Abstract
Multidrug resistance (MDR) can be a serious complication for the treatment of cancer as well as for microbial and parasitic infections. Dysregulated overexpression of several members of the ATP-binding cassette transporter families have been intimately linked to MDR phenomena. Three paradigm ABC transporter members, ABCB1 (P-gp), ABCC1 (MRP1) and ABCG2 (BCRP) appear to act as brothers in arms in promoting or causing MDR in a variety of therapeutic cancer settings. However, their molecular mechanisms of action, the basis for their broad and overlapping substrate selectivity, remains ill-posed. The rapidly increasing numbers of high-resolution atomic structures from X-ray crystallography or cryo-EM of mammalian ABC multidrug transporters initiated a new era towards a better understanding of structure–function relationships, and for the dynamics and mechanisms driving their transport cycles. In addition, the atomic structures offered new evolutionary perspectives in cases where transport systems have been structurally conserved from bacteria to humans, including the pleiotropic drug resistance (PDR) family in fungal pathogens for which high resolution structures are as yet unavailable. In this review, we will focus the discussion on comparative mechanisms of mammalian ABCG and fungal PDR transporters, owing to their close evolutionary relationships. In fact, the atomic structures of ABCG2 offer excellent models for a better understanding of fungal PDR transporters. Based on comparative structural models of ABCG transporters and fungal PDRs, we propose closely related or even conserved catalytic cycles, thus offering new therapeutic perspectives for preventing MDR in infectious disease settings.
Keywords: yeast, multidrug transporter, anticancer, antifungal resistance, ABC transporters, mechanism
1. Introduction
1.1. ABC Transporters and Clinical Relevance of MDR
The ATP-binding cassette (ABC) transporter family is one of the largest protein superfamilies present in all living organisms, from prokaryotes to eukaryotes [1,2,3,4,5]. ABC transporters can operate as exporters or importers in an ATP-dependent manner, and mediate the membrane translocation of bewildering substrate spectra against concentration gradients [6,7,8]. In addition, ABC proteins can function as ion channels, channel regulators, receptors, proteases, protein sensors or are even involved in mRNA translation and ribosome biogenesis [9,10,11]. Remarkably, conserved architectures offer specific yet broad substrate-binding regions and somehow form a translocation path that operates in a unidirectional way in eukaryotes. The wide substrate range includes cationic anticancer drugs, antifungal drugs, steroids, phospholipids, bile acids, antibiotics, peptides, ions, heavy metals, carbohydrates and glucocorticoids, as well as toxins [12,13,14,15]. The hallmark domain organization of ABC transporters entails four core units, two evolutionarily conserved nucleotide-binding domains (NBDs) and two transmembrane-spanning domains (TMDs), typically consisting of twelve hydrophobic transmembrane-spanning helices (TMHs). These four domains are normally arranged as a full-transporter in a single protein as TMD1–NBD1–TMD2–NBD2 or in a reverse configuration NBD1–TMD1–NBD2–TMD2. Alternatively, half-transporters come in NBD–TMD or TMD–NBD arrangements, which require at least homo- or hetero-dimerization for a functional complex [16,17,18,19]. In addition, some members contain additional domains or motifs such as the TMD0 domain or the R-domain regulatory motif [8,20,21].
The NBD is a universally conserved domain that consumes ATP and somehow fuels the dynamic switch of the transporter structure from an inward substrate-binding state to an outward substrate-releasing conformation. The catalytic cycle drives the conformational switch at the TMD and enables the substrate translocation through an as yet elusive transport pathway [22,23]. The TMDs are more diverse in sequence and show much less conservation, but clearly are essential for forming putative substrate translocation pores. They must handle a broad spectrum of chemically diverse substrates and inhibitors [24,25]. Notably, the communication between NBD and TMD and the dynamics underlying the entire transport cycle of ABC transporters remain unclear. While certain elements or stages of the transport cycles may be conserved among subfamilies, the expanding number of atomic structures and the resulting mechanistic information for distinct ABC transporters make unifying mechanisms less likely, challenging earlier notions about a unified catalytic cycle [8,16,17,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. No matter what the actual catalytic cycle or mechanism of a given type I or type II exporter may be, a tantalizing possibility is that a basic conserved mechanism operates for PDR and ABCG, but slightly different transport mechanisms could be a consequence of the nature of substrates that would distinctly affect the kinetics and dynamics of the cycle.
The human ABC transporter family of 48 genes served to categorize subfamilies into the ABCA to ABCG nomenclature [46,47,48], although the surge of recent atomic structures and functional considerations made it clear that a new and improved nomenclature based on structure–function relationships is needed [43]. Remarkably, inborn errors of several human ABC transporters lead to prominent genetic diseases [49], including cystic fibrosis (ABCC7 or CFTR) [50,51], hepatic cholestasis (ABCB11 or BSEP) [52,53], plant sterol sitosterolemia (ABCG5/G8) [54,55,56,57], neonatal hyperinsulinemic hypoglycemia or non-insulin-dependent childhood diabetes (ABCC8) [58], gout (ABCG2 or BCRP) [59], Dubin–Johnson syndrome (ABCC2 or MRP2) [60,61] and Stargardt’s macular dystrophies and retinophathies (ABCA4) [62], peroxisomal adrenoleukodystrophy or ALD (ABCD1) [63,64,65], immune deficiency—class I MHC antigen presentation (ABCB2/B3, TAP) [66,67,68], cholesterol transport and HDL assembly or Tangier’s disease (ABCA1, ABCG1) [69,70,71,72,73,74,75], pseudoxanthoma elasticum or PXE (ABCC6) [76,77,78,79,80,81,82], dilated cardiomyopathy (ABCC9) [83], defective earwax synthesis (ABCC11) [84,85], lung surfactant deficiency (ABCA3) [86,87,88,89], lamella and harlequin ichthyosis (ABCA12) [90,91,92], pregnancy-related cholestasis (ABCB4) [93,94] and sideroblastic anemia (ABCB7) [95,96,97,98].
1.2. Mammalian ABC Multidrug Transporters
Most, if not all, eukaryotic ABC transporters function as unidirectional exporters and use ATP consumption to drive transport. Some have been implicated in uptake processes as well, although this remains controversial [39,99]. Importantly, ectopic or dysregulated overexpression of certain ABC transporters often contributes to or promotes MDR phenomena in several but not all human cancer types [2,10,11,100,101,102]. Based on sequence similarity and domain arrangement, mammalian ABCs fall into two major groups, referred to as type I and type II exporters [12], although recently, a new classification has been proposed [18]. At least three MDR exporters have been linked to MDR in human tumors, including P-glycoprotein (P-gp/MDR1/ABCB1) [103,104,105,106], MRP1 (MDR-associated protein 1/ABCC1) [107] and BCRP (Breast Cancer Resistance/ABCG2) [108,109,110]. All three share rather broad and partially overlapping drug specificity [14,111]. Most substrates of ABCB1 and ABCG2 are cationic hydrophobic compounds [112], which may probably be expelled directly from the lipid phase as originally proposed by the “hydrophobic vacuum cleaner” model [105,113,114] or from the outer membrane leaflet by a floppase-like function [5,14,19,109,111,115,116]. A similar mechanism has been proposed in ABCA1 for the cholesterol loading of apolipoprotein A-I (apoA-I) [5,116,117]. P-gp, MRP1 and ABCG2 are normally residing in the plasma membrane of epithelial organ linings (such as liver, intestine, blood–brain barrier, placenta and mammary epithelium) [118,119]. Their physiological tasks include vital roles in cellular detoxification and in organ protection by excretion of toxic compounds or xenobiotic molecules [120]. Substrates are amphipathic, lipid-soluble compounds of extremely diverse chemical spaces, ranging from small molecules to bulky lipophilic cations and conjugated organic anions [14,112,121].
ABCB1 or P-glycoprotein (P-gp) or MDR1 (encoded by the MDR1 gene) was identified from a multidrug-resistant KB carcinoma cell line [103,122,123] as the first mammalian type I exporter class. P-gp is expressed on apical membranes of epithelial cells in colon, small intestine, liver, placenta, kidney, gut, pancreatic, bile duct and blood–brain barrier [124,125]. Homozygous P-gp knock-out mice showed a 100-fold increase in drug (ivormectin) permeability at the blood–brain barrier, which led to the discovery of its physiological role in organ protection [126,127,128]. ABCB1 transports a diverse array of substances, including chemotherapeutic drugs, steroids, several phospholipids, fluorescent dyes, peptides and ionophores [113]. Furthermore, ABCB1 is believed to function as a floppase-like lipid transporter [43,129]. Despite huge therapeutic promises, numerous clinical studies on ABCB1 inhibitors or reversal agents [130,131,132,133,134,135,136,137,138] showed marginal to no benefits, thus rendering attempts to translate P-gp inhibitors into the clinic so far futile efforts [111,139]. Of note, despite an almost highly conserved primary sequence identity, the closest P-gp homologue, ABCB4/MDR2, has not been implicated in drug transport or cancer MDR [140], as it resides in the canalicular and appears to have a restricted substrate spectrum limited to phosphatidycholine-related phospholipids in the canalicular membrane.
ABCC1 or MRP1 or multidrug resistance-associated protein1 (encoded by the ABCC1 gene) was discovered as the second member of MDR exporters, cloned from a multidrug-resistant P-gp-negative human lung cancer cell line with doxorubicin tolerance [107]. ABCC1 is mostly on the basolateral surface of polarized epithelial cells, with moderate to high abundance in the gastrointestinal tract, kidney, bladder, testis, ovary, endometrium, adipose tissues, appendix and tonsils. Low-level expression is found in brain, lung, liver, gall bladder, pancreas, bone marrow and skin [141,142,143] to excrete a variety of endogenous substances, including glutathione, prostaglandins, C4-leukotrienes glucuronide conjugates, sulfate conjugates, heavy metal oxyanions and, most importantly, conjugated metabolites of otherwise hydrophobic compounds [14,112,144,145].
ABCG2 or BCRP or Breast Cancer Resistance Protein (encoded by the ABCG2 gene) was originally isolated from P-gp-negative multidrug-resistance breast cancer cell lines [109,110]. ABCG2 homes to the apical membranes in many epithelial cells and tissues, including lung, gut, intestine, liver, breast, placenta, hematopoietic stem cells and especially in the blood–brain barrier [109,110,119,146]. ABCG2 is a half-transporter carrying a TMD at the C-terminus, requiring homo-dimerization to form a full functional molecule. ABCG2 is overexpressed in many solid tumors as well as acute myeloid leukemia (AML) and acute lymphocytic leukemia (ALL). Dysregulated ABCG2 overexpression is linked with poor prognosis in several cancer types [139,147], with particularly low survival in AML patients [134,137,148,149,150,151]. Like P-gp, ABCG2, as well as PDRs such as Yor1, Pdr5, Cdr1 or Snq2, show extremely broad substrate specificity (Table 1), all in all transporting hundreds of diverse compounds, including dietary xenobiotics, toxins, metabolites, vitamins, lipids, steroids, antibiotics and antifungal as well as anticancer drugs [152,153,154,155]. Of note, the many exceptions seen for each transporter make a generalization of substrate preferences for a given ABCG or PDR transporter challenging without experimental evidence. Remarkably, however, despite their pronounced structural conservation, additional ABCG family members such as ABCG1, ABCG4 and the heterodimeric ABCG5/G8 transporter have not been associated with MDR phenotypes in cancer [15,115,156,157,158,159,160,161,162].
Table 1.
Known ABC transporters in non-pathogenic yeasts.
| Phylogeny | Species | Gene Name | UniProt ID | Length | Substrates | References | |
|---|---|---|---|---|---|---|---|
| Exporter type II | ABCG/PDR | S. cerevisiae | PDR5 | P33302 | 1511 | Drugs, PC, PE, PS, Steroids, Herbicides | [163,164,165,166,167,168,169,170,171,172] |
| PDR10 | P51533 | 1564 | Regulate PDR12 trafficking, Herbicides, Lipids | [173,174,175] | |||
| PDR11 | P40550 | 1411 | Sterol | [99,176] | |||
| PDR12 | Q02785 | 1511 | Weak acids, Fluorescein | [177,178] | |||
| PDR15 | Q04182 | 1529 | Herbicide, Detergent | [174,175,179] | |||
| PDR18 | P53756 | 1333 | Herbicides, Ethanol, Ergosterol | [180,181,182,183] | |||
| AUS1 | Q08409 | 1394 | Sterol | [99,158,184] | |||
| SNQ2 | P32568 | 1501 | Drugs, Steroids, Mutagens, Chemicals | [169,185,186] | |||
| S. pombe | BFR1 | P41820 | 1530 | Brefeldin A, Tributyltin | [187] | ||
| Exporter type I | ABCB/MDR | S. cerevisiae | ATM1 * | P40416 | 690 | Fe/S proteins | [188,189,190] |
| MDL1 * | P33310 | 695 | Peptides | [191,192] | |||
| STE6 | P12866 | 1290 | a-factor | [193,194] | |||
| S. pombe | HMT1 * | Q02592 | 830 | Phytochelatin conjugated Cd2+ | [195,196] | ||
| MAM1 | P78966 | 1336 | M-factor | [195,196] | |||
| ABCC/MRP | S. cerevisiae | YOR1 | P53049 | 1477 | Oligomycin, Reveromycin, Beavericin, Metal ions | [197] | |
| YCF1 * | P39109 | 1515 | GS-conjug. Cd2+, Metals | [170,198,199,200] | |||
| YBT1 * | P32386 | 1661 | Metal ions, Bile acid, PC | [201,202] | |||
| VMR1 * | P38735 | 1592 | Drugs, Metal ions | [203] | |||
| BPT1 * | P14772 | 1559 | Metal ions, Bile acid, GS-conjugates | [204] | |||
| S. pombe | PMD1 | P36619 | 1362 | Drugs | [205] |
* All transporters located in the plasma membrane, except for Atm1, Mlt1 and Ybt1, Vmr1, Ycf1 and Hmt1, residing in the mitochondrial and vacuolar membrane. GS: glutathione, PC: phosphatidylcholine, PE: phosphatidylethanolamine, PS: phosphatidylserine.
Collectively, P-gp, MRP1 and ABCG2 act as brothers in arms to ensure the physiological detoxification of endogenous metabolites as well as exogenous xenobiotics across most epithelial barriers, including placenta, testis, mammary epithelium, liver and GI tract as well as the blood–brain barrier [119,139,146,152,206]. However, how, and sometimes even if, they actually cause clinical MDR in cancer has remained a highly controversial issue, often subject to intense discussions in the field [102,207]. As for microbial anti-infective MDR, it has been generally accepted though that bacterial ABC transporters [208,209,210,211,212] and fungal PDR transporters [124,213,214,215,216] are key causes for clinical MDR, often setting an unsurmountable roadblock in antimicrobial treatments [10,101,217,218,219].
1.3. ABC Multidrug Transporters in Fungal Kingdoms
Invasive fungal diseases account for ~1.5 million deaths per year worldwide [220,221]. The increasing numbers of immunosuppressed people, including the elderly, transplant recipients, cancer and HIV/AIDS patients will most likely increase future cases of infections by opportunistic pathogens like Candida species (spp.) [222]. Candida spp. are commensal colonizers and part of the microflora present on mucosal and epithelial barriers such as the gastrointestinal and urogenital tracts. Candida spp. are a major part of the physiological mycobiome species [223], along with several thousand bacterial species constituting tissue-specific microbiomes [224,225,226,227,228,229]. Several Candida spp. can cause life-threatening invasive systemic disease in severely immunocompromised individuals [230]. The small number of chemical entities in antifungal drugs have been very problematic in the past, especially after prolonged use or after extensive prophylaxis, as was the case for pronounced azole resistance in HIV patients. Hence, the propensity to develop MDR is lower when larger drug arsenals against different targets are available [231]. For example, C. auris is a newly emerging pan-resistant fungal pathogen first reported from an ear infection in Japan in 2009 [232]. Within a decade, C. auris appeared in more than 40 countries around the globe, causing hospital outbreaks of invasive candidemia [233,234,235,236,237,238,239,240]. Importantly, C. auris is also causing severe superinfections with viruses, as seen in a recent co-infection of COVID-19 patients in a Mexican hospital ICU, leading to a dramatic overall mortality of 83%. In fact, intrinsic MDR in other Candida spp. such as C. glabrata and C. kruzei have also been increasing over the last decade [230,241,242]. Importantly, among other mechanisms, such as drug target gene mutations [243,244], efflux-based MDR/PDR has been recognized as a major cause of fungal anti-infective drug resistance [219,235,244,245,246,247].
Fungal ABC proteins are also quite diverse and are implicated in many biological functions, contributing to pivotal cellular processes, including cellular detoxification and stress adaptation [214,248,249]. Owing to space constraints, we will limit our discussion to paradigm fungal PDR family members implicated in drug resistance phenomena, but refer the reader to numerous recent reviews discussing fungal ABC proteins at large [249,250]. Fungal ABC proteins of the PDR subfamily are the closest eukaryotic orthologues of human ABCG family exporters [245,251]. For instance, C. albicans and C. glabrata harbor 27 and 18 ABC proteins in total, respectively [250]. Interestingly, Cryptococcus neoformans and Aspergillus fumigatus harbor even larger numbers, with 54 and 49 ABC transporters, respectively [252,253]. While we are not discussing transporters which are not linked to MDR phenomena, we still provide a comprehensive list of all known ABC transporters in non-pathogenic yeasts (Table 1) and their phylogenetic relationships (Figure 1A). MRP-like yeast ABC transporters including Yor1, Ycf1, Ybt1, Vmr1 and Bpt1 mediate vacuolar detoxification and heavy metal resistance [214]. Of note, Ycf1, which also has a rudimentary R-domain motif as present in human CFTR [50], was the first yeast homologue of mammalian MRP [254], while pathogenic fungi such as C. albicans harbor only Yor1 and Mlt1 (Table 2).
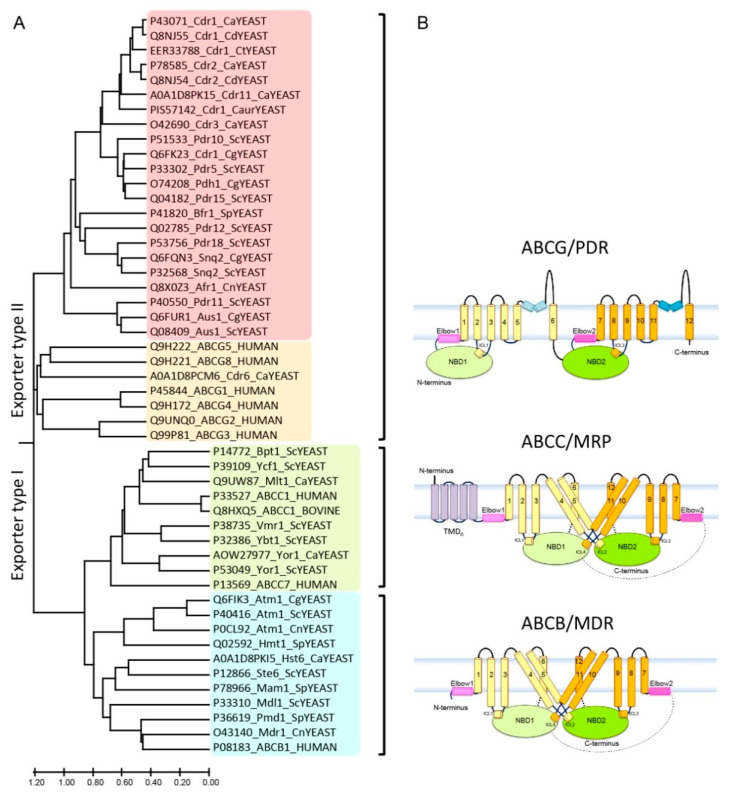
Figure 1.
Phylogeny and structural organization of ABC transporters in mammals and yeast. (A) The phylogenetic tree shows the evolutionary relationships of ABC transporter subfamilies in yeast and mammals. Some 29 ABC transporters were subjected to amino acid sequence alignments. Branch length was analyzed using MEGA-X, and represents the evolutionary distance in the units of the number of amino acid substitutions per site. Names are given in the UniProt code, protein name and organism, respectively. The analysis reveals two major exporters subfamilies referred to as type I and II. Type I was sub-classified into ABCB/MDR (blue) and ABCC/MRP (green) subgroups. The type II family represents ABCG/PDR subgroups with the fungal (red) and mammalian transporters (orange). Ca: Candida albicans, Cg: Candida glabrata, Caur: Candida auris, Cd: Candida dubliniensis, Ct: Candida tropicalis, Cn: Cryptococcus neoformans, Sc: Saccharomyces cerevisiae, Sp: Schizosaccharomyces pombe. (B) Predicted membrane topologies of three MDR ABC exporter families. The transporters hold several diagnostic hallmark domains, including two NBDs (NBD1: light green; NBD2: green), two TMD regions usually with 6 putative membrane-spanning helices each (TMD1: light yellow; TMD2: bright orange), elbow helix (pink), re-entry helix (blue) and TMD0 (purple), respectively.
Table 2.
