Abstract
Introduction
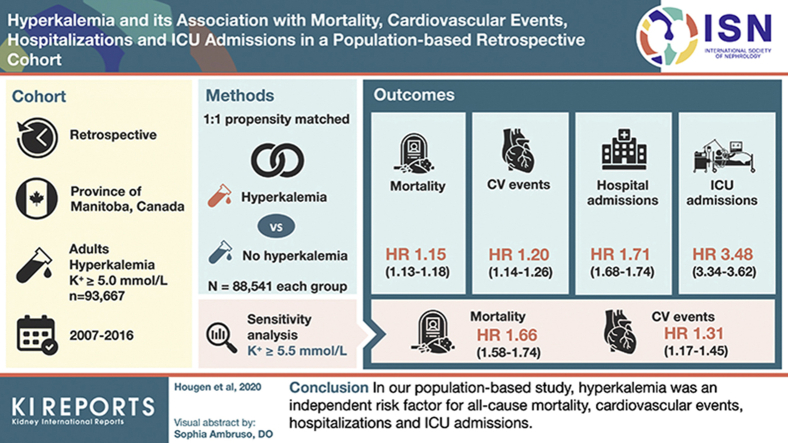
Hyperkalemia is a common, potentially life-threatening condition in patients with chronic kidney disease (CKD). We studied the association between hyperkalemia and mortality, cardiovascular events, hospitalizations, and intensive care unit (ICU) admissions.
Methods
We performed a retrospective cohort study using administrative databases in Manitoba, Canada. All adults (≥18 years of age) with potassium tests between January 2007 and December 2016 were included, with follow-up until March 31, 2017. Propensity score matching was performed among patients with de novo hyperkalemia (serum potassium ≥ 5.0 mmol/l) and patients who were nonhyperkalemic. The association between hyperkalemia and normokalemia and mortality was assessed using multivariate Cox proportional hazards regression models, adjusting for patient characteristics in a 1:1 propensity score–matched sample. Secondary outcomes included cardiovascular events, hospitalizations, and ICU admissions. A sensitivity analysis was performed with hyperkalemia defined as serum potassium ≥ 5.5 mmol/l.
Results
Of 93,667 patients with de novo hyperkalemia, 36% had diabetes mellitus (DM), 28% had CKD, and 21% had heart failure (HF). In the propensity score–matched sample of 177,082 individuals, hyperkalemia was associated with an increased risk for all-cause mortality (hazard ratio [HR] 1.15 [95% confidence interval {CI} 1.13–1.18], P < 0.001), cardiovascular events (HR 1.20 [95% CI 1.14–1.26], P < 0.001), short-term mortality (odds ratio [OR] 1.29 [95% CI 1.24–1.34], P < 0.001), hospitalizations (OR 1.71 [95% CI 1.68–1.74]), and ICU admissions (OR 3.48 [95% CI 3.34–3.62], P < 0.001). Findings were unchanged when a threshold of serum potassium ≥ 5.5 mmol/l was used.
Conclusion
Hyperkalemia was an independent risk factor for all-cause mortality, cardiovascular events, hospitalizations, and ICU admissions. This finding expands our understanding of important clinical outcomes associated with hyperkalemia.
Keywords: diabetes, hyperkalemia, kidney disease, mortality, population
Graphical abstract
See Commentary on Page 1203
Hyperkalemia is a common but potentially life-threatening electrolyte disturbance in patients with CKD, HF, DM, or hypertension.1, 2, 3, 4, 5, 6 Reported incidence in the general population ranges from 2.6% to 7%,4, 5, 6, 7 with rates as high as 73% in patients with CKD.4
Hyperkalemia can result from several mechanisms. Potassium shifts from the intracellular to the extracellular space can occur because of insulin deficiency, metabolic acidosis, or beta adrenergic blockade. Excretion of potassium is decreased in states where the glomerular filtration rate (GFR) or distal sodium delivery is severely reduced or distal tubular potassium secretion mechanisms are impaired. The combination of excess dietary potassium intake and impaired renal excretion can result in sharp increases in serum potassium.8 Several chronic diseases are associated with hyperkalemia. CKD is often associated with decreased GFR, tubulointerstitial dysfunction, and metabolic acidosis, all of which contribute to hyperkalemia.9 In DM, insulin deficiency, hypertonicity in hyperglycemic states, and hyporeninemic hypoaldosteronism may lead to hyperkalemia.9 Similarly, in cardiovascular (CV) disease, especially HF, decreased tubular sodium delivery and the use of medications that interfere with the renin-angiotensin-aldosterone (RAAS) axis can predispose patients to hyperkalemia.9
The potential immediate adverse consequences of acute hyperkalemia are well described in the literature. As a major intracellular cation, elevated extracellular potassium levels can lower the resting cardiac membrane potential and lead to life-threatening conduction blocks and tachyarrhythmias or bradyarrhythmias.2,10 Possible neuromuscular complications include paresthesia, fasciculation, ascending paralysis, and flaccid quadriplegia8 There is no clear threshold of hyperkalemia at which these complications are expected to occur and these manifestations may differ by patient, but higher potassium values generally confer a greater risk.10,11
The potential long-term outcomes associated with hyperkalemia remain poorly described, likely in part because of the difficulty of isolating the effects of hyperkalemia from associated comorbid conditions that confer a poorer outcome. Although several observational studies have described the association between hyperkalemia and excess mortality,4,5 few studies have explored other important clinical outcomes, such as hospitalizations and CV events. We therefore examined the association between de novo hyperkalemia and short term (≤ 30 days) and long-term (> 30 days) all-cause mortality, CV events, hospitalizations, and ICU admissions.
