 2002; Pica 2012). However, two open‐label studies (Kamm 2008; Mahmud 2002), and four of seven single‐blind studies (Courtney 1992; Dignass 2009a; Hawthorne 2012; Kane 2008b), utilized investigator‐performed endoscopy as an endpoint, which may protect against bias provided the endoscopist is blinded. The methods used for blinding were not described in one study and this study was rated as unclear (Green 1992). The remaining studies were at low risk of performance and detection bias.
Incomplete outcome data
Thirteen studies were at unclear risk for incomplete outcome data because reasons for withdrawal were not described (Andreoli 1987; Deventer 2001; Dew 1983; Green 1998; Hanauer 1996; Hawthorne 2012; Kruis 2001; Miner 1995; Pica 2012; Rijk 1992; Rutgeerts 1989; Sandberg‐Gertzen 1986; Travis 1994).
Selective reporting
All studies were at low risk of bias for selective reporting.
Other potential sources of bias
All studies appeared free from other potential sources of bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Summary of findings 1. Oral 5‐aminosalicylic acid versus placebo for maintenance of remission in ulcerative colitis.
| Oral 5‐ASA vs placebo for maintenance of remission in ulcerative colitis | ||||||
| Patient or population: people with quiescent UC Settings: outpatient Intervention: oral 5‐ASA Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Oral 5‐ASA | |||||
|
Failure to maintain clinical or endoscopic remission Follow‐up: 6–12 months |
584 per 1000 | 373 per 1000 (334 to 416) | RR 0.68 (0.61 to 0.76) | 1555 (8 studies) | ⊕⊕⊕⊕ High | Clinical remission defined using the revised SDAI (rectal bleeding = 0, mucosal appearance ≤ 2). |
| Failure to adhere to study medication | Outcome not reported. | Not reported. | ||||
|
Adverse events Follow‐up: 6–12 months |
400 per 1000 | 372 per 1000 (292 to 472) | RR 0.93 (0.73 to 1.18) | 1132 (5 studies) | ⊕⊕⊕⊝ Moderatea | Common adverse events included headache, nausea, abdominal pain, dyspepsia, bloating, influenza syndrome, rhinitis, diarrhea, and nasopharyngitis. |
|
Serious adverse events Follow‐up: 6–12 months |
18 per 1000 |
11 per 1000 (3 to 33) |
RR 0.60 (0.19 to 1.84) |
826 (3 studies) |
⊕⊕⊝⊝ Lowb | Serious adverse events included UC aggravation, acute pancreatitis, moderate ventricular dysfunction, intestinal obstruction, and esophagitis. |
|
Withdrawal due to adverse event Follow‐up: 6–12 months |
45 per 1000 | 55 per 1000 (34 to 88) | RR 1.22 (0.76 to 1.95) | 1454 (7 studies) | ⊕⊕⊕⊝ Moderatec | Common adverse events leading to withdrawal included UC aggravation diarrhea, headache, and paresthesia. |
|
Exclusion/withdrawal after entry Follow‐up: 6–12 months |
185 per 1000 |
209 per 1000 (162 to 266) |
RR 1.13 (0.88 to 1.44) |
1074 (5 studies) |
⊕⊕⊕⊝ Moderated | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) come from control arm of meta‐analysis, based on included trials. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). 5‐ASA: 5‐aminosalicylic acid; CI: confidence interval; RR: risk ratio; SDAI: Sutherland Disease Activity Index; UC: ulcerative colitis. | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aDowngraded one level due to serious imprecision (478 events). bDowngraded two levels due to very serious imprecision (11 events). cDowngraded one level due to serious imprecision (70 events). dDowngraded one level due to serious imprecision (202 events).
Summary of findings 2. Oral 5‐aminosalicylic acid versus sulfasalazine for maintenance of remission in ulcerative colitis.
| Oral 5‐ASA vs SASP for maintenance of remission in ulcerative colitis | ||||||
| Patient or population: people with quiescent ulcerative colitis Settings: outpatient Intervention: oral 5‐ASA Comparison: SASP | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| SASP | Oral 5‐ASA | |||||
|
Failure to maintain clinical or endoscopic remission Follow‐up: 6–18 months |
429 per 1000 | 489 per 1000 (441 to 544) | RR 1.14 (1.03 to 1.27) | 1655 (12 studies) | ⊕⊕⊕⊕ High | Clinical or endoscopic remission defined as the absence of colitis symptoms together with an absence of inflammation on sigmoidoscopy. |
| Failure to adhere to study medication | Outcome not reported. | Not reported. | ||||
|
Adverse event Follow‐up: 6–18 months |
158 per 1000 | 170 per 1000 (130 to 222) | RR 1.07 (0.82 to 1.40) | 1138 (7 studies) | ⊕⊕⊕⊝ Moderatea | Commonly reported adverse events in the SASP‐controlled trials included: headache, anorexia or appetite loss, nausea, vomiting, abdominal pain, dyspepsia, excessive flatus, bloating, urticaria, and rash. |
| Serious adverse events | Outcome not reported. | Not reported. | ||||
|
Withdrawal due to adverse event Follow‐up: 6–18 months |
54 per 1000 | 69 per 1000 (47 to 102) | RR 1.27 (0.87 to 1.87) | 1585 (10 studies) | ⊕⊕⊕⊝ Moderateb | Common adverse events leading to withdrawal included diarrhea, abdominal pain, indigestion, and rash. |
|
Exclusion/withdrawal after entry Follow‐up: 6–18 months |
154 per 1000 |
200 per 1000 (160 to 251) |
RR 1.30 (1.04 to 1.63) |
1497 (9 studies) |
⊕⊕⊕⊝ Moderatec | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) come from control arm of meta‐analysis, based on included trials. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). 5‐ASA: 5‐aminosalicylic acid; CI: confidence interval; RR: risk ratio; SASP: sulfasalazine. | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aDowngraded one level due to imprecision (182 events). bDowngraded one level due to imprecision (97 events). cDowngraded one level due to imprecision (259 events).
Summary of findings 3. Once‐daily dosing versus conventional dosing for maintenance of remission in ulcerative colitis.
| Once‐daily dosing vs conventional dosing for maintenance of remission in ulcerative colitis | ||||||
| Patient or population: people with quiescent UC Settings: outpatient Intervention: OD oral 5‐ASA Comparison: conventional dosing of 5‐ASA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conventionally dosed oral 5‐ASA | OD oral 5‐ASA | |||||
|
Failure to maintain clinical or endoscopic remission Follow‐up: 12–13 months |
391 per 1000 | 367 per 1000 (344 to 395) | RR 0.94 (0.88 to 1.01) | 3910 (10 studies) | ⊕⊕⊕⊕ High | Clinical or endoscopic remission defined as a mucosal score of 0 or 1 (endoscopic remission), or a bloody stool score of 0 and an UC‐DAI < 2/Simple Clinical Colitis Activity Index score of ≤ 2 points (clinical remission). |
|
Failure to adhere to study medication regimen Follow‐up: 6–13 months |
73 per 1000 | 86 per 1000 (52 to 140) | RR 1.18 (0.72 to 1.93) | 2306 (9 studies) | ⊕⊕⊕⊝ Moderatea | Adherence to medication regimen calculated using objective data (pill count or pharmacy data) in 6/9 studies in the analysis. 2 studies used participant self‐report to calculate adherence and 1 study did not describe how adherence was assessed. |
|
Adverse event Follow‐up: 6–13 months |
490 per 1000 | 481 per 1000 (451 to 510) | RR 0.98 (0.92 to 1.04) | 3497 (8 studies) | ⊕⊕⊕⊕ High | Common adverse events included flatulence, dyspepsia, abdominal pain, nausea, diarrhea, headache, nasopharyngitis, inflammation of the upper respiratory tract, gastroenteritis. dental caries, and worsening of UC. |
|
Serious adverse events Follow‐up: 6–13 months |
22 per 1000 |
26 per 1000 (17 to 41) |
RR 1.20 (0.77 to 1.87) |
3196 (7 studies) |
⊕⊕⊕⊝ Moderateb | Serious adverse events included UC aggravation, acute pancreatitis, anal fistula, pneumonia, melena, nephrolithiasis, and hypersensitivity pneumonitis. |
|
Withdrawal due to adverse events Follow‐up: 6–13 months |
14 per 1000 | 17 per 1000 (11 to 27) | RR 1.18 (0.74 to 1.89) | 4340 (8 studies) | ⊕⊝⊝⊝ Very lowc,d | Adverse events leading to withdrawal included UC aggravation, flatulence, nausea, and abdominal distension. |
|
Exclusion/withdrawal after entry Follow‐up: 6–13 months |
150 per 1000 |
148 per 1000 (127 to 172) |
RR 0.99 (0.85 to 1.15) |
3737 (7 studies) |
⊕⊕⊕⊕ High | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) come from control arm of meta‐analysis, based on included trials. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). 5‐ASA: 5‐aminosalicylic acid; CI: confidence interval; OD: once daily; RR: risk ratio; SDAI: Sutherland Disease Activity Index; UC: ulcerative colitis; UC‐DAI: Ulcerative Colitis Disease Activity Index. | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aDowngraded one level due to imprecision (190 events). bDowngraded one level due to imprecision (76 events). cDowngraded one level due to imprecision (67 events). dDowngraded two levels due to risk of bias (two studies open label and high risk of bias).
Summary of findings 4. Oral 5‐aminosalicylic acid versus comparator 5‐aminosalicylic acid formulation for maintenance of remission in ulcerative colitis.
| Oral 5‐ASA vs comparator 5‐ASA formulation for maintenance of remission in ulcerative colitis | ||||||
| Patient or population: people with quiescent UC Settings: outpatient Intervention: oral 5‐ASA (balsalazide, Pentasa and olsalazine) Comparison: comparator oral 5‐ASA (Asacol and Salofalk) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Comparator Oral 5‐ASA | Oral 5‐ASA | |||||
|
Failure to maintain clinical or endoscopic remission Follow‐up: 6–18 months |
407 per 1000 | 439 per 1000 (370 to 521) | RR 1.08 (0.91 to 1.28) | 707 (6 studies) | ⊕⊕⊝⊝ Lowa,b | Clinical or endoscopic remission was defined as either the Harvey Bradshaw Index (score < 3) and by a sigmoidoscopy (score 0–1) or the absence of symptoms or the presence of only mild symptoms. |
| Failure to adhere to study medication regimen | Outcome not reported. | Not reported. | ||||
|
Adverse event Follow‐up: 6–12 months |
686 per 1000 | 645 per 1000 (569 to 734) | RR 0.94 (0.83 to 1.07) | 357 (4 studies) | ⊕⊕⊝⊝ Lowc,d | Common adverse events included dyspepsia, abdominal pain, nausea, distension, diarrhea, headache, nasopharyngitis or respiratory infections, influenza‐like disorder, and rash. |
|
Serious adverse events Follow‐up: 12 months |
109 per 1000 |
61 per 1000 (15 to 24) |
RR 0.56 (0.14 to 2.22) |
95 (1 study) |
⊕⊕⊝⊝ Lowe | Serious adverse events reported included urinary tract infection, severe complication of UC, cardiac arrest, ischemic heart, fracture of the scaphoid, and spigelian hernia. |
|
Withdrawal due to adverse events Follow‐up: 6–12 months |
44 per 1000 | 56 per 1000 (25 to 124) | RR 1.25 (0.0.56 to 2.78) | 457 (5 studies) | ⊕⊝⊝⊝ Verylowf,g | Common adverse events leading to withdrawal included headache, lethargy, hypertension, malaise, and abdominal pain. |
|
Exclusion/withdrawal after entry Follow‐up: 6–12 months |
222 per 1000 |
273 per 1000 (200 to 378) |
RR 1.23 (0.90 to 1.70) |
457 (5 studies) |
⊕⊕⊕⊝ Moderateh | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) come from control arm of meta‐analysis, based on included trials. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). 5‐ASA: 5‐aminosalicylic acid; CI: confidence interval; OD: once daily; RR: risk ratio; SDAI: Sutherland Disease Activity Index; UC: ulcerative colitis. | ||||||
| GRADE Working Group grades of evidence High certainty: further research is very unlikely to change our confidence in the estimate of effect. Moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low certainty: we are very uncertain about the estimate. | ||||||
aDowngraded one level due to serious imprecision (300 events). bDowngraded one level due to risk of bias. Two studies in pooled analysis were single blind and one was open label. cDowngraded one level due to serious imprecision (236 events). dDowngraded one level due to risk of bias. One study in the pooled analysis was open label. eDowngraded two levels due to serious imprecision (8 events). fDowngraded two levels due to very serious imprecision (23 events). gDowngraded one level due to risk of bias. One study in the pooled analysis due was single blind and another was open label. hDowngraded one level due to imprecision (114 events).
5‐Aminosalicylic acid versus placebo
Endoscopic or clinical relapse
Eight trials (1555 participants) reported treatment outcomes in terms of failure to maintain clinical or endoscopic remission (Ardizzone 1999; Gordon 2016; Hanauer 1996; Hawkey 1997; Lichtenstein 2010; Miner 1995; Sandberg‐Gertzen 1986; Wright 1993). At six to 12 months, 37% (335/907) of 5‐ASA participants relapsed compared to 52% (335/648) of placebo participants (RR 0.68, 95% CI 0.61 to 0.76; I² = 10%; high‐certainty evidence; Analysis 1.1). There was a trend towards greater efficacy with higher doses of 5‐ASA with a benefit for the 1 g/day to 1.9 g/day (RR 0.65, 95% CI 0.56 to 0.75; I² = 0%) and the 2 g/day or greater subgroups (RR 0.73, 95% CI 0.60 to 0.89; I² = 71%). The pooled RR was similar when calculated exclusively with those trials with endpoints at 12 months (RR 0.68, 95% CI 0.61 to 0.76) (Ardizzone 1999; Miner 1995; Wright 1993). Two trials involving olsalazine had a pooled RR of 0.76 (95% CI 0.58 to 0.99) (Sandberg‐Gertzen 1986; Wright 1993). Two trials involving Asacol (Ardizzone 1999; Hanauer 1996), had a pooled RR of 0.73 (95% CI 0.60 to 0.88). See Table 1.
1.1. Analysis.

Comparison 1: 5‐Aminosalicylic acid (5‐ASA) versus placebo, Outcome 1: Failure to maintain clinical or endoscopic remission at 6–12 months
Adherence to medication regimen
None of the studies reported adherence to medication regimen.
Adverse events
Five studies (1132 participants) reported the proportion of participants who experienced at least one AE (Gordon 2016; Hanauer 1996; Lichtenstein 2010; Miner 1995; Wright 1993). There was no difference in the incidence of AEs between 5‐ASA and placebo participants at six to 12 months. About 44% (306/702) of 5‐ASA participants experienced at least one AE compared to 40% (172/430) of placebo participants (RR 0.93, 95% CI 0.73 to 1.18; I² = 56%; moderate‐certainty evidence; Analysis 1.2). The heterogeneity appeared to be a result of the inclusion of one specific trial (Wright 1993). Wright 1993 reported a significantly higher AE rate in the 5‐ASA group compared to placebo, mostly due to a high rate of olsalazine‐related diarrhea in the 5‐ASA group. To investigate if this study was the source of the heterogeneity, we repeated the analysis excluding this trial. The pooled analysis of the ITT population now included four studies and 1031 participants (Gordon 2016; Hanauer 1996; Lichtenstein 2010; Miner 1995). Overall, 45% (294/653) of 5‐ASA participants experienced at least one AE compared to 45% (170/378) of placebo participants (RR 0.91, 95% CI 0.79 to 1.06; I² = 12%; Analysis 1.3). Commonly reported AEs in the placebo‐controlled trials included: headache, nausea, abdominal pain, dyspepsia, bloating, influenza syndrome, rhinitis, diarrhea, and nasopharyngitis. See Table 1.
1.2. Analysis.

Comparison 1: 5‐Aminosalicylic acid (5‐ASA) versus placebo, Outcome 2: Development of any adverse event at 6–12 months
1.3. Analysis.

Comparison 1: 5‐Aminosalicylic acid (5‐ASA) versus placebo, Outcome 3: Development of any adverse event (sensitivity analysis) at 6–12 months
Serious adverse events
Three studies (826 participants) reported SAEs (Gordon 2016; Hanauer 1996; Lichtenstein 2010). About 1% (6/550) of participants in the 5‐ASA group compared to 2% (5/276) of participants in the placebo group at six to 12 months had at least one SAE (RR 0.60, 95% CI 0.19 to 1.84; I² = 0%; low‐certainty evidence; Analysis 1.4). Reported SAEs included UC aggravation, acute pancreatitis, moderate ventricular dysfunction, intestinal obstruction, and esophagitis. See Table 1.
1.4. Analysis.

Comparison 1: 5‐Aminosalicylic acid (5‐ASA) versus placebo, Outcome 4: Development of any serious adverse event at 6–12 months
Withdrawals due to adverse events
Seven studies (1454 participants) reported the proportion of participants withdrawn due to AEs (Ardizzone 1999; Gordon 2016; Hanauer 1996; Hawkey 1997; Lichtenstein 2010; Miner 1995; Wright 1993). There were withdrawals due to AEs for 5% (43/855) of 5‐ASA participants compared to 5% (27/599) of placebo participants at six to 12 months (RR 1.22, 95% CI 0.76 to 1.95; I² = 37%; moderate‐certainty evidence; Analysis 1.5). The heterogeneity appeared to be a result of the inclusion of one specific trial (Wright 1993). To investigate if this study was the source of the heterogeneity, we repeated the analysis excluding this trial. The pooled analysis of the ITT population now included six studies and 1353 participants (Ardizzone 1999; Gordon 2016; Hanauer 1996; Hawkey 1997; Lichtenstein 2010; Miner 1995). Overall, 4% (31/806) of 5‐ASA participants were withdrawn due to AEs compared to 5% (25/547) of placebo participants (RR 0.86, 95% CI 0.50 to 1.47; I² = 0%; Analysis 1.6). Common AEs leading to withdrawal include UC aggravation, diarrhea, headache, and paresthesia. See Table 1.
1.5. Analysis.

Comparison 1: 5‐Aminosalicylic acid (5‐ASA) versus placebo, Outcome 5: Withdrawal from study due to adverse event at 6–12 months
1.6. Analysis.

Comparison 1: 5‐Aminosalicylic acid (5‐ASA) versus placebo, Outcome 6: Withdrawal from study due to adverse event (sensitivity analysis) at 6–12 months
Withdrawals after study entry
Five studies (1074 participants) reported the proportion of participants excluded or withdrawn after entry (Ardizzone 1999; Hanauer 1996; Lichtenstein 2010; Miner 1995; Wright 1993). About 19% (113/592) of 5‐ASA participants were withdrawn or excluded after entry compared to 18% (89/482) of placebo participants at six to 12 months (RR 1.13, 95% CI 0.88 to 1.44; I² = 11%; moderate‐certainty evidence; Analysis 1.7). See Table 1.
1.7. Analysis.

Comparison 1: 5‐Aminosalicylic acid (5‐ASA) versus placebo, Outcome 7: Exclusion/withdrawal after entry (not due to relapse) at 6–12 months
5‐Aminosalicylic acid versus sulfasalazine
Twelve trials (1655 participants) compared the efficacy of 5‐ASA and SASP (Andreoli 1987; Ardizzone 1995; Dew 1983; Ireland 1988a; Kiilerich 1992; Kruis 1995; McIntyre 1988; Mulder 1988; Nilsson 1995; Rijk 1992; Riley 1988; Rutgeerts 1989). Eight studies limited the dose of SASP to 2 g/day; one trial to 4 g/day; one trial had a mean dose of SASP of 2.7 g/day, which ranged from 2.4 g/day to 4.4 g/day (see Characteristics of included studies). See Table 2.
Endoscopic or clinical relapse
The outcome was defined as the failure to maintain clinical or endoscopic remission (withdrawals and relapses). About 48% (416/871) of 5‐ASA participants relapsed compared to 43% (336/784) of SASP participants at six to 18 months (RR 1.14, 95% CI 1.03 to 1.27; I² = 17%; high‐certainty evidence; Analysis 2.1).
2.1. Analysis.

Comparison 2: 5‐Aminosalicylic acid (5‐ASA) versus sulfasalazine (SASP), Outcome 1: Failure to maintain clinical or endoscopic remission at 6–18 months
An analysis was done limited to those studies with endpoints at 12 months (Andreoli 1987; Ardizzone 1995; Kiilerich 1992; Mulder 1988; Nilsson 1995; Rijk 1992; Riley 1988; Rutgeerts 1989), and there was no difference between the 5‐ASA and SASP groups (RR 1.10, 95% CI 0.98 to 1.23). Similarly, when the analysis was limited to studies that did not use olsalazine (Andreoli 1987; Ardizzone 1995; Dew 1983; McIntyre 1988; Mulder 1988; Riley 1988; Rutgeerts 1989), there was no difference between groups (RR 1.08, 95% CI 0.92 to 1.26; Analysis 2.2).
2.2. Analysis.

Comparison 2: 5‐Aminosalicylic acid (5‐ASA) versus sulfasalazine (SASP), Outcome 2: Failure to maintain remission (trials without olsalazine) at 6–12 months
Three trials involving Claversal had a pooled RR of 1.15 (95% CI 0.95 to 1.40) (Andreoli 1987; Ardizzone 1995; Rutgeerts 1989). When the five trials involving olsalazine were pooled, the resulting odds ratio was 1.20 (95% CI 1.04 to 1.38), thus demonstrating that SASP was more effective than olsalazine for maintenance of remission (Ireland 1988a; Kiilerich 1992; Kruis 1995; Nilsson 1995; Rijk 1992). See Table 2.
Adherence to medication regimen
None of the studies reported adherence to medication regimen.
Adverse events
Seven studies (1138 participants) reported the proportion of participants who experienced at least one AE (Andreoli 1987; Ireland 1988a; Kruis 1995; McIntyre 1988; Mulder 1988; Nilsson 1995; Rutgeerts 1989). About 16% (98/608) of 5‐ASA participants and 16% (84/530) of SASP participants experienced at least one AE at six to 18 months (RR 1.07, 95% CI 0.82 to 1.40; I² = 41%; moderate‐certainty evidence; Analysis 2.3). Three olsalazine trials including 634 participants that were homogeneous (I² = 0%) had a pooled odds ratio of 1.27 (95% CI 0.92 to 1.76) (Ireland 1988a; Kruis 1995; Nilsson 1995). Commonly reported AEs in the SASP trials included: headache, anorexia or appetite loss, nausea, vomiting, abdominal pain, dyspepsia, excessive flatus, bloating, urticaria and rash. Five studies involving olsalazine (Ireland 1988a; Kiilerich 1992; Kruis 1995; Nilsson 1995; Rijk 1992),and two studies involving Claversal (Andreoli 1987; Rutgeerts 1989), reported diarrhea. See Table 2.
2.3. Analysis.

Comparison 2: 5‐Aminosalicylic acid (5‐ASA) versus sulfasalazine (SASP), Outcome 3: Development of any adverse event at 6–18 months
Serious adverse events
None of the studies reported SAEs.
Withdrawals due to adverse events
Ten studies (1585 participants) reported the proportion of participants withdrawn due to AEs (Ardizzone 1995; Ireland 1988a; Kiilerich 1992; Kruis 1995; McIntyre 1988; Mulder 1988; Nilsson 1995; Rijk 1992; Riley 1988; Rutgeerts 1989). About 7% (56/832) of 5‐ASA participants were withdrawn due to AEs compared to 5% (41/753) of SASP participants at six to 18 months (RR 1.27, 95% CI 0.87 to 1.87; I² = 0%; moderate‐certainty evidence; Analysis 2.4).
2.4. Analysis.

