Abstract
Background
Ventilator‐associated pneumonia (VAP) is defined as pneumonia developing in people who have received mechanical ventilation for at least 48 hours. VAP is a potentially serious complication in these patients who are already critically ill. Oral hygiene care (OHC), using either a mouthrinse, gel, swab, toothbrush, or combination, together with suction of secretions, may reduce the risk of VAP in these patients.
Objectives
To assess the effects of oral hygiene care (OHC) on incidence of ventilator‐associated pneumonia in critically ill patients receiving mechanical ventilation in hospital intensive care units (ICUs).
Search methods
Cochrane Oral Health’s Information Specialist searched the following databases: Cochrane Oral Health’s Trials Register (to 25 February 2020), the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, 2020, Issue 1), MEDLINE Ovid (1946 to 25 February 2020), Embase Ovid (1980 to 25 February 2020), LILACS BIREME Virtual Health Library (1982 to 25 February 2020) and CINAHL EBSCO (1937 to 25 February 2020). We also searched the VIP Database (January 2012 to 8 March 2020). The US National Institutes of Health Trials Registry (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform were searched for ongoing trials. No restrictions were placed on the language or date of publication when searching the electronic databases.
Selection criteria
We included randomised controlled trials (RCTs) evaluating the effects of OHC (mouthrinse, gel, swab, toothbrush or combination) in critically ill patients receiving mechanical ventilation for at least 48 hours.
Data collection and analysis
At least two review authors independently assessed search results, extracted data and assessed risk of bias in included studies. We contacted study authors for additional information. We reported risk ratio (RR) for dichotomous outcomes and mean difference (MD) for continuous outcomes, using the random‐effects model of meta‐analysis when data from four or more trials were combined.
Main results
We included 40 RCTs (5675 participants), which were conducted in various countries including China, USA, Brazil and Iran. We categorised these RCTs into five main comparisons: chlorhexidine (CHX) mouthrinse or gel versus placebo/usual care; CHX mouthrinse versus other oral care agents; toothbrushing (± antiseptics) versus no toothbrushing (± antiseptics); powered versus manual toothbrushing; and comparisons of other oral care agents used in OHC (other oral care agents versus placebo/usual care, or head‐to‐head comparisons between other oral care agents). We assessed the overall risk of bias as high in 31 trials and low in two, with the rest being unclear.
Moderate‐certainty evidence from 13 RCTs (1206 participants, 92% adults) shows that CHX mouthrinse or gel, as part of OHC, probably reduces the incidence of VAP compared to placebo or usual care from 26% to about 18% (RR 0.67, 95% confidence intervals (CI) 0.47 to 0.97; P = 0.03; I2 = 66%). This is equivalent to a number needed to treat for an additional beneficial outcome (NNTB) of 12 (95% CI 7 to 128), i.e. providing OHC including CHX for 12 ventilated patients in intensive care would prevent one patient developing VAP. There was no evidence of a difference between interventions for the outcomes of mortality (RR 1.03, 95% CI 0.80 to 1.33; P = 0.86, I2 = 0%; 9 RCTs, 944 participants; moderate‐certainty evidence), duration of mechanical ventilation (MD ‐1.10 days, 95% CI ‐3.20 to 1.00 days; P = 0.30, I2 = 74%; 4 RCTs, 594 participants; very low‐certainty evidence) or duration of intensive care unit (ICU) stay (MD ‐0.89 days, 95% CI ‐3.59 to 1.82 days; P = 0.52, I2 = 69%; 5 RCTs, 627 participants; low‐certainty evidence). Most studies did not mention adverse effects. One study reported adverse effects, which were mild, with similar frequency in CHX and control groups and one study reported there were no adverse effects.
Toothbrushing (± antiseptics) may reduce the incidence of VAP (RR 0.61, 95% CI 0.41 to 0.91; P = 0.01, I2 = 40%; 5 RCTs, 910 participants; low‐certainty evidence) compared to OHC without toothbrushing (± antiseptics). There is also some evidence that toothbrushing may reduce the duration of ICU stay (MD ‐1.89 days, 95% CI ‐3.52 to ‐0.27 days; P = 0.02, I2 = 0%; 3 RCTs, 749 participants), but this is very low certainty. Low‐certainty evidence did not show a reduction in mortality (RR 0.84, 95% CI 0.67 to 1.05; P = 0.12, I2 = 0%; 5 RCTs, 910 participants) or duration of mechanical ventilation (MD ‐0.43, 95% CI ‐1.17 to 0.30; P = 0.25, I2 = 46%; 4 RCTs, 810 participants).
Authors' conclusions
Chlorhexidine mouthwash or gel, as part of OHC, probably reduces the incidence of developing ventilator‐associated pneumonia (VAP) in critically ill patients from 26% to about 18%, when compared to placebo or usual care. We did not find a difference in mortality, duration of mechanical ventilation or duration of stay in the intensive care unit, although the evidence was low certainty. OHC including both antiseptics and toothbrushing may be more effective than OHC with antiseptics alone to reduce the incidence of VAP and the length of ICU stay, but, again, the evidence is low certainty. There is insufficient evidence to determine whether any of the interventions evaluated in the studies are associated with adverse effects.
Keywords: Adult; Child; Humans; Chlorhexidine; Chlorhexidine/therapeutic use; Critical Illness; Incidence; Intensive Care Units; Intensive Care Units/statistics & numerical data; Length of Stay; Mouthwashes; Mouthwashes/therapeutic use; Oral Hygiene; Oral Hygiene/methods; Pneumonia, Ventilator-Associated; Pneumonia, Ventilator-Associated/epidemiology; Pneumonia, Ventilator-Associated/mortality; Pneumonia, Ventilator-Associated/prevention & control; Randomized Controlled Trials as Topic; Respiration, Artificial; Respiration, Artificial/adverse effects; Respiration, Artificial/statistics & numerical data; Toothbrushing; Toothbrushing/instrumentation; Toothbrushing/methods
Plain language summary
Oral hygiene care for critically ill patients to prevent ventilator‐associated pneumonia
Why is this question important?
Ventilator‐associated pneumonia (VAP) is a lung infection. It develops in patients who are on artificial breathing machines (ventilators) in hospitals for more than 48 hours. Often, these patients are very ill – they may have had a heart attack or stroke, a serious accident, or major surgery. They may be unable to breathe on their own because they are unconscious or sedated while they receive treatment.
Ventilators supply patients with oxygen through a tube placed in the mouth or nose, or through a hole in the front of the neck. If germs enter through the tube and get into the patient’s lungs, this can lead to VAP. VAP is a potentially very serious complication in patients who are already very ill. It can cause worsening health and increases patients’ risk of dying.
Keeping a patient’s mouth clean and free of disease (oral hygiene) could help to prevent VAP. Oral hygiene care includes:
‐ mouthwash;
‐ antiseptic (a substance that destroys harmful micro‐organisms in the mouth) gel for the gums and teeth;
‐ a soft foam sponge (swab) or toothbrush, to clean the mouth and teeth; and
‐ tools (e.g. a suction tube) to suck away excess fluid, toothpaste or other debris from the mouth.
These can be used alone, or in combination.
To find out if oral hygiene care does prevent VAP, and whether some types of oral hygiene care are better than others, we reviewed the evidence from research studies.
How did we identify and evaluate the evidence?
First, we searched for randomised controlled studies. These are clinical studies where people are randomly put into one of two or more treatment groups, to compare the effects of different treatments. We then compared the results, and summarised the evidence from all the studies. Finally, we rated our confidence in the evidence, based on factors such as study size and methods, and the consistency of findings across studies.
What did we find?
We found 40 studies that involved a total of 5675 people. All the people in the studies received treatment in hospital intensive care units. They required assistance from healthcare staff for their oral hygiene care. Most studies involved adults only, though one study focussed on children and another on newborn babies. The studies took place in a range of countries, including China (10 studies), Brazil (6 studies), the USA (6 studies) and Iran (5 studies).
Studies compared a range of oral health care (such as mouthwashes, gels or toothbrushes) against either:
‐ a placebo (dummy) treatment;
‐ usual care; or
‐ another oral health care treatment.
Here we report the findings for two comparisons:
1) Chlorhexidine (CHX, an antiseptic) in the form of mouthwash or gel, against placebo or usual care (13 studies); and
2) Toothbrushing against no tooth brushing, with or without an antiseptic (8 studies).
CHX against placebo or usual care
The evidence suggests that, compared to placebo or usual care, CHX:
‐ probably prevents VAP from developing in very ill patients (13 studies);
‐ probably has little or no effect on the risk of dying (9 studies);
‐ may make little to no difference to patients’ length of stay in the intensive care unit (5 studies).
We do not know if CHX affects the length of time patients spend on a ventilator, or if it leads to adverse (unwanted) effects. This is because we have too little confidence in the evidence, because studies either:
‐ reported imprecise or inconsistent results;
‐ were conducted in ways likely to introduce error into the results; or
‐ reported too little information.
Toothbrushing against no toothbrushing, with or without an antiseptic
The evidence suggests that, compared to no toothbrushing, toothbrushing may:
‐ prevent VAP from developing in very ill patients (5 studies);
‐ have little or no effect on the risk of dying (5 studies);
‐ make little to no difference to how long people spend on ventilators (4 studies).
We do not know if toothbrushing affects patients’ length of stay in the intensive care unit, or if it leads to adverse effects. This is because we have too little confidence in the evidence, because studies either:
‐ reported imprecise or inconsistent results; or
‐ were conducted in ways likely to introduce error into the results.
What does this mean?
Oral hygiene with CHX probably prevents VAP from developing in very ill patients treated in intensive care units. It probably has little or no effect on patients’ risk of dying, or length of stay in the intensive care unit.
Toothbrushing may prevent VAP from developing in very ill patients treated in intensive care units. It may have little or no effect on patients’ risk of dying, or how long patients spend on a ventilator.
We do not know if CHX or toothbrushing lead to adverse effects, because there is insufficient robust evidence about this.
How‐up‐to date is this review?
The evidence in this Cochrane Review is current to February 2020.
Summary of findings
Summary of findings 1. Chlorhexidine (mouthrinse or gel) versus placebo/usual care for critically ill patients to prevent ventilator‐associated pneumonia.
| Chlorhexidine (mouthrinse or gel) versus placebo/usual care for critically ill patients to prevent ventilator‐associated pneumonia (VAP) | ||||||
|
Population: critically ill adults and children receiving mechanical ventilation
Setting: intensive care units (ICU)
Intervention: chlorhexidine (mouthrinse or gel) Comparison: placebo or usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control (placebo or usual care) | Chlorhexidine (mouthrinse or gel) | |||||
| Incidence of VAP Follow‐up: mean 1 month | 261 per 10001 | 175 per 1000 (123 to 253) | RR 0.67 (0.47 to 0.97) | 1206 (13 studies) | ⊕⊕⊕⊝ moderate2 | This equates to an NNTB of 12 (95% CI 7 to 128); probably reduces the incidence of VAP |
| Mortality Follow‐up: mean 1 month | 190 per 10001 | 247 per 1000 (192 to 319) | RR 1.03 (0.80 to 1.33) | 944 (9 studies) | ⊕⊕⊕⊝ moderate3 | The evidence does not show a difference in mortality |
| Duration of ventilation Days of ventilation required Follow‐up: mean 1 month | The mean duration of ventilation in the control groups ranged from 7 to 12 days | The mean duration of ventilation in the intervention groups was 1.10 days fewer (3.20 fewer to 1.00 more) | 594 (4 studies) | ⊕⊝⊝⊝ verylow4 | The evidence does not show a difference in duration of ventilation | |
| Duration of ICU stay Follow‐up: mean 1 month | The mean duration of ICU stay in the control groups ranged from 10 to 15 days | The mean duration of ICU stay in the intervention groups was 0.89 days fewer (3.59 fewer to 1.82 more) | 627 (5 studies) | ⊕⊕⊝⊝ low 5 |
The evidence does not show a difference in duration of ICU stay | |
| Adverse effects | Most of the studies did not provide information on adverse events. Information on adverse events were identified from 2 studies. One study stated there were none, the other study reported on mild reversible irritation of the oral mucosa | ⊕⊝⊝⊝ very low6 | There was a lack of evidence about adverse effects | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; NNTB: number needed to treat for an additional beneficial outcome; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Assumed risk was based on the median event rate in the control groups of the included studies.
2Downgraded one level due to substantial heterogeneity (I2 = 66%).
3Downgraded one level due to imprecision.
4Downgraded three levels due to serious imprecision, substantial heterogeneity (I2 = 74%), and serious risk of bias: two studies at high risk of bias.
5Downgraded two levels due to serious imprecision and substantial heterogeneity (I2 = 69%).
6Downgraded three levels due to very serious imprecision and serious inconsistency: only two studies reported on this outcome, and they did not report data adequately enough to enable us to evaluate the risk of adverse events.
Summary of findings 2. Toothbrushing (± antiseptics) versus no toothbrushing (± antiseptics) for critically ill patients to prevent ventilator‐associated pneumonia.
| Toothbrushing (± antiseptics)versus no toothbrushing (± antiseptics)for critically ill patients to prevent ventilator‐associated pneumonia (VAP) | ||||||
|
Population: critically ill adults receiving mechanical ventilation
Setting: intensive care units (ICUs)
Intervention: toothbrushing (± antiseptics) Comparison: no toothbrushing (± antiseptics) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No toothbrushing | Toothbrushing | |||||
|
Incidence of VAP Follow‐up: mean 1 month |
259 per 10001 | 179 per 1000 (106 to 236) | RR 0.61 (0.41 to 0.91) | 910 (5 studies)2 | ⊕⊕⊝⊝ low3 | There may be a reduction in the incidence of VAP |
| Mortality Follow‐up: mean 1 month | 250 per 10001 | 210 per 1000 (168 to 263) | RR 0.84 (0.67 to 1.05) | 910 (5 studies)2 | ⊕⊕⊝⊝ low4 | The evidence does not show a difference in mortality |
| Duration of ventilation Follow‐up: mean 1 month | The mean duration of ventilation in the control groups ranged from 10 to 11 days | The mean duration of ventilation in the intervention groups was 0.43days fewer (1.17 fewer to 0.30 more) | 810 (4 studies) | ⊕⊕⊝⊝ low5 | The evidence does not show a difference in duration of ventilation | |
| Duration of ICU stay Follow‐up: mean 1 month | The mean duration of ICU stay in the control groups ranged from 13 to 16 days | The mean duration of ICU stay in the intervention groups was 1.89days fewer (3.52 fewer to 0.27 fewer) | 749 (3 studies) | ⊕⊝⊝⊝ very low6 | There may be a reduction in the duration of ICU stay | |
| Adverse effects | Most of the studies did not provide information on adverse events. Information on adverse events was identified from two studies, which stated that there were none. | ⊕⊝⊝⊝ very low7 | There is a lack of evidence about adverse effects. | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Assumed risk was based on the outcomes in the control groups of the included studies. 2Four studies compared toothbrushing + chlorhexidine with chlorhexidine alone, one study compared toothbrushing with no toothbrushing (no chlorhexidine in either group), another study compared toothbrushing + povidone iodine with povidone iodine alone. 3Downgraded two levels due to very serious risk of bias: five studies at high risk of bias. 4Downgraded two levels due to very serious risk of bias: five studies at high risk of bias. 5Downgraded two levels due to very serious risk of bias: four studies at high risk of bias. 6Downgraded three levels due to serious imprecision and very serious risk of bias: three studies at high risk of bias. 7Downgraded three levels due to very serious imprecision and serious inconsistency: only two studies reported on this outcome, with data that did not enable us to evaluate the risk of adverse events.
Background
Description of the condition
Patients in intensive care units (ICUs) in hospital frequently require mechanical ventilation because their ability to breathe unassisted is impaired due to trauma, or as a result of a medical condition or recent surgery. These critically ill patients are also dependent on hospital staff to meet their needs for nutrition and hygiene, including oral hygiene.
Overall, the research suggests that oral health deteriorates following admission to a critical care unit (Sachdev 2013; Terezakis 2011). Endotracheal intubation and critical illness reduce oral immunity, may be associated with mechanical injury of the mouth or respiratory tract, increase the likelihood of dry mouth, and the presence of the endotracheal tube may also make access for oral care more difficult (Alhazzani 2013; Labeau 2011). Dental plaque accumulates rapidly in the mouths of critically ill patients and as the amount of plaque increases, colonisation by microbial pathogens is likely (Fourrier 1998; Sands 2016; Scannapieco 1992). Plaque colonisation may be exacerbated in the absence of adequate oral hygiene care and by the drying of the oral cavity due to prolonged mouth opening, which reduces the buffering and cleansing effects of saliva. In addition, the patient's normal defence mechanisms for resisting infection may be impaired (Alhazzani 2013; Terpenning 2005). Dental plaque is a complex biofilm which, once formed, is relatively resistant to chemical control, requiring mechanical disruption (such as toothbrushing) for maximum impact (Marsh 2010).
One of the complications that may develop in ventilated patients is ventilator‐associated pneumonia (VAP). VAP is generally defined as a pneumonia developing in a patient who has received mechanical ventilation for at least 48 hours (ATS Guideline 2005). It is thought that the endotracheal tube, which delivers the necessary oxygen to the patient, may also act as a conduit for pathogenic bacteria, which multiply in the oral cavity and move down the tube into the lungs. Micro‐aspiration of pharyngeal secretions may also occur around an imperfect seal of the cuff of the endotracheal tube in a ventilated patient. Several studies have shown that micro‐aspiration contributes to the development of nosocomial pneumonia (Azoulay 2006; Mojon 2002; Scannapieco 1992).
VAP is a relatively common nosocomial infection in critically ill patients, with pooled incidence from 23.8% to 36.0% in recent systematic reviews (Ding 2017; Li 2020), with some indications that incidence is decreasing as understanding of the risk factors and preventative measures improves. Another systematic review estimated the attributable mortality of VAP to be 13% (Melsen 2013). Cohort studies have found that duration of ICU stay is increased in patients who develop VAP, but it is unclear whether this is cause or effect (Apostolopoulou 2003; Cook 1998).
Antibiotics, administered either intraorally as topical pastes or systemically, have been used to prevent VAP, and these interventions are evaluated in other Cochrane systematic reviews (D'Amico 2009; Arthur 2016). As the overuse of systemic antibiotics may be associated with the development of multidrug‐resistant pathogens, there is merit in using other approaches to prevent infections such as VAP.
Description of the intervention
This systematic review evaluates various types of oral hygiene care as a means of reducing the incidence of VAP in critically ill patients receiving mechanical ventilation for at least 48 hours. Oral hygiene care is promoted in clinical guidelines as a means of reducing the incidence of VAP, but the evidence base is limited (Khasanah 2019; Tablan 2004).
Oral hygiene care includes the use of mouthrinse, gel, swab or toothbrushing (either manual or powered) etc. to remove plaque and debris from the oral cavity. Oral hygiene care also involves suction to remove excess fluid, toothpaste, and debris, and may be followed by the application of an antiseptic gel. Antiseptics are broadly defined to include saline, chlorhexidine, povidone iodine, cetylpyridium, and possibly others (but exclude antibiotics).
How the intervention might work
Patients on mechanical ventilation often have a very dry mouth due to prolonged mouth opening, which may be exacerbated by the side effects of medications used in their treatment. In healthy individuals, saliva functions to maintain oral health through its lubricating, antibacterial, and buffering properties (Labeau 2011), but patients on ventilators lack sufficient saliva for this to occur, and the usual stimuli (e.g. food intake) for saliva production are absent.
Routine oral hygiene care is designed to remove plaque and debris, as well as replacing some of the functions of saliva, moistening and rinsing the mouth. Toothbrushing, with either a manual or powered toothbrush, removes plaque from teeth and gums and disrupts the biofilm within which plaque bacteria multiply (Whittaker 1996; Zanatta 2011). It is hypothesised that using an antiseptic, such as chlorhexidine gluconate or povidone iodine, as either a rinse or a gel, may further reduce the bacterial load or delay a subsequent increase in bacterial load.
However, it is important, that during oral hygiene care for critically ill patients in ICUs, the plaque and debris are removed from the oral cavity with care by trained healthcare professionals, in order to avoid aspiration of contaminated fluids into the respiratory tract. Raising the head of the bed, and careful use of appropriately‐maintained closed suction systems, together with an appropriately‐fitted cuff around the endotracheal tube are other important aspects of care of critically ill patients that are not part of this systematic review.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important reviews to produce and keep up‐to‐date on the Cochrane Library (Worthington 2015). The periodontal expert panel identified the topic of this review as a priority at that time and this was confirmed in our recent priority setting update (Cochrane Oral Health Priority Setting Exercise).
Other Cochrane Reviews have evaluated the use of topical antibiotic pastes applied to the oral cavity to prevent VAP (selective oral decontamination (D'Amico 2009), probiotics (Bo 2014), and systemic antibiotics (Arthur 2016)). Other published reviews have evaluated aspects of oral hygiene care, such as toothbrushing (Alhazzani 2013) or use of chlorhexidine (Pineda 2006), and broader reviews have noted the lack of available evidence (Berry 2007; Shi 2004). Some previous clinical guidelines recommended the use of oral hygiene care, but also suggested a lack of available evidence as a basis for specifying the essential components of such care (Muscedere 2008; Tablan 2004).
In terms of oral hygiene care including chlorhexidine, despite the accumulating evidence supporting its effectiveness in VAP prevention, its use for patients requiring mechanical ventilation remains a conflicting topic (Martin‐Loeches 2018) due to potential adverse effects such as hypersensitivity (Pemberton 2012), oral mucosa lesions (Plantinga 2016), reduced bacterial susceptibility (La Combe 2018) and increased risk of mortality (Price 2014).
The goal of this Cochrane Review was to evaluate all oral hygiene care interventions (excluding the use of antibiotics) used in ICU for patients on ventilators for at least 48 hours, to determine the effects of oral hygiene care on the development of VAP. We planned to summarise all the available research in order to facilitate the provision of evidence‐based care for these vulnerable patients.
Objectives
To assess the efficacy and safety of oral hygiene care in the prevention of VAP among critically ill patients receiving mechanical ventilation for at least 48 hours in hospital intensive care units (ICUs).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) of oral hygiene care interventions. We did not consider quasi‐randomised studies for inclusion.
Types of participants
Critically ill patients in hospital settings receiving mechanical ventilation for a minimum of 48 hours, without ventilator‐associated pneumonia or respiratory infection at baseline. We included trials where only some of the participants were receiving mechanical ventilation if the outcome of ventilator‐associated pneumonia was reported and data were available for those who had been treated with mechanical ventilation for a minimum of 48 hours and then developed nosocomial pneumonia.
We included trials where participants were undergoing a surgical procedure that involved mechanical ventilation (e.g. cardiac surgery) only if the oral hygiene care was given during the period of mechanical ventilation that had a minimum duration of 48 hours. We excluded trials where patients received a single preoperative dose of antibacterial rinse or gargle, and received mechanical ventilation only for the duration of the surgery, with no further mechanical ventilation and oral hygiene care during the postoperative period.
Types of interventions
Intervention group: received oral hygiene care procedures such as healthcare professional assisted toothbrushing, oral and pharyngeal cavity rinse, decontamination of oropharyngeal cavities with antiseptics;
Control group: received no treatment, placebo, 'usual care', or a different specific oral hygiene care procedure.
We excluded trials where the intervention being evaluated was a type of suction system or variation of method, timing, or place where mechanical ventilation was introduced (e.g. emergency room or ICU).
We excluded trials of selective decontamination using topical antibiotics administered to the oral cavity or oropharynx, because these interventions are covered in another Cochrane Review (D'Amico 2009). We also excluded trials of probiotics administered to prevent respiratory infections, as these are covered in a separate review (Hao 2015).
Types of outcome measures
We included studies that aimed to assess at least one of our primary outcomes, as we consider these essential for trials about the prevention of VAP.
Primary outcomes
Incidence of VAP (defined as pneumonia developing in a patient who has received mechanical ventilation for at least 48 hours)
Mortality (either all‐cause ICU mortality if these data were available, or all‐cause 30‐day mortality)
Secondary outcomes
Duration of mechanical ventilation
Duration of ICU stay
Systemic antibiotic use
Oral health indices such as gingival index, plaque index, bleeding index, periodontal index, etc.
Adverse effects of the interventions
Caregivers' preferences for oral hygiene care
Economic data
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for randomised controlled trials and controlled clinical trials without language or publication status restrictions:
Cochrane Oral Health's Trials Register (searched 25 February 2020) (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 1) in the Cochrane Library (searched 25 February 2020) (Appendix 2);
MEDLINE Ovid (1946 to 25 February 2020) (Appendix 3);
Embase Ovid (1980 to 25 February 2020) (Appendix 4);
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature; 1937 to 25 February 2020) (Appendix 5);
LILACS BIREME Virtual Health Library (Latin American and Caribbean Health Science Information database; from 1982 to 25 February 2020) (Appendix 6);
We also searched:
VIP Database (January 2012 to 8 March 2020) (Appendix 7).
For previous versions of this review, we searched the Chinese Biomedical Literature Database, the China National Knowledge Infrastructure and the Wan Fang Database from inception to 14 January 2013 (see Appendix 8 for details). However, for this update, we did not search these databases as we found that they were adequately covered by searches of the VIP Database.
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. The Embase subject search was combined with a subject strategy adaptation of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials, as described in the Cochrane Handbook for Systematic Reviews of Interventions, Technical Supplement to Chapter 4 (Lefebvre 2019).
Searching other resources
The following trials registries were searched for ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 25 February 2020) (see Appendix 9);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 25 February 2020) (see Appendix 10).
We manually checked all the references lists of the included studies and relevant systematic reviews to identify any additional studies.
We contacted the first or corresponding authors of the included studies, other experts in the field, and manufacturers of oral hygiene products to request unpublished relevant information.
We checked that none of the included studies in this review were retracted due to error or fraud.
We did not perform a separate search for adverse effects of interventions used; we considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
At least two of six review authors independently examined each title and abstract of articles obtained from the searches. The search was designed to be sensitive and include controlled clinical trials; these were filtered out early in the selection process if they were not randomised. We resolved disagreements by discussion among all authors. We linked multiple reports from a study, and designated the report with the most complete follow‐up data as the primary source of data.
We obtained copies of potentially relevant reports and examined them in detail to determine whether the study fulfilled the eligibility criteria. We resolved any queries by discussion. We attempted to contact study authors to obtain additional information as necessary. We excluded studies when the only information available was from the abstract and this was insufficient to enable full assessment of risk of bias.
Data extraction and management
At least two of six review authors independently extracted data from each included study onto structured data extraction forms that we had designed in advance. We resolved any disagreements by discussion. We extracted the following items:
General characteristics of the study: authors, year of publication, country where the study was performed, funding, language of publication, study duration, citation, contact details for the authors and identifier.
Specific trial characteristics: we collected basic study design characteristics: sequence generation, allocation sequence concealment, blinding, incomplete outcome data and selective outcome reporting, etc., and presented them in the table of 'Characteristics of included studies. We included verbatim quotes on the first three issues from original reports.
Participants: total number, setting, age, sex, country, ethnicity, sociodemographic details (e.g. education level), diagnostic criteria for VAP and the presence of comorbid conditions.
Interventions: we collected details of all experimental and control interventions, such as dosages for drugs used and routes of delivery, format for oral hygiene care, timing and duration of the oral care procedures. We also collected information on any co‐interventions administered.
Outcomes: we collected the incidence of VAP or other respiratory diseases and mortality (directly and indirectly attributable), duration of mechanical ventilation, duration of ICU stay, systemic antibiotic use, oral health indices, and adverse outcomes resulting from the interventions, etc. We specified all outcome variables in terms of definition, timing, units and scales.
Other results: we also collected summary statistics, sample size, key conclusions, comments and any explanations provided for unexpected findings by the study authors. We contacted the lead authors of included studies if there were issues to be clarified.
Assessment of risk of bias in included studies
At least two of six review authors assessed the risk of bias of each included study, using the Cochrane domain‐based, two‐part tool as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We contacted study authors for clarification or missing information where necessary. We resolved any disagreements concerning risk of bias by discussion. We completed a 'Risk of bias' table for each included study. For each domain of risk of bias, we described what was reported to have happened in the study in order to provide a rationale for the second part, which involved assigning a judgement of 'low risk' of bias, 'high risk' of bias, or 'unclear risk' of bias.
For each included study, we assessed the following seven domains of risk of bias.
Random sequence generation (selection bias): use of simple randomisation (e.g. random‐number table, computer‐generated randomisation, central randomisation by a specialised unit), restricted randomisation (e.g. random permuted blocks), stratified randomisation and minimisation were assessed as low risk of bias. Other forms of simple randomisation such as repeated coin‐tossing, throwing dice or dealing cards were also considered as low risk of bias (Schulz 2002). Where a study report used the phrase 'randomised' or 'random allocation' but with no further information, we assessed it as unclear for this domain.
Allocation concealment (selection bias): use of centralised/remote allocation, pharmacy‐controlled randomisation and sequentially‐numbered, sealed, opaque envelopes were assessed as low risk of bias. If a study report did not mention allocation concealment, we assessed it as unclear for this domain.
Blinding of participants and personnel (performance bias): participants in included studies were in intensive care and on mechanical ventilation and were therefore unlikely to be aware of the treatment group to which they were assigned. We therefore assessed caregiver and outcome assessor blinding. Where no placebo was used, caregivers would be aware of the assigned intervention and this would introduce a risk of performance bias. If a study was described as double‐blind and a placebo was used, we assumed that caregivers were blinded to the allocated treatment. If blinding was not mentioned and no placebo was used, we assumed that no blinding of caregivers occurred and we assessed this domain as being at high risk of bias.
Blinding of outcome assessment (detection bias): if outcome assessor blinding was not mentioned in the trial report, we assessed this domain as being at unclear risk of bias.
Incomplete outcome data (attrition bias): where we judged the overall rate of attrition to be high, we assessed the risk of attrition bias as high. If numbers of participants and/or reasons for exclusion were significantly different in each arm of the study, we assessed the risk of attrition bias as high. If numbers of participants randomised or evaluated in each arm of the study were not reported, we assessed this domain as unclear.
Selective reporting (reporting bias): if the study did not report outcomes stated in the Methods section, or reported outcomes without estimates of variance, we assessed the study as being at high risk of reporting bias.
Other bias: any other potential source of bias that might feasibly alter the magnitude of the effect estimate, e.g. baseline imbalance between study arms in important prognostic factors (e.g. clinical pulmonary infection scores (CPIS), antibiotic exposure), early stopping of the trial, or co‐interventions or differences in other treatment between study arms. We described any other potential sources of bias and assessed their risk of bias.
We summarised the overall risks of bias as follows.
| Risk of bias | Interpretation | In outcome | In included studies |
| Low risk of bias | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information is from studies at low risk of bias |
| Unclear risk of bias | Plausible bias that raises some doubt about the results | Unclear risk of bias for one or more key domains | Most information is from studies at low or unclear risk of bias |
| High risk of bias | Plausible bias that seriously weakens confidence in the results | High risk of bias for one or more key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results |
We present the risk of bias graphically by: (a) proportion of studies with each judgement (low, high, or 'unclear risk of bias) for each domain, and (b) cross‐tabulation of judgements by study and by domain (Figure 1; Figure 2).
1.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
2.

