Abstract
Misfolding of the cellular prion protein, PrPC, into the amyloidogenic isoform, PrPSc, which forms infectious protein aggregates, the so-called prions, is a key pathogenic event in prion diseases. No pathogens other than prions have been identified to induce misfolding of PrPC into PrPSc and propagate infectious prions in infected cells. Here, we found that infection with a neurotropic influenza A virus strain (IAV/WSN) caused misfolding of PrPC into PrPSc and generated infectious prions in mouse neuroblastoma cells through a hit-and-run mechanism. The structural and biochemical characteristics of IAV/WSN-induced PrPSc were different from those of RML and 22L laboratory prions-evoked PrPSc, and the pathogenicity of IAV/WSN-induced prions were also different from that of RML and 22L prions, suggesting IAV/WSN-specific formation of PrPSc and infectious prions. Our current results may open a new avenue for the role of viral infection in misfolding of PrPC into PrPSc and formation of infectious prions.
Subject terms: Neurology, Neurological disorders, Prion diseases
Introduction
Neuronal accumulation of misfolded proteins or protein aggregates plays a key role in the pathogenesis of many neurodegenerative disorders, including Alzheimer’s disease (AD) and Parkinson’s disease (PD)1–4. In AD, β-amyloid (Aβ) peptides, Aβ1-40 and Aβ1-42, are aggregated and neurofibrillary tangles, which consist of hyperphosphorylated tau, are intracellularly accumulated in the brain1. Misfolded α-synuclein with phosphorylated serine residues, particularly serine 129, is accumulated in the dopaminergic neurons of the midbrains’ substantia nigra in PD4. Interestingly, lines of evidence point out the possible role of viral infections in induction of the misfolding or aggregation of these proteins5,6. Human herpes virus-1 (HSV-1) infection was shown to increase the intracellular levels of Aβ1-40 and Aβ1-42 in human neuroblastoma and glioblastoma cultured cells7. Aβ1-42 was accumulated in the brains of mice infected with HSV-17. Infection with the highly pathogenic, neurotropic H5N1 avian influenza A virus (IAV) has also been shown to induce accumulation of phosphorylated α-synuclein in the neurons of the substantia nigra pars compacta in mice8. However, the causal relationship between virus infections and induction of protein misfolding or protein aggregation needs to be further explored.
Prion diseases, which include Creutzfeldt-Jakob disease in humans and scrapie and bovine spongiform encephalopathy in animals, are a group of fatal neurodegenerative disorders caused by accumulation of infectious protein aggregates, or prions, in the brain9,10. Prions consist of the misfolded, amyloidogenic isoform of prion protein, designated PrPSc, which is produced through conformational conversion of the normal cellular counterpart, PrPC, a glycoprotein tethered to the plasma membrane via a glycosylphosphatidylinositol moiety and expressed most abundantly in the brain, particularly by neurons9,10. Prions, or PrPSc aggregates, propagate through the so-called self-templating mechanism, in which PrPSc aggregates function as a template for PrPC to undergo conformational conversion into PrPSc9,10. However, it is unknown whether virus infection could also evoke the conversion of PrPC into PrPSc and the subsequent formation of infectious prions in neuronal cells.
In this study, we show that infection with a neurotropic IAV strain A/WSN/33 (H1N1) (hereafter referred to as IAV/WSN) induced not only the conversion of PrPC into PrPSc but also the formation of infectious prions in cultured mouse neuroblastoma N2a cells. These results indicate that IAV/WSN infection plays a causal role in misfolding of PrPC into PrPSc and formation of infectious prions, further strengthening the role of virus infections in induction of the protein misfolding or aggregation associated with neurodegenerative diseases.
Results
IAV/WSN infection induces formation of PrPSc and infectious prions in neuroblastoma cells
To test if the conversion of PrPC into PrPSc and the formation of infectious prion could be induced in cultured neuronal cells by virus infection, we used the neurotropic IAV strain, IAV/WSN to infect mouse PrPC-overexpressing N2a cells, termed N2aC24 cells11, at different multiplicities of infection (MOIs). Western blotting showed that N2aC24 cells express PrPC 4.1 times higher than N2a cells (Supplementary Fig. 1). No N2aC24 cells survived infection with 0.1 or 1.0 MOI of IAV/WSN (Fig. 1a). Only a small proportion of cells survived infection with 0.01 MOI of IAV/WSN (Fig. 1a). Amazingly, Western blotting using large amounts (300 μg) of total proteins showed proteinase K (PK)-resistant PrP in the surviving cells at 7 and 8 days post-infection (dpi) (Fig. 1b). No PK-resistant PrP was observed in control IAV/WSN-uninfected N2aC24 cells (Fig. 1b). Viral proteins, HA, NP, and M2, were detectable in infected cells by 8 dpi (Fig. 1b). Immunofluorescent staining with anti-PrP monoclonal antibody 132 (anti-PrP mAb132), which recognizes residues 119–127 of mouse PrP and specifically detects PrPSc under partially denatured conditions12, also showed the mAb132-positive signals in infected cells at 8 dpi (Fig. 1c). Double immunofluorescent staining revealed the mAb132-positive signals in viral protein M2-positive cells (Fig. 1d), suggesting that PrPC is converted into PrPSc-like PrP in IAV/WSN-infected cells. The surviving cells, designated as N2aC24(R1) cells, grew and were passaged with a 1:10 split in IAV/WSN-free medium. PrPSc-like PK-resistant PrP became easily detectable in N2aC24(R1) cells after passages on Western blotting even with lower amounts (30 μg) of total proteins, and their signal intensities were increased during the passages (Fig. 1e), suggesting that PrPSc-like PrP generated in N2aC24(R1) cells has a potential to propagate. No PK-resistant PrP was still observed in IAV/WSN-uninfected N2aC24 cells even after 20 passages with a 1:10 split (Fig. 1e). Viral proteins became undetectable in N2aC24(R1) cells (Fig. 1f), suggesting that persistent IAV/WSN infections is not required for maintenance of PrPSc-like PrP production in N2aC24(R1) cells. These results indicate that IAV/WSN infection could induce the conversion of PrPC into PrPSc-like PrP in N2aC24 cells. We repeated the same experiments and obtained the same results, showing that PrPC is converted into PrPSc-like PrP in N2aC24 cells after IAV/WSN infection (Fig. 2a). In total, the same results were observed in 4 independent experiments of IAV/WSN infection in N2aC24 cells. To confirm that PrPC in N2aC24(R1) cells is not mutated, we amplified the PrP-coding sequences in N2aC24 and N2aC24(R1) cells by PCR and subjected them to DNA sequence analysis. No mutations were found in the PrP-coding sequences in N2aC24(R1) cells as well as in N2aC24 cells (Supplementary Fig. 2), indicating that PrPC is not mutated in N2aC24(R1) cells. We also detected PrPSc-like PK-resistant PrP in parental N2a cells, which express mouse PrPC only at endogenous levels, at 5 passages after infection with IAV/WSN, indicating that overexpression of PrPC is not necessary for IAV/WSN infection to induce conversion of PrPC into PrPSc-like PrP (Fig. 2b).
