Abstract
This study measured therapist behaviors in relation to subsequent habituation within exposure tasks, and also tested their direct and indirect relationships (via habituation) with clinical outcomes of exposure therapy. We observed 459 videotaped exposure tasks with 111 participants in three clinical trials for pediatric obsessive-compulsive disorder (POTS trials). Within exposure tasks, therapist behaviors and patient fear were coded continuously. Outcomes were habituation and post-treatment change in symptom severity, global improvement, and treatment response. More therapist behaviors that encourage approach—and less use of accommodation, unrelated talk, and externalizing language—predicted greater subsequent habituation during individual exposure tasks (exposure-level), and also predicted improved patient clinical outcomes via higher ‘total dose’ of habituation across treatment (patient-level indirect effect). For six of seven therapist behaviors analyzed, the relationship with subsequent habituation within exposure differed by patient fear (low, moderate, or high) at the time the behavior was used. Two therapist behaviors had direct effects in the opposite direction expected; more unrelated talk and less intensifying were associated with greater patient symptom reduction. Results shed light on the “black box” of in-session exposure activities and point to specific therapist behaviors that may be important for clinical outcomes. These behaviors might be best understood in the context of changing patient fear during exposure tasks. Future studies should test whether therapist behaviors can be experimentally manipulated to produce improvement in clinical outcomes.
Keywords: Exposure, CBT, therapist, OCD, mechanism
Despite clear efficacy, exposure therapy for anxiety and obsessive-compulsive disorder (OCD) is rarely used in practice settings (Higa-McMillan, Francis, Rith-Najarian, & Chorpita, 2016). When used, therapists report a “cautious” exposure delivery approach that deviates from specialist recommendations (Deacon, Lickel, Farrell, Kemp, & Hipol, 2013). Even after intensive therapist training, exposure is associated with the largest research versus practice gaps in treatment integrity (McLeod et al., 2017)—and of all CBT components learned, therapists report exposure as particularly difficult to implement and sustain (Chu, 2015). Reduced exposure quality may contribute to low sustainability (e.g., if therapists try exposure but stop when they do not observe improvement) and could partially explain why exposure-based CBT has not outperformed usual care in some effectiveness trials (e.g., Weisz et al., 2013). Training therapists to reproduce high quality exposures could improve outcomes and sustainability, but factors that contribute to quality have not been empirically identified. Therapist adherence and/or competence are monitored for quality control in clinical trials but have generally failed to predict treatment outcomes. Moreover, some trial therapists have better outcomes than others, even when adherence is universally high and patients are relatively homogeneous (Huppert et al., 2001). General characteristics (e.g., age, gender) have not explained these “therapist effects,” but more experience and exposure specialty training have related to better patient outcomes (Huppert et al., 2001; Crawford et al., 2017). This suggests that therapist delivery approach is important but does not shed light on specific aspects of delivery that might be useful to improve quality.
Several studies have examined exposure characteristics in relation to clinical trial outcomes. Peris, Caporino, and colleagues (2017) report that a higher proportion of “challenging” exposures and greater child mastery and compliance predict improved outcomes among youth in the Child and Adolescent Multimodal treatment Study (CAMS). In a small sample of youth with OCD, Kircanski and Peris (2015) found greater improvement among those with more exposure tasks targeting multiple OCD symptoms and lower peak distress during the last exposure task in a session. However, virtually all studies of exposure characteristics in clinical trials have relied on non-independent reporters (e.g., therapists, patients) and used study-specific measures with unknown psychometric properties. This presents a challenge for understanding important features of exposure with enough detail to ensure they can be replicated and raises the possibility that positive findings reflect a confound with clinical change. For example, using a treatment hierarchy to measure completion of challenging exposures raises the possibility that patients reach challenging tasks because they are getting better (Garcia, 2017). Overall, research has been hampered by a lack of valid and objective measures—prompting researchers to describe exposure as “a black box that needs unpacking” (Garcia, 2017).
Therapist Behaviors and Treatment Mechanism
Measuring observable therapist behaviors during exposure could offer a window into clinical trial delivery approaches and provide concrete information for training. Moreover, behaviors of interest might be guided by the mechanistic theory that underpins exposure. In general, theorized mechanisms of behavioral treatments usually relate to a core learning process (e.g., reinforcement, extinction) and context variables that influence learning are defined using function (i.e. what they do) rather than topography (i.e. what they look like). For example, a therapist could provide a child with a small toy (a topographical behavior), but it might be most relevant to determine whether this behavior functions as positive reinforcement (e.g., by observing whether the toy was desirable to the child and contingent upon engaging in a goal behavior). Therapist behaviors are a central part of the treatment learning context, and several efficacious behavioral treatments for youth use function to define desirable therapist behaviors (e.g., Parent-Child Interaction Therapy, Eyberg, 2005). Despite theoretical connections between therapist behaviors and treatment mechanisms, few studies have tested them empirically.
Elucidating links between therapist behaviors and mechanisms might have advantages for improving psychotherapy quality. First, therapist behaviors that engage a mechanism may show the strongest links with outcomes. This seems particularly important in exposure; recent work suggests that the effects of exposure-based CBT are treatment specific and not well explained by general processes (e.g., alliance; Strauss, Huppert, Simpson, & Foa, 2018). Second, measuring mechanism with linked therapist behaviors could facilitate feedback in practice settings—when measurement is both practical and proximal (i.e. occurring early/often throughout treatment). Providing therapists with regular feedback improves patient outcomes and proximal feedback is particularly effective for shaping behavior (e.g., Delgadillo et al., 2018). Thus, early and ongoing feedback might accelerate therapist learning during initial exposure practice and facilitate tailoring or course-correction during any individual patient’s treatment.
Therapist Behaviors and Mechanism in Exposure Therapy
Exposure is rooted in a strong behavioral theory of mechanism that centers on fear extinction learning (Craske et al., 2018). Exposure also elicits other forms of acute distress (e.g., disgust, incompleteness) which we include under the term ‘fear’ for parsimony. Variants of mechanistic theory differ with respect to the neurocognitive underpinnings of exposure learning (e.g., inhibitory learning, emotional processing; Craske et al, 2018), yet there are many more similarities than differences across them with respect to recommended delivery (Himle, 2015). Most theories also implicate some form of fear change as a signal or facilitator of learning. Fear change is practical to assess and commonly used in practice, and within-exposure fear changes could be particularly useful as a proximal outcome to aid training (i.e. close in time to therapist behaviors). Specific fear changes thought to be relevant for exposure mechanism include fear activation, fear reduction (or habituation), and fear variability. Unfortunately, these have largely shown inconsistent relationships with treatment outcomes (e.g., Jacoby and Abramowitz, 2016).
Aiming to address measurement limitations that may contribute to inconsistent fear change findings, Benito et al. (2018) used independent observers to continuously rate fear changes during exposure in three trials for youth with OCD. Importantly, habituation ratings summed all fear decreases throughout each exposure and also parsed out decreases that were explained by an observable exposure event (thus unlikely to signal therapeutic learning). Such events are common and could include planned or unplanned change in the exposure stimulus, introduction of safety signals or distractors, accommodation, avoidance, escape, rituals, and more. Fear reduction associated with these antecedents did not predict outcomes, but reduction occurring “on its own” (habituation) predicted symptom reduction, global improvement, and treatment response. Other types of fear changes (fear activation, fear variability) did not predict any outcomes. Altogether, these findings suggest that observed habituation within exposure may be uniquely useful as a proximal marker of patient learning.
Fear-decreasing therapist behaviors.
Therapist behaviors that function to reduce short-term fear could interfere with habituation occurring “on its own” and result in poorer outcomes. This idea is consistent with guidelines from exposure specialists, who generally recommend against a “cautious” delivery style using techniques such as distraction, relaxation, or accommodation (e.g., Abramowitz, Deacon & Whiteside, 2012). However, translational work has yielded mixed findings for distraction during exposure (e.g., Senn & Radomsky, 2018). While family accommodation has been linked to higher symptom severity and poorer exposure outcomes (e.g., Lebowitz, Panza, & Bloch, 2016), studies have not examined the role of therapist accommodation. Despite consistent clinical recommendations to avoid fear-decreasing behaviors, none have been examined empirically in relation to treatment outcomes.
