Abstract
Background:
Postoperative residual neuromuscular blockade related to non-depolarizing neuromuscular blocking agents may be associated with pulmonary complications. In this study, we sought to determine whether sugammadex was associated with a lower risk of postoperative pulmonary complications, compared to neostigmine.
Methods:
Adult patients from Vanderbilt University Medical Center National Surgical Quality Improvement Program database who underwent general anesthesia procedures between January 2010 and July 2019 were included in an observational cohort study. In early 2017, a wholesale switch from neostigmine to sugammadex occurred at Vanderbilt University Medical Center. We therefore identified all patients receiving non-depolarizing neuromuscular blockades and reversal with neostigmine or sugammadex. An inverse probability of treatment weighting propensity score analysis approach was applied to control for measured confounding. The primary outcome was postoperative pulmonary complications, determined by retrospective chart review and defined as the composite of the three postoperative respiratory occurrences: pneumonia, prolonged mechanical ventilation, and unplanned intubation.
Results:
Of 10,491 eligible cases, 7800 patients received neostigmine and 2691 received sugammadex. A total of 575 (5.5%) patients experienced postoperative pulmonary complications (5.9% neostigmine vs. 4.2% sugammadex). Specifically, 306 (2.9%) patients had pneumonia (3.2% vs. 2.1%), 113 (1.1%) prolonged mechanical ventilation (1.1% vs. 1.1%), and 156 (1.5%) unplanned intubation (1.6% vs. 1.0%). After propensity score adjustment, we found a lower absolute incidence rate of postoperative pulmonary complications over time (adjusted odds ratio, 0.91 [per year]; 95% CI, 0.87 to 0.96; p < .001). No difference was observed on the odds of postoperative pulmonary complications in patients receiving sugammadex, in comparison to neostigmine (adjusted odds ratio, 0.89; 95% CI, 0.65 to 1.22; p = 0.468).
Conclusions:
Among 10,491 patients at a single academic tertiary care center, we found switching neuromuscular blockade reversal agents was not associated with the occurrence of postoperative pulmonary complications.
Introduction
Neuromuscular blocking agents are commonly administered during general anesthesia to facilitate endotracheal intubation and to optimize surgical conditions.1 However, residual neuromuscular blockade remains a complication of non-depolarizing neuromuscular blocking agents. Clinically, residual neuromuscular blockade is associated with adverse physiological effects, including impaired pharyngeal function, decreased functional residual capacity, and impaired hypoxic ventilatory response,2,3 which contribute to multiple postoperative complications, including weakness, aspiration, reintubation, and pneumonia.4–9 Thus, appropriate reversal guided by neuromuscular transmission monitoring is critical to decreasing the risk of postoperative pulmonary complications.10
Neostigmine, an acetylcholinesterase inhibitor reversal agent, may decrease the likelihood of postoperative pneumonia.11 However, it is ineffective in reversing deep neuromuscular blockade.12 Additionally, neostigmine may be associated with paradoxical muscle weakness if administered when full recovery of neuromuscular function has occurred.13 Moreover, muscarinic side effects, including bradycardia, double vision, and postoperative nausea and vomiting are an important consideration in routine use.14 Sugammadex, a novel reversal agent, has been approved by the Food and Drug Administration in 2015 as an alternative to neostigmine and entered broad usage. Reversal using sugammadex has been reported to lower the incidence of residual paralysis,15 with more rapid reversal, less bradycardia,16 and a lower hospital readmission rate.17 The association between postoperative pulmonary complications and sugammadex reversal, however, remains unclear.
The primary aim of this analysis is to determine if reversal with sugammadex is associated with a lower risk of pulmonary complications within the 30-day postoperative period compared with reversal with neostigmine. We hypothesized that use of sugammadex was protective for the development of postoperative pulmonary complications.
Materials & Methods
This retrospective observational cohort study received approval from the Institutional Review Board at Vanderbilt University Medical Center (VUMC). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement was used to report this study and the manuscript adheres to the applicable guildlines.18
Data Collection
Data were derived from a local, single center copy of the National Surgical Quality Improvement Program (NSQIP) database, merged with data from the electronic health record and anesthetic record.19,20 Our primary outcome, postoperative pulmonary complication, was defined as the composite of the three National Surgical Quality Improvement Program-tracked postoperative respiratory occurrences: pneumonia, requiring mechanical ventilation for more than 48 hours, and unplanned intubation. A global rank composite methodology was applied to develop the composite pulmonary complications with severity ranking.21 Outcome data were obtained by combining our local, National Surgical Quality Improvement Program outcomes data with our local, identified electronic health record data. Vanderbilt University Medical Center National Surgical Quality Improvement Program data were abstracted from the medical record by a trained surgical clinical reviewer. After the transmission of deidentified data to National Surgical Quality Improvement Program, our National Surgical Quality Improvement Program chart abstractor team downloaded the data from the National Surgical Quality Improvement Program site to create a local, identified copy. These data were loaded into our Perioperative Data Warehouse on a quarterly basis. An electronic data query was designed to collect baseline, perioperative and postoperative data from the copy of Vanderbilt University Medical Center National Surgical Quality Improvement Program database and the supplemental demographic, clinical, and intraoperative data regarding medications were obtained from Vanderbilt University Medical Center Perioperative Data Warehouse. The National Surgical Quality Improvement Program and Vanderbilt University Medical Center Perioperative Data Warehouse are the source of the data used; National Surgical Quality Improvement Program has not verified and is not responsible for the validity of the statistical analysis or the conclusions derived by this study. The sample size was based on our available National Surgical Quality Improvement Program data, and a statistical power analysis of cohorts of cases and controls was performed prior to the study.
Practice Changes
Sugammadex was introduced at Vanderbilt University Medical Center in May 2016 and was initially restricted to emergency reversal of a rapid sequence intubation dosage of rocuronium, resulting in infrequent usage in the operating room. In March 2017, its locally approved indication was broadened to include routine reversal, and it replaced neostigmine in the standard pharmacy tray distributed to operating rooms. This resulted in an immediate, wholesale switch from utilization of neostigmine to sugammadex at that time.
We have previously described that our institution, like our peer institutions, has gradually adopted utilization of lung protective ventilation strategies in the operating room.22 In addition to practice changes that appear to have occurred without active quality improvement intent, we have also developed and implemented clinical decision support to identify patients at risk of acute lung injury and recommend usage of lung protective ventilation strategies. Two separate clinical decision support interventions were made, in June 2014 and again in March 2017, respectively. Analysis of these changes has demonstrated that they were not effective, i.e. did not impact adoption of lung protective ventilation strategies when the background rate of practice change was considered. Additionally, we modified our default ventilator settings in April 2017 to a tidal volume of 450 mL (from 600 ml) and positive end-expiratory pressure (PEEP) of 5 cm H2O (from none).
Our institution has also focused on the development and implementation of enhanced recovery after surgery protocols that seek to minimize exposure to opioids in the preoperative, intraoperative, and postoperative phases. These protocols also emphasize the importance of goal-directed fluid therapy, appropriate postoperative nausea and vomiting prophylaxis, glycemic control, and usage of lung protective ventilation. We have described this work previously in colorectal patient populations,23 and surgical weight loss patients,24 and the scope of these implementations includes 14 service lines. Within our colorectal patient population, we have also show that implementation of these protocols has been broadly associated with the reduction of postoperative complications.25
In addition to these practice changes described above, we have also performed focused work on improving our documentation of neuromuscular blockade depth. This work began in September 2015 and continued through November 2016, and has been previously described.26 The effect of these changes to our documentation practices was modest.
