Abstract
Chronic pain is a common and costly condition, and some people with chronic pain engage in problematic opioid use. There is a critical need to identify factors underlying this co-occurrence, so that treatment can be targeted to improve outcomes. We propose that difficulty with emotion regulation (ER) is a transdiagnostic factor that underlies the co-occurrence of chronic pain and problematic opioid use (CP-POU). In this narrative review, we draw from prominent models of ER to characterize the literature characterizing ER in chronic pain and CP-POU. We conclude that chronic pain is associated with various ER difficulties, including emotion identification and the up- and down-regulation of both positive and negative emotion. Little research has examined ER specifically in CP-POU; however, initial evidence suggests CP-POU is characterized by difficulties with ER that are similar to those found in chronic pain more generally. There is great potential in expanding the treatment of ER to improve pain-related outcomes in chronic pain and CP-POU. More research is needed, however, to elucidate ER in CP-POU and to determine which types of ER strategies are optimal for different clinical presentations and categories of problematic opioid use.
Keywords: chronic pain, problematic opioid use, emotion regulation
Editor’s note.
This article is part of a special issue, “Psychology’s Role in Addressing the Dual Crises of Chronic Pain and Opioid-Related Harms,” published in the September 2020 issue of American Psychologist. Tonya M. Palermo and Robert D. Kerns served as guest editors of the special issue with Elizabeth A. Klonoff as advisory editor.
Introduction
Chronic pain—pain that persists or recurs for over 3 months—is common across the lifespan, occurring in approximately 10–30% of adults and children (Johannes, Le, Zhou, Johnston, & Dworkin, 2010; King et al., 2011; Nahin, 2015). Chronic pain can cause significant physical, social, and vocational impairment; and is comorbid with depression, anxiety, and posttraumatic stress disorder (PTSD) in both youth and adults (Asmundson & Katz, 2009; Noel, Groenewald, Beals-Erickson, Gebert, & Palermo, 2016; Rayner et al., 2016). Moreover, recent estimates suggest that one in four people with chronic pain engage in opioid use that is inconsistent with medical prescriptions, and one in ten meet criteria for opioid addiction (Vowles et al., 2015). Identifying transdiagnostic factors—processes that contribute to the development or maintenance of multiple diagnostic categories—that underlie both chronic pain and problematic opioid use (CP-POU) can enhance the precision and efficiency of psychological interventions to treat this common comorbidity. In this review, we examine difficulties with emotion regulation (ER), as a transdiagnostic factor that is important to CP-POU.
Elucidating the role of ER in chronic pain is particularly important because pain is defined as an unpleasant sensory and affective experience (Melzack, 1975); thus, regulating affect is central to the chronic pain experience. Difficulty with ER has been identified as a key transdiagnostic factor underlying both psychiatric and substance use disorders (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Fernandez, Jazaieri, & Gross, 2016). If ER represents a transdiagnostic factor underlying CP-POU, it can be targeted in interventions to improve outcomes in both chronic pain and problematic opioid use domains. Prescription opioid use is common among adults and adolescents with chronic pain. Recent nationally-representative studies estimate a 38% 12-month prevalence in adults and 20% lifetime prevalence in adolescents of using prescription opioids (Han et al., 2017; McCabe et al., 2017). Unfortunately, vague and evolving terminology poses a challenge to defining problematic opioid use. In this article, we adopt the terminology used by Vowles and colleagues (2015) who, based on expert recommendations, defined problematic opioid use as comprised of misuse (i.e., use inconsistent with physician prescription), abuse (i.e., intentional prescription opioid use for a nonmedical purpose), and addiction (i.e., continued use with actual or potential for harm).
In the current review, we define ER as the multifaceted process of modifying one’s emotional experience and trajectory towards a desired state. Many models have been developed to conceptualize the complexities of ER, and we draw on several of the most prominent in the current review. Gross’s Extended Process Model of ER (Gross, 1998, 2015) organizes ER into a series of progressive stages: emotion identification, strategy selection, and strategy implementation. ER strategies can be viewed as functioning to up-regulate (i.e., activate or enhance) or down-regulate (i.e., minimize, attenuate) emotion, and emotions can be organized into dimensions of negative affect (NA; general negative mood states) and positive affect (PA; general positive mood states). NA and PA occur independently of one another, such that people can experience both positive and negative emotions at any point in time (Watson & Clark, 1997). We categorize ER strategies in a 2 × 2 framework involving the down- and up-regulation of both NA and PA. A complementary model proposes a two-dimensional framework whereby ER strategies are classified as explicit (conscious) or implicit (non-conscious) as well as controlled (engaging top-down processes) or automatic (engaging few or no top-down processes; Braunstein, Gross, & Ochsner, 2017). Where possible, we characterize specific ER strategies according to this model throughout this review. Finally, ER is influenced by developmental and cultural factors, although this is often overlooked in research and practice; in our review, we highlight developmental and cultural considerations that define the context of ER. We acknowledge, however, that ER is a topic of rich debate, and no single model fully accounts for its complexities. Moreover, we appreciate the value of related frameworks, such as the earlier literature on coping (e.g., primary and secondary appraisal; problem- versus emotion-focused coping (Lazarus, 1991) and the debate regarding whether certain ER processes are best viewed as short-term strategies or as longer-term adaptations.
The overarching goal of this review is to examine ER as a transdiagnostic factor with treatment implications for CP-POU; accordingly, we focus on literature that has the clearest implications for clinical research, assessment, and intervention in people with chronic pain or CP-POU. Thus, we review literature that has examined emotion identification and ER strategy engagement in these populations, and we identify specific gaps that point the way to future research on CP-POU.
Emotion Regulation in Chronic Pain
We begin by describing emotion identification and then review ER strategy engagement, organized as the down- and up-regulation of NA and PA. In each section, we first highlight findings from the general chronic pain literature and then examine implications for CP-POU.
Emotional Identification
Emotion identification involves becoming aware of one’s emotions, differentiating among them, and labeling the correctly. Emotion identification is thought to precede ER strategy engagement, particularly explicit strategies, in order to achieve desired emotional states (Gross, 2015; Kashdan, Barrett, & McKnight, 2015). Some research has reported deficits in emotional awareness in people with chronic pain (Baeza-Velasco, Carton, Almohsen, Blotman, & Gely-Nargeot, 2012), which is associated with greater pain intensity (Smith et al., in press). Lane et al. (2009) proposed a neuroscience model suggesting that people with pain often have difficulties with awareness of emotional states and preferentially view and describe their experience in somatic terms. In addition to facilitating explicit ER, emotion identification has implicit ER benefits; for example, applying a verbal label to one’s affective state can reduce NA (Torre & Lieberman, 2018). Among patients with chronic pain, difficulties with affect labeling may result in less effective execution of explicit ER strategies and reduce access to affect labeling as an implicit form of ER. In the short-term, this could lead to worse pain, problematic opioid use, and deterioration in mood.
Alexithymia refers to the inability to label and describe one’s emotional state as well as a preference for externally-oriented rather than introspective thinking. A recent meta-analysis of 77 studies concluded that individuals with chronic pain have substantially elevated levels of alexithymia compared to pain-free controls, and alexithymia was positively related to pain intensity and pain interference as well as depression and anxiety (Aaron, Fisher, de la Vega, Lumley, & Palermo, 2019). Although much of this evidence is cross-sectional, a handful of prospective studies suggest that greater baseline alexithymia predicts poorer pain outcomes, such as persistent pain after surgery for breast cancer (Baudic et al., 2016). Alexithymia may even be a stronger predictor of change in symptom severity than anxiety and depression (Porcelli, De Carne, & Leandro, 2017). It should be noted, however, that critics have conceptualized alexithymia as a Western construct that pathologizes non-Western cultures that do not value individualism and emotional expression (Dere et al., 2013; Kirmayer, 1987).
Affect differentiation refers to the ability to experience PA and NA independently (Davis, Zautra, & Smith, 2004). During periods of heightened pain or stress, people are less able to differentiate between PA and NA, resulting in inverse correlations between PA and NA. In contrast, during periods of low pain or stress, PA and NA vary with greater independence (Davis et al., 2004; Potter, Zautra, & Reich, 2000). PA has been characterized as a “resilience resource” in patients with chronic pain due to its association with reduced negative affective reactivity to pain (Strand et al., 2006; Zautra, Johnson, & Davis, 2005). Thus, the ability to preserve PA despite the presence of NA is adaptive. Emotion differentiation refers to the ability to make fine-grained distinctions among emotional states. It is usually assessed in vivo using ecological momentary assessment or in the laboratory by evoking emotional experiences, and determined by examining within-person correlations of numerical emotion ratings (Kashdan et al., 2015). An enhanced ability to differentiate among emotional states improves the likelihood that ER will be successful and has been linked to better pain-related outcomes (Connelly et al., 2007).
