Abstract
Background:
Despite the availability of effective and affordable treatments, only 14% of hypertensive Indians have controlled blood pressure. Increased hypertension treatment coverage (the proportion of individuals initiated on treatment) and adherence (proportion of patients taking medicines as recommended) promise population health gains. However, governments and other payers will not invest in a large-scale hypertension control program unless it is both affordable and effective.
Objective:
To investigate if a national hypertension control intervention implemented across the private and public sector facilities in India could save overall costs of CVD prevention and treatment.
Methods:
We developed a discrete-time microsimulation model to assess the cost-effectiveness of population-level hypertension control intervention in India for combinations of treatment coverage and adherence targets. Input clinical parameters specific to India were obtained from large-scale surveys such as the Global Burden of Disease as well as local clinical trials. Input hypertensive medication cost parameters were based on government contracts. The model projected antihypertensive treatment costs, avoided CVD care costs, changes in disability-adjusted life year (DALYs) and incremental cost per DALY averted (represented as incremental cost-effectiveness ratio or ICER) over 20 years.
Results:
Over 20 years, at 70% coverage and adherence, the hypertension control intervention would avert 1.68% DALYs and be cost-saving overall. Increasing adherence (while keeping coverage constant) resulted in greater improvement in cost savings compared to increasing coverage (while keeping adherence constant). Results were most sensitive to the cost of antihypertensive medication, but the intervention remained highly cost-effective under all one-way sensitivity analyses.
Conclusion:
A national hypertension control intervention in India would most likely be budget neutral or cost-saving if the intervention can achieve and maintain high levels of both treatment coverage and adherence.
Keywords: hypertension, cost-effectiveness, developing countries, health policy, preventive care
Introduction
Globally, cardiovascular diseases (CVDs) account for 31% of all deaths, 80% of which occur in low- and middle-income countries (LMICs) [1]. India, one of the largest LMICs, is estimated to have suffered an economic loss of $94 billion due to CVDs in 2017 [2]. In the last 20 years, the annual incidence of CVDs has almost doubled to 7.4 million, and 60 million Indians are currently living with CVDs [3]. The burden of CVDs in India is projected to increase further due to population growth and aging, which could jeopardize the recent progress in poverty reduction [2,4].
High blood pressure is the single largest preventable risk factor for CVDs and is estimated to account for more than half of the CVD deaths [5]. Low cost and effective blood-pressure lowering treatments are available, which can reduce the morbidity and mortality associated with hypertension [6]. However, in India, 14% of hypertensive individuals above 50 years of age and 8% of hypertensive individuals younger than 50 have their blood pressure under control, largely due to low awareness of hypertensive status and lack of medication adherence [6,7,8,9,10].
Blood pressure control can be improved by implementing a package of increased hypertension screening and a simplified hypertension treatment protocol, enabled by trained health care workers and a robust health information system [9,11,12,13]. Such an intervention, if scaled to cover 70% of all hypertensive individuals worldwide, could avert 7.4 million CVD-related deaths in the next 25 years [6,14]. Lifestyle modifications such as increased physical activity, reduced sodium and trans-fat intake, and tobacco cessation can further improve health outcomes, but lifestyle modifications were found to be difficult to maintain [15,16]. Thus, several pilot projects for improving antihypertensive care delivery are currently being implemented in India based on the principles of increased status awareness and medication adherence [9,17,18]. However, their focus on public health facilities severely limit their potential impact as more than 80% of the hypertensive patients seek treatment in the private sector, where chronic care is often suboptimal and leads to poor outcomes [10,19,20,21]. Thus, a public health intervention to improve hypertension control must cover both public and private sectors, perhaps through a government-run health insurance program. But, given the government’s financial constraints, this is more likely if the intervention is cost-saving and affordable for the health system and not merely ‘cost-effective’ [22,23].
In our study, we set out to investigate if a national hypertension control intervention implemented across the private and public sector facilities could save overall costs of CVD prevention and treatment. We determine the level of coverage and adherence required for the intervention to be cost-saving. We further investigate the total budgetary resources required for such an intervention and the expected savings in healthcare expenditure due to the prevention of CVDs.
Methods
Microsimulation Model
We developed a discrete-time microsimulation model for two hypothetical cohorts comprising of 10,000 individuals each (males and females) of 40–69 years of age at the beginning of the simulation. We calculated the costs and disability-adjusted life years (DALYs) for these cohorts over 20 years using cycle time of one month. The outcome measured was the incremental cost per DALY averted (represented as incremental cost-effectiveness ratio or ICER). Our analysis was conducted from the perspective of the government as a payor that allocates budget for such an intervention.
The structure of the model is illustrated in Figure 1. Each individual is at risk for myocardial infarction (MI) or stroke based on their risk factors, which include age, sex, systolic blood pressure, smoking habit, and body mass index. After a first event, individuals with history of MI or stroke (together defined as cardiovascular disease or CVD in our study) face a higher risk of death as well as recurrence of MI or stroke compared to an individual without the history. Individuals on antihypertensive medication experience reduced risk of CVD. We used Python 3.7 to construct the model and perform the analysis.
Figure 1.
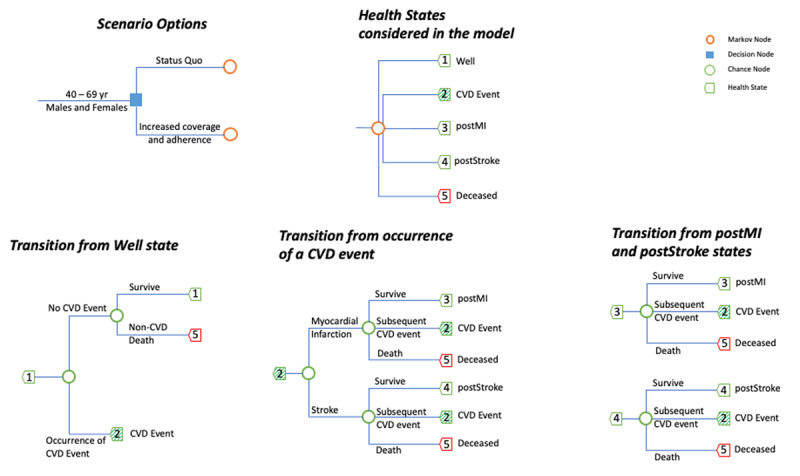
Structure of the microsimulation model.
The above microsimulation model was used with a cycle time of one month to estimate costs and DALYs in two hypothetical cohort of 10,000 individuals (males and females respectively) with ages 40-69yr at the start of the simulation. Multiple scenarios with combinations of coverage and adherence were simulated, and the incremental cost per DALY averted was calculated in reference to the status quo of 17% coverage and 30% adherence. The blue square indicates the choice between various intervention scenarios, and the orange circle indicates the chosen intervention. The health states (indicated by green pentagon) comprises of (1) well (no past CVD event), (2) occurrence of a CVD event, (3) surviving post a myocardial infarction (postMI), (4) surviving post a stroke (postStroke), and (5) deceased state. The blue-colored branches from each heath state lead to another heath state based on the probability of the intermediate event (indicated by the green circle). The (2) CVD event is a transitionary markov state and comprises of either an occurrence of MI or stroke.
CVD = Cardiovascular disease, MI = Myocardial infarction, DALYs = Disability adjusted life year.