Comparison 2: 5‐Aminosalicylic acid (5‐ASA) versus sulfasalazine (SASP), Outcome 4: Withdrawal from study due to adverse event at 6–18 months
In five olsalazine trials including 906 participants, 9.2% of those receiving olsalazine and 6.2% of those receiving SASP were withdrawn because of AEs (RR 1.61, 95% CI, 1.01 to 2.56) (Ireland 1988a; Kiilerich 1992; Kruis 1995; Nilsson 1995; Rijk 1992). The results from two Claversal trials including 422 participants were not different (RR 1.10, 95% CI, 0.48 to 2.54) (Ardizzone 1995; Rutgeerts 1989). Nine studies involving 1497 participants reported the proportion of participants excluded or withdrawn after entry (excluding relapses) (Ireland 1988a; Kiilerich 1992; Kruis 1995; McIntyre 1988; Mulder 1988; Nilsson 1995; Rijk 1992; Riley 1988; Rutgeerts 1989). See Table 2.
Withdrawals after study entry
About 19% (150/788) of 5‐ASA participants were excluded or withdrawn after entry compared to 15% (109/709) of SASP participants at six to 18 months (RR 1.30, 95% CI 1.04 to 1.63; Analysis 2.5). There was no significant heterogeneity detected (I² = 29%). Withdrawals or exclusions after entry were significantly higher in five olsalazine trials involving 906 participants (Ireland 1988a; Kiilerich 1992; Kruis 1995; Nilsson 1995; Rijk 1992). About 17% of olsalazine participants were withdrawn or excluded after entry compared to 12% of SASP participants (RR 1.51, 95% CI 1.09 to 2.08). Common AEs leading to withdrawal include diarrhea, abdominal pain, indigestion, and rash. See Table 2.
2.5. Analysis.

Comparison 2: 5‐Aminosalicylic acid (5‐ASA) versus sulfasalazine (SASP), Outcome 5: Exclusion/withdrawal after entry (not due to relapse) at 6–18 months
Once‐daily dosing versus conventional dosing
Endoscopic or clinical relapse
Three trials (1871 participants) reported treatment outcomes in terms of failure to maintain clinical or endoscopic remission at six months (D'Haens 2012; Kane 2003b; Sandborn 2010). About 19% (177/939) of once‐daily participants relapsed compared to 18% (172/932) of conventional‐dosing participants (RR 1.02, 95% CI 0.85 to 1.23; I² = 0%; Analysis 3.1). None of the subgroup comparisons by formulation showed any differences in efficacy between once‐daily dosing and conventional dosing. However, only two formulations were evaluated in this pooled analysis.
3.1. Analysis.

Comparison 3: Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]), Outcome 1: Failure to maintain clinical or endoscopic remission at 6 months
Ten trials (3910 participants) reported treatment outcomes in terms of failure to maintain clinical or endoscopic remission at 12 to 13 months (Dignass 2009a; Hawthorne 2012; Kamm 2008; Kane 2008b; Kruis 2011; Park 2019; Prantera 2009; Sandborn 2010; Suzuki 2017; Watanabe 2013). About 37% (717/1939) of once‐daily participants relapsed compared to 39% (770/1971) of conventional‐dosing participants (RR 0.94, 95% CI 0.88 to 1.01; I² = 32%; high‐certainty evidence; Analysis 3.2). The subgroup comparison for Pentasa favored once‐daily dosing compared to conventional twice‐daily dosing (RR 0.75, 95% CI 0.60 to 0.93). None of the other subgroup comparisons (by formulation) showed any differences in efficacy between once‐daily dosing and conventional dosing. See Table 3.
3.2. Analysis.

Comparison 3: Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]), Outcome 2: Failure to maintain clinical or endoscopic remission at 12–13 months
Adherence to medication regimen
Nine trials (2306 participants) reported adherence with study medication at study endpoint (Dignass 2009a; Hawthorne 2012; Kamm 2008; Kane 2003b; Kane 2008b; Kruis 2011; Park 2019; Prantera 2009; Watanabe 2013). Overall, 9% (106/1152) of participants in the once‐daily group failed to adhere to their medication regimen compared to 7% (84/1154) of participants in the conventional‐dosing group (RR 1.18, 95% CI 0.72 to 1.93; I² = 57%; moderate‐certainty evidence; Analysis 3.3) (6 months for Kane 2003b, 13 months for Watanabe 2013, and 12 months for the other studies in the pooled analysis). The heterogeneity appeared to be a result of the inclusion of two specific trials (Hawthorne 2012; Kamm 2008). Kamm 2008 reported a higher compliance rate of 99.6% in the twice‐daily dosing group compared to 93.3% in the once‐daily group. Hawthorne 2012 reported a higher compliance rate of 97.1% in the once‐daily dosing group compared to 85.5% in the three times‐daily dosing group. To investigate if these studies were the source of the heterogeneity, we repeated the analysis excluding these trials. The pooled analysis of the ITT population now included seven studies and 1642 participants (Dignass 2009a; Kane 2003b; Kane 2008b; Kruis 2011; Park 2019; Prantera 2009; Watanabe 2013). Overall, 11% (88/830) of participants in the once‐daily group failed to adhere to their medication regimen compared to 8% (67/812) of participants in the conventional‐dosing group (RR 1.22, 95% CI 0.92 to 1.62; I² = 0%; Analysis 3.4). See Table 3.
3.3. Analysis.

Comparison 3: Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]), Outcome 3: Failure to adhere to study medication regimen at study endpoint at 6–13 months
3.4. Analysis.

Comparison 3: Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]), Outcome 4: Failure to adhere to study medication regimen at 6–13 months (sensitivity analysis – excluding outliers)
Adverse events
Eight studies (3497 participants) reported the proportion of participants who experienced at least one AE (D'Haens 2012; Dignass 2009a; Kamm 2008; Kruis 2011; Park 2019; Prantera 2009; Suzuki 2017; Watanabe 2013). About 48% of once‐daily (835/1739) and 49% (862/1758) of conventional‐dosing participants experienced at least one AE at six to 13 months (RR 0.98, 95% CI 0.92 to 1.04; I² = 0%; high‐certainty evidence; Analysis 3.5). The most common AEs reported in the trials assessing once‐daily dosing included flatulence, dyspepsia, abdominal pain, nausea, diarrhea, headache, nasopharyngitis, inflammation of the upper respiratory tract, gastroenteritis, dental caries, and worsening of UC. See Table 3.
3.5. Analysis.

Comparison 3: Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]), Outcome 5: Development of any adverse event at 6–13 months
Serious adverse events
Seven studies (3196 participants) reported the proportion of participants who experienced at least one SAE (D'Haens 2012; Dignass 2009a; Kamm 2008; Kruis 2011; Park 2019; Prantera 2009; Suzuki 2017). About 3% (41/1587) of participants in the once‐daily group experienced at least one SAE compared to 2% (35/1609) of participants in the conventional‐dosing group at six to 13 months (RR 1.20, 95% CI 0.77 to 1.87; I² = 0%; moderate‐certainty evidence; Analysis 3.6). Reported SAEs included UC aggravation, acute pancreatitis, anal fistula, pneumonia, melena, nephrolithiasis, and hypersensitivity pneumonitis. See Table 3.
3.6. Analysis.

Comparison 3: Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]), Outcome 6: Development of serious adverse events at 6–13 months
Withdrawals due to adverse events
Eight studies (4340 participants) reported the proportion of participants who were withdrawn due to AEs (D'Haens 2012; Dignass 2009a; Kamm 2008; Kruis 2011; Prantera 2009; Sandborn 2010; Suzuki 2017; Watanabe 2013). Withdrawals due to AEs were 2% (36/2160) in the once‐daily group compared to 1% (31/2180) in the conventional‐dosing group at six to 13 months (RR 1.18, 95% CI 0.74 to 1.89; I² = 15%; very low‐certainty evidence; Analysis 3.7). See Table 3.
3.7. Analysis.

Comparison 3: Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]), Outcome 7: Withdrawal due to adverse event at 6–13 months
Withdrawals after study entry
Seven studies (3737 participants) reported the proportion of participants who were excluded or withdrawn after entry (D'Haens 2012; Dignass 2009a; Kamm 2008; Kruis 2011; Prantera 2009; Sandborn 2010; Watanabe 2013). Approximately 15% (276/1858) of once‐daily and 15% of conventional‐dosing (281/1879) participants were excluded or withdrawn after entry at six to 13 months (RR 0.99, 95% CI 0.85 to 1.15; I² = 0%; high‐certainty evidence; Analysis 3.8). Common AEs leading to withdrawal include UC aggravation, flatulence, nausea, and abdominal distension. See Table 3.
3.8. Analysis.

Comparison 3: Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]), Outcome 8: Exclusion/withdrawal after entry (not due to relapse) at 6–13 months
5‐Aminosalicylic acid versus comparator 5‐aminosalicylic acid formulation
Endoscopic or clinical relapse
Six studies (707 participants) reported treatment outcomes in terms of the failure to maintain clinical or endoscopic remission at six to 18 months (Courtney 1992; Deventer 2001; Green 1998; Ito 2010; Kruis 2001; Mahmud 2002). The overall pooled RR showed no difference in relapse between various formulations of 5‐ASA (including balsalazide, Pentasa, and olsalazine) and comparator formulations of 5‐ASA (including Asacol and Salofalk). About 44% (158/358) of participants in the 5‐ASA group relapsed compared to 41% (142/349) of participants in the 5‐ASA comparator group. The pooled RR of relapse was 1.08 using a fixed‐effect model (95% CI 0.91 to 1.28; I² = 31%; Analysis 4.1). The GRADE analysis indicated that the overall certainty of the evidence for the primary outcome (failure to maintain clinical or endoscopic remission) was low due to sparse data (300 events) and a high risk of bias (lack of blinding) in two studies in the pooled analysis. See Table 4.
4.1. Analysis.

Comparison 4: 5‐Aminosalicylic acid (5‐ASA) versus comparator 5‐ASA, Outcome 1: Failure to maintain clinical or endoscopic remission at 6–18 months
Adherence to medication regimen
None of the studies reported adherence to medication regimen.
Adverse events
Four studies (357 participants) reported the proportion of participants who experienced at least one AE between various formulations of 5‐ASA (including balsalazide, Pentasa, and olsalazine) and comparator formulations of 5‐ASA (including Asaco and Salofalk) (Green 1998; Ito 2010; Kruis 2001; Mahmud 2002). About 64% (116/182) of participants in the 5‐ASA group experienced at least one AE compared to 69% (120/175) of participants in the 5‐ASA comparator group at six to 12 months (RR 0.94, 95% CI 0.83 to 1.07; I² = 8%; low‐certainty evidence; Analysis 4.2). The most common AEs reported in these trials included dyspepsia, abdominal pain, nausea, distension, diarrhea, headache, nasopharyngitis or respiratory infections, influenza‐like disorder, and rash. See Table 4.
4.2. Analysis.

Comparison 4: 5‐Aminosalicylic acid (5‐ASA) versus comparator 5‐ASA, Outcome 2: Development of any adverse event at 6–12 months
Serious adverse events
One study (95 participants) reported on the proportion of participants who experienced at least one SAE (Green 1998). About 6% (3/49) of participants in the 5‐ASA group experienced at least one SAE compared to 11% (5/46) of participants in the 5‐ASA comparator group (RR 0.56, 95% CI 0.14 to 2.22; Analysis 4.3). Commonly reported SAEs included a urinary tract infection, a severe complication of UC, cardiac arrest, ischemic heart disease, fracture of the scaphoid, and a spigelian hernia. See Table 4.
4.3. Analysis.

Comparison 4: 5‐Aminosalicylic acid (5‐ASA) versus comparator 5‐ASA, Outcome 3: Development of any serious adverse event at 12 months
Withdrawals due to adverse events
Five studies (457 participants) reported the proportion of participants who were withdrawn due to AEs (Courtney 1992; Green 1998; Ito 2010; Kruis 2001; Mahmud 2002). About 6% (13/232) of participants in the 5‐ASA group were withdrawn due to AEs compared to 4% (10/225) of participants in the 5‐ASA comparator group at 12 months (RR 1.25, 95% CI 0.56 to 2.78; I² = 0%; very low‐certainty evidence; Analysis 4.4). Common AEs leading to withdrawal include headache, lethargy, hypertension, malaise, and abdominal pain. See Table 4.
4.4. Analysis.

Comparison 4: 5‐Aminosalicylic acid (5‐ASA) versus comparator 5‐ASA, Outcome 4: Withdrawal from study due to adverse event at 6–12 months
Withdrawals after study entry
Five studies (457 participants) reported the proportion of participants who were excluded or withdrawn after entry between various formulations of 5‐ASA (including balsalazide, Pentasa, and olsalazine) and comparator formulations of 5‐ASA (including Asacol and Salofalk) (Courtney 1992; Green 1998; Ito 2010; Kruis 2001; Mahmud 2002). About 28% (64/232) of participants in the 5‐ASA group were excluded or withdrawn after entry compared to 22% (50/225) of participants in the 5‐ASA comparator group at six to 12 months (RR 1.23, 95% CI 0.90 to 1.70; I² = 0%; moderate‐certainty evidence; Analysis 4.5). See Table 4.
4.5. Analysis.

Comparison 4: 5‐Aminosalicylic acid (5‐ASA) versus comparator 5‐ASA, Outcome 5: Exclusion/withdrawal after entry (not due to relapse) at 6–12 months
5‐Aminosalicylic acid dose ranging
Several randomized trials looked at dose‐ranging for various formulations of 5‐ASA including Asacol, balsalazide, olsalazine, Salofalk, and Pentasa.
Endoscopic or clinical relapse
Four studies examined the efficacy of various doses of Asacol for maintenance of clinical or endoscopic remission (Deventer 2001; Hanauer 1996; Paoluzi 2005; Pica 2012). Pica 2012 found no difference in efficacy between Asacol 4.8 g/day compared to 2.4 g/day. About 29% (16/56) of participants in the Asacol 4.8 g/day group relapsed compared to 36% (20/56) in the 2.4 g/day group (RR 0.80, 95% CI 0.46 to 1.38; 112 participants; very low‐certainty evidence; Analysis 5.1). Deventer 2001 found no difference in efficacy between Asacol 3.2 g/day compared to 2 g/day. About 51% (70/138) of participants in the Asacol 3.2 g/day group relapsed compared to 48% (59/124) of participants in the 2 g/day group (RR 1.07, 95% CI 0.83 to 1.37; 262 participants; Analysis 5.1). Paoluzi 2005 found no difference in efficacy between Asacol 2.4 g/day compared to 1.2 g/day. About 70% (56/80) of participants in the Asacol 2.4 g/day group relapsed compared to 74% (56/76) in the 1.2 g/day group (RR 0.95, 95% CI 0.78 to 1.16; 156 participants; Analysis 5.1). Hanauer 1996 found no difference in efficacy between Asacol 1.6 g/day compared to 0.8 g/day. About 56% (49/87) of participants relapsed in the 1.6 g/day group compared to 56% (50/90) of participants in the 0.8 g/day group (RR 1.01, 95% CI 0.78 to 1.32; 177 participants; Analysis 5.1).
5.1. Analysis.

Comparison 5: 5‐Aminosalicylic acid (5‐ASA) (dose ranging), Outcome 1: Failure to maintain clinical or endoscopic remission at 6–18 months
Three studies examined the efficacy of various doses of balsalazide (3 g/day to 6 g/day) for maintenance of clinical or endoscopic remission (Giaffer 1992a; Green 1992; Kruis 2001). Two of these studies compared balsalazide 6 g/day to 3 g/day (Green 1992; Kruis 2001). About 23% (24/104) of participants in the 6 g/day group relapsed compared to 33% (37/112) of participants in the 3 g/day group (RR 0.76, 95% CI 0.21 to 2.79; 216 participants). However, these results should be interpreted with caution as there was significant heterogeneity (I² = 86%). Giaffer 1992a compared balsalazide 4 g/day to 2 g/day and found a difference favoring the 4 g/day dose group. About 37% (25/68) of participants in the 4 g/day group relapsed compared to 55% (36/65) of participants in the 2 g/day group (RR 0.66, 95% CI 0.45 to 0.97; 133 participants; Analysis 5.1).
Travis 1994 found no significant difference in efficacy between olsalazine 2 g/day and 1 g/day. About 40% of participants in both dose groups relapsed (RR 1.01, 95% CI 0.66 to 1.54; 127 participants; Analysis 5.1). Kruis 2011 found a difference between Salofalk granules 3 g/day and 1.5 g/day. About 25% (55/217) of participants in the Salofalk 3 g/day group relapsed compared to 39% (83/212) of participants in the 1.5 g/day group (RR 0.65, 95% CI 0.49 to 0.86; 429 participants; Analysis 5.1). Fockens 1995 found no significant difference in efficacy between Pentasa 3.0 g/day and 1.5 g/day. About 28% (23/82) of participants in the 3.0 g/day group relapsed compared to 38% (33/87) in the 1.5 g/day group (RR 0.74, 95% CI 0.48 to 1.15; 169 participants; Analysis 5.1).
Adherence to medication regimen
None of the studies reported adherence to medication regimen.
Adverse events
Five dose‐ranging studies (977 participants) reported the proportion of participants who experienced at least one AE at six to 12 months (Hanauer 1996; Kruis 2001; Kruis 2011; Paoluzi 2005; Travis 1994). Kruis 2011 found a difference in the proportion of participants who experienced at least one AE between Salofalk 3 g/day and 1.5 g/day both dosed once daily. About 41% (89/217) of participants in the 3 g/day group experienced at least one AE compared to 55% (117/212) of participants in the 1.5 g/day group (RR 0.74, 95% CI 0.61 to 0.91; 429 participants; Analysis 5.2). Hanauer 1996 found a difference in the proportion of participants who experienced at least one AE between Asacol 1.6 g/day and 0.8 g/day. About 41% (36/87) of participants in the Asacol 1.6 g/day group experienced at least one AE compared to 22% (20/90) of participants in the 0.8 g/day group (RR 1.86; 95% CI 1.18 to 2.95; 177 participants; Analysis 5.2). There were no differences in the incidence of AEs between Asacol 2.4 g/day and 1.2 g/day (RR 2.85, 95% CI 0.12 to 68.95; 156 participants), balsalazide 6.0 g/day and 3.0 g/day (RR 1.40, 95% CI 0.88 to 2.24; 88 participants; Analysis 5.2), and olsalazine 2.0 g/day and 1.0 g/day (RR 1.37, 95% CI 0.94 to 1.99; 127 participants; Analysis 5.2). Common AEs include headaches, abdominal pain, and diarrhea.
5.2. Analysis.

Comparison 5: 5‐Aminosalicylic acid (5‐ASA) (dose ranging), Outcome 2: Development of any adverse event at 6–12 months
Serious adverse events
Two studies (606 participants) reported on the incidence of SAEs between the high‐dose and low‐dose groups (Hanauer 1996; Kruis 2001). About 3% (9/304) of participants in the high‐dose group compared to 3% (8/302) of participants in the low‐dose 5‐ASA group experienced an SAE at six 12 months (RR 1.11, 95% CI 0.43 to 2.82; low‐certainty evidence; Analysis 5.3). The trials did not report the specific SAEs.
5.3. Analysis.

Comparison 5: 5‐Aminosalicylic acid (5‐ASA) (dose ranging), Outcome 3: Development of any serious adverse event at 6–12 months
Withdrawals due to adverse events
Seven dose‐ranging studies (1260 participants) reported the proportion of participants who were withdrawn due to AEs at six to 12 months (Fockens 1995; Giaffer 1992a; Green 1992; Hanauer 1996; Kruis 2001; Kruis 2011; Paoluzi 2005). There were no differences in withdrawal due to AEs between Asacol 2.4 g/day and 1.2 g/day (RR 2.85, 95% CI 0.12 to 68.95; 1 study, 156 participants; Analysis 5.4); Asacol 1.6 g/day and 0.8 g/day (RR 0.34, 95% CI 0.04 to 3.25; 1 study, 177 participants; Analysis 5.4); balsalazide 6.0 g/day and 3.0 g/day (RR 0.59, 95% CI 0.21 to 1.70; 2 studies, 196 participants; Analysis 5.4); balsalazide 4.0 g/day and 2.0 g/day (RR 1.43, 95% CI 0.54 to 3.80; 1 study, 133 participants; Analysis 5.4); and Pentasa 3.0 g/day and 1.5 g/day (RR 1.06, 95% CI 0.07 to 16.69; 1 study, 169 participants; Analysis 5.4). Common AEs leading to withdrawal included headache, hypertension, malaise, and abdominal pain.
5.4. Analysis.

Comparison 5: 5‐Aminosalicylic acid (5‐ASA) (dose ranging), Outcome 4: Withdrawal from study due to adverse event at 6–12 months
Withdrawals after study entry
Eight dose‐ranging studies (1387 participants) reported the proportion of participants who were excluded or withdraw after entry at six to 12 months (Fockens 1995; Giaffer 1992a; Green 1992; Hanauer 1996; Kruis 2001; Kruis 2011; Paoluzi 2005; Travis 1994). There was a difference between balsalazide 6.0 g/day and 3.0 g/day (RR 0.47, 95% CI 0.26 to 0.84; 2 studies, 196 participants; Analysis 5.5) and between Salofalk 3 g/day and 1.5 g/day (RR 0.66, 95% CI 0.46 to 0.93; 1 study, 429 participants; Analysis 5.5). There were no significant differences in exclusions or withdrawals after entry between Asacol 2.4 g/day and 1.2 g/day (RR 0.95, 95% CI 0.38 to 2.40; 1 study, 156 participants; Analysis 5.5); Asacol 1.6 g/day and 0.8 g/day (RR 1.23, 95% CI 0.80 to 1.90; 1 study, 177 participants; Analysis 5.5); balsalazide 4.0 g/day and 2.0 g/day (RR 1.27, 95% CI 0.77 to 2.12; 1 study, 133 participants; Analysis 5.5); olsalazine 2.0 g/day and 1.0 g/day (RR 1.75, 95% CI 0.83 to 3.70; 1 study, 127 participants; Analysis 5.5); and Pentasa 3.0 g/day and 1.5 g/day (RR 0.83, 95% CI 0.44 to 1.55; 1 study, 169 participants; Analysis 5.5).
5.5. Analysis.