Implications for co-occurring CP-POU
Few studies have examined emotion identification in people with CP-POU, although one study found that alexithymia was positively associated with prescription opioid misuse among people with chronic pain (Oberleitner et al., 2019). The larger literature on emotion identification in substance use disorders, however, consistently reports difficulties with emotion identification; for example, alexithymia is elevated in individuals with alcohol use disorders (Cruise & Becerra, 2018). A daily diary study showed that when college students experienced intense NA, greater momentary emotion differentiation resulted in less subsequent alcohol consumption (Kashdan, Ferssizidis, Collins, & Muraven, 2010). Higher emotion differentiation also predicted a lower likelihood of relapse following residential substance abuse treatment (Anand, Chen, Lindquist, & Daughters, 2017).These studies suggest that more precise awareness of negative emotions during stressful periods may protect against self-medicating NA.
ER Strategy Engagement
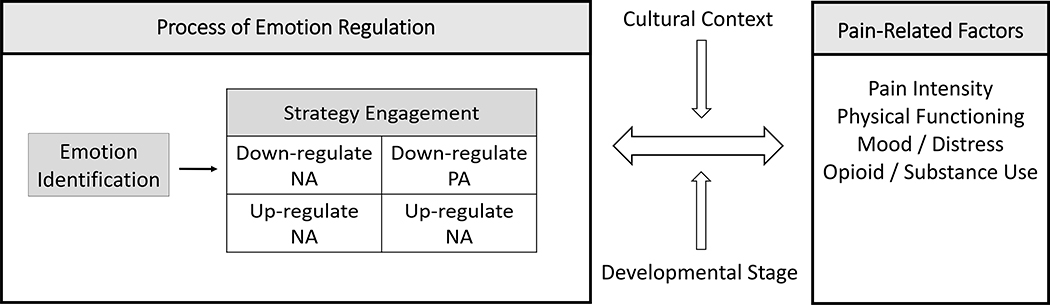
The engagement of ER strategies, whether explicit or implicit, is influenced by an individual’s goals and the potential competition between the short- and long-term implications of those goals (Gross & Thompson, 2007). Discrepancies between the proximal and distal outcomes of ER are especially relevant to people who have either chronic pain or CP-POU, given that these conditions are characterized by the tendency to seek immediate relief of salient aversive states at the potential cost of long-term function. For example, patients with chronic pain commonly withdraw from activity to protect against the possibility of short-term exacerbations of pain and NA, even though avoidance is associated with long-term physical and emotional decline (Vlaeyen & Linton, 2012). Similarly, opioid medications are optimally analgesic when used to relieve acute pain, but repeated use can engender physical and psychological dependence. Prescription opioid addiction is often marked by a cycle in which opioid withdrawal introduces a new aversive state of both pain and NA, distinct from that associated with the original chronic pain condition (Vowles et al., 2015).Thus, ER is often driven by goals that are short-term (e.g., pain relief) as well as long-term (e.g., eschewing patterns of opioid dependence). Below, we organize our review of ER strategies relevant to CP-POU according to the down- and up-regulation of both NA and PA. We outline possible short- and long-term outcomes of effective versus ineffective ER in Figure 1.
Figure 1.
Emotion Regulation in Chronic Pain
Note. This diagram depicts a bidirectional relationship between emotion regulation and pain-related factors, which is moderated by cultural context and developmental stage. “Process of Emotion Regulation“ is adapted from Gross (2015).
Down-Regulation of NA
The experience of chronic pain is often associated with periods of NA, which can be difficult to down-regulate. The inability to successfully down-regulate NA can exacerbate pain-related outcomes and lead to problematic opioid use. In both children and adults, the influential Fear Avoidance Model of chronic pain delineates how negative affective states (e.g., fear of pain, depression) and difficulty implementing effective strategies to down-regulate negative affect can lead to a perpetuating cycle that ultimately exacerbates pain and disability (Simons & Kaczynski, 2012; Vlaeyen & Linton, 2000). A systematic review of experimental studies examining classical conditioning in chronic pain suggests that this cycle may be perpetuated in part by implicit and automatic ER processes, whereby some patients with chronic pain have difficulty differentiating between threat and safety cues which could increase fear and anxiety (Harvie, Moseley, Hillier, & Meulders, 2017). The Fear Avoidance Model has garnered decades of empirical support (Vlaeyen & Linton, 2012) and a common goal of pain psychology interventions is to identify strategies typically associated with poor pain-related outcomes (e.g., pain catastrophizing) and replace them with explicit ER strategies more likely to lead to positive outcomes. For example, ER strategies such as cognitive reappraisal, relaxation, and behavioral activation can function to reduce NA and are common components of pain interventions (Ehde, Dillworth, & Turner, 2014).
Pain catastrophizing—an exaggerated negative cognitive orientation towards pain involving magnification of the threat value of pain, helplessness in the context of pain, and difficulty inhibiting pain-related thoughts—is a key component of the Fear Avoidance Model and has been studied extensively in both youth and adults with chronic pain (Miller, Meints, & Hirsh, 2018; Quartana, Campbell, & Edwards, 2009). Pain catastrophizing relates to negative expectancies, such as the belief that pain will never get better, which can exacerbate pain via nocebo effects which operate implicitly (Darnall & Colloca, 2018). Pain catastrophizing may emerge when attempts at ER via problem solving fail, which can fuel and exacerbate worry, ultimately increasing NA (Eccleston & Crombez, 2007). Higher pain catastrophizing is associated with worse pain severity and disability and altered pain processing (Goodin et al., 2009; Meints, Mawla, et al., 2019) as well as heightened psychological distress (Edwards, Cahalan, Mensing, Smith, & Haythornthwaite, 2011; Miller et al., 2018); and it prospectively predicts chronic pain-related outcomes, such as the development of persistent post-surgical pain (Theunissen, Peters, Bruce, Gramke, & Marcus, 2012). Pain catastrophizing is a common target of cognitive interventions for pain, and reductions in pain catastrophizing often mediate positive treatment outcomes (Smeets, Vlaeyen, Kester, & Knottnerus, 2006).
Cognitive reappraisal involves identifying thoughts that work against an individual and reframing them in more adaptive ways. Reappraisal is a core technique in cognitive behavioral therapy (CBT) for pain, and shifts in cognitive reappraisal over the course of CBT predict better treatment outcomes (Williams, Eccleston, & Morley, 2012). Reappraisal is often taught as an alternative to pain catastrophizing. When used as an explicit strategy, reappraisal is typically effortful and controlled; however, a goal of interventions is that reappraisal will become more implicit with continued practice. Over time, reappraisal may change expectations and beliefs about pain implicitly, which could lead to improvements in pain and affect (Atlas & Wager, 2012). It is important to note that although reappraisal is often considered an “adaptive” approach to down-regulating NA, reappraisal may not always be realistic or effective. For example, in very negative situations (e.g., living in an oppressive environment), it may be difficult to generate helpful reinterpretations. Reappraisal is also less likely to successfully down-regulate NA during high intensity stressors, as reappraisal requires greater cognitive resources than some other ER strategies (e.g., distraction; Ford & Troy, 2019).
Avoidance strategies—emotional, cognitive, and behavioral—aim to reduce actual or anticipated NA by preventing or delaying an aversive experience (Volders, Boddez, De Peuter, Meulders, & Vlaeyen, 2015). Avoidance can operate explicitly (e.g., conscious avoidance of an uncomfortable situation) or implicitly (e.g., occurring automatically as a result of conditioning links between avoidance behavior and reduced aversive states). Dozens of studies support the view that avoidance—although often reducing pain and NA in the short term—leads to long-term increases in pain, disability, and mood problems in both children and adults with chronic pain (Andrews, Strong, & Meredith, 2012; Kroska, 2016; Simons & Kaczynski, 2012). These findings underscore the importance of treatment techniques designed to promote approach strategies (e.g., behavioral activation, emotional disclosure) as a way of encouraging patients to confront experiences or stimuli that may be uncomfortable in the short-term but adaptive in the long-term.