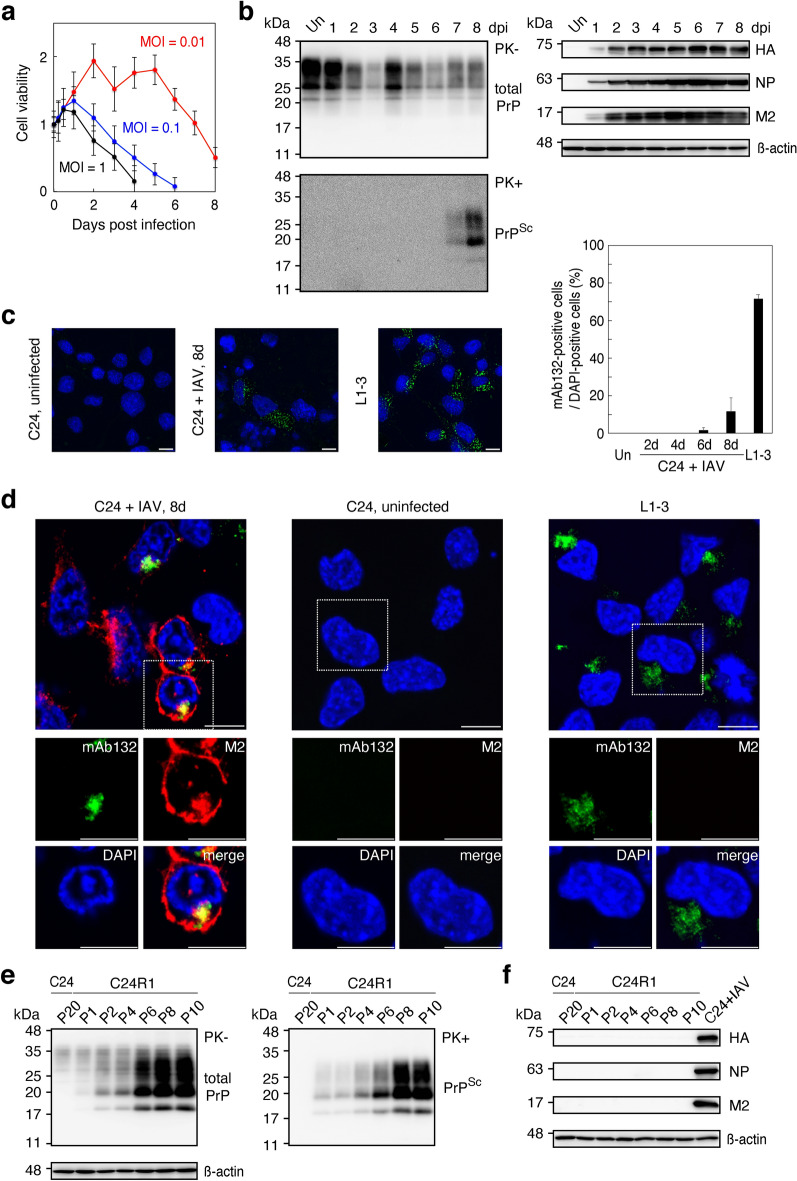
Figure 1.
IAV/WSN infection induces conversion of PrPC to PrPSc in N2aC24 cells. (a) Cell viability of N2aC24 cells after infection with different MOIs of IAV/WSN. Cell viability was determined by counting of live cells. (b) Western blotting of IAV/WSN-uninfected (Un) N2aC24 cells and -infected N2aC24 cells at various time points with 6D11 anti-PrP antibody, anti-HA antibody, anti-NP antibody, and anti-M2 antibody after treatment with ( +) or without (-) PK (20 μg/mg of proteins). PK-untreated 15 μg proteins from each cell lysate were used for detection of total PrP, HA NP, and M2 and PK-treated 300 μg proteins for PrPSc. (c) Left panels: Immunofluorescent staining of PrPSc (green) using 132 anti-PrP antibody in IAV/WSN-uninfected and -infected N2aC24 cells at 8 dpi and in 22L prion-infected N2aC24L1-3 cells. Right panel: The percentage (%) of 132 anti-PrP antibody-positive cells to DAPI-positive cells in at least 3 fields (145 × 109 μm/field) of IAV/WSN-uninfected (Un) and -infected N2aC24 cells at various time points and in 22L prion-infected N2aC24L1-3 (L1-3) cells. Blue, DAPI; bar, 10 μm. (d) Double immunofluorescent staining for PrPSc (green) and M2 (red) using 132 anti-PrP antibody and anti-HA antibody in IAV/WSN-uninfected and -infected N2aC24 cells at 8 dpi and in 22L prion-infected N2aC24L1-3 cells. Blue, DAPI; bar, 10 μm. (e) Left panel: Western blotting with 6D11 antibody of IAV/WSN-uninfected N2aC24 (C24) cells after 20 passages in IAV/WSN-free medium and N2aC24(R1) (C24R1) cells serially passaged after IAV/WSN infection using 15 μg proteins for total PrP (Left panel) and 30 μg proteins for PrPSc (Right panel). β-actin was used as an internal control. P, passages. (f) Western blotting of 15 μg proteins from N2aC24 and N2aC24(R1) cells with anti-HA antibody, anti-NP antibody, and anti-M2 antibody. IAV/WSN-infected N2aC24 cells were used as a positive control for the viral proteins. β-actin was used as an internal control. P, passages. Full length blots of Western blot images are shown in Supplementary Figs. 5c-e, 6, and 7.
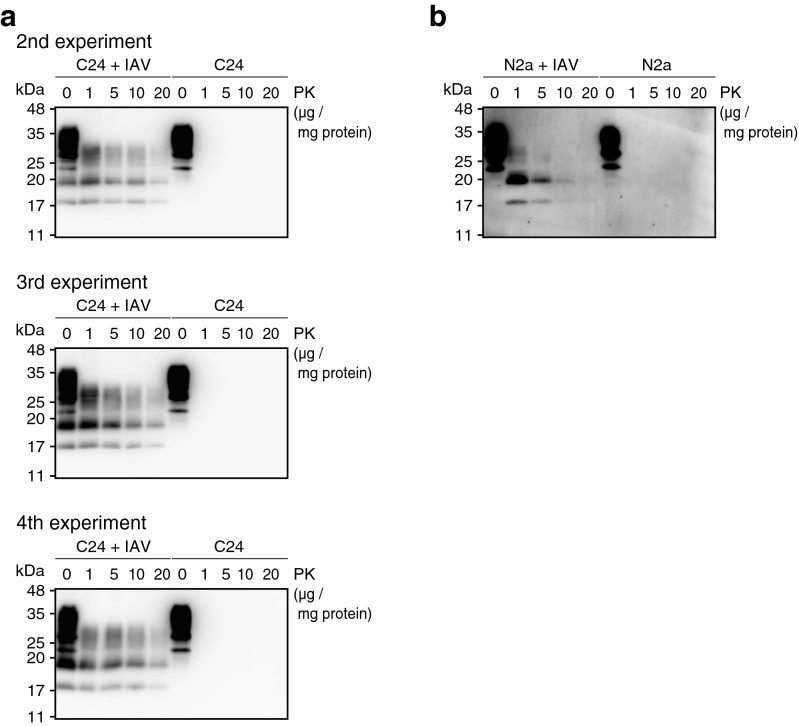
Figure 2.