Comparison 5: 5‐Aminosalicylic acid (5‐ASA) (dose ranging), Outcome 5: Exclusion/withdrawal after entry (not due to relapse) at 6–12 months
Discussion
Summary of main results
This updated systematic review largely confirms the results of previous meta‐analyses (Feagan 2012; Sutherland 1993; Sutherland 1997; Sutherland 2006; Wang 2016). This updated review includes 44 studies and 9967 participants which greatly increases statistical power. The results of this systematic review provide strong evidence that point towards a number of conclusions.
The effectiveness of oral 5‐ASA preparations for maintenance of remission in quiescent UC was confirmed. Oral 5‐ASA is superior to placebo for maintenance of remission in UC. There may be a trend towards greater efficacy with higher doses of 5‐ASA with a benefit for the 1 g/day to 1.9 g/day and the 2 g/day or greater dosage groups.
An interesting result was that SASP had a modest benefit over 5‐ASA. When the pooled analysis was limited to trials with endpoints at 12 months, the difference was no longer significant. Nevertheless, certain limitations may have resulted from having combined all trials regardless of whether relapse was defined in terms of clinical or endoscopic criteria. It is possible that the 'superiority' of SASP over 5‐ASA reflects the ITT analysis that was employed. This technique considers all participants who received the medication and penalizes medications with high dropout rates (e.g. olsalazine). A per protocol analysis, which includes those participants who are compliant and who tolerate the medication, might not support a 'superiority' claim.
When data for maintenance therapy were subgrouped according to the specific 5‐ASA preparation, olsalazine was significantly inferior to SASP. Firm conclusions regarding other preparations, which have generally been subject to less‐rigorous clinical evaluation, could not be surmised. In the case of olsalazine, it appeared that the reduced efficacy was influenced by the significantly higher proportions of withdrawals due to AEs and total exclusions or withdrawals of participants receiving olsalazine compared to those receiving SASP. In fact, if the analysis of efficacy was restricted to relapses as treatment failures, excluding withdrawals for other reasons, there was no significant difference between olsalazine and SASP (data not shown). The difference may also be related to a misclassification bias in which participants who developed diarrhea were falsely classified as treatment relapses rather than having experienced AEs.
The overall superiority of SASP over 5‐ASA for maintenance therapy may also be attributable to certain pharmacological properties of SASP, including potential therapeutic effects of the sulfapyridine moiety, that are not observed with other 5‐ASA delivery systems. The mechanisms of action of SASP and its metabolites have been reviewed by Greenfield 1993.
It was apparent that the newer 5‐ASA preparations had adverse effects in several participants. However, the incidence of AEs, SAEs, and withdrawals due to the 5‐ASA formulations did not significantly differ from that associated with placebo. There was also no apparent difference between the number of AEs caused by SASP and 5‐ASA. It should be noted that there may have been a bias in favor of SASP since many of the studies involved participants who were known to have tolerated SASP in the past. This may have minimized SASP‐related AEs in these trials.
In contrast to these results, olsalazine was associated with a significantly higher proportion of withdrawals due to AEs relative to SASP. The most common AE attributed to olsalazine was diarrhea, an effect previously observed in approximately 10% of participants receiving the drug (Ireland 1988b). It has been suggested that protocol alterations may reduce withdrawal rates in future trials since it has been reported that encouraging participants to take olsalazine with meals appears to reduce the incidence of diarrhea to approximately 3% of participants (Jarnerot 1996). However, four of the five olsalazine‐SASP trials reported that such recommendations were in fact made (Kiilerich 1992; Kruis 1995; Nilsson 1995; Rijk 1992).
High‐certainty evidence suggests that 5‐ASA administered once daily is as effective as conventional dosing (twice or three times daily) for maintenance of remission over six‐ and 12‐month periods in participants with quiescent UC. With the exception of Pentasa, subgroup analyses by drug formulation showed no significant differences in efficacy between once‐daily and conventional dosing for maintenance of remission. Dignass 2009a found that 2 g of Pentasa dosed once daily was superior to 1 g Pentasa dosed twice daily for maintenance of remission at 12 months. The other Pentasa study found no difference between once‐daily and conventional dosing for maintenance of remission. A plausible biological explanation for the Dignass 2009a finding is not readily apparent to us.
The results of this meta‐analysis suggest that there is no difference in safety between once‐daily and conventional‐dose 5‐ASA. There were no differences between once‐daily and conventional‐dose 5‐ASA for safety outcomes including the overall incidence of AEs, SAEs, or withdrawal from treatment due to an AE. In keeping with the well‐established safety profile of 5‐ASA, most of the AEs reported in the studies assessing once‐daily dosing were mild to moderate in intensity. Common AEs included gastrointestinal symptoms (e.g. flatulence, abdominal pain, nausea, and diarrhea), headache, and worsening UC.
Important patient preference and adherence differences may exist between dosing regimens. In the study that measured participant preference, most participants preferred once‐daily dosing to conventional dosing (Sandborn 2010). Although it is generally believed that administration of fewer pills and less‐frequent dosing improves both efficacy and adherence, we could not demonstrate the superiority of once‐daily dosing for either of these outcomes. This result suggests that patient adherence may not be enhanced by once‐daily dosing in the clinical trial setting. Several possible explanations exist for these observations, however the most plausible one concerns the unique aspects of the clinical trial environment. It is noteworthy that adherence with medication was remarkably high in the studies that measured this outcome (Dignass 2009a; Hawthorne 2012; Kamm 2008; Kruis 2011; Prantera 2009). The pooled adherence rate for the maintenance of remission studies was 86% for the once‐daily dosing group compared to 89% for the conventional‐dosing group. These rates likely reflect the highly supervised environment in which the studies were conducted. Adherence with medication in clinical trials is generally greater than in clinical practice since participants are highly selected volunteers who are more likely, in general, to be adherent with drug regimens (Andrade 1995; Kane 2001; Kane 2006; Kane 2008a). In addition, adherence is continuously reinforced during the clinical trial process. Thus, it may be difficult to detect differences in adherence between once‐daily and multiple‐dose regimens in this setting.
Accordingly, a need exists to compare dosing regimens in large‐scale community‐based studies. In this regard, reported adherence rates in community‐based studies range from 40% to 60% and are especially poor among patients in remission (Kane 2001; Kane 2003a; Levy 1999; Shale 2003). However, whether once‐daily dosing regimens improve adherence in the community remains unknown. Although Kane 2003b demonstrated significantly higher adherence among people receiving once‐daily dosing compared to conventional dosing at three months, there were no significant differences at six months. This time‐dependent effect has been observed in a larger study (Sandborn 2010). Sandborn 2010 found significantly higher adherence among participants using once‐daily dosing compared to conventional dosing at three months. However, there was no significant difference in adherence at six and 12 months (Sandborn 2010).
Experience from other indications suggest that factors other than the dosing regimen are important for long‐term compliance (Brixner 2007; Kane 2008a). Long‐term observations in people with UC as well as in other conditions indicate that patients' and physicians' behaviors play a dominant role in adherence (Beaulieu 2009; Magowan 2006). The patient–physician relationship should reinforce adherence through education, open communication, and mutual agreement regarding the value of treatment (Kane 2008a). To ensure continued adherence in a community‐based setting, Sandborn 2010 have emphasized the importance of healthcare providers evaluating and reinforcing compliance with patients after three months of maintenance therapy.
There may be little or no difference in efficacy between the various formulations of oral 5‐ASA. The overall pooled RR (6 studies, 707 participants) showed no difference in relapse between various formulations of 5‐ASA (including balsalazide, Pentasa, and olsalazine) and comparator formulations of 5‐ASA (including Asacol and Salofalk). However, a GRADE analysis indicated that the overall certainty of the evidence for the primary outcome (failure to maintain clinical or endoscopic remission at 12 months) was low due to a high risk of bias (single blind and open‐label) in three studies in the pooled analysis and sparse data (see Table 4). However, the open‐label study (Mahmud 2002), and one of the single‐blind studies (Courtney 1992), included endoscopy as an endpoint, which may provide some protection against performance and detection bias.
Pharmacokinetic studies suggest that systemic exposure to 5‐ASA is similar for all oral 5‐ASA formulations and 5‐ASA prodrugs (Sandborn 2002a; Sandborn 2002b; Sandborn 2002c; Sandborn 2003). The excretory function of the kidneys (as measured by the glomerular filtration rate) does not change during maintenance therapy with oral 5‐ASA or olsalazine, and nephrotoxicity is rare for Pentasa or Asacol, suggesting that the systemic exposure to 5‐ASA that occurs for doses used in clinical practice is safe for all drugs in this class (Sandborn 2002a). With the exception of olsalazine‐related diarrhea, there appears to be no difference in safety between the various formulations of oral 5‐ASA. The overall pooled RRs showed no differences in the incidence of AEs, SAEs, withdrawal due to AEs, or exclusions or withdrawals after entry. These results suggest that there may be little or no difference in safety across oral 5‐ASA formulations. Treatment with SASP and olsalazine may not be preferable due to the high frequency of AEs. When deciding which 5‐ASA formulations to use, physicians and patients should consider dose‐response data, adherence issues related to dose forms (size of dose form and total number of pills or capsules per day), and price (Sandborn 2002a).
Few dose‐ranging maintenance studies were performed, which limits the conclusions that can be drawn. Hanauer 1996 compared Asacol at a dosage of 1.6 g/day to 0.8 g/day and found no difference in relapse rates between groups. Deventer 2001 compared 3.2 g/day to 2 g/day and found no difference in relapse rates between groups. Paoluzi 2005 compared Asacol at a dosage of 2.4 g/day to 1.2 g/day and found no difference in relapse rates between groups. However, participants in the higher‐dosage group remained in remission longer, compared to participants in the low‐dose group. Paoluzi 2005 recommended a dosage of 2.4 g/day due to the significantly longer time to relapse in the higher‐dosage group. Pica 2012 compared 4.8 g/day to 2.4 g/day and found no difference in relapse rates between groups. Further research may be needed to determine the ideal dosage of Asacol for maintenance therapy.
Three studies compared the efficacy of high‐dose balsalazide (4.0 g/day to 6.0 g/day) to low dose balsalazide (2.0 g/day to 3.0 g/day). Giaffer 1992a found balsalazide 4.0 g/day to be significantly superior to 2.0 g/day for preventing relapses over 12 months. There were no differences in safety between groups noted. A pooled analysis of two studies comparing balsalazide 6.0 g/day to 3.0 g/day found no significant difference in relapse rates. However, these results should be interpreted with caution due to a high degree of heterogeneity and sparse data. The high degree of heterogeneity was due to the two studies having conflicting results. Green 1992 found no differences in relapse rates between the 6.0 g/day and 3.0 g/day groups at either six or 12 months. Green 1992 noted no differences in safety. Kruis 2001 found 6.0 g/day to be superior to 3 g/day for preventing relapse over 26 weeks with no differences in safety. Differences in patient populations may explain these findings. Green 1992 included participants with a very distal extent of UC and a large proportion of participants had long‐term remission at entry (e.g. greater than one year). Kruis 2001 suggested that people with more extensive UC or with frequent relapses may benefit from a higher dose of maintenance therapy.
Kruis 2011 investigated different doses of once‐daily Salofalk (3 g or 1.5 g) and found that significantly fewer participants relapsed at 12 months in the group receiving 3 g once‐daily (25%) group compared to participants in the 1.5 g group (39%). This analysis involved 439 participants and provided moderate‐certainty evidence (based on GRADE analysis) that 3 g Salofalk once daily is superior to 1.5 g Salofalk once daily for maintenance treatment of UC. There were no differences in safety between groups. In a post hoc analysis, Kruis 2011 observed that participants with active inflammation at baseline in the 3 g group continued to maintain a higher rate of remission than participants receiving lower doses (i.e. 1.5 g once daily or 0.5 g three times daily). Kruis 2011 concluded that 3 g once daily is an appropriate dose for maintenance of remission, and may be beneficial for people with signs of inflammation or in whom endoscopic data are not available. No other maintenance studies looked at dose‐ranging for once‐daily treatment using other 5‐ASA formulations.
Travis 1994 compared the efficacy of olsalazine 2.0 g/day to 1.0 g/day and 0.5 g/day. There was no significant difference in relapse at 12 months between the 2.0 g/day and 1.0 g/day groups. A dosage of 2.0 g/day was significantly superior to 0.5 g/day for preventing relapse. There were no differences in safety noted. Subgroup analysis showed that participants with proctitis and recent relapse may benefit from a dosage of 2.0 g/day (Travis 1994). Fockens 1995 compared the efficacy of Pentasa 3.0 g/day to 1.5 g/day. Although there was a trend favoring the higher dose, there was no significant difference in prevention of relapse over one year. The higher dosage was not associated with a higher incidence of AEs (Fockens 1995).
Overall completeness and applicability of evidence
Evidence presented in this review is applicable to most patients with mild‐to‐moderate UC. The review examined 5‐ASA compared to placebo, SASP, and comparator 5‐ASA. The review also examined 5‐ASA dose‐ranging studies and once‐daily compared to conventional‐dosing studies. All the efficacy and safety outcomes we aimed to report on were included in the studies. The review found the efficacy outcomes for 5‐ASA versus placebo, 5‐ASA versus SASP, and once‐daily versus conventional dosing to be of moderate‐ to high‐certainty evidence. Therefore, this implies this area does not need additional studies. However, the evidence regarding the safety outcomes for most comparisons ranged from very low to moderate. In addition, the efficacy outcomes for the oral 5‐ASA versus comparator 5‐ASA and high‐dose versus low‐dose oral 5‐ASA ranged from low to moderate. Therefore, additional studies assessing these efficacy and safety outcomes may change the overall results.
Quality of the evidence
Fourteen studies were at low risk and 30 studies were at unclear risk for randomization because the methods of randomization were not described. Twenty‐five studies were at low risk and 19 studies were at unclear risk for allocation concealment because the methods were not adequately described. Thirty‐two studies were double blind and at low risk of bias. One study was at unclear risk because the placebo capsules were not described in detail and 10 studies were at high risk of bias because they were either single blind or open label. Thirty‐one studies were at low risk of bias and thirteen studies were at unclear risk for incomplete outcome data because the number of dropouts or reasons for withdrawal (or both) were not provided.
For the oral 5‐ASA versus placebo comparison, the certainty of the evidence for the outcome failure to maintain clinical or endoscopic remission was high. The certainty of the evidence for the outcomes AEs, withdrawal due to AEs, and exclusion/withdrawal after entry was moderate due to sparse data, and SAEs was low due to very sparse data (Table 1). For the studies comparing 5‐ASA with SASP, the certainty of the evidence for the outcome failure to maintain clinical or endoscopic remission was high. The certainty of the evidence for AEs, withdrawal due to AEs, and exclusion/withdrawal after entry was moderate due to sparse data (Table 2). For the studies comparing once‐daily dosing to conventional dosing for maintenance of remission in UC, the certainty of the evidence for failure to maintain clinical or endoscopic remission, AEs, and exclusion/withdrawal after entry was high. The certainty of the evidence for SAEs and failure to adhere to study medication outcomes was moderate due to sparse data, and lastly, withdrawal due to AEs was low due to sparse data and risk of bias (Table 3). For the studies comparing different oral 5‐ASA formulations the certainty of the evidence for exclusion/withdrawal after entry was moderate due to sparse data. Failure to maintain clinical or endoscopic remission, AEs, and SAEs were rated as low‐certainty evidence due to sparse data and risk of bias. Withdrawal due to AEs was very low‐certainty evidence due to very sparse data and risk of bias (Table 4).
Potential biases in the review process
The methods and reporting of this review were based on the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). We conducted a comprehensive literature search and two review authors independently screened the studies, extracted the data, assessed the risk of bias, and performed a GRADE analysis to minimize the bias. Despite these standardized processes, there are some potential limitations to making general conclusions from this review. Almost every study utilized a unique clinical or endoscopic index. Unlike Crohn's disease, the lack of standard indices in UC prevented the collection of consistent treatment efficacy data and makes comparisons across clinical studies difficult. In addition, results were periodically obscured in several studies that failed to specify the treatment arm to which certain excluded participants were initially randomized.
Agreements and disagreements with other studies or reviews
We identified two other systematic reviews that assessed the use of 5‐ASA for maintenance of remission in UC (Ford 2011a; Ford 2011b).
Ford 2011a is a systematic review and meta‐analysis assessing the efficacy of 5‐ASA in people with UC. The review identified 11 trials of 5‐ASAs compared to placebo in people with quiescent UC. The review concluded 5‐ASA was highly effective for preventing relapse in UC and there was no difference between the types of 5‐ASA therapy (SASP, olsalazine) used for preventing relapse in UC. The review also suggested that 5‐ASA doses of 2.0 g/day or greater have greater efficacy in comparison to the other doses. The results of our current Cochrane Review agree with the Ford review. We also found that the 5‐ASA group had lower relapse rates compared to the placebo group.
Ford 2011b is a systematic review and meta‐analysis that studied once‐daily dosing compared to conventional dosing for people with quiescent UC taking 5‐ASAs. The results showed that the relapse rates, non‐compliance, and AEs did not differ between the once‐daily and conventional dosing schedules. The study concluded that once‐daily dosing is as effective as conventional dosing for the prevention of relapse in people with UC. The results of this current Cochrane Review also concluded there are no differences in the relapse, non‐compliance/adherence, and AE rates between the once‐daily and conventional dosing groups. Therefore, the results of both reviews agree with each other.
Authors' conclusions
Implications for practice.
It is clear that oral 5‐aminosalicylic acid (5‐ASA) preparations have yet to be proven to be more clinically beneficial than sulfasalazine (SASP). Male infertility is associated with SASP and not with 5‐ASA (Kjaergaard 1989; Riley 1987), so 5‐ASA may be preferred for patients concerned about fertility. 5‐ASA therapy is more expensive than SASP, so SASP may be the preferred option where cost is an important factor. Patients who are intolerant to SASP may prefer 5‐ASA. Oral 5‐ASA administered once daily is as effective and safe as conventional dosing (twice or three times daily) for maintenance of remission in quiescent ulcerative colitis. Once‐daily dosing does not appear to enhance adherence in the clinical trial setting. There may be little or no difference in efficacy or safety between the various formulations of 5‐ASA. When selecting among the various 5‐ASA formulations, physicians and patients should consider dose‐response data, adherence issues, and price (Sandborn 2002a).
Implications for research.
With limited research funding, careful thought should be given prior to commissioning new trials of 5‐ASA preparations for the treatment of quiescent ulcerative colitis. Future trials comparing 5‐ASA with placebo or SASP may not be justified. There does not appear to be any difference in efficacy or safety between the various formulations of 5‐ASA. However, the overall certainty of the evidence from the studies examining differences in efficacy between various 5‐ASA formulations was low due to sparse data and risk of bias. Future trials should look at enhancing patient adherence with medication. Adherence to therapy is important for treatment success and may be an important predictor of relapse. Future trials could assess whether once‐daily dosing regimens improve adherence in the community.
What's new
| Date | Event | Description |
|---|---|---|
| 11 June 2019 | New search has been performed | Updated review with new authors. |
| 11 June 2019 | New citation required but conclusions have not changed | A new literature search was conducted on 11 June 2019. Three new studies were added. |
History
Review first published: Issue 4, 1997
Appendices
Appendix 1. Search strategies
MEDLINE search strategy:
1. random$.tw.
2. factorial$.tw.
3. (crossover$ or cross over$ or cross‐over$).tw.
4. placebo$.tw.
5. single blind.mp.
6. double blind.mp.
7. triple blind.mp.
8. (singl$ adj blind$).tw.
9. (double$ adj blind$).tw.
10. (tripl$ adj blind$).tw.
11. assign$.tw.
12. allocat$.tw.
13. randomized controlled trial/
14. or/1‐13
15. (colitis and ulcerat*).mp.
16. ulcerative colitis.mp. or exp ulcerative colitis/
17. (inflammatory bowel disease* or IBD).mp.
18. 19 or 20 or 21
19. 18 and 22
20. 5‐aminosalicylic acid.mp. or exp Mesalamine/
21. Mesalazine.mp. or exp Mesalamine/
22. Sulfasalazine.mp. or exp Sulfasalazine/
23. sulphasalazine.mp. or exp Sulfasalazine/
24. 24 or 25 or 26 or 27
25. 23 and 28
Embase search strategy:
1. random$.tw.
2. factorial$.tw.
3. (crossover$ or cross over$ or cross‐over$).tw.
4. placebo$.tw.
5. single blind.mp.
6. double blind.mp.
7. triple blind.mp.
8. (singl$ adj blind$).tw.
9. (double$ adj blind$).tw.
10. (tripl$ adj blind$).tw.
11. assign$.tw.
12. allocat$.tw.
13. crossover procedure/
14. double blind procedure/
15. single blind procedure/
16. triple blind procedure/
17. randomized controlled trial/
18. or/1‐17
19. (colitis and ulcerat*).mp.
20. ulcerative colitis.mp. or exp ulcerative colitis/
21. (inflammatory bowel disease* or IBD).mp.
22. 19 or 20 or 21
23. 18 and 22
24. 5‐aminosalicylic acid.mp. or exp Mesalamine/