As we indicate in Figure 1, the effectiveness of ER is influenced by cultural context and developmental stage. For example, Eccleston and colleagues (Eccleston, Fisher, Vervoort, & Crombez, 2012) proposed that pain catastrophizing may be developmentally normative in childhood—a time of imaginative thinking, egocentrism, and limited control over emotions and the external world. Moreover, children’s catastrophizing can function to elicit support from caregivers. Relying on external sources for ER (i.e., “extrinsic” ER) is common in childhood and a shift towards more internal, or “intrinsic,” ER occurs throughout adolescence and young adulthood (Gross, 2015). Cross-culturally, there are also differences in how intrinsic versus extrinsic ER is valued, and pain catastrophizing may represent a normative response to elicit support in some cultures (Meints, Cortes, Morais, & Edwards, 2019). A meta-analysis of associations between fear avoidance and chronic pain intensity from over 100 studies around the world found that cultural values moderate the association: the relationship between fear avoidance and pain intensity was stronger in cultures that placed greater value on collectivism (versus individualism), restraint (versus indulgence), and hierarchies of power (Kroska, 2016).
Implications for CP-POU
Problematic opioid use may serve to regulate NA: the vast majority (95%) of patients with CP-POU reported that their opioid use functioned in part to reduce anxiety, depression, and/or anger (Garland, Hanley, Thomas, Knoll, & Ferraro, 2015). Another study suggested that individuals with chronic pain who engaged in prescription opioid misuse compared to those who used opioids as prescribed had lower distress tolerance (McHugh et al., 2016). Alleviating NA via substance use creates powerful negative reinforcement contingencies which operate implicitly and can increase future substance use (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). Many studies have documented the close link between negative affective states and craving for illicit substances, including opioids (Koob & Volkow, 2016). Martel and colleagues showed that NA and pain catastrophizing were cross-sectionally associated with prescription opioid misuse, and that craving had an indirect effect on that relationship (Martel, Dolman, Edwards, Jamison, & Wasan, 2014; Martel, Jamison, Wasan, & Edwards, 2014). A daily diary study of adults with sickle cell disease showed that daily pain intensity and NA were associated with greater use of prescription opioid medication. Moreover, pain catastrophizing moderated the positive relationship between pain intensity and opioid use, such that even when pain intensity was low, relatively high pain catastrophizing was associated with greater opioid use (Finan et al., 2018). Among adults prescribed opioid medication for chronic low back pain, a daily diary study showed that greater opioid use was preceded by elevated pain and NA and followed by reductions in pain and NA (Carpenter, Lane, Bruehl, & Trull, 2019). This bidirectional relationship between opioid use and NA and pain was observed in individuals with no recent history of prescription opioid misuse, suggesting that opioid use may function to regulate affect even when used as prescribed.
Patients with chronic pain who misuse prescription opioids versus use as prescribed may have more pronounced difficulties down-regulating NA. A laboratory study showed that attempts to down-regulate NA via reappraisal were less successful in people with chronic pain who also misused prescription opioids than in those who used opioids as prescribed (Garland, Bryan, Nakamura, Froeliger, & Howard, 2017). In a laboratory study of opioid-treated patients with chronic pain, reappraisal-based ER was more common among individuals with low, versus high, risk for prescription opioid misuse, and was associated with lower emotional distress, diminished craving, and lower prescription opioid misuse (Garland et al., 2018). A recent controlled pilot intervention among patients with an opioid use disorder who were receiving methadone therapy targeted the down-regulation of NA via CBT strategies, including reappraisal. Those who received CBT reported greater abstinence from nonmedical opioid use than control patients receiving drug counseling (Barry et al., 2019).
With respect to developmental considerations, a nationally-representative survey revealed that use of prescribed opioids by 12th grade was associated with a 33% increase in the relative risk of opioid misuse later in adulthood. This effect was strongest among youth who reported little to no history of drug use and who reported strong disapproval of marijuana. The authors suggested that in opioid-naïve youth, prescription opioid use could have temporary ER benefits that reinforce future misuse, creating pathways for abuse and addiction (Miech, Johnston, O’Malley, Keyes, & Heard, 2015). Yet there is little research on ER in adolescents with CP-POU, and these hypothesized pathways have not been tested empirically. Adolescence can be a time of intense emotional experiences, particularly as ER strategies are developing (Nook et al., In Press). There is a need to understand how ER motivates or maintains problematic opioid use during this period of development and to tailor prevention efforts accordingly.
Up-Regulation of NA
The repeated finding that emotional avoidance is linked to the presence and severity of chronic pain suggests the potential value of reversing avoidance through emotional activation and processing. Such benefits may be particularly true when targeting primary negative emotions such as anger or sadness (McCollough & Magill, 2009) stemming from trauma and other life adversities—experiences that are more prevalent in people with chronic pain compared to controls (Asmundson & Katz, 2009). Some individuals access and express these negative emotions, for example, by journaling or talking to others about stressful experiences. In contrast, people who tend to suppress such negative emotions due to fear of undesirable psychological or interpersonal consequences may benefit from developing explicit strategies to up-regulate their NA.
Various interventions promote increased awareness of, or exposure to, negative emotions in people with chronic pain. For example, exposure-based treatment for chronic pain focuses on activating the fear associated with pain, movement, and potential tissue damage in a controlled setting in order to extinguish fear (Vlaeyen, Morley, Linton, Boersma, & de Jong, 2012). Such pain exposure therapy can be emotionally-challenging, however, and the benefits of this intervention may be enhanced by helping patients use explicit strategies to down-regulate their negative emotions while they engage in exposure (Boersma et al., 2019). Expressive writing or verbal emotional disclosure about stressful or traumatic experiences has been shown to have small but positive benefits for people with chronic pain (Lumley, Sklar, & Carty, 2011). Emotional awareness and expression therapy (EAET) was developed to address the unresolved trauma, psychological conflict, and relational problems that are commonly found in patients with chronic pain. EAET helps patients disclose emotionally-difficult experiences, overcome fears of expressing their avoided emotions, and make important changes in relationships (Lumley & Schubiner, 2019). Controlled trials have shown the pain-reducing benefits of EAET for patients with fibromyalgia, irritable bowel syndrome, chronic pelvic pain, and non-specific musculoskeletal pain (Carty et al., 2018; Jazi, Sultzer, Lumley, Osato, & Yarns, 2019; Lumley et al., 2017; Thakur et al., 2017). Therapies developed for trauma and psychological conflict, including eye movement desensitization and reprocessing (Tesarz, Wicking, Bernardy, & Seidler, 2019) and short-term psychodynamic therapy (Abbass et al., In Press) also show promise for patients with chronic pain. The goal of these exposure-based interventions is usually the reduction in pain and symptom severity, which contrasts with goal of CBT and acceptance-based interventions—improvements in functioning despite pain.
Awareness or experiencing avoided negative emotions plays a role in other chronic pain interventions. For example, a goal of mindfulness-based interventions is to increase awareness and acceptance of ongoing emotional experiences, and these interventions have been found to have positive, albeit modest benefits for people with chronic pain (Hilton et al., 2017). Through formal and informal exercises, CBT promotes exposure to activities that can elicit fear (e.g., through activity pacing) and other negative thoughts and emotions (e.g., through completion of automatic thought records; Ehde et al., 2014). Acceptance and Commitment Therapy encourages patients to engage with difficult thoughts and emotions (e.g., through mindfulness and cognitive diffusion exercises) to reduce associated fear (McCracken & Vowles, 2014). These exposure practices implicitly weaken or eliminate learned contingencies between fear and associated stimuli, including movement, thoughts, and emotions. Creating positive expectancies at the beginning of exposure treatment—by providing a treatment rationale, addressing specific concerns, offering reassurance, and delivering evidence-based pain education—likely contribute to improved treatment engagement and outcomes (Darnall & Colloca, 2018).
Implications for CP-POU
As with chronic pain generally, adaptive emotional expression is likely to be impaired in CP-POU specifically, although this has been little studied. One cross-sectional study found that ambivalence over emotional expression was positively associated with the presence of problematic prescription opioid use and opioid use disorder in people with chronic pain (Oberleitner et al., 2019). Results from a national survey in the United States found that individuals with both PTSD and chronic pain are at greater risk for an opioid use disorder (Bilevicius, Sommer, Asmundson, & El-Gabalawy, 2018). Some scholars propose that PTSD and opioid use disorders share neural underpinnings, such as deficiencies in the processing of natural rewards, which could drive their frequent co-occurrence (Elman & Borsook, 2019). Although additional research is needed to understand the drivers of CP-POU, the elevated rates of PTSD among these patients suggest the value of testing interventions that target trauma in this population, particularly treatments that process difficult trauma-related emotions.