ABC efflux transporters mediating MDR in pathogenic fungi.
| Phylogeny | Species | Gene | UniProt ID | Length | Substrates | References | |
|---|---|---|---|---|---|---|---|
| Exporter type II | ABCG/PDR | C. albicans | CDR1 | P43071 | 1501 | Drugs, PC, PE, PS, Steroids | [217,260,263,267,268,269,270] |
| CDR2 | P78595 | 1499 | Drugs, PC, PE, PS, Steroids | [218,260,271] | |||
| CDR3 | O42690 | 1501 | Drugs, PC, PE, PS, Steroids | [260,272] | |||
| CDR6/ROA1 | A0A1D8PCM6 | 1274 | Azole, Membrane fluidity | [273] | |||
| CDR11 | A0A1D8PK15 | 1512 | Drugs, Fosmanogepix | [274] | |||
| C. glabrata | CDR1 | Q6FK23 | 1499 | Drugs | [275,276] | ||
| PDH1 | O74208 | 1542 | Drugs | [277,278] | |||
| SNQ2 | Q6FQN3 | 1507 | Drugs | [279] | |||
| AUS1 | Q6FUR1 | 1398 | Sterol | [280,281] | |||
| C. auris | CDR1 | PIS57142 | 1508 | Drugs | [236,237,239] | ||
| C. dubliniensis | CDR1 | Q8NJ55 | 1501 | Drugs | [282] | ||
| CDR2 | Q8NJ54 | 1500 | Drugs | [282] | |||
| C. tropicalis | CDR1 | EER33788 | 1498 | Drugs | [283,284,285] | ||
| C. neoformans | AFR1 | Q8X0Z3 | 1543 | Drugs | [286] | ||
| Exporter type I | ABCB/MDR | C. albicans | HST6 | A0A1D8PKI5 | 1323 | A-factor | [287,288] |
| C. glabrata | ATM1 * | Q6FIK3 | 727 | Fe/S | [289] | ||
| C. neoformans | MDR1 | O43140 | 1408 | Drugs | [290] | ||
| ATM1 * | P0CL92 | 734 | Fe/S | [290] | |||
| ABCC/MRP | C. albicans | YOR1 | AOW27977 | 1488 | Oligomycin, Beauvericin | [291,292] | |
| MLT1 * | Q9UW87 | 1606 | PC, Ni(II) | [180] |
* All transporters located in the plasma membrane, except for Atm1 and Mlt1, residing in the mitochondrial and vacuolar membrane, respectively. GS: glutathione, PC: phosphatidylcholine, PE: phosphatidylethanolamine, PS: phosphatidylserine.
The fungal PDR (ABCG) or pleiotropic drug resistance family is the largest subfamily of ABC transporters of the type II exporter class [251]. PDR transporters are the closest structural orthologues of all mammalian ABCG subfamily transporters (Figure 1A), sharing the same topological orientation and domain arrangements with mammalian ABCG5/ABCG8 [255] and ABCG2 [256,257,258,259] (Supplementary Figure S1). PDR transporters in fungal pathogens implicated in clinical antifungal resistance in C. albicans include Cdr1, Cdr2, Cdr3, Cdr6 and Cdr11, in C. glabrata (Cdr1, Pdh1, Snq2 and Aus1) [260], in C. auris (Cdr1), in C. tropicalis (Cdr1), in C. dubliniensis (Cdr1 and Cdr2) and in Cryptococcus neoformans (Afr1) (Table 2). All are highly conserved in non-pathogenic yeasts (Table 1). Their overexpression in pathogens causes hallmark MDR phenotypes seen for mammalian or bacterial ABC transporters [111,141,217,218,235,261,262,263,264].
Diversity of fungal PDR transporters and evolutionary relationships to mammalian ABC transporters. Most ABC proteins from non-pathogenic baker’s yeasts (Table 1) are also found in various numbers and functions in pathogenic fungi (Table 2). A phylogenetic tree analysis suggests two major groups, referred to as exporter type I and type II [4,248,265,266], contain three MDR, MRP and PDR subfamilies (Figure 1A). While type I exporters (MDR/ABCB and MRP/ABCC) hold a TMD1–NBD1–TMD2–NBD2 configuration, all PDR/ABCG type II exporters adopt a “reverse” architecture, such as NBD1–TMD1–NBD2–TMD2 (Figure 1B). By contrast with the mammalian ABCG subfamily, all fungal PDR proteins are full-size transporters (Figure 1B).
2. Atomic Structures of Eukaryotic Multidrug ABC Efflux Exporters
Several high-resolution structures, obtained through X-ray crystallography or cryo-EM approaches in the past five years, provided a better understanding of the structure–function relationships of mammalian type I and type II exporters (Table 3). However, despite ever-increasing structural information, the path from static atomic structures to precise molecular mechanisms has turned out to be a rocky road for scientists and drug discovery. Thus, we are still far from understanding the conformational dynamics as well as the mechanics driving their transport cycles. Each half-molecule of ABCB and ABCC type I exporters harbor at least six transmembrane helices that extend into the intracellular loops linked to their coupling helices, thus connecting to both the proximal NBD and crossing over to the distal NBD [8,31,39,293,294,295,296]. In the ATP-free apo state, if it ever exists inside cells, these exporters maintain an inward-facing configuration, whereby both NBDs appear apart to offer access for ATP and possibly substrates (Figure 2A) [297]. Importantly, while the ABCC subfamily shares a highly similar overall fold with ABCB, MRP transporters have an additional N-terminal domain known as TMD0 [20,298,299]. Notably, CFTR also adds the so-called R(egulatory)-domain residing in the core of the channel between the N-terminal and the C-terminal TMDs [21,300,301] (Figure 1B).
Table 3.
Atomic structures of eukaryotic MDR ABC transporters.
| Subfamily | PDB ID | Function | References |
|---|---|---|---|
| ABCB1 (P-gp) | 4F4C, 4M1M, 4M2S, 4M2T, 4Q9H, 4Q9J, 4Q9K, 4Q9L, 4XWK, 5KPF, 6KPI, 5KPJ, 5KO2, 5KOY, 6C0V, 6GDI, 6Q81, 6QEX, 6QEE, 6FN4, 6FN1, 3G5U, 3G60, 3G61 | Multidrug export, detoxification | [255,296,302,303,304,305,306,308,309,310] |
| ABCC1 (MRP1) | 5UJA, 5UJ9, 6BHU, 6UY0 | Multidrug, leukotriene and sphingolipid export, detoxification | [298,312] |
| ABCG2 (BCRP) | 5NJG, 5NJ3, 6ETI, 6FEQ, 6HIJ, 6HCO, 6HBU, 6HZM, 6VXH, 6VXI, 6VXJ | Multidrug export, detoxification and urate transport | [256,257,258,259] |
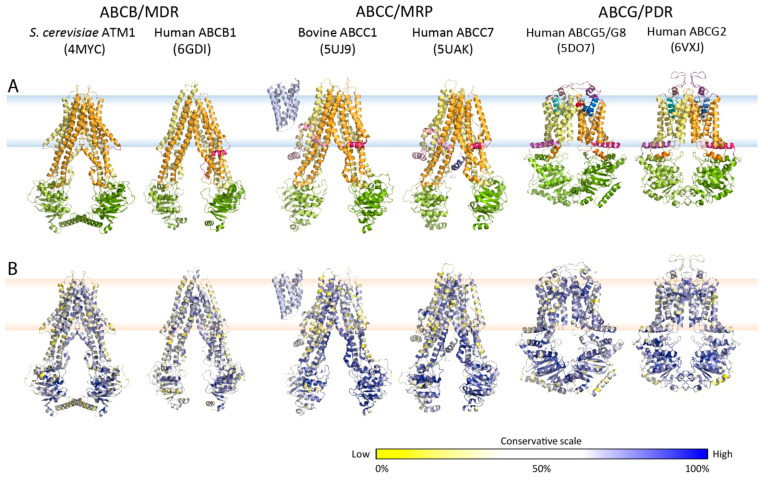
Figure 2.
Atomic structures, folds and evolutionary conservation of MDR exporters. (A) Crystal or cryo-EM particle structures of multidrug resistance-related ABC exporters from the type I (ABCB and ABCC) and type II families (ABCG subfamily) using the color codes as shown in Figure 1B. (B) Conservation analysis of ABC exporters from panel A. Multiple sequence alignments of amino acid sequences from Table 1 and Table 2 were generated for all subfamilies. The degree of conservation was calculated and indicated as a color gradient ranging from low conservation (yellow) to high conservation (blue).
At present, the available atomic structures of type I exporters are as listed in Table 3. For the ABCB1 subfamily, many conformations, including inward-facing, outward-facing, occluded state, substrate-bound, inhibitor-bound and antibody-bound, have been solved, all in all yielding 24 structures in the PDB [296,302,303,304,305,306,307,308,309,310]. For the ABCC subfamily, four cryo-EM structures are available for bovine ABCC1 in the PDB [311,312]. Furthermore, seven structures are available for CFTR [300,301,313,314,315], and 12 structures for ABCC8 or SUR1 [316,317,318,319,320]. Strikingly, the first atomic structure of the heterodimeric ABCG subfamily member ABCG5/G8 came as a surprise, as the X-ray crystals revealed an unexpected compact fold, in which NBDs were located in close proximity to the TMDs. In addition, the molecule held a lid-like structure at the extracellular roof of the translocation pathway. This fold resembled bacterial importers more than a prototypic export pump [38]. This structure paved the way for solving the human ABCG2 transporter, for which now 11 atomic structures are available in the PDB [256,257,258,259] (Table 3).
3. Key Residues and Motifs Are Conserved in Multidrug Transporters ABCG/PDR
The mammalian ABCGs are the closest orthologues of yeast PDR transporters [216,245,250,251,321], especially Pdr5 and Cdr1 [166,322,323] (Supplementary Figure S1). To identify conserved regions of fungal ABC proteins based on mammalian ABC structures, we determined a conservation score for the fungal PDR family, and mapped conserved residues into the atomic structures of mammalian orthologues (Figure 2B). We subjected the fungal ABCG/PDR subfamily to multiple sequence alignments with the mammalian ABCGs (Supplementary Figure S1), showing that NBDs hold several highly conserved motifs related to ATP consumption. Although TMDs are usually more diverse, several regions are also preserved between PDR and ABCG, implying that these domains are pivotal for an evolutionarily related catalytic cycle.
Conservation in the NBD. First, the NBDs in fungal PDRs share highly conserved motifs as well as residues with ABCG required for ATP-binding and hydrolysis [45,153,324,325,326], including Walker A, Q-loop, Hot spot helix, Signature motif, Pro-loop, Walker B, D-loop and H-loop, respectively [327]. The alignment indicates that fungal NBDs adopt a RecA-like structure, an ATPase-containing fold that was first seen in RecA, which is involved in DNA recombination, and was later found in many ATPases [328] (Supplementary Figure S1 and Table 4). There are only minor differences though, as ABCG2 and ABCG5/G8 are half-transporters that require homo- or hetero-dimerization, while all fungal PDRs are full-size transporters, some of which with asymmetric deviant ATP-binding sites (Table 4). In the first NBD of PDR transporters, the glutamine (Q) in the Q-loop is replaced by glutamate (E), the Pro-loop disappeared and histidine (H) in the H-loop is substituted by tyrosine (Y). Hence, the notion emerged that fungal PDRs would follow an asymmetric catalytic cycle [173,216,306,329,330].
Table 4.
The human ABCG2 and fungal Cdr1 multidrug exporters share conserved motifs.
| Location | Conserved Motif | Functional Role | Human ABCG2 | Candida albicans Cdr1 | |
|---|---|---|---|---|---|
| First Half | Second Half | ||||
| NBD | Walker A | ATP hydrolysis (phosphate binding) * | G79–S88 | G187–T195 | G895–T903 |
| Q-loop | TMD–NBD communication | Q126 | E238 ** | Q942 | |
| Hot spot | Triple helical bundle | L134–A149 | L246–P261 | S950–S965 | |
| Signature | NBD dimerization and phosphate binding | V186–R193 | V303–R310 | V996–R1008 | |
| Pro loop | NBD dimerization | P204 | ? | P1019 | |
| Walker B | ATP hydrolysis | I206–E211 | I323–N238 | L1021–E1027 | |
| D-loop | NBD dimerization | L216–D217 | L333–D334 | L1032–D1033 | |
| H-loop | ATP hydrolysis | H243 | Y361 ** | H1059 | |
| Elbow helix | Conserved R | Salt bridge, THB | R383 | R503 | R1185 |
| ECL1 | Conserved R | Salt bridge | R426 | R456 | ? |
| TMH2 | Conserved F | Clamping | F439 | F559 | F1239 |
| ICL1 | Conserved E (1) | Salt bridge and intracellular gating | E451 | E570 | D1255 |
| Conserved E (2) | Salt bridge | E458 | E576 | E1261 | |
| Conserved Y | Salt bridge, THB | Y464 | Y584 | Y1257 | |
| TMH3 | Conserved D/E | Intracellular gating | D477 | E597 | E1280 |
| Valve | Conserved hydrophobic | Valve | G553–L555 | G672–V674 | G1362–L1364 |
| Re-entry helix | Conserved P | Kinked helix | P574 | P692 | P1382 |
| Conserved E | Salt bridge | E585 | E704 | ? | |
| ECL3 | Conserved C (1) | Intra/intermolecular disulfide bond | C592 | C712 | C1418 |
| conserved C (2) | Intra/intermolecular disulfide bond | C603 | ? | C1441 | |
| conserved C (3) | Intra/intermolecular disulfide bond | C608 | C732 | C1444 | |
Conservation in the TMD region. Second, the general architecture and configuration of TMDs are maintained, as each TMD in ABCG/PDR transporters contains six putative membrane-spanning helices, and a rather short first intracellular loop contains the coupling helix. The large ECL is part of the lid architecture in the extracellular region. Interestingly, two putative helices residing at both lipid bilayer leaflets, which are important for function, as they restrict dynamic movements during transport cycle, are only found in the ABCG subfamily [40,42]. The amino acid alignments reveal the consensus sites present in conserved motifs and domains (Figure 1B and Supplementary Figure S1).
The elbow helix is a 15-residue amphipathic helix sharing highly conserved residues among all ABCG/PDR members. This elbow helix is an intrinsic part of the triple helical bundle (THB), which also engages the hot spot helix from the NBD and the coupling helix from the first intracellular loop (ICL1) [332]. Importantly, the center of the elbow helix contains a highly conserved arginine (R), which is essential for a salt bridge interaction with a glutamate (E) residue in ICL1 to stabilize the THB [40].
The transmembrane helix 1 (TMH1) is a prototypic 20-residue membrane-spanning helix, following the elbow helix in all ABCG/PDR exporters. The small extracellular loop 1 (ECL1) is a short linker connecting TMH1 and TMH2 at the cell surface. Notably, ECL1 in the first half holds a conserved arginine (R), which is important for salt bridge formation with a conserved glutamate (E) in the re-entry helix of the same molecule [42]. TMH2 is thought to be a part of the substrate/inhibitor binding zone in human ABCG2 [333]. A conserved phenylalanine (F) in the middle of TMH2 may be a recognition site for both substrates and inhibitors [333].
The intracellular loop 1 (ICL1) spans over 30 residues in the ABCG/PDR subfamily and holds a critical U-turn motif. ICL1 operates as the coupling helix for the NBD–TMD communication by participating in a triple helical bundle (THB). The entire THB functions as a molecular spring that controls the catalytic cycle by regulating the conformational switch. Indeed, two conserved negative residues within ICL1 of human ABCG2, E451 and E585, are thought to control the intracellular gating mechanism and engage in salt bridges with the elbow helix, respectively. Remarkably, ICL1 holds an essential tyrosine residue that is conserved in all ABCG/PDR transporters. This Y464 contributes a salt bridge interaction within the THB complex for stabilization of the transmission interface.
TMH3 also has several conserved residues within the ABCG/PDR group such as negative residues (E or D), proline, as well as positive amino acids (K or R). D477 at the start of TMH3 in human ABCG2 is on top of the transmission interface and may contribute to an intracellular gate. ECL2 is again rather short, containing only eight residues with a kink, connecting TMH3 and TMH4 at the cell surface.
The hydrophobic valve is a kinked domain just after TMH5, consisting of the conserved “glycine-Φ-Φ” (Φ is hydrophobic residue) motif that subtends the extracellular bilayer leaflet. The valve is pivotal for controlling substrate transport through a putative translocation pathway whose precise nature and dynamics remains obscure. The re-entry helix is the counterpart of the elbow helix and is unique, establishing a kinked hallmark motif in the ABCG/PDR subfamily with several conserved residues. In addition, ECL3 is the only large extracellular loop, and a main part of the extracellular roof architecture. Interestingly, ECL3 in human ABCG2 has three cysteines, which form intra- and inter-molecular disulfide formations, and perhaps facilitate dimerization and drug release [334,335]. Likewise, conserved cysteines in fungal PDR transporters may engage in an intra-molecular disulfide bond to stabilize the PDR biogenesis. Finally, TMH6 is followed by a very small but highly conserved C-terminus that contains several positive charges at the C-terminus.
4. C. albicans PDR/Cdr1 Holds All Conserved Motifs Critical for ABCG Function
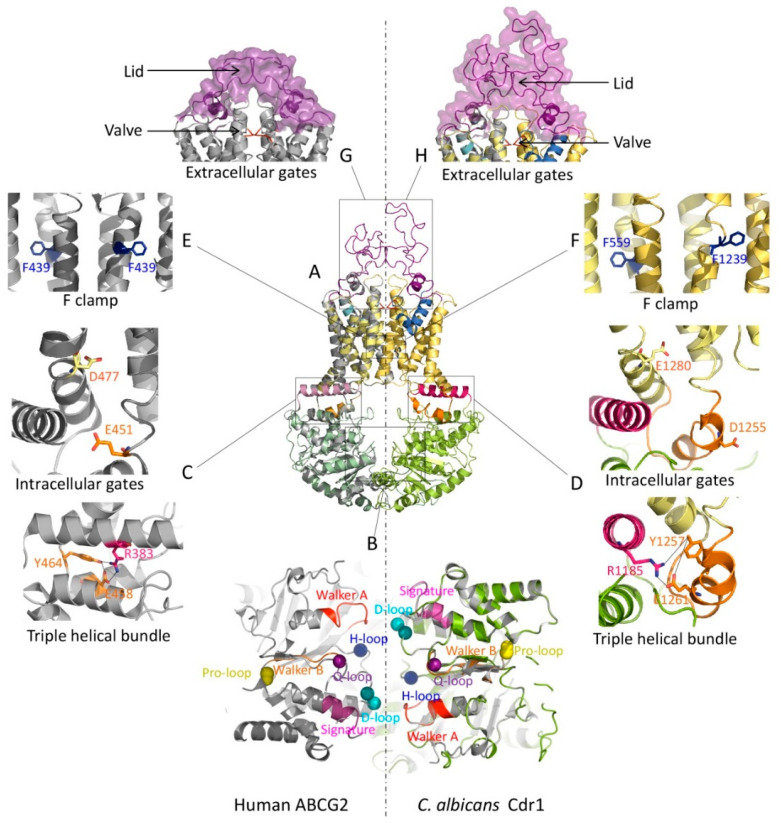
The atomic structures from X-ray crystallography and cryo-EM of mammalian ABCGs suggest a rather unique fold resembling an importer rather than an exporter [38,256,257,258,259]. Indeed, mammalian ABCGs and fungal PDR exporters share conserved and superimposable topologies with all functional motifs in equivalent places (Figure 1A, Figure 2B, Supplementary Figure S1 and Table 4). Hence, we generated homology models of Cdr1 from C. albicans, using human ABCG2 (PDB ID 6VXF) as a template (Figure 3A). Remarkably, the Cdr1 structural model perfectly mirrored the human ABCG2 conformation, since each pivotal motif important for function is also present in Cdr1 (Figure 3).
Figure 3.
Type II mammalian and fungal ABCG/PDR exporters share functional domains. (A) A homology model of the PDR exporter Cdr1 from C. albicans was generated using the SWISS-MODEL tool (color ribbon, NBD: green, TMD: yellow, elbow helix: pink, ICL: orange, valve: red, re-entry helix: blue and ECL: purple). The Cdr1 model was superimposed with the cryo-EM structure of human ABCG2 (PDB ID: 6VXF) (gray ribbon). (B) Zoom-in top view of the NBD dimer from panel A at the NBD–NBD interface shows essential conserved motifs (Walker A: red, Q-loop: violet, signature: pink, Pro-loop: yellow, Walker B: orange, D-loop: cyan and H-loop: blue). The transmission interfaces of human ABCG2 (C) and C. albicans Cdr1 (D) show a network cluster of triple helical bundles (THB) with conserved tyrosine residues as part of a salt bridge between elbow helix and ICL. Two negative residues are shown as the intracellular gates. Conserved residues are shown as sticks with color-coding as in the topology model. The conserved phenylalanine F clamp F439 in human ABCG2 (E) and the putative F clamp in C. albicans Cdr1 (F) are indicated as sticks. At the extracellular gates, the valve-like structures at the top of central cavity (red) are shown at the corresponding position of human ABCG2 (G) and C. albicans Cdr1 (H). The lid-structure formed by ECLs is shown as a violet ribbon with a surface. The homo-dimeric human ABCG2 transporter has a symmetric lid (G), while the full-size C. albicans Cdr1 transporter has a larger ECL forming the outer lid and part of the roof architecture (H).