Reproducible de novo formation of PrPSc in N2aC24 and N2a cells after infection with IAV/WSN. (a) Western blotting of N2aC24 cells at 5 passages after infection with or without IAV/WSN using 6D11 antibody after treatment with different concentrations of PK. Results are shown from three other independent experiments. (b) Western blotting of N2a cells at 5 passages after infection with or without IAV/WSN using 6D11 antibody after treatment with different concentrations of PK. Full length blots of Western blot images are shown in Supplementary Fig. 8.
We then investigated if IAV/WSN infection could also induce formation of infectious prions in N2aC24 cells, by intracerebrally inoculating N2aC24(R1) cell lysate into ICR indicator mice. All the mice inoculated with N2aC24(R1) cell lysate developed abnormal symptoms at 177 ± 4 (mean ± standard deviation, 10/10 inoculated mice were infected) days post-inoculation (dpi) (Fig. 3a). In contrast, none of the mice inoculated with control IAV/WSN-uninfected N2aC24 cell lysate developed any abnormal symptoms by 208 dpi (0/5 inoculated mice were infected) (Fig. 3a). Western blotting showed accumulation of PrPSc in the brains of N2aC24(R1)-inoculated, terminally ill mice, but not in control mice sacrificed at 208 dpi (Fig. 3b). Immunohistochemistry also showed the widespread accumulation of PrPSc in the brains of N2aC24(R1)-inoculated, terminally ill mice, but not in control mice sacrificed at 208 dpi (Fig. 3c). Vacuolation was also observed throughout the brain sections from N2aC24(R1)-inoculated, terminally ill mice, but not from control mice sacrificed at 208 dpi (Fig. 3d; Supplementary Fig. 3). These results show that mice inoculated with N2aC24(R1) cell lysate developed prion disease, indicating that IAV/WSN infection could also induce the formation of infectious prions in N2aC24 cells.
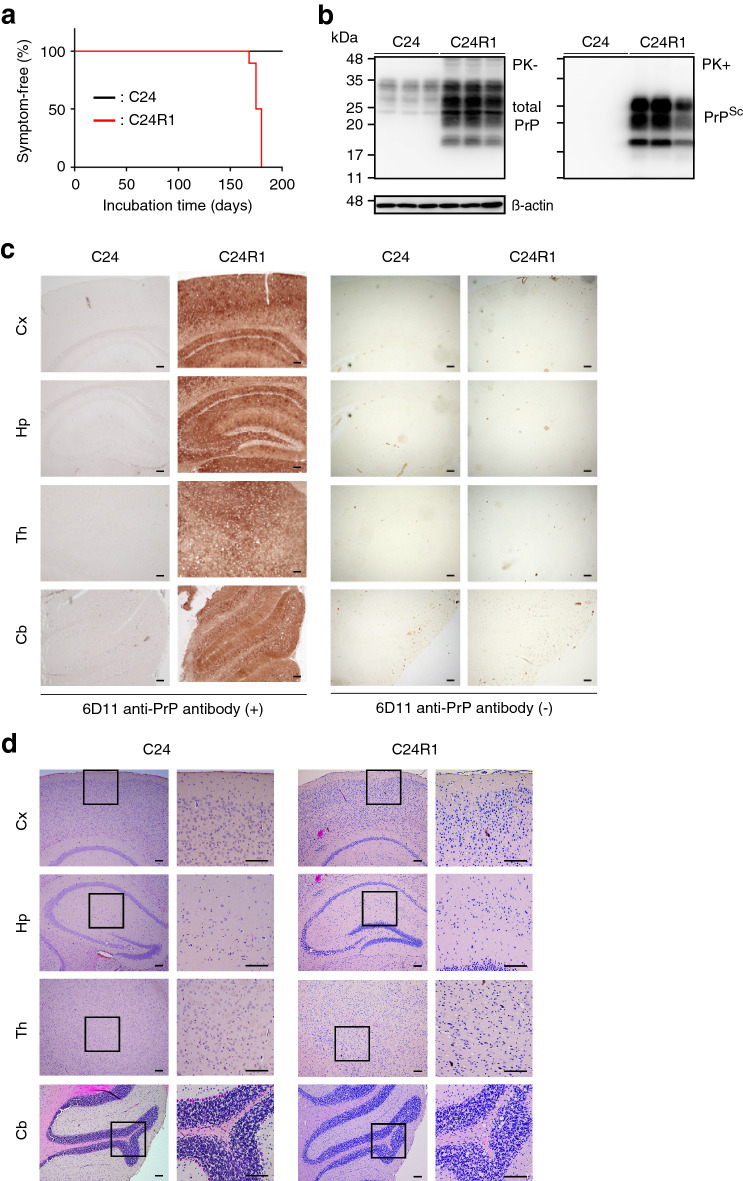
Figure 3.
IAV/WSN infection induces de novo formation of infectious prions in N2aC24 cells. (a) The percentage of symptom-free mice after intracerebral inoculation with cell lysates from control N2aC24 and N2aC24(R1) cells. (b) Western blotting of brains from mice sacrificed at 208 dpi with the N2aC24 cell lysate and from mice symptomatic after inoculation with N2aC24(R1) cell lysate with 6D11 antibody after treatment with or without PK (20 μg/mg of proteins). PK-untreated 20 μg proteins from each brain homogenate were used for detection of total PrP and PK-treated 40 μg proteins for PrPSc. β-actin was used as an internal control. (c) Immunohistochemistry of brains from mice sacrificed at 208 dpi with the N2aC24 cell lysate and from mice terminally ill after inoculation with N2aC24(R1) cell lysate with or without 6D11 antibody. Bars, 100 μm. (d) Hematoxylin–eosin staining of brains from mice sacrificed at 208 dpi with the N2aC24 cell lysate and from mice terminally ill after inoculation with N2aC24(R1) cell lysate. Cx, cerebral cortex; Hp, hippocampus; Th, thalamus; Cb, cerebellum. Bars, 100 μm. Full length blots of Western blot images are shown in Supplementary Fig. 9a, b.
Blockage of IAV/WSN infection prevents formation of PrPSc in neuroblastoma cells
To confirm that IAV/WSN infection is responsible for the conversion of PrPC into PrPSc detected in N2aC24(R1) cells (hereafter PrPSc-like PrP is referred to PrPSc), we blocked IAV/WSN infection in N2aC24 cells using anti-IAV/WSN mouse sera and investigated the cells for PrPSc on Western blotting. No viral proteins were detectable in N2aC24 cells at 4 dpi with 0.01 MOI of IAV/WSN after treatment with the anti-sera at the time of infection (Fig. 4a), indicating that the anti-sera successfully blocked IAV/WSN infection in N2aC24 cells. PK-resistant PrP fragments were also undetectable in the cells after 5 passages (Fig. 4b). In contrast, HA viral protein was detectable in IAV/WSN-infected N2aC24 cells after treatment with control sera (Fig. 4a). PK-resistant PrP fragments were also observed in the cells after 5 passages (Fig. 4b). We also blocked IAV/WSN infection in N2aC24 cells using the anti-IAV agent oseltamivir. HA viral protein levels in infected N2aC24 cells were decreased at 4 dpi in a dose-dependent manner of the agent (Fig. 4c). Production of PrPSc was also inhibited in the cells after 5 or 10 passages in a dose-dependent manner by the agent (Fig. 4d). These results indicate that blockade of IAV/WSN infection prevented the conversion of PrPC into PrPSc in N2aC24 cells, confirming that IAV/WSN infection is essential for the conversion of PrPC into PrPSc in N2aC24 cells. These results also rule out the possibility that IAV/WSN preparations, culture media, or N2aC24 cells used in the experiments might have been accidentally contaminated with laboratory prions and therefore PrPC might have been converted into PrPSc in N2aC24 cells by the contaminating prions not by infection with IAV/WSN.
