Abstract
Background
The effective control of moisture and microbes is necessary for the success of restoration procedures. The rubber dam, as an isolation method, has been widely used in dental restorative treatments. The effects of rubber dam usage on the longevity and quality of dental restorations still require evidence‐based discussion. This review compares the effects of rubber dam with other isolation methods in dental restorative treatments. This is an update of the Cochrane Review first published in 2016.
Objectives
To assess the effects of rubber dam isolation compared with other types of isolation used for direct and indirect restorative treatments in dental patients.
Search methods
Cochrane Oral Health's Information specialist searched the following electronic databases: Cochrane Oral Health's Trials Register (searched 13 January 2021), Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 12) in the Cochrane Library (searched 13 January 2021), MEDLINE Ovid (1946 to 13 January 2021), Embase Ovid (1980 to 13 January 2021), LILACS BIREME Virtual Health Library (Latin American and Caribbean Health Science Information database; 1982 to 13 January 2021), and SciELO BIREME Virtual Health Library (1998 to 13 January 2021). We also searched Chinese BioMedical Literature Database (CBM, in Chinese) (1978 to 13 January 2021), VIP database (in Chinese) (1989 to 13 January 2021), and China National Knowledge Infrastructure (CNKI, in Chinese) (1994 to 13 January 2021). We searched ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform, OpenGrey, and Sciencepaper Online (in Chinese) for ongoing trials. There were no restrictions on the language or date of publication when searching the electronic databases.
Selection criteria
We included randomised controlled trials (including split‐mouth trials) over one month in length assessing the effects of rubber dam compared with alternative isolation methods for dental restorative treatments.
Data collection and analysis
Two review authors independently screened the results of the electronic searches, extracted data, and assessed the risk of bias of the included studies. Disagreement was resolved by discussion. We strictly followed Cochrane's statistical guidelines and assessed the certainty of the evidence using GRADE.
Main results
We included six studies conducted worldwide between 2010 and 2015 involving a total of 1342 participants (of which 233 participants were lost to follow‐up). All the included studies were at high risk of bias.
Five studies compared rubber dam with traditional cotton rolls isolation. One study was excluded from the analysis due to inconsistencies in the presented data. Of the four remaining trials, three reported survival rates of the restorations with a minimum follow‐up of six months. Pooled results from two studies involving 192 participants indicated that the use of rubber dam isolation may increase the survival rates of direct composite restorations of non‐carious cervical lesions (NCCLs) at six months (odds ratio (OR) 2.29, 95% confidence interval (CI) 1.05 to 4.99; low‐certainty evidence). However, the use of rubber dam in NCCLs composite restorations may have little to no effect on the survival rates of the restorations compared to cotton rolls at 12 months (OR 1.38, 95% CI 0.45 to 4.28; 1 study, 30 participants; very low‐certainty evidence) and at 18 months (OR 1.00, 95% CI 0.45 to 2.25; 1 study, 30 participants; very low‐certainty evidence) but the evidence is very uncertain. At 24 months, the use of rubber dam may decrease the risk of failure of the restorations in children undergoing proximal atraumatic restorative treatment in primary molars but the evidence is very uncertain (hazard ratio (HR) 0.80, 95% CI 0.66 to 0.97; 1 study, 559 participants; very low‐certainty evidence).
None of the included studies mentioned adverse effects or reported the direct cost of the treatment.
Authors' conclusions
This review found some low‐certainty evidence that the use of rubber dam in dental direct restorative treatments may lead to a lower failure rate of the restorations compared with cotton roll usage after six months. At other time points, the evidence is very uncertain. Further high‐quality research evaluating the effects of rubber dam usage on different types of restorative treatments is required.
Plain language summary
Does using a thin sheet of rubber (rubber dam) to isolate teeth from the rest of the mouth during a dental procedure improve the success of tooth repairs?
Key messages
‐ When a rubber dam is used to isolate teeth instead of cotton rolls, tooth repairs may be more likely to remain in place and be in good condition after six months. ‐ We need to conduct more studies in this area, to strengthen the evidence. These studies need to use robust methods, follow people beyond six months, and investigate adverse (unwanted) effects and costs.
Why do we isolate teeth when they are being repaired?
When dental practitioners need to repair a tooth, they often isolate it from the rest of the mouth to:
‐ keep away saliva to prevent it from impairing the bonding of materials; ‐ reduce aerosols produced during the dental procedure to a certain extent; ‐ stop materials, liquids or instruments used for the repair from being swallowed or damaging the mouth.
What do dental practitioners use to isolate teeth?
A common method for isolating teeth from the rest of the mouth is to use cotton rolls and a straw‐like tube that sucks up saliva. This technique uses simple, inexpensive equipment, but requires frequent replacement of sodden cotton rolls.
An alternative option is to use a thin sheet of rubber (rubber dam). First, the dental practitioner makes a small hole in the sheet. They then place it over the tooth to be treated, creating a barrier around it. The sheet can be held in place with several methods, such as clasps placed over the tooth or a small piece of rubber wedged between teeth.
What did we want to find out?
We wanted to find out if rubber dams improve the success of tooth repairs when compared against other methods for isolating teeth. We also wanted to know if they are associated with unwanted (adverse) effects.
What did we do?
We searched for studies that compared using a rubber dam against another method for isolating teeth. We compared and summarized the results of these studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found six studies that involved 1342 people in total (mostly children). Teeth needed repairing for a range of reasons, including caries (holes in teeth created by bacteria) and loss of hard tissue at the base of teeth. The studies compared rubber dams against:
‐ cotton rolls (five studies); and ‐ the Isolite system (a new method that combines plastic blocks, a shield for the tongue and cheek, and a tube that sucks up saliva and other mouth contents) (one study).
Rubber dam compared against cotton rolls
The evidence suggests that when a rubber dam is used rather than cotton rolls, tooth repairs may be more likely to remain in place and be in good condition after six months (2 studies). There is not enough robust evidence for us to determine if this is the case beyond six months.
Rubber dam compared against the Isolite system
The evidence is not robust enough for us to determine if using a rubber dam improves the success of tooth repairs when compared against the Isolite system.
Side effects
No study investigated side effects.
What are the limitations of the evidence?
The evidence is based on a small number of studies conducted in ways that may have introduced errors into their results.
How up to date is this evidence?
The evidence is up to date to January 2021.
Summary of findings
Summary of findings 1. Rubber dam versus cotton rolls for restorative treatment in dental patients.
| Rubber dam versus cotton rolls for restorative treatment in dental patients | ||||||
|
Patient or population: dental patients requiring restorative treatment
Settings: dental clinics in China and Brazil; primary school in Kenya
Intervention: rubber dam Comparison: cotton rolls | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Cotton rolls | Rubber dam | |||||
| Survival rate of restorations Assessed clinically and radiographically Follow‐up: mean 6 months | Study population | OR 2.29 (1.05 to 4.99) | 192 (2 studies) | ⊕⊕⊝⊝ Lowa,b | The use of rubber dam may result in a higher survival rate of the restorations compared to cotton rolls at 6 months' follow‐up Other time points:
|
|
| 811 per 1000 | 908 per 1000 (818 to 955) | |||||
| Adverse events | Outcome not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; HR: hazard ratio; OR: odds ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aThe certainty of the evidence was downgraded by 1 level for high risk of bias. bThe certainty of the evidence was downgraded by 1 level for imprecision due to small sample size which did not meet the optimal information size (OIS). cThe certainty of the evidence was downgraded by 1 level for imprecision due to wide CIs overlapping no effect. dThe certainty of the evidence was downgraded by 2 levels for imprecision (single study).
Background
Description of the condition
Restorative dental treatments are used to repair damage to teeth caused by caries or trauma. Direct restorative dental treatments (commonly known as 'fillings') repair damage to the visible tooth, such as restorations using either amalgam or a resin composite material. Indirect restorations are prepared outside the person's mouth, using a dental impression from the prepared tooth. Examples of indirect restorations include inlays, onlays, crowns, bridges, and veneers.
Successful restorations depend on a number of factors, but perhaps the most important ones are moisture and microbe control. Excluding moisture and saliva from the tooth or root being restored facilitates the bonding of the restorative material to the tooth and decreases the risk of infection or re‐infection. Poor bonding or secondary caries may compromise the success or longevity of the restoration, or both.
Description of the intervention
A common method of isolation and moisture control in restorative dentistry is the use of cotton rolls combined with aspiration by saliva ejector. This technique is widely available and low cost, but has the disadvantage that the dentist is required to replace sodden cotton rolls frequently during the treatment to keep the operative field dry.
An alternative method of isolation of the tooth undergoing restorative treatment is a rubber dam, an isolation method introduced to the dental profession by Dr Sanford C Barnum on 15 March 1864 (Elderton 1971a; Elderton 1971b; Elderton 1971c). Since then, many researchers have improved its application and it is now a frequently used, practical alternative to cotton balls (Bhuva 2008; Carrotte 2000; Carrotte 2004; Reuter 1983). A rubber dam is usually a small sheet of latex (though non‐latex versions are available) placed in a frame. A small hole is made in the sheet and placed over the tooth to be treated. The rubber dam is held on to the tooth being restored by means of a small clamp. This isolates the tooth from the rest of the person's mouth, which keeps the tooth to be restored dry and relatively less exposed to intraoral bacteria.
Potential advantages of the use of a rubber dam include superior isolation of the tooth to be treated from the saliva in the mouth (Cochran 1989), providing the dentist with improved visibility, reduced mirror fogging, enhanced visual contrast, soft tissue retraction (Reid 1991), and preventing oral soft tissues from contact with irritating or harmful materials used during operative procedures, such as phosphoric acids or sodium hypochlorite (Lynch 2003). Even when it comes to overall health, results from some studies have indicated its protective effect on the person, by preventing ingestion or aspiration of instruments (Susini 2007; Tiwana 2004), materials, or irritants (Cohen 1987), as well as reducing patients' exposure to mercury during the removal of amalgam restorations (Berglund 1991). There is also a reduction in the risk of cross‐infection in the dental practice by decreasing the microbial content of splatters and air turbine aerosols produced during dental treatment (Harrel 2004). During the coronavirus disease (COVID‐19) pandemic, rubber dam treatment has been recommended for routine care by a number of governments across the world (Kumbargere 2020).
