Abstract
Background
Pressure ulcers (also known as pressure injuries, pressure sores, decubitus ulcers and bed sores) are localised injuries to the skin or underlying soft tissue, or both, caused by unrelieved pressure, shear or friction. Alternating pressure (active) air surfaces are widely used with the aim of preventing pressure ulcers.
Objectives
To assess the effects of alternating pressure (active) air surfaces (beds, mattresses or overlays) compared with any support surface on the incidence of pressure ulcers in any population in any setting.
Search methods
In November 2019, we searched the Cochrane Wounds Specialised Register; the Cochrane Central Register of Controlled Trials (CENTRAL); Ovid MEDLINE (including In‐Process & Other Non‐Indexed Citations); Ovid Embase and EBSCO CINAHL Plus. We also searched clinical trials registries for ongoing and unpublished studies, and scanned reference lists of relevant included studies as well as reviews, meta‐analyses and health technology reports to identify additional studies. There were no restrictions with respect to language, date of publication or study setting.
Selection criteria
We included randomised controlled trials that allocated participants of any age to alternating pressure (active) air beds, overlays or mattresses. Comparators were any beds, overlays or mattresses.
Data collection and analysis
At least two review authors independently assessed studies using predetermined inclusion criteria. We carried out data extraction, 'Risk of bias' assessment using the Cochrane 'Risk of bias' tool, and the certainty of the evidence assessment according to Grading of Recommendations, Assessment, Development and Evaluations methodology.
Main results
We included 32 studies (9058 participants) in the review. Most studies were small (median study sample size: 83 participants). The average age of participants ranged from 37.2 to 87.0 years (median: 69.1 years). Participants were largely from acute care settings (including accident and emergency departments). We synthesised data for six comparisons in the review: alternating pressure (active) air surfaces versus: foam surfaces, reactive air surfaces, reactive water surfaces, reactive fibre surfaces, reactive gel surfaces used in the operating room followed by foam surfaces used on the ward bed, and another type of alternating pressure air surface. Of the 32 included studies, 25 (78.1%) presented findings which were considered at high overall risk of bias.
Primary outcome: pressure ulcer incidence
Alternating pressure (active) air surfaces may reduce the proportion of participants developing a new pressure ulcer compared with foam surfaces (risk ratio (RR) 0.63, 95% confidence interval (CI) 0.34 to 1.17; I2 = 63%; 4 studies, 2247 participants; low‐certainty evidence). Alternating pressure (active) air surfaces applied on both operating tables and hospital beds may reduce the proportion of people developing a new pressure ulcer compared with reactive gel surfaces used on operating tables followed by foam surfaces applied on hospital beds (RR 0.22, 95% CI 0.06 to 0.76; I2 = 0%; 2 studies, 415 participants; low‐certainty evidence).
It is uncertain whether there is a difference in the proportion of people developing new pressure ulcers between alternating pressure (active) air surfaces and the following surfaces, as all these comparisons have very low‐certainty evidence: (1) reactive water surfaces; (2) reactive fibre surfaces; and (3) reactive air surfaces.
The comparisons between different types of alternating pressure air surfaces are presented narratively. Overall, all comparisons suggest little to no difference between these surfaces in pressure ulcer incidence (7 studies, 2833 participants; low‐certainty evidence).
Included studies have data on time to pressure ulcer incidence for three comparisons. When time to pressure ulcer development is considered using a hazard ratio (HR), it is uncertain whether there is a difference in the risk of developing new pressure ulcers, over 90 days' follow‐up, between alternating pressure (active) air surfaces and foam surfaces (HR 0.41, 95% CI 0.10 to 1.64; I2 = 86%; 2 studies, 2105 participants; very low‐certainty evidence). For the comparison with reactive air surfaces, there is low‐certainty evidence that people treated with alternating pressure (active) air surfaces may have a higher risk of developing an incident pressure ulcer than those treated with reactive air surfaces over 14 days' follow‐up (HR 2.25, 95% CI 1.05 to 4.83; 1 study, 308 participants). Neither of the two studies with time to ulcer incidence data suggested a difference in the risk of developing an incident pressure ulcer over 60 days' follow‐up between different types of alternating pressure air surfaces.
Secondary outcomes
The included studies have data on (1) support‐surface‐associated patient comfort for comparisons involving foam surfaces, reactive air surfaces, reactive fibre surfaces and alternating pressure (active) air surfaces; (2) adverse events for comparisons involving foam surfaces, reactive gel surfaces and alternating pressure (active) air surfaces; and (3) health‐related quality of life outcomes for the comparison involving foam surfaces. However, all these outcomes and comparisons have low or very low‐certainty evidence and it is uncertain whether there are any differences in these outcomes.
Included studies have data on cost effectiveness for two comparisons. Moderate‐certainty evidence suggests that alternating pressure (active) air surfaces are probably more cost‐effective than foam surfaces (1 study, 2029 participants) and that alternating pressure (active) air mattresses are probably more cost‐effective than overlay versions of this technology for people in acute care settings (1 study, 1971 participants).
Authors' conclusions
Current evidence is uncertain about the difference in pressure ulcer incidence between using alternating pressure (active) air surfaces and other surfaces (reactive water surfaces, reactive fibre surfaces and reactive air surfaces). Alternating pressure (active) air surfaces may reduce pressure ulcer risk compared with foam surfaces and reactive gel surfaces used on operating tables followed by foam surfaces applied on hospital beds. People using alternating pressure (active) air surfaces may be more likely to develop new pressure ulcers over 14 days' follow‐up than those treated with reactive air surfaces in the nursing home setting; but as the result is sensitive to the choice of outcome measure it should be interpreted cautiously. Alternating pressure (active) air surfaces are probably more cost‐effective than reactive foam surfaces in preventing new pressure ulcers.
Future studies should include time‐to‐event outcomes and assessment of adverse events and trial‐level cost‐effectiveness. Further review using network meta‐analysis adds to the findings reported here.
Plain language summary
Do beds, mattresses and mattress toppers with air‐filled surfaces that regularly redistribute pressure under the body prevent pressure ulcers?
Key messages
Beds, mattresses and mattress toppers that regularly redistribute pressure under the body may reduce the chance of pressure ulcers developing when compared with surfaces that:
‐ apply a constant pressure to the skin; and
‐ are made of foam or gel.
However, they may increase the risk of pressure ulcers developing among nursing home residents when compared with air surfaces that apply constant pressure.
More research is needed to strengthen the evidence that compares air‐filled and other surfaces. Future studies should focus on effects that are important to decision‐makers, including:
‐ whether and when pressure ulcers develop;
‐ unwanted effects; and
‐ costs.
What are pressure ulcers?
Pressure ulcers are also known as pressure sores or bed sores. They are wounds to the skin and underlying tissue caused by prolonged pressure or rubbing. They often occur on bony parts of the body, such as heels, elbows, hips and the bottom of the spine. People who have mobility problems or who lie in bed for long periods are at risk of developing pressure ulcers.
What did we want to find out?
There are beds, mattresses and mattress toppers specifically designed for people at risk of pressure ulcers. These can be made of a range of materials (such as foam, air cells or water bags) and are divided into two groups:
‐ reactive (static) surfaces that apply a constant pressure to the skin, unless a person moves or is repositioned; and
‐ active (alternating pressure) surfaces that regularly redistribute the pressure under the body.
We wanted to find out if active, air‐filled surfaces:
‐ prevent pressure ulcers;
‐ are comfortable and improve people’s quality of life;
‐ have health benefits that outweigh their costs (cost‐effectiveness); and
‐ have any unwanted effects.
What did we do?
We searched the medical literature for studies that evaluated the effects of beds, mattresses and mattress toppers with an active, air‐filled surface. We compared and summarised their results, and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found 32 studies (9058 people, average age: 69 years) that lasted between three and 180 days (average: 14 days). The studies compared active, air‐filled surfaces with:
‐ foam, fibre, water‐filled or gel surfaces; and
‐ other air‐filled surfaces.
Pressure ulcer prevention
The evidence suggests that active, air‐filled surfaces may reduce the risk of pressure ulcers developing when compared with:
‐ foam surfaces;
‐ gel surfaces used on operating tables followed by foam surfaces used on hospitals beds, for people who undergo surgery.
However, active, air‐filled surfaces may increase the risk of pressure ulcers developing when compared with reactive air surfaces (1 study, 308 nursing home residents, duration: 14 days).
It is unclear if active air‐filled surfaces prevent pressure ulcers compared with surfaces other than reactive foam, gel or air‐filled surfaces.
The type of active, air‐filled surface used may make little to no difference for preventing pressure ulcers.
Other effects
Active, air‐filled surfaces are probably more cost‐effective than foam. Mattresses with an active, air‐filled surface are probably more cost‐effective than mattress toppers with the same surface.
We did not find sufficiently robust and clear evidence to determine how active, air‐filled surfaces affect comfort, quality of life and unwanted effects.
What limited our confidence in the evidence?
Most studies were small (83 people on average) and more than two‐thirds of them (25) used methods likely to introduce errors in their results.
How up‐to‐date is this review?
The evidence in this Cochrane Review is current to November 2019.
Summary of findings
Background
Description of the condition
Pressure ulcers (also known as pressure injuries, pressure sores, decubitus ulcers and bed sores) are localised injuries to the skin or underlying soft tissue, or both, caused by unrelieved pressure, shear or friction (NPIAP 2016). Pressure ulcer severity is generally classified using the National Pressure Injury Advisory Panel (NPIAP) system (NPIAP 2016).
Stage 1: intact skin with a local appearance of non‐blanchable erythema.
Stage 2: partial‐thickness skin loss with exposed dermis.
Stage 3: full‐thickness skin loss.
Stage 4: full‐thickness skin and tissue loss with visible fascia, muscle, tendon, ligament, cartilage or bone.
Unstageable pressure injury: full‐thickness skin and tissue loss that is obscured by slough or eschar so that the severity of injury cannot be confirmed.
A deep tissue pressure injury: local injury of persistent, non‐blanchable deep red, maroon, purple discolouration or epidermal separation revealing a dark wound bed or blood‐filled blister.
These above stages of pressure ulcer are consistent with those described in another commonly used system: the International Classification of Diseases for Mortality and Morbidity Statistics of the World Health Organization 2019.
Pressure ulcers are relatively common, complex wounds affecting people across different care settings. A systematic review found that prevalence estimates for people affected by pressure ulcers in communities of the UK, USA, Ireland, and Sweden ranged from 5.6 to 2300 per 10,000 depending on the nature of the population surveyed (Cullum 2016). A subsequent cross‐sectional survey of people receiving community health services in one city in the UK estimated that 1.8 people per 10,000 have a pressure ulcer (Gray 2018).
Pressure ulcers confer a heavy burden in terms of personal impact and health service resource use. Having a pressure ulcer may impair physical, social and psychological activities (Gorecki 2009). Ulceration impairs health‐related quality of life (Essex 2009); can result in longer institution stays (Theisen 2012); and increases the risk of systemic infection (Espejo 2018). There are also substantial impacts on health systems. A 2015 systematic review of 14 studies across a range of care settings in Europe and North America, showed that pressure ulcer‐related treatment costs ranged between EUR 1.71 and EUR 470.49 per person, per day (Demarré 2015). In the UK, the annual average National Health Service cost attributable to managing one person with a pressure ulcer in the community was estimated to be GBP 1400 for a Stage 1 pressure ulcer and more than GBP 8500 for more severe stages (2015/2016 prices; Guest 2018). In Australia, the annual cost of treating pressure ulcers was estimated to be AUD 983 million (95% confidence interval (CI) 815 to 1151 million) at 2012/2013 prices (Nguyen 2015). The serious consequences of pressure ulceration have led to an intensive focus on their prevention.
Description of the intervention
Pressure ulcers are considered largely preventable. Support surfaces are specialised medical devices designed to relieve or redistribute pressure on the body, or both, in order to prevent pressure ulcers (NPIAP S3I 2007). Types of support surface include, but are not limited to, integrated bed systems, mattresses and overlays (NPIAP S3I 2007).
Classification of support surface type can now be based on the NPIAP Support Surface Standards Initiative (S3I) terms and definitions related to support surfaces (NPIAP S3I 2007). According to the NPIAP S3I terms and definitions support surfaces may:
be powered (i.e. require electrical power to function) or non‐powered;
passively redistribute body weight (i.e. reactive pressure redistribution), or mechanically alternate the pressure on the body to reduce the duration of pressure (i.e. active pressure redistribution);
be made of a range of materials including but not limited to: air‐cells, foam materials, fibre materials, gel materials, sheepskin for medical use, and water‐bags;
be constructed of air‐filled cells that have small holes on the surface for blowing out air to dry skin (i.e. low‐air‐loss feature) or have fluid‐like characteristics via forcing filtered air through ceramic beads (i.e. air‐fluidised feature), or have neither of these features.
Full details of support surface classifications are listed in Appendix 1. A widely used type of support surface is the alternating pressure (active) air bed, mattress or overlay (traditionally termed alternating pressure, or dynamic air bed, mattress or overlay). Examples of types of alternating pressure air beds, mattresses or overlays include:
powered active air mattresses (e.g. Nimbus II, MicroPulse, large‐celled ripple);
powered active low‐air‐loss mattresses;
powered hybrid system air mattresses (e.g. TheraPulse);
powered hybrid system low‐air‐loss mattresses.
These mattresses are made of air‐cells that intermittently inflate and deflate via electrically powered pumps (Clark 2011; NPIAP S3I 2007). Additionally, these active, alternating pressure air mattresses can have an integrated reactive element to create so‐called 'hybrid' mattresses (Fletcher 2015). Alternating pressure (active) air mattresses can have low‐air‐loss features designed to influence the microclimate environment by keeping the skin dry (since moisture is thought to potentially increase friction on skin and increase the risk of skin damage) (Clark 2011; Wounds International 2010).
How the intervention might work
Support surfaces that can prevent pressure ulceration aim to redistribute pressure beneath the body, facilitating blood flow to tissues and preventing skin and soft tissue distortion (Wounds International 2010). Active support surfaces (e.g. alternating pressure (active) air bed, mattress or overlay) achieve pressure redistribution by frequently changing the points of contact between the surface and body, reducing the duration of the pressure applied to specific anatomical sites (Clark 2011; NPIAP S3I 2007). This contrasts with the mode of action of reactive support surfaces, which is more passive and includes immersion (i.e. 'sinking' of the body into a support surface) and envelopment (i.e. conforming of a support surface to the irregularities of the body). These devices distribute the pressure over a greater area, thereby reducing the magnitude of the pressure at specific sites (Clark 2011).
Why it is important to do this review
Support surfaces are widely used for pressure ulcer prevention and are the focus of recommendations in international and national guidelines (EPUAP/NPIAP/PPPIA 2019; NICE 2014). Since the publication of the Cochrane Review, 'Support surfaces for pressure ulcer prevention' (McInnes 2015), there has been a substantial increase in the number of relevant randomised controlled trials (RCTs) published; recognition of the NPIAP S3I 2007 terms and definitions related to support surfaces; and new Cochrane methodological requirements, such as the use of GRADE assessments (Guyatt 2008). These developments mean that it is important to update the evidence base.
In considering this evidence update, we took into account the size and complexity of 'Support surfaces for pressure ulcer prevention' (McInnes 2015), which included all support surface types. An alternative approach is to split the review into multiple new titles, each with a narrower focus. We consulted on this splitting option via an international survey in August 2019. The potential new titles suggested were based on clinical use, the new terms and definitions related to support surfaces (NPIAP S3I 2007), a relevant network meta‐analysis (Shi 2018a), and current clinical practice guidelines (EPUAP/NPIAP/PPPIA 2019; NICE 2014). We received responses from 29 health professionals involved in pressure ulcer prevention activity in several countries (Australia, Belgium, China, Italy, the Netherlands and the UK). In total, 83% of respondents supported splitting the review into suggested titles and 17% were unsure (no respondent voted against splitting). The new review titles are:
Alternating pressure (active) air surfaces for preventing pressure ulcers;
Foam surfaces for preventing pressure ulcers;
Reactive air surfaces for preventing pressure ulcers; and
Alternative reactive support surfaces (non‐foam and non‐air‐filled) for preventing pressure ulcers.
We bring the results of these new reviews together in an overview with a network meta‐analysis (Salanti 2012), in order to compare simultaneously all support surfaces and to rank them based on the probabilities of each being the most effective for preventing pressure ulcers (Shi 2021).
This particular review compares alternating pressure (active) air beds, mattresses or overlays with any surface.
Objectives
To assess the effects of alternating pressure (active) air surfaces (beds, mattresses or overlays) compared with any support surface on the incidence of pressure ulcers in any population in any setting.
Methods
Criteria for considering studies for this review
Types of studies
We included published and unpublished RCTs (including multi‐arm studies, cluster‐RCTs and cross‐over trials), regardless of the language in which they were reported. We also included RCTs with particular designs (factorial design, n‐of‐1 trial design (i.e. a randomised controlled cross‐over trial in a single participant)). We excluded studies using quasi‐random allocation methods (e.g. alternation).
Types of participants
We included studies in any populations, including those defined as being at risk of ulceration, as well as those with existing pressure ulcers at baseline (when the study measured pressure ulcer incidence).
Types of interventions
This review focused on alternating pressure (active) air beds or mattresses in general. Eligible studies included a specific bed, overlay or mattress with active pressure redistribution (or alternating pressure) capabilities. These included, but were not limited to, specific active mattresses identified in Shi 2018a; namely:
powered active air mattresses (also known as alternating pressure air mattresses); or
powered active low‐air‐loss mattresses (also known as dynamic low‐air‐loss mattresses); or
powered hybrid system air mattresses (e.g. Softform Premier Active air mattresses); or
powered hybrid system low‐air‐loss mattresses (e.g. TheraPulse ATP mattresses).
In this review, we considered hybrid mattresses to be systems that incorporate both active and reactive pressure redistribution modes in a single unit and could apply either of the two modes as required by the user. For those using such hybrid mattresses, potential pressure ulcer risk reduction may result from both modes being used interchangeably over time, rather than being the result of constantly applying a single mode.
We included studies where two or more support surfaces were used sequentially over time or in combination, where the support surface(s) of interest were included in one of the study arms.
We included studies comparing eligible alternating pressure (active) air beds, overlays or mattresses with any comparator defined as a support surface. Comparators could be:
non‐alternating pressure (active) air surfaces, including: reactive air surfaces (e.g. static air overlays, dry flotation mattresses, air‐fluidised bed), foam mattresses, and non‐foam and non‐air‐filled surfaces (e.g. reactive gel surfaces such as a gel pad used on an operating table, reactive fibre surfaces such as Silicore fibre overlay, reactive water surfaces, reactive sheepskin surfaces such as Australian Medical Sheepskins overlay); or
a different type of alternating pressure (active) air surface.
We included studies in which co‐interventions (e.g. repositioning) were delivered, provided that co‐interventions between a study’s arms were the same (i.e. interventions randomised were the only systematic difference).
Types of outcome measures
We considered the primary and secondary outcomes described below. If a study was otherwise eligible (i.e. eligible study design, participants and interventions) but did not report any review‐relevant outcomes, we contacted the study authors where possible to clarify whether they measured a relevant outcome but did not report it. We placed the study in 'Studies awaiting classification' if we could not establish whether it measured an outcome or not. We excluded the study if the study authors confirmed that they did not measure any review‐relevant outcomes.
For a study that measured an outcome at multiple time points, we considered outcome measures at three months as the primary interest of this review (Schoonhoven 2007), regardless of the time points specified as being of primary interest by the study. If the study did not report three‐month outcome measures, we considered those closest to three months in this review. Where a study only reported a single time point, we considered these data in this review. Where the study did not specify a time point for their outcome measurement, we assumed this was the final duration of follow‐up noted.
Primary outcomes
Our primary outcome was pressure ulcer incidence. We recorded two outcome measures (the proportion of participants developing a new pressure ulcer; and time to pressure ulcer development) where available. However, we considered the proportion of participants developing a new pressure ulcer as the primary outcome for this review. Time to pressure ulcer development was our preferred measure; however, we did not expect it to be reported in many studies. We extracted and analysed time‐to‐event data but focused on the binary outcome in our conclusions. We accepted authors' definitions of an incident ulcer regardless of which pressure ulcer severity classification was used to measure or grade new pressure ulcers. We also considered the outcome of pressure ulcer incidence irrespective of whether studies report ulcers by stages or as a non‐stratified value.
We did not consider subjective outcome measures (e.g. 'better' or 'worse' skin condition) as measures of pressure ulcer incidence.
Secondary outcomes
Support‐surface‐associated patient comfort. We considered patient comfort outcome data in this review only if the evaluation of patient comfort was pre‐planned and was systematically conducted across all participants in the same way in a study. The definition and measurement of this outcome varied from one study to another; for example, the proportion of participants who report comfort, or comfort measured by a scale with continuous (categorical) numbers. We planned to include these data with different measurements in separate meta‐analyses when possible.
All reported adverse events (measured using surveys or questionnaires, other data capture process or visual analogue scale). We included data where study authors specified a clear method for collecting adverse event data. Where available, we extracted data on all serious and all non‐serious adverse events as an outcome. We recorded where it was clear that events were reported at the participant level or whether multiple events per person were reported, in which case appropriate adjustments were required for data clustering (Peryer 2019). We considered the assessment of any event in general defined as adverse by participants, health professionals, or both.
Health‐related quality of life (measured using a standardised generic questionnaire such as EQ‐5D (Herdman 2011), 36‐item Short Form (SF‐36; Ware 1992), or pressure ulcer‐specific questionnaires such as the PURPOSE Pressure Ulcer Quality of Life (PU‐QOL) questionnaire (Gorecki 2013), at noted time points). We did not include ad hoc measures of quality of life or qualitative interviews of quality of life because these measures were unlikely to be validated.
Cost‐effectiveness: within‐trial cost‐effectiveness analysis comparing mean differences in effects with mean cost differences between the two arms: we extracted data on incremental mean cost per incremental gain in benefit (incremental cost‐effectiveness ratio (ICER)). We also considered other measures of relative cost‐effectiveness (e.g. net monetary benefit, net health benefit).
Search methods for identification of studies
Electronic searches
We searched the following electronic databases to identify reports of relevant clinical trials:
the Cochrane Wounds Specialised Register (searched 14 November 2019);
the Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 10) in the Cochrane Library (searched 14 November 2019);
Ovid MEDLINE including In‐Process & Other Non‐Indexed Citations (1946 to 14 November 2019);
Ovid Embase (1974 to 14 November 2019);
EBSCO CINAHL Plus (Cumulative Index to Nursing and Allied Health Literature; 1937 to 14 November 2019).
The search strategies for the Cochrane Wounds Specialised Register, CENTRAL, Ovid MEDLINE, Ovid Embase and EBSCO CINAHL Plus can be found in Appendix 2. We combined the Ovid MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision) (Lefebvre 2019). We combined the Embase search with the Ovid Embase filter developed by the UK Cochrane Centre (Lefebvre 2019). We combined the CINAHL Plus search with the trial filter developed by Glanville 2019. There were no restrictions with respect to language, date of publication or study setting.
We also searched the following clinical trials registries:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov) (searched 20 November 2019);
World Health Organization (WHO) International Clinical Trials Registry Platform (https://www.who.int/clinical-trials-registry-platform) (searched 20 November 2019).
Search strategies for clinical trial registries can be found in Appendix 2.
Searching other resources
For previous versions of McInnes 2015, the review authors of McInnes 2015 contacted experts in the field of wound care to enquire about potentially relevant, ongoing and recently published studies. In addition, the review authors of McInnes 2015 contacted manufacturers of support surfaces for details of any studies manufacturers were conducting. This approach did not yield any additional studies; therefore, we did not repeat it for this review.
We identified other potentially eligible studies or ancillary publications by searching the reference lists of retrieved included studies, as well as relevant systematic reviews, meta‐analyses and health technology assessment reports.
When necessary, we contacted authors of key papers and abstracts to request further information about their trials.
We did not perform a separate search for adverse effects of interventions used. We considered adverse effects described in included studies only.
Data collection and analysis
We carried out data collection and analysis according to the methods stated in the published protocol (Shi 2020), which were based on the Cochrane Handbook for Systematic Reviews of Interventions (Li 2019). Changes from the protocol or previous published versions of the review are documented in Differences between protocol and review.
Selection of studies
One review author re‐checked the RCTs included in McInnes 2015 for eligibility (CS). Two review authors (CS and AJB, or JCD) independently assessed the titles and abstracts of the new search results for relevance using Rayyan (Ouzzani 2016) (Differences between protocol and review) and then independently inspected the full‐text of all potentially eligible studies. The two review authors (CS and AJB, or JCD) resolved disagreements through discussion and by involving a third review author if necessary.
Data extraction and management
One review author checked data from the studies included in McInnes 2015 and extracted additional data where necessary (CS). A second review author or researcher (SR, AJB, EM, Zhenmi Liu, Gill Norman, or Melanie Stephens) checked any new data extracted.
For new included studies, one review author (CS) independently extracted data and another review author or researcher (SR, AJB, EM, Zhenmi Liu, Gill Norman, or Melanie Stephens) checked all data (Differences between protocol and review). We resolved any disagreements through discussion and, if necessary, with the involvement of another review author. Where necessary, we contacted the authors of included studies to clarify data.
We extracted these data using a pre‐prepared data extraction form:
basic characteristics of studies (first author, publication type, publication year, and country);
funding sources;
care setting;
characteristics of participants (trial eligibility criteria, average age in each arm or in a study, proportions of participants by gender, and participants’ baseline skin status);
support surfaces being compared (including their descriptions);
details on any co‐interventions;
follow‐up duration;
the number of participants enrolled;
the number of participants randomised to each arm;
the number of participants analysed;
participant withdrawals with reasons;
the number of participants developing new ulcers (by ulcer stages where possible);
time to pressure ulceration outcome data;
patient support‐surface‐associated comfort;
adverse event outcome data;
health‐related quality of life outcome data; and
cost‐effectiveness outcome data.
We (CS and NC) classified specific support surfaces in the included studies into intervention groups using the NPIAP S3I terms and definitions related to support surface (NPIAP S3I 2007). Therefore, to accurately assign specific support surfaces to intervention groups, we extracted full descriptions of support surfaces from included studies, and when necessary, supplemented the information with that from external sources such as other publications about the same support surface, manufacturers’ or product websites, and expert clinical opinion (Shi 2018b). If we were unable to define or classify any of the specific support surfaces evaluated in an included study, we extracted available data and reported these as additional data outside the main review results.
Assessment of risk of bias in included studies
Two review authors or researchers (CS and SR, AJB, EM, Zhenmi Liu, Gill Norman, or Melanie Stephens) independently assessed the risk of bias of each included study using the Cochrane 'Risk of bias' tool (see Appendix 3). This tool has seven specific domains: sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete data (attrition bias), selective outcome reporting (reporting bias), and other issues (Higgins 2017). We assessed performance bias, detection bias, and attrition bias for each of the review outcomes separately (Higgins 2017). We noted that it is often impossible to blind participants and personnel in device trials. In this case, performance bias may be introduced if knowledge of treatment allocation results in deviations from intended interventions, differential use of co‐interventions or care between groups not specified in the study protocol that may influence outcomes. We attempted to understand if, and how, included studies compensated for challenges in blinding; for example, implementing strict protocols to maximise consistency of co‐interventions between groups to reduce the risk of performance bias. We also noted that pressure ulcer incidence is a subjective outcome. Compared with blinded assessment, non‐blinded assessment of subjective outcomes tends to be associated with more optimistic effect estimates of experimental interventions in RCTs (Hróbjartsson 2012). Therefore, we judged non‐blinded outcome assessment as being at high risk of detection bias. In this review, we included the issues of differential diagnostic activity and unit of analysis under the domain of 'other issues'. For example, unit of analysis issues occurred where a cluster‐randomised trial had been undertaken but analysed at the individual level in the study report.
For the studies included in McInnes 2015, one review author (CS) checked the 'Risk of bias' judgements and, where necessary, updated them. A second review author or researcher (SR, AJB, EM, Zhenmi Liu, Gill Norman, or Melanie Stephens) checked any updated judgement. We assigned each 'Risk of bias' domain a judgement of high, low, or unclear risk of bias. We resolved any discrepancy through discussion and by involving another review author where necessary. Where possible, useful and feasible, when a lack of reported information resulted in a judgement of unclear risk of bias, we planned to contact study authors for clarification.
We present our assessment of risk of bias for the proportion of participants developing a new pressure ulcer outcome using two 'Risk of bias' summary figures. One is a summary of bias for each item across all studies, and the second shows a cross‐tabulation of each study by all of the 'Risk of bias' items.
Once we had given our judgements for all 'Risk of bias' domains, we judged the overall risk of bias for each outcome across studies as:
low risk of bias, if we judged all domains to be at low risk of bias;
unclear risk of bias, if we judged one or more domains to be at unclear risk of bias and other domains were at low risk of bias but no domain was at high risk of bias; or
high risk of bias, as long as we judged one or more domains as being at high risk of bias, or all domains had unclear 'Risk of bias' judgements, as this could substantially reduce confidence in the result.
We resolved any discrepancy between review authors through discussion and by involving another review author where necessary.
For studies using cluster randomisation, we planned to consider the risk of bias in relation to recruitment bias, baseline imbalance, loss of clusters, incorrect analysis and comparability with individually randomised studies (Eldridge 2019; Higgins 2019; Appendix 3). However, we did not include any studies with a cluster design.
Measures of treatment effect
For meta‐analysis of pressure ulcer incidence data, we present the risk ratio (RR) with its 95% confidence interval (CI). For continuous outcome data, we present the mean difference (MD) with 95% CIs for studies that use the same assessment scale. If studies reporting continuous data used different assessment scales, we planned to report the standardised mean difference (SMD) with 95% CIs. However, this was not undertaken in the review.
For time‐to‐event data (time to pressure ulcer development), we present the hazard ratio (HR) with its 95% CI. If included studies reporting time‐to‐event data did not report an HR, then, when feasible, we estimated this using other reported outcomes, such as numbers of events, through employing available statistical methods (Parmar 1998; Tierney 2007).
Unit of analysis issues
We noted whether studies presented outcomes at the level of cluster (e.g. ward, research site) or at the level of participants. We also recorded whether the same participant was reported as having multiple pressure ulcers.
Unit of analysis issues may occur if studies randomise at the cluster level but the incidence of pressure ulcers is observed and data are presented and analysed at the level of participants (clustered data). We noted whether data regarding participants within a cluster were (incorrectly) treated as independent within a study, or were analysed using within‐cluster analysis methods. If clustered data were incorrectly analysed, we recorded this as part of the 'Risk of bias' assessment.
If a cluster‐RCT was not correctly analysed, where possible, we planned to use available information (see below) to adjust for clustering ourselves, in accordance with guidance in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019):
the number of clusters randomly assigned to each intervention; or the average (mean) number of participants per cluster;
outcome data ignoring the cluster design for the total number of participants; and
estimate of the intra‐cluster (or intra‐class) correlation coefficient (ICC).
However, we did not adjust for clustering for the two studies with an n‐of‐1 trial design because they did not report sufficient information to facilitate this.
Cross‐over trials
For cross‐over trials, we only considered outcome data at the first intervention phase (i.e. prior to cross‐over) as eligible.
Studies with multiple treatment groups
If a study had more than two eligible study arms, where appropriate, we combined results across these arms to make single pair‐wise comparisons (Higgins 2019).
Dealing with missing data
Data are commonly missing from study reports. Reasons for missing data could be the exclusion of participants after randomisation, withdrawal of participants from a study, or loss to follow‐up. The exclusion of these data from analysis may break the randomisation and potentially introduces bias.
Where there were missing data and where relevant we contacted study authors to pose specific queries about these data. In the absence of other information, for pressure ulcer incidence we assumed that participants with missing data did not develop new pressure ulcers for the main analysis (i.e. we added missing data to the denominator but not the numerator). We examined the impact of this assumption through undertaking a sensitivity analysis (see Sensitivity analysis).
Note that when a study did not specify the number of randomised participants prior to dropout, we used the available number of participants as the number randomised.
Assessment of heterogeneity
Assessing heterogeneity can be a complex, multifaceted process. Firstly, we considered clinical and methodological heterogeneity; that is, the extent to which the included studies varied in terms of participant, intervention, outcome and other characteristics including duration of follow‐up, clinical settings, and overall study‐level 'Risk of bias' judgement (Deeks 2019). In terms of the duration of follow‐up, in order to assess the relevant heterogeneity, we recorded and classed assessment of outcome measures from:
up to eight weeks as short‐term;
more than eight weeks to 16 weeks as medium‐term; and
more than 16 weeks as long‐term.
We supplemented this assessment of clinical and methodological heterogeneity with information regarding statistical heterogeneity, assessed using the Chi2 test. We considered a P value less than 0.10 to indicate statistically significant heterogeneity given that the Chi2 test has low power, particularly in the case where studies included in a meta‐analysis have small sample size. We carried out this statistical assessment in conjunction with the I2 statistic (Higgins 2003), and the use of prediction intervals for random‐effects meta‐analyses (Borenstein 2017; Riley 2011).
The I2 statistic is the percentage of total variation across studies due to heterogeneity rather than chance (Higgins 2003). Very broadly, we considered that I2 values of 25% or less may indicate a low level of heterogeneity and values of 75% or more may indicate very high heterogeneity (Higgins 2003). For random‐effects models, where the meta‐analysis had more than 10 included studies and no clear funnel plot asymmetry, we also planned to present 95% prediction intervals (Deeks 2019). We planned to calculate prediction intervals following methods proposed by Borenstein 2017.
Random‐effects analyses produce an average treatment effect, with 95% confidence intervals indicating where the true population average value is likely to lie. Prediction intervals quantify variation away from this average due to between‐study heterogeneity. The interval conveys where a future study treatment effect estimate is likely to fall based on the data analysed to date (Riley 2011). Prediction intervals are always wider than confidence intervals (Riley 2011).
It is important to note that prediction intervals will reflect heterogeneity of any source, including from methodological issues as well as clinical variation. For this reason, some authors have suggested that prediction intervals are best calculated for studies at low risk of bias, to ensure intervals that have meaningful clinical interpretation (Riley 2011). We had planned to calculate prediction intervals for all studies to assess heterogeneity and then to explore the impact of risk of bias in subgroup analysis as detailed below. However, we did not calculate any prediction intervals because all conducted meta‐analyses contained fewer than 10 studies.
Assessment of reporting biases
We followed the systematic framework recommended by Page 2019 to assess risk of bias due to missing results (non‐reporting bias) in the meta‐analysis of pressure ulcer incidence data. To make an overall judgement about risk of bias due to missing results, we:
identified whether pressure ulcer incidence data were unavailable by comparing the details of outcomes in trials registers, protocols or statistical analysis plans, if available, with reported results. If the above information sources were unavailable, we compared outcomes in the conference abstracts or in the methods section of the publication, or both, with the reported results. If we found non‐reporting of study results, we then judged whether the non‐reporting was associated with the nature of findings by using the 'Outcome Reporting Bias In Trials' (ORBIT) system (Kirkham 2018);
assessed the influence of definitely missing pressure ulcer incidence data on meta‐analysis; and
assessed the likelihood of bias where a study had been conducted but not reported in any form. For this assessment, we considered whether the literature search was comprehensive and planned to produce a funnel plot for meta‐analysis for seeking more evidence about the extent of missing results, provided there were at least 10 included studies (Peters 2008; Salanti 2014).
However, we did not produce a funnel plot for any meta‐analysis because all analyses in this review had fewer than 10 included studies.
Data synthesis
We summarised the included studies narratively and synthesised data using meta‐analysis where applicable. We structured comparisons according to type of comparator and then by outcomes ordered by follow‐up period.
We considered clinical and methodological heterogeneity and undertook pooling when studies appeared appropriately similar in terms of participants, support surfaces and outcome type. Where statistical synthesis of data from more than one study was not possible or considered inappropriate, we conducted a narrative review of eligible studies.