Eligibility
Eligible patients received general anesthesia with the use of a non-depolarizing neuromuscular blocking agents, and were performed between January 2010 and July 2019. These cases had previously been selected for National Surgical Quality Improvement Program review using the National Surgical Quality Improvement Program sampling methodology and followed by trained surgical clinical reviewers using consistent data definitions. Of note, during the study period, several sampling methodology changes were introduced by the National Surgical Quality Improvement Program. While all cases were included based on a randomization schedule prescribed by the American College of Surgeons before January 2011, hospitals were allowed to selectively include higher volumes of chosen procedures under the Procedure Targeted Program since then. Meanwhile, a change to targeted sampling was made in January 2015 by eliminating ventral hernia repair and replacing it with appendectomy, a high-volume, low risk operation that is monitored as a bellwether for procedural variation which may lead to increasing complications.
For each eligible case, we identified patients with the intraoperative administration of neuromuscular blockade, followed by use of a reversal agent (neostigmine or sugammadex). The patients who received intermediate-acting nondepolarizing neuromuscular blocking agents (cisatracurium, vecuronium, or rocuronium) were included in the cohort.27 The National Surgical Quality Improvement Program sampling methodology automatically filters out pediatric patients (birth to 18 years of age), transplantation cases, and those cases that resulted from complications of another diagnostic or surgical procedure within the previous 30 days.11 Furthermore, patients who received cisatracurium were excluded from further analysis.28 Moreover, patients receiving both sugammadex and neostigmine were excluded from the study. Additionally, we excluded surgical cases with incomplete intraoperative medication documentation in terms of neuromuscular blocking agents and reversal agents.
Primary Outcomes
1). Postoperative Pneumonia Definition
Patients were defined as having postoperative pneumonia if they met the National Surgical Quality Improvement Program definition of pneumonia after surgery. Pneumonia is defined by National Surgical Quality Improvement Program as the presence of at least one definitive chest radiologic examination and at least one sign of pneumonia (fever, leukopenia, leukocytosis, or altered mental status with no other cause), as well as at least one microbiologic laboratory finding (positive cultures from blood, bronchoalveolar lavage, or pleural fluid specimens) or at least two symptoms (new onset of purulent sputum, new onset of or worsening cough, dyspnea or tachypnea, rales or rhonchi breath sounds, or worsening gas exchange).11,29 Patients with an underlying pulmonary or cardiac disease are required to have at least two or more definitive serial chest radiological exams. Patients who were known or suspected to have pneumonia prior to surgery were excluded. Of note, the pneumonia definition was updated in 2012, which strengthened requirements for radiographic and laboratory data. And in 2015, an additional clarification was added, allowing physician documentation of the absence of pneumonia to contravene the surveillance-based assignment of the occurrence.
2). On Ventilator Greater Than 48 Hours Definition
Patients with a cumulative duration of ventilator-assisted respirations greater than 48 hours during the postoperative hospitalization and any subsequent hospitalizations within 30 days after a principal operative procedure are assigned a postoperative occurrence of On Ventilator Greater than 48 Hours.29 Patients who are intubated prior to surgery are excluded.
3). Unplanned Intubation Definition
Patients were defined as having unplanned intubation if they met the National Surgical Quality Improvement Program definition of unplanned intubation. Unplanned intubation is defined by National Surgical Quality Improvement Program as requiring placement of an endotracheal tube secondary to the onset of respiratory or cardiac failure as evidenced by severe respiratory distress, hypoxia, hypercarbia or respiratory acidosis within 30 days of the operation.29 Intubation for a return to the operating room is not included. In 2012, the unplanned intubation definition was broadened to include emergent airway management for any reason, including reintubation before leaving the operating room.
The primary outcome was the development of postoperative pneumonia, prolonged mechanical ventilation or unplanned intubation using global rank composite methodology.21 Postoperative occurrence of pneumonia, prolonged mechanical ventilation, and unexpected intubation were determined as clinical end points of interest, then were combined to form a composite outcome using the global rank method. The global rank is a composite of two or more outcomes that are assessed independently, and that can be naturally ordered. In our study, unplanned intubation was considered most severe, followed by prolonged ventilation, and pneumonia. The global rank was the hierarchical order of the most severe outcome that occurred within the postoperative follow-up period with 0 indicating no complication, 1 indicating pneumonia, 2 indicating prolonged mechanical ventilation, and 3 indicating unplanned intubation. Meanwhile, we summed up the global rank for patients that had more than one postoperative respiratory complication. Thus, the global rank composite ranging from 0 to 6 captured the incidence and severity of postoperative pulmonary complications.
Statistical Analysis
Demographic, clinical, and procedural variables were used to characterize the study population with means and standard deviations (SDs) for parametric variables, with medians and interquartile range for nonparametric variables and with percentages for categorical variables. The incident rates of the postoperative pulmonary complications following neostigmine and sugammadex use were reported.
To control for potential confounding variables, we performed a propensity score analysis with inverse probability of treatment weighting.30 This is a propensity score weighting method that mimics a matched analysis. This method allows for the use of all available data, and does not require specification of a matching algorithm, which is a source of uncertainty in matched analyses.31 We identified patients who had received intermediate-acting non-depolarizing neuromuscular blockers (vecuronium, or rocuronium) and reversal (neostigmine or sugammadex). The propensity score model was constructed by regressing the odds of receiving sugammadex versus neostigmine onto patient age, sex, weight, body mass index, American Society of Anesthesiologists (ASA) physical status classification, emergency surgery status, duration of the surgical procedure, procedure type (classified using Clinical Classifications Software Groupers),32 selected Elixhauser comorbidities associated with the risk of postoperative pulmonary complications (chronic pulmonary disease, congestive heart failure, paralysis, liver disease, and cardiac arrhythmia),33 primary surgeon volume, primary attending anesthesiologist volume, and whether or not the surgery occurred during normal business hours. Following the automate Harrell’s knot placement suggestions, a restricted cubic splines approach was applied on patient age for modeling non-linear associations. Body mass index was recategorized into four levels: Underweight (body mass index ≤ 18.5 kg/m2), Normal (18.5 < body mass index 25 kg/m2), Overweight (25 < body mass index ≤ 30 kg/m2), and Obesity (body mass index ≥ 30 kg/m2).34 Primary surgeon volume (the number of surgeries performed by the primary surgeon) was modeled as a categorical variable with two levels: low-volume (≤ 100 cases), and high-volume (> 100 cases); and primary attending anesthesiologist volume was modeled using the same logic.11 Of note, primary surgeon volume and primary attending anesthesiologist volume were restricted to the analyzed cohort, which therefore underestimated the actual procedure volume due to registry sampling. Meanwhile, for a case with multiple attendings, the first attending anesthesiologist was defined as the primary attending. In addition, last train-of-four prior to the administration of reversal agents was not included in primary analysis due to incompleteness of the data. The propensity scores weights were computed for each case,31 and the balance between the propensity score weighted cohorts was assessed using the standardized difference before and after propensity score weighting.
