Abstract
Objective
To assess trends of stroke hospitalization rates, inpatient mortality, and health care resource use in young (aged ≤44 years), midlife (aged 45-64 years), and older (aged ≥65 years) adults.
Patients and Methods
We studied the National Inpatient Sample database (January 1, 2002 to December 31, 2017) to analyze stroke-related hospitalizations. We identified data using the International Classification of Diseases, Ninth/Tenth Revision codes.
Results
Of 11,381,390 strokes, 79% (n=9,009,007) were ischemic and 21% (n=2,372,383) were hemorrhagic. Chronic diseases were more frequent in older adults; smoking, alcoholism, and migraine were more prevalent in midlife adults; and coagulopathy and intravenous drug abuse were more common in young patients with stroke. The hospitalization rates of stroke per 10,000 increased overall (31.6 to 33.3) in young and midlife adults while decreasing in older adults. Although mortality decreased overall and in all age groups, the decline was slower in young and midlife adults than older adults. The mean length of stay significantly decreased in midlife and older adults and increased in young adults. The inflation-adjusted mean cost of stay increased consistently, with an average annual growth rate of 2.44% in young, 1.72% in midlife, and 1.45% in older adults owing to the higher use of health care resources. These trends were consistent in both ischemic and hemorrhagic stroke.
Conclusion
Stroke-related hospitalization and health care expenditure are increasing in the United States, particularly among young and midlife adults. A higher cost of stay counterbalances the benefits of reducing stroke and mortality in older patients.
Abbreviations and Acronyms: AAPC, average annual percent change; HCUP, Healthcare Cost and Utilization Project; ICD-9/10-CM, International Classification of Diseases, Ninth/Tenth Revision, Clinical Modification; LOS, length of stay; NIS, Nationwide Inpatient Sample
The epidemiologic profile of stroke has evolved over the years in the United States. Stroke remained the fifth major cause of death in the country, accounting for more than 140,000 deaths each year.1,2 Stroke imparts a significant economic burden on the health system and costs around $34 billion per annum in the United States.3 The National Health and Aging Trends Study reported that care costs for elderly stroke survivors are approximately $40 billion per year.4 Over the years, advances in stroke care through structured quality enhancement programs have resulted in an overall decline in stroke.5 However, stroke-related morbidity and mortality vary across different age groups.1,5
The relative decline in stroke-related mortality among older adults (aged ≥65 years) was found to be almost twice the rate of decline in midlife (45-64 years) adults between 1999 and 2003.1,5 The Atherosclerosis Risk in Communities Study cohort demonstrated an approximately 50% decline in incident stroke among older patients but stable stroke rates in younger adults. However, stroke-related mortality rates were reduced in the latter between 1987 and 2011.6 In contrast, another National Inpatient Sample (NIS) report from 1995 to 2012 illustrated a significant increase in stroke hospitalization rates in young adults aged 18 to 54 years.5
In the backdrop of fluctuating patterns, assessing the most recent stroke-stratified trends by age groups becomes relevant to public health interventions to prevent the onset of stroke and subsequent treatment strategies. Moreover, there is a paucity of data on the economic burden of stroke across different age categories. To address these evidence gaps, we analyzed data from the largest US administrative claims–based database and examined characteristics and trends in the prevalence, mortality, health care resource use, and stroke expenditure across different age groups in the country.
Patients and Methods
Setting
The NIS database is part of the Healthcare Cost and Utilization Project (HCUP) databases,7 sponsored by the Agency for Healthcare Research and Quality. The NIS is the largest publicly available all-payer administrative claims–based database of hospital inpatient stays, which contains the clinical and resource use information abstracted from discharges from 47 US states covering greater than 97% of the US population. The annual sample encompasses approximately 8 million discharges, representing 20% of US inpatient hospitalizations across different geographic regions and hospital types. This study was exempt from institutional review board approval given the NIS database's deidentified nature and public availability.
Study Design
We conducted a longitudinal observational analysis using data from January 1, 2002, to December 31, 2017, to identify stroke-related hospitalizations in adults (aged ≥18 years) as captured in NIS. We identified stroke-related hospitalizations using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and ICD, Tenth Revision, Clinical Modification (ICD-10-CM) codes, respectively. Supplemental Table 1 (available online at https://mcpiqojournal.org) reports a complete list of diagnosis codes).
Exposures
The exposure of interest for the present analysis was age, and this was modeled in 3 groups as young (aged ≤44 years), midlife (aged 45-64 years), and older (aged ≥65 years) adults.8, 9, 10, 11, 12
Outcomes
Several relevant features were described among patients with stroke, including demographic characteristics, frequency of stroke subtypes (ischemic and hemorrhagic), comorbid conditions (based on 29 Elixhauser comorbid conditions using ICD-9-CM and ICD-10-CM codes),13 insurance/payer, household income, and discharge disposition. We classified discharge disposition as: (1) home (routine or with home health), (2) short-term care facility (short-term rehabilitation or inpatient rehabilitation), (3) long-term care facility (skilled nursing and intermediate-care facility), and (4) against medical advice. We then computed trends in stroke hospitalization rates, inpatient mortality, mean length of stay (LOS), and adjusted mean cost of care.