However, there are real and perceived negative effects to the use of rubber dams. Most often cited are concerns over patient's acceptance, time needed for application, cost of materials and equipment, insufficient training, and inconvenience (Hill 2008; Koshy 2002; Stewardson 2002). Latex allergy, fracture (Sutton 1996) or dental structure loss (Mendes 2018) or chipping of near apical thin veneer margins (Schuh 2019) caused by rubber dam clamps, and damage to the mucosa when placing or removing the rubber dam, in rare cases, may also impede the wide use of rubber dam. In addition, despite its clinical value, a significantly higher aerosol level on dentists may be another issue that merits attention (Al‐Amad 2017).
A number of modifications of rubber dam techniques have been described. John Mamoun suggested the use of a rubber dam with a custom prosthesis to achieve dry‐field isolation of the distal molars with short clinical crowns (Mamoun 2002). Also, the split rubber dam technique used when preparing teeth for indirect restoration could promote operating efficiency (Perrine 2005). Further developments in rubber dam techniques are ongoing.
How the intervention might work
Creating a physical barrier around a treatment site to reduce contamination due to moisture and microbes is common practice in medical and dental procedures. Isolating the tooth to be restored from the contamination of moisture or saliva in restoration placement may promote the bonding of the restorative materials to the tooth, while rubber dam usage is highly recommended for endodontics for reasons of safety and cross‐infection control. The use of a rubber dam in restorative dentistry has the added advantage of providing the dentist with a broader work surface which also traps small pieces of debris and treatment solutions protecting the person from inadvertently swallowing these. When rubber dams are used in association with amalgam restorations, they may reduce the person's exposure to potentially harmful adverse effects of mercury ingestion (Halbach 2008; Kremers 1999).
Why it is important to do this review
Both rubber dam and cotton rolls are currently used in dentistry to isolate the treatment field and to exclude moisture. Both methods have advantages and disadvantages, from the different points of view of patient and dentist. Throughout the COVID‐19 pandemic, the routine use of rubber dam during dental operations was highlighted for its excellent role in aerosol isolation (Kumbargere 2020). There has been a review concluding the importance of rubber dam usage in endodontic treatments, that failure to use rubber dam led to a negative impact on root canal treatment outcomes and a higher risk for patients to swallow or aspirate materials and instruments (Ahmad 2009). However, its effects on restorations' performance in patients receiving dental restorative treatment are still unclear. Several randomised controlled trials have been conducted to determine whether the use of a rubber dam for restorative treatments influences the treatment outcomes (Carvalho 2010; Kemoli 2010; Ma 2012; Loguercio 2015). The results from these trials appear to be conflicting. In addition, some recently emerging alternative isolation methods (e.g. the Isolite system, the 'Teflon tape technique') showed better acceptance and operability over the 'gold‐standard' rubber dam (Alhareky 2014; Schuh 2019). It is therefore still necessary to conduct a summarization and description of such evidence.
This is an update of the Cochrane Review first published in 2016 (Wang 2016) to summarize the evidence on the effectiveness of rubber dam as an isolation and moisture reduction technique in restorative dentistry, together with any adverse or negative effects. This information would then assist both dentists and their patients in making informed decisions about the benefits and possible negative effects of different isolation and moisture control techniques to be used for specific dental restorations.
Objectives
To assess the effects of rubber dam isolation compared with other types of isolation used for direct and indirect restorative treatments in dental patients.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) (including split‐mouth trials) over one month in length.
Types of participants
People undergoing any type of direct or indirect restorative treatment. There were no restrictions of age or gender.
Restorative treatments included direct anterior restorations, direct posterior restorations, inlays, onlays, veneers, crowns, etc.
Types of interventions
The intervention group received a rubber dam for isolation and moisture control, either alone or combined with other active treatment (such as saliva aspiration). The comparison (control) group received an alternative method of isolation and moisture control (such as cotton rolls) with or without the same active treatment as in the intervention group.
Types of outcome measures
Primary outcomes
Survival rate of the restorations at 6 months, 1, 2, 5, and 10 years after restorative treatments. Survival means the restorations were still correctly present or having only a slight wear or defect at the margin less than 0.5 mm in depth when assessed. If the restorations were either completely lost, or were fractured with defects 0.5 mm in depth or greater, had secondary caries or inflammation of the pulp, any of these situations were labelled as treatment failures.
Adverse events. Any reported adverse events related to any of the active interventions during the treatment phase. These included events affecting the operator or the patient (e.g. damage to skin or mucosa, allergic reactions to latex).
Secondary outcomes
Clinical evaluation of restoration's quality, including colour match, cavo‐surface marginal discolouration, anatomic form, marginal adaptation and caries, which were assessed at baseline (i.e. within one month following the placement) as well as 6 months, 1, 2, 5, and 10 years of subsequent recalls. The evaluation should be based upon the US Public Health Service (USPHS) criteria and its evolution (Hickel 2007), which had specific clinical criteria followed for the assessment of each category.
Costs: the direct cost of the treatment, the time needed to accomplish the treatment.
Participant acceptance/satisfaction. Participants expressed satisfaction with the procedure using any validated instrument.
Search methods for identification of studies
For the identification of studies included or considered for this review, we developed detailed search strategies for each database searched. We based these on the search strategy developed for MEDLINE but revised appropriately for each database to take account of differences in controlled vocabulary and syntax rules. There were no language restrictions in the searches. We translated papers when necessary.
Electronic searches
Cochrane Oral Health's Information Specialist conducted systematic searches in the following databases for randomised controlled trials and controlled clinical trials. There were no language, publication year or publication status restrictions:
Cochrane Oral Health's Trials Register (searched 13 January 2021) (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 12) in the Cochrane Library (searched 13 January 2021) (Appendix 2);
MEDLINE Ovid (1946 to 13 January 2021) (Appendix 3);
Embase Ovid (1980 to 13 January 2021) (Appendix 4);
LILACS BIREME Virtual Health Library (Latin American and Caribbean Health Science Information database; 1982 to 13 January 2021) (Appendix 5);
SciELO BIREME Virtual Health Library (Scientific Electronic Library Online; 1998 to 13 January 2021) (Appendix 6).
We also searched:
Chinese BioMedical Literature Database (CBM, in Chinese) (1978 to 13 January 2021) (Appendix 7);
VIP database (in Chinese, 1989 to 13 January 2021) (Appendix 8);
China National Knowledge Infrastructure (CNKI, in Chinese) (1994 to 13 January 2021) (Appendix 9).
Searching other resources
Searching for unpublished and ongoing studies
Cochrane Oral Health's Information Specialist searched the following sources for unpublished and ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov/; searched 13 January 2021) (Appendix 10);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 13 January 2021) (Appendix 11);
OpenGrey (1980 to 13 January 2021) (Appendix 12).
We also searched:
Sciencepaper Online (in Chinese, to 13 January 2021) (Appendix 13).
Handsearching
We handsearched the following journals:
Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology (1995 to October 2015 and then updated to 13 January 2021);
Journal of Endodontics (1975 to October 2015 and then updated to 13 January 2021);
International Endodontic Journal (1967 to October 2015 and then updated to 13 January 2021);
Caries Research (1967 to October 2015 and then updated to 13 January 2021);
Journal of Dental Research (1970 to October 2015 and then updated to 13 January 2021);
International Journal of Oral Science (2009 to October 2015 and then updated to 13 January 2021);
Dental Traumatology (1985 to October 2015 and then updated to 13 January 2021);
Australian Endodontic Journal (1967 to October 2015 and then updated to 13 January 2021).
In addition, we explored the following Chinese dental journals:
Chinese Journal of Stomatology (2005 to October 2015 and then updated to 13 January 2021);
West China Journal of Stomatology (2005 to October 2015 and then updated to 13 January 2021);
Journal of International Stomatology (2005 to October 2015 and then updated to 13 January 2021);
Journal of Clinical Stomatology (2005 to October 2015 and then updated to 13 January 2021);
Journal of Practical Stomatology (2005 to October 2015 and then updated to 13 January 2021);
Journal of Comprehensive Stomatology (2005 to October 2015 and then updated to 13 January 2021);
Journal of Modern Stomatology (2005 to October 2015 and then updated to 13 January 2021);
Chinese Journal of Conservative Dentistry (2005 to October 2015 and then updated to 1 January 2019, due to the publication suspension);
Chinese Journal of Dental Prevention and Treatment (2005 to October 2015 and then updated to 13 January 2021).
Reference lists and contacts
We screened the references of the included articles for studies. We contacted authors and experts in the field to identify unpublished randomised controlled trials.
We checked that none of the included studies in this review were retracted due to error or fraud.
We did not perform a separate search for adverse effects of interventions used, we considered adverse effects described in included studies only.
Data collection and analysis
Two review authors (Cheng Miao (CM), Xiaoyu Yang (XY)) independently selected studies, extracted and managed data, and assessed risk of bias. We resolved any differences of opinion by discussion.
Selection of studies
We used a two‐step process to identify studies to be included in this review. We screened titles and abstracts from the electronic searches to identify studies which may have met the inclusion criteria for this review. We obtained full‐text copies of all apparently eligible studies and two review authors evaluated these further in detail to identify those studies which actually met all the inclusion criteria. We recorded those studies which did not meet the inclusion criteria in the excluded studies section of the review and noted the reason for exclusion in the Characteristics of excluded studies table.
Data extraction and management
We designed and piloted a data extraction form on two included studies. The data extraction form included the following information.
Article title, publication time, journal, reviewer ID.
Inclusion re‐evaluation.
Types of studies: methods of randomisation, methods of allocation concealment, methods of blinding, location of the study, number of centres, time frame, source of funding.
Types of participants: source of participants, types of disease, diagnostic criteria, age, sex, eligibility criteria, numbers of participants randomised to each group, number evaluated in each group.
Types of intervention and comparison: details of the treatments received in the intervention and comparison groups, together with the type of restoration procedure and any co‐interventions used.
Types of outcome measures: outcome, time point that the outcome was recorded, exact statistics.
Assessment of risk of bias in included studies
The review authors assessed the risk of bias for each included study in each of seven domains using RoB 1 as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For each domain, we presented explanations and judged them as low risk, unclear risk, and high risk. The domains and explanations were as follows.
Random sequence generation (selection bias): selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence.
Allocation concealment (selection bias): selection bias (biased allocation to interventions) due to inadequate concealment of the allocation sequence from those involved in the enrolment and assignment of participants.
Blinding of participants and personnel (performance bias): performance bias due to knowledge of the allocated interventions by participants and personnel during the study.
Blinding of outcome assessment (detection bias): detection bias due to knowledge of the allocated interventions by outcome assessors.
Incomplete outcome data (attrition bias): attrition bias due to amount, nature, or handling of incomplete outcome data.
Selective reporting (reporting bias): reporting bias due to selective outcome reporting.
Other bias: bias due to problems not covered elsewhere in the table.