The cohorts with computed propensity score weights were analyzed, and the primary exposure variable, the association between reversal with sugammadex versus neostigmine and the distribution of the global rank composite for pulmonary complications, was assessed using multivariable weighted ordinal logistic regression. Many other intraoperative covariates, including surgery date, intraoperative tidal volume (median volume per ideal body weight35), and intraoperative opioid administration (morphine equivalents in mg/kg · h) were controlled as covariates in the regression model to adjust for any possible residual confounding and secular trends that might confound the assessment of two reversal agents. Associations were summarized using the ordinal odds ratios and 95% confidence intervals (CIs) and tested using a Wald-type test with 5% type-I error rate. The ordinal odds ratio is interpreted as follows: Let the ordinal global rank composite for pulmonary complications be denoted by Y and one of its levels by y (e.g., 0, 1, 2, 3, 4, 5, or 6). The ordinal odds are the odds that Y ≥ y, which is the probability that Y ≥ y divided by one minus itself .36 Thus, in this study, the odds ratio is interpreted as the fold-change in the odds of more severe postoperative pulmonary complications, associated with sugammadex versus neostigmine. A diagnostic goodness-of-link test was examined to discriminate the model fit.37
Sensitivity Analyses
Several sensitivity analyses were prespecified. First, the associations between reversal with sugammadex versus neostigmine and the odds of each individual outcome (i.e., pneumonia, prolonged mechanical ventilation, and unplanned intubation) were assessed and summarized using weighted multivariable logistic regression as sensitivity analyses. Surgery date, intraoperative tidal volume, and intraoperative opioid administration were controlled as covariates in all three logistic regression models.
Additionally, we implemented a sensitivity analysis using interrupted time series segmented regression to evaluate the possibility of secular trends that were not explained by the propensity score weighted ordinal logistic regression. The cohort was split into three groups by date of surgery: before January 1, 2013 [neostigmine period I (before the implementation of new Ventilator-Associated Events definitions)], from January 1, 2013 to March 31, 2017 [neostigmine period II (after the implementation of new Ventilator-Associated Events definitions)], and after April 1, 2017 (sugammadex period). The data in three groups were divided into quarterly subsets, to adjust for variation in case volume.
A protocol with priori analytic plan was written and filed to IRB at Vanderbilt University Medical Center before data were accessed. A two-sided hypothesis testing with p-value of less than 0.05 was deemed to indicate statistical significance. All statistical programming was implemented in SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
There were 10,817 surgical cases included in Vanderbilt University Medical Center National Surgical Quality Improvement Program database who received general anesthesia with the intraoperative administration of neuromuscular blockade, followed by use of a reversal agent. A total of 326 cases were excluded from analysis; 1 patient was under the age of 18 at the time of surgery, 9 received both sugammadex and neostigmine, 52 had incomplete intraoperative medication documentation, and 264 received cisatracurium. A priori power analysis showed that we would need to study at least 3,919 cases (2,506 receiving neostigmine and 1,413 receiving sugammadex) to detect a clinically relevant ordinal odds ratio of 0.7 with power of 0.8 in comparing patients who received neostigmine versus sugammadex. Our study included a total of 10,491 cases that met the inclusion criteria. Of all eligible cases, 7,800 patients received neostigmine and 2,691 received sugammadex, the overall incident rate of postoperative pulmonary complications was 5.9% for neostigmine subgroup, and 4.2% for sugammadex subgroup, respectively. Specifically, a total of 306 (2.9%) patients experienced postoperative pneumonia (3.2% neostigmine vs. 2.1% sugammadex), 113 (1.1%) prolonged mechanical ventilation (1.1% vs. 1.1%), and 156 (1.5%) unplanned intubation (1.6% vs. 1.0%) (Table 1).
Table 1.
Patient Demographics and Clinical Characteristics of the Study Sample.
| Variables | Reversal with Neostigmine (n = 7,800) |
Reversal with Sugammadex (n = 2,691) |
|---|---|---|
| Age in years, mean (SD) | 52 (16) | 51 (17) |
| Body mass index in kg/m2, mean (SD) | 29.8 (8.1) | 29.9 (8.1) |
| Weight in kg, mean (SD) | 89.0 (27.4) | 89.4 (27.1) |
| Sex (%) | ||
| Female | 4,163 (53.4%) | 1,414 (52.6%) |
| ASA Classifications (%) | ||
| I | 289 (3.7%) | 145 (5.4%) |
| II | 2,765 (35.5%) | 843 (31.3%) |
| III | 4,462 (57.2%) | 1,601 (59.5%) |
| IV & V | 284 (3.6%) | 102 (3.8%) |
| ASA Emergency (%) | 627 (8.0%) | 294 (10.9%) |
| Primary Surgeon Volume (%) | ||
| high-volume | 6,318 (81.0%) | 1,890 (70.2%) |
| Primary Attending Anesthesiologist Volume (%) | ||
| high-volume | 4,832 (62.0%) | 1,085 (40.3%) |
| Surgery Duration in mins, median (Interquartile Range) | 176 (127–247) | 190 (130–268) |
| Hospital Length of Stay in days, median (Interquartile Range) | 3 (1–6) | 3 (1–5) |
| Intraoperative Tidal Volume (median volume per ideal body weight) in mL/kg, median (Interquartile Range) | 8.3 (7.4–9.4) | 7.5(6.8–8.3) |
| Intraoperative Opioid Administration (morphine equivalents) in mg/kg · h, median (Interquartile Range) | 0.1 (0.1–0.2) | 0.1 (0.0–0.1) |
| Surgical Service (%) | ||
| General Surgery | 4,515 (57.9%) | 1,361 (50.6%) |
| Oncology Surgery | 1,202 (15.4%) | 376 (14.0%) |
| Trauma Surgery | 912 (11.7%) | 364 (13.5%) |