Once the decision to pool was made, we used a random‐effects model, which estimated an underlying average treatment effect from studies. Conducting meta‐analysis with a fixed‐effect model in the presence of even minor heterogeneity may provide overly narrow confidence intervals. We used the Chi2 test and I2 statistic to quantify heterogeneity but not to guide choice of model for meta‐analysis (Borenstein 2009). We exercised caution when meta‐analysed data were at risk of small study effects because use of a random‐effects model may be unsuitable here. In this case, or where there were other reasons to question the choice of a fixed‐effect or random‐effects model, we assessed the impact of the approach using sensitivity analyses to compare results from alternate models (Thompson 1999).
We performed meta‐analyses largely using Review Manager 5.4 (Review Manager 2020). We presented data using forest plots where possible. For dichotomous outcomes, we presented the summary estimate as an RR with 95% CI. Where continuous outcomes were measured, we presented an MD with 95% CI. We planned to report SMD estimates where studies measured the same outcome using different methods. For time‐to‐event data, we presented the summary estimates as HRs and 95% CIs.
Subgroup analysis and investigation of heterogeneity
Investigation of heterogeneity
When important heterogeneity occurred, we planned to follow these steps, proposed by Cipriani 2013, to investigate further:
check the data extraction and data entry for errors and possible outlying studies;
if outliers existed, perform sensitivity analysis by removing them; and
if heterogeneity was still present, we planned to perform subgroup analyses for study‐level characteristics (see below) in order to explain heterogeneity as far as possible. However, we did not undertake any subgroup analysis because meta‐analyses in this review included fewer than 10 studies.
Subgroup analysis
We investigated heterogeneity using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2019). We planned to perform subgroup analyses for binary and categorical factors (or meta‐regression for continuous factors) to determine whether the size of treatment effects was influenced by these four study‐level characteristics:
risk of bias (binary: low or unclear risk of bias; and high risk of bias; Schulz 1995);
settings (categorical: acute care and other hospital settings; long‐term care settings; operating theatre setting; and intensive care unit);
baseline skin status (categorical: participants at risk, mixed skin status or non‐reporting; non‐blanchable erythema; existing ulcers of Stage 2 or serious; Shi 2018c); and
follow‐up duration (continuous).
We did not perform subgroup analysis/meta‐regression when the number of studies included in the meta‐analysis was not reasonable (i.e. fewer than 10).
We planned to compare subgroup findings using the 'Test for Subgroup Differences’ in Review Manager 5.4 (Review Manager 2020).
Sensitivity analysis
We assessed the robustness of meta‐analysis of pressure ulcer incidence data through doing sensitivity analyses as follows.
Impact of considering specific alternating pressure (active) air surfaces as different surfaces rather than as a general group. We undertook a sensitivity analysis to examine whether disentangling specific alternating pressure (active) air surfaces that were listed in Types of interventions from alternating pressure (active) air surface as a single intervention affected the meta‐analysis results.
Impact of the selection of pressure ulcer incidence outcome measure. The proportion of participants developing a new pressure ulcer was the primary outcome measure for this review but we also analysed time to pressure ulcer development, where data were available.
Impact of missing data. The primary analysis assumed that participants with missing data did not develop new pressure ulcers. We also analysed pressure ulcer incidence by only including data for the participants for whom we had endpoint data (complete cases). We noted that when a study only had complete case data (i.e. missing data or the numbers of participants randomised were not reported), complete case data were considered in the related main analysis (Differences between protocol and review).
Impact of altering the effects model used. We used a random‐effects model for the main analysis, followed by a fixed‐effect analysis.
Summary of findings and assessment of the certainty of the evidence
We presented the main, pooled results of the review in 'Summary of findings' tables. These tables present key information concerning the certainty of evidence, the magnitude of the effects of the interventions examined and the sum of available data for the main outcomes (Schünemann 2019). These tables also include an overall grading of the certainty of the evidence associated with each of the main outcomes that we assessed using the GRADE approach via GRADEpro GDT software. The GRADE approach defines the certainty of a body of evidence as the extent to which one can be confident that an estimate of effect or association is close to the true quantity of specific interest.
The GRADE assessment involves consideration of five factors: within‐trial risk of bias, directness of evidence, heterogeneity, precision of effect estimates, and risk of publication bias (Schünemann 2019). The certainty of evidence can be assessed as being: high, moderate, low or very low. RCT evidence has the potential to be high certainty. We did not downgrade the certainty of evidence for the risk of bias factor in a specific circumstance. That is if the blinding of participants and personnel was the only domain resulting in our judgement of overall high risk of bias for the included studies; however for these studies it was impossible to blind participants and personnel.
When downgrading for imprecision, we followed the methods described in Guyatt 2011: either considering both the optimal information size (OIS) and the 95% CI of each meta‐analysis if they were estimable; or considering the sample size, the number of events and other effectiveness indicators if the calculation of OIS and undertaking a meta‐analysis were not applicable. Where necessary, we used the GRADE 'default' minimum important difference values (RR = 1.25 and 0.75) as the thresholds to judge if a 95% CI was wide (imprecise) so as to include the possibility of clinically important harm and benefit (Guyatt 2011).
We presented a separate 'Summary of findings' table for all but one comparison evaluated in this review. The exception was the comparison of alternating pressure (active) air surfaces versus another type of alternating pressure (active) air surfaces; see Differences between protocol and review. We presented these outcomes in the 'Summary of findings' tables:
proportion of participants developing a new pressure ulcer;
time to pressure ulcer development;
support‐surface‐associated patient comfort;
all reported adverse events;
health‐related quality of life; and
cost‐effectiveness.
We prioritised the time points and method of outcome measurement specified in Types of outcome measures for presentation in ‘Summary of findings’ tables’. Where we did not pool data for some outcomes within a comparison, we conducted a GRADE assessment for each of these outcomes and presented these assessments in a narrative format in 'Summary of findings' tables (Differences between protocol and review).
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; and Characteristics of ongoing studies.
Results of the search
The electronic searches identified 1624 records, including 1164 from electronic databases and 460 from trial registries. We excluded 218 duplicate records and screened 1406 records, of which 233 were identified as potentially eligible and obtained as full‐text. Following full‐text screening, we considered 54 records of 31 studies eligible for inclusion in this review (Andersen 1982; Aronovitch 1999; Ballard 1997; Beeckman 2019; Bliss 1967; Bliss 1995; Cavicchioli 2007; Conine 1990; Daechsel 1985; Demarre 2012; Finnegan 2008; Gray 2008; Grindley 1996; Hampton 1997; Jiang 2014; Laurent 1998; Malbrain 2010; Nixon 2006; Nixon 2019; Phillips 1999; Price 1999; Pring 1998; Rosenthal 2003; Russell 2000; Sanada 2003; Sauvage 2017; Sideranko 1992; Stapleton 1986; Taylor 1999; Theaker 2005; Whitney 1984).
From other resources, we identified Rafter 2011 by scanning the reference lists of the 14 systematic reviews or meta‐analyses that were identified via the electronic searches (Chou 2013; Huang 2013; McGinnis 2011; McInnes 2015; McInnes 2018; Mistiaen 2010; De Oliveira 2017; Rae 2018; Reddy 2006; Reddy 2008; Serraes 2018; Shi 2018a; Smith 2013; Yao 2018), as well as the clinical practice guidelines listed in Searching other resources.
In total, we included 32 studies in the review, of which one was a conference abstract (Laurent 1998). See Figure 1.
1.
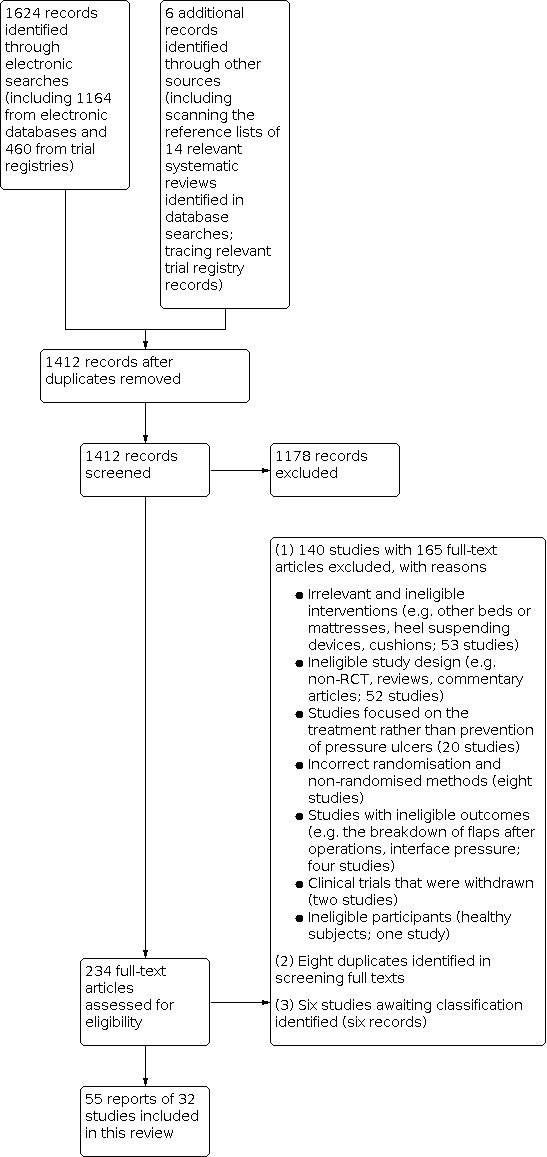
Study flow diagram
Included studies
Types of studies
Of the 32 included RCTs, 26 had a parallel group design: four studies with three arms and 22 with two arms. Six studies had particular design features:
two studies applied cross‐over design (Ballard 1997; Grindley 1996);
one study had a 2 × 2 factorial design (Laurent 1998), containing the comparison of alternating pressure (active) air surfaces versus standard hospital surfaces in an intensive care unit (ICU);
one study appeared to be a multi‐arm, multi‐stage trial design with eight arms, of which seven were randomised and eligible for this review (Bliss 1995);
two studies used a series of n‐of‐1 trial design (i.e. a randomised controlled crossover trial in a single participant) (Phillips 1999; Pring 1998).
Of the 32 included studies, 10 were conducted at more than one research site (Ballard 1997; Beeckman 2019; Cavicchioli 2007; Demarre 2012; Gray 2008; Jiang 2014; Nixon 2006; Nixon 2019; Rosenthal 2003; Sauvage 2017). Except for Jiang 2014 in China and Sanada 2003 in Japan, all of the included studies were conducted in high‐income and upper‐middle‐income economies in Europe and North America, including Belgium, Canada, Denmark, France, Italy, the UK and the USA.
Of the 30 studies that clearly stated duration of follow‐up, the median was 14 days (range: 3 to 180 days).
Types of participants
Age and sex at baseline
Of the 32 studies, 31 enrolled a total of 9058 participants (median study sample size: 83 participants, or the number of individual trials comprising a series of n‐of‐1 trials; range: 10 to 2029) whilst one (Hampton 1997) did not specify the number of participants. The average participant age was specified for 29 studies and ranged between 37.2 and 87.0 years (median: 69.1 years). The sex of the participants was specified for 26 studies; within these, 3654 (44.4%) of participants were male and 4571 (55.6%) were female.
Skin status at baseline
Of the 32 studies, 27 (8620 participants) recruited people at risk of having a new ulcer with risk assessed largely using the Waterlow, Norton or Braden scales. In 18 of these studies, 3812 (44.2%) participants were free of pressure ulcers at baseline; in nine studies, 4808 (55.8%) participants with superficial ulcers were enrolled (Bliss 1967; Bliss 1995; Cavicchioli 2007; Grindley 1996; Malbrain 2010; Nixon 2006; Nixon 2019; Rafter 2011; Whitney 1984). Two studies did not specify the skin status at baseline (Hampton 1997; Laurent 1998); one study stated that their participants had no risk of developing a pressure ulcer (Ballard 1997); and two studies recruited people with severe full‐thickness pressure ulcers alone (Finnegan 2008; Rosenthal 2003).
Care settings
Participants were from a variety of settings, including:
a mixture of secondary and community in‐patient facilities (Nixon 2019),
acute care settings (including accident and emergency departments, and hospitals in general) (Andersen 1982; Aronovitch 1999; Bliss 1967; Bliss 1995; Cavicchioli 2007; Demarre 2012; Finnegan 2008; Gray 2008; Hampton 1997; Jiang 2014; Laurent 1998; Nixon 2006; Price 1999; Rafter 2011; Russell 2000; Sanada 2003; Stapleton 1986; Taylor 1999; Whitney 1984),
intensive care units (Malbrain 2010; Sideranko 1992; Theaker 2005), and
community and long‐term care settings (including hospice, community, nursing homes, extended care facilities, rehabilitation wards, long‐term facilities and geriatric units) (Ballard 1997; Beeckman 2019; Conine 1990; Daechsel 1985; Grindley 1996; Phillips 1999; Pring 1998; Rosenthal 2003; Sauvage 2017).
Types of interventions
The studies investigated a wide range of alternating pressure (active) air surfaces with alternating pressure cycle periods ranging from 7.5 to 30 minutes. Of these studies, Sanada 2003 included two types of alternating pressure (active) air surfaces. Hybrid systems with alternating pressure (active) and continuously static (reactive) capabilities were used in five studies (Gray 2008; Hampton 1997; Rafter 2011; Taylor 1999; Theaker 2005). Alternating pressure (active) air surfaces with low air loss features were used in two studies (Rosenthal 2003; Theaker 2005). Three studies (Andersen 1982; Conine 1990; Daechsel 1985) did not specify the type (or cycle time) of the alternating pressure (active) air surfaces they used.
Full details of alternating pressure (active) air surfaces and comparators are listed in Appendix 4 and in results below. Four studies used comparator group surfaces defined by study authors as 'standard hospital surfaces' that could not be classified further using the NPIAP S3I support surface terms and definitions (Andersen 1982; Bliss 1967; Laurent 1998; Sanada 2003). Of these four studies, Sanada 2003 reported use of a 'standard hospital surface' made of polyester (Paracare®) whilst the remaining three studies did not specify the type of surface they referred to as standard hospital surfaces.
Twelve studies specified co‐interventions they applied (e.g. repositioning, cushions) (Beeckman 2019; Bliss 1967; Conine 1990; Daechsel 1985; Finnegan 2008; Gray 2008; Jiang 2014; Malbrain 2010; Price 1999; Rosenthal 2003; Sanada 2003; Whitney 1984). All twelve stated or indicated that the same co‐interventions were applied in all study groups.
Funding sources
Of the 32 included studies, 18 specified the details of funding sources. Eleven studies were completely or partly funded by industry or received mattresses under evaluation from industries (Aronovitch 1999; Ballard 1997; Beeckman 2019; Bliss 1995; Daechsel 1985; Finnegan 2008; Grindley 1996; Price 1999; Rafter 2011; Russell 2000; Theaker 2005), and seven studies were supported by public funding (Bliss 1967; Conine 1990; Demarre 2012; Jiang 2014; Nixon 2006; Nixon 2019; Stapleton 1986).
Excluded studies
We excluded 140 studies (with 165 records). The main reasons for these 140 exclusions were: irrelevant and ineligible interventions (53 studies); ineligible study design (e.g. non‐RCT, reviews, commentary articles; 52 studies); studies focused on the treatment rather than prevention of pressure ulcers (20 studies); incorrect randomisation and non‐randomised methods (eight studies); studies with ineligible outcomes (four studies); clinical trials that were withdrawn (two studies; NCT02634892; NCT02735135); and ineligible participants (healthy subjects; one study). We also identified eight duplicates in screening full texts (see Figure 1).
Ongoing studies
We did not identify any ongoing studies.
Studies awaiting classification
There were six studies (six records) about which we could not make eligibility decisions. We were unable to determine whether Gardner 2008 measured one or more outcomes relevant to this review. We could not obtain the full‐text of five studies (in part due to more limited access to intra‐library loans during the COVID‐19 period) despite extensive efforts made (Chaloner 2000; Henn 2004; Knight 1999; Mastrangelo 2010b; Melland 1998).
Risk of bias in included studies
We summarise 'Risk of bias' assessments for the primary outcome of this review in Figure 2 and Figure 3.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
We judged seven of the 32 studies as having an unclear overall risk of bias for the primary outcome (Gray 2008; Grindley 1996; Jiang 2014; Malbrain 2010; Rosenthal 2003; Sideranko 1992; Taylor 1999). We judged all the remaining 25 studies as having findings at a high overall risk of bias, of which two had an unclear risk of bias judgements for all domains (Hampton 1997; Stapleton 1986) and 23 had one or more domains with a high risk of bias judgement (Andersen 1982; Aronovitch 1999; Ballard 1997; Beeckman 2019; Bliss 1967; Bliss 1995; Cavicchioli 2007; Conine 1990; Daechsel 1985; Demarre 2012; Finnegan 2008; Laurent 1998; Nixon 2006; Nixon 2019; Phillips 1999; Price 1999; Pring 1998; Rafter 2011; Russell 2000; Sanada 2003; Sauvage 2017; Theaker 2005; Whitney 1984). Of these 23 studies, 15 had a high risk of bias judgement for the primary outcome in domains of blinding of participants and personnel, blinding of outcome assessment, or both (Andersen 1982; Beeckman 2019; Daechsel 1985; Demarre 2012; Finnegan 2008; Laurent 1998; Nixon 2006; Nixon 2019; Price 1999; Pring 1998; Rafter 2011; Russell 2000; Sauvage 2017; Theaker 2005; Whitney 1984).
Publication bias
We ran a comprehensive search and were able to locate one eligible study, Rafter 2011, from other resources and one conference abstract, Laurent 1998. We considered the risk of having missed published reports to be low. We were unable to assess for the risk of non‐publication of studies with negative findings as we could not present funnel plots given the small number of included studies in each analysis.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
Summary of findings 1. Alternating pressure (active) air surfaces compared with foam surfaces for pressure ulcer prevention.
| Alternating pressure (active) air surfaces compared with foam surfaces for pressure ulcer prevention | ||||||
| Patient or population: pressure ulcer prevention Setting: any care setting Intervention: alternating pressure (active) air surfaces Comparison: foam surfaces | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with foam surfaces | Risk with alternating pressure (active) air surfaces | |||||
| Proportion of participants developing a new pressure ulcer Follow‐up: median 90 days | Study population | RR 0.63 (0.34 to 1.17) | 2247 (4 RCTs) | ⊕⊕⊝⊝ Lowa,b | Alternating pressure (active) air surfaces may reduce the proportion of participants developing a new pressure ulcer compared with foam surfaces. | |
| 104 per 1,000 | 66 per 1,000 (35 to 122) | |||||
| Time to pressure ulcer development Follow‐up: median 60 days | Study population | HR 0.41 (0.10 to 1.64) | 2105 (2 RCTs) | ⊕⊝⊝⊝ Very lowb,c,d | It is uncertain if there is any difference in the risk of developing a new pressure ulcer at any time point up to 90 days when alternating pressure (active) air surfaces are compared with foam surfaces. | |
| 98 per 1,000 | 41 per 1,000 (10 to 156) | |||||
| Support surface‐associated patient comfort Follow‐up: 30 days | Sauvage 2017 presented data for the questionnaire's subscales as numbers and percentages, and reported no significant difference in the overall satisfaction between study groups (P = 0.21). | ‐ | 76 (1 RCT) | ⊕⊝⊝⊝ Very lowe,f | It is uncertain if there is any difference in support surface‐associated patient comfort between alternating pressure (active) air surfaces and foam surfaces. | |
| All reported adverse events Follow‐up: range 30 days to 6 months | Nixon 2019 and Sauvage 2017 reported similar rates of adverse events between their study arms. Rosenthal 2003 reported 1 death but did not specify which study group the death was associated with. | ‐ | 2181 (3 RCTs) | ⊕⊝⊝⊝ Very lowg,h | It is uncertain if there is any difference in all reported adverse events between alternating pressure (active) air surfaces and foam surfaces. | |
| Health‐related quality of life (90‐day EQ‐5D‐5L, expressed as utility values ranging from −1 to 1 with 1 representing perfect health, 0 representing death, and −1 representing worse than death) Follow‐up: 90 days | The mean health‐related quality of life (90‐day EQ‐5D‐5L) was 0.52. | MD 0.00 (0.05 lower to 0.05 higher) | ‐ | 267 (1 RCT) | ⊕⊕⊝⊝ Lowi | It is unclear if there is a difference in health‐related quality of life measured using EQ‐5D‐5L at 90‐day follow‐up between alternating pressure (active) air surfaces and foam surfaces. |
| Health‐related quality of life (90‐day PU‐QoL‐UI, expressed as utility values ranging from −1 to 1 with 1 representing perfect health, 0 representing death, and −1 representing worse than death) Follow‐up: 90 days | The mean health‐related quality of life (90‐day PU‐QoL‐UI) was 0.60. | MD 0.00 (0.03 lower to 0.03 higher) | ‐ | 233 (1 RCT) | ⊕⊕⊝⊝ Lowi | It is unclear if there is a difference in health‐related quality of life measured using the PU‐QoL‐UI at 90‐day follow‐up between alternating pressure (active) air surfaces and foam surfaces. |
| Cost‐effectiveness Follow‐up: 90 days | Incremental cost‐effectiveness ratio (ICER) = GBP –101699 and Net Monetary Benefit (NMB) = GBP –2114 in the probabilistic analysis, meaning alternating pressure (active) air surfaces has lower costs and higher quality‐adjusted life‐year (QALY) values. Alternating pressure (active) air surfaces had a 99% probability of being cost‐effective at a threshold of GBP 20,000 and alternating pressure (active) air surfaces dominated reactive foam surfaces. | ‐ | 1 RCT | ⊕⊕⊕⊝ Moderatej | Alternating pressure (active) air surfaces are probably cost‐effective compared with reactive foam surfaces. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; HR: hazard ratio; MD: mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded once for risk of bias (2 studies with about 50% of weight in the analysis had either 1 domain other than performance bias at high risk of bias or all domains at unclear risk of bias; 2 studies with about 50% of weight in the analysis had domains other than performance bias at unclear risk of bias). bDowngraded once for moderate imprecision because, even though the optimal information size (OIS) was met, the wide confidence interval crossed RR = 0.75. cDowngraded once for high risk of bias in 1 study with 40% of analysis weight but low risk of bias in domains other than performance bias in another study. dDowngraded twice for substantial inconsistency (I2 = 86%; Chi2 test P = 0.009; point estimates and confidence intervals largely vary between studies). eDowngraded twice for high risk of detection bias. fDowngraded once for imprecision due to small sample size. gDowngraded once for unclear risk of bias in 2 studies with about half weight. hDowngraded twice for substantial inconsistency. iDowngraded twice for substantial imprecision due to small sample size. jDowngraded once for imprecision for the EQ‐5D‐5L outcome of the relevant study.
Summary of findings 2. Alternating pressure (active) air surfaces compared with reactive air surfaces for pressure ulcer prevention.
| Alternating pressure (active) air surfaces compared with reactive air surfaces for pressure ulcer prevention | ||||||
| Patient or population: pressure ulcer prevention Setting: any care setting Intervention: alternating pressure (active) air surfaces Comparison: reactive air surfaces | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with reactive air surfaces | Risk with alternating pressure (active) air surfaces | |||||
| Proportion of participants developing a new pressure ulcer Follow‐up: median 14 days | Study population | RR 1.61 (0.90 to 2.88) | 1648 (6 RCTs) | ⊕⊝⊝⊝ Very lowa,b | It is uncertain if the proportion of people developing a new pressure ulcer is decreased or increased when alternating pressure (active) air surfaces are compared with reactive air surfaces. | |
| 22 per 1,000 | 36 per 1,000 (20 to 64) | |||||
| Time to pressure ulcer development Follow‐up: 14 days | Study population | HR 2.25 (1.05 to 4.83) | 308 (1 RCT) | ⊕⊕⊝⊝ Lowc | People treated with alternating pressure (active) air surfaces may have a higher risk of developing an incident pressure ulcer than those treated with reactive air surfaces at any time within 14 days. | |
| 52 per 1,000 | 113 per 1,000 (54 to 227) | |||||
| Support surface‐associated patient comfort Follow‐up: median 11 days | Three studies appeared to report equivalent comfort between their study arms (Cavicchioli 2007; Jiang 2014; Price 1999) whilst Finnegan 2008 seemed to suggest that the use of alternating pressure (active) air surfaces was associated with better comfort than reactive air surfaces. | ‐ | 1364 (4 RCTs) | ⊕⊝⊝⊝ Very lowd,e | It is uncertain if there is any difference in support surface‐associated patient comfort between alternating pressure (active) air surfaces and reactive air surfaces. | |
| All reported adverse events | Included studies did not report this outcome. | |||||
| Health‐related quality of life | Included studies did not report this outcome. | |||||
| Cost effectiveness | Included studies did not report this outcome. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; HR: hazard ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded twice for high risk of bias in domains other than performance bias in 3 studies with more than 54% analysis weight. bDowngraded once for moderate imprecision as, despite the fact that the OIS was met, the wide confidence interval crossed RR = 1.25. cDowngraded twice for high risk of detection bias. dDowngraded once for high overall risk of bias in 3 small studies but unclear risk of bias in 1 large study. eDowngraded twice for substantial inconsistency due to the large variation of outcome measurement methods and findings.
Summary of findings 3. Alternating pressure (active) air surfaces compared with reactive water‐filled surfaces for pressure ulcer prevention.
| Alternating pressure (active) air surfaces compared with reactive water‐filled surfaces for pressure ulcer prevention | ||||||
| Patient or population: pressure ulcer prevention Setting: any care setting Intervention: alternating pressure (active) air surfaces Comparison: reactive water‐filled surfaces | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with reactive water‐filled surfaces | Risk with alternating pressure (active) air surfaces | |||||
| Proportion of participants developing a new pressure ulcer Follow‐up: median 10 days | Study population | RR 1.21 (0.52 to 2.83) | 358 (2 RCTs) | ⊕⊝⊝⊝ Very lowa,b | It is uncertain if the proportion of people developing a new pressure ulcer is decreased or increased when alternating pressure (active) air surfaces are compared with reactive water surfaces. | |
| 52 per 1,000 | 63 per 1,000 (27 to 148) | |||||
| Time to pressure ulcer development | Included studies did not report this outcome. | |||||
| Support surface‐associated patient comfort | Included studies did not report this outcome. | |||||
| All reported adverse events | Included studies did not report this outcome. | |||||
| Health‐related quality of life | Included studies did not report this outcome. | |||||
| Cost effectiveness | Included studies did not report this outcome. | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded twice for high risk of detection bias in 1 study with more than 60% analysis weight and unclear overall risk of bias in another study. bDowngraded twice for substantial imprecision as the OIS was not met and the confidence interval was very wide and crossed RRs = 0.75 and 1.25.
Summary of findings 4. Alternating pressure (active) air surfaces compared with reactive fibre surfaces for pressure ulcer prevention.
| Alternating pressure (active) air surfaces compared with reactive fibre surfaces for pressure ulcer prevention | ||||||
| Patient or population: pressure ulcer prevention Setting: acute care setting Intervention: alternating pressure (active) air surfaces Comparison: reactive fibre surfaces | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with reactive fibre surfaces | Risk with alternating pressure (active) air surfaces | |||||
| Proportion of participants developing a new pressure ulcer Follow‐up: range 17.7 days to 3 months. | Study population | RR 0.90 (0.68 to 1.19) | 285 (3 RCTs) | ⊕⊝⊝⊝ Very lowa,b | It is uncertain if the proportion of people developing a new pressure ulcer is decreased or increased when alternating pressure (active) air surfaces are compared with reactive fibre surfaces. | |
| 424 per 1,000 | 381 per 1,000 (288 to 504) | |||||
| Time to pressure ulcer development | Included studies did not report this outcome. | |||||
| Support surface‐associated patient comfort Follow‐up: 3 months. |
19 dropouts among 93 people using alternating pressure (active) air surfaces; and 17 of 94 using reactive fibre surfaces with discomfort as the reason given. | ‐ | 187 (1 RCT) | ⊕⊝⊝⊝ Very lowb,c,d | It is uncertain if there is any difference in support surface‐associated patient comfort between alternating pressure (active) air surfaces and reactive fibre surfaces. | |
| All reported adverse events | Included studies did not report this outcome. | |||||
| Health‐related quality of life | Included studies did not report this outcome. | |||||
| Cost effectiveness | Included studies did not report this outcome. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded twice for high risk of bias in domains other than performance bias in 2 studies with more than 80% of analysis weight. bDowngraded once for imprecision as the OIS was not met. cDowngraded once for indirectness as the outcome measured (i.e. dropouts due to discomfort) was not directly relevant to comfort. dDowngraded once for high overall risk of bias.
Summary of findings 5. Alternating pressure (active) air surfaces on operating tables and subsequently on ward beds compared with reactive gel surfaces on operating tables followed by foam surfaces on ward beds for pressure ulcer prevention.
| Alternating pressure (active) air surfaces on operating tables and subsequently on ward beds compared with reactive gel surfaces on operating tables followed by foam surfaces on ward beds for pressure ulcer prevention | ||||||
| Patient or population: pressure ulcer prevention Setting: operating room Intervention: alternating pressure (active) air surfaces on operating tables and subsequently on ward beds Comparison: reactive gel surfaces on operating tables followed by foam surfaces on ward beds | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with reactive gel surfaces used on operating tables followed by foam surfaces applied on hospital beds | Risk with alternating pressure (active) air surfaces | |||||
| Proportion of participants developing a new pressure ulcer Follow‐up: 7 days | Study population | RR 0.22 (0.06 to 0.76) | 415 (2 RCTs) | ⊕⊕⊝⊝ Lowa,b | Alternating pressure (active) air surfaces applied on both operating tables and hospital beds may reduce the proportion of people developing a new pressure ulcer compared with reactive gel surfaces used on operating tables followed by foam surfaces applied on hospital beds. | |
| 68 per 1,000 | 15 per 1,000 (4 to 52) | |||||
| Time to pressure ulcer development | Included studies did not report this outcome. | |||||
| Support surface‐associated patient comfort | Included studies did not report this outcome. | |||||
| All reported adverse events Follow‐up: 7 days | Approximately 1/2 of the participants in each group reported adverse events. No difference in adverse events between groups was reported. None of the adverse events were related to the mattresses assigned. | ‐ | 198 (1 RCT) | ⊕⊝⊝⊝ Very lowc,d | It is uncertain if there is any difference in all reported adverse events between alternating pressure (active) air surfaces applied on both operating tables and hospital beds and reactive gel surfaces used on operating tables followed by foam surfaces applied on hospital beds. | |
| Health‐related quality of life | Included studies did not report this outcome. | |||||
| Cost effectiveness | Included studies did not report this outcome. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded once for risk of bias (1 study with 36% of analysis weight was at high risk of attrition bias whilst the other study was at unclear risk of bias for more than 1 domain other than performance bias). bDowngraded once for imprecision as, despite the fact that the OIS was met, the 95% CI crossed RR = 0.75. cDowngraded once for unclear risk of bias in more than 1 domain other than performance bias. dDowngraded twice for imprecision due to small sample size.
See Table 1; Table 2; Table 3; Table 4; Table 5.
Unless otherwise stated, random‐effects analysis was used throughout. Each pooled result presented is an average effect, rather than a common effect and should be interpreted as such.
We have not reported data from the four studies with comparator group surfaces that we could not classify in the main body of the results (Andersen 1982; Bliss 1967; Laurent 1998; Sanada 2003). For completeness, we summarise the results of these studies in Appendix 5.
We performed data analyses for the following comparisons and outcomes. Where applicable, we performed pre‐specified sensitivity analyses as noted in Sensitivity analysis.
Comparison 1: Alternating pressure (active) air surfaces versus foam surfaces (six studies, 2427 participants)
One study, Bliss 1995, randomised participants to three types of foam mattresses (in three individual trial arms) which we combined into a single study arm for analysis against the relevant comparison, which was a type of alternating pressure (active) air surface. However, this study and Whitney 1984 (in total 180 participants) reported no outcomes directly relevant to this review and so none of their data were analysable. Rosenthal 2003 evaluated an alternating pressure (active) air surface with a low‐air‐loss feature. The remaining studies compared a standard alternating pressure (active) air surface with a foam surface comparison.
Primary outcomes
Proportion of participants developing a new pressure ulcer (median follow‐up duration 90 days, minimum 30 days, maximum 6 months or unspecified)
Four studies (2247 participants) reported data for this outcome and the data from these studies were pooled (Nixon 2019; Rosenthal 2003; Sauvage 2017; Stapleton 1986). Alternating pressure (active) air surfaces (83/1125 (7.4%)) may reduce the proportion of participants developing pressure ulcers compared with foam surfaces (117/1122 (10.4%)); however, this is low‐certainty evidence. The RR was 0.63 (95% CI 0.34 to 1.17; I2 = 63%; Analysis 1.1). Evidence certainty was downgraded once for risk of bias (two studies contributing 50% weight in the meta‐analysis had either one domain other than performance bias at high risk of bias, or all domains at unclear risk of bias; two studies contributing 50% of weight in the meta‐analysis had domains other than performance bias at low or unclear risk of bias), and once for imprecision as, despite the fact that the optimal information size (OIS) was met, the wide confidence interval crossed RR = 0.75.
1.1. Analysis.

Comparison 1: Alternating pressure (active) air surfaces compared with reactive foam surfaces, Outcome 1: Proportion of participants developing a new pressure ulcer
Subgroup analysis
We considered the studies included in Analysis 1.1 heterogeneous in terms of all pre‐specified subgroup factors (overall 'risk of bias', care settings, skin status at baseline, and follow‐up) and there was some indication of statistical heterogeneity (Chi2 test P value = 0.07; Tau2 = 0.18; I2 = 63%). We noticed that, of the four studies, Sauvage 2017 reported a greater treatment effect than the other three. Once the extreme value was removed (Sauvage 2017), I2 went from 63% to 0%, but the overall estimate remained consistent with the main analysis (RR 0.79, 95% CI 0.60 to 1.03; Chi2 test P value = 0.83; Tau2 = 0.00; I2 = 0%). Of the four studies, Sauvage 2017 differed from the others in terms of care settings: Sauvage 2017 was conducted at long‐term care settings whilst the others were at acute care settings. However, as noted in Subgroup analysis and investigation of heterogeneity, because there were fewer than 10 studies, we did not undertake a subgroup analysis.
Sensitivity analyses
We performed sensitivity analyses for the following factors but did not use complete case data for a sensitivity analysis because the four included studies did not report missing data.
Sensitivity analysis deconstructing different types of alternating pressure (active) air surfaces into single groups . Splitting the class of alternating pressure (active) air surfaces resulted in two independent analyses: (1) alternating pressure (active) air surfaces compared with foam surfaces (Nixon 2019; Sauvage 2017; Stapleton 1986); and (2) alternating pressure (active) low‐air‐loss surfaces compared with foam surfaces (Rosenthal 2003). There were insufficient data to show whether results were consistent across these subgroups.
Sensitivity analysis with fixed‐effect (rather than random‐effects) model . The use of a fixed‐effect model resulted in a RR of 0.71 (95% CI 0.55 to 0.93; I2 = 63%). The results suggest that the effect size of our outcome of interest is sensitive to the type of effect model chosen.
Post hoc sensitivity analysis using pressure ulcer incidence data fromNixon 2019only . In Analysis 1.1, Nixon 2019 was the largest study (with data for 2029 participants) and was the only study having all domains other than performance bias at low risk of bias for this outcome. Using pressure ulcer incidence data from Nixon 2019 made little difference to the pooled effect estimate (RR 0.78, 95% CI 0.57 to 1.05; I2 = 0%).
Sensitivity analysis with time to pressure ulcer development as pressure ulcer incidence measure (medianfollow‐up duration 60 days, minimum 30 days, maximum 90 days) . Two studies (2105 participants) reported this outcome measure (Nixon 2019; Sauvage 2017), and the data from these were pooled. Analysis 1.2 resulted in a HR of 0.41 (95% CI 0.10 to 1.64; I2 = 86%) which was consistent with the main analysis. It is uncertain whether there is a difference in the risk of developing a new pressure ulcer, over 60 days' follow‐up, between alternating pressure (active) air surfaces and foam surfaces. Evidence is of very low certainty, downgraded once for high risk of bias in one study with 40% of analysis weight, twice for substantial inconsistency, and once for imprecision.