We categorised the overall risk of bias according to Additional Table 2 and summarised the risk of bias graphically.
1. Category of overall risk of bias.
| Risk of bias | Interpretation | Within a study | Across studies |
| Low risk of bias | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information is from studies at low risk of bias |
| Unclear risk of bias | Plausible bias that raises some doubt about the results | Unclear risk of bias for ≥ 1 key domains | Most information is from studies at low or unclear risk of bias |
| High risk of bias | Plausible bias that seriously weakens confidence in the results | High risk of bias for ≥ 1 key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results |
Measures of treatment effect
For the primary outcome of survival/success rate of the restorative treatment, we expressed the measure of the treatment effect as a hazard ratio (HR) or risk ratio (RR) with 95% confidence interval (CI). If the studies did not quote HRs, we calculated the log HRs and the standard errors (SE) from the available summary statistics or Kaplan‐Meier curves according to the methods proposed by Parmar and colleagues (Parmar 1998), or requested the data from study authors. For the primary outcome of incidence of adverse events, we used the RR and 95% CIs to estimate the treatment effect.
For the secondary outcomes of costs and restoration's quality, we used RR and 95% CIs for dichotomous data and mean difference (MD) and 95% CIs for continuous data. For the secondary outcome of participant acceptance/satisfaction and its preference data, P values were calculated using a binomial test.
Unit of analysis issues
The unit of analysis was the participant.
Cross‐over/split‐mouth trials
We assessed carry‐over or carry‐across effect of designs if we considered them a problem. For an ideal study (which reported MD and standard deviation (SD) of both groups and the MD together with SD/SE between the two groups), we calculated the intracluster correlation coefficient (ICC); if more than one ideal study existed, we calculated a mean ICC. We used this ICC in the calculation of MD and SD/SE of the other similar cross‐over/split‐mouth studies. If there was no ideal study, we assumed the ICC was 0.5 (Higgins 2021).
Trials with multiple intervention arms
For randomised controlled trials with multiple treatment arms, there were two steps to deal with this problem. First, we tried to combine treatment arms, or we analysed the most relevant treatment and controls groups. For such trials, we collected the data in all the groups and recorded details in the Characteristics of included studies table.
Dealing with missing data
Where information about trial procedures was incomplete or unclear in a trial report, or data were missing or incomplete, the review authors attempted to contact the trial authors to obtain clarification. Where we could not obtain missing data, we did not include the trial in the meta‐analysis but described the results narratively. Where SDs were missing from continuous outcome data, we attempted to calculate these based on other available data (e.g. CIs, SEs, t values, P values, F values), as discussed in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2021).
Assessment of heterogeneity
We considered two types of heterogeneity.
Clinical heterogeneity
We judged clinical heterogeneity from the similarity between the types of participants, interventions, and outcome measures in each trial.
Statistical heterogeneity
We calculated statistical heterogeneity through the Chi2 test and measured the effect using the I2 statistic or P value (P value < 0.1 indicated statistically significant heterogeneity). The classification of statistical heterogeneity was as follows.
0% to 40% implied slight heterogeneity.
30% to 60% moderate heterogeneity.
50% to 90% substantial heterogeneity.
75% to 100% considerable heterogeneity.
Assessment of reporting biases
We planned to report bias using a funnel plot if the number of included studies had exceeded 10. The asymmetry of the funnel plot would indicate a possibility of reporting bias. Further detection would use Begg's test (Begg 1994) for dichotomous data and Egger's test (Egger 1997) for continuous data.
Data synthesis
We planned to carry out meta‐analyses only when there were little clinical heterogeneity and statistical heterogeneity (I2 less than 75%). We combined data using a fixed‐effect model if there were only two or three studies, or a random‐effects model if there were four or more studies. For meta‐analysis involving split‐mouth studies, we adopted the generic inverse variance (GIV) method, where for dichotomous data log odds ratio (OR) and its SE were calculated using Becker‐Balagtas (BB) marginal method (Elbourne 2002) and ICC was assumed equal to 0.5; for continuous data in the form of MD and SDs for each intervention group separately, the SD of the differences was estimated using the intervention‐specific SDs and an imputed correlation coefficient (Corr) (Higgins 2011).
Subgroup analysis and investigation of heterogeneity
If the number of studies in one outcome exceeded 10, we planned to use meta‐regression to detect clinical heterogeneity (using Stata software (Stata 2017)). If there was clinical heterogeneity, we planned to perform subgroup analysis of the following:
types of restorative treatments;
age of the participants;
location of the restoration (anterior/posterior teeth);
types of adhesives.
Due to the small number of eligible studies and a lack of suitable data from the included studies, we were unable to do subgroup analyses; however, we will consider carrying this out if more eligible studies are included in future updates of this review.
Sensitivity analysis
We planned to perform a sensitivity analysis to detect the stability of the outcomes. If there had been a sufficient number of included trials, we would have based sensitivity analysis on risk of bias (low risk of bias versus high or unclear risk of bias).
Summary of findings and assessment of the certainty of the evidence
We developed a summary of findings table for the main comparisons and primary outcomes (survival rate of restorations and adverse events) of this review using GRADEpro GDT software (GRADEpro GDT). We assessed the certainty of the body of evidence with reference to the overall risk of bias of the included studies, the directness of the evidence, the consistency of the results (heterogeneity), the precision of the effect estimates, and the risk of publication bias. GRADE categorises the certainty of the body of evidence for each of the outcomes as high, moderate, low, or very low (Atkins 2004; Guyatt 2008; Higgins 2021).
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies tables.
Results of the search
Searches were originally done in August 2012, then repeated in April 2015, October 2015, and August 2016. The first version of this review published in 2016 included four studies (five references) of 781 identified trials.
An updated search was done in February 2020 and January 2021 and 706 references were retrieved, which reduced to 423 after de‐duplication. Handsearching of journals did not identify any additional studies. After reviewing the titles and abstracts, we identified 419 references that did not match our criteria and were discarded. We obtained the full texts of the remaining five studies for further evaluation. We excluded four studies (four references). Only one study was included from the updated search (Loguercio 2015). The second new included study in this update was previously classified as 'awaiting classification' in the review and was included after we obtained methods details from study authors (Alhareky 2014).
The review includes a total of six studies (seven references): two newly included studies (Alhareky 2014; Loguercio 2015) and four from the previous version (Ammann 2013; Carvalho 2010; Kemoli 2010; Ma 2012).
We have presented this process as a flow chart in Figure 1.
1.
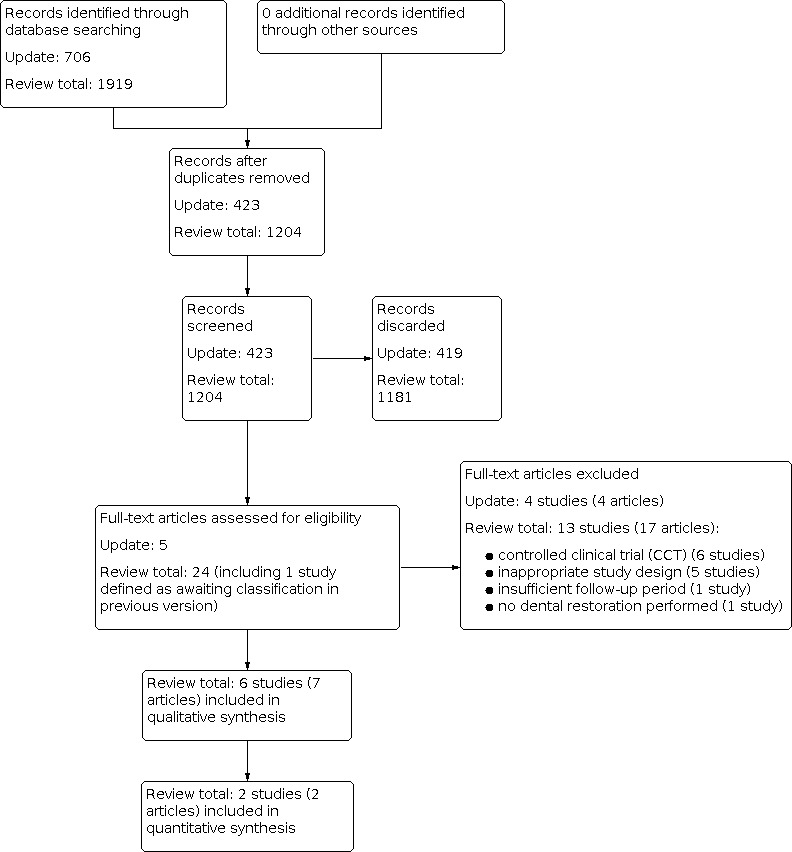
Study flow diagram.
Included studies
We included six randomised controlled trials (RCTs) (Alhareky 2014; Ammann 2013; Carvalho 2010; Kemoli 2010; Ma 2012; Loguercio 2015), which were published between 2010 and 2015. See Characteristics of included studies table for further details.
Characteristics of the trial designs and settings
Four included RCTs used a parallel design (Ammann 2013; Carvalho 2010; Kemoli 2010; Ma 2012) and two trials (Alhareky 2014; Loguercio 2015) were designed as split‐mouth RCTs. The studies were conducted in the USA (Alhareky 2014), Germany (Ammann 2013), Brazil (Carvalho 2010; Loguercio 2015), Kenya (Kemoli 2010), and China (Ma 2012). One study was carried out in a private dental clinic (Ammann 2013), one in a dental clinic of a hospital (Ma 2012), two in clinics of dental schools (Alhareky 2014; Loguercio 2015), and two in schools (Carvalho 2010; Kemoli 2010). One study performed a sample size calculation, but did not mention the method used (Kemoli 2010). The other five studies did not mention a sample size calculation (Ammann 2013; Carvalho 2010; Ma 2012; Loguercio 2015; Alhareky 2014). One study did not state its funding source (Ma 2012), three studies stated that they received industry funding (Ammann 2013; Kemoli 2010; Loguercio 2015); and the remaining two stated that they received non‐industry funding (Alhareky 2014; Carvalho 2010).
Characteristics of the participants
The trials included 1342 participants (of which 233 participants were lost to follow‐up) with different age ranges and receiving various restorative treatments. Ammann 2013 enrolled 72 children aged from 5.9 to 11.9 years, and Alhareky 2014 enrolled 42 children, aged from 7 to 16 years; all the included children undertook pit and fissure sealant of premolars or molars. Ma 2012 (162 participants, unknown age range) and Loguercio 2015 (30 adults, mean age of 45 years) studied participants with non‐carious cervical lesions (NCCLs) receiving resin composite restorations. Kemoli 2010 (804 children, aged 7 to 8 years) and Carvalho 2010 (232 children, aged 6 to 7 years) included children undertaking proximal primary atraumatic restorative treatment (ART) in primary molars. All the participants of these included studies received direct dental restorative treatments.