| Emergency General Surgery | 320 (4.1%) | 306 (11.4%) |
| Vascular Surgery | 500 (6.4%) | 171 (6.4%) |
| Hepatobiliary Surgery | 312 (4.0%) | 107 (4.0%) |
| Others | 39 (0.5%) | 6 (0.2%) |
| Normal Business Hours Surgery (%) | ||
| Yes | 6,823 (87.5%) | 2,495 (92.7%) |
| Selected Elixhauser comorbidities (%) | ||
| Chronic Pulmonary Disease | 399 (5.1%) | 436 (16.2%) |
| Congestive Heart Failure | 243 (3.1%) | 162 (6.0%) |
| Paralysis | 28 (0.4%) | 20 (0.7%) |
| Liver Disease | 308 (4.0%) | 381 (14.2%) |
| Cardiac Arrhythmia | 432 (5.6%) | 448 (16.7%) |
| Year of Surgery | ||
| 2010 | 974 (12.5%) | - |
| 2011 | 1,080 (13.9%) | - |
| 2012 | 1,074 (13.8%) | - |
| 2013 | 1153 (14.8%) | - |
| 2014 | 1,085 (13.9%) | - |
| 2015 | 1,121 (14.3%) | - |
| 2016 | 1,064 (13.6%) | 3 (0.1%) |
| 2017 | 241 (3.1%) | 921 (34.2%) |
| 2018 | 8 (0.1%) | 1,121 (41.7%) |
| 2019 | - | 646 (24.0%) |
| Pulmonary Complications Rate (%) | ||
| Pneumonia | 249 (3.2%) | 57 (2.1%) |
| Prolonged mechanical ventilation | 84 (1.1%) | 29 (1.1%) |
| Unplanned intubation | 128 (1.6%) | 28 (1.0%) |
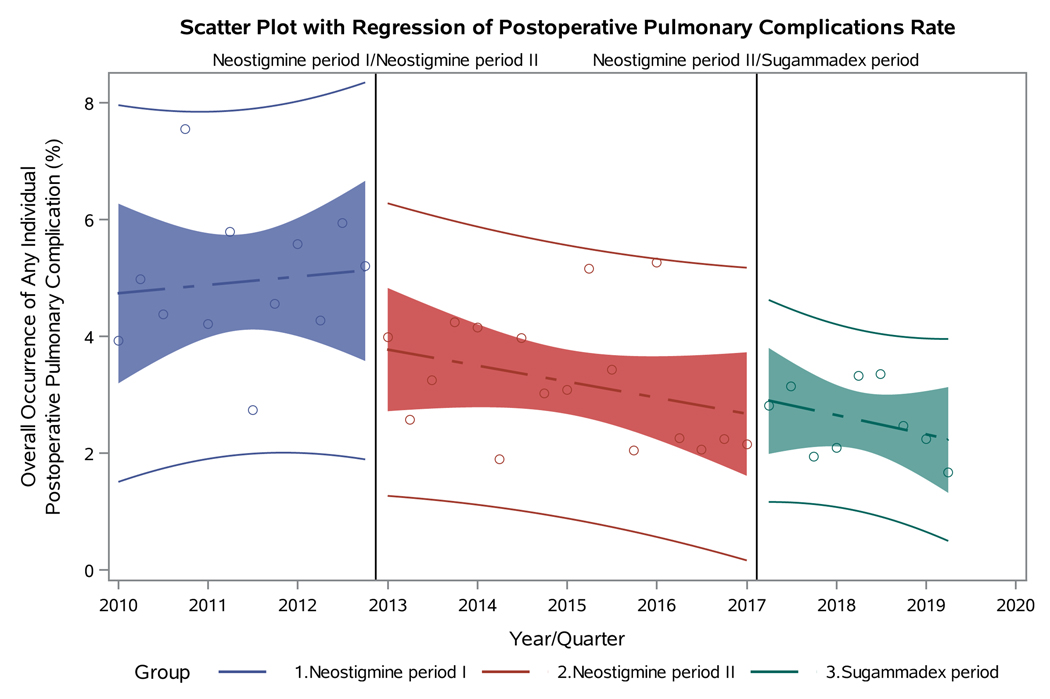
The standardized mean differences of the patient demographics and clinical characteristics before and after propensity score weighting are presented in Table 2. The standardized differences compared the difference in means in units of the pooled standard deviation, enabling comparison of the relative balance of variables measured across different units. Figure 1 shows the standardized differences of two groups. After propensity score weighting, the differences of patient age, sex, body mass index, selected Elixhauser comorbidities, ASA physical status, emergency surgery status, surgery duration, procedure type, primary surgeon, primary anesthesiologist, and the total logit propensity score were balanced across groups, with all standardized differences less than 0.05.
Table 2.
Standardized Differences between Neostigmine-Reversed and Sugammadex-Reversed Groups before and after Inverse Probability of Treatment Propensity Score Weighting.
| Variable | Observations | Mean Difference | Standard Deviation | Standardized Difference | Percent Reduction | Variance Ratio |
|---|---|---|---|---|---|---|
| Logit Prop Score | All | 0.64 | 0.8 | 0.80 | 1.6 | |
| Weighted | −0.01 | −0.01 | 98.3% | 0.9 | ||
| ASA Class | All | 0.02 | 0.6 | 0.03 | 1.1 | |
| Weighted | −0.01 | −0.01 | 69.0% | 1.1 | ||
| Age | All | −0.88 | 16 | −0.05 | 1.1 | |
| Weighted | 0.05 | 0.00 | 93.9% | 1.1 | ||
| Weight | All | 0.87 | 27.3 | 0.03 | 1.0 | |
| Weighted | −1.02 | −0.04 | 0.0% | 0.9 | ||
| Body Mass Index | All | 0.00 | 0.8 | 0.01 | 1.0 | |
| Weighted | 0.00 | 0.00 | 31.9% | 1.0 | ||
| Hospital Length of Stay | All | −0.19 | 5 | −0.04 | 0.9 | |
| Weighted | 0.13 | 0.03 | 28.4% | 1.4 | ||
| Surgical Procedure | All | −0.93 | 51.6 | −0.02 | 1.0 | |
| Weighted | −1.95 | −0.04 | 0.0% | 0.9 | ||
| Surgery Duration | All | 18.61 | 112 | 0.17 | 1.4 | |
| Weighted | −1.71 | −0.02 | 90.8% | 1.1 | ||
| Chronic Pulmonary Disease (Elixhauser) | All | 0.11 | 0.3 | 0.36 | 2.8 | |
| Weighted | 0.00 | −0.01 | 98.5% | 1.0 | ||
| Congestive Heart Failure (Elixhauser) | All | 0.03 | 0.2 | 0.14 | 1.9 | |
| Weighted | 0.01 | 0.04 | 74.2% | 1.2 | ||
| Paralysis (Elixhauser) | All | 0.00 | 0.1 | 0.05 | 2.1 | |
| Weighted | 0.00 | 0.01 | 73.9% | 1.2 | ||
| Liver Disease (Elixhauser) | All | 0.10 | 0.3 | 0.36 | 3.2 | |
| Weighted | 0.00 | −0.01 | 97.3% | 1.0 | ||
| Cardiac Arrhythmia (Elixhauser) | All | 0.11 | 0.3 | 0.36 | 2.6 | |
| Weighted | 0.00 | 0.00 | 99.1% | 1.0 | ||
| Sex | All | −0.01 | 0.5 | −0.01 | 1.0 | |
| Weighted | 0.00 | 0.00 | 86.0% | 1.0 | ||
| Emergency Case | All | −0.02 | 0.3 | −0.07 | 1.2 | |
| Weighted | −0.01 | −0.03 | 55.8% | 1.1 | ||
| During Business Hours | All | 0.01 | 0.2 | 0.05 | 1.2 | |
| Weighted | 0.01 | 0.02 | 53.4% | 1.1 | ||
| Primary Attending Anesthesiologist Volume | All | 0.22 | 0.5 | 0.44 | 1.0 | |
| Weighted | 0.00 | 0.00 | 99.4% | 1.0 | ||
| Primary Surgeon Volume | All | 0.10 | 0.4 | 0.23 | 1.3 | |
| Weighted | 0.01 | 0.01 | 93.9% | 1.0 |
Standard deviation of all observations used to compute standardized differences.
Figure 1.
Visualization of the standardized differences between neostigmine-reversed and sugammadex-reversed groups before and after inverse probability of treatment propensity score weighting. (Negligible difference is 0.05.)
From the result of primary analysis, a later surgery date was found to be associated with a reduced probability of getting postoperative pulmonary complications (adjusted odds ratio, 0.91 [per year]; 95% CI, 0.87 to 0.96; p < .001). The intraoperative tidal volume (adjusted odds ratio, 0.98 [per mL/kg]; 95% CI, 0.95 to 1.00; p = 0.078), and opioid administration (adjusted odds ratio, 1.07 [per mg/kg · h]; 95% CI, 0.52 to 2.17; p = 0.856) were not associated with the risk of postoperative pulmonary complications. Compared to the patients receiving neostigmine, no difference was found regarding the occurrence of postoperative pulmonary complications for the patients receiving neuromuscular blockade followed by reversal with sugammadex (adjusted odds ratio, 0.89; 95% CI, 0.65 to 1.22; p = 0.468). Logit link function was found among the best in terms of the goodness-of-link test (p = 0.020). (Digital Supplemental Content 1 for full model results and diagnostics)
Three sensitivity analyses revealed more specific associations with each individual outcome. In comparing patients who received neostigmine, the adjusted odds ratio of having postoperative pneumonia in sugammadex group was 0.94 (95% CI, 0.66 to 1.34; p = 0.750), having prolonged mechanical ventilation was 0.83 (95% CI, 0.48 to 1.44; p = 0.508) and having unplanned intubation was 1.17 (95% CI, 0.73 to 1.86; p = 0.509), respectively.