25. Mesalazine.mp. or exp Mesalamine/
26. Sulfasalazine.mp. or exp Sulfasalazine/
27. sulphasalazine.mp. or exp Sulfasalazine/
28. 24 or 25 or 26 or 27
29. 23 and 28
Cochrane Library search strategy:
1. MeSH descriptor: [Colitis, Ulcerative] explode all trees
2. colitis
3. #1 or #2
4. 5‐ASA
5. 5‐aminosalicylic acid
6. Mesalamine
7. Sulfasalazine
8. Salazosulfapyridine
9. Sulphasalazine
10. #4 or #5 or #6 or #7 or #8 or #9
11. #3 and #10
Cochrane IBD Specialized Register:
1. 5‐ASA (ab/ti)
2. 5‐Amino* (ab/ti)
3. Mesala* (ab/ti)
4. Sulfa* (ab/ti)
5. Sulpha* (ab/ti)
6. 1 or 2 or 3 or 4 or 5
7. Colitis (ab/ti)
8. 6 and 7
ClinicalTrials.gov
5‐ASA and Ulcerative Colitis
Data and analyses
Comparison 1. 5‐Aminosalicylic acid (5‐ASA) versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Failure to maintain clinical or endoscopic remission at 6–12 months | 8 | 1555 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.61, 0.76] |
| 1.1.1 Dose of 5‐ASA: < 1 g | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.59, 1.00] |
| 1.1.2 Dose of 5‐ASA: 1–1.9 g | 6 | 1116 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.56, 0.75] |
| 1.1.3 Dose of 5‐ASA: ≥ 2 g | 2 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.60, 0.89] |
| 1.2 Development of any adverse event at 6–12 months | 5 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.73, 1.18] |
| 1.2.1 Dose of 5‐ASA: < 1 g | 1 | 133 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.51, 1.31] |
| 1.2.2 Dose of 5‐ASA: 1–1.9 g | 3 | 693 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.08] |
| 1.2.3 Dose of 5‐ASA: ≥ 2 g | 2 | 306 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [0.14, 20.58] |
| 1.3 Development of any adverse event (sensitivity analysis) at 6–12 months | 4 | 1031 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.79, 1.06] |
| 1.3.1 Dose of 5‐ASA: < 1 g | 1 | 133 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.51, 1.31] |
| 1.3.2 Dose of 5‐ASA: 1–1.9 g | 3 | 693 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.83, 1.08] |
| 1.3.3 Dose of 5‐ASA: ≥ 2 g | 1 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.25, 1.12] |
| 1.4 Development of any serious adverse event at 6–12 months | 3 | 826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.19, 1.84] |
| 1.4.1 Dose of 5‐ASA: < 1 g | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.03, 7.46] |
| 1.4.2 Dose of 5‐ASA: 1–1.9 g | 3 | 693 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.18, 2.15] |
| 1.5 Withdrawal from study due to adverse event at 6–12 months | 7 | 1454 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.76, 1.95] |
| 1.5.1 Dose of 5‐ASA: < 1 g | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.15, 13.38] |
| 1.5.2 Dose of 5‐ASA: 1–1.9 g | 5 | 1015 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.54, 1.78] |
| 1.5.3 Dose of 5‐ASA: ≥ 2 g | 2 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.80 [0.78, 4.15] |
| 1.6 Withdrawal from study due to adverse event (sensitivity analysis) at 6–12 months | 6 | 1353 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.50, 1.47] |
| 1.6.1 Dose of 5‐ASA: < 1 g | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.15, 13.38] |
| 1.6.2 Dose of 5‐ASA: 1–1.9 g | 5 | 1015 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.54, 1.78] |
| 1.6.3 Dose of 5‐ASA: ≥ 2 g | 1 | 205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.07, 1.60] |
| 1.7 Exclusion/withdrawal after entry (not due to relapse) at 6–12 months | 5 | 1074 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.88, 1.44] |
| 1.7.1 Dose of 5‐ASA: < 1 g | 1 | 177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.58, 1.40] |
| 1.7.2 Dose of 5‐ASA: 1–1.9 g | 3 | 591 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.87, 1.71] |
| 1.7.3 Dose of 5‐ASA: ≥ 2 g | 2 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.69, 2.29] |
Comparison 2. 5‐Aminosalicylic acid (5‐ASA) versus sulfasalazine (SASP).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Failure to maintain clinical or endoscopic remission at 6–18 months | 12 | 1655 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [1.03, 1.27] |
| 2.2 Failure to maintain remission (trials without olsalazine) at 6–12 months | 7 | 749 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.92, 1.26] |
| 2.3 Development of any adverse event at 6–18 months | 7 | 1138 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.82, 1.40] |
| 2.4 Withdrawal from study due to adverse event at 6–18 months | 10 | 1585 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.87, 1.87] |
| 2.5 Exclusion/withdrawal after entry (not due to relapse) at 6–18 months | 9 | 1497 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [1.04, 1.63] |
Comparison 3. Once‐daily (OD) versus conventional dosing (twice [BID] or three times daily [TID]).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Failure to maintain clinical or endoscopic remission at 6 months | 3 | 1871 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.85, 1.23] |
| 3.1.1 Asacol (OD vs BID or TID) | 2 | 1045 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.83, 1.46] |
| 3.1.2 MMX (OD) vs Asacol (BID) | 1 | 826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.75, 1.23] |
| 3.2 Failure to maintain clinical or endoscopic remission at 12–13 months | 10 | 3910 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.88, 1.01] |
| 3.2.1 Asacol (OD vs BID or TID) | 5 | 2039 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.91, 1.06] |
| 3.2.2 MMX (OD) vs Asacol (BID) | 1 | 331 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.74, 1.33] |
| 3.2.3 Pentasa (OD vs BID) | 2 | 654 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.60, 0.93] |
| 3.2.4 MMX (OD vs BID) | 1 | 451 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.87, 1.47] |
| 3.2.5 Salofalk granules (OD vs TID) | 1 | 435 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.60, 1.10] |
| 3.3 Failure to adhere to study medication regimen at study endpoint at 6–13 months | 9 | 2306 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.72, 1.93] |
| 3.4 Failure to adhere to study medication regimen at 6–13 months (sensitivity analysis – excluding outliers) | 7 | 1642 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.92, 1.62] |
| 3.5 Development of any adverse event at 6–13 months | 8 | 3497 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.92, 1.04] |
| 3.6 Development of serious adverse events at 6–13 months | 7 | 3196 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.77, 1.87] |
| 3.7 Withdrawal due to adverse event at 6–13 months | 8 | 4340 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.74, 1.89] |
| 3.8 Exclusion/withdrawal after entry (not due to relapse) at 6–13 months | 7 | 3737 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.85, 1.15] |
Comparison 4. 5‐Aminosalicylic acid (5‐ASA) versus comparator 5‐ASA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Failure to maintain clinical or endoscopic remission at 6–18 months | 6 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.91, 1.28] |
| 4.1.1 Asacol comparator | 5 | 615 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.87, 1.26] |
| 4.1.2 Salofalk comparator | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.86, 1.98] |
| 4.2 Development of any adverse event at 6–12 months | 4 | 357 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.83, 1.07] |
| 4.2.1 Asacol comparator | 3 | 265 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.85, 1.08] |
| 4.2.2 Salofalk comparator | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.51, 1.34] |
| 4.3 Development of any serious adverse event at 12 months | 1 | 95 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.14, 2.22] |
| 4.3.1 Asacol comparator | 1 | 95 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.14, 2.22] |
| 4.4 Withdrawal from study due to adverse event at 6–12 months | 5 | 457 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.56, 2.78] |
| 4.4.1 Asacol comparator | 4 | 365 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.61, 4.42] |
| 4.4.2 Salofalk comparator | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.16, 2.90] |
| 4.5 Exclusion/withdrawal after entry (not due to relapse) at 6–12 months | 5 | 457 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.90, 1.70] |
| 4.5.1 Asacol comparator | 4 | 365 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.81, 1.80] |
| 4.5.2 Salofalk comparator | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.76, 2.16] |
Comparison 5. 5‐Aminosalicylic acid (5‐ASA) (dose ranging).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Failure to maintain clinical or endoscopic remission at 6–18 months | 10 | 1781 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.72, 1.00] |
| 5.1.1 Asacol 4.8 g vs 2.4 g/day | 1 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.46, 1.38] |
| 5.1.2 Asacol 3.2 g vs 2 g/day | 1 | 262 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.83, 1.37] |
| 5.1.3 Asacol 2.4 g vs 1.2 g/day | 1 | 156 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.78, 1.16] |
| 5.1.4 Asacol 1.6 g vs 0.8 g/day | 1 | 177 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.78, 1.32] |
| 5.1.5 Balsalazide 6.0 g vs 3.0 g/day | 2 | 216 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.21, 2.79] |
| 5.1.6 Balsalazide 4.0 g vs 2.0 g/day | 1 | 133 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.45, 0.97] |
| 5.1.7 Olsalazine 2.0 g vs 1.0 g/day | 1 | 127 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.66, 1.54] |
| 5.1.8 Salofalk granules 3 g vs 1.5 g once daily | 1 | 429 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.49, 0.86] |
| 5.1.9 Pentasa 3.0 g vs 1.5 g/day | 1 | 169 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.48, 1.15] |
| 5.2 Development of any adverse event at 6–12 months | 5 | 977 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.87, 1.19] |
| 5.2.1 Asacol 2.4 g vs 1.2 g/day | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.85 [0.12, 68.95] |
| 5.2.2 Asacol 1.6 g vs 0.8 g/day | 1 | 177 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [1.18, 2.95] |
| 5.2.3 Balsalazide 6.0 g vs 3.0 g/day | 1 | 88 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.88, 2.24] |
| 5.2.4 Olsalazine 2.0 g vs 1.0 g/day | 1 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.94, 1.99] |
| 5.2.5 Salofalk granules 3 g vs 1.5 g once daily | 1 | 429 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.61, 0.91] |
| 5.3 Development of any serious adverse event at 6–12 months | 2 | 606 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.43, 2.82] |
| 5.3.1 Asacol 1.6 g vs 0.8 g/day | 2 | 606 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.43, 2.82] |
| 5.4 Withdrawal from study due to adverse event at 6–12 months | 7 | 1260 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.53, 1.61] |
| 5.4.1 Asacol 2.4 g vs 1.2 g/day | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.85 [0.12, 68.95] |
| 5.4.2 Asacol 1.6 g vs 0.8 g/day | 1 | 177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.04, 3.25] |
| 5.4.3 Balsalazide 6.0 g vs 3.0 g/day | 2 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.21, 1.70] |
| 5.4.4 Balsalazide 4.0 g vs 2.0 g/day | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.54, 3.80] |
| 5.4.5 Salofalk granules 3 g vs 1.5 g once daily | 1 | 429 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.29, 3.33] |
| 5.4.6 Pentasa 3.0 g vs 1.5 g/day | 1 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.07, 16.69] |
| 5.5 Exclusion/withdrawal after entry (not due to relapse) at 6–12 months | 8 | 1387 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.71, 1.05] |
| 5.5.1 Asacol 2.4 g vs 1.2 g/day | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.38, 2.40] |
| 5.5.2 Asacol 1.6 g vs 0.8 g/day | 1 | 177 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.80, 1.90] |
| 5.5.3 Balsalazide 6.0 g vs 3.0 g/day | 2 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.26, 0.84] |
| 5.5.4 Balsalazide 4.0 g vs 2.0 g/day | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.77, 2.12] |
| 5.5.5 Olsalazine 2.0 g vs 1.0 g/day | 1 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [0.83, 3.70] |
| 5.5.6 Salofalk granules 3 g vs 1.5 g once daily | 1 | 429 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.46, 0.93] |
| 5.5.7 Pentasa 3.0 g vs 1.5 g/day | 1 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.44, 1.55] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andreoli 1987.
| Study characteristics | ||
| Methods | Randomized, double‐blind trial comparing 5‐ASA and SASP. Allocation of drugs performed using a table of random numbers. | |
| Participants | Participants with UC in remission (n = 13). | |
| Interventions | 5‐ASA 0.75 g/day (n = 7), or SASP 1.5 g/day (n = 6) for 12 months. | |
| Outcomes | Development of a new acute phase within 12 months from the beginning of the survey was considered a negative result. | |
| Notes | Abstract. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Unclear risk | Not described. |
| Other bias | Unclear risk | Not described. |
Ardizzone 1995.
| Study characteristics | ||
| Methods | Single‐center, randomized, double‐blind comparison of Claversal and SASP. Clinical, endoscopic, and histologic exams performed at entry, after 6 months, and after 12 months. | |
| Participants | Participants, ages 18–61 years, with clinical and endoscopically quiescent UC, who had an episode of active disease requiring systemic corticosteroids at least once in the previous 12 months (n = 88). | |
| Interventions | 5‐ASA (Claversal) 1 g daily (n = 44), or SASP 2 g daily (n = 44), for 1 year. Topical corticosteroids were permitted for short‐term treatment of mild distal relapses. | |
| Outcomes | Relapse of disease defined as appearance of bloody diarrhea with endoscopic signs of inflammation requiring systemic steroids (major relapse). 'Minor relapses' defined as those requiring a few days of treatment with topical corticosteroids. Number of withdrawals due to adverse effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Ardizzone 1999.
| Study characteristics | ||
| Methods | Single‐center, randomized, double‐blind, placebo‐controlled trial. | |
| Participants | Adults (ages 18–75 years) with confirmed diagnosis of intermittent chronic UC in stable clinical, endoscopic, and histologic remission for ≥ 1 year (n = 112). | |
| Interventions | Asacol 1.2 g/day (n = 54) or identical placebo (n = 58) for 1 year. | |
| Outcomes |
Primary outcome: maintenance of remission. Relapse defined as increased stool frequency with blood or mucus and evidence of disease activity on sigmoidoscopy. Secondary outcomes: adverse events, compliance. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, identical placebo, drugs were provided in identical blister packages. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Courtney 1992.
| Study characteristics | ||
| Methods | Randomized single‐blind trial. | |
| Participants | Adults (ages 16–75 years) with UC in remission (n = 100). | |
| Interventions | Olsalazine 1.0 g /day (n = 50) or 5‐ASA (Asacol) 1.2 g/day (n = 50) for 12 months. | |
| Outcomes | Remission defined as absence of symptoms or the presence of only mild stable symptoms of colitis. Relapse defined as development of new symptoms of colitis sufficiently severe to warrant the introduction of systemic steroid therapy (by a blinded investigator). Adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomly allocated to treatment groups using a computer‐generated code. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Single‐blind (observer). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
D'Haens 2012.
| Study characteristics | ||
| Methods | Multicenter, double‐blind, double‐dummy, randomized, non‐inferiority trial comparing the efficacy and safety of OD MMX mesalamine (2.4 g/day) with twice‐daily 5‐ASA (Asacol, 1.6 g/day) in participants with UC who were in endoscopic remission. | |
| Participants | Adults (ages ≥ 18 years) with a diagnosis of UC (confirmed by histology) that was considered to be in remission for ≥ 30 days on a stable dose of 5‐ASA (≤ 2.4 g/ day) or the equivalent dose of SASP (≤ 6.2 g/ day), with an endoscopy score ≤ 1; and had a combined symptom score (stool frequency and rectal bleeding) of ≤ 1. All participants had experienced ≥ 1 acute flare of UC (defined as a documented episode of increased bowel frequency with rectal bleeding for which UC therapy was intensified) in past 12 months, with ≥ 2 acute flares in their medical history (n = 826). | |
| Interventions | MMX mesalamine (2.4 g/day) OD (n = 415) or Asacol (1.6 g/day) BID (n = 411) for 6 months. | |
| Outcomes |
Primary outcome: endoscopic remission at 6 months defined as a modified UC‐DAI endoscopy subscore of ≤ 1 point. Secondary outcomes: maintenance of mucosal healing with no or mild symptoms (combined modified UC‐DAI‐defined stool frequency and rectal bleeding subscores of ≤ 1 point) at 6 months; time to relapse (relapse defined as withdrawal due to lack of efficacy), measured from the date of randomization to the date the participant withdrew due to relapse; modified UC‐DAI score and its components (rectal bleeding, stool frequency, endoscopy, and Physician's Global Assessment scores); and safety and tolerability of study treatments. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Randomization performed centrally via an interactive voice response system. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy (matched placebos). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Deventer 2001.
| Study characteristics | ||
| Methods | Randomized, multicenter (46), single‐blind trial. | |
| Participants | Participants with quiescent UC for > 1 month but < 3 years (n = 388). | |
| Interventions | Asacol 2 g/day (n = 124), Asacol 3.2 g/day (n = 138), or Salofalk 2 g/day (n = 126) for 18 months. | |
| Outcomes | Primary outcome: remission at 18 months. | |
| Notes | Abstract publication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Single‐blind. Sigmoidoscopies were videotaped at study entry and after 9 and 18 months of treatment and blindly scored for disease activity by 2 gastroenterologists. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts and reasons for withdrawal were not described. |
| Selective reporting (reporting bias) | Unclear risk | Secondary outcomes not described. |
| Other bias | Unclear risk | Abstract publication. |
Dew 1983.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy trial. | |
| Participants | Adults (n = 67) with UC in remission (≤ 3 stools daily without blood or slime and normal sigmoidoscopic findings). | |
| Interventions | 5‐ASA (Asacol mean dose 2.7 g/day; range: 2.4–4.4 g/day; n = 32) or SASP (mean dose 2.3 g/day; range 2–4 g/day; n = 25) for 6 months. | |
| Outcomes | Relapse defined as recurrence of symptoms with sigmoidoscopic changes including contact or spontaneous mucosal hemorrhages, pus, or ulceration. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy (identical placebo pills). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 10/67 participants withdrew. 4 SASP participants withdrew due to headaches. We do not know which groups the other 6 participants belonged to. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Dignass 2009a.
| Study characteristics | ||
| Methods | Multicenter, randomized, investigator‐blinded, non‐inferiority trial. | |
| Participants | Adults (ages ≥ 18 years) with an established diagnosis of UC and in clinical remission (UC‐DIA < 2 at entry) (n = 362). | |
| Interventions | 5‐ASA (Pentasa) 2 g OD (n = 169) or 5‐ASA 1 g BID (n = 184) for 12 months. | |
| Outcomes |
Primary outcome: maintenance of clinical remission at 12 months. Secondary outcomes: time to relapse, UC‐DAI total and subscores, adherence, global acceptability of treatment, and adverse events. |
|
| Notes | 6 participants in the OD group and 3 in the BID group were excluded from the ITT analysis for major entry criteria violation. Adherence was self‐reported by participants using a VAS scale. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Participants randomized centrally using an interactive voice response system. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Single‐blind (investigator), outcomes assessed by blinded investigator. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Fockens 1995.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind trial. | |
| Participants | Adults (ages 18–75 years) with UC in remission for ≥ 1 month and up to 3 years (n = 169). | |
| Interventions | 5‐ASA (Pentasa) 1.5 g/day (n = 87) or 3.0 g/day (n = 82) for 12 months. | |
| Outcomes |
Primary outcome: maintenance of remission at 12 months. Secondary outcomes: serious adverse events. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated: randomization was performed with the SAS statistical package in balanced blocks of 10 participants. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: placebo pills were identical to 5‐ASA tablets in appearance, weight, and taste. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Giaffer 1992a.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind trial. | |
| Participants | Participants with UC in clinical (minimal or no symptoms) and sigmoidoscopic (non‐friable mucosa) remission (n = 133). | |
| Interventions | Balsalazide 2 g/day (n = 65) or 4 g /day (n = 68). | |
| Outcomes | Relapse at 12 months and adverse events. Symptomatic relapse was defined as recurrence of previous symptoms with increased stool frequency and associated blood. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: placebo and trial drug were in identical hard gelatin capsules. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Gordon 2016.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, placebo‐controlled trial. | |
| Participants | Adults (ages ≥ 18 years) with confirmed diagnosis of mild‐to‐moderate UC in remission (SDAI rectal bleeding score 0 and a screening sigmoidoscopy score 1 for mucosal appearance) for ≥ 1 month, but not for > 12 months, (n = 257). | |
| Interventions | 5‐ASA 1.5 g capsules (n = 164) OD or placebo (n = 93). | |
| Outcomes |
Primary outcome: remission at 6 months. Secondary outcomes: percentage of participants maintaining a revised SDAI < 2 with no individual component of the revised SDAI score > 1 and a score of 0 for rectal bleeding at 6 months; percentage of participants with a change from baseline in scores for stool frequency, rectal bleeding, and physician's rating of disease activity at 1, 3, and 6 months; percentage of participants with a change from baseline in mucosal appearance score at 6 months; mean change from baseline in the revised SDAI at 6 months; and duration of remission. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: matching capsules used as placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Green 1992.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind trial. | |
| Participants | Adults (ages 19–78 years) with UC in clinical and sigmoidoscopic remission (n = 108). | |
| Interventions | Balsalazide 3 g/day (n = 54) or balsalazide 6 g/day (n = 54) for 12 months. | |
| Outcomes |
Primary outcome: relapse at 12 months. Relapse defined on clinical (7 days of increased stool frequency with or without blood and mucus), sigmoidoscopic (friable mucosa or spontaneous hemorrhage) and histological grounds. Secondary outcomes: adverse events. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Double‐blind. Dummy capsules were not described in detail. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Green 1998.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, parallel‐group trial. | |
| Participants | Adults (ages 18–80 years) with UC in remission (n = 99). | |
| Interventions | Balsalazide 3 g/day (n = 50) or Asacol 1.2 g/day (n = 49) for 12 months. | |
| Outcomes |
