Abstract
Hallucinogens are a loosely defined group of compounds including LSD, N,N-dimethyltryptamines, mescaline, psilocybin/psilocin, and 2,5-dimethoxy-4-methamphetamine (DOM), which can evoke intense visual and emotional experiences. We are witnessing a renaissance of research interest in hallucinogens, driven by increasing awareness of their psychotherapeutic potential. As such, we now present a narrative review of the literature on hallucinogen binding in vitro and ex vivo, and the various molecular imaging studies with positron emission tomography (PET) or single photon emission computer tomography (SPECT). In general, molecular imaging can depict the uptake and binding distribution of labelled hallucinogenic compounds or their congeners in the brain, as was shown in an early PET study with N1-([11C]-methyl)-2-bromo-LSD ([11C]-MBL); displacement with the non-radioactive competitor ketanserin confirmed that the majority of [11C]-MBL specific binding was to serotonin 5-HT2A receptors. However, interactions at serotonin 5HT1A and other classes of receptors and pleotropic effects on second messenger pathways may contribute to the particular experiential phenomenologies of LSD and other hallucinogenic compounds. Other salient aspects of hallucinogen action include permeability to the blood–brain barrier, the rates of metabolism and elimination, and the formation of active metabolites. Despite the maturation of radiochemistry and molecular imaging in recent years, there has been only a handful of PET or SPECT studies of radiolabeled hallucinogens, most recently using the 5-HT2A/2C agonist N-(2[11CH3O]-methoxybenzyl)-2,5-dimethoxy- 4-bromophenethylamine ([11C]Cimbi-36). In addition to PET studies of target engagement at neuroreceptors and transporters, there is a small number of studies on the effects of hallucinogenic compounds on cerebral perfusion ([15O]-water) or metabolism ([18F]-fluorodeoxyglucose/FDG). There remains considerable scope for basic imaging research on the sites of interaction of hallucinogens and their cerebrometabolic effects; we expect that hybrid imaging with PET in conjunction with functional magnetic resonance imaging (fMRI) should provide especially useful for the next phase of this research.
Keywords: hallucinogens, molecular imaging, PET, SPECT, serotonin receptors
Contents:
Introduction
- Binding Sites of Hallucinogens in Vitro
-
2.1.The Nature of Agonist-Receptor Interactions
-
2.2.Affinities of LSD at Neuroreceptors in Vitro
-
2.3.Affinities of Hallucinogenic Phenylethylamines in Vitro
-
2.4.Affinities of Hallucinogenic Tryptamines in Vitro
-
2.5.The Strange Case of Ibogaine
-
2.1.
- Ex vivo/In vitro Binding Studies with Hallucinogens
-
3.1.LSD Derivatives
-
3.2.Phenyethylamine Derivatives
-
3.1.
- Molecular Imaging Studies in Vivo with Hallucinogens
-
4.1.LSD Derivatives
-
4.2.Phenylethylamine Derivatives
-
4.3.Tryptamine Derivatives
-
4.4.Competition from Hallucinogens at Dopamine Receptors in Vivo
-
4.5.Competition from Hallucinogens at Serotonin Receptors in Vivo
-
4.1.
- Metabolism of Hallucinogenic Compounds and Tracers
-
4.1.LSD
-
5.2.Phenylethylamine Derivatives
-
5.3.Tryptamine Derivatives
-
4.1.
Ayahuasca and Pharmahuasca
- Effects of Hallucinogens on Energy Metabolism and Perfusion
-
7.1.Cerebral Glucose Metabolic Rate
-
7.2.Cerebral Blood Flow
-
7.1.
General Conclusions
References
1. Introduction
Structurally diverse ergolines, phenylethylamines, and tryptamines known collectively as hallucinogens induce perceptual and affective changes, extending from sensory distortions (illusions) to sensing of non-existent objects (hallucinations), with varying degree of control over or insight into the altered state. The sites of hallucinogen binding and action in the central nervous system are amenable to study by molecular imaging with positron emission tomography (PET) or single photon emission computer tomography (SPECT), and can now be studied by functional magnetic resonance imaging (fMRI) of cerebral perfusion and connectivity [1]. A prohibition against hallucinogen research established in many countries the 1970s was until recently an impediment to progress in our understanding of the phenomenology and physiology of hallucinogen action [2,3]; PubMed hits for the search term “hallucinogen” peaked in 1974, troughed around 1990, and have sustained a high level since 2010. Analysis of the literature in the past decade shows a shift in emphasis from preclinical studies especially of lysergic acid diethylamide (LSD) (1) towards more clinical applications, especially involving psilocybin (2) [4]. Indeed, there is now considerable interest in exploring the psychotherapeutic potential of hallucinogens, with 13 trials of psilocybin (2) undertaken in 2020 alone [5]. The renewed exploration of hallucinogens in a therapeutic setting raises important ethical and scientific consideration, and highlights the need for basic research on the action of hallucinogens in human brain [6,7]. The only recent review on imaging of hallucinogen actions focusses mainly on the fMRI literature [8]. Given this background, we now present a narrative review of the present state of the molecular imaging literature on hallucinogenic molecules. We emphasize first the selectivity and affinity of hallucinogenic compounds for serotonin receptors in vitro, discuss their fitness as radioligands for autoradiographic binding studies, and finally review the rather sparse literature on PET and SPECT studies with hallucinogens. Our aim is to extract general principles from the available results, and identify topics for future research in this domain.
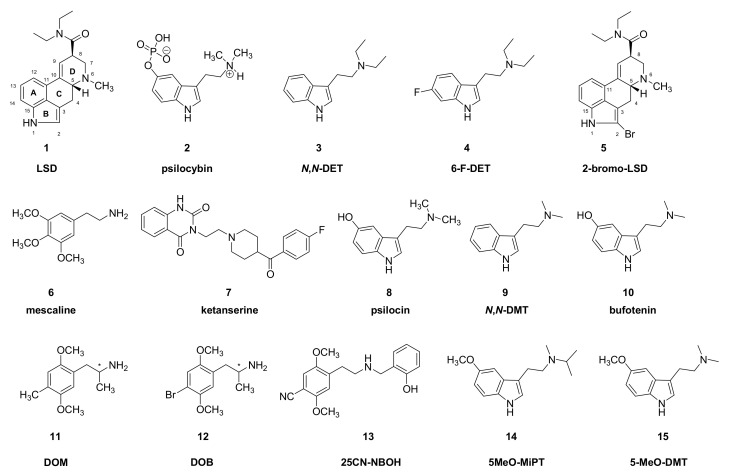
While various ancient peoples knew about plant- and animal-derived hallucinogens, the modern era of interest in hallucinogens began with the accidental discovery of the mind-altering effects of the ergot derivative LSD (1) (Figure 1). The extraordinary nature of experiences provoked by hallucinogens naturally motivated scientists to seek an understanding of their psychopharmacology and mechanisms of action. Hallucinogens belong to a variety of structural classes, including ergolines, phenylethylamines, and tryptamines (Figure 1, Figure 2, Figure 3 and Figure 5). As presented below, there is a general agreement that hallucinogens of the psychedelics class are agonists at serotonin 5HT2A receptors; although drugs of diverse other pharmacological classes can also induce hallucinations, we mainly confine this review to serotoninergic substances. However, the full spectrum of a given hallucinogen’s action may well entail actions at other serotonin receptors as well as receptors of dopamine, noradrenaline, histamine, trace amines, and neurotransmitter uptake sites (e.g., [9,10]). The spectrum of target engagement must somehow account for the overlapping and distinct aspects of the phenomenologies of different hallucinogenic drugs. Indeed, small structural modifications of certain molecules can decisively influence their hallucinogenic potency. For example, unlike N,N-diethyltryptamine (N,N-DET, 3), the corresponding diethyl compound, 6-fluoro-N,N-diethyltryptamine (4) is without hallucinogenic action in humans [11]. Similarly, 2-bromo-LSD (BOL-148, 5), despite its engagement with serotonin 5HT2A receptors, does not evoke hallucinations [12], except perhaps in rare cases [13]. Recent investigation of this phenomenon indicated that halogenation of N,N-DET (3) did not alter its affinity for serotonin 5HT2A receptors or various other receptor types, but disabled the intracellular response to agonism, i.e., stimulation of phosphotidyl inositol (PI) turnover [14], which may be a necessary property of effective hallucinogens. However, hallucinogenic activity is not a simple binary phenomenon, but encompasses a range of visual and sensory experiences. For example, mescaline (6) tends to evoke a characteristic visual experience of “geometricization” of three-dimensional objects, as is depicted in certain Amerindian art traditions. Visual hallucinations hint at a pharmacological action in the visual cortex [15], which is a theme amenable to analysis using a neural network approach [16]. It remains unclear how the particulars of mescaline (6) pharmacology might account for its greater propensity to evoke a specific type of visual experience. Despite the broadly overlapping serotonin receptor binding profiles of hallucinogenic tryptamines, interactions at other receptor types may contribute to their overall psychopharmacology or the particular phenomenology of hallucinogenic experiences [17]. Indeed, pretreatment of volunteers with the selective 5HT2A/C antagonist ketanserin (7), while largely abolishing the hallucinations elicited by psilocybin (2), did not attenuate binocular rivalry switching [18] or effects on attentional tracking performance [19]. Furthermore, a compilation of reports for a broad range of substances shows that interactions of serotonin, dopamine, glutamate, and opioid receptors all contribute to aspects of the subjective experience [20]. Other relevant factors for psychedelic action include the relationship between plasma kinetics of a drug, permeability for the blood–brain barrier, duration of target engagement in the central nervous system, and the intensity of psychedelic experience. Finally, the phenomena of “flashbacks” and hallucinogen-persisting perception disorder (HPPD) sometimes occurring in LSD (1) users [21] may call for reassessing the notion that visual hallucinations are only due to acute pharmacological activation of serotonin receptors [22].
Figure 1.
Chemical structures of LSD and some classic hallucinogenic compounds—(*) indicates chiral centers.
The first phase of molecular imaging of hallucinogenic compounds employed in vitro binding techniques for assessing affinities and ex vivo methods for revealing the cerebral uptake and binding of radiopharmaceuticals in brain of living animals (e.g., [23]). Molecular imaging by positron emission tomography (PET) and single photon computer tomography (SPECT) have emerged in recent years as mature technologies for monitoring neuroreceptor availability in living brain, for measuring the extent of target engagement by psychoactive drugs [24,25], and to detect physiological responses of the brain to a pharmacological challenge. PET/SPECT methods are admirably suited for studying the cerebral uptake and binding of hallucinogens and for testing effects of psychoactive compounds on physiological markers such as the cerebral metabolic rate for glucose (CMRglc) or cerebral blood flow (CBF). However, this literature is rather sparse; indeed, some well-known hallucinogens remain entirely uninvestigated by molecular imaging techniques.
2. Binding Sites of Hallucinogens In Vitro
2.1. The Nature of Agonist-Receptor Interactions
Agonism at serotonin receptors is an essential property of hallucinogens. Most serotonin receptors couple to intracellular second messenger systems by one or more guanine nucleotide binding proteins (G-proteins); the presence of guanosine triphosphate (GTP) or its metabolically stable analogues in the receptor binding assay disfavors the binding of agonist ligands, but has no effect on antagonist binding. Thus, the addition of GTP to a binding assay causes a substantial loss of affinity of an agonist ligand in vitro, manifesting in a shift to the right of a displacement curve against the bonding of a labelled antagonist ligand. In general, agonist binding stimulates GTP/GDP exchange, which results in activation of the enzyme adenylate cyclase in the case of the Gs-type G-protein, inhibition of adenylyl cyclase in the case of Gi/o, and stimulation of phospholipase C in the case of Gq/11, among many possible signal transduction pathways. For example, agonists of 5HT1A sites such as 8-hydroxy-DPAT have no intrinsic effect on cyclic AMP (cAMP) production in rat hippocampal neurons, but inhibit the stimulation of adenylyl cyclase provoked by other receptor types [26], thus suggesting receptor coupling to second messenger systems via Gi/o-type G-proteins. In another assay system, the increased retention of [35S]-guanosine-5-O-(3-thio)-triphosphate in membranes reveals agonist interactions. Indeed, that assay may serve as a forensic tool for operationally predicting the hallucinogenic properties of members of a series of tryptamine derivatives [27]. However, the mouse head-twitch response behavioral paradigm and rat trials of drug discrimination may serve better to predict hallucinogenic potency of drugs in humans [28].
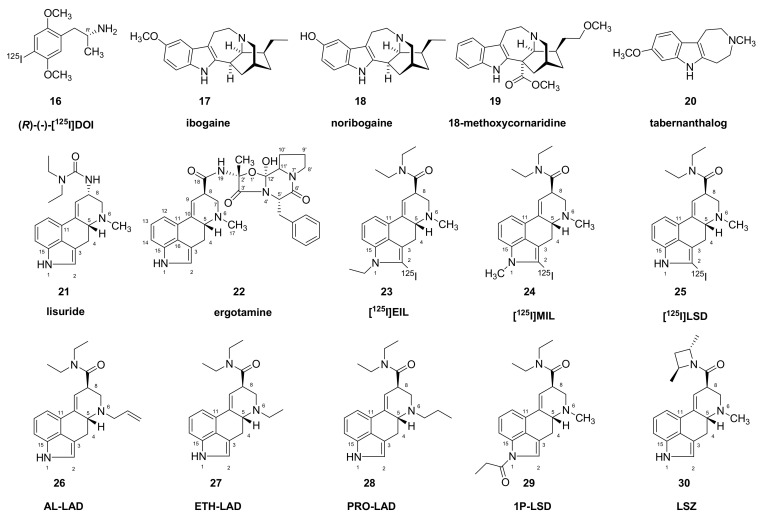
While the preponderance of evidence indicates that 5HT2A agonism is a necessary property of hallucinogens, this is not sufficient, since certain 5-HT2A receptor agonists such as lisuride (21) and ergotamine (22) (Figure 2) do not evoke hallucinations (e.g., [29]). Explaining this phenomenon may call for arguments from non-classical pharmacology, whereby agonists can engage different signal transduction pathways through the same receptor. Serotonin 5HT2A receptors typically couple to the Gq/11-mediated signaling pathway, which activates phospholipase C (PLC) to stimulate the formation of inositol phosphates and diacylglycerol, leading to Ca2+ release from the endoplasmic reticulum [30]. Although some hallucinogens only weakly stimulate this pathway, hallucinogenic potency may correlate with the efficacy in activating PLC [31]. On the other hand, LSD (1) was more effective at activating the 5HT2A/2C-coupled phospholipase A2 (PLA2) pathway that mediates arachidonic acid release, whereas the non-hallucinogenic compound 3-trifluoromethylphenyl-piperazine preferentially activated the PLC-IP pathway [32]. Hallucinogenic effects at 5HT2A receptors may also entail activation of the pertussis toxin (PTX)-sensitive heterotrimeric Gi/o proteins [33]. As such, it may be the second messenger pathways rather than the particular receptor targets that mediate psychedelic action. Furthermore, the 5HT2A receptor forms a functional heterodimer with the mGluR2 receptor, which evokes allosteric effects on serotonin agonist binding [34]; this interaction reduces the hallucinogen-specific Gi/o protein signaling and behavior and may account for the lack of hallucinogenic action of 2-bromo-LSD (5) noted above. Certainly, the 5HT2A/mGluR2 dimer adds an additional level of complexity to the mechanism of action of hallucinogens.
Figure 2.
Structure of selected ibogaine and lisuride derivatives.