Methods
The study protocol was approved by the health research ethics board at the University of Manitoba (H2018:181 [HS21778]). The reporting of this study follows the STROBE Statement for cohort studies (Supplementary Table S1).
Data Source, Study Design, and Participants
We used linked provincial administrative health databases in Manitoba, Canada to perform a retrospective cohort study. Accessed databases were housed at the Manitoba Center for Health Policy and included the Manitoba Health Insurance Registry (a list of all Manitoba residents), Medical Services and Claims (medical claims data), Canadian Institute for Health Information Discharge Abstract Database (hospitalization events and discharge diagnoses), Shared Health Diagnostic Services (laboratory tests), Drug Program Information Network (medications), and Vital Statistics (deaths). Deidentified information in the databases is linked to each individual through a unique scrambled personal health identification number.
The study period ran from January 1, 2007 through March 31, 2017. We included all adults (≥18 years of age) with de novo hyperkalemia between January 1, 2007 and December 31, 2016. Hyperkalemia was identified through the Shared Health Diagnostic Services laboratory test data that contained laboratory results for inpatient and outpatients’ tests in the province. De novo hyperkalemia was defined as an individual who had a serum potassium test result ≥ 5.0 mmol/l but no previous tests showing hyperkalemia (to exclude recurrent hyperkalemia). The index date was defined as the date of the first serum potassium value qualifying for hyperkalemia. We used 5.0 mmol/l as our hyperkalemia threshold as this cutoff has previously been shown to be of clinical importance.5,12, 13, 14, 15 We also examined hyperkalemia stratified by severity (≥ 5.0, ≥ 5.5, ≥ 6.0, ≥ 6.5, and ≥ 7.0 mmol/l). Patients were followed until the end of the study period (March 31, 2017), death, or migration from the province. We excluded patients from the de novo hyperkalemia group if they had < 365 days of observation time before the index date, if they had received dialysis or a kidney transplant before their index date, or if the incident serum potassium level was ≥ 10.0 mmol/l (to exclude probably spurious results). Baseline comorbidities, such as hypertension, HF, and CKD, were defined using validated codes (Supplementary Table S2).
For our propensity match, when designing our comparator group (patients without hyperkalemia) we selected all patients in the province who had a potassium test during the study period but did not have hyperkalemia as being eligible for inclusion. We randomly assigned an index date to participants without hyperkalemia so that they would have comparable lookback and observation windows for covariate and outcome ascertainment, respectively. Those whose random index date resulted in negative follow-up time were excluded.
Study Outcomes
Outcomes of interest included all-cause mortality, short (≤ 30 days) and long-term (> 30 days) mortality, CV events, hospitalizations, and ICU admissions. Mortality was determined through the Manitoba Health Insurance Registry when the reason for cessation of insurance coverage was death. CV events were defined as hospitalizations where the primary reason was atrial fibrillation, HF, ischemic heart disease, myocardial infarction, peripheral vascular disease, stroke, or unstable angina, according to International Classification of Diseases, 9th and 10th revision codes. Hospitalizations and ICU admissions were defined as all admissions to hospital or the ICU occurring after the index date until the end of follow-up. All hospitalizations and ICU admissions were counted following the index date; therefore, patients may have experienced >1 outcome. We expressed the incidence of our clinical outcomes in patients with de novo hyperkalemia in a rate of number of events per 100 person-years at risk.
Statistical Analysis
We collected patient baseline demographics, comorbidities including DM, CKD, HF, hypertension, and CV disease, previous hospitalization, and medications associated with increased risk of hyperkalemia including RAAS inhibitors (RAASis), azole antifungals, beta-blockers, cyclosporine, digoxin, heparin, prescription nonsteroidal anti-inflammatory drugs, potassium supplements, tacrolimus, and trimethoprim, as well as hyperkalemia recurrences (defined as an additional serum potassium measurement ≥ 5.0 mmol/l that took place >7 days beyond the index date). We used propensity score matching to adjust for the effect of potential confounders (age, sex, baseline comorbidities, and medications) and to isolate the independent contribution of hyperkalemia to outcome probability. We derived the propensity score for propensity of hyperkalemia using logistic regression and reported the C-statistic and max rescaled R2 to evaluate model discrimination and fit. We executed a 1:1 propensity score match without replacement of patients with hyperkalemia to those without hyperkalemia within a caliper distance of 20% of the pooled standard deviation of the logit of the propensity score to create the matched hyperkalemia and control groups. Covariates in the propensity score model included the aforementioned baseline variables. We used a nonparsimonious multivariable logistic regression model, in which hyperkalemia was modeled using all baseline patient characteristics mentioned above. We assessed balance in our groups using the standardized mean difference where a standardized mean difference > 0.1 was considered unbalanced.