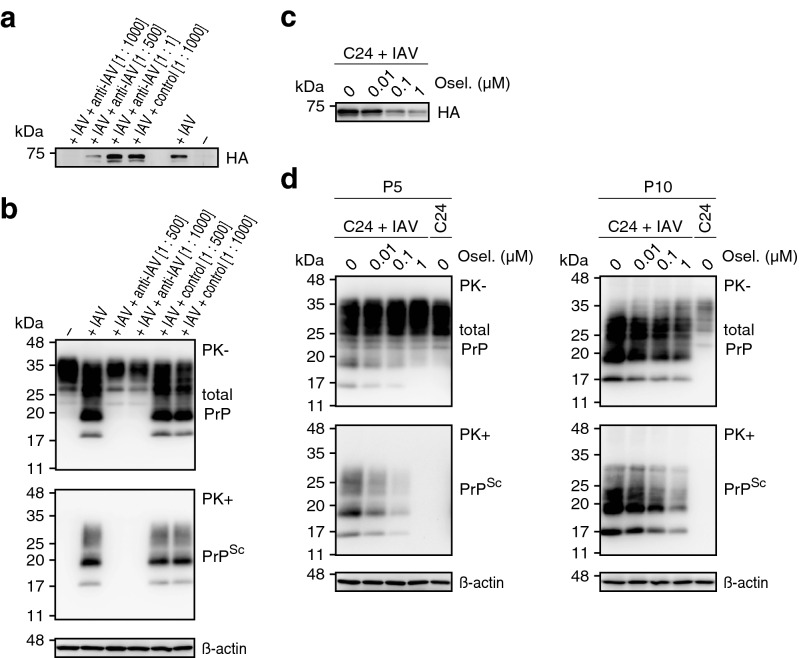
Figure 4.
Blockage of IAV/WSN infection prevents formation of PrPSc in N2aC24 cells. (a) Western blotting with anti-HA antibody of 15 μg proteins from IAV/WSN-uninfected (-) and -infected ( +) N2aC24 cells at 4 dpi after treatment with anti-IAV/WSN serum or control serum. (b) Western blotting with 6D11 antibody after treatment with or without PK (20 μg/mg of proteins) of IAV/WSN-uninfected (-) and -infected ( +) N2aC24 cells at 5 passages after treatment with anti-IAV/WSN serum or control serum. PK-untreated 15 μg proteins from each cell lysate were used for detection of total PrP and PK-treated 30 μg proteins for PrPSc. β-actin was used as an internal control. (c) Western blotting with anti-HA antibody of 15 μg proteins from IAV/WSN-infected ( +) N2aC24 cells at 4 dpi after treatment with different concentrations of oseltamivir (Osel). (d) Western blotting with 6D11 antibody after treatment with or without PK (20 μg/mg of proteins) of IAV/WSN-uninfected and -infected N2aC24 cells at 5 (Left panels) and 10 (Right panels) passages after treatment with different concentrations of Osel. PK-untreated 15 μg proteins from each cell lysate were used for detection of total PrP and PK-treated 30 μg proteins for PrPSc. β-actin was used as an internal control. Full length blots of Western blot images are shown in Supplementary Fig. 9c, d, and 10.
IAV/WSN-evoked prions have distinct pathogenicity
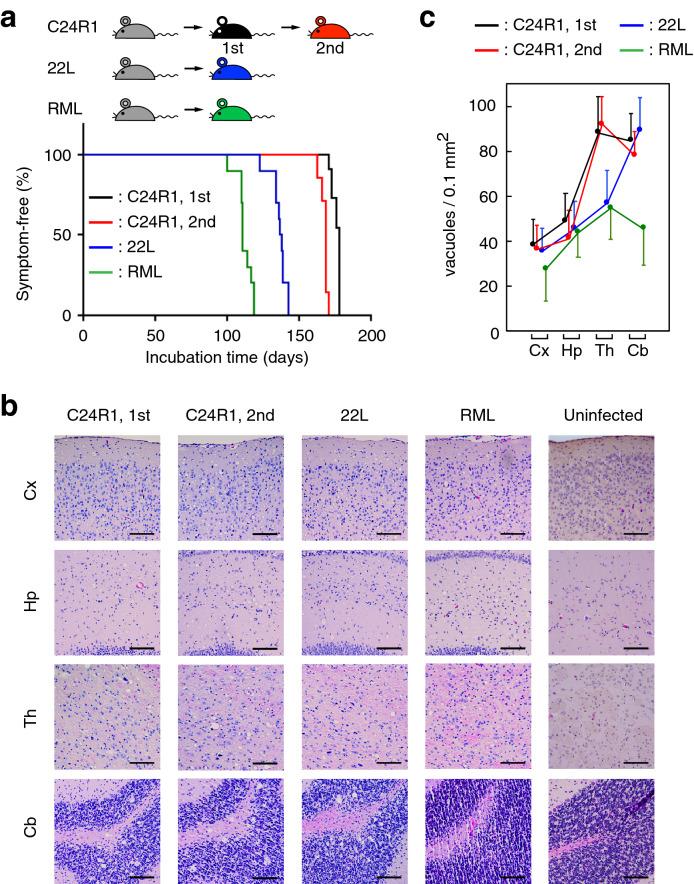
We characterized the pathogenic properties of prions in N2aC24(R1) cells (hereafter referred to as N2aC24(R1) prions) by comparison with RML and 22L scrapie prions, both of which are regularly used in our laboratory. To this end, we serially inoculated brain homogenates from N2aC24(R1)-infected, terminally ill mice into ICR mice via an intracerebral route. Brain homogenates from mice infected with mouse-adapted 22L or RML prions were also similarly inoculated into ICR mice. Mice primarily and secondarily inoculated with N2aC24(R1)-infected brain homogenates showed similar incubation times of 176 ± 3 (11/11 inoculated mice were infected) and 168 ± 3 (7/7 inoculated mice were infected) days, respectively (Fig. 5a). However, these incubation times were significantly longer than those of mice inoculated with RML- and 22L-infected brain homogenates. Incubation times of mice inoculated with RML and 22L prions were 112 ± 6 (10/10 inoculated mice were infected) and 137 ± 6 (10/10 inoculated mice were infected) days, respectively (Fig. 5a). Vacuolation pattern in the brain was also different among N2aC24(R1)-, RML-, and 22L-infected, terminally ill mice. The number of vacuoles in N2aC24(R1)-infected brains were high in the thalamus and cerebellum and low in the cerebral cortex and hippocampus (Fig. 5b, c). However, it was high in the cerebellum, intermediate in the thalamus, and low in the cerebral cortex and hippocampus of 22L-infected mice, and intermediate in the thalamus and low in the cerebral cortex, hippocampus, and cerebellums of RML-infected mice (Fig. 5b, c; Supplementary Fig. 4). These results suggest that N2aC24(R1) prions have different pathogenic properties from RML and 22L laboratory prions.
