Abstract
Background
Many reviews and meta-analyses had been conducted to investigate risk factors for sleep disorders in the general population. However, no similar research has been performed in the military population though insomnia and sleep-disordered breathing are quite prevalent in that population.
Objectives
To investigate risk factors for insomnia and sleep-disordered breathing in military personnel.
Methods
A systematic literature search was performed from inception to March 2021 and 6496 records were produced. Two authors independently screened records for eligibility. Results were presented as odds ratios, and a random-effect model was used to pool results. Data analysis was performed respectively according to military personnel type (i.e., veteran, active-duty personnel). Risk factors were sorted into three categories: sociodemographic, army-specific, and comorbidity. This meta-analysis was registered in PROSPERO before data analysis (registration No: CRD42020221696).
Results
Twenty-seven articles were finally included in the quantitative analysis. For sleep-disordered breathing in active-duty personnel, four sociodemographic (i.e., overweight/obesity, higher body mass index, male gender, >35 years old) and one comorbidity (i.e., depression) risk factors were identified. For insomnia in active-duty personnel, four sociodemographic (i.e., aging, alcohol dependence, white race, and female gender), two army-specific (i.e., deployment experience, combat experience), and four comorbidity (i.e., depression, post-traumatic stress disorder, traumatic brain injury, and anxiety) risk factors were identified. For insomnia in veterans, one army-specific (i.e., combat experience) and one comorbidity (i.e., post-traumatic stress disorder) risk factor was identified.
Conclusions
Several risk factors were identified for insomnia and sleep-disordered breathing in the current meta-analysis. Risk factors for veterans and active-duty personnel were partially different. Research on sleep breathing disorders remains limited, and more convincing evidence would be obtained with more relevant studies in the future.
Introduction
Healthy sleep requires good sleep quality, adequate sleep duration, regular circadian rhythm, and absence of sleep disorders. Military personnel have more difficulties fulfilling these requirements, because they need to keep up with their daily training and carry out deployment or combat tasks. Military tasks are always of high intensity and require the personnel to operate under extreme and harsh conditions, including cold stress [1], heat stress [2], and high altitude [3]. When deployed, the disturbed time schedule and latent danger place extreme pressure on soldiers, damaging their daily sleep patterns. A newly formed 5 h on/10 h off time schedule on navy ships results in poor sleep hygiene and abundant sleep debt [4]. Consensus has been reached that adults should sleep at least seven hours per night on a regular basis to maintain health whereas sleep need increases to nine hours in adolescence and early adulthood [5, 6]. This age range coincides with active-duty military personnel [7]. However, it is quite common for military personnel to sleep less than six hours per night [8]. A study on militarily relevant tasks after long-term sleep loss finds that mental-effort-requiring tasks were more influenced than those requiring only physical energy [9].
The prevalence of sleep disorders are surprisingly high in military personnel [10]. Insomnia and sleep-disordered breathing (SDB) are quite prevalent in the military [11–14]. Insomnia is defined as difficulties initiating or maintaining sleep or waking up too early and inability to return to sleep, accompanied by fatigue during wakefulness [15]. The common diagnosis tool for insomnia is the International Classification of Diseases and International Classification of Sleep Disorders. The Insomnia Severity Index (ISI) [16], a self-reported questionnaire, is also widely used for identifying insomnia with higher scores indicating more severe insomnia symptoms. Insomnia could cause serious harm to the military as it can affect cognitive functions such as working memory [17], executive function [17], and declarative memory [18] and increase the risk for motor vehicle accidents among military personnel [19]. SDB, defined as breathing problems during sleep, includes obstructive sleep apnea (OSA), central sleep apnea (CSA), sleep-related hypoventilation disorders, and sleep-related hypoxemia disorder [20–22]. Growing evidence indicates that apnea and subsequent compensatory hyperpnea could have adverse cardiovascular consequences [23], and OSA has a positive correlation with death [24]. SA could weaken working memory, executive functions, and many other aspects of cognition ability [25].
Potential sociodemographic risk factors for developing SDB and insomnia are of vital importance because officers could know in advance which population is at higher risk for developing certain sleep disorders and implement early intervention for high-risk groups. Military personnel are more likely to experience traumatic events during deployment and develop comorbidities such as post-traumatic stress disorder (PTSD) [26] and depression [27] as a result. Poorer sleep quality [28] and higher prevalence of OSA [29] were found in patients with PTSD. It had been widely agreed that depression can lead to sleep impairment. Traumatic brain injury (TBI) could result in poorer sleep quality [30] and higher prevalence of insomnia [31]. Therefore, this study planned to examine three major categories of risk factors: sociodemographic, army-specific, and comorbidity.
Young and Punjabi [32, 33] reviewed risk factors for OSA in a nonmilitary sample. Risk factors for SDB in the general population are obesity [32], snoring [34, 35], aging [32, 36, 37], and cardiovascular factors such as hypertension [38, 39], smoking [32, 33], and alcohol dependence [33]. Ohayon [31] reviewed the epidemiology of insomnia in the general sample. Notwithstanding, there was no systematic review focusing on risk factors for sleep disorders in the military to our best knowledge.
We aimed to investigate risk factors (i.e., sociodemographic, army-specific, and comorbidity) for insomnia and SDB in the military.
Materials and methods
The literature search process was performed according to the Preferred Reporting Items for Systemic Reviews and Meta-Analysis (PRISMA) checklist [40] (S2 File) and was registered with PROSPERO (S1 File) before the data analysis (registration No: CRD42020221696).
Database searching
PubMed, Embase, PsycINFO, and Web of Science were searched from inception to April 2020, limited to papers published in the English language. Search terms were as follows: sleep OR sleep problem OR sleep disorder OR sleep disturbance AND veteran* OR soldier* OR army OR navy OR marine OR troop OR air force OR armed OR peacekeeper* OR defense AND risk OR predictor* OR prediction OR predisposition. The full search strategy is presented in S3 File. In all, 5105 records were identified through searching while another nine were included by hand-searching the references of meta-analyses and reviews in this area. The search was further updated in March 2021 to ensure the completeness of our search scope.
Eligibility criteria
Four independent authors (Huang, Xu, Meng, Li) reviewed all titles and abstracts to determine eligibility. Full texts were screened when eligibility could not be determined by the titles or abstract alone, and any discrepancies were resolved by consensus to identify articles that met the following inclusion criteria: (a) investigating risk factors for insomnia and SDB in military populations; (b) including a sample of military personnel, veterans, or both; (c) containing effect sizes such as risk ratio (RR), odds ratio (OR), hazard ratio (HR) and corresponding 95% confidence interval (CI), or standard error (SE) or data able to calculate the above parameters; (d) study design: cohort, case-control, or cross-sectional.
The exclusion criteria were as follows: (a) including both active-duty personnel and veterans while data of each group cannot be extracted separately; (b) having no controls or comparative group who are not exposed to studied risk factor; (c) not containing data essential to calculate needed effect sizes and cannot be obtained from authors; (d) using continuous data to describe sleep disorder severity; (e) not published in English.
Data extraction
A Standardized Excel form was used by two independent authors to reduce probable errors. The data extraction form involved (a) general information: study design, country, subject type, male proportion, average age, and standard deviation (SD), sleep disorder type, diagnostic method, etc.; (b) sociodemographic factors: body mass index (BMI), marital status, race, gender, age, education level, alcohol dependence, smoking, income, etc.; (c) army-specific factors: rank, combat experience and time, deployment experience and time, military experience, etc.; and (d) comorbidities: PTSD, TBI, depression, anxiety, etc. The above factors and corresponding events and totals for cases and controls or calculated effect sizes such as ORs, RRs, or HRs were extracted. Crude effect sizes were extracted to reduce the bias brought by different confounders of different studies. Adjusted effect sizes were included when they were the only results.