Risk of bias summary graph: review authors' judgements about each risk of bias item for each included study
Measures of treatment effect
For dichotomous outcomes, we computed the effect measure as the risk ratio (RR) together with the 95% confidence interval (CI). For continuous outcomes, we used the mean difference (MD) with 95% CI to estimate the summary effect. If different scales were used, we calculated the standardised mean difference (SMD).
Unit of analysis issues
The unit of analysis was the participant. The indices of plaque and gingivitis were measured as mean values for the participants. Episodes of care were also related back to individual participants.
Dealing with missing data
We contacted the lead author of studies requesting that they supply any missing data. We planned to obtain missing standard deviations using the methods outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
To detect heterogeneity among studies in a meta‐analysis, we applied a Chi2 test with a 0.10 level of significance as the cut‐off value. We quantified the impact of statistical heterogeneity using the I2 statistic. To interpret the results, we used the thresholds of I2 recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011):
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity.
If considerable heterogeneity existed, we investigated it using subgroup analyses.
Assessment of reporting biases
Only a proportion of research projects conducted are ultimately published in an indexed journal and become easily identifiable for inclusion in systematic reviews. Reporting biases arise when the reporting of research findings is influenced by the nature and direction of the findings of the research. We investigated and attempted to minimise potential reporting biases in this review, including publication bias, time lag bias, multiple (duplicate) publication bias, and language bias.
We planned to construct funnel plots where there were more than 10 studies in an outcome. We planned to investigate any asymmetry in the funnel plot (indicating possible publication bias) by undertaking statistical analysis using the methods introduced by Egger 1997 (continuous outcome) and Rücker 2008 (dichotomous outcome) (such analysis would have been done in Stata).
Data synthesis
We undertook meta‐analyses for similar comparisons and the same outcomes across studies. We used random‐effects models providing there were four or more trials in any one meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We proposed several subgroup analyses a priori. We decided to undertake a subgroup analysis according to whether participants' teeth were cleaned by toothbrushing or not, as we hypothesised that antiseptics would be less effective if toothbrushing was not used to disrupt dental plaque biofilm. We also planned to perform subgroup analyses by grouping studies according to concentration of the intervention.
Sensitivity analysis
To determine whether the intervention effects of oral hygiene care were robust, we planned to perform sensitivity analyses to assess the effect on the estimates of effect of studies with questionable diagnostic criteria for VAP, by excluding studies with high risk of bias, or by changing our assumptions about missing data.
If the results had not changed substantially in sensitivity analyses, we would have regarded our conclusions as stable with a higher degree of certainty. If sensitivity analyses had identified particular factors that greatly influenced the conclusions of the review, we would have explored the plausible causes of the uncertainties and interpreted the results with more caution.
Summary of findings and assessment of the certainty of the evidence
Consistent with the last version of this review, we prepared 'Summary of findings' tables for two main comparisons: chlorhexidine versus placebo/usual care, and toothbrushing versus no toothbrushing, using the GRADE system for evaluating certainty of the evidence from systematic reviews (Guyatt 2008; Higgins 2011) and the software GRADEpro (GRADEpro 2020). We included the following outcomes in the 'Summary of findings' tables: incidence of VAP, mortality, duration of ventilation, duration of ICU stay, and adverse effects. We assessed the certainty of the body of evidence with reference to the overall risk of bias of the included studies, the directness of the evidence, the consistency of the results, the precision of the estimates, and the risk of publication bias. We classified the certainty of the body of evidence into four categories: high, moderate, low and very low.
Results
Description of studies
Results of the search
For this review update, we identified 385 records from electronic databases and other resources after removal of duplicates. At least two review authors screened all records against the review inclusion criteria. We discarded 350 records as not relevant, and identified 10 additional records of studies awaiting classification (see Characteristics of studies awaiting classification) and two ongoing trials (see Characteristics of ongoing studies). We requested full‐text copies of the remaining 23 references. At least two review authors assessed these papers to determine their eligibility: we excluded 10 studies for reasons described in Characteristics of excluded studies; four studies await classification until we have further information (see Characteristics of studies awaiting classification); and we deemed nine studies eligible for inclusion. In the previous version of the review, there were 38 included studies, but we excluded seven of these from this update (Chen 2008; DeRiso 1996; Fourrier 2000; Fourrier 2005; Jacomo 2011; Munro 2009; Sebastian 2012) (see below and Characteristics of excluded studies tables for details). Therefore, the total number of studies in this update is 40. The study selection process is depicted in Figure 3.
3.
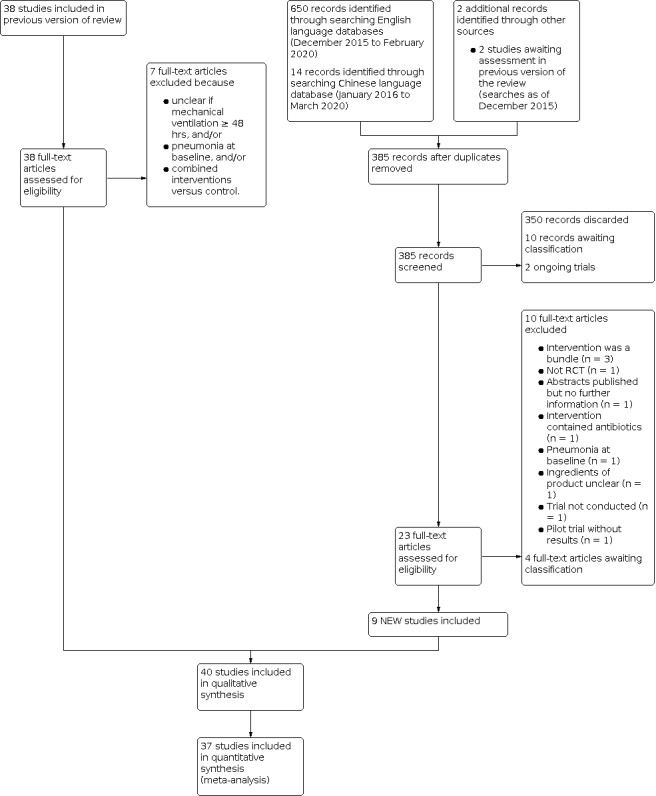
Study flow diagram
Included studies
We included 40 RCTs in this review.
Setting
Ten of the included studies were conducted in China (Feng 2012; Fu 2019; Hu 2009; Long 2012; Mo 2016; Tang 2013; Xu 2007; Xu 2008; Yao 2011; Zhao 2012), six in the USA (Bopp 2006; Fields 2008; Grap 2011; Prendergast 2012; Scannapieco 2009; Stefanescu 2013), six in Brazil (Bellissimo‐Rodrigues 2009; Caruso 2009; De Lacerda 2017; Kusahara 2012a; Meinberg 2012; Tuon 2017), five in Iran (Hanifi 2017; Irani 2019; Khaky 2018; Meidani 2018; Nobahar 2016), three in Spain (Lorente 2012; Pobo 2009; Roca Biosca 2011), two in France (Seguin 2006; Seguin 2014), two in India (Dahiya 2012; Panchabhai 2009), two in Australia (Berry 2011; Berry 2013), and one each in Croatia (Cabov 2010), Thailand (Tantipong 2008), Turkey (Ozcaka 2012), and the Netherlands (Koeman 2006).
All studies took place in ICUs in hospitals. Most of the studies were two‐arm parallel‐group RCTs, but seven studies had three arms (Berry 2011; Berry 2013; Fu 2019; Meidani 2018; Scannapieco 2009; Seguin 2006; Xu 2007).
Participants
There were 5675 participants randomly allocated to treatment in 39 RCTs, and the other trial (Fields 2008) did not state how many participants were included. The criteria for inclusion in these studies generally specified no prior intubation, no clinically‐apparent pneumonia at baseline, and an expected requirement for mechanical ventilation for a minimum of 48 hours. Participants were critically ill and required assistance from nursing staff for their oral hygiene care. In two of the included studies, participants were children (Kusahara 2012a; Stefanescu 2013); one of which enrolled only neonates (Stefanescu 2013). In the remaining studies, only adults participated.
In seven studies, participants were either medical or surgical patients (Berry 2013; De Lacerda 2017; Koeman 2006; Meinberg 2012; Mo 2016; Nobahar 2016; Panchabhai 2009); in another seven studies, participants were described as trauma patients (Grap 2011; Hanifi 2017; Irani 2019; Prendergast 2012; Scannapieco 2009; Seguin 2006; Seguin 2014); four studies recruited surgical patients only (Fu 2019; Kusahara 2012a; Yao 2011; Zhao 2012); six studies recruited medical patients only (Cabov 2010; Fields 2008; Ozcaka 2012; Stefanescu 2013; Tang 2013; Tantipong 2008); and in the remaining studies, it was not clearly stated whether participants were medical, surgical, or trauma cases.
Nine of the included studies specifically excluded edentulous participants (De Lacerda 2017; Fields 2008; Grap 2011; Lorente 2012; Ozcaka 2012; Pobo 2009; Prendergast 2012; Roca Biosca 2011; Tuon 2017), and the remaining studies did not report whether or not participants were dentate.
Classification of the interventions
We classified the interventions into three broad groups.
-
Chlorhexidine
Chlorhexidine solution (applied as mouthrinse, spray or on a swab)
Chlorhexidine gel
-
Toothbrushing
Powered
Manual
-
Other agents
Povidone iodine
Saline
Bicarbonate
Triclosan
Furacilin
Listerine
Biotene OralBalance
Hydrogen peroxide
Potassium permanganate
Ozonated water
Nanosil
Miswak
These interventions were used either singly or in combinations. We evaluated the following comparisons.
Chlorhexidine versus placebo/usual care, with or without toothbrushing (13 studies: Bellissimo‐Rodrigues 2009; Berry 2011; Cabov 2010; Fu 2019; Grap 2011; Koeman 2006; Kusahara 2012a; Meidani 2018; Meinberg 2012; Ozcaka 2012; Scannapieco 2009; Tantipong 2008; Tuon 2017)
Chlorhexidine versus other oral care agents (7 studies), including potassium permanganate (Meidani 2018; Panchabhai 2009), ozonated water (Hanifi 2017), miswak (Irani 2019), Nanosil (Khaky 2018), hydrogen peroxide (Bopp 2006; Dahiya 2012).
Toothbrushing versus no toothbrushing (in addition to usual care) (8 studies: Bopp 2006; De Lacerda 2017; Fields 2008; Lorente 2012; Long 2012; Pobo 2009; Roca Biosca 2011; Yao 2011)
Powered toothbrushing versus manual toothbrushing (one study: Prendergast 2012)
Other oral care agents (17 studies), including saline (Caruso 2009; Hu 2009; Mo 2016; Seguin 2006; Tang 2013; Xu 2007; Xu 2008), bicarbonate (Berry 2011; Berry 2013), povidone iodine (Feng 2012; Seguin 2006; Seguin 2014), triclosan (Zhao 2012), furacilin (Feng 2012), Listerine (Berry 2013), Biotene OralBalance (Stefanescu 2013), hydrogen peroxide (Nobahar 2016), potassium permanganate (Meidani 2018)
There was some variation between the studies in the number of episodes of OHC per day, with most of the studies delivering two to four episodes of OHC daily. Seventeen studies delivered two episodes of OHC a day (Berry 2011; Bopp 2006; Dahiya 2012; De Lacerda 2017; Fields 2008; Fu 2019; Hu 2009; Irani 2019; Kusahara 2012a; Nobahar 2016; Panchabhai 2009; Prendergast 2012; Scannapieco 2009; Tuon 2017; Xu 2007; Xu 2008; Yao 2011); eight studies had three episodes a day (Bellissimo‐Rodrigues 2009; Cabov 2010; Hanifi 2017; Khaky 2018; Long 2012; Lorente 2012; Meidani 2018; Pobo 2009), and seven studies had four episodes a day (Feng 2012; Koeman 2006; Meinberg 2012; Mo 2016; Ozcaka 2012; Tantipong 2008; Zhao 2012). One study delivered OHC every two hours (Berry 2013), another only once (Grap 2011), and, in the remaining three studies, it was unclear (Caruso 2009; Roca Biosca 2011; Tang 2013).
In some of the included studies, the control intervention described as 'placebo' may have had some antibacterial activity, but this was considered by the trialists to be negligible compared to the active intervention. Such control interventions included saline (Feng 2012; Fu 2019; Hu 2009; Ozcaka 2012; Seguin 2006; Tantipong 2008; Tuon 2017), potassium permanganate (Panchabhai 2009), half‐strength hydrogen peroxide (Bopp 2006), placebo gel (Koeman 2006; Kusahara 2012a; Meinberg 2012), base solution (Scannapieco 2009) or water (Berry 2011; Berry 2013). In two trials, the nature of the placebo was not specified (Bellissimo‐Rodrigues 2009; Meidani 2018).
In eight studies, the control group received usual/standard care (Caruso 2009; Fields 2008; Hu 2009; Grap 2011; Pobo 2009; Roca Biosca 2011; Seguin 2006; Yao 2011) (for specific details see Characteristics of included studies), and in nine studies, there was a head‐to‐head comparison between two potentially active interventions (Berry 2013; Dahiya 2012; Feng 2012; Hanifi 2017; Irani 2019; Khaky 2018; Meidani 2018; Panchabhai 2009; Prendergast 2012).
Measures of primary outcomes
Incidence of VAP
The primary outcome of our review is ventilator‐associated pneumonia (VAP), defined as pneumonia developing in a person who has been on mechanical ventilation for at least 48 hours. VAP was fully reported by 38 of the included studies (Bellissimo‐Rodrigues 2009; Berry 2011; Berry 2013; Bopp 2006; Cabov 2010; Caruso 2009; Dahiya 2012; De Lacerda 2017; Feng 2012; Fu 2019; Grap 2011; Hanifi 2017; Hu 2009; Irani 2019; Khaky 2018; Koeman 2006; Kusahara 2012a; Long 2012; Lorente 2012; Meidani 2018; Meinberg 2012; Mo 2016; Nobahar 2016; Ozcaka 2012; Panchabhai 2009; Pobo 2009; Prendergast 2012; Scannapieco 2009; Seguin 2006; Seguin 2014; Stefanescu 2013; Tang 2013; Tantipong 2008; Tuon 2017; Xu 2007; Xu 2008; Yao 2011; Zhao 2012). One study only reported that there was no difference in VAP between the two arms of the study (Roca Biosca 2011). One study reported that the VAP rate dropped to zero in the intervention group but the control group event rate was not reported (Fields 2008).
Diagnostic criteria for the outcome of ventilator‐associated pneumonia were specified in 37 studies. Seventeen studies used Pugin's criteria (Cook 1998; Pugin 1991), which form the basis of the CPIS score, based on the presence of an infiltrate on chest radiograph, plus two or more of the following: temperature greater than 38.5º C or less than 35º C, white blood cell count greater than 11,000/mm3 or less than 4000/mm3, mucopurulent or purulent bronchial secretions, or more than 20% increase in fraction of inspired oxygen required to maintain saturation above 92% (Berry 2011; Berry 2013; Cabov 2010; Caruso 2009; Grap 2011; Hanifi 2017; Koeman 2006; Kusahara 2012a; Meinberg 2012; Pobo 2009; Scannapieco 2009; Seguin 2006; Seguin 2014; Tantipong 2008; Yao 2011). Three studies used the modified clinical pulmonary infection score (MCPIS) (Irani 2019; Khaky 2018; Nobahar 2016). In Ozcaka 2012, no specific criteria were reported, but communication with the author confirmed that participants with new pulmonary infiltrates or opacities on the chest X‐ray were prediagnosed with VAP; lower tracheal mini‐bronchoalveolar lavage (mini‐BAL) samples were taken and then participants were diagnosed according to CPIS criteria. Those who had a score of six or more and the presence of 104 or more colony‐forming units/mL of a target potential respiratory bacterial pathogen (PRP) in mini‐BAL were diagnosed with VAP.
A further six studies used the CDC criteria as described in Horan 2008 (Bellissimo‐Rodrigues 2009; Dahiya 2012; Fields 2008; Meidani 2018; Panchabhai 2009; Tuon 2017). Stefanescu 2013 used CDC criteria for diagnosis of neonatal VAP.
Five studies used the criteria of the Chinese Society of Respiratory Diseases: presence of new infiltrates on chest radiographs developed after 48 hours of mechanical ventilation with any two of the following items: (a) temperature greater than 38º C, (b) change in characteristics of bronchial secretions from mucoid to mucopurulent or purulent, (c) white cell count greater than 10,000/mm3, (d) positive culture of tracheal aspirate or positive culture of bronchoalveolar lavage fluid or both, or (e) arterial oxygen tension/inspiratory fraction of oxygen PaO2/FiO2 decreased over 30% within the period of ventilation (Feng 2012; Mo 2016; Tang 2013; Xu 2007; Xu 2008).
De Lacerda 2017 used the American Thoracic Society criteria (ATS Guideline 2005) for diagnosis. Hu 2009 reported the outcome of VAP based on clinical examination plus three criteria: chest radiograph, white cell count and culture of the aspirate from lower respiratory tract (but no precise parameters were specified). In Lorente 2012, the diagnosis of VAP was made by an expert panel blinded to the allocated intervention, but the diagnostic criteria were not specified. Prendergast 2012 had a single diagnostic criterion of a new or worsening pulmonary infiltrate on chest radiograph. Two studies used positive culture from the lower respiratory tract as criteria for diagnosis of VAP (Long 2012; Zhao 2012).
The remaining three studies with the outcome of VAP did not report their diagnostic criteria (Bopp 2006; Fu 2019; Roca Biosca 2011).
Among the above‐mentioned studies that provided data on incidence of VAP, 28 reported their follow‐up length/time point of measurement for this outcome. In 10 of these studies, the length of follow‐up was between three to nine days (Berry 2011; Berry 2013; Dahiya 2012; Grap 2011; Hanifi 2017; Irani 2019; Khaky 2018; Nobahar 2016; Prendergast 2012; Yao 2011), while in another 10 studies, the length of follow‐up was between 10 to 30 days (Caruso 2009; De Lacerda 2017; Hu 2009; Ozcaka 2012; Pobo 2009; Scannapieco 2009; Seguin 2014; Tang 2013; Xu 2008; Zhao 2012). In the remaining five studies, the reported end of follow‐up was discharge from the ICU (Bellissimo‐Rodrigues 2009; Cabov 2010; Kusahara 2012a; Panchabhai 2009; Stefanescu 2013).
Mortality
Twenty‐two studies reported the outcome of mortality, either as ICU mortality or 30‐day mortality (Bellissimo‐Rodrigues 2009; Cabov 2010; Caruso 2009; De Lacerda 2017; Fu 2019; Kusahara 2012a; Long 2012; Lorente 2012; Meidani 2018; Meinberg 2012; Mo 2016; Ozcaka 2012; Panchabhai 2009; Pobo 2009; Prendergast 2012; Scannapieco 2009; Seguin 2006; Seguin 2014; Stefanescu 2013; Tang 2013; Tantipong 2008; Yao 2011). Where ICU mortality was reported, we used these data; where ICU mortality was not reported, we used 30‐day mortality.
Measures of secondary outcomes
Duration of ventilation
Seventeen studies reported this outcome (Bellissimo‐Rodrigues 2009; Caruso 2009; De Lacerda 2017; Fu 2019; Hu 2009; Koeman 2006; Long 2012; Lorente 2012; Meidani 2018; Ozcaka 2012; Pobo 2009; Prendergast 2012; Scannapieco 2009; Seguin 2006; Tang 2013; Xu 2008; Zhao 2012). Berry 2013 and Meinberg 2012 reported the median duration of ventilation or the range for each group or both, but we could not combine these data in a meta‐analysis. Unless explicitly reported otherwise, we have assumed that all studies used similar methods to calculate these data including participants who died. Stefanescu 2013 reported only a P value for the difference between groups in duration of ventilation.
Duration of ICU stay
Sixteen studies reported this outcome (Bellissimo‐Rodrigues 2009; Bopp 2006; Caruso 2009; De Lacerda 2017; Fu 2019; Koeman 2006; Kusahara 2012a; Lorente 2012; Meidani 2018; Ozcaka 2012; Panchabhai 2009; Pobo 2009; Prendergast 2012; Seguin 2006; Seguin 2014; Zhao 2012). Berry 2013 and Meinberg 2012 reported the median ICU stay and the range for each group, but we could not combine these data in a meta‐analysis. Unless explicitly reported otherwise, we have assumed that all studies used similar methods to calculate these data including participants who died.
Systemic antibiotic therapy
Five studies reported some measure of systemic antibiotic use. Irani 2019, Seguin 2014 and Tuon 2017 reported the number of participants who were treated with antibiotics. Scannapieco 2009 reported the mean number of days of systemic antibiotic use in the intervention and control groups. Berry 2013 reported only a P value for the difference between groups in antibiotic administration.
Oral health indices
Plaque indices were mentioned as outcomes in five studies (Fu 2019; Ozcaka 2012; Roca Biosca 2011; Scannapieco 2009; Yao 2011). Complete data for plaque indices were reported in two studies (Fu 2019; Ozcaka 2012), and were supplied by the corresponding author of one study (Yao 2011). Scannapieco 2009 reported this outcome in graphs only, and Roca Biosca 2011 did not report any estimate of variance, so we could not use these data in this review.
Adverse effects
Most studies did not mention adverse effects in their reports. Two studies reported the adverse effects of the interventions (Seguin 2014; Tantipong 2008); four studies reported that there were no adverse effects (Berry 2011; Berry 2013; De Lacerda 2017; Ozcaka 2012); and one study (Stefanescu 2013) reported no significant difference between groups with respect to adverse events in buccal mucosa.
Excluded studies
In this update, we excluded 17 studies for the reasons summarised below. Seven studies that we included in the previous version of the review are excluded from this version (Chen 2008; DeRiso 1996; Fourrier 2000; Fourrier 2005; Jacomo 2011; Munro 2009; Sebastian 2012).
Guo 2017 and Sebastian 2012 were excluded because the participants had pneumonia at baseline.
In Fourrier 2005, it was unclear if some of the participants had pneumonia at baseline and if all those who developed VAP had been on mechanical ventilation for at least 48 hours.
DeRiso 1996 and Fourrier 2000 were excluded because it was unclear if all those who developed VAP had been on mechanical ventilation for at least 48 hours.
In Jacomo 2011, it was unclear how many participants were on mechanical ventilation for at least 48 hours.
Nasiriani 2016 was excluded because the authors replaced 22 dropouts with new participants (selection method unknown) and thereby compromised the randomisation.
Four studies were excluded because the intervention of interest was a bundle that included not only OHC (Atashi 2018; Chen 2008; Dale 2019; Haghighi 2017).
Tsai 2017 was reported as abstract only and our attempts to find a full publication or obtain sufficient data to enable inclusion in this review were unsuccessful.
Wang 2016 was excluded because the CHX solution used for interventions contained antibiotics.
Tian 2017 was excluded because authors did not report either the ingredients or product name of the 'biological enzyme disinfectant' used, therefore we could not judge whether it contained antibiotics. The authors' contact information was also not provided.
One study was excluded because it was a pilot trial and patient outcomes were not collected (NCT01657396).
Da Collina 2017 was excluded because the trial was not performed.
For further information, see the Characteristics of excluded studies table, which also provides information on studies excluded in the last version of this review.
Risk of bias in included studies
Overall risk of bias
Overall, we rated just two of the included studies (5%) as having low risk of bias for all domains (Koeman 2006; Seguin 2014), and nine studies (23%) were at unclear risk of bias for at least one domain. Over two‐thirds of the included studies (29 studies, 73%) were at high risk of bias in at least one domain (see Figure 1; Figure 2).
Allocation
Sequence generation
Twenty‐three of the included studies clearly described a random method of sequence generation and we assessed them as at low risk of bias for this domain. The remaining 17 studies stated that allocation was random but provided no further details and we therefore assessed them as having unclear risk of bias for this domain (Bellissimo‐Rodrigues 2009; Caruso 2009; Dahiya 2012; Feng 2012; Fields 2008; Khaky 2018; Long 2012; Meidani 2018; Meinberg 2012; Ozcaka 2012; Panchabhai 2009; Roca Biosca 2011; Tang 2013; Tuon 2017; Xu 2007; Xu 2008; Zhao 2012).
Allocation concealment
Allocation concealment was clearly described in 20 of the included studies and we assessed them as at low risk of bias for this domain. In 22 studies, allocation concealment was not described in sufficient detail to determine risk of bias and we rated these studies as having unclear risk of bias (Cabov 2010; Caruso 2009; Feng 2012; Fu 2019; Grap 2011; Hanifi 2017; Irani 2019; Khaky 2018; Long 2012; Lorente 2012; Meidani 2018; Mo 2016; Nobahar 2016; Ozcaka 2012; Panchabhai 2009; Tang 2013; Tantipong 2008; Tuon 2017; Xu 2007; Xu 2008; Yao 2011; Zhao 2012). We assessed Bopp 2006 as having high risk of bias because the allocation was not concealed from the researchers.
The risk of selection bias based on combined assessment of these two domains was high in one study (Bopp 2006), unclear in 24 studies (Dahiya 2012; Cabov 2010; Caruso 2009; Feng 2012; Fields 2008; Fu 2019; Grap 2011; Hanifi 2017; Khaky 2018; Long 2012; Lorente 2012; Meidani 2018; Mo 2016; Nobahar 2016; Irani 2019; Panchabhai 2009; Roca Biosca 2011; Tang 2013; Tantipong 2008; Tuon 2017; Xu 2007; Xu 2008; Yao 2011; Zhao 2012), and low in the remaining 15 studies.
Blinding
Eight studies were described as double‐blind and we assessed them as having low risk of performance bias (Bellissimo‐Rodrigues 2009; Cabov 2010; Koeman 2006; Kusahara 2012a; Meinberg 2012; Ozcaka 2012; Scannapieco 2009; Seguin 2014). There was insufficient information to determine whether blinding occurred in four studies (Caruso 2009; Nobahar 2016; Tuon 2017; Zhao 2012). In the remaining 28 studies, blinding of the participants and their caregivers to the allocated treatment was not possible because the active and control treatments were so different, and no placebos were used. We assessed these studies as having high risk of performance bias.
Blinding of outcome assessment was possible in all of the included studies and was described in 21 studies (Bellissimo‐Rodrigues 2009; Berry 2011; Berry 2013; Cabov 2010; Caruso 2009; Dahiya 2012; De Lacerda 2017; Hanifi 2017; Hu 2009; Irani 2019; Kusahara 2012a; Lorente 2012; Meinberg 2012; Ozcaka 2012; Panchabhai 2009; Pobo 2009; Prendergast 2012; Scannapieco 2009; Seguin 2014; Tantipong 2008; Yao 2011), which we assessed as being at low risk of detection bias. One of the included studies reported no blinding of outcome assessment and we assessed it as having high risk of detection bias (Bopp 2006). In the remaining 18 studies, there was insufficient information provided and we rated the risk of detection bias as unclear.
Incomplete outcome data
In the studies included in this review, loss of participants during the course of the study is to be expected, as these critically ill people leave the intensive care unit either because they recover and no longer require mechanical ventilation, or because they die from their illness. In 27 of the included studies, either all the randomised participants were included in the outcome, or the number of losses/withdrawals and the reasons given were similar in both arms of the study, and we assessed these studies as at low risk of attrition bias (Bellissimo‐Rodrigues 2009; Bopp 2006; Cabov 2010; Caruso 2009; Dahiya 2012; De Lacerda 2017; Feng 2012; Fu 2019; Irani 2019; Koeman 2006; Kusahara 2012a; Long 2012; Lorente 2012; Meinberg 2012; Mo 2016; Nobahar 2016; Ozcaka 2012; Pobo 2009; Seguin 2006; Seguin 2014, Stefanescu 2013; Tang 2013; Tuon 2017; Xu 2007; Xu 2008; Yao 2011; Zhao 2012).
We rated eight of the included studies as having high risk of attrition bias, because the numbers and reasons for withdrawal/exclusion were different in each arm of the study, or because the number of participants withdrawn or excluded from the outcomes evaluation was high and insufficient information was provided (Berry 2011; Berry 2013; Fields 2008; Grap 2011; Hu 2009; Prendergast 2012; Roca Biosca 2011; Scannapieco 2009). In the remaining five studies, there was insufficient information available to determine the risk of attrition bias.
Selective reporting
Twenty‐seven of the included studies reported the outcomes specified in their Methods section in full, or this information was supplied by trial authors, and we assessed these studies as being at low risk of reporting bias (Bellissimo‐Rodrigues 2009; Berry 2011; Cabov 2010; Caruso 2009; Dahiya 2012; De Lacerda 2017; Feng 2012; Fu 2019; Hanifi 2017; Koeman 2006; Kusahara 2012a; Long 2012; Lorente 2012; Mo 2016; Ozcaka 2012; Panchabhai 2009; Pobo 2009; Prendergast 2012; Seguin 2006; Seguin 2014; Stefanescu 2013; Tang 2013; Tuon 2017; Xu 2007; Xu 2008; Yao 2011; Zhao 2012).
Six studies did not report all the outcomes specified in their Methods sections (Grap 2011; Irani 2019; Khaky 2018; Meinberg 2012; Nobahar 2016; Roca Biosca 2011); two studies reported outcomes as percentages only, with unclear denominators for each arm (Berry 2013; Hu 2009); and one study did not report the number of participants evaluated (Fields 2008). We rated these nine trials as at high risk of reporting bias.
We assessed the remaining four trials as being at unclear risk of reporting bias, because there was insufficient information reported to make a clear judgement (Bopp 2006; Meidani 2018; Scannapieco 2009; Tantipong 2008).
Other potential sources of bias
We rated five studies as at high risk of other bias. Three studies were stopped early (Berry 2011; Meinberg 2012; Pobo 2009). Berry 2011 was stopped due to withdrawal of one of the investigational products by a regulatory authority. Pobo 2009 was stopped after 37% of the planned 400 participants had been recruited because there appeared to be no difference between the study arms in the outcome of VAP. Meinberg 2012 was stopped due to "futility"; however, we were unsure whether this was the main problem. Grap 2011 did not report baseline data for each randomised treatment group but the trial report noted that there was a "statistically significant difference in gender and CPIS score between groups at baseline", and we considered that this difference was likely to have biased the results. In Scannapieco 2009, the imputations used for the missing data were unclear and the pre‐study exposure to systemic antibiotics was greater in the control group, so we assessed this study as having high risk of other bias.
In 15 studies, we rated the risk of other bias as unclear (Berry 2013; Dahiya 2012; De Lacerda 2017; Fields 2008; Fu 2019; Kusahara 2012a; Long 2012; Meidani 2018; Panchabhai 2009; Roca Biosca 2011; Stefanescu 2013; Tang 2013; Tantipong 2008; Yao 2011; Zhao 2012). The reasons for this are as follows.
In Berry 2013, ineligible participants were included in the ITT analysis, but reasons for ineligibility in each group were not given;
In Dahiya 2012; Fields 2008; Meidani 2018 and Roca Biosca 2011, the study reports contained insufficient information for us to be confident that study methodology was robust;
In Stefanescu 2013, more infants in the control group received a complete course of antenatal steroids compared to infants in the Biotene OralBalance group (P = 0.045). A complete course of antenatal steroids improves antenatal lung maturity and function and may reduce the risk of VAP (Roberts 2017). This imbalance is likely to lead to an underestimate of the benefit of the active treatment;
In Kusahara 2012a, there was a statistically significant difference in the age of the children in each arm of the study and we were unclear whether this was associated with potential bias;
Panchabhai 2009 reported baseline characteristics only for those participants completing the study;
In Tang 2013, a detailed description about the intervention methods and frequency of oral care in each group was not reported;
Tantipong 2008 included participants treated in different units of the hospital where care and co‐interventions were likely to have been different;
In Yao 2011, there was no information as to how the edentulous participants in each arm were treated;
Long 2012 and Zhao 2012 reported the criteria for VAP diagnosis as being positive culture of lower respiratory tract secretions, with no other criteria, and it was unclear if this would have introduced a bias in these unblinded studies;
Fu 2019 did not report the criteria used for VAP diagnosis, and it was unclear if this would have introduced a bias;
In De Lacerda 2017, there was an imbalance between two groups in the method of CHX application (CHX gel vs. CHX solution).
We assessed the remaining 20 studies as having low risk of other bias.
Effects of interventions
Comparison 1: Chlorhexidine versus placebo/usual care (with or without toothbrushing)
Chlorhexidine antiseptic was evaluated in 13 studies included in this review.
Concentration of the chlorhexidine used was 2% in four studies (Koeman 2006; Meinberg 2012; Tantipong 2008; Tuon 2017), 0.2% in three studies (Berry 2011; Cabov 2010; Meidani 2018), and 0.12% in the remaining studies.
We assessed seven of the 13 studies as having high risk of bias (Berry 2011; Fu 2019; Grap 2011; Meidani 2018; Meinberg 2012; Scannapieco 2009; Tantipong 2008), one study as at low risk of bias (Koeman 2006;), and the remaining five studies as at unclear risk of bias.
We subgrouped these studies according to whether chlorhexidine was administered as a liquid mouthrinse or a gel, and whether chlorhexidine was used in conjunction with toothbrushing or not.
Incidence of VAP
Overall, the meta‐analysis of 13 studies using any form of chlorhexidine (seven studies at high risk of bias, five at unclear risk of bias and one at low risk of bias) showed that CHX probably reduced the incidence of VAP (risk ratio (RR) 0.67, 95% confidence interval (CI) 0.47 to 0.97, P = 0.05, I2 = 72%; 1206 participants; moderate‐certainty evidence) (Analysis 1.1). This equates to a number needed to treat for an additional beneficial outcome (NNTB) of 12 (95% CI 7 to 128).
1.1. Analysis.

Comparison 1: Chlorhexidine versus placebo/usual care, Outcome 1: Incidence of VAP
Six studies (429 participants) compared chlorhexidine solution (2%, 0.12% or 0.2%) with either placebo (Bellissimo‐Rodrigues 2009; Fu 2019; Meidani 2018; Ozcaka 2012; Tuon 2017) or 'usual care' (Grap 2011) without toothbrushing. Four of these studies reported the use of a swab, either to clean the mouth prior to chlorhexidine application or to ensure that the chlorhexidine solution was applied to all oral surfaces. Tuon 2017 applied CHX through mouth‐rinsing. In the other study (Meidani 2018), the mode of application was unclear. The meta‐analysis showed a reduction in VAP in the chlorhexidine group (RR 0.57, 95% CI 0.33 to 1.00, P = 0.05, I2 = 72%) (Analysis 1.1, subgroup 1.1.1).
A further two studies (297 participants) compared chlorhexidine gel (0.2% or 2%) versus placebo, with no toothbrushing in either group (one of the studies administered 0.2% chlorhexidine gel three times daily following rinsing of the mouth and aspiration of rinse (Cabov 2010), and the other study used a gel with higher chlorhexidine concentration (2%) and applied the gel using a swab (Koeman 2006)). Meta‐analysis showed a reduction in the risk of VAP for CHX gel (RR 0.53, 95% CI 0.29 to 0.97, P = 0.04, I2 = 0%) (Analysis 1.1, subgroup 1.1.2).
Three studies (332 participants) compared chlorhexidine solution (2%, 0.12% or 0.2%) with placebo (with toothbrushing in both groups). The meta‐analysis showed no evidence of a difference in VAP between the groups (RR 0.74, 95% CI 0.29 to 1.89, P = 0.53, I2 = 53%) (Analysis 1.1, subgroup 1.1.3).
Two further studies (Kusahara 2012a; Meinberg 2012, including 52 adults and 96 children), at high and unclear risk of bias, compared chlorhexidine gel (2% and 0.12%) with placebo (with toothbrushing in both groups) and found no difference in the incidence of VAP (RR 1.22, 95% CI 0.83 to 1.79, P = 0.32, I2 = 0%) (Analysis 1.1, subgroup 1.1.4).
Mortality
The outcome of mortality was reported in nine studies (944 participants), and overall the meta‐analysis showed that there may not be a difference between chlorhexidine and placebo/usual care (RR 1.02, 95% CI 0.84 to 1.23, P = 0.86, I2 = 0%; moderate‐certainty evidence) (Analysis 1.2). There was no evidence of a difference in mortality between (P = 0.99, I2 = 0%) or within the subgroups (chlorhexidine mouthrinse/gel with or without toothbrushing) (Analysis 1.2).
1.2. Analysis.

Comparison 1: Chlorhexidine versus placebo/usual care, Outcome 2: Mortality
Duration of ventilation
From the four studies (594 participants) that reported data in a way that could be combined in meta‐analysis, we did not find evidence of a difference in the duration of ventilation (days) between groups receiving chlorhexidine compared to those receiving placebo/usual care (mean difference (MD) ‐1.10 days, 95% CI ‐3.20 to 1.00 days, P = 0.30, I2 = 74%; very low‐certainty evidence) (Analysis 1.3).
1.3. Analysis.

Comparison 1: Chlorhexidine versus placebo/usual care, Outcome 3: Duration of ventilation (days)
There was some evidence of a reduction in duration of ventilation in Analysis 1.3, subgroup 1.3.1 (MD ‐2.63 days, 95% CI ‐3.35 to ‐1.90 days, P < 0.00001, I2 = 0%), and insufficient evidence (based on a single study) to determine whether or not there was a difference in Analysis 1.3, subgroup 1.3.2 or Analysis 1.3, subgroup 1.3.3.
A further study (Meinberg 2012), comparing chlorhexidine gel and placebo, also found no difference in duration of ventilation (Additional Table 3).
1. Other outcome data from included studies.
| Comparison | Number of participants | Outcome | Data | Effect estimate (95% CI) |
| CHX versus sodium bicarbonate versus water (Berry 2011) | CHX group: 33; sodium bicarbonate group: 33; water group: 43 | Adverse events | No adverse events were reported associated with interventions | |
| Listerine versus sodium bicarbonate versus sterile water (Berry 2013) | Listerine group: 127; sodium bicarbonate group: 133; sterile water group: 138 | Duration of mechanical ventilation | No significant difference between groups in median ventilation hours (81 hours, SD 1058) | |
| Duration of ICU stay | No significant difference between groups in median length of ICU stay (5 days, SD 29) | |||
| Systemic antibiotic use | No significant difference between groups (P = 0.21) | |||
| Adverse events | No adverse events were reported associated with interventions | |||
| CHX + toothbrushing versus control (Bopp 2006) | CHX + toothbrushing group: 2; control group: 3 | Incidence of VAP | 0 cases in CHX + toothbrushing group and 1 case in control group | |
| Duration of ventilation | Mean 5.5 days (SD 0.39) in toothbrushing group and mean 5 days (SD 0.81) in control group | |||
| Duration of ICU stay | Mean 18 days (SD 1.67) in toothbrushing group and mean 10.3 days (SD 2.70) in control group | |||
| Toothbrush + CHX versus CHX alone (De Lacerda 2017) | Toothbrush + CHX group: 105; CHX group: 108 | Adverse events | No adverse events were reported associated with interventions | |
| Nasosil versus CHX (Khaky 2018) | Nasosil group: 37; CHX group: 38 | Mortality | The Mann‐Whitney test showed that there was no significant difference between the two groups in the mortality rate on the first and fifth day of study (P > 0.05) | |
| CHX versus placebo (Koeman 2006) | CHX group: 127; placebo group:130 | Mortality |
HR | HR 1.12 (95% CI 0.72 to 1.17) |
| CHX versus placebo (Meinberg 2012) | CHX group: 28; placebo group: 24 | Duration of mechanical ventilation | Median days in CHX group 8.5 (interquartile range, 7.3 to 14.7) and median days in placebo group 6 (4 to 12.7) (P = 0.17) | |
| Duration of ICU stay | Median days in CHX group 12 (interquartile range, 9 to 29) and median days in placebo group 11 (5 to 16) (P = 0.36) | |||
| Powered toothbrush + standard oral care versus standard oral care alone (Pobo 2009) | Toothbrush group: 74; control group: 73 | Adverse events | No adverse events were reported associated with interventions | |
| Powered toothbrush + CHX versus CHX alone (Roca Biosca 2011) | Powered toothbrush group: 29; CHX alone group: 32 | Plaque index | Mean in toothbrush group 1.68 and mean in control group 1.91; no estimates of variance but reported that P = 0.7 (no difference) | |
| Incidence of VAP | OR 0.78 (95% CI 0.36 to 1.68, P = 0.56) | |||
| CHX (once daily or twice daily) versus placebo (Scannapieco 2009) | CHX 1x/day group: 47; CHX 2x/day group: 50; placebo group: 49 | Plaque index | No difference between the 3 groups (data presented graphically) | |
| Biotene OralBalance versus control (Stefanescu 2013) | Biotene OralBalance group: 20; control group: 21 | Duration of mechanical ventilation | No difference between groups (P = 0.77) | |
| Adverse events | No significant difference between groups with respect to adverse events in buccal mucosa |
CHX = chlorhexidine; CI = confidence interval; CPIS = Clinical Pulmonary Infection Score; HR = hazard ratio; ICU = intensive care unit; OR = odds ratio; P = probability; SD = standard deviation; VAP = ventilator‐associated pneumonia
Duration of ICU stay
There was no evidence of a difference between those receiving chlorhexidine compared to placebo/usual care in the outcome of duration of ICU stay (days) (MD ‐0.89 days, 95% CI ‐3.59 to 1.82 days, P = 0.69, I2 = 79%, 5 RCTs, 627 participants; low‐certainty evidence). There was some evidence of a reduction in duration of ICU stay in Analysis 1.4, subgroup 1.4.1 (MD ‐2.92 days, 95% CI ‐4.18 to ‐1.66 days, P < 0.00001, I2 = 18%, three RCTs, 274 participants), no evidence of a difference in Analysis 1.4, subgroup 1.4.2 (MD 1.32 days, 95% CI ‐2.43 to 5.07 days, P = 0.49, one RCT, 257 participants), and insufficient evidence (based on a single study with very low precision) to determine whether or not there was a difference in Analysis 1.4, subgroup 1.4.3.
1.4. Analysis.

Comparison 1: Chlorhexidine versus placebo/usual care, Outcome 4: Duration of ICU stay (days)
Another study (Meinberg 2012) compared chlorhexidine gel with placebo and also found no difference in duration of ICU stay (Additional Table 3).
Use of systemic antibiotics
One trial (146 participants) reported this outcome, but there was insufficient evidence to determine whether or not there was a difference in duration of systemic antibiotic therapy between the chlorhexidine and control groups (MD 0.65 days, 95% CI ‐0.58 to 1.88, P = 0.30) (Analysis 1.5).
1.5. Analysis.

Comparison 1: Chlorhexidine versus placebo/usual care, Outcome 5: Duration of systemic antibiotic therapy (days)
Tuon 2017 compared chlorhexidine solution and placebo and found no evidence of a difference in the number of participants treated with systemic antibiotics (Analysis 1.6).
1.6. Analysis.

Comparison 1: Chlorhexidine versus placebo/usual care, Outcome 6: Number of participants treated with systemic antibiotics
Oral health indices: plaque index
Two of the studies in this group reported numerical data for the outcome of plaque index (Fu 2019; Ozcaka 2012); one study used a four‐point ordinal scale as the plaque index and found significant reduction in the CHX group (Fu 2019), while the other study measured the proportion of participants presented with dental plaque and found no significant difference between groups (Ozcaka 2012) (Analysis 1.7). A further study (Scannapieco 2009) found no difference in plaque indices between the chlorhexidine and control groups (Additional Table 3).
1.7. Analysis.

Comparison 1: Chlorhexidine versus placebo/usual care, Outcome 7: Plaque index
Adverse effects
Two studies in this group reported on adverse effects. Tantipong 2008 found mild reversible irritation of the oral mucosa in 10% of the chlorhexidine participants compared to 1% of the control group participants (Analysis 1.8). Berry 2011 stated that there were no adverse events in either group (Additional Table 3).
1.8. Analysis.

Comparison 1: Chlorhexidine versus placebo/usual care, Outcome 8: Adverse effects
Adverse effects were not mentioned in the other studies in this group.
Other outcomes
The outcomes of caregivers' preferences and cost were not reported.
Heterogeneity
The substantial statistical heterogeneity found for the outcome of VAP incidence is likely to be due to clinical differences between these studies, attributable to variability in the frequency, application method, volume, and concentration of chlorhexidine solution (Analysis 1.1).
In subgroup 1.1.1, all of the six studies used a placebo control and the volume of chlorhexidine (2%, 0.12% or 0.2%) used varied between 10 and 15 mL administered either two, three, or four times daily. One study used a single application by swab of a very small volume of chlorhexidine within 12 hours after intubation (Grap 2011). All the studies involved adult participants.
Sensitivity analyses and subgroup analyses
For the primary outcomes, we conducted a sensitivity analysis excluding studies at high risk of bias. The estimate remained similar for both VAP incidence (RR 0.78, 95% CI 0.56 to 1.10, P = 0.16, I2 = 26%; 603 participants) compared with 0.70, and mortality (RR 1.04, 95% CI 0.81 to 1.33, P = 0.77, I2 = 0%; 330 participants) compared with 1.06 (analyses not shown).
In addition, we also performed subgroup analyses by grouping the included studies according to chlorhexidine concentration (0.12% vs 0.2% vs 2%). Results of these subgroup analyses suggest no evidence of a difference between subgroups in either incidence of VAP (P = 0.64) or mortality (P = 0.91) (analyses not shown).
Comparison 2: Chlorhexidine versus other oral care agents
Seven studies were included in this comparison (Bopp 2006; Dahiya 2012; Hanifi 2017; Irani 2019; Khaky 2018; Meidani 2018; Panchabhai 2009). All of the studies were at high risk of bias. Bopp 2006 was a very small pilot study (n = 5) and the data from this study are recorded in Additional Table 3.
Concentration of the chlorhexidine used was 0.2% in five studies (Dahiya 2012; Hanifi 2017; Irani 2019; Meidani 2018; Panchabhai 2009), and 0.12% in two studies (Bopp 2006; Khaky 2018). Six of these seven studies reported numerical data, and we subgrouped them according to the oral care agents used in control groups, including potassium permanganate (Meidani 2018; Panchabhai 2009), ozonated water (Hanifi 2017), Nanosil (Khaky 2018), hydrogen peroxide (Dahiya 2012), and miswak (Irani 2019).
Incidence of VAP
Meidani 2018 and Panchabhai 2009 compared chlorhexidine with potassium permanganate, and found no evidence of a difference in incidence of VAP (RR 0.87, 95% CI 0.50 to 1.52, P = 0.63, I2= 0%) (Analysis 2.1, subgroup 2.1.1).
2.1. Analysis.

Comparison 2: Chlorhexidine versus other oral care agents, Outcome 1: Incidence of VAP
A single study (Hanifi 2017) compared chlorhexidine with ozonated water, and found some evidence for a benefit for ozonated water (Analysis 2.1, subgroup 2.1.2). The results of this study have not been replicated, so should be interpreted with caution.
A single study (Khaky 2018) compared chlorhexidine with Nanosil, and found some evidence for a benefit for Nanosil (Analysis 2.1, subgroup 2.1.3). The results of this study have not been replicated, so should be interpreted with caution.
A single study (Dahiya 2012) compared chlorhexidine with hydrogen peroxide, and found no evidence of a difference in incidence of VAP (Analysis 2.1, subgroup 2.1.4).
A further study (Irani 2019) compared chlorhexidine with miswak, and found no evidence of a difference in incidence of VAP (Analysis 2.1, subgroup 2.1.5).
The pilot study by Bopp 2006 reported a reduction in VAP associated with chlorhexidine but the evidence was insufficient (Additional Table 3).
Mortality
Meidani 2018 and Panchabhai 2009 compared chlorhexidine with potassium permanganate, and found no evidence of a difference in mortality (RR 1.11, 95% CI 0.89 to 1.38, P = 0.34, I2= 37%) (Analysis 2.2, subgroup 2.2.1).
2.2. Analysis.