The NBDs in Cdr1 are in closer contact and hold all conserved regions required for ABCG2 function (ATPase activity, A-loop, Walker A and B, Q-loop, mutational hot spot helix, signature loop, Pro-loop, D-loop and H-loop). The N-terminal and C-terminal NBDs form a head-to-tail dimer upon ATP-binding [336,337], with a RecA-like and an α-helical subdomain [327] (Figure 3B). Nonetheless, the fungal NBD1 has three minor differences, in that (i) a glutamine residue in the Q-loop is replaced with glutamate, (ii) the histidine residue in the H-loop is substituted with tyrosine and (iii) the Pro-loop is missing but contains a glycine instead [337] (Table 4). The non-identical deviant NBDs in fungal PDRs [41,216,338,339] may support an asymmetric catalytic cycle as proposed for ABCG5/G8 [38,339,340,341], whereas “symmetric” cycles require the presence of fully conserved “canonical” ATP-binding sites in both NBDs.
Stabilizing salt bridges maintain proper folding and dynamics. At least two salt bridges appear conserved in Cdr1 (Supplementary Figure S1), connecting the elbow helix with the coupling helix (R503 to E576, and R1185 to E1261) (Figure 3D), respectively. However, the salt bridge within ICL1 seems absent in fungal PDR, and a salt bridge at the upper membrane leaflet is found only in the first half of Cdr1 (R456 in ECL1 to E704 in the re-entry helix) (Table 4).
The triple helical bundle (THB) is part of the transmission interface and extremely conserved in Cdr1. Remarkably, the THB is present in diverse ABC transporters, including ABCB1 and LPS extractor, as well as in the antibiotic exporter MacB [332]. This may reflect a universal function in mediating NBD–TMD cross-talk, thus constituting a key element for controlling and driving the conformational switch to drive substrates through the translocation pathway. Moreover, the most highly conserved Y464 residue is essential for ATP consumption, and engages in a salt bridge to stabilize the entire transmission interface in the center of NBD–elbow–ICL1 cluster (Table 4 and Figure 3C,D). Thus, the THB constitutes a cluster of limited conformational flexibility, taking advantage of Y464 and its salt bridge with E458 in ICL1 and/or between elbow helix R383 and E458 [332] (Table 4 and Figure 3C). As for Cdr1, the proposed THB cluster is present in both N- and C-terminal domains. At the N-terminus, Y584 connects to R503 (elbow helix) and E576 (in the coupling helix), whereas at the C-terminal domain, Y1257 bridges to R1185 (second elbow helix) and E1261 in the second coupling helix (Table 4 and Figure 3D). This finding strongly supports the notion for THB as an essential structure acting at the transmission interface to control the entire transport cycle [332].
The mechanism of intracellular gating in PDR/ABCG2 must be crucial for substrate/inhibitor entry into the transport pathway of the exporter, but as yet is little understood. In human ABCG2, two negative residues are conserved in all ABCG/PDR transporters, represented by E451 (between TMH2 and ICL1) and D477 (beginning of TMH3). Interestingly enough, they are pivotal for drug transport, but do not affect ATP hydrolysis [40] (Table 4 and Figure 3C). Since this region around the transmission interface undergoes dynamic movements during the catalytic cycle, E451 and D477 may not be part of a drug-binding zone but rather provide an entry route and gating functions [332]. In fungal PDRs, both negative residues are conserved (Supplementary Figure S1) and Cdr1 indeed contains the corresponding positions with E570 and E597 in the N-terminal part, and D1255 and E1280 in the C-terminal domain (Table 4 and Figure 3D).
The so-called phenylalanine clamp formed by two F residues is located in the substrate-binding zone of ABCG/PDR transporters. Interestingly, the THM2 in the ABCG/PDR subfamily contains at least 4–5 conserved F residues (Supplementary Figure S1). TMH2 occupies space in the middle of the transmembrane core, where a putative binding zone around the central cavity is present. In human ABCG2, F439 (Figure 3E), located in the middle of TMH2, is implicated in binding both substrates and inhibitors [333]. Remarkably, a new cryo-EM structure of ABCG2 illustrates that the aromatic side chains of both phenylalanine residues could contribute to a binding site [259], and thus play a role as a clamp for both substrate and inhibitor recognition [259,333]. Remarkably, the Cdr1 homology model suggests that the conserved residues in both TMDs (Supplementary Figure S1) are F559 in TMH2 and F1239 in TMH8 (Figure 3F) and equivalent to F439 in ABCG2 (Figure 3E). Hence, conserved phenylalanine in or nearby substrate/inhibitor-binding zones of ABCG/PDR provide a clamping mechanism to trap substrates and/or inhibitors.
Extracellular gating at the membrane interface and subsequent drug release from the outward-facing state is regulated by two conserved motifs, a hydrophobic valve and a flexible lid architecture in the roof [42]. The hydrophobic valve in ABCG/PDR transporters is contributed by two half-molecules, thus generating a physical gate for outward-directed substrate translocation from the central into the upper cavity. The atomic structures of mammalian ABCGs [38,256,259] indeed reveal a unique valve-like motif in the core of the transporter, separating the central cavity from the upper cavity. This conserved “glycine-Φ-Φ” motif plays a critical role as a hydrophobic valve that controls water flow through the transport pathway [42] (Supplementary Figure S1). The glycine adds a flexible kink, whereas two hydrophobic aliphatic leucines build a hydrophobic barrier to prevent water flow or substrate leakage. Human ABCG2 has the “G553-L554-L555” motif, whereas Cdr1 has “G672-F673-V674” and “G1362-V1363-L1364” in the first and second half, respectively (Table 4 and Figure 3G,H). Interestingly, a similar extracellular gating mechanism may also operate in CmABCB1, which possesses a gate at the outer membrane border to regulate substrate translocation [35,295].
A flexible but compact lid is part of the roof architecture formed by a rather large extracellular domain in ABCG/PDR. The roof is another unique motif in the ABCG/PDR subfamily. In human ABCG2, this roof is maintained by an intramolecular C592–C608 disulfide bond that strengthens the compact lid architecture. This lid may establish the second gating mechanism to regulate drug release from the outer cavity [334,335] (Figure 3G). Notably, the covalent C603–C603 inter-molecular link is key for homo-dimer formation in human ABCG2, but not essential for function [334,342]. The last extracellular loop of fungal PDR is slightly larger than the equivalent loop in mammalian ABCG2 (Supplementary Figure S1), where 2–3 conserved cysteine residues are present (Table 4). The overall similarity in the roof architecture also supports the notion of a conserved extracellular gating mechanism in ABCG/PDR transporters (Figure 3G,H).
5. Model for a Conserved Catalytic Transport Cycle of ABCG/PDR Transporters
Mammalian ABCG and fungal PDR share all hallmark domains as well as numerous conserved residues essential for function (Figure 3). Based on these striking similarities, we wish to propose a unified mechanism for the transport cycle of type II ABCG/PDR multidrug transporters (Figure 4). Several studies suggest that more than half of all known ABC transporters including human ABCG5/G8 utilize non-equivalent or deviant NBDs [43,216,259,306,329,343,344]. Interestingly, ABCG2 appears as a perfect homo-dimer molecule, although it may have some asymmetries in the NBD dimers [325,341,345]. Therefore, the “primordial” alternating access model [30,36,324,346,347] forms a rational basis for our model (Figure 4). The ABCG/PDR transporters in the apo drug-free state are in an inward-facing configuration, with the bottom of the NBD dimer connected. We propose that ABCG/PDR subfamilies have asymmetric catalytic cycles, as proposed for human ABCG2 [341]. In this state, only one nucleotide-binding site is occupied by ATP, which could support an “intermediate” NBD dimerization state, with one free site remaining accessible for ATP. The intracellular gate formed by two negative residues at the membrane border of the ICL1 in the transmission interface is open, thus offering a path for substrate/inhibitor entry [40]. The central cavity provides free binding zones to accommodate compounds of variable chemical spaces [157,348]. The aromatic rings in the conserved F clamp establish accessible binding/trapping sites [333]. The hydrophobic valve at the top of the central cavity is almost completely closed and blocks water leakage through the translocation pathway [42]. The lid-forming roof architecture also remains closed in the inward-facing state, with a compact loop structure that limits the space in the upper cavity. Since ABCG/PDR exporters have an uncoupled ATP hydrolysis cycle, the catalytic cycle would still be active even without substrate(s) [33,40,42]. Drug substrates (2a) or inhibitors (2b) can access the central cavity and the translocation pathway through the intracellular gate(s) [40] before getting trapped in the binding zones [157] by the F clamp located in TMH2 in each TMD [333]. This is a critical step which also prevents substrate escape from the central transport pathway. By contrast, the binding of an inhibitor (2b) at the region below the valve, would lock the conformation in the inward–open state and inhibit ATP hydrolysis activity as indicated by cryo-EM particle structures [257]. Whether a compound is an inhibitor or a transport substrate for ABCG/PDR transporters is solely determined by the affinity that sets the on versus off rates, and by the kinetics underlying the interactions in the binding zones [33]. Indeed, biochemistry data also suggest that certain inhibitors inhibit ATPase activity [349,350,351]. Binding of the second ATP molecule functions as a molecular glue that triggers complete NBD dimerization, thus inducing the conformational switch of the TMDs into a substrate-occluded state (3). The mechanical movement at the transmission interface requires the THB as a rigid structure of limited dynamics [332]. Subsequently, the central cavity is compressed, hence creating peristaltic pressure that drives substrates along the central translocation channel through the concomitantly opening valve. Further, the full NBD dimerization pushes the transporter into a compressed state, imposing a squeezing motion on the central cavity that generates pressure critical for opening the valve. The hydrophobic valve also serves as the first barrier for an extracellular gating to ensure unidirectional transport. A retrograde backflow of substrates is therefore prevented by the outward hydrostatic pressure and by the tight valve that would close when resetting the transporter [42]. Accordingly, the space of the upper cavity is then enlarged to accommodate substrates [42]. The limited dynamics and stability of the extracellular roof is supported by a conserved salt bridge between ECL1 and the re-entry helix [42]. The compact lid, which is mainly formed by ECL, then constitutes the second barrier at the extracellular interface. Once the lid has opened, it allows for substrate release into the extracellular space. Finally, ATP hydrolysis at one (or both sites) releases Pi and ADP, thus initiating the reset of the transporter with two NBDs in the original inward–open-facing state [43]. The resulting accessible ATP site also opens the intracellular gate enabling a new cycle of substrate recognition. This catalytic cycle reflects the current knowledge about the catalytic cycles of ABCG2/PDR transporters, whereby biochemical, structural, genetic and mutational data have been integrated.
Figure 4.
Proposed catalytic cycles of mammalian/fungal type II exporters (ABCG/PDR). In the apo substrate-free state (1), the exporter adopts an inward-facing conformation. We propose that NBDs are open with ATP present in at least one NBD or both, which mediates partial NBD dimerization leaving only one accessible ATP-binding region. The intracellular gate(s) at the transmission interface provides access for substrate or inhibitor entry. The aromatic rings at the conserved F clamp form accessible binding sites at the closed transporter valve subtending the closed ECL. Drug substrates (2a) or inhibitors (2b) can enter through intracellular gate(s), preceding their trapping in distinct binding zones in the central cavity. Binding of ATP at the second binding site or both triggers full NBD dimerization and triggers a first conformational change, setting an occluded state (3). The communication between NBD and TMD is regulated via a rigid triple helical bundle (THB) as a key part of the transmission interface. The NBD dimerization compresses the central cavity space to drive substrate movement through the translocation, thus engaging a push and squeeze motion to open the valve. Substrates shift into the upper cavity and are released by the subsequent opening of the ECL lid (4). ATP hydrolysis at one NBD site may be enough to reset the catalytic cycle and to convert the transporter molecule into the inward-facing drug-recognizing state (5). The structures show NBDs (green), elbow helix (pink), TMDs (yellow), ICL (orange), ECL (purple), phenylalanine clamp (blue hexagon), valve (red), substrates (cyan) and inhibitors (red). For more details and references see the main text.
6. Conclusions and Future Perspectives
The increase in atomic structures of ABC transporters, and data from extensive biochemical and genetic experiments, have been propelling the field, since they have yielded novel insights and a better understanding of ABC transporter mechanisms. At the same time, while atomic structures have been invaluable, they have to be interpreted with caution, especially when biochemistry or genetics are not in line with structural data [265] or when biological relevance appears doubtful. Indeed, the painful history of ABC transporter structures [207,265], shows that even higher resolution structures suffer from their static nature that only reflects snapshots of a catalytic cycle. Thus, we need atomic structures reflecting more than a single conformation and possibly many transition states [352], as well as extensive validation by biochemistry and genetics, to validate their biological relevance and define catalytic cycles. Furthermore, there is an unmet need for more interdisciplinary collaborations that also engage alternative structural approaches like NMR [353,354,355,356] as well as complementary biophysical methods [265,357,358,359] to expand our mechanistic views of ABC transporters in all living kingdoms.
The past few years challenge previous notions that a unified transport mechanism exists for MDR exporters from all three major classes, such as ABCB1/MDR1/P-gp [35,293,295,302,303,307,310], ABCC1/MRP1 [298,311,312] and ABCG2/BCRP [256,257,258,259] (Table 3). While early homology modeling attempts of the ABCG/PDR family yielded incorrect folds due to using type I exporter templates rather than exporter type II [360,361,362,363], the use of proper coordinates have now validated the usefulness of modeling for dissecting mechanisms of ABC transport cycles [40,256]. Of note, we have taken a “reverse” approach here, since we exploited human ABCG2 and ABCG5/G8 structures to model evolutionarily conserved fungal PDR transporters. This not only yielded new testable homology models, but also hinted that catalytic cycles may have been conserved at least in orthologous families such as human ABCG and fungal PDR. Of note, four cryo-EM structures of yeast Pdr5 [339] at atomic resolutions from 2.8 to 3.5 Å just emerged [339]. Most remarkably, as we show here for Cdr1, the paradigm yeast Pdr5 efflux pump shows similar transitional movements during the catalytic cycle [339], strongly supporting the proposed catalytic cycle for PDR/ABCG transporters operating as uncoupled peristaltic pumps [339]. Twist and Squeeze may be used by different types of transporters, and these driving mechanisms may appear related or even similar when looking at it from the mechanics, as either Twist or Squeeze or a combination of both can result in peristaltic pressure during the switch. While there are many challenges remaining ahead of us, the reversal of clinical MDR phenomena in fungal pathogens in infectious disease settings have regained attention, especially since the catalytic cycle of human ABCG2 likely reflects the mode of action of fungal PDR transporters implicated in anti-infective drug resistance.
Acknowledgments
Open Access Funding by the Austrian Science Fund (FWF). This work was supported by grants from the Austrian Science Fund FWF-SFB-035-20 to K.K. We are very much indebted to Ian D. Kerr, Thomas Stockner and Yuan Eric Lee for constructive and helpful discussions. We also appreciate the constructive and helpful comments from reviewer 2.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijms22094806/s1. Figure S1. Amino acid sequence alignment of fungal ABC transporters (PDR subfamily) and mammalian ABCG subfamily.
Author Contributions
N.K. performed all analysis and prepared figures. N.K. and K.K. interpreted the data and wrote the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Austrian Science Fund (FWF-SFB-035-20 to K.K.).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors confirm that all data are fully available without restrictions. All relevant data are provided in the manuscript and in the Supplementary Materials.
Data and Analysis
Figures and phylogenetic analyses were generated by BioEdit, ClustalX2 and MEGA-X. The homology model was generated using SWISS-MODEL using a Cdr1 sequence from UniProt (accession no. P43071), using the human ABCG2 as a template (PDB ID 6VXF). The molecular visualizations were performed using PyMOL, v1.8.4.