The interrupted time series segmented analysis was conducted to evaluate the incident rate of postoperative pulmonary complications over time. One hundred and four cases were excluded from segmented analysis due to the overlaps: 89 patients in the neostigmine period (3.3%) cohort received sugammadex, and 15 patients in the sugammadex period (0.2%) received neostigmine. No significant trend change was found in the incidence of any composite postoperative pulmonary complication during the neostigmine period I (4.7% to 5.2%, p = 0.719), the neostigmine period II (3.8% to 2.6%, p = 0.156), and the sugammadex period (3.0% to 2.2%, p = 0.335). However, a significant downtrend was observed after combining the neostigmine period I and II (slop: - 0.03, p = 0.004), which was consistent with the primary analysis. No immediate change was observed with the transition from the neostigmine period I to neostigmine period II (5.2% [offset] to 3.8%; p = 0.167), and from the neostigmine period II to sugammadex period (2.6% [offset] to 3.0%; p = 0.660) (Fig 2).
Figure 2.
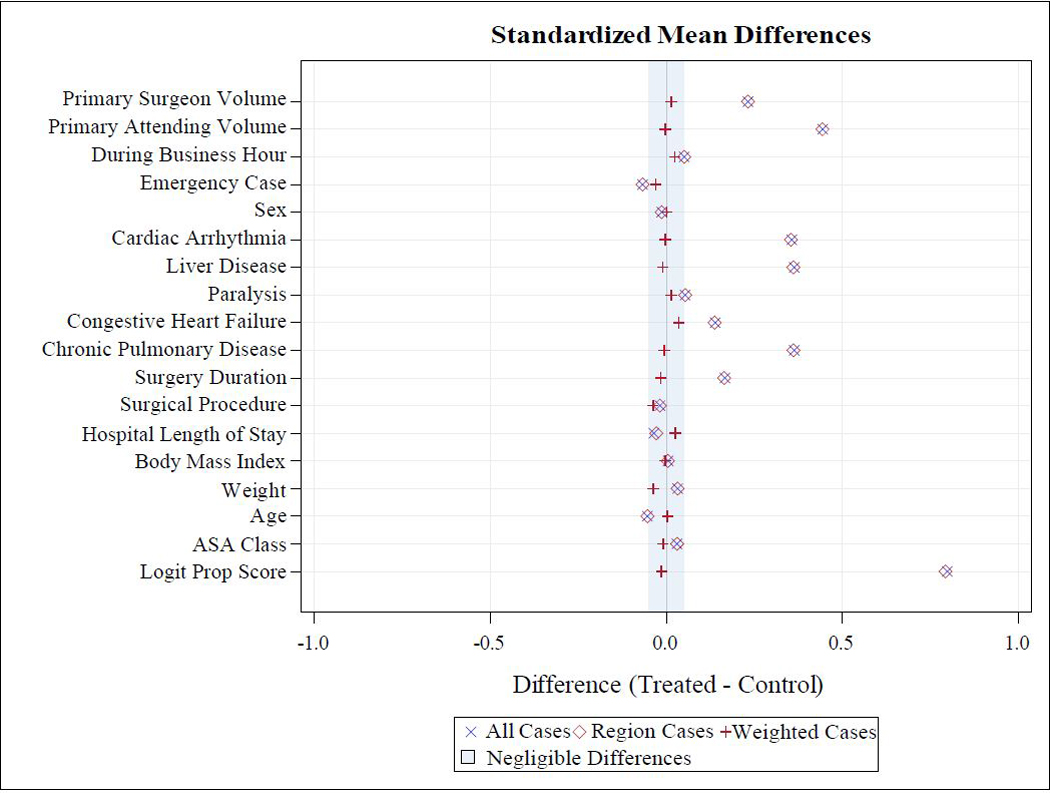
Visualization of the overall occurrence of the postoperative pulmonary complications over time.
Several post hoc sensitivity analyses were performed. To minimize the potential impact of the definition and sampling strategy changes in 2013 and 2015, we restricted the propensity score analyses to the cases after 2013 and 2015 respectively. For cases after 2013, no significant difference was observed in the incidence of postoperative pulmonary complications for the patients receiving sugammadex (adjusted odds ratio, 0.88; 95% CI, 0.58 to 1.33; p = 0.540), as were cases after 2015 (adjusted odds ratio, 0.80; 95% CI, 0.45 to 1.27; p = 0.296). Moreover, to evaluate the temporal change before sugammadex was widely used in our institution (neostigmine period I and II), we restricted the analysis to patient receiving neostigmine, and found the later date of the surgery was associated with a reduced probability of getting postoperative pulmonary complications (adjusted odds ratio, 0.89 [per year]; 95% CI, 0.84 to 0.95; p < .001).
Discussion
In this retrospective observational study, we found the choice of neuromuscular blockade reversal agents in general anesthesia was not associated with the occurrence of postoperative pulmonary complications.
Our results contribute to delineating the associations of neostigmine and sugammadex with respiratory outcomes that were observed in the literature. Although sugammadex was demonstrated to decrease residual postoperative paralysis and minor respiratory events, a systematic review of 1,553 patients by Abad-Gurumeta et al. found no difference in critical respiratory events such as intubation and invasive or non-invasive ventilation.38 Similarly, the 2017 Cochrane review indicated no difference in risks of serious adverse event between the two drugs at any dose, which included cases of pneumonia and respiratory failure.15 A multi-center observational cohort study (POPULAR) of 22,803 European patients showed that the choice of sugammadex instead of neostigmine was not associated with improved pulmonary outcomes, including suspected pulmonary infection.39 Chae et al. also reported no differences in 30-day postoperative outcomes following sugammadex and acetylcholinesterase inhibitor use.40 Thus, our results are in line with previous published studies.
Although a recent observational study found a 31% reduction in reintubation and initiation of non-invasive ventilation during a system-wide transition from neostigmine to sugammadex, its authors attributed the significant reduction to less demand for non-invasive ventilation, and the study was not sufficiently powered to detect difference in reintubation, due to low incidence.41 While a meta-analysis by Carron et al. found lower likelihood of respiratory adverse events in sugammadex group than neostigmine, their analysis did not stratify events based on severity.42 In addition, a recent multi-center observational cohort study (STRONGER) by Kheterpal et al. reported the sugammadex administration was associated with a 30% reduced risk of pulmonary complications compared to neostigmine, however, temporal bias may account for some of the reduction in complications given its five-year study period.33
In comparison to previous studies, our analysis captured a more comprehensive picture of pulmonary complications by examining a global rank composite of pneumonia, prolonged mechanical ventilation, and unplanned intubation up to 30 days after surgery, using rigorously-defined outcomes and consistent data definitions. Specifically, compared to the patients receiving neostigmine, patients who received sugammadex were not observed to be associated with a reduced risk of any individual pulmonary complication within 30 postoperative days. While sugammadex is well known for its use in reducing the risk of postoperative residual neuromuscular blockade in well controlled studies, this has not always improved clinical measures of postoperative strength and has not always reduced postoperative pulmonary complications.43,44 In daily clinical practice, the data regarding its impact on postoperative pulmonary complications has been mixed.45 We observed a lower absolute incidence rate of postoperative pulmonary complications over time, however, we were simply unable to distinguish that from background improvements that we observed in our cohort. While we didn’t observe a relationship between intraoperative tidal volumes and reduced pulmonary complication rates in this study, we made improvements which resulted in more consistent usage of lung protective ventilation and decreases in postoperative pulmonary complication.46,47 As compared with other hospitals,48 it is possible that our institution already was performing well with respective to postoperative pulmonary complications, well enough that switching from neostigmine to sugammadex did not generate a detectable signal in terms of improvement in our overall postoperative complication rate. In addition, given the statistical power of our study, clinically meaningful associations could be missed, and an adequately powered study may yield the opposite conclusion.