Probability of Clinical Events
We used the WHO Study on global AGEing and adult health (SAGE) dataset to obtain levels of risk factors for the Indian population of relevant ages and used the Globorisk calculator to determine the risk of an MI or stroke based on these risk factors [24,25]. Survival after a CVD event was obtained from the Global Burden of Disease (GBD) 2017 study [26], and all-cause mortality rates were determined using India-specific WHO lifetables [27]. CVD risk reduction due to hypertension treatment was based on age, initial systolic blood pressure (SBP) and medication dosage for each individual [28]. The 30-day risk of death after MI and stroke were derived from local studies [29,30], and the death rate after non-fatal CVD event was calibrated based on GBD data. Probabilities for reinfarction and recurrence of stroke were obtained from published literature [31,32,33]. Selected input values and their sources are shown in Table 1, with the complete list of values provided in Table S2–S7 of the Appendix.
Table 1.
Select input parameters for the microsimulation model.
| Input Parameter | Value | Source(s) |
|---|---|---|
| Population characteristics | ||
| Individual profiles consisting of Age, Sex, Systolic blood pressure, BMI and Smoking habit | WHO SAGE [24] | |
| Baseline status-awareness ratio | 40.8% | PURE Study [34] |
| Baseline treatment initiation ratio | 77.7% | PURE Study [34] |
| Baseline treatment persistence ratio | 61% | Van Wijk et al. 2005 [35] |
| Baseline medication compliance ratio | 50.3% | Dennis et al. 2011 [36] |
| Blood pressure increase with increase in age of an individual | Age and initial SBP-specific | Simulated based on model developed by Bellows et al. 2019 [37] |
| Mortality and risk of cardiovascular diseases | ||
| Non-CVD death rate | 0.005–0.176 (Age- and sex- specific)# | Calculated from WHO lifetables and GBD 2017 [3, 27] |
| Probability of first-time cardiovascular disease (CVD) event | Individual risk characteristic specific | Obtained from the Globorisk Office Calculator standardized for India [25] |
| Acute CVD Events | ||
| Myocardial Infarction (MI) | ||
| Probability of MI if CVD event occurs | 37.6– 66.7% (Age- and sex- specific)# | Calculated based on GBD 2017 [3] |
| 30-day fatality | 0.01–0.13 (Age- and sex– specific)# | Calibrated based on findings of Huffman et al. 2018 [29] |
| Reinfarction (in 30 days) | 0.0120 (0.0099–0.0141)ψ | ACS QUIK Study by Huffman et al. 2018 [29] |
| Acute Stroke (in 30 days) | 0.0060 (0.0045–0.0075)ψ | ACS QUIK Study by Huffman et al. 2018 [29] |
| Stroke | ||
| Probability of Stroke if CVD event occurs | 33.2–62.3% (Age- and sex- specific)# | Calculated based on GBD 2017 [3] |
| 30-day fatality | 0.12, 0.13 (Sex-specific)# | Calibrated based on a multi-site study by Pandian and Sudhan 2013 [30] |
| Repeat Stroke (in 30 days) | 0.15 (0.1–0.2)ψ | Petty et al. 1998 [32] |
| Chronic CVD Events | ||
| Ischemic Heart Disease (IHD) | ||
| Monthly risk of mortality | 0.001–0.019 (Age- and sex- specific)# | Calibrated based on GBD 2017 [3] |
| Reinfarction | 0.079 (0.073–0.085)ψ | Based on Steg et al. 2007 [31] and derived by Lin et al. 2019 [33] |
| Acute Stroke | 0.014 (0.012–0.016)ψ | Based on Steg et al. 2007 [31], and derived by Lin et al. 2019 [33] |
| Stroke | ||
| Monthly risk of mortality | 0.001–0.013 (Age- and sex- specific)# | Calibrated based on GBD 2017 [3] |
| Acute MI | 0.043 (0.038–0.048)ψ | Based on Steg et al. 2007 [31], and derived by Lin et al. 2019 [33] |
| Acute Stroke | 0.037 (0.033–0.041)ψ | Based on Steg et al. 2007 [31], and derived by Lin et al. 2019 [33] |
| Relative risk of fatality for an individual with two or more CVD events | 1.5 | Smolina et al. 2012 [38] |
| Effect of antihypertensive medication | ||
| Medication protocol for an individual | Initial SBP-specific# | Based on India Hypertension Control Initiative (IHCI) implemented in Punjab [39,40] |
| IHD relative risk due to medication | 0.32–0.89 (Age- and initial SBP-specific)# | Based on findings by Law et al. 2009 [28] |
| Stroke relative risk due to medication | 0.20–0.89 (Age- and initial SBP-specific)# | Based on findings by Law et al. 2009 [28] |
| IHD relative risk if partially adherent | 0.66–0.95 (Age- and initial SBP-specific) | Calculated based on a linear relationship between adherence and efficacy as considered by Cherry et al. 2009 [41] |
| Stroke relative risk if partially adherent | 0.60–0.95 (Age- and initial SBP-specific) | Calculated based on a linear relationship between adherence and efficacy as considered by Cherry et al. 2009 [41] |
| Costs | ||
| Programmatic Cost of Intervention | $0.13 per individual per annum# | Calculated from resource costs of India Hypertension Control Initiative |
| Antihypertensive treatment | ||
| Antihypertensive medication (per individual per annum) in public sector | $0.88–17.90 (Drug and dosage specific)§ | Drug costs based on government rate contracts [42], and the type and dosage drug dispensed is based on the treatment protocol |
| Antihypertensive medication (per individual per annum) in private sector | $5.42–$125.14 (Drug and dosage specific)§ | Average cost from Indian online drug retailer 1mg.com [43], and the type and dosage drug dispensed is based on the treatment protocol |
| Out-patient consultations (per visit) | $1.94 ($1.36–$2.47)§ | Based on Indian public healthcare sector study by Prinja et al. 2020 [44] |
| One-time diagnostic tests | $2.27 | Government rate contracts [45] |
| Acute CVD care | ||
| In-patient costs for MI | $1040 | WHO Choice [46] inflated to 2019–20 |
| In-patient costs for Stroke | $940 | WHO Choice [46] inflated to 2019–20 |
| Chronic CVD care | ||
| Secondary care medication in public sector (per individual per annum) | $92, $184 (Dosage-specific)§ | International Drug Price Indicator inflated to 2019–20 [47] |
| Secondary care medication in private sector (per individual per annum) | $227, $454 (Dosage-specific)§ | Mean cost from Indian online drug retailer 1mg.com [43] |
| Outpatient cost for IHD (per annum) | $45 | WHO Choice [46] inflated to 2019–20 |
| Outpatient cost for Stroke (per annum) | $67 | WHO Choice [46] inflated to 2019–20 |
| Disability Weights | ||
| Disutility due to daily medication | 0.049 (0.031–0.072)ψ | GBD disability weights [48] |
| Acute Events | ||
| Myocardial Infarction | 0.432 (0.288–0.579)ψ | GBD disability weights [48] |
| Stroke | 0.570 (0.377–0.707)ψ | GBD disability weights [48] |
| Occurrence of second or later CVD event | 0.985 (0.992–0.989)ψ | GBD disability weights and Lin et al. 2019 [33] |
| Chronic States | ||
| Ischemic Heart Disease | 0.08 (0.02–0.24)ψ | GBD disability weights [48] |
| Stroke | 0.135 (0.01–0.437)ψ | GBD disability weights [48] |
| Alive post 2+ CVD Events | 0.242 (0.11–0.437)ψ | GBD disability weights [48] |
The ranges marked with # are further expanded in the Appendix Table S2–5 since the specific value for an individual is based on an individual’s age, sex, and/or SBP. The cost ranges marked with § are based on the specific drug and dosage administered to an individual and has been further expanded in the Appendix Table S6–9. The ranges with the superscript of ψ are 95% confidence intervals with the values sampled based on a β distribution in the simulation runs.