Comparison 2: Chlorhexidine versus other oral care agents, Outcome 2: Mortality
A single study (Khaky 2018) compared chlorhexidine with Nanosil, and found no evidence of a difference in mortality (Analysis 2.2, subgroup 2.2.2).
Use of systemic antibiotics
A single study (Irani 2019) compared chlorhexidine with miswak, and found no evidence of a difference in the number of participants treated with systemic antibiotics (Analysis 2.3).
2.3. Analysis.

Comparison 2: Chlorhexidine versus other oral care agents, Outcome 3: Number of participants treated with systemic antibiotics
Other outcomes
The duration of mechanical ventilation, duration of ICU stay, oral health indices, adverse effects, caregivers' preferences and cost were not reported.
Comparison 3: Toothbrushing versus no toothbrushing (with or without antiseptics)
The eight studies included in this comparison (Bopp 2006; De Lacerda 2017; Fields 2008; Long 2012; Lorente 2012; Pobo 2009; Roca Biosca 2011; Yao 2011) had toothbrushing as part of the intervention versus no toothbrushing in the control group. The studies were all at high risk of bias. Two studies used powered toothbrushes (Pobo 2009; Roca Biosca 2011), and six used manual toothbrushes. Bopp 2006 was a very small pilot study (n = 5) and the data from this study are recorded in Additional Table 3. Fields 2008 reported no numerical data at all. Roca Biosca 2011 did not report data for each arm of the study and we were not able to obtain these data from the authors. Available data from this study are recorded in Additional Table 3.
Incidence of VAP
There is some low‐certainty evidence that toothbrushing may be beneficial in reducing the incidence of VAP in the combined meta‐analysis of five studies (RR 0.61, 95% CI 0.41 to 0.91, P = 0.01, I2 = 40%, 910 participants, low‐certainty evidence) (Analysis 3.1).
3.1. Analysis.

Comparison 3: Toothbrushing versus no toothbrushing, Outcome 1: Incidence of VAP
One small study (Yao 2011; 53 participants) at high risk of bias, compared usual care plus the addition of twice daily toothbrushing with a powered toothbrush, to usual care alone, and found a reduction in VAP. The usual‐care intervention comprised the participant's bed being elevated 30° to 45°, hypopharyngeal suctioning, lips moistened with 'toothette' swab and water, then further hypopharyngeal suctioning. A second study with 147 participants, also assessed at high risk of bias (Pobo 2009), compared powered toothbrushing plus usual care including chlorhexidine, with usual care alone, and found no difference in the outcome of VAP. The combined estimate from these studies showed no difference in the incidence of VAP (RR 0.49, 95% CI 0.16 to 1.53, P = 0.22, I2 = 75%) (Analysis 3.1, subgroup 3.1.1), with the heterogeneity probably due to the additional exposure to chlorhexidine in both groups of only one of the studies.
In De Lacerda 2017 and Lorente 2012 (649 participants), where the intervention group received toothbrushing with a manual toothbrush as well as chlorhexidine compared to chlorhexidine alone in the control group, there was no evidence of a difference in the incidence of VAP between the intervention and control groups (RR 0.74, 95% CI 0.50 to 1.09, P = 0.13, I2 = 0%) (Analysis 3.1, subgroup 3.1.2).
A further study (Long 2012; 61 participants) compared toothbrushing plus povidone iodine with povidone iodine alone, and found some evidence for a benefit for toothbrushing (Analysis 3.1, subgroup 3.1.4). The results of this study have not been replicated, so should be interpreted with caution.
Bopp 2006 was a very small pilot study (n = 5) of toothbrushing versus none, and the data are reported in Additional Table 3. There were no numerical outcome data in the study by Fields 2008 the report makes the statement that "the VAP rate dropped to zero within a week of beginning the every 8 hours toothbrushing regimen in the intervention group." This rate of zero incidence of VAP was reportedly sustained for six months. Roca Biosca 2011 recruited 117 participants and reported a summary estimate for the outcome of VAP, with no difference between powered toothbrushing and no toothbrushing (Additional Table 3).
Mortality
Five studies (910 participants) evaluated the effect of toothbrushing, as an addition to oral care, on the outcome of mortality (De Lacerda 2017; Long 2012; Lorente 2012; Pobo 2009; Yao 2011). The comparisons were different in each trial and did not provide evidence of a difference in mortality with or without toothbrushing (RR 0.86, 95% CI 0.70 to 1.05, P = 0.14, I2 = 0%; low‐certainty evidence) (Analysis 3.2).
3.2. Analysis.

Comparison 3: Toothbrushing versus no toothbrushing, Outcome 2: Mortality
In Pobo 2009 and Yao 2011 (200 participants), where the intervention group received toothbrushing with a powered toothbrush as well as usual care compared to usual care alone in the control group, there was no evidence of a difference in mortality (RR 1.31, 95% CI 0.17 to 9.91, P = 0.79, I2 = 55%) (Analysis 3.2, subgroup 3.2.1).
Two studies (De Lacerda 2017; Lorente 2012) with 649 participants) compared toothbrushing combined with chlorhexidine and chlorhexidine alone, and found no evidence of a difference in mortality (RR 0.87, 95% CI 0.68 to 1.12, P = 0.28, I2= 0%) (Analysis 3.2, subgroup 3.2.2).
Another single study (Long 2012; 61 participants) compared toothbrushing combined with povidone iodine and povidone iodine alone, also reported no evidence of a difference in mortality (Analysis 3.2, subgroup 3.2.4).
Duration of ventilation
Meta‐analysis of three trials of chlorhexidine (De Lacerda 2017; Lorente 2012; Pobo 2009; 749 participants) reported the outcome of mean duration of mechanical ventilation, and showed a significant reduction associated with toothbrushing (MD ‐1.46 days, 95% CI ‐2.69 to ‐0.23 days, P = 0.02, I2 = 0%; fixed‐effect model) (Analysis 3.3, subgroup 3.3.1). However, a further trial of povidone iodine failed to show a benefit for toothbrushing for this outcome (Long 2012). The data from Bopp 2006 are reported in Additional Table 3.
3.3. Analysis.

Comparison 3: Toothbrushing versus no toothbrushing, Outcome 3: Duration of ventilation (days)
Duration of ICU stay
Meta‐analysis of three trials of chlorhexidine (De Lacerda 2017; Lorente 2012; Pobo 2009; 749 participants) reported the outcome of mean duration of ICU stay and found that there may be a reduction associated with toothbrushing (MD ‐1.89 days, 95% CI ‐3.52 to ‐0.27 days, P = 0.02, I2 = 0%; fixed‐effect model; very low‐certainty evidence) (Analysis 3.4). The data from Bopp 2006 are reported in Additional Table 3.
3.4. Analysis.

Comparison 3: Toothbrushing versus no toothbrushing, Outcome 4: Duration of ICU stay (days)
Use of systemic antibiotics
This outcome was not reported by any of the studies in this group.
Oral health indices: plaque score
One study (Yao 2011) also reported the outcome of plaque score in each group after seven to eight days. The study showed evidence of reduced plaque in the toothbrushing group (Analysis 3.5).
3.5. Analysis.

Comparison 3: Toothbrushing versus no toothbrushing, Outcome 5: Plaque score
Roca Biosca 2011 reported plaque scores, without any estimates of variance. The trial report stated that there was no difference between the groups (Additional Table 3).
Adverse effects
Pobo 2009 and De Lacerda 2017 reported that there were no adverse effects reported in either arm of the study and none of the other studies in this comparison mentioned adverse effects (Additional Table 3).
Other outcomes
The outcomes of caregivers' preferences and cost were not reported.
Comparison 4: Powered toothbrushing versus manual toothbrushing
One small study of 78 participants (Prendergast 2012), assessed at high risk of bias, compared the use of a powered toothbrush as a component of 'comprehensive oral care' with a control group receiving manual toothbrushing and standard oral care.
In this study, there was no difference between the intervention and control groups for the outcomes of incidence of VAP, mortality or mean duration of ventilation or ICU stay (Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.4). There were no adverse effects mentioned in this study. The outcomes of oral health indices, systemic antibiotic therapy, caregivers' preferences for oral hygiene care or cost were not reported in the study.
4.1. Analysis.

Comparison 4: Powered toothbrush versus manual toothbrush, Outcome 1: Incidence of VAP
4.2. Analysis.

Comparison 4: Powered toothbrush versus manual toothbrush, Outcome 2: Mortality
4.3. Analysis.

Comparison 4: Powered toothbrush versus manual toothbrush, Outcome 3: Duration of ventilation (days)
4.4. Analysis.

Comparison 4: Powered toothbrush versus manual toothbrush, Outcome 4: Duration of ICU stay (days)
Comparison 5: Other oral care agents
Fifteen studies were included in this comparison, with a total of 3062 participants randomised to treatments (Berry 2011; Berry 2013; Caruso 2009; Feng 2012; Hu 2009; Meidani 2018; Mo 2016; Nobahar 2016; Seguin 2006; Seguin 2014; Stefanescu 2013; Tang 2013; Xu 2007; Xu 2008; Zhao 2012). Twelve of these studies were at high risk of bias, two studies were at unclear risk of bias (Caruso 2009; Zhao 2012) and Seguin 2014 was at low risk of bias. The studies evaluated the effects of other oral care agents with a potential antiseptic effect on the outcomes of VAP, mortality, duration of ventilation, duration of ICU stay, number of participants treated with systemic antibiotics and adverse effects.
Incidence of VAP
Three studies (356 participants) compared povidone iodine rinse with a saline rinse or placebo (Feng 2012; Seguin 2006; Seguin 2014). They showed evidence of a reduction in VAP in the povidone iodine group (RR 0.69, 95% CI 0.50 to 0.95, P = 0.02, I2 = 74%, fixed‐effect model) (Analysis 5.1, subgroup 5.1.1).
5.1. Analysis.

Comparison 5: Other oral care agents, Outcome 1: Incidence of VAP
Seguin 2006 (67 participants) also compared povidone iodine rinse with usual care (suction alone with no rinse) and found a reduction in VAP in the povidone iodine group (Analysis 5.1, subgroup 5.1.2). The result of this study has not been replicated, so should be interpreted with caution.
Four studies (488 participants) (Mo 2016; Tang 2013; Xu 2007; Xu 2008), all at high risk of bias, which compared a saline rinse with a saline‐soaked swab, found that saline rinse may reduce the incidence of VAP (RR 0.47, 95% CI 0.37 to 0.62, P < 0.001, I2 = 84%, fixed‐effect model) (Analysis 5.1, subgroup 5.1.3).
Two studies (Caruso 2009; Seguin 2006; 324 participants), both at high risk of bias, compared a saline rinse with usual care (no rinse) and found a reduction in VAP (RR 0.60, 95% CI 0.39 to 0.91, P = 0.02, I2 = 64%, fixed‐effect model) (Analysis 5.1, subgroup 5.1.4). While this result should be interpreted cautiously due to the high risk of bias, there appeared to be some evidence that the use of a saline rinse was associated with reduction of VAP.
Hu 2009 and Xu 2007, both at high risk of bias, compared both saline rinse plus swab in 153 participants, with a saline‐soaked swab alone (usual care) and found that the combined rinse plus swab may reduce the incidence of VAP (RR 0.41, 95% CI 0.23 to 0.72, P = 0.002, I2 = 0%, fixed‐effect model) (Analysis 5.1, subgroup 5.1.5).
Two studies (Berry 2011; Berry 2013; 347 participants), both at high risk of bias, compared bicarbonate rinse plus toothbrushing with a water rinse plus toothbrushing and found no evidence of a difference in the incidence of VAP (RR 1.57, 95% CI 0.62 to 3.99, P = 0.34, I2 = 43%, fixed‐effect model) (Analysis 5.1, subgroup 5.1.6).
A single study compared triclosan rinse with saline rinse and found no difference in the outcome of VAP over the duration of the study (Zhao 2012) (Analysis 5.1, subgroup 5.1.7). The results of this study have not been replicated, so should be interpreted with caution.
A single three‐arm study compared povidone iodine, furacilin and usual care (Feng 2012). It found both antiseptics combined with toothbrushing were more effective than usual care (Analysis 5.1, subgroup 5.1.1 and Analysis 5.1, subgroup 5.1.9) with insufficient evidence of a difference between the two antiseptic solutions (Analysis 5.1, subgroup 5.1.8).
A single study (Berry 2013), comparing Listerine with water, and Listerine with bicarbonate, found no evidence of a difference in VAP incidence (Analysis 5.1, subgroups 5.1.10 and 5.1.11).
A single study (Stefanescu 2013; 41 participants) compared Biotene OralBalance with control and found no difference in incidence of VAP (Analysis 5.1, Subgroup 5.1.12).
A single study (Nobahar 2016) compared hydrogen peroxide with normal saline, and found a reduction in VAP (Analysis 5.1, subgroup 5.1.13). The result of this study has not been replicated, so should be interpreted with caution.
Another single study (Meidani 2018) compared potassium permanganate with placebo, and found no evidence of a difference in VAP incidence (Analysis 5.1, subgroup 5.1.14).
Mortality
Eight studies reported mortality in the following comparisons (Analysis 5.2).
5.2. Analysis.

Comparison 5: Other oral care agents, Outcome 2: Mortality
Povidone iodine versus saline/placebo: two studies (217 participants) (RR 1.00, 95% CI 0.66 to 1.50, P = 0.98, I2 = 65%; fixed‐effect model); no evidence to suggest a difference in mortality.
Povidone iodine versus usual care: a single study (67 participants) reported no difference.
Saline rinse versus saline swab: two studies (270 participants) (RR 0.29, 95% CI 0.12 to 0.69; P = 0.005, I2 = 0%; fixed‐effect model), suggesting a significant reduction in mortality for saline rinse.
Saline rinse plus swab versus saline swab (usual care): a single study (47 participants) reported no difference.
Saline rinse versus usual care: two studies (324 participants) (RR 1.10, 95% CI 0.87 to 1.39, P = 0.43, I2 = 2%; fixed‐effect model); no evidence to suggest a difference in mortality.
Biotene OralBalance versus control: a single study (41 participants) reported no difference.
Potassium permanganate versus placebo: a single study (100 participants) reported no difference.
Duration of ventilation
Six studies reported duration of ventilation (days) in the following comparisons (Analysis 5.3).
5.3. Analysis.

Comparison 5: Other oral care agents, Outcome 3: Duration of ventilation (days)
Povidone iodine versus saline/placebo: a single study (67 participants) reported no difference.
Povidone iodine versus usual care: a single study (67 participants) reported no difference.
Saline rinse versus usual care: two studies (324 participants) (MD ‐0.40 days, 95% CI ‐2.55 to 1.75 days, P = 0.72, I2 = 0%); no evidence to suggest a difference in duration of ventilation.
Saline rinse plus swab versus saline swab (usual care): a single study (47 participants) reported a statistically significant effect in favour of shorter duration for the saline rinse plus swab.
Saline rinse versus saline swab: two studies (176 participants) (MD ‐6.83 days, 95% CI ‐8.94 to ‐4.72 days; P < 0.00001, I2 = 65%) suggested saline rinse led to shorter duration of ventilation.
Triclosan rinse versus saline: a single study (324 participants) reported that triclosan led to shorter duration of ventilation than saline.
Berry 2013, comparing Listerine with water, and Listerine with bicarbonate, found no difference among groups in median ventilation hours. Another study (Stefanescu 2013), comparing Biotene OralBalance and control, also found no difference between groups in duration of ventilation. (Additional Table 3).
Duration of ICU stay
Four studies reported duration of ICU stay (days) in the following comparisons (Analysis 5.4).
5.4. Analysis.

Comparison 5: Other oral care agents, Outcome 4: Duration of ICU stay (days)
Povidone iodine versus saline/placebo: two studies (217 participants) (MD ‐0.35 days, 95% CI ‐3.90 to 3.21 days, P = 0.85, I2 = 0%; fixed‐effect model); no evidence to suggest a difference.
Povidone iodine versus usual care: a single study (67 participants) reported no difference.
Saline rinse versus usual care: two studies (324 participants) (MD ‐1.17 days, 95% CI ‐3.95 to 1.60 days, P = 0.41, I2 = 32%; fixed‐effect model); no evidence to suggest a difference in duration of ICU stay.
Triclosan rinse versus saline: a single study (324 participants) reported that triclosan led to shorter stay in ICU than saline.
Another study (Berry 2013), comparing Listerine with water, and Listerine with bicarbonate, found no difference among groups in median ICU length of stay (Additional Table 3).
Use of systemic antibiotics
Seguin 2014, comparing povidone iodine and placebo, showed no evidence of a difference in the number of participants treated with systemic antibiotics (Analysis 5.5). Berry 2013, comparing Listerine with water, and Listerine with bicarbonate, found no difference among groups in antibiotic administration. See Additional Table 3.
5.5. Analysis.