We used Cox proportional hazards regression to analyze the effect of hyperkalemia on mortality and CV events. We used logistic regression for the analysis of short-term mortality as censoring is negligible over such short time intervals and we used negative binomial regression to assess the effect of hyperkalemia on all-cause hospitalizations and ICU admissions. The proportional hazards assumption was tested for by plotting Schoenfeld residuals against time and visual inspection for uniformity. Outcomes from our models were expressed in HRs and ORs where appropriate with 95% CIs. All statistical analyses were performed using SAS software (version 9.4; SAS Institute Inc., Cary, NC).
Sensitivity Analyses
Several sensitivity analyses were performed. First, we restricted the study population to individuals who had the de novo hyperkalemia episode in the outpatient setting. Second, we included only patients with ≥ 2 values with serum potassium values ≥ 5.0 mmol/l. Third, we used a threshold value of serum potassium ≥ 5.5 mmol/l to define hyperkalemia. In these analyses we examined the risk of all-cause mortality and CV events in the entire population.
Results
Study Population
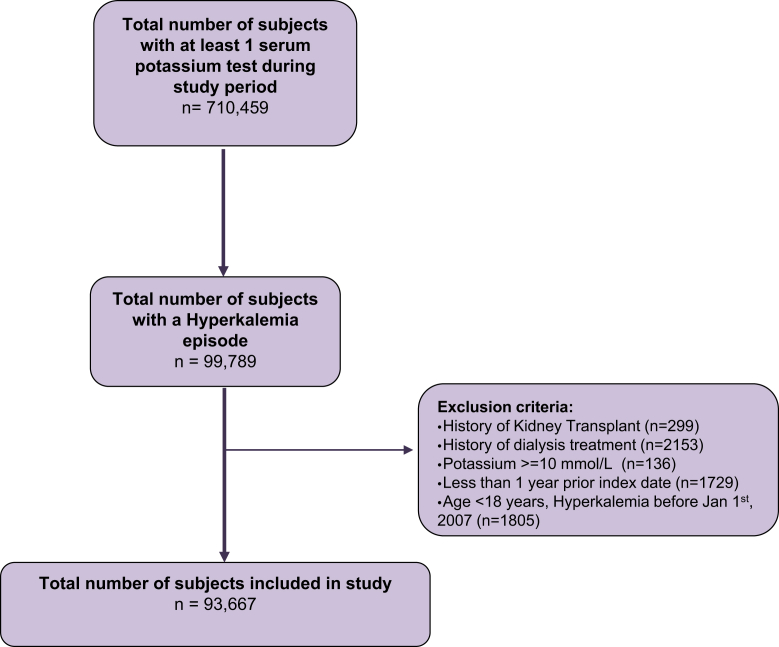
A total of 93,667 patients experienced an episode of de novo hyperkalemia while meeting our inclusion and exclusion criteria (Figure 1). The total follow-up time was 306,698 person-years, corresponding to an average of 3.27 years per person. The baseline characteristics of patients with and without de novo hyperkalemia are summarized in Table 1. Among 93,667 patients, the mean age was 64.15 ± 18.09 years, a higher proportion were male (54.2%), and the mean serum potassium level at baseline was 5.29 mmol/l. Among hyperkalemic events, the majority (80.5%) were mild (5.0 mmol/l to < 5.5 mmol/l), or moderate (13.0%; 5.5 mmol/l to < 6.0 mmol/l). Higher potassium values were uncommon (6.6%), with only 3.6% between 6.0 and < 6.5 mmol/l, 1.5% between 6.5 and <7.0 mmol/l, and 1.5% ≥ 7.0 mmol/l (Table 1). This distribution of potassium values was similar in patients with CKD, DM, HF, or hypertension. Patients with higher potassium levels (≥ 7.0 mmol/l) were younger, had more frequency of CKD and DM compared with those with serum potassium levels between 5 and 5.5 mmol/L (Supplementary Table S3).
Figure 1.
Flow chart of patient selection to the study.
Table 1.
Baseline characteristics stratified by comorbidities
| Characteristic | Overall, n = 93,667 | CKD, n = 26,566 | DM, n = 33,548 | HF, n = 19,374 | HTN, n = 65,161 |
|---|---|---|---|---|---|
| Demographics | |||||
| Age, yr, mean ± SD | 64.15 ± 18.09 | 70.02 ± 16.08 | 66.23 ± 15.04 | 75.57 ± 13.24 | 69.52 ± 14.90 |
| Female, n (%) | 43,541 (45.64) | 13,491 (50.78) | 14,662 (43.70) | 9454 (48.80) | 30,088 (46.17) |
| Hyperkalemia severity, K+ mmol/l | |||||
| ≥5.0–<5.5 | 75,364 (80.5) | 20,683 (77.9) | 26,520 (79.1) | 14,861 (76.7) | 52,316 (80.3) |
| ≥5.5–<6.0 | 12,139 (13.0) | 3917 (14.7) | 4683 (14.0) | 2974 (15.4) | 8683 (13.3) |
| ≥6.0–<6.5 | 3349 (3.6) | 1095 (4.1) | 1283 (3.8) | 870 (4.5) | 2302 (3.5) |
| ≥6.5–<7.0 | 1378 (1.5) | 437 (1.6) | 522 (1.6) | 345 (1.8) | 943 (1.4) |
| ≥7.0 | 1437 (1.5) | 434 (1.6) | 540 (1.6) | 324 (1.7) | 917 (1.4) |
CKD, chronic kidney disease; DM, diabetes mellitus; HF, heart failure; HTN, hypertension; K+, potassium.