Costs
We calculated direct medical costs over 20 years for each individual. These costs include the cost of antihypertensive treatment (outpatient consultation, diagnostic tests, and drugs), acute CVD events (hospital care costs including consultations, room cost, procedures, surgeries, and drugs), and chronic CVD care (outpatient consultations and drugs). We obtained unit costs for antihypertensive medications, chronic CVD care and acute CVD care based on government rate contracts, the International Drug Price Indicator, and WHO CHOICE, respectively [43,46,47]. Programmatic costs are based on the India Hypertension Control Initiative (IHCI), a population-level hypertension control program that has so far enrolled more than 800,000 patients across 25 districts in six states of India [11,49]. This national hypertension-control program aims to increase detection at health facilities by strengthening opportunistic screening, simplifying and standardizing treatment, improving availability of blood pressure monitoring equipment and antihypertensive drugs, and better tracking of patients through a robust information technology platform. The human resources and technology costs to deliver the IHCI program components were determined based on expert interviews and have been factored in as the programmatic cost of the intervention. We used the exchange rate of ₹ 70 to $1 for conversion of costs from Indian rupees to US dollars.
Utility Values of Health States
We used disability weights from the GBD study to quantify health loss experienced by individuals who develop fatal or non-fatal CVD [48]. In line with other cost-effectiveness studies, we accounted for loss in wellbeing only. Future costs and DALYs were discounted at 3% per annum.
Analysis of Coverage and Adherence Scenarios
In the main analysis, we simulated multiple scenarios of hypertension management with varying levels of coverage and adherence. Coverage was defined as the proportion of hypertensive individuals initiated on treatment and was simulated by modifying (i) the proportion of hypertensive individuals who were aware of their blood pressure, and (ii) the proportion of status-aware individuals who were eligible for and initiated on treatment. According to the simplified treatment protocol of IHCI, any individual with SBP ≥ 140 mmHg on readings from two separate occasions is eligible for treatment [39,40]. We defined adherence as the proportion of individuals initiated on treatment who take medications as prescribed, and was assessed by modifying (i) the proportion of individuals who persist with treatment for more than one year after initiation, and (ii) the proportion of individuals highly compliant to medication interval and dosage (proportion of drugs consumed >80%) among those who persist with treatment for more than one year [50]. We calculated the direct medical cost per patient, and applied it based on the number of patients adherent on treatment every cycle duration. The programmatic cost was calculated at the population level and applied as a constant across different scenarios of coverage and adherence.
We simulated an aspirational scenario of 70% coverage and adherence (referenced as 70% scenario henceforth). The scenario was compared against the prevailing coverage and adherence in India, which we termed as status quo. The status quo was simulated with a coverage of 17%, an adherence of 30%, and the National Program for Prevention and Control of Cancer, Diabetes, CVD and Stroke (NPCDCS) treatment guideline (individuals are initiated on treatment if either SBP ≥ 180 mmHg or 10-yr CVD risk > 20%) [34,35,36,51,52]. We simulated the 70% scenario because it has been proposed as an immediately achievable target that national programs should aspire [6]. Additionally, we analyzed scenarios with coverage of 40%, 60%, 80%, and 100% and adherence of 40%, 60%, 80%, and 100%.
Sensitivity Analysis
We tested the robustness of our results through one-way sensitivity analysis by changing values of key input parameters in a set of independent simulation runs. These included increased medication cost and programmatic cost, reduced baseline CVD risk due to possible overestimation using Globorisk calculator, NPCDCS treatment guideline [52], inclusion of disutility of chronic medication and longer and shorter time horizons. Further we simulated a public private sector mix with 80% of the patients accessing hypertension care in the private sector [19], where the private sector medication cost was based on average listed price from an Indian online drug retailer [43]. We ran our model 1000 times with values of input parameters drawn jointly from their respective distributions and calculated costs and DALYs.
Threshold for Cost-Effectiveness
All ICERs were reported in 2019 US dollars per DALY averted. Scenarios with an ICER below India’s per-capita GDP (US $2338) were considered as cost-effective and scenarios with ICER below half of India’s per-capita GDP (US $1169) were considered as highly cost-effective [53,54]. The scenarios where the overall spending reduced while DALYs averted increased were considered as cost-saving scenarios, and the ICERs were not calculated for such scenarios.
We recognized the criticism around cost-effectiveness vis-à-vis affordability of a program [22]. Thus, along with ICERs, we also calculated the budget impact and required investment in primary care to substantiate the required resources for a hypertension management initiative. Also, our cost-effectiveness threshold of per-capita GDP was stricter and more realistic for India (an LMIC) than WHO’s three times the per-capita GDP [55,56].
Ethics Approval
We used publicly available, de-identified data for our analysis in the study, and thus did not seek approval from institutional review boards. Our study conforms to Consolidated Health Economic Evaluation Reporting Standards guidelines, with the filled checklist available in Table S17 of the Appendix [57].
Results
Cost-Effectiveness Analysis of Scenarios
Over 20 years, in the 70% scenario (coverage and adherence at 70%), the intervention was cost-saving among both females and males. The scenario averted 5.85% and 3.78% events and 6.1% and 3.76% deaths among females and males compared to status quo. In this scenario, the increase in per-capita antihypertensive medication cost ($18.5 for females and $13.7 for males) was offset by the decrease in CVD treatment cost (–$22.1 for females and –$16.8 for males). In a threshold analysis, we found that the scenario remained highly cost-effective for an increase in incremental cost of up to 11.8% for every individual in the cohort. We have summarized the result in Table 2, with the detailed results in tables S11–13 of the Appendix.
Table 2.
Costs and health outcomes associated with 70% coverage and adherence in a hypertension control intervention for individuals between 40–69 yrs from 2020–40
| ICER ($/DALY averted, 95% UI) | DALYs Averted (percent, 95% UI) | CVD Events Averted (percent, 95% UI) | Per-capita incremental costs over 20 years^ | Annual net expenditure^,ψ (in ‘000 US $) | Proba-bility of Cost Saving# | ||||
|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | Female | Male | Antihypertensive Treatment ($, 95% UI) | CVD Treatment ($, 95% UI) | ||
| Cost-saving | Cost-Saving | 2.17 (2.15 to 2.19) |
1.30 (1.29 to 1.32) |
5.85 (5.82 to 5.89) |
3.78 (3.75 to 3.81) |
18.04 (17.95 to 18.13) |
–19.43 (–19.55 to –19.3) |
–$26,740 | 0.721 |
The results are based on 1000 simulation runs with a time horizon of 20 years in two hypothetical cohorts of 10,000 individuals (males and females respectively) with ages 40–69 yrs at the start of the simulation. The status quo is based on 17% coverage, 30% adherence, and the NPCDCS medication guideline.
^ Negative values indicate cost-saving, i.e., lower expenditure compared to status quo, and the values are calculated based on the estimated Indian population of age 40–69 yrs in 2020.
ψ The estimated population of age 40–69 yrs in 2020 was used to calculate the annual expenditure for the population.