Comparison 5: Other oral care agents, Outcome 5: Number of participants treated with systemic antibiotics
Adverse effects
Seguin 2014 found no evidence of a difference in the occurrence of acute respiratory distress syndrome, agitation and/or hypertension, epistaxis, oxygen desaturation and aspiration (Analysis 5.6). Berry 2013 found no adverse events associated with interventions. Stefanescu 2013, comparing Biotene OralBalance and control, found no significant difference between groups with respect to adverse events in buccal mucosa. See Additional Table 3.
5.6. Analysis.
Comparison 5: Other oral care agents, Outcome 6: Adverse effects
Discussion
Summary of main results
In this updated review, we included 40 randomised controlled trials evaluating interventions in the oral hygiene care of critically ill patients receiving mechanical ventilation for at least 48 hours in intensive care units. We classified these trials into five broad groups, based on the intervention, control and co‐interventions used.
Chlorhexidine (CHX) antiseptic versus placebo/usual care (with or without toothbrushing)
There is moderate‐certainty evidence from 13 RCTs that the use of chlorhexidine (either as a mouthrinse or a gel) probably reduces the incidence of ventilator‐associated pneumonia (VAP) from 26% to about 18% (see Table 1). However, there may be no difference in mortality (moderate‐certainty evidence), duration of mechanical ventilation (very low‐certainty evidence) or duration of ICU stay (low‐certainty evidence). There is insufficient evidence to determine the effect of chlorhexidine on the other secondary outcomes of this review.
CHX antiseptic versus other oral care agents
Six RCTs compared CHX with other oral care agents, two of which suggested no evidence of a difference between chlorhexidine and potassium permanganate in incidence of VAP or mortality. Due to variation in comparisons and outcomes among trials, there is insufficient evidence concerning the effects of CHX and other oral care agents.
Toothbrushing versus no toothbrushing (with or without antiseptics)
Based on six RCTs (low‐certainty evidence), toothbrushing may be beneficial in reducing the incidence of VAP. Also, very low‐certainty evidence from 3 RCTs shows that toothbrushing might reduce the duration of ICU stay. No evidence of a difference was found between toothbrushing or no toothbrushing for the outcomes of mortality (low‐certainty evidence) or duration of ventilation (low‐certainty evidence) (see Table 2).
Oral care with powered toothbrush versus oral care with manual toothbrush
From the single study in this comparison, there is insufficient evidence to determine the effects of powered versus manual toothbrushing on the outcomes of VAP, mortality, duration of mechanical ventilation or duration of ICU stay.
Oral care with other solutions
The studies in this comparison, most of which were at high overall risk of bias, made different comparisons. For the reduction of VAP, there is some weak evidence that povidone iodine rinse is more effective than saline/placebo, use of saline rinse is more effective than saline swab, use of both a saline swab and a saline rinse may be more effective than a saline swab alone, and use of saline rinse may be more effective than usual care. There is no evidence of a difference between bicarbonate rinse and a water rinse.
For the outcome of mortality, we found no evidence of a difference between povidone iodine rinse and saline/placebo or between saline rinse and usual care. We found some very weak evidence of a difference between saline rinse and saline swab.
For the duration of ventilation, we found no evidence of a difference between saline rinse and usual care, and some weak evidence that saline rinse leads to shorter duration of ventilation compared to saline swab. For the duration of ICU stay, we found no evidence of a difference between povidone iodine and saline/placebo or between saline rinse and usual care.
Overall completeness and applicability of evidence
In this review, we have included studies that compared active oral hygiene care interventions with either placebo or usual care. We recognise that the use of a placebo is a better control comparison in research studies because it enables the masking of caregivers to whether group participants are in the active or control group, thus eliminating some possible performance bias. However, we chose to include pragmatic studies where 'usual care' was the control comparator, despite recognising that in many instances 'usual care' was not specified and may have varied between participants and between individual caregivers. Where there was no blinding, we assessed studies as being at high risk of performance and detection bias.
There are some other variables that may have influenced the outcomes in the included studies. These include the number of episodes of OHC a day, the 'dose' of the antiseptic, and whether participants were dentate or edentulous. Most of the studies stated that they delivered between two and four episodes of OHC per day. Nine studies specified that edentulous people were excluded, one study focussed on newborns, but most of the included studies did not report whether or not participants were dentate. We investigated whether there was a dose‐response effect and could find no evidence for this.
We also recognise that participation in a research study is likely to have a positive effect on the performance of 'usual care', improving both the quality of care and compliance with routine practice ‐ a Hawthorne effect (McCarney 2007). The combination of a 'usual‐care' control group, the absence of caregiver blinding in most cases, and the Hawthorne effect of being part of a study may have reduced the observed difference in effect between the active and control interventions in these studies. None of the studies included in this review reported compliance with oral hygiene care protocols.
Another area of variability between the studies (and possibly also between studies and usual practice) is the diagnosis of VAP, which is at least partly subjective and may be based on variable diagnostic criteria. Most of the included studies stated the criteria used to diagnose VAP, of which the two most common were the original or modified version of the clinical pulmonary infection score (CPIS) based on Pugin's criteria (Cook 1998; Pugin 1991) and Centers for Disease Control (CDC) criteria as described in Horan 2008. Five studies conducted in China used Chinese Society of Respiratory Diseases (CSRD) criteria for diagnosis of VAP (Feng 2012; Mo 2016; Tang 2013; Xu 2007; Xu 2008).
Currently there is no clearly accepted gold standard for the diagnosis of VAP, and when different criteria are applied to the same cohort of patients, the estimated VAP prevalence could vary widely (Klompas 2007). In light of the limited sensitivity and specificity of the traditional VAP diagnosis, the US Centers for Disease Control (CDC) has developed a new surveillance criterion, ventilator‐associated event (VAE), to incorporate all complications (including VAP) leading to the worsening of gas exchange in mechanically‐ventilated patients. However, the advent of a more objective and definitive diagnosis of VAP may depend on further development of biomarker technologies, which may not occur in the near future (Waters 2015).
This review has not found evidence that oral hygiene care including both toothbrushing and chlorhexidine is different from oral hygiene care with chlorhexidine alone in reducing VAP. Only one of the trials of toothbrushing that reported the outcome of VAP also reported plaque levels as an indicator of the effectiveness of the toothbrushing carried out in this trial (Yao 2011). This small trial (53 participants), which we assessed as being at high risk of bias, did not use chlorhexidine in either group, and found a reduction in both plaque and VAP in the powered toothbrushing group compared to the non‐toothbrushing group. Three other trials of toothbrushing in our meta‐analysis (De Lacerda 2017 (manual), Lorente 2012 (manual), Pobo 2009 (powered toothbrush)), with a combined total of 796 participants, included exposure to chlorhexidine in both intervention and control groups. Meta‐analysis of these four trials with high risk of bias showed no evidence of a difference in the outcome of VAP (analyses not shown). A further study (Roca Biosca 2011), included in this review and also at high risk of bias, could not be included in the meta‐analysis, but also found no difference between oral care with chlorhexidine and toothbrushing and oral care with chlorhexidine alone. All six of these studies described the toothbrushing intervention in detail, and noted that nurses delivering the intervention received specific training. While the presence of ventilator tubes in the mouths of trial participants makes effective toothbrushing difficult, it seems likely that, despite this, the toothbrushing intervention was carried out thoroughly within these trials.
Earlier cohort studies noted that patients in ICU who developed VAP were likely to have increased length of stay in the ICU (Apostolopoulou 2003; Cook 1998). However, our Cochrane Review has not evaluated duration of ICU stay in patients who develop VAP. The studies in our review reported mean length of ICU stay and the standard deviation for each arm of the study. We have combined these in meta‐analyses based on an assumption that the duration of ICU stay in each arm of each trial follows an approximately normal distribution. In fact, the distribution of duration of stay in ICU is likely to be skewed, and the means are likely to be a poor indicator of the effect of oral hygiene care on duration of ICU stay.
Our review did not consider the cost‐effectiveness of the interventions, but may explore this in the next update of the review.
The increasing incidence of bacteria that are resistant to current antibiotics is of concern worldwide, and one of the reasons for bacterial resistance is the overuse of systemic antibiotics (Gyssens 2011). Oral hygiene care, using antiseptics such as chlorhexidine to reduce the risk of VAP, could potentially also result in a reduced requirement for these patients to be treated with systemic antibiotics. Because only three of the 40 studies included in this review provided data about the use of systemic antibiotics in study participants, we do not have sufficient information to determine whether there was any effect on systemic antibiotic use.
It is interesting that only one of the studies that evaluated chlorhexidine reported adverse reactions to chlorhexidine (mild reversible irritation of the oral mucosa) (Tantipong 2008). Hypersensitivity is a rare but potentially severe side effect of chlorhexidine (Pemberton 2012). In over 2000 participants included in these studies, there was no report of hypersensitivity to chlorhexidine. However, it is notable that in six of the included studies (De Lacerda 2017; Khaky 2018; Kusahara 2012a; Meidani 2018; Ozcaka 2012; Scannapieco 2009), a prior history of hypersensitivity to chlorhexidine was an exclusion criterion during participant recruitment. In view of reports in the UK of two cases of serious adverse events associated with irrigation of dry socket with chlorhexidine mouthrinse, it is recommended that all members of the dental team prescribing chlorhexidine products are aware of the potential for both minor and serious adverse effects (Pemberton 2012).
Quality of the evidence
For the first main comparison of interest in this review (comparison between chlorhexidine and placebo/usual care), although only one of the trials was assessed at low risk of bias (Koeman 2006) for all domains, we did not consider that the impact of bias reduced our confidence in the outcome of VAP incidence and mortality, because sensitivity analysis according to risk of bias did not alter the size or direction of the effect. However, due to substantial heterogeneity and serious imprecision, we considered the certainty of the evidence for VAP incidence and mortality to be moderate. We downgraded the certainty of evidence for duration of ICU stay and duration of ventilation to low and very low, mainly because of serious imprecision, substantial heterogeneity and high risk of bias. Most studies did not provide information on adverse events, and the scant information we could obtain from two studies prompted us to downgrade the certainty of evidence to very low (see Table 1).
For the second main comparison of interest (comparison between toothbrushing and no toothbrushing), all of the included trials were at high risk of bias. Therefore, we considered the certainty of evidence for incidence of VAP, mortality, duration of ventilation and duration of ICU stay to be low or very low, mainly due to the existence of very serious risk of bias, substantial heterogeneity and/or serious imprecision. Also, as only two studies provided limited information on adverse events, we downgraded the certainty of evidence for adverse effects to very low (see Table 2).
Potential biases in the review process
In order to reduce the risk of publication bias, we conducted a broad search for both published and unpublished studies, with no restrictions on language. We searched the reference lists of included studies and contacted many of the study authors in order to obtain information that was not included in the published reports. We also searched the reference lists of other published reviews of oral hygiene care for critically ill patients. However, our search strategy did not include the term 'mortality'. It is possible that studies looked at OHC and all‐cause mortality without mentioning 'VAP' or 'pneumonia', and these may not have been identified by our searches. To our knowledge, we have not missed any studies, but we will therefore consider adding mortality‐related terms to our search strategy in the next update of this review, to ensure that all potentially eligible studies can be identified and assessed.
For this review we also chose very broad inclusion criteria, which has resulted in a clinically heterogeneous group of studies including adults, children and neonates, and a range of indications for ICU care, including medical conditions, surgery and trauma where patients were ventilated for over 48 hours. In some of the included studies, the precise details of what was involved in the oral hygiene care intervention were poorly described, making it difficult to determine the similarity between studies in oral hygiene care practices. There was also potential variation in the methods used for intubation and for the calculation of duration outcomes (e.g. duration of mechanical ventilation, duration of ICU stay) (Contentin 2014), both of which were not always clearly specified.
One other potential bias in this review is the variation in and the subjective nature of criteria/methods used for VAP diagnosis (Klompas 2007). Also, we have made a number of changes to the methods of this review since the publication of the protocol (see Differences between protocol and review). Some of these changes were clarifications, and some were undertaken to take account of other Cochrane Reviews published or in preparation, to avoid unnecessary duplication of effort. We acknowledge that post hoc changes to the review methods may introduce a risk of bias into this review.
Agreements and disagreements with other studies or reviews
A previous meta‐analysis by Pineda 2006 found that the use of chlorhexidine for oral decontamination did not reduce the incidence of nosocomial pneumonia. However, their meta‐analysis included only four studies and the outcome was nosocomial pneumonia rather than VAP. Another systematic review by Labeau 2011 included 14 studies of either chlorhexidine or povidone iodine antiseptics and found that the use of antiseptics as part of oral hygiene care reduced the incidence of VAP by approximately one‐third. Our review confirmed these findings.
One systematic review looked at the effects of selective digestive/oropharyngeal decontamination and topical oropharyngeal chlorhexidine on the prevention of death in general intensive care (Price 2014), and claimed that CHX may be associated with increased mortality (odds ratio (OR) 1.25, 95% CI 1.05 to 1.50). Reasons for the discrepancy between this finding and ours mainly include differences in the review scope (e.g. whether focussed on adults, general intensive care only) and review methodology (e.g. requiring that participants were ventilated for at least 48 hours, inclusion of studies for which only abstracts were available). In a recent cluster‐randomised trial, Wittekamp and colleagues studied the effects of decontamination strategies on ventilated patients in ICUs with moderate to high levels of antibiotic resistance, and found no significant difference in 28‐day mortality between CHX mouthrinse and standard care (Wittekamp 2018). However, the primary focus of this trial was bloodstream infections caused by multidrug‐resistant gram‐negative bacteria, and its design and methodology did not meet our eligibility criteria. More trials are needed of the association between CHX usage and ICU mortality, to provide more insight into this issue.
Another two systematic reviews have looked at the effects of chlorhexidine with different concentrations. One claimed that the use of higher concentration chlorhexidine was associated with higher mortality (Klompas 2014), and the other stated that chlorhexidine with the concentration of 0.12% had the best effect in reducing VAP incidence (Zhang 2013). However, these findings were all based on trivial differences in point estimates, with wide confidence intervals for each estimate and statistically non‐significant differences between concentrations. The results of our sensitivity analyses do not support the dose‐response relationships that they proposed, and confirm that differences between concentrations were statistically non‐significant.
Although this review found evidence that the use of chlorhexidine as part of oral care reduces the incidence of VAP, there was no evidence of a reduction in mortality. This is in contrast to a review by Price 2014 which claimed that CHX is possibly associated with increased mortality. There has been some debate in the literature about the attributable mortality of VAP. In 2017, the panel of ERS/ESICM/ESCMID/ALAT guidelines noticed an unclear balance between potential reduction in VAP incidence and potential increase in mortality, and therefore decided not to issue a recommendation on the use of chlorhexidine in oral decontamination until more safety data become available (Torres 2017).
Authors' conclusions
Implications for practice.
Effective oral hygiene care is important for ventilated patients in intensive care to reduce ventilator‐associated pneumonia. The definition of oral hygiene care varied among the studies included in this review, but common elements included cleaning of the teeth and gums with a swab or gauze, toothbrushing, and rinsing the mouth. Compared with placebo/usual care, chlorhexidine mouthwash or gel, as part of OHC, probably reduces the incidence of developing ventilator‐associated pneumonia in critically ill patients from 26% to about 18%. However, there is no evidence of a benefit for mortality or duration of mechanical ventilation or ICU stay. Low‐certainty evidence suggests that OHC including both antiseptics and toothbrushing may be more effective than OHC with antiseptics alone for reducing VAP incidence and length of ICU stay, but there was no evidence for a reduction in mortality or duration of mechanical ventilation. There is insufficient evidence to determine whether any of the interventions evaluated in the studies are associated with adverse effects.
Implications for research.
Although the included studies provided some evidence for the benefits of oral hygiene care for critically ill patients to prevent ventilator‐associated pneumonia, incomplete reporting of studies is a major limitation. More consistent use of the CONSORT statement for reporting of randomised controlled trials (CONSORT 2012) would increase the value of research.
Detailed reporting of methods, such as generation of allocation sequence, allocation concealment, and numbers and reasons for withdrawals and exclusions.
Use of a placebo where possible to enable blinding.
Full reporting of methods used to diagnose ventilator‐associated pneumonia.
Reporting of adverse effects of interventions.
Further trials of oral hygiene care (including use of manual or powered toothbrushes, or swabs) should use well‐defined outcomes including both measures of effectiveness of plaque removal and prevention of ventilator‐associated pneumonia. They should also state explicitly whether those patients who have died during the study were included in the calculation of duration outcomes (e.g. duration of ICU stay, duration of mechanical ventilation), and describe in detail the type and frequency of all interventions given to participants (especially 'usual care').
Future studies may also consider adopting the new definitions and diagnostic criteria (ventilator‐associated event, VAE) developed by the US CDC (Waters 2015), which is likely to overcome the limitations of traditional VAP diagnosis and facilitate high‐quality synthesis of research findings.
Feedback
Mortality data for chlorhexidine, 23 November 2016
Summary
Hua and colleagues examined the effect of chlorhexidine (CHX) on mortality (analysis 1.2) and found no benefit of CHX compared to placebo (risk ratio (RR) 1.09, 95% confidence interval (CI) 0.96 to 1.23).a Those results differ from those derived in a recent meta‐analysis by our group (odds ratio (OR) 1.25, 95% CI 1.05 to 1.50).b The review authors specifically discussed this and suggested that this discrepancy could be accounted for by differences in review methodology.
We fully agree. We sought to explore the effect of CHX (and selective digestive or oropharygneal decontamination) on mortality in general adult intensive care units so we excluded studies on cardiac surgery patients and children. We did include a study by MacNaughton and colleagues that was published only as an abstractc. Hua and colleagues suggested that our inclusion of this abstract might contribute to the observed difference in the two pooled estimates. However, removal of this study from our meta‐analysis led to a very similar result (OR 1.29, 95% CI 1.07 to 1.56).
When considering the studies included in both our reviews, there were three studies that both Hua and colleagues and we identified but handled differently. We wonder if this accounts for much of the observed discrepancy.
Berry and colleaguesd: the primary outcome of this study was bacterial growth at day 4. Berry and colleagues accordingly excluded patients who had died within 96 hours from their analysis; this is shown in Figure 1 of their paper. Although Hua and colleagues state that they used intensive care unit (ICU) mortality when available, they appear to have used these 96‐hour mortality data in their pooled estimates. Berry and colleagues did not publish ICU mortality data but we managed to obtain the data from them.
Koeman et ale: the authors omitted mortality data from this moderately large (relevant arms consisting of 257 patients) and robust trial from their pooled estimates. We included these data. Of note, other meta‐analyses on this subject that have examined mortality have included this study in their pooled estimates; Hua et al are unique in choosing to exclude it (references on request).
Munro and colleaguesf Hua and colleagues chose to use the “day 3 analysis sample” rather than obtaining intention‐to‐treat data. This means they have included only 192 patients out of an enrolled population of 547 (the largest randomised controlled trial on this subject published to date). In their paper, Munro and colleagues explained how this group came about: “Of the 547 enrolled patients, 249 were still endotracheally intubated on study day 3; of these, 209 patients had complete day 3 CPIS [Clinical Pulmonary Infection Score] data. Because of missing values on some of the components of the CPIS, only 192 patients had CPIS values on both days 1 and 3, and their data could be analyzed completely.” Accordingly, 298 patients have been excluded either owing to extubation or death and 57 patients have been excluded owing to lack of data for a scoring system that is irrelevant to the outcome of death.
In summary, the authors have, in our view, three relevant omissions in their dataset. These might be for reasons such as being unable to contact authors, as indeed was the case for one of our included studiesg. Nevertheless, there has been substantial attrition of potentially available data in their pooled estimate and accordingly we question if they are correct in their claim that their result “reflects the current evidence base”.
I do not have any affiliation with or involvement in any organisation with a financial interest in the subject matter of my comment.
References:
aHua F, Xie H, Worthington HV, Furness S, Zhang Q, Li C. Oral hygiene care for critically ill patients to prevent ventilator‐associated pneumonia. Cochrane Database of Systematic Reviews 2016, Issue 10. Art. No.: CD008367. DOI: 10.1002/14651858.CD008367.pub3. bPrice R, MacLennan G, Glen J. Selective digestive or oropharyngeal decontamination and topical oropharyngeal chlorhexidine for prevention of death in general intensive care: systematic review and network meta‐analysis. BMJ 2014; 348: g2197. cMacNaughton PD, Bailey J, Donlin N, Branfield P, Williams A, Rowswell H. A randomised controlled trial assessing the efficacy of oral chlorhexidine in ventilated patients. Intensive Care Medicine 2004; 30: S12. dBerry AM, Davidson PM, Masters J, Rolls K, Ollerton R. Effects of three approaches to standardized oral hygiene to reduce bacterial colonization and ventilator associated pneumonia in mechanically ventilated patients: A randomised control trial. International Journal of Nursing Studies 2011; 48: 681‐8. eKoeman M, Van der Ven AJ, Hak E, Joore HC, Kaasjager K, De Smet AM, et al. Oral decontamination with chlorhexidine reduces the incidence of ventilator‐associated pneumonia. American Journal of Respiratory Critical Care Medicine 2006; 173: 1348‐55. fMunro CL, Grap MJ, Jones DJ, McClish DK, Sessler CN. Chlorhexidine, toothbrushing and preventing ventilator associated pneumonia in critically ill adults. American Journal of Critical Care 2009; 18: 428‐38. gPanchabhai TS, Dangayach NS, Krishnan A, Kothari VM, Karnad DR. Oropharyngeal cleansing with 0.2% chlorhexidine for prevention of nosocomial pneumonia in critically ill patients. Chest 2009; 135: 1150‐6.
Reply
We thank Price and colleagues for their feedback on our reviewa. We know that the association between oral care using CHX and ICU mortality has been a hot topic in recent years, with lots of new discussions in the literature.b,c,d,
In the Discussion section of our review, we mentioned the Price 2014 reviewc and said, “Reasons for the discrepancy between this finding and ours mainly include differences in the review scope (e.g. whether focussed on adults, general intensive care only) and reviewmethodology (e.g. inclusion of studies for which only abstracts are available).”
Firstly, in their review, Price and colleaguesc excluded trials carried out on cardiac surgery patients and children, while our review did not have such restrictions. Also, one of our main inclusion criteria for trials and participants was mechanical ventilation for a minimum of 48 hours, but Price and colleaguesc did not state such a requirement. Therefore, the questions that these two reviews tried to answer were essentially different. For instance, the DeRiso 1996 studye, which enrolled only cardiac surgery patients, was included in our review but not in Price 2014c. If Price 2014 was to include this study, the pooled OR would become 1.19 (95% CI 0.96 to 1.46). Actually, other similar systematic reviewsb,f have also included DeRiso 1996. In addition, according to a post hoc subgroup analysis, we found that the mortality results of the adult trials and the child trials included in our Analysis 1.2 were not significantly different (P = 0.14), indicating that analysing these two types of trials separately may not be necessary.
Secondly, there is potential risk in directly using unpublished trial data from previous systematic reviews. Such data may or may not be trustworthy. One perfect example here is that for the same MacNaughton 2004 studyg, an abstract that did not clearly report results for mortality, data used in Price 2014 (29/101 for treatment, 29/93 for control)c and Klompas 2014 (36/91 for treatment, 33/88 for control)b differed substantially. In terms of Koeman 2006, we noticed that both Price and colleaguesc and Klompas and colleaguesb used data provided in a previous systematic reviewf, but without verifying the data by contacting original authors. As documented in our 'Characteristics of included studies' table, we tried to contact Koeman and colleaguesh for data confirmation but failed (invalid email address). Plus, if we used the same Koeman data as in Price 2014c, our pooled RR would remain similar (1.11, 95% CI 0.99 to 1.25).
We noticed that for multiple studies, including Berry 2011i and Munro 2009j, the data that we used for Analysis 1.2 were different from those used in the Price review [3]. As all of these data were extracted for the previously published version of our reviewk, we re‐examined these data and agree that the inclusion of the 96‐hour mortality data in Berry 2011 is inappropriate and we have therefore decided to exclude these data from our Analysis 1.2. After this revision, our pooled RR remains 1.09 (95% CI 0.96 to 1.23). As to other studies included in this analysis, no mistakes in the use of data were found so we do not plan to make other modifications.
As described in our Abstract and Methods section, the predetermined primary objective of our review was to assess the effects of oral hygiene care on the incidence of ventilator‐associated pneumonia (VAP) in critically ill patients receiving mechanical ventilation in ICUs. The participants that we were interested in were those who received mechanical ventilation for at least 48 hours and therefore were at risk of developing VAP. Thus, our use of the Day 3 sample data in Munro 2009j was reasonable. The same reason (predetermined PICO) can also explain the differences between our review and Price 2014c for the data of Panchabhai 2009l, Cabov 2010m and Bellissimo‐Rodrigues 2009n. Authors of the previous version of our reviewk obtained relevant data that met our criteria from the original authors of those studies.
Thank you for your interest in our work.
References
aHua F, Xie H, Worthington HV, Furness S, Zhang Q, Li C. Oral hygiene care for critically ill patients to prevent ventilator‐associated pneumonia. Cochrane Database of Systematic Reviews 2016, Issue 10. Art. No.: CD008367. DOI: 10.1002/14651858.CD008367.pub3. bKlompas M, Speck K, Howell MD, Greene LR, Berenholtz SM. Reappraisal of routine oral care with chlorhexidine gluconate for patients receiving mechanical ventilation: systematic review and meta‐analysis. JAMA Internal Medicine 2014; 174: 751‐61. cPrice R, MacLennan G, Glen J, Su DC. Selective digestive or oropharyngeal decontamination and topical oropharyngeal chlorhexidine for prevention of death in general intensive care: systematic review and network meta‐analysis. BMJ 2014; 348: g2197. dKlompas M, Li LL, Kleinman K, Szumita PM, Massaro AF. Associations between ventilator bundle components and outcomes. JAMA Internal Medicine 2016; 176: 1277‐83. eDeRiso AJ, 2nd, Ladowski JS, Dillon TA, Justice JW, Peterson AC. Chlorhexidine gluconate 0.12% oral rinse reduces the incidence of total nosocomial respiratory infection and nonprophylactic systemic antibiotic use in patients undergoing heart surgery. Chest 1996; 109: 1556‐61. fChan EY, Ruest A, Meade MO, Cook DJ. Oral decontamination for prevention of pneumonia in mechanically ventilated adults: systematic review and meta‐analysis. BMJ 2007; 334: 889. gMacNaughton P, Bailey J, Donlin N, Branfield P, Williams A, Rowswell H. A randomised controlled trial assessing the efficacy of oral chlorhexidine in ventilated patients. Intensive Care Medicine 204; 30: S12. hKoeman M, Van der ven AJ, Hak E, Joore HC, Kaasjager K, et al. Oral decontamination with chlorhexidine reduces the incidence of ventilator‐associated pneumonia. American Journal of Respiratory Critical Care Medicine 2006; 173: 1348‐55. iBerry AM, Davidson PM, Masters J, Rolls K, Ollerton R. Effects of three approaches to standardized oral hygiene to reduce bacterial colonization and ventilator associated pneumonia in mechanically ventilated patients: a randomised control trial. International Journal of Nursing Studies 2011; 48: 681‐8. jMunro CL, Grap MJ, Jones DJ, McClish DK, Sessler CN. Chlorhexidine, toothbrushing, and preventing ventilator‐associated pneumonia in critically ill adults. American Journal of Critical Care 2009; 18: 428‐37; quiz 438. kShi Z, Xie H, Wang P, Zhang Q, Wu Y, Chen E, et al. Oral hygiene care for critically ill patients to prevent ventilator‐associated pneumonia. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No.: CD008367 DOI: 10.1002/14651858.CD008367.pub2. lPanchabhai TS, Dangayach NS, Krishnan A, Kothari VM, Karnad DR. Oropharyngeal cleansing With 0.2% chlorhexidine for prevention of nosocomial pneumonia in critically iII patients an open‐label randomized trial with 0.01% potassium permanganate as control. Chest 2009; 135: 1150‐6. mCabov T, Macan D, Husedzinovic I, Skrlin‐Subic J, Bosnjak D, Sestan‐Crnek S, et al. The impact of oral health and 0.2% chlorhexidine oral gel on the prevalence of nosocomial infections in surgical intensive‐care patients: a randomized placebo‐controlled study. Wien Klin Wochenschr 2010; 122: 397‐404. nBellissimo‐Rodrigues F, Bellissimo‐Rodrigues WT, Viana JM, Teixeira CA, Nicolini E, Auxiliadora‐Martins M, et al. Effectiveness of oral rinse with chlorhexidine in preventing nosocomial respiratory tract infections among intensive care unit patients. Infection Control & Hospital Epidemiology 2009; 30: 952‐8.
Contributors
Comment: Richard Price, Graeme MacLennan, John Glen and Brian H Cuthbertson on behalf of the SuDDICU collaboration (Selective Decontamination of the Digestive tract in critically ill patients treated in Intensive Care Unit).
Reply: Review authors Fang Hua, Susan Furness and Helen Worthington.
What's new
| Date | Event | Description |
|---|---|---|
| 1 May 2020 | New citation required and conclusions have changed | In the previous version, we found no evidence of a benefit from toothbrushing patients in intensive care; however, in our updated review, we found low‐certainty evidence that it may reduce the incidence of VAP and very low certainty evidence that it may reduce the length of ICU stay. In this update, we found the number needed to treat for an additional beneficial outcome from CHX is probably 12, whereas it was 17 in the previous version. |
| 25 February 2020 | New search has been performed | Inclusion criteria modified. New search run, which found 9 new studies for inclusion. Seven previously included studies now excluded. Added new comparison (CHX versus other oral care agents) and reclassified included studies accordingly. |
History
Protocol first published: Issue 2, 2010 Review first published: Issue 8, 2013
| Date | Event | Description |
|---|---|---|
| 6 March 2017 | Feedback has been incorporated | See Feedback section for comments regarding different interpretations in other reviews of the effects of chlorhexidine on mortality in critically ill patients. |
| 6 March 2017 | Amended | Edits to Analysis 1.2 and 4.2. In response to the feedback, review authors decided that mortality data derived from trial flow diagrams in Berry 2011 and Berry 2013 should not be used. This does not change the mortality results: chlorhexidine versus placebo, RR 1.09 (95% CI 0.96 to 1.23). Removal of Berry 2011 and 2013 mortality data also means no conclusions can be drawn about the effect on mortality of bicarbonate rinse versus water, Listerine versus water or Listerine versus bicarbonate (previous analyses 4.2.6, 4.2.7, 4.2.8). |
| 20 July 2016 | New citation required but conclusions have not changed | 6 new studies included. 3 previously included studies now excluded. Some changes to Methods (see 'Differences between protocol and review' section). |
| 17 December 2015 | New search has been performed | Search updated. |
| 27 November 2013 | Amended | Minor typographical error. |
Notes
This is the second update of a review originally published in 2013 (Shi 2013) and first updated in 2016 (Hua 2016).
Acknowledgements
For the 2020 update, we would like to thank Philip Riley, Ana Jeroncic, Anne‐Marie Glenny, Laura MacDonald and Janet Lear at Cochrane Oral Health, as well as Jennifer Hilgart, Richard Price, Julián Balanta‐Melo and SK Sidhu for their helpful commentsm and Anne Lethaby for copy editing.
We would also like to thank Anne Littlewood, Information Specialist of Cochrane Oral Health (COH), for refining search strategies and providing searching results from the databases of COH's Trials Register, CENTRAL, MEDLINE, Embase, LILACS, CINAHL, ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform. For help with the translations of foreign papers, our thanks go to Sepideh Banava (Persian), Kim Kun Hyung (Korean), Luisa Fernandez‐Mauleffinch (Portuguese) and Roca Biosca (Spanish).
We would like to acknowledge the contributions of Zongdao Shi, Ping Wang, Yan Wu, E Chen, Linda Ng and Ian Needleman as authors of the original review published in 2013 (Shi 2013), and the contributions of Susan Furness and Huixu Xie as authors of the 2016 update (Hua 2016).
Appendices
Appendix 1. Cochrane Oral Health's Trials Register search strategy
Cochrane Oral Health’s Trials Register is available via the Cochrane Register of Studies. For information on how the register is compiled, see https://oralhealth.cochrane.org/trials.
#1 ((critical* AND ill*):ti,ab) AND (INREGISTER) #2 ((depend* and patient*):ti,ab) AND (INREGISTER) #3 (("critical care" or " intensive care" or ICU or CCU):ti,ab) AND (INREGISTER) #4 ((intubat* or ventilat*):ti,ab) AND (INREGISTER) #5 ((#1 or #2 or #3 or #4)) AND (INREGISTER) #6 ((pneumonia or "nosocomial infect*" or VAP):ti,ab) AND (INREGISTER) #7 (#5 and #6) AND (INREGISTER)
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 MeSH descriptor Critical illness this term only #2 (critical* in All Text near/6 ill* in All Text) #3 (depend* in All Text near/6 patient* in All Text) #4 MeSH descriptor Critical care this term only #5 (intensive‐care in All Text or "intensive care" in All Text or critical‐care in All Text or "critical care" in All Text) #6 ICU in Title, Abstract or Keywords #7 ((intubat* in All Text near/5 patient* in All Text) or (ventilat* in All Text near/5 patient* in All Text)) #8 (#1 or #2 or #3 or #4 or #5 or #6 or #7) #9 (VAP in Title, Abstract or Keywords or VAP in Title, Abstract or Keywords) #10 "nosocomial infection*" in Title, Abstract or Keywords #11 MeSH descriptor Pneumonia, Ventilator‐Associated this term only #12 pneumonia in All Text #13 (#9 or #10 or #11 or #12) #14 MeSH descriptor Oral health this term only #15 MeSH descriptor Oral hygiene explode all trees #16 MeSH descriptor Dentifrices explode all trees #17 MeSH descriptor Mouthwashes explode all trees #18 MeSH descriptor Periodontal diseases explode all trees #19 periodont* in All Text #20 ("oral care" in All Text or "oral health" in All Text or oral‐health in All Text or "mouth care" in All Text or "oral hygien*" in All Text or oral‐hygien* in All Text or "dental hygien*" in All Text or decontaminat* in All Text) #21 (mouthwash* in All Text or mouth‐wash* in All Text or mouth‐rins* in All Text or mouthrins* in All Text or "oral rins*" in All Text or oral‐rins* in All Text or "artificial saliva" in All Text or "saliva substitut*" in All Text or ( (denture* in All Text near/6 clean* in All Text) or toothpaste* in All Text) or dentifrice* in All Text) #22 (#14 or #15 or #16 or #17 or #18 or #19 or #20 or #21) #23 (#8 and #13) #24 (#22 and #23)
Appendix 3. MEDLINE Ovid search strategy
1. CRITICAL ILLNESS/ 2. (critical$ adj5 ill$).mp. 3. (depend$ adj5 patient$).mp. 4. INTENSIVE CARE/ 5. ("intensive care" or intensive‐care or "critical care" or critical‐care).mp. 6. ICU.mp. or CCU.ti,ab. 7. ((intubat$ or ventilat$) adj5 patient$).mp. 8. or/1‐7 9. PNEUMONIA, VENTILATOR‐ASSOCIATED/ 10. pneumonia.ti,ab. 11. VAP.ti,ab. 12. "nosocomial infection".mp. 13. or/9‐12 14. exp ORAL HYGIENE/ 15. exp DENTIFRICES/ 16. MOUTHWASHES/ 17. ANTI‐INFECTIVE AGENTS, LOCAL/ 18. Cetylpyridinium/ 19. Chlorhexidine/ 20. Povidone‐Iodine/ 21. ("oral care" or "mouth care" or "oral hygien$" or oral‐hygien$ or "dental hygien$").ti,ab. 22. (mouthwash$ or mouth‐wash$ or mouth‐rins$ or mouthrins$ or "oral rins$" or oral‐rins$ or toothpaste$ or dentifrice$ or toothbrush$ or chlorhexidine$ or betadine$ or triclosan$ or cepacol or Corsodyl or Peridex or Hibident or Prexidine or Parodex or Chlorexil or Peridont or Eludril or Perioxidin or Chlorohex or Savacol or Periogard or Chlorhexamed or Nolvasan or Sebidin or Tubulicid or hibitane).mp. 23. (antiseptic$ or antiinfect$ or "local microbicide$" or "topical microbicide$").mp. 24. or/14‐23 25. 8 and 13 and 24
Appendix 4. Embase Ovid search strategy
1. CRITICAL ILLNESS/ 2. (critical$ adj5 ill$).mp. 3. (depend$ adj5 patient$).mp. 4. INTENSIVE CARE/ 5. ("intensive care" or intensive‐care or "critical care" or critical‐care).mp. 6. (ICU or CCU).ti,ab. 7. ((intubat$ or ventilat$) adj5 patient$).mp. 8. or/1‐7 9. PNEUMONIA, VENTILATOR‐ASSOCIATED/ 10. pneumonia.ti,ab. 11. VAP.ti,ab. 12. "nosocomial infection".mp. 13. or/9‐12 14. exp ORAL HYGIENE/ 15. exp DENTIFRICES/ 16. MOUTHWASHES/ 17. ANTI‐INFECTIVE AGENTS, LOCAL/ 18. Cetylpyridinium/ 19. Chlorhexidine/ 20. Povidone‐Iodine/ 21. ("oral care" or "mouth care" or "oral hygien$" or oral‐hygien$ or "dental hygien$").ti,ab. 22. (mouthwash$ or mouth‐wash$ or mouth‐rins$ or mouthrins$ or "oral rins$" or oral‐rins$ or toothpaste$ or dentifrice$ or toothbrush$ or chlorhexidine$ or betadine$ or triclosan$ or cepacol or Corsodyl or Peridex or Hibident or Prexidine or Parodex or Chlorexil or Peridont or Eludril or Perioxidin or Chlorohex or Savacol or Periogard or Chlorhexamed or Nolvasan or Sebidin or Tubulicid or hibitane).mp. 23. (antiseptic$ or antiinfect$ or "local microbicide$" or "topical microbicide$").mp. 24. or/14‐23 25. 8 and 13 and 24
This subject search was linked to the Cochrane search filter for identifying randomised trials in Embase (2016 version) as referenced in Lefebvre 2019.
1. Randomized controlled trial/ 2. Controlled clinical study/ 3. random$.ti,ab. 4. randomization/ 5. intermethod comparison/ 6. placebo.ti,ab. 7. (compare or compared or comparison).ti. 8. ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 9. (open adj label).ti,ab. 10. ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 11. double blind procedure/ 12. parallel group$1.ti,ab. 13. (crossover or cross over).ti,ab. 14. ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 15. (assigned or allocated).ti,ab. 16. (controlled adj7 (study or design or trial)).ti,ab. 17. (volunteer or volunteers).ti,ab. 18. human experiment/ 19. trial.ti. 20. or/1‐19 21. random$ adj sampl$ adj7 ("cross section$" or questionnaire$1 or survey$ or database$1)).ti,ab. not (comparative study/ or controlled study/ or randomi?ed controlled.ti,ab. or randomly assigned.ti,ab.) 22. Cross‐sectional study/ not (randomized controlled trial/ or controlled clinical study/ or controlled study/ or randomi?ed controlled.ti,ab. or control group$1.ti,ab.) 23. (((case adj control$) and random$) not randomi?ed controlled).ti,ab. 24. (Systematic review not (trial or study)).ti. 25. (nonrandom$ not random$).ti,ab. 26. "Random field$".ti,ab. 27. (random cluster adj3 sampl$).ti,ab. 28. (review.ab. and review.pt.) not trial.ti. 29. "we searched".ab. and (review.ti. or review.pt.) 30. "update review".ab. 31. (databases adj4 searched).ab. 32. (rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys or trout or marmoset$1).ti. and animal experiment/ 33. Animal experiment/ not (human experiment/ or human/) 34. or/21‐33 35. 20 not 34
Appendix 5. CINAHL EBSCO search strategy
S25 S14 and S24 S24 S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 S23 (antiseptic* or antiinfect* or "local microbicide*" or "topical microbicide*") S22 (mouthwash* or mouth‐wash* or mouth‐rins* or mouthrins* or "oral rins*" or oral‐rins* or toothpaste* or dentifrice* or toothbrush* or chlorhexidine* or betadine* or triclosan* or cepacol or Corsodyl or Peridex or Hibident or Prexidine or Parodex or Chlorexil or Peridont or Eludril or Perioxidin or Chlorohex or Savacol or Periogard or Chlorhexamed or Nolvasan or Sebidin or Tubulicid or hibitane) S21 ("oral care" or "mouth care" or "oral hygien*" or oral‐hygien* or "dental hygien*") S20 (MH Povidone‐Iodine) S19 (MH Chlorhexidine) S18 (MH "Antiinfective Agents, Local") S17 MH MOUTHWASHES S16 (MH "DENTIFRICES+") S15 (MH "Oral Hygiene+") S14 S8 AND S13 S13 S9 or S10 or S11 or S12 S12 TI pneumonia or AB pneumonia S11 MH PNEUMONIA, VENTILATOR‐ASSOCIATED S10 TI "nosocomial infection" and AB "nosocomial infection" S9 TI VAP or AB VAP S8 S1 or S2 or S3 or S4 or S5 or S6 or S7 S7 ((intubat* N5 patient*) or (ventilat* N5 patient*)) S6 TI ICU or AB ICU or TI CCU or AB CCU S5 (intensive‐care or "intensive care" or critical‐care or "critical care") S4 MH CRITICAL CARE S3 (depend* N6 patient*) S2 (critical* N6 ill*) S1 MH CRITICAL ILLNESS
Appendix 6. LILACS BIREME Virtual Health Library search strategy
(Mh Critical illness or "Enfermedad Crítica" or "Estado Terminal" or "critical illness$" or Mh Intensive care or "Cuidados Intensivos" or "Terapia Intensiva" or "critical care" or "intensive care" or "ICU" or "CCU" or intubate$ or ventilate$) [Words] and (Mh Pneumonia, Ventilator‐Associated or "Neumonia Asociada al Ventilador" or "Pneumonia Associada à Ventilação Mecânica" or (ventilator AND pneumonia)) [Words] and (Mh Oral hygiene or "oral hygiene" or "Higiene Bucal" or "oral care" or "mouth care" or mouthwash$ or mouthrins$ or toothpaste$ or dentifrice$ or chlorhexidine or betadine or triclosan or Clorhexidina or Clorexidina or "Antisépticos Bucales" or "Antissépticos Bucais" or "Cepillado Dental" or "Escovação Dentária" or antiseptic$ or antiinfective$)
Appendix 7. VIP search strategy
(R=口腔 AND R=肺炎 AND R=随机) limited to (核心期刊 AND Time=2012‐2016)
Appendix 8. Search strategies used for previous versions of this review
Chinese Biomedical Literature Database search strategy
#1 缺省[智能]:危重 ‐限定:1978‐2012
#2 缺省:ICU ‐限定:1978‐2012
#3 缺省:VAP ‐限定:1978‐2012
#4 缺省:插管 ‐限定:1978‐2012
#5 #4 or #3 or #2 or #1
#6 缺省:口腔护理
#7 缺省[智能]:口腔清洁
#8 缺省:口腔卫生
#9 缺省[智能]:刷牙
#10 #9 or #8 or #7 or #6
#11 #10 and #5
#12 缺省[智能]:随机
#13 缺省:随机对照
#14 #13 or #12
#15 #14 and #11
China National Knowledge Infrastructure search strategy
#1 数据库:中国期刊全文数据库 检索条件:((题名=VAP) 或者 (摘要=ICU) 或者 (题名=危重))并且(摘要=呼吸机相关性肺炎) 或者 (摘要=插管) (模糊匹配);2003‐2012;全部期刊;时间排序; 单库检索
#2 数据库:中国期刊全文数据库 检索条件: (题名=口腔护理) 或者 (摘要=口腔去污染) 或者 (题名=口腔清洁) 或者 (摘要=刷牙) 或者 (主题=口腔卫生) (模糊匹配);时间排序; 单库检索(结果中检索)
#3 数据库:中国期刊全文数据库 检索条件: (题名=随机对照) 或者 (摘要=随机) 或者 (题名=随机对照实验) 或者 (摘要=随机分配) 或者 (主题=随机隐藏) (模糊匹配);时间排序; 单库检索(结果中检索)
Wan Fang Database search strategy
1. ((全部字段 =(模糊匹配) "危重") ) ;按相关度排序
2. ((全部字段 =(模糊匹配) "ICU") ) ;按相关度排序
3. ((全部字段 =(模糊匹配) "VAP") ) ;按相关度排序
4. ((全部字段 =(模糊匹配) "口腔") ) ;按相关度排序
5. ((全部字段 =(模糊匹配) "刷牙") ) ;按相关度排序
6. ((全部字段 =(模糊匹配) "去污染") ) ;按相关度排序
7. ((全部字段 =(模糊匹配) "洗必泰") ) ;按相关度排序
8. ((全部字段 =(模糊匹配) "口腔冲洗") ) ;按相关度排序