Fear-increasing therapist behaviors.
Behaviors that increase or maintain fear might provide opportunities for habituation within exposures. Several theories describe the importance of sustained fear during exposure (e.g., Jacoby & Abramowitz, 2016) and specialists generally recommend an “intense” delivery style (Abramowitz, Deacon & Whiteside, 2012.) While there is some evidence that sustained intensity produces better outcomes (Deacon et al., 2013), it has been difficult to disentangle effects of delivery intensity (i.e. manner of delivery) from dose intensity (i.e. amount delivered). Despite clinical recommendations, empirical support has yet to be established for therapist use of fear increasing behaviors during exposure in clinical treatment.
Fear-neutral therapist behaviors.
Fear-neutral strategies may keep patients engaged and/or support learning without having a clear function on short-term fear (e.g., by improving motivation, self-efficacy, or cognitive processing). Treatment manuals often include cognitive or coping strategies, education about the principles of treatment, and strategies that “externalize” symptoms so that they are discussed as separate from a patient (e.g., Freeman & Garcia, 2008). There is some evidence that coping during exposure tasks does not relate to outcomes (Benito, Conelea, Garcia, & Freeman, 2012; Hedtke, Kendall, & Tiwari, 2009), although it is possible that prompts to use coping skills could be most helpful at specific times (e.g., when fear is high). However, fear-neutral strategies remain largely unexamined.
Therapist behaviors for exposure ‘titration’.
There may be a need to balance exposure difficulty with tolerability despite clear theorized disadvantages of fear-decreasing behaviors and advantages of fear-increasing behaviors. Specialists suggest that skilled therapists monitor ongoing fear changes during exposure and facilitate a “delicate balance between exposure intensity and optimal anxiety” (Chu et al., 2015, p. 12). In addition to overall use of fear increasing, decreasing, or neutral behaviors, therapist titration—selection of these behaviors in response to changing fear—could be relevant for exposure quality. For example, it may helpful to use fear-increasing behaviors when fear is low. To optimize practice recommendations, it will be important to evaluate the effect of therapist behaviors used at different levels of patient fear.
Summary and Current Study
Defining therapist behaviors according to short-term function on fear (increase, decrease, or neutral) generally mirrors specialist recommendations for delivering exposure. These categories are also relevant for habituation, a possible marker of initial exposure learning. Linking therapist behaviors to habituation within an exposure task could facilitate feedback in practice, which might aid therapist learning, enhance exposure quality, and ultimately improve outcomes. Despite this, it is unclear how therapist behaviors relate to patient learning in the context of clinical exposures, and delivery recommendations have yet to be empirically validated. Finally, little is known about the delivery approaches of trial therapists—a barrier to reproducing quality across research or practice settings. This study aimed to address these gaps. Specifically, we aimed to characterize the behaviors of clinical trial therapists during exposure tasks (Aim 1); examine therapist behaviors used during times of low, moderate, and high patient fear and determine whether these relate to subsequent habituation within the same exposure (exposure-level analyses; Aim 2); and examine relationships between therapist behaviors and clinical outcomes, including direct and indirect effects via habituation (patient-level analyses; Aim 3). Figure 1 illustrates these aims within the conceptual framework used to design this study. Independent observers completed microanalytic coding of 459 videotaped exposures for 111 youth with OCD who received exposure in one of three randomized controlled trials. Clinical outcomes were assessed by independent evaluators (IE) at baseline and post-treatment.
Figure 1.
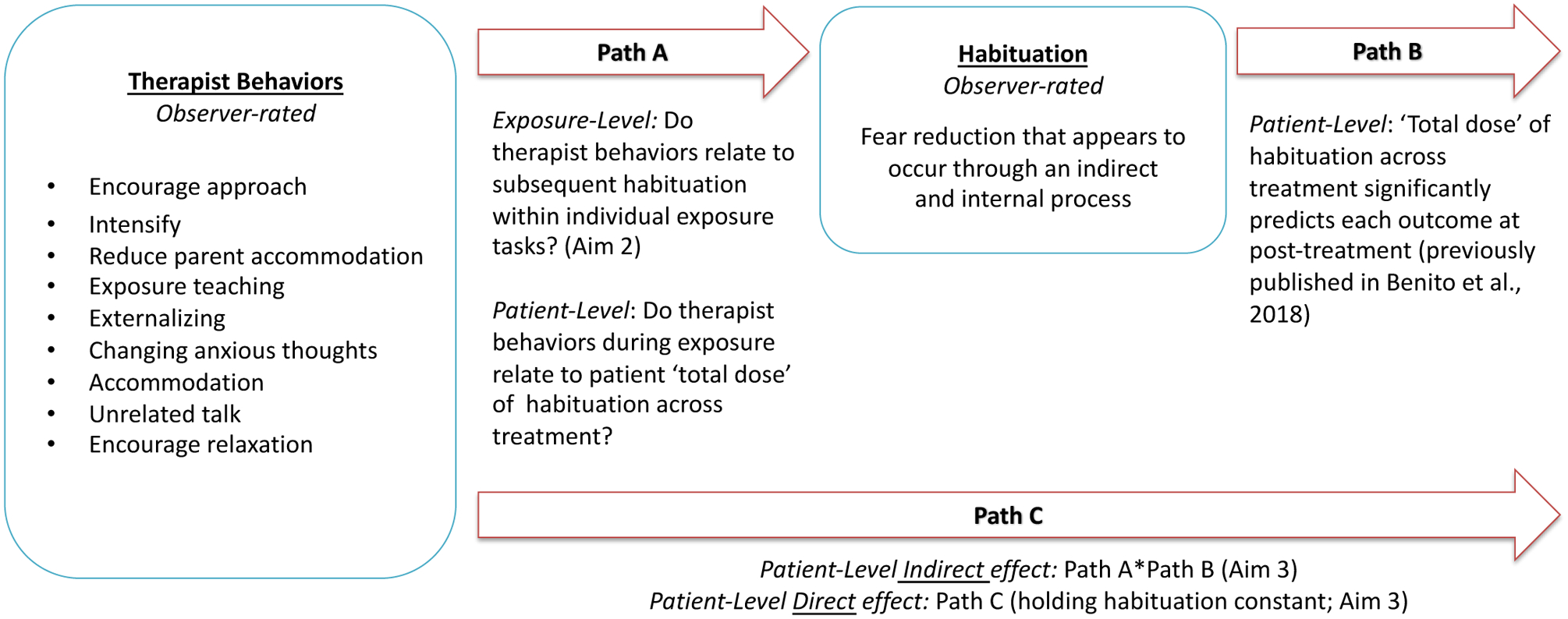
Conceptual model with related study methods and aims
Method
Original Treatment Trials
Relevant Institutional Review Boards approved procedures for the original trials and the current study. Treatment in the Pediatric OCD Treatment Study (POTS) trials occurred at three sites and results support the efficacy of exposure-based CBT (Franklin et al., 2011; Freeman et al., 2014; Pediatric OCD Treatment Study (POTS) Team, 2004). In POTS I, 112 participants age 7–17 were randomly assigned to receive CBT alone, medication management (MM) alone, CBT and MM, or pill placebo. In POTS II, 124 participants age 7–17 were randomly assigned to receive MM alone, MM plus instruction in CBT (iCBT), or MM plus full CBT. In POTS Jr., 127 youth age 5–8 were randomly assigned to receive CBT or relaxation therapy (RT).
POTS trials used published CBT manuals (Freeman & Garcia, 2008; March & Mulle, 1998) where most sessions included exposure (11 sessions in POTS I and II, 8 sessions in POTS Jr.). CBT was provided by 32 trained therapists; all participated in weekly cross-site supervision and review of session videotapes confirmed greater than 80% adherence to session elements. Manuals did not specifically guide exposure process (e.g., duration, intensity, rationale, therapist behaviors). Although the trials occurred at a time when emotional processing theory (EPT) was a dominant theory of exposure mechanism, therapists were not routinely trained to specifically facilitate habituation. Medication protocols differed across the trials. In POTS I, youth began sertraline after being randomized to a condition with MM, and dose was rapidly titrated upward during the first four weeks of treatment. In POTS II, all enrolled youth were considered partial medication responders (i.e. had already optimized medications and were still seeking treatment). All youth in POTS II were already stable on medications at baseline, and the protocol did not permit upward titration during treatment. POTS Jr. did not include medication management.
