Abstract
Importance:
The prevalence of and the mortality related to methamphetamine use has doubled over the past 10 years and there is evidence suggesting that methamphetamine use disorder could be the next substance use crisis in the United States and possibly world-wide.
Observation:
The neurobiology of methamphetamine use disorder extends beyond the acute effect of the drug as a monoaminergic modulator and includes intracellular pathways focused on oxidative stress, neuro- and excitotoxicity, and neuroinflammation. Similarly, the clinical picture extends beyond the acute psychostimulatory symptoms to include complex cardiovascular and cerebrovascular signs and symptoms that need to be identified by the clinician. Although there are no pharmacological treatments for methamphetamine use disorder, cognitive behavioral therapy, behavioral activation and contingency management show modest efficacy.
Conclusion and Relevance:
There is a need to better understand the complex neurobiology of this disorder and to develop interventions aimed at novel biological targets. Parsing the disorder into different processes, e.g. craving or mood-related alterations, and targeting the neural systems and biological pathways underlying these processes may lead to greater success in identifying disease modifying interventions. Finally, mental health professionals need to be trained in recognizing early cardiovascular and cerebrovascular warning signs to mitigate the mortality associated with methamphetamine use disorder.
Introduction
In the wake of the opioid crisis, methamphetamine has re-emerged as a challenge to mental health providers and researchers alike. Methamphetamine is now available in different forms such as ice, powder, and pills with different pharmacokinetic characteristics that make them popular among certain types of users 1. Recent seizure data suggest that its production and trafficking is spreading into new areas of the globe 2. According to the “Automation of Reports and Consolidated Orders System”, methamphetamine consumption increased 4-fold between 2015 and 2016 and total stimulant usage doubled in the last decade 3. From 2011 through 2016, the age-adjusted rate of drug overdose deaths involving methamphetamine more than tripled 4. Moreover, drug overdose deaths involving cocaine, amphetamines, or both substances combined increased 42.4% from 12,122 in 2015 to 17,258 in 2016 5. Based on the most recent data from the National Survey on Drug Use and Health, 12-month prevalence of individuals age 12 and above reporting methamphetamine use has increased by 195% from its low in 2010 to 2018 (Figure 1) and it is estimated that 1.86 million Americans used methamphetamine in 2018. These numbers underline the importance of paying attention to the possibility of the next substance use crisis. However, whereas opioid use disorder can be treated pharmacologically 6 and behaviorally 7, there are significant challenges for the treatment of methamphetamine use disorder (MUD). This review will focus on three specific aspects of MUD. First, the neurobiology of methamphetamine is more complex than the traditional view of it as a monoaminergic modulator. Second, the clinical presentation is not limited to the symptoms associated with use disorder but extend to medical presentations, most notably the cardio- and cerebrovascular systems. Third, pharmacological interventions focused on modulating the monoaminergic pathways have largely failed and new pharmacological approaches are necessary to focus on novel treatment targets. In the final section several suggestions will be proposed for both clinicians and researchers to advance the understanding of MUD.
Figure 1:
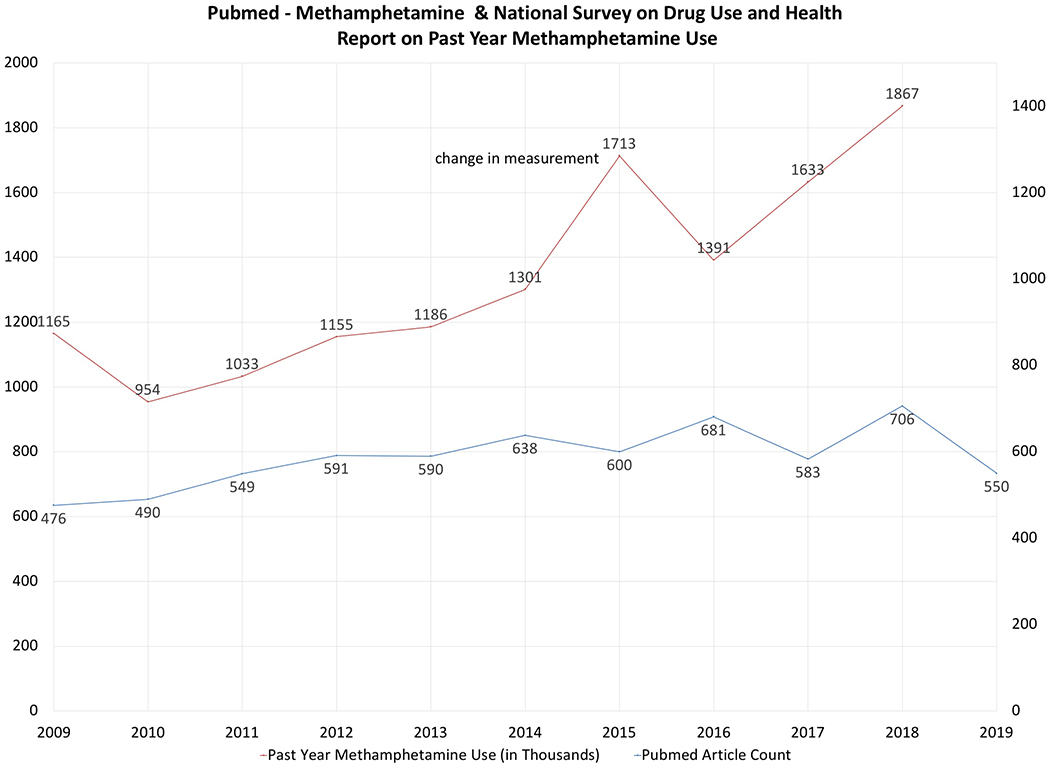
Summary statistics of articles published mentioning methamphetamine and past year methamphetamine use from 2009-2019
Biological Pathways, Neural Basis and Cognition
Methamphetamine has been conceptualized primarily as a releaser of dopamine, serotonin, noradrenaline, and adrenaline from nerve terminals in the central and peripheral nervous system (e.g. 8), which occurs via a number of different mechanisms, including: (1) redistributing catecholamines from synaptic vesicles to the cytosol; (2) reversing the plasma membrane transport of neurotransmitter; (3) blocking the activity of monoamine transporters; (4) decreasing the expression of dopamine transporters at the cell surface; (5) inhibiting monoamine oxidase activity; and (6) increasing the activity and expression of tyrosine hydroxylase, the critical enzyme for synthesizing dopamine 9. However, there has been a substantial expansion of methamphetamine-driven neurobiological targets over the past decade. Methamphetamine modulates at least three different molecular cascades, which have been described