Primary outcome: remission at 3 and 12 months. Secondary outcomes: symptom‐free days, symptoms over 3 months, adverse events (diary cards). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy, identical placebos. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 13 (26%) participants withdrew from the balsalazide group compared to 5 (11%) participants in the Asacol group. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Hanauer 1996.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, placebo‐controlled trial. Randomization performed within centers by means of codes using specific participants numbers computer‐generated for each study site before the study began. In addition to daily diaries, clinical assessments, endoscopy, and laboratory analyses were performed at entry, 1, 3, and 6 months. | |
| Participants | Participants (ages 18–75 years) with UC in remission for ≥ 1 month recruited from 17 study sites. Presence of symptoms such as loose stools or abdominal cramps were not reasons for exclusion. Corticosteroid or topical rectal therapy was stopped ≥ 1 month before entry (n = 264). | |
| Interventions | 5‐ASA (Asacol) 0.8 g/day (n = 90) or 5‐ASA 1.6 g/day (n = 87) or matched placebo (n = 87) for 6 months. 400 mg pills packaged in 4 bottles, each labeled with the time of day at which its contents were to be taken. Compliance was monitored by pill count. | |
| Outcomes | Treatment outcome rated as 'success' (maintenance of remission as indicated by endoscopic evaluation) or 'failure' (endoscopic relapse or withdrawal), and was reported on an ITT basis. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Placebo pills identical to the 5‐ASA pills in odor and appearance but contained no active ingredients. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 75 participants excluded from the primary efficacy analysis for the following reasons: failure to meet study entry criteria (n = 36), non‐compliance with study medication (n = 18), non‐compliance with study procedures (n = 3), concomitant medication violation (n = 10), loss to follow‐up (n = 4), and voluntary withdrawal (n = 4). Numbers of participants excluded were similar in the 3 groups. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Hawkey 1997.
| Study characteristics | ||
| Methods | International, multicenter, randomized, double‐blind study comparing 5‐ASA and placebo for their ability to maintain remission in UC. | |
| Participants | Participants (ages ≥ 18 years) with UC in remission as defined by normal sigmoidoscopic appearances with no rectal bleeding during the week before entry. Participants already receiving salicylates could enter; those receiving oral or rectal steroids could only do so if these were tapered over 2 weeks prior to entry (n = 323). | |
| Interventions | 1 × 5‐ASA 400 mg capsule + 2 placebo capsules 4 times per day (n = 99) or 3 placebo capsules 4 times per day (n = 111) for 6 months. All capsules were identical in appearance. | |
| Outcomes | Primary outcomes: maintenance of remission. Relapse defined as a sigmoidoscopic score of ≥ 1 or 3 consecutive days of rectal bleeding caused by UC or liquid stools for 1 week. Number of participants withdrawing due to adverse events. | |
| Notes | Primary objective was the measurement of the efficacy of zileuton (n = 113) in UC. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Centralized randomization: concealed randomization schedules were held at each participating hospital for code break in the event of serious adverse events. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Each capsule was identical in appearance. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Hawthorne 2012.
| Study characteristics | ||
| Methods | Multicenter, single‐blind, randomized, non‐inferiority study comparing once‐daily 5‐ASA to conventional‐dosed 5‐ASA (TID) for maintenance of remission in UC. | |
| Participants | Adults with UC taking 5‐ASA or SASP in remission for > 4 weeks and < 2 years (n = 213). | |
| Interventions | Asacol 2.4 g/day OD (3 × 800 mg pills; n = 103) or Asacol 2.4 g/day TID (1 × 800 mg pill 3 times per day, n = 110) for 1 year. | |
| Outcomes |
Primary outcome: relapse rates over 1 year. Relapse defined as typical symptoms of relapse with a Baron sigmoidoscopy score of 2 or 3. Secondary outcomes: adherence. |
|
| Notes | Investigator‐blinded. Adherence was self‐reported by participants. Adherence also was calculated in subgroup of participants (n = 58) using "Medication Event Monitoring System (MEMS®)" based in a bottle cap which records each time the bottle is opened. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Investigator‐blinded, outcomes assessed by blinded investigator. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Ireland 1988a.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy trial comparing olsalazine and SASP. Randomization in blocks of 10, and the drugs dispensed by hospital pharmacy. At entry, 3, and 6 months, a history, clinical exam, sigmoidoscopy, and rectal biopsy were performed. | |
| Participants | Outpatients (ages 18–75 years) with UC in remission (without a relapse for previous 6 months) taking a mean dose of 2 g/day SASP, recruited over 18 months (n = 164). | |
| Interventions | SASP 2 g/day, plus olsalazine‐matched placebo (n = 82) or olsalazine 1 g/day, plus SASP‐matched placebo (n = 82) for 6 months. | |
| Outcomes | Relapse defined as increased stool frequency with or without blood or mucus and with evidence of inflammation on sigmoidoscopy. Withdrawals and occurrence of adverse effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts generally balanced across groups with similar reasons for withdrawal with the exception of a greater number of participants withdrawing from the olsalazine group (n = 10) due to diarrhea (n = 3 in SASP group). |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Ito 2010.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy, non‐inferiority trial. | |
| Participants | Adults (ages ≥ 16 to < 65 years) with quiescent (UC‐DAI of ≤ 2 and bloody stool score of 0) UC (n = 131). | |
| Interventions | Pentasa 2.25 g/day (n = 66) or Asacol 2.4 g/day (n = 65) for 48 weeks. | |
| Outcomes |
Primary outcome: proportion of participants without bloody stools. Secondary outcomes: time to bloody stools, proportion of participants without relapse, time to relapse, decrease in UC‐DAI, and adverse events. Relapse was defined as a bloody stool score of ≥ 1 and UC‐DAI of ≥ 3. |
|
| Notes | 1 participant from the Pentasa group was excluded from the ITT analysis due to a GCP violation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. Treatment assignment balanced using a biased‐coin minimization algorithm. |
| Allocation concealment (selection bias) | Low risk | Centralized randomization: a person independent from the study oversaw the random allocation. The randomization code was sealed and stored until the blind was removed. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Kamm 2008.
| Study characteristics | ||
| Methods | Multicenter, randomized, open‐label trial. | |
| Participants | Adults were entered following induction of remission after an acute flare of mild‐to‐moderate UC (n = 451) in clinical and endoscopic remission (modified UC‐DAI score ≤ 1, with rectal bleeding and stool frequency scores 0, combined PGA and sigmoidoscopy score ≤ 1, no mucosal friability and ≥ 1 point reduction from baseline in sigmoidoscopy score). | |
| Interventions | MMX mesalazine 2.4 g/day OD (n = 225) or MMX mesalazine 2.4 g/day in 2 divided doses of 1.2 g (n = 234) for 12 months. | |
| Outcomes |
Primary outcome: safety and tolerability over 12 months. Secondary outcomes: proportion of participants in remission at 12 months, changes from baseline in components of the modified UC‐DAI, and adherence. |
|
| Notes | Compliance with study medication was calculated by pill count at study visits. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Centralized randomization: participants randomized via an interactive voice recognition system. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Kane 2003b.
| Study characteristics | ||
| Methods | Single‐center, investigator‐blinded, randomized trial. | |
| Participants | Adults with UC in remission (defined as absence of blood in stools, urgency, or cramping) for ≥ 4 months prior to entry (n = 22). | |
| Interventions | 5‐ASA (Asacol) dosed OD (n = 12) or 5‐ASA BID or TID (n = 10) for 6 months. | |
| Outcomes |
Primary outcome: presence of absence of disease activity at end of 6‐month treatment. Relapse defined as HBI > 3. Secondary outcomes: adherence and participant satisfaction with treatment. |
|
| Notes | Mean dose of Asacol in OD group was 2.5 g/day. Mean dose of Asacol in the conventional‐dosed group was 2.7 g/day. Adherence calculated using pharmacy data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐numbers table. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Investigator‐blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Unclear risk | Study appeared free of other sources of bias. |
Kane 2008b.
| Study characteristics | ||
| Methods | 2 center, investigator‐blinded, randomized trial. | |
| Participants | Adults with UC in remission (defined as absence of blood in stools, urgency, or cramping) for ≥ 4 months prior to entry (n = 20). | |
| Interventions | 5‐ASA (Asacol) OD (n = 12) or 5‐ASA BID or TID (n = 8) for 12 months. | |
| Outcomes |
Primary outcome: remission and relapse at 12 months. Remission defined as modified UC‐DAI ≤ 3 and relapse was defined as UC‐DAI > 3. Secondary outcomes: adherence and adverse events. |
|
| Notes | Adherence calculated using pharmacy data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Investigator‐blinded, participant assessed by blinded physician at 6‐ and 12‐month assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 participant in the OD 5‐ASA group died. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Kiilerich 1992.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy comparison of olsalazine and SASP. Randomization scheme computer‐generated, stratified for each center and performed in blocks of 4 consecutive participants within each center. Clinical exam, sigmoidoscopy, and blood tests performed at entry and after 6 and 12 months (or upon relapse). | |
| Participants | Outpatients (ages 18–80 years), with UC in remission, but who had ≥ 2 attacks of UC, were recruited from March 1988 to March 1989 (n = 226). | |
| Interventions | Olsalazine 1 g/day (n = 114) or SASP 2 g/day (n = 112), in a double‐dummy method for 12 months. Participants were instructed to take medications with meals. Participants were questioned upon clinical exam to verify their compliance. | |
| Outcomes | Relapse defined as inflammation of the rectal mucosa grade 3–4 on sigmoidoscopy (no distinct vessels in the mucosa, spontaneous bleeding, or bleeding by contact with the sigmoidoscope). Total failure rate. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Kruis 1995.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind comparison of 3 doses of olsalazine and a standard dose of SASP. Randomization scheme computer‐generated and performed in blocks of 8 and stratified for each center. Clinical assessments performed at entry, 2, 4, and 6 months. Endoscopic exam performed at entry and after 6 months (or at relapse). | |
| Participants | Participants with confirmed UC in remission were recruited at 15 centers in 3 countries. No concomitant medications were permitted (n = 148). | |
| Interventions | Olsalazine 0.5 g/day or olsalazine 1.25 g/day or olsalazine 2.0 g/day or SASP 2 g/day for 6 months. Participants were instructed to take medications with meals. Medications were similar in color, size, and weight. Full dosage was reached after 5 days. Compliance was monitored. | |
| Outcomes | Relapse defined as a change in the endoscopic grading, and corresponding histologic assessment, to at least moderate activity. Withdrawals. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization scheme computer‐generated and performed in blocks of 8 and stratified for each center. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Study was double‐blind and the medication was similar in color, size, and weight. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Kruis 2001.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double dummy, 3‐armed, parallel‐group trial. | |
| Participants | Adults (ages 18–70 years) with UC in remission for < 1 year (n = 133). | |
| Interventions | Balsalazide 3 g BID (n = 40) or balsalazide 1.5 g BID (n = 48) or Salofalk 0.5 g TID (n = 44) for 26 weeks. | |
| Outcomes |
Primary outcome: proportion of participants in clinical remission at 26 weeks. Secondary outcomes: CAI, endoscopic score, urine analysis, adverse events. Clinical remission defined as a CAI < 6. Endoscopic findings were also classified according to Rachmilewitz and an EI score < 4 was considered to indicate remission. Relapse defined as CAI > 6 and EI > 4. |
|
| Notes | 1 participant randomized to the balsalazide 1.5 g group did not receive any study medication and was excluded from ITT analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy, identical placebos. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Participants were more likely to dropout from the low‐dose balsalazide group (26.5%) due to lack of efficacy than the high‐dose balsalazide (7.5%) or the Salofalk (13.6%) group. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Kruis 2011.
| Study characteristics | ||
| Methods | Randomized, multicenter, double‐blind, double‐dummy, parallel‐group, phase III trial. | |
| Participants | Adults (ages 18–75 years) with endoscopically and histologically confirmed UC (n = 648) in remission (CAI ≤ 4 and EI ≤ 3). | |
| Interventions | 5‐ASA (Salofalk granules) 3.0 g/day dosed OD (n = 217) or 5‐ASA 1.5 g/day dosed OD (n = 212) or 5‐ASA 0.5 g dosed TID (1.5 g/day n = 218) for 1 year. | |
| Outcomes |
Primary outcome: clinical remission at the final visit (relapse was defined as CAI > 4 and increase of ≥ 3 from baseline. Secondary outcomes: clinical remission at month 12 in participants with mucosal inflammation at baseline (EI > 1), endoscopic remission at month 12, change from baseline to month 12 in number of stools and number of bloody stools per week, adherence, and adverse events. |
|
| Notes | 1 participant from the 3.0 g/day OD group was excluded from the ITT analysis for not receiving any study medication. Adherence was calculated by pill count at study visits and by patient diary. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization list. |
| Allocation concealment (selection bias) | Low risk | Randomization was performed centrally in blocks of 3 using a computer‐generated randomization list. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Lichtenstein 2010.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, placebo‐controlled trial. | |
| Participants | Adults (≥ 18 years) with UC (n = 305) in remission (revised SDAI rectal bleeding = 0 and mucosal appearance < 2). Relapse defined as SDAI rectal bleeding score ≥ 1 and a mucosal appearance score ≥ 2, a UC flare, or initiation of medication to treat a UC flare. | |
| Interventions | 5‐ASA granules (Apriso) 1.5 g/day dosed OD (n = 209) or placebo (n = 96) for 6 months. | |
| Outcomes |
Primary outcome: percentage of participants who were relapse free at 6 months. Secondary outcomes: percentages of participants with each level of change from baseline in rectal bleeding score, mucosal appearance score, physician's rating of disease activity; and stool frequency on SDAI at months 1, 3, and 6, and end of treatment; percentage of participants classified as treatment success, relapse‐free duration, and adverse events. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, matching placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Mahmud 2002.
| Study characteristics | ||
| Methods | Single center, randomized, parallel‐group trial. | |
| Participants | Adults (ages ≥ 18–70 years) with confirmed diagnosis of UC in remission (n = 40). | |
| Interventions | Asacol 1.2 g/day (n = 20) or olsalazine 1 g/day (n = 20) for 9 months. | |
| Outcomes | Clinical remission, laboratory assessments, and adverse events. Remission defined as HBI < 3 and a sigmoidoscopy score of 0 to 1. | |
| Notes | Primary objective was to evaluate the effects of 9 months of therapy with Asacol or olsalazine on renal function. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated code. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
McIntyre 1988.
| Study characteristics | ||
| Methods | Randomized, double‐blind trial. Extent of disease was initially classified by most recent barium enema, sigmoidoscopy, and rectal biopsy as: extensive, substantial, left‐sided, proctosigmoiditis, or proctitis. Evaluation continued throughout study at 4, 8, 16, and 24 weeks by clinical exam, sigmoidoscopy, and rectal biopsy (if deterioration occurred). | |
| Participants | Adults (ages 18–79 years) with UC with clinical and sigmoidoscopic (non‐friable mucosa) remission, and who were not currently on maintenance therapy, or who agreed to substitute trial capsules for maintenance SASP (n = 79). | |
| Interventions | Balsalazide 2 g/day (n = 41) or SASP 2 g/day (n = 38) in identical 500 mg capsules, for 6 months. | |
| Outcomes | Relapse defined as the recurrence of previous symptoms. Participants completing 6 months without recurrence were classified as maintaining remission; the rest were considered treatment failures. Exclusions, withdrawals, and occurrence of adverse effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: identical capsules. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Miner 1995.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, placebo‐controlled, parallel‐design trial. Participants stratified according to location of disease. Clinical assessments at entry, 1, 2, 3, 6, 9, and 12 months. At entry and final visit, sigmoidoscopy and histologic assessments performed. Participants kept daily diaries. | |
| Participants | Adults (ages ≥ 18 years), previously diagnosed with UC and in remission. Use of immunosuppressives required 90‐day washout and steroids required 60‐day washout (n = 205). | |
| Interventions | Controlled‐release 5‐ASA (Pentasa) 4 g/day in 250 mg capsules (n = 103) or identical‐appearing placebo (n = 102) for 48 weeks, distributed in blister packaging. Compliance verified by pill count. | |
| Outcomes | Recurrence of disease defined as 1 of the following: sigmoidoscopic index ≥ 5, and ≥ 5 trips to the toilet per day or rectal bleeding for 3 of 7 continuous days; sigmoidoscopic index ≥ 5, with missing data for toilet visits or rectal bleeding; missing data for final sigmoidoscopic index and early termination due to insufficient therapeutic effect. | |
| Notes | Failure rate calculated as "1 – reported remission rate." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Identical placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 34 participants in the placebo group dropped out due to adverse reaction compared to 14 in the 5‐ASA group. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Mulder 1988.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy trial. Evaluation at entry involved clinical, endoscopic, and histologic examinations. Follow‐ups occurred at 3, 6, 9, and 12 months after entry. | |
| Participants | Outpatients (ages ≥ 18 years), with UC in remission for between 1 month and 5 years, who had not taken steroids or azathioprine during the month before entry (n = 78). | |
| Interventions | 5‐ASA (Pentosa) 1.5 g/day as 6 pills + 6 SASP‐matched placebo pills (n = 42) or 6 5‐ASA‐matched placebo pills + SASP 3 g/day as 6 pills (n = 36) for 12 months. Participants were to take medication in 3 doses before or after main meals. Placebo pills matched in appearance, weight, and taste. | |
| Outcomes | Remission rates, adverse effects, and withdrawals. If the data obtained at each exam were assessed as 'normal' or 'in remission', the participant was considered to have remained in remission. If, at any time, the participant had not been considered 'normal' or 'in remission', then the participant was considered to have relapsed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy: placebo pills were identical in appearance, weight, and taste. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 participants dropped out (2 from Pentasa group and 1 from SASP group). |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Nilsson 1995.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind, double‐dummy trial. Clinical assessments performed after every 3 months or more frequently if relapse was suspected. Rigid sigmoidoscopy performed at entry and after 6 and 18 months. | |
| Participants | People with UC in remission, with ≥ 2 episodes of active disease during the last 5 years. No other concomitant medications were permitted (n = 322). | |
| Interventions | Olsalazine 1 g/day + SASP‐matched placebo (n = 161) or SASP 2 g/day + olsalazine‐matched placebo (n = 161) for 6, 9, 12, 15, or 18 months. Participants were instructed to take medication with meals. Full treatment regimen was reached after 7 days. Compliance was verified by pill counts. | |
| Outcomes | Relapse was defined as macroscopic changes in the rectum of grade 3 or 4 on a 4‐point scale. Other measures of efficacy were changes in number of stools per day, blood in stools, and consistency of stools. Failure rates reported on an ITT basis. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy (matched placebos). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Paoluzi 2005.
| Study characteristics | ||
| Methods | Single‐center, randomized, investigator‐blind trial. | |
| Participants | Adults (ages > 18 years) with confirmed UC in clinical, endoscopic, and histologic remission (n = 156). | |
| Interventions | 5‐ASA (Asacol) 2.4 g/day (n = 80) or 5‐ASA 1.2 g/day (n = 76) for 12 months. | |
| Outcomes |
Primary outcome: maintenance of remission (Truelove and Witts). Secondary outcomes: time to relapse, adverse events. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Investigator‐blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Park 2019.
| Study characteristics | ||
| Methods | Prospective, multicenter, randomized trial. | |
| Participants | Adults with UC that extended beyond the sigmoid colon and who had been maintaining their remission (partial Mayo score of ≤ 2) by taking 5‐ASA compounds for ≥ 3 months (n = 180). | |
| Interventions | 5‐ASA (Asacol) 2.4 g OD (n = 91) or 5‐ASA divided daily dose of 800 mg TID or 5‐ASA 1200 mg BID (n = 89). | |
| Outcomes |
Primary outcome: adherence rate to 5‐ASA during 12‐month of follow‐up. Secondary outcomes: relapse rate (a partial Mayo score > 3), treatment satisfaction, adverse events rate, laboratory markers change during the follow‐up period. |
|
| Notes | Adherence monitored by pill count and self‐report. Adherence by pill count was reported in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants randomized in a 1:1 ratio via computerized randomization. |
| Allocation concealment (selection bias) | Low risk | Registration center allocated study drugs randomly to eligible participants. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Pica 2012.
| Study characteristics | ||
| Methods | Randomized open‐label trial. | |
| Participants | People with UC in remission (n = 112). | |
| Interventions | 5‐ASA (Asacol) 4.8 g/day (n = 56) or 5‐ASA 2.4 g/day (n = 56) for 12 months. | |
| Outcomes | Remission at 12 months. | |
| Notes | Abstract publication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open label. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts and reasons for withdrawal were not described. |
| Selective reporting (reporting bias) | Unclear risk | Secondary outcomes were not described. |
| Other bias | Unclear risk | Abstract publication. |
Prantera 2009.
| Study characteristics | ||
| Methods | Double‐blind, double‐dummy, parallel‐group, randomized trial. | |
| Participants | Adults (ages 18–75 years) in remission (modified UC‐DAI score ≤ 1 supported by a rectal sigmoidoscopy in preceding 3 months or colonoscopy in preceding 6 months) for ≥ 1 month prior to entry and had experienced ≥ 1 clinical or endoscopic relapse within the previous 12 months were recruited from centers in Italy, Poland, and Ukraine (n = 331). | |
| Interventions | MMX 5‐ASA (Asacol) 2.4 g/day (n = 162) OD or 5‐ASA 2.4 g/day (n = 169) in 2 divided doses of 1.2 g for 12 months. | |
| Outcomes |