In the special case of presynaptic autoreceptors, silencing of neuronal electrical activity upon drug application is a functional indicator of agonism. Early electrophysiological research showed that administration of LSD (1) at a low dose (5–10 µg/kg) provoked silencing of serotonin neurons in the rat dorsal raphé [35], presumably via activation of 5HT1A autoreceptors. Various other hallucinogenic compounds (psilocin (8), N,N-dimethyltryptamine [DMT (9)], and bufotenin (10)) inhibit serotonin neuron activity with a potency following the rank order of their potency as hallucinogens [36]. In electrophysiological studies, treatment with 5-HT1A receptor antagonist WAY-100,635 (500 μg/kg, i.v.) prevented the inhibitory effect of LSD (1) on the firing rate of dopaminergic ventral tegmental neurons in the rat brain [37]. In the same study, treatment with a blocker of the trace amine-associated receptor (TAAR) type 1 also interfered in the effects of LSD (1) on dopamine neuron activity. In vitro binding competition studies indicated that LSD (1) and other hallucinogens possess some affinity for TAAR1 [9].
2.2. Affinities of LSD at Neuroreceptors In Vitro
LSD (1), and likewise mescaline (6) (2 mg/kg), and 2,5-dimethoxyphenylisopropylamine (DOM, 11), silence noradrenergic neurons of the locus coeruleus (but potentiate their response to sensory stimuli) via their effects at serotonin 5HT2-like receptors [38]. Thus, to the first approximation, LSD (1) and some other hallucinogens act as agonists at serotonin autoreceptors to inhibit serotonin (43) release, while also acting at post-synaptic heteroceptors (5HT2) to reduce noradrenaline release This action can have the net effect of shifting the bias of serotonin signaling towards the 5HT2A receptors, while blunting noradrenaline signaling. Other research has shown that LSD (1) acts as a full or partial agonist at a broad range of serotonin receptors, including 5-HT1A, 5-HT2A, 5-HT2B, 5-HT2C, and 5-HT6 [39], and has relatively high affinity at dopamine D3 receptors in rat striatum cryostat sections [40]. Competition binding studies in vitro indicate that LSD (1) has a Ki of 3 nM at 5HT1A sites, 4 nM at 5HT2A sites, and 15 nM at 5HT2C sites [9]. In the same study, it was reported that LSD (1) has moderate affinity (Ki) at α1a sites (670 nM) and dopamine D1 sites (310 nM) and high affinity at α2 adrenergic sites (12 nM), dopamine D2 (25 nM) and D3 sites (100 nM), but little affinity for monoamine transporters. Others reported Ki values for LSD (1) of 0.54 nM at 5HT2A/C sites labelled with [3H]ketanserin, 0.43 nM at 5HT1A sites, and 6.6 nM at 5HT1B sites [41], thus confirming the considerable 5HT1-binding propensity of LSD (1).
2.3. Affinities of Hallucinogenic Phenylethylamines In Vitro
Under the same assay conditions as with LSD above in [41], the hallucinogenic compounds DOM (11), 4-bromo-2,5-dimethoxyphenylisopropylamine (DOB, 12) and various other phenylpropylamines had nM affinity only at [3H]-ketanserin (mainly 5HT2A) binding sites in vitro. That series of compounds had 10-fold lower affinity at 5HT2C sites and 1000-fold lower affinity at 5HT1A and 5HT1B sites, indicating much greater selectivity than LSD (1). A newer phenethylamine derivative 25CN-NBOH (13) had even higher 5HT2A selectivity over 5HT2C and 5HT2B receptors than other reported compounds [42].
Mescaline (3,4,5-trimethoxyphenethylamine, 6) is a hallucinogenic and psychostimulant natural product occurring in the peyote cactus (Lophophora williamsii) and other Mesoamerican cacti, which has been used for millennia for ritual and visionary purposes. Mescaline (6) binds with rather low affinity (Ki) as an agonist at 5HT1A sites (5 µM), 5HT2A/C (6 µM against [3H]-ketanserin), alpha2 (1.4 µM) and TAAR1 (3.3 µM) receptors [9,43]. Mescaline (6) was the first hallucinogen synthesized in the laboratory, and perhaps for this reason found early application in autoradiographic studies [44].
Psilocybin (2) ([3-(2-dimethlyaminoethyl)-1H-indol-4-yl] dihydrogen phosphate) is a naturally occurring hallucinogen from mushrooms of Psylocybe and other genera, which was first isolated in 1959 by the Swiss chemist Albert Hoffman. Initially distributed in the 1960s for use in psychotherapy, psilocybin (2) is again finding this application after a hiatus of four decades. Strictly speaking, psilocybin (2) is a prodrug, which undergoes rapidly hydrolysis in the gut and liver to yield the active and brain-penetrating metabolite psilocin (8). In vitro binding studies indicate that psilocin (8) is an agonist with moderate affinity (Ki) of 49 nM at 5HT2A sites, 94 nM at 5HT2C sites and 123 nM at 5HT1A sites, but >µM affinity at dopamine and adrenergic receptors [9]. Screening indicated a moderate affinity for psilocin (2) at 5HT2B sites [45], which may have some bearing on the propensity of psilocybin to cause cardiac valvulopathy. The corresponding Ki values against [123I]-DOI indicated ten-fold higher affinity at 5HT2A sites [10,14], which is presumably indicative of the greater competition between an agonist drug at agonist-labelled receptors, as has been established for the case of dopamine D2/3 receptors [46].
2.4. Affinities of Hallucinogenic Tryptamines In Vitro
The prototypic tryptamine hallucinogen DMT (9) had a Ki of 0.5 µM [47] or 2 µM [48] against (mainly) 5HT2A/C sites labelled with [3H]-ketanserin, indicating rather low affinity in vitro. Other displacement studies against [3H]-ketanserin likewise showed µM Ki at 5HT2A/C sites and insensitivity to addition of GTP, suggesting an antagonist interaction [49]. Prima facia, this seems unlikely since DMT (9) substituted for a 5HT2A agonist in a rat behavioral drug discrimination trial against the antagonist ketanserin (7) [50]. Furthermore, pretreatment with ketanserin (40 mg) blocked the visual hallucinations and electroencephalographic effects otherwise evoked by DMT (9) in healthy volunteers [51]. The generally low affinity of DMT (15) seen in [3H]-ketanserin displacement studies in vitro seems at odds with its much greater potency in functional assays, which showed a 38 nM EC50 for calcium mobilization in vitro [52]. This discrepancy doubtless reflects the ten-fold better competition of a series of indolylalkylamines such as 5-MeO-DMT (15) against [123I]-DOI (16)-labelled 5HT2A agonist sites as compared to [3H]-ketanserin-labelled 5HT2A antagonist sites [53]. On the other hand, in the displacement study [49], DMT had a 100 nM Ki against 5HT1A sites labeled with the agonist [3H]8-hydroxy-DPAT and a clear shift to the right in the displacement curve in the presence of GTP, indicating agonism. Others reported that DMT (9) had Kis of 0.25 µM at 5HT2A sites, 0.4 µM at 5HT2C sites, and only 0.1 µM at 5HT1A sites [9], again suggesting that DMT (9) may have a preferred action at 5HT1A sites. DMT (9) also showed an interaction with moderate affinity at sigma receptors [54]. Indeed, the activity of DMT (9) at sigma-1 receptors mediates cytoprotective properties against hypoxic neuron injury in vitro, and in the reperfusion injury model in vivo [55].
5-methoxy-N-methyl-N-isopropyltryptamine (5-MeO-MiPT, 14) is a hallucinogenic substituted tryptamine with moderate affinity at 5HT1A receptors (Ki = 60 nM) and 5HT2A (receptors Ki = 160 nM) [9]. 5-MeO-DMT (15) has similar affinity at 5HT2A receptors (Ki = 200 nM), under binding conditions where LSD (1) had a Ki of only 1 nM [47], and had >100-fold selectivity for 5HT1A/B/C receptors relative to 5HT2A receptors in vitro [56]. Thus, 5HT1A selectivity may be a general property of tryptamine hallucinogens. The 5-MeO-DMT (15) active metabolite 5-hydroxy-DMT (5-HO-DMT; bufotenine (10)) is a hallucinogenic compound present at psychoactive doses in the skin of the Colorado river toad Incilius alvarius, and other toad species. Bufotenine (10) had a Ki of 14 nM against 5HT2A binding sites labelled with the agonist [125I]-R-(-)DOI (16) [10]. Despite its relatively low affinity in vitro [56], 5-MeO-DMT (15) had a comparably high EC50 of 4 nM at 5HT2A sites in a functional assay of intracellular calcium mobilization [52], confirming its higher potency at these sites compared to DMT (9). Indeed, the strong association between hallucinogenic properties of a broad range of structural classes of molecules with 5HT2A affinity supports the use of antagonist drugs like ketanserin (7) as a treatment for drug-induced hallucinations [47]. On the other hand, pretreatment with the 5HT1A antagonist pindolol potentiated the hallucinogenic effect of intravenous DMT (9) in healthy volunteers, suggesting a breaking effect of 5HT1A receptors on 5HT2A-evoked hallucinations in humans [57]. Furthermore, the IC50 of DMT (9) and its derivatives at 5HT2A sites did not seem to correlate with visual hallucination intensity in humans [52].
2.5. The Strange Case of Ibogaine
Ibogaine (17) is a psychoactive compound from root bark of the iboga tree (Tabernanthe iboga), which is known as an oneirogen for the dreamlike quality of the hallucinations it can provoke. The characteristics of the ibogaine (17) structure are an indole, a tetrahydroazepine, and a bicyclic isoquinouclidine. An anecdotal report that ibogaine (17) reduced opioid craving found support from rat studies showing an attenuation of the morphine-induced dopamine release in rat striatum [58]. By some accounts, ibogaine (17) can protect from relapse from a wide range of abused substances of distinct pharmacology. Unlike other hallucinogens discussed in this review, ibogaine (17) was without notable affinity for serotonin 5HT2A receptors. However, its metabolite noribogaine (18) possessed some affinity (Ki 2 µM) as a partial agonist for µ-opioid [59] and κ-opioid receptors [60], although much less so than the κ-opioid agonist hallucinogen Salvinorum A. Ibogaine (17) also had some affinity for NMDA receptors, displacing [3H]MK801 from caudate membranes with an IC50 of 5 µM [61], which may account for its dissociative side effects. Ibogaine (17) also had moderately high affinity (Ki 2 µM) at dopamine transporters [62], albeit by binding to their inward facing conformation, which may attenuate amphetamine-evoked dopamine release. Ibogaine (17) and its metabolite noribogaine (18) enhanced the Gi/o-mediated inhibition of adenylyl cyclase by morphine or serotonin, while having no intrinsic effect on basal or forskolin-stimulated adenylyl cyclase [63]. This phenomenon may account for ibogaine’s (17) putative efficacy in treating addiction.
Ibogaine (17) has a considerable degree of toxicity, which has led to a number of fatalities. The less toxic ibogaine (17) congener 18-methoxycoronaridine (19) is likewise a putative anti-addictive compound, apparently due to its antagonism at α3β4 nicotinic acetylcholine receptors [64]. Tabernanthalog (20) and a series of other ibogaine (17) analogues lacking the isoquinuclidine retained the capacity to promote synaptic plasticity, while being much less cardiotoxic and teratogenic than ibogaine (17) itself [65].
3. Ex Vivo/In Vitro Binding Studies with Hallucinogens
3.1. LSD Derivatives
Early research into structure-function indicated that methylation of ergotamines at the N1 position enhances serotonin antagonism in the isolated rat uterus assay [66], while decreasing hallucinogenic potency predicted from a quantitative structure-activity relationship (QSAR) study [67].N-methyl-2-[125I]-iodo-lysergic acid diethylamide ([125I]-MIL, 24) was developed as a presumably non-hallucinogenic ligand for the molecular imaging of serotonin receptors, whereby N-methylation of [125I]-LSD (25) was intended to impart greater selectivity and sensitivity for 5HT2 receptors [23]. Studies in vitro with rat forebrain homogenates indicated that [125I]-MIL (24) had an apparent KD of 0.14 nM at 5HT2A receptors. However, [125I]-MIL (24) also showed a KD of 0.4 nM for 5HT2C receptors in vitro. The specific binding of [125I]-MIL (24) in mouse brain peaked at 45 min post injection, when the binding ratio relative to cerebellum was 4 in frontal cortex and 2 in striatum; lesser cortical binding and more rapid washout from frontal cortex was seen in corresponding studies with [125I]-LSD (25). In other ex vivo studies, ketanserin (7) evoked a dose-dependent displacement of [125I]-MIL (24) in mouse striatum and cortex, suggesting an IC50 of about 30 µg/kg ketanserin (7). Rat autoradiographic studies with [125I]-MIL (24) revealed that repeated doses with the non-hallucinogenic psychostimulant MDMA evoked a substantial down-regulation of 5HT2-like receptors [68], which may be a marker of the phenomenon of tolerance to certain hallucinogens.
D-(+)-N-ethyl-2-[125I]iodo-lysergic acid diethylamide ([125I]-EIL, 23) was developed as a ligand for molecular imaging of serotonin receptors. It had very high affinity for 5HT2A receptors in rat cerebral cortex, with a dissociation constant (KD) of 0.2 nM [69]. Following the precedent of N1-methylation, we suppose that [125I]-EIL (23) is likely to be an antagonist. Ex vivo studies indicated an extraordinary persistence of its specific binding in mouse brain relative to cerebellum, whereby the binding ratio was 9 at 16 h post injection. Ketanserin (7) displaced the cerebral binding, but dopamine D2 or adrenergic antagonists were without effect, consistent with a main interaction of [125I]-EIL (23) at 5HT2A sites. However, the authors predicted that [125I]-EIL (23) might also bind to 5HT2C receptors of the choroid plexus.
The active D-enantiomer of LSD (1) had 1000-fold higher affinity for serotonin receptors than the L-enantiomer [70]. Autoradiographic studies with D-[125I]-LSD (25) (200 pM) showed abundant binding in the extended striatum and the cerebral cortex, and nearly complete displacement of the cortical binding be co-incubation with R-(-)-DOB ((-)12, 500 pM), but only 50% displacement in striatum, consistent with the ambivalence of LSD (1) for dopamine and serotonin receptors [71]. Other autoradiographic studies with R-[125I]-DOI (16) showed an abundance of LSD-displaceable binding in the deep layers of the cerebral cortex and in the claustrum. However, there was only sparse binding in striatum, consistent with the ligand’s considerable specificity for serotonin receptors [72]. More detailed autoradiographic examination of D-[125I]-LSD (25) binding in rat brain indicated a single population of binding sites (KD 170 pM) in cerebral cortex, where the Bmax was about 4 pmol/g wet weight [73]. The binding in striatum was of similar density, but with a higher apparent KD (300 pM), indicative of the slightly lower affinity of LSD (1) for dopamine D2-like receptors. However, other binding studies with [125I]-LSD (25) revealed a significant ketanserin (7) displaceable component in rat striatum sections, ranging from 30% in rostral parts to 74% in the caudal regions [74].
3.2. Phenylethylamine Derivatives
Autoradiographic analysis of the rat brain revealed the time-dependent distribution of radioactivity at various times after intravenous injection of [14C]-psilocin at a dose of 10 mg/kg [75]. There was rapid initial cerebral uptake, resulting in concentrations of approximately 1% ID/g (injected dose/gram) at one-minute post injection. At 60 and 120 min post injection, binding remained high in the anterior cingulate cortex, amygdala, and hippocampus, with relatively lower concentrations in white matter. There was substantial washout of radioactivity from brain between four and eight hours post injection. This pharmacokinetic analysis was of total brain radioactivity, uncorrected for possible brain-penetrating metabolites, or metabolism in brain.