Outcome measurement
The primary outcomes of this meta-analysis were risk factors for insomnia and SDB in military communities. The association between sleep disorders and associated factors was assessed using OR. Therefore, the merged results were all presented as OR and 95%CI.
Study quality assessment
Two authors (Huang, Xu) assessed the quality of the included studies separately. The Newcastle-Ottawa Scale, one of the most commonly used tools for assessing methodological quality of non-randomized studies, was utilized to assess the quality of included cohort and case control studies. Each article was evaluated from three aspects (i.e., selection, comparability, exposure/outcome) including eight detailed questions. The Agency for Healthcare Research and Quality was utilized to assess cross-sectional studies. An answer of “NO or “UNCLEAR” is scored “0”, and “YES” is scored “1”.
Statistical analysis
We examined risk factors for insomnia and SDB in military personnel based on OR or original data, which include number of participants exposed and not exposed to risk factors and number of participants with sleep disorders in the two groups. Considering variation in the diagnostic tools, participant characteristics, and study type of the included articles, a random-effect model was used to estimate the pooled ORs with 95% CIs. I2 statistic was used to measure heterogeneity with I2 values below 25%, 50%, and 75% representing low, moderate, and high level of heterogeneity, respectively. Further subgroup and sensitivity analyses to control heterogeneity level were not feasible as most of the outcomes contained limited number of studies due to detailed sorting based on their characteristics.
Data were analyzed using Revman 5.4 and Stata 16. For studies only providing continuous data for probable factors (e.g., specific BMI instead of obese or not) and those still meaningful after being transferred into ORs, standard mean difference (SMD) was transferred into OR based on the assumption that continuous variables within two intervention groups have equal SD logistic distributions [41, 42], using the following equation:
The corresponding SE can be calculated from 95%CI by the following equation:
Outliers were identified by visually checking the forest plots, and those that do not overlap with the 95%CI of pooled effect size were removed from the quantitative analysis.
As for publication bias assessment, for risk factors containing more than 10 articles, funnel plot was used to assess publication bias. For those containing less than 10 but more than 2 articles, Egger’s test was utilized in factors using lnOR and corresponding SE to merge results, and Harbord’s test was utilized in factors using original data (i.e., number of participants exposed or not exposed to risk factor and corresponding number of participants developing targeted sleep disorder) to merge results.
Results
Study selection
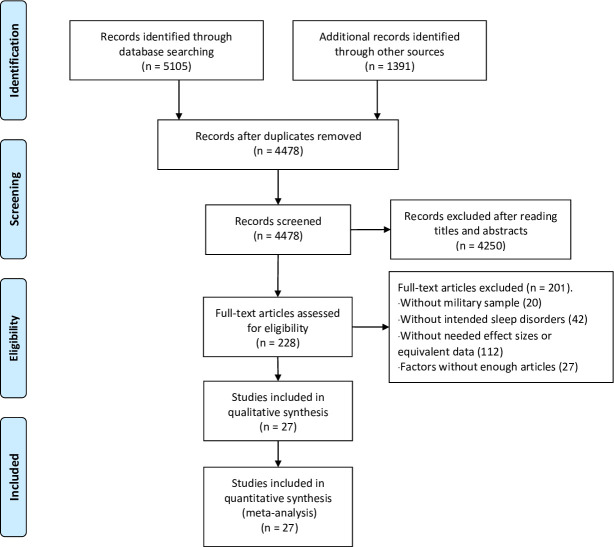
PubMed, Embase, PsycINFO, and Web of Science were searched from inception to April 2020 with 5105 records obtained. Nine records were included by hand-searching the references of meta-analyses and reviews in this area; 3714 records remained after the removal of duplications. Two authors independently screened the titles and abstracts of the remaining studies and excluded 3530 studies that did not meet eligibility requirements (i.e., no military participants, irrelevant of sleep disorders, no needed effect sizes). One hundred eighty-four full texts were read independently by two trained assistants; 139 records were excluded for not meeting the inclusion criteria. Twenty-five records were further excluded since their studying factors did not contain a sufficient volume of literature to perform meta-analysis. Another three records were excluded for mixed data for veterans and active-duty personnel with 17 articles included for quantitative analysis in the first stage of search. We updated our search in March 2021, included another 1382 records, and included 10 more articles for quantitative analysis after screening. As a result, a total of 27 articles were included in this meta-analysis. See the process in Fig 1.
Fig 1. PRISMA flow-chart.
Study characteristics
Detailed information of the 27 selected articles is presented in Table 1. The detailed information of quality assessment is provided in S4 File. No publication bias exist except for one factor (i.e., white race for insomnia risk in veterans) (S5 File). Thirteen studies explored SDB’s risk factors, and 19 explored risk factors for insomnia. SDB patients were diagnosed using the Berlin Questionnaire (BQ) in two studies [34, 43], the 9th and 10th edition of ICD in three studies [44–46], the 2nd or 3rd edition of ICSD in two studies [47, 48], the Apnea Hypopnea Index (AHI) in four studies [47–50], previously documented information in two studies [51, 52], self-reported SDB in one study [53], and no diagnose tool in one study [54]. As for the definition of insomnia, two studies used the 9th and 10th edition of ICD [44, 55], three used the 2nd and 3rd edition of ICSD [47, 48, 56], seven used the ISI [48, 57–62], one used the Brief Insomnia Questionnaire (BIQ) [63], four used a self-edited questionnaire [63–66], two used self-reported data [53, 67], and one used documented information [52].
Table 1. Study characteristics.