Current Sample
Participants were those randomized to receive CBT (with or without MM), completing a post-treatment assessment, and with at least one exposure video available for coding (N = 111). This sample includes five patients that dropped from treatment but remained for post-treatment assessment and includes 46 youth receiving MM with CBT (41.1%). Prior analyses examining the link between fear change metrics and clinical outcomes used this same sample (Benito et al., 2018), which is representative of original trial participants’ baseline severity (CYBOCS M = 25.15 SD = 4.67, indicating “severe” symptoms), age (M = 10.17, SD = 3.41), sex (55.4% female), and race/ethnicity (91.2% White, 3.5% Black, 4.4% other race, 5.3% Hispanic). The proportion of youth by trial (24.1% POTS I, 27.7% POTS II, 48.2% POTS. Jr.) and site (33.0% Brown, 38.4% Duke, 28.6% Penn) is consistent with the number of youth originally randomized, except that it includes a lower proportion of youth from POTS I and from the Penn site (due to higher rates of missing or damaged video). The exposure sample (N = 459) was drawn from 48.0% of protocol exposure sessions, and equally represents early (32.0%), middle (32.0%), and late (36.0%) treatment sessions. Mean exposures observed for each patient was 4.00 (SD = 3.08).
Exposure Process Coding System (EPCS)
EPCS uses Noldus Observer software (Noldus XT v. 9.0, 2009), which links video files with coding data and generates start and stop timestamps each time a code is observed. EPCS codes continuously assess patient fear, habituation, and in-session behaviors (therapist, patient, and parent behaviors if applicable). Illustration of EPCS data capture using two example exposures is available in Figure 1 of the Supplementary Materials. Coder training. EPCS coders were masked to trial IE data (baseline characteristics, treatment progress and outcome) and included four bachelor’s level research assistants and one post-doctoral fellow. Coders were trained to criterion (K or ICC > .80) and attended weekly meetings throughout the study. The first author reviewed 10% of coded exposures to prevent drift. Coding Procedures. Before coding, sessions were viewed to determine exposure start and stop times. Exposure start occurred with therapist statement that an exposure was starting, presentation of an exposure stimulus, or at least two SUDS ratings or other assessment of difficulty regarding a present task. When fear occurred in anticipation of a chosen task, we coded this time as part of the exposure. Exposure stop occurred with therapist statement that exposure was over, withdrawal of the stimulus (without reintroduction) or change in session focus without reference to ongoing exposure.
Codes of interest in the current study include patient fear, habituation, and therapist behaviors (Table 1). EPCS samples observer-rated fear continuously, starting at the onset of the exposure for the duration of the exposure task. Fear is rated on a 0 to 5 scale, where 0 indicates no fear (no verbal or behavioral evidence of fear) and 5 indicates maximum fear (patient verbally and/or behaviorally expresses highest possible levels of fear and/or appears very uncomfortable, with indicators that may include high levels of stereotypic movement, anxious verbalizations, sweating, crying, or refusals). This code demonstrated excellent psychometric properties in prior analyses with the current sample (Benito et al., 2018), including construct validity with patient-reported SUDS and good to excellent inter-coder reliability for each observed fear level. In the current study, we used this code to calculate duration of low (0–1), moderate (2–3), and high (4–5) patient fear. As coders rated patient fear, they also judged whether each instance of fear decrease was associated with an antecedent likely to explain the reduction (e.g., rituals, avoidance, accommodation, reduction of task difficulty, change in stimulus, distraction, attempts to ‘make’ fear reduce). Fear decreases not better explained by such events were judged to be habituation. EPCS-rated habituation demonstrated strong psychometric properties in prior analyses with the current sample (Benito et al., 2018), including excellent inter-coder reliability and predictive validity with patient clinical outcomes. Given the complexity of habituation measurement considerations, Supplemental Figures 2 and 3 illustrate the calculation method using an example exposure, and we refer readers to Benito et al., 2018 for additional detail and rationale. The cumulative sum of habituation (sum of all habituation fear decreases throughout each exposure task) is a primary outcome at the exposure- and patient-levels in this study.
Table 1.
Observer Rated Therapist Behaviors
| Behavior | Definition |
|---|---|
| Fear Increasing | |
| Encourage Approach | Therapist facilitates patient physical or mental contact with the exposure stimulus, including redirection to the exposure task (e.g., “Try to keep looking at the picture”), discouraging avoidance or rituals (e.g., “Remember to resist the urge to ask for reassurance”), requests to describe fear content (e.g., “What are the worries saying right now?”), discussion of the exposure stimulus (e.g., “Ok, we’ve got the trash can out”), or other actions that keep the patient engaged with the exposure task. |
| Intensify | Therapist changes the exposure task to make it more difficult (e.g., asks patient to put contaminant on both hands instead of one) or makes a statement likely to increase fear by providing new relevant information (e.g., “This carpet hasn’t been washed for a really long time”) or new relevant opinion (e.g., “Wow, that is a lot of vomit”). |
| Reduce Parent Accommodation | Therapist discourages parent accommodation behavior during the exposure; this could occur independent of or in response to-actual occurrence of parent accommodation (e.g., “Your mom is going to try and resist any OCD questions”). |
| Fear Neutral | |
| Teaching | Therapist provides brief instruction about a CBT principle or symptom that relates to the current exposure (e.g., “Remember, your job during exposures is to practice ‘riding the anxiety wave’”). Teaching that is not relevant for the current exposure or that functions as a distraction from the exposure would be coded as unrelated talk. |
| Externalizing | Therapist refers to OCD or anxiety as being separate from the patient, which may include a patient-selected name if developmentally appropriate (e.g., “You’re the boss of Mr. Worry”). Externalizing was coded only when occurring in a statement without another code of interest. For example, the statement “Don’t let those worries trick you into giving up!” contains elements of both externalizing and encouraging approach but would be coded as encourage approach. |
| Changing Anxious Thoughts | Therapist leads the child to use a cognitive or coping strategy to manage fear during the exposure (e.g., evaluating the likelihood of a feared consequence, using coping statements such as “I am brave”). This code is used when the therapist elicits or prompts patient use of a strategy; if the therapist supplies fear-reducing information (e.g., stating that the actual risk is low) it would be coded as accommodation. |
| Fear Decreasing | |
| Accommodation | Therapist changes the exposure task to make it less difficult (e.g., instructs patient to decrease contact with the exposure stimulus) or makes a statement likely to decrease fear by providing new relevant information (e.g., “I eat this all the time and nothing bad happened to me”) or new relevant opinion (e.g., “I think you’ll be ok”). |
| Unrelated Talk | Therapist makes a statement that is not related to the current exposure and could serve to decrease patient focus on the exposure task. Content may be general (e.g., “What are you guys up to this weekend?”) or include CBT components with limited relevance for patient experience of the ongoing exposure task (e.g., extended psychoeducation about etiology of anxiety, planning homework for a different exposure). |
| Encourage Relaxation | Therapist leads the child to use relaxation techniques, such as taking deep breaths, muscle relaxation, or pleasant imagery (e.g., “Remember how to control your breathing?”). |
EPCS-rated therapist behaviors (Table 1) were iteratively developed using theory and pilot testing, and initially demonstrated good psychometric properties in a sample of young children with OCD (Benito et al., 2012). Inter-coder reliability in this sample was adequate to excellent across behaviors (15% double-coded; k range .71–.92). Therapist behaviors are mutually exclusive with one another but occur concurrently with fear ratings. Exposure-level therapist behavior durations were created by summing the duration of all relevant behaviors within each exposure, excluding any duration that occurred after an instance of habituation. We excluded durations after habituation for two reasons: 1) therapist behaviors might have different effects if habituation has already occurred (e.g., if encouraging contact with the exposure stimulus is less potent when one is already “used to it”), and 2) to establish temporal order of therapist behaviors in relation to habituation within exposures. Final therapist behavior variables were calculated as a proportion of time (behavior duration/exposure duration or relevant fear level duration). Patient-level therapist behavior variables were created by summing exposure-level variables within patients (across treatment). When more than one exposure occurred in a session, exposure-level values were first summed across exposure tasks to create one session-level value. The patient-level “total dose” was then calculated as the product of the session value and the number of exposure sessions attended. This mirrors calculations used for patient-level habituation as in Benito et al. (2018). Final therapist behavior variables were calculated as a proportion of time (total dose of behavior duration/total dose of exposure duration).