Figure 5.
Different pathological properties of prions in N2aC24(R1) cells from RML and 22L prions. (a) The percentage of symptom-free mice after the 1st intracerebral inoculation with brain homogenates from N2aC24(R1) cell lysate-inoculated, terminally ill mice, the 2nd intracerebral inoculation with brain homogenates from terminally ill mice firstly inoculated with N2aC24(R1)-infected mouse brain homogenates, and intracerebral inoculation with RML- or 22L-infected mouse brain homogenates. (b) HE staining of the brains of terminally ill mice in (a). Bars, 100 μm. (c) Vacuole counts at different brain areas of terminally ill mice [5 fields in each brain area from each mouse group (n = 3)] in (b). Cx, cerebral cortex; Hp, hippocampus; Th, thalamus; Cb, cerebellum. Error bars, standard deviation.
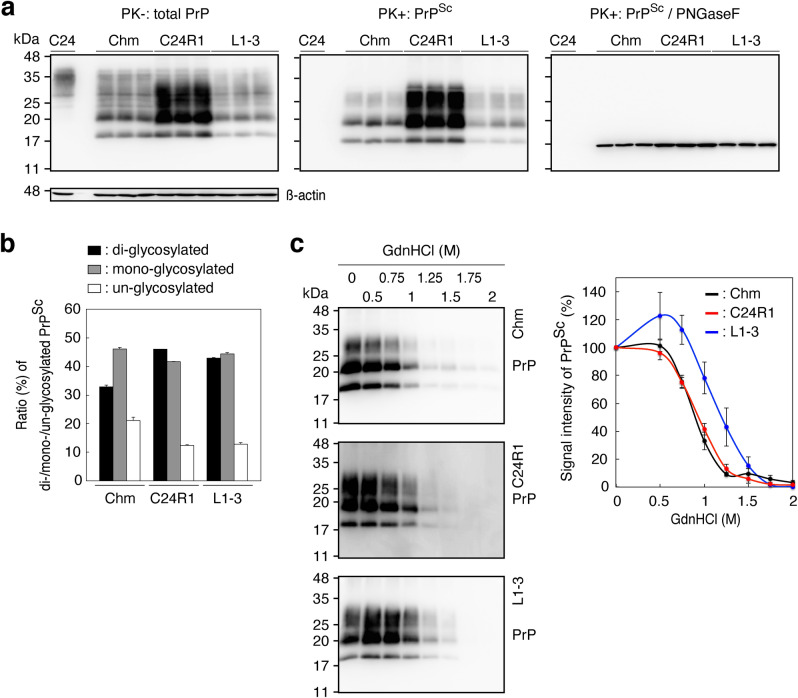
We also structurally and biochemically investigated PrPSc in N2aC24(R1) cells by comparison with PrPSc in 22L-infected N2aC24L1-3 and RML-infected N2aC24LChm cells 11. Di-, mono-, and un-glycosylated forms of PrPSc from N2aC24(R1) cells migrated similarly to those of PrPSc in N2aC24L1-3 and N2aC24Chm cells (Fig. 6a), suggesting that PrPSc from N2aC24(R1), N2aC24L1-3, and N2aC24Chm cells have the same PK cleavage site. Indeed, the deglycosylated, PK-resistant fragment of PrPSc from N2aC24(R1) cells migrated at the same position as that of PrPSc from N2aC24L1-3 and N2aC24Chm cells (Fig. 6a). However, the ratio of di-, mono-, and un-glycosylated, PK-resistant fragments of PrPSc from N2aC24(R1) cells was different from that from N2aC24Chm cells, but similar to that from N2aC24L1-3 cells (Fig. 6b). In contrast, the Gdn-HCl concentration required to denature 50% of PrPSc, the [Gdn-HCl]1/2 value, was similar for PrPSc from N2aC24(R1) and N2aC24Chm cells (0.9 and 0.9 M, respectively), but different for PrPSc from N2aC24(R1) and N2aC24L1-3 cells (0.9 and 1.2 M, respectively) (Fig. 6c). These results suggest that PrPSc in N2aC24(R1) cells could also be structurally and biochemically different from PrPSc in N2aC24L1-3 and N2aC24Chm cells.
Figure 6.
Different biochemical properties of PrPSc in N2aC24(R1) cells from PrPSc in RML- and 22L-infected N2aC24 cells. (a) Western blotting of N2aC24(R1), RML-infected N2aC24Chm (Chm), and 22L-infected N2aC24L1-3 cells (L1-3) with 6D11 antibody after treatment with or without PK (20 μg/mg of proteins). PK-untreated 15 μg proteins from each cell lysate were used for detection of total PrP (Left panel) and PK-treated 30 μg proteins for PrPSc (Middle panel) Aliquots of the PK-treated samples were also treated with PNGase F before Western blotting (Right panel). β-actin was used as an internal control. (b) Ratio (%) of di-, mono-, and un-glycosylated PrPSc in the Middle panel of (a). (c) Western blotting (Left panels) of PrPSc and its signal intensities (Right panel, n = 3) in RML-infected N2aC24Chm (Chm, Upper panel), N2aC24(R1) (Middle panel), and 22L-infected N2aC24L1-3 cells (L1-3, Lower panel) with 6D11 antibody after treatment with different concentrations of GdnHCl. Full length blots of Western blot images are shown in Supplementary Fig. 11.
Discussion
In the present study, we identified a neurotropic IAV strain, IAV/WSN, as the first non-prion pathogen that has a potential to induce the conversion of PrPC into PrPSc and the formation of infectious prions in cultured neuroblastoma cells. These results may open a new door to exploring the role of virus infections in the conversion of PrPC into PrPSc and the formation of infectious prions in prion diseases.
PrPSc was detected in viral protein M2-positive N2aC24 cells during the early period of IAV/WSN infection on immunofluorescent staining, suggesting that PrPC could be converted into PrPSc in IAV/WSN-infected N2aC24 cells themselves. Consistent with this, blockade of IAV/WSN infection in N2aC24 cells using anti-IAV/WSN sera or anti-IAV agent prevented the conversion of PrPC into PrPSc. However, after long culture of the surviving N2aC24 cells, termed N2aC24(R1) cells, viral proteins disappeared while PrPSc levels were increased in the cells, suggesting that IAV/WSN infection could induce the conversion of PrPC into PrPSc in N2aC24 cells in a hit-and-run fashion. It is thought that a critical step for PrPC to constitutively convert into PrPSc is the formation of PrPSc seeds through the oligomerization of nascently produced PrPSc molecules, and that once the PrPSc seeds are formed, PrPC is constitutively converted into PrPSc via the self-templating mechanism, where PrPC undergoes conformational conversion into PrPSc on the template of PrPSc seeds9,10. This may explain why persistent IAV/WSN infection is not required for maintenance of the conversion of PrPC into PrPSc in N2aC24(R1) cells. A similar hit-and-run mechanism has been also proposed for H5N1 avian IAV to induce the accumulation of misfolded α-synuclein in infected neurons8. In vitro protein misfolding cyclic amplification studies have shown that RNA and lipid molecules can function as cofactors for PrPC to convert into PrPSc and subsequently form infectious prions13,14. IAVs are negative-stranded, segmented, enveloped RNA viruses15. Thus, IAV/WSN-derived RNA or lipid molecules might be involved in the IAV/WSN-mediated hit-and-run conversion of PrPC into PrPSc in N2aC24 cells. Alternatively, PrPC is postulated to spontaneously convert into PrPSc at low frequency in normal neurons16. Therefore, IAV/WSN infection might increase the frequency of spontaneous conversion of PrPC into PrPSc in N2aC24 cells. We previously reported that PrPC has a protective role against lethal infection of IAV infection in mouse lungs through the octapeptide repeat (OR) region17. It might be thus interesting to investigate if the OR region is also required for IAV/WSN infection to induce conversion of PrPC into PrPSc in N2aC24 cells. No mutations in the PrP-coding sequence were detected in N2aC24(R1) cells. These results rule out the possibility that IAV/WSN infection might cause pathogenic mutations in the PrP-coding sequence, thereby inducing conversion of the mutant PrPC into PrPSc, or that a minority of N2aC24 cells already expressing mutant PrP might be selected after IAV/WSN infection.