as oxidative stress, neuro- and excitotoxicity, and neuroinflammation 10 (Figure 2). For example, mitochondria are the are primary site of oxidative metabolism and are organized in a tubular, dynamic network that undergoes continuous remodeling via fusion or fission 11. Methamphetamine induces changes in morphology of mitochondria in neurons and microglia, which disturbs the mitochondrial homeostasis, morphology, and oxidative stress metabolism towards an increase in oxidative burden conducive to neurodegeneration 12. Methamphetamine also causes single and double strand breaks in DNA due to reactive oxygen species, leading to persisting mutations at the chromosomal level at blood concentrations that are observed in users 13. Methamphetamine-induced neuroinflammation is partially mediated by direct binding to the toll-like receptor 4 (TLR4) transmembrane protein within the ventral tegmental area, which has the downstream effect of elevating dopamine in the nucleus accumbens shell 14. The inflammatory changes in the brain occur largely in microglia, i.e. the primary cells of active immune defense in the central nervous system. The inflammasome is a molecular system that consists of the sensing molecule NLRP3, the adaptor apoptosis-associated speck-like (ASC) protein, and the executive enzyme caspase-1. Methamphetamine upregulates caspase-1 and ASC aggregation, which promotes inflammasome-mediated interleukin 1 beta maturation and secretion mediating microglia-induced neurotoxicity 15. This process also occurs in a number of conditions ranging from neurodevelopmental disorders to neurodegenerative disorders 16. Importantly, the methamphetamine induced cellular dysregulation in neurons and microglia can affect neural processing 17, altered reward motivation due to sickness behavior 18, and reduced prefrontal control 19, which – together - may contribute to the development and maintenance of drug-taking behavior 20. Methamphetamine-induced neurotoxicity has been hypothesized to be the result of interdependent mechanisms including: (1) excessive dopamine, resulting in an increased production of reactive oxygen species such as peroxides that can damage cell structures; (2) ubiquitin-proteasome system dysfunction, activating intracellular degradation systems leading to autophagy; (3) protein nitration, leading to an increase in radical nitric oxide with subsequent cytotoxic effects; (4) endoplasmic reticulum stress, leading to increased apoptosis; (5) increased tumor protein p53 expression in the striatum, altering DNA repair, arresting cell cycles, and dysregulating the expression of stress response genes; (6) inflammatory cytokines, leading to inflammatory activation in the brain; (7) activation of the dopamine D3 receptor, resulting in hyperthermia; and (8) microtubule deacetylation, disrupting the blood brain barrier 21. Together, these neurobiological cascades of oxidative stress, neuro- and excitotoxicity, and neuroinflammation result in a unique metabolic state of the brain, which has been termed the Warburg effect, i.e. when cells favor metabolism via glycolysis rather than the much more efficient oxidative phosphorylation 22. Thus, methamphetamine use acutely, and possibly chronically, places the brain in a different metabolic state characterized by: (1) a quicker but less efficient availability of energy; (2) an increased rate of biosynthesis; (3) acidification of the microenvironment; and (4) altered cell signaling via reactive oxygen species, which promotes an oncogenic and degenerative cell environment. In summary, MUD does not just reflect a dopamine dysregulation but represents an altered brain state that is consistent with those observed in degenerative central nervous system diseases. These complex molecular dysregulations provide an opportunity to identify modifiable drug targets to develop novel pharmacological interventions for MUD.
Figure 2:
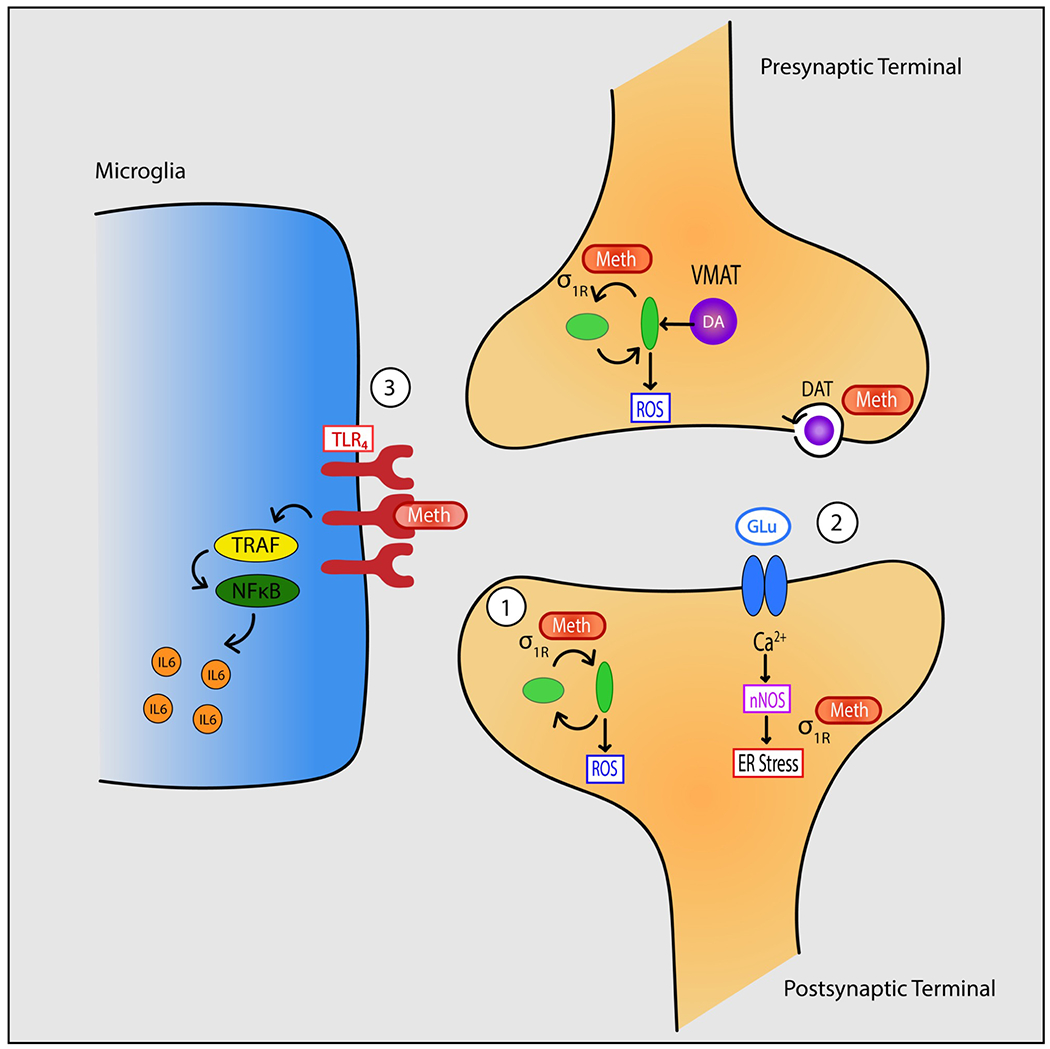
Methamphetamine-induced changes in synaptic and intracellular pathways. Methamphetamine increases dopamine in the synaptic cleft and the cell via its effects on the cell surface dopamine transporter (DAT) and the vesicular monoamine transporter (VMAT), respectively. Methamphetamine: (1) directly alters mitochondrial fusion and fission via sigma-1 receptor (σ1R binding leading to an increase in reactive oxygen species (ROS); (2) increases glutamatergic (GLU) transmission, which via increased intracellular calcium (Ca2+) and nitric oxide synthase (nNOS) leads to endoplasmic reticulum (ER) stress; and (3) binds to the toll-like 4 (TLR4) receptor to activate inflammatory pathways via nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) and tumor necrosis factor receptor associated factors (TRAF) to produce pro-inflammatory cytokines (IL6).