Studies with α-[14C]-mescaline in cat (25 mg/kg) showed a plasma half-life of two hours after intravenous injection, very rapid uptake into brain giving a brain/plasma ratio of 3 at one hour after injection, and persistent retention in brain, with only slight washout at six hours. Autoradiographic studies with [3H]-mescaline in the brain of marmoset monkeys (Callithrex jacchus) showed preferential accumulation in the hippocampus, amygdala, lateral geniculate and anterior cingulate cortex, persisting even 18 h after administration (8 mg, i.p.) [76]. Similar studies in mice with the non-hallucinogenic isomer of mescaline, [3H]-2,3,4-trimethoxy-β-phenylethylamine (4 mg) showed a more homogeneous pattern of binding [77], suggesting that mescaline (6) evokes hallucinations through specific receptors or binding sites. However, sensitive analyses with GS-MS showed a brain:serum ratio of only 0.3 at 60 min after mescaline (6) administration in rats (20 mg/kg, s.c.), with slow washout from brain suggesting a three-hour half-life [78]. Rats showed disruption of the startle reflect at 60 min but not at 10 min after treatment with mescaline (6) at the 10 mg/kg dose (s.c.), which presumably reflects the delay to absorption and brain entry.
2,5-Dimethoxy-4-iodoamphetamine (DOI) is a prototypical phenylethylamine 5-HT2A/2C receptor agonist, although having some affinity for 5HT1A receptors, as does a wide range of its phenylalkylamine derivatives [79]. Autoradiography with [125I]-DOI (16) can be used to study the functional desensitization of serotonin 5HT2-likereceptors after repeated doses of DOI or other agonists. Thus, chronic treatment with (+/−)-DOI (1 mg/kg daily for a week) significantly reduced the binding of [3H]ketanserin, [125I]-LSD (25), and R-[125I]-DOI (16) as measured at single ligand concentrations in rat cortical homogenates [80]. Saturation binding studies indicated that chronic DOI treatment significantly lowered the Bmax values for [3H]-ketanserin and R-[125I]-DOI (16) without altering the KD values. Repeated treatment of rats with (+/−)-DOI (1 mg/kg, i.p.) resulted in an attenuation of the DOI-induced release of the hypothalamic hormone oxytocin, which is indicative of receptor desensitization [81]. This functional desensitization was associated with reduced autoradiographic binding of R-[125I]-DOI (16) in the paraventricular nucleus, despite increased 5HT2A immunoreactivity to western blot analysis, suggesting an internalization process or altered coupling with intracellular G-proteins.
The compounds 2-(4-iodo-2,5-dimethoxyphenyl)-N-(2-methoxybenzyl)ethanamine (25I-NBOMe, 31) and 2-[[2-(4-iodo-2,5dimethoxyphenyl) ethylamino] methyl] phenol (25I-NBOH, 32) (Figure 3) are hallucinogenic 5HT2A agonists that have gained considerable notoriety due to cases of fatal intoxication. They undergo hydroxylation, O-demethylation, N-dealkylation, and dehydrogenation in vivo, mainly via CYP3A4 and CYP2D6 [82]. Relative to 2,5-dimethoxyphenethylamines (2C compounds) and DOI, the N-methoxybenzylated compounds had much higher affinity for 5-HT2A receptors labelled with the antagonist ligand [3H]-MDL100907 in vitro [83]. Binding assays against [3H]-ketanserin/[3H]-mesulergine, [3H]-LSD and [3H]-Cimbi-36 in vitro showed that 25CN-NBOH (13, N-(2-hydroxybenzyl)-2,5-dimethoxy-4-cyanophenylethylamine) had >52-fold Ki2C/Ki2A selectivity ratio and a 37-fold Ki2B/Ki2A ratio, and likewise showed substantial 5HT2A selectivity in functional assays of IP turnover. Various isomers of 25H-NBOMe in which the two methoxy-groups are in different positions (ortho, meta, and para) were compared with respect to their efficacy in activating signaling pathways, in conjunction with molecular docking studies at the 5HT2A receptor binding pocket [66]. In the series examined, several dimethoxy compounds proved to have an efficacy exceeding that of LSD (1).
Figure 3.
Structures of some dimethoxyamphetamines and serotonin receptor antagonists.
4. Molecular Imaging Studies In Vivo with Hallucinogens
4.1. LSD Derivatives
One of the very first receptor PET molecular imaging studies employed N1-([11C]-methyl)-2-bromo-LSD ([11C]-MBL, 33) as a non-hallucinogenic ligand for serotonin 5-HT2A receptors [84]. The authors first tested the pharmacological specificity of MBL in vitro, finding a Ki of 0.5 nM at 5HT2 receptors, versus 4 nM at D2 receptors and weaker interactions with α1 adrenergic (Ki = 250 nM) and serotonin 5HT1A receptors (Ki = 34 nM). A PET study with [11C]-MBL (33) in baboon (0.1 µg/kg body weight) indicated relatively high binding throughout cerebral cortex, with a peak binding ratio of 1.4 at 40 min that tended to decline in the following 45 min; this binding was displaced by ketanserin (7) pretreatment. Similar results were seen in an awake human, with a maximal binding ratio of about 2:1 prevailing in cerebral cortex during 20–60 min post-injection.
4.2. Phenylethylamine Derivatives
In a SPECT study of healthy human volunteers, oral administration of 4-bromo-2,5-dimethoxy-phenylisopropylamine (2,5-dimethoxy-4-bromoamphetamine; DOB, 12) labelled with 77Br or 82Br showed a rather delayed cerebral uptake in brain of human volunteers, which the authors attributed to a metabolite rather than the parent compound [85]. Subsequent SPECT studies with 2,5-dimethoxy-4-[123I]-iodoamphetamine (R-[123I]‑DOI; [1-(4_iodo-2,5-dimethoxyphenyl)-propane-2-amin]) of high specific activity showed high uptake in thalamus, cortex, and striatum, and lesser accumulation in the midbrain and cerebellum in baboon [86]. However, there was no displacement of the uptake by treatment with ketanserin (7), suggesting extensive entry of labelled metabolites into brain.
The phenylethylamine 5-HT2A receptor agonist 2-(4-iodo-2,5-dimethoxyphenyl)- N-(2-[11C-OCH3]methoxybenzyl) ethanamine ([11C]-Cimbi-5, 34) was investigated as a potential PET tracer in rats ex vivo and in pigs in vivo [87]. It had a Ki of 2 nM at 5HT2A and 5HT2B sites, 7 nM at 5HT2C sites, and much less affinity at other neuroreceptors in vitro. Rat-PET studies showed a peak binding ratio at about 30 min after tracer injection, and nearly complete displacement by ketanserin (7) treatment, and pig PET studies showed 75% displacement by ketanserin (7). HPLC analysis of plasma samples indicated that a lipophilic metabolite came to comprise about 20% of the plasma radioactivity; this metabolite was nonetheless absent from brain and thus unlikely to interfere with reference tissue quantitation of [11C]-Cimbi-5 (34) binding. Others conducted a comparative PET study of [11C]-Cimbi-5 (34) and the antagonist [11C]-MDL100907 (35) in living non-human primates, finding that the antagonist ligand had two or three-fold higher BPND than [11C]-Cimbi-5 (34) in most brain regions [88]; pretreatment with MDL100907 did not completely displace [11C]-Cimbi-5 (34) binding in all brain regions, indicating somewhat incomplete selectivity.
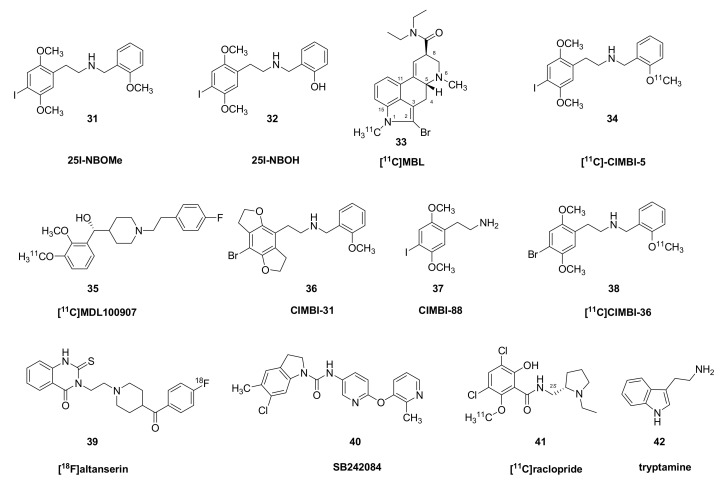
A series of phenylethyalamines in the Cimbi series showed Kis in vitro against the binding of [3H]-MDL100907 ranging from 0.2 nM (Cimbi-31, 36) to 47 nM (Cimbi-88, 37); their receptor agonism was assessed from PI hydrolysis in GF62 cells overexpressing the 5-HT2A receptor [89]. Furthermore, a series of nine structurally similar compounds of the Cimbi phenethylamine class had a ten-fold range in the affinity at 5HT2A sites and a 100-fold range in their ED50 for activation of IP hydrolysis [89]. However, neither property predicted the specific binding (BPND) in brain, which ranged from 0.2 to 1.0. The best of the series with respect to specific signal and washout from cerebellum was [11C]-Cimbi-36 (38). In brain of living rat, [11C]-Cimbi-36 shows preferential uptake in frontal cortical regions and relatively little uptake in the striatum, diencephalon and cerebellum (Figure 4).
Figure 4.
[11C]-Cimbi-36 (38) activity summed over the 45 min scan time in rat brain (right) overlaid on an MR template image in the horizontal plane (left). High activity in cortical regions, especially mPFC, moderate activity in striatal and hippocampal regions and low binding in cerebellum.
Further PET investigations of [11C]-Cimbi-36 (38) in healthy volunteers showed BPNDs, which ranged from 0.25 in striatum to 1.7 in broad cortical regions, and showing a high degree of covariance between repeat measures in the same subjects [90]. In a head-to-head study there was generally high correlation between [11C]-Cimbi-36 (38) and [18F]-altanserin (39) BPND estimates in most brain regions, but significantly greater binding of [11C]-Cimbi-36 (38) in hippocampus and choroid plexus. The authors interpreted this to indicate the composite of 5HT2A and 5HT2C receptors in that structure; whereas [11C]-Cimbi-36 is nearly equipotent at 5HT2A and 5HT2C receptors, altanserin has nearly 100-fold selectivity for 5HT2A binding sites [91]. Similar studies in non-human primate supported those findings, showing a high degree of concord between [11C]-Cimbi-36 (38) and [11C]-MDL100907 (35) binding in most brain areas, and substantial displaceability by ketanserin (7) in all regions but cerebellum [92]. However, there was only partial displaceability of [11C]-Cimbi-36 (38) binding in hippocampus and choroid plexus by treatment with the 5HT2C antagonist SB 242084 (40), again consistent with a mixed signal in those regions. The metabolism of [11C]-Cimbi-36 (38) in humans is characterized by loss of the [11C]-methoxy label (generating [11C]-formaldehyde) or demethylation of the other methoxygroup, yielding a relatively hydrophobic radiometabolite [93].
4.3. Tryptamine Derivatives
DMT (9) obtained a brain:blood partition ratio of about 5:1 after intraperitoneal injection in the rat, but disappears rapidly from tissue and circulation due to metabolism [94]. A planar scintigraphy study examined the biodistribution of radioactivity in rabbits following intravenous injection of 2-[131I]iodo-DMT [95]. The brain activity reached a peak about 30 s after injection, when the brain:blood ratio was approximately unity in the olfactory bulb, thus indicating very fast passage across the blood–brain barrier. Remarkably, traces of activity remained in the olfactory bulb (but not elsewhere in the brain) for several days after administration; the authors suggested that this might reflect trapping in vesicles and noted that a rabbit study with 2-[131I]-iodo-tryptamine showed no comparable retention in brain. They authors did not undertake any displacement studies to confirm specific binding, nor did they pretreat the rabbits with a monoamine oxidase (MAO) inhibitor, arguing that the intravenous route of administration avoided first pass metabolism in the liver.
4.4. Competition from Hallucinogens at Dopamine Receptors In Vivo
In the PET competition paradigm, reductions in the availability of sites for radioligand binding can reveal occupancy or target engagement after challenge with another pharmaceutical that interacts with the same target. Alternatively, a treatment that mobilizes the release on an endogenous neurotransmitter can also evoke displacement of the radiopharmaceutical in living brain. This is a well-established paradigm for detecting competition at dopamine D2/3 receptors in living striatum. In one such PET study, healthy volunteers were scanned with the D2/3 antagonist [11C]-raclopride (41), first in a placebo baseline, and again after administering a psychoactive dose of psilocybin (2) (0.25 mg/kg p.o.) [96]. Comparison of the two scans revealed a global 20% decline in [11C]-raclopride (41) binding in the striatum, which is similar to the displacements evoked by amphetamine or other strong releasers of dopamine. Furthermore, the decline in the ventral striatum correlated with individual ratings for euphoria and depersonalization. In formal terms, the reduced [11C]-raclopride (41) binding could be indicative of competition from psilocin (8) at the D2/3 receptors, or enhanced release of endogenous dopamine. Rat microdialysis studies showed that psilocin (8) (10 mg/kg) evoked a transient 40% increase in interstitial dopamine levels [97], which would seem insufficient to account for the 20% displacement by low dose psilocybin (2) in humans. Nor does the reported affinity of psilocin (8) at dopamine receptors seem sufficient to support a significant direct occupancy in vivo.
The effects of intravenous challenge with acute LSD (1) (2.5 µg/kg) on dopamine D2/3 receptor availability was tested in a [11C]-raclopride (41) PET study of anesthetized pigs [98]. There was no immediate effect on the striatal [11C]-raclopride (41) BPND, but there was a 19% decline at four hours after the challenge, which seemed consistent with a high affinity component of the displacement of [3H]-raclopride binding by LSD (1) in pig brain sections. Furthermore, their rat microdialysis studies did not indicate any effect of LSD (1) on dopamine release per se, suggesting that the [11C]-raclopride (41) binding reduction must be due to direct competition from LSD. However, the time delay to a main effect suggests that some other pharmacological mechanism or methodological factor may have been at play. The pharmacokinetics of oral LSD (1) (100 and 200 µg) in human subjects indicated a mean plasma half-life of 2–6 h and a persistently close relationship between the individual LSD (1) concentration in plasma and the magnitude of subjective response within subjects, with moderate counterclockwise hysteresis during the 12 h after dosing [99]. Thus, one might have expected simple competition by LSD (1) at [11C]-raclopride binding sites in pig brain in the first post LSD (1) scan, rather than with a delay of several hours.
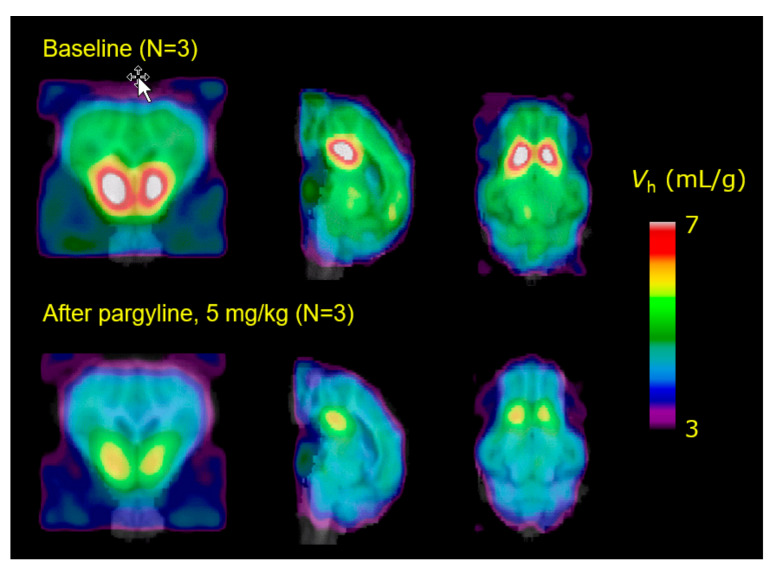
Further PET studies of a generalization of the ayahuasca phenomenon (see below) were intended to test the hypothesis that MAO inhibition should potentiate the amphetamine-evoked release of dopamine in living striatum. Here, we used the amphetamine challenge paradigm to detect increased competition by dopamine at striatal dopamine D2/3 receptors labelled by [11C]-raclopride. The amphetamine challenge evoked the expected 15% displacement of [11C]-raclopride in striatum of living pigs, but there was no potentiation of the amphetamine effect in pigs pretreated with pargyline at a dose sufficient to block completely the specific binding of [11C]-harmine (48) (Figure 5) to MAO-A [100]. Neither was the expected potentiation of amphetamine-evoked dopamine release seen in a [11C]-raclopride PET study in rats with MAO inhibition [101]. Conceivably, increased signaling by tyramine or phenylethylamine at TAARs upon the treatment with an MAO inhibitor may have interfered via autoreceptor effects with the potentiation of dopamine release [102]. We have developed [18F]-fluoroethylharmol (49) as an alternative PET tracer for MAO-A in brain [103], with potential applications in the study of the pharmahuasca phenomenon.