Primary outcome: clinical remission and the proportion of participants in clinical and endoscopic remission at 12 months. Secondary outcomes: time to relapse (UC‐DAI > 1) and assessment of the safety and tolerability of MMX mesalazine 2.4 g/day. Participants assessed at screening, entry, and at 3, 6, 9, and 12 months (or early withdrawal). |
|
| Notes | Adherence checked by pill counts at each visit. Adherence defined as taking ≥ 80% of study medication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Centralized randomization. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Rijk 1992.
| Study characteristics | ||
| Methods | Multicenter, randomized, double‐blind comparison of SASP and olsalazine. Randomization used a standard variance allocation method to ensure equal distribution of prognostic factors among both treatments. In addition to patient diaries, clinical exam, blood counts, and urinalysis were performed after 4, 12, 24, 36, and 48 weeks. Sigmoidoscopy and biopsy performed at entry and 48 weeks to verify remission. | |
| Participants | People with UC in remission for ≤ 2 years, and with active colitis in the past (confirmed by endoscopy/biopsies) recruited between December 1985 and January 1989. Remission defined as absence of clinical signs of inflammation (≤ 3 stools/day) and a normal mucosa on sigmoidoscopic assessment. Some participants had taken part in a trial comparing olsalazine and SASP in active UC and had achieved remission after 6–12 weeks of treatment (n = 46). | |
| Interventions | SASP 4 g/day (n = 23) or olsalazine 2 g/day (n = 23), for 48 weeks, full dosage reached by the 5th day. Dose reduction to SASP 3 g and olsalazine 1.5 g allowed in case of adverse effects. Drugs were given in physically indistinguishable capsules in sealed plastic containers. | |
| Outcomes | Relapse defined as a recurrence of symptoms (blood in stools, with or without diarrhea) and signs of inflammation at endoscopy, even without the presence of participant complaints. Adverse effects and withdrawals. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Centralized randomization. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: SASP and olsalazine were given in externally indistinguishable capsules. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 8 participants dropped out from the olsalazine group (3 due to diarrhea) compared to 4 in the SASP group. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Riley 1988.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy, parallel group trial. Randomization governed by a centrally held pharmacy code and medication was prepackaged and equally and randomly allocated to each center. In addition to daily diary records, participants were evaluated at entry and at 4, 12, 24, 36, and 48 weeks for clinical exam, urine specimen, and blood tests. At entry and at completion (or relapse), sigmoidoscopy and biopsy were performed. | |
| Participants | Adult outpatients with chronic UC in clinical remission for ≥ 1 month before entry, recruited from 3 hospitals in close geographic proximity. All had appearance of normal mucosa or only erythema upon entry. All had previously taken SASP maintenance therapy (n = 100). | |
| Interventions | SASP minimum 2 g/day + 5‐ASA‐matched placebo (n = 50) or 5‐ASA minimum 0.8 g/day + SASP‐matched placebo (n = 50) for 48 weeks. Compliance was verified by pill counts. | |
| Outcomes | Relapse indicated by symptomatic disease recurrence. Confirmation of worsened appearance of rectal mucosa verified by sigmoidoscopy. Withdrawals and adverse effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Randomization was governed by a centrally held pharmacy code. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy (matched placebo). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12% of the SASP group withdrew (n = 6) compared to 4% of the 5‐ASA group (n = 2). |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Rutgeerts 1989.
| Study characteristics | ||
| Methods | Randomized, double‐blind, double‐dummy trial. Clinical exam, including blood work and urinalysis performed at entry, and 1, 2, 3, 6, 9, and 12 months (or earlier for relapse). Colonoscopy performed if symptoms recurred. | |
| Participants | Adults with inactive UC controlled (score ≤ 4 on a standard index) for 1 month pretrial on a stable SASP dose of 1.5–2 g/day (n = 334). | |
| Interventions | SASP 1.5–2 g/day (n = 167) or coated 5‐ASA (Claversal) 0.75 g/day (n = 167), dispensed according to a double‐dummy protocol for 12 months. | |
| Outcomes | Relapse defined as a clinical index of ≥ 6. Withdrawals and adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Drug supplies were labeled and randomized in blocks according to a predetermined computer‐generated list. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 60 participants in the 5‐ASA group did not complete the study compared to 41 participants in SASP group. Reasons for withdrawal not adequately described. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Sandberg‐Gertzen 1986.
| Study characteristics | ||
| Methods | Randomized, double‐blind, placebo‐controlled trial. Participants evaluated (clinically, sigmoidoscopically, and histologically) upon entry and completion, plus by regular telephone contact. | |
| Participants | People, of any age, with UC who, after 6 months of olsalazine (Dipentum) therapy, were in remission (n = 102). | |
| Interventions | Azodisal sodium (olsalazine, Dipentum), 1 g/day (n = 52), or identical‐appearing placebo (riboflavin 16 mg; n = 49) for 6 months. Compliance tested by urine and serum analyses and pill count. | |
| Outcomes | Relapse defined as the occurrence of diarrhea with macroscopic blood, together with the finding of active inflammation on sigmoidoscopy. | |
| Notes | 1 placebo participant was excluded from the ITT analysis for entry criteria violation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: identical placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No dropouts reported. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Sandborn 2010.
| Study characteristics | ||
| Methods | 12‐month, multicenter, investigator‐blinded, randomized, non‐inferiority trial of the maintenance of clinical remission in people with mild‐to‐moderate UC. | |
| Participants | Adults (ages ≥ 18 years) with quiescent UC (Simple Clinical Colitis Activity Index ≤ 2) of ≥ 3 months' duration on a stable dose of Asacol 1.6–2.4 g/day were recruited from 193 sites in the USA, Puerto Rico, and Canada for the study (n = 1023). Participants must have experienced ≥ 1 flare of UC within 18 months of entry (n = 1023). | |
| Interventions | 5‐ASA (Asacol) 1.6–2.4 g/day OD (n = 512) or 5‐ASA BID (n = 511) for 12 months. | |
| Outcomes |
Primary outcome: maintenance of remission at 6 months (SSCAI ≥ 5 defined relapse). Secondary outcomes: participant‐defined remission index, adherence (Medication Adherence Rating scale), participant satisfaction and preference with dosing regimen, serious adverse events, adverse events leading to withdrawal. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Randomization performed centrally via an interactive voice response system. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Investigator‐blinded, blinded investigator assessed outcome. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Suzuki 2017.
| Study characteristics | ||
| Methods | Phase III, multicenter, randomized, double‐blind, parallel‐group non‐inferiority trial. | |
| Participants | Participants (ages 16–65 years) at the time of informed consent with UC in remission (bloody stool score 0, and UC‐DAI ≤ 2) (n = 602). | |
| Interventions | 5‐ASA 2.4 g (Asacol 400 mg pill) OD (n = 301) or TID (n = 301) for 48 weeks. | |
| Outcomes | Primary outcome: non‐recurrence rate. Recurrence defined as a bloody stool score > 1 and UC‐DAI > 3. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation manager (who was independent of the study) prepared a study drug allocation table and randomized study drugs. |
| Allocation concealment (selection bias) | Low risk | The allocation manager sealed the study drug allocation table and stored it under strict control until end of trial. The registration center allocated the study drug randomly to the eligible participants. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind trial. The participants, investigators, subinvestigators, staff of the study site, Zeria Pharmaceutical Co, and Kyowa Hakko Kirin Co were blinded to the treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Travis 1994.
| Study characteristics | ||
| Methods | 2‐center, randomized, parallel group dose‐ranging trial. | |
| Participants | Adults with UC in remission (n = 198) for ≥ 3 months. Remission defined as no clinical symptoms of active disease and no signs of active inflammation on sigmoidoscopy (grade 0 or 1: normal or pink mucosa of quiescent colitis without visible vessels). | |
| Interventions | Olsalazine 0.5 g/day (n = 67) or olsalazine 1.0 g/day (n = 65) or olsalazine 2.0 g/day (n = 62) for 12 months. | |
| Outcomes |
Primary outcome: relapse defined as an increase in bowel frequency with blood or mucus and evidence of active disease on sigmoidoscopy. Secondary outcomes: time in remission from start of treatment, laboratory measurements, and adverse events. |
|
| Notes | 4 participants did not receive any study drugs and were excluded from the ITT analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: participants in the lower‐dose group received a physically indistinguishable placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 19% of the 0.5 g/day group withdrew before the end of the study compared to 14% of the 1.0 g/day group and 24% of the 2.0 g/day group. Reasons for withdrawal described but were not attributed to individual treatment groups. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes are reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Watanabe 2013.
| Study characteristics | ||
| Methods | Phase III, double‐blind, double‐dummy, randomized, multicenter non‐inferiority study. Participants assessed at entry and once every 4 weeks until week 52. |
|
| Participants | Participants (ages 15–64 years) with documented diagnosis of UC. All participants were in remission (defined as UC‐DAI score ≤ 2 and rectal bleeding score 0) at study entry, had experienced clinical relapse during the previous year, and were receiving 5‐ASA ≤ 2.25 g/day or salazosulfapyridine 4.5 g/day as maintenance therapy (n = 301). | |
| Interventions | Prolonged‐release oral 5‐ASA (Pentasa; Kyorin Pharmaceutical Co., Ltd., Tokyo, Japan) 1.5–2.25 g/day OD (n = 152) or 5‐ASA TID (n = 149) for 52 weeks. | |
| Outcomes |
Primary outcome: remission at 52 weeks. Secondary outcomes: duration of remission, UC‐DAI at final assessment, adherence, and adverse events. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind, double‐dummy design. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts balanced across groups with similar reasons for withdrawal. |
| Selective reporting (reporting bias) | Unclear risk | Most expected outcomes reported. 12 serious adverse events reported and a causal relationship with the study drug was ruled out; however, the authors did not report to which group these participants belonged. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
Wright 1993.
| Study characteristics | ||
| Methods | Randomized, double‐blind, placebo‐controlled trial. Participants assessed at entry, after 3 weeks, and after 3, 6, 9, and 12 months. Sigmoidoscopy performed at each visit. Biopsy taken at entry, and 6 and 12 months. | |
| Participants | Participants (ages 18–75 years) with inactive UC who were asymptomatic for ≥ 1 week and < 1 month prior to entry (n = 101). Steroid or SASP therapy was stopped ≥ 1 week prior to entry. | |
| Interventions | Olsalazine 2 g/day (500 mg capsules 4 times per day; n = 49) or matching placebo (n = 52) for 1 year. | |
| Outcomes | Clinical relapse defined as a relapse of diarrhea (with or without blood and mucous) thought by the attending physician to warrant introduction of rectal or oral corticosteroids. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Low risk | Adequate. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind: matching placebo. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 participants from the placebo group did not complete the study (1 lost to follow‐up, 1 lost to compliance, 1 initial protocol exclusion). |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Other bias | Low risk | Study appeared free of other sources of bias. |
5‐ASA: 5‐aminosalicylic acid; BID: twice daily; CAI: Clinical Activity Index; EI: Endoscopic Index; GCP: good clinical practice; HBI: Harvey Bradshaw Index; ITT: intention‐to‐treat; MMX: Multi Matrix System; n: number of participants; OD: once daily; PGA: physician global assessment; SASP: sulfasalazine; SDAI: Sutherland Disease Activity Index; TID: three times daily; UC: ulcerative colitis; UC‐DAI: Ulcerative Colitis Disease Activity Index; VAS: Visual Analog Scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andreoli 1994 | Trial compared 5‐ASA enema to sulfasalazine. |
| Bardazzi 1994 | Trial compared intermittent dosing of 5‐ASA (2.4 g/day for first week of the month) with continuous dosing of 5‐ASA (1.6 g/day) for maintenance treatment. |
| d'Albasio 1997 | Trial compared the combination of oral 5‐ASA and 5‐ASA enemas with oral 5‐ASA alone. |
| D'Haens 2017 | Open‐label extension study. |
| Dew 1982b | Treatment duration < 6 months (16 weeks). |
| Dignass 2009b | No control group – dosing study. |
| Dignass 2018 | Not a maintenance study. |
| Eliakim 1990 | Single‐center report of patients who were abstracted from a larger multicenter trial (Rutgeerts 1989). |
| Ewe 1996 | Treatment duration < 6 months (10 days). |
| Fernández‐Bañares 1999 | Trial compared oral 5‐ASA to Plantago ovata seeds. |
| Frieri 2005 | Not a randomized controlled trial. |
| Giaffer 1992b | Treatment duration < 6 months (3 months). |
| Gillespie 2014 | Dosing study, no control group. |
| Gionchetti 1990 | Treatment duration < 6 months. |
| Gionchetti 1996 | Treatment duration < 6 months (2 weeks). |
| Green 2004 | Not a randomized controlled trial. No comparison group. |
| Hanauer 2009 | Not a randomized controlled trial – open‐label extension study. |
| Karamanolis 1996 | Treatment duration < 6 months (2 weeks). |
| Kruis 1997 | Trial compared oral 5‐ASA (Salofalk) to probiotic (Escherichia coli Nissle 1917). |
| Kruis 2004 | Trial compared oral 5‐ASA to probiotic (Escherichia coli Nissle 1917). |
| Levine 2017 | Pediatric study. |
| Mani 1994 | Treatment duration < 6 months (4 weeks). |
| Mantzaris 2004 | Trial compared azathioprine monotherapy to combination of azathioprine and olsalazine for maintenance of remission in people with steroid‐dependent ulcerative colitis. |
| Odes 1997 | Not a randomized controlled trial. |
| Osterman 2014 | Treatment duration < 6 months (6 weeks). |
| Paoluzi 2002 | Trial compared 4 weeks of combined oral and topical 5‐ASA vs 8 weeks of combined oral and topical 5‐ASA. |
| Papatheodoridis 1995 | Treatment duration < 6 months (14 days). |
| Pelech 1998 | Compared oral 5‐ASA to probiotic (Escherichia coli Nissle 1917). |
| Pica 2015 | Dosing study, no control group. |
| Rubin 2017 | Compared once‐daily budesonide to placebo in people who were refractory to 5‐ASA treatment. |
| Scherl 2013 | Dosing study, no control group. |
| Staerk Laursen 1990 | Treatment duration < 6 months (28 days). |
| Stoa‐Birketvedt 1999 | Treatment duration < 6 months (14 days). |
| Sun 2016 | Compared 5‐ASA modified‐release pills to enteric‐coated pills. No control group. |
| Tragnone 1996 | Compared 5‐ASA 800 mg pills (total dose 1.6 g/day) with 5‐ASA 400 mg pills (total dose 1.6 g/day). Treatment duration < 6 months (3 months). |
| Turner 2017 | Pediatric study. |
| Tzivras 1997 | Treatment duration < 6 months (14 days). |
| Yokoyama 2007 | Trial compared oral 5‐ASA with 5‐ASA enemas. |
| Zocco 2006 | Trial compared oral 5‐ASA to probiotic (Lactobacillus GG) to combination of oral 5‐ASA + probiotic. |
5‐ASA: 5‐aminosalicylic acid.
Characteristics of ongoing studies [ordered by study ID]
NCT02280629.
| Study name | Phosphatidylcholine (LT‐02) vs. placebo vs. mesalamine [5‐ASA] for maintenance of remission in ulcerative colitis (PROTECT‐2) |
| Methods | Interventional, phase III study Allocation: randomized Intervention model: parallel assignment Blinding: double‐blind (participant, care provider, investigator, outcomes assessor) Primary purpose: treatment |
| Participants | Inclusion criteria: men or women, ages 18–70 years; historically confirmed diagnosis of ulcerative colitis by endoscopy and histology; participants being in clinical and endoscopic remission at baseline; negative pregnancy test in women of childbearing potential at baseline visit. |
| Interventions | Phosphatidylcholine vs placebo vs 5‐ASA |
| Outcomes |
Primary outcome: percentage of participants who are relapse‐free and are not a treatment failure at 48 weeks Secondary outcome: mean change from baseline in the total modified Disease Activity Index at 48 weeks |
| Starting date | October 2014 |
| Contact information | Contact: Heidrun Heinemann; heidrun.heinemann@drfalkpharma.de Ronald Greinwald; roland.greinwald@drfalkpharma.de |
| Notes | Study completion date October 2018. |
NCT02522780.
| Study name | Mesalamine [5‐ASA] 2 g sachet for the maintenance of clinical and endoscopic remission in ulcerative colitis (UC) |
| Methods | Interventional, phase III study Allocation: randomized Intervention model: parallel assignment Blinding: participant, care provider, investigator, outcomes assessor Primary purpose: treatment |
| Participants | Inclusion criteria: men or women (ages 18–75 years) with ulcerative colitis in remission. |
| Interventions | 5‐ASA vs placebo |
| Outcomes |
Primary outcome: proportion of participants in remission at month 6 defined by the clinical and endoscopic response score based on a modified 9‐point Mayo score Secondary outcomes: proportion of participants in clinical remission, time to relapse, severity of adverse events, and incidence of adverse events, all at month 6 |
| Starting date | February 2016 |
| Contact information | Clinician development support DK0‐Disclosure@ferring.com |
| Notes | Study completion date September 2018. |
Differences between protocol and review
We added serious adverse events as a secondary outcome for this updated review.
Contributions of authors
AM was involved in the search and selection of studies for inclusion in the review, collection of data for the review, assessment of the risk of bias, analysis of data, interpretation of data, and writing the review.
TMN was involved in the co‐ordination of the review, search and selection of studies for inclusion in the review, collection of data for the review, assessment of the certainty in the body of evidence, analysis of data, interpretation of data, and writing the review.
CEP was involved in the design of the review and interpretation of data.
JKM was involved in assessment of the certainty in the body of evidence, interpretation of data, and writing the review.
BGF was involved in the conception of the review, design of the review, and interpretation of data.
Sources of support
Internal sources
-
University of Calgary, Calgary, Alberta, Canada
The University of Calgary provided support for the original version of this review which was published in 1997. The current version of the review was not supported by any internal sources.
External sources
-
Searle Mucosal Defense Unit, Oakville, Ontario, Canada
Searle provided support for the original version of this review which was published in 1997. The current version of the review was not supported by any external sources.
Declarations of interest
AM: none.
TMN: none.
CEP: none.
JKM: none.
BGF has received fees from Abbott/AbbVie, Amgen, Astra Zeneca, Avaxia Biologics Inc., Bristol‐Myers Squibb, Celgene, Centocor Inc., Elan/Biogen, Ferring, JnJ/Janssen, Merck, Nestles, Novartis, Novonordisk, Pfizer, Prometheus Laboratories, Protagonist, Salix Pharma, Takeda, Teva, TiGenix, Tillotts Pharma AG and UCB Pharma for Scientific Advisory Board membership; fees from Abbott/AbbVie, Actogenix, Akros, Albireo Pharma, Amgen, Astra Zeneca, Avaxia Biologics Inc., Avir Pharma, Axcan, Baxter Healthcare Corp., Biogen Idec, Boehringer‐Ingelheim, Bristol‐Myers Squibb, Calypso Biotech, Celgene, Elan/Biogen, EnGene, Ferring Pharma, Roche/Genentech, GiCare Pharma, Gilead, Given Imaging Inc., GSK, Ironwood Pharma, Janssen Biotech (Centocor), JnJ/Janssen, Kyowa Kakko Kirin Co Ltd., Lexicon, Lilly, Lycera BioTech, Merck, Mesoblast Pharma, Millennium, Nektar, Nestles, Novonordisk, Pfizer, Prometheus Therapeutics and Diagnostics, Protagonist, Receptos, Salix Pharma, Serono, Shire, Sigmoid Pharma, Synergy Pharma Inc., Takeda, Teva Pharma, TiGenix, Tillotts, UCB Pharma, Vertex Pharma, VHsquared Ltd., Warner‐Chilcott, Wyeth, Zealand, and Zyngenia for consultancy; payment for lectures from Abbott/AbbVie, JnJ/Janssen, Takeda, Warner‐Chilcott, UCB Pharma; his institution has received grants/grants pending from Abbott/AbbVie, Amgen, Astra Zeneca, Bristol‐Myers Squibb (BMS), Janssen Biotech (Centocor), JnJ/Janssen, Roche/Genentech, Millennium, Pfizer, Receptos, Santarus, Sanofi, Tillotts, and UCB Pharma.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Andreoli 1987 {published data only}
- Andreoli A, Cosintino R, Trotti R, Berri F, Prantera C. 5-aminosalicylic acid (5-ASA) versus salazopirin (SASP) in the oral treatment of active ulcerative colitis (UC) and in remission. Clinical Controversies in Inflammatory Bowel Disease 1987:170. [Google Scholar]
Ardizzone 1995 {published data only}
- Ardizzone S, Petrillo M, Molteni P, Desideri S, Bianchi Porro G. Coated oral 50 aminosalicylic acid (Claversal) is equivalent to sulfasalazine for remission maintenance in ulcerative colitis. Journal of Clinical Gastroenterology 1995;21:287-9. [DOI] [PubMed] [Google Scholar]
- Bianchi Porro GB, Ardizzone S, Fasoli R, Petrillo M, Desideri S. Comparison of mesalazine with sulphasalazine in prophylactic treatment of ulcerative colitis. Gut 1989;30:A1467. [Google Scholar]
Ardizzone 1999 {published data only}
- Ardizzone S, Petrillo M, Imbesi V, Cerutti R, Bollani S, Bianchi Porro G. Is maintenance therapy always necessary for patients with ulcerative colitis? Alimentary Pharmacology and Therapeutics 1999;13:373-9. [DOI] [PubMed] [Google Scholar]
Courtney 1992 {published data only}
- Courtney MG, Nunes DP, Bergin CF, O'Driscoll M, Trimble V, Keeling PW, et al. Randomised comparison of olsalazine and mesalazine in prevention of relapses in ulcerative colitis. Lancet 1992;339:1279-81. [DOI] [PubMed] [Google Scholar]
- Courtney MG, Nunes DP, Bergin CF. Prospective randomized trial of mesalazine versus olsalazine in ulcerative colitis. Gastroenterology 1990;98(5 Part 2):A165. [Google Scholar]
D'Haens 2012 {published data only}
- D'Haens G, Sandborn WJ, Barrett K, Hodgson I, Streck P. Once-daily MMX® mesalamine for endoscopic maintenance of remission of ulcerative colitis. American Journal of Gastroenterology 2012;107(7):1064-77. [DOI] [PubMed] [Google Scholar]
Deventer 2001 {published data only}
- Deventer SJ, Hommes DW, Roskam-Mul MD, Dekker W, Gasthuis K, Wetzels A, et al. Prospective randomized open label blinded endpoint (PROBE) trial of high versus low dose mesalazine for prevention of relapse in patients with UC in remission. Gastroenterology 2001;120(5 Suppl 1):A454. [Google Scholar]
Dew 1983 {published data only}
- Dew MJ, Harries AD, Evans N, Evans BK, Rhodes J. Maintenance of remission in ulcerative colitis with 5-aminosalicylic acid in high doses by mouth. British Medical Journal 1983;287:23-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dew MJ, Harries AD, Evans N, Evans BK, Rhodes J. Maintenance of remission in ulcerative colitis with an oral preparation of 5-aminosalicylic acid in high doses. Gut 1983;24(Suppl 10):A983. [Google Scholar]
Dignass 2009a {published data only}