Conflicts of Interest
The authors have no competing financial interests.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Higgins C.F. ABC Transporters: From Microorganisms to Man. Annu. Rev. Cell Biol. 1992;8:67–113. doi: 10.1146/annurev.cb.08.110192.000435. [DOI] [PubMed] [Google Scholar]
- 2.Kuchler K. The ABC of ABCs: Multidrug resistance and genetic diseases. FEBS J. 2011;278:3189. doi: 10.1111/j.1742-4658.2011.08234.x. [DOI] [PubMed] [Google Scholar]
- 3.Holland I.B. Rise and rise of the ABC transporter families. Res. Microbiol. 2019;170:304–320. doi: 10.1016/j.resmic.2019.08.004. [DOI] [PubMed] [Google Scholar]
- 4.Srikant S. Evolutionary history of ATP-binding cassette proteins. FEBS Lett. 2020;594:3882–3897. doi: 10.1002/1873-3468.13985. [DOI] [PubMed] [Google Scholar]
- 5.Ogasawara F., Kodan A., Ueda K. ABC proteins in evolution. FEBS Lett. 2020;594:3876–3881. doi: 10.1002/1873-3468.13945. [DOI] [PubMed] [Google Scholar]
- 6.Holland I., Blight M.A. ABC-ATPases, adaptable energy generators fuelling transmembrane movement of a variety of molecules in organisms from bacteria to humans. J. Mol. Biol. 1999;293:381–399. doi: 10.1006/jmbi.1999.2993. [DOI] [PubMed] [Google Scholar]
- 7.Rees D.C., Johnson E., Lewinson O. ABC transporters: The power to change. Nat. Rev. Mol. Cell Biol. 2009;10:218–227. doi: 10.1038/nrm2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hollenstein K., Dawson R.J.P., Locher K.P. Structure and mechanism of ABC transporter proteins. Curr. Opin. Struct. Biol. 2007;17:412–418. doi: 10.1016/j.sbi.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Senior A.E., Gadsby D.C. ATP hydrolysis cycles and mechanism inP-glycoprotein and CFTR. Semin. Cancer Biol. 1997;8:143–150. doi: 10.1006/scbi.1997.0065. [DOI] [PubMed] [Google Scholar]
- 10.Lage H. ABC-transporters: Implications on drug resistance from microorganisms to human cancers. Int. J. Antimicrob. Agents. 2003;22:188–199. doi: 10.1016/S0924-8579(03)00203-6. [DOI] [PubMed] [Google Scholar]
- 11.Glavinas H., Krajcsi P., Cserepes J., Sarkadi B. The Role of ABC Transporters in Drug Resistance, Metabolism and Toxicity. Curr. Drug Deliv. 2004;1:27–42. doi: 10.2174/1567201043480036. [DOI] [PubMed] [Google Scholar]
- 12.Dean M., Allikmets R. Complete Characterization of the Human ABC Gene Family. J. Bioenerg. Biomembr. 2001;33:475–479. doi: 10.1023/A:1012823120935. [DOI] [PubMed] [Google Scholar]
- 13.Higgins C.F. ABC transporters: Physiology, structure and mechanism—An overview. Res. Microbiol. 2001;152:205–210. doi: 10.1016/S0923-2508(01)01193-7. [DOI] [PubMed] [Google Scholar]
- 14.Sharom F.J. ABC multidrug transporters: Structure, function and role in chemoresistance. Pharmacogenomics. 2008;9:105–127. doi: 10.2217/14622416.9.1.105. [DOI] [PubMed] [Google Scholar]
- 15.Cuperus F.J., Claudel T., Gautherot J., Halilbasic E., Trauner M. The role of canalicular ABC transporters in cholestasis. Drug Metab. Dispos. 2014;42:546–560. doi: 10.1124/dmd.113.056358. [DOI] [PubMed] [Google Scholar]
- 16.Loo T.W., Clarke D.M. Mutational analysis of ABC proteins. Arch. Biochem. Biophys. 2008;476:51–64. doi: 10.1016/j.abb.2008.02.025. [DOI] [PubMed] [Google Scholar]
- 17.Xiong J., Feng J., Yuan D., Zhou J., Miao W. Tracing the structural evolution of eukaryotic ATP binding cassette transporter superfamily. Sci. Rep. 2015;5:16724. doi: 10.1038/srep16724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas C., Aller S.G., Beis K., Carpenter E.P., Chang G., Chen L., Dassa E., Dean M., Van Hoa F.D., Ekiert D., et al. Structural and functional diversity calls for a new classification of ABC transporters. FEBS Lett. 2020;594:3767–3775. doi: 10.1002/1873-3468.13935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins C.F. Multiple molecular mechanisms for multidrug resistance transporters. Nat. Cell Biol. 2007;446:749–757. doi: 10.1038/nature05630. [DOI] [PubMed] [Google Scholar]
- 20.Cole S.P. Targeting Multidrug Resistance Protein 1 (MRP1,ABCC1): Past, Present, and Future. Annu. Rev. Pharmacol. Toxicol. 2014;54:95–117. doi: 10.1146/annurev-pharmtox-011613-135959. [DOI] [PubMed] [Google Scholar]
- 21.Ford B. CFTR structure: Lassoing cystic fibrosis. Nat. Struct. Mol. Biol. 2017;24:13–14. doi: 10.1038/nsmb.3353. [DOI] [PubMed] [Google Scholar]
- 22.Holland K.A., Holland I.B. Adventures with ABC-proteins: Highly Conserved ATP-dependent Transporters. Acta Microbiol. et Immunol. Hung. 2005;52:309–322. doi: 10.1556/AMicr.52.2005.3-4.4. [DOI] [PubMed] [Google Scholar]
- 23.Jones P.M., George A.M. A reciprocating twin-channel model for ABC transporters. Q. Rev. Biophys. 2014;47:189–220. doi: 10.1017/S0033583514000031. [DOI] [PubMed] [Google Scholar]
- 24.Davidson A.L., Dassa E., Orelle C., Chen J. Structure, Function, and Evolution of Bacterial ATP-Binding Cassette Systems. Microbiol. Mol. Biol. Rev. 2008;72:317–364. doi: 10.1128/MMBR.00031-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford R.C., Beis K. Learning the ABCs one at a time: Structure and mechanism of ABC transporters. Biochem. Soc. Trans. 2019;47:23–36. doi: 10.1042/BST20180147. [DOI] [PubMed] [Google Scholar]
- 26.Locher K.P., Lee A.T., Rees D.C. The E. coli BtuCD structure: A framework for ABC transporter architecture and mechanism. Science. 2002;296:1091–1098. doi: 10.1126/science.1071142. [DOI] [PubMed] [Google Scholar]
- 27.Schmitt L., Tampe R. Structure and mechanism of ABC transporters. Curr. Opin. Struct. Biol. 2002;12:754–760. doi: 10.1016/S0959-440X(02)00399-8. [DOI] [PubMed] [Google Scholar]
- 28.Higgins C.F., Linton K.J. The ATP switch model for ABC transporters. Nat. Struct. Mol. Biol. 2004;11:918–926. doi: 10.1038/nsmb836. [DOI] [PubMed] [Google Scholar]
- 29.Dawson R.J.P., Hollenstein K., Locher K.P. Uptake or extrusion: Crystal structures of full ABC transporters suggest a common mechanism. Mol. Microbiol. 2007;65:250–257. doi: 10.1111/j.1365-2958.2007.05792.x. [DOI] [PubMed] [Google Scholar]
- 30.Oldham M.L., Khare D., Quiocho F.A., Davidson A.L., Chen J. Crystal structure of a catalytic intermediate of the maltose transporter. Nat. Cell Biol. 2007;450:515–521. doi: 10.1038/nature06264. [DOI] [PubMed] [Google Scholar]
- 31.Seeger M.A., van Veen H.W. Molecular basis of multidrug transport by ABC transporters. Biochim. Biophys. Acta. 2009;1794:725–737. doi: 10.1016/j.bbapap.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 32.Procko E., O’Mara M.L., Bennett W.F.D., Tieleman D.P., Gaudet R. The mechanism of ABC transporters: General lessons from structural and functional studies of an antigenic peptide transporter. FASEB J. 2009;23:1287–1302. doi: 10.1096/fj.08-121855. [DOI] [PubMed] [Google Scholar]
- 33.Ernst R., Kueppers P., Stindt J., Kuchler K., Schmitt L. Multidrug efflux pumps: Substrate selection in ATP-binding cassette multidrug efflux pumps—First come, first served? FEBS J. 2009;277:540–549. doi: 10.1111/j.1742-4658.2009.07485.x. [DOI] [PubMed] [Google Scholar]
- 34.Xu K., Zhang M., Zhao Q., Yu F., Guo H., Wang C., He F., Ding J., Zhang P. Crystal structure of a folate energy-coupling factor transporter from Lactobacillus brevis. Nat. Cell Biol. 2013;497:268–271. doi: 10.1038/nature12046. [DOI] [PubMed] [Google Scholar]
- 35.Kodan A., Yamaguchi T., Nakatsu T., Sakiyama K., Hipolito C.J., Fujioka A., Hirokane R., Ikeguchi K., Watanabe B., Hiratake J., et al. Structural basis for gating mechanisms of a eukaryotic P-glycoprotein homolog. Proc. Natl. Acad. Sci. USA. 2014;111:4049–4054. doi: 10.1073/pnas.1321562111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilkens S. Structure and mechanism of ABC transporters. F1000Prime Rep. 2015;7:14. doi: 10.12703/P7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Horsey A.J., Cox M.H., Sarwat S., Kerr I.D. The multidrug transporter ABCG2: Still more questions than answers. Biochem. Soc. Trans. 2016;44:824–830. doi: 10.1042/BST20160014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee J.-Y., Kinch L.N., Borek D.M., Wang J., Wang J., Urbatsch I.L., Xie X.-S., Grishin N.V., Cohen J.C., Otwinowski Z., et al. Crystal structure of the human sterol transporter ABCG5/ABCG8. Nat. Cell Biol. 2016;533:561–564. doi: 10.1038/nature17666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Locher K.P. Mechanistic diversity in ATP-binding cassette (ABC) transporters. Nat. Struct. Mol. Biol. 2016;23:487–493. doi: 10.1038/nsmb.3216. [DOI] [PubMed] [Google Scholar]
- 40.Khunweeraphong N., Stockner T., Kuchler K. The structure of the human ABC transporter ABCG2 reveals a novel mechanism for drug extrusion. Sci. Rep. 2017;7:1–15. doi: 10.1038/s41598-017-11794-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wagner M., Smits S.H.J., Schmitt L. In vitro NTPase activity of highly purified Pdr5, a major yeast ABC multidrug transporter. Sci. Rep. 2019;9:7761. doi: 10.1038/s41598-019-44327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khunweeraphong N., Szöllősi D., Stockner T., Kuchler K. The ABCG2 multidrug transporter is a pump gated by a valve and an extracellular lid. Nat. Commun. 2019;10:1–14. doi: 10.1038/s41467-019-13302-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas C., Tampé R. Structural and Mechanistic Principles of ABC Transporters. Annu. Rev. Biochem. 2020;89:605–636. doi: 10.1146/annurev-biochem-011520-105201. [DOI] [PubMed] [Google Scholar]
- 44.Linton K.J., Higgins C.F. Structure and function of ABC transporters: The ATP switch provides flexible control. Pflügers Arch. Eur. J. Physiol. 2006;453:555–567. doi: 10.1007/s00424-006-0126-x. [DOI] [PubMed] [Google Scholar]
- 45.Oswald C., Holland I.B., Schmitt L. The motor domains of ABC-transporters. What can structures tell us? Naunyn Schmiedebergs Arch. Pharmacol. 2006;372:385–399. doi: 10.1007/s00210-005-0031-4. [DOI] [PubMed] [Google Scholar]
- 46.Dean M., Annilo T. Evolution of the atp-binding cassette (abc) transporter superfamily in vertebrates. Annu. Rev. Genom. Hum. Genet. 2005;6:123–142. doi: 10.1146/annurev.genom.6.080604.162122. [DOI] [PubMed] [Google Scholar]
- 47.Dassa E., Schneider E. The rise of a protein family: ATP-binding cassette systems. Res. Microbiol. 2001;152:203. doi: 10.1016/S0923-2508(01)01214-1. [DOI] [PubMed] [Google Scholar]
- 48.Bouige P., Laurent D., Piloyan L., Dassa E. Phylogenetic and functional classification of ATP-binding cassette (ABC) systems. Curr. Protein Pept. Sci. 2002;3:541–559. doi: 10.2174/1389203023380486. [DOI] [PubMed] [Google Scholar]
- 49.Theodoulou F.L., Kerr I.D. ABC transporter research: Going strong 40 years on. Biochem. Soc. Trans. 2015;43:1033–1040. doi: 10.1042/BST20150139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Riordan J.R., Rommens J.M., Kerem B., Alon N., Rozmahel R., Grzelczak Z., Zielenski J., Lok S., Plavsic N., Chou J.L., et al. Identification of the cystic fibrosis gene: Cloning and characterization of complementary DNA. Science. 1989;245:1066–1073. doi: 10.1126/science.2475911. [DOI] [PubMed] [Google Scholar]
- 51.Harris A., Argent B.E. The cystic fibrosis gene and its product CFTR. Semin. Cell Biol. 1993;4:37–44. doi: 10.1006/scel.1993.1005. [DOI] [PubMed] [Google Scholar]
- 52.Stieger B., Meier P.J. Bile acid and xenobiotic transporters in liver. Curr. Opin. Cell Biol. 1998;10:462–467. doi: 10.1016/S0955-0674(98)80059-8. [DOI] [PubMed] [Google Scholar]
- 53.Strautnieks S.S., Bull L.N., Knisely A.S., Kocoshis S.A., Dahl N., Arnell H., Sokal E., Dahan K., Childs S., Ling V., et al. A gene encoding a liver-specific ABC transporter is mutated in progressive familial intrahepatic cholestasis. Nat. Genet. 1998;20:233–238. doi: 10.1038/3034. [DOI] [PubMed] [Google Scholar]
- 54.Berge K.E., Tian H., Graf G.A., Yu L., Grishin N.V., Schultz J., Kwiterovich P., Shan B., Barnes R., Hobbs H.H. Accumulation of Dietary Cholesterol in Sitosterolemia Caused by Mutations in Adjacent ABC Transporters. Science. 2000;290:1771–1775. doi: 10.1126/science.290.5497.1771. [DOI] [PubMed] [Google Scholar]
- 55.Patel S.B., Salen G., Hidaka H., Kwiterovich P.O., Stalenhoef A.F., Miettinen T.A., Grundy S.M., Lee M.H., Rubenstein J.S., Polymeropoulos M.H., et al. Mapping a gene involved in regulating dietary cholesterol absorption. The sitosterolemia locus is found at chromosome 2p21. J. Clin. Investig. 1998;102:1041–1044. doi: 10.1172/JCI3963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hubacek J.A., Berge K.E., Cohen J.C., Hobbs H.H. Mutations in ATP-cassette binding proteins G5 (ABCG5) and G8 (ABCG8) causing sitosterolemia. Hum. Mutat. 2001;18:359–360. doi: 10.1002/humu.1206. [DOI] [PubMed] [Google Scholar]
- 57.Hobbs H.H., Russell D.W., Brown M.S., Goldstein J.L. The LDL receptor locus in familial hypercholesterolemia: Mutational analysis of a membrane protein. Annu. Rev. Genet. 1990;24:133–170. doi: 10.1146/annurev.ge.24.120190.001025. [DOI] [PubMed] [Google Scholar]
- 58.Aguilar-Bryan L., Nichols C.G., Wechsler S.W., Clement J.P., Boyd A.E., Gonzalez G., Herrera-Sosa H., Nguy K., Bryan J., Nelson D.A. Cloning of the beta cell high-affinity sulfonylurea receptor: A regulator of insulin secretion. Science. 1995;268:423–426. doi: 10.1126/science.7716547. [DOI] [PubMed] [Google Scholar]
- 59.Woodward O.M., Köttgen M., Coresh J., Boerwinkle E., Guggino W.B. Identification of a urate transporter, ABCG2, with a common functional polymorphism causing gout. Proc. Natl. Acad. Sci. USA. 2009;106:10338–10342. doi: 10.1073/pnas.0901249106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Paulusma C.C., Bosma P.J., Zaman G.J., Bakker C.T., Otter M., Scheffer G.L., Scheper R.J., Borst P., Elferink R.P.O. Congenital jaundice in rats with a mutation in a multidrug resistance-associated protein gene. Science. 1996;271:1126–1128. doi: 10.1126/science.271.5252.1126. [DOI] [PubMed] [Google Scholar]
- 61.Kartenbeck J., Leuschner U., Mayer R., Keppler D. Absence of the canalicular isoform of the MRP gene-encoded conjugate export pump from the hepatocytes in Dubin-Johnson syndrome. Hepatology. 1996;23:1061–1066. doi: 10.1053/jhep.1996.v23.pm0008621134. [DOI] [PubMed] [Google Scholar]
- 62.Allikmets R. A photoreceptor cell-specific ATP-binding transporter gene (ABCR) is mutated in recessive Stargardt macular dystrophy. Nat. Genet. 1997;17:122. doi: 10.1038/ng0997-122a. [DOI] [PubMed] [Google Scholar]
- 63.Berger J., Forss-Petter S., Eichler F. Pathophysiology of X-linked adrenoleukodystrophy. Biochimie. 2014;98:135–142. doi: 10.1016/j.biochi.2013.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shani N., Watkins P.A., Valle D. PXA1, a possible Saccharomyces cerevisiae ortholog of the human adrenoleukodystrophy gene. Proc. Natl. Acad. Sci. USA. 1995;92:6012–6016. doi: 10.1073/pnas.92.13.6012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aubourg P. Adrenoleukodystrophy and other peroxisomal diseases. Curr. Opin. Genet. Dev. 1994;4:407–411. doi: 10.1016/0959-437X(94)90029-9. [DOI] [PubMed] [Google Scholar]
- 66.Seyffer F., Tampé R. ABC transporters in adaptive immunity. Biochim. Biophys. Acta (BBA) Gen. Subj. 2015;1850:449–460. doi: 10.1016/j.bbagen.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 67.Suh W., Cohen-Doyle M., Fruh K., Wang K., Peterson P., Williams D. Interaction of MHC class I molecules with the transporter associated with antigen processing. Science. 1994;264:1322–1326. doi: 10.1126/science.8191286. [DOI] [PubMed] [Google Scholar]
- 68.De La Salle H., Hanau D., Fricker D., Urlacher A., Kelly A., Salamero J., Powis S.H., Donato L., Bausinger H., Laforet M., et al. Homozygous human TAP peptide transporter mutation in HLA class I deficiency. Science. 1994;265:237–241. doi: 10.1126/science.7517574. [DOI] [PubMed] [Google Scholar]
- 69.Gelissen I.C., Harris M., Rye K., Quinn C., Brown A.J., Kockx M., Cartland S., Packianathan M., Kritharides L., Jessup W. ABCA1 and ABCG1 synergize to mediate cholesterol export to apoA-I. Arterioscler. Thromb. Vasc. Biol. 2006;26:534–540. doi: 10.1161/01.ATV.0000200082.58536.e1. [DOI] [PubMed] [Google Scholar]
- 70.Yvan-Charvet L., Ranalletta M., Wang N., Han S., Terasaka N., Li R., Welch C., Tall A.R. Combined deficiency of ABCA1 and ABCG1 promotes foam cell accumulation and accelerates atherosclerosis in mice. J. Clin. Investig. 2007;117:3900–3908. doi: 10.1172/JCI33372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brooks-Wilson A., Marcil M., Clee S.M., Zhang L.-H., Roomp K., Van Dam M., Yu L., Brewer C., Collins J.A., Molhuizen H.O., et al. Mutations in ABC1 in Tangier disease and familial high-density lipoprotein deficiency. Nat. Genet. 1999;22:336–345. doi: 10.1038/11905. [DOI] [PubMed] [Google Scholar]
- 72.Bodzioch M., Orsó E., Klucken J., Langmann T., Böttcher A., Diederich W., Drobnik W., Barlage S., Büchler C., Porsch-Özcürümez M., et al. The gene encoding ATP-binding cassette transporter 1 is mutated in Tangier disease. Nat. Genet. 1999;22:347–351. doi: 10.1038/11914. [DOI] [PubMed] [Google Scholar]
- 73.Rust S., Rosier M., Funke H., Real J.T., Amoura Z., Piette J.-C., Deleuze J.-F., Brewer H.B., Duverger N., Denèfle P., et al. Tangier disease is caused by mutations in the gene encoding ATP-binding cassette transporter 1. Nat. Genet. 1999;22:352–355. doi: 10.1038/11921. [DOI] [PubMed] [Google Scholar]
- 74.Tanaka A.R., Ikeda Y., Abe-Dohmae S., Arakawa R., Sadanami K., Kidera A., Nakagawa S., Nagase T., Aoki R., Kioka N., et al. Human ABCA1 contains a large amino-terminal extracellular domain homologous to an epitope of Sjogren’s Syndrome. Biochem. Biophys. Res. Commun. 2001;283:1019–1025. doi: 10.1006/bbrc.2001.4891. [DOI] [PubMed] [Google Scholar]
- 75.Laffitte B.A., Repa J.J., Joseph S.B., Wilpitz D.C., Kast H.R., Mangelsdorf D.J., Tontonoz P. LXRs control lipid-inducible expression of the apolipoprotein E gene in macrophages and adipocytes. Proc. Natl. Acad. Sci. USA. 2001;98:507–512. doi: 10.1073/pnas.98.2.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Váradi A., Szabó Z., Pomozi V., De Boussac H., Fülöp K., Arányi T. ABCC6 as a target in pseudoxanthoma elasticum. Curr. Drug Targets. 2011;12:671–682. doi: 10.2174/138945011795378612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Legrand A., Cornez L., Samkari W., Mazzella J.-M., Venisse A., Boccio V., Auribault K., Keren B., Benistan K., Germain D.P., et al. Mutation spectrum in the ABCC6 gene and genotype–phenotype correlations in a French cohort with pseudoxanthoma elasticum. Genet. Med. 2017;19:909–917. doi: 10.1038/gim.2016.213. [DOI] [PubMed] [Google Scholar]
- 78.Pulkkinen L., Nakano A., Ringpfeil F., Uitto J. Identification of ABCC6 pseudogenes on human chromosome 16p: Implications for mutation detection in pseudoxanthoma elasticum. Qual. Life Res. 2001;109:356–365. doi: 10.1007/s004390100582. [DOI] [PubMed] [Google Scholar]
- 79.Le Saux O., Beck K., Sachsinger C., Silvestri C., Treiber C., Göring H.H., Johnson E.W., De Paepe A., Pope F.M., Pasquali-Ronchetti I., et al. A Spectrum of ABCC6 Mutations Is Responsible for Pseudoxanthoma Elasticum. Am. J. Hum. Genet. 2001;69:749–764. doi: 10.1086/323704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bergen A.A., Plomp A.S., Schuurman E.J., Terry S.F., Breuning M.H., Dauwerse H.G., Swart J., Kool M., Van Soest S., Baas F., et al. Mutations in ABCC6 cause pseudoxanthoma elasticum. Nat. Genet. 2000;25:228–231. doi: 10.1038/76109. [DOI] [PubMed] [Google Scholar]