The pathogenic properties of prions in N2aC24(R1) cells were different from those of RML and 22L laboratory prions in mice, suggesting that IAV/WSN infection might produce a new type of prion strain in N2aC24 cells. The pathogenic properties of different prion strains are considered to be enciphered in the strain-specific different conformation of PrPSc18,19. Consistent with this, PrPSc molecules in N2aC24(R1) cells were biochemically and structurally different from those in RML-infected N2aC24Chm and 22L-infected N2aC24L1-3 cells. It is thus possible that IAV/WSN infection might induce the conversion of PrPC into an IAV/WSN-specific form of PrPSc, thereby conferring new pathogenic properties on prions in an IAV/WSN-specific way. According to the unified theory proposed by Weissmann, nucleic acid molecules have been suggested to be a factor contributing to strain-specific properties of prions20. It is thus interesting to investigate whether IAV/WSN-RNA molecules are involved in generation of IAV/WSN-specific form of PrPSc.
Prion infections cause acquired prion diseases in infected individuals, such as variant and iatrogenic CJDs in humans and BSE in animals, through inducing the conversion of PrPC into PrPSc in the brain21. However, more than 85% cases of the diseases are sporadic in humans and their etiologies remain unknown22. Influenza-related acute neurologic complications such as seizure and encephalopathy have been reported in 1 to 4 cases per 100,00 children-years after infection with seasonal IAVs23. H5N1 avian IAV has been also shown to cause encephalitis in a child24. Epidemiological studies showed that the risk for Parkinson’s disease was 2–threefold higher in persons born during the 1918 H1N1 IAV pandemic than in those born prior to 1918 or after 192425,26. These facts suggest that IAV infection could cause neurological complications either acutely or chronically. Our current results may thus raise the future question of whether neurotropic virus infections, including neurotropic IAV infection, might cause or be associated with sporadic prion diseases. Elucidation of the mechanism of the IAV/WSN infection-evoked conversion of PrPC into PrPSc and formation of infectious prions in N2aC24 cells could be helpful for further understanding of the pathogenic mechanism of sporadic prion diseases.
Methods
Ethics statement
This study was approved by The Ethics Committee of Animal Care and Experimentation of Tokushima University (approval no. T27-102). Animals were cared for in accordance with The Guiding Principle for Animal Care and Experimentation of Tokushima University and with Japanese Law for Animal Welfare and Care. This study was carried out in compliance with the ARRIVE guidelines. All experiments in this study were performed under biosafety level 2 conditions.
Antibodies
The antibodies used in this study are: 6D11 mouse anti-PrP Ab (SIG-399810; BioLegend, San Diego, CA), anti-influenza-HA Abs (GTX127357; GeneTex, Irvine, CA), anti-influenza-NP Abs (GTX125989; GeneTex), anti-influenza-M2 Abs (GTX125951; GeneTex), mouse anti-ß-actin Ab (A1978; Sigma-Aldrich, St. Louis, MO), anti-mouse IgG horseradish peroxidase (HRP)-linked Ab (NA931; GE Healthcare, Little Chalfont, England), anti-rabbit IgG HRP-linked Ab (NA934; GE Healthcare), Alexa Fluor 488-conjugated goat anti-mouse IgG Abs (A11001; Thermo Fisher Scientific, Rockford, IL), and Alexa Fluor 594-conjugated goat anti-rabbit IgG Abs (A11012; Thermo Fisher Scientific). Mouse anti-PrP monoclonal Ab clone 132 was kindly gifted from M. Horiuchi, Hokkaido University12.
Cells and animals
N2a mouse neuroblastoma (CCL-131, ATCC; kindly gifted from M. Horiuchi, Hokkaido University), N2aC24, N2aC24L1-3, and N2aC24Chm cells11 were maintained at 37˚C with 5% CO2 in air in Dulbecco’s Modified Eagle Medium (D-MEM) (043–30,085; Wako Pure Chemical Industries, Osaka, Japan) supplemented with 1 × Penicillin–Streptomycin Mixed Solution (26,253–84; Nakalai Tesque, Osaka, Japan), which 100 U/mL penicillin and 100 µg/mL streptomycin, and with 10% heat-inactivated fetal bovine serum (FBS) (10,437–028; Gibco, Rockford, IL). Cells were split at 10- to 15-fold dilution every 4 to 5 days by dissociation in phosphate-buffered saline (PBS) (11,482–15; Nakalai Tesque, Osaka, Japan) containing 2.5 g/L trypsin and 1 mM EDTA (32,777–15; Nakalai Tesque). Crl:CD1(ICR) and C57BL/6 mice were purchased from Charles River Laboratories Japan (Kanagawa, Japan).
Virus preparation
Influenza A/WSN/33 (H1N1) virus was prepared as described previously17.
Determination of virus titers
Aliquots from the serially tenfold diluted virus solutions were inoculated into Madin-Darby canine kidney cells (MDCK) (CCL-34, ATCC) in a 96-well plate. After 14 h of incubation at 37˚C, the cells were washed 3 times with PBS and fixed with 4% paraformaldehyde at 4˚C for 30 min. The cells were then washed 3 times with PBS, permeabilized by incubation with 0.3% Triton X-100 in PBS at RT for 20 min. After washing with PBS 3 times, the cells were incubated with anti-influenza-NP Abs in PBS at RT for 2 h. The cells were then washed with PBS 3 times and incubated with Alexa Fluor 488-conjugated goat anti-rabbit IgG Abs in PBS at RT for 1 h. The fluorescent-positive cells were counted using an IX-71 microscope (Olympus, Tokyo, Japan). Infectious units (IFU)/mL were defined as the number of the positive cells in 1 mL of virus solution.
Preparation of mouse serum
Intranasal administration in mice with IAV/WSN (3,000 IFU/20 µL) or PBS was performed as reported previously17. At 14 days post-infection, blood was collected and incubated at 25 °C for 30 min and then at 4 °C for 14 h to make it clot. Serum was harvested by centrifugation at 1,000 × g at 4 °C for 20 min in a T15A61 rotor (Hitachi, Tokyo, Japan) and stored in multiple aliquots at −80 °C until use.
Virus infection of cells
Cells were cultured in a 6-well plate at a density of 6 × 105 cells/well for 16 h, and then infected with IAV/WSN at defined multiplicities of infection (MOIs). Cell viability was indicated by the number of living cells. Mouse serum and oseltamivir (153–03,441; Wako Pure Chemical Industries) were inoculated into cells at the same time as IAV/WSN.
