Abstract
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus causing the coronavirus disease 2019 (COVID-19) pandemic is known to lead to the complicated sequelae of severe acute respiratory distress syndrome. Proning has been used as an adjunctive treatment to improve oxygenation in both ventilated and non-ventilated patients. Although patients respond well to this strategy, complications from this arise as well. It is hypothesized that COVID-19 intensive care unit (ICU) proned ventilation is associated with new cases of foot drops or compressive unilateral ankle dorsiflexion weakness during the early 2020 COVID-19 pandemic. Five patients presented to an acute rehabilitation facility with unilateral ankle dorsiflexion weakness after ICU proned ventilation during the COVID-19 pandemic. Three patients were found to have primarily subacute left sensory-motor dysmyelinating common peroneal neuropathies located around the fibular head. Two patients were found to have primarily subacute sensory-motor dysmyelinating right-sided common peroneal neuropathies above the fibular head and distal to biceps femoris muscle. Compressive unilateral common peroneal neuropathies during the pandemic are possibly related to the impromptu, unconventional, and unfamiliar use of proned ventilation.
Keywords: prone positioning, foot drop, compression neuropathy, electromyography, nerve conduction study (ncs), covid-19
Introduction
The coronavirus disease (COVID-19) virus can cause a spectrum of sequelae, the most serious being fatal acute respiratory distress syndrome (ARDS) and multi-organ failure in patients worldwide. The prevalence of ARDS in COVID-19 patients during early 2020 was about 17% [1]. One essential strategy in combating COVID-19-related ARDS includes proned ventilation, a non-conventional infrequently used intensive care unit (ICU) technique to improve oxygenation and reduce ventilatory lung injury [2]. Proning is a usually safe adjuvant treatment in both intubated and non-intubated patients to improve oxygenation and decrease mortality in ARDS [2-6].
Many hospitals have developed their own variation of the proning protocol. One of the commonly used proning methods is the “Cornish Pasty” technique [7]. The “Cornish Pasty” technique is described in the following order: (1) team plans procedure, (2) sheets are placed over and under the patient, (3) pillows are placed under the chest and pelvis, (4) pressure areas are checked to be protected, (5) lines are checked and made safe/secured, (6) team wraps the patient in sheets, (7) the patient is turned in a lateral recumbent position, (8) lines and vitals are checked and secured safely, and (9) the patient is ultimately proned. After being proned, the patient is maintained in the “swimmer’s position” or “swimmer’s crawl” where the head is facing in one direction with the ipsilateral arm raised up and the ipsilateral hip and knee flexed [7-11]. The contralateral arm and leg are placed extended alongside the patient’s body [7,8]. A pillow is placed on the shoulder, chest, and hip ipsilaterally to where the patient is facing [7,8]. Alternatively, the patient can be placed in a “modified swimmer’s” position where the arms are bilaterally placed on the sides of the patient [10]. Pressure areas are reassessed with a cushion placed on face, palms, patella, and pre-tibial regions [7,8]. The patient is then placed in reverse Trendelenburg position [7], and the ankles are placed neutrally with the feet offloaded [9-11].
Proning is maintained with body positions alternated on an average of every 2-4 hours for 16-18 hours prone in either the swimmer’s position or other positions where the limbs are adjusted to avoid common pressure points [7-11]. Ghelichkhani and Esmaeili in 2020 recommended the need to change patient positioning and switch sides every two hours with multiple healthcare providers to prevent complications [12]. The optimal methodology, duration, and timing of proning in ventilated COVID-19 patients during the pandemic is currently unknown.
Given the assumed need for long duration of this position to maximize benefits, the side effects of this maneuver may have been overlooked, resulting in complications such as brachial plexus injuries, ischemic optic neuropathy, decubitus ulcers, tube dislodgements, transient desaturations, and compressive neuropathies [4,5,11-16].