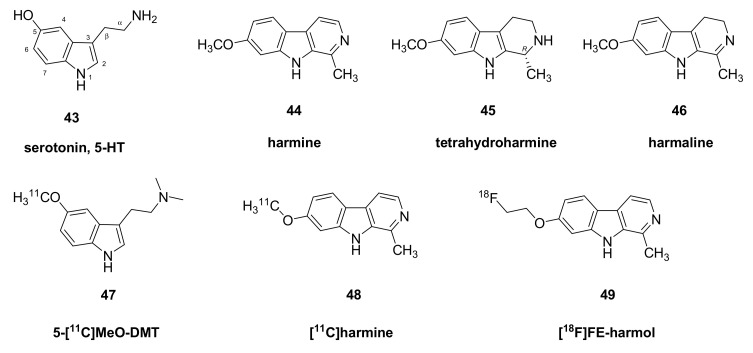
Figure 5.
Structures of serotonin and some indole alkaloids.
4.5. Competition from Hallucinogens at Serotonin Receptors In Vivo
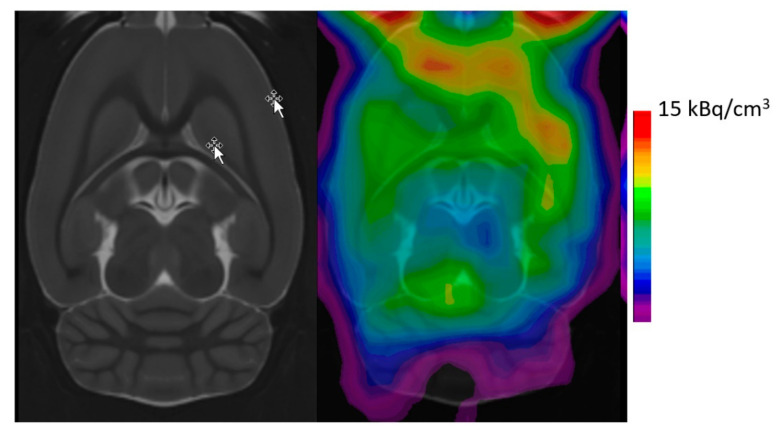
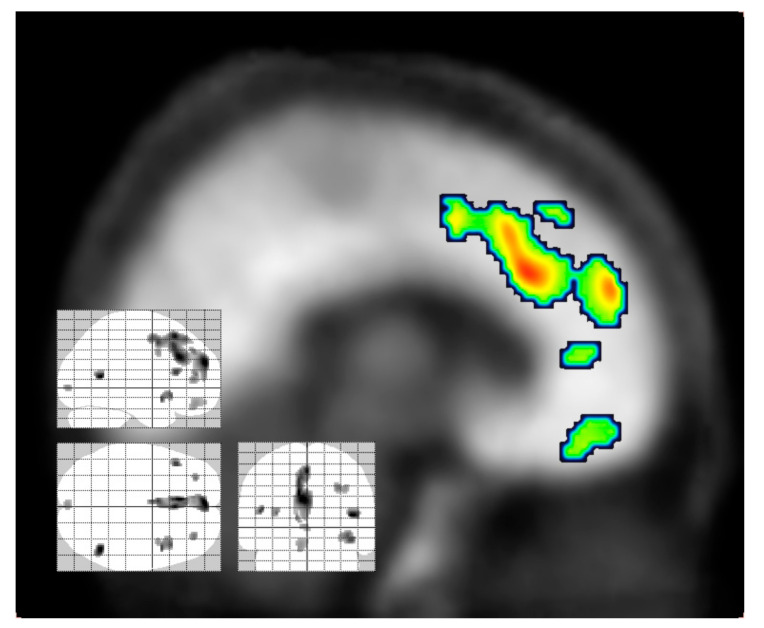
In a generalization of the competition PET model, reductions in the availability of binding sites for the serotonin 5HT2A antagonist [18F]-altanserin (39) are indicative of increased release of endogenous serotonin after challenge with dexfenfluramine [104], and/or target engagement by competing drugs. In a PET study of 11 healthy young male subjects, [18F]-altanserin (39) binding was measured at baseline, and (two weeks later) again at 75 min after administration of psilocybin (2) (20 mg). The drug treatment provoked widespread 50% decreases in the uptake (DV’) of the tracer in the dorsolateral prefrontal cortex, orbitofrontal cortex, medial temporal cortex, and other cortical regions. Voxelwise regression analysis showed that the binding reductions in the anterior cingulate spreading to the dorsomedial prefrontal cortex correlated with higher scores in the Altered States of Consciousness Rating Scale (5D-ASC) (Figure 6).
Figure 6.
Inverse Correlation of 5D-ASC Global Scale scores and [18F]-altanserin (39) apparent distribution volume [DV’]. Results of a voxel based correlation analysis (Δ 5D-ASC global vs. ΔDV’, threshold p < 0.005, uncorrected) using Statistical Parametric Mapping [105]. Reproduced with permission.
In an exemplary study of its type, Madsen et al. tested the occupancy of psilocin (8) at serotonin 5HT2A receptors in brain of human volunteers relative to plasma drug concentrations after administration of psilocybin (2) at doses in the range of 3 to 30 mg [106]. In the Madsen PET study, cerebral 5HT2A receptor availability was measured using the agonist ligand [11C]-Cimbi-36 (38). Results indicated a dose-dependent brain receptor occupancy as high as 76%, which occurred when the plasma psilocin (8) concentration was about 100 nM. Furthermore, the intensity of the psychedelic experience correlated with receptor occupancy, and with the plasma psilocin (8) concentration, assuming a single site model. These calculations assumed steady states in the drug concentration and intensity during the PET measurement, which the authors showed to be approximately true on the time scale of about two hours. Their data also showed a rough relationship between the duration of the hallucinogenic experience (60–360 min) and the interval in which the plasma psilocin (8) concentration exceeding approximately 10 nM. Interestingly, the occupancy by psilocin (8) at [11C]-Cimbi-36 (38) agonist binding sites (circa 60%) was quite similar to the displacement of [18F]-altanserin (39) by a similar dose of psilocybin (2) reported by Hasler et al. [105]. This finding calls into question the assumption that agonist receptor ligands are intrinsically fitter than antagonist ligands for the detection of competition from other agonists. Nonetheless, Jorgensen et al. argued that the occupancy of 5HT2A sites labelled with [11C]-Cimbi-36 (38) by endogenous serotonin in anesthetized pig increased from 17% at baseline to 44% after fenfluramine treatment, which transiently increased the interstitial serotonin content in cortex ten-fold according to microdialysis [104]. This sensitivity of [11C]-Cimbi-36 (38) binding to fenfluramine challenge seemed to exceed that reported earlier for [18F]-altanersin (39) in healthy human volunteers, albeit at a lower relatively lower dose of fenfluramine in human [104].
At baseline in healthy individuals, at least, there was no significant association between the trait for openness to experience with 5HT2A availability, either measured with the antagonist [18F]altanserin (39), or with the agonist ([11C]-Cimbi-36 (38) [107]. However, a single dose of psilocybin (2) provoked in healthy individuals a long-lasting increase in scores for the personality traits of openness to experience and mindfulness, which correlated inversely with reductions in [11C]-Cimbi-36 (38) binding [106]. Recent work shows that a single dose of psilocybin (2) at a presumably hallucinogenic dose (0.1 mg/kg, i.v.) reduced by up to 50% the cortical abundance of 5HT2A binding sites labelled in vitro with [3H]-MDL100907 or [3H]-Cimbi-36 [108]. Other examinations in the same pig brain samples with the synaptic vesicle protein 2A (SV2A) ligand [3H]-UCB-J showed a significant 5–10% increase in synaptic density in hippocampus, occurring in association with the down-regulation of serotonin receptors. This phenomenon suggests that the benefits of psilocybin (2) in a therapeutic setting may be due to an enhancement of synaptic density and or plasticity; it might be more correct to suggest that the treatment reinstates the synaptic overshoot that occurs early in post-natal brain development, which may set the stage for plastic changes in synaptic plasticity.
In a recent rodent study, a single dose of DOI exerted rapid effects on the dendritic spine structure in frontal cortex that were dependent on 5HT2A receptors [109]. The same treatment evoked chromatin changes that persisted long after the DOI treatment, suggesting that therapeutic responses to hallucinogen treatment may arise through persistent and epigenetic changes in synaptic architecture. Others have recently used chronic two-photon microscopy to monitor synaptic spine density in mouse cortex [110]. In female mice, a single dose of psilocybin (1 mg/kg, i.p.) evoked a 20% increase spine density in layer V of the frontal cortex that persisted for up to 34 days, along with a sharp increase in spine dimension that peaked at day one and declined over the following week; these changes were scarcely evident in male mice. Overall, these structural studies concur with the SV2A results discussed above, and fit into a general framework whereby rapid antidepressant responses to ketamine also occur along with dendritic expansion, albeit by a different mechanism [111].
5. Metabolism of Hallucinogenic Compounds
5.1. LSD
LSD (1, 100 µg) attained a maximal plasma concentration of 4 nM at two hours after oral administration in healthy volunteers, and declined thereafter with an approximately four hour half-life [99]. The subjective effects, both good and bad, closely tracked the plasma concentrations, as did physiological responses, such as heart rate and blood pressure increases. The metabolism of LSD (1) is complex, but the predominant pathway in human involves microsomal formation of 2-oxo-3-hydroxy-LSD; whereas N-demethylation occurs in animals, this may not be an important pathway in humans [112].
5.2. Phenylethylamines
After intravenous of [14C]-psilocin in the rat, there was rapid uptake of radioactivity in the brain, followed by substantial biliary elimination [113]. Chromatographic analysis indicated that the major eliminated metabolites were the glucoronate and 4-hydroxyindoleacetic acid. In rats, metabolism of psilocin (8) occurs in part by oxidative deamination to 4-hydroxy-3-indoleacetic acid, but in humans, the predominant metabolite is psilocin-glucuronate [114]. As noted above, psilocybin (2) undergoes rapid de-phosphorylation after oral administration, and the centrally active metabolite psilocin (8) had a plasma elimination half-life of about three hours in healthy humans [115].
The diemethoxyphenethylamines such as [11C]-Cimbi-36 are metabolized in pigs and humans by demethylation, usually in the 5-position, and subsequently glucuronation [116]. Comparison of two forms of [11C]-Cimbi-36 showed that labelling on the 5-position yielded a lower specific binding in pig brain, apparently due to the formation of [11C]-formaldehyde or other brain-penetrating labelled metabolites [117]. A recent detailed pharmacokinetic analysis of the 5HT2A-prefering agonist 25CN-NBOH showed a complex metabolic profile in living rats, with debenzylation, demethylation, and hydroxylation, mediated by perhaps half a dozen cytochrome enzymes; the compound showed good distribution across the blood–brain barrier, measured ex vivo [118].
5.3. Tryptamimes
Remarkably, there is evidence that DMT (9) may be an endogenous neurotransmitter. Ultracentrifugation studies of rat brain indicated that DMT (9) is present in a neuronal vesicle fraction, along with its precursor, tryptamine (42) [119]. The enzyme indolethylamine-N-methyltransferase (INMT) is present in mammalian brain [120] and can catalyze the formation of DMT (9) from tryptamine (42), or bufotenin (10) from serotonin [121]. The brain enzyme uses S-adenosylmethionine as a methyl donor for the successive formation of N-methyltryptamine and then DMT (9) [122]. The INMT enzyme co-localizes in ventral horn cholinergic synapses called C-boutons/C-terminals expressing the sigma1 receptor, which was previously implicated in the neuroprotective action of DMT (9) [123]. Cerebral microdialysis studies in rats indicated a cortical interstitial DMT (9) concentration of about 1 nM, which was similar to that measured for serotonin in the same samples. The cortical DMT (9) measurements were unaffected by removal of the pineal gland, which has the highest INMT activity and DMT (9) concentration in the body, thus indicating local formation in brain [124]. Indeed, the production of DMT (9) by the pineal gland would hardly suffice to provoke central effects via its release into the circulation and subsequent uptake across the blood–brain barrier [125], which may cast doubt upon the plausibility of a physiological role for DMT (9). The substituted tryptamine compounds are characterized by rapid metabolism in vivo through O-demethylation by CYP2D6, and by oxidative deamination by MAO [126], such that the main metabolites of 5-MeO-DMT (15) in mouse urine are DMT-glucuronate and 5-methoxy-indoleacetic acid [127]. As shall be discussed below in some detail, the importance of MAO-A for the first past metabolism of DMT (9) accounts for the Ayahuasca effect, in which the hallucinogenic effects of oral DMT (9) are potentiated by co-treatment with an MAO inhibitor. This may have some bearing on the possible physiological actions of endogenous DMT (9), at least under conditions of pharmacological MAO inhibition.
6. Ayahuasca and Pharmahuasca
As noted above, DMT (9) undergoes rapidly metabolism by MAO in the gut and liver, and does not normally attain sufficient blood levels to evoke a hallucinogenic experience, unless taken at very high doses. Ayahuasca refers to a traditional method to enhance the effectiveness of DMT (9) by co-treatment with an MAO inhibitor. Ayahuasca is a Quechua word from Aya meaning “spirit, soul” in reference to its visionary effects and Waska, meaning “rope” or “woody vine”, referring to its source from the vine Banisteriopsis caapi together with the leaves of the shrub Psychotria viridis. The latter plant contains DMT (9), a hallucinogenic tryptamine that acts as a 5-HT1A/2A/2C agonist [54,128]. However, Banisteriopsis caapi supplies various β-carboline alkaloids (harmine (44), tetrahydroharmine (45), and harmaline (46)) that act as reversible inhibitors of MAO type A (IC50 2 nM [129]). Thus, the consumption of the two plants together results in a potentiation of the absorption of DMT (9), which provokes a hallucinogenic experience lasting 2–4 h. Practiced since pre-Columbian times, Ayauhuasca retains an important ritual function among certain Amerindians, and Brazilian law protects its use as such. Ayahuasca, or its chemical equivalent known as pharmahuasca, has emerged as a tool for psychotherapy in the contexts of affective and substance use disorders [130,131], thus calling for a better understanding of its possible mechanisms of action.