| Included study | Study design | Participant type | Male/Female | Age | Disorder type | Diagnose tool |
|---|---|---|---|---|---|---|
| M (SD) | ||||||
| Baird et al. 2018 [51] | cross-sectional | Veterans | 214/0 | 69 (4) | SDBa | Documented diagnosis |
| Cairns et al. 2017 [49] | cross-sectional | Veterans | 1370/130 | 52.8 (13.5) | SDBa | AHId |
| Crump et al. 2019 [45] | cohort | Active-duty personnel | 1547478/0 | 18 | SDBa | ICDe-10 |
| Langton et al. 2016 [46] | cohort | Active-duty personnel | 467885/ | / | SDBa | ICDe-9 |
| Lee et al. 2013 [34] | cross-sectional | Active-duty personnel | 665/0 | 21.76 (1.19) | SDBa | BQc |
| Mysliwiec et al. 2015 [54] | cross-sectional | Active-duty personnel | 106/3 | 34.3 (8.23) | SDBa | / |
| Pilakasiri et al. 2018 [43] | cross-sectional | Active-duty personnel | 1036/71 | 26.9 (8) | SDBa | BQc |
| Iqbal et al. 2016 [50] | cross-sectional | Veterans | 214/0 | 63 (6) | SDBa | AHId |
| Mysliwiec et al. 2013 [68] | cross-sectional | Active-duty personnel | 676/49 | 35.5 (8.6) | SDBa, Insomnia | AHId, ICSDg-2 |
| Martindale et al. 2020 [52] | cross-sectional | Veterans | 256/37 | 41.63 (10.14) | SDBa, Insomnia | Documented diagnosis |
| Caldwell et al. 2019 [44] | cohort | Active-duty personnel | / | / | SDBa, Insomnia | ICDe-9 |
| Foster et al. 2017 [48] | cross-sectional | Active-duty personnel | 108/101 | 34.3 (8.52) | SDBa, Insomnia | ICSDg-3, ISIh, AHId |
| Kanefsky et al. 2019 [69] | cross-sectional | Active-duty personnel | 113/5 | 32.82 (7.73) | SDBa, Insomnia | Self-reported |
| Hermes et al. 2014 [55] | cross-sectional | Veterans | 5037101/492099 | 61.2 (16.3) | Insomnia | ICDe-9 |
| Klingaman et al. 2017 [63] | cross-sectional | Active-duty personnel | 18790/2514 | 27 (7.4) | Insomnia | SEQf |
| Lopez et al. 2013 [64] | cross-sectional | Veterans | 144/22 | 56 (15) | Insomnia | SEQf |
| Martin et al. 2017 [56] | cross-sectional | Veterans | 0/660 | 50.9 (17.7) | Insomnia | ICSDg-2 |
| Taylor et al. 2016 [57] | cross-sectional | Active-duty personnel | 3719/359 | 27.43 (6.14) | Insomnia | ISIh |
| Pettersson et al. 2016 [65] | cross-sectional | Veterans | 966/115 | 36.1 (9.9) | Insomnia | SEQf |
| Adrian et al. 2018 [58] | cross-sectional | Active-duty personnel | 2640/239 | / | Insomnia | ISIh |
| Colvonen et al. 2020 [59] | cross-sectional | Veterans | 4597/955 | 34.81 (9.07) | Insomnia | ISIh |
| Mosti et al. 2019 [70] | cross-sectional | Active-duty personnel | 580023/90524 | 29.5 (7.5) | Insomnia | BIQi |
| King et al. 2017 [60] | cohort | Veterans | 247/21 | 31 (8) | Insomnia | ISIh |
| Scoglio et al. 2017 [61] | cross-sectional | Veterans | 118/46 | 35.15 (9.19) | Insomnia | ISIh |
| Sandman et al. 2013 [67] | cross-sectional | Veterans | 23005/23669 | / | Insomnia | Self-reported |
| Hu et al. 2020 [66] | cross-sectional | Veterans | 1025/49 | / | Insomnia | SEQf |
| Gaffey et al. 2020 [62] | cross-sectional | Veterans | 534/575 | 43.8 (10.9) | Insomnia | ISIh |
Note
a: Sleep-disordered breathing
b: Neurobehavioral Symptom Inventory
c: Berlin Questionnaire
d: Apnea Hypopnea Index
e: International Classification of Diseases
f: Self-edited questionnaire
g: International Classification of Sleep Disorders
h: Insomnia Severity Index
i: Brief Insomnia Questionnaire
/: no corresponding data.
The total sample consisted of 21,923,699 in the military population and 28,223 in the general population. The percentage of male participants was 91.73% in the military population and 45.93% in the general population. The ages ranged from less than 20 years old to more than 75 years old. Of the 27 studies, 13 included a total of 16,335,530 active-duty military personnel while the remaining 14 included a total of 5,588,169 veterans. Twenty-one studies were in the U.S., and the remaining six were in Australia (one), Sweden (two), Korea (one), Thailand (one), and Finland (one). All studies were written in English. Publish dates ranged from 2013 to 2020. Extracted factors had to contain a minimum of two articles to be entered into the analysis. Final presented outcomes were divided into three groups: sociodemographic, army-specific, and comorbidities. Information was mostly collected through network or questionnaire. Risk or preventive factors for SDB and insomnia in active-duty personnel or veterans were discussed, respectively.
Risk factors for SDB in active-duty personnel
Sociodemographic factors
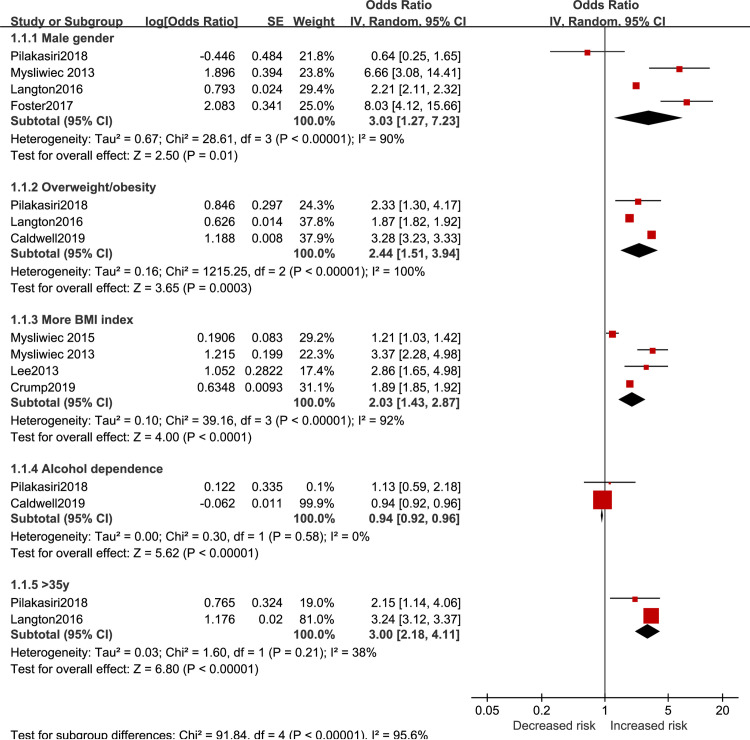
The results of sociodemographic effect on SDB risk in active-duty personnel are reported in Fig 2. SDB risk was significantly higher in the overweight and obese population (OR = 2.44, 95%CI 1.51 to 3.94), and higher BMI was associated with higher risk (OR = 2.03, 95%CI 1.43 to 2.87). Being male (OR = 3.03 95%CI 1.27 to 7.23) and older than 35 years old (OR = 3.00 95%CI 2.18 to 4.11) could increase SDB risk as well. Results showed that alcohol dependence led to a slight but significant decrease of risk (OR = 0.94, 95%CI 0.92 to 0.96).
Fig 2. Sociodemographic factors for SDB in active-duty personnel.
Comorbidity factors
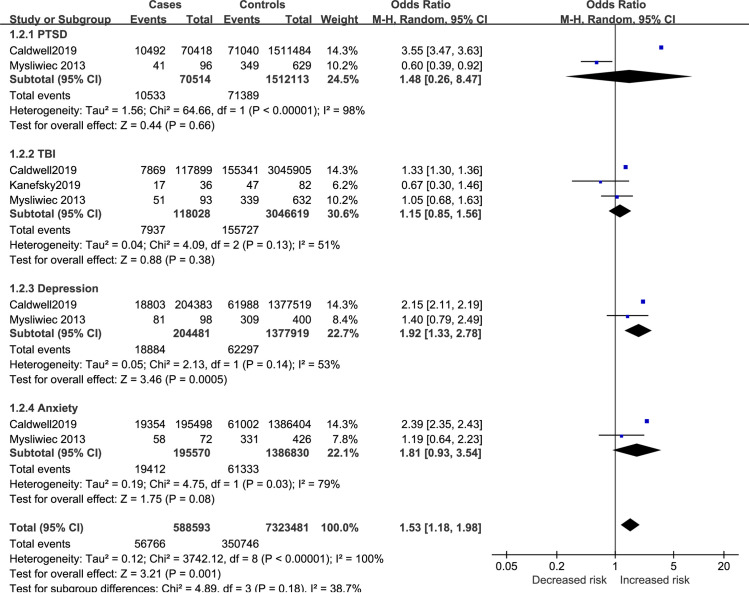
Results of comorbidity effect on SDB risk in active-duty personnel are reported in Fig 3. Depression was found to increase SDB risk (OR = 1.92, 95%CI 1.33 to 2.78) while PTSD (OR = 1.48, 95%CI 0.26 to 8.47), TBI (OR = 1.15, 95%CI 0.85 to 1.56), and anxiety (OR = 1.81, 95%CI 0.93 to 3.54) had no influence on SDB risk. The pooled result of the four comorbidities showed significant increase for SDB risk in active-duty personnel (OR = 1.53, 95%CI 1.18 to 1.98).