Compressive neuropathies associated with mechanical ventilation in prone positioning are rarely cited in the literature. Some risk factors for neuropathies include severe weight loss, diabetes mellitus, habitual leg crossing, compressive masses, and fibrous bands [16]. Electrodiagnostic studies are used to help diagnose, localize, determine severity, and monitor recovery after a nerve injury has been identified [17].
Although patients with COVID-19-related ARDS respond well to proning, complications have been identified in the literature, and are not limited to dermatological, cardiopulmonary, and neuromusculoskeletal conditions [18]. It is hypothesized that new cases of compressive unilateral ankle dorsiflexion weakness may be associated with a course of ICU proned ventilation during the early 2020 COVID-19 pandemic.
Case presentation
Cases were obtained from the inpatient rehabilitation facility and acute hospital electronic medical records. Cases included in the study had the following criteria: (1) a history of being COVID-19 positive, (2) a history of ICU proning, (3) unilateral ankle dorsiflexion weakness, (4) admission to an acute inpatient rehabilitation facility from March to June 2020, (5) recent discharge from an acute care hospital from March to June 2020, and (6) electromyography (EMG) and nerve conduction studies (NCS) conducted to elucidate the etiology of unilateral ankle dorsiflexion weakness. The exclusion criteria for the cases were no EMG/NCS conducted, premorbid unilateral/bilateral limb or ankle dorsiflexion weakness, prior neuropathy, severe weight loss, prior nutritional deficiencies, compressive masses, or cancer metastasis. Institutional Review Board approval was not necessary given the fact that all care was performed according to the standard medical practice and that these trends were noted retrospectively. Five patients were found to satisfy the above inclusion criteria. See Table 1 for patient demographics.
Table 1. Patient demographics.
EMG: electromyography; NCS: nerve conduction studies
| Age | Gender | COVID-19 history | Proned | Medical co-morbidities | Foot drop | Side | EMG/NCS conducted |
| 63 | Male | Yes | Yes | Hypertension | Yes | Left | Yes |
| 68 | Male | Yes | Yes | Hypertension, hyperlipidemia, hypothyroidism | Yes | Left | Yes |
| 55 | Female | Yes | Yes | Hypertension, chronic obstructive pulmonary disease | Yes | Left | Yes |
| 55 | Male | Yes | Yes | Human immunodeficiency virus, hepatitis C virus, chronic obstructive pulmonary disease | Yes | Right | Yes |
| 30 | Male | Yes | Yes | Obesity, active smoker | Yes | Right | Yes |
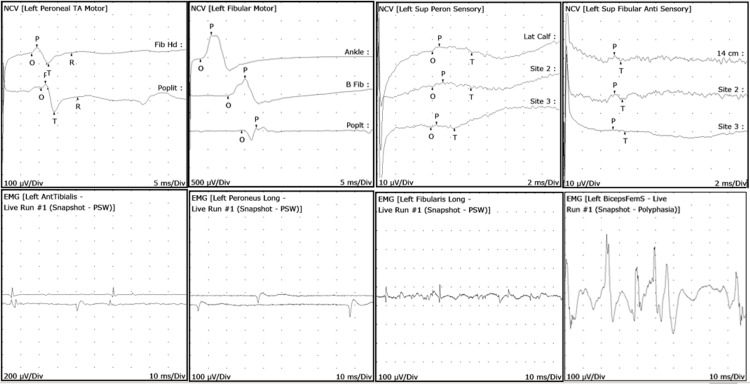
Three patients on EMG/NCS had primarily subacute left sensory-motor, primarily dysmyelinating common peroneal neuropathies. Two patients had right-sided primarily subacute sensory-motor dysmyelinating common peroneal neuropathies. Three of the left-sided injuries were localized at or above the common peroneal nerve with conduction blocks at the superficial peroneal nerve. Two patients were found to have primarily sensory-motor dysmyelinating right-sided common peroneal neuropathy above the fibular head and distal to biceps femoris muscle. One patient had sural nerve involvement. Needle examination revealed abnormal potentials at peroneal innervated muscles. None of the patients revealed lumbar radiculopathy or plexopathy. See Figure 1 for representative left lower extremity EMG/NCS waveforms. All patients had improvements of unilateral ankle dorsiflexion weakness after conventional rehabilitation.