Statistical Analyses
The national estimates of the entire US hospitalized population were calculated using the Agency for Healthcare Research and Quality sampling and weighting method. Before 2012, the Nationwide Inpatient Sample (NIS) contains discharge data from a national sample of community hospitals.14 In 2012, the Nationwide Inpatient Sample was renamed the National Inpatient Sample to reflect the sampling methodology change. The National Inpatient Sample uses a redesigned sampling method for a more accurate representation of national discharge data. The revised database contains a sample of discharge records from all hospitals participating in HCUP (compared with the previous NIS that contained all discharge records from a sample of hospitals). The new NIS contains data for more than 7 million hospital stays each year that can be weighted to make national estimates. To account for this methodology change, HCUP came up with new weights that would allow for trend analysis if applied to years before 2012. These weights were calculated in the same way as the weights for the redesigned 2012 NIS. Therefore, the weights “trendwt” replaces standard discharge weights in years before 2012, whereas standard discharge weights are used after 2012. Further details on weights performed in the analysis are available at https://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp.
We defined cost of care as estimated total expense in US dollars incurred because of hospital services provided (eg, wages, supplies, and utility costs). The NIS database provides the estimates of hospital charges; the bill charged by a hospital for admission. To further calculate the actual cost, HCUP provides Cost-to-Charge Ratio files to estimate the cost of resource use for inpatient hospitals. For the cost, HCUP compiles the information from the hospital accounting reports collected by the Centers for Medicare & Medicaid Services. Because Cost-to-Charge Ratio is a ratio between hospital charges and actual cost, the estimate can be multiplied with each hospital charge to obtain the cost of care per patient per hospital stay. We adjusted the cost of the stay for inflation with comparison to December 2017 (https://data.bls.gov/cgi-bin/cpicalc.pl).13
We estimated the annual stroke-related hospitalization rates per 10,000 US adults (Supplemental Table 2, available online at https://mcpiqojournal.org). We calculated the weighted average of the annual percent change (AAPC) with 95% CIs in stroke rates and the absolute number and proportion of mortality for the entire study period using the Joinpoint Regression Program, version 4.7.0.0. The software takes trend data (eg, absolute counts, rates, or proportion) and fits the simplest joinpoint model that the data allow. The user supplies the minimum and maximum number of joinpoints. The program starts with the minimum number of joinpoints (eg, 0 joinpoints, which is a straight line) and tests whether more joinpoints are statistically significant and must be added to the model (up to that maximum number). This enables the user to test that an apparent change in trend is statistically significant. The tests of significance use a Monte Carlo permutation method. The models may incorporate estimated variation for each point (eg, when the responses are age-adjusted rates) or use a Poisson model of variation. The models may also be linear on the log of the response (eg, for calculating annual percentage rate change).15
Categorical variables were presented as number and percentage, and continuous variables were reported as mean ± SD or median and interquartile range. Categorical variables were compared across age strata (young, midlife, and older) using Pearson χ2 test and Fisher exact test, and continuous variables were compared using Kruskal-Wallis testing.
Temporal trends in continuous variables were examined graphically and with linear regression. We performed subgroup analyses for ischemic and hemorrhagic stroke (Supplemental Tables 3-8, available online at https://mcpiqojournal.org). We performed prespecified analyses to determine the components of cost of care (Supplemental Table 9, available online at https://mcpiqojournal.org). We set statistical significance (2 sided) at .05. Analyses were performed using Statistical Package for Social Science (SPSS), version 26 (IBM Corp).
Results
Study Population
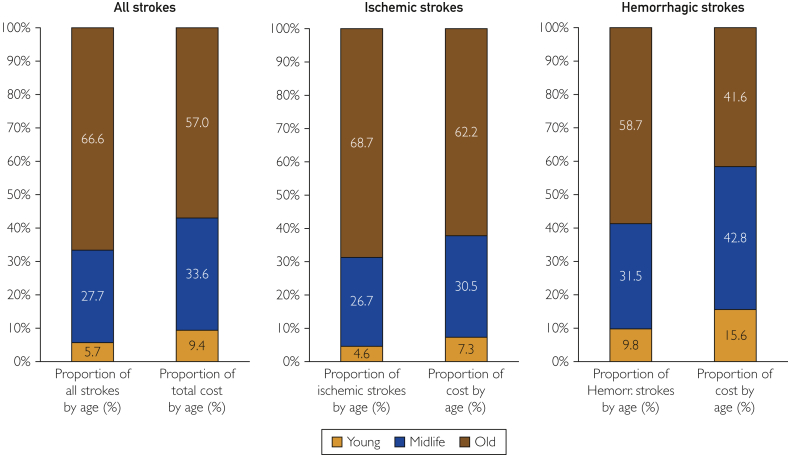
Between 2002 and 2017, a total of 11,381,390 weighted cases of stroke were identified. Of these, 79% (n=9,009,007) were ischemic strokes and 21% (n=2,372,383) were hemorrhagic strokes (Table 1). Overall, the largest age group was the older (66.6% [n=7,583,675] of all stroke hospitalizations), followed by midlife (27.7% [n=3,148,862]) and young (5.7% [n=648,853]) adults (Figure 1). Of all stroke hospitalizations, older individuals had the highest proportion of ischemic stroke hospitalizations (81.6% [n=6,190,274]), while the highest proportion of hemorrhagic strokes was noted in young (35.9% [n=232,685]) patients. Among ischemic stroke hospitalizations (n=9,009,007), 68.7% (n=90,274) occurred in older patients; 26.7% (n=2,402,565), in midlife adults; and 4.6% (n=416,168), in young adults. However, among hemorrhagic stroke hospitalizations (n=2,373,383), 58.7% (n=1,393,401) occurred in older patients, 31.5% (n=746,297) occurred in midlife adults, and 9.8% (n=232,685) occurred in young adults.