Characteristics of the interventions
The active intervention in each of the included trials was rubber dam isolation in dental restorative treatments. Five of the included trials used a comparison group of cotton rolls (Ammann 2013; Carvalho 2010; Kemoli 2010; Loguercio 2015; Ma 2012) while one employed the Isolite system as the alternative isolation method (Alhareky 2014).
Characteristics of the outcome measures
Four studies reported the survival rate or failure rate of the restorations (Additional Table 3) (Carvalho 2010; Kemoli 2010; Ma 2012; Loguercio 2015). There was variability between the studies in their criteria for 'survival or failure of the restorations.' Carvalho 2010 and Kemoli 2010 defined survival of the restorations as the restorations being present with marginal defects 0.5 mm or less in depth and general wear 0.5 mm or less in depth at the deepest point. Ma 2012 defined failure as the restoration being absent at the time of evaluation. Loguercio 2015 defined retained as restoration retained, no fractures/ cracks, small hairline crack, or two or more or larger hairline cracks or chipping or both (not affecting the marginal integrity) according to the World Dental Federation (FDI) criteria used for clinical evaluation. None of the four studies reported adverse events. Alhareky 2014 and Ammann 2013 did not report survival rate or adverse effects.
2. Effects of intervention: survival/loss rate.
| Study ID | Restorative treatment | Time points | Result parameters | Results | Comment |
| Ma 2012 | Composite restorations of NCCLs | 6 months after the restoration | Loss rate | Lower failure rate in rubber dam group | Chinese reference, translated |
| Carvalho 2010 | Proximal ART restorations in primary molars | 6, 12, 18, and 24 months after the restoration | Cumulative survival rate of restorations | Both groups had similar survival rate | Excluded from analysis due to inconsistent data |
| Kemoli 2010 | Proximal ART restorations in primary molars | Within 2 hours, 1 week, 1 month, 5 months, 1 year, 1.5, and 2 years after the restoration | Survival rate of restorations | Significant higher 2‐year survival rate was observed in rubber dam group compared to cotton roll isolation group | ‐ |
| Loguercio 2015 | Composite restorations of NCCLs | 6, 12, and 18 months after the restoration | Retention rate of restorations | No statistical difference between any pair of groups at the 6, 12, and 18‐month recall (P > 0.05) | ‐ |
ART: atraumatic restorative treatment; NCCLs: non‐carious cervical lesions.
Loguercio 2015 also evaluated the performance of the restorations regarding aesthetics, function, and biological properties. Two studies (Alhareky 2014; Loguercio 2015) assessed the level of participants acceptance/satisfaction of rubber dam compared with cotton rolls or Isolite system isolation, by choosing a preferred isolation method and so on. None of the included studies reported the direct cost of the treatment. But the treatment time when using rubber dam or cotton rolls as the isolation method was evaluated in Ammann 2013 and Loguercio 2015, while Alhareky 2014 reported the difference of chair time between rubber dam and the Isolite system. In addition, Loguercio 2015 also assessed and monitored the gingival tissue damage of the two groups (rubber dam versus cotton rolls/retraction cord) at baseline and during follow‐up.
Excluded studies
We listed all the excluded studies and the reasons for their exclusion in the Characteristics of excluded studies table.
Six studies were controlled clinical trials (CCT) (Ganss 1999; Huth 2004; Sabbagh 2011; Smales 1993; Straffon 1985; van Dijken 1987). Five studies used an inappropriate study design (Daudt 2013; Favetti 2021; Luz 2012; NCT01506830; Raskin 2000). Daudt 2013, Favetti 2021 and Raskin 2000 performed randomisation and analysis at the tooth level without accounting for the clustering effect of teeth within individual participants. For NCT01506830, the study claimed to be performed using a split‐mouth design, but it was not carried out it in an appropriate way. In Luz 2012, the use of rubber dam is not the only variable, specifically, different restorative operations were performed in two groups. One study (Al‐Amad 2017) with insufficient follow‐up length, failed to provide required results, and evaluated the effect of rubber dam use on bacterial contamination of the dentist’s head rather than its influence on dental restorations as outcome. One study investigated the nature of tooth colour change resulting from dehydration due to rubber dam application and performed no dental restorations (Ibrahim 2020).
Risk of bias in included studies
All of the included studies were at high risk of bias overall, based on a judgement of high risk of bias for two domains (Alhareky 2014; Ammann 2013; Carvalho 2010; Kemoli 2010), or one domain (Ma 2012; Loguercio 2015).
Details of the assessments made are available in the risk of bias section of the Characteristics of included studies table and in the risk of bias graph (Figure 2) and risk of bias summary (Figure 3).
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Method of randomisation
Alhareky 2014; Ammann 2013; Carvalho 2010; Kemoli 2010; and Loguercio 2015 clearly stated the methods of randomisation used in the articles. Thus, we assessed these five studies at low risk of bias. We judged Ma 2012 at unclear risk of bias in its method of randomisation, because there was insufficient information to make a clear judgement.
Allocation concealment
We were unable to make a judgement of high or low risk of bias for allocation concealment as it was not adequately reported in five studies (Alhareky 2014; Ammann 2013; Carvalho 2010; Kemoli 2010; Ma 2012). While one study performed allocation concealment by tossing a coin before the restorative intervention (Loguercio 2015).
Blinding
We judged all of the included studies at high risk of performance bias, because the types of interventions did not permit blinding of the operators or the participants (Alhareky 2014; Ammann 2013; Carvalho 2010; Kemoli 2010; Loguercio 2015; Ma 2012).
We assessed three studies at low risk of detection bias (Carvalho 2010; Kemoli 2010; Loguercio 2015). In Carvalho 2010, they explicitly reported the blinding of outcome assessors; in Loguercio 2015, authors definitely illustrated that two experienced examiners, who were blinded and calibrated by training before evaluation, both evaluated all the restorations once independently and discussed to solve divergence; and in Kemoli 2010, as the authors clearly stated that the outcome assessors were calibrated and were not the operators, we believed that the outcome assessors had high possibility of being blinded. Two studies were at unclear risk of bias in the blinding of outcome assessment, because they did not mention the blinding of outcome assessors (Ammann 2013; Ma 2012). One study (Alhareky 2014) collecting patients self‐evaluation was considered at high risk of detection bias.
Incomplete outcome data
We judged attrition bias as being low in four studies, because they reported no losses to follow‐up (Alhareky 2014; Ammann 2013; Loguercio 2015; Ma 2012). Kemoli 2010 reported that 19.1% of the participants were lost to follow‐up, but did not provide information about the distribution of attrition between treatment groups. Thus, we assessed this study as having an unclear risk of bias for this domain. We also judged Carvalho 2010 at unclear risk of bias, because the reasons for the exclusions of participants were not fully described even though the number of exclusions in each group was comparable (14.7% in the control group and 18.5% in the rubber dam group). The cut‐off points used for deciding the risk of attrition bias may be subjective; therefore, readers of this review could interpret the risk of bias for this domain differently.
Selective reporting
We considered two studies as being at high risk of reporting bias (Ammann 2013; Carvalho 2010). In Ammann 2013, the authors did not fully report the data on the treatment time in fissure sealing; and in Carvalho 2010, as the survival/failure rate was not consistent with the number of restorations considered as success or failure presented, we were unable to use the data for analysis. We assessed Alhareky 2014; Kemoli 2010; Loguercio 2015; and Ma 2012 at low risk of reporting bias, because they fully reported all the prespecified outcomes.
Other potential sources of bias
Ma 2012 did not report the characteristics of participants at baseline to allow an assessment of the comparability of the intervention and control groups. Thus, we judged it at unclear risk of other bias. We considered Ammann 2013 and Carvalho 2010 at low risk of bias for other potential sources of bias, because they reported the comparability of the treatment and control groups at baseline. We also judged Alhareky 2014 and Loguercio 2015 as at low risk of other bias, as in these two split‐mouth studies, we could not find any contamination or carry‐across effect. In Kemoli 2010, there was a substantial baseline imbalance in the dental arch between rubber dam and cotton roll isolation groups, which might have influenced the performance of the restorations, so we assessed this study at high risk of bias for other potential sources of bias.
Effects of interventions
See: Table 1
Rubber dam versus cotton rolls
Five studies, at high risk of bias, compared rubber dam isolation method with cotton rolls as the alternative isolation method, and evaluated 1067 participants.
Primary outcomes
Survival rate of the restorations
Four studies reported the survival/loss rate of the restorations with rubber dam and cotton rolls isolation methods (Carvalho 2010; Kemoli 2010; Loguercio 2015; Ma 2012) (Additional Table 3). Ma 2012 reported the loss rate of the restorations at 6 months after treatment. Loguercio 2015 reported the restoration retention rates of two groups during follow‐ups of 6, 12, and 18 months respectively, with no significant statistical differences (P > 0.05). The results of meta‐analysis indicated that rubber dam usage may result in a higher retention rate of restorations in participants with non‐carious cervical lesions (NCCLs) receiving resin composite restorative treatment at six months, but the evidence is uncertain (odds ratio (OR) 2.29, 95% confidence interval (CI) 1.05 to 4.99; 2 studies, 192 participants, 222 teeth; low‐certainty evidence; Analysis 1.1). The evidence from a single study (Loguercio 2015) suggested that the usage of rubber dam may result in no difference in survival rate of NCCLs at 12 months (OR 1.38, 95% CI 0.45 to 4.28; 30 participants, 60 teeth; very low‐certainty evidence; Analysis 1.2), and 18 months (OR 1.00, 95% CI 0.45 to 2.25; 30 participants, 60 teeth; very low‐certainty evidence; Analysis 1.3). Carvalho 2010 reported the cumulative survival rate of dental restorations at 6, 12, 18, and 24 months. However, the number of restorations reported to have been performed at the start of the evaluation period and the number of restorations that failed at the end of the evaluation period were not consistent with the reported survival rate. Due to these inconsistencies, we were unable to include the data of this study in our analyses. Kemoli 2010 suggested a possible difference in the survival rate of dental restorations at two years in favour of rubber dam usage but the evidence was very uncertain (hazard ratio (HR) 0.80, 95% CI 0.66 to 0.97; 559 participants; very low‐certainty evidence; Analysis 1.4).