9. ((全部字段 =(模糊匹配) "危重") ) 或 ((全部字段 =(模糊匹配) "ICU") ) 或 ((全部字段 =(模糊匹配) "VAP") )
10. ((全部字段 =(模糊匹配) "口腔") ) 或 ((全部字段 =(模糊匹配) "刷牙") ) 或 ((全部字段 =(模糊匹配) "去污染") ) 或 ((全部字段 =(模糊匹配) "洗必泰") ) 或 ((全部字段 =(模糊匹配) "口腔冲洗") )
11. ( ((全部字段 =(模糊匹配) "口腔") ) 或 ((全部字段 =(模糊匹配) "刷牙") ) 或 ((全部字段 =(模糊匹配) "去污染") ) 或 ((全部字段 =(模糊匹配) "洗必泰") ) 或 ((全部字段 =(模糊匹配) "口腔冲洗") ) ) 与 ( ((全部字段 =(模糊匹配) "口腔") ) 或 ((全部字段 =(模糊匹配) "刷牙") ) 或 ((全部字段 =(模糊匹配) "去污染") ) 或 ((全部字段 =(模糊匹配) "洗必泰") ) 或 ((全部字段 =(模糊匹配) "口腔冲洗") ) 与 ((全部字段 =(模糊匹配) "危重") ) 或 ((全部字段 =(模糊匹配) "ICU") ) 或 ((全部字段 =(模糊匹配) "VAP") ) )
Appendix 9. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
ventilator and pneumonia and "oral hygiene"
Appendix 10. World Health Organization International Clinical Trials Registry Platform search strategy
ventilator and pneumonia and "oral hygiene"
Data and analyses
Comparison 1. Chlorhexidine versus placebo/usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Incidence of VAP | 13 | 1206 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.47, 0.97] |
| 1.1.1 Chlorhexidine solution versus placebo (no toothbrushing in either group) | 6 | 429 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.33, 1.00] |
| 1.1.2 Chlorhexidine gel versus placebo (no toothbrushing in either group) | 2 | 297 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.29, 0.97] |
| 1.1.3 Chlorhexidine solution versus placebo (toothbrushing both groups) | 3 | 332 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.29, 1.89] |
| 1.1.4 Chlorhexidine gel versus placebo (toothbrushing both groups) | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.83, 1.79] |
| 1.2 Mortality | 9 | 944 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.84, 1.23] |
| 1.2.1 Chlorhexidine solution versus placebo (no toothbrushing in either group) | 4 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.80, 1.33] |
| 1.2.2 Chlorhexidine gel versus placebo (no toothbrushing in either group) | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.2.3 Chlorhexidine solution versus placebo (toothbrushing both groups) | 2 | 382 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.72, 1.40] |
| 1.2.4 Chlorhexidine gel versus placebo (toothbrushing both groups) | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.59, 1.68] |
| 1.3 Duration of ventilation (days) | 4 | 594 | Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐3.20, 1.00] |
| 1.3.1 Chlorhexidine solution versus placebo (no toothbrushing in either group) | 3 | 263 | Mean Difference (IV, Random, 95% CI) | ‐2.63 [‐3.35, ‐1.90] |
| 1.3.2 Chlorhexidine gel versus placebo (no toothbrushing in either group) | 1 | 257 | Mean Difference (IV, Random, 95% CI) | 2.21 [‐0.30, 4.72] |
| 1.3.3 Chlorhexidine solution versus placebo (toothbrushing both groups) | 1 | 74 | Mean Difference (IV, Random, 95% CI) | ‐1.30 [‐4.20, 1.60] |
| 1.4 Duration of ICU stay (days) | 5 | 627 | Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐3.59, 1.82] |
| 1.4.1 Chlorhexidine solution versus placebo (no toothbrushing in either group) | 3 | 274 | Mean Difference (IV, Random, 95% CI) | ‐2.92 [‐4.18, ‐1.66] |
| 1.4.2 Chlorhexidine gel versus placebo (no toothbrushing in either group) | 1 | 257 | Mean Difference (IV, Random, 95% CI) | 1.32 [‐2.43, 5.07] |
| 1.4.3 Chlorhexidine gel versus placebo (toothbrushing both groups) | 1 | 96 | Mean Difference (IV, Random, 95% CI) | 5.00 [‐2.20, 12.20] |
| 1.5 Duration of systemic antibiotic therapy (days) | 1 | 146 | Mean Difference (IV, Fixed, 95% CI) | 0.65 [‐0.58, 1.88] |
| 1.5.1 Chlorhexidine solution versus placebo (toothbrushing both groups) | 1 | 146 | Mean Difference (IV, Fixed, 95% CI) | 0.65 [‐0.58, 1.88] |
| 1.6 Number of participants treated with systemic antibiotics | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.6.1 Chlorhexidine solution versus placebo (no toothbrushing in either group) | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.53, 1.38] |
| 1.7 Plaque index | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.7.1 Chlorhexidine solution versus placebo (no toothbrushing in either group) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.8 Adverse effects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.8.1 Reversible mild irritation of oral mucosa | 1 | 207 | Risk Ratio (M‐H, Fixed, 95% CI) | 10.29 [1.34, 78.97] |
Comparison 2. Chlorhexidine versus other oral care agents.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Incidence of VAP | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1.1 Chlorhexidine versus potassium permanganate | 2 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.50, 1.52] |
| 2.1.2 Chlorhexidine versus ozonated water | 1 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.60 [1.12, 6.03] |
| 2.1.3 Chlorhexidine versus Nanosil | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.76 [1.17, 65.78] |
| 2.1.4 Chlorhexidine versus hydrogen peroxide | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.06, 1.28] |
| 2.1.5 Chlorhexidine versus miswak | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 13.00 [0.76, 222.31] |
| 2.2 Mortality | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.2.1 Chlorhexidine versus potassium permanganate | 2 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.89, 1.38] |
| 2.2.2 Chlorhexidine versus Nanosil | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.87 [0.24, 98.18] |
| 2.3 Number of participants treated with systemic antibiotics | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.3.1 Chlorhexidine versus miswak | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. Toothbrushing versus no toothbrushing.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Incidence of VAP | 5 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.41, 0.91] |
| 3.1.1 Powered toothbrush + usual care (± CHX) versus usual care (± CHX) | 2 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.16, 1.53] |
| 3.1.2 Toothbrush + CHX versus CHX alone | 2 | 649 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.50, 1.09] |
| 3.1.3 Toothbrush + povidone iodine versus povidone iodine alone | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.13, 0.98] |
| 3.2 Mortality | 5 | 910 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.67, 1.05] |
| 3.2.1 Powered toothbrush + usual care versus usual care | 2 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.17, 9.91] |
| 3.2.2 Toothbrush + CHX versus CHX alone | 2 | 649 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.68, 1.12] |
| 3.2.3 Toothbrush + povidone iodine versus povidone iodine alone | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.15, 2.22] |
| 3.3 Duration of ventilation (days) | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.3.1 Toothbrush + CHX versus CHX alone | 3 | 749 | Mean Difference (IV, Fixed, 95% CI) | ‐1.46 [‐2.69, ‐0.23] |
| 3.3.2 Toothbrush + povidone iodine versus povidone iodine alone | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | 0.13 [‐0.78, 1.04] |
| 3.4 Duration of ICU stay (days) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.4.1 Toothbrush + CHX versus CHX alone | 3 | 749 | Mean Difference (IV, Fixed, 95% CI) | ‐1.89 [‐3.52, ‐0.27] |
| 3.5 Plaque score | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.5.1 Powered toothbrush versus usual care | 1 | 49 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.22 [‐1.83, ‐0.60] |
Comparison 4. Powered toothbrush versus manual toothbrush.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Incidence of VAP | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1.1 Powered toothbrush + comp oral care versus manual toothbrush + std oral care | 1 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.37, 1.91] |
| 4.2 Mortality | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.2.1 Powered toothbrush + comp oral care versus manual toothbrush + std oral care | 1 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.16, 7.10] |
| 4.3 Duration of ventilation (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.3.1 Powered toothbrush + comp oral care versus manual toothbrush + std oral care | 1 | 78 | Mean Difference (IV, Fixed, 95% CI) | 0.00 [‐1.78, 1.78] |
| 4.4 Duration of ICU stay (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.4.1 Powered toothbrush + comp oral care versus manual toothbrush + std oral care | 1 | 78 | Mean Difference (IV, Fixed, 95% CI) | ‐2.00 [‐5.93, 1.93] |
Comparison 5. Other oral care agents.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Incidence of VAP | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1.1 Povidone iodine versus saline/placebo | 3 | 356 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.50, 0.95] |
| 5.1.2 Povidone iodine versus usual care | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.06, 0.63] |
| 5.1.3 Saline rinse versus saline swab | 4 | 488 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.37, 0.62] |
| 5.1.4 Saline rinse versus usual care | 2 | 324 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.39, 0.91] |
| 5.1.5 Saline rinse + swab versus saline swab (usual care) | 2 | 153 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.23, 0.72] |
| 5.1.6 Bicarbonate rinse versus water | 2 | 347 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [0.62, 3.99] |
| 5.1.7 Triclosan rinse versus saline | 1 | 324 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.71, 1.12] |
| 5.1.8 Furacilin versus povidone iodine | 1 | 136 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.23, 1.04] |
| 5.1.9 Furacilin versus saline | 1 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.14, 0.58] |
| 5.1.10 Listerine versus water | 1 | 265 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.36, 3.28] |
| 5.1.11 Listerine versus bicarbonate | 1 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.35, 3.16] |
| 5.1.12 Biotene versus control | 1 | 41 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.28, 1.41] |
| 5.1.13 Hydrogen peroxide versus normal saline | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.15, 0.96] |
| 5.1.14 Potassium permanganate versus placebo | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.21, 1.05] |
| 5.2 Mortality | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.2.1 Povidone iodine versus saline/placebo | 2 | 217 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.66, 1.50] |
| 5.2.2 Povidone iodine versus usual care | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.31, 2.40] |
| 5.2.3 Saline rinse versus saline swab | 2 | 270 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.12, 0.69] |
| 5.2.4 Saline rinse + swab versus saline swab (usual care) | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.11, 1.28] |
| 5.2.5 Saline rinse versus usual care | 2 | 324 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.87, 1.39] |
| 5.2.6 Biotene versus control | 1 | 41 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.13, 3.76] |
| 5.2.7 Potassium permanganate versus placebo | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.48, 4.12] |
| 5.3 Duration of ventilation (days) | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.3.1 Povidone iodine versus saline | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐4.36, 2.36] |
| 5.3.2 Povidone iodine versus usual care | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐3.00 [‐7.67, 1.67] |
| 5.3.3 Saline rinse versus usual care | 2 | 324 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐2.55, 1.75] |
| 5.3.4 Saline rinse + swab versus saline swab | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐3.91 [‐5.85, ‐1.97] |
| 5.3.5 Saline rinse versus saline swab | 2 | 176 | Mean Difference (IV, Fixed, 95% CI) | ‐6.83 [‐8.94, ‐4.72] |
| 5.3.6 Triclosan rinse versus saline | 1 | 324 | Mean Difference (IV, Fixed, 95% CI) | ‐5.24 [‐5.64, ‐4.84] |
| 5.4 Duration of ICU stay (days) | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.4.1 Povidone iodine versus saline/placebo | 2 | 217 | Mean Difference (IV, Fixed, 95% CI) | ‐0.35 [‐3.90, 3.21] |
| 5.4.2 Povidone iodine versus usual care | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | ‐4.00 [‐10.99, 2.99] |
| 5.4.3 Saline rinse versus usual care | 2 | 324 | Mean Difference (IV, Fixed, 95% CI) | ‐1.17 [‐3.95, 1.60] |
| 5.4.4 Triclosan rinse versus saline | 1 | 324 | Mean Difference (IV, Fixed, 95% CI) | ‐4.97 [‐5.55, ‐4.39] |
| 5.5 Number of participants treated with systemic antibiotics | 1 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.66, 1.05] |
| 5.5.1 Povidone iodine versus saline/placebo | 1 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.66, 1.05] |
| 5.6 Adverse effects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.6.1 Acute respiratory distress syndrome | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.00 [0.62, 195.61] |
| 5.6.2 Agitation and/or hypertension | 1 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.12, 1.86] |
| 5.6.3 Epistaxis | 1 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.63] |
| 5.6.4 Oxygen desaturation | 1 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.06, 15.17] |
| 5.6.5 Aspiration | 1 | 167 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.90 [0.12, 70.07] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bellissimo‐Rodrigues 2009.
| Study characteristics | ||
| Methods | Study design: RCT, 2 parallel groups Location: Sao Paulo, Brazil Number of centres: 1 Study period: March 2006 to February 2008 Funding source: not stated |
|
| Participants | Setting: ICU in tertiary care hospital Inclusion criteria: all patients admitted to ICU with expected stay > 48 hours Not all participants received mechanical ventilation. Exclusion criteria: previous chlorhexidine sensitivity, pregnancy, formal indication for chlorhexidine use, prescription of another oral topical medication Number randomised: 200 (only 133 on ventilators) Number evaluated: 194 Baseline characteristics: ‐ Intervention group age: median 62.5 (17 ‐ 89) M/F: 47/51; APACHE II Score: median 17 (5 ‐ 35) ‐ Control group age: median 54.0 (15 ‐ 85) M/F: 51/45; APACHE II Score: median 19 (5 ‐ 41) |
|
| Interventions |
Comparison: 0.12% chlorhexidine solution versus placebo Experimental group (n = 64 on vent): 0.12% chlorhexidine solution applied orally 3 times daily. Oral hygiene was conducted by nurses specially trained in the protocol. 3 times daily after mechanical cleaning of the mouth by a nurse, 15 mL of study solution was applied and attempts made to distribute solution over all oral surfaces. Control group (n = 69 on vent): same protocol conducted with placebo solution, which was identical in colour, consistency, smell and taste |
|
| Outcomes | 1. Respiratory tract infections (VAP for those on ventilators) 2. Respiratory tract infection‐free survival time 3. Time from ICU admission to first RTI 4. Duration of mechanical ventilation 5. Length of ICU stay 6. Total mortality 7. Mortality due to RTI 8. Antibiotic use 9. Microbiological culture of endotracheal secretions 10. Adverse effects |
|
| Notes | Sample size calculation: "to have sufficient power to detect a 69% difference in incidence of VAP with α = 5% and β = 20% it was estimated that 96 patients per group were required". Only 133/194 of patients evaluated received mechanical ventilation. Email sent 3 September 2012. Reply received The Cochrane calculator was used to calculate the SD value for duration of mechanical ventilation, but the SD obtained seemed inappropriate and was therefore not used in data synthesis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomised" Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | "only the pharmacist knew which code numbers corresponded to which type of solution". |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6/200 participants were excluded from the analysis. 1 control participant needed to receive chlorhexidine treatment, and a further 3 in the control group and 2 in the experimental group were excluded due to protocol violation. Unlikely to have introduced a bias |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Berry 2011.
| Study characteristics | ||
| Methods | Study design: feasibility study – single‐blind parallel‐group RCT with 3 groups Location: Australia Number of centres: 1 Study period: not stated Funding source: hospital |
|
| Participants | Setting: 20‐bed adult intensive care unit in a university hospital Inclusion criteria: all intubated patients admitted to the unit were considered for inclusion in the study provided they met the following criteria: able to be randomised within 12 hours of intubation, aged over 15 years and next‐of‐kin able to give informed consent. Exclusion criteria: patients were ineligible for study participation if they: required specific oral hygiene procedures in relation to maxillofacial trauma or dental trauma/surgery; had been in the ICU previously during the current period of hospitalisation; received irradiation or chemotherapy on admission to the ICU or in the preceding 6 weeks; or suffered an autoimmune disease. Informed consent was obtained for all participants and agreement to participate could be withdrawn at any time. Number randomised: 225 (71, 76, 78 in groups 1, 2, 3) Number evaluated: 109 (33, 33, 43 in groups 1, 2, 3) Group 1 (chlorhexidine 0.2% aqueous) group: age: 58.2 ± 19.4; M/F: 35/36; APACHE II Score: 22.8 ± 7.8 Group 2 (sodium bicarbonate mouthwash rinsed 2‐hourly): age: 60.4 ± 17.5; M/F: 42/24; APACHE II Score: 22.0 ± 7.5 Group 3 (sterile water rinsed 2‐hourly): age: 59.1 ± 18.1; M/F: 44/34; APACHE II Score: 21.6 ± 7.8 |
|
| Interventions |
Comparison: Chlorhexidine 0.2% versus sodium bicarbonate versus water Group 1: Twice daily irrigation with chlorhexidine 0.2% aqueous oral rinse with 2‐hourly irrigation with sterile water Group 2: Sodium bicarbonate mouthwash rinsed 2‐hourly Group 3: Sterile water rinsed 2‐hourly (used as the control in this review) "All treatment options included a comprehensive cleaning of the mouth using a soft, pediatric toothbrush 3 times a day". |
|
| Outcomes | 3 outcome variables were reported: 1. Microbial colonisation of dental plaque (or gums in edentulous participants) 2. Incidence of VAP 3. Adverse events |
|
| Notes | Sample size calculation: Feasibility study to inform sample size calculation for main study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...randomisation into one of three groups according to a balanced randomisation table prepared by biostatistician" |
| Allocation concealment (selection bias) | Low risk | Study packs were identical in outward appearance and allocation remained blinded until study pack opened by attending nurse. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants: blinding not possible, but non‐blinding of caregivers may have introduced a risk of bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Microbiologist and radiologists who assessed outcomes were blinded to allocated treatment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 102/225 participants evaluated. High rate of attrition and reasons varied in each group. Death rate higher in group B, breach of inclusion criteria more likely in groups B & C |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | High risk | Study stopped early due to withdrawal of investigational product by regulator. |
Berry 2013.
| Study characteristics | ||
| Methods | Study design: 3‐arm parallel‐group RCT Location: Australia Number of centres: 1 Study period: not stated Funding source: Pfizer provided product only |
|
| Participants | Setting: ICU in a 1000‐bed tertiary referral teaching hospital Inclusion criteria: admitted to ICU, able to be randomised within 12 hours of intubation; aged over 15 years; next‐of‐kin able to give informed consent Exclusion criteria: required specific oral hygiene procedures following facio‐maxillary or dental trauma/surgery; had received irradiation or chemotherapy on admission to the ICU or in the preceding 6 weeks; diagnosed with autoimmune disease; had previous ICU admission during current period of hospitalisation Number randomised: 398 (group A: 138; group B: 133; group C: 127) Number evaluated: 398 (group A: 138; group B: 133; group C: 127); however, 11% of these participants were ineligible Baseline characteristics: ‐ Group A: Age: 58.82 (16.7); M/F: 84/54; APACHE II Score: 20.86 (7.7) ‐ Group B: Age: 54.93 (19.5); M/F: 79/54; APACHE II Score: 21.38 (8.0) ‐ Group C: Age: 59.96 (18.0); M/F: 73/54; APACHE II Score: 21.21 (8.0) |
|
| Interventions |
Comparison: Sterile water versus sodium bicarbonate versus Listerine Group A: Control – sterile water mouth rinses, 20 mL every 2 hours. Group B: Sodium bicarbonate mouth wash (6.5 g/L sterile water), 20 mL every 2 hours Group C: Listerine mouth wash, 20 mL instilled twice a day and sterile water every 2 hours for remaining time All 3 groups received mechanical cleaning of the oral cavity with a small, soft‐bristled toothbrush and general‐purpose toothbrush 3 times a day. Curved‐tip dental syringes were used to instil mouth rinses. During the study period, VAP preventive measures including head of the bed elevation, stress ulcer prophylaxis and endotracheal cuff occlusive pressure between 22 and 30 cm H2O were maintained. |
|
| Outcomes | 1. Incidence of VAP 2. Dental plaque colonisation 3. Systemic antibiotic administration (unclear if systemic) 4. Adverse effects |
|
| Notes | Sample size calculation: reported for inhibition of microbial growth on dental plaque, not VAP Emailed study investigator 10 April 2016 for publication details or full unpublished study data |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomisation numbers were computer generated”. |
| Allocation concealment (selection bias) | Low risk | “Nurses were blinded to the study option until the study packs were opened”. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Nurses were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Microbiologists…and…radiologists also blinded to the treatment code” |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 245 randomised participants (62%) were no longer in the study on the 4th day; Intention‐to‐treat analysis was used but unsure how and whether appropriate. |
| Selective reporting (reporting bias) | High risk | VAP data were only presented as percentages; 24 participants died within 4 days but unclear how many died after that; exact data for systemic antibiotic administration was not reported. |
| Other bias | Unclear risk | Ineligible patients were included in the ITT but reasons for ineligibility in each group were not given. |
Bopp 2006.
| Study characteristics | ||
| Methods | Study design: pilot study, 2‐arm RCT Location: USA Number of centres: 1 Study period: February 2002 to August 2002 Funding source: grant from American Dental Hygienists' Association's Institute for Oral Health |
|
| Participants | Setting: critical care unit Inclusion criteria: orally and nasally intubated patients entering critical care unit Exclusion criteria: taking metronidazole, history of allergy to chlorhexidine, sensitive to alcohol, risk for endocarditis, history of other serious illness (specified), those with pneumonia Number randomised: 5 Number evaluated: 5 Baseline characteristics: ‐ Intervention group: age: 40, range 28 ‐ 52; M/F: 0/2 ‐ Control group: age: 73.7, range 62 ‐ 81; M/F: 2/1 |
|
| Interventions |
Comparison: 0.12% chlorhexidine + suction toothbrush versus suction swab + hydrogen peroxide Experimental group (n = 2): twice daily oral hygiene care with 0.12% chlorhexidine gluconate during intubation period plus oral cleaning with PlaqVac suction toothbrush Control group (n = 3): standard oral care 6 times daily using a suctioning soft foam swab and half‐strength hydrogen peroxide, plus oral lubricant |
|
| Outcomes | Microbial colonisation VAP, mortality | |
| Notes | Sample size calculation: this was a pilot study. Data were not used in meta‐analysis on advice of statistician. Email sent to contact author 14 November 2012, reply received 19 November 2012 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...randomly assigned to either control or experimental treatment by the flip of a coin" |
| Allocation concealment (selection bias) | High risk | Coin toss was undertaken by researcher. No allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible. Reply from contact author "they were not blinded" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Reply from contact author "they were not blinded" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluation |
| Selective reporting (reporting bias) | Unclear risk | VAP planned and reported in this pilot study. Microbial culture data not reported per person, and mortality was also reported |
| Other bias | Low risk | No other sources of bias detected |
Cabov 2010.
| Study characteristics | ||
| Methods | Study design: 2 parallel‐arm RCT Location: Croatia Number of centres: 1 Study period: March 2008 to December 2008 Funding source: supported by Croatian Ministry of Science Education and Sports Grant number 065‐1080057‐0429 |
|
| Participants | Setting: surgical ICU in university hospital Inclusion criteria: aged > 18 years, medical condition suggesting hospitalisation in ICU > 3 days, eventual requirement for mechanical ventilation by oropharyngeal or nasotracheal ventilation Exclusion criteria: number randomised: 60. 40 of the 60 participants (17 and 23 in each group) were on mechanical ventilation Number evaluated: 60 Baseline characteristics: ‐ Intervention group: age: 57 ± 16; M/F: 19/11 ‐ Control group: age: 52 ± 19; M/F: 20/10 |
|
| Interventions |
Comparison: Chlorhexidine gel versus placebo Experimental group (n = 17): 3 times daily, following standard oral care comprising rinsing mouth with bicarbonate isotonic serum, followed by gentle oropharyngeal sterile aspiration; participants received application of 0.2% chlorhexidine gel applied by nurses to dental gingival and oral surfaces using a sterile gloved finger Control group (n = 23): standard oral care, 3 times daily as above followed by administration of placebo gel In both groups, gel was left in place and oral cavity was not rinsed |
|
| Outcomes | Simplified acute physiological score (SAPS), dental status, dental plaque, plaque culture, nosocomial infections, mortality | |
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...randomized into two groups using a computer‐generated balanced randomization table" |
| Allocation concealment (selection bias) | Unclear risk | Unclear who conducted the allocation and whether it was concealed from the investigators |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluations |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Caruso 2009.
| Study characteristics | ||
| Methods | Study design: 2‐arm RCT Location: Brazil Number of centres: 1 Study period: August 2001 to December 2004 Funding source: Not stated |
|
| Participants | Setting: closed medical surgical ICU unit in oncologic hospital Inclusion criteria: patients aged > 18 years expected to need mechanical ventilation for > 72 hours through orotracheal or tracheotomy tube Exclusion criteria: previous mechanical ventilation within past month, mechanical ventilation for > 6 hours prior to study enrolment, contraindication to bronchoscopy and expected to die or stop treatment within 48 hours Number randomised: 262 Number evaluated: 262 Baseline characteristics: ‐ Intervention group: age: 65 ± 14 years; M/F: 66/64 ‐ Control group: age: 63 ± 6 years; M/F: 70/62 |
|
| Interventions |
Comparison: Saline rinse versus usual care Experimental group (n = 130): instillation of 8 mL of isotonic saline prior to tracheal suctioning, which was conducted by respiratory therapists Control group (n = 132): tracheal suction alone with no saline instillation Aspirations were carried out when 1 of the following occurred: visible airway secretion into endotracheal tube, discomfort or participant asynchrony, noisy breathing, increased peak expiratory pressures, or decreased tidal volume during ventilation attributed to airway secretion. |
|
| Outcomes | 1. Incidence of VAP 2. Duration of ventilation in ICU 3. Length of stay in ICU 4. ICU mortality 5. Tracheal colonisation 6. Suctions per day, chest radiographs |
|
| Notes | Sample size calculation: estimated that 130 participants per group required to give 80% power with α = 5% to detect a decrease in VAP from 30% to 15%. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomised" No details of method of sequence generation provided in report |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Attending physicians and nurses blinded to study group. Intervention carried out by respiratory therapists available on ICU 24/7 |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessment conducted by physicians and nurses blinded to allocated treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluation |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported in full |
| Other bias | Low risk | No other sources of bias identified |
Dahiya 2012.
| Study characteristics | ||
| Methods | Study design: RCT Location: New Delhi, India Number of centres: 1 Study period: not reported Funding source: not reported |
|
| Participants | Setting: ICU of All India Institute of Medical Sciences Inclusion criteria: adult patients (> 18 years) admitted to ICU on mechanical ventilation for < 24 hours Exclusion criteria: not reported Number randomised: 70 (CHX: 35; H2O2: 35) Number evaluated: 70 (CHX: 35; H2O2: 35) Baseline characteristics: not reported; only stated that the demographic characteristics including age and sex were comparable between two groups (P > 0.05) |
|
| Interventions |
Comparison: 0.2% chlorhexidine gluconate solution versus hydrogen peroxide solution Oral decontamination was done for the groups twice daily at 8:00 a.m. and 7.00 p.m. for three consecutive days by the investigator. CHX: oral decontamination with 0.2% chlorhexidine gluconate solution (15 mL) twice daily at 8 a.m. and 7 p.m. for three consecutive days H2O2: oral decontamination using H2O2 with normal saline in a ratio of 1:8 (16 mL) twice daily at 8 a.m. and 7 p.m. for three consecutive days |
|
| Outcomes | 1. Incidence of VAP 2. Oropharyngeal colonisation |
|
| Notes | Sample size calculation: not reported Other information of note: study investigator replied to email 18 March 2020 and stated that 1) all included patients received MV for over 48 hours, 2) the CDC standard was used for diagnosis, and 3) VAP diagnosis was made at 48 and 72 hours. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | “random assignment was done by using numbered sealed envelope method”. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described and not possible. Difference between intervention and control means caregivers would be aware of who was in each group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Unclear risk | Insufficient information in the trial report to produce confidence in the methodology of this trial |
De Lacerda 2017.
| Study characteristics | ||
| Methods | Study design: two‐arm parallel‐group RCT Location: Brazil Number of centres: 4 Study period: July 2013 to January 2014 Funding source: Research Fund Program of Academic Strengthening of University of Pernambuco, and participating hospitals’ resources |
|
| Participants | Setting: clinical/surgical and cardiology ICU Inclusion criteria: age equal or greater than 18 years, expected to remain on mechanical ventilation for > 48 h, without evidence of pulmonary infection at admission Exclusion criteria: individuals without teeth, suspicion of pneumonia at the time of intubation, pregnancy, tracheostomy and chlorhexidine allergy Number randomised: 213 (gp A: 105; gp B: 108) Number evaluated: 213 (gp A: 105; gp B: 108) Baseline characteristics: ‐Gp A: (age: 59.4 ± 14.5; M/F: 51/54; APACHE II Score: 21.9 ± 7.5) ‐Gp B: (age: 63.2 ± 14.5; M/F: 54/54; APACHE II Score: 22.2 ± 7.7) |
|
| Interventions |
Comparison: Toothbrushing + CHX gelversus CHX solution only Gp A (toothbrushing + CHX gel): individuals undergoing oral hygiene every 12 h through aspiration of oropharyngeal secretion. Immediately after, toothbrushing was carried out on all tooth surfaces, tongue and mucosal surface of the mouth through the use of toothbrushes with small and soft bristles, and dental gel based on 0.12% CHX gluconate. After these steps, they proceeded with rinsing and suction through a catheter coupled to own toothbrush for the purpose of aspiration. Gp B (CHX solution only): individuals undergoing oral hygiene every 12 h, through aspiration of oropharyngeal secretion, immediately applying 15 mL of 0.12% CHX gluconate oral solution using a swab on all tooth surfaces, tongue and mucosal surface of the mouth All participants underwent the standard protocol for VAP prevention, which included maintaining a semirecumbent body position, with head elevation of ≥ 30°, gastrointestinal bleeding prophylaxis, deep venous thrombosis prophylaxis and daily interruption of sedation with assessing the possibility of extubation. |
|
| Outcomes | 1. Incidence of VAP 2. Duration of mechanical ventilation 3. Duration of ICU stay 4. Mortality rate in ICU |
|
| Notes | Sample size calculation: reported for VAP incidence Other information of note: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Patients were randomized...by means of opaque sealed envelopes containing the results from a computer generated random list.” |
| Allocation concealment (selection bias) | Low risk | “Patients were randomized by means of opaque sealed envelopes containing the results from a computer generated random list”. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Researchers and physicians were blinded but nurses responsible for oral hygiene care were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “Researchers and physicians did not know to which of both groups the individuals belonged, providing information to blind”. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluation |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Unclear risk | The method of CHX application was imbalanced between two groups (CHX gel vs. CHX solution). |
Feng 2012.
| Study characteristics | ||
| Methods | Study design: single‐centre RCT with 3 parallel groups (2 groups included in this review) Location: China Number of centres: 1 ICU in a city hospital Study period: February 2009 to January 2011 Funding source: not stated |
|
| Participants | Inclusion criteria: entry ICU, with orotracheal intubation and ventilation Exclusion criteria: pulmonary infection, stomatitis or oral tumours before intubation, accompanied by ulcer of the digestive tract, malignant tumours of the body, taking steroids > 3 days, diabetes Number randomised: 204 Number evaluated: 204 Intervention group: 0.05% povidone iodine: n = 71; mean age: 43.7 ± 8.1 years Intervention group: 1/5000 furacilin: n = 65; mean age: 38.5 ± 11.6 years Control group: saline n = 68; mean age: 40.3 ± 8.5 years Baseline characteristics: not specified |
|
| Interventions |
Comparison: Povidone iodine + toothbrushing versus furacilin versus saline + toothbrushing Group A (n = 71): toothbrushing along the slits between the teeth with 0.05% povidone iodine by nurses, then the oropharyngeal cavity was rinsed with 50 mL of the solution and it was suctioned out completely. This procedure was repeated 4 times a day. Group B (n= 65): toothbrushing along the slits between the teeth with 1/5000 furacilin by nurses Control group (n = 68): toothbrushing along the slits between the teeth with 0.9% saline by nurses, then the oropharyngeal cavity was rinsed with 50 mL of the saline and it was suctioned out completely. This procedure was repeated 4 times a day. |
|
| Outcomes | 4 outcome variables were reported: 1. Incidence of VAP 2. Rates of oral ulcer or herpes, or both 3. Oral cleanliness ‐ no odour, no foreign bodies and visually clean surfaces of tube and equipment 4. Throat swab culture |
|
| Notes | Diagnosis of VAP was according to Chinese Society of Respiratory Diseases criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were divided into three groups according to randomisation principle". |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described and not possible for the caregivers who would be aware of who was in each group |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not specified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in the outcome evaluation |
| Selective reporting (reporting bias) | Low risk | The results were fully reported. |
| Other bias | Low risk | No other sources of bias identified |
Fields 2008.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Location: Akron Ohio, USA Number of centres: 1 Study period: October 2005 to March 2006 Funding source: internal hospital funding |
|
| Participants | Setting: 24‐bed stroke, neurological and medical ICU Inclusion criteria: any mechanically‐ventilated patient on the stroke/medical ICU intubated in the hospital for < 24 hours, no previous diagnosis of pneumonia Exclusion criteria: patients with prior tracheotomies, younger than 18 years, AIDS secondary to immunocompromised systems, edentulous patients Number randomised: not stated Number evaluated: not stated Baseline characteristics: not reported |
|
| Interventions |
Comparison: Toothbrushing 8‐hourly versus usual care Experimental group: Nurse brushed patient's teeth, tongue and hard palate for > 1 minute, then used toothette swab to swab patient's teeth, tongue and hard palate for > 1 minute, then apply moisturiser to lips. Mouth and pharynx were suctioned as needed using catheter which was replaced every 24 hours. Oral assessment every 12 hours. Oral care kit #2 provided for each participant, with worksheet #2 Control group: Usual care (unspecified) which could include up to 2 toothbrushings daily and toothette mouthcare as needed. Nurses used oral care kit #1 and worksheet #1 |
|
| Outcomes | 1. Incidence of VAP | |
| Notes | Sample size calculation: "Desired sample size was 200 ventilator dependent patients or 2000 ventilator days". Email sent to authors 3 September 2012 requesting numbers of patients treated. No reply received. Trial included in text as narrative only |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "..a plastic bin labelled 1‐350, containing sealed envelopes which each had either worksheet #1 or #2, plus information about the trial to give to families". No mention of whether envelopes were sequentially numbered. Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Allocation contained in sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible; both nurses and participants would have known allocated treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome of VAP assessed by infection control nurse. Unclear whether this person was blinded to allocated treatment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The study neither reported the number of participants randomised nor the number analysed. |
| Selective reporting (reporting bias) | High risk | No numerical data were reported in this paper. VAP incidence was not reported by treatment group or with any measure of variance. |
| Other bias | Unclear risk | Insufficient information in the trial report to produce confidence in the methodology of this trial |
Fu 2019.
| Study characteristics | ||
| Methods | Study design: 3‐arm parallel‐group RCT Location: China Number of centres: 1 Study period: May 2015 to May 2017 Funding source: not reported |
|
| Participants | Setting: tertiary hospital Inclusion criteria: age between 18 and 75, male or female, complete medical record, mechanical ventilation of > 48 h Exclusion criteria: severe burns of the respiratory tract, patients who need oral surgery, extubation within 48 h, already had pneumonia, patients who may die within 48 h, severe coagulation disorders, incomplete medical record Number randomised: 120 (gp A: 40; gp B: 40; gp C: 40) Number evaluated: 120 (gp A: 40; gp B: 40; gp C: 40) Baseline characteristics: ‐Gp A: age: 49.96 (9.02); M/F: 21/19; APACHE II Score: 22.96 (2.88) ‐Gp B: age: 50.30 (8.67); M/F: 20/20 ; APACHE II Score: 22.67 (3.05) ‐Gp C: age: 50.12 (8.49); M/F: 22/18; APACHE II Score: 23.15 (2.49) |
|
| Interventions |
Comparison: 0.2% CHX solutionversus 0.12% CHX solution versus usual care Gp A (0.2% CHX solution): cleaning of tongue, teeth and gum with swab soaked in 0.2% CHX, twice a day, for 30 days consecutively Gp B (0.12% CHX solution): cleaning of tongue, teeth and gum with swab soaked in 0.12% CHX, twice a day, for 30 days consecutively Gp C (usual care): cleaning of tongue, teeth and gum with swab soaked in normal saline, twice a day, for 7 days consecutively All groups also received cleaning of mucus and secretions. |
|
| Outcomes | 1. Incidence of VAP 2. Duration of mechanical ventilation 3. Duration of ICU stay 4. Duration of hospital stay 5. Mortality 6. Plaque index 7. Microbial colonisation |
|
| Notes | Sample size calculation: not reported Other information of note: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “120 patients receiving mechanical ventilation were randomly allocated to 3 groups using the random number table method”. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described and not possible. Difference between intervention and control means caregivers would be aware of who was in each group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Unclear risk | 1. Criteria for VAP diagnosis were not reported. 2.The time point for plaque index measurement was not reported. |
Grap 2011.
| Study characteristics | ||
| Methods | Study design: RCT Location: Virginia, USA Number of centres: 2 units in same hospital, level 1 trauma centre Study period: not stated Funding source: Triservice Nursing research programme grant TSNRP MDA‐905‐03‐TS02 |
|
| Participants | Setting: surgical trauma ICU & neuroscience ICU Inclusion criteria: patients intubated within 12 hours of admission to trauma centre (intubation may have occurred in emergency department, in the field or in pre‐hospital setting) Exclusion criteria: previous endotracheal tube placed in 48 hours prior to admission, clinical diagnosis of pneumonia on admission, burn injuries, edentulous persons Number randomised: 152, 7 lost, enrolled sample 145 (71/74) (only 75 were still intubated after 48 hours) Number evaluated: at 48 or 72 hours = 60 (36/24) (for VAP) 39 (21/18) Baseline characteristics: not reported for each randomised group Those with 48/72 hour data: ‐ Experimental group: n = 36, M/F 27/9, APACHE II 70.69 ± 30.14 ‐ Control group: n = 24, M/F 11/13, APACHE II 60.46 ± 23.45 |
|
| Interventions |
Comparison: chlorhexidine applied by swab versus usual care Experimental group: 1 x 5 mL dose of chlorhexidine 0.12% applied to all areas of the oral cavity by swab within 12 hours after intubation. All participants received the usual oral comfort care (details not reported). Control group: usual oral comfort care |
|
| Outcomes | 1. Incidence of VAP 2. CPIS score 3. APACHE III 4. TRISS 5. Oral health (DMFT) |
|
| Notes | Sample size calculation: not reported (but pilot study published in 2004) Email sent and reply received to clarify the data |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The subjects were randomised to a treatment group or control group using a block randomisation scheme". |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible because no placebo used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Huge attrition, and reasons for losses not described for each group. Conclusions based on 39/152 (26%) of those originally randomised to treatment or control |
| Selective reporting (reporting bias) | High risk | Primary outcome planned was development of VAP but inclusion criteria used in this study meant that fewer than half those randomised were at risk of developing VAP. |
| Other bias | High risk | Study report noted statistically significant difference in gender and CPIS score between groups at baseline. No baseline characteristics data reported for each randomised group, and likely that important prognostic factors e.g. place of intubation, surgery, may have been different in each group |
Hanifi 2017.
| Study characteristics | ||
| Methods | Study design: 2‐arm parallel‐group RCT Location: Iran Number of centres: 1 Study period: Oct 2013 to March 2014 Funding source: Zanjan University of Medical Sciences |
|
| Participants | Setting: ICU Inclusion criteria: The patient should undergo mechanical ventilation for at least 12 hours, being in the age range of 18 to 70 years, no history of pneumonia and aspiration during the hospitalisation, or chemotherapy, and no maxillofacial fractures, scalds, pregnancy, anaemia, alcohol intoxication, or a recent myocardial infarction Exclusion criteria: Separation from the mechanical ventilation before the end of the study period, vomiting during the use of gastrointestinal tract, death, or being dissuaded from continuing in any part of the study either by the patients’ guardians or the doctors… If the patient was diagnosed with pneumonia based on the clinical pulmonary infection score (CPIS) during the first 12 hours, they were not included in the study. Number randomised: 80 (gp A: 40; gp B: 40) Number evaluated: 74 (gp A: 39; gp B: 35) Baseline characteristics: ‐Gp A: Age: 14.42 ± 1.39*; M/F: 25/14; APACHE II score: not reported ‐Gp B: Age: 44.61 ± 1.78*; M/F: 25/10; APACHE II score: not reported |
|
| Interventions |
Comparison: 0.05 ppm ozonated water versus 0.2% CHX Gp A (ozonated water): Both of these mouthwashes were applied identically 3 times a day. Before the intervention, patients’ mouth and trachea received standard suctioning. The swab impregnated with either of the mouthwashes was rubbed rotationally on the upper gums from the right to the left side of the mouth. It was, then, changed and rubbed rotationally on the lower gums from left to right. Two other swabs impregnated with the mouthwash were used to cleanse the upper and lower teeth. After using the swabs and having prepared by the suction, the cuff pressure of the ET tube was increased to 35 mmHg via a manometer specifically used to measure the ET tube cuff pressure. Then, approximately 15 mL of the mouthwash was inserted into the patient’s mouth and 30 seconds later the suctioning process was conducted. Immediately after the intervention, the cuff pressure was reduced to 15 to 20 mmHg. This intervention occurred over a 4‐day period. Gp B (CHX): same as gp A, different mouthwash |
|
| Outcomes | 1. VAP incidence | |
| Notes | Sample size calculation: to determine the sample size, a pilot study was conducted. By considering α = 0.01, ß = 0.1, P1 = 0.13 and P2 = 0.5, the sample size of each group was estimated as 40. Other information of note: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “a range of numbers was randomly selected by the table of random numbers”. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Double‐blind means subjects and outcome assessor; blinding of the caregivers not described and not possible. Difference between intervention and control means caregivers would be aware of who was in each group. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “VAP infection check‐up was carried out by the anaesthesiologist, the only observer blind to the intervention method”. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Although the attrition rate (7.5%) was relatively low, the number of dropouts was unbalanced between groups, and the reason for each dropout was not clearly reported. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Hu 2009.
| Study characteristics | ||
| Methods | Study design: RCT Location: Beijing, China Number of centres: 1 Study period: Not stated Funding source: No external funding |
|