- 81.Germain D.P. Pseudoxanthoma elasticum: Evidence for the existence of a pseudogene highly homologous to the ABCC6 gene. J. Med. Genet. 2001;38:457–461. doi: 10.1136/jmg.38.7.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Le Saux O., Urban Z., Tschuch C., Csiszar K., Bacchelli B., Quaglino D., Pasquali-Ronchetti I., Pope F.M., Richards A., Terry S.F., et al. Mutations in a gene encoding an ABC transporter cause pseudoxanthoma elasticum. Nat. Genet. 2000;25:223–227. doi: 10.1038/76102. [DOI] [PubMed] [Google Scholar]
- 83.Bienengraeber M., Olson T.M., Selivanov V.A., Kathmann E.C., O’Cochlain F., Gao F., Karger A.B., Ballew J.D., Hodgson D.M., Zingman L.V., et al. ABCC9 mutations identified in human dilated cardiomyopathy disrupt catalytic KATP channel gating. Nat. Genet. 2004;36:382–387. doi: 10.1038/ng1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yoshiura K.-I., Kinoshita A., Ishida T., Ninokata A., Ishikawa T., Kaname T., Bannai M., Tokunaga K., Sonoda S., Komaki R., et al. A SNP in the ABCC11 gene is the determinant of human earwax type. Nat. Genet. 2006;38:324–330. doi: 10.1038/ng1733. [DOI] [PubMed] [Google Scholar]
- 85.Tammur J., Prades C., Arnould I., Rzhetsky A., Hutchinson A., Adachi M., Schuetz J.D., Swoboda K.J., Ptácek L.J., Rosier M., et al. Two new genes from the human ATP-binding cassette transporter superfamily, ABCC11 and ABCC12, tandemly duplicated on chromosome 16q12. Gene. 2001;273:89–96. doi: 10.1016/S0378-1119(01)00572-8. [DOI] [PubMed] [Google Scholar]
- 86.Anandarajan M., Paulraj S., Tubman R. ABCA3 Deficiency: An unusual cause of respiratory distress in the newborn. Ulst. Med. J. 2009;78:51–52. [PMC free article] [PubMed] [Google Scholar]
- 87.Kröner C., Wittmann T., Reu S., Teusch V., Klemme M., Rauch D., Hengst M., Kappler M., Cobanoglu N., Sismanlar T., et al. Lung disease caused byABCA3mutations. Thorax. 2017;72:213–220. doi: 10.1136/thoraxjnl-2016-208649. [DOI] [PubMed] [Google Scholar]
- 88.Shulenin S., Nogee L.M., Annilo T., Wert S.E., Whitsett J.A., Dean M. ABCA3Gene Mutations in Newborns with Fatal Surfactant Deficiency. N. Engl. J. Med. 2004;350:1296–1303. doi: 10.1056/NEJMoa032178. [DOI] [PubMed] [Google Scholar]
- 89.Yoshida I., Ban N., Inagaki N. Expression of ABCA3, a causative gene for fatal surfactant deficiency, is up-regulated by glucocorticoids in lung alveolar type II cells. Biochem. Biophys. Res. Commun. 2004;323:547–555. doi: 10.1016/j.bbrc.2004.08.133. [DOI] [PubMed] [Google Scholar]
- 90.Scott C.A., Rajpopat S., Di W.-L. Harlequin ichthyosis: ABCA12 mutations underlie defective lipid transport, reduced protease regulation and skin-barrier dysfunction. Cell Tissue Res. 2012;351:281–288. doi: 10.1007/s00441-012-1474-9. [DOI] [PubMed] [Google Scholar]
- 91.Lefévre C. Mutations in the transporter ABCA12 are associated with lamellar ichthyosis type 2. Hum. Mol. Genet. 2003;12:2369–2378. doi: 10.1093/hmg/ddg235. [DOI] [PubMed] [Google Scholar]
- 92.Thomas A.C., Cullup T., Norgett E.E., Hill T., Barton S., Dale B.A., Sprecher E., Sheridan E., Taylor A.E., Wilroy R.S., et al. ABCA12 Is the Major Harlequin Ichthyosis Gene. J. Investig. Dermatol. 2006;126:2408–2413. doi: 10.1038/sj.jid.5700455. [DOI] [PubMed] [Google Scholar]
- 93.Johnston R.C., Stephenson M.L., Nageotte M.P. Novel heterozygous ABCB4 gene mutation causing recurrent first-trimester intrahepatic cholestasis of pregnancy. J. Perinatol. 2014;34:711–712. doi: 10.1038/jp.2014.86. [DOI] [PubMed] [Google Scholar]
- 94.Dixon P., Weerasekera N., Linton K., Donaldson O., Chambers J., Egginton E., Weaver J., Nelson-Piercy C., De Swiet M., Warnes G., et al. Heterozygous MDR3 missense mutation associated with intrahepatic cholestasis of pregnancy: Evidence for a defect in protein trafficking. Hum. Mol. Genet. 2000;9:1209–1217. doi: 10.1093/hmg/9.8.1209. [DOI] [PubMed] [Google Scholar]
- 95.Pondarre C., Campagna D.R., Antiochos B., Sikorski L., Mulhern H., Fleming M.D. Abcb7, the gene responsible for X-linked sideroblastic anemia with ataxia, is essential for hematopoiesis. Blood. 2006;109:3567–3569. doi: 10.1182/blood-2006-04-015768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shimada Y., Okuno S., Kawai A., Shinomiya H., Saito A., Suzuki M., Omori Y., Nishino N., Kanemoto N., Fujiwara T., et al. Cloning and chromosomal mapping of a novel ABC transporter gene (hABC7), a candidate for X-linked sideroblastic anemia with spinocerebellar ataxia. J. Hum. Genet. 1998;43:115–122. doi: 10.1007/s100380050051. [DOI] [PubMed] [Google Scholar]
- 97.Allikmets R., Raskind W.H., Hutchinson A., Schueck N.D., Dean M., Koeller D.M. Mutation of a Putative Mitochondrial Iron Transporter Gene (ABC7) in X-Linked Sideroblastic Anemia and Ataxia (XLSA/A) Hum. Mol. Genet. 1999;8:743–749. doi: 10.1093/hmg/8.5.743. [DOI] [PubMed] [Google Scholar]
- 98.Bekri S., Kispal G., Lange H., Fitzsimons E., Tolmie J., Lill R., Bishop D.F. Human ABC7 transporter: Gene structure and mutation causing X-linked sideroblastic anemia with ataxia with disruption of cytosolic iron-sulfur protein maturation. Blood. 2000;96:3256–3264. doi: 10.1182/blood.V96.9.3256. [DOI] [PubMed] [Google Scholar]
- 99.Kohut P., Wüstner D., Hronska L., Kuchler K., Hapala I., Valachovic M. The role of ABC proteins Aus1p and Pdr11p in the uptake of external sterols in yeast: Dehydroergosterol fluorescence study. Biochem. Biophys. Res. Commun. 2011;404:233–238. doi: 10.1016/j.bbrc.2010.11.099. [DOI] [PubMed] [Google Scholar]
- 100.Gottesman M.M. Mechanisms of Cancer Drug Resistance. Annu. Rev. Med. 2002;53:615–627. doi: 10.1146/annurev.med.53.082901.103929. [DOI] [PubMed] [Google Scholar]
- 101.Piddock L.J.V. Multidrug-resistance efflux pumps ? not just for resistance. Nat. Rev. Genet. 2006;4:629–636. doi: 10.1038/nrmicro1464. [DOI] [PubMed] [Google Scholar]
- 102.Borst P. Looking back at multidrug resistance (MDR) research and ten mistakes to be avoided when writing about ABC transporters in MDR. FEBS Lett. 2020;594:4001–4011. doi: 10.1002/1873-3468.13972. [DOI] [PubMed] [Google Scholar]
- 103.Ueda K., Cardarelli C., Gottesman M.M., Pastan I. Expression of a full-length cDNA for the human “MDR1” gene confers resistance to colchicine, doxorubicin, and vinblastine. Proc. Natl. Acad. Sci. USA. 1987;84:3004–3008. doi: 10.1073/pnas.84.9.3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kartner N., Riordan J.R., Ling V. Cell surface P-glycoprotein associated with multidrug resistance in mammalian cell lines. Science. 1983;221:1285–1288. doi: 10.1126/science.6137059. [DOI] [PubMed] [Google Scholar]
- 105.Gottesman M.M., Ling V. The molecular basis of multidrug resistance in cancer: The early years of P-glycoprotein research. FEBS Lett. 2005;580:998–1009. doi: 10.1016/j.febslet.2005.12.060. [DOI] [PubMed] [Google Scholar]
- 106.Ling V., Thompson L.H. Reduced permeability in CHO cells as a mechanism of resistance to colchicine. J. Cell. Physiol. 1974;83:103–116. doi: 10.1002/jcp.1040830114. [DOI] [PubMed] [Google Scholar]
- 107.Cole S.P., Bhardwaj G., Gerlach J.H., Mackie J.E., Grant C.E., Almquist K.C., Stewart A.J., Kurz E.U., Duncan A.M., Deeley R.G. Overexpression of a transporter gene in a multidrug-resistant human lung cancer cell line. Science. 1992;258:1650–1654. doi: 10.1126/science.1360704. [DOI] [PubMed] [Google Scholar]
- 108.Miyake K., Mickley L., Litman T., Zhan Z., Robey R., Cristensen B., Brangi M., Greenberger L., Dean M., Fojo T., et al. Molecular cloning of cDNAs which are highly overexpressed in mitoxantrone-resistant cells: Demonstration of homology to ABC transport genes. Cancer Res. 1999;59:8–13. [PubMed] [Google Scholar]
- 109.Lee J.S., Scala S., Matsumoto Y., Dickstein B., Robey R., Zhan Z., Altenberg G., Bates S.E. Reduced drug accumulation and multidrug resistance in human breast cancer cells without associated P-glycoprotein or MRP overexpression. J. Cell. Biochem. 1997;65:513–526. doi: 10.1002/(SICI)1097-4644(19970615)65:4<513::AID-JCB7>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 110.Doyle L.A., Yang W., Abruzzo L.V., Krogmann T., Gao Y., Rishi A.K., Ross D.D. A multidrug resistance transporter from human MCF-7 breast cancer cells. Proc. Natl. Acad. Sci. USA. 1998;95:15665–15670. doi: 10.1073/pnas.95.26.15665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sarkadi B., Homolya L., Szakács G., Váradi A. Human Multidrug Resistance ABCB and ABCG Transporters: Participation in a Chemoimmunity Defense System. Physiol. Rev. 2006;86:1179–1236. doi: 10.1152/physrev.00037.2005. [DOI] [PubMed] [Google Scholar]
- 112.Leslie E.M., Deeley R.G., Cole S.P. Multidrug resistance proteins: Role of P-glycoprotein, MRP1, MRP2, and BCRP (ABCG2) in tissue defense. Toxicol. Appl. Pharmacol. 2005;204:216–237. doi: 10.1016/j.taap.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 113.Sharom F.J. The P-glycoprotein multidrug transporter. Essays Biochem. 2011;50:161–178. doi: 10.1042/bse0500161. [DOI] [PubMed] [Google Scholar]
- 114.Sharom F.J. Complex Interplay between the P-Glycoprotein Multidrug Efflux Pump and the Membrane: Its Role in Modulating Protein Function. Front. Oncol. 2014;4:41. doi: 10.3389/fonc.2014.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zein A.A., Kaur R., Hussein T.O., Graf G.A., Lee J.-Y. ABCG5/G8: A structural view to pathophysiology of the hepatobiliary cholesterol secretion. Biochem. Soc. Trans. 2019;47:1259–1268. doi: 10.1042/BST20190130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Okamoto Y., Tomioka M., Ogasawara F., Nagaiwa K., Kimura Y., Kioka N., Ueda K. C-terminal of ABCA1 separately regulates cholesterol floppase activity and cholesterol efflux activity. Biosci. Biotechnol. Biochem. 2020;84:764–773. doi: 10.1080/09168451.2019.1700775. [DOI] [PubMed] [Google Scholar]
- 117.Nagao K., Tomioka M., Ueda K. Function and regulation of ABCA1-membrane meso-domain organization and reorganization. FEBS J. 2011;278:3190–3203. doi: 10.1111/j.1742-4658.2011.08170.x. [DOI] [PubMed] [Google Scholar]
- 118.van Herwaarden A.E., Schinkel A.H. The function of breast cancer resistance protein in epithelial barriers, stem cells and milk secretion of drugs and xenotoxins. Trends Pharmacol. Sci. 2006;27:10–16. doi: 10.1016/j.tips.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 119.Giacomini K.M., Huang S., Tweedie D.J., Benet L.Z., Brouwer K.L.R., Chu X., Dahlin A., Evers R., Fischer V., Hillgren K.M., et al. Membrane transporters in drug development. Nat. Rev. Drug Discov. 2010;9:215–236. doi: 10.1038/nrd3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Martinez L., Arnaud O., Henin E., Tao H., Chaptal V., Doshi R., Andrieu T., Dussurgey S., Tod M., Di Pietro A., et al. Understanding polyspecificity within the substrate-binding cavity of the human multidrug resistance P-glycoprotein. FEBS J. 2014;281:673–682. doi: 10.1111/febs.12613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kimura Y., Morita S., Matsuo M., Ueda K. Mechanism of multidrug recognition by MDR1/ABCB1. Cancer Sci. 2007;98:1303–1310. doi: 10.1111/j.1349-7006.2007.00538.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Juliano R., Ling V. A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim. Biophys. Acta (BBA) Biomembr. 1976;455:152–162. doi: 10.1016/0005-2736(76)90160-7. [DOI] [PubMed] [Google Scholar]
- 123.Chen C.-J., Chin J.E., Ueda K., Clark D.P., Pastan I., Gottesman M.M., Roninson I.B. Internal duplication and homology with bacterial transport proteins in the mdr1 (P-glycoprotein) gene from multidrug-resistant human cells. Cell. 1986;47:381–389. doi: 10.1016/0092-8674(86)90595-7. [DOI] [PubMed] [Google Scholar]
- 124.Ambudkar S.V., Dey S., Hrycyna C.A., Ramachandra M., Pastan I., Gottesman M.M. Biochemical, cellular, and pharmacological aspects of the multidrug transporter. Annu. Rev. Pharmacol. Toxicol. 1999;39:361–398. doi: 10.1146/annurev.pharmtox.39.1.361. [DOI] [PubMed] [Google Scholar]
- 125.Savas B., Cole S.P., Akoglu T.F., Pross H.F. P-glycoprotein-mediated multidrug resistance and cytotoxic effector cells. Nat. Immun. 1992;11:177–192. [PubMed] [Google Scholar]
- 126.Schinkel A., Smit J., van Tellingen O., Beijnen J., Wagenaar E., van Deemter L., Mol C., van der Valk M., Robanus-Maandag E., Riele H.T., et al. Disruption of the mouse mdr1a P-glycoprotein gene leads to a deficiency in the blood-brain barrier and to increased sensitivity to drugs. Cell. 1994;77:491–502. doi: 10.1016/0092-8674(94)90212-7. [DOI] [PubMed] [Google Scholar]
- 127.Doran A., Obach R.S., Smith B.J., Hosea N.A., Becker S., Callegari E., Chen C., Chen X., Choo E., Cianfrogna J., et al. The impact of p-glycoprotein on the disposition of drugs targeted for indications of the central nervous system: Evaluation using the mdr1a/1b knockout mouse modeL. Drug Metab. Dispos. 2004;33:165–174. doi: 10.1124/dmd.104.001230. [DOI] [PubMed] [Google Scholar]
- 128.Borst P., Schinkel A.H. P-glycoprotein ABCB1: A major player in drug handling by mammals. J. Clin. Investig. 2013;123:4131–4133. doi: 10.1172/JCI70430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ruetz S., Gros P. Phosphatidylcholine translocase: A physiological role for the mdr2 gene. Cell. 1994;77:1071–1081. doi: 10.1016/0092-8674(94)90446-4. [DOI] [PubMed] [Google Scholar]
- 130.Abraham J., Edgerly M., Wilson R., Chen C., Rutt A., Bakke S., Robey R., Dwyer A., Goldspiel B., Balis F., et al. A Phase I Study of the P-Glycoprotein Antagonist Tariquidar in Combination with Vinorelbine. Clin. Cancer Res. 2009;15:3574–3582. doi: 10.1158/1078-0432.CCR-08-0938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dantzig A.H., Shepard R.L., Cao J., Law K.L., Ehlhardt W.J., Baughman T.M., Bumol T.F., Starling J.J. Reversal of P-glycoprotein-mediated multidrug resistance by a potent cyclopropyldibenzosuberane modulator, LY335979. Cancer Res. 1996;56:4171–4179. [PubMed] [Google Scholar]
- 132.Starling J.J., Shepard R.L., Cao J., Law K.L., Norman B.H., Kroin J.S., Ehlhardt W.J., Baughman T.M., Winter M.A., Bell M.G., et al. Pharmacological characterization of LY335979: A potent cyclopropyldibenzosuberane modulator of P-glycoprotein. Adv. Enzym. Regul. 1997;37:335–347. doi: 10.1016/S0065-2571(96)00021-0. [DOI] [PubMed] [Google Scholar]
- 133.Benderra Z., Faussat A.-M., Sayada L., Perrot J.-Y., Chaoui D., Marie J.-P., Legrand O. Breast Cancer Resistance Protein and P-Glycoprotein in 149 Adult Acute Myeloid Leukemias. Clin. Cancer Res. 2004;10:7896–7902. doi: 10.1158/1078-0432.CCR-04-0795. [DOI] [PubMed] [Google Scholar]
- 134.Benderra Z., Faussat A.M., Sayada L., Perrot J.-Y., Tang R., Chaoui D., Morjani H., Marzac C., Marie J.-P., Legrand O. MRP3, BCRP, and P-Glycoprotein Activities are Prognostic Factors in Adult Acute Myeloid Leukemia. Clin. Cancer Res. 2005;11:7764–7772. doi: 10.1158/1078-0432.CCR-04-1895. [DOI] [PubMed] [Google Scholar]
- 135.Damiani D., Tiribelli M., Calistri E., Geromin A., Chiarvesio A., Michelutti A., Cavallin M., Fanin R. The prognostic value of P-glycoprotein (ABCB) and breast cancer resistance protein (ABCG2) in adults with de novo acute myeloid leukemia with normal karyotype. Haematology. 2006;91:825–828. [PubMed] [Google Scholar]
- 136.Damiani D., Tiribelli M., Michelutti A., Geromin A., Cavallin M., Fabbro D., Pianta A., Malagola M., Damante G., Russo D., et al. Fludarabine-based induction therapy does not overcome the negative effect of ABCG2 (BCRP) over-expression in adult acute myeloid leukemia patients. Leuk. Res. 2010;34:942–945. doi: 10.1016/j.leukres.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 137.Heuvel-Eibrink M.M.V.D., Wiemer E.A.C., Prins A., Meijerink J.P.P., Vossebeld P.J.M., Van Der Holt B., Pieters R., Sonneveld P. Increased expression of the breast cancer resistance protein (BCRP) in relapsed or refractory acute myeloid leukemia (AML) Leukemia. 2002;16:833–839. doi: 10.1038/sj.leu.2402496. [DOI] [PubMed] [Google Scholar]
- 138.Heuvel-Eibrink M.M.V.D., Van Der Holt B., Burnett A.K., Knauf W.U., Fey M.F., Verhoef G.E.G., Vellenga E., Ossenkoppele G.J., Löwenberg B., Sonneveld P. CD34-related coexpression of MDR1 and BCRP indicates a clinically resistant phenotype in patients with acute myeloid leukemia (AML) of older age. Ann. Hematol. 2007;86:329–337. doi: 10.1007/s00277-007-0269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Robey R.W., Polgar O., Deeken J., To K.W., Bates S.E. ABCG2: Determining its relevance in clinical drug resistance. Cancer Metastasis Rev. 2007;26:39–57. doi: 10.1007/s10555-007-9042-6. [DOI] [PubMed] [Google Scholar]
- 140.Sticova E., Jirsa M. ABCB4 disease: Many faces of one gene deficiency. Ann. Hepatol. 2020;19:126–133. doi: 10.1016/j.aohep.2019.09.010. [DOI] [PubMed] [Google Scholar]
- 141.Nikaido H. Multidrug Resistance in Bacteria. Annu. Rev. Biochem. 2009;78:119–146. doi: 10.1146/annurev.biochem.78.082907.145923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Giaccone G., Van Ark-Otte J., Rubio G.J., Gazdar A.F., Broxterman H.J., Dingemans A.-M.C., Flens M.J., Scheper R.J., Pinedo H.M. MRP is frequently expressed in human lung-cancer cell lines, in non-small-cell lung cancer and in normal lung. Int. J. Cancer. 1996;66:760–767. doi: 10.1002/(SICI)1097-0215(19960611)66:6<760::AID-IJC9>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 143.Nooter K., Bosman F.T., Burger H., Van Wingerden K.E., Flens M.J., Scheper R.J., Oostrum R.G., Boersma A.W.M., Van Der Gaast A., Stoter G. Expression of the multidrug resistance-associated protein (MRP) gene in primary non-small-cell lung cancer. Ann. Oncol. 1996;7:75–81. doi: 10.1093/oxfordjournals.annonc.a010484. [DOI] [PubMed] [Google Scholar]
- 144.Keppler D., Jedlitschky G., Leier I. Transport function and substrate specificity of multidrug resistance protein. Methods Enzymol. 1998;292:607–616. doi: 10.1016/s0076-6879(98)92047-x. [DOI] [PubMed] [Google Scholar]
- 145.Deeley R.G., Cole S.P. Substrate recognition and transport by multidrug resistance protein 1 (ABCC1) FEBS Lett. 2005;580:1103–1111. doi: 10.1016/j.febslet.2005.12.036. [DOI] [PubMed] [Google Scholar]
- 146.Do T.M., Noel-Hudson M., Ribes S., Besengez C., Smirnova M., Cisternino S., Buyse M., Calon F., Chimini G., Chacun H., et al. ABCG2- and ABCG4-mediated efflux of amyloid-beta peptide 1-40 at the mouse blood-brain barrier. J. Alzheimers Dis. 2012;30:155–166. doi: 10.3233/JAD-2012-112189. [DOI] [PubMed] [Google Scholar]
- 147.Diestra J.E., Scheffer G.L., Català I., Maliepaard M., Schellens J.H.M., Scheper R.J., Germà-Lluch J.R., Izquierdo M.A. Frequent expression of the multi-drug resistance-associated protein BCRP/MXR/ABCP/ABCG2 in human tumours detected by the BXP-21 monoclonal antibody in paraffin-embedded material. J. Pathol. 2002;198:213–219. doi: 10.1002/path.1203. [DOI] [PubMed] [Google Scholar]
- 148.Ross D.D., Karp J.E., Chen T.T., Doyle L.A. Expression of breast cancer resistance protein in blast cells from patients with acute leukemia. Blood. 2000;96:365–368. doi: 10.1182/blood.V96.1.365. [DOI] [PubMed] [Google Scholar]