# The probability of cost-saving was calculated based on the number of simulations runs which saved overall costs among the 1000 simulation runs.
Budgetary implications of implementing the scenarios
The annual health expenditure on combined antihypertensive and CVD treatment reduced by $26.74 million ($26.74 mn) for the 70% scenario. We observed that an additional investment of $347.2 mn on hypertension control intervention resulted in a saving of $374 mn in CVD treatment expenditure.
Increasing Coverage vis-à-vis Adherence
In Figure 2, we plot the ICERs, incremental cost, and DALYs averted compared to status quo for varying coverage and adherence levels. An increase of coverage and adherence to 60% was almost budget neutral with an ICER of $3.97, and incremental cost between –0.01% and 0.06%. None of the scenarios with 40% treatment adherence was cost-saving. However, at 40% coverage, a cost-saving scenario could be achieved at 100% treatment adherence.
Figure 2.
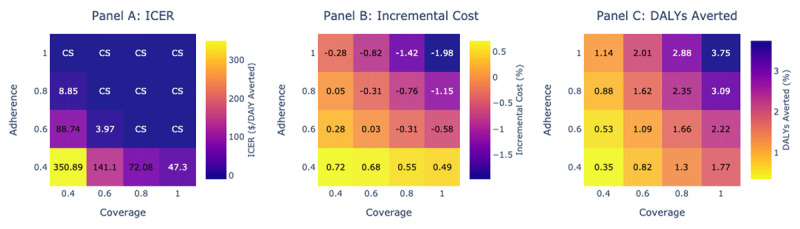
Increasing coverage vis-à-vis adherence.
We assessed multiple scenarios of coverage and adherence to antihypertensive treatment compared to the status quo (coverage = 17%, adherence = 30%), and present the cost-effectiveness (panel A), incremental cost (panel B) and DALYs averted (panel C). Each column provides information for a coverage scenario with varying adherence, and each row provides information for a adherence scenario with varying treatment coverage. In panel A, the cells in blue indicate a cost-saving scenario, and cells in purple and yellow indicate a highly cost-effective scenario. The gradient of cell color is indicative of the changing cost-effectiveness. In panel B and C, the incremental cost and DALYs averted is presented with different scenarios of coverage and adherence compared to status quo. In general, moving from yellow to blue is advantageous. The results are based on 1000 simulation runs with a time horizon of 20 years in two hypothetical cohort of 10,000 individuals (males and females respectively) with ages of 40–69 yrs at the start of the simulation.
ICER = Incremental Cost Effectiveness Ratio, DALY = Disability Adjusted Life Year, CS = Cost Saving.
We also found that increasing adherence was more beneficial in improving cost savings. For example, increasing adherence to 80% while keeping coverage at 40% increased cost by 0.05% whereas increasing coverage to 80% while keeping adherence at 40% increased cost by 0.48%. However, 0.88% DALYs were averted in the former instance whereas 1.3% DALYs were averted in the latter instance.
One-way Sensitivity Analysis
In one-way sensitivity analysis for the 70% scenario, the ICER increased to $120 for females and $90 for males when the antihypertensive medication cost was doubled. Also, when the programmatic cost was quadrupled, the ICER increased to $101 and $149 for females and males, respectively. The scenario was not cost-saving for the entire population with either of the changes. We observed an increase in ICER to $59 and $57 for females and males respectively when the baseline CVD risk was reduced by 20%. If we adopted the current NPCDCS treatment guideline, the scenario was cost-saving among both females and males. However, the health benefits were lower; 4.4% and 2.9% events averted among females and males respectively compared to 5.9% and 3.8% in the simplified protocol. If we consider the intervention with public-private mix, it is highly cost-effective with an ICER of $421 for females and $247 for males. With a reduced time-horizon of 10 years, the scenario remained highly cost-effective with ICERs of $134 for the entire population ($142 for females and $125 for males). If the time horizon was increased to 40 years, the intervention remains cost-saving among both females and males. The inclusion of disutility for being on chronic medication presented higher DALYs compared to status quo in 96% of the simulations. When the NPCDCS guideline was adopted with medication disutility, 54% of the simulations showed an increase in DALYs. We, thus, did not calculate the ICER for the scenarios. We have presented the incremental cost and DALYS averted along with ICER for each one-way sensitivity analysis in Figure 3.
Figure 3.
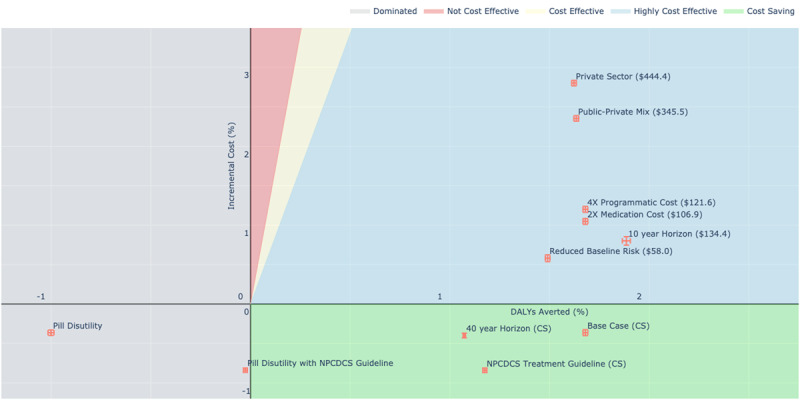
Incremental costs and DALYs averted under changes in sensitivity parameters.
We assessed the robustness of our model through changes in select input parameters in a one-way sensitivity analysis. The x-axis and y-axis represent the DALYs averted and incremental cost compared to the status quo, and the error bars are based on the 95% confidence intervals. The text in the parenthesis along with the scenario name is the ICER ($/DALYs averted), with CS representing cost-saving scenario. The base case analysis) was cost-saving. If the medication cost was increased, the scenarios were no longer cost-saving, but the ICERs were below $110 and thus highly cost-effective. When the programmatic cost was quadrupled, the scenario did not save overall costs, but remained highly cost-effective. Under the assumption that the Globorisk calculator overestimates CVD risk, we ran the simulation with a 20% reduction in baseline risk and found the scenario no longer saved costs. If the treatment protocol was changed to the current NPCDCS guideline the cost savings increased. If the simulations were run with a reduced time horizon of 10 years, the scenario was highly cost-effective. When the simulations were run for a longer time-horizon of 40 years, the cost-savings increased. The values in the green band indicate cost savings, whereas the values in blue band indicate high cost-effectiveness. The results are based on 1000 simulation runs in two hypothetical cohort of 10,000 individuals (males and females respectively) with ages of 40–69 yrs at the start of simulation, with a high cost-effectiveness threshold of 0.5* GDP ($1169).
ICER = Incremental Cost Effectiveness Ratio, GDP = Gross Domestic Product.
Discussion
Hypertension, the single largest preventable risk factor for CVDs, has a control rate of only 14% in India. Due to constraints on healthcare funding, a national hypertension control intervention is more likely to be scaled up if it is cost-saving. We find that such an intervention in India with a target of 70% coverage and adherence would be cost-saving and will save $25.6 mn annually on CVD prevention and treatment. There is an increase in savings as the coverage and adherence increases, with 100% coverage and adherence to antihypertensive treatment, potentially saving $145.5 mn annually. We also observe that at an adherence and coverage of 60%, the intervention starts being budget neutral. If an intervention needs to focus on either coverage or adherence, increasing adherence improves cost savings as it imparts higher benefit of the medication. However, a higher health impact is achieved by increasing coverage compared to adherence, since a larger proportion of hypertensive population is brought under treatment.