Table 1.
Demographic and Clinical Variables in Stroke Across Study Groupsa
| Variable | Age Groups |
||
|---|---|---|---|
| Young | Midlife | Older | |
| Stroke (N=11,381,390), no. (%) | 648,853 (5.7) | 3,148,862 (27.7) | 7,583,675 (66.6) |
| Stroke subtypes, no. (%) | |||
| Hemorrhagic stroke | 232,685 (35.9) | 746,297 (23.7) | 1,393,401 (18.4) |
| Ischemic stroke | 416,168 (64.1) | 2,402,565 (76.3) | 6,190,274 (81.6) |
| Demographic characteristics | |||
| Age (y), median (interquartile range) | 38 (32-42) | 57 (52-61) | 79 (72-85) |
| Female sex, no. (%) | 316,349 (48.8) | 1,356,485 (43.1) | 4,239,664 (55.9) |
| Race, no. (%) | |||
| White | 280,513 (51.0) | 1,577,611 (58.4) | 4,878,285 (75.6) |
| Black | 144,786 (26.3) | 663,286 (24.6) | 767,825 (11.9) |
| Hispanic | 79,451 (14.4) | 272,158 (10.1) | 434,061 (6.7) |
| Others | 45,428 (8.3) | 188,528 (7.0) | 372,510 (5.8) |
| Comorbid conditions, no. (%) | |||
| Hypertension | 285,357 (45.0) | 2,230,605 (72.5) | 5,664,427 (76.5) |
| Diabetes mellitus | 106,987 (16.9) | 1,085,248 (35.2) | 2,299,152 (31.1) |
| Smoking | 157,436 (24.3) | 819,978 (26.0) | 528,627 (7.0) |
| Alcoholism | 45,622 (7.2) | 271,611 (8.8) | 169,193 (2.3) |
| Heart failure | 50,616 (7.8) | 376,819 (12.0) | 1,493,850 (19.7) |
| Migraine | 17,503 (2.7) | 91,937 (2.9) | 130,712 (1.7) |
| Previous stroke | 51,859 (8.0) | 423,873 (13.5) | 1,184,302 (15.6) |
| Cancer | 27,427 (4.2) | 164,192 (5.2) | 428,556 (5.7) |
| Metastatic cancer | 12,581 (1.9) | 105,533 (3.4) | 198,774 (2.6) |
| Coronary artery disease | 27,928 (4.3) | 526,981 (16.7) | 2,075,762 (27.4) |
| Chronic lung disease | 50,629 (8.0) | 437,259 (14.2) | 1,232,923 (16.7) |
| Vascular disease | 37,981 (6.0) | 220,963 (7.2) | 684,907 (9.3) |
| Anemia | 78,493 (12.4) | 350,164 (11.4) | 1,040,623 (14.1) |
| Coagulopathy | 45,757 (7.2) | 179,989 (5.9) | 360,478 (4.9) |
| Atrial fibrillation/flutter | 18,713 (2.9) | 273,159 (8.7) | 2,233,581 (29.5) |
| Liver cirrhosis | 7,977 (1.2) | 56,646 (1.8) | 46,239 (0.6) |
| Long-term dialysis/end-stage renal disease | 17,503 (2.7) | 91,937 (2.9) | 130,712 (1.7) |
| Intravenous drug use | 54,148 (8.3) | 136,123 (4.3) | 2,3587 (0.3) |
| Insurance/payer, no. (%) | |||
| Medicare | 61,152 (9.5) | 616,972 (19.6) | 6,736,387 (88.9) |
| Medicaid | 176,252 (27.2) | 594,758 (18.9) | 118,907 (1.6) |
| Private insurance | 279,426 (43.2) | 1,401,584 (44.6) | 580,990 (7.7) |
| Self-pay | 92039 (14.2) | 347932 (11.1) | 50123 (0.7) |
| No charge/others | 37950 (5.9) | 179329 (5.7) | 88485 (1.2) |
| Household income, no. (%) | |||
| 0-25th percentile | 202,581 (32.1) | 1,013,034 (33.0) | 1,956,900 (26.3) |
| 26th-50th percentile | 162,419 (25.7) | 792,401 (25.8) | 1,935,811 (26.0) |
| 51st-75th percentile | 144,440 (22.9) | 690,366 (22.5) | 1,809,418 (24.3) |
| 76th-100th percentile | 122,630 (19.4) | 571,451 (18.6) | 1,734,281 (23.3) |
For all comparisons, statistical significance was P<.001.