There is abundance of preclinical evidence indicating that MAO inhibition potentiates the central action hallucinogenic tryptamines. For example, treatment of rats with harmaline (46) (2–15 mg/kg, i.p.) greatly potentiated the behavioral effects of 5-MeO-DMT (15), causing hyperactivity at a subthreshold dose of the tryptamine compound (2 mg/kg, i.p.) [132]. Furthermore, 5-MeO-DMT (15) (1 mg/kg i.p.) was without effect on pre-pulse inhibition of the startle reflex in rats, unless following upon treatment with an MAO-A inhibitor; the pretreatment increased the plasma concentrations of 5-MeO-DMT (15), without altering the formation of the active metabolite, bufotenin [133]. Finally, deuterium substitution of 5-MeO-DMT (15), which results in reduced metabolism, increased its behavioral effects in rats to a profile similar to that evoked by ordinary 5-MeO-DMT (15) in conjunction with MAO-A inhibition [56].
We have attempted to investigate the basis of Ayahuasca polypharmacology in PET studies using the hallucinogen 5-[11C]MeO-DMT (47), instead of labelled DMT (9). There was rapid uptake of 5-[11C]MeO-DMT (47) in brain of anesthetized pigs, but with little evidence of heterogenous distribution matching that expected for a 5HT2A ligand; indeed, efforts to increase its uptake in pig brain by pretreatment with the MAO inhibitor pargyline (Figure 7) or displace its binding in pig brain with ketanserin (7) were unsuccessful. We were unable to account for the negative results, but suppose that the Bmax/KD ratio may simply have been too low to impart a measurable BPND. This pharmacological identity of the “hotspot” in pig ventral striatum remains unknown.
Figure 7.
Mean parametric maps of the total distribution volume of 5-[11C]-MeO-DMT (47) in brain of groups of three pigs at baseline and after treatment with the irreversible MAO A/B inhibitor, pargyline. There was no evidence of potentiation of the tracer uptake by blockade of MAO, nor was the binding in ventral striatum displaceable in studies with ketanserin (7) pretreatment (Jensen and Cumming, unpublished observations).
7. Effects of Hallucinogens on Energy Metabolism and Cerebral Blood Flow
7.1. Cerebral Glucose Metabolic Rate
Agonism at serotonin receptors might have intrinsic effects on neuronal energy metabolism. The 2-[14C]deoxyglucose autoradiographic method gives qualitative or quantitative estimates of the local rate of cerebral glucose consumption (CMRglc) based on the semi-irreversible metabolic trapping of the tracer in living cells. Administration to awake (but immobilized) rats of LSD (1) (15 or 150 µg/kg, i.v.) evoked widespread 10–30% reductions in CMRglc, notably throughout neocortex, and in thalamus, lateral geniculate, the basal ganglia, and the raphé nuclei, but with little effect in cerebellum [134]. In that study, treatment with 5-MeO-DMT (15, 0.2 or 2 mg/kg, i.v.) provoked similar patterns of reduced CMRglc, although generally of lower magnitude than the reductions seen with LSD (1). These rather widespread reductions of CMRglc stand in contrast to findings with selective agonists of 5HT1A receptors (1 mg/kg 8-hydroxy-2-(di-N-propylamino)tetralin) or 5HT1B receptors (3 mg/kg 5-methoxy 3-(1,2,3,6-tetrahydro-4-pyridinyl)-1H indole succinate). Both of those treatments evoked increased 2-[14C]-deoxyglucose trapping in cerebellum and motor cortex, and decreases in hippocampus, whereas the 5HT2B agonist also evoked large increases in the basal ganglia [135]. Thus, one might suppose that net effects of hallucinogens on cerebral glucose metabolism results from drug actions at multiple serotonin receptor types, which may have opposing individual effects. Clearly, there is a need to undertake quantitative CMRglc studies with other hallucinogens of greater subtype specificity than is afforded by LSD (1) or 5-MeO-DMT (15). In addition, gender differences in response to psilocin [136] or the stress due to immobilization may also have been factors influencing the effects on CMRglc in rat brain.
The effect of psilocybin (2) (15 or 20 mg, p.o.) on CMRglc was tested in a human [18F]-fluorodeoxyglucose (FDG) PET study, in which post-drug findings were compared with the volunteers’ own baseline PET recordings [137]. Results in a mixed gender group of (n = 10) healthy volunteers indicated a global increase in CMRglc after treatment, which was most distinct (+25%) in the frontal cortex, anterior cingulate and medial temporal cortex, with lesser increases (+15%) in the basal ganglia and sensorimotor and occipital cortical regions. The increases in CMRglc were bilateral and roughly symmetrical, but with a tendency for more pronounced increases in the right hemisphere. Several of the regional increases correlated positively with scores in “hallucinatory ego disintegration”, which lead the authors to compare psilocybin (2) effects with the hypermetabolism in frontal cortex reported during acute exacerbations in patients with chronic schizophrenia.
Another human PET study investigated FDG uptake in eight subjects starting 90 min after administration of psilocybin (2) (0.2 mg/kg, p.o.), with quantitation relative to an arterialized venous blood input function. Relative to a control group, the treatment provoked 5–10% increases in CMRglc in frontal operculum, anterior cingulate cortex, and inferior temporal cortex, along with 5–10% decreases in the precentral cortex and thalamus in a study by Gouzoulis-Mayfrank et al. [138]. Whereas Vollenweider et al. [137] reported symmetrical changes in CMRglc, Gouzoulis-Mayfrank et al. [138] saw greater effects in the right hemisphere. They also reported significant correlations between scores in psychometric tests with CMRglc changes in several brain regions. There was relatively little overlap between the patterns of altered CMRglc in subjects receiving psilocybin (2) versus the non-hallucinogenic indirect serotonin/dopamine agonist methylendioxymetamphetamine (MDMA). This may relate to the greater pharmacological specificity of psilocybin (2), which is a mixed 5HT2/5HT1 agonist. However, that study calculated psilocybin-induced CMRglc changes relative to values in an untreated control group [138]; comparison relative to own baseline values as in the earlier study [137] might have given a more sensitive indication of the pattern of psilocybin effects.
7.2. Cerebral Perfusion
PET studies with [15O]-water in anesthetized pig did not indicate any effects of LSD (1) treatment on cerebral perfusion [98]. In contrast, arterial spin labeling (ASL) measurements of cerebral perfusion indicated that LSD (1) increased CBF in visual cortex of human volunteers [139]. The increased CBF and the extent of the functional connectivity of the visual cortex correlated with the intensity of visual hallucinations; we suppose that anesthesia may have interfered in the effects of LSD (1) on CBF in the pig PET study. Furthermore, we did not measure plasma levels of LSD (1) in the pig, so we cannot exclude that possibility of mis-injection of LSD (1), perhaps due to adherence the drug to plastic syringes.
Perfusion SPECT studies in a group of (n = 12) healthy men showed that administration of mescaline evoked reduced blood flow in the frontal lobe, especially on the right side, which was correlated with impairment in a face/non-face task associated with the right frontal lobe [140]. A group of 15 healthy males with previous hallucinogen experience had perfusion SPECT scans before and after receiving authentic Ayahuasca at a dose of 1 mg DMT (9)/kg [141]. In contrast to results for mescaline, the Ayahuasca treatment provoked bilateral activations of perfusion in the anterior insula (which were more pronounced in the right hemisphere), along with activation in the right anterior cingulate/frontomedial cortex, and the left amygdala. These activations coincided with distinct increases in score in a hallucinogen rating scale. The authors interpreted these findings in functional anatomic terms as indicative of increased interoception and somatic awareness (insula), motivational state (cingulate) and emotional arousal (amygdala). This increased right side perfusion after Ayahuasca [141] and the right side hypermetabolism after psilocybin [137] seem at odds with the right side hypoperfusion after mescaline [140]. These discrepancies could well relate to differing actions of the hallucinogens, which may be distinct with respect to effects on flow-metabolism coupling. This could result in the generally opposite effects on perfusion and glucose consumption.
In a clinical trial of Ayahuasca, a group of 17 patients with recurrent major depressive disorder received a single dose of authentic Ayahuasca containing approximately 120 mg DMT (9) and 32 mg harmine (44) [142]. The investigators administered various psychometric rating scales in the hours and weeks after the single treatment, and recorded SPECT scans for CBF at baseline and at eight hours after the drug administration. The score in the Clinician Administered Dissociative States Scale (CADSS) peaked at about 80 min after drug administration, and the mean Hamilton depression rating scales declined from 25 to 15 in the three hours after administration, and remained around 10 during the following three weeks. Parametric mapping of CBF changes indicated increases in some very small clusters (<50 voxels) localized to the left nucleus accumbens, right insula, and left cingulate cortex, which the authors felt to be regions activated by antidepressant treatments. While similar in distribution, the magnitude of the CBF response in depression patients was distinctly less than that in the study of healthy volunteers by Riba et al. [141]. This could indicate a functional inactivation of serotonin receptors in the depressed state.
In a case study using SPECT, a patient suffering from alcohol dependence underwent a trial treatment with ibogaine hydrochloride (17 HCl, 1.5 g) followed two days later with vaporized 5-MeO-DMT (15, 5–7 mg) [143]. The patient experience insightful visions during the ibogaine (17) treatment, and later reported a decline in alcohol consumption. Relative to baseline perfusion SPECT imaging, there were post-treatment increases in brain perfusion in bilateral caudate nuclei, left putamen, right insula, as well as temporal and occipital cortex and cerebellum.
In recent years, functional MRI (fMRI) measures of perfusion with arterial spin labelling (ASL) have come to supersede SPECT and PET methods. In one such study, mixed gender groups of (n = 29) volunteers underwent an ASL examination of cerebral perfusion after treatment with psilocybin at a low dose (0.16 mg/kg) or high dose (0.22 mg/kg) [144]. The psilocybin treatments evoked absolute reductions in perfusion in widespread brain regions including the neocortex, insula, hippocampus, and striatum; the authors showed that global normalization resulted in apparent increases in perfusion in frontal regions. This seems generally consistent with findings in another fMRI study, which showed decreased BOLD signal and absolute perfusion in hub regions including the thalamus and cingulate cortex of (n = 15) healthy volunteers treated with psilocybin [145]. Interestingly, these same brain regions have a notably dense serotonin innervation; hybrid scanning with fMRI-ASL in conjunction with serotonin receptor PET imaging may held to establish the relationship between hallucinogen binding sites and cerebral perfusion. The ASL findings generally concur with SPECT perfusion studies in healthy controls showing reduced cerebral perfusion after treatment with hallucinogens. Since this review focusses on molecular brain imaging, we refer readers elsewhere for a comprehensive review of fMRI studies on hallucinogen actions [8].
8. General Conclusions
There is general agreement that the hallucinogenic compounds reviewed herein share the property of agonism at 5HT2A sites, but some compounds also have high affinity at other serotonin receptor subtypes, notably 5HT2C and 5HT1A. Indeed, 5-MeO-DMT (15) has considerably higher affinity at 5HT1-like sites compared to 5HT2-like sites in vitro [56], and 5HT1A and 5HT2A/B antagonists are equally effective in blocking its behavioral effects in rats [133]. While the 5HT2A-prefering antagonist ketanserin (7) can relieve visual hallucinations, aspects of the experience evoked by some compounds may well be due to effects at other serotonin receptor subtypes, or in some cases through binding to dopamine receptors and plasma membrane transporters. Comparisons of affinity and selectivity of various compounds is sometimes difficult due to disagreement between results of displacement studies (Ki) and estimates of affinity (KD) in vitro. The possibility that hallucinogens may activate multiple second messenger systems pathways including adenylyl cyclase and phospholipase C adds an additional layer of complexity, especially considering that slight structural modifications of certain hallucinogens can attenuate hallucinogenic potency without necessarily modifying affinity at key receptor targets.
Early studies using radiolabeled hallucinogens such as [14C]-psilocin (8) confirmed that hallucinogenic compounds rapidly enter the brain, being relatively unhindered at the blood–brain barrier. This is not always the case; the low octanol:water partition coefficient for bufotenine (10) and the predicted low permeability to the blood–brain barrier, has been invoked to explain its relatively low hallucinogenic potency, despite moderate activity in serotonin receptor functional assays [146]. Most hallucinogens undergo two-phase metabolism, whereby de-alkylation precedes glucuronate conjugation; the pharmacokinetics of particular compounds can determine their pharmacodynamic responses. Tryptamine derivatives such as DMT (9) tend to undergo rapid metabolism, such that the hallucinogenic experience lasts only some minutes after administration, whereas LSD (1) has plasma half-life of several hours in humans. There is general agreement between the time course of hallucinogenic experiences and plasma concentrations of the relevant compound. Given this, we can expect that pharmacogenetic studies should reveal factors relating to individual vulnerability to hallucinogenic compounds. The Ayahuasca phenomenon presents an interesting case where treatment with non-hallucinogenic inhibitors of monoamine oxidase, but attenuating metabolism, augments the intensity and duration of the experience evoked by DMT (9).
Despite early success with N1-([11C]-methyl)-2-bromo-LSD ([11C]-MBL, 33), there have been relatively few molecular imaging studies of radiolabeled hallucinogen analogues, either in humans or experimental animals. More commonly, hallucinogens serve as a pharmacological challenge to determine indirect effects on availability of dopamine D2 receptors labelled with [11C]-raclopride (41), or occupancy at serotonin receptors labelled with some other radiotracer. A very few PET studies have examined the effects of treatment with a hallucinogen on cerebral metabolism to FDG-PET or cerebral blood flow; the limited available data indicate hypermetabolism despite hypoperfusion, which implies that hallucinogens may alter flow-metabolism coupling in brain. Thus, there is an enormous scope to undertake PET and SPECT studies of hallucinogen binding at various receptor sites, and to examine the effects of acute and chronic exposure on cerebral metabolism and synaptic density markers.
Acknowledgments
The authors thank János Marton of ABX advanced biochemical compounds, Radeberg, Germany for generously providing the chemical structure figures. Kristian Nygaard Mortensen, Center for Translational Neuromedicine, University of Copenhagen generously provided the structural reference MR image in Figure 4.
Author Contributions
P.C. and C.M.-S. conceptualized the review. All authors contributed to writing of the manuscript and approved its final state. All authors have read and agreed to the published version of the manuscript.