Previous studies have estimated that 3.8% of the non-communicable disease deaths in South Asia can be averted through increased coverage of antihypertensive treatment and the chronic diseases death rate can be reduced by 2% per annum by scaling treatment coverage to 70% [6,14]. We quantified the required economic resources and projected the health gains and cost savings for an intervention based on the tenets of IHCI, a national scale hypertension control program being implemented in India. Our study illustrates the effect of increasing coverage and adherence and enhances the understanding of previous studies on government-run insurance programs [51,58], scaling treatment coverage [59], increased opportunistic screening [60,61], and improved adherence [41]. The insights from our results are likely to hold for other LMICs with similar healthcare sector characteristics (growing disease burden of non-communicable diseases, low per-capita expenditure on primary care, and spending constraints of the respective governments on healthcare) [4,62]. However, the cost of hypertensive medication is low in India, and cost-effectiveness studies from other developing nations highlight the need to keep medication cost low for a successful scale up of hypertension control programs [63,64].
A previous study on government-run primary care insurance in India estimated an ICER of $469 per DALY averted at 34% treatment coverage and the NPCDCS treatment guideline [51]. In our model, the use of NPCDSC guidelines increased cost savings but averted fewer DALYs compared to the simplified treatment protocol. There is growing evidence that simpler, easy-to-follow treatment protocols can increase treatment coverage and improve downstream health outcomes [9,12,39]. Use of a simplified treatment protocol results in low CVD risk patients being initiated on treatment, and thus an increase in the overall expenditure on medication. However, inexpensive and generic version of the IHCI treatment protocol’s first-line drug, amlodipine, is widely available in the country. It is known to be safe and rarely leads to discontinuation due to adverse events [39]. Thus, treatment persistence is expected to be higher among individuals initiated on treatment and adverse event costs minimal.
With increased coverage, a larger proportion of hypertensive individuals will incur disutility due to the need to take daily medications for their remaining lifetimes. The disutility is due to the need of regular medication, and is a cause for patients to drop out of treatment [48,65]. In our sensitivity analysis, we find an increase in DALYs while increasing coverage for both the simplified and NPCDCS protocol. Previous cost-effectiveness studies have also shown that medication disutility exceeds the health gains when coverage of treatment is increased [58,66]. Though the concept of providing care based on an individual’s medication disutility is at its infancy in LMICs, treatment persistence could be improved if the patient-physician interaction includes exploration and addressal of the disutility.
In our study, we have not explored possible mechanisms to achieve increased coverage and adherence, and the additional programmatic cost associated with it. Though recent hypertension control pilots such as IHCI and mPower Heart project provide possible models of implementation, they currently do not serve patients in the private sector [11,17]. Our sensitivity analysis establishes that if the intervention paid for both public and private sector medication cost, the intervention will still be highly cost-effective. A comprehensive public health hypertension control program extended to both public and private sector will ensure that effective treatment can be availed by patients irrespective of their choice of providers.
The design of such a program can be further facilitated by frameworks and strategies outlined by WHO and World Heart Federation. WHO Package of Essential Noncommunicable (PEN) Disease Interventions can help administrators identify gaps in service delivery and improve health workforce training [67]. One of PEN’s components, the HEARTS technical package, was adopted in the implementation of IHCI [68]. The roadmap set by the World Heart Federation to reduce premature mortality due to CVDs by 25% by 2025 also helps identify and bridge the gaps for health systems to achieve the theoretical efficacy of the programs [69]. The roadmap helps identify the requirements from a health system to achieve the objectives. The mPower Heart project adopted the roadmap’s advocacy of task-shifting, decision-support systems, and improved tracking [17]. Further, while our study focusses on hypertension management, the frameworks set by WHO PEN and World Heart Federation can also help in designing preventive measures such as tobacco cessation and lifestyle improvements.
Our study is timely since several LMICs have recently initiated steps towards universal health coverage [70]. Their success will critically depend on the appropriate allocation of funds between preventive and curative services [51]. Under the Government of India’s national health insurance program, Ayushman Bharat [71], budgeted expenditure for hospitalization costs is thrice than that budgeted for the upgradation of health and wellness centres [71,72,73]. Increased investment in preventive programs such as the one studied here is necessary to ultimately reduce secondary and tertiary care expenditure, especially with the rapidly growing disease burden [4]. Also, such a preventive and primary healthcare program will further lower healthcare inequity and reduce out-of-pocket expenditure for households [21,74].
An implementation of such a large-scale intervention will not only need increased governmental support and commitment but also inter-departmental collaboration as expenditure on antihypertensive treatment and accrual of monetary benefits from CVD prevention will likely affect the budgets of different departments [9]. Although the intervention is cost-saving over 20 years, it will need a significant upfront investment. For instance, at 70% coverage and adherence, an annual expenditure of $347 mn in primary care would be needed, which represents 4% increase in India’s current health budget and is 14 times the current allocation for NPCDCS [75]. Though the required increase might appear daunting compared to the current allocation, it is important to note that India’s public health budget, at 1.28% of the GDP, is criticized for being low compared to the country’s needs and economic growth [14,76,77].
Our analysis has limitations. Our model assumes that changes in coverage and adherence are instantaneous although they may take up to five years in practice [14]. Although the programmatic cost during such a ramp-up period will be higher than that during steady-state, we expect our results to hold since the scenarios continued to be highly cost-effective even with quadrupled programmatic costs. Due to a lack of data from the Indian context, we were unable to model serious adverse events such as hypotension and electrolyte abnormality caused by antihypertensive treatment [78,79]. But their inclusion is unlikely to affect our results substantively as, firstly, less than 1% of hypertensive patients experience serious adverse events, and, secondly, we find that the 70% scenario is not highly cost-effective only if expenditure due to serious adverse events increases the cost incurred by more than 11.8% for every individual in the population. We did not capture the costs and disability due to other hypertension-related diseases, such as chronic kidney disease, due to lack of India-specific data but their inclusion will make the intervention scenarios more cost-saving than currently estimated. In terms of the cost-effectiveness thresholds, while we recognize that an opportunity-cost-based threshold would be more appropriate, we followed the per-capita GDP threshold due to a lack of consensus on the methods and data for the former [56].
Our model parameters are reliant on the GBD dataset by the Institute of Health Metrics and Evaluation. Though the GBD estimates have faced recent criticism from WHO member states, we believe the estimates are more transparent in terms of data availability and free from political pressures than other available estimates [80,81]. Further, we utilize the mortality and incidence estimates from the GBD dataset whereas most of the criticism is directed towards the estimates of DALYs. Also, we report the 95% uncertainty intervals for DALYs averted in our results (Table 2, Figure 3, and the detailed results in the supplementary appendix), and it accounts for some of the variability due to bias in GBD estimates of disease burden.
Conclusion
The mathematic modeling study, utilizing India-specific data sources, found that scaling up antihypertensive treatment to cover 70% of the hypertensive individuals will save overall costs on CVD prevention and treatment. Achieving the cost-saving or budget-neutral scenario will require high levels of both coverage and adherence, which in turn, will require a sizeable investment in the short-term and will yield a reduction in expenditure in the long term.