Fig 3. Comorbidity factors for SDB in active-duty personnel.
Risk factors for SDB in veterans
Comorbidity factor
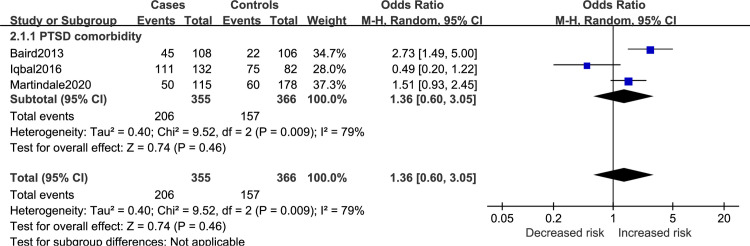
Results regarding the comorbidity factor for SDB in veterans is reported in Fig 4. PTSD had no significant influence on SDB risk (OR = 1.36; 95%CI 0.60 to 3.05).
Fig 4. Comorbidity factor for SDB in veterans.
Risk factors for insomnia in active-duty personnel
Sociodemographic factors
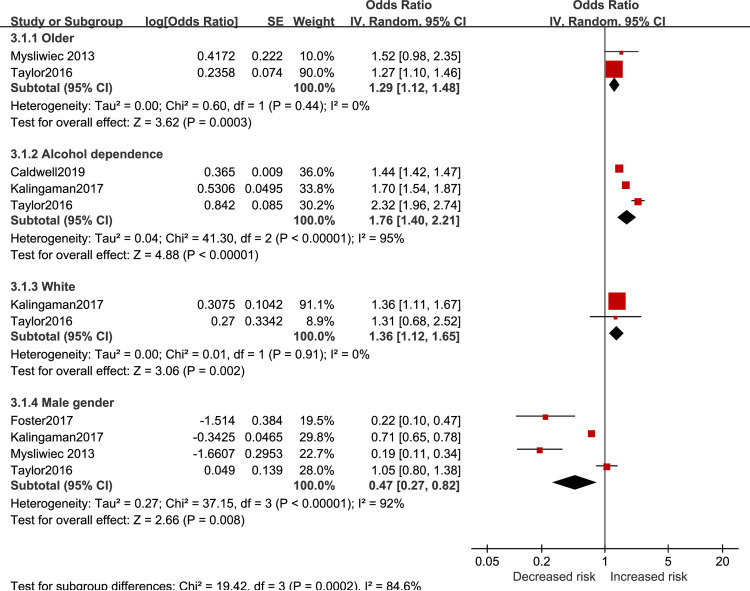
Results regarding the sociodemographic effect on insomnia risk in active-duty personnel are reported in Fig 5. Aging (OR = 1.29 95%CI 1.12 to 1.48), having alcohol dependence (OR = 1.76 95%CI 1.40 to 2.21), and being white (OR = 1.36 95%CI 1.12 to 1.65) showed higher risk for insomnia. Males participants were at lower risk for developing insomnia (OR = 0.47 95%CI 0.27 to 0.82).
Fig 5. Sociodemographic factors for insomnia in active-duty personnel.
Army-specific factors
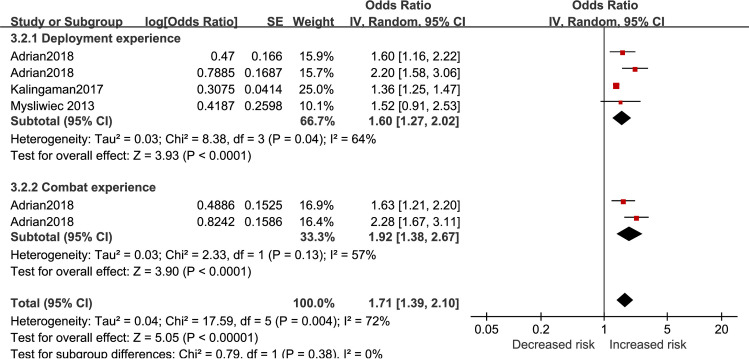
Results of army-specific effect on insomnia risk are reported in Fig 6. Deployment experience (OR = 1.60, 95%CI 1.27 to 2.02) and combat exposure (OR = 1.92, 95%CI 1.38 to 2.67) led to higher insomnia risk. The total effect of army-specific factors showed a significant increase of insomnia risk (OR = 1.71, 95%CI 1.39 to 2.10).
Fig 6. Army-specific factors for insomnia in active-duty personnel.
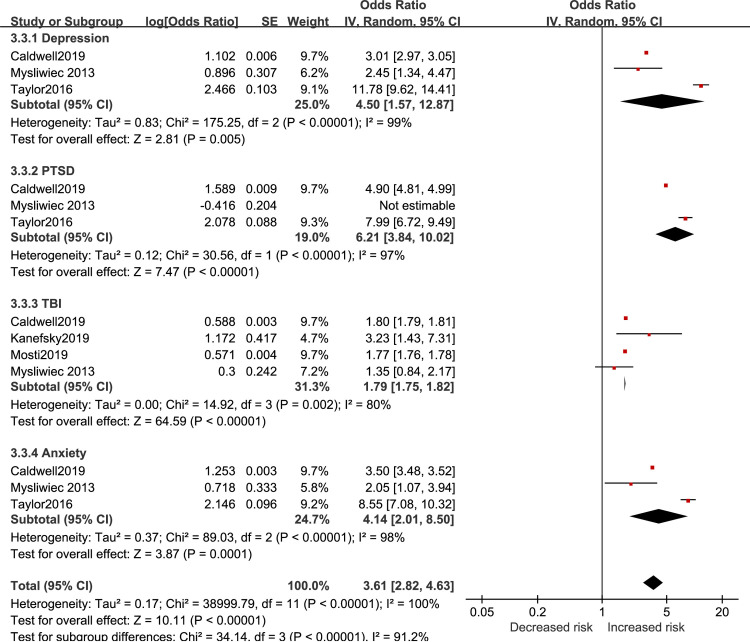
Comorbidity factors
Results of comorbidity effect for insomnia risk are reported in Fig 7. One included article in the PTSD category was identified as an outlier and excluded during data analysis [13]. Depression (OR = 4.50, 95%CI 1.57 to 12.87), PTSD (OR = 6.21, 95% 3.84 to 10.02), TBI (OR = 1.79, 95%CI 1.75 to 1.82), and anxiety (OR = 4.14, 95%CI 2.01 to 8.50) could increase insomnia risk. Total effect of the four comorbidities was found to increase insomnia risk with a relatively large effect (OR = 3.61, 95%CI 2.82 to 4.63).
Fig 7. Comorbidity factors for insomnia in active-duty personnel.