Figure 1.
Contribution of young, midlife, and older adults in stroke and cost burden in United States.
Demographic and Comorbidity Profile
The demographic characteristics and comorbidity burden of stroke hospitalizations varied significantly across age groups (Table 1). Midlife hospitalized stroke patients were more frequently men (57% [n=1,792,377]), while older patients were more frequently women (56% [n=4,239,664/3,344,011]). White race was the most frequent in all age groups, particularly in the older group (75.6% [n=4,878,285]), while the largest proportions of blacks (26.3% [n=144,786]), Hispanics (14.4% [n=79,451]), and others (8.3% [n=45,428]) were observed in the young group.
The prevalence of most chronic conditions, including hypertension, coronary artery disease, heart failure, vascular disease, and atrial fibrillation/flutter, was higher in older adults (P<.001 for all). However, stroke hospitalization in young and midlife adults was strongly associated with smoking, alcoholism, and intravenous drug abuse, the latter being particularly significant in young adults (8.3% [n=54,148]) (P<.001 for all). These patterns were consistent in ischemic and hemorrhagic stroke (Supplemental Tables 5 and 7, respectively).
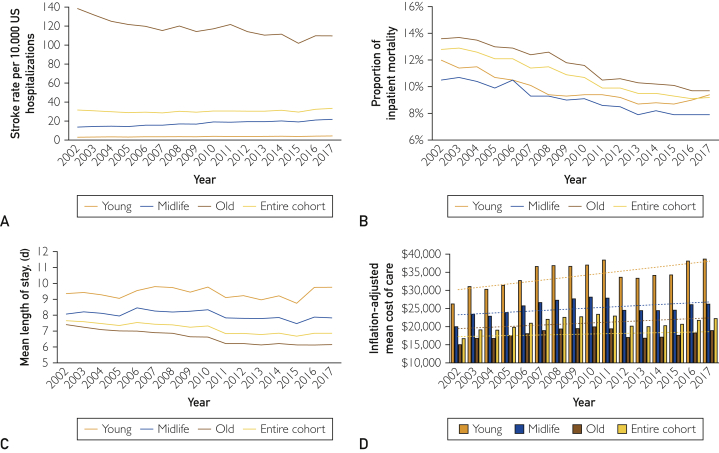
Temporal Trends in Stroke Hospitalization
During the study period, the overall hospitalization rates of stroke per 10,000 hospitalizations in the United States increased from 31.6 (95% CI, 31.5 to 31.7) to 33.3 (95% CI, 33.2 to 33.4), with AAPC of 1.5 (95% CI, 1.0, 1.9; Figure 2A). The hospitalization rates of stroke increased in young individuals (3.00 [95% CI, 2.9 to 3.1] to 4.3 [95% CI, 4.2 to 4.4]; AAPC, 2.0 [95% CI, 1.6 to 2.4]) and particularly in midlife adults, which made up the largest increased rate of the 3 age groups (13.6 [95% CI, 13.5 to 13.7] to 21.8 [95% CI, 21.7 to 21.9]; AAPC, 3.2 [95% CI, 2.7 to 3.6]). Conversely, these rates decreased over time in older persons (138.6 [95% CI, 138.3 to 138.9] to 109.7 [95% CI, 109.4 to 110.0]; AAPC, −1.4 [95% CI, −1.8 to −0.9]).
Figure 2.
Trends in: (A) stroke rates per 10,000 US hospitalizations in entire cohort, young, midlife, and older adults; (B) inpatient mortality in entire cohort, young, midlife, and older adults admitted with stroke; (C) length of stay in entire cohort, young, midlife, and older adults admitted with stroke; and (D) mean adjusted cost of stay in entire cohort, young, midlife, and older adults admitted with stroke.
These trends were consistent in ischemic and hemorrhagic stroke (Supplemental Figures 1 and 2, respectively, available online at https://mcpiqojournal.org).