Data Accessibility Statements
Data and materials created as part of the study have been made publicly available and can be accessed at persistent doi 10.5281/zenodo.4046041. The WHO SAGE Wave 1 dataset and the Globorisk calculator were received upon request from the respective authors and have not been shared in the online repository. The detailed method, input parameters, and simulation results are provided in the Supplementary Appendix.
Additional File
The additional file for this article can be found as follows:
Cost effectiveness of improved hypertension management in India through increased treatment coverage and adherence: a mathematical modelling study.
Acknowledgements
The authors would like to thank Sagri Negi for help in determining the programmatic cost of the Indian Hypertension Control Initiative and providing constructive comments on the manuscript.
Competing Interests
Dr. Deo reports grants from Resolve to Save Lives, outside the submitted work. Drs. Moran, Pathni, and Sharma report personal fees from Resolve to Save Lives, an initiative of Vital Strategies, during the conduct of the study. Dr. Kunwar reports grants from Resolve to Save Lives, during the conduct of the study. Resolve to Save Lives is funded by Bloomberg Philanthropies, the Bill & Melinda Gates Foundation, and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation. Resolve to Save Lives is the international technical partner for India Hypertension Control Initiative, which is being implemented by Indian Council of Medical Research, Ministry of Health and Family Welfare and World Health Organization. Mr. Das has nothing to disclose.
Author Contributions
SD and AEM developed the idea. HD along with SD and AEM designed the study and drafted the article. HD conducted the statistical analysis and prepared the figures. HD, SD, AEM, and AKP interpreted data. All authors participated in the critical revision of the manuscript and provided final approval.
References
- 1.WHO. Cardiovascular diseases (CVDs) – Fact Sheet. World Health Organ; 2017. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed July 2, 2020). [Google Scholar]
- 2.Bloom D, Cafiero E, McGovern M, Prettner K, Stanciole A, Weiss J, et al. The economic impact of non-communicable disease in China and India: Estimates, projections, and comparisons. Cambridge, MA: National Bureau of Economic Research; 2013. DOI: 10.3386/w19335 [DOI] [Google Scholar]
- 3.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2017 (GBD 2017) Results. Seattle, United States: Institute for Health Metrics and Evaluation (IHME); 2018. [Google Scholar]
- 4.Huffman MD, Rao KD, Pichon-Riviere A, Zhao D, Harikrishnan S, Ramaiya K, et al. A cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low- and middle-income countries. PLoS ONE. 2011; 6: e20821. DOI: 10.1371/journal.pone.0020821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campbell NRC, Lackland DT, Niebylski ML, the World Hypertension League and International Society of Hypertension Executive Committees. High blood pressure: why prevention and control are urgent and important-A 2014 fact sheet from the World Hypertension League and the International Society of Hypertension. J Clin Hypertens. 2014; 16: 551–3. DOI: 10.1111/jch.12372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kontis V, Cobb LK, Mathers CD, Frieden TR, Ezzati M, Danaei G. Three public health interventions could save 94 million lives in 25 years: Global impact assessment analysis. Circulation. 2019; 140: 715–25. DOI: 10.1161/CIRCULATIONAHA.118.038160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low- and middle-income countries: Prevalence, awareness and control. Int J Epidemiol. 2014; 43: 116–28. DOI: 10.1093/ije/dyt215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prenissl J, Manne-Goehler J, Jaacks LM, Prabhakaran D, Awasthi A, Bischops AC, et al. Hypertension screening, awareness, treatment, and control in India: A nationally representative cross-sectional study among individuals aged 15 to 49 years. PLOS Med. 2019; 16: e1002801. DOI: 10.1371/journal.pmed.1002801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frieden TR, Varghese CV, Kishore SP, Campbell NRC, Moran AE, Padwal R, et al. Scaling up effective treatment of hypertension—A pathfinder for universal health coverage. J Clin Hypertens. 2019; 21: 1442–9. DOI: 10.1111/jch.13655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atun R, Jaffar S, Nishtar S, Knaul FM, Barreto ML, Nyirenda M, et al. Improving responsiveness of health systems to non-communicable diseases. The Lancet. 2013; 381: 690–7. DOI: 10.1016/S0140-6736(13)60063-X [DOI] [PubMed] [Google Scholar]
- 11.The Indian Council of Medical Research. Press Release: Expansion for India Hypertension Control Initiative (IHCI). New Delhi: The Indian Council of Medical Research; 2019. [Google Scholar]
- 12.Jaffe MG, Young JD. The Kaiser Permanente Northern California Story: Improving hypertension control from 44% to 90% in 13 years (2000 to 2013). J Clin Hypertens. 2016; 18: 260–1. DOI: 10.1111/jch.12803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. HEARTS Technical Package. WHO; n.d. http://www.who.int/cardiovascular_diseases/hearts/en/ (accessed March 6, 2020). [Google Scholar]
- 14.Lim SS, Gaziano TA, Gakidou E, Reddy KS, Farzadfar F, Lozano R, et al. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. The Lancet. 2007; 370: 2054–62. DOI: 10.1016/S0140-6736(07)61699-7 [DOI] [PubMed] [Google Scholar]
- 15.Hedayati SS, Elsayed EF, Reilly RF. Non-pharmacological aspects of blood pressure management: What are the data? Kidney Int. 2011; 79: 1061–70. DOI: 10.1038/ki.2011.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Migneault JP, Dedier JJ, Wright JA, Heeren T, Campbell MK, Morisky DE, et al. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African-Americans: A randomized controlled trial. Ann Behav Med. 2012; 43: 62–73. DOI: 10.1007/s12160-011-9319-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ajay VS, Jindal D, Roy A, Venugopal V, Sharma R, Pawar A, et al. Development of a smartphone-enabled hypertension and diabetes mellitus management package to facilitate evidence-based care delivery in primary healthcare facilities in India: The mPower Heart Project. J Am Heart Assoc. 2016; 5: e004343. DOI: 10.1161/JAHA.116.004343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Praveen D, Patel A, McMahon S, Prabhakaran D, Clifford GD, Maulik PK, et al. A multifaceted strategy using mobile technology to assist rural primary healthcare doctors and frontline health workers in cardiovascular disease risk management: Protocol for the SMARTHealth India cluster randomised controlled trial. Implement Sci. 2013; 8: 1–8. DOI: 10.1186/1748-5908-8-137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Engelgau MM, Karan A, Mahal A. The economic impact of non-communicable diseases on households in India. Glob Health. 