Risk factors for insomnia in veterans
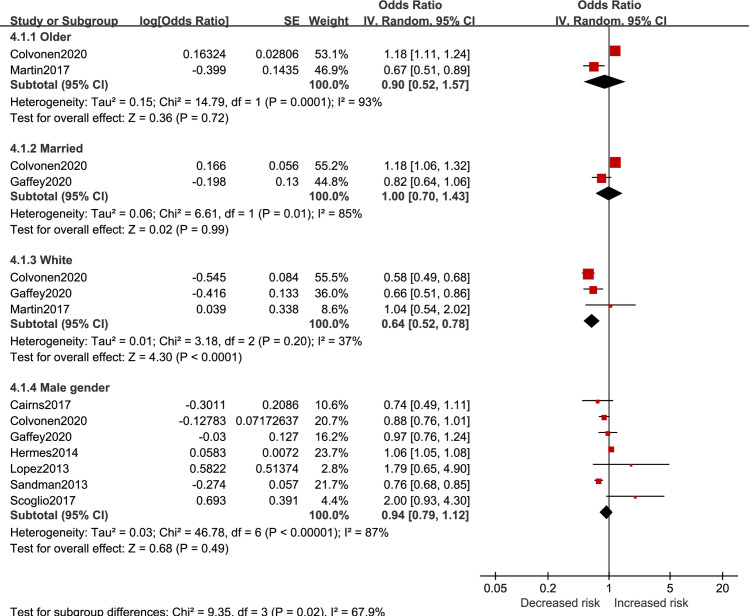
Sociodemographic factors
Results of sociodemographic factors for insomnia risk in veterans are reported in Fig 8. Being white (OR = 0.64, 95%CI 0.52 to 0.78) was related to lower insomnia risk. Aging (OR = 0.90, 95%CI 0.52 to 1.57), marriage (OR = 1.00, 95%CI 0.70 to 1.43), and male gender (OR = 0.94, 95%CI 0.79 to 1.12) had no significant influence for insomnia risk.
Fig 8. Sociodemographic factors for insomnia in veterans.
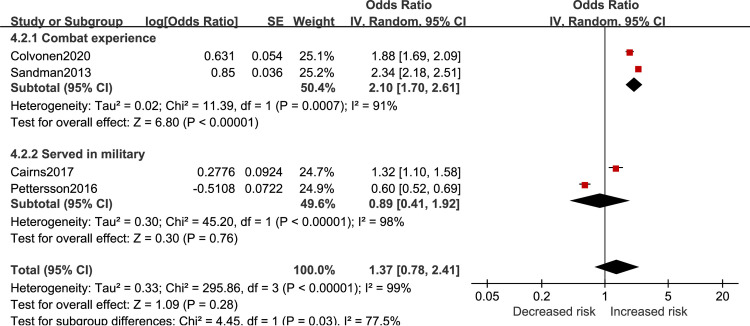
Army-specific factors
Results of army-specific effect on insomnia risk in veterans are reported in Fig 9. Combat experience was associated with greater risk of developing insomnia (OR = 2.10, 95%CI 1.70 to 2.61). Experience of serving in military had no effect on insomnia risk (OR = 0.89, 95%CI 0.41 to 1.92). The total effect of army-specific showed no significant influence on insomnia risk (OR = 1.37, 95%CI 0.78 to 2.41).
Fig 9. Army-specific factors for insomnia in veterans.
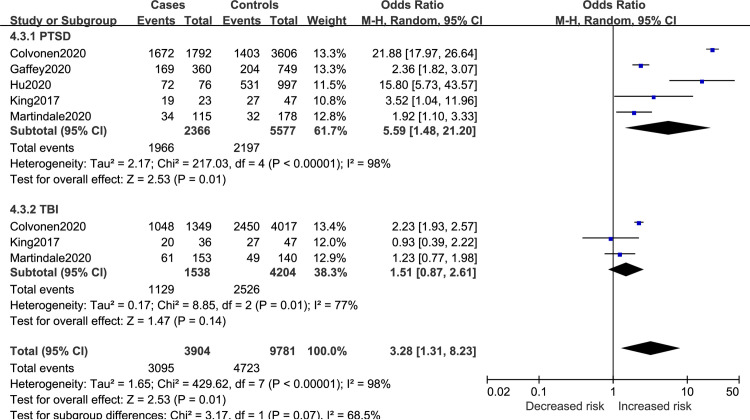
Comorbidity factors
Results of comorbidities for insomnia risk in veterans are reported in Fig 10. The final merged results revealed that PTSD (OR = 5.59, 95%CI 1.48 to 21.20) could increase insomnia risk while TBI (OR = 1.51, 95%CI 0.87 to 2.61) had no influence on the risk of developing insomnia. The total effect of the two comorbidities demonstrated a tendency to increase insomnia risk (OR = 3.28, 95%CI 1.31 to 8.23).
Fig 10. Comorbidity factors for insomnia in veterans.
Discussion
The pooled outcomes identified four sociodemographic (i.e., overweight/obesity, higher BMI, male gender, >35 years old) and one comorbidity (i.e., depression) risk factors for SDB in active duty personnel; four sociodemographic (i.e., aging, alcohol dependence, white race and female gender), two army-specific (i.e., deployment experience, combat experience), and four comorbidity (i.e., depression, PTSD, TBI and anxiety) risk factors for insomnia in active duty personnel; and one army-specific (i.e., combat experience) and one comorbidity (i.e., PTSD) risk factor for insomnia in veterans.
Gaining more weight (i.e., obesity or higher BMI) was associated with higher SDB risk in active-duty personnel with a medium effect size. This outcome is similar to evidence provided in previous studies and suggests that it is quite important for military personnel to maintain proper weight because it impacts not only their ability to fight but also SDB risk. Alcohol dependence showed higher insomnia risk (OR = 1.76 95%CI 1.4 to 2.21) and a small but significant decrease of SDB risk (OR = 0.94 95%CI 0.92 to 0.96) in active-duty personnel. However, we think more articles are needed in the future to reach a more accurate and convincing conclusion considering that only two articles were included in this latter analysis.
Age plays an important role in the development of soldiers’ retirement policy with the consideration that soldiers could be at higher risk for many disorders including SDB when older than a certain age. In the current analysis, pooled evidence showed 3-times-higher SDB risk for active-duty personnel and 3.64-times-higher SDB risk for veterans older than 35 years old. As soldiers aged, insomnia risk increased in the active-duty personnel group. More studies are needed to confirm the age point where the steepest turning point of risk for SDB or insomnia appears and could help guide policy development.
Merely serving in the military does not increase insomnia risk for veterans. However, deployment experience and combat experience could increase insomnia risk. These outcomes indicate that influences that lead to higher risk of insomnia come from deployment or combat experience rather than military serving experience. Thus, future research should break down deployment and combat experiences into more specific categories of possible influences to figure out which factor plays a more important role in the developing of insomnia.
The effects of comorbidities on insomnia risk in active-duty personnel were quite remarkable. Patients with any of the four comorbidities (i.e., depression, PTSD, TBI, anxiety) were 3.61 times more likely to develop insomnia compared with healthy controls in active-duty personnel. This result suggests more concern or even early preventive treatment should be given to soldiers with these comorbidities even when they do not exhibit relevant symptoms. In contrast, effects of comorbidity factors on SDB risk were mostly insignificant. The only exception is that depression could increase SDB risk in active-duty personnel. However, considering only two to three studies were included in the analysis of comorbidity factors for SDB risk, results of this section should be updated when more studies are available in the future.
Combat experience could bring higher insomnia risk for both of the two groups. However, the effect of some factors on insomnia risk could differ in veteran and active-duty personnel groups. Aging is a risk factor for insomnia in active-duty personnel while no significant result was observed in veterans. White people were less likely to develop insomnia in veterans while the opposite result was observed in active-duty personnel. TBI brought higher insomnia risk in active-duty personnel while no significant effect of TBI was observed in veterans. Three possible factors may explain this situation: First, symptoms of comorbidities (e.g., TBI) caused by military service gradually improve over time after proper treatment. Second, the life and work environments of veterans and active-duty personnel are totally different, so potential influencing factors could serve as mediators to influence the relationship between risk factors and outcomes. Third, the number of included studies is insufficient, and the results may be biased. More in-depth comparison between veteran and active-duty personnel is not yet possible, as many factors could only be analyzed in one group since suitable articles are limited. Data on risk factors for SDB in veterans is most insufficient with PTSD being the only analyzable factor, making the comparison of SDB risk between active-duty personnel and veterans impossible.