- 149.Sargent J.M., Williamson C.J., Maliepaard M., Elgie A.W., Scheper R.J., Taylor C.G. Breast cancer resistance protein expression and resistance to daunorubicin in blast cells from patients with acute myeloid leukaemia. Br. J. Haematol. 2001;115:257–262. doi: 10.1046/j.1365-2141.2001.03122.x. [DOI] [PubMed] [Google Scholar]
- 150.van der Kolk D.M., Vellenga E., Scheffer G.L., Müller M., Bates S.E., Scheper R.J., de Vries E.G.E. Expression and activity of breast cancer resistance protein (BCRP) in de novo and relapsed acute myeloid leukemia. Blood. 2002;99:3763–3770. doi: 10.1182/blood.V99.10.3763. [DOI] [PubMed] [Google Scholar]
- 151.Steinbach D., Sell W., Voigt A., Hermann J., Zintl F., Sauerbrey A. BCRP gene expression is associated with a poor response to remission induction therapy in childhood acute myeloid leukemia. Leukemia. 2002;16:1443–1447. doi: 10.1038/sj.leu.2402541. [DOI] [PubMed] [Google Scholar]
- 152.van Herwaarden A.E., Wagenaar E., Merino G., Jonker J.W., Rosing H., Beijnen J.H., Schinkel A.H. Multidrug transporter ABCG2/breast cancer resistance protein secretes riboflavin (vitamin B2) into milk. Mol. Cell Biol. 2007;27:1247–1253. doi: 10.1128/MCB.01621-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Robey R.W., To K.K., Polgar O., Dohse M., Fetsch P., Dean M., Bates S.E. ABCG2: A perspective. Adv. Drug Deliv. Rev. 2009;61:3–13. doi: 10.1016/j.addr.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Robey R.W., Ierano C., Zhan Z., Bates S.E. The challenge of exploiting ABCG2 in the clinic. Curr. Pharm. Biotechnol. 2011;12:595–608. doi: 10.2174/138920111795163913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Tarr P.T., Tarling E.J., Bojanic D.D., Edwards P.A. Baldán, Ángel Emerging new paradigms for ABCG transporters. Biochim. Biophys. Acta (BBA) Mol. Cell Biol. Lipids. 2009;1791:584–593. doi: 10.1016/j.bbalip.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Patel S.B., Graf G.A., Temel R.E. Thematic Review Series: Lipid Transfer Proteins ABCG5 and ABCG8: More than a defense against xenosterols. J. Lipid Res. 2018;59:1103–1113. doi: 10.1194/jlr.R084244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Khunweeraphong N., Mitchell-White J., Szöllősi D., Hussein T., Kuchler K., Kerr I.D., Stockner T., Lee J. Picky ABCG5/G8 and promiscuous ABCG2 - a tale of fatty diets and drug toxicity. FEBS Lett. 2020;594:4035–4058. doi: 10.1002/1873-3468.13938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jacquier N., Schneiter R. Mechanisms of sterol uptake and transport in yeast. J. Steroid Biochem. Mol. Biol. 2012;129:70–78. doi: 10.1016/j.jsbmb.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 159.Wang F., Li G., Gu H.-M., Zhang D.-W. Characterization of the Role of a Highly Conserved Sequence in ATP Binding Cassette Transporter G (ABCG) Family in ABCG1 Stability, Oligomerization, and Trafficking. Biochemistry. 2013;52:9497–9509. doi: 10.1021/bi401285j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hegyi Z., Homolya L. Functional Cooperativity between ABCG4 and ABCG1 Isoforms. PLoS ONE. 2016;11:e0156516. doi: 10.1371/journal.pone.0156516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Tarling E.J., Edwards P.A. ATP binding cassette transporter G1 (ABCG1) is an intracellular sterol transporter. Proc. Natl. Acad. Sci. USA. 2011;108:19719–19724. doi: 10.1073/pnas.1113021108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Vaughan A.M., Oram J.F. ABCA1 and ABCG1 or ABCG4 act sequentially to remove cellular cholesterol and generate cholesterol-rich HDL. J. Lipid Res. 2006;47:2433–2443. doi: 10.1194/jlr.M600218-JLR200. [DOI] [PubMed] [Google Scholar]
- 163.Dujon B., Albermann K., Aldea M., Alexandraki D., Ansorge W., Arino J., Benes V., Bohn C., Bolotin-Fukuhara M., Bordonné R., et al. The nucleotide sequence of Saccharomyces cerevisiae chromosome XV. Nat. Cell Biol. 1997;387:98–102. doi: 10.1038/387s098. [DOI] [PubMed] [Google Scholar]
- 164.Kolaczkowski M., Michel V.D.R., Cybularz-Kolaczkowska A., Soumillion J.-P., Konings W.N., André G. Anticancer Drugs, Ionophoric Peptides, and Steroids as Substrates of the Yeast Multidrug Transporter Pdr5p. J. Biol. Chem. 1996;271:31543–31548. doi: 10.1074/jbc.271.49.31543. [DOI] [PubMed] [Google Scholar]
- 165.Balzi E., Wang M., Leterme S., Van Dyck L., Goffeau A. PDR5, a novel yeast multidrug resistance conferring transporter controlled by the transcription regulator PDR1. J. Biol. Chem. 1994;269:2206–2214. doi: 10.1016/S0021-9258(17)42155-7. [DOI] [PubMed] [Google Scholar]
- 166.Bissinger P.H., Kuchler K. Molecular cloning and expression of the Saccharomyces cerevisiae STS1 gene product. A yeast ABC transporter conferring mycotoxin resistance. J. Biol. Chem. 1994;269:4180–4186. doi: 10.1016/S0021-9258(17)41760-1. [DOI] [PubMed] [Google Scholar]
- 167.Kralli A., Bohen S.P., Yamamoto K.R. LEM1, an ATP-binding-cassette transporter, selectively modulates the biological potency of steroid hormones. Proc. Natl. Acad. Sci. USA. 1995;92:4701–4705. doi: 10.1073/pnas.92.10.4701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kean L.S., Grant A.M., Angeletti C., Mahé Y., Kuchler K., Fuller R.S., Nichols J.W. Plasma Membrane Translocation of Fluorescent-labeled Phosphatidylethanolamine Is Controlled by Transcription Regulators, PDR1 and PDR3. J. Cell Biol. 1997;138:255–270. doi: 10.1083/jcb.138.2.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Mahé Y., Lemoine Y., Kuchler K. The ATP Binding Cassette Transporters Pdr5 and Snq2 of Saccharomyces cerevisiae Can Mediate Transport of Steroids in Vivo. J. Biol. Chem. 1996;271:25167–25172. doi: 10.1074/jbc.271.41.25167. [DOI] [PubMed] [Google Scholar]
- 170.Watanabe M., Mizoguchi H., Nishimura A. Disruption of the ABC transporter genes PDR5, YOR1, and SNQ2, and their participation in improved fermentative activity of a sake yeast mutant showing pleiotropic drug resistance. J. Biosci. Bioeng. 2000;89:569–576. doi: 10.1016/S1389-1723(00)80059-6. [DOI] [PubMed] [Google Scholar]
- 171.Khakhina S., Johnson S.S., Manoharlal R., Russo S.B., Blugeon C., Lemoine S., Sunshine A.B., Dunham M.J., Cowart L.A., Devaux F., et al. Control of Plasma Membrane Permeability by ABC Transporters. Eukaryot. Cell. 2015;14:442–453. doi: 10.1128/EC.00021-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Bauer B.E., Wolfger H., Kuchler K. Inventory and function of yeast ABC proteins: About sex, stress, pleiotropic drug and heavy metal resistance. Biochim. Biophys. Acta (BBA) Biomembr. 1999;1461:217–236. doi: 10.1016/S0005-2736(99)00160-1. [DOI] [PubMed] [Google Scholar]
- 173.Rockwell N.C., Wolfger H., Kuchler K., Thorner J. ABC Transporter Pdr10 Regulates the Membrane Microenvironment of Pdr12 in Saccharomyces cerevisiae. J. Membr. Biol. 2009;229:27–52. doi: 10.1007/s00232-009-9173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Parle-McDermott A.G., Hand N.J., Goulding S.E., Wolfe K.H. Sequence of 29 kb around the PDR10 locus on the right arm of Saccharomyces cerevisiae chromosome XV: Similarity to part of chromosome I. Yeast. 1996;12:999–1004. doi: 10.1002/(SICI)1097-0061(199609)12:10B<999::AID-YEA976>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 175.Wolfger H., Mahé Y., Parle-McDermott A., Delahodde A., Kuchler K. The yeast ATP binding cassette (ABC) protein genes PDR10 and PDR15 are novel targets for the Pdr1 and Pdr3 transcriptional regulators. FEBS Lett. 1997;418:269–274. doi: 10.1016/S0014-5793(97)01382-3. [DOI] [PubMed] [Google Scholar]
- 176.Purnelle B., Skala J., Goffeau A. The product of theYCR105 gene located on the chromosome III fromSaccharomyces cerevisiae presents homologies to ATP-dependent permeases. Yeast. 1991;7:867–872. doi: 10.1002/yea.320070813. [DOI] [PubMed] [Google Scholar]
- 177.Piper P., Mahé Y., Thompson S., Pandjaitan R., Holyoak C., Egner R., Mühlbauer M., Coote P., Kuchler K. The pdr12 ABC transporter is required for the development of weak organic acid resistance in yeast. EMBO J. 1998;17:4257–4265. doi: 10.1093/emboj/17.15.4257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Nygård Y., Mojzita D., Toivari M., Penttilä M., Wiebe M.G., Ruohonen L. The diverse role of Pdr12 in resistance to weak organic acids. Yeast. 2014;31:219–232. doi: 10.1002/yea.3011. [DOI] [PubMed] [Google Scholar]
- 179.Wolfger H., Mamnun Y.M., Kuchler K. The Yeast Pdr15p ATP-binding Cassette (ABC) Protein Is a General Stress Response Factor Implicated in Cellular Detoxification. J. Biol. Chem. 2004;279:11593–11599. doi: 10.1074/jbc.M311282200. [DOI] [PubMed] [Google Scholar]
- 180.Khandelwal N.K., Kaemmer P., Förster T.M., Singh A., Coste A.T., Andes D.R., Hube B., Sanglard D., Chauhan N., Kaur R., et al. Pleiotropic effects of the vacuolar ABC transporter MLT1 of Candida albicans on cell function and virulence. Biochem. J. 2016;473:1537–1552. doi: 10.1042/BCJ20160024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Vethanayagam J.G., Flower A.M. Decreased gene expression from T7 promoters may be due to impaired production of active T7 RNA polymerase. Microb. Cell Factories. 2005;4:3. doi: 10.1186/1475-2859-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Godinho C.P., Prata C.S., Pinto S., Cardoso C., Bandarra N.M., Fernandes F., Sá-Correia I. Pdr18 is involved in yeast response to acetic acid stress counteracting the decrease of plasma membrane ergosterol content and order. Sci. Rep. 2018;8:1–13. doi: 10.1038/s41598-018-26128-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Godinho C.P., Costa R., Sá-Correia I. The ABC transporter Pdr18 is required for yeast thermotolerance due to its role in ergosterol transport and plasma membrane properties. Environ. Microbiol. 2020;23:69–80. doi: 10.1111/1462-2920.15253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Henneberry A.L., Sturley S.L. Sterol homeostasis in the budding yeast, Saccharomyces cerevisiae. Semin. Cell Dev. Biol. 2005;16:155–161. doi: 10.1016/j.semcdb.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 185.Servos J., Haase E., Brendel M. Gene SNQ2 of Saccharomyces cerevislae, which confers resistance to 4-nitroquinoline-N-oxide and other chemicals, encodes a 169 kDa protein homologous to ATP-dependent permeases. Mol. Genet. Genom. 1993;236–236:214–218. doi: 10.1007/BF00277115. [DOI] [PubMed] [Google Scholar]
- 186.Decottignies A., Lambert L., Catty P., Degand H., Epping E.A., Moye-Rowley W.S., Balzi E., Goffeau A. Identification and Characterization of SNQ2, a New Multidrug ATP Binding Cassette Transporter of the Yeast Plasma Membrane. J. Biol. Chem. 1995;270:18150–18157. doi: 10.1074/jbc.270.30.18150. [DOI] [PubMed] [Google Scholar]
- 187.Akiyama K., Iwaki T., Sugimoto N., Chardwiriyapreecha S., Kawano M., Nishimoto S., Sugahara T., Sekito T., Kakinuma Y. Bfr1p is responsible for tributyltin resistance in Schizosaccharomyces pombe. J. Toxicol. Sci. 2011;36:117–120. doi: 10.2131/jts.36.117. [DOI] [PubMed] [Google Scholar]
- 188.Srinivasan V., Pierik A.J., Lill R. Crystal Structures of Nucleotide-Free and Glutathione-Bound Mitochondrial ABC Transporter Atm1. Science. 2014;343:1137–1140. doi: 10.1126/science.1246729. [DOI] [PubMed] [Google Scholar]
- 189.Leighton J., Schatz G. An ABC transporter in the mitochondrial inner membrane is required for normal growth of yeast. EMBO J. 1995;14:188–195. doi: 10.1002/j.1460-2075.1995.tb06989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kispal G., Csere P., Prohl C., Lill R. The mitochondrial proteins Atm1p and Nfs1p are essential for biogenesis of cytosolic Fe/S proteins. EMBO J. 1999;18:3981–3989. doi: 10.1093/emboj/18.14.3981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Dean M., Allikmets R., Gerrard B., Stewart C., Kistler A., Shafer B., Michaelis S., Strathern J. XIIXVI. Yeast sequencing reports. Mapping and sequencing of two yeast genes belonging to the ATP-binding cassette superfamily. Yeast. 1994;10:377–383. doi: 10.1002/yea.320100310. [DOI] [PubMed] [Google Scholar]
- 192.Young L., Leonhard K., Tatsuta T., Trowsdale J., Langer T. Role of the ABC Transporter Mdl1 in Peptide Export from Mitochondria. Science. 2001;291:2135–2138. doi: 10.1126/science.1056957. [DOI] [PubMed] [Google Scholar]
- 193.Kuchler K., Sterne R.E., Thorner J. Saccharomyces cerevisiae STE6 gene product: A novel pathway for protein export in eukaryotic cells. EMBO J. 1989;8:3973–3984. doi: 10.1002/j.1460-2075.1989.tb08580.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.McGrath J.P., Varshavsky A. The yeast STE6 gene encodes a homologue of the mammalian multidrug resistance P-glycoprotein. Nat. Cell Biol. 1989;340:400–404. doi: 10.1038/340400a0. [DOI] [PubMed] [Google Scholar]
- 195.Ortiz D.F., Kreppel L., Speiser D.M., Scheel G., McDonald G., Ow D.W. Heavy metal tolerance in the fission yeast requires an ATP-binding cassette-type vacuolar membrane transporter. EMBO J. 1992;11:3491–3499. doi: 10.1002/j.1460-2075.1992.tb05431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Ortiz D.F., Ruscitti T., McCue K.F., Ow D.W. Transport of Metal-binding Peptides by HMT1, A Fission Yeast ABC-type Vacuolar Membrane Protein. J. Biol. Chem. 1995;270:4721–4728. doi: 10.1074/jbc.270.9.4721. [DOI] [PubMed] [Google Scholar]
- 197.Christensen P.U., Davey J., Nielsen O. The Schizosaccharomyces pombe mam1 gene encodes an ABC transporter mediating secretion of M-factor. Mol. Genet. Genom. 1997;255:226–236. doi: 10.1007/s004380050493. [DOI] [PubMed] [Google Scholar]
- 198.Decottignies A., Grant A.M., Nichols J.W., de Wet H., McIntosh D.B., Goffeau A. ATPase and Multidrug Transport Activities of the Overexpressed Yeast ABC Protein Yor1p. J. Biol. Chem. 1998;273:12612–12622. doi: 10.1074/jbc.273.20.12612. [DOI] [PubMed] [Google Scholar]
- 199.Nagy Z., Montigny C., Leverrier P., Yeh S., Goffeau A., Garrigos M., Falson P. Role of the yeast ABC transporter Yor1p in cadmium detoxification. Biochimie. 2006;88:1665–1671. doi: 10.1016/j.biochi.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 200.Katzmann D.J., Hallstrom T.C., Voet M., Wysock W., Golin J., Volckaert G., Moye-Rowley W.S. Expression of an ATP-binding cassette transporter-encoding gene (YOR1) is required for oligomycin resistance in Saccharomyces cerevisiae. Mol. Cell. Biol. 1995;15:6875–6883. doi: 10.1128/MCB.15.12.6875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Falcón-Pérez J.M., Martínez-Burgos M., Molano J., Mazón M.J., Eraso P. Domain Interactions in the Yeast ATP Binding Cassette Transporter Ycf1p: Intragenic Suppressor Analysis of Mutations in the Nucleotide Binding Domains. J. Bacteriol. 2001;183:4761–4770. doi: 10.1128/JB.183.16.4761-4770.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Sasser T.L., Lawrence G., Karunakaran S., Brown C., Fratti R.A. The Yeast ATP-binding Cassette (ABC) Transporter Ycf1p Enhances the Recruitment of the Soluble SNARE Vam7p to Vacuoles for Efficient Membrane Fusion. J. Biol. Chem. 2013;288:18300–18310. doi: 10.1074/jbc.M112.441089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Gulshan K., Moye-Rowley W.S. Vacuolar Import of Phosphatidylcholine Requires the ATP-Binding Cassette Transporter Ybt1. Traffic. 2011;12:1257–1268. doi: 10.1111/j.1600-0854.2011.01228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Wawrzycka D., Sobczak I., Bartosz G., Bocer T., Ułaszewski S., Goffeau A. Vmr 1p is a novel vacuolar multidrug resistance ABC transporter in Saccharomyces cerevisiae. FEMS Yeast Res. 2010;10:828–838. doi: 10.1111/j.1567-1364.2010.00673.x. [DOI] [PubMed] [Google Scholar]
- 205.Klein M., Mamnun Y.M., Eggmann T., Schüller C., Wolfger H., Martinoia E., Kuchler K. The ATP-binding cassette (ABC) transporter Bpt1p mediates vacuolar sequestration of glutathione conjugates in yeast. FEBS Lett. 2002;520:63–67. doi: 10.1016/S0014-5793(02)02767-9. [DOI] [PubMed] [Google Scholar]
- 206.Durmus S., Hendrikx J.J., Schinkel A.H. Apical ABC Transporters and Cancer Chemotherapeutic Drug Disposition. Adv. Cancer Res. 2015;125:1–41. doi: 10.1016/bs.acr.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 207.Jones P.M., George A.M. Is the emperor wearing shorts? The published structures of ABC transporters. FEBS Lett. 2020;594:3790–3798. doi: 10.1002/1873-3468.13941. [DOI] [PubMed] [Google Scholar]
- 208.El-Awady R., Saleh E., Hashim A., Soliman N., Dallah A., Elrasheed A., Elakraa G. The Role of Eukaryotic and Prokaryotic ABC Transporter Family in Failure of Chemotherapy. Front. Pharmacol. 2017;7:535. doi: 10.3389/fphar.2016.00535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Orelle C., Mathieu K., Jault J.-M. Multidrug ABC transporters in bacteria. Res. Microbiol. 2019;170:381–391. doi: 10.1016/j.resmic.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 210.Lubelski J., Konings W.N., Driessen A.J.M. Distribution and Physiology of ABC-Type Transporters Contributing to Multidrug Resistance in Bacteria. Microbiol. Mol. Biol. Rev. 2007;71:463–476. doi: 10.1128/MMBR.00001-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Du D., Wang-Kan X., Neuberger A., Van Veen H.W., Pos K.M., Piddock L.J.V., Luisi B.F. Multidrug efflux pumps: Structure, function and regulation. Nat. Rev. Genet. 2018;16:523–539. doi: 10.1038/s41579-018-0048-6. [DOI] [PubMed] [Google Scholar]
- 212.Piddock L.J.V. Clinically Relevant Chromosomally Encoded Multidrug Resistance Efflux Pumps in Bacteria. Clin. Microbiol. Rev. 2006;19:382–402. doi: 10.1128/CMR.19.2.382-402.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Sipos G., Kuchler K. Fungal ATP-binding cassette (ABC) transporters in drug resistance & detoxification. Curr. Drug Targets. 2006;7:471–481. doi: 10.2174/138945006776359403. [DOI] [PubMed] [Google Scholar]
- 214.Jungwirth H., Kuchler K. Yeast ABC transporters—A tale of sex, stress, drugs and aging. FEBS Lett. 2005;580:1131–1138. doi: 10.1016/j.febslet.2005.12.050. [DOI] [PubMed] [Google Scholar]
- 215.Gulshan K., Moye-Rowley W.S. Multidrug Resistance in Fungi. Eukaryot. Cell. 2007;6:1933–1942. doi: 10.1128/EC.00254-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Golin J., Ambudkar S.V. The multidrug transporter Pdr5 on the 25th anniversary of its discovery: An important model for the study of asymmetric ABC transporters. Biochem. J. 2015;467:353–363. doi: 10.1042/BJ20150042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Sanglard D., Kuchler K., Ischer F., Pagani J.L., Monod M., Bille J. Mechanisms of resistance to azole antifungal agents in Candida albicans isolates from AIDS patients involve specific multidrug transporters. Antimicrob. Agents Chemother. 1995;39:2378–2386. doi: 10.1128/AAC.39.11.2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Sanglard D., Ischer F., Monod M., Bille J. Susceptibilities of Candida albicans multidrug transporter mutants to various antifungal agents and other metabolic inhibitors. Antimicrob. Agents Chemother. 1996;40:2300–2305. doi: 10.1128/AAC.40.10.2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Prasad R., Rawal M.K. Efflux pump proteins in antifungal resistance. Front. Pharmacol. 2014;5:202. doi: 10.3389/fphar.2014.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.McDaniel A.L., Alger H.M., Sawyer J.K., Kelley K.L., Kock N.D., Brown J.M., Temel R.E., Rudel L.L. Phytosterol Feeding Causes Toxicity in ABCG5/G8 Knockout Mice. Am. J. Pathol. 2013;182:1131–1138. doi: 10.1016/j.ajpath.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Brown G.D., Denning D.W., Gow N.A.R., Levitz S.M., Netea M.G., White T.C. Hidden Killers: Human Fungal Infections. Sci. Transl. Med. 2012;4:165. doi: 10.1126/scitranslmed.3004404. [DOI] [PubMed] [Google Scholar]