Temporal Trends in In-Hospital Case Fatality
The proportion of fatal stroke hospitalizations was highest in older (11.6% [n=877,340]) than in young (9.8% [n=63,328]) and midlife (9.0% [n=281,560]) adults hospitalized from stroke in the United States (P<.001). Overall, the absolute number of deaths significantly decreased from 85,980 to 73,910 (AAPC, −1.1; 95% CI, −1.6 to −0.6]). Although inpatient case fatality decreased in all age groups (Figure 2B), the decline was slower in young (AAPC, −2.0; 95% CI, −2.7 to −1.3]) and midlife (AAPC, −2.3; 95% CI, −2.8 to −1.7]) adults compared with older (AAPC, −2.6; 95% CI, −3.0 to −2.2]) adults. These results were consistent in ischemic and hemorrhagic strokes (Supplemental Figures 3 and 4, respectively, available online at https://mcpiqojournal.org).
Trends in LOS and Resource Use
The mean LOS significantly decreased over time overall (from 7.7 to 6.9 days) in midlife (from 8.1 to 7.8 days) and older patients (from 7.4 to 6.2 days), but increased in young adults (from 9.4 to 9.8 days; P<.001 for trend; Figure 2C). The highest proportion of patients discharged home was observed in the midlife group (55.2% [n=1,734,978]), to a short-term care facility in the young group (6.3% [n=40,553]), and to a long-term care facility in the older group (48.2% [n=3,646,559]; Table 2). Although these trends were consistent in ischemic stroke, the mean LOS increased in both young (from 10.7 to 11.9 days) and midlife (from 10.3 to 10.8 days) patients and decreased in older adults in hemorrhagic stroke (from 7.9 to 7.2 days; P<.001 for trend; Supplemental Figures 5 and 6, respectively, available online at https://mcpiqojournal.org).
Table 2.
Distribution of Economic Variables in Stroke Across Study Groupsa
| Variable | Age Groups |
||
|---|---|---|---|
| Young | Midlife | Older | |
| Discharge disposition, no. (%) | 645,420 | 3,141,130 | 7,557,808 |
| Died | 63,328 (9.8) | 281,560 (9.0) | 877,340 (11.6) |
| Home | 389,983 (60.4) | 1,734,978 (55.2) | 2,753,723 (36.3) |
| Short-term care facility | 40,553 (6.3) | 148,538 (4.7) | 258,800 (3.4) |
| Long-term care facility | 142,152 (21.9) | 939,180 (29.9) | 3,646,559 (48.2) |
| Against medical advice | 11,404 (1.8) | 36,874 (1.2) | 21,386 (0.3) |
| Resource use | |||
| Cost ($), median (interquartile range) | 13,694 (7,321-32,523) | 10,678 (6,328-22,467) | 9,052 (5,605-16,531) |
| Length of stay (d), median (interquartile range) | 5 (2-11) | 4 (2-9) | 4 (3-8) |
For all comparisons, statistical significance was P<.001.
Over the entire study period, the cumulative overall inflation-adjusted cost of stroke was $224.5 billion, which accounted for $14 billion per year. Of this expenditure, 57.0% ($127.9 billion) was represented by older; 33.6% ($75.4 billion), by midlife; and 9.4% ($21.1 billion), by young adults. The cumulative total inflation-adjusted cost of ischemic stroke was $169.6 billion, accounting for $10.6 billion per year. Of this amount, 62.2% ($105.5 billion) was contributed by older; 30.5% ($51.7 billion), by midlife; and 7.3% ($12.3 billion), by young adults. The cumulative total inflation-adjusted hemorrhagic stroke cost was $66.1 billion, accounting for $4.1 billion per year, of which 41.6% ($27.4 billion) was contributed by older; 42.8% ($28.3 billion), by midlife; and 15.6% ($10.3 billion), by young adults.
The inflation-adjusted mean cost of stay increased consistently overall ($16,687 to $22,224) and in young ($26,266 to $38,626), midlife ($19,967 to $26,213), and older ($15,016 to $18,907) patients (Figure 2D). However, the average annual growth rate was highest in young adults (2.44%) compared with midlife (1.72%) and older (1.45%) patients.
This increase in cost was partly explained by prolonged LOS and higher use of thrombolysis, thrombectomy, craniotomy, echocardiogram, ventilators, cardiopulmonary resuscitation, tracheostomy, septic shock, vasopressors, and blood transfusions in young adults (Supplemental Table 9). These trends were consistent in ischemic and hemorrhagic strokes (Supplemental Figures 7 and 8, respectively, available online at https://mcpiqojournal.org).
Discussion
In this contemporary US national stroke hospitalization analysis, we observed several important patterns. First, the demographic profile, comorbidity burden, and type of stroke varied across age groups. Second, the rates of stroke hospitalizations increased among young and midlife adults but decreased in older patients, resulting in an overall increase over time. Third, inpatient mortality decreased, but the decline was slow in young and midlife adults compared with older patients. Fourth, the mean LOS increased in young adults and decreased in midlife and older patients; and fifth, the mean cost of stay increased, but the average annual growth rate was highest for young adults compared with midlife and older patients. The relatively higher increase in the cost of care in young adults was partly explained by longer LOS and increased health care resource use. These trends were consistent in ischemic and hemorrhagic strokes.