1.2. Analysis.

Comparison 1: Alternating pressure (active) air surfaces compared with reactive foam surfaces, Outcome 2: Time to pressure ulcer development
Secondary outcomes
Support‐surface‐associated patient comfort (follow‐up duration 30 days)
Only Sauvage 2017 (76 participants) reported this outcome, defined by the study authors as the perception of patient comfort and measured using a satisfaction questionnaire. Sauvage 2017 reported no significant difference in the overall satisfaction between study groups (P = 0.21); no other information was reported. We are uncertain whether there is any difference between alternating pressure (active) air surfaces and foam surfaces in patient comfort responses. Evidence is of very low certainty, downgraded twice for high risk of detection bias, and once for imprecision.
All reported adverse events (median follow‐up duration 90 days, minimum 30 days, maximum 6 months)
Three studies (2181 participants) reported this outcome (Nixon 2019; Rosenthal 2003; Sauvage 2017). We did not pool these data as the definitions of adverse events varied between studies (Table 6). It is uncertain if there is any difference in adverse events between alternating pressure (active) air surfaces and foam surfaces. Evidence is of very low certainty, downgraded once for unclear risk of bias in two studies with about half weight, and twice for inconsistency.
1. All reported adverse events.
| Study ID | Alternating pressure (active) air surfaces | Foam surfaces | Comment |
| Nixon 2019 | Related and unexpected serious adverse events: 0 Expected adverse events/ serious adverse events: 163/1017 The proportion of deaths: 82/1017, 8.1% Re‐admission rates: 82/1017, 8.1% Fall rates: 152/1017, 14.9% |
Related and unexpected serious adverse events: 0 Expected adverse events/ serious adverse events: 167/1013 The proportion of deaths: 84/1013, 8.3% Re‐admission rates: 62/1013, 6.1% Fall rates: 159/1013, 15.7% |
Similar between groups |
| Rosenthal 2003 | See comment | See comment | One death; but the authors did not specify which group the death was in. |
| Sauvage 2017 |
|
|
Events other than discomfort and hyperalgesia did not involve the mattresses. |
Health‐related quality of life (follow‐up duration 90 days)
Only Nixon 2019 (2029 participants) reported health‐related quality of life, measured using the EQ‐5D‐5L (with 267 participants only) and PU‐QoL‐UI (with 233 participants only). It is unclear if there is a difference in health‐related quality of life (measured using either the EQ‐5D‐5L or PU‐QoL‐UI) at 90 days follow‐up between alternating pressure (active) air surfaces and foam surfaces (low‐certainty evidence). Nixon 2019 reported a MD in the 90‐day EQ‐5D‐5L of 0.00 (95% CI ‐0.05 to 0.05) between 118 participants using alternating pressure (active) air surfaces and 149 using foam surfaces; and a MD in 90‐day PU‐QoL‐UI of 0.00 (95% CI ‐0.03 to 0.03) between 107 participants using alternating pressure (active) air surfaces and 126 using foam surfaces (Analysis 1.3). Evidence certainty was downgraded twice for imprecision due to small sample sizes for this outcome.
1.3. Analysis.

Comparison 1: Alternating pressure (active) air surfaces compared with reactive foam surfaces, Outcome 3: Health‐related quality of life
Cost‐effectiveness (follow‐up duration 90 days)
Only Nixon 2019 (2029 participants) reported the incremental cost per quality‐adjusted life‐years (QALYs) gained based on within‐trial analyses. Moderate‐certainty evidence suggests that alternating pressure (active) air surfaces have a 99% probability of being cost‐effective at a threshold of GBP 20,000 compared with reactive foam surfaces. Evidence certainty was downgraded once for imprecision for the EQ‐5D‐5L outcome from which QALY scores were calculated.
Comparison 2: Alternating pressure (active) air surfaces versus reactive air surfaces (seven studies, 1728 participants)
Seven studies made this comparison (Beeckman 2019; Cavicchioli 2007; Finnegan 2008; Jiang 2014; Malbrain 2010; Price 1999; Sideranko 1992).
Primary outcomes
Proportion of participants developing a new pressure ulcer (median follow‐up duration 14 days, minimum 5 days, maximum 15 days)
Six studies (1648 participants) reported this outcome (Beeckman 2019; Cavicchioli 2007; Finnegan 2008; Jiang 2014; Malbrain 2010; Sideranko 1992) and the data from these were pooled. It is uncertain whether there is a difference in the proportion of participants developing a new ulcer between alternating pressure (active) air surfaces (32/799 (4.0%)) and reactive air surfaces (19/849 (2.2%)). The RR was 1.61 (95% CI 0.90 to 2.88; I2 = 3%; Analysis 2.1). Evidence is of very low certainty, downgraded twice for high risk of bias in domains other than performance bias for three studies contributing over 54% weight in the meta‐analysis, and once for imprecision as, despite the fact that the OIS was met, the wide confidence interval crossed RR = 1.25.
2.1. Analysis.

Comparison 2: Alternating pressure (active) air surfaces compared with reactive air surfaces, Outcome 1: Proportion of participants developing a new pressure ulcer
Subgroup analysis
We considered the studies in Analysis 2.1 heterogeneous in terms of care settings, skin status at baseline, and overall 'risk of bias'. However, we did not perform any pre‐specified subgroup analysis because, as noted in Subgroup analysis and investigation of heterogeneity, the number of included studies was fewer than 10, meaning it would be difficult to meaningfully interpret the results.
Sensitivity analyses
Sensitivity analysis with complete case data . This resulted in a RR of 1.62 (95% CI 0.90 to 2.89; I2 = 3%). The evidence was consistent with the main analysis Analysis 2.1.
Sensitivity analysis with fixed‐effect (rather than random‐effects) model . The use of a fixed‐effect model resulted in a RR of 1.72 (95% CI 1.00 to 2.97; I2 = 3%) so this was consistent with the main analysis.
Sensitivity analysis with time to pressure ulcer development as pressure ulcer incidence measure (follow‐up duration of 14 days). Only Beeckman 2019 (308 participants) reported this outcome. Low‐certainty evidence suggests that people treated with alternating pressure (active) air surfaces may be at more risk of developing an incident pressure ulcer over 14 days' follow‐up than those treated with reactive air surfaces in a nursing home setting (HR 2.25; 95% CI 1.05 to 4.83; Analysis 2.2). The results are sensitive to the choice of format for the primary outcome measure so the main analysis results should be interpreted cautiously. Evidence certainty is low, downgraded twice for high risk of detection bias.
2.2. Analysis.

Comparison 2: Alternating pressure (active) air surfaces compared with reactive air surfaces, Outcome 2: Time to pressure ulcer development
Secondary outcomes
Support‐surface‐associated patient comfort (median follow‐up duration 11 days, minimum 5 days, maximum 14 days)
Four studies (1364 participants) reported this outcome (Cavicchioli 2007; Finnegan 2008; Jiang 2014; Price 1999). The four studies report a range of different measures for this outcome and they cannot be pooled (see Table 7). We are uncertain about any difference in patient comfort responses between alternating pressure (active) air surfaces and reactive air surfaces. Evidence is of very low certainty, downgraded once for high overall risk of bias in three small studies but unclear risk of bias in one large study, and twice for substantial inconsistency.
2. Support‐surface‐associated patient comfort results reported in the included studies.
| Study ID | Results | Comment | |
| Comparison: alternating pressure (active) air surfaces compared with reactive air surfaces | |||
| Cavicchioli 2007 | Dropouts due to discomfort and/or not agreeing to use the assigned modality in alternating low pressure: 5 of 86 | Dropouts due to discomfort and/or not agreeing to use the assigned modality in continuous low pressure: 4 of 84 | |
| Finnegan 2008 | Comfortable: 11/15 Uncomfortable: 2/15 No view: 2/15 |
Comfortable: 4/18 Uncomfortable: 7/18 No view: 7/18 |
Outcome was a categorical response from participants of comfortable, uncomfortable or no view. |
| Jiang 2014 | More than the median (score of 4): 68/462 Less than the median (score of 4): 394/462 |
More than the median (score of 4): 68/482 Less than the median (score of 4): 414/482 |
The level of patients’ comforts measured by asking patients’ feelings after using the mattress (1 = very uncomfortable, 2 = uncomfortable, 3 = just comfortable, 4 = comfortable, 5 = very comfortable) Chi2 = 0.071, P = 0.789 |
| Price 1999 | Mean 60 (SD 25) for 26 individuals in NIMBUS II | Mean 67 (SD 18) for 24 individuals in Repose | Patient comfort measured using a 100 mm visual analogue scale. |
| Comparison: alternating pressure (active) air surfaces compared with another type of alternating pressure (active) air surfaces | |||
| Ballard 1997 | 5 of 10 (50.0%) participants responded that the Debut mattress was more comfortable than their normal bed | 6 of 10 (60.0%) participants responded that the Nimbus mattress was less comfortable than their normal bed |
Preference for the Debut over the Nimbus mattress (Wilcoxon signed ranks exact test P = 0.019) Data available at the second phase of the cross‐over trial only. |
| Demarre 2012 | Withdrawing due to discomfort in Multi‐stage group: 11/298 (3.7%) | Withdrawing due to discomfort in Single‐stage: 16/312 (5.1%) |
|
| Grindley 1996 | 10 responded Nimbus II is more comfortable and 2 responded Pegasus Airwave is more comfortable. 4 responded no preference | 10 responded Nimbus II is more comfortable and 2 responded Pegasus Airwave is more comfortable. 4 responded no preference |
Data available at the second phase of the cross‐over trial only. |
| Nixon 2006 | Alternating pressure air mattress: 186/982 (18.9%) | Alternating pressure air overlay: 230/989 (23.3%) |
|
| Pring 1998 | Refused to be nursed on Nimbus II due to discomfort: 4 patients (10.3%) | Refused to be nursed on Pegasus Airwave due to discomfort: 20 (51.3%) Refused to be nursed on Quattro DC2000: No data |
Significant differences between the 3 mattresses in relation to comfort (one‐way analysis of variance F = 18.28, P < 0.01). Quattro DC2000 more comfortable than Nimbus II and Pegasus Airwave (P < 0.01 in both cases). Data prior to cross‐over of the n‐of‐1 trial were not available. |
| Rafter 2011 | Patients' opinions on the comfort aspects of Dyna‐Form Mercury Advance: all 3 slept well | Patients' opinions on the comfort aspects of Softform Premier Active: all 3 slept well |
Six of ten patients responded to the comfort questionnaire. |
| Taylor 1999 | Trinova: 11/18 (61.1%) comfortable | NA |
Only one arm has data (18/22 completed the questionnaire). |
All reported adverse events
Not reported.
Health‐related quality of life
Not reported.
Cost‐effectiveness
Not reported.
Comparison 3: Alternating pressure (active) air surfaces versus reactive water surfaces (three studies, 414 participants)
Three studies compared alternating pressure (active) air surfaces with reactive water surfaces (Andersen 1982; Bliss 1995; Sideranko 1992). Of these, Bliss 1995 (56 participants) reported the outcome of the numbers of treatment sessions in which pressure ulcers developed or worsened, which we considered not directly relevant to this review.
Primary outcomes
Proportion of participants developing a new pressure ulcer (median follow‐up duration 10.0 days, minimum 10.0 days, maximum 17.7 days)
We pooled available data from two studies (358 participants; Andersen 1982; Sideranko 1992). It is uncertain whether there is a difference in the proportion of participants developing a new pressure ulcer between alternating pressure (active) air surfaces (12/186 (6.5%)) compared with reactive water surfaces (9/172 (5.2%)). The RR was 1.21 (95% CI 0.52 to 2.83; I2 = 0%; Analysis 3.1). Evidence is of very low certainty, downgraded twice for high risk of detection bias in one study contributing over 60% weight in the meta‐analysis and unclear overall risk of bias in another study, and twice for substantial imprecision as the OIS was not met and the confidence interval was very wide and crossed RRs = 0.75 and 1.25.
3.1. Analysis.

Comparison 3: Alternating pressure (active) air surfaces compared with reactive water surfaces, Outcome 1: Proportion of participants developing a new pressure ulcer
The included studies did not report data on time to pressure ulcer incidence.
Subgroup analysis
We considered studies heterogeneous in terms of care setting, and overall 'risk of bias'. However, we did not perform any pre‐specified subgroup analysis because, as noted in Subgroup analysis and investigation of heterogeneity, the number of included studies was fewer than 10, meaning it would be difficult to meaningfully interpret the results.
Sensitivity analyses
Sensitivity analysis with fixed‐effect (rather than random‐effects) model . The use of a fixed‐effect model resulted in a RR of 1.21 (95% CI 0.53 to 2.78; I2 = 0%). The evidence remained consistent with the main analysis Analysis 3.1 (Appendix 6).
Secondary outcomes
None reported.
Comparison 4: Alternating pressure (active) air surfaces versus reactive fibre surfaces (four studies, 384 participants)
Four studies made this comparison (Bliss 1995; Conine 1990; Daechsel 1985; Stapleton 1986). Of these, Bliss 1995 randomised participants into two types of fibre‐filled surfaces (in two individual study arms) that we combined into a single study arm. Bliss 1995 reported the outcome of the numbers of treatment sessions in which pressure ulcers developed or worsened, which we considered not directly relevant to this review.
Primary outcomes
Proportion of participants developing a new pressure ulcer (minimum follow‐up duration 17.7 days, maximum three months or unspecified)
All four studies (384 participants) reported this outcome (Bliss 1995; Conine 1990; Daechsel 1985; Stapleton 1986).
We pooled the data from three studies (285 participants). It is uncertain whether there is a difference in the proportion of participants developing a new pressure ulcer between alternating pressure (active) air surfaces (54/141 (38.3%)) and reactive fibre surfaces (61/144 (42.4%)). The RR was 0.90 (95% CI 0.68 to 1.19; I2 = 0%; Analysis 4.1). Evidence is of very low certainty, downgraded twice for high risk of bias in domains other than performance bias in two studies contributing over 80% weight to the meta‐analysis, and once for imprecision as the OIS was not met.
4.1. Analysis.

Comparison 4: Alternating pressure (active) air surfaces compared with reactive fibre surfaces, Outcome 1: Proportion of participants developing a new pressure ulcer
The included studies did not report data on time to pressure ulcer incidence.
Subgroup analysis
We considered these studies heterogeneous in terms of care settings, participants' average age and skin status at baseline. However, we did not perform any pre‐specified subgroup analysis because, as noted in Subgroup analysis and investigation of heterogeneity, the number of included studies was fewer than 10, meaning it would be difficult to meaningfully interpret the results.
Sensitivity analyses
Sensitivity analysis using complete case data . This resulted in a RR of 0.93 (95% CI 0.72 to 1.20; I2 = 0%). The evidence is consistent with the main analysis Analysis 4.1 (Appendix 6).
Sensitivity analysis with fixed‐effect (rather than random‐effects) model . The use of a fixed‐effect model resulted in a RR of 0.90 (95% CI 0.68 to 1.20; I2 = 0%) and this remained consistent with the main analysis Analysis 4.1 (Appendix 6).
Secondary outcomes
Support‐surface‐associated patient comfort (follow‐up duration of three months)
Only Conine 1990 (187 participants) reported this outcome. We are uncertain about any difference between alternating pressure (active) air surfaces and reactive fibre surfaces in patient comfort responses. Conine 1990 reported 19 dropouts among 93 people using alternating pressure (active) air surfaces; and 17 of 94 using reactive fibre surfaces. The reason for dropout was given as discomfort. Evidence is of very low certainty, downgraded once for high overall risk of bias for this outcome, once for indirectness, and once for imprecision.
All reported adverse events using allocated support surfaces
Not reported.
Health‐related quality of life
Not reported.
Cost‐effectiveness
Not reported.
Comparison 5: Alternating pressure (active) air surfaces on operating tables and subsequently on postoperative ward beds versus reactive gel surfaces used on operating tables followed by foam surfaces on postoperative ward beds (two studies, 415 participants)
Two studies (415 participants) were included in this comparison (Aronovitch 1999; Russell 2000).
Primary outcomes
Proportion of participants developing a new pressure ulcer (follow‐up duration of seven days)
Both studies (415 participants) reported this outcome and these data were pooled (Aronovitch 1999; Russell 2000). Alternating pressure (active) air surfaces applied on both operating tables and hospital beds (3/210 (1.4%)) may reduce the proportion of people developing a new pressure ulcer compared with reactive gel surfaces used on operating tables followed by foam surfaces applied on hospital beds (14/205 (6.8%)); however, this is low‐certainty evidence. The RR is 0.22 (95% CI 0.06 to 0.76; I2 = 0%; Analysis 5.1). Evidence certainty was downgraded once for risk of bias (one study contributing 36% of weight to the meta‐analysis was at high risk of attrition bias whilst the other study was at unclear risk of bias for more than one domain other than performance bias) and once for imprecision as, despite the fact that the OIS was met, the 95% CI crossed RR = 0.75.
5.1. Analysis.

Comparison 5: Alternating pressure (active) air surfaces on operating tables and subsequently on ward beds compared with reactive gel surfaces on operating tables followed by foam surfaces on ward beds, Outcome 1: Proportion of participants developing a new pressure ulcer
The included studies did not report data on time to pressure ulcer incidence.
Subgroup analysis
We considered both studies similar in terms of care settings, follow‐up duration, overall risk of bias, participant characteristics and interventions: statistical heterogeneity was low (Chi2 test P value = 0.55; Tau2 = 0.00; I2 = 0%). Because the number of included studies was less than 10, we did not undertake a subgroup analysis.
Sensitivity analyses
Sensitivity analysis with fixed‐effect (rather than random‐effects) model . The use of a fixed‐effect model resulted in a RR of 0.21 (95% CI 0.06 to 0.72; I2 = 0%) and this remained consistent with the main analysis Analysis 5.1 (Appendix 6).
Secondary outcomes
Support‐surface‐associated patient comfort
None reported.
All reported adverse events (follow‐up duration of seven days)
Only Russell 2000 (198 participants) reported this outcome. It is uncertain if there is a difference between alternating pressure (active) air surfaces and the alternative in adverse events. The study authors claimed that approximately one half of people in each group reported one or more types of adverse events, with no difference between groups reported. The study authors also noted that no adverse events were considered to be related to the mattresses assigned. Evidence is of very low certainty, downgraded once for unclear risk of bias in more than one domain other than performance bias, and twice for imprecision due to small sample size.
Health‐related quality of life
Not reported.
Cost‐effectiveness
Not reported.
Comparison 6: Comparison between two types of alternating pressure (active) air surfaces (ten studies, 2868 participants)
We included 10 studies (2868 participants) that compared two or more different types of alternating pressure (active) air surfaces (Ballard 1997; Demarre 2012; Gray 2008; Grindley 1996; Hampton 1997; Nixon 2006; Pring 1998; Rafter 2011; Taylor 1999; Theaker 2005). Specifically, three studies included an alternating pressure (active) air surface with a hybrid (active/reactive) function (Gray 2008; Hampton 1997; Taylor 1999); Rafter 2011 and Theaker 2005 compared two types of alternating pressure (active) air surface that could both be classed as hybrid air surfaces, and one type of hybrid air surface used in Theaker 2005 also had a low‐air‐loss feature. The remaining five studies compared different types of standard alternating pressure (active) air surfaces.
We did not pool data from the 10 studies as such comparisons are not meaningful beyond the individual study level. We summarise study findings narratively below with key outcome data presented in Table 7 and Table 8.
3. Pressure ulcer incidence results reported in studies that compared different types of alternating pressure (active) air surfaces.
| Study ID | Results | Comment | |
| Comparison: alternating pressure (active) air surfaces compared with other types of alternating pressure (active) air surfaces | |||
| Demarre 2012 | Alternating pressure (active) air surfaces (Hill‐Rom ClinActiv)
|
Alternating pressure (active) air surfaces (Hill‐Rom Alto mattress)
|
|
| Gray 2008 | Alternating pressure (active) air surfaces (hybrid air surfaces: Softform Premier Active Mattress)
|
Alternating pressure (active) air surfaces
|
|
| Hampton 1997 | Alternating pressure (active) air surfaces (hybrid air surfaces: Cairwave Therapy System)
|
Alternating pressure (active) air surfaces
|
|
| Nixon 2006 | Alternating pressure (active) air surfaces (mattresses)
|
Alternating pressure (active) air surfaces (overlays)
|
|
| Rafter 2011 | Alternating pressure (active) air surfaces (hybrid air surfaces: Dyna‐Form Mercury Advance)
|
Alternating pressure (active) air surfaces (hybrid air surfaces: Softform Premier Active)
|
|
| Taylor 1999 | Alternating pressure (active) air surfaces (hybrid air surfaces: Pegasus Trinova)
|
Alternating pressure (active) air surfaces
|
|
| Theaker 2005 | Alternating pressure (active) air surfaces (hybrid air surfaces: KCI TheraPulse bed with low‐air‐loss feature)
|
Alternating pressure (active) air surfaces (hybrid air surfaces: Hill‐Rom Duo mattress)
|
|
IQR ‐ interquartile range
Primary outcomes
Proportion of participants developing a new pressure ulcer (median follow‐up period one month, minimum 10.5 days, maximum six months)
Seven studies (2833 participants) reported this outcome with no study showing a difference in the proportion of people with incident pressure ulcers between different types of alternating pressure (active) air surfaces (Demarre 2012; Gray 2008; Hampton 1997; Nixon 2006; Rafter 2011; Taylor 1999; Theaker 2005). See Table 8. These study findings were considered to be of low certainty overall, downgraded once for risk of bias as two small studies were at high risk of bias in domains other than performance bias and all the remaining five studies were at unclear risk of bias in at least one domain other than performance bias, and once for imprecision as the number of events was relatively low and the 95% CIs in each study included both benefits and harms as well as no effect.
Two studies (2581 participants) reported time to pressure ulcer development (Demarre 2012; Nixon 2006; follow‐up period 14 and 60 days). Neither of these studies suggested a difference in the risk of developing an incident pressure ulcer over 60 days' follow‐up between these support surfaces. This is consistent with the pressure ulcer risk finding. Evidence is of low certainty, downgraded once for unclear risk of bias in domains other than performance bias in both included studies, and once for imprecision as the 95% CIs of both studies included both benefits and harms as well as no effect.
Secondary outcomes
Support‐surface‐associated patient comfort (median follow‐up duration 10.5 days, minimum 3 days, maximum 60 days)
Seven studies (2705 participants) reported this outcome (Ballard 1997; Demarre 2012; Grindley 1996; Nixon 2006; Pring 1998; Rafter 2011; Taylor 1999). The studies reported a range of different measures and outcome data cannot be easily interpreted (see Table 7). We are uncertain if there is a difference in support‐surface‐associated patient comfort between different types of alternating pressure (active) air surfaces. Evidence is of very low certainty, downgraded once for risk of bias (three small studies with a high risk of bias judgement for at least one domain other than performance bias, and all the rest having an unclear judgement for at least one domain other than performance bias), once for inconsistency in terms of comfort results across studies, and once for strongly suspected publication bias.
All reported adverse events (median follow‐up duration 60 days)
Only Nixon 2006 (1971 participants) reported this outcome for its comparison of mattress and overlay formats of alternating air (active) surfaces. We are uncertain if there is a difference in the adverse events between the two formats of alternating pressure (active) air surfaces. Nixon 2006 reported that 377 adverse events were observed among 308 participants within 60 days. However, the study authors did not report these data by study groups, although they did present surface‐related adverse events by study groups (10 participants in alternating pressure air mattresses and four in alternating pressure air overlays). Evidence is of very low certainty, downgraded twice for high overall risk of bias for this outcome due to high attrition bias, and twice for imprecision due to small sample size.
Health‐related quality of life
Not reported.
Cost‐effectiveness (follow‐up duration median 60 days)
Only Nixon 2006 (1971 participants) reported this outcome using a trial‐based, cost‐effectiveness analysis for its comparison of mattress and overlay formats of alternating air (active) surfaces. The cost‐effectiveness acceptability curve indicated that, on average, alternating pressure mattresses were associated with an 80% probability of being cost‐saving compared with alternating pressure overlays. Evidence is of moderate certainty, downgraded once for an unclear risk of bias in one domain other than performance bias: Nixon 2006 was at an unclear risk of detection bias in terms of both the health benefit (time to pressure ulcer development) and costs in the economic analysis.
In its base case analysis, Nixon 2006 reported that alternating pressure air mattresses were associated with a delay in pressure ulcer development and lower overall costs (mean difference in total costs between overlay and mattress groups: GBP 283.60 per participant on average, 95% CI GBP 377.59 to GBP 976.79; and the mean difference in the restricted Kaplan–Meier estimates of time to pressure ulcer onset between overlay and mattress groups: –10.63 days, 95% bias‐corrected CI of the difference –24.40 to 3.09 days). The analysis was from the perspective of the UK National Health Service (NHS) and Personal Social Service; but there was no cost discounting due to the time horizon being less than one year.
Discussion
Summary of main results
We report evidence from 32 RCTs on the effects of alternating pressure (active) air beds or mattresses compared with any support surface on the incidence of pressure ulcers in any setting and population. We did not analyse data reported in four studies that compared alternating pressure (active) air surfaces with 'standard hospital surfaces' that were not well described, because the term ‘standard hospital surface’ does not represent a single recognisable surface internationally or over time. We summarise key findings for six specific comparisons that had data analyses as follows:
Alternating pressure air surfaces versus foam surfaces: alternating pressure (active) air surfaces may reduce the proportion of people developing incident pressure ulcers compared with foam surfaces (4 studies, 2247 participants; low‐certainty evidence). It is uncertain whether there is any difference in the risk of developing a new pressure ulcer over 60 days' follow‐up (2 studies, 2105 participants; very low‐certainty evidence); in support‐surface‐associated patient comfort (1 study, 76 participants; very low‐certainty evidence); in health‐related quality of life at 90 days' follow‐up (1 study, 2029 participants; low‐certainty evidence); as well as in the number of all reported adverse events (3 studies, 2181 participants; very low‐certainty evidence) between these types of support surfaces. We found moderate‐certainty cost‐effectiveness evidence that alternating pressure (active) air surfaces are probably more cost‐effective than foam surfaces. Although there were negligible differences in participant‐reported health utility in those allocated to alternating pressure (active) air surfaces and foam surfaces, the difference in costs between these trial arms (with the arm of foam surfaces having higher costs) meant the cost‐effectiveness finding favoured the alternating pressure (active) air surfaces (Nixon 2019).
Alternating pressure air surfaces versus reactive air surfaces: it is uncertain if there is any difference between alternating pressure (active) air surfaces and reactive air surfaces in the proportion of participants developing a new pressure ulcer (6 studies, 1648 participants; very low‐certainty evidence). When we considered time to pressure ulcer development as our primary outcome, we found that people using alternating pressure (active) air surfaces may be more likely to develop an incident pressure ulcer than those treated with reactive air surfaces over 14 days' follow‐up in a nursing home setting (1 study, 308 participants; low‐certainty evidence). For our secondary outcome, we are uncertain if there is a difference in support‐surface‐associated patient comfort between alternating pressure (active) air surfaces and reactive air surfaces (4 studies, 1364 participants; very low‐certainty evidence).
Alternating pressure air surfaces versus reactive water surfaces: it is uncertain if there is a difference in the proportion of participants developing a new pressure ulcer between alternating pressure (active) air surfaces and reactive water‐filled surfaces (2 studies, 358 participants; very low‐certainty evidence). We did not find data for our secondary outcomes.
Alternating pressure air surfaces versus reactive fibre surfaces: it is uncertain if there is a difference in the proportion of participants developing a new pressure ulcer between alternating pressure (active) air surfaces and reactive fibre surfaces (3 studies, 285 participants; very low‐certainty evidence). We also found it is uncertain if there is a difference in support surface associated patient comfort between these support surfaces (1 study, 187 participants; very low‐certainty evidence).
Alternating pressure (active) air surfaces on operating tables and subsequently on ward beds versus reactive gel surfaces used on operating tables followed by foam surfaces on ward beds. Alternating pressure (active) air surfaces applied on both operating tables and hospital beds may reduce the proportion of people developing a new pressure ulcer compared with reactive gel surfaces used on operating tables followed by foam surfaces applied on hospital beds (2 studies, 415 participants). However, this is low‐certainty evidence. We are uncertain if there is any difference in adverse events between these support surfaces (1 study, 198 participants; very low‐certainty evidence).
Alternating pressure air surfaces versus alternating pressure air surfaces: we found low‐certainty evidence suggesting little to no difference in the risk of developing a new pressure ulcer when treated with different forms of alternating pressure (active) air surfaces (7 studies, 2833 participants). We are uncertain whether there is any difference in support‐surface‐associated patient comfort and adverse effects between different forms of alternating pressure (active) air surfaces (very low‐certainty evidence). There is moderate‐certainty evidence that alternating pressure air mattresses are probably more cost‐effective than alternating pressure air overlays.
Overall completeness and applicability of evidence
As detailed in Search methods for identification of studies, we ran a comprehensive set of literature searches to maximise the relevant research included here.
Whilst use of support surfaces is relevant to adults and children, all participants in the included studies were adults (with the reported average age ranging from 37.2 to 87.0 years, median of 69.1 years). Across the included studies, more than half (55.6%) of enrolled participants were female. Almost all of the studies enrolled people who were at (high) risk of pressure ulceration (with risk assessed using a risk assessment tool (e.g. the Braden scale)), and who were ulcer‐free at the time of recruitment. Nine of the included studies (with 4808 participants) did include participants with superficial pressure ulcers at baseline.
Most of the included studies were small (half had fewer than 100 participants). Nine studies enrolled more than 200 participants (Andersen 1982; Aronovitch 1999; Beeckman 2019; Bliss 1995; Demarre 2012; Jiang 2014; Laurent 1998; Nixon 2006; Nixon 2019), of which six studies enrolled more than 400 participants (Andersen 1982; Bliss 1995; Demarre 2012; Jiang 2014; Nixon 2006; Nixon 2019). These six trials together accounted for 73% (6624/9058) of the participants in the review.
The geographical scope of the included studies was limited. Almost all of the studies were from Europe and North America. Only one large trial was from China (Jiang 2014), and another one was from Japan (Sanada 2003).
The included studies recruited participants from a variety of care settings including: acute care settings (19 studies); community and long‐term care settings (nine studies), or both (one study), and intensive care units (three studies). Whilst five of the six comparisons included studies from a variety of care settings, due to a limited number of included studies for these four comparisons, we could not perform pre‐specified subgroup analysis by different care settings. Thus, for these five comparisons, we are unable to drawn conclusions about potential modification of treatment effects in different care settings. An exception to this is the comparison of the alternating pressure (active) air surface on operating tables and subsequently on the ward bed with the reactive gel surface on operating tables followed by the foam surface applied on ward beds. This evidence suggests the beneficial effects of using alternating pressure (active) air surfaces on both operating tables and hospital ward beds. There were no data specifically for operating rooms.
We recognise that alternating pressure (active) air surfaces can have a range of cell sizes (e.g. large cells, small cells) and other features (e.g. being able to operate as a hybrid surface switching between active and reactive modes; low‐air‐loss; see Appendix 4). In this review, we considered all these specific types (e.g. alternating pressure (active) low‐air‐loss surfaces, and hybrid air surfaces) as alternating pressure (active) air surfaces because they have the same underlying mechanism of redistributing pressure activity (i.e. mechanically alternating pressure). Some health professionals have expressed an interest in the effectiveness of support surfaces defined as hybrid based on having a mixed composition of materials; for example, surfaces made from alternating pressure air cells on a foam layer as opposed to only air cells. When exploring the evidence in this way, we identified very limited evidence. Such exploration may be important for future work if deemed a clinical priority.
We did not analyse data reported in another four studies comparing alternating pressure (active) air surfaces with 'standard hospital surfaces'. Those surfaces were labelled with that term by the original study authors, and we could not define them using the NPIAP S3I 2007 support surfaces terms and definitions. However, for completeness of all relevant evidence, we reported the data from these studies in Appendix 5.
Another potential limitation in the included studies is the large variation in duration of follow‐up (ranging from three days to 180 days, median of 14 days). This is partly because different follow‐up durations are appropriate in different care settings. For example, participants staying in acute care settings are more likely to be discharged after a short‐term hospital stay, whilst those staying at community and long‐term care settings will typically stay for longer. The short median duration of follow‐up may contribute to an under‐estimation of pressure ulcer incidence across study groups of the included studies because most pressure ulcers would occur in the first two to four weeks after hospital admission (Schoonhoven 2007), and some incident pressure ulcers may have been missed in these studies.
Quality of the evidence
We implemented the GRADE approach for assessing the certainty of the evidence and found that most included evidence from our 19 meta‐analyses or syntheses across six comparisons was of low and very low certainty. Downgrading of evidence was largely due to the high risk of bias of findings and imprecision due to small study sizes in terms of participants or event numbers, or both. There was also some inconsistency across studies and publication bias for some comparisons.
Limitations in study design
We downgraded once or twice for study limitations for almost all evidence. We assessed risk of bias according to seven domains: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, selective outcome reporting, incomplete follow‐up, and other potential biases. Of the 32 studies, we judged 25 as being at high overall risk of bias, and only seven at unclear overall risk of bias. The prevalence of high overall risk of bias is partly due to the non‐blinding of participants and personnel for most of comparisons. We acknowledged that such blinding of participants and personnel is impractical for almost all comparisons. Therefore, we did not downgrade certainty of evidence for studies at high overall risk of bias solely due to the possible presence of performance bias.
Ten studies were also at high risk of bias due to unblinded outcome assessment. Unblinded assessment has been found to exaggerate odds ratios (from subjective binary outcomes) by, on average, 36% (Hróbjartsson 2012). The outcome assessment of pressure ulcer incidence is subjective and blinded assessment ‐ whilst operationally challenging ‐ can be undertaken; for example, through masked adjudication of photographs of pressure areas (Baumgarten 2009). Therefore, we considered unblinded pressure ulcer incidence assessment could substantially bias effect estimates in the included studies and downgraded the certainty of evidence for detection bias on a study‐by‐study basis.
Indirectness of evidence
In general, we considered that the participants, interventions, and outcomes in the included studies were within the scope of the published review protocol and there was no indirectness. Therefore, we did not downgrade for indirectness, with the exception of one piece of included evidence: the evidence for support‐surface‐associated patient comfort outcome in the comparison of alternating pressure (active) air surfaces versus reactive fibre surfaces. In the only included study for this outcome, the reason for dropout was considered as discomfort. Therefore, the evidence may not be directly relevant to the comfort outcome of this review.
Inconsistency of results and unexplained heterogeneity
Statistical heterogeneity was low for most of the evidence syntheses (15/19) we performed and we did not downgrade for inconsistency for these pieces of evidence. The low statistical heterogeneity was partly because eight of the 19 syntheses included only one study. One of the 19 meta‐analyses suggested some heterogeneity (I2 = 63% in Analysis 1.1). However, we did not downgrade for inconsistency for this because our additional exploratory analyses suggested the heterogeneity could be well explained by excluding a study with an extreme value. We downgraded for inconsistency for the rest (four) of the meta‐analyses or narrative syntheses. None of these four analyses included more than seven studies. Despite the fact that we found heterogeneity in terms of overall risk of bias, care settings, outcome measurement methods, or follow‐up durations between their included studies, we investigated their heterogeneity using subgroup analysis and we considered their heterogeneity (inconsistency) unexplained.
We have to note that, although we planned to calculate prediction intervals to understand the implications of heterogeneity, all analyses included a small number (up to seven) of included studies which was fewer than the 10 needed for this calculation.
Imprecision of results
We downgraded once or twice for imprecision for most comparisons. Study sample sizes were small in most cases (median sample size: 83; range: 10 to 2029) with often small numbers of events and wide associated confidence intervals around effect estimates. Confidence intervals often crossed the line of null effect and RRs = 0.75 and/or 1.25, thus meaning we could not discern whether the true population effect was likely to be beneficial or harmful.
Publication bias
We did not downgrade the certainty of evidence for publication bias in almost all meta‐analyses. This is because (1) we have confidence in the comprehensiveness of our literature searches; and (2) we did not find any clear evidence of non‐reporting bias of study results. Although we planned to perform funnel plots for meta‐analysis to visually inspect for publication bias, there was no analysis including more than ten studies.