Clinical Outcomes
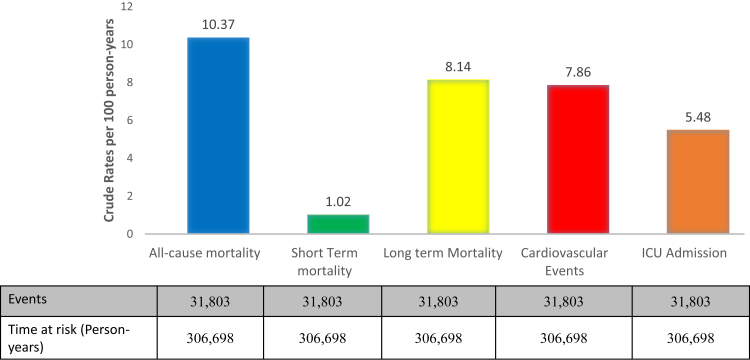
There were 31,803 deaths corresponding to a rate of 10.37 per 100 person-years, with 24,371 (76.63%) deaths occurring >30 days after the index event and 7432 (23.36%) occurring <30 days after the index event (short-term mortality; Figure 2). There were 24,036 CV events, 16,779 ICU admissions, 223,377 all-cause hospitalizations, and 803 instances of acute dialysis after the index hyperkalemia event (crude rates of 7.86/100 person-years, 5.48/100 person-years, 0.74 per person-years, and 6.96/1000 person-years, respectively).
Figure 2.
Outcomes, time at risk, and crude rates. ICU, intensive care unit.
Patients with de novo hyperkalemia from high-risk subgroups consistently experienced higher rates of adverse outcomes compared with the study cohort (Supplementary Table S4).
Propensity-Matched Cohort
In our propensity-matched cohort, 88,541 patients with de novo hyperkalemia were matched to 88,541 patients without a hyperkalemic episode. The matched groups were balanced by age, sex, baseline comorbidities, and the use of medications that affect potassium levels (Table 2). The logistic regression model comparing those with and without hyperkalemia achieved a C-statistic of 0.76 and a max rescaled R2 of 18.0% indicating good discrimination and fit.
Table 2.
Baseline characteristics: Propensity score match of patients with and without hyperkalemia
| Characteristic | With hyperkalemia, n = 88,541 | Without hyperkalemia, n = 88,541 | SMD |
|---|---|---|---|
| Demographics | |||
| Age, yr, mean ± SD | 63.6 ± 18.0 | 64.8 ± 18.3 | 0.066 |
| Female, n (%) | 41,053 (46.4) | 40,969 (46.3) | 0.002 |
| Baseline comorbidities, n (%) | |||
| Chronic kidney disease | 21,977 (24.8) | 20,426 (23.1) | 0.041 |
| Diabetes mellitus | 29,893 (33.8) | 30,128 (34.0) | 0.006 |
| Heart failure | 15,777 (17.8) | 14,624 (16.5) | 0.034 |
| Hypertension | 60,386 (68.2) | 63,038 (71.2) | 0.065 |
| Cardiovascular disease | 13,811 (15.6) | 13,286 (15.0) | 0.016 |
| Previous hospitalization | 65,800 (74.3) | 65,857 (74.4) | 0.001 |
| Medications, n (%) | |||
| RAAS inhibitors | |||
| Current usersa | 29,816 (33.7) | 29,490 (33.3) | 0.008 |
| Nonusersb | 11,383 (12.8) | 11,510 (13.0) | 0.004 |
| Never usersc | 47,342 (53.5) | 47,541 (53.7) | 0.004 |
| Azole antifungals | |||
| Current users | 194 (0.2) | 159 (0.2) | 0.009 |
| Nonusers | 5072 (5.7) | 5026 (5.7) | 0.002 |
| Never users | 83,356 (94.1) | 83,275 (94.1) | 0.004 |
| Beta-blockers | |||
| Current users | 19,363 (21.9) | 19,304 (21.8) | 0.002 |
| Nonusers | 7116 (8.0) | 7064 (8.0) | 0.002 |
| Never users | 62,062 (70.1) | 62,173 (70.2) | 0.003 |
| Cyclosporine | |||
| Current users | 89 (0.1) | 74 (0.1) | 0.005 |
| Nonusers | 58 (0.1) | 57 (0.1) | <0.001 |
| Never users | 88,394 (99.8) | 88,410 (99.9) | 0.004 |
| Digoxin | |||
| Current users | 2620 (3.0) | 2510 (2.8) | 0.007 |
| Nonusers | 1230 (1.4) | 1119 (1.3) | 0.010 |
| Never users | 84,691 (95.7) | 84,912 (95.9) | 0.012 |
| Heparin | |||
| Current users | 479 (0.5) | 450 (0.5) | 0.004 |
| Nonusers | 3284 (3.7) | 3355 (3.8) | 0.004 |
| Never users | 84,778 (95.8) | 84,736 (95.7) | 0.002 |
| Prescription NSAIDs | |||
| Current users | 4728 (5.4) | 4665 (5.3) | 0.003 |
| Nonusers | 28,574 (32.3) | 29,287 (33.0) | 0.017 |
| Never users | 55,239 (62.4) | 54,589 (61.7) | 0.015 |
| Potassium supplements | |||
| Current users | 2477 (2.8) | 2464 (2.8) | <0.001 |
| Nonusers | 4620 (5.2) | 4504 (5.1) | 0.006 |
| Never users | 81,444 (92.0) | 81,573 (92.1) | 0.005 |
| Tacrolimus | |||
| Current users | 79 (0.1) | 61 (0.1) | 0.007 |
| Nonusers | 19 (∼0) | 13 (∼0) | 0.005 |
| Never users | 88,446 (99.9) | 88,467 (99.9) | 0.008 |
| Trimethoprim | |||
| Current users | 1663 (1.9) | 1481 (1.7) | 0.015 |
| Nonusers | 16,378 (18.5) | 16,640 (18.8) | 0.007 |
| Never users | 70,500 (79.6) | 70,420 (79.5) | 0.002 |
NSAID, nonsteroidal anti-inflammatory drug; RAAS, renin-angiotensin-aldosterone system; SD, standard deviation; SMD, standardized mean difference.