Clinical Outcome Measures
All clinical outcome measures were administered at baseline (week 0) and/or post-treatment (week 12 in POTS I and II; week 14 in POTS Jr) by IEs who were masked to treatment condition and not otherwise involved in the study. IEs were trained to a reliable standard on each measure (k or ICC > .80) through joint interviews, videotape reviews, and participation in monthly cross-site supervision conferences. Reliability was checked regularly on randomly selected videotapes, and IEs were retrained to criterion if they fell below 80% agreement.
OCD symptom severity.
The Children’s Yale Brown Obsessive Compulsive Scale (CY-BOCS; Scahill et al., 1997) is the gold-standard measure of pediatric OCD severity, with total scores ranging from 0 (no illness) to 40 (extreme severity). The CY-BOCS has excellent psychometric properties, including sensitivity to change in treatment (Scahill et al., 1997). CY-BOCS change from baseline to post-treatment, where lower (negative) values indicate greater symptom reduction, is a primary outcome at the patient-level in the current study.
Global improvement.
The Clinical Global Impression-Improvement scale (CGI; Guy, 1976) measures global improvement on a 1 (very much improved) to 7 (very much worse) scale, and has excellent psychometric properties, including sensitivity to change in treatment. Post-treatment CGI score is a primary outcome at the patient-level in the current study.
Treatment response.
Participants were classified as treatment responders when having CY-BOCS change ≥ 30% from baseline to post-treatment and a post-treatment CGI score ≥ 2 (indicating “much improved” or “very much improved”). This method of calculating treatment response incorporates dimensional symptom reduction as well as clinically meaningful global change. Treatment response is a primary outcome at the patient-level in the current study.
Analytic approach
Analyses were conducted using Generalized Linear Mixed Models (GLMMs) in SAS 9.4 (SAS Institute, Cary, NC, 2003) in PROC GLIMMIX. A random intercept for study (POTS I, POTS II, or POTS Jr.) was included in all models. Models did not include other random intercepts due to insufficient observations for stable estimates at each of many nested levels (i.e. exposures within sessions, sessions within patients, patients within therapists and study, and therapists within site). All analyses included a fixed effect of the relevant duration variable (overall exposure duration or duration at low/moderate/high fear). Therefore, any significant therapist behavior effects would be over and above any effect of exposure duration or fear level duration. Distributions and link functions were chosen with theory (e.g., Poisson for count) and examination of model residuals (e.g., heterogeneity of variance across linear predictions). Distribution of the predictor was also examined in relation to the dependent variable. When preliminary inspection revealed deviations from homoscedasticity or normality, we first applied square root, followed by cube root transformations until deviations were corrected. Relationships between predictors and outcomes were tested with significance of slope parameters. Slope estimates were based on transformed predictors and are not interpretable in original units.
To test path A at the exposure level (Aim 2, Figure 1) we separately modeled the fixed effect of each therapist behavior (overall and during low/moderate/high patient fear) on habituation. To test path A at the patient level, we separately modeled the fixed effect of each therapist behavior on habituation; we did not test patient-level models by fear level due to patient sample size constraints. Results of Path B were previously published (Benito et al., 2018), finding significant relationships between habituation and each clinical outcome. Although significance of Paths A and B would establish that an indirect effect is present (i.e. mediation effect), it does not provide confidence intervals around the indirect effect. Therefore, we used the asymmetric distribution of the product approach (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002) to generate 95% confidence intervals around estimates of indirect effects (Aim 3, Figure 1). This approach has demonstrated better power and Type I error rates compared with those that assume a normal distribution of the indirect effect (e.g, Z-test), and matches results of high performing (but computationally demanding) re-sampling methods such as bias-corrected bootstrapping in nearly all cases (MacKinnon, Lockwood, & Williams, 2004). In contrast to the indirect effect, a direct effect is the relationship between a predictor and an outcome while controlling for the mediator. To quantify direct effects (i.e. holding habituation constant; Aim 3, Figure 1), we modeled the fixed effect of each behavior with fixed effects of exposure duration and habituation on each outcome: symptom severity change (Gaussian), global improvement (binomial), and treatment response (binary). We did not quantify total effects (i.e. relationship between therapist behaviors and outcomes without habituation in the model; step 1 in Baron and Kenny, 1986) because this step is eliminated in contemporary approaches and its requirement can obscure true relationships among study variables (e.g., if a direct effect and indirect effect are opposite in sign; Fairchild & McDaniel, 2017).
Patient-level analyses were conducted with 86 patients for whom we observed at least one instance of habituation during sampled exposures. In previous patient-level analyses with this same sample (Benito et al., 2018), habituation significantly predicted clinical outcomes in these 86 patients. However, the remaining 25 of 111 patients in the sample had zero observed instances of habituation; mean clinical outcomes in this subgroup differed significantly from the model-predicted mean using the rest of the sample. Follow-up analyses found that the subgroup with zero observed habituations had significantly fewer coded sessions but no other differences on any study variables, suggesting that the pattern of results in this subgroup was an artifact of insufficient session sampling for detecting the true absence of an infrequent event at the patient level (Benito et al., 2018; Suen & Ary, 2014). Because EPCS variables were observed continuously within each coded exposure task, insufficient sampling is not a relevant concern for detecting the absence of habituation at the exposure level. Therefore, the exposure-level analyses reported below include all observed exposures (N = 459) for all patients (N = 111). We also conducted a parallel set of analyses including only those exposures for patients included in patient-level analyses (i.e. those with greater than zero observed habituation; N = 396 exposures, N = 86 patients); results were identical to those reported for the full exposure sample below.
Results
Descriptive statistics for exposure- and patient-level variables are presented in Table 2. Therapist behaviors that address parent accommodation and those that encourage use of relaxation were present in too few exposures (< 3%) to complete analyses.
Table 2.
Exposure- and Patient Level Descriptive Statistics
| Exposure-Level (N = 459) | Patient-Level (N = 86) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low Feara | Moderate Fearb | High Fearc | Overall | Overall | ||||||
| Exposure Duration (minutes) | % presentd | % presentd | % presentd | % present | % presente | |||||
| Total Duration | 95.9 | 74.1 | 13.5 | -- | -- | |||||
| Duration excl. after habituationf | 94.8 | 73.6 | 12.2 | -- | -- | |||||
| Therapist Behaviors (percent time)g | ||||||||||
| Encourage Approach | 94.3 | 94.675 | 87.5 | 97.6 | 100.0 | |||||
| Intensify | 43.0 | 46.5 | 25.0 | 59.9 | 90.8 | |||||
| Discourage Accommodation | 0.9 | 2.1 | 1.8 | 2.6 | 11.5 | |||||
| Exposure Teaching | 20.7 | 34.0 | 33.9 | 42.5 | 75.9 | |||||
| Externalizing | 32.2 | 45.3 | 44.6 | 54.3 | 82.8 | |||||
| Change Thoughts | 6.9 | 20.7 | 19.6 | 21.4 | 50.6 | |||||
| Accommodation | 17.5 | 35.5 | 53.6 | 40.5 | 79.3 | |||||
| Unrelated Talk | 18.9 | 25.2 | 23.2 | 31.4 | 60.9 | |||||
| Relaxation | 1.2 | 1.2 | 1.8 | 1.7 | 5.8 | |||||
fear 0–1 out of 5;
fear 2–3 out of 5;
fear 4–5 out of 5;
percent exposures in which variable was observed;
percent patients in which variable was observed,
duration of exposure excluding any time that occurred after an instance of habituation;
percent time behavior was observed (of total time at fear level or overall)
Exposure-level Results (N = 459 exposures)
Path A results are presented in Table 3. Longer duration of moderate fear—but shorter duration of low fear—related to greater subsequent habituation within exposures. Overall exposure duration and duration of high fear did not relate to habituation. While fear was moderate or high—but not while it was low—encouraging approach and intensifying behaviors predicted greater subsequent habituation. While patient fear was low or moderate—but not while it was high—therapist accommodation and unrelated talk predicted less subsequent habituation. Overall use of externalizing language predicted reduced habituation. Exposure teaching predicted less subsequent habituation when used during moderate fear, but overall use was not significant. Changing anxious thoughts was associated with less subsequent habituation when used during low fear, but with greater habituation when used while fear was high.