It is also noteworthy that an overall downtrend of postoperative pulmonary complications was observed over time at our medical center (adjusted odds ratio, 0.91 [per year]), with a downward trend even during the neostigmine period after 2013. Several initiatives have been reported to reduce the likelihood of postoperative pulmonary complications in general surgery patients over time.48,49 Specific to our institute, one possible contributor is the implementation of new Ventilator-Associated Events definitions by the National Healthcare Safety Network in 2013, which included more objective criteria for Ventilator-Associated Pneumonia.50 Additionally, our National Surgical Quality Improvement Program data were also subjected to changes in oversampling of certain procedures over time. For instance, we began to oversample appendectomies in 2015. Despite its emergent nature, appendectomies are not at high-risk for pulmonary complications. Also of note, during this period, our institution also implemented enhanced recovery after surgery protocols that have been shown to shorten length of hospital stay and lower rates of complications.51 And finally, our department had multiple quality improvement initiatives over the time period studied to encourage utilization of train-of-four ratio monitoring.52 Thus, the reduction of the occurrence of postoperative pulmonary completions over time is multifactorial and should not be attributed to change in reversal agent, as it occurred before the adoption of sugammadex. The conclusion has been further confirmed by the post hoc sensitivity analyses.
While we did not observe a lower occurrence of postoperative pulmonary complications with sugammadex, it has been shown to reduce postoperative residual neuromuscular blockade and its associated complications.39 A 2017 Cochrane review showed that sugammadex can reverse neuromuscular block up to 17 times faster than neostigmine, depending on dosage.16 Furthermore, sugammadex had an estimated of 40% fewer overall adverse events, especially in risks of postoperative nausea and vomiting, bradycardia, and postoperative residual paralysis.16
There are important limitations to our study. First, our retrospective study design is prone to bias due to residual confounding. However, we adjusted for measured known confounders through an inverse probability of treatment weighting propensity score analysis approach. Furthermore, since a sampled cohort was analyzed in this study, it enormously underestimated the surgical volumes of surgeons and attending anesthesiologists; and it may also introduce sampling bias to certain anesthesia subspecialties. Moreover, while the measured administrative diagnoses were statistically indiscernible between two study groups after propensity score weighting, other unmeasured perioperative data elements may or may not be balanced. For instance, potential confounders such as the type of anesthesia providers, fluid administration, and last train-of-four were not controlled in the primary analysis. We were unable to control for the last train-of-four, due to missing data for approximately 40% of patients, which might cause the unmatched depth of neuromuscular block at the time of reversal between two study groups. Therefore, further study is needed to determine if the last train-of-four value is a meaningful contributor to our findings. Second, since there is no standardized definition of postoperative pulmonary complication, studies evaluating postoperative pulmonary complication use different combinations of individual adverse outcomes.53 A systematic review for the American College of Physicians showed that about 60% of 16 studies used a combination of pneumonia and respiratory failure to define postoperative pulmonary complications.54 While the composite pulmonary outcome has yet to be validated as a reliable marker for postoperative pulmonary complications, the global rank methodology has been widely used in clinical trials.21,55 Moreover, the impact of the changes in Ventilator-Associated Events definitions on our findings was not addressed in this study. Third, another limitation of our study is the adoption and eventually wide utilization of sugammadex at our institution over the study period. Since the temporal nature of this change was a potential confounder which could not be controlled by propensity score matching approach, we conducted several post hoc sensitivity analyses and an interrupted time series segmented analysis, and did not observe a difference in pulmonary complications after adjustment between the periods of neostigmine and sugammadex use. In addition, despite the advantages of National Surgical Quality Improvement Program, this study is subject to the less generalizable population due to the nature of single-center data, focusing on general surgery cases, and changes in data sampling methodology.
In conclusion, our single-center retrospective observational study of 10,491 general surgery patients showed no significant difference in the risk of composite outcome of pulmonary complications as defined by pneumonia, prolonged mechanical ventilation, and unplanned intubation in patients whose neuromuscular blockade was reversed with sugammadex in comparison to neostigmine within 30-day postoperative period. Future investigations are therefore needed to validate our findings in a large-scale, multicenter randomized controlled trial. Additional examinations across different risk subgroups for pulmonary complications, and on the cost-effectiveness of sugammadex usage would also necessary.
Supplementary Material
Acknowledgements:
Funding Statement: REF receives ongoing support from the NIH - National Center for Advancing Translational Sciences (NCATS) #1KL2TR002245. GL and REF receive ongoing support from the National Heart, Lung, and Blood Institute (NHLBI) #K23HL148640. Other authors departmental funding.
Conflict of Interest: GL: Stock in Johnson and Johnson. REF: Grant funding and consulting fees from Medtronic; Stock in Johnson and Johnson and 3M.
Footnotes
Clinical Trial and Registry URL: Not applicable.
Summary Statement: No differences were found in the rate of postoperative pulmonary complications in propensity-score matched patients reversed with neostigmine versus sugammadex.
Contributor Information
Gen Li, Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN, United States
Robert E. Freundlich, Department of Anesthesiology, Department of Biomedical Informatics, Vanderbilt University Medical Center, Nashville, TN, United States.
Rajnish K. Gupta, Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN, United States
Christina J. Hayhurst, Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN, United States
Chi H. Le, School of Medicine, Vanderbilt University, Nashville, TN, United States
Barbara J. Martin, Quality Safety and Risk Prevention, Vanderbilt University Medical Center, Nashville, TN, United States.
Matthew S. Shotwell, Department of Biostatistics, Department of Anesthesiology, Vanderbilt University Medical Center, Nashville, TN, United States
Jonathan P. Wanderer, Department of Anesthesiology, Department of Biomedical Informatics, Vanderbilt University Medical Center, Nashville, TN, United States.