2012; 8: 9. DOI: 10.1186/1744-8603-8-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Babu V, Sahu SK, Kanungo S. Hypertension control status and quality of care for hypertension among patients availing treatment from private sector: A cross-sectional study in urban field practice area of JIPMER, Puducherry. J Fam Med Prim Care. 2019; 8: 72–6. DOI: 10.4103/jfmpc.jfmpc_248_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balarajan Y, Selvaraj S, Subramanian S. Health care and equity in India. The Lancet. 2011; 377: 505–15. DOI: 10.1016/S0140-6736(10)61894-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bilinski A, Neumann P, Cohen J, Thorat T, McDaniel K, Salomon JA. When cost-effective interventions are unaffordable: Integrating cost-effectiveness and budget impact in priority setting for global health programs. PLOS Med. 2017; 14: e1002397. DOI: 10.1371/journal.pmed.1002397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kostova D, Spencer G, Moran AE, Cobb LK, Husain MJ, Datta BK, et al. The cost-effectiveness of hypertension management in low-income and middle-income countries: A review. BMJ Glob Health. 2020; 5: e002213. DOI: 10.1136/bmjgh-2019-002213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kowal P, Chatterji S, Naidoo N, Biritwum R, Fan W, Lopez Ridaura R, et al. Data Resource Profile: The World Health Organization study on global ageing and adult health (SAGE). Int J Epidemiol. 2012; 41: 1639–49. DOI: 10.1093/ije/dys210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ueda P, Woodward M, Lu Y, Hajifathalian K, Al-Wotayan R, Aguilar-Salinas CA, et al. Laboratory-based and office-based risk scores and charts to predict 10-year risk of cardiovascular disease in 182 countries: A pooled analysis of prospective cohorts and health surveys. Lancet Diabetes Endocrinol. 2017; 5: 196–213. DOI: 10.1016/S2213-8587(17)30015-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018; 392: 1789–858. DOI: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO. Global Health Observatory data repository. Geneva: World Health Organization; 2018. [Google Scholar]
- 28.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009; 338: b1665. DOI: 10.1136/bmj.b1665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huffman MD, Mohanan PP, Devarajan R, Baldridge AS, Kondal D, Zhao L, et al. Effect of a quality improvement intervention on clinical outcomes in patients in India with acute myocardial infarction: The ACS QUIK randomized clinical trial. JAMA. 2018; 319: 567–78. DOI: 10.1001/jama.2017.21906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pandian JD, Sudhan P. Stroke epidemiology and stroke care services in India. J Stroke. 2013; 15: 128–34. DOI: 10.5853/jos.2013.15.3.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steg PhG, Bhatt DL, Wilson PWF, D’Agostino R, Ohman EM, Röther J, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007; 297: 1197–206. DOI: 10.1001/jama.297.11.1197 [DOI] [PubMed] [Google Scholar]
- 32.Petty GW, Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Survival and recurrence after first cerebral infarction: A population-based study in Rochester, Minnesota, 1975 through 1989. Neurology. 1998; 50: 208–16. DOI: 10.1212/WNL.50.1.208 [DOI] [PubMed] [Google Scholar]
- 33.Lin JK, Moran AE, Bibbins-Domingo K, Falase B, Pedroza Tobias A, Mandke CN, et al. Cost-effectiveness of a fixed-dose combination pill for secondary prevention of cardiovascular disease in China, India, Mexico, Nigeria, and South Africa: A modelling study. Lancet Glob Health. 2019; 7: e1346–58. DOI: 10.1016/S2214-109X(19)30339-0 [DOI] [PubMed] [Google Scholar]
- 34.Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013; 310: 959–68. DOI: 10.1001/jama.2013.184182 [DOI] [PubMed] [Google Scholar]
- 35.Van Wijk BL, Klungel OH, Heerdink ER, de Boer A. Rate and determinants of 10-year persistence with antihypertensive drugs: JHypertens. 2005; 23: 2101–7. DOI: 10.1097/01.hjh.0000187261.40190.2e [DOI] [PubMed] [Google Scholar]
- 36.Dennis T, Meera NK, Binny K, Sekhar MS, Kishore G, Sasidharan S. Medication adherence and associated barriers in hypertension management in India. CVD Prev Control. 2011; 6: 9–13. DOI: 10.1016/j.cvdpc.2010.11.001 [DOI] [Google Scholar]
- 37.Bellows BK, Ruiz-Negrón N, Bibbins-Domingo K, King JB, Pletcher MJ, Moran AE, et al. Clinic-based strategies to reach united states million hearts 2022 blood pressure control goals: A simulation study. Circ Cardiovasc Qual Outcomes. 2019; 12: e005624. DOI: 10.1161/CIRCOUTCOMES.118.005624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smolina K, Wright FL, Rayner M, Goldacre MJ. Long-term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circ Cardiovasc Qual Outcomes. 2012; 5: 532–40. DOI: 10.1161/CIRCOUTCOMES.111.964700 [DOI] [PubMed] [Google Scholar]
- 39.Jaffe MG, Frieden TR, Campbell NRC, Matsushita K, Appel LJ, Lackland DT, et al. Recommended treatment protocols to improve management of hypertension globally: A statement by Resolve to Save Lives and the World Hypertension League (WHL). J Clin Hypertens. 2018; 20: 829–36. DOI: 10.1111/jch.13280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.India Hypertension Management Intiative. Punjab Hypertension Protocol n.d. [Google Scholar]
- 41.Cherry SB, Benner JS, Hussein MA, Tang SSK, Nichol MB. The clinical and economic burden of nonadherence with antihypertensive and lipid-lowering therapy in hypertensive patients. Value Health. 2009; 12: 489–97. DOI: 10.1111/j.1524-4733.2008.00447.x [DOI] [PubMed] [Google Scholar]
- 42.TSMSIDC. Medicines-Rate Contract. Telangana State Med Serv Infrastruct Dev Corp; n.d. http://tsmsidc.telangana.gov.in/content.php?U=20%20&&%20T=Medicines-Rate%20Contract (accessed January 7, 2020). [Google Scholar]
- 43.1mg. About 1mg: India’s leading digital consumer healthcare platform 2020. https://www.1mg.com/aboutUs (accessed May 15, 2020).
- 44.Prinja S, Chauhan AS, Bahuguna P, Selvaraj S, Muraleedharan VR, Sundararaman T. Cost of delivering secondary healthcare through the public sector in India. PharmacoEconomics. 2020; 4: 249–61. DOI: 10.1007/s41669-019-00176-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Central Government Health Scheme, GoI. Rate List for Hyderabad – CGHS Hyderabad w.e.f 17/11/2014. Hyderabad, India: Government of India; 2014. [Google Scholar]
- 46.WHO. Country-specific inpatient and outpatient estimates in 2010 currency. Geneva: World Health Organization; 2010. [Google Scholar]
- 47.MSH. International Medical Products Price Guide. Arlington, Virginia: Management Sciences for Health; 2016. [Google Scholar]
- 48.Salomon JA, Vos T, Hogan DR, Gagnon M, Naghavi M, Mokdad A, et al. Common values in assessing health outcomes from disease and injury: Disability weights measurement study for the Global Burden of Disease Study 2010. The Lancet. 2012; 380: 2129–43. DOI: 10.1016/S0140-6736(12)61680-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.WHO. Community drug distribution at doorsteps: Essential health services decentralized to care for hypertensives under the IHCI initiative 2020. https://www.who.int/india/news/feature-stories/detail/community-drug-distribution-at-doorsteps-essential-health-services-decentralized-to-care-for-hypertensives-under-the-ihci-initiative (accessed August 23, 2020).