Table 3. Path A (exposure-level):a.
Relationships between therapist behaviors and subsequent habituation within exposures
| Low Fearb | Moderate Fearc | High Feard | Overall | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | 95% CI | Estimate | SE | 95% CI | Estimate | SE | 95% CI | Estimate | SE | 95% CI |
| −0.008 | 0.689 | −1.362, 1.347 | 2.998 | 0.431 | 2.152, 3.845 | 1.726 | 0.721 | 0.308, 3.144 | 2.087 | 0.872 | 0.373, 3.801 |
| −0.400 | 0.209 | −0.810, 0.011 | 1.165 | 0.411 | 0.357, 1.974 | 1.728 | 0.215 | 1.306–2.149 | 0.545 | 0.356 | −0.154, 1.244 |
| −4.347 | 0.906 | −6.127, −2.566 | −1.846 | 0.537 | −2.902, −0.791 | −0.174 | 1.597 | −3.313, 2.964 | −5.380 | 0.631 | −6.621, −4.140 |
| −3.543 | 1.182 | −5.866, −1.220 | −3.668 | 0.801 | −5.243, −2.094 | −0.842 | 1.498 | −3.786, 2.103 | −3.993 | 0.910 | −5.781, −2.206 |
| −1.309 | 0.760 | −2.803, 0.185 | −2.872 | 2.160 | −7.116, 1.372 | 0.054 | 0.485 | −0.900, 1.007 | −2.131 | 0.730 | −3.565, −0.696 |
| −4.341 | 0.829 | −5.970, −2.712 | 0.122 | 0.577 | −1.011, 1.255 | 3.203 | 1.382 | 0.487, 5.920 | −0.459 | 0.491 | −1.424, 0.506 |
| −0.435 | 1.706 | −3.788, 2.917 | −1.156 | 0.330 | −1.805, −0.507 | 0.138 | 1.287 | −2.392, 2.667 | −1.277 | 1.357 | −3.943, 1.390 |
| −0.016 | 0.005 | −0.026, −0.005 | 0.012 | 0.003 | 0.007, 0.018 | 0.004 | 0.006 | −0.008, 0.015 | −0.005 | 0.004 | −0.012, 0.002 |
N = 459 exposures;
Fear 0–1 out of 5;
Fear 2–3 out of 5;
Fear 4–5 out of 5;
Proportion of time the behavior was observed during each fear category--low, moderate, high, or overall (of total time at the relevant fear category);
duration of exposure excluding any time that occurred after an instance of habituation
p < .05; higher proportion of behavior or duration associated with less habituation
p < .05; higher proportion of behavior or duration associated with more habituation
Patient-level Results (N = 86 patients)
Results for Path C indirect effects are presented in Table 4; results of Path C direct effects are reported in text where significant (full results are available in Table 1 of the Supplementary Materials). Greater total exposure duration across treatment had a significant indirect relationship with all clinical outcomes via habituation, but direct effects were not significant (p > .05). In older mediation approaches (e.g., Baron and Kenny, 1986), this pattern of findings (i.e. presence of a significant indirect effect when the direct effect is not significant) would be termed “full mediation.” Encouraging approach predicted better clinical outcomes indirectly via habituation, but direct effects were not significant (p > .05). Intensifying behavior did not have a significant indirect relationship with any outcomes, but had a significant direct effect such that more intensifying related to attenuated change in symptom severity (Slope Est. = 29.135, SE = 3.663, 95% CI [21.844, 36.427]). Therapist unrelated talk predicted poorer clinical outcomes indirectly via habituation, but had a significant direct effect in the opposite direction such that more unrelated talk was associated with greater reduction in symptom severity (Slope Est. = −14.964, SE = 2.098, 95% CI [−19.140, −10.788]). Greater use of accommodation and externalizing language predicted poorer clinical outcomes indirectly via habituation, but the direct effect was not significant (p > .05). Changing anxious thoughts did not have a significant indirect or direct relationship with any outcomes (p > .05). There was a significant indirect effect of exposure teaching; however, this should not be interpreted as a significant finding because path A was not significant (i.e. does not exhibit joint significance; e.g., MacKinnon et al., 2002).
Table 4. Path C indirect effects (patient-level)a:
Relationships between therapist behaviors and clinical outcomes (via habituation)
| Indirect Effects | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Habituation | Severity Δ | Global Improvement | Responder | |||||||||
| Therapist Behaviorb | Est | SE | 95% CI | Est | SE | 95% CI | Est | SE | 95% CI | Est | SE | 95% CI |
| Encourage Approach | 1.486 | 0.627 | 0.240, 2.732 | −2.749 | 0.433 | −3.432, −1.762 | −0.416 | 0.069 | −0.522, −0.241 | 0.802 | 0.138 | 0.590, 1.152 |
| Intensify | 0.189 | 1.065 | −1.929, 2.306 | −0.350 | 0.735 | −1.861, 1.162 | −0.053 | 0.117 | −0.297, 0.217 | 0.102 | 0.234 | −0.385, 0.641 |
| Accommodation | −1.646 | 0.780 | −3.198, −0.094 | 3.045 | 0.538 | 2.203, 4.277 | 0.461 | 0.086 | 0.331, 0.680 | −0.889 | 0.172 | −1.148, −0.450 |
| Unrelated Talk | −1.537 | 0.511 | −2.55, −0.520 | 2.843 | 0.353 | 2.270, 3.642 | 0.430 | 0.056 | 0.342, 0.569 | −0.830 | 0.112 | −1.007, −0.552 |
| Externalizing | −1.800 | 0.812 | −3.415, −0.185 | 3.330 | 0.560 | 2.446, 4.608 | 0.504 | 0.089 | 0.366, 0.730 | −0.972 | 0.179 | −1.247, −0.520 |
| Change Thoughts | −0.469 | 0.884 | −2.227, 1.289 | 0.868 | 0.610 | −0.318, 2.180 | 0.131 | 0.097 | −0.057, 0.367 | −0.253 | 0.194 | −0.631, 0.218 |
| Exposure Teaching | 0.956 | 0.790 | −0.616, 2.527 | −1.769 | 0.545 | −2.697, −0.535 | −0.268 | 0.087 | −0.410, −0.046 | 0.516 | 0.174 | 0.231, 0.960 |
| Durationc | 0.010 | 0.001 | 0.008, 0.011 | −0.019 | 0.001 | −0.020, −0.017 | −0.003 | 0.000 | −0.003, −0.003 | 0.005 | 0.000 | 0.005, 0.006 |
N = 86 patients;
Est. proportion of time per patient (of est. duration for each patient);
duration excluding time during exposure that followed an instance of habituation
p < .05; higher proportion of behavior or duration associated with less desirable clinical outcome
p < .05; higher proportion of behavior or duration associated with more desirable clinical outcome
Discussion
Overall, results support several specific therapist behaviors that significantly predict both habituation and clinical outcomes in exposure therapy. More therapist behavior that encourages approach, less accommodation, less unrelated talk, and less use of externalizing language were consistently linked with greater habituation and better clinical outcomes. These results are broadly consistent with clinical recommendations and the behavioral theory that underpins exposure. Findings also point to the importance of considering patient fear when evaluating the link between therapist behaviors and subsequent habituation during an exposure task; six of the seven behaviors we analyzed had different results depending upon patient fear at the time the behavior was used (low, moderate, or high fear). Notably, therapist behavior effects were significant even when accounting for exposure duration and patient fear level, underscoring their importance in addition to exposure “dose” and intensity. Below, we discuss findings for each predictor and consider clinical and research implications.