Others have proposed that compulsive drug taking is the result of an imbalance between an orbitofrontal cortex-dorsomedial striatal “go” circuit and an opposing dorsolateral frontal-striatal “stop” circuit 23. Numerous studies have focused on examining evidence of structural and functional alterations within these circuits. For example, methamphetamine users show widespread gray and white matter alterations, particularly affecting the frontostriatal system 24 as well as prominent reductions in the left superior temporal gyrus and the right inferior parietal lobe, which provide contextual information to the dorsolateral frontal circuits 25. Moreover, abnormalities include deficits in markers of dopaminergic and serotonergic neurotransmitter systems, differences in glucose metabolism and deficits in gray matter 26. Chronic methamphetamine users show aberrant patterns of brain connectivity and function within both orbitofrontal-striatal and dorsolateral frontal-striatal systems when engaged in cognitive tasks and at rest 27. Functional neuroimaging studies have shown that methamphetamine users show changes in orbitofrontal cortex during empathic processing 28, in salience and dorsolateral frontal functioning areas during decision-making 29,30, and in both dorsolateral and inferior frontal areas during inhibitory processing 31. Interestingly, lower cortico-striatal connectivity as measured by resting state functional magnetic resonance imaging (fMRI) has been associated with higher concentration of peripherally measured cytokines 32, which may provide evidence for the link between neuroinflammation and brain processing changes in MUD. Although functional brain activation differences during various behavioral tasks among MUD individuals have been used to predict relapse 33-35, none of these measures have thus far been clinically useful 36, i.e. have been able to aid in the diagnosis, prognosis or treatment of the disorder 37.
The impact of methamphetamine on cognition has been heavily debated (e.g. see 38) and a dearth of longitudinal studies makes it difficult to assess whether the observed cognitive dysfunctions are pre-existing, a consequence of the exposure, or a consequence of behaviors that are associated with substance use disorders in general. Nevertheless, several recent studies that provide a more cohesive picture of cognitive problems that exist both shortly after cessation of use and to some extent after longer periods of abstinence. For example, MUD subjects in early abstinence but post-acute withdrawal show poorer performance on tasks examining motor and processing speed, verbal fluency, and attention 39. Even following prolonged abstinence, individuals with MUD perform more poorly than matched comparison subjects on learning efficiency, visual-spatial processing, comprehension knowledge, retrieval fluency, processing speed, and psychomotor speed 40. In addition, dysfunctions of impulsivity have been associated with greater of severity of use 41 and earlier age of use onset 42. Global assessments of cognitive function support the idea that more than 2/3 of individuals with MUD show cognitive impairment 43, the extent of which is linked to older age, longer duration and higher frequency of use. Aside from providing an objective assessment of the impact of methamphetamine use, neuropsychological assessment can also be used as a prognostic indicator. For example, cognitive measures such as problems with sustained attention can predict reduced treatment motivation 44 and different forms of impulsivity predict poorer 6-week outcomes in treatment 45. Taken together, methamphetamine is associated with a moderate dysfunction of a number of cognitive processes, limiting the degree to which individuals with MUD are able to focus attention on goal-directed activity away from methamphetamine use in early abstinence. Given that neuropsychological function has some predictive utility for treatment retention and success, more work needs to be done to determine whether any of these cognitive dysfunctions can be remediated by targeted interventions.
Clinical Presentation
The acute behavioral effects of methamphetamine include 46 increased energy and alertness, decreased need for sleep, euphoria, increased sexuality, excessive talking, weight loss, sweating, tightened jaw muscles, grinding teeth, and loss of appetite. Symptoms exacerbated by methamphetamine can be divided into three factors: (1) positive psychotic symptoms such as suspiciousness, unusual thought content, hallucinations, and bizarre behavior; (2) affective symptoms including depression, suicidality, guilt, hostility, somatic concern, and self-neglect; and (3) psychomotor symptoms, such as tension, excitement, distractibility, and motor hyperactivity 47. The clinical picture can be complex and mimics a variety of psychiatric disorders. The transition from casual to compulsive methamphetamine use can be rapid and some have reported that it takes on average about 50 days from the onset of drug use to the first drug craving, 60 days to regular use, and 85 days to compulsive use 48. Although most methamphetamine-associated psychoses are brief lasting hours to days, in some cases psychotic episodes may persist for longer than 6 months and can reoccur during periods of abstinence from the drug 49. On average, 36.5% of methamphetamine using individuals, regardless of age or sex, report psychotic symptoms, but if one takes lifetime symptoms into account this number increases to 42.7% 50. Some have suggested that self-reported psychotic illness is more prevalent among users of crystal methamphetamine than other forms of methamphetamine 51, which may be related to its purity and the self-selection of individuals who use this form of the drug. The psychiatric comorbidity of MUD is complex 52 because there is evidence for both pre-existing factors that increase risk for psychiatric disorder, e.g. a prevalence of 44% of moderate to severe childhood abuse or neglect 53. Moreover, early lifetime adversity such as emotional or sexual trauma may also increase the likelihood of MUD due to fact that some individuals use methamphetamine as a coping method 54. In addition, there are other co-existing psychiatric disorders such as mood disorders (16.0%), psychotic disorders (13.0%) and anxiety disorders (7.0%) 55. Both early life trauma and psychiatric comorbidity can adversely affect both age of first use 56 as well as treatment success 57.