Strengths and limitations
Systematic search strategy was used to get comprehensive records in four databases, and articles of different countries were included. The search terms were identified after careful discussions and consultations among researchers. There was no similar meta-analyses or reviews exploring the risk factors for sleep disorder in a military sample to our knowledge, so this research provided findings of practical significance and could help to guide future research.
Nevertheless, several limitations could not be ignored. More than half of the studies included were cross-sectional, and as a result, the ability to explain the causal relationships between these factors and sleep disorders was restricted. Considering the number of studies could be quite small after sorted into different subgroups, relatively lenient entry criteria were drawn up to ensure a sufficient number of articles to get meaningful results. Consequently, many outcomes were accompanied by high heterogeneity because assessment tools varied across studies. Outliers were identified and excluded to reduce heterogeneity, while further subgroup analysis could not be performed due to the much-detailed grouping in this study.
Implications
In this preliminary meta-analysis, several risk and protective factors for insomnia and SDB were identified, providing deeper views into detection of those at higher risk of developing sleep disorders in military group and guidance for future research. However, the lack of usable data was quite prominent and there would be an urgent need for prospective cohort studies of risk factors for sleep impairment in the military sample.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
1.Yunxiang Tang Grant number CWS20J007 Logistics department, 2.Yunxiang Tang Grant number 20BJZ09) Logistics department, 3.Yunxiang Tang Grant number 201944816) Training department, 4.Tong Su Grant number 2019QNP014) Logistics department. These funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Jones DM, Bailey SP, Roelands B, Buono MJ, Meeusen R. Cold acclimation and cognitive performance: A review [Internet]. Vol. 208, Autonomic Neuroscience: Basic and Clinical. Elsevier B.V.; 2017. [cited 2020 Nov 18]. p. 36–42. Available from: https://pubmed.ncbi.nlm.nih.gov/29158117/ [DOI] [PubMed] [Google Scholar]
- 2.Gauer R, Army W, Bragg F, Carolina N, Meyers BK. Heat-Related Illnesses. Am Fam Physician [Internet]. 2019. April 15 [cited 2020 Nov 18];99(8):482–9. Available from: https://pubmed.ncbi.nlm.nih.gov/30990296/ [PubMed] [Google Scholar]
- 3.Sharma R, Cramer NP, Perry B, Adahman Z, Murphy EK, Xu X, et al. Chronic Exposure to High Altitude: Synaptic, Astroglial and Memory Changes. Sci Rep [Internet]. 2019;9(1):1–13. Available from: 10.1038/s41598-018-37186-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shattuck NL, Matsangas P. Operational assessment of the 5-h on/10-h off watchstanding schedule on a US Navy ship: sleep patterns, mood and psychomotor vigilance performance of crewmembers in the nuclear reactor department. Ergonomics [Internet]. 2016. May 3 [cited 2021 Feb 16];59(5):657–64. Available from: https://pubmed.ncbi.nlm.nih.gov/26360772/ 10.1080/00140139.2015.1073794 [DOI] [PubMed] [Google Scholar]
- 5.Carskadon MA. Patterns of sleep and sleepiness in adolescents [Internet]. Vol. 17, Pediatrician. Pediatrician; 1990 [cited 2021 Feb 16]. p. 5–12. Available from: https://pubmed.ncbi.nlm.nih.gov/2315238/ [PubMed]
- 6.Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. In: Sleep [Internet]. Associated Professional Sleep Societies,LLC; 2015. [cited 2021 Feb 16]. p. 843–4. Available from: https://pubmed.ncbi.nlm.nih.gov/26039963/ 10.5665/sleep.4716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jan I. Maby POK, William W, Pearce Teresa D., Cowan ALK David N., Wada Camille B. et al. Accession medical standards analysis and research activity (amsara) 2017 annual report. Silver Spring, MD: Walter Reed Army Inst Res. 2018; [Google Scholar]
- 8.Miller NL, Shattuck LG. Sleep patterns of young men and women enrolled at the United States Military Academy: Results from year 1 of a 4-year longitudinal study. Sleep [Internet]. 2005. July 1 [cited 2021 Feb 16];28(7):837–41. Available from: https://pubmed.ncbi.nlm.nih.gov/16124662/ 10.1093/sleep/28.7.837 [DOI] [PubMed] [Google Scholar]
- 9.Capaldi VF, Balkin TJ, Mysliwiec V. Optimizing Sleep in the Military: Challenges and Opportunities. Chest [Internet]. 2019. January 1 [cited 2021 Feb 16];155(1):215–26. Available from: https://pubmed.ncbi.nlm.nih.gov/30218649/ 10.1016/j.chest.2018.08.1061 [DOI] [PubMed] [Google Scholar]
- 10.Troxel WM, Shih RA, Pedersen ER, Geyer L, Fisher MP, Griffin BA, et al. Sleep in the Military: Promoting Healthy Sleep Among U.S. Servicemembers. 2015. [cited 2021 Feb 16]; Available from: https://www.rand.org/pubs/research_reports/RR739.html [PMC free article] [PubMed] [Google Scholar]
- 11.Taylor DJ, Pruiksma KE, Hale WJ, Kelly K, Maurer D, Peterson AL, et al. Prevalence, Correlates, and Predictors of Insomnia in the US Army prior to Deployment. Sleep. 2016;39(10):1795–806. 10.5665/sleep.6156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Capener DC, Brock MS, Hansen SL, Matsangas P, Mysliwiec V. An Initial Report of Sleep Disorders in Women in the U.S. Military. Mil Med [Internet]. 2018. September 1 [cited 2021 Feb 16];183(9–10):e266–71. Available from: https://pubmed.ncbi.nlm.nih.gov/29425355/ 10.1093/milmed/usx116 [DOI] [PubMed] [Google Scholar]
- 13.Mysliwiec V, Gill J, Lee H, Baxter T, Pierce R, Barr TL, et al. Sleep disorders in US military personnel: A high rate of comorbid insomnia and obstructive sleep apnea. Chest [Internet]. 2013. [cited 2021 Feb 16];144(2):549–57. Available from: https://pubmed.ncbi.nlm.nih.gov/23681455/ 10.1378/chest.13-0088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mysliwiec V, Matsangas P, Baxter T, McGraw L, Bothwell NE, Roth BJ. Comorbid insomnia and obstructive sleep apnea in military personnel: Correlation with polysomnographic variables. Mil Med [Internet]. 2015. [cited 2021 Feb 16];179(3):294–300. Available from: https://pubmed.ncbi.nlm.nih.gov/24594464/ [DOI] [PubMed] [Google Scholar]
- 15.Buysse DJ. Insomnia. Jama [Internet]. 2013;309(7):706–16. Available from: http://jama.jamanetwork.com/%0Ahttps://jamanetwork.com/journals/jama/fullarticle/1653540 10.1001/jama.2013.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med [Internet]. 2001. [cited 2021 Mar 10];2(4):297–307. Available from: https://pubmed.ncbi.nlm.nih.gov/11438246/ 10.1016/s1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 17.de Zambotti M, Goldstone A, Colrain IM, Baker FC. Insomnia disorder in adolescence: Diagnosis, impact, and treatment. Vol. 39, Sleep Medicine Reviews. 2018. p. 12–24. 10.1016/j.smrv.2017.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cross NE, Carrier J, Postuma RB, Gosselin N, Kakinami L, Thompson C, et al. Association between insomnia disorder and cognitive function in middle-Aged and older adults: A cross-sectional analysis of the Canadian Longitudinal Study on Aging. Sleep. 2019;42(8):1–10. 10.1093/sleep/zsz114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Erickson EA, Stahlman S, McNellis MG. Insomnia and motor vehicle accident-related injuries, active component, U.S. Armed Forces, 2007–2016. MSMR [Internet]. 2017. December [cited 2021 Feb 16];24(12):2–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29328680 [PubMed] [Google Scholar]