Exposure and Fear Duration
Exposure duration did not predict habituation at the exposure level but predicted better treatment outcomes via habituation (indirect effect) at the patient level. This difference might be explained by different sources of variability at each level: duration at the exposure level is influenced by the length of individual exposures, while duration at the patient level is influenced by both exposure length and number of exposures over a course of treatment. However, moderate fear duration did relate to greater subsequent habituation within a given exposure. Altogether, these findings suggest that longer individual exposures of moderate difficulty and more exposures across treatment may be preferred for maximizing habituation, and in turn, clinical outcomes. This is consistent with the findings of prior studies where more exposures robustly predicted better outcome (Peris, Caporino et al., 2017). Interestingly, we also found that high fear did not relate to habituation and was relatively uncommon in this sample of clinical trial exposures—suggesting that a high level of fear is not necessary for successful exposures.
Fear-Increasing Behaviors
Therapist encourage approach behavior had a significant indirect effect, but direct effects were not significant—suggesting that it relates to better clinical outcomes primarily via increased “total dose” of habituation across treatment. At the exposure level, encourage approach and intensifying behaviors predicted greater subsequent habituation—when used while patient fear was moderate or high, but not while it was low. Though surprising given our titration hypothesis (i.e. fear-increasing techniques could help when fear is low), we speculate that this finding could relate to a problem with exposure task selection. Low fear could occur when a task is “too easy” or does not accurately target fears; therapist attempts to increase fear may not have the desired effect when the task itself is suboptimal. Rather than continue, the persistence of low fear might cue therapists to choose a new task. We did not examine exposure task selection, and future studies will be needed to determine whether task selection problems could explain our finding.
Surprisingly, greater therapist use of intensifying behavior was associated with attenuated symptom reduction when holding habituation constant (i.e. direct effect). This seems inconsistent with common clinical recommendations to conduct intense exposures (e.g., Abramowitz, Whiteside & Deacon, 2012) and with prior studies suggesting that challenging exposures may be beneficial (Peris, Caporino et al., 2017). However, it is likely that selection of challenging exposure tasks differs from therapist intensifying behavior during exposure. For example, it may be easier to foster collaboration while choosing an exposure task, whereas “on the fly” therapist intensifying behaviors could sometimes be viewed by families as non-collaborative. Although there is ample evidence that use of exposure is not associated with reduced therapeutic alliance (e.g., Kendall et al., 2009), therapist collaborative style predicts improved outcomes among youth receiving exposure-based CBT (Podell et al., 2013). Future studies are needed to explore this possibility, and to understand the circumstances under which therapist intensifying behavior should be used versus avoided during exposures.
Therapist behaviors that address parent accommodation were present in too few exposures (< 3%) to permit analyses. Parents were only present for a portion of the exposures we observed (54.2%), which likely reflects the developmental range of our sample (i.e. parents may not always be present for exposures with adolescents) and other clinical needs (e.g., when parent absence is purposeful, such as when parents serve as a safety signal). Although this could contribute to low rates of therapist behavior that addresses parent accommodation, this finding is still surprising given that POTS treatment manuals specifically include components that aim to reduce parent accommodation. However, these components were separate from exposure in the manuals. Although therapists were highly adherent to these components, manuals did not provide guidance about how they might be incorporated into in-office exposures. There is strong evidence that outcomes are improved when exposure-based treatment also addresses family processes including accommodation (Peris, Rozenman et al., 2017). Future studies should aim to understand whether it is helpful to address accommodation during in-office exposure, which may be an important opportunity for family members to engage in guided skill practice.
Fear-Decreasing Behavior
While patient fear was low or moderate—but not while high—therapist accommodation and unrelated talk predicted less subsequent habituation during exposure tasks. This is consistent with general clinical recommendations to avoid these behaviors, although it indicates that some accommodation and unrelated talk might be used when fear is high without negatively impacting treatment. Therapist accommodation had a significant indirect relationship with treatment outcomes, but direct effects were not significant--suggesting that accommodation relates to poorer clinical outcomes primarily via reduced habituation across treatment. This is consistent with the literature on family accommodation (e.g., Lebowitz, 2016) and extends these findings to therapist behaviors in the context of in-session exposure. Notably, therapist accommodation was common, though its duration on average was brief—occurring in 40% of exposure tasks and with nearly 80% of patients during treatment. This could relate to the way accommodation was defined, which may encompass some behaviors that are clinically appropriate (e.g., modifying an exposure task to make it easier when it seems too hard). This idea is also consistent with our finding that accommodation does not seem contraindicated when fear is high.
Therapist unrelated talk predicted poorer outcomes indirectly via habituation, which is consistent with clinical recommendations to avoid distraction but discrepant from some translational findings (e.g., Senn & Radomsky, 2018). A significant but opposite direct effect suggests that unrelated talk relates to greater symptom reduction when holding constant its negative effect on habituation. Though we defined unrelated talk using function during exposure (i.e. as distraction), this code encompassed a variety of content that could have contributed to improvement via pathways other than within-exposure learning (e.g., rapport-building, homework planning). Future studies should seek to understand which components of “unrelated talk” might be important; one strategy could be to avoid these during exposure but incorporate them into other parts of a session. This interesting finding underscores the need to consider whether treatment elements could operate through different mechanisms, and to generate clinical recommendations that are informed about how those elements interact with one another.
Fear Neutral Behaviors
Therapist externalizing language emerged as a consistent predictor of reduced habituation and poorer clinical outcomes. Although externalizing is thought to reduce blame for symptoms and illustrate the rationale for exposure, this finding could have been influenced by our use of decision rules to ensure that therapist behaviors were mutually exclusive. Externalizing behavior was only coded when other behaviors of interest were absent (e.g., accommodation or intensifying), though our experience suggests it commonly occurred with such behaviors. As a result, we may have captured therapist externalizing language that is relatively “functionless.” It could also be that externalizing language is fear reducing for some patients and/or in some contexts. For example, patients with fears that relate to personal responsibility or who experience thought-action-fusion may be overly reassured by therapist externalizing language that implies limited responsibility for fear cognitions. Another possibility is that therapists use more externalizing language in response to patient characteristics that interfere with treatment (e.g., high family conflict or difficulty understanding exposure rationale). Future research should examine externalizing more closely to understand how it relates to poorer outcomes in exposure.
Exposure teaching showed opposite relationships at the exposure vs. patient-levels. Although the patient-level effect was not significant, this seems conceptually reasonable given that exposure teaching draws on principles relevant beyond a single exposure. It could be distracting or reassuring within an exposure but promote learning across exposures. Future studies should test this with particular attention to within- vs. across-exposure effects. We also found a mixed pattern of results for changing anxious thoughts; consistent with our hypothesis, it was associated with less habituation when used during low fear, but with more when used during high fear. It did not relate to clinical outcomes at the patient-level. However, we note that POTS manuals include fewer sessions devoted to teaching cognitive and coping skills compared with other CBT manuals for youth and our results may not generalize to those protocols. Future studies will need to examine this in a wider variety of treatment protocols and practice settings.
Summary of Clinical Implications
During a given exposure, therapists should consider the link between their own behaviors and subsequent habituation, which may depend upon patient fear at the time the behavior is used. Low fear. Longer duration of low fear is associated with less subsequent habituation but encouraging approach and intensifying during this time does not appear to be of benefit. When low fear persists, it could be advisable to select a new exposure (although we did not test that strategy). Therapists should avoid accommodation, unrelated talk, and changing anxious thoughts. Moderate fear. Longer duration of moderate fear relates to greater subsequent habituation. Specific therapist behaviors that might be of additional benefit during this time include encouraging approach and intensifying. Therapists should avoid exposure teaching, accommodation, and unrelated talk. High fear. High fear was uncommon and did not relate to habituation, suggesting that it is not necessary for successful exposure. When fear is high, therapists should consider encouraging approach and changing anxious thoughts. Accommodation and unrelated talk during high fear were not associated with reduced habituation; judicious use of these may be acceptable during this time.