The path to using methamphetamine involves at least two trajectories. First, younger users take methamphetamine primarily for recreational and performance enhancement purposes, whereas those initiating at a later age may use to “self-medicate” e.g. stressful life events 58. This is consistent with the observation that the rate of females, who are much more likely than males report using methamphetamine for weight-related issues, is higher among adolescent relative to adult users 59. Second, there is emerging evidence of individuals using methamphetamine as an opioid substitute, to obtain a synergistic high, or to balance out the effects of opioids 60. Recent longitudinal evidence suggests that increase of cannabis use among adolescents may increase the probability of initiating other illicit drugs such as methamphetamine via both biological and social processes 61, providing some evidence for the “gateway hypothesis” 62. Similar to many other substance use disorders, the course of MUD is often characterized by repeated periods of intense use with intermittent sobriety and relapse 63,64. Those who do not engage in treatment only show 5-year remission rates up to 30% 65 and of those who engage in treatment, 61% relapse within the first 12 months and another 14% relapse during years 2-5 64. These findings underscore that MUD is a chronic, relapsing and possibly degenerative condition, which is consistent with the profound molecular changes induced by methamphetamine.
The most severe medical problems and the leading cause of death associated with MUD are cardiovascular and cerebrovascular disease 66. Methamphetamine-related strokes 67 have been on the rise, occurring most often in young men, and are primarily hemorrhagic in nature. Methamphetamine is associated with vasoconstriction, pulmonary hypertension, atherosclerotic plaque formation, cardiac arrhythmias, and cardiomyopathy 68. Methamphetamine-associated cardiomyopathy 69 is characterized by left ventricular dilatation and impaired left ventricular ejection fraction as well as elevated tissue markers of inflammation and fibrosis 70. On the electrocardiogram, these individuals frequently show tachyarrhythmias, right axis deviation, left ventricular hypertrophy, P pulmonale pattern, inferior Q waves, lateral T wave inversion, and longer QTc interval 71. Symptoms preceding death attributed solely to methamphetamine toxicity include collapse, breathing difficulty, and hyperthermia, which may be a consequence of acute abnormal enlargement of the heart 72. Methamphetamine also contributes significantly to opioid mortality statistics, as the drug is also present in 63% of opioid deaths 73. It is important to emphasize that in individuals who present with acute intoxication with methamphetamine, symptoms of dyspnea, angina, palpitations, cough, and hemoptysis should prompt the clinician to closely monitor the medical status to prevent mortality.
Interventions
There are very limited pharmacological options for which there is sufficient efficacy data to treat MUD 74. Table 1 summarizes all intervention trials registered at http://clinicialtrials.gov that contained the term “methamphetamine”. Of the 159 registered studies, 65 represented randomized clinical trials (RCTs); of those, 25 reported results, of which 14 resulted in publications with identifiable PMIDs. Examining these publications, 8 reported no effect, 3 reported some effect, and 3 reported effects that did not speak to the efficacy of the intervention. Moreover, reports submitted to http://clinicaltrials.gov were either mostly unclear with respect to efficacy or reported null results (see supplemental table). This short summary is consistent with conclusions by others who conducted meta-analyses. Specifically, examining 49 studies investigating 20 potential pharmacotherapies, a total of 35 studies related to 33 Phase II quality, i.e. efficacy studies, RCTs 75. For the 5 medications that were subject to multiple RCTs, 4 of these— methylphenidate, bupropion, modafinil, and naltrexone— demonstrated some limited evidence of benefit for reducing methamphetamine use. The authors concluded that none of these drugs showed sufficient and consistent evidence of effectiveness to support its use in routine treatment. This assessment is similar to another study, which concluded that (1) no agent demonstrated a broad and strong effect in achieving methamphetamine abstinence in Phase II trials 76 and (2) there was not sufficient evidence available for dopamine analogue treatment after the initial withdrawal-period 77. Studies of anticonvulsants, antipsychotics, opioid antagonists, varenicline, and atomoxetine provided either low-strength or insufficient evidence of no effect on the outcomes of interest, i.e. abstinence, defined as 3 or more consecutive weeks with negative urine drug screens 78. Immunotherapy has been suggested as an alternative form of treatment for drug abuse; however, none of the anti-drug immunotherapies have reached phase III clinical trials so far 79. Although some have reported that that the combination of pharmacological treatments aimed at treating psychiatric target symptoms and brief cognitive behavioral treatment in a research setting outperformed control conditions 80, there is no sufficient evidence that pharmacological interventions by themselves are useful for the treatment of MUD.
Table 1:
Treatment Studies and Failures
| Results | ClinicalTrials.gov “Methamphetamine” | n | % Total | %RCT |
|---|---|---|---|---|
| Total | 159 | |||
| Randomized Intervention Model | 65 | 40.88% | ||
| With some results reported | 25 | 15.72% | 38.46% | |
| Publications | 14 | 8.81% | 21.54% | |
| PMIDs | No Effect | 8 | 5.03% | 12.31% |
| Some Effect | 3 | 1.89% | 4.62% | |
| Unclear | 3 | 1.89% | 4.62% | |
| Others | No Effect | 5 | 3.14% | 7.69% |
| Some Effect | 0 | 0.00% | 0.00% | |
| Unclear | 6 | 3.77% | 9.23% |
Note. RCT = randomized controlled trials.