Up-Regulation of PA
PA includes states that vary from high activation (e.g., excitement; enthusiasm) to low activation (e.g., calm; peaceful), and recent years have growing interest in ER strategies that up-regulate PA. Strategies such as humor and celebration often function to promote high activation PA, and strategies such as relaxation training or meditation training often function to promote low activation PA. In populations with chronic illness, engaging such ER strategies augment positive emotionality in the face of chronically aversive states including stress and pain (Tugade & Fredrickson, 2007). Practices that increase compassion towards others are common in mindfulness-based interventions, and pilot trials have found that compassion-focused interventions such as loving kindness meditation have resulted in improvements in pain-related outcomes (Carson et al., 2005; Penlington, 2019). Downward comparison (i.e., comparing oneself favorably to others) has been associated with increased PA and decreased depressive symptoms among patients with chronic pain (Affleck, Tennen, Urrows, Higgins, & Abeles, 2000; Jensen & Karoly, 1992). Similarly, benefit finding is associated with reduced functional impairments in patients with rheumatoid arthritis (Tennen, Affleck, Urrows, Higgins, & Mendola, 1992) and prospectively predicts improved PA in patients with fibromyalgia (Affleck, Urrows, Tennen, Higgins, & Abeles, 1996). Engaging strategies that up-regulate PA occur implicitly for some people, whereas others may benefit from learning explicit ER strategies to up-regulate their PA. Among patients with chronic pain, experimental PA manipulations have relieved acute pain (Finan & Garland, 2015), but positive psychology interventions have not yet yielded robust effects on chronic pain outcomes (Hausmann et al., 2018). Given substantial individual differences in ER abilities and needs, pre-treatment phenotyping may help determine which patients are most likely to benefit from interventions that seek to boost positive emotions.
Implications for CP-POU
Results from experimental studies suggest that patients with chronic pain and opioid misuse have reduced sensitivity to natural rewards (Garland, Bryan, Nakamura, et al., 2017). Clinical trials have demonstrated that Mindfulness Oriented Recovery Enhancement (MORE)—a mindfulness-based intervention that targets the processing of natural rewards—improves pain and reduces risk for problematic opioid use in patients with chronic pain. This intervention appears to operate by positive ER mechanisms, increasing subjective, physiological (Garland, Howard, Zubieta, & Froeliger, 2017), and neurophysiological (Garland, Froeliger, & Howard, 2015) responses to natural rewards. Improved reward responsiveness predicts improvements in pain-related outcomes (Garland & Howard, 2018) and reductions in opioid misuse (Garland, Atchley, Hanley, Zubieta, & Froeliger, 2019). Compared to support group controls, MORE patients were 2.75 times more likely to exhibit PA regulation in daily life (assessed by ecological momentary assessment), and increases in daily PA correlated with reductions in opioid misuse (Garland, Bryan, Finan, et al., 2017). However, the promising findings of MORE need replication, long-term follow-up, and comparison with other active treatments.
When evaluating the potential utility of targeting ER in treatments, it is important to consider patients’ baseline level of affective functioning and how that may affect implementation. Some studies suggest that anhedonia, a deficit in the ability to experience pleasure, is elevated among patients with chronic pain (Narayana et al., 2015) and those with an opioid use disorder (Kiluk, Yip, DeVito, Carroll, & Sofuoglu, 2019). In a recent meta-analysis across three samples of patients with chronic pain on chronic opioid therapy, anhedonia was more pronounced among those misusing opioids than medication-adherent patients (Garland, Trøstheim, Eikemo, Ernst, & Leknes, 2019). It is possible that a treatment designed specifically to increase PA in people with anhedonia would be particularly helpful for patients with CP-POU. One randomized trial in a non-pain sample of adults with elevated depression or anxiety and functional impairment showed that a treatment targeting the up-regulation of PA was superior to a CBT treatment that sought to down-regulate negative affect (Craske et al., 2019), suggesting anhedonia can be successfully targeted in treatment.
Down-Regulation of PA
Of the four categories of ER regulation we are proposing, the down-regulation of PA has received the least empirical attention in chronic pain and the broader literatures, so it is not clear how relevant this form of ER is for chronic pain. The primary functions of down-regulating PA include maintaining a realistic perspective (e.g., modulating high expectations), navigating social interactions (e.g., empathizing with a friend who has received bad news), and modulating outward expression (e.g., suppressing inappropriate laughter; Gross, 2014). Living with chronic pain often involves modulating hopes and expectations to maintain a realistic perspective of one’s functional ability, although this can be difficult, and such expectations likely vary within and between individuals and depends on context (Gross, 2014). Strategies such as activity pacing can help people with chronic pain recognize their limits and set activity goals that are in line with their functional abilities (Crombez, Eccleston, Van Damme, Vlaeyen, & Karoly, 2012).
Implications for CP-POU
We are not aware of research investigating PA down-regulation in CP-POU; however, problems with elevated PA may present several challenges to patients with CP-POU that should be investigated. Difficulties modulating high expectations and corresponding failure to meet high expectations could result in increased pain and negative affect, which might drive problematic opioid use. Difficulties down-regulating expectations related to opioid misuse, such as minimizing the risk of or ignoring signs of addiction, may also contribute to a greater likelihood of engaging in prescription opioid misuse.
Implications, Limitations, and Future Directions
This review describes ER difficulties in chronic pain and CP-POU. Our theoretical model highlights the potential value of conceptualizing ER with respect to stage (e.g., emotion identification, ER strategy), the up- and down- regulation of both PA and NA, consideration of the explicit-implicit and automatic-controlled dimensions, and cultural context and development stage. ER influences outcomes related to both pain and problematic opioid use and may represent a valuable transdiagnostic intervention target, particularly among people with CP-POU. However, additional theoretical and empirical development is needed to more comprehensively understand the role of ER in chronic pain and CP-POU and implications for treatment.
Although research has examined ER in chronic pain generally, few studies have examined ER in CP-POU specifically, and it is unclear whether findings from the chronic pain literature generalize to people with CP-POU. Given limited research in this area, it is also difficult to conclude whether difficulties with ER are more pronounced among individuals with chronic pain who engage in problematic opioid use compared to those who use opioid medications as prescribed. We have collapsed various types of problematic opioid use—misuse, abuse, and addiction—and ER may differ among these types of POU. The variability in how these terms are defined and assessed across studies poses challenges to a literature review. In addition, most studies in this nascent field are cross-sectional and correlational and have relatively small samples. Longitudinal, experimental, and intervention designs are needed and with better measurement of ER, such as ecological momentary or observational assessments.
One intriguing avenue of future research is elucidating the role of ER in the transition from opioid use as prescribed to misuse, abuse, and addiction. It is possible that difficulties with ER may lead to prescription opioid misuse in individuals with chronic pain who are prescribed opioid medications (Figure 1). For example, difficulties with emotion identification, a lack of explicit strategies to down-regulate negative affect, or a tendency to rely implicitly on opioid use as a strategy for reducing suffering could all contribute to prescription opioid misuse. Over time, reliance on ineffective ER strategies could strengthen behavioral contingencies between prescription opioid use and (temporary) mood improvements, contributing to prescription opioid abuse and addiction and other poor long-term outcomes. If different types of problematic opioid use are driven by different ER pathways, intervention targets and approaches should differ. Another limitation is that opioid-related outcomes are rarely reported in clinical trials of chronic pain interventions, even though many trials include patients who use opioids (Eccleston et al., 2017); thus, it is unclear whether these interventions reduce opioid misuse, or whether problematic opioid use and pain outcomes are best targeted separately. Whereas treating ER as a transdiagnostic factor may be appropriate for some forms of CP-POU (e.g., misuse), it may be inadequate for other forms of CP-POU (e.g., abuse).
It is important to recognize that negative emotions are not always “bad,” and their experience and expression can serve important psychological functions. Most ER research in chronic pain has focused on the problems associated with negative emotions and the value of improving people’s ability to down-regulate negative affect in treatment. In recent years, some studies have focused on the up-regulation of PA, and although initial results are encouraging, more research is needed to determine if the benefits are clinically significant (Hausmann et al., 2018). Relatively less attention has been given to the potential benefits of up-regulating negative emotions, and there may be value in distinguishing between primary and secondary emotions (McCollough & Magill, 2009). Whereas primary emotions are usually adaptive—motivating behavior to redress an interpersonal or intrapsychic difficulty (e.g., anger at violation or injustice, sadness at loss, fear of actual danger, guilt in response to doing harm), secondary emotions (e.g., anxiety, depression, shame, numbness, tension) are usually inhibitory—blocking adaptive behavior. It is reasonable that the former should be targeted for up-regulation via awareness or exposure, whereas the latter, for down-regulation.