Nonwhite individuals, including blacks, Hispanics, and others, represented a large proportion in the young adult group, whereas 3 of 4 stokes in the older group occurred in white persons. These findings are consistent with prior published data.16,17 In the national Reasons for Geographic and Racial Differences in Stroke Study (2003-2007), age and sex-adjusted black/white incidence rate ratios were higher (4.02) for adults aged 45 to 54 years, while the incidence rate ratio decreased for those 85 years and older (0.86).17 In the Greater Cincinnati/Northern Kentucky Stroke Study, risk ratios for blacks vs whites varied from 4.18 in 35- to 44-year-old to 1.66 in 65- to 74-year-old patients.16 Similarly, the Brain Attack Surveillance in Corpus Christi Project demonstrated that Hispanics had a higher relative risk for stroke (2.04) than non-Hispanics whites at a younger age (45-59 years), but not at an older age (≥75 years; risk ratio, 1.12).18
These trends toward a higher proportion of individuals from minority groups among young stroke cases likely emerge from a multitude of factors, including a higher prevalence of cardiometabolic risk factors compared with whites of the same age, such as hypertension and diabetes and earlier onset of vascular risk factors in blacks,19, 20, 21 lower socioeconomic status,17 lower access to care,16,22 genetic predisposition such as the higher propensity of cavernous malformations in Hispanics,23 and limited awareness among racial minorities,18,24 among other factors. For instance, a county-based study illustrated that Hispanics had less awareness regarding risk factors and preventive strategies and were less likely to perceive stroke symptoms compared with whites.24
The data reported here confirm a continuation of prior national patterns by illustrating a higher frequency of hemorrhagic stroke in younger and midlife adults vs ischemic stroke in older adults.5 The distribution of particular risk factors among different age groups might have influenced the distribution of stroke subtypes. For instance, the common risk factors for hemorrhagic stroke are smoking, alcohol use, drug abuse, and coagulopathy, which occurred more frequently in the nonelderly population. Similarly, chronic conditions, particularly key cardiovascular diseases such as atrial fibrillation, explain a higher proportion of ischemic stroke in older adults.
In the Atherosclerosis Risk in Communities Study, the age-adjusted incidence of stroke decreased in older (aged ≥65 years) patients (absolute decrease of 1.35/1000 person-years) but remained flat in younger (aged <65 years) patients (absolute decrease of 0.09/1000 person-years) between 1987 and 2011.6 In the Brain Attack Surveillance in Corpus Christi Project (2000-2010), ischemic stroke rates decreased in adults 60 years and older but were static in those aged 45 to 59 years.25 The previous NIS report up to 2012 showed higher rates of acute ischemic stroke hospitalizations in those aged 18 to 44 years, stagnant rates for hemorrhagic stroke, and reduction in hemorrhagic stroke rates in specific demographic subsets aged 45 to 54 years.5 Our study also demonstrated a reduction in stroke in older adults; however, we report 2% and 3% annual increases in hospitalization rates among young and midlife adults, respectively. Unhealthy lifestyle behaviors such as smoking, drug abuse, and hypertension have likely contributed to these shifting trends.5 In this regard, the decline in mortality was slower in younger and midlife adults than older patients. The notable improvement in the prognosis of older patients may reflect progress in medical therapy, cardiovascular risk mitigation, and use of quality improvement programs.5,26 However, the growing stroke burden in young and midlife patients highlights that cardiovascular prevention and management strategies might not have penetrated equally in nonelderly patients and indicate that targeted efforts to these subgroups are necessary.
Preliminary national data reported that the total estimated cost of stroke was $45.5 billion in 2014 to 2015.2 The direct estimated cost (encompassing outpatient visits, inpatient stays, emergency department visits, prescribed medicines, and home health care facilities) was $28.0 billion.2 The total direct cost of care in stroke is projected to increase from $36.7 to $94.3 billion between 2015 and 2035, with significant growth expected to occur in patients 80 years and older.27 Between 2002 and 2017, we document the total inflation-adjusted cost of more than $42.5 billion per year for stroke hospitalizations, of which more than half was contributed by older patients owing to a higher stroke burden compared with the other age groups. Although this pattern was consistent for ischemic stroke, more than 50% of the cost was contributed by midlife and young adults in hemorrhagic stroke, which was disproportionally higher than their combined stroke burden. Similarly, while the cost of stay increased in older patients, the average annual growth rate in the expenditure was relatively higher among young adults vs midlife (absolute difference, 0.71%) and older (absolute difference, 1.05%) patients, owing to extended LOS and use of health care resources.
In this context, the growing use of advanced interventional procedures such as thrombectomy may affect care costs. In a review of studies conducted in high-income countries, intravenous thrombolytics imparted costs ranging from $4000 to $75,000 per quality-adjusted life-year saved.28 According to the World Health Organization, an intervention is cost-effective if it costs less than 3 times the annual gross domestic product or gross national income per capita of a country per each quality-adjusted life-year saved or disability-adjusted life-year averted.29 Based on this standard, thrombolytics for acute stroke treatment are not a cost-effective investment, at least for low-income countries.30 Moreover, an increase in indirect cost should be accounted for given the tradeoff between improving life expectancy and potentially increasing morbidity.