| Participants | Setting: ICU in second affiliated hospital of PLA General Hospital Inclusion criteria: Patients in ICU receiving mechanical ventilation Exclusion criteria: Unclear Number randomised: 47 Number evaluated: Unclear Baseline characteristics: Not reported for each randomised group in total Those with 48/72 hour data: ‐ Experimental group: n = 25, M/F 16/9, age range 19 ‐ 68 ‐ Control group: n = 22, M/F 13/9, age range 22 ‐ 60 |
|
| Interventions |
Comparison: Saline swab + rinse versus saline swab Experimental group: Lips, teeth, tongue and palate were swabbed with a saline saturated cotton ball and the oral cavity was rinsed with saline twice daily. Control group: Lips, teeth, tongue and palate were swabbed with saline saturated cotton ball twice daily. |
|
| Outcomes | VAP, mortality, days on ventilator, days in hospital, halitosis, ulceration | |
| Notes | Information translated from Chinese paper by Shi Zongdao and colleagues. Unable to confirm outcome data with trial authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Email from author "the sequence was generated by using a random number table". |
| Allocation concealment (selection bias) | Low risk | Email from author "allocation was concealed using opaque envelopes numbered with inclusion sequence". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and caregivers were not blinded to interventions received. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Email from author "the outcome assessors were a group of nurses not involved with the interventions". Probably blinded to allocated treatment group. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The number of participants included in the outcome assessments at each time point was unclear. VAP reported as percentages only |
| Selective reporting (reporting bias) | High risk | All planned outcomes reported but as percentages only |
| Other bias | Low risk | No other sources of bias identified |
Irani 2019.
| Study characteristics | ||
| Methods | Study design: 2‐arm parallel‐group RCT Location: Iran Number of centres: One Study period: 2018 Funding source: No funding was received for this study. |
|
| Participants | Setting: ICU Inclusion criteria: Anaesthetised patients aged 18‐65 years, insertion of endotracheal tube on admission to ICU and its maintenance during the study, lack of "immunoi", hepatitis, or HIV infection, scoring below 11 based on Beck oral assessment scale, no history of herbal allergy, no hospitalisation prior to admission to ICU, no history/symptom of gastric content aspiration, no coagulation disorders, no removable denture, at least 24 hours past the admission to ICU, no pregnancy, no chronic pulmonary disease (including chronic obstructive pulmonary disease, lung cancer, and chest trauma), scoring below 5 based on the modified clinical pulmonary infection score at the onset of the study Exclusion criteria: Patient’s death, patient’s transfer to other departments before the end of the study, any visible oral injury and bleeding caused by endotracheal intubation or oropharyngeal airway insertion after the start of the study, removal of endotracheal tube for any reason, endotracheal re‐intubation or tracheostomy at the time of the study, diagnosis of aspiration symptoms after the start of the study as documented in the patient’s admission records, restriction in oral care practices and thus risk of aspiration, developing pneumonia 48 hours after starting the study as diagnosed by the physician, withdrawal of mechanical ventilation before 96 hours, and requiring cardiopulmonary resuscitation Number randomised: 70 (group A: 35; group B: 35) Number evaluated: 70 (group A: 35; group B: 35) Baseline characteristics: ‐ Group A (Miswak): Age: 33.65 (13.51); M/F: 29/6; Glasgow Coma Scale (GCS): 5.8 (1.24) ‐ Group B (Chlorhexidine): Age: 34.83 (13.95); M/F: 26/9; GCS: 5.7 (1.36) |
|
| Interventions |
Comparison: Miswak versus Chlorhexidine Miswak: For five consecutive days, oral care was provided twice a day (every 12 hours) using miswak in the intervention group and 0.2% chlorhexidine mouthwash in the control group…After that, miswak was wetted using cool water, which had been boiled for 15 minutes; it was used to gently brush back and forth all interior, exterior, and masticatory surfaces of the teeth. Chlorhexidine: Oral care procedure was similar to the intervention group except that, instead of miswak, a cotton swab dipped in 0.2% chlorhexidine was administered. |
|
| Outcomes | 1. Incidence of VAP | |
| Notes | Sample size calculation: Using the following formula and the incidence rate of VAP reported by Yao 2011, the sample size was estimated at 16 for each group within the confidence interval of 95% and statistical power of 95%. In order to ensure sample size adequacy and to take account of possible attrition, 35 patients were allocated to each group (total = 70). Other information of note: None |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “…randomly divided into the intervention and control groups through coin flipping (heads = intervention group, tails = control group)” |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This was single‐blinded; only the outcome assessor was blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “To meet the blinding criterion, patients and the physician responsible for pneumonia diagnosis were not aware of the distribution of the two study groups.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: The study flow diagram was not provided. Insufficient information to permit judgement |
| Selective reporting (reporting bias) | High risk | Data for the dosage of antibiotic in each group at the time of admission was planned but not reported. |
| Other bias | Low risk | No other sources of bias identified |
Khaky 2018.
| Study characteristics | ||
| Methods | Study design: Two‐arm parallel‐group RCT Location: Iran Number of centres: one Study period: November 2016 to May 2017 Funding source: Not mentioned |
|
| Participants | Setting: ICU Inclusion criteria: age between 18 to 70 years old, lack of clear trauma to the jaw and face that prevents oral care, having tracheal tube, locating the patient under mechanical ventilation, lack of pneumonia or respiratory infections at the beginning of entry to the hospital (MCPIS < 7) up to 48 hours after intubation and there was no ban in respect of using Nanosil or Chlorhexidine such as allergy. Exclusion criteria: none Number randomised: 80 (gp A: 40; gp B: 40) Number evaluated: 75 (gp A: 37; gp B: 38) Baseline characteristics: ‐Gp A: (Age: 41.6 ± 15.9; M/F: 29/11; APACHE II score: not reported) ‐Gp B: (Age: 44.1 ± 16.5; M/F: 27/13; APACHE II score: not reported) |
|
| Interventions |
Comparison: Nanosil versus 2% Chlorhexidine Gp A (Nanosil): Patients in the case group received oral care with same method except that Nanosil was used instead of chlorhexidine. The intervention continued for five days or until obtaining the exit criteria. Gp B (Chlorhexidine): Patients in the control group received standard treatment. For these patients, oral care was done by 15 mL of a 2% chlorhexidine solution, 3 times per day for five days that involved brushing the teeth, suctioning oral secretions, and rubbing the oropharyngeal mucosa. |
|
| Outcomes | 1. VAP incidence (five days after initiation of intubation) 2. Mortality (five days after initiation of intubation) 3. MCPIS 4. SOFA 5. GCS |
|
| Notes | Sample size calculation: Not reported Other information of note: None |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described and not possible. Difference between intervention and control meant caregivers would have been aware of who was in each group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | “During the study, 3 patients in the case group and 2 patients in the control group were excluded.” Reasons for exclusion were not provided. |
| Selective reporting (reporting bias) | High risk | Mortality‐related data were not reported. |
| Other bias | Low risk | No other sources of bias identified |
Koeman 2006.
| Study characteristics | ||
| Methods | Study design: multicentre randomised double‐blind placebo‐controlled trial with 3 parallel groups Location: 2 university hospitals and 3 general hospitals in the Netherlands Number of centres: 5 hospitals (2 surgical and 5 mixed ICUs) Study period: February 2001 to March 2003 Funding source: ZONMw Netherlands Organization for Health Research and Development (project number 2200.0046) |
|
| Participants | Inclusion criteria: consecutive adult patients (> 18 years of age) needing mechanical ventilation for at least 48 hours were included within 24 hours after intubation and start of mechanical ventilation. Exclusion criteria: immunocompromised status pre‐admission, pregnancy, physical condition not allowing oral application of study medication Age group: not stated Number randomised: 385 Number evaluated: 379 Group A: Chlorhexidine group: n = 127; mean age: 60.9 ± 15.3; M/F: 71/57; APACHE II: 22.2 ± 7.02 Group B: Chlorhexidine/COL group: n = 128; mean age: 62.4 ± 19.1; M/F: 66/61; APACHE II: 23.7 ± 7.38 Group C: Control group: n = 130; mean age: 62.1 ± 15.9; M/F: 93/37; APACHE II: 21.8 ± 7.43 |
|
| Interventions |
Comparison: Chlorhexidine (in petroleum jelly) versus petroleum jelly alone Group A: Chlorhexidine group (n = 127): oral decontamination with chlorhexidine (2%) in vaseline petroleum jelly Group B: Chlorhexidine/COL group (n = 128): oral decontamination with chlorhexidine plus colistin antibiotic chlorhexidine/colistin (CHX/COL 2%/2%) in vaseline petroleum jelly Group C: Control (n = 130): oral decontamination with vaseline petroleum jelly Trial medication was administered 4 times daily, after removing remnants of the previous dose with a gauze moistened with saline. Approximately 2 cm of paste, approximately 0.5 g, was put on a gloved fingertip and administered to each side of the buccal cavity. |
|
| Outcomes | The following outcome variables were reported for each group. 1. Incidence of VAP 2. Incidence of early onset VAP 3. Days ventilated (mean ± SD) 4. ICU stay (mean ± SD) 5. Days in hospital after ICU discharge (mean ± SD) 6. Changes of endotracheal colonisation through cultures in 3 time windows after ventilation, 1 to 3 days, 5 to 8 days and 9 to 12 days, respectively |
|
| Notes | Sample size calculation: reported in paper together with planned sequential analysis Only group A and group C included in this review Email sent to author 26 August 2016 requesting mortality data but failed due to invalid email address |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...randomly assigned to one of three study groups by computerised randomisation schedule. Randomization was stratified by hospital". |
| Allocation concealment (selection bias) | Low risk | The interventions were produced by an independent unit and we considered allocation was concealed from the research team. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind, placebo‐controlled |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The study was discontinued in 6 participants: 5 participants withdrew consent, 1 due to adverse event. Intention‐to‐treat analysis included all participants for primary outcome. |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported |
| Other bias | Low risk | Unlikely |
Kusahara 2012a.
| Study characteristics | ||
| Methods | Study design: double‐blind placebo‐controlled RCT Location: Sao Paulo, Brazil Number of centres: 1, tertiary care hospital affiliated with Federal University of Sao Paulo, Brazil Study period: 36 months, dates not stated Funding source: grant from Fundacao de Amparo a Pesquisa do Estado de Sao Paulo (04‐13361‐2) |
|
| Participants | Setting: PICU Inclusion criteria: Children admitted to PICU likely to require ventilation within 24 hours of admission Exclusion criteria: Newborn, confirmed diagnosis of pneumonia at admission, known hypersensitivity to chlorhexidine, tracheostomy, duration of ventilation < 48 hours, intubated for > 24 hours prior to PICU admission Number randomised: 96 (46/50) Number evaluated: 96, at day 2: 44/45, at day 4: 23/23 Baseline characteristics: ‐ Intervention group: Age: 12 ± 49.75 months; M/F: 28/18 ‐ Control group: Age: 34.5 ± 58.8 months; M/F: 32/18 |
|
| Interventions |
Toothbrushing + 0.12% chlorhexidine gel versus toothbrushing + placebo Experimental group: Oral care with toothbrushing and oral gel containing chlorhexidine twice daily (08:00 & 20:00 hours). Mouth was divided into 4 quadrants and each brushed in a defined pattern. With child in lateral position, gel was applied directly to toothbrush, and all tooth surfaces (vestibular, lingual, occlusal and incisal) were cleaned and ventral surface of tongue was brushed posterior to anterior. Each quadrant was rinsed with water and excess fluid and debris were removed with continuous suction. Finally, oral foam applicator was immersed in the gel and applied all over the gingival surfaces of the participant. Control group: Oral care with toothbrushing and placebo oral gel twice daily. With child in lateral position, gel was applied directly to toothbrush, and all tooth surfaces (vestibular, lingual, occlusal and incisal) were cleaned and ventral surface of tongue was brushed posterior to anterior. Each quadrant was rinsed with water and excess fluid and debris were removed with continual suction. Finally, oral foam applicator was immersed in the gel and applied all over the gingival surfaces of the participant. |
|
| Outcomes | 1. Incidence of VAP 2. Duration of ventilation in PICU 3. Length of stay in PICU 4. Hospital mortality 5. Tracheal colonisation with Gram +ve & ‐ve organisms |
|
| Notes | Sample size calculation: reported that this was not done "due to the absence of previous research on this population" Email correspondence with Prof Pedreira confirmed that Pedreira 2009 and Kusahara 2012a both refer to the same study (NCT 01083407 & NCT0410682 at ClinicalTrials.gov) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "..randomised into two groups using a balanced randomisation table generated by True Epistat Program" |
| Allocation concealment (selection bias) | Low risk | Both chlorhexidine and identical placebo gels were supplied by pharmacy in identical containers and only the pharmacist was aware of the gel type for each participant. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind. Identical placebo used so that neither participants nor clinical staff were aware of allocated treatment |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind. Only the pharmacist was aware of the gel type for each participant. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in the outcome evaluation |
| Selective reporting (reporting bias) | Low risk | One primary and 4 secondary outcomes reported in full |
| Other bias | Unclear risk | Statistically significant difference in mean age of children in each group. This may have introduced a bias. |
Long 2012.
| Study characteristics | ||
| Methods | Study design: single‐centre RCT with 2 parallel groups Location: China Number of centres: 1 ICU in the university hospital Study period: February 2010 to March 2012 Funding source: programme for Masters degree |
|
| Participants | Inclusion criteria: patients admitted to ICU, with oral intubation, receiving mechanical ventilation ≥ 48 hours, age ≥ 18 years, patients or their relatives agreed to participate in the study Exclusion criteria: intubated in emergency e.g. after cardiac arrest, operations upon the oral cavity, trauma of the respiratory tract, with severe bleeding or coagulation disorders Number randomised: 70 Number evaluated: 61 (the other 9 were death or ventilation < 48 hours) ‐ Intervention group: mean age: 60.06 ± 10.71 years, M/F 20/11, APACHE 17.94 ± 1.24 ‐ Control group: mean age: 63.67 ± 10.02 years, M/F 18/12, APACHE 18.23 ± 0.57 |
|
| Interventions |
Comparison: povidone iodine + toothbrushing vs povidone iodine alone Experimental group (n = 31): modified oral nursing method: swab with 0.1% povidone iodine immediately before intubation, then toothbrushing and rinsing with 0.1% povidone iodine, 3 times a day Control group (n = 30): usual oral nursing method: swab with cotton balls soaked with 0.1% povidone iodine |
|
| Outcomes | 3 outcome variables were available: 1. Incidence of VAP 2. Mortality 3. Ventilation days |
|
| Notes | Microbial examinations for the aspirate secretions obtained from inferior respiratory tract every day after intubation were referred for diagnosis of VAP. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...patients were randomly assigned into 2 groups, observing group and control group with 35 cases in each group". |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described and not possible for the caregivers who would be aware of who was in each group |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not specified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9 randomised participants were excluded from analysis; numbers and reasons similar for each group |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Unclear risk | Results of microbial examination of the aspirate secretions from the inferior respiratory tract as tool of VAP diagnosis may not be enough. |
Lorente 2012.
| Study characteristics | ||
| Methods | Study design: Parallel‐group RCT Location: Tenerife, Spain Number of centres: 1 Study period: August 2010 to August 2011 Funding source: Hospital funding |
|
| Participants | Setting: medical/surgical ICU Inclusion criteria: consecutive patients undergoing invasive mechanical ventilation for at least 24 hours Exclusion criteria: edentulous, aged < 18 years, pregnant, HIV positive, white blood cells < 1000 cells/mm3, solid or haematological tumour, immunosuppressive therapy, mechanical ventilation duration < 24 hours Number randomised: 436 (217/219) Number evaluated: 436 Baseline characteristics: ‐ Intervention group: age: 61.0 ± 15.6 years; M/F: 146/71 ‐ Control group: age: 60.4 ± 16.6 years; M/F: 145/74 |
|
| Interventions |
Toothbrushing + 0.12% chlorhexidine gel vs chlorhexidine alone Experimental group (n = 217): oral cleansing performed with 0.12% chlorhexidine‐impregnated gauze, and oral cavity injection, followed by manual brushing of the teeth with a brush impregnated with 0.12% chlorhexidine (tooth by tooth on the anterior and posterior surfaces, the gum line and the tongue for a period of 90 seconds) Control group (n = 219): oral cleansing performed with 0.12% chlorhexidine‐impregnated gauze, and oral cavity injection only In both groups, nurse performed oral care every 8 hours. First endotracheal cuff pressure was tested, oropharyngeal secretions were aspirated, then chlorhexidine‐impregnated gauze was used to cleanse the teeth, tongue and mucosal surfaces, followed by injection of 10 mL 0.12% of chlorhexidine digluconate into oral cavity, and finally after 30 seconds the OParea was suctioned. |
|
| Outcomes | 1. Incidence of VAP 2. Duration of ventilation 3. ICU mortality 4. Tracheal colonisation with gram +ve & ‐ve organisms 5. Antibiotic exposure |
|
| Notes | Sample size calculation: estimated that 218 participants required in each group to give 80% power and α error of 5%, to show a reduction in VAP from 15% to 7.5% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...a list of random numbers generated with Excel software (Microsoft, Seattle, WA)" |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The diagnosis of VAP was made by an expert panel, blinded to group assignment". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants are included in the outcome evaluations. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported in full |
| Other bias | Low risk | No other sources of bias identified |
Meidani 2018.
| Study characteristics | ||
| Methods | Study design: 3‐arm parallel‐group RCT Location: Iran Number of centres: 1 Study period: 2011 to 2012 Funding source: fully sponsored by Research Council of Isfahan University of Medical Sciences, Isfahan, Iran |
|
| Participants | Setting: ICU Inclusion criteria: ICU‐admitted patients on ventilator for more than 48 hours, age over 18 years, no fever at the time of entering the ICU, no pneumonia, no allergy to the drugs used Exclusion criteria: in the case of patients who died or were released from hospital before the due date or patients with the appearance of drug complications were excluded from the study. They were also excluded if they had pneumonia before 48 h of hospitalisation or ventilation. Number randomised: 150 (gp A: 50; gp B: 50; gp C: 50) Number evaluated: 150 (gp A: 50; gp B: 50; gp C: 50) Baseline characteristics: ‐Gp A: (Age: 50.6 ± 19.1; M/F: 37/13; APACHE II score: not reported) ‐Gp B: (Age: 49.8 ± 22.7; M/F: 37/13; APACHE II score: not reported) ‐Gp C: (Age: 51.7 ± 18.9; M/F: 33/17; APACHE II score: not reported) |
|
| Interventions |
Comparison: 0.2% CHX versus 0.01% potassium permanganate versus control Gp A (CHX), B (potassium permanganate) and C (control): mouth and pharynx washing of selected patients was done by the trained nurses, three times a day, each time for 5 minutes, for 1 week by tongue depresson and sterile gas with 10cc solution |
|
| Outcomes | 1. Incidence of VAP 2. Mortality |
|
| Notes | Sample size calculation: not mentioned Other information of note: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of method of sequence generation provided in report |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described and not possible. Difference between intervention and control meant caregivers would be aware of who was in each group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "In case of patient’s death or release from hospital before due date or appearance of drug complications, they were excluded from the study. They were also excluded if they had pneumonia before 48 h of hospitalization or ventilation." |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information in the trial report to produce confidence in the methodology of this trial |
Meinberg 2012.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Location: Brazil Number of centres: 1 Study period: July 2007 to December 2009 Funding source: not stated |
|
| Participants | Setting: surgical ICU Inclusion criteria: > 18 years, receiving mechanical ventilation within 24 hours of admission, expected to require ventilation for > 72 hours Exclusion criteria: aspiration pneumonia, tracheostomy, pregnancy and immunosuppression Number randomised: 52 (28/24) Number evaluated: 52 (28/24) Baseline characteristics: ‐ Intervention group: age: 40.1 ± 14.6 years; APACHE II 17.9 ± 4.5 ‐ Control group: age: 41.0 ± 19.0 years; APACHE II 16.7 ± 6.8 |
|
| Interventions |
Comparison: toothbrushing + 2% chlorhexidine gel versus toothbrushing + placebo gel Experimental group (n = 28): toothbrushing plus chlorhexidine gel 2% 4 times daily Control group (n = 24): toothbrushing plus placebo gel 4 times daily |
|
| Outcomes | 1. VAP 2. Mortality 2. ICU mortality 3. Duration of intubation 4. Duration of ICU stay 5. Duration of hospital stay |
|
| Notes | Errors in numbers reported for duration of intubation in Table 2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This was undertaken by the pharmacist. |
| Allocation concealment (selection bias) | Low risk | "only the pharmacist responsible for preparing the solutions and for the randomisation process knew the contents of the distributed gel tubes". |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "only the pharmacist responsible for preparing the solutions and for the randomisation process knew the contents of the distributed gel tubes", "placebo group (gel with same colour and consistency)" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "only the pharmacist responsible for preparing the solutions and for the randomisation process knew the contents of the distributed gel tubes". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | Adverse events not reported. Data not fully reported. Data errors |
| Other bias | High risk | Study terminated due to 'futility'. Reason for termination unclear |
Mo 2016.
| Study characteristics | ||
| Methods | Study design: 2‐arm parallel‐group RCT Location: China Number of centres: 1 Study period: December 2012 to May 2015 Funding source: not reported |
|
| Participants | Setting: Department of Cardio‐Thoracic Surgery Inclusion criteria: mechanical ventilation > 48 hours Exclusion criteria: patients with pulmonary infections or oral diseases Number randomised: 210 (gp A: 105; gp B: 105) Number evaluated: 210 (gp A: 105; gp B: 105) Baseline characteristics: ‐ Gp A: Age: 59.14 (12.06); M/F: 60/45 ‐ Gp B: Age: 56.71 (10.53); M/F: 68/37 |
|
| Interventions |
Comparison: saline rinse vs saline swab (usual care) Gp A: rinse with saline for 10 minutes each time, 4 times per day Gp B: swab with saline 4 times per day |
|
| Outcomes | 1. Incidence of VAP 2. Mortality |
|
| Notes | Sample size calculation: Not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “randomised patients to the experimental and control group using a random number table” |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not described and not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessor blinding not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in analysis |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Nobahar 2016.
| Study characteristics | ||
| Methods | Study design: 2‐arm parallel‐group RCT Location: Iran Number of centres: 1 Study period: May 23 2013 to December 23 2012 Funding source: Research and Technology Deputy of Semnan University of Medical Sciences (Grant no. 514) |
|
| Participants | Setting: ICU Inclusion criteria: being over the age of 18, having been under mechanical ventilation for over 48 hours, having had no more than one intubation attempt, no facial or oral trauma, no contraindications to neither mouthwash use nor to 30◦ bedhead elevation, no history of HP allergies, and no evidence suggesting VAP or aspiration Exclusion criteria: having had pneumonia prior to the beginning of the study and in the first 48 hours of mechanical ventilation, transfer from other departments and the elapse of 24 hours since the insertion of the tracheal tube, the removal of the tracheal tube for any reason during the 5 days the study was being conducted, and the patient’s death or transfer from the internal unit to the surgery ICU and vice versa at any time during the 5 days of the study Number randomised: 68 (HP group: 34; control group: 34) Number evaluated: 68 (HP group: 34; control group: 34) Baseline characteristics: ‐ HP group: (age: 66 ± 15.5; M/F: 17/17; APACHE II score: not reported) ‐ Control group: (age: 63.4 ± 20.5; M/F: 18/16; APACHE II score: not reported) |
|
| Interventions |
Comparison: 3% hydrogen peroxide (HP) versus 0.9% normal saline (NS) HP: after wearing sterile gloves, the patient’s oral mucosal membrane, tongue and gingiva were washed using 4–6 cotton swabs (depending on the patient’s oral health) soaked in 15 cc of 3% HP. Any excess discharges were collected through suction pumps under similarly equal conditions. The application of these mouthwash formulas continued for five days. Control: after wearing sterile gloves, the patient’s oral mucosal membrane, tongue and gingiva were washed using 4–6 cotton swabs (depending on the patient’s oral health) soaked in 15 cc of 0.9% NS. Any excess discharges were collected through suction pumps under similarly equal conditions. The application of these mouthwash formulas continued for five days. Conditions of using the mouthwash were similar in both groups, and after washing their hands, the bedhead was elevated 30◦ in order to prevent aspiration of secretions. Before the application of mouthwash and after elevating the bedhead, the tracheal tube and mouth secretions were suctioned out using a green nelaton catheter size 14. The suction nozzle was replaced after each application of the mouthwash. This procedure was repeated twice every day at 8 a.m. and 4 p.m. |
|
| Outcomes | Incidence of VAP | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Patients were randomly divided into two groups by the use of a coin toss, where heads were assigned to the intervention and tails to the control group”. |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Impossible to blind health providers due to the obvious difference between hydrogen peroxide and normal saline |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | Planned baseline information (e.g. occupation, the department referring the patient to the ICU, duration of hospital stay) and results regarding adverse effects were not reported. |
| Other bias | Low risk | No other sources of bias identified |
Ozcaka 2012.
| Study characteristics | ||
| Methods | Study design: double‐blind placebo‐controlled RCT Location: Izmir, Turkey Number of centres: 1 Study period: November 2007 to November 2009 Funding source: "The study was funded solely by the institutions of the authors". |
|
| Participants | Setting: respiratory ICU Inclusion criteria: patients aged 18 or over, admitted to respiratory ICU expecting to require ventilation for > 48 hours Exclusion criteria: witnessed episode of aspiration, confirmed diagnosis of post‐obstructive pneumonia, known hypersensitivity to chlorhexidine, diagnosed thrombocytopenia, pregnancy, oral mucositis, readmission to same ICU, expected survival < 1 week, edentulism Number randomised: 66 Number evaluated: 61 Baseline characteristics: ‐ Intervention group: age: 60.5 ± 14.7 years ‐ Control group: age: 56.0 ± 18.2 years |
|
| Interventions |
Comparison: chlorhexidine solution vs saline Experimental group (n = 32): oral mucosa was swabbed with 0.2% chlorhexidine on sponge pellets, 4 times daily. Excess rinse was suctioned from patient's mouth after 1 minute. Control group (n = 34): oral mucosa was swabbed with saline on sponge pellets, 4 times daily. Excess rinse was suctioned from patient's mouth after 1 minute. Deep suctioning was performed in both groups every 6 hours and following position changes to remove pooled secretions from around the cuff of the endotracheal tube. |
|
| Outcomes | 1. Incidence of VAP 2. Mortality 3. Duration of ventilation in ICU 4. Length of stay in ICU 5. Presence of potential respiratory pathogens in minibronchoalveolar lavage |
|
| Notes | Sample size calculation: estimated that 28 participants would be required in each group to give 81% power with α of 5%, to show a reduction in VAP from 70% to 30% Email sent 22 January 2013 and reply received 29 January 2013 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The randomisation prepared a set of subject identification (SID) numbers which had assigned treatment". Description unclear |
| Allocation concealment (selection bias) | Unclear risk | "Study nurse obtained the SID number when the patient was enrolled". |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Assignment of treatment was blinded to patients and to all investigators, including periodontist,...respiratory ICU physicians and outcome statisticians". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Assignment of treatment was blinded to patients and to all investigators, including periodontist,...respiratory ICU physicians and outcome statisticians". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 66 participants randomised, 1 secondary exclusion from each group, and 2 and 1 early deaths in chlorhexidine and control groups, respectively. Unlikely to have introduced a bias |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Panchabhai 2009.
| Study characteristics | ||
| Methods | Study design: open‐label RCT Location: Mumbai, India Number of centres: 1 Study period: 8 months ‐ dates not stated Funding source: not stated |
|
| Participants | Setting: ICU (mixed medical and surgical), tertiary care hospital Inclusion criteria: all patients admitted to ICU during study period who signed consent Exclusion criteria: pregnant women, those with pneumonia at baseline, those for whom oral care was contraindicated, those with allergy to chlorhexidine Number randomised: 512 Number evaluated: 471 (only 88/83 = 171 on mechanical ventilation) Baseline characteristics (given for 471 who completed the trial only): ‐ Intervention group: age: 35.2 ± 15.9; M/F: 136/88; APACHE II score: 12 ± (9 ‐ 17) ‐ Control group: age: 36.9 ± 16.2; M/F: 171/76; APACHE II score: 14 ± (9 ‐ 19) |
|
| Interventions |
Comparison: chlorhexidine vs potassium permanganate Experimental group (n = 250): oral and pharyngeal suction of pooled secretions followed by swabbing of the oral cavity, teeth, palate, buccal spaces, posterior pharyngeal wall, and hypopharynx with normal saline. Then oropharyngeal cleansing, following the same procedure, twice daily with 0.2% chlorhexidine solution Control group (n = 262): oral and pharyngeal suction of pooled secretions followed by swabbing of the oral cavity, teeth, palate, buccal spaces, posterior pharyngeal wall, and hypopharynx with normal saline. Then oropharyngeal cleansing twice daily, following the same procedure, with 0.01% potassium permanganate solution Non‐intubated participants, rinsed with water, then rinsed and gargled with 10 mL of study solution. No eating/drinking for 1 hour post‐intervention |
|
| Outcomes | 1. Incidence of nosocomial pneumonia 2. Day of development of pneumonia 3. Mortality (hospital) 4. Duration of ICU stay |
|
| Notes | Sample size calculation: "This study had a statistical power of 75% to detect a 50% reduction in the incidence of nosocomial pneumonia in the study group with 95% level of confidence. Assuming the incidence of pneumonia in the control group was 16%, 506 subjects were required". Email sent to author 14 November 2012 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "..randomly assigned to treatment .... by concealed simple random sampling" No details of sequence generation provided |
| Allocation concealment (selection bias) | Unclear risk | "..concealed simple randomisation" Unclear whether allocation was concealed from researchers |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Open‐label RCT |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Open‐label RCT but "two independent, blinded reviewers made the diagnosis of nosocomial pneumonia". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 26/250 (10%) and 15/262 (5.7%) were excluded from the analysis in the chlorhexidine and control groups, respectively. Reasons given were ICU stay < 48 hours, 14/250 versus 6/262, and protocol violation 12/250 and 9/262, respectively. |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported in full |
| Other bias | Unclear risk | Baseline parameters only reported for those who completed the study |
Pobo 2009.
| Study characteristics | ||
| Methods | Study design: prospective, single‐blind, randomised trial with parallel groups Location: Spain Number of centres: 1 ICU at a hospital Study period: not stated Funding source: supported by Fondo de Investigaciones Sanitarias (FISS 06/060), Centro de Investigación Biomédica en Red Enfermedades Respiratorias (06/06/36), and the Agency for the Administration of University and Research Grants (2005/SGR/920) |
|
| Participants | Inclusion criteria: intubated adults without evidence of pulmonary infection, expected to remain ventilated for > 48 hours. Randomised within 12 hours of intubation Exclusion criteria: edentulous, suspicion of pneumonia at time of intubation or evidence of massive aspiration during intubation, tracheostomy (or expected within 48 hours), recent enrolment in other trials, pregnancy, and chlorhexidine allergy Age group: adults Intervention group: n = 74; age: 55.3 ± 17.9; M/F: 49/25; mean APACHE II score: 18.8 ± 7.1 Control group: n = 73; age: 52.6 ± 17.2; M/F: 46/27; mean APACHE II score: 18.7 ± 7.3 Number randomised: 147 (74 in toothbrush group and 73 in standard care group) Number evaluated: 147 |
|
| Interventions |
Comparison: powered toothbrush + standard oral care vs standard oral care alone Group 1 (n = 74): standard oral care plus toothbrush group: besides the standard oral care, toothbrushing was performed tooth by tooth, on anterior and posterior surfaces, and along the gumline, the tongue was also brushed. A powered toothbrush was used (Braun Oral B AdvancePower 450 TX, Braun GmbH). This procedure was repeated once every 8 hours Group 2 (n = 73): standard oral care: maintaining head elevation at 30°. After aspiration of oropharyngeal secretions and adjustment of endotracheal cuff pressure, a gauze containing 20 mL of 0.12% chlorhexidine digluconate was applied to all the oral surfaces including tongue and mucosal surface, and 10 mL of 0.12% chlorhexidine digluconate was injected into oral cavity, being aspirated after 30 seconds, repeated every 8 hours |
|
| Outcomes | The following outcome variables were reported for each group: 1. Incidence of VAP 2. Incidence of suspected VAP per 1000 days of mechanical ventilation 3. Mean days of mechanical ventilation (mean ± SD) 4. ICU length of stay (mean ± SD) 5. Mortality |
|
| Notes | In the review, the standard oral care group was viewed as the intervention with chlorhexidine and the other group was viewed as the control with toothbrushing Sample size calculation: estimated that 200 participants would be required in each group to show a 50% reduction in VAP with 80% power and α error of 5%. After 147 of planned 400 participants were randomised, the study was stopped by the steering committee due to no difference in VAP between the groups. NCT 00842478 at ClinicalTrials.gov |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by means of a computer‐generated list, stratified for antibiotic use at admission |
| Allocation concealment (selection bias) | Low risk | The list was concealed in opaque sealed envelopes opened by the nurse within 12 hours of intubation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible. Participants unlikely to be aware of treatment, but caregivers were aware |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Investigators and attending physicians were blinded to assigned groups. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals. All randomised participants included in the analysis |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported, including adverse events |
| Other bias | High risk | Study stopped early after recruitment of 147 of planned 400 participants because no differences between groups were found and revised estimates indicated that 1500 participants would need to be recruited to show a difference. Numbers not feasible in this centre |
Prendergast 2012.
| Study characteristics | ||
| Methods | Study design: prospective, randomised trial with 2 parallel groups. NCT 00518752 Location: USA Number of centres: 1 neuroscience ICU at a tertiary medical centre Study period: August 2007 to August 2009 Funding source: not stated |
|
| Participants | Inclusion criteria: all patients aged at least 18 years admitted to neuroscience ICU, intubated within 24 hours of admission Exclusion criteria: pregnancy, edentulous, aged < 18 years, facial fractures or trauma affecting oral cavity, unstable cervical fractures, anticipated extubation within 24 hours, grim prognosis Intervention group: n = 38; age: 54 ± 17.8; M/F: 19/19 Control group: n = 40; age: 51 ± 18.4; M/F: 23/17 Number randomised: 78 (38 in comprehensive group and 40 in standard care group) Number evaluated: variable (fewer than 11 participants/group) |
|
| Interventions |
Comparison: powered toothbrush + comprehensive oral care vs manual toothbrush + standard oral care Group 1 (n = 38): tongue scraping using a low‐profile tongue scraper with posterior to anterior sweeping motion across the dorsal surface of the tongue, then toothbrushing with Oral B vitality powered toothbrush + Biotene (non‐foaming) toothpaste for 2 minutes. Then a liberal application of Oral Balance gel. Care performed twice daily Group 2 (n = 40): standard oral care: using manual paediatric toothbrush, toothpaste with 1000 ppm fluoride with SLS and water‐based inert lubricant ("KY jelly"). Care performed twice daily |
|
| Outcomes | The following outcome variables were reported for each group: 1. Oral and sputum cultures every 48 hours 2. Incidence of suspected VAP (day 2‐6) 3. ICU length of stay (mean ± SD) 4. Mortality |
|
| Notes | Sample size calculation: not reported NCT 00518752 at ClinicalTrials.gov |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "..randomized ... using a computer generated list maintained in a separate locked cabinet" |
| Allocation concealment (selection bias) | Low risk | "..list was maintained in a separate locked cabinet from enrolment forms to prevent manipulation of eligibility judgements". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Diagnosis of VAP by examination of chest radiographs, by physicians blinded to allocated treatment (information in Prendergast dissertation) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Unclear how many were assessed at each time point but paper stated that "less than 11 patients in each group at each time point" |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Roca Biosca 2011.
| Study characteristics | ||
| Methods | Study design: Single‐blind RCT Location: Tarragona, Spain Number of centres: 1 Study period: June 2006 to May 2009 Funding source: Grant from Health Investigation Fund (FISS 06/060) |
|
| Participants | Setting: ICU (14‐bed) Inclusion criteria: adults aged > 18 years, requiring mechanical ventilation for at least 48 hours, no pneumonia at baseline, at least 2 premolars and 1 incisor, consenting to take part Exclusion criteria: edentulous, suspected pneumonia < 18 years, requiring < 48 hours mechanical ventilation, tracheotomy, moribund (death expected within 72 hours) allergic to chlorhexidine Number randomised: 147 Number evaluated: not stated Baseline characteristics: report stated that there were no differences in gender, age, diagnosis, APACHE scores between the groups at baseline. No supporting data reported |
|
| Interventions |
Comparison: powered toothbrush + standard oral care vs standard oral care alone Experimental group: Standard oral hygiene protocol + powered toothbrush. Participant was elevated to 35°, oropharyngeal secretions were aspirated, intubation cuff pressure checked, then teeth, tongue and oral cavity cleaned with swab soaked in 10 mL 0.12% chlorhexidine digluconate. Solution left for 30 seconds then excess was aspirated. All tooth surfaces then brushed using a powered toothbrush Control group: Standard oral hygiene protocol alone as described for treatment group |
|
| Outcomes | 4 outcome variables planned: 1. Plaque index (Silness 1964) days 1, 5 and 10 2. Plaque cultures 3. VAP 4. Halitosis |
|
| Notes | Sample size calculation: not reported Translated from Portuguese by Luisa Fernandez‐Mauleffinch Email to authors sent 14 November 2012 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Group assignment was done randomly by sealed envelope". Method of sequence generation not described |
| Allocation concealment (selection bias) | Low risk | "Group assignment was done randomly by sealed envelope". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants or personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study described as single blind but unclear who was blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Numbers of participants included in outcome of plaque index were 74 and 73 at day 0, 60 and 57 at day 5, and 29 and 32 at day 10 for toothbrush and control groups respectively. Reasons for missing outcome data are extubation, need for tracheotomy, VAP, death or intubation for total of 28 days. No information as to numbers missing by group for each reason |
| Selective reporting (reporting bias) | High risk | Planned outcomes of plaque index and microbiological culture reported, but data for VAP and halitosis in each group not reported |
| Other bias | Unclear risk | Insufficient information in trial report to be clear about potential for other bias |
Scannapieco 2009.
| Study characteristics | ||
| Methods | Study design: A randomised, double‐blind, placebo‐controlled clinical trial Location: USA Number of centres: 1 18‐bed trauma ICU Study period: March 2004 until November 2007 Funding source: USPH grant R01DE‐14685 from the National Institute of Dental and Craniofacial Research |
|
| Participants | Inclusion criteria: Those admitted to the ICU who were expected to be intubated and mechanically ventilated within 48 hours of admission Exclusion criteria: A witnessed aspiration suspected with chemical pneumonitis; a confirmed diagnosis of post‐obstructive pneumonia e.g. advanced lung cancer; a known hypersensitivity to chlorhexidine; absence of consent; a diagnosed thrombocytopenia (platelet count < 40 and/or a INR > 2, or other coagulopathy); a do‐not‐intubate order; children < 18 years; pregnant women; legal incarceration; transfer from another ICU; oral mucositis; immunosuppression either HIV‐ or drug‐induced e.g. organ transplant patients or those on long‐term steroid therapy; and readmission to the ICU Number randomised: 175 Number evaluated: 146 Intervention group (chlorhexidine 1): n = 47; mean age: 44.8 ± 19.9; M/F: 43/15; mean APACHE II score: 18.5 ± 4.1 Intervention group (chlorhexidine 2): n = 50; mean age: 47.6 ± 19.1; M/F: 44/14; mean APACHE II score: 19.7 ± 6.1 Control group: n = 49; mean age: 50.0 ± 22.5; M/F: 36/23; mean APACHE II score: 19.1 ± 6.1 |
|
| Interventions |
Comparison: chlorhexidine twice per day + toothbrush vs chlorhexidine once per day + toothbrush vs placebo + toothbrush Intervention group: chlorhexidine (0.12% CHX gluconate) was applied using a rinse‐saturated oral foam applicator (Sage Products, Cary, IL, USA) once a day (placebo at other time). Intervention group: chlorhexidine (0.12% CHX gluconate) was applied using a rinse‐saturated oral foam applicator (Sage Products, Cary, IL, USA) twice a day (in the morning at about 8 a.m. and in the evening at about 8 p.m.). Control group: placebo was applied using a rinse‐saturated oral foam applicator twice per day. All groups had routine oral care using a suction toothbrush (Sage Products, Cary, IL, USA) twice a day and as needed to brush teeth and the surface of the tongue or approximately 1‐2 minutes, and applying suction at completion and as needed during the brushing. |
|
| Outcomes | 1. Incidence of VAP (diagnosed as the presence of more than 104 CFU of pathogen/ml of bqBAL fluid) 2. Death 3. Days ventilated 4. Days in hospital 5. Antibiotic use |
|
| Notes | Sample size calculation: estimated that 53 participants per arm would give 90% power to detect a 505 decrease in colonisation. For outcomes 2‐5, the P values were for 3‐group comparisons. NCT00123123 at ClinicalTrials.gov |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A web‐based enrolment system which allocated randomised participant identification numbers |
| Allocation concealment (selection bias) | Low risk | The oral topical treatment for each box was formulated and prepared by the hospital pharmacy. Sealed envelopes containing a random number were generated in blocks of 6 to provide concealment of participant assignment from the investigators. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Assignment of treatment was blinded to patients and all investigators including outcome assessors, statisticians and care providers". |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Assignment of treatment was blinded to patients and all investigators including outcome assessors, statisticians and care providers". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 175 participants were randomised, microbiological baseline data were available for 146 participants, 115 had full data at 48 hours. > 20% dropouts in all groups. ITT analysis used for 175 participants but unclear what imputation was used to account for losses |