Funding
MP is funded by a Sapere Aude fellowship from the Danish Independent Research Fund (0169-00030B).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
MP has an ongoing research collaboration with the company Compass Pathways Plc (London, UK).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Muller F., Liechti M.E., Lang U.E., Borgwardt S. Advances and challenges in neuroimaging studies on the effects of serotonergic hallucinogens: Contributions of the resting brain. Prog. Brain Res. 2018;242:159–177. doi: 10.1016/bs.pbr.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Petranker R., Anderson T., Farb N. Psychedelic Research and the Need for Transparency: Polishing Alice’s Looking Glass. Front. Psychol. 2020;11:1681. doi: 10.3389/fpsyg.2020.01681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doblin R.E., Christiansen M., Jerome L., Burge B. The Past and Future of Psychedelic Science: An Introduction to This Issue. J. Psychoact. Drugs. 2019;51:93–97. doi: 10.1080/02791072.2019.1606472. [DOI] [PubMed] [Google Scholar]
- 4.Lawrence D.W., Sharma B., Griffiths R.R., Carhart-Harris R. Trends in the Top-Cited Articles on Classic Psychedelics. J. Psychoact. Drugs. 2021:1–16. doi: 10.1080/02791072.2021.1874573. [DOI] [PubMed] [Google Scholar]
- 5.Tullis P. How ecstasy and psilocybin are shaking up psychiatry. Nature. 2021;589:506–509. doi: 10.1038/d41586-021-00187-9. [DOI] [PubMed] [Google Scholar]
- 6.Dos Santos R.G., Bouso J.C., Rocha J.M., Rossi G.N., Hallak J.E. The Use of Classic Hallucinogens/Psychedelics in a Therapeutic Context: Healthcare Policy Opportunities and Challenges. Risk Manag. Healthc. Policy. 2021;14:901–910. doi: 10.2147/RMHP.S300656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dos Santos R.G., Hallak J.E., Baker G., Dursun S. Hallucinogenic/psychedelic 5HT2A receptor agonists as rapid antidepressant therapeutics: Evidence and mechanisms of action. J. Psychopharmacol. 2021 doi: 10.1177/0269881120986422. [DOI] [PubMed] [Google Scholar]
- 8.Dos Santos R.G., Osorio F.L., Crippa J.A.S., Hallak J.E.C. Classical hallucinogens and neuroimaging: A systematic review of human studies: Hallucinogens and neuroimaging. Neurosci. Biobehav. Rev. 2016;71:715–728. doi: 10.1016/j.neubiorev.2016.10.026. [DOI] [PubMed] [Google Scholar]
- 9.Rickli A., Moning O.D., Hoener M.C., Liechti M.E. Receptor interaction profiles of novel psychoactive tryptamines compared with classic hallucinogens. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2016;26:1327–1337. doi: 10.1016/j.euroneuro.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 10.McKenna D.J., Peroutka S.J. Differentiation of 5-hydroxytryptamine2 receptor subtypes using 125I-R-(-)2,5-dimethoxy-4-iodo-phenylisopropylamine and 3H-ketanserin. J. Neurosci. 1989;9:3482–3490. doi: 10.1523/JNEUROSCI.09-10-03482.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalir A., Szara S. Synthesis and Pharmacological Activity of Fluorinated Tryptamine Derivatives. J. Med. Chem. 1963;6:716–719. doi: 10.1021/jm00342a019. [DOI] [PubMed] [Google Scholar]
- 12.Karst M., Halpern J.H., Bernateck M., Passie T. The non-hallucinogen 2-bromo-lysergic acid diethylamide as preventative treatment for cluster headache: An open, non-randomized case series. Cephalalgia Int. J. Headache. 2010;30:1140–1144. doi: 10.1177/0333102410363490. [DOI] [PubMed] [Google Scholar]
- 13.Tfelt-Hansen P. Is BOL-148 hallucinogenic? Cephalalgia Int. J. Headache. 2011;31:635–636. doi: 10.1177/0333102410392069. [DOI] [PubMed] [Google Scholar]
- 14.Blair J.B., Kurrasch-Orbaugh D., Marona-Lewicka D., Cumbay M.G., Watts V.J., Barker E.L., Nichols D.E. Effect of ring fluorination on the pharmacology of hallucinogenic tryptamines. J. Med. Chem. 2000;43:4701–4710. doi: 10.1021/jm000339w. [DOI] [PubMed] [Google Scholar]
- 15.Bressloff P.C., Cowan J.D., Golubitsky M., Thomas P.J., Wiener M.C. What geometric visual hallucinations tell us about the visual cortex. Neural Comput. 2002;14:473–491. doi: 10.1162/089976602317250861. [DOI] [PubMed] [Google Scholar]
- 16.Schartner M.M., Timmermann C. Neural network models for DMT-induced visual hallucinations. Neurosci. Conscious. 2020;2020:niaa024. doi: 10.1093/nc/niaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shulgin A.T., Shulgin A. THIKAL, The Continuation. Transform Press; Berkely, CA, USA: 1997. pp. 337–338. [DOI] [Google Scholar]
- 18.Carter O.L., Hasler F., Pettigrew J.D., Wallis G.M., Liu G.B., Vollenweider F.X. Psilocybin links binocular rivalry switch rate to attention and subjective arousal levels in humans. Psychopharmacology. 2007;195:415–424. doi: 10.1007/s00213-007-0930-9. [DOI] [PubMed] [Google Scholar]
- 19.Carter O.L., Pettigrew J.D., Hasler F., Wallis G.M., Liu G.B., Hell D., Vollenweider F.X. Modulating the rate and rhythmicity of perceptual rivalry alternations with the mixed 5-HT2A and 5-HT1A agonist psilocybin. Neuropsychopharmacology. 2005;30:1154–1162. doi: 10.1038/sj.npp.1300621. [DOI] [PubMed] [Google Scholar]
- 20.Zamberlan F., Sanz C., Martinez Vivot R., Pallavicini C., Erowid F., Erowid E., Tagliazucchi E. The Varieties of the Psychedelic Experience: A Preliminary Study of the Association Between the Reported Subjective Effects and the Binding Affinity Profiles of Substituted Phenethylamines and Tryptamines. Front. Integr. Neurosci. 2018;12:54. doi: 10.3389/fnint.2018.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orsolini L., Papanti G.D., De Berardis D., Guirguis A., Corkery J.M., Schifano F. The “Endless Trip” among the NPS Users: Psychopathology and Psychopharmacology in the Hallucinogen-Persisting Perception Disorder. A Systematic Review. Front. Psychiatry. 2017;8:240. doi: 10.3389/fpsyt.2017.00240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martinotti G., Santacroce R., Pettorruso M., Montemitro C., Spano M.C., Lorusso M., di Giannantonio M., Lerner A.G. Hallucinogen Persisting Perception Disorder: Etiology, Clinical Features, and Therapeutic Perspectives. Brain Sci. 2018:8. doi: 10.3390/brainsci8030047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffman B.J., Scheffel U., Lever J.R., Karpa M.D., Hartig P.R. N1-methyl-2-125I-lysergic acid diethylamide, a preferred ligand for in vitro and in vivo characterization of serotonin receptors. J. Neurochem. 1987;48:115–124. doi: 10.1111/j.1471-4159.1987.tb13135.x. [DOI] [PubMed] [Google Scholar]
- 24.Son H., Jang K., Lee H., Kim S.E., Kang K.W., Lee H. Use of Molecular Imaging in Clinical Drug Development: A Systematic Review. Nucl. Med. Mol. Imaging. 2019;53:208–215. doi: 10.1007/s13139-019-00593-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cumming P., Abi-Dargham A., Grunder G. Molecular imaging of schizophrenia: Neurochemical findings in a heterogeneous and evolving disorder. Behav. Brain Res. 2021;398:113004. doi: 10.1016/j.bbr.2020.113004. [DOI] [PubMed] [Google Scholar]
- 26.Dumuis A., Sebben M., Bockaert J. Pharmacology of 5-hydroxytryptamine-1A receptors which inhibit cAMP production in hippocampal and cortical neurons in primary culture. Mol. Pharmacol. 1988;33:178–186. [PubMed] [Google Scholar]
- 27.Nonaka R., Nagai F., Ogata A., Satoh K. In vitro screening of psychoactive drugs by [(35)S]GTPgammaS binding in rat brain membranes. Biol. Pharm. Bull. 2007;30:2328–2333. doi: 10.1248/bpb.30.2328. [DOI] [PubMed] [Google Scholar]
- 28.Halberstadt A.L., Chatha M., Klein A.K., Wallach J., Brandt S.D. Correlation between the potency of hallucinogens in the mouse head-twitch response assay and their behavioral and subjective effects in other species. Neuropharmacology. 2020;167:107933. doi: 10.1016/j.neuropharm.2019.107933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adams L.M., Geyer M.A. Patterns of exploration in rats distinguish lisuride from lysergic acid diethylamide. Pharmacol. Biochem. Behav. 1985;23:461–468. doi: 10.1016/0091-3057(85)90022-X. [DOI] [PubMed] [Google Scholar]
- 30.Hannon J., Hoyer D. Molecular biology of 5-HT receptors. Behav. Brain Res. 2008;195:198–213. doi: 10.1016/j.bbr.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 31.Parrish J.C., Braden M.R., Gundy E., Nichols D.E. Differential phospholipase C activation by phenylalkylamine serotonin 5-HT 2A receptor agonists. J. Neurochem. 2005;95:1575–1584. doi: 10.1111/j.1471-4159.2005.03477.x. [DOI] [PubMed] [Google Scholar]
- 32.Berg K.A., Maayani S., Goldfarb J., Scaramellini C., Leff P., Clarke W.P. Effector pathway-dependent relative efficacy at serotonin type 2A and 2C receptors: Evidence for agonist-directed trafficking of receptor stimulus. Mol. Pharmacol. 1998;54:94–104. doi: 10.1124/mol.54.1.94. [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez-Maeso J., Weisstaub N.V., Zhou M., Chan P., Ivic L., Ang R., Lira A., Bradley-Moore M., Ge Y., Zhou Q., et al. Hallucinogens recruit specific cortical 5-HT(2A) receptor-mediated signaling pathways to affect behavior. Neuron. 2007;53:439–452. doi: 10.1016/j.neuron.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 34.Gonzalez-Maeso J., Ang R.L., Yuen T., Chan P., Weisstaub N.V., Lopez-Gimenez J.F., Zhou M., Okawa Y., Callado L.F., Milligan G., et al. Identification of a serotonin/glutamate receptor complex implicated in psychosis. Nature. 2008;452:93–97. doi: 10.1038/nature06612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aghajanian G.K., Foote W.E., Sheard M.H. Lysergic acid diethylamide: Sensitive neuronal units in the midbrain raphe. Science. 1968;161:706–708. doi: 10.1126/science.161.3842.706. [DOI] [PubMed] [Google Scholar]
- 36.Aghajanian G.K., Hailgler H.J. Hallucinogenic indoleamines: Preferential action upon presynaptic serotonin receptors. Psychopharmacol. Commun. 1975;1:619–629. [PubMed] [Google Scholar]
- 37.De Gregorio D., Posa L., Ochoa-Sanchez R., McLaughlin R., Maione S., Comai S., Gobbi G. The hallucinogen d-lysergic diethylamide (LSD) decreases dopamine firing activity through 5-HT1A, D2 and TAAR1 receptors. Pharmacol. Res. 2016;113:81–91. doi: 10.1016/j.phrs.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 38.Rasmussen K., Aghajanian G.K. Effect of hallucinogens on spontaneous and sensory-evoked locus coeruleus unit activity in the rat: Reversal by selective 5-HT2 antagonists. Brain Res. 1986;385:395–400. doi: 10.1016/0006-8993(86)91090-5. [DOI] [PubMed] [Google Scholar]
- 39.Passie T., Halpern J.H., Stichtenoth D.O., Emrich H.M., Hintzen A. The pharmacology of lysergic acid diethylamide: A review. Cns Neurosci. Ther. 2008;14:295–314. doi: 10.1111/j.1755-5949.2008.00059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Minuzzi L., Cumming P. Agonist binding fraction of dopamine D2/3 receptors in rat brain: A quantitative autoradiographic study. Neurochem. Int. 2010;56:747–752. doi: 10.1016/j.neuint.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 41.Titeler M., Lyon R.A., Glennon R.A. Radioligand binding evidence implicates the brain 5-HT2 receptor as a site of action for LSD and phenylisopropylamine hallucinogens. Psychopharmacology. 1988;94:213–216. doi: 10.1007/BF00176847. [DOI] [PubMed] [Google Scholar]
- 42.Jensen A.A., Halberstadt A.L., Marcher-Rorsted E., Odland A.U., Chatha M., Speth N., Liebscher G., Hansen M., Brauner-Osborne H., Palner M., et al. The selective 5-HT2A receptor agonist 25CN-NBOH: Structure-activity relationship, in vivo pharmacology, and in vitro and ex vivo binding characteristics of [(3)H]25CN-NBOH. Biochem. Pharmacol. 2020;177:113979. doi: 10.1016/j.bcp.2020.113979. [DOI] [PubMed] [Google Scholar]
- 43.Cassels B.K., Saez-Briones P. Dark Classics in Chemical Neuroscience: Mescaline. ACS Chem. Neurosci. 2018;9:2448–2458. doi: 10.1021/acschemneuro.8b00215. [DOI] [PubMed] [Google Scholar]
- 44.Neff N., Rossi G.V., Chase G.D., Rabinowitz J.L. Distribution and Metabolism of Mescaline-C14 in the Cat Brain. J. Pharmacol. Exp. Ther. 1964;144:1–7. [PubMed] [Google Scholar]
- 45.Lee H.M., Roth B.L. Hallucinogen actions on human brain revealed. Proc. Natl. Acad. Sci. USA. 2012;109:1820–1821. doi: 10.1073/pnas.1121358109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cumming P., Wong D.F., Gillings N., Hilton J., Scheffel U., Gjedde A. Specific binding of [(11)C]raclopride and N-[(3)H]propyl-norapomorphine to dopamine receptors in living mouse striatum: Occupancy by endogenous dopamine and guanosine triphosphate-free G protein. J. Cereb. Blood Flow Metab. 2002;22:596–604. doi: 10.1097/00004647-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 47.Sadzot B., Baraban J.M., Glennon R.A., Lyon R.A., Leonhardt S., Jan C.R., Titeler M. Hallucinogenic drug interactions at human brain 5-HT2 receptors: Implications for treating LSD-induced hallucinogenesis. Psychopharmacology. 1989;98:495–499. doi: 10.1007/BF00441948. [DOI] [PubMed] [Google Scholar]
- 48.Harms A., Gundisch D., Muller C.E., Kovar K.A. Development of a 5-hydroxytryptamine(2A) receptor binding assay for high throughput screening using 96-well microfilter plates. J. Biomol. Screen. 2000;5:269–278. doi: 10.1177/108705710000500410. [DOI] [PubMed] [Google Scholar]
- 49.Deliganis A.V., Pierce P.A., Peroutka S.J. Differential interactions of dimethyltryptamine (DMT) with 5-HT1A and 5-HT2 receptors. Biochem. Pharmacol. 1991;41:1739–1744. doi: 10.1016/0006-2952(91)90178-8. [DOI] [PubMed] [Google Scholar]
- 50.Smith R.L., Canton H., Barrett R.J., Sanders-Bush E. Agonist properties of N,N-dimethyltryptamine at serotonin 5-HT2A and 5-HT2C receptors. Pharmacol. Biochem. Behav. 1998;61:323–330. doi: 10.1016/S0091-3057(98)00110-5. [DOI] [PubMed] [Google Scholar]