1.1. Analysis.

Comparison 1: Rubber dam versus cotton rolls, Outcome 1: Survival rate (6 months)
1.2. Analysis.

Comparison 1: Rubber dam versus cotton rolls, Outcome 2: Survival rate (12 months)
1.3. Analysis.

Comparison 1: Rubber dam versus cotton rolls, Outcome 3: Survival rate (18 months)
1.4. Analysis.

Comparison 1: Rubber dam versus cotton rolls, Outcome 4: Survival rate (24 months)
Adverse events
None of the included studies reported this outcome.
Secondary outcomes
Clinical evaluation of restoration's quality
Loguercio 2015, evaluated the performance of the restorations quality at baseline and during follow‐up (6, 12, and 18 months) and suggested no significant differences (P > 0.05, Fisher exact test for comparisons between groups and McNemar test for comparison among follow‐ups) regarding marginal staining and marginal adaptation of NCCLs restorations between rubber dam and cotton rolls/retraction cords groups.
Costs
None of the included studies reported the direct cost of the treatment. But two studies, at high risk of bias, reported the total time required for the restoration treatment (Ammann 2013; Loguercio 2015). Ammann 2013, evaluating 72 children, reported 12.4% less time (108 seconds) needed to accomplish fissure sealing using rubber dam compared to using cotton rolls as the isolation method. Loguercio 2015 reported the mean operation time of NCCL lesions restoration and its standard deviation (SD) for each group. The analysis results suggested little to no differences between groups (mean difference (MD) ‐0.40, 95% CI ‐2.26 to 1.46; 30 participants, 60 teeth; very low‐certainty evidence; Analysis 1.5).
1.5. Analysis.

Comparison 1: Rubber dam versus cotton rolls, Outcome 5: Chair time
Participant acceptance/satisfaction
Loguercio 2015 evaluated participants' acceptance/satisfaction by asking patients about their subjective feeling or preferences. The evidence did not support higher acceptance and preference rate for rubber dam than cotton rolls (P = 0.85 from binomial test on 28 participants; very low‐certainty evidence). The other four studies did not report the level of participant acceptance/satisfaction.
Rubber dam versus the Isolite system
One included study with 42 participants, at high risk of bias, compared rubber dam with the Isolite system (IS) as the alternative isolation method (Alhareky 2014).
Primary outcomes
Survival rate of the restorations
Alhareky 2014 did not report on our primary outcome of survival rate of the restorations.
Adverse events
Alhareky 2014 did not report this outcome.
Secondary outcomes
Clinical evaluation of restoration's quality
Alhareky 2014 did not report on our secondary outcome of clinical evaluation of restorations' quality.
Costs
Alhareky 2014 did not report the direct cost of the treatment but reported the intervention‐specific mean operation times and their SDs, and suggested that the use of the Isolite system may decrease the operation time of pit and fissure sealing for permanent molars compared to rubber dam but the evidence was very uncertain (MD 9.36, 95% CI 8.42 to 10.30; 42 participants, 168 teeth; very low‐certainty evidence; Analysis 2.1).
2.1. Analysis.

Comparison 2: Rubber dam versus the Isolite system, Outcome 1: Chair time
Participant acceptance/satisfaction
Alhareky 2014 suggested that the rubber dam may be associated with significantly lower satisfaction but the evidence was very uncertain, mainly explained by worse comfort (31%, P = 0.02) and less preferences (26%, P = 0.002).
Discussion
Summary of main results
Six studies met the inclusion criteria for this review; five studies evaluated the effects of rubber dam versus cotton roll isolation methods (Ammann 2013; Carvalho 2010; Kemoli 2010; Loguercio 2015; Ma 2012) while the remaining study made a comparison with the Isolite system (Alhareky 2014) on direct restorative treatments in dental patients, including pit and fissure sealing in permanent premolars or molars, proximal atraumatic restorative treatment (ART) in primary molars, and composite resin restorations of non‐carious cervical lesions (NCCLs) in permanent teeth. We assessed the certainty of the body of evidence based upon the GRADE approach, which takes into account the risk of bias of the included studies, the directness of the evidence, the consistency of the results (heterogeneity), the precision of the effect estimates, and the risk of publication bias (GRADE 2004). We have provided a summary of this certainty assessment for survival rates of rubber dam usage compared to cotton rolls at 6, 12, 18, and 24 months (Table 1).
The effect of rubber dam usage during dental restorative treatments on the restorations longevity remained undefinable. Compared to traditional cotton rolls, rubber dam isolation may favour a higher survival rate or a lower loss rate of dental direct restorations at 6 months after surgery (low‐certainty evidence) and at 24 months after surgery but the evidence is very uncertain for this longer follow‐up. Very uncertain evidence from a single small study suggested little to no effect on restorations survival at 12‐ and 18‐month follow‐ups.
We did not analyse the data for rubber dam versus cotton rolls in Carvalho 2010, because we found inconsistencies in the reported data. Ammann 2013 did not evaluate the survival rate of fissure sealants.
None of the included studies reported our second primary outcome of adverse events.
Overall completeness and applicability of evidence
The identified studies in the review did not address the objectives of the review sufficiently. Six studies were eligible for inclusion, and they only investigated participants receiving pit and fissure sealing, resin composite restorations of NCCLs and proximal ART restorative treatments. We found no eligible randomised controlled trials (RCTs) or split‐mouth trials enrolling participants receiving other types of restorative treatments such as inlays, onlays, etc. Furthermore, except for Loguercio 2015, other included studies did not fully report the outcomes and consequently the evidence was incomplete. Adverse effects, direct cost, restorations' quality and patients' acceptance are all important aspects in rubber dam usage (Hill 2008; Koshy 2002; Stewardson 2002). There were no included studies reporting adverse effects or the direct cost of the treatment, while three trials compared operation time cost among groups using different isolation methods (Alhareky 2014; Ammann 2013; Loguercio 2015). The quality of restorations at baseline and during follow‐ups was evaluated in only one study (Loguercio 2015). Two studies reported the acceptance/satisfaction of rubber dam compared to traditional cotton rolls isolation (Loguercio 2015) or the Isolite system, a new approach (Alhareky 2014).
Although four of the included studies reported the survival/loss rate, due to inconsistencies in data presentation, mainly due to differences in the restorative treatments carried out, follow‐up time points, or criteria used for the definition of 'survival/failure' among studies, we could only pool data from two studies comparing rubber dam with cotton rolls after adhesive restorations of NCCLs at six‐month follow‐up to address this primary outcome.
Quality of the evidence
The body of evidence that we identified did not allow for robust conclusions about the effects of rubber dam isolation for restorative treatment to be made. We included six studies, which analysed 1109 participants. We excluded one study from the analysis due to inconsistencies in the presented data (Carvalho 2010). The remaining five studies were at high risk of bias (Alhareky 2014; Ammann 2013; Kemoli 2010; Loguercio 2015; Ma 2012). When such risk of bias issues were considered alongside the fact that evidence for each outcome was concluded from one or two small studies and had wide confidence intervals including no effect (leading to serious or very serious imprecision), this resulted in us rating the evidence as very low or low certainty. These GRADE ratings can be interpreted as a lack of confidence in the effect estimates. Further research is likely to change the estimates and our confidence in them.
Potential biases in the review process
We searched multiple databases with no language restrictions, intending to limit bias by including all relevant studies. However, we did not include all of the included studies into the analysis, and this could have introduced bias into the review as it may distort our overall view of the effects of the rubber dam isolation method. Our subjective assessments that a loss to follow‐up of more than 20% constitutes a high attrition rate could also be interpreted as bias by some readers. However, we have presented all the related information, rationales for the method used, and our assessments with the intention of transparency and to allow the readers to reach their own conclusion.
Agreements and disagreements with other studies or reviews
To our knowledge, one systematic review has studied the influence of different operatory field isolation techniques on the longevity of dental restorations (Cajazeira 2014). Their inclusion criteria differed from the inclusion criteria of this review in that they only included studies evaluating the effects of the operatory field isolation techniques (rubber dam or cotton rolls/saliva ejector) on the longevity of direct restorations performed with tooth‐coloured materials in primary or permanent posterior teeth, and having a follow‐up period of at least 12 months. Moreover, the Cajazeira 2014 review included two studies that we excluded: Huth 2004, which we excluded since randomised allocation of participants was not performed between the two isolation groups in the study, and Raskin 2000, which we excluded due to inappropriate study design (randomisation and analysis at tooth level without accounting for the clustering effect of teeth within participants). They finally included four studies into the analysis (Carvalho 2010; Huth 2004; Kemoli 2010; Raskin 2000), and concluded that the use of rubber dam might not influence the longevity of restorations in comparison to using cotton rolls/saliva ejector.
There were also two retrospective studies discussing patients‐ and treatment‐related factors that might affect the primary teeth restorations' survival time. The results were in agreement with this review. Bücher 2015 drew the Kaplan‐Meier curve to reflect cumulative survival distributions of all 2388 subjects during eight‐year follow‐up, and concluded that the use of dental dam resulted in a significantly lower risk of fillings lost (hazard ration (HR) = 0.58, P = 0.02) overall. Similarly, Dalpian 2018, enrolling 316 restorations with a 36‐month follow‐up, also drew a conclusion through the survival curves, that restorations placed with rubber dam displayed significantly higher survival probability.
Although there is still no robust evidence on the effect of rubber dam usage in improving the survival rate and shortening treatment time of dental restorations, it does not mean that rubber dam usage is not important during restorative treatments. The usage of rubber dam still has numerous advantages, such as preventing accidental swallowing of restorative instruments or tooth fragments, protecting soft tissues from sharp instruments, or helping in behaviour management in children. Its important role in blocking cross‐infection of patients in hospital, especially under the coronavirus disease (COVID‐19) pandemic at present, should also be emphasized. Clinicians still need to practice rubber dam placement, and never using a rubber dam would not be an acceptable approach.
Authors' conclusions
Implications for practice.
Low‐ and very low‐certainty evidence suggests that compared to traditional cotton rolls isolation method, the use of rubber dam in dental direct restorative treatments may lead to a higher survival rate of dental restorations and to little or no difference in operation time. However, due to a high risk of bias in the analysed studies, the small number of included studies, and that the type of restorative treatments varied among studies, the effects estimate should be interpreted with caution. This review found no evidence to support or refute any adverse effects that the rubber dam isolation method may have on patients.
Implications for research.