| Selective reporting (reporting bias) | Unclear risk | Planned microbiological outcomes were reported only in graphs with no data presented. |
| Other bias | High risk | Problems with data analysis due to unclear denominator and imputations. Pre‐study antibiotic exposure higher in control group |
Seguin 2006.
| Study characteristics | ||
| Methods | Study design: 3‐arm parallel RCT Location: Rennes, France Number of centres: 1 Study period: August 2001 to January 2003 Funding source: not stated |
|
| Participants | Setting: surgical ICU Inclusion criteria: adults (> 18 years) with closed head trauma admitted to ICU and expected to need mechanical ventilation for at least 2 days Exclusion criteria: admitted > 12 hours after initial trauma, those with facial, thoracic, abdominal or spinal injuries, known history of reaction to iodine or of respiratory disease, chest infiltrates at admission or need for curative antibiotics Number randomised: 110 (38/36/36) Number evaluated: 98 (36/31/31) Baseline characteristics: ‐ Iodine group: age: 38 ± 17 years; M/F: 28/10 ‐ Saline group: age: 38 ± 16 years; M/F: 24/12 ‐ Control group: age: 41 ± 18 years; M/F: 23/13 |
|
| Interventions |
Comparison: povidone iodine versus saline versus usual care (no rinse) Iodine group (n = 38): nasopharynx and oropharynx rinsed 4‐hourly with 20 mL of 10% povidone iodine aqueous solution (Betadine oral rinse solution) reconstituted in a 60 mL solution with sterile water, followed by aspiration of oropharyngeal secretions Saline group (n = 36): nasopharynx and oropharynx rinsed 4‐hourly with 60 mL saline, followed by aspiration of oropharyngeal secretions Control group (n = 36): standard regimen without any instillation but with aspiration of oropharyngeal secretions For all participants, the suction catheters were inserted as distally as possible. Procedures were reported on patient charts. |
|
| Outcomes | 1. Incidence of VAP ‐ early and late onset 2. Duration of ventilation in surgical ICU 3. Length of stay in surgical ICU 4. Surgical ICU mortality |
|
| Notes | Sample size calculation: estimated that 30 participants in each group would provide 80% power with α error = 5% to detect a reduction in VAP from 50% to 20% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomly assigned to received one of three regimens according to computer‐generated random number codes kept in sealed envelopes". |
| Allocation concealment (selection bias) | Low risk | "Patients were randomly assigned to received one of three regimens according to computer‐generated random number codes kept in sealed envelopes". |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear information about blinding of outcome assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12 randomised participants (11%) excluded from analysis. 6 participants (1/3/2 in each group) were withdrawn because unexpected recovery meant that they were not on mechanical ventilation for 48 hours and a further 6 participants (1/2/3) died. Unlikely to have introduced a bias |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported in full |
| Other bias | Low risk | No other sources of bias identified |
Seguin 2014.
| Study characteristics | ||
| Methods | Study design: 2‐arm parallel‐group RCT Location: France Number of centres: 6 Study period: May 2008 to May 2011 Funding source: French Ministry of Health |
|
| Participants | Setting: ICU Inclusion criteria: > 18 years, closed traumatic brain injury (Glasgow Coma Score ≤ 8), expected mechanical ventilation ≥ 48 hours. Protocol amended to include patients with cerebral haemorrhage Exclusion criteria: patients in whom oral care procedure could not be performed within 12 hours after intubation, or had tetraplegia, facial trauma, pulmonary contusion involving > 1 lobe, aspiration pneumonia, current curative antimicrobial therapy, known allergy to povidone‐iodine, pregnancy. Number randomised: 179 (povidone‐iodine: 91; control: 88) Number evaluated: 150 (povidone‐iodine: 78; control: 72) Baseline characteristics: ‐ Povidone iodine*: age: 48 (19); M/F: 60/25; SAPS II score: 47 (11) ‐ Control*: age: 48 (18); M/F: 64/18; SAPS II score: 46 (12) * data presented on participants analysed |
|
| Interventions |
Comparison: povidone‐iodine vs placebo Povidone iodine: betadine 10% oral antiseptic solution portioned in identical vials containing 125 mL of product. Participants received nasopharynx and oropharynx rinsing with 20 mL of povidone iodine (10%) using a 60 mL syringe (final concentration 3.3%). The solution was progressively injected in the buccal and pharyngeal cavities and regularly suctioned during 2 minutes, every 4 hours. The protocol was continued until extubation or until day 30. Placebo: used as above |
|
| Outcomes | 1. Incidence of VAP 2. VAP as time to first occurrence 3. Incidence of early (< 7 days) and late (≥ 7 days) VAP 4. Incidence density of VAP per 1000 ventilator days 5. ICU and 90‐day mortality 6. Duration of ICU and hospital stay 7. Number of ventilation‐free days 8. Oropharayngeal and tracheal colonisation by potentially pathogenic microorganisms 9. Incidence of ventilator‐associated tracheobronchitis 10. Incidence of acute respiratory distress syndrome 11. Events of other nosocomial infections 12. Systemic antibiotic use 13. Adverse effects: agitation/hypertension, epistaxis, oxygen desaturation, aspiration, others |
|
| Notes | Sample size calculation: reported for VAP | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Randomization was centralized and performed by the pharmacy of the coordinating centre, stratified by centre and by type of patients (trauma or cerebral haemorrhage), and equilibrated by blocks of 4”. Probably done well using computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | “Randomization was centralized and performed by the pharmacy of the coordinating centre, stratified by centre and by type of patients (trauma or cerebral haemorrhage), and equilibrated by blocks of 4”. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | “The placebo was identical to povidone‐iodine in terms of colour, small and texture. Both povidone‐iodine and placebo were portioned in identical vials”. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “An independent diagnosis validation committee...blindly classified each patient as positive or negative for VAP.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 16% attrition rate for VAP incidence, but the numbers and reasons for lost to follow‐up were similar in each group. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Stefanescu 2013.
| Study characteristics | ||
| Methods | Study design: 2‐arm parallel‐group RCT Location: USA Number of centres: 1 Study period: June 2010 to January 2012 Funding source: Forsyth Medical Center Sara Lee for Women’s Health and WFSM Department of Paediatric Research Funds |
|
| Participants | Setting: neonatal ICU Inclusion criteria: extremely low birth weight, gestational age ≤ 28 weeks, receipt of mechanical ventilation of at least 3 days in the first week of life and in the interval between days 7 and 10 of life; a parent provided written informed consent Exclusion criteria: chromosomal or major congenital anomaly, the attending physician did not intend to provide full medical support Number randomised: 41 (biotene: 20; control: 21) Number evaluated: 41 (biotene: 20; control: 21) Baseline characteristics: ‐ Biotene: (median gestational age: 24 weeks (24‐25); M/F: 7/13) ‐ Control: (median gestational age: 25 weeks (24‐25); M/F: 11/10) |
|
| Interventions |
Comparison: biotene vs control Biotene: timed oral care performed using sterile foam‐tip swabs with OralBalance Gel from 2 mL single use twist‐tip vials, and involved hygiene of buccal mucosa, tongue and areas around endotracheal tube, every 4 hours from enrolment to final extubation. Control: timed oral care performed using sterile foam tip swabs with sterile water from 2 mL single use twist‐tip vials, and involved hygiene of buccal mucosa, tongue and areas around endotracheal tube, every 4 hours from enrolment to final extubation. All infants received VAP bundling, consisting of good hand hygiene and use of gloves when handling respiratory secretions, head of bed elevation, avoidance of routine use of saline with tracheal suctioning process, and weekly change of ventilator circuits. |
|
| Outcomes | 1. Incidence of VAP 2. Number of VAP per 1000 ventilator days 3. Mortality 4. Length of hospital stay 5. Duration of mechanical ventilation 6. Micro‐organism colonisation in tracheal aspirate 7. Adverse effects |
|
| Notes | Sample size calculation: not reported; a pilot study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “We used blocked randomisation with varying block size”. Probably done using computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | “Group assignments were provided in sealed envelopes which were kept secure by the investigational pharmacist, who was responsible for identifying the group to which each randomised patient was allocated”. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | “the primary limitation to our study was that we did not blind the staff to the intervention”. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "All radiographs where VAP was suspected were reviewed with the paediatric radiologists who were blinded to individual study assignment”. Potential for bias in deciding whether VAP was suspected |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Unclear risk | More infants in the control group received a complete course of antenatal steroids compared to infants in the biotene group (P = 0.045). A complete course of antenatal steroids improves neonatal lung maturity and function and may reduce the risk of VAP (Roberts 2017). This imbalance is likely to lead to an underestimate of the benefit of the active treatment. |
Tang 2013.
| Study characteristics | ||
| Methods | Study design: RCT Location: adult ICU (China) Number of centres: 1 Study period: 14 months (dates not given) Funding source: unclear |
|
| Participants | Setting: adult ICU Inclusion criteria: all patients admitted to the ICU with receipt of mechanical ventilation of at least 48 hours were assessed for inclusion in the study. Exclusion criteria: unclear Number randomised: 60 (gp A: 30; gp B: 30) Number evaluated: 60 (gp A: 30; gp B: 30) Baseline characteristics: age: 56 (13.22); M/F: 38/22 "Age and sex comparable between groups" |
|
| Interventions |
Comparison: saline rinse vs saline swab Gp A: rinse oral cavity with saline Gp B: saline swab with saline cotton ball |
|
| Outcomes | 1. VAP 2. Mortality 3. Duration of ventilation |
|
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not mentioned and not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessor blinding not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in analysis |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Unclear risk | The authors did not give a detailed description about the intervention methods and frequency of oral care in each group. |
Tantipong 2008.
| Study characteristics | ||
| Methods | Study design: single‐centre RCT with 2 parallel groups Location: Thailand Number of centres: 1 tertiary care university hospital Study period: January 2006 through March 2007 Funding source: Thailand Research Fund and Faculty of Medicine Siriraj Hospital |
|
| Participants | Inclusion criteria: eligible patients were adults aged ≧ 18 years who were hospitalised in intensive care units (36 beds) or general medical wards (240 beds) at Siriraj Hospital and who received mechanical ventilation. Exclusion criteria: patients who had pneumonia at enrolment or who had a chlorhexidine allergy Number randomised: 207 Number evaluated: 207 (110 participants received mechanical ventilation for > 48 hours) ‐ Experimental group: n = 102; age: 56.5 ± 20.1; M/F: 50/52; mean APACHE II score: 16.7 ± 7.9 ‐ Control group: n = 105; age: 60.3 ± 19.1; M/F: 51/54; mean APACHE II score: 18.2 ± 8.1 Participants' demographic characteristics between groups did not differ significantly. |
|
| Interventions |
Comparison: toothbrush + chlorhexidine vs toothbrush + placebo Experimental group (n = 102): received oral care 4 times a day with brushing the teeth, suctioning any oral secretions, and rubbing the oropharyngeal mucosa with 15 mL of a 2% chlorhexidine solution, until their endotracheal tubes were removed. Control group (n = 105): same oral care procedure with normal saline solution |
|
| Outcomes | 1. Incidence of VAP 2. Number of cases of VAP per 1000 ventilator days 3. Incidence of VAP for participants who received mechanical ventilation for > 2 days 4. Overall mortality 5. Mean days of mechanical ventilation (mean ± SD) 6. Rate of irritation of oral mucosa |
|
| Notes | Sample size calculation: estimated that 108 participants required in each group to give 80% power to detect a 50% decrease in VAP with 5% Type 1 error | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...randomized...by stratified randomization according to sex and hospital location of eligible patient" |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned and probably not done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded as chlorhexidine solution had different odour and taste from saline |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The assessors who determined whether a participant developed pneumonia were unaware of the participant's study group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | All randomised participants included in outcome evaluation but only 53% of participants on ventilators for > 2 days and therefore at risk of VAP |
| Selective reporting (reporting bias) | Unclear risk | Planned outcome VAP but not all participants at risk and information unclear. Mortality reported |
| Other bias | Unclear risk | Only 60% of study participants received ventilation in ICU and only 53% of participants received mechanical ventilation for > 48 hours. Likely that nursing care protocols were different in general medical wards compared to ICUs |
Tuon 2017.
| Study characteristics | ||
| Methods | Study design: 2‐arm parallel group RCT Location: Brazil Number of centres: 1 Study period: June 2014 to March 2015 Funding source: no funding |
|
| Participants | Setting: ICU Inclusion criteria: hospital admission followed by MV; age >= 18 years, patients identified as having a high probability of MV for > 48 h and permanent teeth (anterior and posterior) Exclusion criteria: failure to provide written informed consent, hospitalisation > 24 h, recent use of antibiotics (< 1 week), recent admission to another hospital or emergency room, suspected infection in the upper or lower respiratory tract, fewer than four culture samples Number randomised: 16 (intervention group: 8; control group: 8) Number evaluated: 16 (intervention group: 8; control group: 8) Baseline characteristics: ‐ Intervention group: age: 53.1; M/F: 5/3; APACHE II score: not reported) ‐ Control group: age: 42.8; M/F: 4/4; APACHE II score: not reported) |
|
| Interventions |
Comparison: 2% CHX vs placebo (0.9% normal saline) CHX: patients received oral washing with 15 mL of 2% CHX digluconate by a trained nursery team. The CHX solution was gently brushed into the gum, oral mucosa and tongue two times daily until ICU discharge. Placebo: patients underwent mouthwashing with a 0.9% NaCl solution |
|
| Outcomes | 1. Incidence of VAP 2. Microbiological profiles |
|
| Notes | Sample size calculation: not mentioned Other information of note: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding not described and not possible. Difference between intervention and control meant caregivers would be aware of who was in each group. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluation |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Xu 2007.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Location: Nanjing, China Number of centres: 1 Study period: December 2004 to June 2006 Funding source: no external funding |
|
| Participants | Setting: ICU in drum tower hospital of Nanjing University Inclusion criteria: critically ill adult patients in ICU receiving mechanical ventilation Exclusion criteria: patients with severe oral diseases, mechanical ventilation for > 24 hours prior to study entry, those who refused oral care protocol Number randomised: 164 Number evaluated: 164 Baseline characteristics: not reported for each randomised group |
|
| Interventions |
Comparison: saline swab vs saline rinse versus both Experimental group A (n = 58): rinsing the oropharyngeal cavity with saline for 5‐10 seconds, followed by suction aspiration, repeated 5‐10 times twice daily for 7 days Experimental group B (n = 62): both wipe and rinse as above, twice daily for 7 days Control group (n = 44): usual care ‐ wiping the oropharyngeal cavity with saline‐soaked cotton ball twice daily for 7 days |
|
| Outcomes | VAP, stomatitis, fungal infection | |
| Notes | Diagnosis of VAP was according to Chinese Society of Respiratory Diseases criteria. Information translated from Chinese paper by Shi Zongdao and colleagues |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly allocated" but no details of sequence generation described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluation |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported |
| Other bias | Low risk | No other sources of bias identified |
Xu 2008.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Location: Shandong, China Number of centres: 1 Study period: not stated Funding source: no external funding |
|
| Participants | Setting: ICU of the second hospital of Shandong University Inclusion criteria: adults entering ICU receiving mechanical ventilation expected to last > 48 hours Exclusion criteria: patients with pulmonary infections Number randomised: 116 Number evaluated: 116 Baseline characteristics: not reported for each randomised group |
|
| Interventions |
Comparison: saline rinse vs saline swab Experimental group (n = 64): rinse of the oropharyngeal cavity with saline for 5‐10 seconds, followed by suction aspiration and repeated 5‐10 times, twice daily Control group (n = 52): standard oral care comprising scrubbing with a cotton ball soaked in saline, twice daily |
|
| Outcomes | VAP, duration of ventilation (days) | |
| Notes | Diagnosis of VAP was according to Chinese Society of Respiratory Diseases criteria. Information translated from Chinese paper by Shi Zongdao and colleagues |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly allocated". Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in the outcome evaluation |
| Selective reporting (reporting bias) | Low risk | Both outcomes listed in Methods were reported in the Results section. |
| Other bias | Low risk | No other sources of bias identified |
Yao 2011.
| Study characteristics | ||
| Methods | Study design: single‐blind pilot RCT (NCT00604916) Location: Taiwan Number of centres: 1 Study period: March to November 2007 Funding source: grants from Taiwan National Science Council and Career Development grant from National Health Research Institutes |
|
| Participants | Setting: surgical ICU Inclusion criteria: intubated and ventilated postoperative patients expected to be in ICU > 48 hours and expected to require mechanical ventilation for 48 to 72 hours with nasal or endotracheal intubation Exclusion criteria: pneumonia at baseline Number randomised: 53 Number evaluated: 53 (VAP), 50 at day 3‐4, 42 at day 7‐8 Baseline characteristics: ‐ Intervention group: age: 60.7 ± 16.0; M/F: 17/11; APACHE II score: 19.6 ± 5.2 ‐ Control group: age: 60.5 ± 16.5; M/F: 17/8; APACHE II score: 19.4 ± 4.4 |
|
| Interventions |
Comparison: oral care + toothbrushing twice a day vs usual oral care Experimental group: standardised oral care protocol twice daily for 15‐20 minutes for 7 days from trained intervention nurse. Bed elevated 30° to 45°, hypopharyngeal suctioning, mouth moistened with 5‐10 mL purified water, buccal surfaces of teeth cleaned with powered toothbrush and lingual tooth surfaces and tongue, gums and mucosa massaged with soft paediatric toothbrush. Oral cavity then cleaned with toothette swab connected to a suction tube and rinsed with 50 mL water + hypopharyngeal suctioning Control group: received oral care protocol, twice daily for 10‐15 minutes provided by same trained intervention nurse. Participants elevated, hypopharyngeal suctioning, lips moistened with toothette swab and water, then further hypopharyngeal suctioning |
|
| Outcomes | 1. Oral Assessment Guide (OAG) score 2. Plaque score (Turesky‐Gilmore‐Glickman modification of Quigley‐Hein plaque index with disclosing dye. Recorded 1 tooth from each quadrant (prioritising premolars and incisors) scores summed) 3. Duration of ventilation 4. Length of ICU stay 5. Incidence of VAP (defined as CPIS > 6) 4. Mortality (ICU) |
|
| Notes | Sample size calculation: pilot study NCT 00604916 at ClinicalTrials.gov Email sent to author 14 November 2012. Reply received 12 December 2012 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...randomized using a computer generated randomization table" |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned in trial report Unclear whether allocation was concealed from researchers prior to assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Experimental group received toothbrushing (both powered and manual) and control group did not, so blinding of participants and personnel not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes assessed blinded to allocated treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | VAP outcome assessed in all randomised participants. For oral health and plaque outcomes, 8/28 (experimental) and 7/25 (control) participants lost (transferred to ward) and 2/28 participants in experimental group died |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported, but denominators unclear for VAP and mortality. However, this information was supplied by email from the authors. |
| Other bias | Unclear risk | 3/28 (11%) and 1/25 (4%) participants in experimental and control groups were edentulous. Unclear how the intervention and outcomes were applied in these participants |
Zhao 2012.
| Study characteristics | ||
| Methods | Study design: single‐centre RCT with 2 parallel groups Location: China Number of centres: 1 surgical ICU in city hospital Study period: May 2010 to April 2011 Funding source: not stated |
|
| Participants | Inclusion criteria: admission into the ICU, orally intubated, receiving mechanical ventilation Exclusion criteria: not specified Number randomised: 324 (162 per group) Number evaluated: 324 Age group: mean 66.25 ± 15.28 Baseline characteristics were comparable. |
|
| Interventions |
Comparison: Yikou (triclosan) rinse vs saline Experimental group: oral cavity swab with 15 mL of Yikou gargle (triclosan was main ingredient), 4 times a day Control group: oral cavity swab with normal saline, 4 times a day Secretions were aspirated using suction once daily and sent to lab for culture. |
|
| Outcomes | 1. Incidence of VAP in < 4 days of ventilation and within 4 to 10 days of ventilation 2. Mechanical ventilation days 3. ICU stay days 4. Culture of the samples taking from oropharyngeal cavity and inferior respiratory tract (Table 3, detection rates of microbial pathogens before and after oral nursing care were listed) |
|
| Notes | Diagnosis of VAP was mainly determined by microbial examination of the aspirate secretions from the inferior respiratory tract, which was performed every day. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly divided into 2 groups" |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding not described and unclear whether Yikou and saline had the same appearance and odour |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not specified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The main results were all reported. |
| Selective reporting (reporting bias) | Low risk | The results were fully reported. |
| Other bias | Unclear risk | Only the results of microbial examination of the aspirate secretions from the inferior respiratory tract as tool of VAP diagnosis was mentioned and its diagnostic efficacy may not be enough. |
AIDS = acquired immunodeficiency syndrome APACHE II = Acute Physiology and Chronic Health Evaluation II CAO = caries/absent/occluded CDC = Centers for Disease Control CHX = chlorhexidine COL = colistin CPIS = Clinical Pulmonary Infection Score DMFT = decayed/missing/filled teeth ED = emergency department ET = endotracheal tube GCS = Glasgow coma scale gp = group HIV = human immunodeficiency viruses HP = hydrogen peroxide ICU = intensive care unit INR = international normalised ratio IQRs = interquartile ranges ITT = intention‐to‐treat MCPIS = modified clinical pulmonary infection score M/F = male/female MV = mechanical ventilation NaCI = sodium chloride NS = normal saline OAG = oral assessment guide PICU = paediatric intensive care unit ppm = parts per million RCT = randomised controlled trial RTI = respiratory tract infection SAPS = Simplified Acute Physiologic Score SD = standard deviation SID = subject identification SLS = sodium lauryl sulfate SOFA = sequential organ failure assessment TRISS = Trauma Injury Severity Score UTI = urinary tract infection VAP = ventilator‐associated pneumonia vs = versus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abusibeih 2010 | Quasi‐randomised trial |
| Anon 2012 | Abstract only; insufficient information to assess |
| Atashi 2018 | A complex bundle versus a simpler bundle, which is outside the scope of this review |
| Baradari 2012 | Not aimed to assess VAP incidence or mortality |
| Bellissimo‐Rodrigues 2014 | Intervention was dental care, not dental hygiene care |
| Bordenave 2011 | Identified from ClinicalTrials.gov website as ongoing study, but email from contact author on 8 November 2012 confirmed that this study did not proceed due to lack of funding |
| Buckley 2013 | Not RCT |
| Chao 2009 | Not RCT |
| Chen 2008 | CHX versus saline: the intervention group received "routine oral care" but the control group did not |
| Da Collina 2017 | Published protocol identified, but email from contact author on 18 March 2020 confirmed that this trial was not performed due to the withdrawal of the dentist (PhD student) who would carry out the treatment of patients |
| Dale 2019 | Protocol for a trial on a bundle including suctioning |
| Darnell 2015 | Not RCT |
| DeRiso 1996 | Unclear if all those who developed VAP had been on mechanical ventilation for at least 48 hours |
| Epstein 1994 | The participants involved in the study were not critically ill |
| Fan 2012 | The ingredients of the mouthwash used in the trial were not reported, so we could not judge whether it contained antibiotics or not |
| Fan 2015 | The CHX solution used in interventions contained antibiotics |
| Ferozali 2007 | The target population was long‐term care residents, not critically ill people in hospitals |
| Fourrier 2000 | Unclear if all those who developed VAP had been on mechanical ventilation for at least 48 hours |
| Fourrier 2005 | Unclear if all those who developed VAP had been on mechanical ventilation for at least 48 hours; some of the participants had pneumonia at baseline |
| Genuit 2001 | Not RCT |
| Grap 2004 | Not aiming to assess VAP incidence or mortality |
| Gu 2013 | Not RCT |
| Guo 2007 | RCT, but patients had lung trauma (injury before receiving the oral nursing intervention) |
| Guo 2017 | Participants had pneumonia at baseline |
| Haghighi 2017 | The interventions being tested in the experimental group included adjustment of the endotracheal tube cuff pressure, mouth and throat deep suctioning, and lip moistening in addition to oral hygiene care, which were outside the scope of the review |
| Houston 2002 | Likely that fewer than 10% of study participants had mechanical ventilation for a minimum of 48 hours |
| Jacomo 2011 | Unclear how many participants have been on mechanical ventilation for at least 48 hours |
| Jafari 2007 | Abstract only; insufficient information to assess |
| Kusahara 2012b | Not aiming to assess VAP incidence or mortality |
| Labeau 2013 | Not RCT |
| Lai 1997 | RCT of critically ill people, unclear how many were on mechanical ventilation; outcome candidiasis |
| Li 2011 | Participants allocated to groups by alternation (quasi‐RCT) |
| Li 2012 | The mouthwash (Kouitai) used in the trial contained both chlorhexidine and metronidazole, and the latter is an antibiotic |
| Liang 2007 | The participants involved in the study did not use mechanical ventilation |
| Liao 2015 | Not RCT |
| Liwu 1990 | Clinical controlled trial, not an RCT |
| MacNaughton 2004 | Abstract only; insufficient information to assess |
| Maury 2015 | Not RCT |
| McCartt 2010 | Not aiming to assess VAP incidence or mortality |
| McCoy 2012 | Not RCT |
| Munro 2009 | Some of the participants had pneumonia at baseline |
| Munro 2015 | Intervention was preintubation oral hygiene care |
| Nasiriani 2016 | Randomisation compromised as the authors replaced 22 dropouts with new participants (selection method unknown) |
| NCT01657396 | Identified from ClinicalTrials.gov website, but email from contact author on 9 March 2020 confirmed that this trial was a pilot trial to test whether a larger trial was feasible and hence patient outcomes were not the primary measures |
| Needleman 2011 | Not aiming to assess VAP incidence or mortality |
| Ogata 2004 | The target population was patients about to receive orotracheal intubation ‐ they were not on mechanical ventilation. Study about gargling with povidone iodine before oral intubation to reduce the transport of bacteria into the trachea, not oral care intervention in critically ill patients to reduce VAP |
| Pawlak 2005 | Not RCT |
| Pelucchi 2013 | Systematic review not RCT |
| Pivkina 2014 | Abstract only; insufficient information to assess |
| Sands 2015 | Not RCT |
| Santos 2008 | Email reply from Dr Santos stated that “The nurse put the first admission on biotene and the second admission on cetylpyridium, the third admission on biotene and so on.” Alternation as an allocation method is not random and therefore this study was excluded |
| Sebastian 2012 | Most of the children admitted to ICU had pneumonia at baseline |
| Segers 2006 | The participants involved in the study did not use mechanical ventilation |
| Seo 2011 | Not RCT |
| Swartz 2015 | Not RCT |
| Tattevin 2015 | Not RCT |
| Tian 2017 | Authors did not report either the ingredients or product name of the 'biological enzyme disinfectant' used, therefore we could not judge whether it contained antibiotics; contact information of the authors was not provided |
| Tsai 2017 | Abstract only; insufficient information to assess; email address unavailable |
| Ueda 2004 | The target population was people in nursing homes, not critically ill people in hospitals |
| Wang 2006 | Quasi‐RCT |
| Wang 2012 | The interventions being tested in the experimental group included elevation of the head of the bed, closed endotracheal suctioning in addition to oral nursing care, which was outside the scope of the review |
| Wang 2016 | CHX solution contained antibiotics |
| Yin 2004 | RCT aiming to improve oral cleanliness. Unlikely that participants received mechanical ventilation |
| Yun 2011 | Not RCT |
| Zouka 2010 | Abstract only; insufficient information to include in review. Emailed contact author 6 November 2012 without response |
CHX = chlorhexidine ICU = intensive care unit RCT = randomised controlled trial VAP = ventilator‐associated pneumonia
Characteristics of studies awaiting classification [ordered by study ID]
Chacko 2017.
| Methods | RCT |
| Participants | Patients ventilated through an orotracheal tube, and recruited within 4 to 6 hours of intubation; aged 16 years and older, receiving VAP bundle care |
| Interventions | CHX + toothbrushing (and suction) versus CHX alone |
| Outcomes | VAP, use of antibiotics, ventilator days, length of ICU stay |
| Notes | Emailed study investigator on 16 March 2020 for length of follow‐up/time point of VAP diagnosis |
Hashemi 2018.
| Methods | RCT |
| Participants | Patients admitted to ICU |
| Interventions | Chlorhexidine mouthwash versus stop‐snoring mouthwash |
| Outcomes | Incidence of VAP |
| Notes | Full texts in Persian. Sent to translators on 31 March 2020 for assistance |
Hashemi 2019.
| Methods | RCT |
| Participants | Patients admitted to ICU |
| Interventions | Chlorhexidine mouthwash versus herbal cinnamol mouthwash |
| Outcomes | Incidence of VAP |
| Notes | Full texts in Persian. Sent to translators on 31 March 2020 for assistance |
IRCT20110427006318N12.
| Methods | RCT |
| Participants | Patients 18 to 75 years old under mechanical ventilation for more than 48 hours, Glasgow Coma scale between 6 and 11, feeding with gastric tube, no contraindications to oral care, propolis insensitivity |
| Interventions | Propolis versus CHX |
| Outcomes | VAP |
| Notes | Emailed study investigator on 16 March 2020 to confirm whether published in full |
IRCT2013050813278N1.
| Methods | RCT |
| Participants | Age between 18 to 65 years, having oral endotracheal tube, no pneumonia or immunosuppressive diseases before the start of the study according to judgement of a physician, be permitted to perform oral care for patients according to doctor, not having dentures, no history of allergy to chlorhexidine, the absence of wound, infection and oral trauma, without underlying lung problems |
| Interventions | CHX + brushing versus CHX |
| Outcomes | Oral health; pneumonia |
| Notes | Emailed study investigator on 16 March 2020 to confirm whether study published in full |
IRCT201512115363N8.
| Methods | RCT |
| Participants | Age between 20 to 50 years; admission less than 24 hours in ICU; intubated patient; satisfaction of patients and patients' families; the absence of pneumonia |
| Interventions | Rose extract + CHX versus CHX |
| Outcomes | Mortality, VAP, connection to ventilator days, length of intensive care unit stay |
| Notes | Emailed study investigator on 16 March 2020 to ask whether study published in full |
IRCT2016052828134N1.
| Methods | RCT |
| Participants | 18 to 65 years old, having endotracheal tube through the mouth; admitted to ICU less than 12 hours; having natural teeth; no history of antibiotic use within preceding two weeks; not pregnant; no history of allergy to herbal compounds; no HIV; no use of steroid drugs; no injury in or around the mouth; no pneumonia; no leukopenia and neutropenia and serum albumin < 2/5 mg/dL |
| Interventions | Aloe vera versus saline |
| Outcomes | Pneumonia, dental plaque index |
| Notes | Emailed study investigator on 16 March 2020 to ask whether study published in full |
IRCT2017022032676N1.
| Methods | RCT |
| Participants | Age between 18 and 65, intubated, under mechanical ventilation in 48 hours after admission |
| Interventions | Persica versus CHX |
| Outcomes | Pneumonia, complication, ICU mortality, intubation duration |
| Notes | Emailed study investigator on 16 March 2020 to confirm whether published in full |
IRCT2017050727819N4.
| Methods | RCT |
| Participants | Oral intubation, 30 to 50 years old, lack of pulmonary infection, lack of sensitivity to herbal combination, no history of immunosuppressive drugs, no history of diabetes, level of consciousness 3 to 8, no wound in the mouth |
| Interventions | Orthodentol versus CHX |
| Outcomes | Pneumonia |
| Notes | Emailed study investigator on 16 March 2020 to confirm study whether published in full |
IRCT20171225038053N1.
| Methods | RCT |
| Participants | Fewer than 48 hours passed since the patient was admitted to the intensive care unit, lack of specific lesion of mouth and around it by using the Beck criterion |
| Interventions | CHX versus CHX + hydrogen peroxide |
| Outcomes | Incidence of VAP |
| Notes | Emailed study investigator on 16 March 2020 to confirm whether study published in full |
IRCT20180520039739N2.
| Methods | RCT |
| Participants | Patients with age of 2 months to 14 years who need mechanical ventilation for at least 48 hours admission in paediatric ICU |
| Interventions | CHX versus dine mouthwash (Dineh Iran) |
| Outcomes | Incidence of VAP |
| Notes | Emailed study investigator on 16 March 2020 to confirm whether study published in full |
IRCT20191012045066N1.
| Methods | RCT |
| Participants | Patient required to have an endotracheal tube, no mucosal inflammation or severe trauma to the mouth, no chronic disease and immune deficiency, has teeth, does not have re‐intubation, on the first day of patient intubation |
| Interventions | CHX versus CHX + toothbrushing |
| Outcomes | Clinical pneumonia infection score, oral health score |
| Notes | Emailed study investigator on 16 March 2020 to confirm whether study published in full |
Jamshidi 2016.
| Methods | RCT |
| Participants | Patients admitted to ICUs of Ayatollah Mousavi Hospital of Zanjan that received intubation within 24 hours |
| Interventions | CHX oral swab versus toothbrushing vs toothbrushing + CHX oral swab |
| Outcomes | Incidence of VAP |
| Notes | Full texts in Persian. Sent to translators on 31 March 2020 for assistance |
Mehrabadi 2015.
| Methods | RCT |
| Participants | Intubated patients in ICUs of educational hospitals in Arak in 2014 |
| Interventions | Echinacea versus normal saline |
| Outcomes | Incidence of VAP |
| Notes | Full texts in Persian. Sent to translators on 31 March 2020 for assistance |
CHX = chlorhexidine; HIV = human immunodeficiency viruses; ICU = intensive care unit; OA = oral assessment; RCT = randomised controlled trial; VAP = ventilator‐associated pneumonia; vs = versus
Characteristics of ongoing studies [ordered by study ID]
RBR‐7p6568.
| Study name | Oral hygiene in critically ill patients ‐ a randomized controlled trial |
| Methods | RCT |
| Participants | Patients admitted to the intensive care unit of the Clinical Hospital of the Federal University of Uberlandia from 2019 to 2020; dependent on mechanical ventilation for more than 48 hours; regardless of gender; over 18 years old; head trauma victim |
| Interventions | CHX versus cetylpyridinium versus water |
| Outcomes | Mortality; ventilator‐associated pneumonia; adverse events; days of extubation time, length of stay in the intensive care unit and length of hospital stay |
| Starting date | May 2019 |
| Contact information | drapaulacunhavieira@gmail.com |
| Notes | Emailed study investigator 16 March 2020 to confirm whether published in full. Reply received 21 March 2020 ‐ ongoing trial |
TCTR20190530003.
| Study name | Efficacy of moraceae with chlorhexidine mouthwash on microbial flora of critically ill intubated patients |
| Methods | RCT |
| Participants | Adults (age more than 18 years); admitted in the medical intensive care unit within 24 hours; having a tracheal tube and expect to go on mechanical ventilation at least 48 hours; no contraindication for moraceae or chlorhexidine mouthwash |
| Interventions | CHX + moraceae versus CHX |
| Outcomes | Oral microbial flora; adverse events; oral health; ventilator‐associated pneumonia |
| Starting date | May 2019 |
| Contact information | vveerapong@gmail.com |
| Notes | Emailed study investigator 8 March 2020 to confirm whether published in full. Reply received 8 March 2020 ‐ ongoing trial |
CHX = chlorhexidine; ICU = intensive care unit; OA = oral assessment; RCT = randomised controlled trial; VAP = ventilator‐associated pneumonia
Differences between protocol and review
For this 2020 update:
We added another comparison (Comparison 2: CHX versus other oral care agents) to better accommodate head‐to‐head trials, and re‐classified the included studies accordingly.
We added another subgroup analysis ‐ intervention concentration.
We excluded some trials that had been included in the original review, but on further investigation did not meet the inclusion criteria, in particular, the requirement to ensure participants did not have pneumonia at baseline and to consider only participants who had been on mechanical ventilation for at least 48 hours.
Changes to methodology between 2013 and 2016 versions:
As the purpose of this systematic review is to determine the effects of oral hygiene care on the development of VAP in a group of very ill patients in intensive care, we excluded studies that reported only intermediate outcomes, such as microbial colonisation or CPIS scores, because the relationship between these outcomes and VAP or mortality is unclear.
We dropped the outcome 'microbial colonisation'. We excluded studies that only reported this outcome, and not VAP incidence or mortality, as an analysis of this outcome for the included studies would lead to selective reporting. Additionally, most traditional criteria for VAP diagnosis already incorporate results of microbial colonisation laboratory tests (Waters 2015).
We undertook a subgroup analysis for a dose‐response relationship for chlorhexidine, as research suggested a possible relationship between chlorhexidine dose and mortality/effectiveness in VAP reduction (Klompas 2014; Zhang 2013).
We used the risk ratio (RR) rather than the odds ratio (OR) for the binary data, in line with current Cochrane Oral Health policy, as this made interpretation of the results easier.
We only searched the VIP database for Chinese studies, because the previous search strategies are no longer valid.
We added the outcomes reported in the 'Summary of findings tables' to the Methods section.
Differences between the protocol and the first version of the review (2013):
1) We clarified inclusion criteria.
Participants in trials should not have a respiratory infection at baseline.
The interventions must include an oral hygiene care component. We excluded trials where the intervention being evaluated was a type of suction system or variation of method, timing, or place where mechanical ventilation was introduced (e.g. emergency room or ICU).
Minimum duration of mechanical ventilation of 48 hours, in order for the diagnosis of nosocomial pneumonia, either during the period of ventilation or within 48 hours of extubation, to be considered ventilator‐associated pneumonia.
Outcome of mortality defined as either all‐cause ICU mortality or, where this was not available, all‐cause 30‐day mortality. We considered that the effect of the underlying condition(s) on mortality would be similar in each randomised treatment group during this period.
In order to avoid duplication, we excluded trials where the intervention was selective decontamination of the digestive tract with antibiotics, as these interventions are included in another Cochrane Review (D'Amico 2009).
Likewise, we excluded trials where the intervention was probiotics, as these interventions are included in another Cochrane Review (Hao 2015).
2) We updated the text in the Methods section of this review about the 'Risk of bias' assessment in line with the latest version of the Cochrane Handbook for Systematic Reviews of Interventions, and we added more details about the process followed.
Contributions of authors
Conducting and writing the initial review: QZ, HW Conducting and writing the 2016 update of this review: QZ, CL, HW, FH Co‐ordinating the update: FH Developing search strategy and undertaking searches for the update: TZ, XW, CL, FH Screening search results for the update: TZ, XW, QZ, HW, FH Extracting data and assessing risk of bias for the update: TZ, XW, FH Analysing and interpreting data for the update: TZ, XW, HW, FH Writing the review update: TZ, XW, FH Approving the final review update prior to submission: TZ, XW, QZ, CL, HW, FH
Sources of support
Internal sources
School and Hospital of Stomatology, Wuhan University, China
Division of Dentistry, School of Medical Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, UK
-
Manchester Academic Health Sciences Centre (MAHSC), UK
Cochrane Oral Health is supported by MAHSC and the NIHR Manchester Biomedical Research Centre
-
West China College of Stomatology of Sichuan University and the Chinese Cochrane Center, China
The 2013 version of this review was supported by the West China College of Stomatology, Sichuan University academically and in manpower resource; statistical analysis was supported by the Chinese Cochrane Center
External sources
Wuhan Young and Middle‐aged Medical Talents Training Program (No. [2019]87), China
-
Cochrane Oral Health Global Alliance, Other
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oral-health.cochrane.org/partnerships-alliances). Contributors over the past two years have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; NHS Education for Scotland, UK; and the Swiss Society for Endodontology, Switzerland.
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Evidence Synthesis Programme, the NIHR, the NHS or the Department of Health and Social Care.
CMB funding SR0510, Project of Development of Systematic Review supported by Chinese Medical Board of New York, USA
Declarations of interest
Tingting Zhao: none known Xinyu Wu: none known Qi Zhang: none known Chunjie Li: none known Helen V Worthington: none known. I am an Editor with Cochrane Oral Health. Fang Hua: none known. I am an Editor with Cochrane Oral Health.
These authors contributed equally to this work.
These authors contributed equally to this work.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Bellissimo‐Rodrigues 2009 {published data only}
- Bellissimo-Rodrigues F, Bellissimo-Rodrigues WT, Viana JM, Teixeira GC, Nicolini E, Auxiliadora-Martins M, et al. Effectiveness of oral rinse with chlorhexidine in preventing nosocomial respiratory tract infections among intensive care unit patients. Infection Control & Hospital Epidemiology 2009;30(10):952-8. [DOI] [PubMed] [Google Scholar]
Berry 2011 {published data only}
- Berry AM, Davidson PM, Masters J, Rolls K, Ollerton R. Effects of three approaches to standardized oral hygiene to reduce bacterial colonization and ventilator associated pneumonia in mechanically ventilated patients: a randomised control trial. International Journal of Nursing Studies 2011;48(6):681-8. [DOI] [PubMed] [Google Scholar]
Berry 2013 {published data only}
- Berry A M. A comparison of Listerine and sodium bicarbonate oral cleansing solutions on dental plaque colonisation and incidence of ventilator associated pneumonia in mechanically ventilated patients: a randomised control trial. Intensive & Critical Care Nursing 2013;29(5):275-81. [DOI] [PubMed] [Google Scholar]
Bopp 2006 {published data only}
- Bopp M, Darby M, Loftin KC, Broscious S. Effects of daily oral care with 0.12% chlorhexidine gluconate and a standard oral care protocol on the development of nosocomial pneumonia in intubated patients: a pilot study. Journal of Dental Hygiene 2006;80(3):9. [PubMed] [Google Scholar]
Cabov 2010 {published and unpublished data}
- Cabov T, Macan D, Husedzinovic I, Skrlin-Subic J, Bosnjak D, Sestan-Crnek S, et al. The impact of oral health and 0.2% chlorhexidine oral gel on the prevalence of nosocomial infections in surgical intensive-care patients: a randomized placebo-controlled study. Wiener Klinische Wochenschrift 2010;122(13-14):397-404. [DOI] [PubMed] [Google Scholar]
Caruso 2009 {published data only}
- Caruso P, Denari S, Ruiz SAL, Demarzo SE, Deheinzelin D. Saline instillation before tracheal suctioning decreases the incidence of ventilator-associated pneumonia. Critical Care Medicine 2009;37(1):32-8. [DOI] [PubMed] [Google Scholar]
Dahiya 2012 {published data only}
- Dahiya U. Decontamination with chlorhexidine gluconate reduces the incidence of ventilator associated pneumonia. Nursing Journal of India 2012;103:89-91. [PubMed] [Google Scholar]
De Lacerda 2017 {published data only}