Additionally, a higher proportion of patients being discharged to short-term care facilities might have further contributed to the disease's growing economic burden on young adults. On the same note, the perceived benefits of stroke and mortality reduction were counterbalanced by increasing the cost of a stay, further amplified by a higher proportion of discharge disposition to long-term care facilities. These concerning statistics should inform health stakeholders, including policymakers, payers, and providers, and call for urgent efforts to ensure value-based care to the patients.
This analysis has several shortcomings. Given the NIS database's inherent limitations, which exclusively focuses on hospitalizations rather than patients, longitudinal estimates of recurrent hospitalization rates cannot be computed. Therefore, patients with multiple strokes over time cannot be identified and hence can potentially influence the estimates. We could not adjust for opportunity cost in this analysis. We could not analyze information regarding the anatomy of stroke, severity of the stroke, disability caused by stroke, and relevant outcomes. Also, the NIS is an administrative database and relies on ICD coding for billing purposes, which is subject to misclassification.31 The ICD coding system changed from ICD-9-CM to ICD-1- CM from 2015 to 2016. Moreover, the method of collecting samples after 2011 changed. That said, we adjusted for these issues using weights provided by HCUP. Our analyses did not account for the outpatient clinical and economic burden of stroke and were restricted to in-hospital data. Also, the NIS database does not contain information on pharmacotherapy or laboratory values. Despite these limitations, the NIS data set is a well-validated tool to analyze a variety of diseases, procedures, and health care expenditures with reasonable accuracy.32
Conclusion
The last 16 years have witnessed significant temporal changes in stroke hospitalization rates, inpatient mortality, and associated cost expenditure, which varied significantly across different age groups. Young adults demonstrated an increased burden of stroke and cost of care and slowed in mortality than midlife and older patients. Older adults demonstrated reductions in stroke and mortality at the expense of a higher cost of care over time. Further public health interventions aimed at preventing the onset of stroke across all age groups, particularly in young and midlife adults, and interventions to reduce the cost of care while maximizing value are needed to curb these trends.
Footnotes
Potential Competing Interests: Dr Virani reports grant support: Department of Veterans Affairs, World Heart Federation, Tahir, and Jooma Family Honorarium; American College of Cardiology (Associate Editor for Innovations, acc.org) Steering Committee member; Patient and Provider Assessment of Lipid Management registry at the Duke Clinical Research Institute (no financial remuneration). The other authors report no competing interests.
Supplemental material can be found online at http://mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.Centers for Disease Control and Prevention. Underlying cause of death 1999-2019. Accessed July 1, 2020. https://wonder.cdc.gov/wonder/help/ucd.html.
- 2.Virani S.S., Alonso A., Benjamin E.J., on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics–2020 update: a report from the American Heart Association. Circulation. 2020;141(9):e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 3.Benjamin E.J., Blaha M.J., Chiuve S.E., American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skolarus L.E., Freedman V.A., Feng C., Wing J.J., Burke J.F. Care received by elderly US stroke survivors may be underestimated. Stroke. 2016;47(8):2090–2095. doi: 10.1161/STROKEAHA.116.012704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.George M.G., Tong X., Bowman B.A. Prevalence of cardiovascular risk factors and strokes in younger adults. JAMA Neurol. 2017;74(6):695–703. doi: 10.1001/jamaneurol.2017.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koton S., Schneider A.L., Rosamond W.D. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014;312(3):259–268. doi: 10.1001/jama.2014.7692. [DOI] [PubMed] [Google Scholar]
- 7.HCUP NIS Database Documentation. Healthcare Cost and Utilization Project (HCUP). Accessed July 2, 2020. https://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp.