- Bokemeyer B, Hommes D, Gill I, Broberg P, Dignass A. Mesalazine in left-sided ulcerative colitis: efficacy analyses from the PODIUM trial on maintenance of remission and mucosal healing. Journal of Crohn's and Colitis 2012;6(4):476-82. [DOI] [PubMed] [Google Scholar]
- Dignass A, Bokemeyer B, Mross M, Oudkerk Pool M. Symptom resolution and clinical remission in patients with mild-to-moderate ulcerative colitis: analysis of the PODIUM trial. Journal of Crohn's and Colitis 2013;7:S153-4. [Google Scholar]
- Dignass A, Bokemeyer B, Stijnen T, Klugmann T, Oudkerk M, Veerman H. Impact of once-daily versus twice-daily mesalazine (Pentasa) on relief of rectal bleeding and stool frequency: results from a multinational randomised controlled trial. In: Canadian Journal of Gastroenterology. Vol. 23. 2009.
- Dignass A, Bokemeyer B, Stijnen T, Tan T, Borner N, Oudkerk Pool M, et al. Safety of once-daily vs twice-daily mesalazine (Pentasa) dosing. Results from a 12-month randomised controlled trial in maintenance of remission of ulcerative colitis. Canadian Journal of Gastroenterology 2009;23:S73. [Google Scholar]
- Dignass A, Stijnen T, Mross MR, Vermeire S, Veerman H, Bhatt A. Pentasa (mesalazine) once or twice daily for the management of maintenance of remission of ulcerative colitis: demographic and baseline data of a 12 month single blind randomised controlled trial. Gastroenterology 2007;132(4 Suppl 1):A502-3. [Google Scholar]
- Dignass A, Vermeire S, Adamek H, Befrits R, Bokemeyer B, Börner N, et al. Improved remission rates from once- versus twice-daily mesalazine (Pentasa) granules for the maintenance of remission in ulcerative colitis: results from a multinational randomised controlled trial. In: UEGW – Abstract Database. 2007:OP-G-378.
- Dignass AU, Bokemeyer B, Adamek H, Mross M, Vinter-Jensen L, Börner N, et al. Mesalamine once daily is more effective than twice daily in patients with quiescent ulcerative colitis. Clinical Gastroenterology and Hepatology 2009;7(7):762-9. [DOI] [PubMed] [Google Scholar]
- Dignass AU, Bokemeyer B, Adamek HE, Mross MR, Vinter-Jensen L, Boerner N, et al. Maintenance therapy with once-daily 2 g mesalazine (Pentasa) treatment improves remission rates in subjects with ulcerative colitis compared to twice daily 1 g mesalazine: data from a randomised controlled trial. Gastroenterology 2008;134(4 Suppl 1):A494. [Google Scholar]
- Dignass AU, Bokemeyer B, Adamek HE, Mross MR, Vinter-Jensen L, Boerner N, et al. Treatment acceptability in a randomised controlled trial of once-daily or twice-daily mesalazine (Pentasa) for the maintenance of remission in ulcerative colitis. Gastroenterology 2008;134(4 Suppl 1):A495-6. [Google Scholar]
- Dignass AU, Bokemeyer B, Stijnen T, Veerman H. Impact of once-daily versus twice-daily mesalazine (Pentasa) on relief of rectal bleeding and stool frequency: results from a multinational randomised controlled trial. Gastroenterology 2009;136(5 Suppl 1):A685. [Google Scholar]
- Dignass AU, Muls V, Silvennoinen J, Pool MO, Befrits R, Broberg P, et al. The PODIUM trial of once-daily versus twice-daily mesalazine dosing in ulcerative colitis: maintenance of mucosal healing. Gastroenterology 2010;1:S520. [Google Scholar]
- Vermeire S, Befrits R, Bokemeyer B, Gill I, Hommes DW, Broberg P, et al. Efficacy of once-daily versus twice-daily mesalazine (Pentasa): sub-analysis of the left-sided colitis population in the randomised PODIUM trial. Gastroenterology 2010;1:S522. [Google Scholar]
Fockens 1995 {published data only}
- Fockens P, Mulder CJ, Ferwada J, Tytgat GN, the Dutch Pentasa Study Group. Relapse prevention of ulcerative colitis: double-blind comparison of 1.5 gram versus 3 gram oral mesalazine (Pentasa). Gastroenterology 1993;104:A701. [Google Scholar]
- Fockens P, Mulder CJ, Tytgat GN, Blok P, Ferwerda J, Meuwissen SG, et al. Comparison of the efficacy and safety of 1.5 compared with 3.0 g oral slow-release mesalazine (Pentasa) in the maintenance treatment of ulcerative colitis. Dutch Pentasa Study Group. European Journal of Gastroenterology and Hepatology 1995;7(11):1025-30. [DOI] [PubMed] [Google Scholar]
Giaffer 1992a {published data only}
- Giaffer MH, Holdsworth CD, Lennard-Jones JE, Rodrigues CA, McIntyre PB, Manjunatha S, et al. Improved maintenance of remission in ulcerative colitis by balsalazide 4 g/day compared with 2 g/day. Alimentary Pharmacology and Therapeutics 1992;6:479-85. [DOI] [PubMed] [Google Scholar]
Gordon 2016 {published data only}
- Gordon GL, Zakko S, Murthy U, Sedghi S, Pruitt R, Barrett AC, et al. Once-daily mesalamine formulation for maintenance of remission in ulcerative colitis. Journal of Clinical Gastroenterology 2016;50(4):318-25. [DOI] [PubMed] [Google Scholar]
Green 1992 {published data only}
- Green JR, Swan CH, Rowlinson A, Gibson JA, Brown P, Kerr GD, et al. Short report: comparison of two doses of balsalazide in maintaining ulcerative colitis in remission over 12 months. Alimentary Pharmacology and Therapeutics 1992;6:647-52. [DOI] [PubMed] [Google Scholar]
- Green JR, Swan CH, Rowlinson AE, Gibson JA, Brown P, Kerr GD, et al. A three-year prospective study of the maintenance of remission of ulcerative colitis by a new 5-ASA releasing agent, balsalazide. Gastroenterology 1992;102(4 Part 2):A631. [Google Scholar]
Green 1998 {published data only}
- Green JR, Gibson JA, Kerr GD, Swarbrick ET, Lobo AJ, Holdsworth CD, et al. Maintenance of remission of ulcerative colitis: a comparison between balsalzide 3 g daily and mesalazine 1.2 g daily over 12 months. Alimentary Pharmacology and Therapeutics 1998;12:1207-16. [DOI] [PubMed] [Google Scholar]
Hanauer 1996 {published data only}
- Hanauer S, Powers B, Robinson M, Mayle J, Elson C. Maintenance of remission of ulcerative colitis by mesalamine (Asacol) versus placebo. Gastroenterology 1994;106:A696. [Google Scholar]
- Hanauer SB, Sninsky CA, Robinson M, Powers BJ, McHattie JD, Mayle JE, et al. An oral preparation of mesalamine as long-term maintenance therapy for ulcerative colitis. A randomized, placebo-controlled trial. Annals of Internal Medicine 1996;124:204-11. [DOI] [PubMed] [Google Scholar]
Hawkey 1997 {published data only}
- Hawkey CJ, Dube LM, Rountree LV, Linnen PJ, Lancaster JF, the European Zileuton Study Group for Ulcerative Colitis. A trial of zileuton versus mesalazine or placebo in the maintenance of remission of ulcerative colitis. Gastroenterology 1997;112:718-24. [DOI] [PubMed] [Google Scholar]
Hawthorne 2012 {published data only}
- Hawthorne AB, Stenson R, Gillespie D, Swarbrick ET, Dhar A, Kapur KC, et al. Once daily asacol in maintenance therapy for ulcerative colitis: a one-year singe-blind randomised trial. Gut 2011;60:A37-8. [Google Scholar]
- Hawthorne AB, Stenson R, Gillespie D, Swarbrick ET, Dhar A, Kapur KC, et al. Once daily mesalazine as maintenance therapy for ulcerative colitis (UC): a one-year single-blind randomised trial. Gastroenterology 2011;140(5 Suppl 1):S65. [Google Scholar]
- Hawthorne AB, Stenson R, Gillespie D, Swarbrick ET, Dhar A, Kapur KC, et al. One-year investigator-blind randomized multicenter trial comparing Asacol 2.4 g once daily with 800 mg three times daily for maintenance of remission in ulcerative colitis. Inflammatory Bowel Disease 2012;18(10):1885-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ireland 1988a {published data only}
- Ireland A, Jewell DP. Comparative trial of olsalazine and sulfasalazine for the maintenance treatment of ulcerative colitis (UC). Gastroenterology 1987;92:A1447. [Google Scholar]
- Ireland A, Mason CH, Jewell DP. Controlled trial comparing olsalazine and sulphasalazine for the maintenance treatment of ulcerative colitis. Gut 1988;29:835-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewell DP, Ireland A. Controlled trial comparing olsalazine and sulfasalazine for maintenance treatment of ulcerative colitis. Scandinavian Journal of Gastroenterology. Supplement 1988;148:45-7. [DOI] [PubMed] [Google Scholar]
Ito 2010 {published data only}
- Ito H, Iida M, Matsumoto T, Suzuki Y, Aida Y, Yoshida T, et al. Direct comparison of two different mesalamine formulations for the maintenance of remission in patients with ulcerative colitis: a double-blind, randomized study. Inflammatory Bowel Diseases 2010;16(9):1575-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kamm 2008 {published data only}
- Kamm MA, Colombel J, Kornbluth A, Diebold R, Barrett K, Karlstadt RG, et al. A randomized comparison of once- versus twice-daily MMX® mesalamine for the maintenance of remission in mild-to-moderate ulcerative colitis. Gastroenterology 2007;132(4 Suppl 1):A510. [Google Scholar]
- Kamm MA, Lichtenstein GR, Sandborn WJ, Schreiber S, Lees K, Barrett K, et al. Randomised trial of once- or twice-daily MMX mesalazine for maintenance of remission in ulcerative colitis. Gut 2008;57(7):893-902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamm MA, Schreiber S, Butler T, Barrett K, Stephenson D, Joseph RE. Safety analysis of MMX mesalazine for the maintenance of remission of mild-to-moderate ulcerative colitis: results of 4-month interim data analysis. In: UEGW Abstract Database. 2006:MON-G-230.
- Rubin D, Dubinsky M, Panaccione R, Siegel C, Binion D, Kane S, et al. Ulcerative colitis: patients’ perceptions compared with other chronic diseases. Inflammatory Bowel Diseases 2008;14(S1):S22. [Google Scholar]
- Sandborn W, Kamm M, Lichtenstein G, Barrett K, Joseph R. MMX™ mesalamine for the maintenance of remission in mild-to-moderate ulcerative colitis. Inflammatory Bowel Diseases 2008;14(S1):S24. [DOI] [PubMed] [Google Scholar]
Kane 2003b {published data only}
- Kane S, Huo D, Magnanti K. A pilot feasibility study of once daily versus conventional dosing mesalamine for maintenance of ulcerative colitis. Clinical Gastroenterology and Hepatology 2003;1(3):170-3. [DOI] [PubMed] [Google Scholar]
Kane 2008b {published data only}
- Kane S, Holderman W, Jacques P, Miodek T. Once daily versus conventional dosing of pH-dependent mesalamine long-term to maintain quiescent ulcerative colitis: preliminary results from a randomized trial. Patient Preference and Adherence 2008;2(2):253-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kiilerich 1992 {published data only}
- Kiilerich S, Ladefoged K, Rannem T, Ranlov P. Prophylactic effects of olsalazine (OLZ) versus sulfasalazine (SASP) in 12 months' maintenance treatment of ulcerative colitis. Gastroenterology 1991;100(5 Part 2):A220. [Google Scholar]
- Kiilerich S, Ladefoged K, Rannem T, Ranlov PJ. Prophylactic effects of olsalazine versus sulphasalazine during 12 months maintenance treatment of ulcerative colitis. Danish Olsalazine Study Group. Gut 1992;33:252-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kruis 1995 {published data only}
- Kruis W, Brandes JW, Schreiber S, Theuer D, Krakamp B, Schutz E. Olsalazine versus mesalazine in the treatment of mild to moderate ulcerative colitis. Alimentary Pharmacology & Therapeutics 1998;12(8):707-15. [DOI] [PubMed] [Google Scholar]
- Kruis W, Judmaier G, Kayasseh L, Stole M, Theuer D, Scheurlen C, et al. Double-blind dose-finding study of olsalazine versus sulphasalazine as maintenance therapy for ulcerative colitis. European Journal of Gastroenterology and Hepatology 1995;7:391-6. [PubMed] [Google Scholar]
- Kruis W, Judmaier G, Kayasseh L, Stolte M, Scheurlen C, Hentschel E, et al. Double-blind dose-finding study of olsalazine vs. sulfasalazine for maintenance therapy of ulcerative colitis. Gastroenterology 1992;102:A649. [PubMed] [Google Scholar]
- Kruis W, Stolte M. A double-blind dose finding study of olsalazine for the maintenance treatment of quiescent ulcerative colitis. Gastroenterology 1991;100(5 Part 2):A222. [PubMed] [Google Scholar]
Kruis 2001 {published data only}
- Kruis W, Schreiber S, Theuer D, Brandes JW, Schutz E, Howaldt S, et al. Low dose balsalazide (1.5 g twice daily) and mesalazine (0.5 g three times daily) maintained remission of ulcerative colitis but high dose balsalazide (3.0 g twice daily) was superior in preventing relapses. Gut 2001;49(6):783-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kruis 2011 {published data only}
- Kruis W, Greinwald R, Mueller R. Optimal dosing of mesalamine for maintenance of clinical remission in patients with distal ulcerative colitis and residual endoscopic activity: a subgroup analysis of a double-blind, double-dummy, randomized, controlled, dose-ranging study. Gastroenterology 2013;144(5 Suppl 1):S768. [Google Scholar]
- Kruis W, Jonaitis L, Pokrotnieks J, Acute G, Mikhailova TL, Horynski M, et al. Once Daily 3g mesalamine is the optimal dose for maintaining clinical remission in ulcerative colitis: a double-blind, double-dummy, randomized, controlled, dose-ranging study. Gastroenterology 2008;134(4 Suppl 1):A489. [Google Scholar]
- Kruis W, Jonaitis L, Pokrotnieks J, Mikhailova TL, Horynski M, Bátovský M, et al. Randomised clinical trial: a comparative dose-finding study of three arms of dual release mesalazine for maintaining remission in ulcerative colitis. Alimentary Pharmacology and Therapeutics 2011;33(3):313-22. [DOI] [PubMed] [Google Scholar]
Lichtenstein 2010 {published data only}
- Lichtenstein GR, Gordon GL, Zakko S, Murthy U, Sedghi S, Pruitt R, et al. Clinical trial: once-daily mesalamine granules for maintenance of remission of ulcerative colitis – a 6-month placebo-controlled trial. Alimentary Pharmacology and Therapeutics 2010;32(8):990-9. [DOI] [PubMed] [Google Scholar]
Mahmud 2002 {published data only}
- Mahmud N, O'Toole D, O'Hare N, Freyne PJ, Weir DG, Kelleher D. Evaluation of renal function following treatment with 5-aminosalicylic acid derivatives in patients with ulcerative colitis. Alimentary Pharmacology and Therapeutics 2002;16(2):207-15. [DOI] [PubMed] [Google Scholar]
McIntyre 1988 {published data only}
- McIntyre PB, Rodrigues CA, Lennard-Jones JE, Barrison IG, Walker JG, Baron JH. Double blind controlled comparison of balsalazide and sulphasalazine in maintenance therapy of patients with ulcerative colitis [abstract]. Gut 1986;27:A1271. [DOI] [PubMed] [Google Scholar]
- McIntyre PB, Rodrigues CA, Lennard-Jones JE, Barrison IG, Walker JG, Baton JH, et al. Balsalazine in the maintenance treatment of patients with ulcerative colitis, a double-blind comparison with sulphasalazine. Alimentary Pharmacology and Therapeutics 1988;2:237-43. [DOI] [PubMed] [Google Scholar]
Miner 1995 {published data only}
- Miner P, Hanauer S, Robinson M, Schwartz J, Arora S, Pentasa UC Maintenance Study Group. Safety and efficacy of controlled-release mesalamine for maintenance of remission in ulcerative colitis. Digestive Diseases and Sciences 1995;40:296-304. [DOI] [PubMed] [Google Scholar]
- Miner P, Schwartz J, Aora S, Robinson M, Hanauer S, the Pentasa Study Group. Maintenance of remission in ulcerative colitis (UC) patients with controlled-release mesalamine capsules (Pentasa). Gastroenterology 1992;102:A666. [Google Scholar]
Mulder 1988 {published data only}
- Mulder CJ, Tytgat GN, Weterman IT, Dekker W, Blok P, Schrijver M, et al. Double-blind comparison of slow-release 5-aminosalicylate and sulfasalazine in remission maintenance in ulcerative colitis. Gastroenterology 1988;95:1449-53. [DOI] [PubMed] [Google Scholar]
- Mulder CJ, Tytgat GN, Weterman IT. Double blind evaluation of slow-release 5-aminosalicylic acid (Pentasa) and salazopyridin (Salazopyrin) in the maintenance therapy of ulcerative colitis. Gastroenterology 1988;94(5 Part 2):A313. [Google Scholar]
Nilsson 1995 {published data only}
- Nilsson A, Danielsson A, Lofberg R, Benno P, Bergman L, Fausa O, et al. Olsalazine versus sulphasalazine for relapse prevention in ulcerative colitis: a multicenter study. American Journal of Gastroenterology 1995;90:381-7. [PubMed] [Google Scholar]
Paoluzi 2005 {published data only}
- Paoluzi OA, Iacopini F, Pica R, Crispino P, Marcheggiano A, Consolazio A, et al. Comparison of two different daily dosages (2.4 vs. 1.2 g) of oral mesalazine in maintenance of remission in ulcerative colitis patients: 1-year follow-up study. Alimentary Pharmacology and Therapeutics 2005;21(9):1111-9. [DOI] [PubMed] [Google Scholar]
- Paoluzi OA, Pica R, Crispino P, Iacopini F, Consolazio A, Rivera M, et al. Doubling daily dosage of oral mesalazine (2.4 vs. 1.2 g) in the maintenance therapy of pts with ulcerative colitis delays but does not reduce incidence of relapses: a 1-year follow-up study. Gastroenterology 2005;128(4 Suppl 2):A585. [Google Scholar]
Park 2019 {published data only}
- Park SK, Eun CS, Seo GS, Lim J, Kim TO, Park DI. The effects and adherence of Asacol comparing 2.4 g once daily with 800 mg three times or 1200 mg twice daily for maintain therapy in the ulcerative colitis: prospective multicentre randomised study. Journal of Crohn's & Colitis 2018;12(Suppl 1):S367. [Google Scholar]
- Park SK, Park SH, Eun CS, Seo GS, Im JP, Kim TO, et al. Adherence to Asacol once daily versus divided regimen for maintenance therapy in ulcerative colitis: a prospective, multicenter, randomized study. Intestinal Research 2019;17(3):349-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pica 2012 {published data only}
- Pica R, Cassieri C, Cocco A, Marcheggiano A, Occhigrossi G, Zippi M, et al. Randomised open label trial comparing two different dosages of oral mesalazine in the maintenance treatment of ulcerative colitis. Italian Journal of Medicine 2012;1:108. [Google Scholar]
Prantera 2009 {published data only}
- Kohn A, Prantera C, Caprilli R, Campieri M, Cottone M, Pallone F, et al. Maintenance treatment of ulcerative colitis with 5-aminosalicylic acid (5-ASA): results from the Italian population of a one year, randomized, multinational study comparing MMx® with Asacol®. Gastroenterology 2009;136(5 Suppl 1):390. [Google Scholar]
- Prantera C, Kohn A, Campieri M, Caprilli R, Cottone M, Pallone F, et al. Clinical trial: ulcerative colitis maintenance treatment with 5-ASA: a 1-year, randomized multicentre study comparing MMX with Asacol. Alimentary Pharmacology and Therapeutics 2009;30(9):908-18. [DOI] [PubMed] [Google Scholar]
Rijk 1992 {published data only}
- Rijk MC, Lier HJ, Tongerson JH. Relapse-preventing effect and safety of sulfasalazine and olsalazine in patients with ulcerative colitis in remission: prospective, double-blind, randomized multicenter study. American Journal of Gastroenterology 1992;87:438-42. [PubMed] [Google Scholar]
- Rijk MC, Tongersen JH. The relapse preventing effect and safety of sulphasalazine and olsalazine in patients with ulcerative colitis in remission. Gastroenterology 1991;100(5 Part 2):A243. [Google Scholar]
Riley 1988 {published data only}
- Riley SA, Mani V, Goodman MJ, Herd ME, Dutt S, Turnberg LA. Comparison of delayed release 5 aminosalicylic acid (mesalazine) and sulfasalazine as maintenance treatment of patients with ulcerative colitis. Gastroenterology 2012;29(5):669-74. [DOI] [PubMed] [Google Scholar]
- Riley SA, Mani V, Goodman MJ, Herd ME, Dutt S, Turnberg LA. Comparison of delayed-release 5-aminosalicylic acid (mesalazine) and sulfasalazine as maintenance treatment for patients with ulcerative colitis. Gastroenterology 1988;94:1383-9. [DOI] [PubMed] [Google Scholar]
- Riley SA, Mani V, Goodman MJ, Turnberg LA. A comparison of delayed-release 5-ASA and sulfasalazine as maintenance treatment in ulcerative colitis. Gastroenterology 1987;92:A1596. [DOI] [PubMed] [Google Scholar]
- Riley SA, Mani V, Goodman MJ, Turnberg LA. A comparison of delayed-release 5-aminosalicylic acid (5-ASA) and sulfasalazine (SSZ) as maintenance treatment of ulcerative colitis (UC). Gut 1987;28:1390. [Google Scholar]
Rutgeerts 1989 {published data only}
- Rutgeerts P. Comparative efficacy of coated, oral 5-aminosalicylic acid (Claversal) and sulphasalazine for maintaining remission of ulcerative colitis. Alimentary Pharmacology and Therapeutics 1989;3:183-91. [PubMed] [Google Scholar]
Sandberg‐Gertzen 1986 {published data only}
- Jarnerot G, Sandberg-Gertzen H. Azodisal sodium, (ADS), Dipentum, as relapse prevention in ulcerative colitis (UC). A double-blind placebo controlled study. Gastroenterology 1985;88(5 Part 2):A1432. [Google Scholar]
- Sandberg-Gertzen H, Jarnerot G, Kraaz W. Azodisal sodium in the treatment of ulcerative colitis: a study of tolerance and relapse prevention properties. Gastroenterology 1986;90:1024-30. [DOI] [PubMed] [Google Scholar]
Sandborn 2010 {published data only}
- Sandborn W, Kane S, Korzenik J, Lashner B, Leighton J, Mahadevan U, et al. Once daily dosing of delayed-release oral mesalamine for maintenance of remission of ulcerative colitis (the QDIEM trial): 6 and 12 month results. Inflammatory Bowel Diseases 2009;15:S15. [Google Scholar]
- Sandborn WJ, Korzenik J, Lashner B, Leighton JA, Mahadevan U, Marion JF, et al. Once-daily dosing of delayed-release oral mesalamine (400-mg tablet) is as effective as twice-daily dosing for maintenance of remission of ulcerative colitis. Gastroenterology 2010;138(4):1286-96. [DOI] [PubMed] [Google Scholar]
Suzuki 2017 {published data only}
- Suzuki Y, lida M, Ito H, Nishino H, Ohmori T, Arai T, et al. 2.4g Mesalamine (Asacol 400mg tablet) once daily is as effective as three times daily in maintenance of remission in ulcerative colitis: a randomized, noninferiority, multi-center trial. Inflammatory Bowel Diseases 2017;23(5):822-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Travis 1994 {published data only}
- Travis SP, Tysk C, Silva HJ, Sandberg-Gertzen H, Jewell DP, Jarnerot G. Optimum dose of olsalazine for maintaining remission in ulcerative colitis. Gut 1994;35:1282-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watanabe 2013 {published data only}
- Watanabe M, Hanai H, Nishino H, Yokoyama T, Terada T, Suzuki Y. Comparison of QD and TID oral mesalazine for maintenance of remission in quiescent ulcerative colitis: a double-blind, double-dummy, randomized multicenter study. Inflammatory Bowel Diseases 2013;19(8):1681-90. [DOI] [PubMed] [Google Scholar]
Wright 1993 {published data only}
- Wright JP, O'Keefe EA, Cuming L, Jaskiewicz K. Olsalazine in maintenance of clinical remission in patients with ulcerative colitis. Digestive Diseases and Sciences 1993;38:1837-42. [DOI] [PubMed] [Google Scholar]
- Wright JP, O'Keefe EA, Cuming L, Jaskiewicz K. Olsalazine in the maintenance of remission in patients with ulcerative colitis. Gastroenterology 1992;102:A714. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Andreoli 1994 {published data only}
- Andreoli A, Spinella S, Levenstein S, Prantera C. 5-ASA enema versus oral sulphasalazine in maintaining remission in ulcerative colitis. Italian Journal of Gastroenterology 1994;26(3):121-5. [PubMed] [Google Scholar]
Bardazzi 1994 {published data only}
- Bardazzi G, d'Albasio G, Bonanomi AG, Trallori G, Messori A, Amorosi A, et al. Intermittent versus continuous 5-aminosalicylic acid treatment for maintaining remission in ulcerative colitis. Italian Journal of Gastroenterology 1994;26(7):334-7. [PubMed] [Google Scholar]
d'Albasio 1997 {published data only}
- d'Albasio G, Pacini F, Camarri E, Messori A, Trallori G, Bonanomi AG, et al. Combined therapy with 5-aminosalicylic acid tablets and enemas for maintaining remission in ulcerative colitis: a randomized double-blind study. American Journal of Gastroenterology 1997;92(7):1143-7. [PubMed] [Google Scholar]
D'Haens 2017 {published data only}
- D'Haens GR, Sandborn WJ, Zou G, Stitt LW, Rutgeerts PJ, Gilgen D, et al. Randomised non-inferiority trial: 1600 mg versus 400 mg tablets of mesalazine for the treatment of mild-to-moderate ulcerative colitis. Alimentary Pharmacology & Therapeutics 2017;46(3):292-302. [DOI] [PubMed] [Google Scholar]
Dew 1982b {published data only}
- Dew MJ, Hughes P, Harries AD, Williams G, Evans BK, Rhodes J. Maintenance of remissions in ulcerative colitis with oral preparation of 5-aminosalicylic acid. British Medical Journal 1982;285:1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dignass 2009b {published data only}
- Dignass A, Bokemeyer B, Stijnen T, Tan T, Borner N, Oudkerk Pool M, et al. Safety of once-daily vs twice-daily mesalazine (Pentasa) dosing. Results from a 12-month randomised controlled trial in maintenance of remission of ulcerative colitis. In: Canadian Journal of Gastroenterology. Vol. 23. 2009.
Dignass 2018 {published data only}