Potential biases in the review process
We followed pre‐specified methods to review evidence in order to prevent potential bias in the review process. For example, we ran comprehensive electronic searches, searched trials registries, and checked the references of systematic reviews identified by the electronic searches.
This review also has limitations. Firstly, some included studies may have considered co‐interventions as 'usual care' but did not fully describe them. We assumed that all studies had provided co‐interventions equally to participants in their study groups if there was nothing to indicate that this was not the case. Secondly, we did not implement pre‐specified subgroup analysis, as mentioned above, mainly because no analysis included more than ten studies. Thirdly, we included a factorial design study ‐ Laurent 1998 ‐ in this review but did not consider the potential interaction between interventions. Fourthly, only Nixon 2019 reported HRs and CIs related to time‐to‐event data. The remaining HRs and CIs we used in related analyses were calculated using the methods described in Tierney 2007. We recognised that those calculated data (and associated meta‐analyses) might be inaccurate. We noted that almost all time‐to‐event data analyses using the HRs and CIs we calculated appeared (or tended) to agree with associated binary data analyses as we expected. Fifthly, four studies described their controls as 'standard hospital surfaces' but did not specify the construction materials of these surfaces. Although we made efforts to collect information on these surfaces, we were not able to classify them. Traditionally, ‘standard hospital surfaces’ meant foam surfaces, but we felt adopting that assumption was unwarranted. Further classification of these surfaces might change the results of some comparisons; for example, alternating pressure (active) air surfaces versus foam surfaces. Finally, we were not able to pre‐specify the comparisons included in this review. This is because specific support surfaces applied could only be known and defined once eligible studies were included. However, we pre‐planned to use the NPIAP S3I 2007 support surface terms and definitions to define specific support surfaces in order to avoid any potential bias.
Agreements and disagreements with other studies or reviews
To our knowledge, among the 14 systematic reviews or meta‐analyses we identified in electronic searches for this review (Chou 2013; Huang 2013; McGinnis 2011; McInnes 2015; McInnes 2018; Mistiaen 2010; De Oliveira 2017; Rae 2018; Reddy 2006; Reddy 2008; Serraes 2018; Shi 2018a; Smith 2013; Yao 2018), two recent comprehensive reviews include alternating pressure (active) air surfaces evidence: Shi 2018a, and the Cochrane Review 'Support surfaces for pressure ulcer prevention' (McInnes 2015).
This review differs from Shi 2018a in how specific alternating pressure (active) air surfaces are classified. In this review, we consider them as a single generic group, whereas Shi 2018a considered alternating pressure (active) low‐air‐loss surfaces, hybrid air surfaces and generic alternating pressure (active) air surfaces as separate groups.
Additionally, Shi 2018a grouped some interventions under the term 'standard hospital surfaces' but concluded that the types of surfaces labelled in this way varied over time, and by setting. In this review, we made great efforts to define surfaces where these surfaces were described as a 'standard hospital surface' in the included studies to ensure they were placed in the correct comparisons. This re‐definition allowed us to define the 'conventional management' used in Aronovitch 1999 and Russell 2000 as reactive gel surfaces followed by foam surfaces, rather than standard hospital surfaces. We classified 'standard hospital surfaces' used in other studies as undefined surfaces.
Shi 2018a reported moderate‐certainty evidence favouring alternating pressure (active) air surfaces. The reasons above may explain some of the inconsistency between the reviews but, importantly, Shi 2018a was a network meta‐analysis.
Shi 2018a indicated an evidence gap around the comparison alternating pressure (active) air surfaces versus foam surfaces, and expected to tackle this gap by including a large, then ongoing study ‐ Nixon 2019 ‐ in data analysis. This review did include this study, but this still resulted in some uncertain evidence with the use of pairwise meta‐analysis methods. Further review work using network meta‐analysis adds to the findings reported here (Shi 2021).
The Cochrane Review McInnes 2015 grouped a variety of reactive surfaces ('Silicore overlay', a 'water mattress', a 'foam pad', and 'static air mattresses') into 'constant low‐pressure devices', concluding that it was unclear whether alternating pressure (active) air surfaces impacted on incident pressure ulceration compared with these constant low‐pressure devices. The conclusions of McInnes 2015 are generally consistent with our review but our review adds more granular findings to the evidence base. By using the NPIAP S3I terms for support surfaces, our review differentiated reactive surfaces from each other, and presents separate analyses for each.
Authors' conclusions
Implications for practice.
Current evidence is uncertain about the difference in pressure ulcer incidence between alternating pressure (active) air surfaces and other surfaces: reactive water surfaces, reactive fibre surfaces and reactive air surfaces. People using alternating pressure (active) air surfaces may reduce pressure ulcer incidence compared with those using foam surfaces. Also, alternating pressure (active) air surfaces applied on both operating tables and hospital beds may reduce pressure ulcer incidence compared with reactive gel surfaces used on operating tables followed by foam surfaces applied on hospital beds. However, people using alternating pressure (active) air surfaces may be more likely to develop an incident pressure ulcer than those treated with reactive air surfaces over 14 days' follow‐up in a nursing home setting. Alternating pressure (active) air mattresses are probably more cost‐effective than overlay versions of this technology for people in acute care settings. Alternating pressure (active) air surfaces are probably more cost‐effective than foam surfaces for people in community and acute care settings.
Implications for research.
Given the large number of different support surfaces available, future studies should prioritise which support surfaces to evaluate on the basis of the priorities of decision‐makers. For example, alternating pressure air surfaces versus reactive air surfaces may be a high priority for future evaluation. All interventions used should be clearly described using the current classification system, and researchers should avoid the use of generic terms such as 'standard hospital surfaces'. Limitations in included studies are largely due to small sample size and sub‐optimal RCT design. The incidence of pressure ulcers can be low in certain settings and this needs to be considered in sample size calculations and when considering the feasibility of trial conduct. Under‐recruitment or over‐estimation of event rates that then fail to occur, or both, can lead to imprecision and less robust effect estimates.
Future studies should also consider carefully the choice of outcomes they report. Time‐to‐event data for pressure ulcer incidence should be used in studies. Careful and consistent assessment and reporting of adverse events needs to be undertaken to generate meaningful data that can be compared between studies. Likewise, patient comfort is an important outcome but poorly defined and reported, and this needs to be considered in future research studies. Further studies should aim to collect and report health‐related quality of life using validated measures. Finally, future studies should nest cost‐effectiveness analysis in their conduct where possible.
Any future studies must be undertaken to the highest standard possible. Whilst it is challenging to avoid the risk of performance bias in trials of support surfaces as blinding of participants and personnel is seldom possible, stringent protocols ‐ for example, in terms of encouraging consistent care and blinded decision‐making ‐ can help to minimise the risk. It is also important to fully describe co‐interventions (e.g. repositioning) and ensure protocols mandate balanced use of these across trial arms. The risk of detection bias can also be minimised with the use of digital photography and adjudicators of the photographs being masked to support surfaces (Baumgarten 2009). Follow‐up periods should be for as long as possible and clinically relevant in different settings. Where possible and useful, data collection after discharge from acute settings may be considered.
What's new
| Date | Event | Description |
|---|---|---|
| 18 August 2021 | Amended | Minor amendment to include link to overview and network meta‐analysis. |
History
Protocol first published: Issue 5, 2020 Review first published: Issue 5, 2021
Acknowledgements
The authors are grateful to the following peer reviewers who provided feedback on both the protocol and the review: Julie Bruce and Zena Moore. Thanks are also due to Denise Mitchell for copy‐editing the protocol, to Jess Sharp for additional copy‐edit feedback, to Faith Armitage for copy‐editing the review and to Nicole Pitcher for writing the Plain Language Summary.
We also would like to thank Zhenmi Liu, Gill Norman and Melanie Stephens for double‐checking data extraction and risk of bias assessment for this review and Cochrane Musculoskeletal, Oral, Skin and Sensory Network Editors Peter Tugwell and Jennifer Hilgart for feedback and final approval of the review for publication.
Appendices
Appendix 1. Full details of classifications of support surfaces
| Overarching class of support surface (as used in this review) | Corresponding subclasses of support surfaces used inShi 2018a | Descriptions of support surfaces | Selected examples (with example brands where possible) |
| Reactive air surfaces | Powered/non‐powered reactive air surfaces | A group of support surfaces constructed of air‐cells, which redistribute body weight over a maximum surface area (i.e. has reactive pressure redistribution mode), with or without the requirement for electrical power. | Static air mattress overlay, dry flotation mattress (e.g. Roho, Sofflex), static air mattress (e.g. EHOB), and static mode of Duo 2 mattress. |
| Powered/non‐powered reactive low‐air‐loss air surfaces | A group of support surfaces made of air‐cells, which have reactive pressure redistribution modes and a low‐air‐loss function, with or without the requirement for electrical power. | Low‐air‐loss hydrotherapy. | |
| Powered reactive air‐fluidised surfaces | A group of support surfaces made of air‐cells, which have reactive pressure redistribution modes and an air‐fluidised function, with the requirement for electrical power. | Air‐fluidised bed (e.g. Clinitron). | |
| Foam surfaces | Non‐powered reactive foam surfaces | A group of support surfaces made of foam materials, which have a reactive pressure redistribution function, without the requirement for electrical power. | Convoluted foam overlay (or pad), elastic foam overlay (e.g. Aiartex, microfluid static overlay), polyether foam pad, foam mattress replacement (e.g. MAXIFLOAT), solid foam overlay, viscoelastic foam mattress/overlay (e.g. Tempur, CONFOR‐Med, Akton, Thermo). |
| Alternative reactive support surfaces (non‐foam or air‐filled): reactive fibre surfaces | Non‐powered reactive fibre surfaces | A group of support surfaces made of fibre materials, which have a reactive pressure redistribution function, without the requirement for electrical power. | Silicore (e.g. Spenco) overlay/pad. |
| Alternative reactive support surfaces (non‐foam or air‐filled): reactive gel surfaces | Non‐powered reactive gel surfaces | A group of support surfaces made of gel materials, which have a reactive pressure redistribution function, without the requirement for electrical power. | Gel mattress, gel pad used in operating theatre. |
| Alternative reactive support surfaces (non‐foam or air‐filled): reactive sheepskin surfaces | Non‐powered reactive sheepskin surfaces | A group of support surfaces made of sheepskin, which have a reactive pressure redistribution function, without the requirement for electrical power. | Australian Medical Sheepskins overlay. |
| Alternative reactive support surfaces (non‐foam or air‐filled): reactive water surfaces | Non‐powered reactive water surfaces | A group of support surfaces based on water, which has the capability of a reactive pressure redistribution function, without the requirement for electrical power. | Water mattress. |
| Alternating pressure (active) air surfaces | Powered active air surfaces | A group of support surfaces made of air‐cells, which mechanically alternate the pressure beneath the body to reduce the duration of the applied pressure (mainly via inflating and deflating to alternately change the contact area between support surfaces and the body; i.e. alternating pressure (or active) mode), with the requirement for electrical power. | Alternating pressure‐relieving air mattress (e.g. Nimbus II, Cairwave, Airwave, MicroPulse), large‐celled ripple. |
| Powered active low‐air‐loss air surfaces | A group of support surfaces made of air‐cells, which have the capability of alternating pressure redistribution as well as low air loss for drying local skin, with the requirement for electrical power. | Alternating pressure low‐air‐loss air mattress. | |
| Powered hybrid system air surfaces | A group of support surfaces made of air‐cells, which offer both reactive and active pressure redistribution modes, with the requirement for electrical power. | Foam mattress with dynamic and static modes (e.g. Softform Premier Active). | |
| Powered hybrid system low‐air‐loss air surfaces | A group of support surfaces made of air‐cells, which offer both reactive and active pressure redistribution modes as well as a low‐air‐loss function, with the requirement for electrical power. | Stand‐alone bed unit with alternating pressure, static modes and low air‐loss (e.g. TheraPulse). | |
| Standard hospital surfaces | Standard hospital surfaces | A group of support surfaces made of any materials, used as‐usual in a hospital and without reactive or active pressure redistribution capabilities, nor any other functions (e.g. low air loss, or air‐fluidised). | Standard hospital (foam) mattress, National Health Service Contract hospital mattress, standard operating theatre surface configuration, standard bed unit and usual care. |
Appendix 2. Search strategies
Cochrane Wounds Specialised Register
1 MESH DESCRIPTOR beds EXPLODE ALL AND INREGISTER
2 mattress* AND INREGISTER
3 (foam or transfoam) AND INREGISTER
4 overlay* AND INREGISTER
5 (pad or pads) AND INREGISTER
6 gel AND INREGISTER
7 (pressure NEXT relie*) AND INREGISTER
8 (pressure NEXT reduc*) AND INREGISTER
9 (pressure NEXT alleviat*) AND INREGISTER
10 ("low pressure" near2 device*) AND INREGISTER
11 ("low pressure" near2 support) AND INREGISTER
12 (constant near2 pressure) AND INREGISTER
13 "static air" AND INREGISTER
14 (alternat* next pressure) AND INREGISTER
15 (air next suspension*) AND INREGISTER
16 (air next bag*) AND INREGISTER
17 (water next suspension*) AND INREGISTER
18 sheepskin AND INREGISTER
19 (turn* or tilt*) next (bed* or frame*) AND INREGISTER
20 kinetic next (therapy or table*) AND INREGISTER
21 (net next bed*) AND INREGISTER
22 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 AND INREGISTER
23 MESH DESCRIPTOR Pressure Ulcer EXPLODE ALL AND INREGISTER
24 (pressure next (ulcer* or sore* or injur*)) AND INREGISTER
25 (decubitus next (ulcer* or sore*)) AND INREGISTER
26 ((bed next sore*) or bedsore*) AND INREGISTER
27 #23 OR #24 OR #25 OR #26 AND INREGISTER
28 #22 AND #27 AND INREGISTER
The Cochrane Central Register of Controlled Clinical Trials (CENTRAL)
#1 MeSH descriptor: [Beds] explode all trees
#2 mattress*:ti,ab,kw
#3 (foam or transfoam):ti,ab,kw
#4 overlay*:ti,ab,kw
#5 "pad" or "pads":ti,ab,kw
#6 "gel":ti,ab,kw
#7 (pressure next relie*):ti,ab,kw
#8 (pressure next reduc*):ti,ab,kw
#9 (pressure next alleviat*):ti,ab,kw
#10 ("low pressure" near/2 device*):ti,ab,kw
#11 ("low pressure" near/2 support):ti,ab,kw
#12 (constant near/2 pressure):ti,ab,kw
#13 "static air":ti,ab,kw
#14 (alternat* next pressure):ti,ab,kw
#15 (air next suspension*):ti,ab,kw
#16 (air next bag*):ti,ab,kw
#17 (water next suspension*):ti,ab,kw
#18 sheepskin:ti,ab,kw
#19 (turn* or tilt*) next (bed* or frame*):ti,ab,kw
#20 kinetic next (therapy or table*):ti,ab,kw
#21 (net next bed*):ti,ab,kw
#22 {or #1‐#21}
#23 MeSH descriptor: [Pressure Ulcer] explode all trees
#24 (pressure next (ulcer* or sore* or injur*)):ti,ab,kw
#25 (decubitus next (ulcer* or sore*)):ti,ab,kw
#26 ((bed next sore*) or bedsore*):ti,ab,kw
#27 {or #23‐#26}
#28 (#22 and #27) in Trials
Ovid MEDLINE
1 exp Beds/
2 mattress*.mp.
3 (foam or transfoam).mp.
4 overlay*.mp.
5 (pad or pads).ti,ab.
6 gel.ti,ab.
7 pressure relie*.mp.
8 pressure reduc*.mp.
9 pressure alleviat*.mp.
10 (low pressure adj2 device*).mp.
11 (low pressure adj2 support).mp.
12 (constant adj2 pressure).mp.
13 static air.mp.
14 (alternat* adj pressure).mp.
15 air suspension*.mp.
16 air bag*.mp.
17 water suspension*.mp.
18 sheepskin.mp.
19 ((turn* or tilt*) adj (bed* or frame*)).mp.
20 (kinetic adj (therapy or table*)).mp.
21 net bed*.mp.
22 or/1‐21
23 exp Pressure Ulcer/
24 (pressure adj (ulcer* or sore*)).mp.
25 (decubitus adj (ulcer* or sore*)).mp.
26 (bed adj (ulcer* or sore*)).mp.
27 or/23‐26
28 and/22,27
29 randomized controlled trial.pt.
30 controlled clinical trial.pt.
31 randomi?ed.ab.
32 placebo.ab.
33 clinical trials as topic.sh.
34 randomly.ab.
35 trial.ti.
36 or/29‐35
37 exp animals/ not humans.sh.
38 36 not 37
39 28 and 38
Ovid Embase
1 exp Bed/
2 mattress*.mp.
3 (foam or transfoam).mp.
4 overlay*.mp.
5 (pad or pads).ti,ab.
6 gel.ti,ab.
7 pressure relie*.mp.
8 pressure reduc*.mp.
9 pressure alleviat*.mp.
10 (low pressure adj2 device*).mp.
11 (low pressure adj2 support).mp.
12 (constant adj2 pressure).mp.
13 static air.mp.
14 (alternat* adj pressure).mp.
15 air suspension*.mp.
16 air bag*.mp.
17 water suspension*.mp.
18 sheepskin.mp.
19 ((turn* or tilt*) adj (bed* or frame*)).mp.
20 (kinetic adj (therapy or table*)).mp.
21 net bed*.mp.
22 or/1‐21
23 exp Decubitus/
24 (pressure adj (ulcer* or sore*)).mp.
25 (decubitus adj (ulcer* or sore*)).mp.
26 (bed adj (ulcer* or sore*)).mp.
27 or/23‐26
28 and/22,27
29 Randomized controlled trials/
30 Controlled clinical study/
31 Single‐Blind Method/
32 Double‐Blind Method/
33 Crossover Procedure/
34 (random* or factorial* or crossover* or cross over* or cross‐over* or placebo* or assign* or allocat* or volunteer*).ti,ab.
35 (doubl* adj blind*).ti,ab.
36 (singl* adj blind*).ti,ab.
37 or/29‐36
38 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/
39 human/ or human cell/
40 and/38‐39
41 38 not 40
42 37 not 41
43 28 and 42
EBSCO CINAHL Plus
S50 S26 AND S49
S49 S48 NOT S47
S48 S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41
S47 S45 NOT S46
S46 MH (human)
S45 S42 OR S43 OR S44
S44 TI (animal model*)
S43 MH (animal studies)
S42 MH animals+
S41 AB (cluster W3 RCT)
S40 MH (crossover design) OR MH (comparative studies)
S39 AB (control W5 group)
S38 PT (randomized controlled trial)
S37 MH (placebos)
S36 MH (sample size) AND AB (assigned OR allocated OR control)
S35 TI (trial)
S34 AB (random*)
S33 TI (randomised OR randomized)
S32 MH cluster sample
S31 MH pretest‐posttest design
S30 MH random assignment
S29 MH single‐blind studies
S28 MH double‐blind studies
S27 MH randomized controlled trials
S26 S20 AND S25
S25 S21 OR S22 OR S23 OR S24
S24 TI decubitus or AB decubitus
S23 TI ( bed sore* or bedsore* ) or AB ( bed sore* or bedsore* )
S22 TI ( pressure ulcer* or pressure sore* ) or AB ( pressure ulcer* or pressure sore* )
S21 (MH "Pressure Ulcer")
S20 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19
S19 TI net bed* or AB net bed*
S18 TI ( kinetic therapy or kinetic table* ) or AB ( kinetic therapy or kinetic table* )
S17 TI ( turn* bed* or tilt* bed* ) or AB ( turn* frame* or tilt* frame* )
S16 TI sheepskin OR AB sheepskin
S15 TI water suspension or AB water suspension
S14 TI air bag* or AB air bag*
S13 TI air suspension or AB air suspension
S12 TI alternat* pressure or AB alternat* pressure
S11 TI static air or AB static air
S10 TI constant N2 pressure or AB constant N2 pressure
S9 TI low pressure N2 support or AB low pressure N2 support
S8 TI low pressure N2 device* or AB low pressure N2 device*
S7 TI pressure alleviat* or AB pressure alleviat*
S6 TI pressure reduc* or AB pressure reduc*
S5 TI pressure relie* or AB pressure relie*
S4 TI ( overlay* or pad or pads or gel ) or AB ( overlay* or pad or pads or gel )
S3 TI ( foam or transfoam ) or AB ( foam or transfoam )
S2 TI mattress* or AB mattress*
S1 (MH "Beds and Mattresses+")
US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov)
bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air | Pressure Ulcer
bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air | Pressure Injury
bed OR mattress OR sheepskin OR gel OR pad OR foam OR pressure OR support OR air | Pressure Ulcers buttock
bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air | Ulcer, Pressure
bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air | Pressure Ulcer Stage 1
bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air | Pressure Ulcers Stage II
bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air | Pressure Ulcers Stage III
World Health Organization International Clinical Trials Registry Platform
pressure ulcer [title] and bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air [intervention]
pressure ulcer [condition] and bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air [intervention]
pressure injury [title] and bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air [intervention]
pressure injury [condition] and bed OR mattress OR sheepskin OR gel OR pad OR foam OR support OR air [intervention]
Appendix 3. Risk of bias
1 'Risk of bias' assessment in individually randomised controlled trials
1. Was the allocation sequence randomly generated?
Low risk of bias
The study authors describe a random component in the sequence generation process such as referring to a random number table, using a computer random number generator, coin tossing, shuffling cards or envelopes, throwing dice, drawing of lots.
High risk of bias
The study authors describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, for example, sequence generated by odd or even date of birth, sequence generated by some rule based on date (or day) of admission, sequence generated by some rule based on hospital or clinic record number.
Unclear
Insufficient information about the sequence generation process to permit judgement of low or high risk of bias.
2. Was the treatment allocation adequately concealed?
Low risk of bias
Participants and study authors enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based and pharmacy‐controlled randomisation); sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes.
High risk of bias
Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on using an open random allocation schedule (e.g. a list of random numbers), assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered), alternation or rotation, date of birth, case record number, any other explicitly unconcealed procedure.
Unclear
Insufficient information to permit judgement of low or high risk of bias. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement, for example if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed.
3. Blinding: was knowledge of the allocated interventions by participants and personnel adequately prevented during the study?
Low risk of bias
Any one of the following.
No blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding.
Blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken.
High risk of bias
Any one of the following.
No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding.
Blinding of key study participants and personnel attempted, but likely that the blinding could have been broken.
Either participants or some key study personnel were not blinded, and the non‐blinding of others likely to introduce bias.
Unclear
Any one of the following.
Insufficient information to permit judgement of low or high risk of bias.
The study did not address this outcome.
4. Blinding: was knowledge of the allocated interventions by outcome assessors adequately prevented during the study?
Low risk of bias
Any one of the following.
No blinding, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding.
Blinding of outcome assessment ensured, and unlikely that the blinding could have been broken.
High risk of bias
Any one of the following.
No blinding or incomplete blinding, and the outcome measurement is likely to be influenced by lack of blinding.
Blinding of outcome assessment attempted, but likely that the blinding could have been broken.
Unclear
Any one of the following.
Insufficient information to permit judgement of low or high risk of bias.
The study did not address this outcome.
5. Were incomplete outcome data adequately addressed?
Low risk of bias
Any one of the following.
No missing outcome data.
Reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias).
Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups.
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate.
For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size.
Missing data have been imputed using appropriate methods.
High risk of bias
Any one of the following.
Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups.
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate.
For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size.
‘As‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomisation.
Potentially inappropriate application of simple imputation.
Unclear
Any one of the following.
Insufficient reporting of attrition/exclusions to permit judgement of low or high risk of bias (e.g. number randomised not stated, no reasons for missing data provided).
The study did not address this outcome.
6. Are reports of the study free of suggestion of selective outcome reporting?
Low risk of bias
Any of the following.
The study protocol is available and all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way.
The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were prespecified (convincing text of this nature may be uncommon).
High risk of bias
Any one of the following.
Not all of the study’s prespecified primary outcomes have been reported.
One or more primary outcomes are reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not prespecified.
One or more reported primary outcomes were not prespecified (unless clear justification for their reporting is provided, such as an unexpected adverse effect).
One or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis.
The study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Unclear
Insufficient information to permit judgement of low or high risk of bias. It is likely that the majority of studies will fall into this category.
7. Other sources of potential bias
Low risk of bias
The study appears to be free of other sources of bias.
High risk of bias
There is at least one important risk of bias. For example, the study:
had a potential source of bias related to the specific study design used; or
has been claimed to have been fraudulent; or
had some other problem.
Unclear
There may be a risk of bias, but there is either:
insufficient information to assess whether an important risk of bias exists; or
insufficient rationale or evidence that an identified problem will introduce bias
2 'Risk of bias' assessment in cluster‐randomised controlled trials (cluster‐RCTs)
1. Recruitment bias
Recruitment bias (or identification bias) is the bias that occurs in cluster‐RCTs if the personnel recruiting participants know individuals’ allocation, even when the allocation of clusters has been concealed appropriately. The knowledge of the allocation of clusters may lead to bias because the individuals' recruitment in cluster trials is often behind the clusters' allocation to different interventions; and the knowledge of allocation can determine whether individuals are recruited selectively.
This bias can be judged through considering the following questions.
Were all the individual participants identified/recruited before randomisation of clusters?
Is it likely that selection of participants was affected by knowledge of the intervention?
Were there baseline imbalances that suggest differential identification or recruitment of individual participants between arms?
2. Baseline imbalance
Baseline imbalance between intervention groups can occur due to chance, problems with randomisation, or identification/recruitment bias. The issue of recruitment bias has been considered above.
In terms of study design, the risk of chance baseline imbalance can be reduced by the use of stratified or pair‐matched randomisation. Minimisation — an equivalent technique to randomisation — can be used to achieve better balance in cluster characteristics between intervention groups if there is a small number of clusters.
Concern about the influence of baseline imbalance can be reduced if studies report the baseline comparability of clusters, or statistical adjustment for baseline characteristics.
3. Loss of clusters
Similar to missing outcome data in individually randomised trials, bias can occur if clusters are completely lost from a cluster‐RCT, and are omitted from the analysis.
The amount of missing data, the reasons for missingness and the way of analysing data given the missingness should be considered in assessing the possibility of bias.
4. Incorrect analysis
Data analyses, which do not take the clustering into account, in cluster‐RCTs will be incorrect. Such analyses lead to a 'unit of analysis error' and over‐precise results (too small standard error) and too small P values. Though these analyses will not result in biased estimates of effect, they (if not correctly adjusted) will lead to too much weight allocated to cluster trials in a meta‐analysis.
Note that the issue of analysis may not lead to concern any more and will not be considered substantial if approximate methods are used by review authors to address clustering in data analysis.
5. Comparability with individually randomised trials
In the case that a meta‐analysis includes, for example, both cluster and individually randomised trials, potential differences in the intervention effects between different trial designs should be considered. This is because the 'contamination' of intervention effects may occur in cluster‐RCTs, which would lead to underestimates of effect. The contamination could be known as a 'herd effect': that is, within clusters, individuals' compliance with using an intervention may be enhanced, which in return affects the estimation of effect.
Appendix 4. Interventions used in the included studies
| Study ID | Specific alternating pressure (active) air surfaces | Specific comparators |
| Alternating pressure (active) air surfaces versus another type of alternating pressure (active) air surface | ||
| Ballard 1997 | Debut MR mattress (SSI Hill‐Rom), with a one‐in‐four alternating cycle lasting 30 minutes | Nimbus (HNE Huntleigh, with a 10‐minute cycle). |
| Demarre 2012 | Alternating air mattress with the multi‐stage inflation and deflation of air cells (Hill‐Rom ClinActiv, with 10‐ to 12‐minute cycle times) | Standard alternating air mattress (Hill‐Rom Alto mattress, with a 10‐minute cycle time) |
| Gray 2008 | Softform Premier Active Mattress (consisting of a foam mattress with a dynamic underlay having a 10‐minute cycle) | Standard alternating pressure air mattress |
| Grindley 1996 | Nimbus II mattress (Huntleigh Healthcare, with a 10‐minute cycle) | Pegasus Airwave (with a 7.5‐minute cycle) |
| Hampton 1997 | Cairwave Therapy System (Pegasus Airwave Ltd, with a 7.5‐minute cycle and a 30‐minute static mode) | Pegasus Airwave |
| Nixon 2006 | Alternating pressure replacement mattress (with a 7.5‐ to 30‐minute cycle time) | Alternating pressure overlay (with a 7.5– to 30‐minute cycle time) |
| Pring 1998 | Nimbus II (with a 10‐minute cycle) | Two comparators were used
|
| Rafter 2011 | Dyna‐Form Mercury Advance (with a 10‐minute cycle), consisting of the foam inside the alternating cells and being a static mattress combined with a dynamic alternating system | Softform Premier Active, consisting of the foam inside the alternating cells and being a static mattress combined with a dynamic alternating system. |
| Taylor 1999 | Pegasus Trinova (an integrated dynamic mattress and chair cushion that have a static mattress in combination with a dynamic alternating system, with a 7.5‐minute cycle) | Alternative dynamic mattress system (with a 10‐minute cycle) |
| Theaker 2005 | KCI TheraPulse bed (with low‐air‐loss feature), either applied at a 5‐ to 10‐minute alternating pressure cycle or continuously static | Hill‐Rom Duo mattress, either applied at a 5‐ to 10‐minute alternating pressure cycle or continuously static |
| Alternating pressure (active) air surfaces versus foam surfaces | ||
| Bliss 1995 | Large cell Ripple bed (with a 10‐minute interval of alternating pressure) | Three types of foam mattresses, each as an arm:
The characteristics (e.g. densities) of these foam were unspecified |
| Nixon 2019 | Alternating pressure air mattress (with a 7.5– to 30‐minute cycle time) | High‐specification foam mattress (high‐density foam, and/or viscoelastic (memory) foam) |
| Rosenthal 2003 | Low‐air‐loss suspension bed (TheraPulse bed) | A medium density polyurethane foam overlay |
| Sauvage 2017 | Alternating pressure air mattress (Axtair One, with a 6‐minute cycle) | Viscoelastic foam mattress (ALOVA mattress, high resilience foam with a density > 34 kg/m3 and an upper layer of viscoelastic foam of density > 75 kg/m3) |
| Stapleton 1986 | Large Cell Ripple (Talley) | Polyether foam pad, more details not specified |
| Whitney 1984 | Alternating pressure mattress (with a 3‐minute cycle) | A polyurethane convoluted foam pad, more details not specified |
| Alternating pressure (active) air surfaces versus reactive air surfaces | ||
| Beeckman 2019 | A range of alternating air pressure support surfaces (with a 3– to 30‐minute cycle time) | Static air support surfaces (Repose) |
| Cavicchioli 2007 | Alternating low pressure modality of Duo2 (Hill‐Rom) | Continuous low pressure modality of Duo2 |
| Finnegan 2008 | A specialised alternating therapy support surface (Nimbus 3 Professional, Huntleigh Healthcare LLC) | Air‐fluidised bed system (Clinitron, Hill‐Rom Inc) |
| Jiang 2014 | Dynamic air mattress (Sanma mattress manufacturing), more details not specified | Static air mattress (WAFFLE® static air mattress, EHOB) |
| Malbrain 2010 | NIMBUS 3 mattress (with a 10‐minute cycle) | ROHO dry floatation mattress overlay |
| Price 1999 | Dynamic flotation mattress NIMBUS II plus Alpha TranCell system | Repose |
| Sideranko 1992 | Alternating air mattress (Lapidus Airfloat System) | Static air mattresses (Gaymar Sof Care bed cushion) |
| Alternating pressure (active) air surfaces versus reactive water surfaces | ||
| Andersen 1982 | Alternating‐pressure air‐mattress, more details not specified | Water‐filled mattresses, more details not specified |
| Bliss 1995 | Large cell Ripple bed (with a 10‐minute interval of alternating pressure) | Ardo Watersoft |
| Sideranko 1992 | Alternating air mattress (Lapidus Airfloat System) | Water mattress (Lotus PXM 3666) |
| Alternating pressure (active) air surfaces versus reactive fibre surfaces | ||
| Bliss 1995 | Large cell Ripple bed (with a 10‐minute interval of alternating pressure) | Two types of fibre‐filled mattresses, each as an arm:
|
| Conine 1990 | Alternating pressure (active) air mattress, more details not specified | Silicore mattress overlay (consisting of siliconised hollow fibers) |
| Daechsel 1985 | Alternating pressure (active) air mattress, more details not specified | Silicore mattress overlay (consisting of siliconised hollow fibers) |
| Stapleton 1986 | Large cell Ripple (Talley) | Spenco pad |
| Alternating pressure (active) air surfaces in operating tables and subsequently on ward beds versus reactive gel surfaces used on operating tables followed by foam surfaces applied on ward beds | ||
| Aronovitch 1999 | MicroPulse System used during and after operations | Conventional management consisting of a gel pad (Action Pad) used in the operating room and a foam mattress or overlay used on the hospital bed |
| Russell 2000 | MicroPulse System used during and after operations | Conventional management consisting of a gel pad (Action Pad) used in the operating room and a foam mattress or overlay used on the hospital bed |
| Alternating pressure (active) air surfaces versus standard hospital surfaces | ||
| Andersen 1982 | Alternating‐pressure air‐mattress, more details not specified | Standard hospital mattress, more details not specified |
| Bliss 1967 | Large‐celled Ripple bed consisting of 14 large cells and with a cycle of four to five minutes | Standard hospital mattress, more details not specified |
| Laurent 1998 | Comparison (a): Nimbus used in ICU and standard mattress applied postoperatively (details of standard mattress not specified) Comparison (b): Nimbus in ICU and Tempur (CLP) used postoperatively |
Comparison (a): standard hospital mattresses used in both ICU and post‐operation (details of standard mattress not specified) Comparison (b): standard mattress in ICU and Tempur (CLP) postoperatively (details of standard mattress not specified) |
| Sanada 2003 | Two types of alternating pressure (active) air surfaces, both alternating pressure at 5‐minute intervals, each as an arm:
|
Standard hospital mattress made of polyester (Paracare®) |
Appendix 5. Results of studies that used undefined surfaces
| Outcomes | Results |
| Comparison: Alternating pressure (active) air surfaces compared with undefined 'standard hospital surfaces' | |
| Proportion of participants developing a new pressure ulcer (median follow‐up duration 15 days, minimum 10 days, maximum 16 days or unspecified) | All four studies (830 participants) reported this outcome and consistently showed that alternating pressure (active) air surfaces could reduce the proportion of participants developing a new pressure ulcer compared with the undefined 'standard hospital surfaces' (Andersen 1982; Bliss 1967; Laurent 1998; Sanada 2003). |
Appendix 6. Sensitivity analyses
| Sensitivity analysis | Studies | Participants | Statistical Method | Effect Estimate |
| Comparison: Alternating pressure (active) air surfaces compared with foam surfaces | ||||
| Outcome: Proportion of participants developing a new pressure ulcer | ||||
|
||||
| Alternating pressure (active) air surfaces compared with foam surfaces | 3 | 2171 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.34, 1.17] |
| Alternating pressure (active) low‐air‐loss surfaces compared with foam surfaces | 1 | 76 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
|
4 | 2247 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.55, 0.93] |
|
2 | Hazard Ratio (IV, Random, 95% CI) | 0.41 [0.10, 1.64] | |
|
1 | 2029 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.57, 1.05] |
| Comparison: Alternating pressure (active) air surfaces compared with reactive air surfaces | ||||
| Outcome: Proportion of participants developing a new pressure ulcer | ||||
|
6 | 1611 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [0.90, 2.89] |
|
6 | 1648 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [1.00, 2.97] |
|
1 | 308 | Hazard Ratio (IV, Random, 95% CI) | 2.25 [1.05, 4.83] |
| Comparison: Alternating pressure (active) air surfaces compared with reactive water surfaces | ||||
| Outcome: Proportion of participants developing a new pressure ulcer | ||||
|
2 | 358 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.53, 2.78] |
| Comparison: Alternating pressure (active) air surfaces compared with reactive fibre surfaces | ||||
| Outcome: Proportion of participants developing a new pressure ulcer | ||||
|
3 | 246 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.72, 1.20] |
|
3 | 285 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.68, 1.20] |
| Comparison: Alternating pressure (active) air surfaces in operating tables and subsequently on ward beds compared with reactive gel surfaces used on operating tables followed by foam surfaces applied on ward beds | ||||
| Outcome: Proportion of participants developing a new pressure ulcer | ||||
|
2 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.06, 0.72] |
Data and analyses
Comparison 1. Alternating pressure (active) air surfaces compared with reactive foam surfaces.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Proportion of participants developing a new pressure ulcer | 4 | 2247 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.34, 1.17] |
| 1.2 Time to pressure ulcer development | 2 | Hazard Ratio (IV, Random, 95% CI) | 0.41 [0.10, 1.64] | |
| 1.3 Health‐related quality of life | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.3.1 90‐day EQ‐5D‐5L | 1 | 267 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐0.05, 0.05] |
| 1.3.2 90‐day PU‐QoL‐UI | 1 | 233 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐0.03, 0.03] |
Comparison 2. Alternating pressure (active) air surfaces compared with reactive air surfaces.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Proportion of participants developing a new pressure ulcer | 6 | 1648 | Risk Ratio (M‐H, Random, 95% CI) | 1.61 [0.90, 2.88] |
| 2.2 Time to pressure ulcer development | 1 | Hazard Ratio (IV, Random, 95% CI) | 2.25 [1.05, 4.83] |
Comparison 3. Alternating pressure (active) air surfaces compared with reactive water surfaces.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Proportion of participants developing a new pressure ulcer | 2 | 358 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.52, 2.83] |
Comparison 4. Alternating pressure (active) air surfaces compared with reactive fibre surfaces.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Proportion of participants developing a new pressure ulcer | 3 | 285 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.68, 1.19] |
Comparison 5. Alternating pressure (active) air surfaces on operating tables and subsequently on ward beds compared with reactive gel surfaces on operating tables followed by foam surfaces on ward beds.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Proportion of participants developing a new pressure ulcer | 2 | 415 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.06, 0.76] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andersen 1982.