- 51.Valle M., Maqueda A.E., Rabella M., Rodriguez-Pujadas A., Antonijoan R.M., Romero S., Alonso J.F., Mananas M.A., Barker S., Friedlander P., et al. Inhibition of alpha oscillations through serotonin-2A receptor activation underlies the visual effects of ayahuasca in humans. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2016;26:1161–1175. doi: 10.1016/j.euroneuro.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 52.Blough B.E., Landavazo A., Decker A.M., Partilla J.S., Baumann M.H., Rothman R.B. Interaction of psychoactive tryptamines with biogenic amine transporters and serotonin receptor subtypes. Psychopharmacology. 2014;231:4135–4144. doi: 10.1007/s00213-014-3557-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Glennon R.A., Dukat M., el-Bermawy M., Law H., De los Angeles J., Teitler M., King A., Herrick-Davis K. Influence of amine substituents on 5-HT2A versus 5-HT2C binding of phenylalkyl- and indolylalkylamines. J. Med. Chem. 1994;37:1929–1935. doi: 10.1021/jm00039a004. [DOI] [PubMed] [Google Scholar]
- 54.Carbonaro T.M., Gatch M.B. Neuropharmacology of N,N-dimethyltryptamine. Brain Res. Bull. 2016;126:74–88. doi: 10.1016/j.brainresbull.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nardai S., Laszlo M., Szabo A., Alpar A., Hanics J., Zahola P., Merkely B., Frecska E., Nagy Z. N,N-dimethyltryptamine reduces infarct size and improves functional recovery following transient focal brain ischemia in rats. Exp. Neurol. 2020;327:113245. doi: 10.1016/j.expneurol.2020.113245. [DOI] [PubMed] [Google Scholar]
- 56.Halberstadt A.L., Nichols D.E., Geyer M.A. Behavioral effects of alpha,alpha,beta,beta-tetradeutero-5-MeO-DMT in rats: Comparison with 5-MeO-DMT administered in combination with a monoamine oxidase inhibitor. Psychopharmacology. 2012;221:709–718. doi: 10.1007/s00213-011-2616-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Strassman R.J. Human psychopharmacology of N,N-dimethyltryptamine. Behav. Brain Res. 1996;73:121–124. doi: 10.1016/0166-4328(96)00081-2. [DOI] [PubMed] [Google Scholar]
- 58.Maisonneuve I.M., Keller R.W., Jr., Glick S.D. Interactions between ibogaine, a potential anti-addictive agent, and morphine: An in vivo microdialysis study. Eur. J. Pharmacol. 1991;199:35–42. doi: 10.1016/0014-2999(91)90634-3. [DOI] [PubMed] [Google Scholar]
- 59.Glick S.D., Maisonneuve I.M., Szumlinski K.K. 18-Methoxycoronaridine (18-MC) and ibogaine: Comparison of antiaddictive efficacy, toxicity, and mechanisms of action. Ann. N. Y. Acad. Sci. 2000;914:369–386. doi: 10.1111/j.1749-6632.2000.tb05211.x. [DOI] [PubMed] [Google Scholar]
- 60.Glick S.D., Maisonneuve I.M., Szumlinski K.K. Mechanisms of action of ibogaine: Relevance to putative therapeutic effects and development of a safer iboga alkaloid congener. Alkaloids. Chem. Biol. 2001;56:39–53. doi: 10.1016/s0099-9598(01)56006-x. [DOI] [PubMed] [Google Scholar]
- 61.Mash D.C., Staley J.K., Pablo J.P., Holohean A.M., Hackman J.C., Davidoff R.A. Properties of ibogaine and its principal metabolite (12-hydroxyibogamine) at the MK-801 binding site of the NMDA receptor complex. Neurosci. Lett. 1995;192:53–56. doi: 10.1016/0304-3940(95)11608-Y. [DOI] [PubMed] [Google Scholar]
- 62.Asjad H.M.M., Kasture A., El-Kasaby A., Sackel M., Hummel T., Freissmuth M., Sucic S. Pharmacochaperoning in a Drosophila model system rescues human dopamine transporter variants associated with infantile/juvenile parkinsonism. J. Biol. Chem. 2017;292:19250–19265. doi: 10.1074/jbc.M117.797092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rabin R.A., Winter J.C. Ibogaine and noribogaine potentiate the inhibition of adenylyl cyclase activity by opioid and 5-HT receptors. Eur. J. Pharmacol. 1996;316:343–348. doi: 10.1016/S0014-2999(96)00690-5. [DOI] [PubMed] [Google Scholar]
- 64.Glick S.D., Maisonneuve I.M., Kitchen B.A., Fleck M.W. Antagonism of alpha 3 beta 4 nicotinic receptors as a strategy to reduce opioid and stimulant self-administration. Eur. J. Pharmacol. 2002;438:99–105. doi: 10.1016/S0014-2999(02)01284-0. [DOI] [PubMed] [Google Scholar]
- 65.Cameron L.P., Tombari R.J., Lu J., Pell A.J., Hurley Z.Q., Ehinger Y., Vargas M.V., McCarroll M.N., Taylor J.C., Myers-Turnbull D., et al. A non-hallucinogenic psychedelic analogue with therapeutic potential. Nature. 2021;589:474–479. doi: 10.1038/s41586-020-3008-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pottie E., Kupriyanova O.V., Brandt A.L., Laprairie R.B., Shevryn V.A., Stove C.P. Serotonin 2A receptor (5-HT2AR) activation by 25H-NBOMe positional isomers; in vitro functional evaluation and molecular docking. Pharmacol. Transl. Sci. 2021;4:479–487. doi: 10.1021/acsptsci.0c00189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gupta S.P., Singh P., Bindal M.C. QSAR studies on hallucinogens. Chem. Rev. 1983;83:633–649. doi: 10.1021/cr00058a003. [DOI] [Google Scholar]
- 68.Scheffel U., Lever J.R., Stathis M., Ricaurte G.A. Repeated administration of MDMA causes transient down-regulation of serotonin 5-HT2 receptors. Neuropharmacology. 1992;31:881–893. doi: 10.1016/0028-3908(92)90126-A. [DOI] [PubMed] [Google Scholar]
- 69.Lever J.R., Scheffel U.A., Musachio J.L., Stathis M., Wagner H.N., Jr. Radioiodinated D-(+)-N1-ethyl-2-iodolysergic acid diethylamide: A ligand for in vitro and in vivo studies of serotonin receptors. Life Sci. 1991;48:PL73–PL78. doi: 10.1016/0024-3205(91)90189-I. [DOI] [PubMed] [Google Scholar]
- 70.Bennett J.P., Jr., snyder S.H. Stereospecific binding of D-lysergic acid diethylamide (LSD) to brain membranes: Relationship to serotonin receptors. Brain Res. 1975;94:523–544. doi: 10.1016/0006-8993(75)90234-6. [DOI] [PubMed] [Google Scholar]
- 71.McKenna D.J., Saavedra J.M. Autoradiography of LSD and 2,5-dimethoxyphenylisopropylamine psychotomimetics demonstrates regional, specific cross-displacement in the rat brain. Eur. J. Pharmacol. 1987;142:313–315. doi: 10.1016/0014-2999(87)90121-X. [DOI] [PubMed] [Google Scholar]
- 72.McKenna D.J., Mathis C.A., Shulgin A.T., Sargent T., 3rd, Saavedra J.M. Autoradiographic localization of binding sites for 125I-DOI, a new psychotomimetic radioligand, in the rat brain. Eur. J. Pharmacol. 1987;137:289–290. doi: 10.1016/0014-2999(87)90239-1. [DOI] [PubMed] [Google Scholar]
- 73.Nakada M.T., Wieczorek C.M., Rainbow T.C. Localization and characterization by quantitative autoradiography of [125I]LSD binding sites in rat brain. Neurosci. Lett. 1984;49:13–18. doi: 10.1016/0304-3940(84)90128-9. [DOI] [PubMed] [Google Scholar]
- 74.Altar C.A., Boyar W.C., Marien M.R. 125I-LSD autoradiography confirms the preferential localization of caudate-putamen S2 receptors to the caudal (peripallidal) region. Brain Res. 1986;372:130–136. doi: 10.1016/0006-8993(86)91465-4. [DOI] [PubMed] [Google Scholar]
- 75.Hopf A., Eckert H. Autoradiographic studies on the distribution of psychoactive drugs in the rat brain. 3. 14C-psilocin. Psychopharmacologia. 1969;16:201–222. doi: 10.1007/BF02456045. [DOI] [PubMed] [Google Scholar]
- 76.Korr H. Autoradiographic studies on the distribution of 3H-mescaline in the brain of the marmoset, Callithrix jacchus. Psychopharmacologia. 1976;46:115–117. doi: 10.1007/BF00421558. [DOI] [PubMed] [Google Scholar]
- 77.Korr H., Seiler N. Autoradiographic studies on the distribution of 3H-2,3,4-trimethoxy-beta-phenylethylamine in the mouse. Psychopharmacologia. 1976;46:53–58. doi: 10.1007/BF00421549. [DOI] [PubMed] [Google Scholar]
- 78.Palenicek T., Balikova M., Bubenikova-Valesova V., Horacek J. Mescaline effects on rat behavior and its time profile in serum and brain tissue after a single subcutaneous dose. Psychopharmacology. 2008;196:51–62. doi: 10.1007/s00213-007-0926-5. [DOI] [PubMed] [Google Scholar]
- 79.Glennon R.A., Raghupathi R., Bartyzel P., Teitler M., Leonhardt S. Binding of phenylalkylamine derivatives at 5-HT1C and 5-HT2 serotonin receptors: Evidence for a lack of selectivity. J. Med. Chem. 1992;35:734–740. doi: 10.1021/jm00082a014. [DOI] [PubMed] [Google Scholar]
- 80.McKenna D.J., Nazarali A.J., Himeno A., Saavedra J.M. Chronic treatment with (+/−)DOI, a psychotomimetic 5-HT2 agonist, downregulates 5-HT2 receptors in rat brain. Neuropsychopharmacology. 1989;2:81–87. doi: 10.1016/0893-133X(89)90010-9. [DOI] [PubMed] [Google Scholar]
- 81.Shi J., Landry M., Carrasco G.A., Battaglia G., Muma N.A. Sustained treatment with a 5-HT(2A) receptor agonist causes functional desensitization and reductions in agonist-labeled 5-HT(2A) receptors despite increases in receptor protein levels in rats. Neuropharmacology. 2008;55:687–692. doi: 10.1016/j.neuropharm.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nielsen L.M., Holm N.B., Leth-Petersen S., Kristensen J.L., Olsen L., Linnet K. Characterization of the hepatic cytochrome P450 enzymes involved in the metabolism of 25I-NBOMe and 25I-NBOH. Drug Test. Anal. 2017;9:671–679. doi: 10.1002/dta.2031. [DOI] [PubMed] [Google Scholar]
- 83.Elmore J.S., Decker A.M., Sulima A., Rice K.C., Partilla J.S., Blough B.E., Baumann M.H. Comparative neuropharmacology of N-(2-methoxybenzyl)-2,5-dimethoxyphenethylamine (NBOMe) hallucinogens and their 2C counterparts in male rats. Neuropharmacology. 2018;142:240–250. doi: 10.1016/j.neuropharm.2018.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wong D.F., Lever J.R., Hartig P.R., Dannals R.F., Villemagne V., Hoffman B.J., Wilson A.A., Ravert H.T., Links J.M., Scheffel U., et al. Localization of serotonin 5-HT2 receptors in living human brain by positron emission tomography using N1-([11C]-methyl)-2-Br-LSD. Synapse. 1987;1:393–398. doi: 10.1002/syn.890010502. [DOI] [PubMed] [Google Scholar]
- 85.Sargent T., 3rd, Kalbhen D.A., Shulgin A.T., Stauffer H., Kusubov N. A potential new brain-scanning agent: 4-77Br-2,5-dimethoxyphenylisoproplamine (4-Br-DPIA) J. Nucl. Med. 1975;16:243–245. [PubMed] [Google Scholar]
- 86.Zea-Ponce Y., Kegeles L.S., Guo N., Raskin L., Bakthavachalam V., Laruelle M. Pharmacokinetics and brain distribution in non human primate of R(-)[123I]DOI, A 5HT(2A/2C) serotonin agonist. Nucl. Med. Biol. 2002;29:575–583. doi: 10.1016/S0969-8051(02)00306-2. [DOI] [PubMed] [Google Scholar]
- 87.Ettrup A., Palner M., Gillings N., Santini M.A., Hansen M., Kornum B.R., Rasmussen L.K., Nagren K., Madsen J., Begtrup M., et al. Radiosynthesis and evaluation of 11C-CIMBI-5 as a 5-HT2A receptor agonist radioligand for PET. J. Nucl. Med. 2010;51:1763–1770. doi: 10.2967/jnumed.109.074021. [DOI] [PubMed] [Google Scholar]
- 88.Prabhakaran J., DeLorenzo C., Zanderigo F., Knudsen G.M., Gilling N., Pratap M., Jorgensen M.J., Daunais J., Kaplan J.R., Parsey R.V., et al. In vivo PET Imaging of [11C]CIMBI-5, a 5-HT2AR Agonist Radiotracer in Nonhuman Primates. J. Pharm. Pharm. Sci. 2019;22:352–364. doi: 10.18433/jpps30329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ettrup A., Hansen M., Santini M.A., Paine J., Gillings N., Palner M., Lehel S., Herth M.M., Madsen J., Kristensen J., et al. Radiosynthesis and in vivo evaluation of a series of substituted 11C-phenethylamines as 5-HT (2A) agonist PET tracers. Eur. J. Nucl. Med. Mol. Imaging. 2011;38:681–693. doi: 10.1007/s00259-010-1686-8. [DOI] [PubMed] [Google Scholar]
- 90.Ettrup A., Svarer C., McMahon B., da Cunha-Bang S., Lehel S., Moller K., Dyssegaard A., Ganz M., Beliveau V., Jorgensen L.M., et al. Serotonin 2A receptor agonist binding in the human brain with [(11)C]Cimbi-36: Test-retest reproducibility and head-to-head comparison with the antagonist [(18)F]altanserin. NeuroImage. 2016;130:167–174. doi: 10.1016/j.neuroimage.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 91.Leysen J.E. Gaps and peculiarities in 5-HT2 receptor studies. Neuropsychopharmacology. 1990;3:361–369. [PubMed] [Google Scholar]
- 92.Finnema S.J., Stepanov V., Ettrup A., Nakao R., Amini N., Svedberg M., Lehmann C., Hansen M., Knudsen G.M., Halldin C. Characterization of [(11)C]Cimbi-36 as an agonist PET radioligand for the 5-HT(2A) and 5-HT(2C) receptors in the nonhuman primate brain. NeuroImage. 2014;84:342–353. doi: 10.1016/j.neuroimage.2013.08.035. [DOI] [PubMed] [Google Scholar]
- 93.Johansen A., Holm S., Dall B., Keller S., Kristensen J.L., Knudsen G.M., Hansen H.D. Human biodistribution and radiation dosimetry of the 5-HT2A receptor agonist Cimbi-36 labeled with carbon-11 in two positions. Ejnmmi Res. 2019;9:71. doi: 10.1186/s13550-019-0527-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cohen I., Vogel W.H. Determination and physiological disposition of dimethyltryptamine and diethyltryptamine in rat brain, liver and plasma. Biochem. Pharmacol. 1972;21:1214–1216. doi: 10.1016/0006-2952(72)90119-0. [DOI] [PubMed] [Google Scholar]
- 95.Vitale A.A., Pomilio A.B., Canellas C.O., Vitale M.G., Putz E.M., Ciprian-Ollivier J. In vivo long-term kinetics of radiolabeled n,n-dimethyltryptamine and tryptamine. J. Nucl. Med. 2011;52:970–977. doi: 10.2967/jnumed.110.083246. [DOI] [PubMed] [Google Scholar]
- 96.Vollenweider F.X., Vontobel P., Hell D., Leenders K.L. 5-HT modulation of dopamine release in basal ganglia in psilocybin-induced psychosis in man--a PET study with [11C]raclopride. Neuropsychopharmacology. 1999;20:424–433. doi: 10.1016/S0893-133X(98)00108-0. [DOI] [PubMed] [Google Scholar]
- 97.Sakashita Y., Abe K., Katagiri N., Kambe T., Saitoh T., Utsunomiya I., Horiguchi Y., Taguchi K. Effect of psilocin on extracellular dopamine and serotonin levels in the mesoaccumbens and mesocortical pathway in awake rats. Biol. Pharm. Bull. 2015;38:134–138. doi: 10.1248/bpb.b14-00315. [DOI] [PubMed] [Google Scholar]
- 98.Minuzzi L., Nomikos G.G., Wade M.R., Jensen S.B., Olsen A.K., Cumming P. Interaction between LSD and dopamine D2/3 binding sites in pig brain. Synapse. 2005;56:198–204. doi: 10.1002/syn.20141. [DOI] [PubMed] [Google Scholar]
- 99.Dolder P.C., Schmid Y., Steuer A.E., Kraemer T., Rentsch K.M., Hammann F., Liechti M.E. Pharmacokinetics and Pharmacodynamics of Lysergic Acid Diethylamide in Healthy Subjects. Clin. Pharmacokinet. 2017;56:1219–1230. doi: 10.1007/s40262-017-0513-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jensen S.B., Olsen A.K., Pedersen K., Cumming P. Effect of monoamine oxidase inhibition on amphetamine-evoked changes in dopamine receptor availability in the living pig: A dual tracer PET study with [11C]harmine and [11C]raclopride. Synapse. 2006;59:427–434. doi: 10.1002/syn.20258. [DOI] [PubMed] [Google Scholar]