Defined as a current user if 150% of the days’ supply of the last prescription of a given exposure covers the date of incident hyperkalemia.
Defined as patients with a prescription for a given exposure for which 150% of the days’ supply of the last prescription days’ supply did not overlap with the index date.
Patients with no record of any prescription for an exposure before the index date.
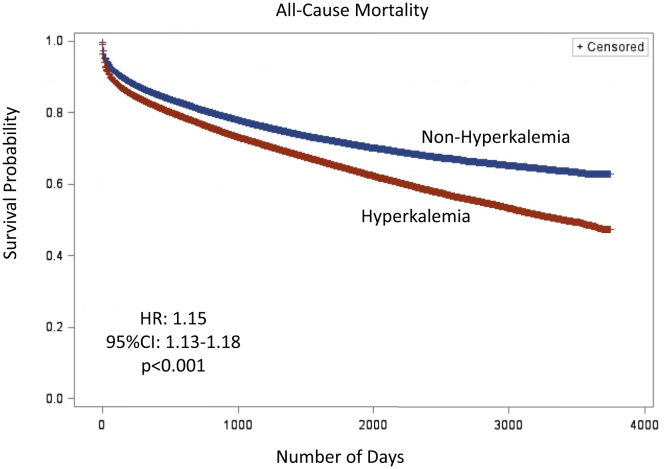
Our Cox proportional hazards regression models showed that a de novo episode of hyperkalemia was associated with a higher risk of all-cause mortality (HR 1.15 [95% CI 1.13–1.18], P < 0.001) and CV events (HR 1.20 [95% CI 1.14–1.26], P < 0.001) in our propensity-matched cohorts (Table 3). The Kaplan–Meier survival curve for all-cause mortality is shown in Figure 3. Short-term mortality was also significantly increased by an episode of hyperkalemia (OR 1.29 [95% CI 1.24–1.34], P < 0.001) in our logistic regression model (Table 4). In our negative binomial regression models, the incidence of hospitalizations (OR 1.71 [95% CI 1.68–1.74], P < 0.001) and ICU admissions (OR 3.48 [95% CI 3.34–3.62], P < 0.001) were also significantly increased after an episode of hyperkalemia (Table 5).
Table 3.
Hazard ratios with 95% confidence intervals and P values of Cox proportional hazards regression models
| Model type | All-cause mortality |
Cardiovascular events |
||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Unadjusted | 3.59 (3.55–3.64) | <0.001 | 4.59 (4.49–4.68) | <0.001 |
| Propensity-matched | 1.15 (1.13–1.18) | <0.001 | 1.20 (1.14–1.26) | <0.001 |
CI, confidence interval; HR, hazard ratio.
Figure 3.
Kaplan–Meier plot for all-cause mortality in patients with and without hyperkalemia. CI, confidence interval; HR, hazard ratio.
Table 4.
Odds ratios with 95% confidence intervals and P values of logistic regression models
| Model type | Short-term mortality |
|
|---|---|---|
| OR (95% CI) | P value | |
| Unadjusted | 3.64 (3.54–3.74) | <0.001 |
| Propensity-matched | 1.29 (1.24–1.34) | <0.001 |
CI, confidence interval; OR, odds ratio.
Table 5.
Odds ratios with 95% confidence intervals and P values of negative binomial regression models
| Model type | Hospitalizations |
ICU admissions |
||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Unadjusted | 2.19 (2.16–2.22) | <0.001 | 8.04 (7.84–8.25) | <0.001 |
| Propensity-matched | 1.71 (1.68–1.74) | <0.001 | 3.48 (3.34–3.62) | <0.001 |
CI, confidence interval; OR, odds ratio.