Results from studies using behavioral interventions to treat MUDs are more encouraging. In a recent network meta-analysis, compared to treatment-as-usual, only contingency management, i.e. a procedure that aims to alter drug use by systematically arranging consequences which are designed to weaken drug use and strengthen abstinence, plus community reinforcement, i.e. adjusting an individual’s environment such that abstinence is more rewarding than using the drug, increased the number of abstinent MUD patients at the end of treatment 81. Others reported that brief cognitive behavioral therapy (CBT) resulted in significant reductions in frequency of methamphetamine use, MUD severity, and number of days of methamphetamine use at weeks 4 and 12 82, findings consistent with a systematic review that finds weak evidence for increased percentage of abstinent days in 90 days and reduced MUD symptoms 83. Similarly, behavioral activation, which aims to maximize activities that are not drug-related but are positively valued by the individual, had a beneficial effect on abstinence in alcohol, tobacco, opioid, and methamphetamine use in 7 of the 8 reviewed studies, and improved depression over time in six studies 84. Finally, several studies demonstrate beneficial effects of exercise on reducing MUD symptoms. For example, an aerobic exercise program provided benefits for methamphetamine-associated craving and improved inhibitory control in individuals with MUD 85. Moreover, exercise by methamphetamine users reduced levels of depression and anxiety over an 8-week period compared to a health education control group 86. Taken together, there is some evidence that contingency management, CBT, behavioral activation, and exercise help to maintain abstinence. There is also encouraging evidence for computer-delivered interventions 87 and app-based approaches 88. Nevertheless, there are two significant shortcomings. First, intervention programs for methamphetamine are plagued by high discontinuation rates. For example, in one large program 51% dropped out within the first two weeks and the average number of days retained was only 60 days 89. Second, there is little understanding as to: (1) how these behavioral interventions affect the underlying neurobiology of MUD; and (2) whether these interventions improve neural processing and cognitive dysfunctions within these individuals.
Conclusion and Relevance
MUD is re-emerging as a significant public health burden, a challenge for the clinician, and a difficult problem to solve for the researcher. First, MUD can develop rapidly, has a complex course characterized by episodes of intense use and intermittent abstinence, has profound medical consequences, is a difficult to treat condition, and results in significant long-term cognitive and neurological deficits. Second, clinicians faced with the presentation of an individual with acute methamphetamine intoxication should examine the patient for evidence of cardiovascular and cerebrovascular signs and symptoms, which are the primary reason for deaths due to methamphetamine. Third, there are several next steps to consider for pragmatically focused program of research. Modifiable biological targets should be examined in MUD individuals that focus on dysregulation of oxidative stress, neuro- and excitotoxicity, and neuroinflammation. Neuromodulatory approaches appear promising in ameliorating impairments associated with MUD. For example, electroencephalography (EEG) neurofeedback targeting the beta frequency band has increased, among other outcomes, periods of abstinence in methamphetamine users 90. Moreover, repetitive transcranial magnetic stimulation (rTMS) targeting frontal regions has resulted in decreased methamphetamine craving and/or increased cognitive-emotional function 91. Real-time fMRI neurofeedback, which demonstrates a beneficial effect on reduction of depressive symptoms 92, may also be helpful in reducing dysphoria present in methamphetamine users. Understanding the neurobiology of exercise-induced craving reduction in MUD 93 may help to delineate novel disease-relevant targets. Fourth, preventative behavioral interventions focused on factors such as childhood trauma and dysregulated negative affect processing that increase the likelihood of initiating or continuing methamphetamine use may help to reduce future use 94. Finally, the neurobiology of this disorder is almost entirely derived from cross-sectional studies, which provide very little mechanistic insights. Thus, longitudinal assessments of brain-related changes are necessary to determine what brain-based treatment targets are modifiable and what brain processes put individuals at high risk for relapse. Taken together, given the limited evidence-based intervention options, it will be critically important to develop an implementation framework such that behavioral interventions can be delivered with high fidelity to maximize treatment effects and help individuals overcome MUD.
Supplementary Material
Acknowledgements
This work has been supported in part by The William K. Warren Foundation, the National Institute on Drug Abuse (U01 DA041089), and the National Institute of General Medical Sciences Center Grant Award Number (1P20GM121312). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank April C. May for her assistance with figures created for this manuscript.
Financial Disclosures
Dr. Paulus is an advisor to Spring Care, Inc., a behavioral health startup, he has received royalties for an article about methamphetamine in UpToDate.
References
- 1.Chomchai C, Chomchai S. Global patterns of methamphetamine use. Curr Opin Psychiatry. 2015;28(4):269–274. [DOI] [PubMed] [Google Scholar]
- 2.Stoneberg DM, Shukla RK, Magness MB. Global Methamphetamine Trends: An Evolving Problem. International Criminal Justice Review. 2017;28(2):136–161. [Google Scholar]
- 3.Piper BJ, Ogden CL, Simoyan OM, et al. Trends in use of prescription stimulants in the United States and Territories, 2006 to 2016. PLoS One. 2018;13(11):e0206100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M. Drugs Most Frequently Involved in Drug Overdose Deaths: United States, 2011-2016. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2018;67(9):1–14. [PubMed] [Google Scholar]
- 5.Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug Overdose Deaths Involving Cocaine and Psychostimulants with Abuse Potential - United States, 2003–2017. MMWR Morbidity and mortality weekly report. 2019;68(17):388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma J, Bao YP, Wang RJ, et al. Effects of medication-assisted treatment on mortality among opioids users: a systematic review and meta-analysis. Mol Psychiatry. 2018. [DOI] [PubMed] [Google Scholar]