Figure 1. EMG/NCS left lower extremity representative waveforms.
EMG: electromyography; NCS: nerve conduction study
Top left two figures (NCS): Left peroneal/fibular motor nerve conduction block noted in popliteal regions indicating compressive neuropathy
Top right two figures (NCS): Left superficial peroneal/fibular sensory nerve conduction is poor and seen with inconsistent responses
Bottom left two figures (EMG): Left anterior tibialis muscle with positive sharp waves (PSWs) and fibrillations (Fibs). Left peroneus longus muscle with PSWs. These indicate acute denervation of the muscles
Bottom right two figures (EMG): Left peroneus/fibularis longus muscle with PSWs which indicates acute muscle denervation. Biceps femoris muscle with polyphasic potentials which indicate subacute denervation of muscle
Discussion
It is possible that all patients with unilateral ankle dorsiflexion weakness developed them during the early 2020 COVID-19 pandemic with proned ventilation. The overwhelming hospital surge created a widespread lack of healthcare providers to turn patients in a timely manner. This quick impromptu implementation of an uncommonly and unfamiliarly used proned protocol possibly resulted in pressure-related injuries. Healthcare providers’ fears of entering the room frequently to change positions due to severe lack of personal protective equipment and uncertainty of viral infectivity while in the room may have been other factors contributing to poor adherence to the proning protocol, and thus, prolonged compressive neuropathy. The EMG/NCS studies and the observation of clinical improvement of patients after conventional rehabilitation support the possibility that the etiology was unilateral compressive neuropathy of the common peroneal nerve.
It is still suspected that laterality may be related to positioning, which brings to light that the “swimmer’s position” should be modified to prevent compression neuropathy. Other metabolic and medical factors are not entirely excluded. COVID-19 pathological side effects may play some unknown role in exacerbating conditions for unilateral ankle dorsiflexion weakness. Weight loss may have also played a role but occurs via a different pathological mechanism. Studies have shown that weight loss-associated foot drops are usually seen with habitual cross-legging, its predilection for both unilateral and bilateral nerve compression, and prior history of weight loss of greater than 25 pounds usually due to dieting, bariatric surgery, and anorexia [19,20].
Conclusions
In conclusion, the cases presented here on the impromptu, unconventional, and unfamiliar use of proned ventilation during the early 2020 COVID-19 pandemic are possibly associated with new cases of compressive unilateral common peroneal neuropathy. In the future, larger-scale studies need to be conducted to validate this association. Improving the detection and reduction of compressive neuropathies may start with further investigation of the safety of the proning protocol. Rehabilitation from any illness is often a long process, and similarly, compressive neuropathies can be debilitating, and it may take up to a year to achieve maximal healing. While proning should continue to be utilized as dictated by the current literature, changing patient positioning at shorter intervals should continually be emphasized along with the early inclusion of physiatrists to better evaluate the need for timely mobilization. Individualized institutional guidelines should be developed and discussed with all involved.