Much of what we know about ER in chronic pain has focused on down-regulating negative affect specifically related to pain. There is value in examining how negative affect more broadly is regulated. For example, catastrophizing about pain likely correlates with a tendency to have catastrophic thoughts about other stressors as well, which may contribute to psychological comorbidity. Distinguishing among types of ER may be particularly important for understanding the complex presentation of CP-POU, which often co-occurs with psychopathology such as PTSD. There may be value in expanding pain-focused interventions, such as CBT, to address a broader range of ER strategies, or applying interventions such as EAET, which address current and developmental life stressors beyond pain.
It is possible that ER phenotype may inform ideal intervention delivery. ER assessment tools typically assess specific domains of ER. For example, widely used ER measures include the Toronto Alexithymia Scale – 20 item (Bagby, Parker, & Taylor, 1994), which assesses levels of alexithymia, and the Emotion Regulation Questionnaire (Gross & John, 2003), which assesses an individual’s tendency to utilize reappraisal and suppression ER strategies. An interesting future direction of this work is to develop a more comprehensive ER assessment tool, which could be useful in tailoring intervention delivery for people with CP-POU.
The current review presents ER research that has focused primarily on explicit and controlled forms of ER, reflecting the state of the clinical chronic pain and CP-POU literature. Although outside the scope of the current review, valuable experimental research has shed light on other forms of ER (i.e., implicit, automatic) which hold implications for the treatment of CP-POU. For example, placebo and nocebo effects alter analgesic response via expectancies that occur automatically and often outside of conscious awareness. Placebo and nocebo effects impact neurobiological and neurochemical aspects of pain processing (Atlas & Wager, 2012; Manaï, van Middendorp, Veldhuijzen, Huizinga, & Evers, 2019). Brief interventions designed to promote positive expectancies about pain interventions have been shown to result in reductions in pain intensity among individuals with chronic pain (Peerdeman et al., 2016). Placebo effects are often incorporated into psychological chronic pain interventions; for example, offering skillful psychosocial education about pain and creating positive expectancies about treatment. Experts have called for more explicit integration of placebo effects into the treatment of CP-POU (Darnall & Colloca, 2018; Manaï et al., 2019). Among individuals with CP-POU, positive expectancies about the analgesic effects of prescription opioid use may increase the experienced benefits of prescription opioids. Negative expectancies about the potential consequences of reducing prescription opioid use may reduce the benefits of other pain treatments, particularly if treatments are introduced as alternatives to prescription opioid use. Expectancies can be assessed and influenced at the beginning of treatment in order to optimize outcomes.
The success of ER is bounded, in part, by cultural differences and developmental stage. Although we refer to these factors in Figure 1, the more explicit integration of developmental stage and cultural context into empirical research is essential to better understand how they impact ER in individuals with CP-POU. Most ER research in chronic pain has been conducted on adults, which limits our knowledge of ER in pediatric samples; this is particularly problematic because ER evolves substantially with development. For example, from early childhood to young adulthood, emotions become increasingly complex, abstract, and mature (Nook et al., In Press) and ER becomes increasingly intrinsic. Youth with chronic pain have elevated rates of trauma and adverse childhood experiences compared to youth without pain (Noel et al., 2016), and results from a large prospective study show that childhood adversity is associated with chronic pain in adulthood (Jones, Power, & Macfarlane, 2009). It is important to understand how early life stressors and family factors impact ER and relate to the development of CP-POU.
Unfortunately, little research speaks to cultural factors that impact ER among individuals with CP or CP-POU. Emotions themselves have different labels, meanings, and values cross-culturally, which can influence ER and pain-related outcomes (Mesquita, Boiger, & De Leersnyder, 2016). For example, European Americans report valuing high activation versus low activation positive emotions whereas Asians and Asian Americans report the opposite pattern. Identifying cultural factors that contribute to ER in people with chronic pain will sharpen our understanding the nature of ER in this population and help us tailor interventions that are sensitive to differences that affect adjustment to pain. The majority of global opioid use occurs in the United States, where racial, ethnic, and socioeconomic biases in the treatment of adult and pediatric have been well established, and evidence of racial bias in the treatment of pain is evident in numerous studies (Hoffman, Trawalter, Axt, & Oliver, 2016). As we chart new territory into the role of ER in CP-POU, we must thoughtfully consider cultural differences to promote equitable and effective treatment for people with chronic pain.
Emotions follow complex and varied trajectories of duration and intensity (Kuppens & Verduyn, 2015) and at any given moment, an individual is balancing numerous, possibly conflicting, ER goals. ER is complex, and conceptual models of ER are evolving. We have incorporated frameworks from several prominent models of ER to organize our review of the literature; however, these models are not comprehensive. We organize ER strategy engagement into the down- and up- regulation of NA and PA, however, specific ER strategies operate across these categories. Engaging in strategies with the goal of down-regulating NA may result in the up-regulation of PA, and similar strategies may be employed with different ER goals. For example, an individual may engage in mindfulness-based practices to either reduce stress or to savor a positive experience depending on the context. There is need for continued theoretical and empirical advancement of ER in chronic pain and CP-POU. Laboratory studies are needed to elucidate ER in CP-POU more precisely. Most of the research on ER in chronic pain and CP-POU has relied of self-report measures, which can be confounded by social desirability or negative affect, and the use of objective measures is needed. In the broader ER literature, numerous studies have delineated neural processes involved ER, particularly the down-regulation of NA. Down-regulating NA generally augments activation in regions of the fronto-parietal network commonly associated with cognitive control (e.g., dorsolateral and ventrolateral prefrontal cortices), and attenuates the function of regions within the limbic system commonly associated with salience detection (e.g., amygdala and the ventral striatum; Ochsner, Silvers, & Buhle, 2012). Neuroimaging studies may help shed light on the neural underpinnings of ER in CP-POU.
Summary and Conclusion
Chronic pain is associated with difficulties in various aspects of ER. Numerous studies confirm that patients with chronic pain have difficulties executing explicit ER strategies for down-regulating negative affect; although, this research is limited by a poor understanding of the role of developmental and cultural factors in these processes. Less research has examined other forms of ER in chronic pain, and even fewer studies have examined ER difficulties in CP-POU. It appears that ER patterns may be similarly problematic in patients with CP-POU, although variation in problematic opioid use may relate to distinct ER difficulties. Research is needed to understand differences in ER among people with chronic pain who range from no opioid use, opioid use as prescribed, and varying degrees of problematic opioid use.
Difficulty down-regulating NA (e.g., fear of pain, craving) increases pain, disability, and problematic opioid use. Interventions that target the successful down-regulation of negative affect with the primary goal of promoting long-term function are the mainstay of CBT-based interventions for chronic pain. However, chronic pain and possibly CP-POU are also characterized by difficulties experiencing and processing negative emotion. Initial research findings from people with chronic pain suggests that experiencing and expressing avoided, adaptive negative emotions can lead to improved pain and mood, and these emotional processes can be targeted in newer therapies such as EAET. Chronic pain and CP-POU are also characterized by difficulty up-regulating positive emotions. Mindfulness practices, such as those in MORE, can promote savoring positive emotions, and initial evidence suggests this treatment can result in positive pain-related outcomes and reductions in opioid use in patients with CP-POU. Addressing gaps highlighted in this review, such as more comprehensive investigation of the up- and down- regulation of both positive and negative affect, is needed to inform the ideal treatment of CP-POU.
Over the past several decades, the cognitive and behavioral aspects of chronic pain have been well-explicated. Although the affective component of pain has long been acknowledged (Melzack, 1975); the scientific study of emotional phenomena—and ER in particular—is more recent (Gross & Barrett, 2013; Lumley, Cohen, et al., 2011). Applying affective science theory and research, such as that on ER, has the potential to increase our understanding of chronic pain and co-occurring problematic opioid use. In the face of dual crises of chronic pain and problematic opioid use, we must identify factors that underlie this co-occurrence and tailor biopsychosocial treatments accordingly. Difficulties with ER characterize both chronic pain and CP-POU and represent a transdiagnostic factor to be studied further and targeted in treatments.
Acknowledgments.
We thank the following funding sources for financial support: PCORI OTS-LBP-2017C1-6486 (RA, SW), R61AT010134 (PF), R01DA048206 (PF), U01HL150835 (PF), DOD W81XWH-16-2-0060 (SW), PCORI H133G140079 (SW), PCORI PCS-1402-10867 (SW), NIH P30AG064201 (FK), NIH R01AG058702 (FK), NIH UG1CA189824 (FW), and NIH U2CNR014637 (FK), and R21AR074020 (ML).