- 7.Carroll KM, Weiss RD. The Role of Behavioral Interventions in Buprenorphine Maintenance Treatment: A Review. Am J Psychiatry. 2017;174(8):738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moszczynska A, Callan SP. Molecular, Behavioral, and Physiological Consequences of Methamphetamine Neurotoxicity: Implications for Treatment. J Pharmacol Exp Ther. 2017;362(3):474–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barr AM, Panenka WJ, MacEwan GW, et al. The need for speed: an update on methamphetamine addiction. JPsychiatry Neurosci. 2006;31(5):301–313. [PMC free article] [PubMed] [Google Scholar]
- 10.Yang X, Wang Y, Li Q, et al. The Main Molecular Mechanisms Underlying Methamphetamine- Induced Neurotoxicity and Implications for Pharmacological Treatment. Frontiers in molecular neuroscience. 2018;11:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fischer F, Hamann A, Osiewacz HD. Mitochondrial quality control: an integrated network of pathways. Trends in biochemical sciences. 2012;37(7):284–292. [DOI] [PubMed] [Google Scholar]
- 12.Borgmann K, Ghorpade A. Methamphetamine Augments Concurrent Astrocyte Mitochondrial Stress, Oxidative Burden, and Antioxidant Capacity: Tipping the Balance in HIV-Associated Neurodegeneration. Neurotox Res. 2018;33(2):433–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ropek N, Al-Serori H, Misik M, et al. Methamphetamine (“crystal meth”) causes induction of DNA damage and chromosomal aberrations in human derived cells. Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association. 2019;128:1–7. [DOI] [PubMed] [Google Scholar]
- 14.Wang X, Northcutt AL, Cochran TA, et al. Methamphetamine Activates Toll-Like Receptor 4 to Induce Central Immune Signaling within the Ventral Tegmental Area and Contributes to Extracellular Dopamine Increase in the Nucleus Accumbens Shell. ACS chemical neuroscience. 2019;10(8):3622–3634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu E, Liu J, Liu H, Wang X, Xiong H. Inflammasome Activation by Methamphetamine Potentiates Lipopolysaccharide Stimulation of IL-1beta Production in Microglia. J Neuroimmune Pharmacol. 2018;13(2):237–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salter MW, Stevens B. Microglia emerge as central players in brain disease. Nature medicine. 2017;23(9):1018–1027. [DOI] [PubMed] [Google Scholar]
- 17.Weinhard L, di Bartolomei G, Bolasco G, et al. Microglia remodel synapses by presynaptic trogocytosis and spine head filopodia induction. Nature communications. 2018;9(1):1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boyle CC, Kuhlman KR, Dooley LN, et al. Inflammation and dimensions of reward processing following exposure to the influenza vaccine. Psychoneuroendocrinology. 2019;102:16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Felger JC, Li Z, Haroon E, et al. Inflammation is associated with decreased functional connectivity within corticostriatal reward circuitry in depression. Mol Psychiatry. 2016;21(10):1358–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kohno M, Link J, Dennis LE, et al. Neuroinflammation in addiction: A review of neuroimaging studies and potential immunotherapies. Pharmacol Biochem Behav. 2019;179:34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu S, Zhu L, Shen Q, Bai X, Di X. Recent advances in methamphetamine neurotoxicity mechanisms and its molecular pathophysiology. Behavioural neurology. 2015;2015:103969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liberti MV, Locasale JW. The Warburg Effect: How Does it Benefit Cancer Cells? Trends in biochemical sciences. 2016;41(3):211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu Y, Salmeron BJ, Krasnova IN, et al. Compulsive drug use is associated with imbalance of orbitofrontal- and prelimbic-striatal circuits in punishment-resistant individuals. Proc Natl Acad Sci U S A. 2019;116(18):9066–9071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lyoo IK, Yoon S, Kim TS, et al. Predisposition to and effects of methamphetamine use on the adolescent brain. Mol Psychiatry. 2015;20(12):1516–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall MG, Alhassoon OM, Stern MJ, et al. Gray matter abnormalities in cocaine versus methamphetamine-dependent patients: a neuroimaging meta-analysis. Am J Drug Alcohol Abuse. 2015;41(4):290–299. [DOI] [PubMed] [Google Scholar]
- 26.Baicy K, London ED. Corticolimbic dysregulation and chronic methamphetamine abuse. Addiction. 2007;102 Suppl 1:5–15. [DOI] [PubMed] [Google Scholar]
- 27.London ED, Kohno M, Morales AM, Ballard ME. Chronic methamphetamine abuse and corticostriatal deficits revealed by neuroimaging. Brain Res. 2015;1628(Pt A):174–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim YT, Lee JJ, Song HJ, et al. Alterations in cortical activity of male methamphetamine abusers performing an empathy task: fMRI study. Hum Psychopharmacol. 2010;25(1):63–70. [DOI] [PubMed] [Google Scholar]
- 29.Aron JL, Paulus MP. Location, location: using functional magnetic resonance imaging to pinpoint brain differences relevant to stimulant use. Addiction. 2007;102(Suppl 1):33–43. [DOI] [PubMed] [Google Scholar]
- 30.Paulus MP, Hozack N, Frank L, Brown GG, Schuckit MA. Decision making by methamphetamine-dependent subjects is associated with error-rate-independent decrease in prefrontal and parietal activation. BiolPsychiatry. 2003;53(1):65–74. [DOI] [PubMed] [Google Scholar]
- 31.Harle KM, Zhang S, Ma N, Yu AJ, Paulus MP. Reduced Neural Recruitment for Bayesian Adjustment of Inhibitory Control in Methamphetamine Dependence. Biological psychiatry : cognitive neuroscience and neuroimaging. 2016;1(5):448–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kohno M, Loftis JM, Huckans M, Dennis LE, McCready H, Hoffman WF. The relationship between interleukin-6 and functional connectivity in methamphetamine users. Neurosci Lett. 2018;677:49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harle KM, Yu AJ, Paulus MP. Bayesian computational markers of relapse in methamphetamine dependence. Neuroimage Clin. 2019;22:101794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stewart JL, Connolly CG, May AC, Tapert SF, Wittmann M, Paulus MP. Striatum and insula dysfunction during reinforcement learning differentiates abstinent and relapsed methamphetamine-dependent individuals. Addiction. 2014;109(3):460–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gowin JL, Harle KM, Stewart JL, Wittmann M, Tapert SF, Paulus MP. Attenuated Insular Processing During Risk Predicts Relapse in Early Abstinent Methamphetamine-Dependent Individuals. Neuropsychopharmacology. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gowin JL, Ernst M, Ball T, et al. Using neuroimaging to predict relapse in stimulant dependence: A comparison of linear and machine learning models. NeuroImage Clinical. 2019;21:101676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moeller SJ, Paulus MP. Toward biomarkers of the addicted human brain: Using neuroimaging to predict relapse and sustained abstinence in substance use disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2018;80(Pt B):143–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hart CL, Marvin CB, Silver R, Smith EE. Is cognitive functioning impaired in methamphetamine users? A critical review. Neuropsychopharmacology. 2012;37(3):586–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang LJ, Chen CK, Lin SK, Chen YC, Xu K, Huang MC. Cognitive profile of ketamine-dependent patients compared with methamphetamine-dependent patients and healthy controls. Psychopharmacology (Berl). 2018;235(7):2113–2121. [DOI] [PubMed] [Google Scholar]