References
- 1.Brueckmann B, Sasaki N, Grobara P, Brueckmann B, Sasaki N, Grobara P, Li MK, Woo T, de Bie J, Maktabi M, Lee J, Kwo J, Pino R, Sabouri AS, McGovern F, Staehr-Rye AK, Eikermann M: Effects of sugammadex on incidence of postoperative residual neuromuscular blockade: a randomized, controlled study. Br J Anaesth. 2015; 115:743–51. [DOI] [PubMed] [Google Scholar]
- 2.Sundman E, Witt H, Olsson R, Ekberg O, Kuylenstierna R, Eriksson LI: The incidence and mechanisms of pharyngeal and upper esophageal dysfunction in partially paralyzed humans: Pharyngeal videoradiography and simultaneous manometry after atracurium. Anesthesiology. 2000; 92:977–84. [DOI] [PubMed] [Google Scholar]
- 3.Eriksson LI, Sundman E, Olsson R, Nilsson L, Witt H, Ekberg O, Kuylenstierna R: Functional assessment of the pharynx at rest and during swallowing in partially paralyzed humans: Simultaneous videomanometry and mechanomyography of awake human volunteers. Anesthesiology. 1997; 87:1035–43. [DOI] [PubMed] [Google Scholar]
- 4.Mirzakhani H, Williams JN, Mello J, Joseph S, Meyer MJ, Waak K, Schmidt U, Kelly E, Eikermann M: Muscle weakness predicts pharyngeal dysfunction and symptomatic aspiration in long-term ventilated patients. Anesthesiology. 2013; 119:389–97. [DOI] [PubMed] [Google Scholar]
- 5.Cedborg AI, Sundman E, Bodén K, Hedström HW, Kuylenstierna R, Ekberg O, Eriksson LI: Pharyngeal function and breathing pattern during partial neuromuscular block in the elderly: effects on airway protection. Anesthesiology. 2014; 120:312–25. [DOI] [PubMed] [Google Scholar]
- 6.Naguib M, Kopman AF, Ensor JE: Neuromuscular monitoring and postoperative residual curarisation: a meta-analysis. Br J Anaesth. 2007; 98:302–16. [DOI] [PubMed] [Google Scholar]
- 7.Murphy GS, Brull SJ: Residual neuromuscular block: lessons unlearned. Part I: definitions, incidence, and adverse physiologic effects of residual neuromuscular block. Anesth Analg. 2010; 111:120–8. [DOI] [PubMed] [Google Scholar]
- 8.Cedborg AI, Sundman E, Bodén K, Hedström HW, Kuylenstierna R, Ekberg O, Eriksson LI: Pharyngeal function and breathing pattern during partial neuromuscular block in the elderly: effects on airway protection. Anesthesiology. 2014; 120:312–25. [DOI] [PubMed] [Google Scholar]
- 9.Berg H, Roed J, Viby-Mogensen J, Mortensen CR, Engbaek J, Skovgaard LT, Krintel JJ: Residual neuromuscular block is a risk factor for postoperative pulmonary complications. A prospective, randomised, and blinded study of postoperative pulmonary complications after atracurium, vecuronium and pancuronium. Acta Anaesthesiol Scand. 1997; 41:1095–1103. [DOI] [PubMed] [Google Scholar]
- 10.McLean DJ, Diaz-Gil D, Farhan HN, Ladha KS, Kurth T, Eikermann M: Dose-dependent association between intermediate-acting neuromuscular-blocking agents and postoperative Respiratory complications. Anesthesiology. 2015; 122:1201–13. [DOI] [PubMed] [Google Scholar]
- 11.Bulka CM, Terekhov MA, Martin BJ, Dmochowski RR, Hayes RM, Ehrenfeld JM: Nondepolarizing neuromuscular blocking agents, reversal, and risk of postoperative pneumonia. Anesthesiology. 2016; 125:647–55. [DOI] [PubMed] [Google Scholar]
- 12.Jones RK, Caldwell JE, Brull SJ, Soto RG: Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology. 2008; 109:816–24. [DOI] [PubMed] [Google Scholar]
- 13.Phillips S, Stewart PA: Catching a unicorn: neostigmine and muscle weakness-not neostigmine for all, but quantitative monitoring for everyone! Anesthesiology. 2018; 129:381–2. [DOI] [PubMed] [Google Scholar]
- 14.Ledowski T, Falke L, Johnston F, Gillies E, Greenaway M, De Mel A, Tiong WS, Phillips M: Retrospective investigation of postoperative outcome after reversal of residual neuromuscular blockade: Sugammadex, neostigmine or no reversal. Eur. J. Anaesthesiol. 2014; 31:423–9. [DOI] [PubMed] [Google Scholar]
- 15.Alday E, Muñoz M, Planas A, Mata E, Alvarez C: Effects of neuromuscular block reversal with sugammadex versus neostigmine on postoperative respiratory outcomes after major abdominal surgery: a randomized-controlled trial. Can J Anesth. 2019; 66:1328–37. [DOI] [PubMed] [Google Scholar]
- 16.Hristovska AM, Duch P, Allingstrup M, Afshari A: Efficacy and safety of sugammadex versus neostigmine in reversing neuromuscular blockade in adults. Cochrane Database Syst Rev. 2017; 8:CD012763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Togioka BM, Yanez D, Aziz MF, Higgins JR, Tekkali P, Treggiari MM: Randomised controlled trial of sugammadex or neostigmine for reversal of neuromuscular block on the incidence of pulmonary complications in older adults undergoing prolonged surgery. Br J Anaesth. 2020; 124:553–61. [DOI] [PubMed] [Google Scholar]
- 18.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative: The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370:1453–7. [DOI] [PubMed] [Google Scholar]
- 19.Hall BL, Hamilton BH, Richards K, Bilimoria KY, Cohen ME, Ko CY: Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: An evaluation of all participating hospitals. Ann Surg. 2009; 250:363–76. [DOI] [PubMed] [Google Scholar]
- 20.Vaid S, Bell T, Grim R, Ahuja V: Predicting risk of death in general surgery patients on the basis of preoperative variables using American College of Surgeons National Surgical Quality Improvement Program data. Perm J. 2012; 16:10–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Subherwal S, Anstrom KJ, Jones WS, Felker MG, Misra S, Conte MS, Hiatt WR, Patel MR: Use of alternative methodologies for evaluation of composite end points in trials of therapies for critical limb ischemia. Am Heart J. 2012; 164:277–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wanderer JP, Ehrenfeld JM, Epstein RH, Kor DJ, Bartz RR, Fernandez-Bustamante A, Vidal Melo MF, Blum JM: Temporal trends and current practice patterns for intraoperative ventilation at U.S. academic medical centers: a retrospective study. BMC Anesthesiol. 2015; 15:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McEvoy MD, Wanderer JP, King AB, Geiger TM, Tiwari V, Terekhov M, Ehrenfeld JM, Furman WR, Lee LA, Sandberg WS: A perioperative consult service results in reduction in cost and length of stay for colorectal surgical patients: evidence from a healthcare redesign project. Perioper Med (Lond). 2016; 5:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.King AB, Spann MD, Jablonski P, Wanderer JP, Sandberg WS, McEvoy MD: An enhanced recovery program for bariatric surgical patients significantly reduces perioperative opioid consumption and postoperative nausea. Surg Obes Relat Dis. 2018; 14:849–56. [DOI] [PubMed] [Google Scholar]
- 25.Hawkins AT, Geiger TM, King AB, Wanderer JP, Tiwari V, Muldoon RL, Ford MM, Dmochowski RR, Sandberg WS, Martin B, Hopkins MB, McEvoy MD: An enhanced recovery program in colorectal surgery is associated with decreased organ level rates of complications: a difference-in-differences analysis. Surg Endosc. 2019; 33:2222–30. [DOI] [PubMed] [Google Scholar]