Acknowledgments
We would like to acknowledge Dr. Lawrence Chang and Dr. Safwan Zar as both first authors.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Chen N, Zhou M, Dong X, et al. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prone positioning in severe acute respiratory distress syndrome. Guérin C, Reignier J, Richard JC, et al. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 3.Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis. Munshi L, Del Sorbo L, Adhikari NKJ, et al. Ann Am Thorac Soc. 2017;14:280–288. doi: 10.1513/AnnalsATS.201704-343OT. [DOI] [PubMed] [Google Scholar]
- 4.The effects of prone position ventilation in patients with acute respiratory distress syndrome. A systematic review and metaanalysis. Mora-Arteaga JA, Bernal-Ramírez OJ, Rodríguez SJ. Med Intensiva. 2015;39:359–372. doi: 10.1016/j.medin.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 5.A comprehensive review of prone position in ARDS. Kallet RH. Respir Care. 2015;60:1660–1687. doi: 10.4187/respcare.04271. [DOI] [PubMed] [Google Scholar]
- 6.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 7.Prone position ventilation in critical care - Portsmouth ICU: version 2. [Jul;2020 ];Brann G, Alexander C, Gonzalez R, et al. http://www.portsmouthicu.com/resources/2016-11-11-Prone-(2016)-Final.pdf 2019
- 8.Kacmarek R, Dimas S, Mack CW. Essentials of Respiratory Care. St. Louis, Missouri: Mosby; 2005. Prone positioning; pp. 789–792. [Google Scholar]
- 9.Pressure injury prevention - PIP tips for prone positioning. [Jul;2020 ];Capasso V, Cox J, Cuddigan J, et al. https://cdn.ymaws.com/npiap.com/resource/resmgr/press_releases/NPIAP_PIP_Tips_for_Proning.pdf 2020
- 10.Good practices for prone positioning at the bedside: construction of a care protocol. Oliveira VM, Weschenfelder ME, Deponti G, et al. Rev Assoc Med Bras (1992) 2016;62:287–293. doi: 10.1590/1806-9282.62.03.287. [DOI] [PubMed] [Google Scholar]
- 11.Massachusetts General Hospital: Prone Positioning Guideline Version 2.0. [Jul;2020 ];https://www.massgeneral.org/assets/MGH/pdf/news/coronavirus/prone-positioning-protocol.pdf 2020
- 12.Prone position in management of COVID-19 patients; a commentary. Ghelichkhani P, Esmaeeili M. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7158870/ Arch Acad Emerg Med. 2020;8:48. [PMC free article] [PubMed] [Google Scholar]
- 13.The prone position in acute respiratory distress syndrome. Ryan DW, Pelosi P. BMJ. 1996;312:860–861. doi: 10.1136/bmj.312.7035.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nursing the ARDS patient in the prone position: the experience of qualified ICU nurses. McCormick J, Blackwood B. Intensive Crit Care Nurs. 2001;17:331–340. doi: 10.1054/iccn.2001.1611. [DOI] [PubMed] [Google Scholar]
- 15.Peroneal nerve palsy: evaluation and management. Poage C, Roth C, Scott B. J Am Acad Orthop Surg. 2016;24:1–10. doi: 10.5435/JAAOS-D-14-00420. [DOI] [PubMed] [Google Scholar]
- 16.UpToDate - prone ventilation for adult patients with acute respiratory distress syndrome. [Jul;2020 ];Malhutra A, Kacmarek RM. http://prone-ventilation-for-adult-patients-with-acute-respiratory-distress-syndrome 2020
- 17.Fibular (peroneal) neuropathy: electrodiagnostic features and clinical correlates. Marciniak C. Phys Med Rehabil Clin N Am. 2013;24:121–137. doi: 10.1016/j.pmr.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 18.Practical proning on ECMO. Daly KJ. Qatar Med J. 2017;2017:19. [Google Scholar]
- 19.Bilateral common peroneal nerve entrapment after excessive weight loss: case report and review of the literature. Margulis M, Ben Zvi L, Bernfeld B. J Foot Ankle Surg. 2018;57:632–634. doi: 10.1053/j.jfas.2017.10.035. [DOI] [PubMed] [Google Scholar]
- 20.Nerve compresion secondary to weight loss. Goizueta-San-Martín G, Pérez-Moro O, Diez-Ramos MF, Fernández-Cuadro M, Gálvez-Rabadá A, Llopis-Miró R. Int J Neurorehabilitation. 2016;3:1–5. [Google Scholar]