Sensitivity Analyses
All sensitivity analyses yielded similar associations of hyperkalemia and all-cause mortality and CV events. In the propensity-matched score sample, those with ≥2 instances of hyperkalemia had a higher risk of all-cause mortality (HR 1.94 [95% CI 1.66–2.28]) and CV events (HR 1.83 [95% CI 1.29–2.61]) compared with those without hyperkalemia. Similarly, in the cohort limited to those with hyperkalemia in the outpatient setting, the results were similar (all-cause mortality: HR 1.05 [95% CI 1.02–1.08]; CV events: HR 1.18 [95% CI 1.12–1.24]).
Finally, the sensitivity analyses among those patients with a serum potassium level ≥ 5.5 mmol/l yielded similar associations between hyperkalemia and all-cause mortality (HR 1.66 [95% CI 1.58–1.74], P < 0.001) and CV events (HR 1.31 [95% CI 1.17–1.45]; Supplementary Tables S5 and S6).
Discussion
In this large, population-based cohort study, we found that hyperkalemia was independently associated with an increased risk of all-cause mortality, CV events, hospitalizations, and ICU admissions. These findings were independent of the hyperkalemia threshold (serum potassium ≥ 5.0 and ≥ 5.5 mmol/l). Taken together, these findings suggest that a single episode of hyperkalemia is associated with a major disease burden that extends well beyond the acute episode, and that elevated potassium levels may contribute to increased health care costs in both the short term and the long term.
Our findings are in keeping with the results of other observational studies on clinical outcomes associated with hyperkalemia. A large cohort study of 900,000 patients receiving medical care from multiple health care providers across the United States examined the association between serum potassium and all-cause mortality, comparing mortality rates in patients with risk factors of HF, CKD, and DM at different ranges of potassium values.5 They found that after adjusting for multiple factors, patients with DM, HF, and CKD had significantly higher mortality rates than control subjects. The study further found that even mild hyperkalemia (potassium 5.0–< 5.5 mmol/l) was independently associated with increased rates of mortality.5
A recent meta-analysis combining 27 international cohorts in the CKD Prognosis Consortium and including >1 million patients has summarized the relationship between serum potassium and all-cause mortality, CV-associated mortality, and end-stage renal disease. This meta-analysis concluded that hyperkalemia > 5.5 mmol/l was associated with an increased risk of all-cause mortality (HR 1.22 [95% CI 1.15–1.29]) as well as CV mortality and end-stage renal disease when compared with a serum potassium of 4.2 mmol/l.4
Fewer studies have looked at other long-term outcomes, such as CV events, hospitalizations, and ICU admissions. In a systematic review of 14 studies examining hyperkalemia in patients with CKD, HF, type 2 DM, or hypertension, the risk of hospitalization was increased with increasing severity of hyperkalemia. This review identified a limited number of studies that reported an association between hyperkalemia and major adverse cardiac events.16
Our study is unique and builds upon the above findings. Our results are externally valid, confirming the previous studies showing an increased association between hyperkalemia and mortality. Our findings are novel in that we additionally found that the association persists beyond 30 days and is associated with long-term mortality. Our study adds to the limited data available regarding clinical outcomes of hospitalizations and CV events and is, to our knowledge, the first study to examine the association between hyperkalemia and ICU admissions. ICU admissions are important because they often carry disproportionately high costs, and morbidity and mortality and should be considered in health economic evaluations of therapies targeting hyperkalemia.
The reasons for the association between hyperkalemia and an increased risk of adverse events may be explained in part by the direct proarrhythmic effects of hyperkalemia, which may result in hypotension, myocardial ischemia, and death.4 It is also possible that some outcomes may result from permanent discontinuation of medications with known CV benefit (e.g., RAASis). In some cases, adverse events may be associated with treatment with sodium polystyrene sulfonate, which has been linked with the rare but serious risk of bowel necrosis.17, 18, 19 In other cases, adverse outcomes may relate to recurrent hyperkalemia, although in our cohort only 36.0% of patients had ≥1 recurrence of hyperkalemia during the study period. Our study also has important research implications. The increased risk of adverse clinical outcomes demonstrated in our study suggests that substantial short- and long-term benefits to patients, payers, and health systems may accrue following the development of safe and effective treatments for hyperkalemia. In this regard, it will be important for future clinical studies to examine whether the use of newer serum potassium–lowering agents, such as patiromer and sodium zirconium cyclosilicate,20, 21, 22, 23, 24, 25, 26, 27, 28, 29 can help prevent short-term complications related to hyperkalemia; allow the resumption and continued use of hyperkalemia-limited cardioprotective agents (e.g., RAASis and mineralocorticoid antagonists); prevent long-term mortality, CV events, and hospitalizations; and reduce health care costs. Studies evaluating the risk versus benefit of resuming medications that contribute to hyperkalemia but which provide CV or other benefits, such as RAASis, is another area of research that should be prioritized.