- 50.Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication compliance and persistence: Terminology and definitions. Value Health. 2008; 11: 44–7. DOI: 10.1111/j.1524-4733.2007.00213.x [DOI] [PubMed] [Google Scholar]
- 51.Basu S, Bendavid E, Sood N. Health and economic implications of national treatment coverage for cardiovascular disease in India: Cost-effectiveness analysis. Circ Cardiovasc Qual Outcomes. 2015; 8: 541–51. DOI: 10.1161/CIRCOUTCOMES.115.001994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rau N, Nayak SK. Practical Guidelines for Hypertension Management. Med. Update 2013, Mumbai, India: The Association of Physicians of India; 2013; 69–73. [Google Scholar]
- 53.IMF. World Economic Outlook, October 2019. Washington, DC: International Monetary Fund; 2019. [Google Scholar]
- 54.Marseille E, Larson B, Kazi DS, Kahn JG, Rosen S. Thresholds for the cost-effectiveness of interventions: alternative approaches. Bull World Health Organ. 2015; 93: 118–24. DOI: 10.2471/BLT.14.138206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leech AA, Kim DD, Cohen JT, Neumann PJ. Use and misuse of cost-effectiveness analysis thresholds in low- and middle-income countries: Trends in cost-per-DALY studies. Value Health. 2018; 21: 759–61. DOI: 10.1016/j.jval.2017.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Woods B, Revill P, Sculpher M, Claxton K. Country-level cost-effectiveness thresholds: Initial estimates and the need for further research. Value Health. 2016; 19: 929–35. DOI: 10.1016/j.jval.2016.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ. 2013; 346: f1049. DOI: 10.1136/bmj.f1049 [DOI] [PubMed] [Google Scholar]
- 58.Rosendaal NTA, Hendriks ME, Verhagen MD, Bolarinwa OA, Sanya EO, Kolo PM, et al. Costs and cost-effectiveness of hypertension screening and treatment in adults with hypertension in rural nigeria in the context of a health insurance program. PLOS ONE. 2016; 11: e0157925. DOI: 10.1371/journal.pone.0157925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Akkazieva B, Chisholm D, Akunov N, Jakab M. The health effects and costs of the interventions to control cardiovascular disease in Kyrgyzstan. Bishkek, Kyrgyz Republic: WHO; 2009. [Google Scholar]
- 60.Nguyen T-P- L, Wright EP, Nguyen T-T, Schuiling-Veninga CCM, Bijlsma MJ, Nguyen T-B-Y, et al. Cost-effectiveness analysis of screening for and managing identified hypertension for cardiovascular disease prevention in Vietnam. PLOS ONE. 2016; 11: e0155699. DOI: 10.1371/journal.pone.0155699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gaziano T, Abrahams-Gessel S, Surka S, Sy S, Pandya A, Denman CA, et al. Cardiovascular disease screening by community health workers can be cost-effective in low-resource countries. Health Aff. (Millwood) 2015; 34: 1538–45. DOI: 10.1377/hlthaff.2015.0349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: A systematic review. BMC Public Health. 2018; 18: 975. DOI: 10.1186/s12889-018-5806-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gu D, He J, Coxson PG, Rasmussen PW, Huang C, Thanataveerat A, et al. The cost-effectiveness of low-cost essential antihypertensive medicines for hypertension control in China: A modelling study. PLOS Med. 2015; 12: e1001860. DOI: 10.1371/journal.pmed.1001860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gad M, Lord J, Chalkidou K, Asare B, Lutterodt MG, Ruiz F. Supporting the development of evidence-informed policy options: An economic evaluation of hypertension management in Ghana. Value Health. 2020; 23: 171–9. DOI: 10.1016/j.jval.2019.09.2749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fontana M, Asaria P, Moraldo M, Finegold J, Hassanally K, Manisty CH, et al. Patient-accessible tool for shared decision making in cardiovascular primary prevention: Balancing Longevity benefits against medication disutility. Circulation. 2014; 129: 2539–46. DOI: 10.1161/CIRCULATIONAHA.113.007595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Moran AE, Odden MC, Thanataveerat A, Tzong KY, Rasmussen PW, Guzman D, et al. Cost-effectiveness of hypertension therapy according to 2014 guidelines. N Engl J Med. 2015; 372: 447–55. DOI: 10.1056/NEJMsa1406751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.World Health Organization. WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Geneva: World Health Organization; 2020. [Google Scholar]
- 68.Reddy TsK, Kunwar A, Durgad K, Tullu F, Sreedhar C, Wassey A, et al. Decentralization of India Hypertension Control Initiative services to maintain continuum of care for hypertensive patients during COVID-19 pandemic in Telangana. WHO South-East Asia J Public Health. 2021; 10: 49. DOI: 10.4103/2224-3151.309873 [DOI] [Google Scholar]
- 69.Adler AJ, Prabhakaran D, Bovet P, Kazi DS, Mancia G, Mungal-Singh V, et al. Reducing cardiovascular mortality through prevention and management of raised blood pressure: A World Heart Federation roadmap. Glob Heart. 2015; 10: 111. DOI: 10.1016/j.gheart.2015.04.006 [DOI] [PubMed] [Google Scholar]
- 70.Reeves A, Gourtsoyannis Y, Basu S, McCoy D, McKee M, Stuckler D. Financing universal health coverage—Effects of alternative tax structures on public health systems: cross-national modelling in 89 low-income and middle-income countries. The Lancet. 2015; 386: 274–80. DOI: 10.1016/S0140-6736(15)60574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Press Information Bureau. Ayushman Bharat for a new India -2022, announced. New Delhi: Government of India; 2018. [Google Scholar]
- 72.Sharma NC. Health budget focuses only on Ayushman Bharat, other schemes ignored. Livemint; 2019. [Google Scholar]
- 73.Bakshi H, Sharma R, Kumar P. Ayushman Bharat Initiative (2018): What we stand to gain or lose! Indian J Community Med Off Publ Indian Assoc Prev Soc Med. 2018; 43: 63–6. DOI: 10.4103/ijcm.IJCM_96_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Prinja S, Chauhan AS, Karan A, Kaur G, Kumar R. Impact of publicly financed health insurance schemes on healthcare utilization and financial risk protection in India: A systematic review. PLOS ONE. 2017; 12: e0170996. DOI: 10.1371/journal.pone.0170996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ministry of Finance. Union Budget. Delhi, India: Government of India; 2019. [Google Scholar]
- 76.The World Bank. World Bank Open Data. Washington, DC: The World Bank; 2014. [Google Scholar]
- 77.Dandona L, Dandona R, Kumar GA, Shukla DK, Paul VK, Balakrishnan K, et al. Nations within a nation: Variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. The Lancet. 2017; 390: 2437–60. DOI: 10.1016/S0140-6736(17)32804-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bahl VK, Jadhav UM, Thacker HP. Management of hypertension with the fixed combination of perindopril and amlodipine in daily clinical practice: Results from the STRONG prospective, observational, multicenter study. Am J Cardiovasc Drugs. 2009; 9: 135–42. DOI: 10.1007/BF03256570 [DOI] [PubMed] [Google Scholar]
- 79.Kumbla DK, Kumar S, Reddy YV, Trailokya A, Naik M. WIN OVER study: Efficacy and safety of olmesartan in Indian hypertensive patients: Results of an open label, non-comparative, multi-centric, post marketing observational study. Indian Heart J. 2014; 66: 340–4. DOI: 10.1016/j.ihj.2014.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mathers CD. History of global burden of disease assessment at the World Health Organization. Arch Public Health. 2020; 78: 77. DOI: 10.1186/s13690-020-00458-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yoon S-J, Kim Y-E, Kim E-J. Why they are different: based on the burden of disease research of WHO and Institute for Health Metrics and Evaluation. BioMed Res Int. 2018; 2018: 1–4. DOI: 10.1155/2018/7236194 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Cost effectiveness of improved hypertension management in India through increased treatment coverage and adherence: a mathematical modelling study.
Data Availability Statement
Data and materials created as part of the study have been made publicly available and can be accessed at persistent doi 10.5281/zenodo.4046041. The WHO SAGE Wave 1 dataset and the Globorisk calculator were received upon request from the respective authors and have not been shared in the online repository. The detailed method, input parameters, and simulation results are provided in the Supplementary Appendix.