- 20.Hanske J, Von Landenberg N, Gild P, Cole A, Jiang W, Lipsitz S, et al. Adverse effects of testosterone replacement therapy for men, a matched cohort study. Eur Urol Suppl [Internet]. 2017;16(3):e448–50. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L618191480 [Google Scholar]
- 21.Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, et al. Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences. J Am Coll Cardiol. 2017;69(7):841–58. 10.1016/j.jacc.2016.11.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Academy of Sleep Medicine.International classification of sleep disorders. 3rd ed. Am Acad Sleep Med. 2014; [Google Scholar]
- 23.Somers VK, Javaheri S. Cardiovascular Effects of Sleep-Related Breathing Disorders. In: Kryger MH, Roth T, Dement WCBT-P and P of SM (Fourth E, editors. Philadelphia: W.B. Saunders; 2005. p. 1180–91. Available from: http://www.sciencedirect.com/science/article/pii/B0721607977501063 [Google Scholar]
- 24.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005. November;353(19):2034–41. 10.1056/NEJMoa043104 [DOI] [PubMed] [Google Scholar]
- 25.Ballesio A, Bacaro V, Vacca M, Chirico A, Lucidi F, Riemann D, et al. Does cognitive behaviour therapy for insomnia reduce repetitive negative thinking and sleep-related worry beliefs? A systematic review and meta-analysis [Internet]. Vol. 55, Sleep Medicine Reviews. 2021. [cited 2020 Oct 27]. Available from: 10.1016/j.smrv.2020.101378 [DOI] [PubMed] [Google Scholar]
- 26.Xue C, Ge Y, Tang B, Liu Y, Kang P, Wang M, et al. A meta-analysis of risk factors for combat-related PTSD among military personnel and veterans. PLoS One [Internet]. 2015. March 20 [cited 2021 Feb 19];10(3). Available from: https://pubmed.ncbi.nlm.nih.gov/25793582/ 10.1371/journal.pone.0120270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blore JD, Sim MR, Forbes AB, Creamer MC, Kelsall HL. Depression in Gulf War veterans: A systematic review and meta-analysis [Internet]. Vol. 45, Psychological Medicine. Cambridge University Press; 2015. [cited 2021 Feb 19]. p. 1565–80. Available from: https://pubmed.ncbi.nlm.nih.gov/25697603/ 10.1017/S0033291714001913 [DOI] [PubMed] [Google Scholar]
- 28.Zhang Y, Ren R, Sanford LD, Yang L, Zhou J, Zhang J, et al. Sleep in posttraumatic stress disorder: A systematic review and meta-analysis of polysomnographic findings [Internet]. Vol. 48, Sleep Medicine Reviews. W.B. Saunders Ltd; 2019. [cited 2021 Feb 19]. Available from: https://pubmed.ncbi.nlm.nih.gov/31518950/ [DOI] [PubMed] [Google Scholar]
- 29.Zhang Y, Weed JG, Ren R, Tang X, Zhang W. Prevalence of obstructive sleep apnea in patients with posttraumatic stress disorder and its impact on adherence to continuous positive airway pressure therapy: a meta-analysis [Internet]. Vol. 36, Sleep Medicine. Elsevier B.V.; 2017. [cited 2021 Feb 19]. p. 125–32. Available from: https://pubmed.ncbi.nlm.nih.gov/28735910/ 10.1016/j.sleep.2017.04.020 [DOI] [PubMed] [Google Scholar]
- 30.Grima N, Ponsford J, Rajaratnam SM, Mansfield D, Pase MP. Sleep disturbances in traumatic brain injury: A meta-analysis [Internet]. Vol. 12, Journal of Clinical Sleep Medicine. American Academy of Sleep Medicine; 2016. [cited 2021 Feb 18]. p. 419–28. Available from: https://pubmed.ncbi.nlm.nih.gov/26564384/ 10.5664/jcsm.5598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002. April;6(2):97–111. 10.1053/smrv.2002.0186 [DOI] [PubMed] [Google Scholar]
- 32.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008. February;5(2):136–43. 10.1513/pats.200709-155MG [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002. May;165(9):1217–39. 10.1164/rccm.2109080 [DOI] [PubMed] [Google Scholar]
- 34.Lee YC, Eun YG, Shin SY, Kim SW. Prevalence of Snoring and High Risk of Obstructive Sleep Apnea Syndrome in Young Male Soldiers in Korea. J Korean Med Sci. 2013;28(9):1373–7. 10.3346/jkms.2013.28.9.1373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim J-W, Lee CH, Rhee CS, Mo J-H. Relationship Between Snoring Intensity and Severity of Obstructive Sleep Apnea. Clin Exp Otorhinolaryngol. 2015. December;8(4):376–80. 10.3342/ceo.2015.8.4.376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jacobson MD, Malik B. Heart failure and sleep apnea. J Am Acad Physician Assist. 2019;32(4):2019–20. [Google Scholar]
- 37.Vozoris NT. Sleep apnea-plus: prevalence, risk factors, and association with cardiovascular diseases using United States population-level data. Sleep Med. 2012. June;13(6):637–44. 10.1016/j.sleep.2012.01.004 [DOI] [PubMed] [Google Scholar]
- 38.Kent BD, Grote L, Ryan S, Pépin J-L, Bonsignore MR, Tkacova R, et al. Diabetes mellitus prevalence and control in sleep-disordered breathing: the European Sleep Apnea Cohort (ESADA) study. Chest. 2014. October;146(4):982–90. 10.1378/chest.13-2403 [DOI] [PubMed] [Google Scholar]
- 39.Durán J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001. March;163(3 Pt 1):685–9. [DOI] [PubMed] [Google Scholar]
- 40.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009. July;6(7):e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Furukawa TA. From effect size into number needed to treat. Lancet. 1999;353(9165):1680. 10.1016/S0140-6736(99)01163-0 [DOI] [PubMed] [Google Scholar]
- 42.Chinn S. A simple method for converting an odds ratio to effect size for use in meta‐analysis. Stat Med. 2000;19(22):3127–31. [DOI] [PubMed] [Google Scholar]
- 43.Pilakasiri A, Mahakit P. Prospective study of the prevalence and co-morbidities of obstructive sleep apnea in active-duty army personnel in the three southernmost provinces of Thailand using questionnaire screening. Mil Med Res. 2018;5. 10.1186/s40779-018-0153-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Caldwell JA, Knapik JJ, Shing TL, Kardouni JR, Lieberman HR. The association of insomnia and sleep apnea with deployment and combat exposure in the entire population of US army soldiers from 1997 to 2011: A retrospective cohort investigation. Sleep [Internet]. 2019;42(8):1–10. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L629850107 10.1093/sleep/zsz112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Crump C, Sundquist J, Winkleby MA, Sundquist K. Cardiorespiratory fitness and long-term risk of sleep apnea: A national cohort study. J Sleep Res [Internet]. 2019; Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L627148122 10.1111/jsr.12851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Langton RS, Neyra J, Downs JW, Niebuhr DW. The Relationship Between Enlistment Body Mass Index and the Development of Obstructive Sleep Apnea in the U.S. Military. Mil Med [Internet]. 2016;181(8):913–9. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L620170392 10.7205/MILMED-D-15-00295 [DOI] [PubMed] [Google Scholar]