Our study has several strengths. First is the use of propensity score matching, a statistical method that attempts to account for observable factors that may affect the likelihood of a patient having an outcome.30 In our cohort, we were able to match 88,541 individuals of 93,667 initially identified hyperkalemic episodes, which resulted in groups that were comparable in baseline characteristics. Therefore, the exclusion of those who could not be suitably matched resulted in only a small reduction in overall sample. Other strengths include our analysis of relevant clinically important outcomes for which there were previously limited data in the literature. The use of a large, population-based sample also adds to the generalizability of our study. We included patients with comorbidities known to be risk factors for hyperkalemia but did not limit our study to any specific high-risk group, such as patients with CKD.
Limitations of the study include its observational nature. While propensity matching reduces the effect of confounding, we cannot exclude residual confounding. In addition, there may have been some data not captured by the databases used in the study. We could not adjust for patient race because those data were not available. The proportional hazards assumption was tested and held, however time dependent is a study limitation. Some over-the-counter medications, such as nonsteroidal anti-inflammatory drugs, would not have been captured, and outpatient serum potassium tests performed at laboratories not affiliated with Shared Health Diagnostic Services were not included, which could represent ~30% of laboratories in Manitoba.
In this large, population-based cohort study of hyperkalemic events and associated adverse clinical outcomes, we found hyperkalemia to be an independent risk factor for short- and long-term mortality, CV events, hospitalizations, and ICU admissions. These findings highlight the substantial health burden imposed by an episode of hyperkalemia and identify additional clinically important outcomes that newer therapies targeting hyperkalemia should seek to improve.
Disclosure
NT has received research support and honoraria from AstraZeneca Canada. The other authors declared no competing interests.
Acknowledgments
This research was supported through funding provided by AstraZeneca Canada. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author Contributions
All authors were involved in the acquisition, analysis, or interpretation of the data and had a role in writing this manuscript. NT had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. NT created the concept and design. IH, PK, CR, CB, and NT provided critical revision of the manuscript for important intellectual content. SJL and RW performed statistical analysis. NT obtained funding for the study and supervised the study.
Footnotes
Table S1. The STROBE Statement: Guidelines for reporting observational studies checklist.
Table S2. Code definitions for baseline comorbidities.
Table S3. Baseline Characteristics stratified by serum potassium levels.
Table S4. Outcomes, time at risk, and crude rates by high-risk subgroup.
Table S5. Baseline characteristics: Propensity score match of patients with and without hyperkalemia.
Table S6. Hazard ratios with 95% confidence intervals and P values of Cox proportional hazards regression models.
Supplementary Material
Table S1. The STROBE Statement: Guidelines for reporting observational studies checklist.
Table S2. Code definitions for baseline comorbidities.
Table S3. Baseline Characteristics stratified by serum potassium levels.
Table S4. Outcomes, time at risk, and crude rates by high-risk subgroup.
Table S5. Baseline characteristics: Propensity score match of patients with and without hyperkalemia.
Table S6. Hazard ratios with 95% confidence intervals and P values of Cox proportional hazards regression models.
References
- 1.Einhorn L., Zhan M., Hsu V. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169:1156–1162. doi: 10.1001/archinternmed.2009.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montford J., Linas S. How dangerous is hyperkalemia? J Am Soc Nephrol. 2017;28:3155–3165. doi: 10.1681/ASN.2016121344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gilligan S., Raphael K. Hyperkalemia and hypokalemia in CKD: prevalence, risk factors, and clinical outcomes. Adv Chronic Kidney Dis. 2017;24:315–318. doi: 10.1053/j.ackd.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Kovesdy C., Matsushita K., Sang Y. Serum potassium and adverse outcomes across the range of kidney function: a CKD Prognosis Consortium meta-analysis. Eur Heart J. 2018;39:1535–1542. doi: 10.1093/eurheartj/ehy100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins A., Pitt B., Reaven N. Association of serum potassium with all-cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017;46:213–221. doi: 10.1159/000479802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nilsson E., Gasparini A., Arnlov J. Incidence and determinants of hyperkalemia and hypokalemia in a large healthcare system. Int J Cardiol. 2017;245:277–284. doi: 10.1016/j.ijcard.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 7.Singer A., Thode H., Jr., Peacock W. A retrospective study of emergency department potassium disturbances: severity, treatment, and outcomes. Clin Exp Emerg Med. 2017;4:73–79. doi: 10.15441/ceem.16.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palmer B., Clegg D. Diagnosis and treatment of hyperkalemia. Cleve Clin J Med. 2017;84:934–942. doi: 10.3949/ccjm.84a.17056. [DOI] [PubMed] [Google Scholar]