Biography



References
- Aaron RV, Fisher E, de la Vega R, Lumley MA, & Palermo TM (2019). Alexithymia in Individuals with Chronic Pain and its Relation to Pain Intensity, Physical Interference, Depression and Anxiety: A Systematic Review and Meta-Analysis. Pain, 160(5), 994–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbass A, Town J, Holmes H, Luyten P, Cooper A, Russell L, … Bernier D (In Press). Short-term Psychodynamic Psychotherapy for Functional Somatic Disorders: A Meta-analysis of Randomized Controlled Trials. Psychotherapy and Psychosomatics. [DOI] [PubMed] [Google Scholar]
- Affleck G, Tennen H, Urrows S, Higgins P, & Abeles M (2000). Downward comparisons in daily life with chronic pain: Dynamic relations with pain intensity and mood. Journal of Social and Clinical Psychology, 19(4), 499–518. [Google Scholar]
- Affleck G, Urrows S, Tennen H, Higgins P, & Abeles M (1996). Sequential daily relations of sleep, pain intensity, and attention to pain among women with fibromyalgia. Pain, 68(2–3), 363–368. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. [DOI] [PubMed] [Google Scholar]
- Anand D, Chen Y, Lindquist KA, & Daughters SB (2017). Emotion differentiation predicts likelihood of initial lapse following substance use treatment. Drug and Alcohol Dependence, 180, 439–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews NE, Strong J, & Meredith PJ (2012). Activity pacing, avoidance, endurance, and associations with patient functioning in chronic pain: a systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation, 93(11), 2109–2121. [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, & Katz J (2009). Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depression and Anxiety, 26(10), 888–901. [DOI] [PubMed] [Google Scholar]
- Atlas LY, & Wager TD (2012). How expectations shape pain. Neuroscience Letters, 520(2), 140–148. [DOI] [PubMed] [Google Scholar]
- Baeza-Velasco C, Carton S, Almohsen C, Blotman F, & Gely-Nargeot MC (2012). Alexithymia and emotional awareness in females with painful rheumatic conditions. Journal of Psychosomatic Research, 73(5), 398–400. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Parker JD, & Taylor GJ (1994). The twenty-item Toronto Alexithymia Scale—I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research, 38(1), 23–32. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological Review, 111(1), 33. [DOI] [PubMed] [Google Scholar]
- Barry DT, Beitel M, Cutter CJ, Fiellin DA, Kerns RD, Moore BA, … Ginn J (2019). An evaluation of the feasibility, acceptability, and preliminary efficacy of cognitive-behavioral therapy for opioid use disorder and chronic pain. Drug and Alcohol Dependence, 194, 460–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baudic S, Jayr C, Albi-Feldzer A, Fermanian J, Masselin-Dubois A, Bouhassira D, & Attal N (2016). Effect of alexithymia and emotional repression on postsurgical pain in women with breast cancer: A prospective longitudinal 12-month study. The Journal of Pain, 17(1), 90–100. [DOI] [PubMed] [Google Scholar]
- Bilevicius E, Sommer JL, Asmundson GJ, & El-Gabalawy R (2018). Posttraumatic stress disorder and chronic pain are associated with opioid use disorder: Results from a 2012–2013 American nationally representative survey. Drug and Alcohol Dependence, 188, 119–125. [DOI] [PubMed] [Google Scholar]
- Boersma K, Södermark M, Hesser H, Flink IK, Gerdle B, & Linton SJ (2019). The efficacy of a transdiagnostic emotion-focused exposure treatment for chronic pain patients with comorbid anxiety and depression: A randomized controlled trial. Pain, 160(8), 1708–1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braunstein LM, Gross JJ, & Ochsner KN (2017). Explicit and implicit emotion regulation: a multi-level framework. Social Cognitive and Affective Neuroscience, 12(10), 1545–1557. doi: 10.1093/scan/nsx096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter RW, Lane SP, Bruehl S, & Trull TJ (2019). Concurrent and lagged associations of prescription opioid use with pain and negative affect in the daily lives of chronic pain patients. Journal of Consulting and Clinical Psychology, 87(10), 872–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson JW, Keefe FJ, Lynch TR, Carson KM, Goli V, Fras AM, & Thorp SR (2005). Loving-kindness meditation for chronic low back pain: Results from a pilot trial. Journal of Holistic Nursing, 23(3), 287–304. [DOI] [PubMed] [Google Scholar]
- Carty JN, Ziadni MS, Holmes HJ, Tomakowsky J, Peters K, Schubiner H, & Lumley MA (2018). The effects of a life stress emotional awareness and expression interview for women with chronic urogenital pain: a randomized controlled trial. Pain Medicine, 20(7), 1321–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connelly M, Keefe FJ, Affleck G, Lumley MA, Anderson T, & Waters S (2007). Effects of day-to-day affect regulation on the pain experience of patients with rheumatoid arthritis. Pain, 131(1–2), 162–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Meuret AE, Ritz T, Treanor M, Dour H, & Rosenfield D (2019). Positive affect treatment for depression and anxiety: A randomized clinical trial for a core feature of anhedonia. Journal of Consulting and Clinical Psychology, 87(5), 457–471. [DOI] [PubMed] [Google Scholar]
- Crombez G, Eccleston C, Van Damme S, Vlaeyen JW, & Karoly P (2012). Fear-avoidance model of chronic pain: the next generation. The Clinical journal of pain, 28(6), 475–483. [DOI] [PubMed] [Google Scholar]
- Cruise KE, & Becerra R (2018). Alexithymia and problematic alcohol use: a critical update. Addictive Behaviors, 77, 232–246. [DOI] [PubMed] [Google Scholar]
- Darnall BD, & Colloca L (2018). Optimizing placebo and minimizing nocebo to reduce pain, catastrophizing, and opioid use: a review of the science and an evidence-informed clinical toolkit. In International Review of Neurobiology (Vol. 139, pp. 129–157): Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, & Smith BW (2004). Chronic pain, stress, and the dynamics of affective differentiation. Journal of Personality, 72(6), 1133–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dere J, Tang Q, Zhu X, Cai L, Yao S, & Ryder AG (2013). The cultural shaping of alexithymia: values and externally oriented thinking in a Chinese clinical sample. Comprehensive Psychiatry, 54(4), 362–368. [DOI] [PubMed] [Google Scholar]
- Eccleston C, & Crombez G (2007). Worry and chronic pain: a misdirected problem solving model. Pain, 132(3), 233–236. [DOI] [PubMed] [Google Scholar]
- Eccleston C, Fisher E, Thomas KH, Hearn L, Derry S, Stannard C, … Moore RA (2017). Interventions for the reduction of prescribed opioid use in chronic non-cancer pain. Cochrane Database of Systematic Reviews(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccleston C, Fisher EA, Vervoort T, & Crombez G (2012). Worry and catastrophizing about pain in youth: A reappraisal. Pain, 153(8), 1560–1562. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Cahalan C, Mensing G, Smith M, & Haythornthwaite JA (2011). Pain, catastrophizing, and depression in the rheumatic diseases. Nature Reviews Rheumatology, 7(4), 216. [DOI] [PubMed] [Google Scholar]
- Ehde DM, Dillworth TM, & Turner JA (2014). Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. American Psychologist, 69(2), 153. [DOI] [PubMed] [Google Scholar]
- Elman I, & Borsook D (2019). The Failing Cascade: Comorbid Post Traumatic-and Opioid Use Disorders. Neuroscience and Biobehavioral Reviews, 103, 374–383. [DOI] [PubMed] [Google Scholar]
- Fernandez KC, Jazaieri H, & Gross JJ (2016). Emotion regulation: a transdiagnostic perspective on a new RDoC domain. Cognitive Therapy and Research, 40(3), 426–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finan PH, Carroll CP, Moscou-Jackson G, Martel MO, Campbell CM, Pressman A, … Haythornthwaite JA (2018). Daily opioid use fluctuates as a function of pain, catastrophizing, and affect in patients with sickle cell disease: an electronic daily diary analysis. The Journal of Pain, 19(1), 46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finan PH, & Garland EL (2015). The role of positive affect in pain and its treatment. The Clinical journal of pain, 31(2), 177–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford BQ, & Troy AS (2019). Reappraisal reconsidered: A closer look at the costs of an acclaimed emotion-regulation strategy. Current Directions in Psychological Science, 28(2), 195–203. [Google Scholar]
- Garland EL, Atchley RM, Hanley AW, Zubieta J-K, & Froeliger B (2019). Mindfulness-Oriented Recovery Enhancement remediates hedonic dysregulation in opioid users: Neural and affective evidence of target engagement. Science advances, 5(10), eaax1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Bryan CJ, Finan PH, Thomas EA, Priddy SE, Riquino MR, & Howard MO (2017). Pain, hedonic regulation, and opioid misuse: modulation of momentary experience by mindfulness-oriented recovery enhancement in opioid-treated chronic pain patients. Drug and Alcohol Dependence, 173, S65–S72. [DOI] [PubMed] [Google Scholar]