- 222.Kullberg B.J., Arendrup M.C. Invasive Candidiasis. N. Engl. J. Med. 2015;373:1445–1456. doi: 10.1056/NEJMra1315399. [DOI] [PubMed] [Google Scholar]
- 223.Iliev I.D., Underhill D.M. Striking a balance: Fungal commensalism versus pathogenesis. Curr. Opin. Microbiol. 2013;16:366–373. doi: 10.1016/j.mib.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Hurabielle C., Link V.M., Bouladoux N., Han S.-J., Merrill E.D., Lightfoot Y.L., Seto N., Bleck C.K.E., Smelkinson M., Harrison O.J., et al. Immunity to commensal skin fungi promotes psoriasiform skin inflammation. Proc. Natl. Acad. Sci. USA. 2020;117:16465–16474. doi: 10.1073/pnas.2003022117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Chen Y.E., Fischbach M.A., Belkaid Y. Erratum: Skin microbiota–host interactions. Nat. Cell Biol. 2018;555:543. doi: 10.1038/nature25994. [DOI] [PubMed] [Google Scholar]
- 226.Chen Y.E., Fischbach M.A., Belkaid Y. Skin microbiota-host interactions. Nature. 2018;553:427–436. doi: 10.1038/nature25177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Mao K., Baptista A.P., Tamoutounour S., Zhuang L., Bouladoux N., Martins A.J., Huang Y., Gerner M.Y., Belkaid Y., Germain R.N. Innate and adaptive lymphocytes sequentially shape the gut microbiota and lipid metabolism. Nat. Cell Biol. 2018;554:255–259. doi: 10.1038/nature25437. [DOI] [PubMed] [Google Scholar]
- 228.Byrd A.L., Belkaid Y., Segre J.A. The human skin microbiome. Nat. Rev. Microbiol. 2018;16:143–155. doi: 10.1038/nrmicro.2017.157. [DOI] [PubMed] [Google Scholar]
- 229.Linehan J.L., Harrison O.J., Han S.-J., Byrd A.L., Vujkovic-Cvijin I., Villarino A.V., Sen S.K., Shaik J., Smelkinson M., Tamoutounour S., et al. Non-classical Immunity Controls Microbiota Impact on Skin Immunity and Tissue Repair. Cell. 2018;172:784–796.e18. doi: 10.1016/j.cell.2017.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Pfaller M.A., Huband M.D., Flamm R.K., Bien P.A., Castanheira M. In Vitro Activity of APX001A (Manogepix) and Comparator Agents against 1706 Fungal Isolates Collected during an International Surveillance Program in 2017. Antimicrob. Agents Chemother. 2019;63 doi: 10.1128/AAC.00840-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Perfect J.R. The antifungal pipeline: A reality check. Nat. Rev. Drug Discov. 2017;16:603–616. doi: 10.1038/nrd.2017.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Satoh K., Makimura K., Hasumi Y., Nishiyama Y., Uchida K., Yamaguchi H. Candida aurissp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol. Immunol. 2009;53:41–44. doi: 10.1111/j.1348-0421.2008.00083.x. [DOI] [PubMed] [Google Scholar]
- 233.Chowdhary A., Sharma C., Meis J.F. Candida auris: A rapidly emerging cause of hospital-acquired multidrug-resistant fungal infections globally. PLoS Pathog. 2017;13:e1006290. doi: 10.1371/journal.ppat.1006290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Lockhart S.R., Etienne K.A., Vallabhaneni S., Farooqi J., Chowdhary A., Govender N.P., Colombo A.L., Calvo B., Cuomo C.A., Desjardins C.A., et al. Simultaneous Emergence of Multidrug-Resistant Candida auris on 3 Continents Confirmed by Whole-Genome Sequencing and Epidemiological Analyses. Clin. Infect. Dis. 2017;64:134–140. doi: 10.1093/cid/ciw691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Arendrup M.C., Patterson T.F. Multidrug-Resistant Candida: Epidemiology, Molecular Mechanisms, and Treatment. J. Infect. Dis. 2017;216(Suppl. 3):S445–S451. doi: 10.1093/infdis/jix131. [DOI] [PubMed] [Google Scholar]
- 236.Kwon Y.J., Shin J.H., Byun S.A., Choi M.J., Won E.J., Lee D., Lee S.Y., Chun S., Lee J.H., Choi H.J., et al. Candida auris Clinical Isolates from South Korea: Identification, Antifungal Susceptibility, and Genotyping. J. Clin. Microbiol. 2019;57 doi: 10.1128/JCM.01624-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Rybak J.M., Doorley L.A., Nishimoto A.T., Barker K.S., Palmer G.E., Rogers P.D. Abrogation of Triazole Resistance upon Deletion of CDR1 in a Clinical Isolate of Candida auris. Antimicrob. Agents Chemother. 2019;63 doi: 10.1128/AAC.00057-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Torres S.R., Kim H.C., Leach L., Chaturvedi S., Bennett C.J., Hill D.J., De Jesus M. Assessment of environmental and occupational exposure while working with multidrug resistant (MDR) fungus Candida auris in an animal facility. J. Occup. Environ. Hyg. 2019;16:507–518. doi: 10.1080/15459624.2019.1594840. [DOI] [PubMed] [Google Scholar]
- 239.Kim S.H., Iyer K.R., Pardeshi L., Muñoz J.F., Robbins N., Cuomo C.A., Wong K.H., Cowen L.E. Genetic Analysis of Candida auris Implicates Hsp90 in Morphogenesis and Azole Tolerance and Cdr1 in Azole Resistance. mBio. 2019;10:e02529-18. doi: 10.1128/mBio.02529-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Meis J.F., Chowdhary A. Candida auris: A global fungal public health threat. Lancet Infect. Dis. 2018;18:1298–1299. doi: 10.1016/S1473-3099(18)30609-1. [DOI] [PubMed] [Google Scholar]
- 241.Colombo A.L., Júnior J.N.D.A., Guinea J. Emerging multidrug-resistant Candida species. Curr. Opin. Infect. Dis. 2017;30:528–538. doi: 10.1097/QCO.0000000000000411. [DOI] [PubMed] [Google Scholar]
- 242.Villanueva-Lozano H., Treviño-Rangel R.D.J., González G.M., Ramírez-Elizondo M.T., Lara-Medrano R., Aleman-Bocanegra M.C., Guajardo-Lara C.E., Gaona-Chávez N., Castilleja-Leal F., Torre-Amione G., et al. Outbreak of Candida auris infection in a COVID-19 hospital in Mexico. Clin. Microbiol. Infect. 2021 doi: 10.1016/j.cmi.2020.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Hameed H.M.A., Islam M.M., Chhotaray C., Wang C., Liu Y., Tan Y., Li X., Tan S., Delorme V., Yew W.W., et al. Molecular Targets Related Drug Resistance Mechanisms in MDR-, XDR-, and TDR-Mycobacterium tuberculosis Strains. Front. Cell. Infect. Microbiol. 2018;8:114. doi: 10.3389/fcimb.2018.00114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Healey K.R., Perlin D.S. Fungal Resistance to Echinocandins and the MDR Phenomenon in Candida glabrata. J. Fungi. 2018;4:105. doi: 10.3390/jof4030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Klein C., Kuchler K., Valachovic M. ABC proteins in yeast and fungal pathogens. Essays Biochem. 2011;50:101–119. doi: 10.1042/bse0500101. [DOI] [PubMed] [Google Scholar]
- 246.Sanglard D. Emerging Threats in Antifungal-Resistant Fungal Pathogens. Front. Med. 2016;3:11. doi: 10.3389/fmed.2016.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Jenull S.T., Kashko M.N., Shivarathri R., Stoiber A., Chauhan M., Petryshyn A., Chauhan N., Kuchler K. Transcriptiome Signatures Predict Phenotypic Variations of Candida auris. Front. Microbiol. Infect. Dis. 2021 doi: 10.3389/fcimb.2021.662563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Kovalchuk A., Driessen A.J.M. Phylogenetic analysis of fungal ABC transporters. BMC Genom. 2010;11:177. doi: 10.1186/1471-2164-11-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Buechel E.R., Pinkett H.W. Transcription factors and ABC transporters: From pleiotropic drug resistance to cellular signaling in yeast. FEBS Lett. 2020;594:3943–3964. doi: 10.1002/1873-3468.13964. [DOI] [PubMed] [Google Scholar]
- 250.Kumari S., Kumar M., Gaur N.A., Prasad R. Multiple roles of ABC transporters in yeast. Fungal Genet. Biol. 2021;150:103550. doi: 10.1016/j.fgb.2021.103550. [DOI] [PubMed] [Google Scholar]
- 251.Moreno A., Banerjee A., Prasad R., Falson P. PDR-like ABC systems in pathogenic fungi. Res. Microbiol. 2019;170:417–425. doi: 10.1016/j.resmic.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 252.Loftus B.J., Fung E., Roncaglia P., Rowley D., Amedeo P., Bruno D., Vamathevan J., Miranda M., Anderson I.J., Fraser J.A., et al. The Genome of the Basidiomycetous Yeast and Human Pathogen Cryptococcus neoformans. Science. 2005;307:1321–1324. doi: 10.1126/science.1103773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Nierman W.C., Pain A., Anderson M.J., Wortman J.R., Kim H.S., Arroyo J., Berriman M., Abe K., Archer D.B., Bermejo C., et al. Genomic sequence of the pathogenic and allergenic filamentous fungus Aspergillus fumigatus. Nat. Cell Biol. 2005;438:1151–1156. doi: 10.1038/nature04332. [DOI] [PubMed] [Google Scholar]
- 254.Szczypka M.S., Wemmie J.A., Moye-Rowley W.S., Thiele D.J. A yeast metal resistance protein similar to human cystic fibrosis transmembrane conductance regulator (CFTR) and multidrug resistance-associated protein. J. Biol. Chem. 1994;269:22853–22857. doi: 10.1016/S0021-9258(17)31723-4. [DOI] [PubMed] [Google Scholar]
- 255.Lee Y.H., Kang H.-M., Kim M.-S., Lee J.-S., Jeong C.-B., Lee J.-S. The protective role of multixenobiotic resistance (MXR)-mediated ATP-binding cassette (ABC) transporters in biocides-exposed rotifer Brachionus koreanus. Aquat. Toxicol. 2018;195:129–136. doi: 10.1016/j.aquatox.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 256.Taylor N.M.I., Manolaridis I., Jackson S.M., Kowal J., Stahlberg H., Locher K.P. Structure of the human multidrug transporter ABCG2. Nat. Cell Biol. 2017;546:504–509. doi: 10.1038/nature22345. [DOI] [PubMed] [Google Scholar]
- 257.Jackson S.M., Manolaridis I., Kowal J., Zechner M., Taylor N.M.I., Bause M., Bauer S., Bartholomaeus R., Bernhardt G., Koenig B., et al. Structural basis of small-molecule inhibition of human multidrug transporter ABCG2. Nat. Struct. Mol. Biol. 2018;25:333–340. doi: 10.1038/s41594-018-0049-1. [DOI] [PubMed] [Google Scholar]
- 258.Manolaridis I., Jackson S.M., Taylor N.M.I., Kowal J., Stahlberg H., Locher K.P. Cryo-EM structures of a human ABCG2 mutant trapped in ATP-bound and substrate-bound states. Nat. Cell Biol. 2018;563:426–430. doi: 10.1038/s41586-018-0680-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Orlando B.J., Liao M. ABCG2 transports anticancer drugs via a closed-to-open switch. Nat. Commun. 2020;11:1–11. doi: 10.1038/s41467-020-16155-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Smriti, Krishnamurthy S., Dixit B.L., Gupta C.M., Milewski S., Prasad R. ABC transporters Cdr1p, Cdr2p and Cdr3p of a human pathogen Candida albicans are general phospholipid translocators. Yeast. 2002;19:303–318. doi: 10.1002/yea.818. [DOI] [PubMed] [Google Scholar]
- 261.Wu C.-P., Hsieh C.-H., Wu Y.-S. The Emergence of Drug Transporter-Mediated Multidrug Resistance to Cancer Chemotherapy. Mol. Pharm. 2011;8:1996–2011. doi: 10.1021/mp200261n. [DOI] [PubMed] [Google Scholar]
- 262.Sanglard D., Ischer F., Monod M., Bille J. Cloning of Candida albicans genes conferring resistance to azole antifungal agents: Characterization of CDR2, a new multidrug ABC transporter gene. Microbiology. 1997;143:405–416. doi: 10.1099/00221287-143-2-405. [DOI] [PubMed] [Google Scholar]
- 263.Prasad R., De Wergifosse P., Goffeau A., Balzi E. Molecular cloning and characterization of a novel gene of Candida albicans, CDR1, conferring multiple resistance to drugs and antifungals. Curr. Genet. 1995;27:320–329. doi: 10.1007/BF00352101. [DOI] [PubMed] [Google Scholar]
- 264.Smits S.H., Schmitt L., Beis K. Self-immunity to antibacterial peptides by ABC transporters. FEBS Lett. 2020;594:3920–3942. doi: 10.1002/1873-3468.13953. [DOI] [PubMed] [Google Scholar]
- 265.Lewinson O., Orelle C., Seeger M.A. Structures of ABC transporters: Handle with care. FEBS Lett. 2020;594:3799–3814. doi: 10.1002/1873-3468.13966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Lewinson O., Livnat-Levanon N. Mechanism of Action of ABC Importers: Conservation, Divergence, and Physiological Adaptations. J. Mol. Biol. 2017;429:606–619. doi: 10.1016/j.jmb.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 267.Hernaez M.L., Gil C., Pla J., Nombela C. Induced expression of the Candida albicans multidrug resistance gene CDR1 in response to fluconazole and other antifungals. Yeast. 1998;14:517–526. doi: 10.1002/(SICI)1097-0061(19980430)14:6<517::AID-YEA250>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 268.Krishnamurthy S., Gupta V., Prasad R., Panwar S.L., Prasad R. Expression of CDR1, a multidrug resistance gene of Candida albicans: Transcriptional activation by heat shock, drugs and human steroid hormones. FEMS Microbiol. Lett. 1998;160:191–197. doi: 10.1111/j.1574-6968.1998.tb12910.x. [DOI] [PubMed] [Google Scholar]
- 269.Shukla S., Saini P., Smriti, Jha S., Ambudkar S.V., Prasad R. Functional Characterization of Candida albicans ABC Transporter Cdr1p. Eukaryot. Cell. 2003;2:1361–1375. doi: 10.1128/EC.2.6.1361-1375.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Larsen B., Anderson S., Brockman A., Essmann M., Schmidt M. Key physiological differences inCandida albicans CDR1 induction by steroid hormones and antifungal drugs. Yeast. 2006;23:795–802. doi: 10.1002/yea.1394. [DOI] [PubMed] [Google Scholar]
- 271.Lamping E., Monk B.C., Niimi K., Holmes A.R., Tsao S., Tanabe K., Niimi M., Uehara Y., Cannon R.D. Characterization of Three Classes of Membrane Proteins Involved in Fungal Azole Resistance by Functional Hyperexpression in Saccharomyces cerevisiae. Eukaryot. Cell. 2007;6:1150–1165. doi: 10.1128/EC.00091-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Balan I., Alarco A.M., Raymond M. The Candida albicans CDR3 gene codes for an opaque-phase ABC transporter. J. Bacteriol. 1997;179:7210–7218. doi: 10.1128/JB.179.23.7210-7218.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Khandelwal N.K., Chauhan N., Sarkar P., Esquivel B.D., Coccetti P., Singh A., Coste A.T., Gupta M., Sanglard D., White T.C., et al. Azole resistance in a Candida albicans mutant lacking the ABC transporter CDR6/ROA1 depends on TOR signaling. J. Biol. Chem. 2018;293:412–432. doi: 10.1074/jbc.M117.807032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Liston S.D., Whitesell L., Kapoor M., Shaw K.J., Cowen L.E. Enhanced Efflux Pump Expression in Candida Mutants Results in Decreased Manogepix Susceptibility. Antimicrob. Agents Chemother. 2020;64 doi: 10.1128/AAC.00261-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Sanglard D., Ischer F., Calabrese D., Majcherczyk P.A., Bille J. The ATP binding cassette transporter gene CgCDR1 from Candida glabrata is involved in the resistance of clinical isolates to azole antifungal agents. Antimicrob. Agents Chemother. 1999;43:2753–2765. doi: 10.1128/AAC.43.11.2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Song J.W., Shin J.H., Kee S.J., Kim S.H., Shin M.G., Suh S.P., Ryang D.W. Expression of CgCDR1, CgCDR2, and CgERG11 in Candida glabrata biofilms formed by bloodstream isolates. Med. Mycol. 2009;47:545–548. doi: 10.1080/13693780802210726. [DOI] [PubMed] [Google Scholar]
- 277.Miyazaki H., Miyazaki Y., Geber A., Parkinson T., Hitchcock C., Falconer D.J., Ward D.J., Marsden K., Bennett J.E. Fluconazole Resistance Associated with Drug Efflux and Increased Transcription of a Drug Transporter Gene, PDH1, inCandida glabrata. Antimicrob. Agents Chemother. 1998;42:1695–1701. doi: 10.1128/AAC.42.7.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Izumikawa K., Kakeya H., Tsai H.-F., Grimberg B., Bennett J.E. Function ofCandida glabrata ABC transporter gene, PDH1. Yeast. 2003;20:249–261. doi: 10.1002/yea.962. [DOI] [PubMed] [Google Scholar]
- 279.Torelli R., Posteraro B., Ferrari S., La Sorda M., Fadda G., Sanglard D., Sanguinetti M. The ATP-binding cassette transporter–encoding gene CgSNQ2 is contributing to the CgPDR1-dependent azole resistance of Candida glabrata. Mol. Microbiol. 2008;68:186–201. doi: 10.1111/j.1365-2958.2008.06143.x. [DOI] [PubMed] [Google Scholar]
- 280.Zavrel M., Hoot S.J., White T.C. Comparison of Sterol Import under Aerobic and Anaerobic Conditions in Three Fungal Species, Candida albicans, Candida glabrata, and Saccharomyces cerevisiae. Eukaryot. Cell. 2013;12:725–738. doi: 10.1128/EC.00345-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Nakayama H., Tanabe K., Bard M., Hodgson W., Wu S., Takemori D., Aoyama T., Kumaraswami N.S., Metzler L., Takano Y., et al. The Candida glabrata putative sterol transporter gene CgAUS1 protects cells against azoles in the presence of serum. J. Antimicrob. Chemother. 2007;60:1264–1272. doi: 10.1093/jac/dkm321. [DOI] [PubMed] [Google Scholar]
- 282.Moran G., Sullivan D., Morschhauser J., Coleman D. The Candida dubliniensis CdCDR1 Gene Is Not Essential for Fluconazole Resistance. Antimicrob. Agents Chemother. 2002;46:2829–2841. doi: 10.1128/AAC.46.9.2829-2841.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Silva S., Hooper S., Henriques M., Oliveira R., Azeredo J., Williams D. The role of secreted aspartyl proteinases in Candida tropicalis invasion and damage of oral mucosa. Clin. Microbiol. Infect. 2011;17:264–272. doi: 10.1111/j.1469-0691.2010.03248.x. [DOI] [PubMed] [Google Scholar]
- 284.Silva S., Negri M., Henriques M., Oliveira R., Williams D.W., Azeredo J. Candida glabrata, Candida parapsilosis and Candida tropicalis: Biology, epidemiology, pathogenicity and antifungal resistance. FEMS Microbiol. Rev. 2012;36:288–305. doi: 10.1111/j.1574-6976.2011.00278.x. [DOI] [PubMed] [Google Scholar]
- 285.Zuza-Alves D.L., Silva-Rocha W.P., Chaves G.M. An Update on Candida tropicalis Based on Basic and Clinical Approaches. Front. Microbiol. 2017;8:1927. doi: 10.3389/fmicb.2017.01927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Sanguinetti M., Posteraro B., La Sorda M., Torelli R., Fiori B., Santangelo R., Delogu G., Fadda G. Role of AFR1, an ABC Transporter-Encoding Gene, in the In Vivo Response to Fluconazole and Virulence of Cryptococcus neoformans. Infect. Immun. 2006;74:1352–1359. doi: 10.1128/IAI.74.2.1352-1359.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Raymond M., Gros P., Whiteway M., Thomas D.Y. Functional complementation of yeast ste6 by a mammalian multidrug resistance mdr gene. Science. 1992;256:232–234. doi: 10.1126/science.1348873. [DOI] [PubMed] [Google Scholar]
- 288.Bennett R.J., Uhl M.A., Miller M.G., Johnson A.D. Identification and Characterization of a Candida albicans Mating Pheromone. Mol. Cell. Biol. 2003;23:8189–8201. doi: 10.1128/MCB.23.22.8189-8201.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Schwarzmuller T., Ma B., Hiller E., Istel F., Tscherner M., Brunke S., Ames L., Firon A., Green B., Cabral V., et al. Systematic phenotyping of a large-scale Candida glabrata deletion collection reveals novel antifungal tolerance genes. PLoS Pathog. 2014;10:e1004211. doi: 10.1371/journal.ppat.1004211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Chang M., Sionov E., Lamichhane A.K., Kwon-Chung K.J., Chang Y.C. Roles of Three Cryptococcus neoformans and Cryptococcus gattii Efflux Pump-Coding Genes in Response to Drug Treatment. Antimicrob. Agents Chemother. 2018;62:e01751-17. doi: 10.1128/AAC.01751-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Ramírez-Zavala B., Manz H., Englert F., Rogers P.D., Morschhäuser J. A Hyperactive Form of the Zinc Cluster Transcription Factor Stb5 CausesYOR1Overexpression and Beauvericin Resistance inCandida albicans. Antimicrob. Agents Chemother. 2018;62 doi: 10.1128/AAC.01655-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Shekhar-Guturja T., Tebung W.A., Mount H., Liu N., Köhler J.R., Whiteway M., Cowen L.E. Beauvericin Potentiates Azole Activity via Inhibition of Multidrug Efflux, BlocksC. albicansMorphogenesis, and is Effluxed via Yor1 and Circuitry Controlled by Zcf29. Antimicrob. Agents Chemother. 2016;60:AAC.01959-16. doi: 10.1128/AAC.01959-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Dawson R.J.P., Locher K.P. Structure of a bacterial multidrug ABC transporter. Nat. Cell Biol. 2006;443:180–185. doi: 10.1038/nature05155. [DOI] [PubMed] [Google Scholar]