For any given patient, therapists should maximize total exposure duration over the course of treatment, which is influenced by both the length of individual exposures and the number of exposures conducted. In general, therapists should spend more time encouraging approach and less time engaging in unrelated talk, accommodation, and externalizing. Therapists may wish to structure sessions to ensure separate time for other treatment components, such as homework planning, which could distract during an exposure task. Therapists might find intensifying helpful for habituation within an exposure, but more intensifying behavior across treatment could be undesirable and additional research on this is needed. Despite these potential implications for exposure delivery, we emphasize that we did not investigate whether therapist behaviors cause habituation or patient outcomes. This warrants considerable attention in future studies before we might draw definitive conclusions about the best way to deliver exposures in practice.
Limitations
Coding system design.
EPCS codes rely on observation, which has limitations for capturing internal processes such as fear change. Future studies should examine how therapist behaviors relate to fear change measures across different units of analysis (e.g., behavioral, physiological, self-report; National Advisory Mental Health Council, 2016). Additionally, codes capture moment-to-moment behaviors within exposure but do not assess other procedures likely to be important for optimizing outcomes (e.g., design/selection of exposure tasks, post-exposure processing). For example, we did not examine whether it would be desirable to repeat exposure tasks or to design tasks that target more than one type of fear. We also did not capture all behaviors during exposure that could be relevant. For example, we did not differentiate among specific cognitive or coping strategies. Though in some ways a limitation, the connection with behavioral theory is also a strength. Definitions incorporate short-term function, which is central to theories of mechanism and could be particularly relevant for treatment outcome. We used habituation within exposures as a proximal outcome because it is theorized to signal initial learning, has high potential for utility in practice settings, and has empirical support. However, initial learning is only one component of successful long-term fear extinction, and future studies should examine therapist behaviors in relation to post-exposure phases of learning (i.e. consolidation and later retrieval of extinction memories). Additionally, there may be other mechanisms through which therapist behaviors could be helpful (e.g., by improving motivation or self-efficacy), and future studies should also examine those.
Pediatric OCD Sample.
Exposures for OCD and therapist behaviors therein might differ from those for other disorders. However, they are likely to be similar; constructs targeted in OCD exposures are also relevant for other anxiety disorders (e.g., disgust in phobias, intolerance of uncertainty in GAD), and the theory of exposure mechanism is shared across disorders. Our sample included youth age 5–17; optimal therapist behaviors could differ for adults. Future studies should examine therapist behaviors over a range of disorders and into adulthood.
Secondary Data Analysis.
This study used data from previous clinical trials, which were not designed to explain outcome variability in a single treatment. As a result, some recordings were missing and not all trial participants or exposures are included in this sample. However, our goal was to examine therapist behaviors in relation to habituation and clinical outcomes rather than to account for results of the original trials. Additionally, some youth in this sample received medication. We did not test the role of medication because its use differed substantially across trials (along with other factors such as age and history of partial or non-response to medication) and it would be difficult to draw meaningful conclusions from any findings. Medication could conceivably enhance or interfere with exposure process; combined treatment with medication has benefit over CBT alone (Freeman et al., 2019), though anxiolytic medications could theoretically interfere with exposure learning (e.g., Otto, McHugh & Kantak, 2010). Finally, two therapist behaviors (addressing parent accommodation and using relaxation) occurred infrequently in this sample and could not be analyzed. Relaxation is among the most common techniques used to treat anxiety or OCD in practice (Higa-McMillan et al., 2016) but was not emphasized in POTS manuals and was explicitly proscribed in POTS Jr because relaxation was a comparison condition. Future studies will need to test these behaviors in other samples.
POTS trials were not powered to isolate variance at each of many nested data levels, and the available sample size across these levels precluded some analyses. We examined exposure- and patient-level relationships in a series of separate analyses because it was conceptually consistent with our goals, but future studies should be prospectively designed and adequately powered to isolate these effects. Studies should test whether therapist behaviors, habituation, or exposure frequency changes over a course of treatment, and whether those changes relate to outcomes. Studies should also explore predictors of therapist behavior at different levels. For example, it seems likely that patient characteristics (e.g., symptom severity) will influence therapist behaviors. However, such effects would not preclude the existence of a causal relationship between therapist behaviors and patient outcomes. As a hypothetical example, it might be true that encouraging approach during exposure produces better outcomes, and that it is more challenging for therapists to do so when patient symptoms are severe. In this case, therapist behavior could be one pathway through which higher symptom severity leads to attenuated outcomes. Experimental methods will be the only way to determine whether a therapist behavior causes a change in patient outcomes and future studies should be designed for this purpose. Present limitations notwithstanding, studies that examine factors associated with outcome variability in a single treatment are an important step toward generating ways to improve the effectiveness of empirically supported treatments (Kazdin & Nock, 2003), and—at present—prospectively designed studies for this purpose are rare.
Supplementary Material
Highlights.
Therapist behaviors relate to clinical outcomes in exposure therapy
Therapist behavior should be considered in relation to patient fear during exposure
Future studies should determine whether therapist behavior changes patient outcomes
Funding:
This work was supported by the National Institutes of Mental Health [R21MH096828 and R33 MH096828]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramowitz JS, Deacon BJ, & Whiteside SPH (2011). Exposure therapy for anxiety: Principles and practice. New York, NY: Guilford Press. [Google Scholar]
- Benito KG, Conelea C, Garcia AM, & Freeman JB (2012). CBT specific process in exposure-based treatments: Initial examination in a pediatric OCD sample. Journal of Obsessive-Compulsive and Related Disorders, 1(2), 77–84. 10.1016/j.jocrd.2012.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benito K, Machan J, Freeman J, Garcia A, Walther M, Frank H, Wellen B, Stewart E, Edmunds J, Kemp J, Sapyta J, & Franklin M(2018). Measuring fear change within exposures: Functionally-defined habituation predicts outcome in three randomized controlled trials for pediatric OCD. Journal of Consulting and Clinical Psychology, 86(7), 615–630. 10.1037/ccp0000315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu BC, Colognori DB, Yang G, Xie M-G, Lindsey Bergman R, & Piacentini J (2015). Mediators of exposure therapy for youth obsessive-compulsive disorder: Specificity and temporal sequence of client and treatment factors. Behavior Therapy, 46(3), 395–408. 10.1016/j.beth.2015.01.003 [DOI] [PubMed] [Google Scholar]
- Craske MG, Hermans D, & Vervliet B (2018). State-of-the-art and future directions for extinction as a translational model for fear and anxiety. Philosophical Transactions of the Royal Society B: Biological Sciences, 373(1742), 20170025. 10.1098/rstb.2017.0025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford EF, Wolf GK, Kretzmer T, Dillon K, Thors C, & Vanderploeg R (2017). Patient, therapist, and system factors influencing the effectiveness of prolonged exposure for veterans with comorbid posttraumatic stress disorder and traumatic brain injury. Nervous and Mental Disease, 205(2), 140–146. 10.1097/NMD.0000000000000594 [DOI] [PubMed] [Google Scholar]
- Deacon B, Kemp J, Dixon L, Sy J, Farrell N, & Zhang A (2013). Maximizing the efficacy of interoceptive exposure by optimizing inhibitory learning: A randomized controlled trial. Behaviour Research and Therapy, 51(9), 588–596. 10.1016/j.brat.2013.06.006 [DOI] [PubMed] [Google Scholar]