| Study characteristics | ||
| Methods |
Study objective: to observe "the development of pressure sores in risk‐patients nursed on these mattresses [water‐mattresses and alternating pressure air‐mattresses and compare] the results with a similar group of patients nursed on ordinary hospital mattresses" Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 10 days Number of arms: 3 Single centre or multi‐site: single centre Study start date and end date: not described Setting: hospital |
|
| Participants |
Baseline characteristics Inclusion criteria: patients with acute conditions and a risk score of 2 or more (i.e. at risk) Exclusion criteria: "those who already had pressure sores" Sex (M:F): 60:101 in control; 73:93 in air; 73:82 in water Age (years): distribution of participants' ages described Baseline skin status: all at risk according to the risk score used by the authors; free of ulcers Group difference: no difference between groups according to age, sex, body weight or risk score Total number of participants: not described; n = 482 available Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating‐pressure air‐mattress
Water mattress
Ordinary hospital mattresses
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials: 1. "opinions on mattresses" described as "the acceptability of the mattress" and rated as the numbers of staff satisfied and the numbers of patients satisfied with different mattresses. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Six hundred patients at risk for pressure sores were randomised in either a control group or one of two experimental groups ... They were allotted to one of the three groups ..." Comment: method of randomisation was not reported |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk |
Outcome group: primary outcome (i.e. the only outcome) Comment: no information provided |
| Blinding of outcome assessment (detection bias) All outcomes | High risk |
Outcome group: primary outcome (i.e. the only outcome) Quote: "One of us [note: study's authors] assessed the condition of the skin ..." Comment: appears to have no blinding, and the pressure ulcer incidence outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk |
Outcome group: primary outcome (i.e. the only outcome) Quote: "Six hundred patients at risk for pressure sores were randomised ..." Quote: "Among the 600 risk‐patients ... 118 dropped out during the first 24 hours before the first dermatologic inspection. This did not impair randomization." Quote: "The groups remained comparable throughout the 10‐day study period" Comment: unclear risk of bias was judged because authors claimed that randomisation was not impaired though the proportion of missing data was high and no reasons for missing data were provided. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Aronovitch 1999.
| Study characteristics | ||
| Methods |
Study objective: "... to determine the efficacy and safety of the experimental system (study group), in comparison with conventional management (control group), for the prevention of pressure ulcers in the operative and postoperative settings" Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 7 days Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: March 1997 to February 1998 Setting: tertiary care facility (operating theatre and wards) |
|
| Participants |
Baseline characteristics Inclusion criteria: "18 years of age or older undergoing a scheduled surgery with general anesthesia for at least 4 hours (actual operative time of 3 hours or more)" Exclusion criteria: patients "participated in a clinical trial within 30 days of the baseline visit ... or had a pressure ulcer at the baseline visit" Sex (M:F): 79:31 in experimental system; 77:27 in conventional management Age (years): mean 63.5 (SD 11.9) in experimental system; 64.7 (11.8) in conventional management Baseline skin status: Modified Knoll scale score ‐ on average less than 4 (range 0 to 13; a score of 12 or higher = at risk of pressure ulcer development) in both groups; and those with pressure ulcers at baseline excluded Group difference: no difference Total number of participants: 217 patients Unit of analysis: individuals Unit of randomisation (per patient): groups of individuals by weeks |
|
| Interventions |
Intervention characteristics Experimental management
Conventional management
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials: No further outcome |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomization was performed by week rather than by patient to decrease protocol error." Comment: unclear risk of bias because the methods were not clear |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk |
Outcome group: primary outcome Comment: no information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk |
Outcome group: primary outcome Quote: "Patients were examined following surgery and daily for pressure ulcers, including number, stage (I‐IV), size (area), location, and appearance." Comment: insufficient information to permit judgement of low or high risk of bias. |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "Seven patients (8.75%) in the control group developed a total of 11 pressure ulcers ..." Comment: high risk of bias because 7 (8.75%) in control group implied 80 of 105 individuals were considered in data analysis, meaning a large proportion of missing data in the control group alone. However, the number of available cases in experimental group is not given. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Ballard 1997.
| Study characteristics | ||
| Methods |
Study objective: to evaluate two alternating‐pressure mattresses for patient comfort and quality of sleep Study design: pilot randomised trial Study grouping: cross‐over design Duration of follow‐up: 3 days for each arm (so 6‐day trial duration) Number of arms: 2 Single centre or multi‐site: 2 centres Study start date and end date: not described Setting: 2 UK nursing homes |
|
| Participants |
Baseline characteristics Inclusion criteria: able and willing to give their informed consent; able to understand and use standardised visual rating scales and questionnaires; without any evidence of existing pressure damage Exclusion criteria: those who were confused; acutely or terminally ill; regularly incontinent of urine or faeces; had any sensory/neurological deficiency; weighed over 150 kg; involved in a simultaneous study; unable to complete the questionnaire or visual analogue scale Sex (M:F): overall 5:5 Age (years): overall mean 84 (range 75 to 90) Baseline skin status: no risk Group difference: not given Total number of participants: n = 10 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Debut MR mattress
Nimbus
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The recruits were randomised to sleep for three nights on either the Debut MR or the Nimbus" Comment: unclear risk of bias because the sequence generation process is not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: high risk of bias because during the study, one withdrawal due to incompatibility with allocated mattress and another person recruited for final analysis |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Beeckman 2019.
| Study characteristics | ||
| Methods |
Study objective: to compare the effectiveness and cost of static air support surfaces versus alternating air pressure support surfaces in a nursing home population at high risk for pressure ulcers Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 14 days Number of arms: 2 Single centre or multi‐site: multi‐site Study start date and end date: April 2017 to May 2018 Setting: nursing home |
|
| Participants |
Baseline characteristics Inclusion criteria: (1) high risk of developing pressure ulcer (Braden score 12 and/or Braden subscale score for mobility 2) and/or pressure ulcer category 1; (2) being bed bound (> 8 hours in bed) and/or chair bound (> 8 hours sitting in a chair); (3) aged > 65 years; and (4) use of an alternating air pressure mattress Exclusion criteria: (1) nursing home residents with a pressure ulcer category II–IV upon admission; (2) those with an expected length of stay < 2 weeks; (3) those who received end‐of‐life care; or (4) those with medical contraindications for the use of static air support devices Sex (M:F): 71:237 overall; 39:115 in static air support surfaces; 32:122 in alternating air pressure surfaces Age (years): mean 87 (SD 7.6) overall; 86.9 (7.9) in static air support surfaces; 86.8 (7.3) in alternating air pressure surfaces Baseline skin status: mean Braden score 13 (SD 2.2) overall; all at risk according to the risk score used by the authors Group difference: no difference between groups Total number of participants: n = 308 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Static air support surfaces
Alternating air pressure support surfaces
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The random allocation sequence was based on a computer‐generated list of random numbers using an online tool (www.randomization.com)." Comment: low risk of bias because of the use of a proper randomisation method. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "When the participants met the inclusion criteria and an informed consent was obtained, they received an allocation number (first available number on the computer‐generated list)." Quote: "Subsequently, a random allocation of each eligible participant was performed based on a computer‐generated list of random numbers." Comment: unclear risk of bias because the process of allocation is not clear for judging if concealment was properly performed and it is unclear who performed allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Outcome group: all outcomes Quote: "The study was not blinded due to the obvious visible difference between the support surfaces (e.g. external control unit)." Comment: high risk of bias because of the understandable challenge of performing blinding. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk |
Outcome group: all outcomes Quote: "The study was not blinded due to the obvious visible difference between the support surfaces (e.g. external control unit). Both support surface types were presented to ward nurses ..." Quote: "During the follow‐up period (days 1–14), the ward nurses collected all data" Quote: "Researchers performed independent and unannounced skin assessments and technical controls weekly" Comment: high risk of bias because of the understandable challenge of performing blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "An intention‐to‐treat analysis was performed." Comment: low risk of bias. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is available and it is clear that the published reports include all outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Bliss 1967.
| Study characteristics | ||
| Methods |
Study objective: to assess different mattresses for preventing pressure sores Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: treatment for 14 days and follow‐up assessments on the 16th day Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: geriatric unit |
|
| Participants |
Baseline characteristics Inclusion criteria: all new patients with a Norton score of 7 or more, and all inpatients with a score 7 or more and still rising, provided they had no, or only superficial, trunk sores at the time Exclusion criteria: patients with severe sores of the trunk Sex (M:F): overall 27:56; large‐celled ripple bed 10:32; control 17:24 Age (years): overall mean 81.2; large‐celled ripple bed 80.4; control 82.1 Baseline skin status: mean baseline Norton score 10.5; free of existing severe ulcers (43 with superficial sore) Group difference: no difference in variables except for sex distributions Total number of participants: n = 83 (70 analysed) Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Large‐celled ripple bed
Ordinary hospital mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "In order to ensure that the distribution of subjects among the various regimens was as random as possible the experimental and control treatments were arranged in a rota. As patients were admitted to the trial they were allocated to the next treatment on the rota in order" Comment: unclear risk of bias because the sequence generation process is not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Outcome group: ulcer incidence Comment: no information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome group: ulcer incidence Quote: "The record forms were all evaluated in a single session by one observer, each being masked in such a way that it was not possible to know to which patient or to which experimental regimen it referred" Comment: low risk of bias because the blinding of assessment is stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome group: ulcer incidence Comment: unclear risk of bias because 7 of 42 in ripple bed and 6 of 41 in control group were excluded from analysis |
| Selective reporting (reporting bias) | High risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. However, incidence outcome data among those with existing ulcers are not available. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias |
Bliss 1995.
| Study characteristics | ||
| Methods |
Study objective: to identify inexpensive and, if possible, non‐mechanical constant low pressure overlays effective for patients at long‐term risk in continuing‐care wards for elderly people. Study design: randomised controlled trial (a poorly designed multi‐arm multi‐stage trial, with re‐randomisation) Study grouping: parallel group Duration of follow‐up: not given; assessment with a mean of 17.7 days Number of arms: 7 (The trial had a Vaperm as control arm but its participants were not randomised. Vaperm data were not extracted for this review.) Single centre or multi‐site: not specified Study start date and end date: not described Setting: hospital |
|
| Participants |
Baseline characteristics Inclusion criteria: patients liable to pressure sores; included those who already had superficial breaks in the skin of the pressure areas Exclusion criteria: patients with superficial sores > 5 cm and discoloured areas > 2 cm diameter Sex (M:F): overall 62:296 (treatment sessions rather than individuals) Age (years): mean 84.4 (range 67 to 97) large‐celled Ripple bed (n = 71 treatment sessions of 34 patients); 85.2 (67 to 97) Preventix (n = 25 sessions of 20 patients); 85.6 (68 to 98) Groove (n = 66 sessions of 36 patients); 86.1 (68 to 98) Modular Propad (n = 60 sessions of 39 patients); 84.4 (68 to 93) Ardo Watersoft (n = 32 sessions of 22 patients); 85.6 (68 to 94) Spenco (n = 63 sessions of 35 patients); 84.3 (67 to 97) Surgicgoods Hollowcore (n = 41 sessions of 30 patients). Baseline skin status: not given; allowed inclusion of those with superficial ulcers Group difference: not given Total number of participants: n = 358 sessions of 216 patients Unit of analysis: treatment sessions of patients Unit of randomisation (per patient): treatment sessions of patients |
|
| Interventions |
Intervention characteristics Groove
Spenco
Propad
Preventix
Surgicgoods
Watersoft
Large‐celled Ripple bed
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the patient was randomly allocated to an experimental overlay by the researcher writing the names of all those available at the time on slips of paper which were folded and offered to the nurse to choose one blind" Comment: low risk of bias because drawing of lots is applied to generate random sequence. |
| Allocation concealment (selection bias) | High risk | Quote: "the patient was randomly allocated to an experimental overlay by the researcher writing the names of all those available at the time on slips of paper which were folded and offered to the nurse to choose one blind. The designated overlay was then placed on the bed" Comment: high risk of bias because it appears difficult to conceal the allocation process as the authors described. The nurse would have knowledge of which overlays were available at the time of consent. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no information provided |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Comment: high risk of bias because some individuals may be repeatedly observed and included in analysis (i.e. correlation issue in analysis). For example, Bliss stated "there were no written criteria determining the decision to stop a trial [i.e. using an overlay as the experimental intervention]. This depended mainly on these experienced nurses' unwillingness to allow it to continue because of enlargement of an existing sore, a new blister, discolouration, oedema ... Patients who developed pressure damage between assessments might also be taken off their overlay ... if they later improved ... they were re‐randomized for another trial period [i.e. comparisons of new overlays]" Additionally, overlays were observed for unequal periods of time. Treatments were discontinued or introduced without pre‐specified stopping rules. Some comparisons are not parallel. |
Cavicchioli 2007.
| Study characteristics | ||
| Methods |
Study objective: to determine whether alternating low pressure or continuous low pressure is most effective in reducing the incidence of pressure ulcers in high risk patients Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 2 weeks Number of arms: 2 Single centre or multi‐site: multi‐site Study start date and end date: March 2004 to November 2006 Setting: acute, post‐acute and long‐term care settings of 3 hospitals |
|
| Participants |
Baseline characteristics Inclusion criteria: those admitted to the unit or deemed "at risk" of pressure ulceration as defined by the Braden Pressure Ulcer Risk Assessment Scale (a total Braden score of ≤ 17 and mobility and activity sub‐scores of ≤ 3 respectively); their admission was expected to last at least 2 weeks and they had up to one grade I pressure ulcer Exclusion criteria: not at risk (Braden ≥ 17 and activity or mobility sub‐scales ≥ 3, respectively) Sex (M:F): 20:49 in alternating low pressure; 20:51 in continuous low pressure Age (years): mean 77 in alternating low pressure; 78 in continuous low pressure Baseline skin status: mean 11.4 (range 7 to 16) in alternating low pressure; 11.9 (6 to 17) in continuous low pressure Group difference: no difference Total number of participants: 170 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating low pressure modality of Duo2 (Hill‐Rom)
Continuous low pressure modality of Duo2 (Hill‐Rom)
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients in the treatment group were randomised to receive either continuous or alternating low pressure on the high‐tech mattress" Comment: the method of randomisation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk |
Outcome group: primary outcome Quote: "... independently from the blinded randomised treatment group (who received the Duo2 high‐tech mattress)." Comment: low risk of bias because blinding method was implemented. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk |
Outcome group: primary outcome Quote: "As there is no visible difference between these two modes, the external observer was blinded as to which one was in use. The external observers assessed all study patients' ... presence (or absence) and grade of both existing and new pressure ulcers" Comment: low risk of bias because outcome assessment was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
Outcome group: primary outcome Comment: high risk of bias because of high proportions of dropouts in both groups and probably using incorrect analysis methods to address missing data. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Conine 1990.
| Study characteristics | ||
| Methods |
Study objective: to determine the efficacy of the alternating air mattress overlay and the silicone mattress overlay in preventing pressure ulcers Study design: sequential randomised controlled trial Study grouping: parallel group Duration of follow‐up: 3 months Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: study took place between 1985 and 1988 Setting: extended care facility for neurological conditions |
|
| Participants |
Baseline characteristics Inclusion criteria: patients in extended care facility for neurological conditions, 18 to 55 years old, with no evidence of skin breakdown for at least 2 weeks prior to the study, and who were at high risk of developing ulcers according to the Norton's Scale (i.e. less than the score of 14) Exclusion criteria: the status of high risk changed during the study Sex (M:F): 31:41 in alternating air mattress; 29:47 in Silicore Age (years): mean 38.8 (SD 13.0) in alternating air mattress; 35.6 (13.0) in Silicore Baseline skin status: mean Norton score 12.9 (SD 2.1) in alternating air mattress; 12.4 (2.3) in Silicore Group difference: no difference Total number of participants: 187 randomised; 148 analysed Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating air mattress
Silicore mattress overlay
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A modified sequential clinical trial ... was used to assign subjects randomly to one of the two mattresses in groups of 20" Comment: the method of randomisation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk |
Outcome group: primary outcome Comment: no information provided but understandably difficult to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk |
Outcome group: primary outcome Quote: "The research assistant ... was responsible for the assessment of all outcome measures. She ... was not informed about the study" Comment: low risk of bias because blinding is likely applied. |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "Thirty‐nine subjects did not complete the trial for reasons shown in Table 3" Comment: high risk of bias because over 20% of 187 randomised individuals missed and most of the dropouts were due to discomfort. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Daechsel 1985.
| Study characteristics | ||
| Methods |
Study objective: to assess 2 commonly used special mattresses in a randomised trial involving adult non‐geriatric chronic neurologic patients Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 3 months Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: long‐term care hospital for chronic neurologic conditions |
|
| Participants |
Baseline characteristics Inclusion criteria: consenting patients in a long‐term care hospital for chronic neurologic conditions ... a) between 19 and 60 years of age, b) free of any evidence of skin breakdown two weeks prior to the study, and c) considered to be at high risk of developing decubitus ulcers (DU) based on assessments conducted by the ward team [Norton scale score of 14 or less; and clinical judgement] Exclusion criteria: Sex (M:F): 10:6 in alternating air mattress; 6:10 in Silicore mattress Age (years): mean 42.6 (SD 13.7) in alternating air mattress; 38.5 (13.82) in Silicore mattress Baseline skin status: mean Norton score 13.35 (SD 1.86) in alternating air mattress; 12.97 (2.28) in Silicore mattress Group difference: no difference Total number of participants: 32 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating air mattress
Silicore mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All were randomly assigned to one of the two types of mattresses" Comment: the method of randomisation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk |
Outcome group: primary outcome Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "one of the investigators (DD) conducted weekly skin checks of the subjects" Comment: high risk of bias for pressure ulcer incidence outcome because it is unlikely that the investigator who assessed skin conditions was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk |
Outcome group: primary outcome Quote: "Thirty‐two patients met the criteria for this study ... all admitted to the trial and completed it" Comment: no missing data. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Demarre 2012.
| Study characteristics | ||
| Methods |
Study objective: to compare the effectiveness of an alternating low pressure air mattress with a standard single‐stage inflation and deflation cycle of the air cells with an alternating low pressure air mattress with multi‐stage inflation and deflation cycle of the air cells Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 14 days Number of arms: 2 Single centre or multi‐site: multi‐site Study start date and end date: December 2007 to January 2010 Setting: 25 wards in 5 hospitals in Belgium. |
|
| Participants |
Baseline characteristics Inclusion criteria: patients at risk for pressure ulcer development according to the Braden scale (less than 17), including those with non‐blanchable erythema Exclusion criteria: patients with a pressure ulcer Grade II to IV on admission, the expected admission time < 3 days; aged < 18 years; with a "do not resuscitate code" specifying ending all therapeutic interventions, weight < 30 kg or > 160 kg, and informed consent not obtained Sex (M:F): overall 241 (39.4%): 369 (60.6%); 111:187 in multi‐stage group; 130: 182 in single‐stage group Age (years): overall mean 76.3 (SD 14.0); 76.15 (14.82) in multi‐stage alternating air mattress; 76.50 (13.20) in single‐stage alternating air mattress Baseline skin status: overall median Braden score 14.0 (interquartile range (IQR) 12.0 to 15.0); 14.0 (12 to 15) in multi‐stage; 14.0 (12 to 15) in single‐stage Group difference: no difference Total number of participants: 610 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Multi‐stage alternating air mattress
Single‐stage alternating air mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Included patients were randomly assigned to the study groups using simple randomisation. The random allocation sequence was based on a computer‐generated list of random numbers" Comment: low risk of bias because of the use of a proper random sequence generation method. |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were enrolled by the ward nurses ... assigned to one of the mattresses by contacting the researcher. The ward nurse received a number of the type of allocated mattress" Comment: low risk of bias because it is likely that allocation sequence was concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Outcome group: All outcomes Quote: "Both mattresses were covered with an identical mattress cover ..." Quote: "The study could not be blinded, because of the visible differences of the external control unit of the study mattresses" Comment: high risk of bias because it is unlikely that participants were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk |
Outcome group: primary outcome Quote: "Daily skin assessment was performed by the ward nurses ... in each patient, in the morning" Quote: "No information was provided to the ward nurses about the differences between the experimental and control study device" Quote: "The lack of a blinded outcome assessment is a first limitation ... the nurses were not informed about the differences in the mattresses in order to minimize the effect of non‐blinding" Comment: unclear risk of bias because efforts were made to reduce bias. Outcome group: comfort outcome Comment: high risk of bias because it is unlikely that patients who reported this outcome were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome group: all outcomes Comment: low risk of bias because ITT analysis was undertaken. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Finnegan 2008.
| Study characteristics | ||
| Methods |
Study objective: to compare the effectiveness of a specialised alternating air pressure mattress replacement system and an air‐fluidised integrated bed in the management of post‐operative flap patients Study design: pilot randomised controlled trial Study grouping: parallel group Duration of follow‐up: mean length of stage 8.0 days (range 0 to 21) Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: tertiary referral centre |
|
| Participants |
Baseline characteristics Inclusion criteria: 18 years or older who were admitted for reconstructive surgery to repair a tissue deficit (full‐thickness pressure ulcer involving muscle, fascia and, in some cases, bone) in the sacral‐coccygeal, trochanteric or ischial region. Exclusion criteria: unlikely or unwilling to comply with the treatment protocol, which included a minimum of 7 days bed rest within the surgical unit, or unable to consent. Sex (M:F): overall 21:12; 7:8 in alternating therapy; 14:4 in air‐fluidised bed Age (years): mean 56 (range 20 to 80); 62 in alternating therapy; 50 in air‐fluidised bed Baseline skin status: severe full‐thickness pressure ulcers Group difference: not described Total number of participants: 40 randomised, 33 analysed Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating therapy
Air‐fluidised bed
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "allocation was determined by using web‐based random‐number software" Comment: low risk of bias due to the use of a proper randomisation method. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Groups were concealed in sealed envelopes" Comment: unclear risk of bias because a proper concealment method is not specified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk |
Outcome group: all outcomes Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "Tissue integrity on discharge was not blinded and determined by the surgical team responsible for this pilot phase." Comment: high risk of bias because no blinding was undertaken. Outcome group: comfort outcome Comment: unclear risk of bias because it is not specified if patients who reported comfort data were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome group: all outcomes. Quote: "four subjects in Group A and three subjects in Group B did not receive the allocated intervention (Fig. 2) and were not included in the follow‐up" Comment: unclear risk of bias because a fair proportion of subjects lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Gray 2008.
| Study characteristics | ||
| Methods |
Study objective: to determine the effect of using the Softform Premier Active™ Mattress versus a standard air mattress on pressure ulcer incidence in 2 acute care of the elderly wards Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: not given (claimed this is a 6 month study) Number of arms: 2 Single centre or multi‐site: 2 acute wards Study start date and end date: not described Setting: acute care of the elderly wards |
|
| Participants |
Baseline characteristics Inclusion criteria: patients considered to be at high risk of pressure ulcer development Exclusion criteria: not given Sex (M:F): not given Age (years): mean 82.4 in Softform Premier Active mattress; 84.0 in standard air mattress Baseline skin status: mean Waterlow risk score 22.2 (range 17 to 29) in Softform Premier Active mattress; 21.6 (range 17 to 29) in standard air mattress Group difference: no difference Total number of participants: n = 100 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Softform Premier Active Mattress
Standard air mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients considered to be at high risk of pressure ulcer development were randomly allocated to a Softform Premier Active or standard air mattress" Comment: unclear risk of bias because the sequence generation process is not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome group: ulcer incidence Quote: "Any pressure ulcers that developed during the study period were graded by a member of the tissue viability department." Comment: unclear risk of bias because blinding of outcome assessment is not described. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome group: ulcer incidence Comment: unclear risk of bias because the numbers randomised to arms are not detailed. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Grindley 1996.
| Study characteristics | ||
| Methods |
Study objective: to compare the performance of the Nimbus II and the Pegasus Airwave mattresses in a hospice setting Study design: randomised controlled trial Study grouping: cross‐over design Duration of follow‐up: 3 days (the first stage of the cross‐over trial) Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: hospice |
|
| Participants |
Baseline characteristics Inclusion criteria: patients with existing pressure sores grade 2* or above or patients without existing pressure sores but at high or very high risk of developing pressure sores (Waterlow risk assessment score of 15 or above); minimum anticipated hospice stay of 7 days; patients spending more than 6 hours in a 24‐hour period on the mattress; patients must give consent Exclusion criteria: mental frailty; existing inpatients already on either of the study mattresses; gross obesity (greater than 30 stones, 190 kg); extreme emaciation (less than 6 stones, 38 kg); unstable spinal metastases Sex (M:F): overall 8:12 Age (years): overall mean 69.05 (SD 14.32) Baseline skin status: overall median Waterlow 22.5 (range 15 to 30) mean 22.65 (SD 4.43); 8 with existing ulcers Group difference: not given Total number of participants: n = 20 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Nimbus II mattress
Pegasus Airwave
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | Challenging to contact the study authors to request data at the first stage of this cross‐over trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed using a random numbers table" Comment: low risk of bias because the sequence generation process is proper. |
| Allocation concealment (selection bias) | Low risk | Quote: "To avoid bias, the order in which the mattresses were allocated was randomised and selected by the investigator from sealed opaque envelopes in sequential order." Comment: low risk of bias because it is likely to conceal allocation properly. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcome group: comfort Quote: "mattress preference questionnaire completed by 16 patients" Comment: unclear risk of bias because no information given on which group the missing are from. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Hampton 1997.
| Study characteristics | ||
| Methods |
Study objective: not described Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 4 months Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: hospitals (Eastbourne NHS Trust) |
|
| Participants |
Baseline characteristics Inclusion criteria: not described Exclusion criteria: not described Sex (M:F): not described Age (years): mean 75 in Cairwave Therapy; not described for Pegasus Baseline skin status: 27 of 36 in Cairwave Therapy at high risk; not described for Pegasus Group difference: not described Total number of participants: 36 in Cairwave Therapy; not described for Pegasus Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Cairwave Therapy System
Pegasus Airwave mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Over a 4‐month period, 36 patients were allocated to rhe Cairwave Therapy System during the randomised controlled trial" Comment: the method of randomisation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Over a 4‐month period, 36 patients were allocated to rhe Cairwave Therapy System during the randomised controlled trial" Comment: the method of concealing allocation was not described. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk |
Outcome group: primary outcome Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk |
Outcome group: primary outcome Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk |
Outcome group: primary outcome Comment: no information provided. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no information provided. |
| Other bias | Unclear risk | Comment: no information provided. |
Jiang 2014.
| Study characteristics | ||
| Methods |
Study objective: to investigate the efficacy of static low‐air‐loss mattress (static LALM) and power pressure air mattress (PPAM) in prevention of pressure ulcers Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 5 days after surgery Number of arms: 2 Single centre or multi‐site: multi‐site Study start date and end date: not described Setting: hospitals |
|
| Participants |
Baseline characteristics Inclusion criteria: age ≥ 18 years, male or female with Braden score ≤ 16 points, general anaesthesia for surgery with operating time ≥ 120 min, admitted to the intensive care unit (ICU) or surgical wards after surgery, clear consciousness, able to express their feelings correctly, had contraindications for using air mattress (doctor’s orders: lying on hard‐bed or flat‐bed), completed informed consent and related information Exclusion criteria: refused to participate in research; in critical condition and repositioning limited by doctor’s orders; using ice blanket; shed from intervention less than 72 hours; unable to determine the efficacy; incomplete data on the efficacy; or safety judgment. Sex (M:F): overall 621:453 Age (years): overall mean 57.94 (SD 15.54) years (range 18 to 88) Baseline skin status: overall mean Braden scores 13.15 (SD 2.25) (range 6 to 17) Group difference: no difference Total number of participants: n = 1074 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Static air mattress
Dynamic air mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We used a random number table to randomize and parallel control design" Comment: low risk of bias because the sequence generation process is proper. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome group: ulcer incidence Comment: low risk of bias because intention‐to‐treat (ITT) analysis performed. Outcome group: comfort Comment: unclear risk of bias because the rates of missing data in both groups are between 10% to 20%. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Laurent 1998.
| Study characteristics | ||
| Methods |
Study objective: to assess the effectiveness of 3 prevention strategies and compare them to the standard mattress Study design: randomised controlled trial Study grouping: factorial design Duration of follow‐up: mean length of stay 15.04 (SD 7.10) Number of arms: 4 Single centre or multi‐site: single centre Study start date and end date: not described Setting: hospital |
|
| Participants |
Baseline characteristics Inclusion criteria: adults over 15 years of age, admitted for major cardiovascular surgery, hospital stay likely to be at least 5 days, with a period on the intensive care unit (ICU) Exclusion criteria: not reported Sex (M:F): 214:98 across 4 groups Age (years): mean 64.0 (SD 11.88) across 4 groups Baseline skin status: not described Group difference: no difference Total number of participants: n = 312 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Standard group
Alternating mattress in ICU
Constant low‐pressure mattress in postoperative hospitalisation
Both mattresses
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomised by blocks" Comment: unclear risk of bias because the randomisation method was not stated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "Given the kind of material tested, blinding was not possible" Comment: high risk of bias as the above statement suggests. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "Given the kind of material tested, blinding was not possible" Comment: high risk of bias as the above statement suggests. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk |
Outcome group: primary outcome Comment: no attrition identified. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Comment: the study appears not to consider the interaction between the effects of the different interventions that results from the factorial design used. |
Malbrain 2010.
| Study characteristics | ||
| Methods |
Study objective: to compare pressure ulcer outcomes in medical intensive care unit (ICU) patients nursed on either a reactive mattress overlay (ROHO®, ROHO Inc, Belleville, IL, USA) or an active alternating pressure mattress (NIMBUS®3, ArjoHuntleigh, Luton Bedfordshire, UK) Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: not specified; mean study duration reported 12.2 days (SD 5.5) in ROHO and 15 (14) in NIMBUS 3 Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: medical ICU of a hospital |
|
| Participants |
Baseline characteristics Inclusion criteria: patients admitted to the ICU with a high pressure ulcer risk (Norton score ≤ 8) and requiring mechanical ventilation for an estimated duration of at least 5 days either (a) with intact skin or (b) with pressure ulcers on admission Exclusion criteria: refused to consent to the study; either of 2 mattresses unavailable for patients admitted Sex (M:F): 8:8 across groups; 5:3 in ROHO; 3:5 in NIMBUS 3 Age (years): mean 64.7 (SD 15.6) across groups; 71.6 (11.9) in ROHO overlay; 56.9 (16.3) in NIMBUS 3 mattress Baseline skin status: mean Norton score 7.2 (SD 0.7) across groups; 7 (0) in ROHO and 7.4 (1.1) in NIMBUS 3 Group difference: different age distributions between groups Total number of participants: n = 16 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics ROHO dry floatation mattress overlay
NIMBUS 3 mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation of patients to products was performed blinded by the insertion of equivalent numbers of labels written with 'active' or 'reactive' placed in identical sealed envelopes that were shuffled and placed in a box and drawn in sequence" Comment: low risk of bias because a simple randomisation was applied. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomisation of patients to products was performed blinded by the insertion of equivalent numbers of labels written with 'active' or 'reactive' placed in identical sealed envelopes that were shuffled and placed in a box and drawn in sequence. When a patient was admitted who fulfilled the inclusion criteria the next envelope was opened by a ward nurse and the patient was assigned to the mattress on the label" Comment: unclear risk of bias because it is unclear if the envelopes were opaque. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk |
Outcome group: primary outcome Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk |
Outcome group: primary outcome Quote: "skin overlying bony prominences was thoroughly inspected in appropriate light by the ICU nurse; the outcome was documented ... any PU’s were assessed independently by the study nurse and study doctor, using ... pressure ulcer scale for healing [PUSH] tool ... category according to EPUAP definitions" Comment: unclear risk of bias because blinding of outcome assessment is not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk |
Outcome group: primary outcome Comment: low risk of bias because it is likely there were no missing data. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Nixon 2006.
| Study characteristics | ||
| Methods |
Study objective: to compare whether differences exist between alternating pressure overlays and alternating pressure mattresses in the development of new pressure ulcers, healing of existing pressure ulcers, and patient acceptability. Study design: randomised controlled trial with cost‐effectiveness analysis Study grouping: parallel group Duration of follow‐up: 30 days; 60 days Number of arms: 2 Single centre or multi‐site: multi‐site Study start date and end date: not described Setting: NHS hospitals |
|
| Participants |
Baseline characteristics Inclusion criteria: participants aged at least 55 years who had been admitted to vascular, orthopaedic, medical, or care of elderly people wards, either as acute or elective admissions, in the previous 24 hours; expected length of stay of at least 7 days and either limitation of activity and mobility (Braden scale activity and mobility scores of 1 or 2; box 25) or an existing pressure ulcer of grade 2 (using the skin grading tool from Nixon et al, 3 box 1); elective surgical patients without limitation of activity and mobility or an existing pressure ulcer Exclusion criteria: those who had a pressure ulcer on admission of grade 3 or worse, had a planned admission to an intensive care unit after surgery, were admitted to hospital more than 4 days before surgery, slept at night in a chair, or weighed more than 140 kg or less than 45 kg Sex (M:F): 346:636 in mattress; 365: 624 in overlay Age (years): mean 75.0 (SD 9.2) in mattress; 75.4 (SD 9.7) in overlay Baseline skin status: total Braden scores not reported; 1558 (79%) of patients bedfast and 1342 (68.1%) patients very limited mobility and 362 completely immobile Group difference: no difference Total number of participants: 1972 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating pressure mattress
Alternating pressure overlay
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was through an independent, secure, 24 hour randomisation automated telephone system, ensuring allocation concealment. We used minimisation so that groups were comparable. We minimised on centre, existing pressure ulcer ... specialty ... and type of admission" Comment: low risk of bias due to the use of a proper randomisation method. |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was through an independent, secure, 24 hour randomisation automated telephone system, ensuring allocation concealment. We used minimisation so that groups were comparable. We minimised on centre, existing pressure ulcer ... specialty ... and type of admission" Comment: low risk of bias due to proper concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Outcome group: all outcomes Quote: "This was an open trial. Owing to the nature of the mattresses under investigation, it was not possible to mask the randomised intervention to the patients participating in the trial, ward nursing staff or the CRNs conducting the skin assessments" Quote: "The PRESSURE Trial CRNs worked closely with ward staff and informed ward staff of the randomised mattress allocation" Comment: high risk of bias because it was impossible to blind participants and personnel but some efforts were made to improve the compliance of using the allocated interventions. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk |
Outcome group: primary outcome Quote: "This was an open trial. Owing to the nature of the mattresses under investigation, it was not possible to mask the randomised intervention to the patients participating in the trial, ward nursing staff or the CRNs conducting the skin assessments ... To minimise the potential for bias it was planned that qualified ward‐based nursing staff (WNs) would record daily skin assessments and CRNs would undertake assessments twice weekly to validate ward staff records, ward staff remaining blind to the CRN record" (HTA report). Comment: unclear risk of bias because of the efforts to reduce detection bias. Outcome group: adverse event Quote: "Adverse events were reviewed by the clinical coordinator, TMG and TSC, who were blind to allocation" Comment: low risk of bias for adverse event outcome. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk |
Outcome group: All outcomes Quote: "The analysis was by intention to treat, with participants being analysed according to the group to which they were randomised ..." Quote: "... 1972 were randomised ... One patient was randomised twice and therefore excluded, providing an intention to treat population of 1971 people ..." Comment: low risk of bias because intention‐to‐treat analysis was done. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is available and all of the study’s pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Nixon 2019.