- 40.Basterfield C, Hester R, Bowden SC. A meta-analysis of the relationship between abstinence and neuropsychological functioning in methamphetamine use disorder. Neuropsychology. 2019;33(5):739–753. [DOI] [PubMed] [Google Scholar]
- 41.Moallem NR, Courtney KE, Ray LA. The relationship between impulsivity and methamphetamine use severity in a community sample. Drug Alcohol Depend. 2018;187:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cservenka A, Ray LA. Self-reported attentional and motor impulsivity are related to age at first methamphetamine use. Addict Behav. 2017;65:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang TY, Fan TT, Bao YP, et al. Pattern and related factors of cognitive impairment among chronic methamphetamine users. Am J Addict. 2017;26(2):145–151. [DOI] [PubMed] [Google Scholar]
- 44.Rubenis AJ, Fitzpatrick RE, Lubman DI, Verdejo-Garcia A. Sustained attention but not effort-based decision-making predicts treatment motivation change in people with methamphetamine dependence. J Subst Abuse Treat. 2018;95:48–54. [DOI] [PubMed] [Google Scholar]
- 45.Rubenis AJ, Fitzpatrick RE, Lubman DI, Verdejo-Garcia A. Impulsivity predicts poorer improvement in quality of life during early treatment for people with methamphetamine dependence. Addiction. 2018;113(4):668–676. [DOI] [PubMed] [Google Scholar]
- 46.Hart CL, Gunderson EW, Perez A, et al. Acute physiological and behavioral effects of intranasal methamphetamine in humans. Neuropsychopharmacology. 2008;33(8):1847–1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McKetin R, Dawe S, Burns RA, et al. The profile of psychiatric symptoms exacerbated by methamphetamine use. Drug Alcohol Depend. 2016;161:104–109. [DOI] [PubMed] [Google Scholar]
- 48.Wang Z, Li WX, Zhi-Min L. Similarity and Difference in Drug Addiction Process Between Heroin- and Methamphetamine-Dependent Users. Subst Use Misuse. 2017;52(4):459–467. [DOI] [PubMed] [Google Scholar]
- 49.Grant KM, LeVan TD, Wells SM, et al. Methamphetamine-associated psychosis. J Neuroimmune Pharmacol. 2012;7(1):113–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lecomte T, Dumais A, Dugre JR, Potvin S. The prevalence of substance-induced psychotic disorder in methamphetamine misusers: A meta-analysis. Psychiatry Res. 2018;268:189–192. [DOI] [PubMed] [Google Scholar]
- 51.Lappin JM, Roxburgh A, Kaye S, et al. Increased prevalence of self-reported psychotic illness predicted by crystal methamphetamine use: Evidence from a high-risk population. Int J Drug Policy. 2016;38:16–20. [DOI] [PubMed] [Google Scholar]
- 52.Salo R, Flower K, Kielstein A, Leamon MH, Nordahl TE, Galloway GP. Psychiatric comorbidity in methamphetamine dependence. Psychiatry Res. 2011;186(2-3):356–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen Y, Zhang J, Sun Y. The relationship between childhood abuse and depression in a sample of Chinese people who use methamphetamine. Int J Clin Health Psychol. 2019;19(3):181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simpson JL, Grant KM, Daly PM, Kelley SG, Carlo G, Bevins RA. Psychological Burden and Gender Differences in Methamphetamine-Dependent Individuals in Treatment. J Psychoactive Drugs. 2016;48(4):261–269. [DOI] [PubMed] [Google Scholar]
- 55.Akindipe T, Wilson D, Stein DJ. Psychiatric disorders in individuals with methamphetamine dependence: prevalence and risk factors. Metabolic brain disease. 2014;29(2):351–357. [DOI] [PubMed] [Google Scholar]
- 56.Svingen L, Dykstra RE, Simpson JL, et al. Associations Between Family History of Substance Use, Childhood Trauma, and Age of First Drug Use in Persons With Methamphetamine Dependence. J Addict Med. 2016;10(4):269–273. [DOI] [PubMed] [Google Scholar]
- 57.McKetin R, Kothe A, Baker AL, Lee NK, Ross J, Lubman DI. Predicting abstinence from methamphetamine use after residential rehabilitation: Findings from the Methamphetamine Treatment Evaluation Study. Drug Alcohol Rev. 2018;37(1):70–78. [DOI] [PubMed] [Google Scholar]
- 58.Yimsaard P, Maes MM, Verachai V, Kalayasiri R. Pattern of Methamphetamine Use and the Time Lag to Methamphetamine Dependence. J Addict Med. 2018;12(2):92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen LY, Strain EC, Alexandre PK, Alexander GC, Mojtabai R, Martins SS. Correlates of nonmedical use of stimulants and methamphetamine use in a national sample. Addict Behav. 2014;39(5):829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ellis MS, Kasper ZA, Cicero TJ. Twin epidemics: The surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend. 2018;193:14–20. [DOI] [PubMed] [Google Scholar]
- 61.Otten R, Mun CJ, Dishion TJ. The social exigencies of the gateway progression to the use of illicit drugs from adolescence into adulthood. Addict Behav. 2017;73:144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kandel D, Kandel E. The Gateway Hypothesis of substance abuse: developmental, biological and societal perspectives. Acta paediatrica (Oslo, Norway : 1992). 2015;104(2):130–137. [DOI] [PubMed] [Google Scholar]
- 63.Hser YI, Evans E, Huang D, Brecht ML, Li L. Comparing the dynamic course of heroin, cocaine, and methamphetamine use over 10 years. Addict Behav. 2008;33(12):1581–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Brecht ML, Herbeck D. Time to relapse following treatment for methamphetamine use: A long-term perspective on patterns and predictors. Drug Alcohol Depend. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lanyon C, Nambiar D, Higgs P, Dietze P, Quinn B. Five-year Changes in Methamphetamine Use, Dependence, and Remission in a Community-recruited Cohort. J Addict Med. 2019;13(2):159–165. [DOI] [PubMed] [Google Scholar]
- 66.Huang MC, Yang SY, Lin SK, et al. Risk of Cardiovascular Diseases and Stroke Events in Methamphetamine Users: A 10-Year Follow-Up Study. J Clin Psychiatry. 2016. [DOI] [PubMed] [Google Scholar]