- De Lacerda Vidal CF, Vidal AK de L, Monteiro JG de M, Cavalcanti A, Henriques AP de C, Olveira M, et al. Impact of oral hygiene involving toothbrushing versus chlorhexidine in the prevention of ventilator-associated pneumonia: a randomized study. BMC Infectious Diseases 2017;17:112 [Erratum appears in BMC Infect Dis. 2017 Feb 27;17 (1):173; PMID: 28241748]. [DOI] [PMC free article] [PubMed]
Feng 2012 {published data only}
- Feng S, Sun X, Chen Y. Application of different mouthwashes in oral nursing for patients with orotracheal intubation. China Medicine and Pharmacy 2012;8(2):100-1. [Google Scholar]
Fields 2008 {published data only}
- Fields LB. Oral care intervention to reduce incidence of ventilator-associated pneumonia in the neurologic intensive care unit. Journal of Neuroscience Nursing 2008;40(5):291-8. [DOI] [PubMed] [Google Scholar]
Fu 2019 {published data only}
- Fu T, Zhong Q, Zheng C. Bacteriostasis effect of oral administration of chlorhexidine on patients with mechanical ventilation and prevention and treatment of ventilator - associated pneumonia. Chinese Nursing Research 2019;33(3):431-4. [Google Scholar]
Grap 2011 {published data only}
- Grap MJ, Munro CL, Hamilton VA, Elswick RK Jr, Sessler CN, Ward KR. Early, single chlorhexidine application reduces ventilator-associated pneumonia in trauma patients. Heart & Lung 2011;40(5):e115-22. [DOI] [PubMed] [Google Scholar]
Hanifi 2017 {published data only}
- Hanifi N, Masoumi M, Jamshidi MR, Faghihzadeh S. The effect of ozonated water and chlorhexidine gluconate on prevention of ventilator-associated pneumonia: a double-blind, randomized, clinical trial. Iranian Red Crescent Medical Journal 2017;19(10):e60576.
Hu 2009 {published data only}
- Hu X, Chen X. Application of improved oral nursing method to orotracheal intubation. Chinese Journal of Misdiagnostics 2009;9(17):4058-9. [Google Scholar]
Irani 2019 {published data only}
- Irani H, Sargazi G, Dahmardeh AR, Mofrad ZP. The effect of oral care with miswak versus chlorhexidine on the incidence of ventilator-associated pneumonia: a clinical trial study. Medical-Surgical Nursing Journal 2019;8(4):e100387. [Google Scholar]
Khaky 2018 {published data only}
- Khaky B, Yazdannik A, Mahjobipoor H. Evaluating the efficacy of nanosil mouthwash on the preventing pulmonary infection in intensive care unit: a randomized clinical trial. Medicinski Arhiv 2018;72:206-9. [DOI] [PMC free article] [PubMed]
Koeman 2006 {published data only}
- *.Koeman M, Van der Ven AJ, Hak E, Joore HC, Kaasjager K, De Smet AG, et al. Oral decontamination with chlorhexidine reduces the incidence of ventilator-associated pneumonia. American Journal of Respiratory & Critical Care Medicine 2006;173(12):1348-55. [DOI] [PubMed] [Google Scholar]
- Koeman M, Van der Ven AJ, Hak E, Joore JC, Kaasjager HA, De Smet AM, et al. Less ventilator-associated pneumonia after oral decontamination with chlorhexidine; a randomised trial. Nederlands Tijdschrift voor Geneeskunde 2008;152(13):752-9. [PubMed] [Google Scholar]
Kusahara 2012a {published data only}
- *.Kusahara DM, Peterlini MA, Pedreira ML. Oral care with 0.12% chlorhexidine for the prevention of ventilator-associated pneumonia in critically ill children: randomised, controlled and double blind trial. International Journal of Nursing Studies 2012;49(11):1354-63. [DOI] [PubMed] [Google Scholar]
- Kusahara DM, Peterlini MAS, Pedreira MLG. Randomized, controlled and double blinded trial of oral decontamination with 0.12% chlorhexidine for the prevention of ventilator-associated pneumonia in children. Pediatric Critical Care Medicine 2011;12(3, Suppl 1):A16. [Google Scholar]
- Pedreira MLG, Kusahara DM, De Carvalho WB, Nunez SC, Peterlini MAS. Oral care interventions and oropharyngeal colonization in children receiving mechanical ventilation. American Journal of Critical Care 2009;18(4):319-29. [DOI] [PubMed] [Google Scholar]
Long 2012 {published data only}
- Long Y, Mou G, Zuo Y, lv F, Feng Q, Du J. Effect of modified oral nursing method on the patients with orotracheal intubation. Journal of Nurses Training 2012;27(24):2290-3. [Google Scholar]
Lorente 2012 {published data only}
- Lorente L, Lecuona M, Jimenez A, Palmero S, Pastor E, Lafuente N, et al. Ventilator-associated pneumonia with or without toothbrushing: a randomized controlled trial. European Journal of Clinical Microbiology and Infectious Diseases 2012;31(10):2621-9. [DOI] [PubMed] [Google Scholar]
Meidani 2018 {published data only}
- Meidani M, Khorvash F, Abbasi S, Cheshmavar M, Tavakoli H. Oropharyngeal irrigation to prevent ventilator-associated-pneumonia: comparing potassium permangenate with chlorhexidine. International Journal of Preventive Medicine 2018;9(1):93. [DOI] [PMC free article] [PubMed]
Meinberg 2012 {published data only}
- Meinberg MC, Cheade M de F, Miranda AL, Fachini MM, Lobo SM. The use of 2% chlorhexidine gel and toothbrushing for oral hygiene of patients receiving mechanical ventilation: effects on ventilator-associated pneumonia [Uso de clorexidina 2% gel e escovacao mecanica na higiene bucal de pacientes sob ventilacao mecanica: efeitos na pneumonia associada a ventilador]. Revista Brasileira de Terapia Intensiva 2012;24(4):369-74. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mo 2016 {published data only}
- Mo ZD, Li XL, Ke JY, Wu JP, Chen XW. Analysis of risk factors in ventilator-associated pneumonia and preventive effect of oral care. Chinese Journal of Nosocomiology 2016;26(3):698-9, 705. [Google Scholar]
Nobahar 2016 {published data only}
- Nobahar M, Razavi Mohammad R, Malek F, Ghorbani R. Effects of hydrogen peroxide mouthwash on preventing ventilator-associated pneumonia in patients admitted to the intensive care unit. Brazilian Journal of Infectious Diseases 2016;20:444-50. [1413-8670] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ozcaka 2012 {published data only}
- Ozcaka O, Basoglu OK, Buduneli N, Tasbakan MS, Bacakoglu F, Kinane DF. Chlorhexidine decreases the risk of ventilator-associated pneumonia in intensive care unit patients: a randomized clinical trial. Journal of Periodontal Research 2012;47(5):584-92. [DOI] [PubMed] [Google Scholar]
Panchabhai 2009 {published data only}
- Panchabhai TS, Dangayach NS, Krishnan A, Kothari VM, Karnad DR. Oropharyngeal cleansing with 0.2% chlorhexidine for prevention of nosocomial pneumonia in critically ill patients: an open-label randomized trial with 0.01% potassium permanganate as control. Chest 2009;135(5):1150-6. [DOI] [PubMed] [Google Scholar]
Pobo 2009 {published data only}
- Pobo A, Lisboa T, Rodriguez A, Sole R, Magret M, Trefler S, et al. A randomized trial of dental brushing for preventing ventilator-associated pneumonia. Chest 2009;136(2):433-9. [DOI] [PubMed] [Google Scholar]
Prendergast 2012 {published data only}
- Prendergast V, Hagell P, Hallberg IR. Electric versus manual tooth brushing among neuroscience ICU patients: is it safe? Neurocritical Care 2011;14(2):281-6. [DOI] [PubMed] [Google Scholar]
- *.Prendergast V, Hallberg IR, Jakobsson U, Renvert S, Moran A, Gonzalez O. Comparison of oropharyngeal and respiratory nosocomial bacteria between two methods of oral care: a randomized controlled trial. Journal of Neuroscience and Neurosurgical Nursing 2012;1(1):10-8. [Google Scholar]
- Prendergast V, Jakobsson U, Renvert S, Hallberg IR. Effects of a standard versus comprehensive oral care protocol among intubated neuroscience ICU patients: results of a randomized controlled trial. Journal of Neuroscience Nursing 2012;44(3):134-46. [DOI] [PubMed] [Google Scholar]
- Prendergast V. Safety and efficacy of oral care for intubated neuroscience intensive care patients. In: Doctoral Dissertation Series 2012-3. Lund, Sweden: Lund University, 2012:1-86. [Google Scholar]
Roca Biosca 2011 {published data only}
- Roca Biosca A, Anguera Saperas L, García Grau N, Rubio Rico L, Velasco Guillén MC. Prevention of mechanical ventilator-associated pneumonia: a comparison of two different oral hygiene methods. Enfermería Intensiva 2011;22(3):104-11. [DOI] [PubMed] [Google Scholar]
Scannapieco 2009 {published data only}
- Scannapieco FA, Yu J, Raghavendran K, Vacanti A, Owens SI, Wood K, et al. A randomized trial of chlorhexidine gluconate on oral bacterial pathogens in mechanically ventilated patients. Critical Care 2009;13(4):R117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seguin 2006 {published data only}
- Seguin P, Tanguy M, Laviolle B, Tirel O, Malledant Y. Effect of oropharyngeal decontamination by povidone-iodine on ventilator-associated pneumonia in patients with head trauma. Critical Care Medicine 2006;34(5):1514-9. [DOI] [PubMed] [Google Scholar]
Seguin 2014 {published data only}
- Seguin P, Laviolle B, Dahyot-Fizelier C, Dumont R, Veber B, Gergaud S, et al. Effect of oropharyngeal povidone-iodine preventive oral care on ventilator-associated pneumonia in severely brain-injured or cerebral hemorrhage patients: a multicenter, randomized controlled trial. Critical Care Medicine 2014;42:1-8. [DOI] [PubMed] [Google Scholar]
Stefanescu 2013 {published data only}
- Stefanescu BM, Hétu C, Slaughter JC, O'Shea TM, Shetty AK. A pilot study of Biotene OralBalance gel for oral care in mechanically ventilated preterm neonates. Contemporary Clinical Trials 2013;35(2):33-9. [DOI] [PubMed] [Google Scholar]
Tang 2013 {published data only}
- Tang J, Chen SL, Deng JL. Efficacy of mouth cavity irrigation in prevention of ventilator-associated pneumonia. Chinese Journal of Nosocomiology 2013;23(17):4119-21. [Google Scholar]
Tantipong 2008 {published data only}
- Silvestri L, Van Saene HK, Milanese M, Zei E, Blazic M. Prevention of ventilator-associated pneumonia by use of oral chlorhexidine. Infection Control & Hospital Epidemiology 2009;30(1):101-3. [DOI] [PubMed] [Google Scholar]
- *.Tantipong H, Morkchareonpong C, Jaiyindee S, Thamlikitkul V. Randomized controlled trial and meta-analysis of oral decontamination with 2% chlorhexidine solution for the prevention of ventilator-associated pneumonia. Infection Control & Hospital Epidemiology 2008;29(2):131-6. [DOI] [PubMed] [Google Scholar]
Tuon 2017 {published data only}
- Tuon FF, Gavrilko O, Almeida S, Sumi ER, Alberto T, Rocha JL, et al. Prospective, randomised, controlled study evaluating early modification of oral microbiota following admission to the intensive care unit and oral hygiene with chlorhexidine. Journal of Global Antimicrobial Resistance 2017;8:159-63. [DOI] [PubMed] [Google Scholar]
Xu 2007 {published data only}
- Xu J, Feng B, He L, Shen H, Chen XY. Influence of different oral nursing methods on ventilator-associated pneumonia and oral infection in the patients undergoing mechanical ventilation. Journal of Nursing Science 2007;7(22):56-7. [Google Scholar]
Xu 2008 {published data only}
- Xu HL. Application of improved oral nursing method to the prevention of ventilator-associated pneumonia. Journal of Qilu Nursing 2008;14(19):15-6. [Google Scholar]
Yao 2011 {published data only}
- Yao L, Chang C, Wang C, Chen C. Effect of an oral care protocol in preventing ventilator associated pneumonia in ICU patients. Critical Care 2008;12(Suppl 2):Abs No P48. [Google Scholar]
- *.Yao LY, Chang CK, Maa SH, Wang C, Chen CC. Brushing teeth with purified water to reduce ventilator-associated pneumonia. Journal of Nursing Research 2011;19(4):289-97. [DOI] [PubMed] [Google Scholar]
Zhao 2012 {published data only}
- Zhao Y. Research on application of Yikou gargle in prevention of ventilation associated pneumonia. Chinese Journal of Nosocomiology 2012;23(22):5232-3. [Google Scholar]
References to studies excluded from this review
Abusibeih 2010 {published data only}
- Abusibeih A, Lev A. Randomized control trial comparing oral care methods and VAP. Intensive Care Medicine 2010;36:S329. [Google Scholar]
Anon 2012 {published data only}
- Anon. EB57 Development of an oral care-based programme for prevention of ventilator-associated pneumonia. Critical Care Nurse 2012;32(2):e34. [Google Scholar]
Atashi 2018 {published data only}
- Atashi V, Yousefi H, Mahjobipoor H, Bekhradi R, Yazdannik A. Effect of oral care program on prevention of ventilator-associated pneumonia in intensive care unit patients: a randomized controlled trial. Iranian Journal of Nursing and Midwifery Research 2018;23(6):486-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baradari 2012 {published data only}
- Baradari AG, Khezri HD, Arabi S. Comparison of antibacterial effects of oral rinses chlorhexidine and herbal mouth wash in patients admitted to intensive care unit. Bratislavske Lekarske Listy 2012;113(9):556-60. [DOI] [PubMed] [Google Scholar]
Bellissimo‐Rodrigues 2014 {published data only}
- Bellissimo-Rodrigues WT, Menegueti MG, Gaspar GG, Nicolini EA, Auxiliadora-Martins M, Basile-Filho A, et al. Effectiveness of a dental care intervention in the prevention of lower respiratory tract nosocomial infections among intensive care patients: a randomized clinical trial. Infection Control and Hospital Epidemiology 2014;35(11):1342-8. [DOI] [PubMed]
Bordenave 2011 {published data only}
- Bordenave C. Evaluation of the effectiveness of a protocol of intensification of mouth care (teeth brushing and chlorhexidine 0.12%) on the colonisation of tracheal aspirations in intubated and ventilated patients in intensive care. Recherche en Soins Infirmiers 2011;2011(106):92-8. [PubMed] [Google Scholar]
Buckley 2013 {published data only}
- Buckley MS, Dzierba AL, Smithburger PL, McAllen KJ, Jordan CJ, Kane-Gill SL. Chlorhexidine for the prevention of ventilator associated pneumonia in critically ill adults. Journal of Infection Prevention 2013;14:162-9. [Google Scholar]
Chao 2009 {published data only}
- Chao YC, Chen Y, Wang KK, Lee R, Tsai H. Removal of oral secretion prior to position change can reduce the incidence of ventilator-associated pneumonia for adult ICU patients: a clinical controlled trial study. Journal of Clinical Nursing 2009;18(1):22-8. [DOI] [PubMed] [Google Scholar]
Chen 2008 {published data only}
- Chen QL, Ye XF, Jiang YZ, Yan MQ. Application of new oral care method to orotracheal intubation. Fujian Medical Journal 2008;30(5):155-7. [Google Scholar]
Da Collina 2017 {published data only}
- Da Collina GA, Tempestini-Horliana ACR, Da Silva DFT, Longo PL, Makabe MLF, Pavani C. Oral hygiene in intensive care unit patients with photodynamic therapy: study protocol for randomised controlled trial. Trials [electronic resource] 2017;18:385. [DOI] [PMC free article] [PubMed]
Dale 2019 {published data only}
- Dale CM, Rose L, Carbone S, Smith OM, Burry L, Fan E, et al. Protocol for a multi-centered, stepped wedge, cluster randomized controlled trial of the de-adoption of oral chlorhexidine prophylaxis and implementation of an oral care bundle for mechanically ventilated critically ill patients: the CHORAL study. Trials 2019;20(1):603. [DOI] [PMC free article] [PubMed]
Darnell 2015 {published data only}
- Darnell J. EB44 TMI: Reducing ventilator-associated pneumonia in the surgical intensive care unit. Critical Care Nurse 2015;35:e20. [Google Scholar]
DeRiso 1996 {published data only}
- DeRiso AJ 2nd, Ladowski JS, Dillon TA, Justice JW, Peterson AC. Chlorhexidine gluconate 0.12% oral rinse reduces the incidence of total nosocomial respiratory infection and nonprophylactic systemic antibiotic use in patients undergoing heart surgery. Chest 1996;109(6):1556-61. [DOI] [PubMed] [Google Scholar]
Epstein 1994 {published data only}
- Epstein J, Ransier A, Lunn R, Spinelli J. Enhancing the effect of oral hygiene with the use of a foam brush with chlorhexidine. Oral Surgery, Oral Medicine, Oral Pathology 1994;77(3):242-7. [DOI] [PubMed] [Google Scholar]
Fan 2012 {published data only}
- Fan T. The effect of a modified oral nursing care method on prevention of ventilator associated pneumonia. Nursing Practice and Research 2012;9(12):99-100. [Google Scholar]
Fan 2015 {published data only}
- Fan YL, Chang QF, Zhang L. Research of oropharyngeal cleaning methods for ventilator associated pneumonia. Chinese Journal of Nosocomiology 2015;25(12):2777-9. [Google Scholar]
Ferozali 2007 {published data only}
- Ferozali F, Johnson G, Cavagnaro A. Health benefits and reductions in bacteria from enhanced oral care. Special Care in Dentistry 2007;27(5):168-76. [DOI] [PubMed] [Google Scholar]
Fourrier 2000 {published data only}
- Fourrier F, Cau-Pottier E, Boutigny H, Roussel-Delvallez M, Jourdain M, Chopin C. Effects of dental plaque antiseptic decontamination on bacterial colonization and nosocomial infections in critically ill patients. Intensive Care Medicine 2000;26(9):1239-47. [DOI] [PubMed] [Google Scholar]
Fourrier 2005 {published data only}
- Fourrier F, Dubois D, Pronnier P, Herbecq P, Leroy O, Desmettre T, et al. Effect of gingival and dental plaque antiseptic decontamination on nosocomial infections acquired in the intensive care unit: a double-blind placebo-controlled multicenter study. Critical Care Medicine 2005;33(8):1728-35. [DOI] [PubMed] [Google Scholar]
Genuit 2001 {published data only}
- Genuit T, Bochicchio G, Napolitano LM, McCarter RJ, Roghman MC. Prophylactic chlorhexidine oral rinse decreases ventilator-associated pneumonia in surgical ICU patients. Surgical Infections 2001;2(1):5-18. [DOI] [PubMed] [Google Scholar]
Grap 2004 {published data only}
- Grap MJ, Munro CL, Elswick RK Jr, Sessler CN, Ward KR. Duration of action of a single, early oral application of chlorhexidine on oral microbial flora in mechanically ventilated patients: a pilot study. Heart & Lung 2004;33(2):83-91. [DOI] [PubMed] [Google Scholar]
Gu 2013 {published data only}
- Gu WJ, Liu JC. Toothbrushing for critically ill mechanically ventilated patients: a duplicated trial included? Critical Care Medicine 2013;41(7):e137-8. [DOI] [PubMed] [Google Scholar]
Guo 2007 {published data only}
- Guo MJ. Study on the new oral nursing for the patient of acute lung brain-storm through tracheal. Chinese Journal of Mordern Nursing 2007;13(26):2537-8. [Google Scholar]
Guo 2017 {published data only}
- Guo S, Xie L, Chen K, Ke C, Dai D, Zhang X, et al. The effects of oral care using hydrogen peroxide combined with sodium bicarbonate on neonatal ventilator associated pneumonia. Chinese Journal of Nursing 2017;52(6):645-8. [Google Scholar]
Haghighi 2017 {published data only}
Houston 2002 {published data only}
- Houston S, Hougland P, Anderson JJ, LaRocco M, Kennedy V, Gentry LO. Effectiveness of 0.12% chlorhexidine gluconate oral rinse in reducing prevalence of nosocomial pneumonia in patients undergoing heart surgery. American Journal of Critical Care 2002;11(6):567-70. [PubMed] [Google Scholar]
Jacomo 2011 {published data only}
- Jacomo AD, Carmona F, Matsuno AK, Manso PH, Carlotti AP. Effect of oral hygiene with 0.12% chlorhexidine gluconate on the incidence of nosocomial pneumonia in children undergoing cardiac surgery. Infection Control & Hospital Epidemiology 2011;32(6):591-6. [DOI] [PubMed] [Google Scholar]
Jafari 2007 {published data only}
- Jafari S, Ranjbar H, Kamrani F, Alavi-Majd H, Yaghmaei F. Effects of chlorhexidine and normal saline on dental plaque formation in ICU patients: a comparative study. Journal of Nurse Midwifery 2007;17(56):36-43. [Google Scholar]
Kusahara 2012b {published data only}
- Kusahara DM, Friedlander LT, Peterlini MAS, Pedreira MLG. Oral care and oropharyngeal and tracheal colonization by Gram-negative pathogens in children. Nursing in Critical Care 2012;17:115-22. [DOI] [PubMed] [Google Scholar]
Labeau 2013 {published data only}
- Labeau SO, Blot SI. Oral care for mechanically ventilated patients involving toothbrushing. Critical Care Medicine 2013;41(7):e136-7. [DOI] [PubMed] [Google Scholar]
Lai 1997 {published data only}
- Lai M, Huang H. Toothpaste mouth care for critically ill patients. Journal of Nursing Science 1997;12(2):106-7. [Google Scholar]
Li 2011 {published data only}
- Li W, Ma X, Peng Y, Cao J, Loo WTY, Hao L, et al. Application of a nano-antimicrobial film to prevent ventilator-associated pneumonia: a pilot study. African Journal of Biotechnology 2011;10(10):1926-31. [Google Scholar]
Li 2012 {published data only}
- Li S, Zhang H, Zhang B. Application of different oral nursing methods to prevent ventilation associated pneumonia. Practical Clinical Medicine 2012;13(5):92-3. [Google Scholar]
Liang 2007 {published data only}
- Liang YL, Lu LQ, Liang JT. Oral cavity nursing study in endotracheal intubation with the Baihu decoction. Journal of Nurses Training 2007;1(22):79-80. [Google Scholar]
Liao 2015 {published data only}
- Liao YM, Tsai JR, Chou FH. The effectiveness of an oral health care program for preventing ventilator-associated pneumonia. Nursing in Critical Care 2015;20(2):89-97. [DOI] [PubMed] [Google Scholar]
Liwu 1990 {published data only}
- Liwu A. Oral hygiene in intubated patients. Australian Journal of Advanced Nursing 1990;7(2):4-7. [PubMed] [Google Scholar]
MacNaughton 2004 {published data only}
- MacNaughton PD, Bailey J, Donlin N, Branfield P, Williams A, Rowswell H. A randomised controlled trial assessing the efficacy of oral chlorhexidine in ventilated patients (029). Intensive Care Medicine 2004;30(Suppl):S12. [Google Scholar]
Maury 2015 {published data only}
- Maury E, London J, Offenstadt G. Community-acquired pneumonia. New England Journal of Medicine 2015;372(3):292. [DOI] [PubMed] [Google Scholar]
McCartt 2010 {published data only}
- McCartt PAM. Effect of Chlorhexidine Oral Spray versus Mechanical Toothbrushing and Chlorhexindine Rinse in Decreasing Ventilator Associated Pneumonia in Critically Ill Adults [PhD thesis]. Gainesville, Florida, USA: University of Florida, 2010. [Google Scholar]
McCoy 2012 {published data only}
- McCoy T, Fields W, Kent N. Evaluation of emergency department evidence-based practices to prevent the incidence of ventilator-acquired pneumonia. Journal of Nursing Care Quality 2012;27(1):83-8. [DOI] [PubMed] [Google Scholar]
Munro 2009 {published data only}
- Munro C, Grap M, Sessler C, McClish D. Effect of oral care interventions on dental plaque in mechanically ventilated ICU adults. American Journal of Critical Care 2007;16(3):309. [Google Scholar]
- *.Munro CL, Grap MJ, Jones DJ, McClish DK, Sessler CN. Chlorhexidine, toothbrushing, and preventing ventilator-associated pneumonia in critically ill adults. American Journal of Critical Care 2009;18(5):428-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Munro 2015 {published data only}
- Munro CL, Grap MJ, Sessler CN, Elswick RK Jr, Mangar D, Karlnoski-Everall R, et al. Preintubation application of oral chlorhexidine does not provide additional benefit in prevention of early-onset ventilator-associated pneumonia. Chest 2015;147(2):328-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nasiriani 2016 {published data only}
- Nasiriani K, Torki F, Jarahzadeh MH, Rashidi Maybodi F. The effect of brushing with a soft toothbrush and distilled water on the incidence of ventilator-associated pneumonia in the intensive care unit. Tanaffos 2016;15:101-7. [1735-0344: (Print) // 1735-0344 (Linking)] [PMC free article] [PubMed] [Google Scholar]
NCT01657396 {unpublished data only}
- NCT01657396. Implementation and evaluaion of revised protocols for oral hygiene for mechanically ventilated patients [Implementation and evaluation of revised protocols for oral hygiene for mechanically ventilated patients in Alberta Health Services Calgary Region - a pilot project.]. www.clinicaltrials.gov/ct2/show/NCT01657396?term=01657396&draw=1&rank=1 (first received 6 August 2012).
Needleman 2011 {published data only}
- Needleman IG, Hirsch NP, Leemans M, Moles DR, Wilson M, Ready DR, et al. Randomized controlled trial of toothbrushing to reduce ventilator-associated pneumonia pathogens and dental plaque in a critical care unit. Journal of Clinical Periodontology 2011;38(3):246-52. [DOI] [PubMed] [Google Scholar]
Ogata 2004 {published data only}
- Ogata J, Minami K, Miyamoto H, Horishita T, Ogawa M, Sata T, et al. Gargling with povidone-iodine reduces the transport of bacteria during oral intubation. Canadian Journal of Anaesthesia 2004;51(9):932-6. [DOI] [PubMed] [Google Scholar]
Pawlak 2005 {published data only}
- Pawlak D, Semar R, Cantos K. Improving frequency of oral care in the medical intensive care unit. American Journal of Infection Control 2005;33(5):E147. [Google Scholar]
Pelucchi 2013 {published data only}
- Pelucchi G, Ciucur M, Giacovelli M, Lucchini A, Luongo M. Oral hygiene [L'igiene del cavo orale]. SCENARIO: Official Italian Journal of ANIARTI 2013;30:23-34. [Google Scholar]
Pivkina 2014 {published data only}
- Pivkina AI, Gusarov VG, Zhivotneva IV, Bodunova GE. Oral care in ventilated patients - can we improve it? Intensive Care Medicine 2014;40:S28. [Google Scholar]
Sands 2015 {published data only}
- Sands KM, Twigg JA, Wise MP. Oral hygiene with chlorhexidine in critically ill patients. JAMA Internal Medicine 2015;175(2):316. [DOI] [PubMed] [Google Scholar]
Santos 2008 {published data only}
- Santos PS, Mello WR, Wakim RCS, Paschoal MG. Use of oral rinse with enzymatic system in patients totally dependent in the intensive care unit [Uso de solução bucal com sistema enzimático em pacientes totalmente dependentes de cuidados em unidade de terapia intensiva]. Revista Brasileira de Terapia Intensiva 2008;20(2):154-9. [PubMed] [Google Scholar]
Sebastian 2012 {published data only}
- Sebastian MR, Lodha R, Kapil A, Kabra SK. Oral mucosal decontamination with chlorhexidine for the prevention of ventilator-associated pneumonia in children - a randomized, controlled trial. Pediatric Critical Care Medicine 2012;13(5):e305-10. [DOI] [PubMed] [Google Scholar]
Segers 2006 {published data only}
- Segers P, Speekenbrink RG, Ubbink DT, Van Ogtrop ML, De Mol BA. Prevention of nosocomial infection in cardiac surgery by decontamination of the nasopharynx and oropharynx with chlorhexidine gluconate: a randomized controlled trial. JAMA 2006;296(20):2460-6. [DOI] [PubMed] [Google Scholar]
Seo 2011 {published data only}
- Seo HK, Choi EH, Kim JH. The effect of oral hygiene for ventilator-associated pneumonia (VAP) incidence. Journal of Korean Critical Care Nursing 2011;4(2):1. [Google Scholar]
Swartz 2015 {published data only}
- Swartz AW. Community-acquired pneumonia. New England Journal of Medicine 2015;372(3):293. [DOI] [PubMed] [Google Scholar]
Tattevin 2015 {published data only}
- Tattevin P, Levy HG, Gould IM. Community-acquired pneumonia. New England Journal of Medicine 2015;372(3):293. [DOI] [PubMed] [Google Scholar]
Tian 2017 {published data only}
- Tian L, Zhu R, Peng Z, Zhao X, Yu Z, Gu Y, et al. Impact of oral care with biological enzyme disinfectants on ventilator-asociated pneumonia in mechanical ventilation patients. Chinese Journal of Nosocomiology 2017;27(1):101-4, 108. [Google Scholar]
Tsai 2017 {published data only}
- Tsai HL, Cheng CJ, Yu CY, Lin HC, Chen CH, Lee LC, et al. The effectiveness of the use of chlorhexidine oral rinse to prevent respiratory-related pneumonia infection. International Journal of Antimicrobial Agents 2017;50:S239.
Ueda 2004 {published data only}
- Ueda K, Yamada Y, Toyosato A, Nomura S, Saitho E. Effects of functional training of dysphagia to prevent pneumonia for patients on tube feeding. Gerodontology 2004;21(2):108-11. [DOI] [PubMed] [Google Scholar]
Wang 2006 {published data only}
- Wang MM. The improvement of oral care in ICU intubated patients. Journal of Mudanjiang Medical College 2006;27(5):80-1. [Google Scholar]
Wang 2012 {published data only}
- Wang YX, He LY, Gao MR, Wang ZW, Li XY. Application of oral nursing care bundle to prevent VAP for critically surgically ill patients. Chinese Archives of General Surgery 2012;6(5):448-50. [Google Scholar]
Wang 2016 {published data only}
- Wang N, Lu B, Yang W, Xu D. ICU patients in clinical studies of oral care solution to reduce lung infection. Chinese Journal of Nosocomiology 2016;26(14):3342-4. [Google Scholar]
Yin 2004 {published data only}
- Yin XR, Liao Y. The improvement of the oral care for patients with orotracheal intubation. West China Medical Journal 2004;19(3):482. [Google Scholar]
Yun 2011 {published data only}
- Yun HY, Lee ES, Kim JY, Kim HS, Kim KA, Kim ES, et al. Effect of tooth-brushing on oral health and ventilator-associated pneumonia of critically ill patients. Journal of Korean Critical Care Nursing 2011;4(2):1. [Google Scholar]
Zouka 2010 {published data only}
- Zouka M, Soultati I, Hari H, Pourzitaki C, Paroutsidou G, Thomaidou E, et al. Oral dental hygiene and ventilator-associated pneumonia prevention in an ICU setting: comparison between two methods (preliminary data of a randomised prospective study). Intensive Care Medicine 2010;36:S103. [Google Scholar]
References to studies awaiting assessment
Chacko 2017 {published data only}
- Chacko R, Rajan A, Lionel P, Thilagavathi M, Yadav B, Premkumar J. Oral decontamination techniques and ventilator-associated pneumonia. British Journal of Nursing 2017;26:594-9. [DOI] [PubMed] [Google Scholar]
Hashemi 2018 {published data only}
- Hashemi ST, Alikiaii B, Ali Fallah-Medvari M, Karimi F, Fallah-Medvari A. Comparison of effects of chlorhexidine mouthwash versus stop-snoring mouthwash in prevention of ventilator-associated pneumonia. Journal of Isfahan Medical School 2018;36:227-32. [Google Scholar]
Hashemi 2019 {published data only}
- Hashemi ST, Alikiaii B, Fallah Medvari MA, Karimi F, Fallah Medvari A. Comparison of effects of chlorhexidine mouthwash with herbal cinnamol mouthwash on prevention of ventilator associated pneumonia. Medical Journal of Tabriz University of Medical Sciences and Health Services 2020;41(6):91-7. [Google Scholar]
IRCT20110427006318N12 {published data only}
- IRCT20110427006318N12. Effect of propolis mouthwash on incidence of pneumonia in hospitalized patient in critical care unit [Effect of propolis mouthwash on incidence of ventilator-associated pneumonia in hospitalized patient in critical care unit]. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20110427006318N12 (first received 2 April 2019).
IRCT2013050813278N1 {published data only}
- IRCT2013050813278N1. The effect of oral care on pulmonary infection in intensive care unit [Comparison of two methods of oral care on oral health and the prevention of ventilator-associated pneumonia in mechanically ventilated patients in intensive care unit]. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2013050813278N1 (first received 25 May 2013).
IRCT201512115363N8 {published data only}
- IRCT201512115363N8. Effect of damask rose extract in the prevention of ventilator-associated pneumonia [Clinical trial to compare the effect of damask rose extract and chlorhexidine in prevention of ventilator-associated pneumonia in critically ill patients]. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT201512115363N8 (first received 4 December 2016).
IRCT2016052828134N1 {published data only}
- IRCT2016052828134N1. Effects of botanical mouthwash of aloe vera on ventilator associated pneumonia of patients having endotracheal tube hospitalized in the intensive care unit. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2016052828134N1 (first received 21 June 2016).
IRCT2017022032676N1 {published data only}
- IRCT2017022032676N1. Comparing the effect of persica and chlorhexidine on the prevention of ventilator associated pneumonia in patient admitted in ICU [Effect of persica and chlorhexidine on the prevention of ventilator associated pneumonia]. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2017022032676N1 (first received 22 April 2017).
IRCT2017050727819N4 {published data only}
- IRCT2017050727819N4. The effects of mouthwash on prevention of pneumonia [The comparison of the effects of orthodentol and chlorhexidine mouthwash on prevention of ventilator associated pneumonia in mechanically ventilated patients]. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2017050727819N4 (first received 26 June 2017).
IRCT20171225038053N1 {published data only}
- IRCT20171225038053N1. Effect of two methods mouth wash (chlorhexidine and chlorhexidine combined with hydrogen peroxide solution) on frequency of oral plaques and ventilator-associated pneumonia in patients undergoing mechanical ventilation [Comparison of the effect of two methods mouth wash (chlorhexidine and chlorhexidine combined with hydrogen peroxide solution) on frequency of oral plaques and ventilator-associated pneumonia in patients undergoing mechanical ventilation in the intensive care unit of Imam Khomeini Educational Center, Urmia, 2017-18]. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20171225038053N1 (first received 9 September 2018).
IRCT20180520039739N2 {published data only}
- IRCT20180520039739N2. Evaluation of effect of chlorhexidine on prevention of ventilator associated pneumonia [Comparison of the effect of Chlorhexidine mouthwash with Dine mouthwash on prevention of ventilator-associated pneumonia in pediatric intensive care unit]. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20180520039739N2 (first received 26 November 2018).
IRCT20191012045066N1 {published data only}
- IRCT20191012045066N1. The effects of oral care program on oropharyngeal complications and the occurrence of ventilator associated pneumonia [Evaluation and comparison of the effects of three oral care programs on oropharyngeal complications and the occurrence of ventilator associated pneumonia in patients undergoing mechanical ventilation]. www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20191012045066N1 (first received 7 November 2019).
Jamshidi 2016 {published data only}
- Jamshidi MR, Qatreh Samany F, Goli Farhood G, Qodrati S, Falakaflaki B. Evaluating the effect of chlorhexidine and tooth brushing in preventing the ventilator associated pneumonia. Journal of Zanjan University of Medical Sciences and Health Services 2016;24(105):9-17. [Google Scholar]
Mehrabadi 2015 {published data only}
- Gholami Mehrabadi M, Khosravi SH, Rezaie K, Malekianzadeh B, Ghorbanpour M, Moslemi A, et al. The effect of Echinacea mouthwash on ventilator associated pneumonia in patients in intensive care units. Medical-Surgical Nursing Journal 2015;4(3):13-20. [Google Scholar]
References to ongoing studies
RBR‐7p6568 {published data only}
- RBR-7p6568. Oral hygiene in critically ill patients [Oral hygiene in critically ill patients - a randomized controlled trial]. www.who.int/trialsearch/Trial2.aspx?TrialID=RBR-7p6568 (first received 8 October 2019).
TCTR20190530003 {published data only}
- TCTR20190530003. Efficacy of moraceae with chlorhexidine mouthwash on microbial flora of critically ill intubated patients [Efficacy of moraceae with chlorhexidine mouthwash on microbial flora of critically ill intubated patients: a randomized controlled pilot study]. www.who.int/trialsearch/Trial2.aspx?TrialID=TCTR20190530003 (first received 29 May 2019). [DOI] [PMC free article] [PubMed]
Additional references
Alhazzani 2013
- Alhazzani W, Smith O, Muscedere J, Medd J, Cook D. Toothbrushing for critically ill mechanically ventilated patients: a systematic review and meta-analysis of randomized trials evaluating ventilator-associated pneumonia. Critical Care Medicine 2013;41(2):646-55. [DOI] [PubMed] [Google Scholar]
Apostolopoulou 2003
- Apostolopoulou E, Bakakos P, Katostaras T, Gregorakos L. Incidence and risk factors for ventilator-associated pneumonia in 4 multidisciplinary intensive care units in Athens. Respiratory Care 2003;48(7):681-8. [PubMed] [Google Scholar]
Arthur 2016
- Arthur LE, Kizor RS, Selim AG, Van Driel ML, Seoane L. Antibiotics for ventilator-associated pneumonia. Cochrane Database of Systematic Reviews 2016, Issue 10. Art. No: CD004267. [DOI: 10.1002/14651858.CD004267.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
ATS Guideline 2005
- American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. American Journal of Respiratory and Critical Care Medicine 2005;171(4):388-416. [DOI] [PubMed] [Google Scholar]
Azoulay 2006
- Azoulay E, Timsit JF, Tafflet M, De Lassence A, Darmon M, Zahar JR, et al. Candida colonization of the respiratory tract and subsequent pseudomonas ventilator-associated pneumonia. Chest 2006;129(1):110-7. [DOI] [PubMed] [Google Scholar]
Berry 2007
- Berry AM, Davidson PM, Masters J, Rolls K. Systematic literature review of oral hygiene practices for intensive care patients receiving mechanical ventilation. American Journal of Critical Care 2007;16(6):552-62. [PubMed] [Google Scholar]
Bo 2014
- Bo L, Li J, Tao T, Bai Y, Ye X, Hotchkiss RS, et al. Probiotics for preventing ventilator-associated pneumonia. Cochrane Database of Systematic Reviews 2014, Issue 10. Art. No: CD009066. [DOI: 10.1002/14651858.CD009066.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
CONSORT 2012
- Altman DG, Moher D, Schultz KF. Improving the reporting of randomised trials: the CONSORT statement and beyond. Statistics in Medicine 2012;31(25):2985-97. [DOI] [PubMed] [Google Scholar]
Contentin 2014
- Contentin L, Ehrmann S, Giraudeau B. Heterogeneity in the definition of mechanical ventilation duration and ventilator-free days. American Journal of Respiratory and Critical Care Medicine 2014;189(8):998-1002. [DOI] [PubMed] [Google Scholar]
Cook 1998
- Cook DJ, Walter SD, Cook RJ, Griffith LE, Guyatt GH, Leasa D, et al. Incidence of and risk factors for ventilator-associated pneumonia in critically ill patients. Annals of Internal Medicine 1998;29(6):433-46. [DOI] [PubMed] [Google Scholar]
D'Amico 2009
- D'Amico R, Pifferi S, Torri V, Brazzi L, Parmelli E, Liberati A. Antibiotic prophylaxis to reduce respiratory tract infections and mortality in adults receiving intensive care. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No: CD000022. [DOI: 10.1002/14651858.CD000022.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ding 2017
- Ding C, Zhang Y, Yang Z, Wang J, Jin A, Wang W, et al. Incidence, temporal trend and factors associated with ventilator-associated pneumonia in mainland China: a systematic review and meta-analysis. BMC Infectious Diseases 2017;17(1):468. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fourrier 1998
- Fourrier F, Duvivier B, Boutigny H, Roussel-Delvallez M, Chopin C. Colonization of dental plaque: a source of nosocomial infections in intensive care unit patients. Critical Care Medicine 1998;26(2):301-8. [DOI] [PubMed] [Google Scholar]
GRADEpro 2020 [Computer program]
- GRADEpro GDT: GRADEpro Guideline Development Tool. Grade Working Group. McMaster University, 2020.
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gyssens 2011
- Gyssens IC. Antibiotic policy. International Journal of Antimicrobial Agents 2011;38 Suppl:11-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hao 2015
- Hao Q, Dong BR, Wu T. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database of Systematic Reviews 2015, Issue 2. Art. No: CD006895. [DOI: 10.1002/14651858.CD006895.pub3] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Horan 2008
- Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. American Journal of Infection Control 2008;36(5):309-32. [DOI] [PubMed] [Google Scholar]
Khasanah 2019
- Khasanah IH, Sae-Sia W, Damkliang J. The effectiveness of oral care guideline implementation on oral health status in critically ill patients. SAGE Open Nursing 2019;5:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klompas 2007
- Klompas M. Does this patient have ventilator-associated pneumonia? JAMA 2007;297(14):1583-93. [DOI] [PubMed] [Google Scholar]
Klompas 2014
- Klompas M, Speck K, Howell MD, Greene LR, Berenholtz SM. Reappraisal of routine oral care with chlorhexidine gluconate for patients receiving mechanical ventilation: systematic review and meta-analysis. JAMA Internal Medicine 2014;174(5):751-61. [DOI: 10.1001/jamainternmed.2014.359.] [DOI] [PubMed] [Google Scholar]
Labeau 2011
- Labeau SO, Van de Vyver K, Brusselaers N, Vogelaers D, Blot SI. Prevention of ventilator-associated pneumonia with oral antiseptics: a systematic review and meta-analysis. Lancet Infectious Diseases 2011;11(11):845-54. [DOI] [PubMed] [Google Scholar]
La Combe 2018
- La Combe B, Bleibtreu A, Messika J, Fernandes R, Clermont O, Branger C, et al. Decreased susceptibility to chlorhexidine affects a quarter of Escherichia coli isolates responsible for pneumonia in ICU patients. Intensive Care Medicine 2018;44(4):531-3. [DOI] [PubMed] [Google Scholar]
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Technical Supplement to Chapter 4: Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, Welch VA (eds). Cochrane Handbook for Systematic Reviews of Interventions, Version 6. Cochrane, 2019. Available from: www.training.cochrane.org/handbook.
Li 2020
- Li Y, Liu C, Xiao W, Song T, Wang S. Incidence, risk factors, and outcomes of ventilator-associated pneumonia in traumatic brain injury: a meta-analysis. Neurocritical Care 2020;32(1):272-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marsh 2010
- Marsh PD. Microbiology of dental plaque biofilms and their role in oral health and caries. Dental Clinics of North America 2010;54(3):441-54. [DOI] [PubMed] [Google Scholar]
Martin‐Loeches 2018
- Martin-Loeches I, Rodriguez AH, Torres A. New guidelines for hospital-acquired pneumonia/ventilator-associated pneumonia: USA vs. Europe. Current Opinion in Critical Care 2018;24(5):347-52. [DOI] [PubMed] [Google Scholar]
McCarney 2007
- McCarney R, Warner J, Iliffe S, Van Haselen R, Griffin M, Fisher P. The Hawthorne Effect: a randomised, controlled trial. BMC Medical Research Methodology 2007;7:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Melsen 2013
- Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infectious Diseases 2013;13(8):665-71. [DOI] [PubMed] [Google Scholar]
Mojon 2002
- Mojon P. Oral health and respiratory infection. Journal of the Canadian Dental Association 2002;68(6):340-6. [PubMed] [Google Scholar]
Muscedere 2008
- Muscedere J, Dodek P, Keenan S, Fowler R, Cook D, Heyland D. Comprehensive evidence-based clinical practice guidelines for ventilator-associated pneumonia: prevention. Journal of Critical Care 2008;23(1):126-37. [DOI] [PubMed] [Google Scholar]
Pemberton 2012
- Pemberton MN, Gibson J. Chlorhexidine and hypersensitivity reactions in dentistry. British Dental Journal 2012;213(11):547-50. [DOI] [PubMed] [Google Scholar]
Pineda 2006
- Pineda LA, Saliba RG, El Solh AA. Effect of oral decontamination with chlorhexidine on the incidence of nosocomial pneumonia: a meta-analysis. Critical Care 2006;10(1):R35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Plantinga 2016
- Plantinga NL, Wittekamp BHJ, Leleu K, Depuydt P, Van den Abeele AM, Brun-Buisson C, et al. Oral mucosal adverse events with chlorhexidine 2% mouthwash in ICU. Intensive Care Medicine 2016;42(4):620-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Price 2014
- Price R, MacLennan G, Glen J, SuDDICU Collaboration. Selective digestive or oropharyngeal decontamination and topical oropharyngeal chlorhexidine for preventionof death in general intensive care: systematic review and network meta-analysis. BMJ 2014;348:g2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pugin 1991
- Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic 'blind' bronchoalveolar lavage fluid. American Review of Respiratory Disease 1991;143(5 Pt 1):1121-9. [DOI] [PubMed] [Google Scholar]
Roberts 2017
- Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database of Systematic Reviews 2017, Issue 3. Art. No: CD004454. [DOI: 10.1002/14651858.CD004454.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sachdev 2013
- Sachdev M, Ready D, Brealey D, Ryu J, Bercades G, Nagle J, et al. Changes in dental plaque following hospitalisation in a critical care unit: an observational study. Critical Care 2013;17(5):R189. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sands 2016
- Sands KM, Twigg JA, Lewis MAO, Wise MP, Marchesi JR, Smith A, et al. Microbial profiling of dental plaque from mechanically ventilated patients. Journal of Medical Microbiology 2016;65(2):147-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scannapieco 1992
- Scannapieco FA, Stewart EM, Mylotte JM. Colonization of dental plaque by respiratory pathogens in medical intensive care patients. Critical Care Medicine 1992;20(6):740-5. [DOI] [PubMed] [Google Scholar]
Schulz 2002
- Schulz KF, Grimes DA. Generation of allocation sequences in randomised trials: chance, not choice. Lancet 2002;359(9305):515-9. [DOI] [PubMed] [Google Scholar]
Shi 2004
- Shi ZD, Yu JR, Luo R, He Y, Liu XC, Chen E. Effect of oral nursing care: a systematic review. Chinese Journal of Evidence Based Medicine 2004;4(12):837-46, 858. [Google Scholar]
Silness 1964
- Silness J, Loe H. Periodontal disease in pregnancy. Correlation between oral hygiene and periodontal condition. Acta odontologica Scandinavica 1964;22:121-35. [DOI] [PubMed] [Google Scholar]
Tablan 2004
- Tablan OC, Anderson L, Besser R, Bridges C, Hajjeh R. Guidelines for preventing healthcare-associated pneumonia: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. Morbidity & Mortality Weekly Report. Recommendations & Reports 2004;55 (RR-3):1-36. [PubMed] [Google Scholar]
Terezakis 2011
- Terezakis E, Needleman I, Kumar N, Moles D, Agudo E. The impact of hospitalization on oral health: a systematic review. Journal of Clinical Periodontology 2011;38(7):628-36. [DOI] [PubMed] [Google Scholar]
Terpenning 2005
- Terpenning M. Geriatric oral health and pneumonia risk. Clinical Infectious Diseases 2005;40(12):1807-10. [DOI] [PubMed] [Google Scholar]
Torres 2017
- Torres A, Niederman MS, Chastre J, Ewig S, Fernandez-Vandellos P, Hanberger H, et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: Guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociación Latinoamericana del Tórax (ALAT). European Respiratory Journal 2017;50(3):1700582. [DOI] [PubMed] [Google Scholar]
Waters 2015
- Waters B, Muscedere J. A 2015 update on ventilator-associated pneumonia: new insights on its prevention, diagnosis, and treatment. Current Infectious Disease Reports 2015;17(8):1-9. [DOI] [PubMed] [Google Scholar]
Whittaker 1996
- Whittaker CJ, Klier CM, Kolenbrander PE. Mechanisms of adhesion by oral bacteria. Annual Review of Microbiology 1996;50:513-52. [DOI] [PubMed] [Google Scholar]
Wittekamp 2018
- Wittekamp BH, Plantinga NL, Cooper BS, Lopez-Contreras J, Coll P, Mancebo J, et al. Decontamination strategies and bloodstream infections with antibiotic-resistant microorganisms in ventilated patients: a randomized clinical trial. JAMA 2018;320(20):2087-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision-making. Evidence-based Dentistry 2015;16(3):69-71. [DOI] [PubMed] [Google Scholar]
Zanatta 2011
- Zanatta FB, Bergoli AD, Werle SB, Antoniazzi RP. Biofilm removal and gingival abrasion with medium and soft toothbrushes. Oral Health and Preventive Dentistry 2011;9(2):177-83. [PubMed] [Google Scholar]
Zhang 2013
- Zhang TT, Tang SS, Fu LJ. The effectiveness of different concentrations of chlorhexidine for prevention of ventilator-associated pneumonia: a meta‐analysis. Journal of Clinical Nursing 2014;23(11-12):1461-75. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Hua 2016
- Hua F, Xie H, Worthington HV, Furness S, Zhang Q, Li C. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database of Systematic Reviews 2016, Issue 10. Art. No: CD008367. [DOI: 10.1002/14651858.CD008367.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shi 2010
- Shi Z, Xie H, Wang P, Wu Y, Chen E, Ng L, et al. Oral hygiene care for critically ill patients to prevent ventilator associated pneumonia. Cochrane Database of Systematic Reviews 2010, Issue 2. Art. No: CD008367. [DOI: 10.1002/14651858.CD008367] [DOI] [PubMed] [Google Scholar]
Shi 2013
- Shi Z, Xie H, Wang P, Zhang Q, Wu Y, Chen E, et al. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No: CD008367. [DOI: 10.1002/14651858.CD008367.pub2] [DOI] [PubMed] [Google Scholar]