- Garland EL, Bryan CJ, Nakamura Y, Froeliger B, & Howard MO (2017). Deficits in autonomic indices of emotion regulation and reward processing associated with prescription opioid use and misuse. Psychopharmacology, 234(4), 621–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Froeliger B, & Howard MO (2015). Neurophysiological evidence for remediation of reward processing deficits in chronic pain and opioid misuse following treatment with Mindfulness-Oriented Recovery Enhancement: exploratory ERP findings from a pilot RCT. Journal of Behavioral Medicine, 38(2), 327–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Hanley AW, Bedford CE, Zubieta J-K, Howard MO, Nakamura Y, … Froeliger B (2018). Reappraisal deficits promote craving and emotional distress among chronic pain patients at risk for prescription opioid misuse. Journal of Addictive Diseases, 37(1–2), 14–22. [DOI] [PubMed] [Google Scholar]
- Garland EL, Hanley AW, Thomas EA, Knoll P, & Ferraro J (2015). Low dispositional mindfulness predicts self-medication of negative emotion with prescription opioids. Journal of Addiction Medicine, 9(1), 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, & Howard MO (2018). Mindfulness-based treatment of addiction: current state of the field and envisioning the next wave of research. Addiction Science & Clinical Practice, 13(1), 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Howard MO, Zubieta J-K, & Froeliger B (2017). Restructuring hedonic dysregulation in chronic pain and prescription opioid misuse: effects of mindfulness-oriented recovery enhancement on responsiveness to drug cues and natural rewards. Psychotherapy and Psychosomatics, 86(2), 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Trøstheim M, Eikemo M, Ernst G, & Leknes S. J. P. m. (2019). Anhedonia in chronic pain and prescription opioid misuse. 1–12. [DOI] [PubMed] [Google Scholar]
- Goodin BR, McGuire L, Allshouse M, Stapleton L, Haythornthwaite JA, Burns N, … Edwards RR (2009). Associations between catastrophizing and endogenous pain-inhibitory processes: sex differences. The Journal of Pain, 10(2), 180–190. [DOI] [PubMed] [Google Scholar]
- Gross J (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. [Google Scholar]
- Gross J (2014). Emotion regulation: Conceptual and empirical foundations In Gross JJ (Ed.), Handbook of Emotion Regulation (pp. 3–20). In: New York, NY: Guilford Press. [Google Scholar]
- Gross J (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26(1), 1–26. [Google Scholar]
- Gross J, & Barrett LF (2013). The emerging field of affective science. Emotion, 13(6), 997. [DOI] [PubMed] [Google Scholar]
- Gross J, & John OP (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85(2), 348. [DOI] [PubMed] [Google Scholar]
- Gross J, & Thompson RA (2007). Emotion regulation: Conceptual foundations. In Gross J (Ed.), Handbook of emotion regulation. Ney York, NY: The Guilford Press. [Google Scholar]
- Han B, Compton WM, Blanco C, Crane E, Lee J, & Jones CM (2017). Prescription opioid use, misuse, and use disorders in US adults: 2015 National Survey on Drug Use and Health. Annals of Internal Medicine, 167(5), 293–301. [DOI] [PubMed] [Google Scholar]
- Harvie DS, Moseley GL, Hillier SL, & Meulders A (2017). Classical conditioning differences associated with chronic pain: a systematic review. The Journal of Pain, 18(8), 889–898. [DOI] [PubMed] [Google Scholar]
- Hausmann LR, Youk A, Kwoh CK, Gallagher RM, Weiner DK, Vina ER, … Ibrahim SA (2018). Effect of a positive psychological intervention on pain and functional difficulty among adults with osteoarthritis: a randomized clinical trial. JAMA network open, 1(5), e182533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, … Sorbero ME (2017). Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Annals of Behavioral Medicine, 51(2), 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman KM, Trawalter S, Axt JR, & Oliver MN (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences, 113(16), 4296–4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jazi AN, Sultzer D, Lumley M, Osato S, & Yarns B (2019). Emotional awareness and expression therapy or cognitive behavior therapy for the treatment of chronic musculoskeletal pain in older veterans: A pilot randomized clinical trial. The American Journal of Geriatric Psychiatry, 27(3), S112–S113. [Google Scholar]
- Jensen MP, & Karoly P (1992). Comparative self-evaluation and depressive affect among chronic pain patients: An examination of selective evaluation theory. Cognitive Therapy and Research, 16(3), 297–308. [Google Scholar]
- Johannes CB, Le TK, Zhou X, Johnston JA, & Dworkin RH (2010). The prevalence of chronic pain in United States adults: results of an Internet-based survey. The Journal of Pain, 11(11), 1230–1239. [DOI] [PubMed] [Google Scholar]
- Jones GT, Power C, & Macfarlane G (2009). Adverse events in childhood and chronic widespread pain in adult life: Results from the 1958 British Birth Cohort Study. Pain, 143(1–2), 92–96. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Barrett LF, & McKnight PE (2015). Unpacking emotion differentiation transforming unpleasant experience by perceiving distinctions in negativity. Current Directions in Psychological Science, 24(1), 10–16. [Google Scholar]
- Kashdan TB, Ferssizidis P, Collins RL, & Muraven M (2010). Emotion differentiation as resilience against excessive alcohol use an ecological momentary assessment in underage social drinkers. Psychological Science, 21(9), 1341–1347. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Yip SW, DeVito EE, Carroll KM, & Sofuoglu M (2019). Anhedonia as a key clinical feature in the maintenance and treatment of opioid use disorder. Clinical Psychological Science, 7(6), 1190–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, & MacDonald AJ (2011). The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain, 152(12), 2729–2738. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ (1987). Languages of suffering healing: Alexithymia as a social and cultural process. Transcultural Psychiatric Research Review, 24(2), 119–136. [Google Scholar]
- Koob GF, & Volkow ND (2016). Neurobiology of addiction: a neurocircuitry analysis. The Lancet Psychiatry, 3(8), 760–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroska EB (2016). A meta-analysis of fear-avoidance and pain intensity: the paradox of chronic pain. Scandinavian journal of pain, 13, 43–58. [DOI] [PubMed] [Google Scholar]
- Kuppens P, & Verduyn P (2015). Looking at emotion regulation through the window of emotion dynamics. Psychological Inquiry, 26(1), 72–79. [Google Scholar]
- Lane RD, Waldstein SR, Critchley HD, Derbyshire SW, Drossman DA, Wager TD, … Lovallo WR (2009). The rebirth of neuroscience in psychosomatic medicine, part II: clinical applications and implications for research. Psychosomatic Medicine, 71(2), 135–151. [DOI] [PubMed] [Google Scholar]
- Lazarus R. S. J. A. p. (1991). Cognition and motivation in emotion. 46(4), 352. [DOI] [PubMed] [Google Scholar]
- Lumley MA, Cohen JL, Borszcz GS, Cano A, Radcliffe AM, Porter LS, … Keefe FJ (2011). Pain and emotion: a biopsychosocial review of recent research. Journal of Clinical Psychology, 67(9), 942–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley MA, & Schubiner H (2019). Emotional Awareness and Expression Therapy for Chronic Pain: Rationale, Principles and Techniques, Evidence, and Critical Review. Current Rheumatology Reports, 21(7), 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley MA, Schubiner H, Lockhart NA, Kidwell KM, Harte SE, Clauw DJ, & Williams DA (2017). Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: a cluster-randomized controlled trial. Pain, 158(12), 2354–2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley MA, Sklar ER, & Carty JN (2011). Emotional disclosure interventions for chronic pain: from the laboratory to the clinic. Translational Behavioral Medicine, 2(1), 73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manaï M, van Middendorp H, Veldhuijzen DS, Huizinga TW, & Evers AW (2019). How to prevent, minimize, or extinguish nocebo effects in pain: a narrative review on mechanisms, predictors, and interventions. Pain reports, 4(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel M, Dolman AJ, Edwards RR, Jamison RN, & Wasan AD (2014). The association between negative affect and prescription opioid misuse in patients with chronic pain: the mediating role of opioid craving. The Journal of Pain, 15(1), 90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel M, Jamison RN, Wasan AD, & Edwards RR (2014). The association between catastrophizing and craving in patients with chronic pain prescribed opioid therapy: a preliminary analysis. Pain Medicine, 15(10), 1757–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, & Boyd CJ (2017). Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976–2015. Pediatrics, 139(4), e20162387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCollough L, & Magill M (2009). Affect-focused short-term dynamic therapy: Empirically supported strategies for resolving affect phobias. In Levy RA & Ablon JS (Eds.), Handbook of evidence-based psychodynamic psychotherapy (pp. 249–277). New York, NY: Humana Press. [Google Scholar]