The fact that we are unable to make a robust conclusion on the effects of using rubber dam isolation during restorative treatments in dental patients demonstrates that more well‐designed randomised controlled trials with longer follow‐up periods are needed. In particular, we found a lack of studies investigating the effects of the isolation methods on the performance of indirect restorations. Further properly designed high‐quality research is required, as we excluded a few studies due to inappropriate statistical analysis, such as performing randomisation and analysis at tooth level without accounting for the clustering effect of teeth within participants. Sufficient and appropriate sample size as well as follow‐up periods should be taken into account before a trial begins. Additionally, studies should report the survival rate of restorations and perform clinical evaluation of the quality of the restorations based upon US Public Health Service criteria. Adverse effects, participant acceptance/satisfaction, and the direct cost of the treatment should also be clearly reported at the participant level per group.
What's new
| Date | Event | Description |
|---|---|---|
| 13 January 2021 | New search has been performed | Searches updated 13 January 2021 |
| 13 January 2021 | New citation required but conclusions have not changed | Review update includes 2 new trials bringing the total to 6 included studies. Conclusions remain the same. New co‐authors |
History
Protocol first published: Issue 5, 2012 Review first published: Issue 9, 2016
Acknowledgements
We would like to thank the Cochrane Oral Health editorial team for their help in conducting this systematic review; Jennifer Hilgart, Nicole Pitcher, Alison Qualtrough, Patrick Sequeira‐Byron, and Trevor Burke for their helpful feedback. We would also like to thank Anne Littlewood for designing the search strategy, conducting and updating database searches; Janet Lear for helping with obtaining full‐text articles; and Luisa Fernandez Mauleffinch for copy editing and facilitating the review.
Appendices
Appendix 1. Cochrane Oral Health's Trials Register search strategy
Cochrane Oral Health's Trials Register is available via the Cochrane Register of Studies. For information on how the register is compiled, see oralhealth.cochrane.org/trials.
("rubber dam*" or "oral dam*" or "dental dam*" or "latex dam*" or Kofferdam* or "Optra dam*" or "Optradam Plus" or Optidam* or Flexidam* or "Hygenic Fiesta")
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 MeSH descriptor Dental restoration, permanent explode all trees #2 MeSH descriptor Dental restoration, temporary explode all trees #3 ( (dental in All Text near/5 restor* in All Text) or (teeth in All Text near/5 restor* in All Text) or (tooth in All Text near/5 restor* in All Text) or (dental in All Text near/5 fill* in All Text) or (teeth in All Text near/5 fill* in All Text) or (tooth in All Text near/5 fill* in All Text) ) #4 MeSH descriptor Dental atraumatic restorative treatment this term only #5 ( (dental in All Text or tooth in All Text or teeth in All Text) and ("atraumatic restorative treatment" in All Text or ART in All Text) ) #6 MeSH descriptor Dental amalgam this term only #7 MeSH descriptor Glass ionomer cements this term only #8 ( (dental in All Text or tooth in All Text or teeth in All Text) and (restor* in All Text and (inlay in All Text or in‐lay in All Text or onlay in All Text or on‐lay in All Text or post* in All Text or dowel* in All Text or pin* in All Text) ) ) #9 ( (dental in All Text or tooth in All Text or teeth in All Text) and (amalgam* in All Text or resin* in All Text or cement* in All Text or ionomer* in All Text or compomer* in All Text or composite* in All Text) ) #10 MeSH descriptor Crowns explode all trees #11 ( (dental in All Text near/5 crown* in All Text) or (tooth in All Text near/5 crown* in All Text) or (teeth in All Text near/5 crown* in All Text) or (dental in All Text near/5 coronal* in All Text) or (tooth in All Text near/5 coronal* in All Text) or (teeth in All Text near/5 coronal* in All Text) ) #12 MeSH descriptor Denture, partial explode all trees #13 MeSH descriptor Dental veneers explode all trees #14 ( (dental in All Text or tooth in All Text or teeth in All Text) and (bridge* in All Text or veneer* in All Text or pontic* in All Text or laminate* in All Text) ) #15 (partial in All Text near/5 denture* in All Text) #16 (#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15) #17 MeSH descriptor Rubber dams this term only #18 ( (rubber in All Text near/6 dam* in All Text) or (oral in All Text near/6 dam* in All Text) or (dental in All Text near/6 dam* in All Text) or (latex in All Text near/6 dam* in All Text) or Kofferdam in All Text) #19 ("Optra Dam" in All Text or "OptraDam Plus" in All Text or OptiDam in All Text or FlexiDam in All Text or "Hygenic Fiesta" in All Text) #20 (#17 or #18 or #19) #21 (#16 and #20)
Appendix 3. MEDLINE Ovid search strategy
1. exp Dental restoration, permanent/ 2. exp Dental restoration, temporary/ 3. ((dental or tooth or teeth) adj5 (restor$ or fill$)).ti,ab. 4. Dental atraumatic restorative treatment/ 5. ((dental or tooth or teeth) and ("atraumatic restorative treatment" or ART)).ti,ab. 6. Dental amalgam/ 7. Glass ionomer cements/ 8. ((dental or tooth or teeth) and (restor$ and (inlay or in‐lay or onlay or on‐lay or post$ or dowel$ or pin$))).mp. 9. ((dental or tooth or teeth) adj5 (amalgam$ or resin$ or cement$ or ionomer$ or compomer$ or composite$)).mp. 10. exp Crowns/ 11. ((dental or tooth or teeth) adj5 (crown$ or coronal$)).ti,ab. 12. exp Denture, Partial/ 13. exp Dental veneers/ 14. ((dental or tooth or teeth) adj5 (bridge$ or veneer$ or pontic$ or laminate$)).mp. 15. (partial adj5 denture$).mp. 16. or/1‐15 17. Rubber dams/ 18. ((rubber adj dam$) or (oral adj dam$) or (dental adj dam$) or (latex adj dam$) or Kofferdam).mp. 19. ("Optra Dam" or "OptraDam Plus" or OptiDam or FlexiDam or "Hygenic Fiesta").mp. 20. or/17‐19
Appendix 4. Embase Ovid search strategy
1. exp Reparative dentistry/ 2. ((dental or tooth or teeth) adj5 (restor$ or fill$)).ti,ab. 3. ((dental or tooth or teeth) and ("atraumatic restorative treatment" or ART)).ti,ab. 4. Dental alloy/ 5. Glass ionomer/ 6. ((dental or tooth or teeth) and (restor$ and (inlay or in‐lay or onlay or on‐lay or post$ or dowel$ or pin$))).mp. 7. ((dental or tooth or teeth) adj5 (amalgam$ or resin$ or cement$ or ionomer$ or compomer$ or composite$)).mp. 8. exp Crowns/ 9. ((dental or tooth or teeth) adj5 (crown$ or coronal$)).ti,ab. 10. exp Denture 11. ((dental or tooth or teeth) adj5 (bridge$ or veneer$ or pontic$ or laminate$)).mp. 12. (partial adj5 denture$).mp. 13. or/1‐12 14. ((rubber adj dam$) or (oral adj dam$) or (dental adj dam$) or (latex adj dam$) or Kofferdam).mp. 15. ("Optra Dam" or "OptraDam Plus" or OptiDam or FlexiDam or "Hygenic Fiesta").mp. 16. 14 or 15 17. 13 and 16
Appendix 5. LILACS BIREME Virtual Health Library search strategy
(dental or dentária or tooth or teeth or dente$ or diente$) [Words] and (Mh Rubber dams or "rubber dam$" or "dique$ de goma" or "dique$ de borracha" or "dental dam$" or "latex dam$" or "oral dam$" or Kofferdam or "Optra Dam" or "OptraDam Plus" or OptiDam or FlexiDam or "Hygenic Fiesta") [Words]
Appendix 6. SciELO BIREME Virtual Health Library search strategy
rubber dam
Appendix 7. Chinese BioMedical Literature Database (CBM) search strategy
1. Mesh: rubber dam 2. Keyword: rubber dam 3. #2 or #1
(This search strategy was translated from Chinese.)
Appendix 8. VIP database search strategy
rubber dam
(This search strategy was translated from Chinese.)
Appendix 9. China National Knowledge Infrastructure (CNKI) search strategy
rubber dam
(This search strategy was translated from Chinese.)
Appendix 10. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
rubber dam
Appendix 11. WHO International Clinical Trials Registry Platform search strategy
rubber dam
Appendix 12. OpenGrey search strategy
rubber dam
Appendix 13. Sciencepaper Online search strategy
rubber dam
(This search strategy was translated from Chinese.)
Data and analyses
Comparison 1. Rubber dam versus cotton rolls.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Survival rate (6 months) | 2 | Odds Ratio (IV, Fixed, 95% CI) | 2.29 [1.05, 4.99] | |
| 1.2 Survival rate (12 months) | 1 | Odds Ratio (IV, Fixed, 95% CI) | 1.38 [0.45, 4.28] | |
| 1.3 Survival rate (18 months) | 1 | Odds Ratio (IV, Fixed, 95% CI) | 1.00 [0.45, 2.25] | |
| 1.4 Survival rate (24 months) | 1 | 559 | Hazard Ratio (IV, Fixed, 95% CI) | 0.80 [0.66, 0.97] |
| 1.5 Chair time | 1 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐2.26, 1.46] |
Comparison 2. Rubber dam versus the Isolite system.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Chair time | 1 | Mean Difference (IV, Fixed, 95% CI) | 9.36 [8.42, 10.30] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alhareky 2014.
| Study characteristics | ||
| Methods | Design: split‐mouth RCT Recruitment period: not reported Administration setting: clinic in the Department of Pediatric Dentistry at Tufts University School of Dental Medicine Country: USA Funding source: in part by US Department of Health and Human Services Health Resources and Services Administration grant D84HP19955 |
|
| Participants | Number of participants randomised: 42 patients Age: 7 to 16 years old, mean age 12.3 years old Sex: 19 males, 23 females Inclusion criteria:
Exclusion criteria:
Number of participants evaluated: 42 patients Withdrawals/loss to follow‐up: none |
|
| Interventions | Total number of groups: 2 Intervention: rubber dam: "First, gingival soft tissue surrounding the tooth was dried. Topical anaesthesia was achieved using 20 per cent benzocaine gel, which was applied for one minute, according to the manufacturer’s instructions. A wingless clamp appropriate for use on molars was selected and then used in conjunction with a latex‐free RD sheet. No bite block was used with the RD" Control: Isolite system: "First, the isthmus (narrow part in the middle of the IS plastic mouthpiece) was placed at the corner of mouth, and the patient was instructed to open widely. The IS mouthpiece was then inserted while folding the cheek shield forward toward the tongue retractor and sliding the isthmus into the cheek. The patient was asked to bite on the bite block part of the IS. Finally, the cheek shield was tucked into the buccal vestibule, and the tongue retractor was tucked into the tongue vestibule. The high‐speed evacuation system was connected to the IS system, and a second high‐speed suction was used to evacuate the mouth during the sealant placement application" Restorative treatments: pit and fissure sealants on permanent molars |
|
| Outcomes | Outcomes:
Time points: immediately after restorative procedure |
|
| Notes | Adverse events: not reported This study was classified into 'studies awaiting classification' in the previous version of this review. It is now included after getting details of the method of randomisation used, preformation of allocation concealment, and funding sources from study authors |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation schedule was generated using R 2.11.1 software (R Foundation for Statistical Computing, Murray Hill, NJ, USA)" Comment: method stated and appropriate |
| Allocation concealment (selection bias) | Unclear risk | Not reported Comment: insufficient information reported to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The operators and patients were not blinded" Comment: high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Patients themselves were assessors by filling in the questionnaire Comment: the examiners were not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None lost to follow‐up Comment: low risk of bias |
| Selective reporting (reporting bias) | Low risk | Comment: the stated objectives and methods of the study appeared to match the listed outcomes, low risk of bias |
| Other bias | Low risk | No contamination and carry‐across effect was detected Comment: low risk of bias |
Ammann 2013.