| Study characteristics | ||
| Methods |
Study objective: to compare the clinical effectiveness and cost‐effectiveness of 2 mattress types: alternating pressure mattresses (APMs) or high specification foam (HSF) Study design: randomised controlled trial (double triangular group sequential design) Study grouping: parallel group Duration of follow‐up: maximum treatment phase of 60 days; 30 days post‐treatment Number of arms: 2 Single centre or multi‐site: multi‐site Study start date and end date: August 2013 to November 2016 Setting: 42 UK secondary/community inpatient facilities |
|
| Participants |
Baseline characteristics Inclusion criteria: inpatient with evidence of acute illness; ≥ 18 years; expected stay ≥ 5 days; expected to comply with follow‐up; on electric profiling bed‐frame; high pressure ulcer (PU) risk due to at least 1 of following: Braden activity score 1/2 and mobility score 1/2; category 1 ulcers; localised skin pain on a healthy/altered/category 1 pressure area Exclusion criteria: had previously participated; current/previous ulcer category ≥ 3; planned intensive care unit (ICU) admission; unable to receive intervention; outside mattress weight limits (< 45 kg or > 180 kg); ethically inappropriate e.g. thought to be in the last few days of their life Sex (M:F): 907:1119 overall; 462:553 in APM; 445:566 in HSF Age (years): median 81 (range 21 to 105) overall; mean 77.8 (SD 13.42) in APM; 78.2 (12.87) in HSF Baseline skin status: overall 78 with a Braden score > 18 (not at risk) in APM and 69 in HSF; 937 with a score ≤ 18 (at risk) in APM; 942 in HSF. At risk and allowed to have category 1 ulcers Group difference: no difference Total number of participants: n = 2029 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating pressure air mattress (APM)
High‐specification foam mattress (HSF)
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomised centrally (24 h automated telephone system, ensuring allocation concealment) on a 1:1 basis using minimisation (with random element) and minimisation factors: centre, PU status, type of facility, and type of consent" Comment: low risk of bias because of the use of a proper randomisation method. |
| Allocation concealment (selection bias) | Low risk | Quote: "Participants were randomised centrally (24 h automated telephone system, ensuring allocation concealment) on a 1:1 basis using minimisation (with random element) and minimisation factors: centre, PU status, type of facility, and type of consent" Comment: low risk of bias because allocation is properly concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Blinding of the research and clinical staff or patients was not possible due to the appearance of the mattresses" Comment: high risk of bias because non‐blinding is clearly stated. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Assessment of risk of bias of the primary endpoint was done with central blind review of photographs and a 10% sample of patients who had skin assessments by a practitioner blinded to previous assessments was performed" Comment: low risk of bias because attempts were made to mask outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All participants recruited were included using Intention‐To‐Treat (ITT) and analysed by randomised allocation" Comment: low risk of bias because ITT analysis was performed. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is available and it is clear that the published reports include all outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Phillips 1999.
| Study characteristics | ||
| Methods |
Study objective: to compare the mattress overlay system with a second dynamic overlay Study design: randomised n‐of‐1 controlled trial, with a series design Study grouping: parallel group Duration of follow‐up: 12 weeks Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: community care |
|
| Participants |
Baseline characteristics Inclusion criteria: those aged over 16 years old and did not have established pressure ulcers; in need of a pressure‐redistributing mattress; with a prognosis of remaining medically stable over 12 weeks; able to provide informed consent Exclusion criteria: not given Sex (M:F): overall 11:26 Age (years): overall median 87 (range 21 to 92) Baseline skin status: median Waterlow score 16 (range 13 to 26); without existing ulcers Group difference: no difference due to the use of n‐of‐1 trial design Total number of participants: n = 37 (the use of n‐of‐1 trial design means 37 trials are run) Unit of analysis: observations of each individual Unit of randomisation (per patient): order of treatment sequence |
|
| Interventions |
Intervention characteristics Viaclin dynamic mattress overlay
Alternative dynamic overlay
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "On entry to the study, subjects were randomly allocated to either the Viaclin or an alternative dynamic overlay" Comment: unclear risk of bias because the sequence generation process is not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: unclear risk of bias because data prior to cross‐over were not available. During the trials, 19 patients withdrew before the end of the trial. |
| Selective reporting (reporting bias) | High risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes. We expected to see outcomes reported by randomised group per period, but this was not the case. |
| Other bias | High risk | Comment: high risk of bias because carry‐over effect is not considered in this study and correlation between repeated measurements on the same individual is not considered in data analysis. Data prior to cross‐over were not available. |
Price 1999.
| Study characteristics | ||
| Methods |
Study objective: to compare the effects on pressure damage prevalence by using 2 different support systems in patients with fractured neck of femur who were at high risk Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: post‐operation 7 days; post‐operation 14 days Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: hospital ward |
|
| Participants |
Baseline characteristics Inclusion criteria: patients with fractured neck of femur (confirmed by X‐ray), who were over 60 years old and identified as being ‘at very high risk’ of developing tissue damage (Medley score > 25) Exclusion criteria: not specified Sex (M:F): 11:29 in Repose; 5:35 in NIMBUS II Age (years): mean 83.5 (range 67.3 to 96.2) in Repose and 80.9 (64.4 to 98.4) in NIMBUS II Baseline skin status: at very high risk defined by Medley score > 25 Group difference: no difference Total number of participants: 80 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Repose
NIMBUS II plus Alpha TranCell
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a concealed computer generated list was used to randomise eligible consecutive consenting patients to one of the support systems" Comment: low risk of bias because of the use of a proper randomisation method. |
| Allocation concealment (selection bias) | Low risk | Quote: "a concealed computer generated list was used to randomise eligible consecutive consenting patients to one of the support systems" Comment: low risk of bias because of a proper concealment method. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Outcome group: primary outcome Comment: high risk of bias because blinding was not possible for this comparison. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "Patients were not assessed blindly as it was considered that displacement for examination would cause excessive discomfort. A team of trained researchers completed all assessments" Comment: high risk of bias because no blinding was done. |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "No patient was excluded from all the analyses" Quote: "Data were not available for the 14‐day follow‐up assessment for a further 12 patients who were transferred to wards or hospitals that were not involved in the study or were discharged home" Comment: high risk of bias because 16 in Repose and 14 in NIMBUS II plus Alpha TranCell actually missed and were not included in analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Pring 1998.
| Study characteristics | ||
| Methods |
Study objective: to compare 3 mattresses in relation to patient pain, comfort and sleep disturbance Study design: randomised controlled trial, with a series design Study grouping: n‐of‐1 trial Duration of follow‐up: 1 week Number of arms: 3 Single centre or multi‐site: single centre Study start date and end date: not described Setting: Regional Rehabilitation Centre. Southern Birmingham Community NHS Trust. |
|
| Participants |
Baseline characteristics Inclusion criteria: all patients admitted to the unit (for patients with neurological disorders aged 16 to 65) with a Waterlow score of 15 and above, with no existing pressure sore or a sore of Grade 2 or lower Exclusion criteria: not given Sex (M:F): not given Age (years): mean 40 years (range 17‐60) overall Baseline skin status: mean Waterlow score 19 (range 16‐26); no existing ulcer, or a sore of Grade 2 or lower Group difference: not given Total number of participants: n = 40 Unit of analysis: treatment sessions Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Nimbus II
Pegasus Airwave
Quattro DC2000
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated to one of three alternating‐pressure mattress replacements." Quote: "The order in which patients used the mattresses was randomly allocated prior to admission to the study" Comment: unclear risk of bias because the sequence generation process was not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Outcome group: all outcomes Quote: "Patients were not given information about the mattresses during the study but it was not possible to disguise the make of mattress" Comment: high risk of bias because non‐blinding of patients is stated. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome group: all outcomes Quote: "Patients were not given information about the mattresses during the study but it was not possible to disguise the make of mattress" Comment: high risk of bias because non‐blinding of patients is stated and this affects the assessment of patient self‐rated outcomes; pain and comfort. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "one patient was withdrawn from the trial due to her clinical condition" Comment: low risk of bias because the rate of dropout is low. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Comment: high risk of bias because the clustering issue probably occurs but is not addressed. |
Rafter 2011.
| Study characteristics | ||
| Methods |
Study objective: to determine the effect of the Dyna‐Form Mercury Advance Mattress versus Softform Premier Active Mattress on pressure ulcer incidence for those in high risk rehabilitation wards over a 1‐month period Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 1 month Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: hospital |
|
| Participants |
Baseline characteristics Inclusion criteria: no existing skin damage or up to category 2 EPUAP pressure ulcers Exclusion criteria: unwilling to participate, re‐admitted with pressure ulcers and weighed above 25 stone Sex (M:F): 0: 5 in Dyna‐Form; and 4:1 in Softform Age (years): median 73 in Dyna‐Form; and 76.8 in Softform Baseline skin status: median Waterlow 21.1 (range 11 to 30) in Dyna‐Form; and 18.4 (15 to 26) Group difference: not specified Total number of participants: 10 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Dyna‐Form Mercury Advance
Softform Premier Active
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients considered to be at high risk of pressure ulcer development were randomly allocated ..." Comment: unclear risk of bias. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Outcome group: primary outcome Comment: high risk of bias because it was unlikely to be possible to blind ward staff who were trained in using both systems for this study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "Their skin was assessed daily for any changes or development of pressure ulcers by ward staff and by the co‐ordinator of the audit three times a week." Comment: high risk of bias because it was unlikely to be possible to blind ward staff. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk |
Outcome group: primary outcome Comment: low risk of bias because of no missing. Outcome group: comfort Comment: high risk of bias because 2 of 5 missed in each group. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Rosenthal 2003.
| Study characteristics | ||
| Methods |
Study objective: to compare the rate of healing when patients were treated with low ‐air‐loss bed, pressure‐relieving bed overlays, and generic total contact seat surface Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 6 months Number of arms: 2 (of 3 arms) considered eligible for inclusion Single centre or multi‐site: multiple site Study start date and end date: not described Setting: long‐term care facilities, and community nursing homes |
|
| Participants |
Baseline characteristics Inclusion criteria: those being alert, able to sit in the 6 months before the study, still sit up with assistance, with a stage III or IV ulcer on the coccyx, trochanter or ischial tuberosities Exclusion criteria: those with sacral pressure ulcers; previously in a trial to treat their current pressure ulcer; already on low‐air‐loss, or transfer to low‐air‐loss planned; skin grafting planned within 1 week; with an active sinus tract or fistula; poor nutrition; requiring antibiotics to treat methicillin‐resistant Staphylococcus aureus, vancomycin‐resistant Enterococci, or active skin infection; osteomyelitis diagnosed; body weight below 60 kg; unable to flex both hip and knee at least 90 degrees Sex (M:F): not given Age (years): mean 69.0 (SD 4.1) in low‐air‐loss (LAL) bed and 68.6 (3.0) in overlay Baseline skin status: all with grade III or IV ulcer Group difference: no difference Total number of participants: n = 76 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Low ‐air‐loss bed
Bed overlay
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed by placing a number corresponding to each experimental condition into a sealed envelope with an equal number of envelopes per condition. A research assistant with no clinical experience drew envelopes by lot as eligible subjects were identified" Comment: low risk of bias because the sequence generation process seems proper. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: unclear risk of bias because the dropout rates are low but are unbalanced (1 death is excluded from analysis and it is unclear which group the death is in; 3 participants withdrawn at 4 weeks due to worsened condition, all in overlay group). |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Russell 2000.
| Study characteristics | ||
| Methods |
Study objective: to determine the efficacy and safety of a multi‐cell pulsating dynamic mattress system in comparison with conventional management for the prevention of pressure ulcers in the operative and postoperative period in patients having cardiovascular surgery. Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 7 days Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: hospital |
|
| Participants |
Baseline characteristics Inclusion criteria: be 18 years of age or older and be scheduled for cardiovascular surgery with general anaesthesia for at least 4 hours with an actual operative time of 3 hours or more Exclusion criteria: had a pressure ulcer at the baseline visit Sex (M:F): 75:23 in multi‐cell pulsating dynamic mattress; 75:25 in conventional management Age (years): mean 65.2 (SD 10.9) in multi‐cell pulsating dynamic mattress; 65.2 (10.6) in conventional management Baseline skin status: mean Knoll score 3.6 (SD 1) in multi‐cell pulsating dynamic mattress; 3.8 (1) in conventional management; no pressure ulcer Group difference: no difference Total number of participants: n = 198 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Multi‐cell pulsating dynamic mattress
Conventional management
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Before surgery, patients were randomly assigned to either the multi‐cell pulsating dynamic mattress system or conventional management. Randomization was done blindly by using a sealed opaque envelope that contained the randomization information (i.e. multi‐cell pulsating dynamic mattress system vs. conventional management)" Comment: unclear risk of bias because randomisation method is not described. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization was done blindly by using a sealed opaque envelope that contained the randomization information (i.e. multi‐cell pulsating dynamic mattress system vs. conventional management)" Comment: unclear risk of bias because randomisation method is not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Outcome group: primary outcome Comment: high risk of bias because it is unlikely that participants were blinded, though no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk |
Outcome group: primary outcome Quote: "Patients were examined immediately post‐surgery for pressure ulcers, including number, stage (I to IV), size (area), location, and appearance. Patients were assessed daily for ... presence of pressure ulcers. A skin risk assessment was performed on days 1, 4, and 7 and on other days if a change in status was noted. Adverse events and concomitant medications were recorded daily" Comment: unclear risk of bias because information on outcome assessment is insufficient for a proper judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk |
Outcome group: primary outcome Quote: "Baseline characteristics and safety were evaluated for all randomised patients (i.e. intent‐to‐treat sample) ... The intent‐to‐treat sample included all patients who signed consent forms and who were placed either on a multi‐cell pulsating dynamic mattress system or on a conventional mattress and had at least 1 day of observation post‐surgery ... An evaluable sample of patients was defined as patients who signed consent forms, had a surgery length of at least 3 hours, and had a minimum of 3 days of observation post‐surgery ... One analysis included the intent‐to‐treat sample (multi‐cell pulsating dynamic mattress system, n = 89; conventional management, n = 96)" Comment: low risk of bias because of the use of intention‐to‐treat (ITT) analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Sanada 2003.
| Study characteristics | ||
| Methods |
Study objective: to examine the effectiveness of a new overlay for at‐risk patients who require head elevation Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: not described Number of arms: 3 Single centre or multi‐site: single centre Study start date and end date: August 1999 to September 2000 Setting: a general acute care unit (hospital) |
|
| Participants |
Baseline characteristics Inclusion criteria: had a Braden score ≤ 16, bed bound, pressure ulcer‐free, required head elevation Exclusion criteria: not described Sex (M:F): 14:15 in double‐layer; 15:11 in single‐layer; 13:14 in standard hospital mattress Age (years): mean 69.5 (SD 14.7) in 29 participants in double‐layer; 73.9 (10.4) in 26 participants in single‐layer; 70.6 (10.7) in 27 participants in standard hospital mattress Baseline skin status: Braden 12.5 (SD 1.7) in double‐layer; 12.1 (1.4) in single‐layer; 12.7 (1.7) in standard; free of pressure ulcers Group difference: no difference Total number of participants: n = 108 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Double‐layer air‐cell overlay
Single‐layer air‐cell overlay
Standard hospital mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The subjects were randomly allocated to the groups by sequentially‐labelled sealed envelopes." Comment: unclear risk of bias because the method of random number generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The subjects were randomly allocated to the groups by sequentially‐labelled sealed envelopes." Comment: unclear risk because it is unclear if the envelopes were opaque. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome group: all outcome (primary outcome) Comment: high risk of bias because 7 of 36 individuals randomised in double‐layer group; 11 of 37 in single‐layer group; and 8 of 35 in standard mattress excluded from analysis. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Sauvage 2017.
| Study characteristics | ||
| Methods |
Study objective: to compare Axtair One, an alternating pressure air mattress (APAM), with a viscoelastic foam mattress (VFM) in elderly patients at moderate to high risk of developing pressure ulcers (PUs). Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 30 days Number of arms: two Single centre or multi‐site: multi‐site Study start date and end date: February 2012 to March 2015 Setting: medium‐ and long‐term stay facilities |
|
| Participants |
Baseline characteristics Inclusion criteria: males and females aged 70 and over, bedridden for at least 15 hours per day, with reduced mobility due to medical problems (such as malnutrition, low blood pressure, urinary incontinence, neurological diseases and sensory disorders), a low to zero positioning capability, a Karnofsky score ≤ 40% and a planned period of hospitalisation of at least 2 weeks, had no PUs at the time of enrolment but had a medium to high risk for developing PUs, as defined by a Braden score ≤14 Exclusion criteria: a weight > 120 kg, body mass index (BMI) < 12 kg/m², a nutritional status score < 12 according to the Mini Nutritional Assessment (MNA), uncompensated nutritional insufficiency and ongoing participation, or within 15 days before, in another clinical research study Sex (M:F): 13:26 in APAM; 9:28 in VFM Age (years): mean 86.03 (SD 5.49) in APAM, 84.59 (6.68) in VFM Baseline skin status: mean Braden score 11.77 (SD 1.27) in APAM, 12.08 (1.26) in VFM; all intact skin Group difference: no difference Total number of participants: n = 76 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating pressure air mattress (APAM)
Viscoelastic foam mattress (VFM)
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was centralised (RANDLIST software v1.2) and globally balanced intracentre with random block sizes established from two possibilities (2 and 4)" Comment: low risk of bias because of the use of a proper randomisation method. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomisation was centralised (RANDLIST software v1.2) and globally balanced intracentre with random block sizes established from two possibilities (2 and 4)" Comment: unclear risk of bias because even though central randomisation was performed, the small block size means that the allocation in the subsequent block is predictable if a prior randomisation sequence has already been known. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "This randomised, controlled, superiority, parallel‐group, open‐label, multicentre ... " Quote: "PUs preventive care had to be performed in compliance with validated care protocols compliant with Good Professional Practice Recommendations" Comment: high risk of bias because open label is clearly stated. Additionally, it is unknown if performance between groups might be unbiased even though there seems to be standardised care plan. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "This randomised, controlled, superiority, parallel‐group, open‐label, multicentre ... " Comment: high risk of bias because open label is clearly stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The population selected for the main analysis were all randomised patients in intention‐to‐treat (ITT)." Comment: low risk of bias because ITT analysis was performed. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Sideranko 1992.
| Study characteristics | ||
| Methods |
Study objective: to compare the pressure‐reducing properties of 3 types of mattress overlays (water, alternating air, and static air mattress surfaces) as used with bed bound patients in a clinical setting Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: mean 10.0 (SD 10.9) days of surgical intensive care unit (SICU) stay in alternating air; 9.4 (8.8) in static air; 8.9 (7.1) in water Number of arms: 3 Single centre or multi‐site: single centre Study start date and end date: not described Setting: 2 surgical ICUs of a hospital |
|
| Participants |
Baseline characteristics Inclusion criteria: a minimum SICU stay of 48 hr; presence of ventilatory support, or some form of haemodynamic support on admission Exclusion criteria: those with any evidence of existing skin breakdown upon admission to the SICUs Sex (M:F): 33:24 across groups Age (years): mean 67.9 (SD 11.1) in alternating air; 63.6 (18.6) in static air; 66.1 (15.6) in water Baseline skin status: free of existing skin breakdown Group difference: no difference Total number of participants: n = 57 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating air
Static air
Water
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... subjects were randomly assigned to be placed on one of the three surfaces studied" Comment: unclear risk of bias because the method of randomisation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome group: all outcomes (primary outcome) Comment: no missing assumed. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Stapleton 1986.
| Study characteristics | ||
| Methods |
Study objective: not provided Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: not described Number of arms: 3 Single centre or multi‐site: single centre Study start date and end date: not described Setting: acute care setting |
|
| Participants |
Baseline characteristics Inclusion criteria: female elderly patients with fractured neck of femur, without existing pressure ulcers, Norton score 14 or less Exclusion criteria: patients did not meet the criteria, or admitted with existing pressure sores Sex (M:F): all female patients (0:32 in large cell Ripple; 0:34 in polyether foam pad; 0:34 in Spenco pad) Age (years): mean 81 across groups Baseline skin status: mean Norton score 12.0 in large cell Ripple; 12.8 in polyether foam pad; 12.9 in Spenco pad; no existing pressure ulcers Group difference: no difference Total number of participants: n = 100 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Large Cell Ripple (Talley)
Polyether foam pad
Spenco pad
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “patients for the first two groups were selected by lottery, and thereafter patients were allocated to each group systematically, in rotation” Comment: unclear risk of bias because it is unclear if a proper randomisation method was applied. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no information provided. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no information provided. |
| Other bias | Unclear risk | Comment: no information provided. |
Taylor 1999.
| Study characteristics | ||
| Methods |
Study objective: "... developing such a data hierarchy to support the adoption of a new PR support surface, the Pegasus Trinova, within an acute care setting" Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: Trinova group mean 10.5 days (SD 1.2); control group 11.6 days (SD 1.4) Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: an acute care setting |
|
| Participants |
Baseline characteristics Inclusion criteria: inpatients within a large NHS trust hospital; provided informed consent; free from pressure damage (including non‐blanching erythema); aged 16 or older; required nursing upon a pressure redistributing support surface Exclusion criteria: not described Sex (M:F): 12:10 in Trinova; 13:9 in alternating pressure air mattress Age (years): mean 66.50 (SD 2.20) in Trinova; mean 70.27 (SD 2.73) in alternating pressure air mattress Baseline skin status: median Waterlow 19 (range 10 to 30) in Trinova; 17 (10 to 35) in alternating pressure air mattress; free of existing ulcers Group difference: no difference Total number of participants: n = 44 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Pegasus Trinova
Alternative dynamic mattress system
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
Outcomes that are not considered in this review but reported in trials:
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomised controlled trial (efficacy data)" Comment: unclear risk because no information about randomisation method provided. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Upon recruitment, the data collector opened the next opaque envelope in sequence to reveal to which mattress group the subject should be allocated" Comment: unclear risk of bias because it is unclear if envelopes were numbered and sealed. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: no information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome group: all outcomes (primary outcome) Comment: low risk of bias because no missing assumed. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Theaker 2005.
| Study characteristics | ||
| Methods |
Study objective: evaluate the effectiveness of 2 devices, the Hill‐Rom Duo mattress and the KCI TheraPulse Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: 20 (5‐127) days length of stay (2 weeks follow‐up after study) Number of arms: 2 Single centre or multi‐site: single centre Study start date and end date: not described Setting: an intensive care unit of a hospital |
|
| Participants |
Baseline characteristics Inclusion criteria: patients admitted to the intensive care unit and classified as being at high‐risk. Exclusion criteria: patients aged < 18 years and those with a pressure sore upon admission; those transferred from other ward areas or hospitals and had been nursed on a pressure‐relieving device other than a Transfoam (Karomed – Division of Verna Ltd, Somerset, UK) or Therarest (KCI Medical Ltd) mattress within the last 7 days Sex (M:F): 20:10 in KCI TheraPulse; 19:13 in Hill‐Rom Duo Age (years): 65 (26‐85) across groups Baseline skin status: at risk; free of existing ulcers Group difference: no difference Total number of participants: n = 62 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics KCI TheraPulse bed
Hill‐Rom Duo mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "... randomly assigned to either a Hill‐Rom Duo mattress or a KCI TheraPulse bed" Quote: "Selection of an unmarked envelope from a pile of envelopes by staff unconnected with the study formed the randomisation process" Comment: low risk of bias because a proper randomisation method applied. |
| Allocation concealment (selection bias) | Unclear risk | Comment: "Selection of an unmarked envelope from a pile of envelopes by staff unconnected with the study formed the randomisation process" Comment: low risk of bias because it is likely that allocation was properly concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Outcome group: all outcomes (primary outcome) Quote: "... unblinded randomised prospective trial" Comment: high risk of bias because it is clearly stated that this is an unblinded trial. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome group: all outcomes (primary outcome) Quote: "If the nurse in charge of the patient’s care had a high level of suspicion that a pressure sore was present, the wound was digitally photographed. For study purposes, the digital photographs were anonymised and analysed subsequently by two independent Tissue Viability Nurses for confirmation of the existence of a pressure sore and assessment of severity" Comment: low risk of bias because efforts were made to minimise the risk of detection bias. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome group: all outcomes (primary outcome) Comment: no attrition. |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias. |
Whitney 1984.
| Study characteristics | ||
| Methods |
Study objective: to provide data that will assist nurses in determining which mattress is the best choice for pressure sore prevention, and under which circumstances Study design: randomised controlled trial Study grouping: parallel group Duration of follow‐up: the average length of study 8.9 days in alternating pressure mattress; 7.6 in foam mattress Number of arms: 2 Single centre or multi‐site: unspecified Study start date and end date: not described Setting: 3 medical‐surgical units. |
|
| Participants |
Baseline characteristics Inclusion criteria: patients on 3 medical‐surgical units who were in bed for 20 out of 24 hours daily Exclusion criteria: not described Sex (M:F): not described Age (years): mean 63.2 (range 19 to 91) Baseline skin status: people with ulcers included (2 has serious decubiti on admission, 1 in each of the groups) Group difference: Total number of participants: n = 51 Unit of analysis: individuals Unit of randomisation (per patient): individuals |
|
| Interventions |
Intervention characteristics Alternating pressure mattress
Foam mattress
|
|
| Outcomes |
Proportion of participants developing a new pressure ulcer
Time to pressure ulcer development
Support‐surface‐associated patient comfort
All reported adverse events using allocated support surfaces
Health‐related quality of life (HRQOL)
Cost‐effectiveness
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "26 were selected at random and placed in the foam mattress group, 25 in the AP mattress group" Comment: unclear risk of bias because it is unclear how the random sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "... the investigators, who assessed the patient and placed him/her in one of the two mattress groups" Comment: high risk of bias because it is likely the investigators performed this study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk |
Outcome group: primary outcome Quote: "In most cases patients were assessed by two investigators as a team, and occasionally by only one of the investigators" Quote: "The investigators who rated patient risk and evaluated skin condition knew the mattress assignment of each patient, making investigator bias possible" Comment: high risk of bias because non‐blinding of outcome assessment is clearly stated. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no information provided. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no information provided. |
| Other bias | Unclear risk | Comment: no information provided. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12618000319279 | Treatment study |
| Allman 1987a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Andrews 1988 | Ineligible study design ‐ not a RCT |
| Anonymous 2006 | Ineligible study design ‐ review article |
| Bell 1993 | Ineligible study design ‐ not a RCT |
| Bennett 1998a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Berthe 2007a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Bliss 1966 | Ineligible study design ‐ not a RCT |
| Bliss 1993 | Ineligible study design ‐ review article |
| Bliss 1995a | Ineligible study design ‐ review article |
| Bliss 2003 | Reproduction of previous work |
| Bliss 2004 | Commentary on a trial |
| Branom 1999 | Treatment study |
| Branom 2001 | Treatment study |
| Brown 2001 | Summary of the Cochrane Review McInnes 2015 |
| Bueno de Camargo 2018a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Cadue 2008 | RCT on heel suspending devices |
| Caley 1994 | Treatment study |
| Cassino 2013 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Cassino 2013b | Incorrect randomisation method (alternation to allocate patients into groups) |
| Chaloner 2000b | Incorrect randomisation method (quasi‐randomisation) |
| ChiCTR1800017466 | Ineligible interventions |
| Chou 2013 | Review articles |
| Cobb 1997b | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Collier 1996a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Cooper 1998a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Cummins 2019 | Ineligible study design ‐ quality improvement project without RCT design |
| Day 1993 | Treatment study |
| Defloor 2005 | Ineligible interventions ‐ different combinations of turning and support surfaces under evaluations |
| De Oliveira 2017 | Review article |
| Devine 1995 | Treatment study |
| Economides 1995 | Ineligible outcome (the breakdown of flaps after operations rather than the incidence of new ulcers or other outcomes) |
| Evans 2000 | Treatment study |
| Ewing 1964a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Exton‐Smith 1982 | Incorrect randomisation method (alternation to allocate patients into groups) |
| Ferrell 1993 | Treatment study |
| Ferrell 1995 | Treatment study |
| Feuchtinger 2006a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Feuchtinger 2006b | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Fleischer 1997 | Ineligible study design |
| García Fernández 2004 | Commentary on a RCT |
| Gazzerro 2008 | Ineligible outcome (wound healing of flap surgery) |
| Gebhardt 1994a | Incorrect randomisation method (randomisation based on participants' hospital numbers) |
| Gebhardt 1994b | Incorrect randomisation method (randomisation based on participants' hospital numbers) |
| Gebhardt 1996 | Incorrect randomisation method |
| Geelkerken 1994 | Commentary |
| Goldstone 1982 | Incorrect randomisation method |
| Gray 1994a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Gray 1998 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Greer 1988 | Treatment study |
| Groen 1999 | Treatment study |
| Gunningberg 2000a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Gunningberg 2001 | Ineligible study design (cross‐sectional design) |
| Haalboom 1994 | Commentary |
| Hale 1990 | Ineligible study design (cost analysis without RCT data) |
| Hampton 1998 | Ineligible study design (not a RCT) |
| Hampton 1999 | Ineligible study design (not a RCT) |
| Hawkins 1997 | Ineligible study design (not a RCT) |
| Hofman 1994 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Holzgreve 1993 | Ineligible study design (not a RCT) |
| Hommel 2008 | Ineligible study design (not a RCT) |
| Hoshowsky 1994 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Hoskins 2007a | Summary of findings of Nixon 2006 |
| Hoskins 2007b | Summary of findings of Nixon 2006 |
| Huang 2013 | Review article |
| Huang 2018 | Ineligible interventions (head pad rather than beds or mattresses) |
| Hungerford 1998 | Commentary on a RCT |
| Iglesias 2006 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Inman 1993 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| IRCT2015110619919N3 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| IRCT2016091129781N1 | Ineligible interventions (cushions rather than beds or mattresses) |
| Ismail 2001 | Ineligible interventions (a number of specific surfaces applied) |
| Jolley 2004a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| JPRN‐UMIN000029680 | Treatment study |
| Kemp 1993 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Keogh 2001 | Ineligible interventions (profiling bed rather than beds or mattresses) |
| Klein 1989 | Review article |
| Lazzara 1991a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Lee 1974 | Ineligible study design (not a RCT) |
| Maklebust 1988 | Ineligible interventions (cushions rather than beds or mattresses) |
| Marutani 2019 | Incorrect randomisation method |
| Mastrangelo 2010a | Treatment study |
| McGinnis 2011 | Review article |
| McGowan 2000 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| McInnes 2015 | Review article |
| McInnes 2018 | Review article |
| Mendoza 2019 | Ineligible participants and outcome (flap closure) |
| Mistiaen 2010 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Mistiaen 2010a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Nakahara 2012 | Ineligible study design (not a RCT) |
| NCT01402765 | Ineligible outcome (interface pressure) |
| NCT02565797 | Ineligible study design (case control design) |
| NCT02634892 | RCT comparing reactive air surfaces versus standard hospital surfaces, withdrawn due to funding issue |
| NCT02735135 | RCT withdrawn due to methodological difficulties |
| NCT03048357 | Ineligible interventions (rotation therapy versus turning) |
| NCT03211910 | Ineligible interventions (not beds or mattresses) |
| NCT03351049 | Ineligible interventions (reactive air surfaces versus reactive surfaces) |
| Nixon 1998 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Ooka 1995 | Ineligible study design (not a RCT) |
| Osterbrink 2005 | Treatment study |
| Ozyurek 2015 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Park 2017a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Rae 2018 | Review article |
| Reddy 2006 | Review article |
| Reddy 2008 | Review article |
| Ricci 2013a | Treatment study |
| Ricci 2013b | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Rithalia 1995 | Ineligible participants (healthy people) |
| Russell 1999 | Treatment study |
| Russell 2000b | Treatment study |
| Russell 2000c | Treatment study |
| Russell 2003a | Treatment study |
| Russell 2003b | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Santy 1994 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Santy 1995 | Review article |
| Scheffel 2011 | Summary of a review |
| Schultz 1999a | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Scott 2000 | Ineligible interventions |
| Scott‐Williams 2006 | Ineligible study design (not a RCT) |
| Serraes 2018 | Review article |
| Shakibamehr 2019 | Ineligible interventions (cushions rather than beds or mattresses) |
| Sharp 2007 | Ineligible study design |
| Shi 2018a | Review article |
| Smith 2013 | Review article |
| Stannard 1993 | Commentary on a RCT |
| Sterzi 2003 | Ineligible study design (not a RCT) |
| Strauss 1991 | Treatment study |
| Takala 1994 | Ineligible study design (not a RCT) |
| Takala 1996 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Tewes 1993 | Review article |
| Vanderwee 2005 | Ineligible intervention (alternating pressure active air surfaces without turning versus foam surfaces plus turning) |
| Van Leen 2011 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Van Leen 2013 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Van Leen 2018 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Van Rijswijk 1994 | Commentary |
| Vermette 2012 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Vyhlidal 1997 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Wallace 2009 | Review article |
| Whittingham 1999 | Ineligible interventions (i.e. comparisons of interventions that are ineligible for inclusion in this review) |
| Yao 2018 | Review article |
Characteristics of studies awaiting classification [ordered by study ID]
Chaloner 2000.
| Methods | Not available |
| Participants | Not available |
| Interventions | Two types of alternating pressure air surfaces |
| Outcomes | Not available |
| Notes | Unable to obtain the full‐text |
Gardner 2008.
| Methods | Randomised controlled trial (two arm) |
| Participants |
Inclusioncriteria: patients at risk of pressure injury (Waterlow score > 9) Exclusioncriteria: under 16 years, unable to tolerate extended time lying supine and with sacral pressure injury of Stage 2 or above Number of participants: 66 Age: on average 68 (12.7) years Gender (M:F): 34:25 Baseline skin status: at risk of ulcer (Waterlow score > 9), without existing severe ulcers |
| Interventions | Airflotation and Ruby mattress
ComfortPlus mattress
|
| Outcomes |
Outcomes of the interest of this review
Outcomes unrelated to this review
|
| Notes |
Henn 2004.
| Methods | Not available |
| Participants | Not available |
| Interventions | Alternating pressure air surfaces and a type of surface that cannot be defined |
| Outcomes | Not available |
| Notes | Unable to obtain the full‐text |
Knight 1999.
| Methods | Not available |
| Participants | Not available |
| Interventions | Pressure‐relieving surfaces that cannot be defined |
| Outcomes | Not available |
| Notes | Unable to obtain the full‐text |
Mastrangelo 2010b.
| Methods | Not available |
| Participants | Not available |
| Interventions | 'Anti‐decubitis lesion mattress cover' that cannot be defined |
| Outcomes | Not available |
| Notes | Unable to obtain the full‐text |
Melland 1998.
| Methods | Not available |
| Participants | Not available |
| Interventions | 'Freedom bed' that cannot be defined |
| Outcomes | Not available |
| Notes | Unable to obtain the full‐text |
Differences between protocol and review
Two review authors independently assessed the titles and abstracts of the new search results for relevance using Rayyan rather than using Covidence.