- McCracken LM, & Vowles KE (2014). Acceptance and commitment therapy and mindfulness for chronic pain: Model, process, and progress. American Psychologist, 69(2), 178–187. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Weiss RD, Cornelius M, Martel MO, Jamison RN, & Edwards RR (2016). Distress intolerance and prescription opioid misuse among patients with chronic pain. The Journal of Pain, 17(7), 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meints SM, Cortes A, Morais CA, & Edwards RR (2019). Racial and ethnic differences in the experience and treatment of noncancer pain. Pain management, 9(3), 317–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meints SM, Mawla I, Napadow V, Kong J, Gerber J, Chan S-T, … Carriere J (2019). The relationship between catastrophizing and altered pain sensitivity in patients with chronic low-back pain. Pain, 160(4), 833–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melzack R (1975). The McGill Pain Questionnaire: major properties and scoring methods. Pain, 1(3), 277–299. [DOI] [PubMed] [Google Scholar]
- Mesquita B, Boiger M, & De Leersnyder J (2016). The cultural construction of emotions. Current Opinion in Psychology, 8, 31–36. [DOI] [PubMed] [Google Scholar]
- Miech R, Johnston L, O’Malley PM, Keyes KM, & Heard K (2015). Prescription opioids in adolescence and future opioid misuse. Pediatrics, 136(5), e1169–e1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MM, Meints SM, & Hirsh AT (2018). Catastrophizing, pain, and functional outcomes for children with chronic pain: a meta-analytic review. Pain, 159(12), 2442–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahin RL (2015). Estimates of pain prevalence and severity in adults: United States, 2012. The Journal of Pain, 16(8), 769–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayana A, Katz N, Shillington AC, Stephenson JJ, Harshaw Q, Frye CB, & Portenoy RK (2015). National Breakthrough Pain Study: prevalence, characteristics, and associations with health outcomes. Pain, 156(2), 252–259. [DOI] [PubMed] [Google Scholar]
- Noel M, Groenewald CB, Beals-Erickson SE, Gebert JT, & Palermo TM (2016). Chronic pain in adolescence and internalizing mental health disorders: A nationally representative study. Pain, 157(6), 1333–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noel M, Wilson AC, Holley A, Durkin L, Patton M, & Palermo TM (2016). Posttraumatic stress disorder symptoms in youth with vs without chronic pain. Pain, 157(10), 2277–2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nook EC, Stavish CM, Sasse SF, Lambert HK, Mair P, McLaughlin KA, & Somerville LH (In Press). Charting the development of emotion comprehension and abstraction from childhood to adulthood using observer-rated and linguistic measures. Emotion. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberleitner LM, Lumley MA, Grekin ER, MZ Smith K, Loree AM, Carty JN, & Valentino D (2019). Problematic prescription opioid use in a chronic pain treatment facility: The role of emotional processes. Substance Use and Misuse, 54(3), 495–505. [DOI] [PubMed] [Google Scholar]
- Ochsner KN, Silvers JA, & Buhle JT (2012). Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Annals of the New York Academy of Sciences, 1251, E1–E24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peerdeman KJ, van Laarhoven AI, Keij SM, Vase L, Rovers MM, Peters ML, & Evers AW (2016). Relieving patients’ pain with expectation interventions: a meta-analysis. Pain, 157(6), 1179–1191. [DOI] [PubMed] [Google Scholar]
- Penlington C (2019). Exploring a compassion-focused intervention for persistent pain in a group setting. British journal of pain, 13(1), 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porcelli P, De Carne M, & Leandro G (2017). The role of alexithymia and gastrointestinal-specific anxiety as predictors of treatment outcome in irritable bowel syndrome. Comprehensive Psychiatry, 73, 127–135. [DOI] [PubMed] [Google Scholar]
- Potter PT, Zautra AJ, & Reich JW (2000). Stressful events and information processing dispositions moderate the relationship between positive and negative affect: Implications for pain patients. Annals of Behavioral Medicine, 22(3), 191. [DOI] [PubMed] [Google Scholar]
- Quartana PJ, Campbell CM, & Edwards RR (2009). Pain catastrophizing: a critical review. Expert Review of Neurotherapeutics, 9(5), 745–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayner L, Hotopf M, Petkova H, Matcham F, Simpson A, & McCracken LM (2016). Depression in patients with chronic pain attending a specialised pain treatment centre: prevalence and impact on health care costs. Pain, 157(7), 1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons LE, & Kaczynski KJ (2012). The Fear Avoidance model of chronic pain: examination for pediatric application. The Journal of Pain, 13(9), 827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeets RJ, Vlaeyen JW, Kester AD, & Knottnerus JA (2006). Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. The Journal of Pain, 7(4), 261–271. [DOI] [PubMed] [Google Scholar]
- Smith R, Gudleski GD, Lane RD, & Lackner JM (in press). Higher Emotional Awareness Is Associated With Reduced Pain in Irritable Bowel Syndrome Patients: Preliminary Results. Psychological Reports. [DOI] [PubMed] [Google Scholar]
- Strand EB, Zautra AJ, Thoresen M, Ødegård S, Uhlig T, & Finset A. J. J. o. p. r. (2006). Positive affect as a factor of resilience in the pain—negative affect relationship in patients with rheumatoid arthritis. 60(5), 477–484. [DOI] [PubMed] [Google Scholar]
- Tennen H, Affleck G, Urrows S, Higgins P, & Mendola R (1992). Perceiving control, construing benefits, and daily processes in rheumatoid arthritis. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement, 24(2), 186. [Google Scholar]
- Tesarz J, Wicking M, Bernardy K, & Seidler GH (2019). EMDR therapy’s efficacy in the treatment of pain. Journal of EMDR Practice and Research, 13(4), 337–344. doi: 10.1891/1933-3196.13.4.337 [DOI] [Google Scholar]
- Thakur ER, Holmes HJ, Lockhart NA, Carty JN, Ziadni MS, Doherty HK, … Lumley MA (2017). Emotional awareness and expression training improves irritable bowel syndrome: A randomized controlled trial. Neurogastroenterology and Motility, 29(12), e13143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theunissen M, Peters ML, Bruce J, Gramke H-F, & Marcus MA (2012). Preoperative anxiety and catastrophizing: a systematic review and meta-analysis of the association with chronic postsurgical pain. The Clinical journal of pain, 28(9), 819–841. [DOI] [PubMed] [Google Scholar]
- Torre JB, & Lieberman MD (2018). Putting feelings into words: Affect labeling as implicit emotion regulation. Emotion Review, 10(2), 116–124. [Google Scholar]
- Tugade MM, & Fredrickson BL (2007). Regulation of positive emotions: Emotion regulation strategies that promote resilience. Journal of happiness studies, 8(3), 311–333. [Google Scholar]
- Vlaeyen J, & Linton SJ (2000). Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain, 85(3), 317–332. [DOI] [PubMed] [Google Scholar]
- Vlaeyen J, & Linton SJ (2012). Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain, 153(6), 1144–1147. [DOI] [PubMed] [Google Scholar]
- Vlaeyen J, Morley S, Linton SJ, Boersma K, & de Jong J (2012). Pain-related fear: exposure based treatment for chronic pain: IASP press. [Google Scholar]
- Volders S, Boddez Y, De Peuter S, Meulders A, & Vlaeyen JW (2015). Avoidance behavior in chronic pain research: a cold case revisited. Behaviour Research and Therapy, 64, 31–37. [DOI] [PubMed] [Google Scholar]
- Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, & van der Goes DN (2015). Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain, 156(4), 569–576. [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1997). Measurement and mismeasurement of mood: Recurrent and emergent issues. Journal of Personality Assessment, 68(2), 267–296. [DOI] [PubMed] [Google Scholar]
- Williams AC, Eccleston C, & Morley S (2012). Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database of Systematic Reviews(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zautra AJ, Johnson LM, & Davis MC (2005). Positive affect as a source of resilience for women in chronic pain. Journal of Consulting and Clinical Psychology, 73(2), 212. [DOI] [PMC free article] [PubMed] [Google Scholar]