- 47.Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep Disorders and Associated Medical Comorbidities in Active Duty Military Personnel. Sleep. 2013;36(2):167–74. 10.5665/sleep.2364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Foster SN, Hansen SL, Capener DC, Matsangas P, Mysliwiec V. Gender differences in sleep disorders in the US military. Sleep Heal. 2017. October;3(5):336–41. 10.1016/j.sleh.2017.07.015 [DOI] [PubMed] [Google Scholar]
- 49.Cairns A, Sarmiento K, Bogan R. Utility of home sleep apnea testing in high-risk veterans. Sleep Breath. 2017;21(3):647–55. 10.1007/s11325-017-1467-8 [DOI] [PubMed] [Google Scholar]
- 50.Iqbal N, Kinoshita LM, Noda A, Friedman L, Yesavage JA, Zeitzer JM. Ubiquity of Undiagnosed Sleep Disordered Breathing in Community-Dwelling Older Male Veterans. Am J Geriatr psychiatry Off J Am Assoc Geriatr Psychiatry. 2016. February;24(2):170–3. 10.1016/j.jagp.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 51.Baird T, McLeay S, Harvey W, Theal R, Law D, O’Sullivan R. Sleep Disturbances in Australian Vietnam Veterans With and Without Posttraumatic Stress Disorder. J Clin sleep Med JCSM Off Publ Am Acad Sleep Med. 2018. May;14(5):745–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martindale SL, Konst MJ, Bateman JR, Arena A, Rowland JA. The role of PTSD and TBI in post-deployment sleep outcomes. Mil Psychol. 2020;32(2):212–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kanefsky R, Motamedi V, Mithani S, Mysliwiec V, Gill JM, Pattinson CL. Mild traumatic brain injuries with loss of consciousness are associated with increased inflammation and pain in military personnel. Psychiatry Res. 2019. September;279:34–9. 10.1016/j.psychres.2019.07.001 [DOI] [PubMed] [Google Scholar]
- 54.Mysliwiec V, Matsangas P, Gill J, Baxter T, O’Reilly B, Collen JF, et al. A comparative analysis of sleep disordered breathing in Active Duty Service Members with and without combat-related Posttraumatic stress disorder. J Clin Sleep Med [Internet]. 2015;11(12):1393–401. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L607836769 10.5664/jcsm.5272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hermes E, Rosenheck R. Prevalence, pharmacotherapy and clinical correlates of diagnosed insomnia among Veterans Health Administration service users nationally. Sleep Med. 2014/04/29. 2014;15(5):508–14. 10.1016/j.sleep.2013.12.010 [DOI] [PubMed] [Google Scholar]
- 56.Martin JL, Schweizer CA, Hughes JM, Fung CH, Dzierzewski JM, Washington DL, et al. Estimated Prevalence of Insomnia among Women Veterans: Results of a Postal Survey. Women’s Heal Issues [Internet]. 2017;27(3):366–73. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L614116481 10.1016/j.whi.2016.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Taylor DJ, Pruiksma KE, Hale WJ, Kelly K, Maurer D, Peterson AL, et al. Prevalence, Correlates, and Predictors of Insomnia in the US Army prior to Deployment. Sleep [Internet]. 2016. October 1 [cited 2021 Feb 16];39(10):1795–806. Available from: https://pubmed.ncbi.nlm.nih.gov/27450687/ 10.5665/sleep.6156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Adrian AL. Soldiers and Leaders With Combat Experience: Unit Health and Climate. 2018;81(4):391–407. [DOI] [PubMed] [Google Scholar]
- 59.Colvonen PJ, Almklov E, Tripp JC, Ulmer CS, Pittman JOE, Afari N. Prevalence rates and correlates of insomnia disorder in post-9/11 veterans enrolling in VA healthcare. Sleep. 2020. December;43(12). 10.1093/sleep/zsaa119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.King PR, Donnelly KT, Warner G, Wade M, Pigeon WR. The natural history of sleep disturbance among OEF/OIF veterans with TBI and PTSD and the role of proxy variables in its measurement. J Psychosom Res. 2017. May;96:60–6. 10.1016/j.jpsychores.2017.03.012 [DOI] [PubMed] [Google Scholar]
- 61.Scoglio AAJ, Shirk SD, Hoff RA, Potenza MN, Mazure CM, Park CL, et al. Gender-Specific Risk Factors for Psychopathology and Reduced Functioning in a Post-9/11 Veteran Sample. J Interpers Violence [Internet]. 2017. February 1 [cited 2021 Mar 10];36(3–4). Available from: https://pubmed.ncbi.nlm.nih.gov/29295023/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gaffey AE, Redeker NS, Rosman L, Mullington JM, Brandt CA, Haskell SG, et al. The role of insomnia in the association between posttraumatic stress disorder and hypertension. J Hypertens. 2020. April;38(4):641–8. 10.1097/HJH.0000000000002311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Klingaman EA, McCarthy JM, Schwartz EK, Gehrman PR, Bennett ME. Targets for the treatment of insomnia in veterans with serious mental illness. J Psychiatr Pract [Internet]. 2017;23(4):270–80. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L623482716 10.1097/PRA.0000000000000240 [DOI] [PubMed] [Google Scholar]
- 64.Lopez MR, Cheng JY, Kanner AM, Carvalho DZ, Diamond JA, Wallace DM. Insomnia symptoms in South Florida military veterans with epilepsy. Epilepsy Behav. 2013;27(1):159–64. 10.1016/j.yebeh.2013.01.008 [DOI] [PubMed] [Google Scholar]
- 65.Pettersson K, Saers J, Lindberg E, Janson C. Sleep disturbances among Swedish soldiers after military service abroad. Ups J Med Sci [Internet]. 2016;121(1):65–9. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L616249715 10.3109/03009734.2016.1144663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hu Y, Chu X, Urosevich TG, Hoffman SN, Kirchner HL, Adams RE, et al. Predictors of Current DSM-5 PTSD Diagnosis and Symptom Severity Among Deployed Veterans: Significance of Predisposition, Stress Exposure, and Genetics. Neuropsychiatr Dis Treat. 2020;16:43–54. 10.2147/NDT.S228802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sandman N, Valli K, Kronholm E, Ollila HM, Revonsuo A, Laatikainen T, et al. Nightmares: Prevalence among the Finnish General Adult Population and War Veterans during 1972–2007. Sleep. 2013. July;36(7):1041–50. 10.5665/sleep.2806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep Disorders and Associated Medical Comorbidities in Active Duty Military Personnel. Sleep. 2013. February;36(2):167–74. 10.5665/sleep.2364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Boland EM, Mosti C, Gehrman PR, Chao LL, Abadjian LR, Esparza IL, et al. Insomnia Severity, Subjective Sleep Quality, and Risk for Obstructive Sleep Apnea in Veterans With Gulf War Illness. J Sleep Res. 2017/10/13. 2016;181(9):1127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mosti CB, Klingaman EA, Brownlow JA, Gehrman PR. Insomnia Prevalence Among U.S. Army Soldiers With History of TBI. Rehabil Psychol [Internet]. 2019; Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L628534147 10.1037/rep0000283 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.