Protease K treatment
All procedures were carried out at 4˚C unless otherwise stated. Cells were rinsed 3 times with PBS (11,482–15; Nakalai Tesque), lysed in a lysis buffer (20 mM Tris–HCl, pH 7.4, 0.5% Triton X-100, 0.2% sodium deoxycholate, 100 mM NaCl), and then centrifuged at 1,500 × g for 5 min to remove insoluble debris. Brain homogenates were prepared as described previously27. The protein concentration in the lysate was determined with the bicinchoninic acid (BCA) protein assay kit (23,225; Pierce, Rockford, IL) using bovine serum albumin (23,209; Pierce) as a standard and adjusted to 3 mg of protein/mL with the lysis buffer. 100 µL of the lysates were digested with 6 µg PK (final concentration, 20 µg PK/mg proteins; 165–21,043; Wako Pure Chemical Industries) at 37 °C for 30 min. For preparation of large amount of proteins, the PK-digested reaction was terminated by addition of Protease Inhibitor Cocktail (25,955–11, Nakalai Tesque) and butanol:methanol (5:1) solution. The insoluble materials were collected by centrifugation at 21,500 × g for 1 h. The resulting pellet was resuspended in a sodium dodecyl sulfate (SDS) sample buffer (62.5 mM Tris–HCl [pH 6.8], containing 5% SDS, 4% ß-mercaptoethanol, 5% glycerol, 0.04% bromophenol blue, 3 mM EDTA) and heated at 95 °C for 10 min before being subjected to Western blotting.
De-glycosylation of PrPSc
Deglycosylation of the PK-digested lysates was performed using peptide N-glycosidase F (PNGase F) (P0704L; New England BioLabs, Beverly, MA) as described previously27. In brief, the PK-digested lysates were denatured in the glycoprotein denaturing buffer (B1704S; New England BioLabs) at 100 °C for 10 min and then treated with PNGase F (P0704L; New England BioLabs) in a reaction buffer containing GlycoBuffer 2 (B3704S; New England BioLabs) and 1% NP-40 (B2704S; New England BioLabs) at 37 °C for 1 h. The lysates were subjected to Western blotting after treatment with SDS sample buffer at 95 °C for 10 min.
Conformational stability assay of PrPSc
Cell lysates were mixed with equal volumes of various concentrations from 0 to 4 M of guanidine hydrochloride (GdnHCl) solution and then incubated at 37 °C for 1 h. The samples were diluted to adjust the final concentration of GdnHCl to 0.2 M by addition of the lysis buffer, and digested with PK at 37 °C for 30 min. The PK treatment was terminated by addition of Protease Inhibitor Cocktail (Nakalai Tesque) and butanol:methanol (5:1) solution. The insoluble materials were collected by centrifugation at 21,500 × g at 4 °C for 1 h in a T15A61 rotor. The resulting pellet was resuspended in the SDS sample buffer, heated at 95 °C for 10 min, and subjected to Western blotting.
Western blotting
Western blotting was performed as described previously27. To evaluate the levels of proteins, their signals were densitometrically measured using LAS-4000 mini-chemiluminescence imaging system (Fuji Film, Tokyo, Japan). Signal intensities were determined by Image Gauge software (Fuji Film).
Immunofluorescence analysis
All manipulations were done at room temperature unless otherwise stated. Cells on coverslips (15 mm No. 1; Matsunami Glass Ind., LTD, Osaka, Japan) were washed three times with PBS and fixed with 4% paraformaldehyde for 15 min. The cells were then washed three times with PBS, treated with 0.1 M glycine in PBS for 10 min, washed three times with PBS, and permeabilized with 0.1% Triton X-100 in PBS for 4 min. For detection of PrPSc, the cells were washed three times with PBS and treated with 5 M guanidium thiocyanate for 10 min12. After washing three times with PBS, the cells were incubated with 5% FBS in PBS for 30 min for blocking and then with the first antibodies in 0.5% FBS in PBS at 4˚C overnight. After removal of the excess antibodies by washing with PBS three times, the cells were incubated with the secondary antibodies and 4’,6-Diamidino-2-phenylindole (DAPI) (340–07,971; Dojindo Laboratories, Kumamoto, Japan) in PBS for 2 h. After washing three times with PBS, the coverslips were mounted with CC/Mount (K002; Diagnostic Biosystems, Pleasanton, CA). Fluorescence images were visualized using BZ-810 (Keyence, Osaka, Japan) and analyzed with BZ-800 analyzer software (Keyence).
Intracerebral inoculation with cell lysates or brain homogenates
Cells (approximately 7.5 × 106 cells) in a 10-cm dish were washed 3 times with PBS and harvested in 500 µL of PBS. The cells were then sonicated and passed through a 27 gauge needle several times to prepare a cell lysate inoculum. The resulting cell lysate inoculum was intracerebrally inoculated into 5- to 6-week-old male ICR mice (20 µL/mouse). 10% (wt/vol) homogenates from single brains in PBS were prepared from terminally ill male mice using a Multibeads shocker (Yasui Kikai, Osaka, Japan) and then diluted to 1% with PBS. Two 1% brain homogenates were mixed in equal amounts and then sonicated and passed through a 27 G needle several times to prepare a brain homogenate inoculum. The resulting inoculum was intracerebrally inoculated into 5- to 6-week-old male ICR mice (20 µL/mouse). Mice were diagnosed as sick when they developed more than five of the following features: emaciation, decreased locomotion, ruffled body hair, ataxic gait, kyphosis, priapism, upright tail, crossing leg, hind leg paresis, and foreleg paresis. Mice were also diagnosed as terminal when they became akinetic.
Immunohistochemistry
Immunohistochemistry was performed as described previously27. In brief, 5 µm-sliced paraffin-embedded brain sections were deparaffinized, rehydrated, and autoclaved in 1 mM HCl at 121 °C for 5 min and washed with PBS. The sections were digested with 50 µg/mL PK in PBS at 37 °C for 30 min and treated with 3 M guanidine thiocyanate at RT for 10 min. After washing with PBS and blocking with 5% FBS in PBS at RT for 1 h, the sections were incubated with 6D11 anti-PrP mAb at RT for 2 h and washed with PBS. The sections were then treated with ImmPRESS reagent anti-mouse IgG (MP-7402; Vector Laboratories, Burlingame, CA) at RT for 1 h and washed with PBS. Signals were visualized by incubation with ImmPACT DAB peroxidase substrate (SK-4105; Vector Laboratories) at RT for 3 min and observed using BIOREVO BZ-9000 microscope (Keyence) with BZ-II analyzer software (Keyence) or BZ-810 (Keyence) with BZ-800 analyzer software (Keyence).
Hematoxylin–eosin (HE) staining
HE staining was performed as described previously27. In brief, paraffin-embedded brain section were deparaffinized, rehydrated, and stained with Mayer’s hematoxylin solution (131–09,665; Wako Pure Chemical Industries) at RT for 5 min and 1% eosin Y solution (051–06,515; Wako Pure Chemical Industries) at RT for 2 min. After washing, the samples were mounted with Softmount (192–16,301; Wako Pure Chemical Industries). Images of sample were observed using BIOREVO BZ-9000 microscope (Keyence, Osaka, Japan) with BZ-II analyzer software (Keyence) or BZ-810 (Keyence) with BZ-800 analyzer software (Keyence).