- Dignass A, Schnabel R, Romatowski J, Pavlenko V, Dorofeyev A, Derova J. Efficacy and safety of a novel high-dose mesalazine tablet in mild to moderate active ulcerative colitis: a double-blind, multicentre, randomised trial. United European Gastroenterology Journal 2018;6(1):138-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eliakim 1990 {published data only}
- Eliakim R, Wengrower D, Ligumsky M, Rachmilewitz D. Comparable efficacy of oral 5-ASA (Mesasal) and sulfasalazine in maintaining ulcerative colitis in remission. Israel Journal of Medical Sciences 1990;26(1):47-9. [PubMed] [Google Scholar]
Ewe 1996 {published data only}
- Ewe K, Becker K, Ueberschaer B. Systemic uptake of 5-aminosalicylic acid from olsalazine and Eudragit L coated mesalazine in patients with ulcerative colitis in remission. Zeitschrift fur Gastroenterologie 1996;34(4):225-9. [PubMed] [Google Scholar]
Fernández‐Bañares 1999 {published data only}
- Fernández-Bañares F, Hinojosa J, Sánchez-Lombraña JL, Navarro E, Martínez-Salmerón JF, García-Pugés A, et al. Randomized clinical trial of Plantago ovata seeds (dietary fiber) as compared with mesalamine in maintaining remission in ulcerative colitis. American Journal of Gastroenterology 1999;94(2):427-33. [DOI] [PubMed] [Google Scholar]
Frieri 2005 {published data only}
- Frieri G, Pimpo M, Galletti B, Palumbo G, Corrao G, Latella G, et al. Long-term oral plus topical mesalazine in frequently relapsing ulcerative colitis. Digestive and Liver Disease 2005;37(2):92-6. [DOI] [PubMed] [Google Scholar]
Giaffer 1992b {published data only}
- Giaffer MH, O'Brien CJ, Holdsworth CD. Clinical tolerance to three 5-aminosalicylic acid releasing preparations in patients with inflammatory bowel disease intolerant or allergic to sulphasalazine. Alimentary Pharmacology and Therapeutics 1992;6(1):51-9. [DOI] [PubMed] [Google Scholar]
Gillespie 2014 {published data only}
- Gillespie D, Hood K, Farewell D, Stenson R, Probert C, Hawthorne AB. Electronic monitoring of medication adherence in a 1-year clinical study of 2 dosing regimens of mesalazine for adults in remission with ulcerative colitis. Inflammatory Bowel Diseases 2014;20(1):82-91. [DOI] [PubMed] [Google Scholar]
Gionchetti 1990 {published data only}
- Gionchetti P, Campieri M, Belluzzi A, Brignola C, Tampieri M, Iannone P, et al. Pentasa in maintenance treatment of ulcerative colitis. Gastroenterology 1990;98:251. [DOI] [PubMed] [Google Scholar]
Gionchetti 1996 {published data only}
- Gionchetti P, Campieri M, Venturi A, Rizzello F, Ferretti M, Brignola C, et al. Systemic availability of 5-aminosalicylic acid: comparison of delayed release and an azo-bond preparation. Alimentary Pharmacology and Therapeutics 1996;10(4):601-5. [DOI] [PubMed] [Google Scholar]
Green 2004 {published data only}
- Green JR, Swan CH, Gibson JA, Kerr GD, Swarbrick ET, Thornton PC. Patient-led variable dosing with balsalazide as long-term therapy for maintenance in ulcerative colitis: a 3-year prospective observational study. Alimentary Pharmacology and Therapeutics 2004;19(4):435-42. [DOI] [PubMed] [Google Scholar]
Hanauer 2009 {published data only}
- Hanauer SB, Lichtenstein GR, Kamm MA, Sandborn WJ, Lees KH, Barrett K, et al. MMX mesalamine for induction and maintenance therapy in mild-to-moderate ulcerative colitis. Gastroenterology and Hepatology 2009;5(7):494-500. [PMC free article] [PubMed] [Google Scholar]
Karamanolis 1996 {published data only}
- Karamanolis DG, Papatheodoridis GV, Xourgias V. Systemic absorption of 5-aminosalicylic acid in patients with inactive ulcerative colitis treated with olsalazine and mesalazine. European Journal of Gastroenterology and Hepatology 1996;8(11):1083-8. [DOI] [PubMed] [Google Scholar]
Kruis 1997 {published data only}
- Kruis W, Schütz E, Fric P, Fixa B, Judmaier G, Stolte M. Double-blind comparison of an oral Escherichia coli preparation and mesalazine in maintaining remission of ulcerative colitis. Alimentary Pharmacology and Therapeutics 1997;11(5):853-8. [DOI] [PubMed] [Google Scholar]
Kruis 2004 {published data only}
- Kruis W, Fric P, Pokrotnieks J, Lukas M, Fixa B, Kascak M, et al. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 2004;53(11):1617-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levine 2017 {published data only}
- Levine A, Yerushalmi B, Kori M, Broide E, Mozer-Glassberg Y, Shaoul R, et al. Mesalamine enemas for induction of remission in pediatric ulcerative colitis refractory to oral mesalamine: a prospective cohort study. Journal of Crohn's & Colitis 2017;11(Suppl 1):S285. [DOI] [PubMed] [Google Scholar]
- Levine A, Yerushalmi B, Kori M, Broide E, Mozer-Glassberg Y, Shaoul R. Mesalamine enemas for induction of remission in pediatric ulcerative colitis refractory to oral Mesalamine: a prospective cohort study. Journal of Pediatric Gastroenterology and Nutrition 2017;64(Suppl 1):49. [DOI] [PubMed] [Google Scholar]
Mani 1994 {published data only}
- Mani V, Gotch P. Comparison of pharmacokinetics and colonic transit time in quiescent ulcerative colitis on mesalazine and olsalazine – a cross over study. Gut 1994;35(Suppl 4):A124. [Google Scholar]
Mantzaris 2004 {published data only}
- Mantzaris GJ, Sfakianakis M, Archavlis E, Petraki K, Christidou A, Karagiannidis A, et al. A prospective randomized observer-blind 2-year trial of azathioprine monotherapy versus azathioprine and olsalazine for the maintenance of remission of steroid-dependent ulcerative colitis. American Journal of Gastroenterology 2004;99(6):1122-8. [DOI] [PubMed] [Google Scholar]
Odes 1997 {published data only}
- Odes HS. 5-Aminosalicylic acid, 1,000-mg caplets versus 500-mg tablets, in maintenance of remission in ulcerative colitis. Journal of Clinical Gastroenterology 1997;24(4):287-8. [DOI] [PubMed] [Google Scholar]
Osterman 2014 {published data only}
- Osterman MT, Aberra F, Cross R, Liakos S, McCabe RP, Shafran I, et al. A randomized controlled trial of mesalamine dose escalation for ulcerative colitis in remission. Gastroenterology 2014;146(5 Suppl 1):S149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paoluzi 2002 {published data only}
- Paoluzi P, D'Albasio G, Pera A, Bianchi Porro G, Paoluzi OA, Pica R, et al. Oral and topical 5-aminosalicylic acid (mesalazine) in inducing and maintaining remission in mild-moderate relapse of ulcerative colitis: one-year randomised multicentre trial. Digestive and Liver Disease 2002;34(11):787-93. [DOI] [PubMed] [Google Scholar]
Papatheodoridis 1995 {published data only}
- Papatheodoridis GV, Xourgias V, Sdonas T, Triantoafyllou M, Tzouvaia M, Karamanolis DG. Systematic load of 5-ASA in patients with inactive ulcerative colitis treated with olsalazine and mesalazine. Gut 1995;37(Suppl 2 Pt 2):A54. [Google Scholar]
Pelech 1998 {published data only}
- Pelech T, Fric P, Fixa B, Komarkova O. Comparison of Mutaflor and mesalazine in the maintenance treatment of inactive ulcerative colitis. Prakticky Lekar 1998;78(10):556-8. [Google Scholar]
Pica 2015 {published data only}
- Pica R, Cassieri C, Cocco A, Zippi M, Marcheggiano A, De Nitto D, et al. A randomized trial comparing 4.8 vs. 2.4 g/day of oral mesalazine for maintenance of remission in ulcerative colitis. Digestive & Liver Disease 2015;47(11):933-7. [DOI] [PubMed] [Google Scholar]
Rubin 2017 {published data only}
- Rubin DT, Cohen RD, Sandborn WJ, Lichtenstein GR, Axler J, Riddell RH, et al. Budesonide multimatrix is efficacious for mesalamine-refractory, mild to moderate ulcerative colitis: a randomised, placebo-controlled trial. Journal of Crohn's & Colitis 2017;11(7):785-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scherl 2013 {published data only}
- Scherl E, Pruitt R, Sedghi S, Barrett A, Bortey E, Paterson C, et al. Long-term safety and tolerability of twice-daily balsalazide disodium tablets in patients with ulcerative colitis. American Journal of Gastroenterology 2013;108:S545. [Google Scholar]
Staerk Laursen 1990 {published data only}
- Staerk Laursen L, Stokholm M, Bukhave K, Rask-Madsen J, Lauritsen K. Disposition of 5-aminosalicylic acid by olsalazine and three mesalazine preparations in patients with ulcerative colitis: comparison of intraluminal colonic concentrations, serum values, and urinary excretion. Gut 1990;31:1271-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stoa‐Birketvedt 1999 {published data only}
- Florholmen J. The systemic load and efficient delivery of active 5-ASA in patients with ulcerative colitis on treatment with Dipentum (olsalazine) and Mesasael (mesalazine). Gut 1994;35(Suppl 4):A121. [DOI] [PubMed] [Google Scholar]
- Stoa-Birketvedt G, Florholmen J. The systemic load and efficient delivery of active 5-aminosalicylic acid in patients with ulcerative colitis on treatment with olsalazine or mesalazine. Alimentary Pharmacology and Therapeutics 1999;13:357-61. [DOI] [PubMed] [Google Scholar]
Sun 2016 {published data only}
- Sun J, Yuan Y. Mesalazine modified-release tablet in the treatment of ulcerative colitis in the remission phase: a Chinese, multicenter, single-blind, randomized controlled study. Advances in Therapy 2016;33(3):410-22. [DOI] [PubMed] [Google Scholar]
Tragnone 1996 {published data only}
- Tragnone A, Elmi G, Tagliente C, Bazzocchi G, Dina R, Euseb V, et al. Oral 5-aminosalicylic acid therapy for the prevention of relapse in patients with ulcerative colitis (UC) during remission: a new therapeutical approach by using 5-ASA tablets 800 mg. A multicenter controlled randomized trial. Gastroenterology 1996;110:A1030. [Google Scholar]
Turner 2017 {published data only}
- Turner D, Yerushalmi B, Kori M, Broide E, Mozer-Glassberg Y, Shaoul R, et al. Once- versus twice-daily mesalazine to induce remission in paediatric ulcerative colitis: a randomised controlled trial. Journal of Crohn's & Colitis 2017;11(5):527-33. [DOI] [PubMed] [Google Scholar]
Tzivras 1997 {published data only}
- Archimandritis A, Hatzis G, Konstandinidis A, Paraskeva K, Tjivras M, Skandalis N. Disposition of 5-ASA by olsalazine (Dipentum) and mesalazine (Asacol) in patients with ulcerative colitis in remission. Gut 1996;39(Suppl 3):A75. [Google Scholar]
- Tzivras M, Konstandinidis A, Hatzis G, Paraskeva K, Skandalis N, Archimandritis A. Systemic absorption of 5-aminosalicylic acid in patients with inactive ulcerative colitis treated with olsalazine and mesalazine. European Journal of Gastroenterology and Hepatology 1997;9(7):729-30. [DOI] [PubMed] [Google Scholar]
Yokoyama 2007 {published data only}
- Yokoyama H, Takagi S, Kuriyama S, Takahashi S, Takahashi H, Iwabuchi M, et al. Effect of weekend 5-aminosalicylic acid (mesalazine) enema as maintenance therapy for ulcerative colitis: results from a randomized controlled study. Inflammatory Bowel Diseases 2007;13(9):1115-20. [DOI] [PubMed] [Google Scholar]
Zocco 2006 {published data only}
- Zocco MA, Dal Verme LZ, Cremonini F, Piscaglia AC, Nista EC, Candelli M, et al. Efficacy of Lactobacillus GG in maintaining remission of ulcerative colitis. Alimentary Pharmacology and Therapeutics 2006;23:1567-74. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT02280629 {published data only}
- NCT02280629. Phosphatidylcholine (LT-02) vs. placebo vs. mesalamine for maintenance of remission in ulcerative colitis (PROTECT-2) [Randomized, double-blind, double-dummy, placebo-controlled, phase III clinical trial on the efficacy and safety of a 48-weeks treatment with gastro-resistant phosphatidylcholine (LT-02) versus placebo versus mesalamine for maintenance of remission in patients with ulcerative colitis]. clinicaltrials.gov/show/NCT02280629 (first received 31 October 2014).
NCT02522780 {published data only}
- NCT02522780. Mesalamine 2 g Sachet for the maintenance of clinical and endoscopic remission in ulcerative colitis (UC) [A randomized, double-blind, placebo-controlled, multicenter study investigating the efficacy and safety of mesalamine 2 g extended release granules (Sachet) for maintenance of clinical and endoscopic remission in ulcerative colitis]. clinicaltrials.gov/show/NCT02522780 (first received 13 August 2015).
Additional references
Andrade 1995
- Andrade SE, Walker AM, Gottlieb LK, Hollenberg NK, Testa MA, Saperia GM, et al. Discontinuation of antihyperlipidemic drugs – do rates reported in clinical trials reflect rates in primary care settings? New England Journal of Medicine 1995;332(17):1125-31. [DOI] [PubMed] [Google Scholar]
Azad Khan 1977
- Azad Khan AK, Piris J, Truelove SC. An experiment to determine the active therapeutic moiety of sulfasalazine. Lancet 1977;2(8044):892-5. [DOI] [PubMed] [Google Scholar]
Beaulieu 2009
- Beaulieu DB Schwartz DA. Medication persistence in patients with ulcerative colitis: meeting the challenges and improving patient outcomes CME. MedScape CME Gastroenterology Posted 22 December 2009.
Brixner 2007
- Brixner D, Magowan S, Accortt N. Evaluation of prescription refill patterns based on daily dosing regimen and pill load for calcium channel blockers. Academy of Managed Care Pharmacy 19th Annual Meeting; 2007 Apr 10–13; San Diego (CA), 2007.
Chan 1983
- Chan RP, Pope DJ, Gilbert AP, Sacra PJ, Baron JH, Lennard-Jones JE. Studies of two novel sulfasalazine analogs, ipsalazide and balsalazide. Digestive Diseases and Sciences 1983;28:609-15. [DOI] [PubMed] [Google Scholar]
Danese 2011
- Danese S, Fiocchi C. Ulcerative colitis. New England Journal of Medicine 2011;365(18):1713-25. [DOI] [PubMed] [Google Scholar]
Das 1973
- Das KM, Eastwood MA, McManus JP, Sircus W. Adverse reactions during salicylazosulfapyridine therapy and the relation with drug metabolism and acetylator phenotype. New England Journal of Medicine 1973;289:491-5. [DOI] [PubMed] [Google Scholar]
Dew 1982a
- Dew MJ, Hughes PJ, Lee MG, Evans BK, Rhodes J. An oral preparation to release drugs in the human colon. British Journal of Clinical Pharmacology 1982;14:405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ediger 2007
- Ediger JP, Walker JR, Graff L, Lix L, Clara I, Rawsthorne P, et al. Predictors of medication adherence in inflammatory bowel disease. American Journal of Gastroenterology 2007;102(7):1417-26. [DOI] [PubMed] [Google Scholar]
Feuerstein 2014
- Feuerstein JD, Cheifetz AS. Ulcerative colitis. Mayo Clinic Proceedings 2014;89(11):1553-63. [DOI] [PubMed] [Google Scholar]
Fleig 1988
- Fleig WE, Laudage G, Sommer H, Wellmann W, Stange EF, Riemann J. Prospective, randomized, double-blind comparison of benzalazine and sulfasalazine in the treatment of active ulcerative colitis. Digestion 1988;40(3):173-80. [DOI] [PubMed] [Google Scholar]
Ford 2011a
- Ford AC, Achkar JP, Khan KJ, Kane SV, Talley NJ, Marshall JK, et al. Efficacy of 5-aminosalicylates in ulcerative colitis: systematic review and meta-analysis. American Journal of Gastroenterology 2011;106:601-16. [DOI] [PubMed] [Google Scholar]
Ford 2011b
- Ford AC, Khan KJ, Sandborn WJ, Kane SV, Moayyedi P. Once-daily dosing vs. conventional dosing schedule of mesalamine and relapse of quiescent ulcerative colitis: systematic review and meta-analysis. American Journal of Gastroenterology 2011;106:2070-7. [DOI] [PubMed] [Google Scholar]
Greenfield 1993
- Greenfield SM, Punchard NA, Teare JP, Thompson RP. Review article: the mode of action of the aminosalicylates in inflammatory bowel disease. Alimentary Pharmacology and Therapeutics 1993;7:369-83. [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hardy 1987
- Hardy JG, Healey JN, Reynolds JR. Evaluation of an enteric-coated delayed-release 5-aminosalicylic acid tablet in patients with inflammatory bowel disease. Alimentary Pharmacology and Therapeutics 1987;1:273-80. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analysis. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JP, Altman DG, Sterne JA. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JP, Deeks JJ, Altman DG. Chapter 16: Special topics in statistics. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Ireland 1988b
- Ireland A, Jewell DP. Olsalazine in patients intolerant of sulfasalazine. Scandinavian Journal of Gastroenterology 1988;23(Suppl 148):101-3. [DOI] [PubMed] [Google Scholar]
Jarnerot 1996
- Jarnerot G. Withdrawal rates because of diarrhoea in Dipentum-treated patients with ulcerative colitis are low when Dipentum is taken with food and dose titrated [abstract]. Gastroenterology 1996;110:A932. [Google Scholar]
Kane 2001
- Kane SV, Cohen RD, Aikens JE, Hanauer SB. Prevalence of nonadherence with maintenance mesalamine in quiescent ulcerative colitis. American Journal of Gastroenterology 2001;96(10):2929-33. [DOI] [PubMed] [Google Scholar]
Kane 2003a
- Kane S, Huo D, Aikens J, Hanauer S. Medication nonadherence and the outcomes of patients with quiescent ulcerative colitis. American Journal of Medicine 2003;114(1):39-43. [DOI] [PubMed] [Google Scholar]
Kane 2006
- Kane SV. Systematic review: adherence issues in the treatment of ulcerative colitis. Alimentary Pharmacology and Therapeutics 2006;23(5):577-85. [DOI] [PubMed] [Google Scholar]
Kane 2008a
- Kane SV, Brixner D, Rubin DT, Sewitch MJ. The challenge of compliance and persistence: focus on ulcerative colitis. Journal of Managed Care Pharmacy 2008;14(1 Suppl A):S2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kjaergaard 1989
- Kjaergaard N, Ambrosius Christensen L, Lauritsen JG, Rasmussen N, Honore Hansen S. Effects of mesalazine substitution on salicylazosulfapyridine-induced seminal abnormalities in men with ulcerative colitis. Scandinavian Journal of Gastroenterology 1989;24:891-6. [DOI] [PubMed] [Google Scholar]
Klotz 1980
- Klotz U, Maier K, Fischer C, Heinkel K. Therapeutic efficacy of sulfasalazine and its metabolites in patients with ulcerative colitis and Crohn's disease. New England Journal of Medicine 1980;303:1499-502. [DOI] [PubMed] [Google Scholar]
Levy 1999
- Levy RL, Feld AD. Increasing patient adherence to gastroenterology treatment and prevention regimens. American Journal of Gastroenterology 1999;94(7):1733-42. [DOI] [PubMed] [Google Scholar]
Loftus 2004
- Loftus EJ. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology 2004;126(6):1504-17. [DOI] [PubMed] [Google Scholar]
Magowan 2006
- Magowan S, Kane S, Lange JL. 5-ASA prescription refill rates for ulcerative colitis are independent of formulation and dosing regimens. American Journal of Gastroenterology 2006;101:S447. [Google Scholar]
Misiewitz 1965
- Misiewitz JJ, Lennard-Jones JE, Connell AM, Baron JH, Jones FA. Controlled trial of sulfasalazine in maintenance therapy for ulcerative colitis. Lancet 1965;1:185-8. [Google Scholar]
Myers 1987
- Myers B, Evans DN, Rhodes J, Evans BK, Hughes BR, Lee MG, et al. Metabolism and urinary excretion of 5-aminosalicylic acid in healthy volunteers when given intravenously or released for absorption at different sites in the gastrointestinal tract. Gut 1987;28:196-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nielsen 1982
- Nielsen OH. Sulfasalazine intolerance: a retrospective study of the reasons for discontinuing treatment with sulfasalazine in patients with chronic inflammatory bowel disease. Scandinavian Journal of Gastroenterology 1982;17:389-93. [DOI] [PubMed] [Google Scholar]
Nielsen 1983
- Nielsen OH, Bondesen S. Kinetics of 5-aminosalicylic acid after jejunal instillation in man. British Journal of Clinical Pharmacology 1983;16:738-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Peppercorn 1972
- Peppercorn MA, Goldman P. The role of intestinal bacteria in the metabolism of salicylazo-sulfapyridine. Journal of Pharmacology and Experimental Therapeutics 1972;181:555-62. [PubMed] [Google Scholar]
Rao 1987
- Rao SS, Cann PA, Holdsworth CD. Clinical experience of the tolerance of mesalazine and olsalazine in patients intolerant of sulfasalazine. Scandinavian Journal of Gastroenterology 1987;22:332-6. [DOI] [PubMed] [Google Scholar]
Rasmussen 1982
- Rasmussen SN, Bondesen S, Hvidberg EF, Hansen SH, Binder V, Halskou S, et al. 5-aminosalicylic acid in a slow-release preparation: bioavailability, plasma level, and excretion in humans. Gastroenterology 1982;83:1062-70. [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Riley 1987
- Riley SA, Lecarpentier J, Mini V, Goodman JJ, Mandal BK, Turnberg LA. Sulfasalazine induced seminal abnormalities in ulcerative colitis: result of mesalazine substitution. Gut 1987;28:1008-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rothfuss 2006
- Rothfuss KS, Stange EF, Herrlinger KR. Extraintestinal manifestations and complications in inflammatory bowel diseases. World Journal of Gastroenterology 2006;12(30):4819-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sandborn 2002a
- Sandborn WJ. Rational selection of oral 5-aminosalicylate formulations and prodrugs for the treatment of ulcerative colitis. American Journal of Gastroenterology 2002;97(12):2939-41. [DOI] [PubMed] [Google Scholar]
Sandborn 2002b
- Sandborn WJ, Hanauer SB, Buch A. Comparable systemic absorption of 5-ASA and N-AC-5-ASA from U.S. Asacol and Colazal. American Journal of Gastroenterology 2002;97:S263. [Google Scholar]
Sandborn 2002c
- Sandborn WJ, Hanauer SB. The pharmacokinetic profiles of oral 5ASA formulations used in the management of ulcerative colitis: a systematic review. American Journal of Gastroenterology 2002;97:S269. [Google Scholar]
Sandborn 2003
- Sandborn WJ, Hanauer SB. Systematic review: the pharmacokinetic profiles of oral mesalazine formulations and mesalazine pro-drugs used in the management of ulcerative colitis. Alimentary Pharmacology and Therapeutics 2003;17(1):29-42. [DOI] [PubMed] [Google Scholar]
Schroeder 1972
- Schroeder H, Campbell DE. Absorption, metabolism, and excretion of salicylazosulfapyridine in man. Clinical Pharmacology and Therapeutics 1972;13:539-51. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JP, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Shale 2003
- Shale MJ, Riley SA. Studies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel disease. Alimentary Pharmacology and Therapeutics 2003;18(2):191-8. [DOI] [PubMed] [Google Scholar]
Svartz 1942
- Svartz N. Salazopyrin, a new sulfanilamide preparation: A. Therapeutic results in rheumatic polyarthritis. B. Therapeutic results in ulcerative colitis. C. Toxic manifestations in treatment with sulfanilamide preparation. Acta Medica Scandinavica 1942;110:557-90. [Google Scholar]
Truelove 1955
- Truelove SC, Witts LJ. Cortisone in ulcerative colitis: final report on a therapeutic trial. British Medical Journal 1955;4947:1041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Truelove 1959
- Truelove SC, Witts LJ. Cortisone and corticotrophin in ulcerative colitis. British Medical Journal 1959;i:387-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Hees 1980
- Van Hees PA, Bakker JH, Tongeren JH. Effect of sulfapyridine, 5-aminosalicylic acid, and placebo in patients with idiopathic proctitis: a study to determine the active therapeutic moiety of sulfasalazine. Gut 1980;21:632-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Willoughby 1982
- Willoughby CP, Aronson JK, Agback H, Bodin NO, Truelove SC. Distribution and metabolism in healthy volunteers of disodium azodisalicylate, a potential therapeutic agent for ulcerative colitis. Gut 1982;23:1081-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Feagan 2012
- Feagan BG, MacDonald JK. Oral 5-aminosalicylic acid for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2012, Issue 10. Art. No: CD000544. [DOI: 10.1002/14651858.CD000544.pub3] [DOI] [PubMed] [Google Scholar]
Sutherland 1993
- Sutherland LR, May GR, Shaffer EA. Sulfasalazine revisited: a meta-analysis of 5-aminosalicylic acid in the treatment of ulcerative colitis. Annals of Internal Medicine 1993;118:540-9. [DOI] [PubMed] [Google Scholar]
Sutherland 1997
- Sutherland LR, Roth DE, Beck PL. Alternatives to sulfasalazine: A meta-analysis of 5-ASA in the treatment of ulcerative colitis. Inflammatory Bowel Diseases 1997;3:65-78. [PubMed] [Google Scholar]
Sutherland 2006
- Sutherland LR, MacDonald JK. Oral 5-aminosalicylic acid for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2006, Issue 2. Art. No: CD000544. [DOI: 10.1002/14651858.CD000544.pub2] [DOI] [PubMed] [Google Scholar]
Wang 2016
- Wang Y, Parker CE, Feagan BG, MacDonald JK. Oral 5-aminosalicylic acid for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2016, Issue 5. Art. No: CD000544. [DOI: 10.1002/14651858.CD000544.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]