- 8.Chen T.S., Incani A., Butler T.C. The demographic profile of young patients (<45 years-old) with acute coronary syndromes in Queensland. Heart Lung Circ. 2014;23(1):49–55. doi: 10.1016/j.hlc.2013.05.648. [DOI] [PubMed] [Google Scholar]
- 9.Morillas P.J., Cabades A., Bertomeu V., Investigadores del PRIMVAC Acute myocardial infarction in patients under 45 years [article in Spanish] Rev Esp Cardiol. 2002;55(11):1124–1131. doi: 10.1016/s0300-8932(02)76774-2. [DOI] [PubMed] [Google Scholar]
- 10.Donahue R.P., Abbott R.D., Reed D.M., Yano K. Physical activity and coronary heart disease in middle-aged and elderly men: the Honolulu Heart Program. Am J Public Health. 1988;78(6):683–685. doi: 10.2105/ajph.78.6.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kramarow E., Lubitz J., Francis R., Jr. Trends in the coronary heart disease risk profile of middle-aged adults. Ann Epidemiol. 2013;23(1):31–34. doi: 10.1016/j.annepidem.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yazdanyar A., Newman A.B. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med. 2009;25(4):563–577. doi: 10.1016/j.cger.2009.07.007. vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alkhouli M., Alqahtani F., Alhajji M., Berzingi C.O., Sohail M.R. Clinical and economic burden of hospitalizations for infective endocarditis in the United States. Mayo Clin Proc. 2020;95(5):858–866. doi: 10.1016/j.mayocp.2019.08.023. [DOI] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research and Quality. Trend weights for HCUP NIS Data. Accessed May 22, 2020. https://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp
- 15.Kim H.J., Fay M.P., Feuer E.J., Midthune D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 16.Kleindorfer D., Broderick J., Khoury J. The unchanging incidence and case-fatality of stroke in the 1990s: a population-based study. Stroke. 2006;37(10):2473–2478. doi: 10.1161/01.STR.0000242766.65550.92. [DOI] [PubMed] [Google Scholar]
- 17.Howard V.J., Kleindorfer D.O., Judd S.E. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol. 2011;69(4):619–627. doi: 10.1002/ana.22385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morgenstern L.B., Smith M.A., Lisabeth L.D. Excess stroke in Mexican Americans compared with non-Hispanic whites: the Brain Attack Surveillance in Corpus Christi Project. Am J Epidemiol. 2004;160(4):376–383. doi: 10.1093/aje/kwh225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sacco R.L., Boden-Albala B., Abel G. Race-ethnic disparities in the impact of stroke risk factors: the northern Manhattan stroke study. Stroke. 2001;32(8):1725–1731. doi: 10.1161/01.str.32.8.1725. [DOI] [PubMed] [Google Scholar]
- 20.Cushman M., McClure L.A., Howard V.J., Jenny N.S., Lakoski S.G., Howard G. Implications of increased C-reactive protein for cardiovascular risk stratification in black and white men and women in the US. Clin Chem. 2009;55(9):1627–1636. doi: 10.1373/clinchem.2008.122093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howard G., Prineas R., Moy C. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke study. Stroke. 2006;37(5):1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]
- 22.Christian J.B., Lapane K.L., Toppa R.S. Racial disparities in receipt of secondary stroke prevention agents among US nursing home residents. Stroke. 2003;34(11):2693–2697. doi: 10.1161/01.STR.0000096993.90248.27. [DOI] [PubMed] [Google Scholar]
- 23.Sahoo T., Johnson E.W., Thomas J.W. Mutations in the gene encoding KRIT1, a Krev-1/rap1a binding protein, cause cerebral cavernous malformations (CCM1) Hum Mol Genet. 1999;8(12):2325–2333. doi: 10.1093/hmg/8.12.2325. [DOI] [PubMed] [Google Scholar]
- 24.Morgenstern L.B., Steffen-Batey L., Smith M.A., Moye L.A. Barriers to acute stroke therapy and stroke prevention in Mexican Americans. Stroke. 2001;32(6):1360–1364. doi: 10.1161/01.str.32.6.1360. [DOI] [PubMed] [Google Scholar]
- 25.Morgenstern L.B., Smith M.A., Sánchez B.N. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Ann Neurol. 2013;74(6):778–785. doi: 10.1002/ana.23972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lackland D.T., Roccella E.J., Deutsch A.F., American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; Council on Functional Genomics and Translational Biology Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45(1):315–353. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dunbar S.B., Khavjou O.A., Bakas T. American Heart Association. Projected costs of informal caregiving for cardiovascular disease: 2015 to 2035: a policy statement from the American Heart Association. Circulation. 2018;137(19):e558–e577. doi: 10.1161/CIR.0000000000000570. [DOI] [PubMed] [Google Scholar]
- 28.Pan F., Hernandez L., Ward A. Cost-effectiveness of stroke treatments and secondary preventions. Expert Opin Pharmacother. 2012;13(12):1751–1760. doi: 10.1517/14656566.2012.699522. [DOI] [PubMed] [Google Scholar]
- 29.Hutubessy R., Chisholm D., Edejer T. Generalized cost-effectiveness analysis for national-level priority-setting in the health sector. Cost Eff Resour Alloc. 2004;1(1):8. doi: 10.1186/1478-7547-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Werner K., Risko N., Burkholder T., Munge K., Wallis L., Reynolds T. Cost-effectiveness of emergency care interventions in low and middle-income countries: a systematic review. Bull World Health Organ. 2020;98(5):341–352. doi: 10.2471/BLT.19.241158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ramirez L., Kim-Tenser M.A., Sanossian N. Trends in acute ischemic stroke hospitalizations in the United States. J Am Heart Assoc. 2016;5(5):e003233. doi: 10.1161/JAHA.116.003233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alkhouli M., Alqahtani F., Ziada K.M., Aljohani S., Holmes D.R., Mathew V. Contemporary trends in the management of aortic stenosis in the USA. Eur Heart J. 2019;41(8):921–928. doi: 10.1093/eurheartj/ehz568. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.