- Delgadillo J, de Jong K, Lucock M, Lutz W, Rubel J, Gilbody S, Ali S, Aguirre E, Appleton M, Nevin J, O’Hayon H, Patel U, Sainty A, Spencer P, & McMillan D (2018). Feedback-informed treatment versus usual psychological treatment for depression and anxiety: A multisite, open-label, cluster randomised controlled trial. The Lancet. Psychiatry, 5(7), 564–572. 10.1016/S2215-0366(18)30162-7 [DOI] [PubMed] [Google Scholar]
- Eyberg S (2005). Tailoring and adapting parent-child interaction therapy to new populations. Education & Treatment of Children, 28(2), 197–201. [Google Scholar]
- Fairchild AJ, & McDaniel HL (2017). Best (but oft-forgotten) practices: Mediation analysis. The American Journal of Clinical Nutrition, 105(6),1259–1271. 10.3945/ajcn.117.152546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin ME, Sapyta J, Freeman JB, Khanna M, Compton S, Almirall D, Moore P, Choate-Summers M, Garcia A, Edson AL, Foa EB, & March JS(2011). Cognitive behavior therapy augmentation of pharmacotherapy in pediatric obsessive-compulsive disorder: The Pediatric OCD Treatment Study II (POTS II) randomized controlled trial. JAMA, 306(11),1224–1232. 10.1001/jama.2011.1344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman J, Benito K, Herren J, Kemp J, Sung J, Georgiadis C, Arora A, Walther M, & Garcia A (2018). Evidence base update of psychosocial treatments for pediatric obsessive-compulsive disorder: Evaluating, improving, and transporting what works. Journal of Clinical Child and Adolescent Psychology, 47(5), 669–698. 10.1080/15374416.2018.149644 [DOI] [PubMed] [Google Scholar]
- Freeman J, & Garcia A (2008) Family based treatment for young children with OCD: Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Freeman J, Sapyta J, Garcia A, Compton S, Khanna M, Flessner C, FitzGerald D, Mauro C, Dingfelder R, Benito K, Harrison J, Curry J, Foa E, March J, Moore P, & Franklin M (2014). Family-based treatment of early childhood obsessive-compulsive disorder: The Pediatric Obsessive-Compulsive Disorder Treatment Study for Young Children (POTS Jr) –A randomized clinical trial. JAMA Psychiatry, 71(6), 689–698. 10.1001/jamapsychiatry.2014.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia A (2017). Exposure tasks in anxiety treatment: A black box that still needs unpacking. Journal of the American Academy of Child and Adolescent Psychiatry, 56(12), 1010–1011. 10.1016/j.jaac.2017.09.432 [DOI] [PubMed] [Google Scholar]
- Guy W (1976). ECDEU Assessment Manual for Psychopharmacology (pp. 217–222). Rockville, MD: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs in Rockville, MD. [Google Scholar]
- Hedtke KA, Kendall PC, & Tiwari S (2009). Safety-seeking and coping behavior during exposure tasks with anxious youth. Journal of Clinical Child and Adolescent Psychology, 38(1), 1–15. 10.1080/15374410802581055 [DOI] [PubMed] [Google Scholar]
- Higa-McMillan CK, Francis SE, Rith-Najarian L, & Chorpita BF (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child and Adolescent Psychology, 45(2), 91–113. 10.1080/15374416.2015.1046177 [DOI] [PubMed] [Google Scholar]
- Himle MB (2015). Let truth be thy aim, not victory: Comment on theory-based exposure process. Journal of Obsessive Compulsive and Related Disorders,6, 183–190. 10.1016/j.jocrd.2015.03.001 [DOI] [Google Scholar]
- Huppert JD, Bufka LF, Barlow DH, Gorman JM, Shear MK, & Woods SW (2001). Therapists, therapist variables, and cognitive-behavioral therapy outcome in a multicenter trial for panic disorder. Journal of Consulting and Clinical Psychology, 69(5), 747–755. 10.1037/0022-006X.69.5.747 [DOI] [PubMed] [Google Scholar]
- Jacoby RJ, & Abramowitz JS (2016). Inhibitory learning approaches to exposure therapy: A critical review and translation to obsessive-compulsive disorder. Clinical Psychology Review, 49, 28–40. 10.1016/j.cpr.2016.07.001 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Nock MK (2003). Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 44(8), 1116–1129. 10.1111/1469-7610.00195 [DOI] [PubMed] [Google Scholar]
- Kendall PC, Comer JS, Marker CD, Creed TA, Puliafico AC, Hughes AA, Martin ED, Suveg C, & Hudson J (2009). In-session exposure tasks and therapeutic alliance across the treatment of childhood anxiety disorders. Journal of Consulting and Clinical Psychology, 77(3), 517–525. 10.1037/a0013686 [DOI] [PubMed] [Google Scholar]
- Kircanski K, & Peris TS (2015). Exposure and response prevention process predicts treatment outcome in youth with OCD. Journal of Abnormal Child Psychology, 43(3), 543–552. 10.1007/s10802-014-9917-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebowitz E, Panza K, & Bloch M (2016). Family accommodation in obsessive-compulsive and anxiety disorders: A five-year update. Expert Review of Neurotherapeutics, 16(1), 45–53. 10.1586/14737175.2016.1126181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104. 10.1037/1082-989X.7.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99. 10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, & Mulle K (1998). OCD in children and adolescents: A cognitive-behavioral treatment manual. New York, NY: Guilford Press. [Google Scholar]
- McLeod B, Southam-Gerow M, Jensen-Doss A, Hogue A, Kendall P, & Weisz J (2017). Benchmarking treatment adherence and therapist competence in individual cognitive-behavioral treatment for youth anxiety disorders. Journal of Clinical Child and Adolescent Psychology, 1–13. 10.1080/15374416.2017.1381914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noldus LPJJ (1991). The Observer: A software system for collection and analysis of observational data. Behavior Research Methods, Instruments, & Computers: A Journal of the Psychonomic Society, Inc, 23(3), 415–429. 10.3758/BF03203406 [DOI] [PubMed] [Google Scholar]
- Otto MW, McHugh RK, & Kantak KM (2010). Combined pharmacotherapy and cognitive-behavioral therapy for anxiety disorders: Medication effects, glucocorticoids, and attenuated treatment outcomes. Clinical Psychology: Science and Practice, 17(2), 91–103. 10.1111/j.1468-2850.2010.01198.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pediatric OCD Treatment Study (POTS) Team. (2004). Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: The Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA, 292(16), 1969–1976. 10.1001/jama.292.16.1969 [DOI] [PubMed] [Google Scholar]
- Peris T, Caporino N, O’Rourke S, Kendall PC, Walkup JT, Albano A, Bergman RL, McCracken JT, Birmaher B, Ginsburg GS, Sakolsky D, Piacentini J, & Compton SN (2017). Therapist-reported features of exposure tasks that predict differential treatment outcomes for youth with anxiety. Journal of the American Academy of Child & Adolescent Psychiatry, 56(12), 2043–1052. 10.1016/j.jaac.2017.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris T, Rozenman M, Sugar C, McCracken J, & Piacentini J (2017). Targeted family intervention for complex cases of pediatric obsessive-compulsive disorder: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 56(12), 1034–1042. 10.1016/j.jaac.2017.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podell JL, Kendall PC, Gosch EA, Compton SN, March JS, Albano A-M, Rynn MA, Walkup JT, Sherrill JT, Ginsburg GS, Keeton CP, Birmaher B, & Piacentini JC (2013). Therapist factors and outcomes in CBT for anxiety in youth. Professional Psychology, Research and Practice, 44(2), 89–98. 10.1037/a0031700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute, Cary NC. (2003). 9.4 [Computer Program]. Sas, S; Version, S T A T.
- Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Cicchetti D, & Leckman JF (1997). Children’s Yale-Brown Obsessive Compulsive Scale: Reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 36(6), 844–852. 10.1097/00004583-199706000-00023 [DOI] [PubMed] [Google Scholar]
- Senn J, & Radomsky A (2018). Too little, too much, or just right? Does the amount of distraction make a difference during contamination-related exposure? Journal of Behavior Therapy and Experimental Psychiatry, 59, 1–11. 10.1016/j.jbtep.2017.10.004 [DOI] [PubMed] [Google Scholar]
- Strauss A, Huppert J, Simpson H, & Foa E (2018). What matters more? Common or specific factors in cognitive behavioral therapy for OCD: Therapeutic alliance and expectations as predictors of treatment outcome. Behaviour Research and Therapy, 105, 43–51. 10.1016/j.brat.2018.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suen HK, & Ary D (2014). Analyzing quantitative behavioral observation data. New York, NY: Psychology Press. [Google Scholar]
- Weisz JR, Kuppens S, Eckshtain D, Ugueto AM, Hawley KM, & Jensen-Doss A (2013). Performance of evidence-based youth psychotherapies compared with usual clinical care: A multilevel meta-analysis. JAMA Psychiatry, 70(7), 750–761. 10.1001/jamapsychiatry.2013.1176 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