| Study characteristics | ||
| Methods | Design: parallel‐group RCT Recruitment period: not stated Administration setting: private dental clinic Country: Germany Funding source: Dentsply DeTrey, Konstanz, Germany |
|
| Participants | Number of participants randomised: 72 (rubber dam: 34; cotton rolls: 38) Randomisation unit: participant Age: 5.9 to 16.9 years, mean age 11.1 years Sex: 23 boys, 49 girls Inclusion criteria:
Exclusion criteria:
Number of participants evaluated: 72 (rubber dam: 34; cotton rolls: 38) Withdrawals/loss to follow‐up: no withdrawals |
|
| Interventions | Number of groups: 2 Intervention: rubber dam: "A suitable rubber dam clamp (Ivoryò; Sigma Dental Systems, Handewitt, Germany) was selected and applied. Afterwards, the rubber dam was placed over the clamp. Several teeth were included in the rubber dam in cases involving premolars, whereas for molars only the treated tooth was isolated" Control: cotton rolls: "The cotton rolls were positioned on the buccal and lingual region of the tooth to be sealed and were fixed by the operator's index finger and middle finger. Additionally, a saliva ejector was placed on the lingual side" Restorative treatment: pit and fissure sealants on premolars/molars |
|
| Outcomes | Outcomes:
Time points: immediately after restorative procedure |
|
| Notes | Adverse events: not stated No details on sample size or power calculation were provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "72 subjects successfully took part in the study and were divided into two parallel groups by a dental assistant by drawing sealed lots (test n = 34; control n = 38)" Comment: method stated and appropriate |
| Allocation concealment (selection bias) | Unclear risk | Not stated Comment: insufficient information reported to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: the operators and the participants could not be blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated Comment: insufficient information reported to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals |
| Selective reporting (reporting bias) | High risk | Quote: "The time needed to finish the fissure sealing treatment was 12.4% (108 s [seconds]) less when using rubber dam (P < 0.05)" Comment: insufficient information reported to use the data in the analysis |
| Other bias | Low risk | Comparable groups at baseline (age, gender, type of teeth treated) |
Carvalho 2010.
| Study characteristics | ||
| Methods | Design: parallel‐group RCT Recruitment period: not stated Administration setting: schools Country: Brazil Funding source: the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) |
|
| Participants | Number of participants randomised: 232; 232 teeth (rubber dam: 115; cotton rolls: 117) Randomisation unit: participant/tooth Age: 6 to 7 years, mean age 6.3 years Sex: 128 boys, 104 girls Inclusion criteria:
Exclusion criteria:
Number of participants evaluated: 155 (rubber dam: 72 teeth; cotton rolls: 83 teeth) Withdrawals/loss to follow‐up: 77 children in total. 48 children were unavailable at the time of assessment. 29 children lost their teeth due to exfoliation or extraction |
|
| Interventions | Number of groups: 2 Intervention: rubber dam: "For the experiment group, a rubber dam was used, fixed with a clamp on the adjacent distal tooth without local anaesthesia" Control: cotton rolls: "New cotton rolls were placed on both sides of the molar without local anaesthesia" Restorative treatment: proximal ART in primary molars |
|
| Outcomes | Outcomes:
Time points: 6, 12, 18, and 24 months after restoration placement Diagnostic criteria: restorations assessed according to the following criteria:
|
|
| Notes | Adverse events: not stated No details on sample size or power calculation provided The survival/failure rate was not consistent with the number of restorations considered as success or failure presented in table 1 of the report. We were unable to use the data in the analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Each child was individually allocated into a group by the use of generated random numbers, and no restrictions were considered" Comment: method stated and appropriate |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Each child was individually allocated into a group by the use of generated random numbers, and no restrictions were considered. The group in charge of making the restorations or those who assessed the restorations did not have access to the randomizations procedure. All children were allocated into the respective group before the restorations were made" Comment: sequence allocation was not adequately described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: the operators and the participants could not be blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "These examiners were blinded to the exposure categories. In other words, at the time of examination of the restoration, the examiners did not know to which group the child belonged to" Comment: examiners were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Throughout the study, a total of 48 (20.7%) children were considered as lost to follow‐up. Others eventually lost their teeth due to exfoliation or extraction. Due to such reasons, a total of 77 restorations (33.2%) were censored (lost to follow‐up), where 34 (14.7%) were from the control group and 43 (18.5%) from the rubber dam group (χ2 [Chi2] = 1.82; df [degrees of freedom] = 1; P = 0.18)" Comment: loss to follow‐up was high (overall 33.2%) and reasons for loss to follow‐up (20.7%) were not explicitly explained |
| Selective reporting (reporting bias) | High risk | Comment: survival/failure rate was not consistent with the number of restorations considered as success or failure presented in table 1. We were unable to use the data in the analysis |
| Other bias | Low risk | Comment: groups at baseline (age, gender, jaw, molar and operator) comparable |
Kemoli 2010.
| Study characteristics | ||
| Methods | Design: parallel‐group RCT Recruitment period: not stated Administration setting: public primary schools Country: Kenya Funding source: Netherlands Universities' Foundation for International Cooperation (NUFFIC), financial support from the University of Nairobi, GC Europe and 3M ESPE (Netherlands) |
|
| Participants | Number of participants randomised: 804; 804 teeth (rubber dam: 404; cotton rolls: 397) Randomisation unit: participant/tooth Age: 6 to 8 years Sex: 454 boys, 350 girls Inclusion criteria:
Exclusion criteria: not stated Number of participants evaluated: 648 (number in each group not stated) Withdrawals/loss to follow‐up:
|
|
| Interventions | Number of groups: 2 Intervention: rubber dam: "The rubber dam (Medium‐dark, Hygenic Dental Dam, HCM ‐ Hygienic Corporation, Malaysia) was used to isolate the tooth to be restored. A 2‐minute gingival application of a topical anaesthetic (Lidocaine 50 mg/g cream) was used prior to the application of the rubber dam clamp (FIT ‐ Kofferdam Klammer, U67, Hager & Werken GmbH & Co KG Germany). No other local analgesic was used in the study" Control: cotton rolls: "The cotton wool rolls were place buccally (maxillary teeth) or lingually and buccally (mandibular teeth)" Restorative treatment: proximal ART in primary molars |
|
| Outcomes | Outcomes:
Time points: within 2 hours of restoring each tooth, after 1 week, and 1, 5, 12, 18, and 24 months after the restoration Diagnostic criteria:
|
|
| Notes | Adverse events: not reported Sample size: calculated sample size was 382, but no details provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using random numbers, the children were assigned to an isolation method, material, operator and assistant. Each child had the restoration randomly placed in the primary molar in either mandibular or maxillary arch" Comment: method stated and appropriate |
| Allocation concealment (selection bias) | Unclear risk | Not stated Comment: insufficient information reported to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: operators and participants could not be blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The evaluators had not restored the cavities but had been trained and calibrated in the technique" Comment: operators were not the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Save for 3 cases that were improperly documented. Because of truancy 38 (4.7%) of the restorations the 801 documented cases could not be evaluated soon after placement, leaving only 763 restorations to be evaluated. Due to the study‐population attrition resulting from dropouts, school‐transferees, absentees and 1 death, only 648 (80.9%) children could be evaluated at the end of 2 years" Comment: overall losses < 20%, and reasons were listed. However, no details on the number and reasons for withdrawals in each group given |
| Selective reporting (reporting bias) | Low risk | Comment: outcomes were reported as planned |
| Other bias | High risk | Comment: groups at baseline (dental arch) not comparable 405 restorations were isolated with rubber dam, 101 of which were restorations in the mandible; and 397 were isolated with cotton rolls, 141 of them were restorations in the mandible (Fisher's Exact Test, P = 0.001) |
Loguercio 2015.
| Study characteristics | ||
| Methods | Design: split‐mouth RCT Recruitment period: April to October 2010 Administration setting: clinic of the School of Dentistry at the State University of Ponta Grossa (Paraná, Brazil) Country: Brazil Funding source: National Council for Scientific and Technological Development (CNPq), restorative products supported by SDI Brazil |
|
| Participants | Number of participants randomised: 30 patients Age: ≥ 20 years (mean = 45 years) Sex: 12 males, 18 females Inclusion criteria:
Exclusion criteria:
Number of participants evaluated: 30 patients Withdrawals/loss to follow‐up: none |
|
| Interventions | Total number of groups: 2 Intervention: rubber dam: "the rubber dam was inserted (Madeitex, São José dos Campos, Brazil) along with the rubber dam retainer No. 212 (KG Sorensen, Barueri, Brazil)" Control: cotton rolls/retraction cord: "a mouth retractor (Arc‐Flex, FGM Dent Prod Ltda, Joinville, Brazil) was applied, and cotton rolls and saliva ejectors were used to keep the operative field dry. The gingival tissue of teeth was retracted with the retraction cord (Proretract, FGM Dent Prod Ltda)" Restorative treatment: adhesive restorations of NCCLs |
|
| Outcomes | Outcomes:
Time points: immediately after restorative procedure, 1 week, 6, 12, and 18 months after the restoration. Diagnostic criteria:
|
|
| Notes | Adverse events: not reported This article was published in November to December 2015 but failed to be retrieved in previous searches up to August 2016. The reason may be the delay in articles being uploaded to electronic databases, and the journal was not included in handsearching |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In each subject, the choice of each isolation method was randomly determined by tossing a coin before the restorative intervention in order to guarantee concealment of the allocation" Comment: method stated and appropriate, low risk of bias |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was conducted by tossing a coin before the restorative intervention Comment: low risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The patient and the operator were not blinded to the procedure, but the examiner was" Comment: high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The patient and the operator were not blinded to the procedure, but the examiner was" Comment: the examiners were blinded, low risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up Comment: low risk of bias |
| Selective reporting (reporting bias) | Low risk | The stated objectives and methods of the study appeared to match the listed outcomes Comment: low risk of bias. |
| Other bias | Low risk | No contamination and carry‐across effect was detected Comment: low risk of bias |
Ma 2012.