- 101.Pedersen K., Simonsen M., Ostergaard S.D., Munk O.L., Rosa-Neto P., Olsen A.K., Jensen S.B., Moller A., Cumming P. Mapping the amphetamine-evoked changes in [11C]raclopride binding in living rat using small animal PET: Modulation by MAO-inhibition. NeuroImage. 2007;35:38–46. doi: 10.1016/j.neuroimage.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 102.Leo D., Mus L., Espinoza S., Hoener M.C., Sotnikova T.D., Gainetdinov R.R. Taar1-mediated modulation of presynaptic dopaminergic neurotransmission: Role of D2 dopamine autoreceptors. Neuropharmacology. 2014;81:283–291. doi: 10.1016/j.neuropharm.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 103.Maschauer S., Haller A., Riss P.J., Kuwert T., Prante O., Cumming P. Specific binding of [(18)F]fluoroethyl-harmol to monoamine oxidase A in rat brain cryostat sections, and compartmental analysis of binding in living brain. J. Neurochem. 2015;135:908–917. doi: 10.1111/jnc.13370. [DOI] [PubMed] [Google Scholar]
- 104.Jorgensen L.M., Weikop P., Villadsen J., Visnapuu T., Ettrup A., Hansen H.D., Baandrup A.O., Andersen F.L., Bjarkam C.R., Thomsen C., et al. Cerebral 5-HT release correlates with [(11)C]Cimbi36 PET measures of 5-HT2A receptor occupancy in the pig brain. J. Cereb. Blood Flow Metab. 2017;37:425–434. doi: 10.1177/0271678X16629483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hasler F.Q.B.B., Treyer V., Schubiger P.A., Buck A., Vollenweider F.X. Role of prefrontal serotonin-2A receptors in self experience during pilocybin-indiced altered states. Neuropsychobiology. 2009;59:60. doi: 10.1159/000209314. [DOI] [Google Scholar]
- 106.Madsen M.K., Fisher P.M., Burmester D., Dyssegaard A., Stenbaek D.S., Kristiansen S., Johansen S.S., Lehel S., Linnet K., Svarer C., et al. Psychedelic effects of psilocybin correlate with serotonin 2A receptor occupancy and plasma psilocin levels. Neuropsychopharmacology. 2019;44:1328–1334. doi: 10.1038/s41386-019-0324-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Stenbaek D.S., Kristiansen S., Burmester D., Madsen M.K., Frokjaer V.G., Knudsen G.M., Fisher P.M. Trait Openness and serotonin 2A receptors in healthy volunteers: A positron emission tomography study. Hum. Brain Mapp. 2019;40:2117–2124. doi: 10.1002/hbm.24511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Raval N.R., Johansen A., Donovan L.L., Ros N.F., Ozenne B., Hansen H.D., Knudsen G.M. A Single Dose of Psilocybin Increases Synaptic Density and Decreases 5-HT2A Receptor Density in the Pig Brain. Int. J. Mol. Sci. 2021:22. doi: 10.3390/ijms22020835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.de la Fuente Revenga M., Zhu B., Guevara C.A., Naler L.B., Saunders J.B., Zhou Z., Toneatti R., Sierra S., Wolstenholme J.T., Beardsley P.M., et al. Prolonged epigenetic and synaptic plasticity alterations following single exposre to a psychedelic in mice. bioRxiv. 2021 doi: 10.1101/2021.02.24.432725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shao L.-X., Liao C., Gregg I., Savalia N.K., Delagarza K., Kwan A.C. Psilocybin iduces rapid and persistent growth of dendritic spines in frontal cortex in vivo. bioRxiv. 2021 doi: 10.1101/2021.02.17.431629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Savalia N.K., Shao L.X., Kwan A.C. A Dendrite-Focused Framework for Understanding the Actions of Ketamine and Psychedelics. Trends Neurosci. 2021;44:260–275. doi: 10.1016/j.tins.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Libanio Osorio Marta R.F. Metabolism of lysergic acid diethylamide (LSD): An update. Drug Metab. Rev. 2019;51:378–387. doi: 10.1080/03602532.2019.1638931. [DOI] [PubMed] [Google Scholar]
- 113.Kalberer F., Kreis W., Rutschmann J. The fate of psilocin in the rat. Biochem. Pharmacol. 1962;11:261–269. doi: 10.1016/0006-2952(62)90050-3. [DOI] [PubMed] [Google Scholar]
- 114.Kamata T., Katagi M., Kamata H.T., Miki A., Shima N., Zaitsu K., Nishikawa M., Tanaka E., Honda K., Tsuchihashi H. Metabolism of the psychotomimetic tryptamine derivative 5-methoxy-N,N-diisopropyltryptamine in humans: Identification and quantification of its urinary metabolites. Drug Metab. Dispos. Biol. Fate Chem. 2006;34:281–287. doi: 10.1124/dmd.105.005835. [DOI] [PubMed] [Google Scholar]
- 115.Brown R.T., Nicholas C.R., Cozzi N.V., Gassman M.C., Cooper K.M., Muller D., Thomas C.D., Hetzel S.J., Henriquez K.M., Ribaudo A.S., et al. Pharmacokinetics of Escalating Doses of Oral Psilocybin in Healthy Adults. Clin. Pharmacokinet. 2017;56:1543–1554. doi: 10.1007/s40262-017-0540-6. [DOI] [PubMed] [Google Scholar]
- 116.Leth-Petersen S., Gabel-Jensen C., Gillings N., Lehel S., Hansen H.D., Knudsen G.M., Kristensen J.L. Metabolic Fate of Hallucinogenic NBOMes. Chem. Res. Toxicol. 2016;29:96–100. doi: 10.1021/acs.chemrestox.5b00450. [DOI] [PubMed] [Google Scholar]
- 117.Johansen A., Hansen H.D., Svarer C., Lehel S., Leth-Petersen S., Kristensen J.L., Gillings N., Knudsen G.M. The importance of small polar radiometabolites in molecular neuroimaging: A PET study with [(11)C]Cimbi-36 labeled in two positions. J. Cereb. Blood Flow Metab. 2018;38:659–668. doi: 10.1177/0271678X17746179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Breusova K., Ernstsen K.G., Palner M., Linnet K., Kristensen J.L., Kretschmann A.C. A quantitative method for the selective 5-HT2A agonist 25CN-NBOH in rat plasma and brain. J. Pharm. Biomed. Anal. 2021;199:114016. doi: 10.1016/j.jpba.2021.114016. [DOI] [PubMed] [Google Scholar]
- 119.Christian S.T., Harrison R., Quayle E., Pagel J., Monti J. The in vitro identification of dimethyltryptamine (DMT) in mammalian brain and its characterization as a possible endogenous neuroregulatory agent. Biochem. Med. 1977;18:164–183. doi: 10.1016/0006-2944(77)90088-6. [DOI] [PubMed] [Google Scholar]
- 120.Axelrod J. Enzymatic formation of psychotomimetic metabolites from normally occurring compounds. Science. 1961;134:343. doi: 10.1126/science.134.3475.343. [DOI] [PubMed] [Google Scholar]
- 121.Dean J.G. Indolethylamine-N-methyltransferase Polymorphisms: Genetic and Biochemical Approaches for Study of Endogenous N,N,-dimethyltryptamine. Front. Neurosci. 2018;12:232. doi: 10.3389/fnins.2018.00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Barker S.A. N, N-Dimethyltryptamine (DMT), an Endogenous Hallucinogen: Past, Present, and Future Research to Determine Its Role and Function. Front. Neurosci. 2018;12:536. doi: 10.3389/fnins.2018.00536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mavlyutov T.A., Baker E.M., Losenegger T.M., Kim J.R., Torres B., Epstein M.L., Ruoho A.E. The Sigma-1 Receptor-A Therapeutic Target for the Treatment of ALS? Adv. Exp. Med. Biol. 2017;964:255–265. doi: 10.1007/978-3-319-50174-1_17. [DOI] [PubMed] [Google Scholar]
- 124.Dean J.G., Liu T., Huff S., Sheler B., Barker S.A., Strassman R.J., Wang M.M., Borjigin J. Biosynthesis and Extracellular Concentrations of N,N-dimethyltryptamine (DMT) in Mammalian Brain. Sci. Rep. 2019;9:9333. doi: 10.1038/s41598-019-45812-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nichols D.E. N,N-dimethyltryptamine and the pineal gland: Separating fact from myth. J. Psychopharmacol. 2018;32:30–36. doi: 10.1177/0269881117736919. [DOI] [PubMed] [Google Scholar]
- 126.Shen H.W., Jiang X.L., Winter J.C., Yu A.M. Psychedelic 5-methoxy-N,N-dimethyltryptamine: Metabolism, pharmacokinetics, drug interactions, and pharmacological actions. Curr. Drug Metab. 2010;11:659–666. doi: 10.2174/138920010794233495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Agurell S., Holmstedt B., Lindgren J.E. Metabolism of 5-methoxy-N,-N dimethyltryptamine- 14 C in the rat. Biochem. Pharmacol. 1969;18:2771–2781. doi: 10.1016/0006-2952(69)90185-3. [DOI] [PubMed] [Google Scholar]
- 128.Keiser M.J., Setola V., Irwin J.J., Laggner C., Abbas A.I., Hufeisen S.J., Jensen N.H., Kuijer M.B., Matos R.C., Tran T.B., et al. Predicting new molecular targets for known drugs. Nature. 2009;462:175–181. doi: 10.1038/nature08506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Samoylenko V., Rahman M.M., Tekwani B.L., Tripathi L.M., Wang Y.H., Khan S.I., Khan I.A., Miller L.S., Joshi V.C., Muhammad I. Banisteriopsis caapi, a unique combination of MAO inhibitory and antioxidative constituents for the activities relevant to neurodegenerative disorders and Parkinson’s disease. J. Ethnopharmacol. 2010;127:357–367. doi: 10.1016/j.jep.2009.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Palhano-Fontes F., Barreto D., Onias H., Andrade K.C., Novaes M.M., Pessoa J.A., Mota-Rolim S.A., Osorio F.L., Sanches R., Dos Santos R.G., et al. Rapid antidepressant effects of the psychedelic ayahuasca in treatment-resistant depression: A randomized placebo-controlled trial. Psychol. Med. 2019;49:655–663. doi: 10.1017/S0033291718001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Berlowitz I., Walt H., Ghasarian C., Mendive F., Martin-Soelch C. Short-Term Treatment Effects of a Substance Use Disorder Therapy Involving Traditional Amazonian Medicine. J. Psychoact. Drugs. 2019;51:323–334. doi: 10.1080/02791072.2019.1607956. [DOI] [PubMed] [Google Scholar]
- 132.Jiang X.L., Shen H.W., Yu A.M. Modification of 5-methoxy-N,N-dimethyltryptamine-induced hyperactivity by monoamine oxidase A inhibitor harmaline in mice and the underlying serotonergic mechanisms. Pharmacol. Rep. PR. 2016;68:608–615. doi: 10.1016/j.pharep.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Halberstadt A.L. Behavioral and pharmacokinetic interactions between monoamine oxidase inhibitors and the hallucinogen 5-methoxy-N,N-dimethyltryptamine. Pharmacol. Biochem. Behav. 2016;143:1–10. doi: 10.1016/j.pbb.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Grome J.J., Harper A.M. Local cerebral glucose utilisation following indoleamine- and piperazine-containing 5-hydroxytryptamine agonists. J. Neurochem. 1986;46:117–124. doi: 10.1111/j.1471-4159.1986.tb12933.x. [DOI] [PubMed] [Google Scholar]
- 135.Kelly P.A., Davis C.J., Goodwin G.M. Differential patterns of local cerebral glucose utilization in response to 5-hydroxytryptamine agonists. Neuroscience. 1988;25:907–915. doi: 10.1016/0306-4522(88)90044-9. [DOI] [PubMed] [Google Scholar]
- 136.Tyls F., Palenicek T., Kaderabek L., Lipski M., Kubesova A., Horacek J. Sex differences and serotonergic mechanisms in the behavioural effects of psilocin. Behav. Pharmacol. 2016;27:309–320. doi: 10.1097/FBP.0000000000000198. [DOI] [PubMed] [Google Scholar]
- 137.Vollenweider F.X., Leenders K.L., Scharfetter C., Maguire P., Stadelmann O., Angst J. Positron emission tomography and fluorodeoxyglucose studies of metabolic hyperfrontality and psychopathology in the psilocybin model of psychosis. Neuropsychopharmacology. 1997;16:357–372. doi: 10.1016/S0893-133X(96)00246-1. [DOI] [PubMed] [Google Scholar]
- 138.Gouzoulis-Mayfrank E., Schreckenberger M., Sabri O., Arning C., Thelen B., Spitzer M., Kovar K.A., Hermle L., Bull U., Sass H. Neurometabolic effects of psilocybin, 3,4-methylenedioxyethylamphetamine (MDE) and d-methamphetamine in healthy volunteers. A double-blind, placebo-controlled PET study with [18F]FDG. Neuropsychopharmacology. 1999;20:565–581. doi: 10.1016/S0893-133X(98)00089-X. [DOI] [PubMed] [Google Scholar]
- 139.Carhart-Harris R.L., Muthukumaraswamy S., Roseman L., Kaelen M., Droog W., Murphy K., Tagliazucchi E., Schenberg E.E., Nest T., Orban C., et al. Neural correlates of the LSD experience revealed by multimodal neuroimaging. Proc. Natl. Acad. Sci. USA. 2016;113:4853–4858. doi: 10.1073/pnas.1518377113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hermle L., Gouzoulis-Mayfrank E., Spitzer M. Blood flow and cerebral laterality in the mescaline model of psychosis. Pharmacopsychiatry. 1998;31(Suppl. 2):85–91. doi: 10.1055/s-2007-979352. [DOI] [PubMed] [Google Scholar]
- 141.Riba J., Romero S., Grasa E., Mena E., Carrio I., Barbanoj M.J. Increased frontal and paralimbic activation following ayahuasca, the pan-Amazonian inebriant. Psychopharmacology. 2006;186:93–98. doi: 10.1007/s00213-006-0358-7. [DOI] [PubMed] [Google Scholar]
- 142.Sanches R.F., de Lima Osorio F., Dos Santos R.G., Macedo L.R., Maia-de-Oliveira J.P., Wichert-Ana L., de Araujo D.B., Riba J., Crippa J.A., Hallak J.E. Antidepressant Effects of a Single Dose of Ayahuasca in Patients With Recurrent Depression: A SPECT Study. J. Clin. Psychopharmacol. 2016;36:77–81. doi: 10.1097/JCP.0000000000000436. [DOI] [PubMed] [Google Scholar]
- 143.Barsuglia J.P., Polanco M., Palmer R., Malcolm B.J., Kelmendi B., Calvey T. A case report SPECT study and theoretical rationale for the sequential administration of ibogaine and 5-MeO-DMT in the treatment of alcohol use disorder. Prog. Brain Res. 2018;242:121–158. doi: 10.1016/bs.pbr.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 144.Lewis C.R., Preller K.H., Kraehenmann R., Michels L., Staempfli P., Vollenweider F.X. Two dose investigation of the 5-HT-agonist psilocybin on relative and global cerebral blood flow. NeuroImage. 2017;159:70–78. doi: 10.1016/j.neuroimage.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 145.Carhart-Harris R.L., Erritzoe D., Williams T., Stone J.M., Reed L.J., Colasanti A., Tyacke R.J., Leech R., Malizia A.L., Murphy K., et al. Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. Proc. Natl. Acad. Sci. USA. 2012;109:2138–2143. doi: 10.1073/pnas.1119598109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.McBride M.C. Bufotenine: Toward an understanding of possible psychoactive mechanisms. J. Psychoact. Drugs. 2000;32:321–331. doi: 10.1080/02791072.2000.10400456. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.