For new included studies, one review author independently extracted data and another review author checked all data, rather than two review authors independently carrying out data extraction.
When a study only had complete case data, we considered complete case data in the related main analysis (i.e. assuming no missing data issue). This was not pre‐planned.
We presented separate 'Summary of findings' tables for five of the six comparisons evaluated in this review. We did not present the table for the comparison between different types of alternating pressure (active) air surfaces.
Where we did not pool data, we conducted a GRADE assessment and presented these assessments in a narrative format in 'Summary of findings' tables. This was not previously planned.
Contributions of authors
Chunhu Shi: conceived the review; designed the review; coordinated the review; extracted data; analysed or interpreted data; undertook quality assessment; performed statistical analysis; produced the first draft of the review; contributed to writing or editing the review; wrote to study authors/experts/companies; approved the final review prior to publication; is guarantor of the review.
Jo Dumville: conceived the review; designed the review; coordinated the review; analysed or interpreted data; checked quality assessment; checked quality of statistical analysis; produced the first draft of the review; contributed to writing or editing the review; advised on the review; secured funding; performed previous work that was the foundation of the current review; approved the final review prior to publication.
Nicky Cullum: conceived the review; designed the review; checked quality of data extraction; contributed to writing or editing the review; advised on the review; secured funding; performed previous work that was the foundation of the current review; approved the final review prior to publication.
Sarah Rhodes: conceived the review; designed the review; checked quality of data extraction; checked quality assessment; checked quality of statistical analysis; contributed to writing or editing the review; advised on the review; approved the final review prior to publication.
Asmara Jammali‐Blasi: checked quality of data extraction; checked quality assessment; contributed to writing or editing the review; performed previous work that was the foundation of the current review; approved the final review prior to publication.
Elizabeth McInnes: conceived the review; designed the review; coordinated the review; checked quality of data extraction; checked quality assessment; contributed to writing or editing the review; advised on the review; performed previous work that was the foundation of the current review; approved the final review prior to publication.
Contributions of the editorial base
Gill Norman (Editor): edited the protocol; advised on methodology, interpretation and content; approved the final protocol prior to publication. Gill Rizzello (Managing Editor): coordinated the editorial process; advised on content; edited the protocol and the review. Sophie Bishop (Information Specialist): designed the search strategy and edited the search methods section. Tom Patterson (Editorial Assistant): edited the reference section of the protocol and the review.
Sources of support
Internal sources
Division of Nursing, Midwifery and Social Work, School of Health Sciences, Faculty of Biology, Medicine and Health, University of Manchester, UK
External sources
-
National Institute for Health Research, UK
This project is funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB‐PG‐1217‐20006). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
-
NIHR Manchester Biomedical Research Centre (BRC), UK
This research was co‐funded by the NIHR Manchester BRC. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
-
National Institute for Health Research (NIHR), UK
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Wounds. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
-
National Institute for Health Research Applied Research Collaboration (ARC), Greater Manchester, UK
Nicky Cullum and Jo Dumville’s work on this project was partially funded by the National Institute for Health Research Applied Research Collaboration Greater Manchester. The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Declarations of interest
Chunhu Shi: I received research funding from the National Institute for Health Research (NIHR; Research for Patient Benefit, Evidence synthesis for pressure ulcer prevention and treatment, PB‐PG‐1217‐20006). I received support from the Tissue Viability Society to attend conferences unrelated to this work. The Doctoral Scholar Awards Scholarship and Doctoral Academy Conference Support Fund (University of Manchester) also supported a PhD and conference attendance respectively; both were unrelated to this work.
Jo Dumville: I am the Chief Investigator on a National Institute for Health Research grant that funded the conduct of this review (Research for Patient Benefit, Evidence synthesis for pressure ulcer prevention and treatment, PB‐PG‐1217‐20006). This research was co‐funded by the NIHR Manchester Biomedical Research Centre and partly funded by the National Institute of Health Research Applied Research Collaboration Greater Manchester. Nicky Cullum: I am Co‐investigator on a National Institute for Health Research grant that funded the conduct of this review (Research for Patient Benefit, Evidence synthesis for pressure ulcer prevention and treatment, PB‐PG‐1217‐20006). This research was co‐funded by the National Institute of Health Research Manchester Biomedical Research Centre, and partly funded by the National Institute of Health Research Applied Research Collaboration Greater Manchester.
My previous and current employers received research grant funding from the NHS Research and Development Programme, and subsequently the NIHR, for previous versions of this review. The funders had no role in the conduct of the review. My previous employer received research grant funding from the NIHR for an RCT comparing different alternating pressure air surfaces for pressure ulcer prevention. This RCT (for which I was the Chief Investigator) is included in this review. I played no part in the data extraction or risk of bias assessment for this study (Nixon 2006).
Sarah Rhodes: my salary is funded from three National Institute of Health Research grants and a grant from Greater Manchester Cancer.
Asmara Jammali‐Blasi: none known.
Elizabeth McInnes: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Andersen 1982 {published data only}
- Andersen KE, Jensen O, Kvorning SA, Bach E. Decubitus prophylaxis: a prospective trial on the efficacy of alternating-pressure air-mattresses and water-mattresses. Acta Dermatovener (Stockholm) 1982;63:227-30. [PubMed] [Google Scholar]
Aronovitch 1999 {published data only}
- Aronovitch SA, Wilber M, Slezak S, Martin T, Utter D. A comparative study of an alternating air mattress for the prevention of pressure ulcers in surgical patients. Ostomy/Wound Management 1999;45(3):34-44. [PubMed] [Google Scholar]
- Aronovitch SA. A comparative, randomized, controlled study to determine safety and efficacy of preventive pressure ulcer systems: preliminary analysis. Advances in Wound Care 1998;11 (3 Suppl):15-6. [PubMed] [Google Scholar]
Ballard 1997 {published data only}
- Ballard K. Pressure-relief mattresses and patient comfort. Professional Nurse 1997;13(1):27-32. [PubMed] [Google Scholar]
Beeckman 2019 {published data only}
- Anrys C, Van Tiggelen H, Verhaeghe S, Van Hecke A, Beeckman D. Independent risk factors for pressure ulcer development in a high-risk nursing home population receiving evidence-based pressure ulcer prevention: results from a study in 26 nursing homes in Belgium. International Wound Journal 2019;16(2):325-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeckman D, Serraes B, Anrys C, Van Tiggelen H, Van Hecke A, Verhaeghe S. A multicentre prospective randomised controlled clinical trial comparing the effectiveness and cost of a static air mattress and alternating air pressure mattress to prevent pressure ulcers in nursing home residents. International Journal of Nursing Studies 2019;97:105-13. [DOI] [PubMed] [Google Scholar]
- NCT03597750. Comparison of static air support devices (Repose®) and alternating-pressure devices in the prevention of pressure ulcers. ClinicalTrials.gov/show/NCT03597750.
Bliss 1967 {published data only}
- Bliss MR, McLaren R, Exton-Smith AN. Preventing pressure sores in hospital: controlled trial of a large-celled ripple mattress. BMJ 1967;1(5537):394-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bliss 1995 {published data only}
- Bliss MR. Preventing pressure sores in elderly patients: a comparison of seven mattress overlays. Age and Ageing 1995;24:297-302. [DOI] [PubMed] [Google Scholar]
- Bliss MR. Randomised controlled trial of seven pressure relieving mattress overlays for preventing pressure sores in elderly patients. In: Conference of the Tissue Viability Society; 1994; Harrogate (UK). 1994:5.
Cavicchioli 2007 {published data only}
- Cavicchioli A, Carella G. Clinical effectiveness of a low-tech versus high-tech pressure-redistributing mattress. Journal of Wound Care 2007;16(7):285-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Conine 1990 {published data only}
- Conine TA, Daechsel D, Choi AK, Lau MS. Costs and acceptability of two special overlays for the prevention of pressure sores. Rehabilitation Nursing 1990;15(3):133-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Conine TA, Daechsel D, Lau MS. The role of alternating air and Silicore overlays in preventing decubitus ulcers. International Journal of Rehabilitation Research 1990;13(1):133-7. [DOI] [PubMed] [Google Scholar]
Daechsel 1985 {published data only}
- Daechsel D, Conine TA. Special mattresses: effectiveness in preventing decubitus ulcers in chronic neurologic patients. Archives of Physical Medicine and Rehabilitation 1985;66(4):246-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Demarre 2012 {published data only}
- Demarre L, Beeckman D, Vanderwee K, Defloor T, Grypdonck M, Verhaeghe S. Multi-stage versus single-stage inflation and deflation cycle for alternating low pressure air mattresses to prevent pressure ulcers in hospitalised patients: a randomised-controlled clinical trial. International Journal of Nursing Studies 2012;49(4):416-26. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Demarre L, Vanderwee K, Beeckman D, Defloor T. Pressure ulcer prevention: randomized controlled trial comparing the effect of a standard alternating pressure air mattress and a alternating low pressure air mattress with gradual inflation and deflation. EWMA Journal 2010;10(2):44. [Google Scholar]
- Demarre L, Vanderwee K, Beeckman D, Defloor T. The effectiveness of a multistage low pressure air mattress in pressure ulcer prevention: an RCT Fourth European Nursing Congress. Journal of Clinical Nursing 2010;19:41. [Google Scholar]
- Demarre L, Verhaeghe S, Van Hecke A, Grypdonck M, Clays E, Vanderwee K, et al. The effectiveness of three types of alternating pressure air mattresses in the prevention of pressure ulcers in Belgian hospitals. Research in Nursing & Health 2013;36(5):439-52. [PMID: ] [DOI] [PubMed] [Google Scholar]
Finnegan 2008 {published data only}
- Finnegan MJ, Gazzerro L, Finnegan JO, Lo P. Comparing the effectiveness of a specialized alternating air pressure mattress replacement system and an air-fluidized integrated bed in the management of post-operative flap patients: a randomized controlled pilot study. Journal of Tissue Viability 2008;17(1):2-9. [DOI] [PubMed] [Google Scholar]
Gray 2008 {published data only}
- Gray D, Cooper P, Bertram M, Duguid K, Pirie G. A clinical audit of the Softform Premier Active™ mattress in two acute care of the elderly wards. Wounds UK 2008;4(4):124-8. [Google Scholar]
Grindley 1996 {published data only}
- Grindley A, Acres J. Alternating pressure mattresses: comfort and quality of sleep. British Journal of Nursing 1996;5(21):1303-10. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hampton 1997 {published data only}
- Hampton S. Evaluation of the new Cairwave Therapy System in one hospital trust. British Journal of Nursing 1997;6(3):167-70. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jiang 2014 {published data only}
- Jiang Q, Li X, Zhang A, Guo Y, Liu Y, Liu H, et al. Multicenter comparison of the efficacy on prevention of pressure ulcer in postoperative patients between two types of pressure-relieving mattresses in China. International Journal of Clinical and Experimental Medicine 2014;7(9):2820-7. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Laurent 1998 {published data only}
- Laurent S. Effectiveness of pressure decreasing mattresses in cardiovascular surgery patients: a controlled clinical trial. In: 3rd European Conference for Nurse Managers, 1997 Oct; Brussels (Belgium). 1998.
Malbrain 2010 {published data only}
- Malbrain M, Hendriks B, Wijnands P, Denie D, Jans A, Vanpellicom J, et al. A pilot randomised controlled trial comparing reactive air and active alternating pressure mattresses in the prevention and treatment of pressure ulcers among medical ICU patients. Journal of Tissue Viability 2010;19(1):7-15. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nixon 2006 {published data only}
- ISRCTN78646179. Randomised controlled trial comparing alternating pressure overlays with alternating pressure mattresses for pressure sore prevention and treatment. isrctn.com/ISRCTN78646179.
- Nelson EA, Nixon J, Mason S, Barrow H, Phillips A, Cullum N. A nurse-led randomised trial of pressure-relieving support surfaces. Professional Nurse 2003;18(9):513-6. [PMID: ] [PubMed] [Google Scholar]
- Nixon J, Cranny G, Iglesias C, Nelson EA, Hawkins K, Phillips A, et al. Randomised, controlled trial of alternating pressure mattresses compared with alternating pressure overlays for the prevention of pressure ulcers: PRESSURE (pressure relieving support surfaces) trial. BMJ 2006;332(7555):1413-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon J, Cranny G, Nelson A, Iglesias C, Phillips A, Hawkins K, et al. Pressure trial clinical and patient outcomes. In: European Wound Management Association; 1998 November; Harrogate, UK. 2005:157.
- Nixon J, Cranny G, Nelson A, Iglesias C, Phillips A, Hawkins K, et al. The NHS Health Technology Assessment Programme. Pressure trial clinical and patient outcomes. EWMA Journal 2006;6(1):38. [Google Scholar]
- Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al. Pressure relieving support surfaces: a randomised evaluation. Health Technology Assessment (Winchester, England) 2006;10(22):1-163. [DOI] [PubMed] [Google Scholar]
- Nixon J, Thorpe H, Barrow H, Phillips A, Nelson EA, Mason SA, et al. Reliability of pressure ulcer classification and diagnosis. Journal of Advanced Nursing 2005;50(6):613-23. [DOI] [PubMed] [Google Scholar]
- Nixon J. Randomised, controlled trial of alternating pressure mattresses compared with alternating pressure overlays for the prevention of pressure ulcers: PRESSURE (pressure relieving support surfaces) trial. BMJ 2006;333:Erratum in: BMJ 2006; 333:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nixon 2019 {published data only}
- Brown S, Smith I, Brown J, Hulme C, Nixon J. Pressure relieving support surfaces: a randomised evaluation 2 (PRESSURE 2). Trials 2013;14(Suppl 1):P68. [Google Scholar]
- Brown S, Smith IL, Brown JM, Hulme C, McGinnis E, Stubbs N, et al. Pressure RElieving Support SUrfaces: a Randomised Evaluation 2 (PRESSURE 2): study protocol for a randomised controlled trial. Trials 2016;17(1):604. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISRCTN01151335. Pressure RElieving Support SUrfaces: a Randomised Evaluation 2. isrctn.com/ISRCTN01151335.
- McGinnis E, Brown S, Collier H, Faulks P, Gilberts R, Greenwood C, et al. Pressure RElieving Support SUrfaces: a Randomised Evaluation 2 (PRESSURE 2) photographic validation sub-study: study protocol for a randomised controlled trial. Trials 2017;18(1):132. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nixon J, Brown S, Smith IL, McGinnis E, Vargas-Palacios A, Nelson EA, et al. Comparing alternating pressure mattresses and high-specification foam mattresses to prevent pressure ulcers in high-risk patients: the PRESSURE 2 RCT. Health Technology Assessment (Winchester, England) 2019;23(52):1-176. [PMID: ] [DOI] [PMC free article] [PubMed]
- Nixon J, Smith IL, Brown S, McGinnis E, Vargas-Palacios A, Nelson EA, et al. Pressure relieving support surfaces for pressure ulcer prevention (PRESSURE 2): clinical and health economic results of a randomised controlled trial. EClinicalMedicine 2019;14:42-52. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Phillips 1999 {published data only}
- Phillips L. Providing correct pressure-relieving devices for optimum outcome. British Journal of Nursing 1999;8(21):1447-52. [PMID: ] [DOI] [PubMed] [Google Scholar]
Price 1999 {published data only}
- Price P, Bale S, Newcombe R, Harding K. Challenging the pressure sore paradigm. Journal of Wound Care 1999;8(4):187-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
Pring 1998 {published data only}
- Pring J, Millman P. Evaluating pressure-relieving mattresses. Journal of Wound Care 1998;7(4):177-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rafter 2011 {published data only}
- Rafter L. Evaluation of patient outcomes: pressure ulcer prevention mattresses. British Journal of Nursing 2011;20(11):32. [DOI] [PubMed] [Google Scholar]
Rosenthal 2003 {published data only}
- Rosenthal MJ, Felton RM, Nastasi AE, Naliboff BD, Harker J, Navach JH. Healing of advanced pressure ulcers by a generic total contact seat: 2 randomized comparisons with low air loss bed treatments. Archives of Physical Medicine and Rehabilitation 2003;84(12):1733-42. [PMID: ] [DOI] [PubMed] [Google Scholar]
Russell 2000 {published data only}
- Dunlop V. Preliminary results of a randomized, controlled study of a pressure ulcer prevention system. Advances in Wound Care 1998;11(3 Suppl):14. [PMID: ] [PubMed] [Google Scholar]
- Lichtenstein S. A 7 day comparative randomized parallel single centre study to determine the safety and efficacy of the Micropulse system for the prevention of pressure ulcers. Micropulse 1997.
- Russell JA, Lichtenstein SL. Randomized controlled trial to determine the safety and efficacy of a multi-cell pulsating dynamic mattress system in the prevention of pressure ulcers in patients undergoing cardiovascular surgery. Ostomy/Wound Management 2000;46(2):46-51, 54-5. [PMID: ] [PubMed] [Google Scholar]
Sanada 2003 {published data only}
- Matsui Y, Miyake S, Kawasaki T, Konya C, Sugama J, Sanada H. Randomized controlled trial of a two layer type air cell mattress in the prevention of pressure ulcers. Japanese Journal of Pressure Ulcers 2001;3(3):331-7. [Google Scholar]
- Sanada H, Sugama J, Matsui Y, Konya C, Kitagawa A, Okuwa M, et al. Randomised controlled trial to evaluate a new double-layer air-cell overlay for elderly patients requiring head elevation. Journal of Tissue Viability 2003;13(3):112-4, 116, 118. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sauvage 2017 {published data only}
- Sauvage P, Touflet M, Pradere C, Portalier F, Michel JM, Charru P, et al. Pressure ulcers prevention efficacy of an alternating pressure air mattress in elderly patients: E(2)MAO a randomised study. Journal of Wound Care 2017;26(6):304-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sideranko 1992 {published data only}
- Sideranko S, Quinn A, Burns K, Froman RD. Effects of position and mattress overlay on sacral and heel pressures in a clinical population. Research in Nursing & Health 1992;15(4):245-51. [DOI] [PubMed] [Google Scholar]
Stapleton 1986 {published data only}
- Stapleton M. Preventing pressure sores--an evaluation of three products. Geriatric Nursing 1986;6(2):23-5. [PMID: ] [PubMed] [Google Scholar]
Taylor 1999 {published data only}
- Taylor L. Evaluating the Pegasus Trinova: a data hierarchy approach. British Journal of Nursing 1999;8(12):771-4, 776-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Theaker 2005 {published data only}
- Theaker C, Kuper M, Soni N. Pressure ulcer prevention in intensive care - a randomised control trial of two pressure-relieving devices. Anaesthesia 2005;60(4):395-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Whitney 1984 {published data only}
- Whitney JD, Fellows BJ, Larson E. Do mattresses make a difference? Journal of Gerontological Nursing 1984;10(9):20-1, 24-5. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12618000319279 {published data only}
- ACTRN12618000319279. Testing the effectiveness of pressure mattresses for people over 65 years residing in the community. www.anzctr.org.au/AnzctrAttachments/374599-Research%20Proposal%20Ethics%20V2%20(FINAL).pdf 2018.
Allman 1987a {published data only}
- Allman RM, Walker JM, Hart MK, Laprade CA, Noel LB, Smith CR. Air-fluidized beds or conventional therapy for pressure sores. A randomized trial. Annals of Internal Medicine 1987;107(5):641-8. [DOI] [PubMed] [Google Scholar]
Andrews 1988 {published data only}
- Andrews J, Balai R. The prevention and treatment of pressure sores by use of pressure distributing mattresses. Care Science and Practice 1989;7(3):72-6. [PubMed] [Google Scholar]
- Andrews J, Balai R. The prevention and treatment of pressure sores by use of pressure distributing mattresses. Decubitus 1988;1(4):14-21. [PubMed] [Google Scholar]
Anonymous 2006 {published data only}
- Anonymous. Effective methods for preventing pressure ulcers. The Journal of Family Practice 2006;55(11):942. [PMID: ] [PubMed] [Google Scholar]
Bell 1993 {published data only}
- Bell JC, Matthews SD. Results of a clinical investigation of four pressure-reduction replacement mattresses. Journal of ET Nursing 1993;20(5):204-10. [PMID: ] [PubMed] [Google Scholar]
Bennett 1998a {published data only}
- Bennett RG, Baran PJ, DeVone LV, Bacetti H, Kristo B, Tayback M, et al. Low airloss hydrotherapy versus standard care for incontinent hospitalized patients. Journal of the American Geriatrics Society 1998;46(5):569-76. [PMID: ] [DOI] [PubMed] [Google Scholar]
Berthe 2007a {published data only}
- Berthe JV, Bustillo A, Mélot C, De Fontaine D. Does a foamy-block mattress system prevent pressure sores? A prospective randomised clinical trial in 1729 patients. Acta Chirurgica Belgica 2007;107(2):155-61. [PubMed] [Google Scholar]
Bliss 1966 {published data only}
- Bliss MR, McLaren R, Exton-Smith AN. Mattresses for preventing pressure sores in geriatric patients. Monthly Bulletin of the Ministry of Health and The Public Health Laboratory Service 1966;25:238-68. [PMID: ] [PubMed] [Google Scholar]
Bliss 1993 {published data only}
- Bliss MR, Thomas JM. An investigative approach. An overview of randomised controlled trials of alternating pressure supports. Professional Nurse 1993;8(7):437-44. [PMID: ] [PubMed] [Google Scholar]
Bliss 1995a {published data only}
- Bliss MR. Managing pressure ulcers. Advances in Wound Care 1995;8(5):6, 8. [PMID: ] [PubMed] [Google Scholar]
Bliss 2003 {published data only}
- Bliss MR. Clinical research in patient support systems. Journal of Tissue Viability 2003;13(4):154-6, 158, 160. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bliss 2004 {published data only}
- Bliss M. Trials of alternating pressure mattresses. Journal of Tissue Viability 2004;14(1):32-3. [PMID: ] [DOI] [PubMed] [Google Scholar]
Branom 1999 {published data only}
- Branom R, Knox L. Low-air-loss vs non-powered/dynamic surfaces in wound management. In: 31st Annual Wound, Ostomy and Continence Conference: Minneapolis (MN). 1999:483.
Branom 2001 {published data only}
- Branom R, Rappl LM. "Constant force technology" versus low-air-loss therapy in the treatment of pressure ulcers. Ostomy/Wound Management 2001;47(9):38-46. [PMID: ] [PubMed] [Google Scholar]
Brown 2001 {published data only}
- Brown SJ. Bed surfaces and pressure sore prevention: an abridged report. Orthopedic Nursing 2001;20(4):38-40. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bueno de Camargo 2018a {published data only}
- Bueno de Camargo WH, Pereira RD, Tanita MT, Heko L, Grion IC, Festti J, et al. The effect of support surfaces on the incidence of pressure injuries in critically ill patients: a randomized clinical trial. Critical Care Research and Practice 2018;2018:Article ID 3712067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02844166. Support surfaces to prevent pressure injuries. clinicaltrials.gov/show/NCT02844166.
Cadue 2008 {published data only}
- Cadue JF, Karolewicz S, Tardy C, Barrault C, Robert R, Pourrat O. Prevention of heel pressure sores with a foam body-support device. A randomized controlled trial in a medical intensive care unit [Efficacite de supports anatomiques en mousse pour la prevention des escarres de talons. Etude controlee randomisee en reanimation medicale]. Presse Medicale (Paris, France: 1983) 2008;37(1 Pt 1):30-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Caley 1994 {published data only}
- Caley L, Jones S, Freer J, Muller JS. Randomized prospective trial: treatment outcomes and cost-effectiveness of two types of low-air-loss therapy. In: Proceedings of the 9th Annual Clinical Symposium on Pressure Ulcer and Wound Management. 1994:1-2.
Cassino 2013 {published data only}
- Cassino R, Ippolito AM, Cuffaro C, Corsi A, Ricci E. A controlled, randomized study on the effectiveness of two overlays in the treatment of decubitus ulcers. Minerva Chirurgica 2013;68(1):105-16. [PubMed] [Google Scholar]
Cassino 2013b {published data only}
- Cassino R, Ippolito AM, Ricci E. Comparison of two mattress overlays in the prevention of pressure ulcers. Acta Vulnologica 2013;11(1):15-21. [Google Scholar]
Chaloner 2000b {published data only}
- Chaloner D, Cave J. Should weaker study designs ever be preferred over randomised controlled trials. Journal of Tissue Viability 2000;10(3 Suppl):7-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
ChiCTR1800017466 {published data only}
- ChiCTR1800017466. The study on the application of fluidized positioner in preventing intraoperative pressure injury. www.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR1800017466 2018.
Chou 2013 {published data only}
- Chou R, Dana T, Bougatsos C, Blazina I, Starmer AJ, Reitel K, et al. Pressure ulcer risk assessment and prevention: a systematic comparative effectiveness review. Annals of Internal Medicine 2013;159(1):28-38. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cobb 1997b {unpublished data only}
- Cobb GA, Yoder LH, Warren JB. Pressure ulcers: patient outcomes on a KinAir bed or EHOB waffle mattress. TriService Nursing Research Program (TSNRP) 1997.
Collier 1996a {published data only}
- Collier ME. Pressure-reducing mattresses. Journal of Wound Care 1996;5(5):207-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cooper 1998a {published data only}
- Cooper PJ, Gray DG, Mollison J. A randomised controlled trial of two pressure-reducing surfaces. Journal of Wound Care 1998;7(8):374-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cummins 2019 {published data only}
- Cummins KA, Watters R, Leming-Lee T. Reducing pressure injuries in the pediatric intensive care unit. Nursing Clinics of North America 2019;54(1):127-40. [PMID: ] [DOI] [PubMed] [Google Scholar]
Day 1993 {published data only}
- Day A, Leonard F. Seeking quality care for patients with pressure ulcers. Decubitus 1993;6(1):32-43. [PMID: ] [PubMed] [Google Scholar]
Defloor 2005 {published data only}
- Defloor T, De Bacquer D, Grypdonck MH. The effect of various combinations of turning and pressure reducing devices on the incidence of pressure ulcers. International Journal of Nursing Studies 2005;42(1):37-46. [PMID: ] [DOI] [PubMed] [Google Scholar]
De Oliveira 2017 {published data only}
- De Oliveira KF, Nascimento KG, Nicolussi AC, Chavaglia SRR, De Araujo CA, Barbosa MH. Support surfaces in the prevention of pressure ulcers in surgical patients: an integrative review. International Journal of Nursing Practice 2017;23(4):doi: 10.1111/ijn.12553. [DOI] [PubMed] [Google Scholar]
Devine 1995 {published data only}
- Devine B. Alternating pressure air mattresses in the management of established pressure sores. Journal of Tissue Viability 1995;5(3):94-8. [Google Scholar]
Economides 1995 {published data only}
- Economides NG, Skoutakis VA, Carter CA, Smith VH. Evaluation of the effectiveness of two support surfaces following myocutaneous flap surgery. Advances in Wound Care 1995;8(1):49-53. [PMID: ] [PubMed] [Google Scholar]
Evans 2000 {published data only}
- Evans D, Land L, Geary A. A clinical evaluation of the Nimbus 3 alternating pressure mattress replacement system. Journal of Wound Care 2000;9(4):181-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ewing 1964a {published data only}
- Ewing MR, Garrow C, Presley TA, Ashley C, Kisella NM. Further experiences in the use of sheep skins as an aid in nursing. Australian Nurses' Journal 1964;1964 September:215-9.
Exton‐Smith 1982 {published data only}
- Exton-Smith AN, Overstall PW, Wedgwood J, Wallace G. Use of the 'air wave system' to prevent pressure sores in hospital. Lancet 1982;1(8284):1288-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ferrell 1993 {published data only}
- Ferrell BA, Osterweil D, Christenson P. A randomized trial of low-air-loss beds for treatment of pressure ulcers. JAMA 1993;269(4):494-7. [PMID: ] [PubMed] [Google Scholar]
Ferrell 1995 {published data only}
- Ferrell BA, Keeler E, Siu AL, Ahn SH, Osterweil D. Cost-effectiveness of low-air-loss beds for treatment of pressure ulcers. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 1995;50(3):M141-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Feuchtinger 2006a {published data only}
- Feuchtinger J. Preventing decubitus ulcer in heart surgery interventions: visco-elastic foam layer on the operating room table--a study [Dekubituspravention wahrend kardiochirurgischer Eingriffe: Viskoelastische Schaumstoffauflage auf dem Operationstisch--eine Studie]. Pflege Zeitschrift 2006;59(8):498-501. [PMID: ] [PubMed] [Google Scholar]
Feuchtinger 2006b {published data only}
- Feuchtinger J, De Bie R, Dassen T, Halfens R. A 4-cm thermoactive viscoelastic foam pad on the operating room table to prevent pressure ulcer during cardiac surgery. Journal of Clinical Nursing 2006;15(2):162-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Fleischer 1997 {published data only}
- Fleischer I, Bryant D. Evaluating replacement mattresses. Nursing Management 1997;28(8):38-41. [PMID: ] [PubMed] [Google Scholar]
García Fernández 2004 {published data only}
- García Fernández FP, Pancorbo Hidalgo PL, Rodríguez Torres M. Utility and cost-effectiveness of air suspension bed in the prevention of pressure ulcers. Gerokomos 2004;15(3):162-7. [Google Scholar]
Gazzerro 2008 {published data only}
- Gazzerro L, Finnegan M. Comparing the effectiveness of alternating air pressure mattress replacement systems and air fluidized integrated beds in the management of flap and graft patients: ten case studies. Journal of Wound, Ostomy, and Continence Nursing 2008;35(3):S63. [DOI] [PubMed] [Google Scholar]
Gebhardt 1994a {published data only}
- Gebhardt K, Bliss MR. A controlled study to compare the efficacy, practicability and cost of pressure relieving supports to prevent and heal pressure sores. In: 2nd European Conference on Advances in Wound Management; 1992 Oct 20-23; Harrogate (UK). 1993:166.
- Gebhardt K. A randomized trial of alternating pressure (AP) and constant low pressure (CLP) supports for the prevention of pressure sores. Journal of Tissue Viability 1994;4(3):93. [Google Scholar]
Gebhardt 1994b {published data only}
- Gebhardt KS, Bliss MR, Winwright PL. A randomised controlled trial to compare the efficacy of alternating and constant low pressure supports for preventing pressure sores in an intensive care unit (ICU). Clinical Science 1994.
Gebhardt 1996 {published data only}
- Gebhardt KS, Bliss MR, Winwright PL, Thomas J. Pressure-relieving supports in an ICU. Journal of Wound Care 1996;5(3):116-21. [DOI] [PubMed] [Google Scholar]
Geelkerken 1994 {published data only}
- Geelkerken RH, Breslau PJ, Hermans J, Wille J, Hofman A, Hamming JJ. Anti-decubitus mattress [Anti-decubitusmatrassen]. Nederlands Tijdschrift voor Geneeskunde 1994;138(36):1834; author reply 1834-5. [PMID: ] [PubMed]
Goldstone 1982 {published data only}
- Goldstone LA, Norris M, O'Reilly M, White J. A clinical trial of a bead bed system for the prevention of pressure sores in elderly orthopaedic patients. Journal of Advanced Nursing 1982;7(6):545-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gray 1994a {published data only}
- Gray D. A randomised clinical trial of two foam mattresses. Aberdeen Royal Hospitals NHS Trust. Medical Support System 1994.
- Gray D. A randomised controlled trial of two foam mattresses. Journal of Tissue Viability 1994;4(3):92. [Google Scholar]
- Gray DG, Campbell M. A randomised clinical trial of two types of foam mattresses. Journal of Tissue Viability 1994;4(4):128-32. [Google Scholar]
- Gray DG, Cooper PJ, Campbell M. A study of the performance of a pressure reducing foam mattress after three years of use. Journal of Tissue Viability 1998;8(3):9-13. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gray 1998 {published data only}
- Gray D, Smith M. A randomized controlled trial of two pressure-reducing foam mattresses. In: European Wound Management Association Conference; 1998 Nov; Harrogate (UK). 1998:4.
- Gray DG, Smith M. Comparison of a new foam mattress with the standard hospital mattress. Journal of Wound Care 2000;9(1):29-31. [PMID: ] [DOI] [PubMed] [Google Scholar]
Greer 1988 {published data only}
- Greer DM, Morris J, Walsh NE, Glenn AM, Keppler J. Cost-effectiveness and efficacy of air-fluidized therapy in the treatment of pressure ulcers. Journal of Enterostomal Therapy 1988;15(6):247-51. [PMID: ] [DOI] [PubMed] [Google Scholar]
Groen 1999 {published data only}
- Groen HW, Groenier KH, Schuling J. Comparative study of a foam mattress and a water mattress. Journal of Wound Care 1999;8(7):333-5. [DOI] [PubMed] [Google Scholar]
Gunningberg 2000a {published data only}
- Gunningberg L, Lindholm C, Carlsson M, Sjoden PO. Effect of visco-elastic foam mattresses on the development of pressure ulcers in patients with hip fractures. Journal of Wound Care 2000;9(10):455-60. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gunningberg 2001 {published data only}
- Gunningberg L, Lindholm C, Carlsson M, Sjoden PO. Reduced incidence of pressure ulcers in patients with hip fractures: a 2-year follow-up of quality indicators. International Journal for Quality in Health Care 2001;13(5):399-407. [PMID: ] [DOI] [PubMed] [Google Scholar]
Haalboom 1994 {published data only}
- Haalboom JR. Anti-decubitus mattresses [Anti-decubitusmatrassen]. Nederlands Tijdschrift voor Geneeskunde 1994;138(26):1309-10. [PMID: ] [PubMed] [Google Scholar]
Hale 1990 {published data only}
- Hale JS, Smith SH. Pressure reduction mattresses versus pressure reduction overlays: a cost analysis. Journal of Enterostomal Therapy 1990;17(6):241-3. [PMID: ] [PubMed] [Google Scholar]
Hampton 1998 {published data only}
- Hampton S. Can electric beds aid pressure sore prevention in hospitals? British Journal of Nursing 1998;7(17):1010-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hampton 1999 {published data only}
- Hampton S. Efficacy and cost-effectiveness of the Thermo contour mattress. British Journal of Nursing 1999;8(15):990-6. [DOI] [PubMed] [Google Scholar]
Hawkins 1997 {published data only}
- Hawkins JE. The effectiveness of pressure-reducing table pads as an intervention to reduce the risk of intraoperatively acquired pressure sores. Military Medicine 1997;162(11):759-61. [PMID: ] [PubMed] [Google Scholar]
Hofman 1994 {published data only}
- Hofman A, Geelkerken RH, Wille J, Hamming JJ, Hermans J, Breslau PJ. Pressure sores and pressure-decreasing mattresses: controlled clinical trial. Lancet 1994;343(8897):568-71. [PMID: ] [DOI] [PubMed] [Google Scholar]
Holzgreve 1993 {published data only}
- Holzgreve A, Waldner M, Waldner PW, Hohlbach G. Bed sore prophylaxis in patients with chronic arterial occlusive disease with a new thermoactive pressure alternating mattress. Langenbecks Archiv für Chirurgie 1993:1117.