Vacuolation profile
Vacuoles in 0.1 mm2 areas of the HE-stained brain slices from mice (n = 3 in each mouse group) were counted in various brain regions, including the cerebral cortex, hippocampus, thalamus, and cerebellum.
DNA sequence analysis
The PrP-coding sequences in N2aC24 and N2aC24(R1) cells were amplified from the genomic DNAs purified using the Get pureDNA Kit-Cell, Tissue (GK03; Dojindo Laboratories, Kumamoto, Japan), by polymerase chain reaction (PCR) with Phusion Hot Start II High-Fidelity DNA Polymerase (F-549S; Thermo Fisher Scientific) and a primer pair (5′-TCGGATCCCGTCATCATGGCGAAC-3′, underlined, initiation codon; 5′-CCTCTAGAGCTCATCCCACGATCAG-3′, underlined, stop codon). The resulting DNA fragments were cloned into a pCR-Blunt II-TOPO vector (Invitrogen) and subjected to DNA sequence analysis using an ABI PRISM 3130xl Genetic Analyzer (Applied Biosystems, Foster city, CA).
Supplementary Information
Acknowledgements
This work was supported in part by JSPS KAKENHI Grant Number 18K07499, Brain Science Foundation, Takeda Science Foundation, The Ichiro Kanehara Foundation for the Promotion of Medical Sciences and Medical Care, and Kobayashi Magobe Memorial Medical Foundation to H.H. and JSPS KAKENHI Grant Number 17K19661 and 19H03548 and Grant-in-Aid for Scientific Research on Innovative Areas (Brain Protein Aging and Dementia Control) Grant Number 17H05701 from MEXT to S.S.
Author contributions
H.H., J.C., K.U., and A.D.P. performed experiments. E.T. and H.K. provided IAV/WSN. H.H. and S.S. wrote the manuscript and S.S. designed and supervised the study. All authors reviewed the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1038/s41598-025-00273-2"
Change history
5/6/2025
This article has been retracted. Please see the Retraction Notice for more detail: 10.1038/s41598-025-00273-2
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-89586-6.
References
- 1.d’Errico, P. & Meyer-Luehmann, M. Mechanisms of pathogenic tau and Aβ protein spreading in Alzheimer’s disease. Front. Aging Neurosci.12, 265 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Billings, L. M., Oddo, S., Green, K. N., McGaugh, J. L. & LaFerla, F. M. Intraneuronal Aβ causes the onset of early Alzheimer’s disease-related cognitive deficits in transgenic mice. Neuron45, 675–688 (2005). [DOI] [PubMed] [Google Scholar]
- 3.Jellinger, K. A. Neuropathological aspects of Alzheimer disease, Parkinson disease and frontotemporal dementia. Neurodegener. Dis.5, 118–121 (2008). [DOI] [PubMed] [Google Scholar]
- 4.Duda, J. E., Lee, V. M. & Trojanowski, J. Q. Neuropathology of synuclein aggregates. J. Neurosci. Res.61, 121–127 (2000). [DOI] [PubMed] [Google Scholar]
- 5.De Chiara, G. et al. Infectious agents and neurodegeneration. Mol. Neurobiol.46, 614–638 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ashraf, G. M. et al. The possibility of an infectious etiology of Alzheimer disease. Mol. Neurobiol.56, 4479–4491 (2019). [DOI] [PubMed] [Google Scholar]
- 7.Wozniak, M. A., Itzhaki, R. F., Shipley, S. J. & Dobson, C. B. Herpes simplex virus infection causes cellular beta-amyloid accumulation and secretase upregulation. Neurosci. Lett.429, 95–100 (2007). [DOI] [PubMed] [Google Scholar]
- 8.Jang, H. et al. Highly pathogenic H5N1 influenza virus can enter the central nervous system and induce neuroinflammation and neurodegeneration. Proc. Natl. Acad. Sci. USA106, 14063–14068 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prusiner, S. B. Prions. Proc. Natl. Acad. Sci. USA95, 13363–13383 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weissmann, C. Birth of a prion: spontaneous generation revisited. Cell122, 165–168 (2005). [DOI] [PubMed] [Google Scholar]
- 11.Fujita, K. et al. Effects of a brain-engraftable microglial cell line expressing anti-prion scFv antibodies on survival times of mice infected with scrapie prions. Cell. Mol. Neurobiol.31, 999–1008 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamasaki, T. et al. Characterization of intracellular localization of PrPSc in prion-infected cells using a mAb that recognizes the region consisting of aa 119–127 of mouse PrP. J. Gen. Virol.93, 668–680 (2012). [DOI] [PubMed] [Google Scholar]
- 13.Deleault, N. R., Harris, B. T., Rees, J. R. & Supattapone, S. Formation of native prions from minimal components in vitro. Proc. Natl. Acad. Sci. USA104, 9741–9746 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang, F., Wang, X., Yuan, C. G. & Ma, J. Generating a prion with bacterially expressed recombinant prion protein. Science327, 1132–1135 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferhadian, D. et al. Structural and functional motifs in influenza virus RNAs. Front. Microbiol.9, 559 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edgeworth, J. A. et al. Spontaneous generation of mammalian prions. Proc. Natl. Acad. Sci. USA107, 14402–14406 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chida, J. et al. Prion protein protects mice from lethal infection with influenza A viruses. PLoS Pathog14, e1007049 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collinge, J. & Clarke, A. R. A general model of prion strains and their pathogenicity. Science318, 930–936 (2007). [DOI] [PubMed] [Google Scholar]
- 19.Wadsworth, J. D., Asante, E. A. & Collinge, J. Review: contribution of transgenic models to understanding human prion disease. Neuropathol. Appl. Neurobiol.36, 576–597 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weissmann, C. A “unified theory” of prion propagation. Nature352, 679–683 (1991). [DOI] [PubMed] [Google Scholar]
- 21.Prusiner, S. B. Molecular biology of prion diseases. Science252, 1515–1522 (1991). [DOI] [PubMed] [Google Scholar]
- 22.Lee, J. et al. Review: Laboratory diagnosis and surveillance of Creutzfeldt-Jakob disease. J. Med. Virol.87, 175–186 (2015). [DOI] [PubMed] [Google Scholar]
- 23.Ekstrand, J. J. Neurologic complications of influenza. Semin. Pediatr. Neurol.19, 96–100 (2012). [DOI] [PubMed] [Google Scholar]
- 24.Mak, G. C. K. et al. Influenza A(H5N1) virus infection in a child with encephalitis complicated by obstructive hydrocephalus. Clin. Infect. Dis.66, 136–139 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martyn, C. N. & Osmond, C. Parkinson’s disease and the environment in early life. J. Neurol. Sci.132, 201–206 (1995). [DOI] [PubMed] [Google Scholar]
- 26.Martyn, C. N. Infection in childhood and neurological diseases in adult life. Br. Med. Bull.53, 24–39 (1997). [DOI] [PubMed] [Google Scholar]
- 27.Hara, H. et al. Prion protein devoid of the octapeptide repeat region delays bovine spongiform encephalopathy pathogenesis in mice. J. Virol.92, e01368-17 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.