- 26.Dunworth BA, Sandberg WS, Morrison S, Lutz C, Wanderer JP, O’Donnell JM: Implementation of Acceleromyography to Increase Use of Quantitative Neuromuscular Blockade Monitoring: A Quality Improvement Project. AANA J. 2018; 86:269–77. [PubMed] [Google Scholar]
- 27.Grosse-Sundrup M, Henneman JP, Sandberg WS, Bateman BT, Uribe JV, Nguyen NT, Ehrenfeld JM, Martinez EA, Kurth T, Eikermann M: Intermediate acting non-depolarizing neuromuscular blocking agents and risk of postoperative Respiratory complications: prospective propensity score matched cohort study. BMJ. 2012; 345:e6329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kopman AF: Sugammadex: A Revolutionary Approach to Neuromuscular Antagonism. Anesthesiology. 2006; 104:631–3. [DOI] [PubMed] [Google Scholar]
- 29.American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP): ACS NSQIP: How It Works. Chicago, Illinois, American College of Surgeons, 2012, pp 1–11. [Google Scholar]
- 30.Austin PC, Stuart EA: Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015; 34:3661–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Austin PC: A comparison of 12 algorithms for matching on the propensity score. Stat Med. 2014; 33:1057–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.HCUP Clinical Classifications Software (CCS) for ICD9-CM: Healthcare Cost and Utilization Project (HCUP). Rockville, MD, Agency for Healthcare Research and Quality, 2006-2009. [PubMed] [Google Scholar]
- 33.Kheterpal S, Vaughn MT, Dubovoy TZ, Shah NJ, Bash LD, Colquhoun DA, Shanks AM, Mathis MR, Soto RG, Bardia A, Bartels K, McCormick PJ, Schonberger RB, Saager L. Sugammadex versus Neostigmine for Reversal of Neuromuscular Blockade and Postoperative Pulmonary Complications (STRONGER): A Multicenter Matched Cohort Analysis. Anesthesiology. 2020; 132:1371–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention: How is BMI interpreted for adults? http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/#InterpretedAdults. [Accessed November 25, 2015]
- 35.Devine BJ: Gentamicin therapy. DICP. 1974; 8:650–5. [Google Scholar]
- 36.Freundlich RE, Li G, Grant B, St Jacques P, Sandberg WS, Ehrenfeld JM, Shotwell MS, Wanderer JP: Patient satisfaction survey scores are not an appropriate metric to differentiate performance among anesthesiologists. J Clin Anesth. 2020; 65:109814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu Q, Shepherd BE, Li C, Harrell FE: Modeling continuous response variables using ordinal regression. Stat Med. 2017; 36:4316–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abad‐Gurumeta A, Ripollés‐Melchor J, Casans‐Francés R, Espinosa A, Martínez-Hurtado E, Fernández-Pérez C, Ramírez JM, López-Timoneda F, Calvo-Vecino JM, Evidence Anaesthesia Review Group: A systematic review of sugammadex vs neostigmine for reversal of neuromuscular blockade. Anaesthesia. 2015; 70:1441–52. [DOI] [PubMed] [Google Scholar]
- 39.Kirmeier E, Eriksson LI, Lewald H, Fagerlund MJ, Hoeft A, Hollmann M, Meistelman C, Hunter JM, Ulm K, Blobner M, POPULAR Contributors: Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicentre, prospective observational study. Lancet Respir Med. 2019; 7:129–40. [DOI] [PubMed] [Google Scholar]
- 40.Chae YJ, Joe HB, Oh J, Lee E, Yi IK: Thirty-day postoperative outcomes following sugammadex use in colorectal surgery patients: retrospective study. J Clin Med. 2019; 8:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krause M, McWilliams SK, Bullard KJ, Mayes LM, Jameson LC, Mikulich-Gilbertson SK, Fernandez-Bustamante A, Bartels K: Neostigmine versus sugammadex for reversal of neuromuscular blockade and effects on reintubation for respiratory failure or newly initiated noninvasive ventilation: an interrupted time series design. Anesth Analg. 2020; 131:141–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Carron M, Zarantonello F, Tellaroli P, Ori C: Efficacy and safety of sugammadex compared to neostigmine for reversal of neuromuscular blockade: a meta-analysis of randomized controlled trials. J Clin Anesth. 2016; 35:1–12. [DOI] [PubMed] [Google Scholar]
- 43.Abola RE, Romeiser J, Rizwan S, Lung B, Gupta R, Bennett-Guerrero E. A Randomized-Controlled Trial of Sugammadex Versus Neostigmine: Impact on Early Postoperative Strength. Can J Anaesth. 2020; 10.1007/s12630-020-01695-4. [DOI] [PubMed] [Google Scholar]
- 44.Han J, Ryu JH, Koo BW, Nam SW, Cho SI, Oh AY: Effects of Sugammadex on Post-Operative Pulmonary Complications in Laparoscopic Gastrectomy: A Retrospective Cohort Study. J Clin Med. 2020; 9:1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miskovic A, Lumb AB: Postoperative pulmonary complications. Br J Anaesth. 2017; 118:317–34. [DOI] [PubMed] [Google Scholar]
- 46.Hawkins AT, Geiger TM, King AB, Wanderer JP, Tiwari V, Muldoon RL, Ford MM, Dmochowski RR, Sandberg WS, Martin B, Hopkins MB, McEvoy MD: An Enhanced Recovery Program in Colorectal Surgery Is Associated With Decreased Organ Level Rates of Complications: A Difference-In-Differences Analysis. Surg Endosc. 2019; 33:2222–30. [DOI] [PubMed] [Google Scholar]
- 47.Wanderer JP, Ehrenfeld JM, Epstein RH, Kor DJ, Bartz RR, Fernandez-Bustamante A, Vidal Melo MF, Blum JM: Temporal Trends and Current Practice Patterns for Intraoperative Ventilation at U.S. Academic Medical Centers: A Retrospective Study. BMC Anesthesiol. 2015; 15:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cassidy MR, Rosenkranz P, Macht RD, Talutis S, McAneny D: The I COUGH multidisciplinary perioperative pulmonary care program: one decade of experience. Jt Comm J Qual Patient Saf. 2020; 46:241–9. [DOI] [PubMed] [Google Scholar]
- 49.Wren SM, Martin M, Yoon JK, Bech F: Postoperative pneumonia-prevention program for the inpatient surgical ward. J Am Coll Surg. 2010; 210:491–5. [DOI] [PubMed] [Google Scholar]
- 50.Centers for Disease Control and Prevention: Ventilator-Associated Event. https://www.cdc.gov/nhsn/PDFs/pscManual/10-VAE_FINAL.pdf [Accessed February 23, 2020].
- 51.Ljungqvist O, Scott M, Fearon KC: Enhanced recovery after surgery: a review. JAMA Surgery. 2017; 152:292–8. [DOI] [PubMed] [Google Scholar]
- 52.Dunworth BA, Sandberg WS, Morrison S, Lutz C, Wanderer JP, O’Donnell JM: Implementation of Acceleromyography to Increase Use of Quantitative Neuromuscular Blockade Monitoring: A Quality Improvement Project. AANA J. 2018; 86:269–77. [PubMed] [Google Scholar]
- 53.Miskovic A, Lumb AB: Postoperative pulmonary complications. Br J Anaesth. 2017; 118:317–34. [DOI] [PubMed] [Google Scholar]
- 54.Smetana GW, Lawrence VA, Cornell JE: Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006; 144:581–95. [DOI] [PubMed] [Google Scholar]
- 55.O’Connor CM, Whellan DJ, Fiuzat M, Punjabi NM, Tasissa G, Anstrom KJ, Benjafield AV, Woehrle H, Blase AB, Lindenfeld J, Oldenburg O: Cardiovascular outcomes with minute ventilation–targeted adaptive servo-ventilation therapy in heart failure: the CAT-HF trial. J Am Coll Cardiol. 2017; 69:1577–87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.