Hommel 2008 {published data only}
- Hommel A, Thorngre KG, Ulander K. How to prevent patients with a hip fracture from developing pressure ulcers. EWMA Journal 2008;8(2):157. [Google Scholar]
Hoshowsky 1994 {published data only}
- Hoshowsky VM, Schramm CA. Intraoperative pressure sore prevention: an analysis of bedding materials. Research in Nursing & Health 1994;17(5):333-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hoskins 2007a {published data only}
- Hoskins A. Alternating pressure mattresses were more cost effective than alternating pressure overlays for preventing pressure ulcers. Evidence-Based Nursing 2007;10(1):23. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hoskins 2007b {published data only}
- Hoskins A. Similar proportions of patients developed pressure ulcers on alternating pressure overlays and alternating pressure mattresses. Evidence-Based Nursing 2007;10(1):22. [PMID: ] [DOI] [PubMed] [Google Scholar]
Huang 2013 {published data only}
- Huang HY, Chen HL, Xu XJ. Pressure-redistribution surfaces for prevention of surgery-related pressure ulcers: a meta-analysis. Ostomy/Wound Management 2013;59(4):36-8, 42, 44, 46, 48. [PMID: ] [PubMed] [Google Scholar]
Huang 2018 {published data only}
- Huang W, Zhu Y, Qu H. Use of an alternating inflatable head pad in patients undergoing open heart surgery. Medical Science Monitor 2018;24:970-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hungerford 1998 {published data only}
- Hungerford K. A specially designed foam mattress replacement reduced pressure ulcers in nursing home residents. Evidence-Based Nursing 1998;1(2):51. [Google Scholar]
Iglesias 2006 {published data only}
- Iglesias C, Nixon J, Cranny G, Nelson EA, Hawkins K, Phillips A, et al. Pressure relieving support surfaces (PRESSURE) trial: cost effectiveness analysis. BMJ 2006;332(7555):1416-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglesias CP, Nixon J, Cranny G, Nelson A, Hawkins K, Philips A, et al. The NHS Health Technology Assessment Programme. Pressure trial: cost effectiveness analysis of two alternating pressure surfaces for the prevention of pressure ulcers. EWMA Journal 2006;6(1):38. [Google Scholar]
- Iglesias CP, Nixon J, Cranny G. Pressure trial: cost effectiveness analysis of two alternating pressure surfaces for the prevention of pressure ulcers. In: European Wound Management Association Conference; 2005 Sept 15-17; Stuttgart (Germany). 2005:156.
Inman 1993 {published data only}
- Inman KJ, Sibbald WJ, Rutledge FS, Clark BJ. Clinical utility and cost-effectiveness of an air suspension bed in the prevention of pressure ulcers. JAMA 1993;269(9):1139-43. [PMID: ] [PubMed] [Google Scholar]
IRCT2015110619919N3 {published data only}
- IRCT2015110619919N3. The effect of silicone protective pad on pressure ulcer. apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2015110619919N3 2016.
IRCT2016091129781N1 {published data only}
- IRCT2016091129781N1. Comparison gum gel and foam cushions to prevent bedsores. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2016091129781N1.
Ismail 2001 {published data only}
- Ismail ZB. Comparative study between the use of a pressure relieving overlay mattress and other mattresses commonly used by homebound patients in the community. Singapore Nursing Journal 2001;28(2):13-6. [Google Scholar]
Jolley 2004a {published data only}
- Jolley DJ, Wright R, McGowan S, Hickey MB, Campbell DA, Sinclair RD, et al. Preventing pressure ulcers with the Australian Medical Sheepskin: an open-label randomised controlled trial. Medical Journal of Australia 2004;180(7):324-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Jolley DJ. A multilevel analysis of three randomised controlled trials of the Australian Medical Sheepskin in the prevention of sacral pressure ulcers. Medical Journal of Australia 2011;194(2):104. [DOI] [PubMed] [Google Scholar]
JPRN‐UMIN000029680 {published data only}
- JPRN-UMIN000029680. Effects of robotic mattress on pressure ulcer healing, comfort level among pressure ulcer patients, and nursing work load: a randomized controlled trial. www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000029680.
Kemp 1993 {published data only}
- Kemp MG, Kopanke D, Tordecilla L, Fogg L, Shott S, Matthiesen V, et al. The role of support surfaces and patient attributes in preventing pressure ulcers in elderly patients. Research in Nursing & Health 1993;16(2):89-96. [PMID: ] [DOI] [PubMed] [Google Scholar]
Keogh 2001 {published data only}
- Keogh A, Dealey C. Profiling beds versus standard hospital beds: effects on pressure ulcer incidence outcomes. Journal of Wound Care 2001;10(2):15-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Klein 1989 {published data only}
- Klein L, Gilroy K. Evaluating mattress overlays and pressure relieving systems: a question of perception or reality? Journal of Enterostomal Therapy 1989;16(2):58-60. [PMID: ] [PubMed] [Google Scholar]
Lazzara 1991a {published data only}
- Lazzara DJ, Buschmann MT. Prevention of pressure ulcers in elderly nursing home residents: are special support surfaces the answer? Decubitus 1991;4(4):42-4, 46, 48. [PMID: ] [PubMed] [Google Scholar]
Lee 1974 {published data only}
- Lee EO, Kim MJ. A comparative study on the effect of gel pad, sheepskin and sponge on prevention and treatment of decubitus ulcers. Journal of Nurses Academic Society 1974;4(3):93-104. [Google Scholar]
Maklebust 1988 {published data only}
- Maklebust J, Brunckhorst L, Cracchiolo-Caraway A, Ducharme MA, Dundon R, Panfilli R, et al. Pressure ulcer incidence in high-risk patients managed on a special three-layered air cushion. Decubitus 1988;1(4):30-40. [PMID: ] [PubMed] [Google Scholar]
Marutani 2019 {published data only}
- JPRN-UMIN000035568. Evaluation of pressure ulcer prevention and QOL for using dual-fit-air-cell-mattresses. www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000035568.
- Marutani A, Okuwa M, Sugama J. Use of 2 types of air-cell mattresses for pressure ulcer prevention and comfort among patients with advanced-stage cancer receiving palliative care: an interventional study. Ostomy Wound Management 2019;65(5):24-32. [PubMed] [Google Scholar]
Mastrangelo 2010a {published data only}
- Mastrangelo D, Farina E, Gallicchio V, De Anna D, Bresadola F. Observational study of the use of antidecubitus mattress covers in the prevention and care of pressure ulcers. Acta Vulnologica 2010;8(2):87-92. [Google Scholar]
McGinnis 2011 {published data only}
- McGinnis E, Stubbs N. Pressure-relieving devices for treating heel pressure ulcers. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No: CD005485. [DOI: 10.1002/14651858.CD005485.pub2] [DOI] [PubMed] [Google Scholar]
McGowan 2000 {published data only}
- McGowan S, Montgomery K, Jolley D, Wright R. The role of sheepskins in preventing pressure ulcers in elderly orthopaedic patients. Primary Intention 2000:127-34.
McInnes 2015 {published data only}
- McInnes E, Jammali-Blasi A, Bell-Syer SE, Dumville JC, Middleton V, Cullum N. Support surfaces for pressure ulcer prevention. Cochrane Database of Systematic Reviews 2015, Issue 9. Art. No: CD001735. [DOI: 10.1002/14651858.CD001735.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
McInnes 2018 {published data only}
- McInnes E, Jammali-Blasi A, Bell-Syer SE, Leung V. Support surfaces for treating pressure ulcers. Cochrane Database of Systematic Reviews 2018, Issue 10. Art. No: CD009490. [DOI: 10.1002/14651858.CD009490.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mendoza 2019 {published data only}
- Mendoza RA, Lorusso GA, Ferrer DA, Helenowski IB, Liu J, Soriano RH, et al. A prospective, randomised controlled trial evaluating the effectiveness of the fluid immersion simulation system vs an air-fluidised bed system in the acute postoperative management of pressure ulcers: a midpoint study analysis. International Wound Journal 2019;16(4):989-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mistiaen 2010 {published data only}
- Mistiaen P, Jolley D, McGowan S, Hickey M, Spreeuwenberg P, Francke A. The Australian Medical Sheepskin prevents pressure ulcers: a combined multilevel analysis of three RCTs. Fourth European Nursing Congress. Journal of Clinical Nursing 2010;19:20. [Google Scholar]
- Mistiaen P, Jolley DJ, McGowan S, Hickey MB, Spreeuwenberg P, Francke AL. 'Australian Medical Sheepskin' in the prevention of decubitus: meta-analysis with individual patient data shows efficacy ['Australische Medische Schapenvacht' ter preventie van decubitus: meta-analyse met individuele patientendata toont effectiviteit]. Nederlands Tijdschrift voor Geneeskunde 2011;155(15):686-91. [PMID: ] [PubMed] [Google Scholar]
- Mistiaen P, Jolley DJ, McGowan S, Hickey MB, Spreeuwenberg P, Francke AL. [Australian Medical Sheepskin for prevention of pressure ulcers: individual patient data meta-analysis shows effectiveness] ['Australische Medische Schapenvacht' ter preventie van decubitus: meta-analyse met individuele patientendata toont effectiviteit]. Nederlands Tijdschrift voor Geneeskunde 2011;155(18):A3034. [PMID: ] [PubMed] [Google Scholar]
- Mistiaen PJ, Jolley DJ, McGowan S, Hickey MB, Spreeuwenberg P, Francke AL. A multilevel analysis of three randomised controlled trials of the Australian Medical Sheepskin in the prevention of sacral pressure ulcers. Medical Journal of Australia 2010;193(11-12):638-41. [PMID: ] [DOI] [PubMed] [Google Scholar]
- NTR878. Cost-effectiveness of the Australian Medical Sheepskin for the prevention of pressure ulcers in somatic nursing home clients. trialregister.nl/trial/864.
Mistiaen 2010a {published data only}
- Mistiaen P, Achterberg W, Ament A, Halfens R, Huizinga J, Montgomery K, et al. Cost-effectiveness of the Australian Medical Sheepskin for the prevention of pressure ulcers in somatic nursing home patients: study protocol for a prospective multi-centre randomised controlled trial (ISRCTN17553857). BMC Health Services Research 2008;8:4. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistiaen P, Achterberg W, Ament A, Halfens R, Huizinga J, Montgomery K, et al. The effectiveness of the Australian Medical Sheepskin for the prevention of pressure ulcers in somatic nursing home patients: a prospective multicenter randomized-controlled trial (ISRCTN17553857). Wound Repair and Regeneration 2010;18(6):572-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Mistiaen P, Ament A, Francke AL, Achterberg W, Halfens R, Huizinga J, et al. An economic appraisal of the Australian Medical Sheepskin for the prevention of sacral pressure ulcers from a nursing home perspective. BMC Health Services Research 2010;10:226. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistiaen P, Francke A, Achterberg W, Ament A, Halfens R, Huizinga J. Australian Medical Sheepskin is effective for the prevention of pressure ulcers. Tijdschrift voor Ouderengeneeskunde 2009;5:186-90.
Nakahara 2012 {published data only}
- Nakahara R, Ohto S, Kato H. Treating pressure ulcers using alternating pressure replacement mattresses. In: 4th Congress of the World Union of Wound Healing Societies; 2012 Sept 2-6; Yokohama (Japan). 2012.
NCT01402765 {published data only}
- NCT01402765. Interface pressure measures for matresses: Nimbus 3 versus Summit. clinicaltrials.gov/show/NCT01402765.
NCT02565797 {published data only}
- NCT02565797. Comparative prevention-effectiveness trial of DabirAIR overlay system. ClinicalTrials.gov/show/NCT02565797.
NCT02634892 {published data only}
- NCT02634892. Pressure Redistributing Overlay with Targeted Cooling Technology (PRO-TECT) for pressure ulcer prevention. ClinicalTrials.gov/show/NCT02634892.
NCT02735135 {published data only}
- NCT02735135. Comparison of 2 mattresses for the prevention of bedsores by measuring skin pressure in the sacral area. clinicaltrials.gov/show/NCT02735135.
NCT03048357 {published data only}
- NCT03048357. Effectiveness of Freedom Bed compared to manual turning in prevention of pressure injuries in persons with limited mobility due to traumatic brain injury and/or spinal cord injury. clinicaltrials.gov/show/NCT03048357.
NCT03211910 {published data only}
- NCT03211910. Sacral Savers: study of prevention and enhanced healing of sacral and trochenteric ulcers. ClinicalTrials.gov/show/NCT03211910.
NCT03351049 {published data only}
- NCT03351049. An RCT on support surfaces for pressure ulcer prevention. ClinicalTrials.gov/show/NCT03351049.
Nixon 1998 {published data only}
- Bridel-Nixon J, McElvenny D, Brown J, Mason S. A randomized controlled trial using a double-triangular sequential design: methodology and management issues. In: European Wound Management Association Conference; 1997 Apr 27-29; Milan (Italy). 1997:65-6.
- Bridel-Nixon J, McElvenny D, Brown J, Mason S. Findings from a double-triangular sequential-design randomized clinical trial of a dry polymer gel pad. In: European Wound Management Association Conference; 1997 Apr 27-29; Milan (Italy). 1997:20-1.
- Brown J, McElvenny D, Nixon J, Bainbridge J, Mason S. Some practical issues in the design, monitoring and analysis of a sequential randomized trial in pressure sore prevention. Statistics in Medicine 2000;19(24):3389-400. [PMID: ] [DOI] [PubMed] [Google Scholar]
- ISRCTN43076542. Pressure sore risk in the operating department. www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN43076542.
- Nixon J, McElvenny D, Mason S, Brown J, Bond S. A sequential randomised controlled trial comparing a dry visco-elastic polymer pad and standard operating table mattress in the prevention of post-operative pressure sores. International Journal of Nursing Studies 1998;35(4):193-203. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ooka 1995 {published data only}
- Ooka M, Kemp MG, McMyn R, Shott S. Evaluation of three types of support surfaces for preventing pressure ulcers in patients in a surgical intensive care unit. Journal of Wound, Ostomy, and Continence Nursing 1995;22(6):271-9. [DOI] [PubMed] [Google Scholar]
Osterbrink 2005 {published data only}
- Osterbrink J, Mayer H, Schroder G. Clinical evaluation of the effectiveness of a multimodal static pressure relieving device. In: 8th European Pressure Ulcer Advisory Panel Open Meeting; 2005 May 5-7; Aberdeen (Scotland). 2005:73.
Ozyurek 2015 {published data only}
- Ozyurek P, Yavuz M. Prevention of pressure ulcers in the intensive care unit: a randomized trial of 2 viscoelastic foam support surfaces. Clinical Nurse Specialist CNS 2015;29(4):210-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Park 2017a {published data only}
- Park KH, Park J. The efficacy of a viscoelastic foam overlay on prevention of pressure injury in acutely ill patients: a prospective randomized controlled trial. Journal of Wound, Ostomy, and Continence Nursing 2017;44(5):440-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rae 2018 {published data only}
- Rae KE, Isbel S, Upton D. Support surfaces for the treatment and prevention of pressure ulcers: a systematic literature review. Journal of Wound Care 2018;27(8):467-74. [DOI] [PubMed] [Google Scholar]
Reddy 2006 {published data only}
- Reddy M, Gill SS, Rochon PA. Preventing pressure ulcers: a systematic review. JAMA 2006;296(8):974-84. [PMID: ] [DOI] [PubMed] [Google Scholar]
Reddy 2008 {published data only}
- Reddy M, Gill SS, Kalkar SR, Wu W, Anderson PJ, Rochon PA. Treatment of pressure ulcers: a systematic review. JAMA 2008;300(22):2647-62. [DOI] [PubMed] [Google Scholar]
Ricci 2013a {published data only}
- Ricci E, Cassino R, Ippolito A. A randomized study on efficacy on 2 overlays in pressure sores treatment. EWMA Journal 2013;13(1):302.
Ricci 2013b {published data only}
- Ricci E, Roberto C, Ippolito A, Bianco A, Scalise MT. A randomized study on the effectiveness of a new pressure-relieving mattress overlay for the prevention of pressure ulcers in elderly patients at risk. EWMA Journal 2013;13(1):27-32. [Google Scholar]
Rithalia 1995 {published data only}
- Rithalia SV. Comparison of performance characteristics of the Nimbus and Airwave mattresses. International Journal of Rehabilitation Research 1995;18(2):182-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Russell 1999 {published data only}
- Russell L. Randomized comparative clinical trial of Pegasus Cairwave mattress and Proactive seating cushion and Huntleigh Nimbus 3 & Aura seating cushion. Journal of Tissue Viability 1999;9(3):103-4. [Google Scholar]
- Russell L. Randomized comparative clinical trial of the Pegasus Cairwave mattress and Proactive seating cushion and the Huntleigh Nimbus III mattress and Alpha Transcell seating cushion. In: European Wound Management Association and Journal of Wound Care Autumn Conference; 1998 Nov; Harrogate (UK). 1998:4.
Russell 2000b {published data only}
- Russell L, Reynolds T, Carr J, Evans A, Holmes M. A comparison of healing rates on two pressure-relieving systems. British Journal of Nursing 2000;9(22):2270-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
Russell 2000c {published data only}
- Russell L, Reynolds TM, Carr J, Evans A, Holmes M. Randomised controlled trial of two pressure-relieving systems. Journal of Wound Care 2000;9(2):52-5. [DOI] [PubMed] [Google Scholar]
Russell 2003a {published data only}
- Russell L, Reynolds TM, Towns A, Worth W, Greenman A, Turner R. Randomized comparison trial of the RIK and the Nimbus 3 mattresses. British Journal of Nursing 2003;12(4):254, 256-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Russell 2003b {published data only}
- Russell LJ, Reynolds TM, Park C, Rithalia S, Gonsalkorale M, Birch J, et al. Randomized clinical trial comparing 2 support surfaces: results of the prevention of pressure ulcers study. Advances in Skin & Wound Care 2003;16(6):317-27. [PMID: ] [DOI] [PubMed] [Google Scholar]
Santy 1994 {published data only}
- Santy JE, Butler MK, Whyman JD. A comparison study of 6 types of hospital mattress to determine which most effectively reduces the incidence of pressure sores in elderly patients with hip fractures in a District General Hospital. Report to Northern & Yorkshire Regional Health Authority 1994.
Santy 1995 {published data only}
- Santy J. Hospital mattresses and pressure sore prevention. Journal of Wound Care 1995;4(7):329-32. [DOI] [PubMed] [Google Scholar]
Scheffel 2011 {published data only}
- Scheffel S, Panfil EM. Mattresses and Co. for prevention of decubitus ulcer. What measures are effective? [Matratzen und Co. zur Dekubituspravention. Welche Massnahmen sind wirksam?]. Pflege Zeitschrift 2011;64(3):162-3. [PubMed] [Google Scholar]
Schultz 1999a {published data only}
- Schultz A, Bien M, Dumond K, Brown K, Myers A. Etiology and incidence of pressure ulcers in surgical patients. AORN Journal 1999;70(3):434, 437-40, 443-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Schultz AA. Study results: prediction and prevention of pressure ulcers in surgical patients. Advances in Wound Care 1998;11(3):11. [PubMed] [Google Scholar]
Scott 2000 {published data only}
- Scott EM. The prevention of pressure ulcers in the operating department. Journal of Wound Care 2000;9(1):18-21. [PMID: ] [DOI] [PubMed] [Google Scholar]
Scott‐Williams 2006 {published data only}
- Scott-Williams S, Lummas AC. Perioperative pressure ulcer assessment and prevention efficacy study of a multilayered pad for the operating room. Ostomy/Wound Management 2006;52(4):110-1. [Google Scholar]
Serraes 2018 {published data only}
- Serraes B, Van Leen M, Schols J, Van Hecke A, Verhaeghe S, Beeckman D. Prevention of pressure ulcers with a static air support surface: a systematic review. International Wound Journal 2018;15(3):333-43. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shakibamehr 2019 {published data only}
- Shakibamehr J, Rad M, Akrami R, Rad M. Effectiveness of tragacanth gel cushions in prevention of pressure ulcer in traumatic patients: a randomized controlled trial. Journal of Caring Sciences 2019;8(1):45-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sharp 2007 {published data only}
- Sharp A. Pilot study to compare the incidence of pressure ulceration on two therapeutic support surfaces in elderly care. In: 17th Conference of the European Wound Management Association; 2007 May 2-4; Glasgow (Scotland). 2007:Oral presentation 114, 73.
Shi 2018a {published data only}
- Shi C, Dumville JC, Cullum N. Support surfaces for pressure ulcer prevention: a network meta-analysis. PLOS One 2018;13(2):e0192707. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2013 {published data only}
- Smith ME, Totten A, Hickam DH, Fu R, Wasson N, Rahman B, et al. Pressure ulcer treatment strategies: a systematic comparative effectiveness review. Annals of Internal Medicine 2013;159(1):39-50. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stannard 1993 {published data only}
- Stannard D. Commentary on the role of support surfaces and patient attributes in preventing pressure ulcers in elderly patients. AACN Nursing Scan In Critical Care 1993;3(6):2-3. [DOI] [PubMed] [Google Scholar]
Sterzi 2003 {published data only}
- Sterzi S, Selvaggi G, Romanelli A, Valente P, Bertolini C. Evaluation of prevalence and incidence of pressure ulcers and their relationship with mattresses used in a general hospital intensive care unit. European Journal of Plastic Surgery 2003;25(7):401-4. [Google Scholar]
Strauss 1991 {published data only}
- Strauss MJ, Gong J, Gary BD, Kalsbeek WD, Spear S. The cost of home air-fluidized therapy for pressure sores. A randomized controlled trial. Journal of Family Practice 1991;33(1):52-9. [PMID: ] [PubMed] [Google Scholar]
Takala 1994 {published data only}
- Takala J, Soini HO, Soppi E, Kataja M, Olkkonen K. Can risk factors for pressure sores be decreased with a special mattress? Duodecim; Laaketieteellinen Aikakauskirja 1994;110(4):407-14. [PubMed] [Google Scholar]
Takala 1996 {published data only}
- Takala J, Varmavuo S, Soppi E. Prevention of pressure sores in acute respiratory failure: a randomised controlled trial. Clinical Intensive Care 1996;7(5):228-35. [Google Scholar]
Tewes 1993 {published data only}
- Tewes M. Prevention and treatment of pressure sores--a neglected research subject? An overview of clinically controlled studies in the period 1987-91 [Tryksarforebyggelse og -behandling--et forsomt forskningsomrade? En gennemgang af klinisk kontrollerede undersogelser i perioden 1987-91]. Vard i Norden 1993;13(2):4-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Vanderwee 2005 {published data only}
- Vanderwee K, Grypdonck MH, Defloor T. Effectiveness of an alternating pressure air mattress for the prevention of pressure ulcers. Age and Ageing 2005;34(3):261-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Leen 2011 {published data only}
- Van Leen M, Hovius S, Neyens J, Halfens R, Schols J. Pressure relief, cold foam or static air? A single center, prospective, controlled randomized clinical trial in a Dutch nursing home. Journal of Tissue Viability 2011;20(1):30-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Leen 2013 {published data only}
- Van Leen M, Hovius S, Halfens R, Neyens J, Schols J. Pressure relief with visco-elastic foam or with combined static air overlay? A prospective, crossover randomized clinical trial in a dutch nursing home. Wounds 2013;25(10):287-92. [PMID: ] [PubMed] [Google Scholar]
Van Leen 2018 {published data only}
- NTR4557. Is lowering of shear and friction forces (cost)effective for prevention of pressure ulcers? trialregister.nl/trial/4435.
- Van Leen M, Halfens R, Schols J. Preventive effect of a microclimate-regulating system on pressure ulcer development: a prospective, randomized controlled trial in Dutch nursing homes. Advances in Skin & Wound Care 2018;31(1):1-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Rijswijk 1994 {published data only}
- Van Rijswijk L. Pressure sores and pressure-decreasing mattresses: controlled clinical trial. Ostomy Wound Management 1994;40(6):12. [Google Scholar]
Vermette 2012 {published data only}
- Vermette S, Reeves I, Lemaire J. Cost effectiveness of an air-inflated static overlay for pressure ulcer prevention: a randomized, controlled trial. Wounds 2012;24(8):207-14. [PMID: ] [PubMed] [Google Scholar]
Vyhlidal 1997 {published data only}
- Vyhlidal SK, Moxness D, Bosak KS, Van Meter FG, Bergstrom N. Mattress replacement or foam overlay? A prospective study on the incidence of pressure ulcers. Applied Nursing Research 1997;10(3):111-20. [DOI] [PubMed] [Google Scholar]
Wallace 2009 {published data only}
- Wallace M. Review: alternative-foam mattresses and some operating-table overlays reduce pressure ulcers more than standard surfaces. Evidence-Based Nursing 2009;12(3):81. [PMID: ] [DOI] [PubMed] [Google Scholar]
Whittingham 1999 {published data only}
- Whittingham K. Randomized control trial of six pressure-redistributing foam mattresses. Journal of Tissue Viability 1999;9(3):104. [Google Scholar]
Yao 2018 {published data only}
- Yao L, Ding N, Yang L, Han C, Jiang L, Jiang B, et al. Effects of different decompression device in the prevention of pressure sore: a network meta-analysis. Chinese Journal of Evidence-Based Medicine 2018;18(10):1086-92. [Google Scholar]
References to studies awaiting assessment
Chaloner 2000 {published data only}
- Chaloner D. A prospective, controlled comparison between two dynamic alternating mattress replacement systems within a community setting. In: 9th European Conference on Advances in Wound Management; 1999 Nov 9-11; Harrogate (UK). 2000.
Gardner 2008 {published data only}
- Gardner A, Dunk AM, Gardner G. Which mattress works best? A clinical trial of the comparative effectiveness of constant low pressure and alternating pressure devices in hospital patients deemed at risk of pressure injury. In: Australian Wound Management Association 7th National Conference. 2008:52.
Henn 2004 {published data only}
- Henn G, Russell L, Towns A, Taylor H. A two-centre prospective study to determine the utility of a dynamic mattress and mattress overlay. In: 2nd World Union of Wound Healing Societies Meeting; 2004 Jul 8-13; Paris (France). 2004:54.
Knight 1999 {published data only}
- Knight M, Simpson J, Fear-Price M. An evaluation of pressure-reducing overlay mattresses in the community situation. In: 9th European Conference on Advances in Wound Management; 1999 Nov 9-11; Harrogate (UK). 1999:25.
Mastrangelo 2010b {published data only}
- Mastrangelo D, Farina E, Gallicchio V, De Anna D, Bresadola F, Farina MA. Initial analyses of the prospective study randomized on the anti-decubitis lesion mattress cover. In: SAWC Spring: the Symposium on Advanced Wounds Care and the Wound Healing Society; 2010 Apr 17-20; Orlando (FL). 2010:S32.
Melland 1998 {published data only}
- Melland HI, Langemo D, Hanson D, Olson B, Hunter S. Clinical trial of the Freedom Bed. Prairie Rose 1998;67(2):11-2a. [PubMed] [Google Scholar]
Additional references
Baumgarten 2009
- Baumgarten M, Margolis DJ, Selekof JL, Moye N, Jones PS, Shardell M. Validity of pressure ulcer diagnosis using digital photography. Wound Repair and Regeneration 2009;17:287-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borenstein 2009
- Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to Meta-Analysis. West Sussex (UK): John Wiley & Sons, Ltd, 2009. [Google Scholar]
Borenstein 2017
- Borenstein M, Higgins JP, Hedges LV, Rothstein HR. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Research Synthesis Methods 2017;8(1):5-18. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cipriani 2013
- Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Annals of Internal Medicine 2013;159(2):130-7. [DOI] [PubMed] [Google Scholar]
Clark 2011
- Clark M. Technology update: understanding support surfaces. Wounds International 2011;2(3):17-21. [Google Scholar]
Cullum 2016
- Cullum N, Buckley H, Dumville J, Hall J, Lamb K, Madden M, et al. Wounds Research for Patient Benefit: A 5-year Programme of Research. Southampton (UK): NIHR Journals Library, 2016. [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JP, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Demarré 2015
- Demarré L, Van Lancker A, Van Hecke A, Verhaeghe S, Grypdonck M, Lemey J, et al. The cost of prevention and treatment of pressure ulcers: a systematic review. International Journal of Nursing Studies 2015;52(11):1754-74. [DOI] [PubMed] [Google Scholar]
Eldridge 2019
- Eldridge S, Campbell M, Campbell M, Dahota A, Giraudeau B, Higgins J, et al. Revised Cochrane risk of bias tool for randomized trials (RoB 2.0): additional considerations for cluster-randomized trials. www.bristol.ac.uk/media-library/sites/social-community-medicine/images/centres/cresyda/RoB2-0_cluster_parallel_guidance.pdf (accessed 1 October 2019).
EPUAP/NPIAP/PPPIA 2019
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, and Pan Pacific Pressure Injury Alliance (EPUAP/NPIAP/PPPIA). Prevention and treatment of pressure ulcers/injuries: quick reference guide. EPUAP/NPIAP/PPPIA 2019.
Espejo 2018
- Espejo E, Andrés M, Borrallo RM, Padilla E, Garcia-Restoy E, Bella F, Complex Wounds Working Group. Bacteremia associated with pressure ulcers: a prospective cohort study. European Journal of Clinical Microbiology & Infectious Diseases: Official Publication of the European Society of Clinical Microbiology 2018;37(5):969-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Essex 2009
- Essex HN, Clark M, Sims J, Warriner A, Cullum N. Health-related quality of life in hospital inpatients with pressure ulceration: assessment using generic health-related quality of life measures. Wound Repair and Regeneration 2009;17(6):797-805. [DOI] [PubMed] [Google Scholar]
Fletcher 2015
- Fletcher J, Gefen A, Jones L, Sanada H, Irvine M. Hybrid support surfaces. Wounds International 2015:1-6.
Glanville 2019
- Glanville J, Dooley G, Wisniewski S, Foxlee R, Noel-Storr A. Development of a search filter to identify reports of controlled clinical trials within CINAHL Plus. Health Information and Libraries Journal 2019;36(1):73-90. [DOI] [PubMed] [Google Scholar]
Gorecki 2009
- Gorecki C, Brown JM, Nelson EA, Briggs M, Schoonhoven L, Dealey C, et al. Impact of pressure ulcers on quality of life in older patients: a systematic review. Journal of the American Geriatrics Society 2009;57(7):1175-83. [DOI] [PubMed] [Google Scholar]
Gorecki 2013
- Gorecki C, Brown JM, Cano S, Lamping DL, Briggs M, Coleman S, et al. Development and validation of a new patient-reported outcome measure for patients with pressure ulcers: the PU-QOL instrument. Health and Quality of Life Outcomes 2013;11:95. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed 30 September 2019. Hamilton (ON): McMaster University (developed by Evidence Prime). Available at gradepro.org.
Gray 2018
- Gray TA, Rhodes S, Atkinson RA, Rothwell K, Wilson P, Dumville JC, et al. Opportunities for better value wound care: a multiservice, cross-sectional survey of complex wounds and their care in a UK community population. BMJ Open 2018;8(3):e019440. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guest 2018
- Guest JF, Fuller GW, Vowden P, Vowden KR. Cohort study evaluating pressure ulcer management in clinical practice in the UK following initial presentation in the community: costs and outcomes. BMJ Open 2018;8(7):e021769. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al, GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso‐Coello P, et al. GRADE guidelines: 4. rating the quality of evidence - study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64:407-15. [DOI] [PubMed] [Google Scholar]
Herdman 2011
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research 2011;21(10):1727-36. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS (editors). Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Higgins 2019
- Higgins JP, Eldridge S, Li T (editors). Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Hróbjartsson 2012
- Hróbjartsson A, Thomsen AS, Emanuelsson F, Tendal B, Hilden J, Boutron I, et al. Observer bias in randomised clinical trials with binary outcomes: systematic review of trials with both blinded and non-blinded outcome assessors. BMJ 2012;344:e1119. [DOI] [PubMed] [Google Scholar]
Kirkham 2018
- Kirkham JJ, Altman DG, Chan AW, Gamble C, Dwan KM, Williamson PR. Outcome reporting bias in trials: a methodological approach for assessment and adjustment in systematic reviews. BMJ 2018;362:k3802. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Li 2019
- Li T, Higgins JP, Deeks JJ (editors). Chapter 5: Collecting data. In Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Nguyen 2015
- Nguyen KH, Chaboyer W, Whitty JA. Pressure injury in Australian public hospitals: a cost-of-illness study. Australian Health Review 2015;39(3):329-36. [DOI] [PubMed] [Google Scholar]
NICE 2014
- National Institute for Health and Care Excellence (NICE). Pressure ulcers: prevention and management. www.nice.org.uk/guidance/cg179 (accessed 8 October 2019).
NPIAP 2016
- National Pressure Injury Advisory Panel (NPIAP). NPUAP Pressure Injury Stages. Available at cdn.ymaws.com/npuap.site-ym.com/resource/resmgr/npuap_pressure_injury_stages.pdf (accessed 18 February 2020).
NPIAP S3I 2007
- National Pressure Injury Advisory Panel (NPIAP) Support Surface Standards Initiative (S3I). Terms and definitions related to support surfaces. Available at cdn.ymaws.com/npiap.com/resource/resmgr/website_version_terms_and_de.pdf (accessed 18 February 2020).
Ouzzani 2016
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan — a web and mobile app for systematic reviews. Systematic Reviews 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Page 2019
- Page MJ, Higgins JP, Sterne JA. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Available from www.training.cochrane.org/handbook.
Parmar 1998
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Statistics in Medicine 1998;17(24):2815-34. [DOI] [PubMed] [Google Scholar]
Peryer 2019
- Peryer G, Golder S, Junqueira DR, Vohra S, Loke YK. Chapter 19: Adverse effects. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Peters 2008
- Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology 2008;61(10):991-6. [DOI] [PubMed] [Google Scholar]
Review Manager 2020 [Computer program]
- The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.4. The Cochrane Collaboration, 2020.
Riley 2011
- Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342:d549. [PMID: ] [DOI] [PubMed] [Google Scholar]
Salanti 2012
- Salanti G. Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Research Synthesis Methods 2012;3(2):80-97. [PMID: ] [DOI] [PubMed] [Google Scholar]
Salanti 2014
- Salanti G, Giovane CD, Chaimani A, Caldwell DM, Higgins JP. Evaluating the quality of evidence from a network meta-analysis. PLOS One 2014;9(7):e99682. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schoonhoven 2007
- Schoonhoven L, Bousema Mente T, Buskens E, on behalf of the prePURSE-study group. The prevalence and incidence of pressure ulcers in hospitalised patients in the Netherlands: a prospective inception cohort study. International Journal of Nursing Studies 2007;44(6):927-35. [DOI] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273(5):408-12. [DOI] [PubMed] [Google Scholar]
Schünemann 2019
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Shi 2018b
- Shi C, Westby M, Norman G, Dumville J, Cullum N. Node-making processes in network meta-analysis of non-pharmacological interventions should be well planned and reported. Journal of Clinical Epidemiology 2018;101:124-5. [DOI] [PubMed] [Google Scholar]
Shi 2018c
- Shi C, Dumville JC, Cullum N. Skin status for predicting pressure ulcer development: a systematic review and meta-analyses. International Journal of Nursing Studies 2018;87:14-25. [DOI] [PubMed] [Google Scholar]
Shi 2021
- Shi C, Dumville JC, Cullum N, Rhodes S, McInnes E, Goh EL, et al. Beds, overlays and mattresses for preventing and treating pressure ulcers: an overview of Cochrane Reviews and network meta-analysis. Cochrane Database of Systematic Reviews 2021, Issue 8. Art. No: CD013761. [DOI: 10.1002/14651858.CD013761.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Theisen 2012
- Theisen S, Drabik A, Stock S. Pressure ulcers in older hospitalised patients and its impact on length of stay: a retrospective observational study. Journal of Clinical Nursing 2012;21(3-4):380-7. [DOI] [PubMed] [Google Scholar]
Thompson 1999
- Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: a comparison of methods. Statistics in Medicine 1999;18(20):2693-708. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tierney 2007
- Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007;8:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ware 1992
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care 1992;30(6):472-83. [PMID: ] [PubMed] [Google Scholar]
World Health Organization 2019
- World Health Organization. EH90 Pressure ulceration. ICD-11 for mortality and morbidity statistics (version: 04/2019). icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f455330172 (accessed 17 February 2020).
Wounds International 2010
- Wounds International. International Review. Pressure Ulcer Prevention: Pressure, Shear, Friction and Microclimate in Context. A Consensus Document. London (UK): Wounds International, 2010. [Google Scholar]
References to other published versions of this review
Shi 2020
- Shi C, Dumville JC, Cullum N, Rhodes S, McInnes E. Alternating pressure (active) air surfaces for preventing pressure ulcers. Cochrane Database of Systematic Reviews 2020, Issue 5. Art. No: CD013620. [DOI: 10.1002/14651858.CD013620] [DOI] [PMC free article] [PubMed] [Google Scholar]