- 67.Lappin JM, Darke S, Farrell M. Stroke and methamphetamine use in young adults: a review. Journal of neurology, neurosurgery, and psychiatry. 2017;88(12):1079–1091. [DOI] [PubMed] [Google Scholar]
- 68.Kevil Christopher G, Goeders Nicholas E, Woolard Matthew D, et al. Methamphetamine Use and Cardiovascular Disease. Arteriosclerosis, Thrombosis, and Vascular Biology. 2019;39(9): 1739–1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Neeki MM, Kulczycki M, Toy J, et al. Frequency of Methamphetamine Use as a Major Contributor Toward the Severity of Cardiomyopathy in Adults </=50 Years. Am J Cardiol. 2016;118(4):585–589. [DOI] [PubMed] [Google Scholar]
- 70.Schurer S, Klingel K, Sandri M, et al. Clinical Characteristics, Histopathological Features, and Clinical Outcome of Methamphetamine-Associated Cardiomyopathy. JACC Heart failure. 2017;5(6):435–445. [DOI] [PubMed] [Google Scholar]
- 71.Paratz ED, Zhao J, Sherwen AK, Scarlato RM, Maclsaac AI. Is an Abnormal ECG Just the Tip of the ICE-berg? Examining the Utility of Electrocardiography in Detecting Methamphetamine-Induced Cardiac Pathology. Heart, lung & circulation. 2017;26(7):684–689. [DOI] [PubMed] [Google Scholar]
- 72.Darke S, Duflou J, Lappin J, Kaye S. Clinical and Autopsy Characteristics of Fatal Methamphetamine Toxicity in Australia. Journal of forensic sciences. 2018;63(5):1466–1471. [DOI] [PubMed] [Google Scholar]
- 73.Gladden R, O’Donnell J, Mattson C, Seth P. Changes in Opioid-Involved Overdose Deaths by Opioid Type and Presence of Benzodiazepines, Cocaine, and Methamphetamine — 25 States, July–December 2017 to January–June 2018. MMWR Morbidity and mortality weekly report. 2019;68:737–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gouzoulis-Mayfrank E, Härtel-Petri R, Hamdorf W, Havemann-Reinecke U, Mühlig S, Wodarz N. Methamphetamine-Related Disorders. Deutsches Arzteblatt international. 2017;114(26):455–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee NK, Jenner L, Harney A, Cameron J. Pharmacotherapy for amphetamine dependence: A systematic review. Drug Alcohol Depend. 2018;191:309–337. [DOI] [PubMed] [Google Scholar]
- 76.Morley KC, Cornish JL, Faingold A, Wood K, Haber PS. Pharmacotherapeutic agents in the treatment of methamphetamine dependence. Expert opinion on investigational drugs. 2017;26(5):563–578. [DOI] [PubMed] [Google Scholar]
- 77.Hartel-Petri R, Krampe-Scheidler A, Braunwarth WD, et al. Evidence-Based Guidelines for the Pharmacologic Management of Methamphetamine Dependence, Relapse Prevention, Chronic Methamphetamine-Related, and Comorbid Psychiatric Disorders in Post-Acute Settings. Pharmacopsychiatry. 2017;50(3):96–104. [DOI] [PubMed] [Google Scholar]
- 78.Chan B, Freeman M, Kondo K, et al. Pharmacotherapy for Methamphetamine/Amphetamine Use Disorder - A Systematic Review and Meta-analysis. Addiction. 2019. [DOI] [PubMed] [Google Scholar]
- 79.Xiaoshan T, Junjie Y, Wenqing W, et al. Immunotherapy for treating methamphetamine, heroin and cocaine use disorders. Drug Discov Today. 2019. [DOI] [PubMed] [Google Scholar]
- 80.Khoramizadeh M, Effatpanah M, Mostaghimi A, Rezaei M, Mahjoub A, Shishehgar S. Treatment of amphetamine abuse/use disorder: a systematic review of a recent health concern. Daru : journal of Faculty of Pharmacy, Tehran University of Medical Sciences. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.De Crescenzo F, Ciabattini M, D’Alo GL, et al. Comparative efficacy and acceptability of psychosocial interventions for individuals with cocaine and amphetamine addiction: A systematic review and network meta-analysis. PLoS Med. 2018;15(12):e1002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Alammehrjerdi Z, Briggs NE, Biglarian A, Mokri A, Dolan K. A Randomized Controlled Trial of Brief Cognitive Behavioral Therapy for Regular Methamphetamine Use in Methadone Treatment. J Psychoactive Drugs. 2019;51(3):280–289. [DOI] [PubMed] [Google Scholar]
- 83.Harada T, Tsutomi H, Mori R, Wilson DB. Cognitive-behavioural treatment for amphetamine-type stimulants (ATS)-use disorders. Cochrane Database Syst Rev. 2018;12:Cd011315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Martinez-Vispo C, Martinez U, Lopez-Duran A, Fernandez Del Rio E, Becona E. Effects of behavioural activation on substance use and depression: a systematic review. Subst Abuse Treat Prev Policy. 2018;13(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wang D, Zhou C, Zhao M, Wu X, Chang YK. Dose-response relationships between exercise intensity, cravings, and inhibitory control in methamphetamine dependence: An ERPs study. Drug Alcohol Depend. 2016;161:331–339. [DOI] [PubMed] [Google Scholar]
- 86.Rawson RA, Chudzynski J, Gonzales R, et al. The Impact of Exercise On Depression and Anxiety Symptoms Among Abstinent Methamphetamine-Dependent Individuals in A Residential Treatment Setting. J Subst Abuse Treat. 2015;57:36–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Campbell AN, Nunes EV, Matthews AG, et al. Internet-delivered treatment for substance abuse: a multisite randomized controlled trial. Am J Psychiatry. 2014;171(6):683–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. https://www.fda.gov/news-events/press-announcements/fda-permits-marketing-mobile-medical-application-substance-use-disorder.
- 89.Cook R, Quinn B, Heinzerling K, Shoptaw S. Dropout in clinical trials of pharmacological treatment for methamphetamine dependence: the role of initial abstinence. Addiction. 2017;112(6):1077–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Keith JR, Rapgay L, Theodore D, Schwartz JM, Ross JL. An assessment of an automated EEG biofeedback system for attention deficits in a substance use disorders residential treatment setting. Psychol Addict Behav. 2015;29(1):17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liang Y, Wang L, Yuan TF. Targeting Withdrawal Symptoms in Men Addicted to Methamphetamine With Transcranial Magnetic Stimulation: A Randomized Clinical Trial. JAMA psychiatry. 2018;75(11):1199–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Young KD, Siegle GJ, Zotev V, et al. Randomized Clinical Trial of Real-Time fMRI Amygdala Neurofeedback for Major Depressive Disorder: Effects on Symptoms and Autobiographical Memory Recall. Am J Psychiatry. 2017;174(8):748–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang D, Zhou C, Chang YK. Acute exercise ameliorates craving and inhibitory deficits in methamphetamine: An ERP study. Physiol Behav. 2015;147:38–46. [DOI] [PubMed] [Google Scholar]
- 94.Glasner-Edwards S, Mooney LJ, Ang A, et al. Mindfulness Based Relapse Prevention for Stimulant Dependent Adults: A Pilot Randomized Clinical Trial. Mindfulness (N Y). 2017;8(1):126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