- 294.Locher K.P. Structure and mechanism of ATP-binding cassette transporters. Philos. Trans. R. Soc. B Biol. Sci. 2008;364:239–245. doi: 10.1098/rstb.2008.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Kodan A., Yamaguchi T., Nakatsu T., Matsuoka K., Kimura Y., Ueda K., Kato H. Inward- and outward-facing X-ray crystal structures of homodimeric P-glycoprotein CmABCB1. Nat. Commun. 2019;10:1–12. doi: 10.1038/s41467-018-08007-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Thonghin N., Collins R.F., Barbieri A., Shafi T., Siebert A., Ford R.C. Novel features in the structure of P-glycoprotein (ABCB1) in the post-hydrolytic state as determined at 7.9 Å resolution. BMC Struct. Biol. 2018;18:1–11. doi: 10.1186/s12900-018-0098-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Beis K. Structural basis for the mechanism of ABC transporters. Biochem. Soc. Trans. 2015;43:889–893. doi: 10.1042/BST20150047. [DOI] [PubMed] [Google Scholar]
- 298.Johnson Z.L., Chen J. Structural Basis of Substrate Recognition by the Multidrug Resistance Protein MRP1. Cell. 2017;168:1075–1085.e9. doi: 10.1016/j.cell.2017.01.041. [DOI] [PubMed] [Google Scholar]
- 299.Szakács G., Jakab K., Antal F., Sarkadi B. Diagnostics of multidrug resistance in cancer. Pathol. Oncol. Res. 1998;4:251–257. doi: 10.1007/BF02905214. [DOI] [PubMed] [Google Scholar]
- 300.Liu F., Zhang Z., Csanády L., Gadsby D.C., Chen J. Molecular Structure of the Human CFTR Ion Channel. Cell. 2017;169:85–95.e8. doi: 10.1016/j.cell.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 301.Zhang Z., Chen J. Atomic Structure of the Cystic Fibrosis Transmembrane Conductance Regulator. Cell. 2016;167:1586–1597.e9. doi: 10.1016/j.cell.2016.11.014. [DOI] [PubMed] [Google Scholar]
- 302.Jin M.S., Oldham M.L., Zhang Q., Chen J. Crystal structure of the multidrug transporter P-glycoprotein from Caenorhabditis elegans. Nat. Cell Biol. 2012;490:566–569. doi: 10.1038/nature11448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Li J., Jaimes K.F., Aller S.G. Refined structures of mouse P-glycoprotein. Protein Sci. 2014;23:34–46. doi: 10.1002/pro.2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Szewczyk P., Tao H., McGrath A.P., Villaluz M., Rees S.D., Lee S.C., Doshi R., Urbatsch I.L., Zhang Q., Chang G. Snapshots of ligand entry, malleable binding and induced helical movement in P-glycoprotein. Acta Crystallogr. Sect. D Biol. Crystallogr. 2015;71:732–741. doi: 10.1107/S1399004715000978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Nicklisch S.C.T., Rees S.D., McGrath A.P., Gökirmak T., Bonito L.T., Vermeer L.M., Cregger C., Loewen G., Sandin S., Chang G., et al. Global marine pollutants inhibit P-glycoprotein: Environmental levels, inhibitory effects, and cocrystal structure. Sci. Adv. 2016;2:e1600001. doi: 10.1126/sciadv.1600001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Esser L., Zhou F., Pluchino K.M., Shiloach J., Ma J., Tang W.-K., Gutierrez C., Zhang A., Shukla S., Madigan J.P., et al. Structures of the Multidrug Transporter P-glycoprotein Reveal Asymmetric ATP Binding and the Mechanism of Polyspecificity. J. Biol. Chem. 2017;292:446–461. doi: 10.1074/jbc.M116.755884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Kim Y., Chen J. Molecular structure of human P-glycoprotein in the ATP-bound, outward-facing conformation. Science. 2018;359:915–919. doi: 10.1126/science.aar7389. [DOI] [PubMed] [Google Scholar]
- 308.Alam A., Kowal J., Broude E., Roninson I., Locher K.P. Structural insight into substrate and inhibitor discrimination by human P-glycoprotein. Science. 2019;363:753–756. doi: 10.1126/science.aav7102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Alam A., Kung R., Kowal J., McLeod R.A., Tremp N., Broude E.V., Roninson I.B., Stahlberg H., Locher K.P. Structure of a zosuquidar and UIC2-bound human-mouse chimeric ABCB1. Proc. Natl. Acad. Sci. USA. 2018;115:E1973–E1982. doi: 10.1073/pnas.1717044115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Aller S.G., Yu J., Ward A., Weng Y., Chittaboina S., Zhuo R., Harrell P.M., Trinh Y.T., Zhang Q., Urbatsch I.L., et al. Structure of P-Glycoprotein Reveals a Molecular Basis for Poly-Specific Drug Binding. Science. 2009;323:1718–1722. doi: 10.1126/science.1168750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Johnson Z.L., Chen J. ATP Binding Enables Substrate Release from Multidrug Resistance Protein 1. Cell. 2018;172:81–89.e10. doi: 10.1016/j.cell.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 312.Wang L., Johnson Z.L., Wasserman M.R., Levring J., Chen J., Liu S. Characterization of the kinetic cycle of an ABC transporter by single-molecule and cryo-EM analyses. eLife. 2020;9:9. doi: 10.7554/eLife.56451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Zhang Z., Liu F., Chen J. Conformational Changes of CFTR upon Phosphorylation and ATP Binding. Cell. 2017;170:483–491.e8. doi: 10.1016/j.cell.2017.06.041. [DOI] [PubMed] [Google Scholar]
- 314.Fay J.F., Aleksandrov L.A., Jensen T.J., Cui L.L., Kousouros J.N., He L., Aleksandrov A.A., Gingerich D.S., Riordan J.R., Chen J.Z. Cryo-EM Visualization of an Active High Open Probability CFTR Anion Channel. Biochemistry. 2018;57:6234–6246. doi: 10.1021/acs.biochem.8b00763. [DOI] [PubMed] [Google Scholar]
- 315.Liu F., Zhang Z., Levit A., Levring J., Touhara K.K., Shoichet B.K., Chen J. Structural identification of a hotspot on CFTR for potentiation. Science. 2019;364:1184–1188. doi: 10.1126/science.aaw7611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Martin G.M., Yoshioka C., Rex E.A., Fay J.F., Xie Q., Whorton M.R., Chen J.Z., Shyng S.-L. Cryo-EM structure of the ATP-sensitive potassium channel illuminates mechanisms of assembly and gating. eLife. 2017;6:6. doi: 10.7554/eLife.24149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Lee K.P.K., Chen J., MacKinnon R. Molecular structure of human KATP in complex with ATP and ADP. eLife. 2017;6:e32481. doi: 10.7554/eLife.32481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Wu J.-X., Ding D., Wang M., Kang Y., Zeng X., Chen L. Ligand binding and conformational changes of SUR1 subunit in pancreatic ATP-sensitive potassium channels. Protein Cell. 2018;9:553–567. doi: 10.1007/s13238-018-0530-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Ding D., Wang M., Wu J.-X., Kang Y., Chen L. The Structural Basis for the Binding of Repaglinide to the Pancreatic KATP Channel. Cell Rep. 2019;27:1848–1857. doi: 10.1016/j.celrep.2019.04.050. [DOI] [PubMed] [Google Scholar]
- 320.Martin G.M., Sung M.W., Yang Z., Innes L.M., Kandasamy B., David L.L., Yoshioka C., Shyng S.-L. Mechanism of pharmacochaperoning in a mammalian KATP channel revealed by cryo-EM. eLife. 2019;8:8. doi: 10.7554/eLife.46417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Muthu V., Gandra R.R., Dhooria S., Sehgal I.S., Prasad K.T., Kaur H., Gupta N., Bal A., Ram B., Aggarwal A.N., et al. Role of flexible bronchoscopy in the diagnosis of invasive fungal infections. Mycoses. 2021 doi: 10.1111/myc.13263. [DOI] [PubMed] [Google Scholar]
- 322.Egner R., Rosenthal F.E., Kralli A., Sanglard D., Kuchler K. Genetic Separation of FK506 Susceptibility and Drug Transport in the Yeast Pdr5 ATP-binding Cassette Multidrug Resistance Transporter. Mol. Biol. Cell. 1998;9:523–543. doi: 10.1091/mbc.9.2.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Cannon R.D., Lamping E., Holmes A.R., Niimi K., Tanabe K., Niimi M., Monk B.C. Candida albicans drug resistance—Another way to cope with stress. Pt 10Microbiology. 2007;153:3211–3217. doi: 10.1099/mic.0.2007/010405-0. [DOI] [PubMed] [Google Scholar]
- 324.Senior A.E., Al-Shawi M.K., Urbatsch I.L. The catalytic cycle of P-glycoprotein. FEBS Lett. 1995;377:285–289. doi: 10.1016/0014-5793(95)01345-8. [DOI] [PubMed] [Google Scholar]
- 325.Kerr I.D., Haider A.J., Gelissen I.C. The ABCG family of membrane-associated transporters: You don’t have to be big to be mighty. Br. J. Pharmacol. 2011;164:1767–1779. doi: 10.1111/j.1476-5381.2010.01177.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Polgar O., Robey R.W., Bates S.E. ABCG2: Structure, function and role in drug response. Expert Opin. Drug Metab. Toxicol. 2007;4:1–15. doi: 10.1517/17425255.4.1.1. [DOI] [PubMed] [Google Scholar]
- 327.Smith P.C., Karpowich N., Millen L., Moody J.E., Rosen J., Thomas P.J., Hunt J.F. ATP Binding to the Motor Domain from an ABC Transporter Drives Formation of a Nucleotide Sandwich Dimer. Mol. Cell. 2002;10:139–149. doi: 10.1016/S1097-2765(02)00576-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Ye J., Osborne A.R., Groll M., Rapoport T.A. RecA-like motor ATPases--lessons from structures. Biochim. Biophys. Acta. 2004;1659:1–18. doi: 10.1016/j.bbabio.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 329.Hohl M., Hürlimann L.M., Böhm S., Schöppe J., Grütter M.G., Bordignon E., Seeger M.A. Structural basis for allosteric cross-talk between the asymmetric nucleotide binding sites of a heterodimeric ABC exporter. Proc. Natl. Acad. Sci. USA. 2014;111:11025–11030. doi: 10.1073/pnas.1400485111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Stockner T., Gradisch R., Schmitt L. The role of the degenerate nucleotide binding site in type I ABC exporters. FEBS Lett. 2020;594:3815–3838. doi: 10.1002/1873-3468.13997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Golin J., Kon Z.N., Wu C.P., Martello J., Hanson L., Supernavage S., Ambudkar S.V., Sauna Z.E. Complete inhibition of the Pdr5p multidrug efflux pump ATPase activity by its transport substrate clotrimazole suggests that GTP as well as ATP may be used as an energy source. Biochemistry. 2007;46:13109–13119. doi: 10.1021/bi701414f. [DOI] [PubMed] [Google Scholar]
- 332.Khunweeraphong N., Kuchler K. The first intracellular loop is essential for the catalytic cycle of the human ABCG2 multidrug resistance transporter. FEBS Lett. 2020;594:4059–4075. doi: 10.1002/1873-3468.13994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Gose T., Shafi T., Fukuda Y., Das S., Wang Y., Allcock A., McHarg A.G., Lynch J., Chen T., Tamai I., et al. ABCG2 requires a single aromatic amino acid to “clamp” substrates and inhibitors into the binding pocket. FASEB J. 2020;34:4890–4903. doi: 10.1096/fj.201902338RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Henriksen U., Fog J.U., Litman T., Gether U. Identification of Intra- and Intermolecular Disulfide Bridges in the Multidrug Resistance Transporter ABCG2. J. Biol. Chem. 2005;280:36926–36934. doi: 10.1074/jbc.M502937200. [DOI] [PubMed] [Google Scholar]
- 335.Wakabayashi K., Nakagawa H., Tamura A., Koshiba S., Hoshijima K., Komada M., Ishikawa T. Intramolecular Disulfide Bond Is a Critical Check Point Determining Degradative Fates of ATP-binding Cassette (ABC) Transporter ABCG2 Protein. J. Biol. Chem. 2007;282:27841–27846. doi: 10.1074/jbc.C700133200. [DOI] [PubMed] [Google Scholar]
- 336.Jones P.M., George A.M. Opening of the ADP-bound active site in the ABC transporter ATPase dimer: Evidence for a constant contact, alternating sites model for the catalytic cycle. Proteins: Struct. Funct. Bioinform. 2009;75:387–396. doi: 10.1002/prot.22250. [DOI] [PubMed] [Google Scholar]
- 337.Prasad R., Banerjee A., Khandelwal N.K., Dhamgaye S. The ABCs of Candida albicans Multidrug Transporter Cdr1. Eukaryot. Cell. 2015;14:1154–1164. doi: 10.1128/EC.00137-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Ernst R., Kueppers P., Klein C.M., Schwarzmueller T., Kuchler K., Schmitt L. A mutation of the H-loop selectively affects rhodamine transport by the yeast multidrug ABC transporter Pdr5. Proc. Natl. Acad. Sci. USA. 2008;105:5069–5074. doi: 10.1073/pnas.0800191105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Harris A., Wagner M., Du D., Raschka S., Gohlke H., Smits S.H.J., Luisi B.F., Schmitt L. Structure and efflux mechanism of the yeast pleiotropic drug resistance transporter Pdr5. bioRxiv. 2021 doi: 10.1101/2021.02.09.430491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Al-Shawi M.K. Catalytic and transport cycles of ABC exporters. Essays Biochem. 2011;50:63–83. doi: 10.1042/bse0500063. [DOI] [PubMed] [Google Scholar]
- 341.Kapoor P., Horsey A.J., Cox M.H., Kerr I.D. ABCG2: Does resolving its structure elucidate the mechanism? Biochem. Soc. Trans. 2018;46:1485–1494. doi: 10.1042/BST20180145. [DOI] [PubMed] [Google Scholar]
- 342.Kage K., Fujita T., Sugimoto Y. Role of Cys-603 in dimer/oligomer formation of the breast cancer resistance protein BCRP/ABCG2. Cancer Sci. 2005;96:866–872. doi: 10.1111/j.1349-7006.2005.00126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Szöllősi D., Szakács G., Chiba P., Stockner T. Dissecting the Forces that Dominate Dimerization of the Nucleotide Binding Domains of ABCB1. Biophys. J. 2018;114:331–342. doi: 10.1016/j.bpj.2017.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Jones P.M., George A.M. Mechanism of the ABC transporter ATPase domains: Catalytic models and the biochemical and biophysical record. Crit. Rev. Biochem. Mol. Biol. 2012;48:39–50. doi: 10.3109/10409238.2012.735644. [DOI] [PubMed] [Google Scholar]
- 345.Ford R.C., Hellmich U.A. What monomeric nucleotide binding domains can teach us about dimeric ABC proteins. FEBS Lett. 2020;594:3857–3875. doi: 10.1002/1873-3468.13921. [DOI] [PubMed] [Google Scholar]
- 346.Jardetzky O. Simple Allosteric Model for Membrane Pumps. Nature. 1966;211:969–970. doi: 10.1038/211969a0. [DOI] [PubMed] [Google Scholar]
- 347.Verhalen B., Dastvan R., Thangapandian S., Peskova Y., Koteiche H.A., Nakamoto R.K., Tajkhorshid E., Mchaourab H.S. Energy transduction and alternating access of the mammalian ABC transporter P-glycoprotein. Nat. Cell Biol. 2017;543:738–741. doi: 10.1038/nature21414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Sarkadi B., Homolya L., Hegedűs T. The ABCG2/BCRP transporter and its variants—From structure to pathology. FEBS Lett. 2020;594:4012–4034. doi: 10.1002/1873-3468.13947. [DOI] [PubMed] [Google Scholar]
- 349.Özvegy C., Váradi A., Sarkadi B. Characterization of Drug Transport, ATP Hydrolysis, and Nucleotide Trapping by the Human ABCG2 Multidrug Transporter. J. Biol. Chem. 2002;277:47980–47990. doi: 10.1074/jbc.M207857200. [DOI] [PubMed] [Google Scholar]
- 350.Glavinas H., Kis E., Pál Á., Kovács R., Jani M., Vági E., Molnár É., Bánsághi S., Kele Z., Janaky T., et al. ABCG2 (Breast Cancer Resistance Protein/Mitoxantrone Resistance-Associated Protein) ATPase Assay: A Useful Tool to Detect Drug-Transporter Interactions. Drug Metab. Dispos. 2007;35:1533–1542. doi: 10.1124/dmd.106.014605. [DOI] [PubMed] [Google Scholar]
- 351.Sarkadi B., Price E.M., Boucher R.C., Germann U.A., Scarborough G.A. Expression of the human multidrug resistance cDNA in insect cells generates a high activity drug-stimulated membrane ATPase. J. Biol. Chem. 1992;267:4854–4858. doi: 10.1016/S0021-9258(18)42909-2. [DOI] [PubMed] [Google Scholar]
- 352.Januliene D., Moeller A. Cryo-EM of ABC transporters: An ice-cold solution to everything? FEBS Lett. 2020;594:3776–3789. doi: 10.1002/1873-3468.13989. [DOI] [PubMed] [Google Scholar]
- 353.Bock C., Löhr F., Tumulka F., Reichel K., Würz J., Hummer G., Schäfer L., Tampé R., Joseph B., Bernhard F., et al. Structural and functional insights into the interaction and targeting hub TMD0 of the polypeptide transporter TAPL. Sci. Rep. 2018;8:15662. doi: 10.1038/s41598-018-33841-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Kaur H., Lakatos-Karoly A., Vogel R., Nöll A., Tampé R., Glaubitz C. Coupled ATPase-adenylate kinase activity in ABC transporters. Nat. Commun. 2016;7:13864. doi: 10.1038/ncomms13864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Rose-Sperling D., Tran M.A., Lauth L.M., Goretzki B., Hellmich U.A. 19F NMR as a versatile tool to study membrane protein structure and dynamics. Biol. Chem. 2019;400:1277–1288. doi: 10.1515/hsz-2018-0473. [DOI] [PubMed] [Google Scholar]
- 356.de Boer M., Gouridis G., Vietrov R., Begg S.L., Schuurman-Wolters G.K., Husada F., Eleftheriadis N., Poolman B., McDevitt C.A., Cordes T. Conformational and dynamic plasticity in substrate-binding proteins underlies selective transport in ABC importers. Elife. 2019;8:e44652. doi: 10.7554/eLife.44652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Bordignon E., Seeger M.A., Galazzo L., Meier G. From in vitro towards in situ: Structure-based investigation of ABC exporters by electron paramagnetic resonance spectroscopy. FEBS Lett. 2020;594:3839–3856. doi: 10.1002/1873-3468.14004. [DOI] [PubMed] [Google Scholar]
- 358.Egloff P., Zimmermann I., Arnold F.M., Hutter C.A.J., Morger D., Opitz L., Poveda L., Keserue H.-A., Panse C., Roschitzki B., et al. Engineered peptide barcodes for in-depth analyses of binding protein libraries. Nat. Methods. 2019;16:421–428. doi: 10.1038/s41592-019-0389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Slotboom D.J., Ettema T.W., Nijland M., Thangaratnarajah C. Bacterial multi-solute transporters. FEBS Lett. 2020;594:3898–3907. doi: 10.1002/1873-3468.13912. [DOI] [PubMed] [Google Scholar]
- 360.Rutledge R.M., Esser L., Ma J., Xia D. Toward understanding the mechanism of action of the yeast multidrug resistance transporter Pdr5p: A molecular modeling study. J. Struct. Biol. 2011;173:333–344. doi: 10.1016/j.jsb.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Rosenberg M.F., Bikadi Z., Chan J., Liu X., Ni Z., Cai X., Ford R.C., Mao Q. The human breast cancer resistance protein (BCRP/ABCG2) shows conformational changes with mitoxantrone. Structure. 2010;18:482–493. doi: 10.1016/j.str.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Rosenberg M.F., Bikádi Z., Hazai E., Starborg T., Kelley L., Chayen N.E., Ford R.C., Mao Q. Three-dimensional structure of the human breast cancer resistance protein (BCRP/ABCG2) in an inward-facing conformation. Pt 8Acta Crystallogr. Sect. D Biol. Crystallogr. 2015;71:1725–1735. doi: 10.1107/S1399004715010676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Wang H., Lee E.-W., Cai X., Ni Z., Zhou L., Mao Q. Membrane Topology of the Human Breast Cancer Resistance Protein (BCRP/ABCG2) Determined by Epitope Insertion and Immunofluorescence†. Biochemistry. 2008;47:13778–13787. doi: 10.1021/bi801644v. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that all data are fully available without restrictions. All relevant data are provided in the manuscript and in the Supplementary Materials.