- 9.Kovesdy C. Updates in hyperkalemia: Outcomes and therapeutic strategies. Rev Endocr Metab Disord. 2017;18:41–47. doi: 10.1007/s11154-016-9384-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiss J., Qu Z., Shivkumar K. The electrophysiology of hypo- and hyperkalemia. Circ Arrhythm Electrophysiol. 2017;10 doi: 10.1161/CIRCEP.116.004667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kovesdy C. Management of hyperkalemia: an update for the internist. Am J Med. 2015;128:1281–1287. doi: 10.1016/j.amjmed.2015.05.040. [DOI] [PubMed] [Google Scholar]
- 12.Faxén J., Xu H., Evans M., Jernberg T., Szummer K., Carrero J.-J. Potassium levels and risk of in-hospital arrhythmias and mortality in patients admitted with suspected acute coronary syndrome. Int J Cardiol. 2019;274:52–58. doi: 10.1016/j.ijcard.2018.09.099. [DOI] [PubMed] [Google Scholar]
- 13.Fitch K., Woolley J.M., Engel T., Blumen H. The clinical and economic burden of hyperkalemia on medicare and commercial payers. Am Health Drug Benefits. 2017;10:202–210. [PMC free article] [PubMed] [Google Scholar]
- 14.Jain N., Kotla S., Little B. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109:1510–1513. doi: 10.1016/j.amjcard.2012.01.367. [DOI] [PubMed] [Google Scholar]
- 15.Goyal A., Spertus J., Gosch K. Serum potassium levels and mortality in acute myocardial infarction. JAMA. 2012;307:157–164. doi: 10.1001/jama.2011.1967. [DOI] [PubMed] [Google Scholar]
- 16.Palacka E., Grandy S., Darlington O., McEwan P., van Doornewaard A. Associations between serum potassium and adverse clinical outcomes: a systematic literature review. Int J Clin Pract. 2019;00 doi: 10.1111/ijcp.13421. [DOI] [PubMed] [Google Scholar]
- 17.US Food and Drug Administration website Kayexalate sodium polystyrene sulfonate, USP. https://www.accessdata.fda.gov/drugsatfda_docs/label/2009/011287s022lbl.pdf Available at:
- 18.Noel J., Bota S., Petrcich W. Risk of hospitalization for serious adverse gastrointestinal events associated with sodium polystyrene sulfonate use in patients of advanced age. JAMA Intern Med. 2019;179:1025–1033. doi: 10.1001/jamainternmed.2019.0631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harel Z., Harel S., Shah P., Wald R., Perl J., Bell C. Gastrointestinal adverse events with sodium polystyrene sulfonate (kayexalate) use: a systematic review. Am J Med. 2013;126:264e9–264e24. doi: 10.1016/j.amjmed.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 20.Kosiborod M., Rasmussen H., Lavin P. Effect of sodium zirconium cyclosilicate on potassium lowering for 28 days among outpatients with hyperkalemia. The HARMONIZE randomized clinical trial. JAMA. 2014;312:2223–2233. doi: 10.1001/jama.2014.15688. [DOI] [PubMed] [Google Scholar]
- 21.Bakris G., Pitt B., Weir M. Effect of patiromer on serum potassium level in patients with hyperkalemia and diabetic kidney disease. The ANETHYST-DN randomized clinical trial. JAMA. 2015;314(2):151–161. doi: 10.1001/jama.2015.7446. [DOI] [PubMed] [Google Scholar]
- 22.Anker S., Kosiborod M., Zannad F. Maintenance of serum potassium with sodium zirconium cyclosilicate (ZS-9) in heart failure patients: results from a phase 3 randomized, double-blind, placebo-controlled trial. Eur J Heart Fail. 2015;17:1050–1056. doi: 10.1002/ejhf.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ash S., Singh B., Lavin P., Stavros F., Rasmussen H. A phase 2 study on the treatment of hyperkalemia in patients with chronic kidney disease suggests that the selective potassium trap, ZS-9, is safe and efficient. Kidney Int. 2015;88:404–411. doi: 10.1038/ki.2014.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Packham D., Rasmussen H., Lavin P. Sodium zirconium cyclosilicate in hyperkalemia. N Engl J Med. 2015;372:222–231. doi: 10.1056/NEJMoa1411487. [DOI] [PubMed] [Google Scholar]
- 25.Kloner R., Gross C., Yuan J., Conrad A., Pergola P. Effect of patiromer in hyperkalemic patients taking and not taking RAAS inhibitors. J Cardiovasc Pharmacol Ther. 2018;23:524–531. doi: 10.1177/1074248418788334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spinowitz B.S., Fishbane S., Pergola P.E. Sodium zirconium cyclosilicate among individuals with hyperkalemia: a 12-month phase 3 study. Clin J Am Soc Nephrol. 2019;14:798–809. doi: 10.2215/CJN.12651018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agarwal R., Rossignol P., Romero A. Patiromer versus placebo to enable spironolactone use in patients with resistant hypertension and chronic kidney disease (AMBER): a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2019;394:1540–1550. doi: 10.1016/S0140-6736(19)32135-X. [DOI] [PubMed] [Google Scholar]
- 28.Meaney C., Beccari M., Yang Y., Zhao J. Systematic review and meta-analysis of patiromer and sodium zirconium cyclosilicate: a new armamentarium for the treatment of hyperkalemia. Pharmacotherapy. 2017;37:401–411. doi: 10.1002/phar.1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Das S., Dey J., Sen S., Mukherjee R. Efficacy and safety of patiromer in hyperkalemia: a systematic review and meta-analysis. J Pharm Pract. 2018;31:6–17. doi: 10.1177/0897190017692921. [DOI] [PubMed] [Google Scholar]
- 30.Raghunathan K., Layton B., Ohnuma T., Shaw A. Observational research using propensity scores. Adv Chronic Kidney Dis. 2016;23:367–372. doi: 10.1053/j.ackd.2016.11.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.