| Study characteristics | ||
| Methods | Design: parallel‐group RCT Recruitment period: 2009 to 2011 Administration setting: dental clinical of hospital Country: China Funding source: not stated |
|
| Participants | Number of participants randomised: 162; 162 teeth (rubber dam: 81; cotton rolls: 81) Randomisation unit: participant/tooth Age: not stated Sex: not stated Inclusion criteria (as translated):
Exclusion criteria: not stated Number of participants evaluated: 162; 162 teeth (rubber dam: 81; cotton rolls: 81) Withdrawals/loss to follow‐up: no losses to follow‐up |
|
| Interventions | Number of groups: 2 Intervention: rubber dam (as translated): "isolated with rubber dam (Optra Dam, Ivoclar Vivadent, 0.22 ~ 0.27 mm)" Control: cotton rolls (as translated): "isolated with cotton rolls placed in buccal and lingual vestibule" Restorative treatment: composite restorations of NCCLs |
|
| Outcomes | Outcomes (as translated):
Time points: 6 months after restorative treatment Diagnostic criteria:
|
|
| Notes | Adverse events: not stated Sample size calculation: no details reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (as translated): "One hundred and sixty‐two patients with non‐carious cervical lesions were stratified randomly distributed into two groups (n = 81) from June 2009 to June 2011" Comment: method of sequence generation not stated. Insufficient information reported to make a judgement |
| Allocation concealment (selection bias) | Unclear risk | Not stated Comment: insufficient information reported to make a judgement |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: operators and participants could not be blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated Comment: insufficient information reported to make a judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Comment: outcomes reported as planned |
| Other bias | Unclear risk | Comment: no data on group comparability provided |
ART: atraumatic restorative treatment; IS: Isolite system; NCCLs: non‐carious cervical lesions; RCT: randomised controlled trial; RD: rubber dam.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Al‐Amad 2017 | Insufficient follow‐up period length. It is a short‐term study evaluating the effect of rubber dam usage on bacterial contamination of the dentist’s head instead of its influence on dental restorations |
| Daudt 2013 | Inappropriate study design. The study set randomisation and analysis units at tooth level without accounting for the clustering effect of teeth within individual participants |
| Favetti 2021 | Inappropriate study design. The study set randomisation and analysis units at tooth level without accounting for the clustering effect of teeth within individual participants |
| Ganss 1999 | Randomisation allocation not performed between the rubber dam and cotton rolls isolation groups |
| Huth 2004 | Study was a CCT as randomisation allocation was not performed between the 2 treatment groups, and using teeth as the analysis unit |
| Ibrahim 2020 | No dental restoration performed. The study assessed the nature of tooth colour change resulting from dehydration due to rubber dam application before a restoration was placed |
| Luz 2012 | Inappropriate study design. The study employed different restorative treatments and materials on participants of 2 groups, in other words, whether rubber barrier was used was not the only variable |
| NCT01506830 | Inappropriate study design. The study authors kindly provided us with a pre‐publication copy of the study and we were able to see that the study claimed to be performed using a split‐mouth design, but not carried out it in an appropriate way |
| Raskin 2000 | Inappropriate study design. The study set randomisation and analysis units at tooth level without accounting for the clustering effect of teeth within individual participants |
| Sabbagh 2011 | Conference abstract without mentioning randomisation allocation between the 2 treatment groups, and author contact failed |
| Smales 1993 | Study was a CCT as randomisation allocation was not performed between the 2 treatment groups, and using teeth as the analysis unit |
| Straffon 1985 | Randomisation allocation not performed between the rubber dam and cotton roll isolation groups and using tooth surfaces as the analysis unit |
| van Dijken 1987 | Study was a CCT as randomisation allocation was not performed between the 2 treatment groups |
CCT: controlled clinical trial.
Differences between protocol and review
Deleted quasi‐randomised controlled trials from inclusion criteria.
Added participant acceptance/satisfaction as a secondary outcome.
Used risk ratio as a measure of the survival/success rate of the restorative treatment.
Specified types of subgroup analyses intended to perform.
Contributions of authors
Screening the search results and retrieving the papers: Cheng Miao (CM), Xiaoyu Yang (XY). Data extraction and risk of bias assessment: CM, XY, and Yan Wang (YW). Analysing the data and interpreting the results: CM, XY, and May CM Wong (MW). Writing the results, discussion, conclusions, and abstract: CM, XY, YW, Chunjie Li (CL), and MW. Providing a clinical perspective: Xuedong Zhou (XZ) and Jing Zou (JZ). XY and CM contributed equally to producing this systematic review.
Sources of support
Internal sources
West China School of Stomatology, Sichuan University, China
West China Hospital of Stomatology, Sichuan University, China
State Key Laboratory of Oral Diseases, Sichuan University, China
External sources
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the Evidence Synthesis Programme, the NIHR, the NHS, or the Department of Health and Social Care.
-
Cochrane Oral Health Global Alliance, Other
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships-alliances). Contributors in the last 2 years have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and Swiss Society of Endodontology, Switzerland.
Declarations of interest
Cheng Miao: none known. Xiaoyu Yang: none known. May CM Wong: none known. May CM Wong is an Editor with Cochrane Oral Health. Jing Zou: none known. Xuedong Zhou: none known. Chunjie Li: none known. Yan Wang: none known.
Author contributed equally to this review update
Author contributed equally to this review update
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Alhareky 2014 {published data only}
- Alhareky MS, Mermelstein D, Finkelman M, Alhumaid J, Loo C. Efficiency and patient satisfaction with the Isolite system versus rubber dam for sealant placement in pediatric patients. Pediatric Dentistry 2014;36(5):400-4. [PubMed] [Google Scholar]
Ammann 2013 {published data only}
- Ammann P, Kolb A, Lussi A, Seemann R. Influence of rubber dam on objective and subjective parameters of stress during dental treatment of children and adolescents - a randomized controlled clinical pilot study. International Journal of Paediatric Dentistry 2013;23(2):110-5. [DOI] [PubMed] [Google Scholar]
Carvalho 2010 {published data only}
- Carvalho TS, Sampaio FC, Diniz A, Bönecker M, Van Amerongen WE. Two years survival rate of Class II ART restorations in primary molars using two ways to avoid saliva contamination. International Journal of Paediatric Dentistry 2010;20(6):419-25. [DOI] [PubMed] [Google Scholar]
Kemoli 2010 {published data only}
- Kemoli AM, Amerongen WE, Opinya GN. Influence of the experience of operator and assistant on the survival rate of proximal ART restorations - two-year results. European Archives of Paediatric Dentistry 2009;10(4):243-8. [DOI] [PubMed] [Google Scholar]
- Kemoli AM, Amerongen WE, Opinya GN. Short communication: influence of different isolation methods on the survival of proximal ART restorations in primary molars after two years. European Archives of Paediatric Dentistry 2010;11(3):136-9. [DOI] [PubMed] [Google Scholar]
Loguercio 2015 {published data only}
- Loguercio AD, Luque-Martinez I, Lisboa AH, Higashi C, Queiroz VA, Rego RO, et al. Influence of isolation method of the operative field on gingival damage, patients' preference, and restoration retention in non-carious cervical lesions. Operative Dentistry 2015;40(6):581-93. [DOI] [PubMed] [Google Scholar]
Ma 2012 {published data only}
- Ma J. Influence of rubber dam isolation on the performance of restorations for teeth wedge-shaped defects. Chinese Community Doctors 2012;14(309):164. [Google Scholar]
References to studies excluded from this review
Al‐Amad 2017 {published data only}
- Al-Amad SH, Awad MA, Edher FM, Shahramian K, Omran TA. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. Journal of Infection and Public Health 2017;10(2):195-200. [DOI] [PubMed] [Google Scholar]
Daudt 2013 {published data only}
- Daudt E, Lopes GC, Vieira LCC. Does operatory field isolation influence the performance of direct adhesive restorations? Journal of Adhesive Dentistry 2013;15(1):27-32. [DOI] [PubMed] [Google Scholar]
- Daudt E, Lopes GC, Vieira LCC. Does the isolation method influence the performance of direct restorations? In: 89th General Session of the International Association for Dental Research; 2011 March 14-19; San Diego (CA). Alexandria (VA): International Association for Dental Research, 2011:Abstract No 1697.
Favetti 2021 {published data only}
- Favetti M, Montagner AF, Fontes ST, Martins TM, Masotti AS, Jardim PDS, et al. Effects of cervical restorations on the periodontal tissues: 5-year follow-up results of a randomized clinical trial. Journal of Dentistry 2021;106:103571. [DOI] [PubMed] [Google Scholar]
Ganss 1999 {published data only}
- Ganss C, Klimek J, Gleim A. One year clinical evaluation of the retention and quality of two fluoride releasing sealants. Clinical Oral Investigations 1999;3:188-93. [DOI] [PubMed] [Google Scholar]
Huth 2004 {published data only}
- Huth KC, Manhard J, Hickel R, Kunzelmann K. Three-year clinical performance of a compomer in stress-bearing restorations in permanent posterior teeth. American Journal of Dentistry 2003;16(4):255-9. [PubMed] [Google Scholar]
- Huth KC, Manhard J, Selbertinger A, Paschos E, Kaaden C, Kunzelmann K, et al. 4-year clinical performance and survival analysis of Class I and II compomer restorations in permanent teeth. American Journal of Dentistry 2004;17(1):51-5. [PubMed] [Google Scholar]
Ibrahim 2020 {published data only}
- Ibrahim SH, Steit SA. Assessment of tooth shade after de-and re-hydration during clinical restorative procedures: a randomized clinical trial. Egyptian Dental Journal 2020;66(4):2705-14. [Google Scholar]
Luz 2012 {published data only}
- Luz PB, Barata JS, Meller CR, Slavutsky SMBD, Araujo FBD. ART acceptability in children: a randomized clinical trial. Revista da Faculdade de Odontologia de Porto Alegre 2012;53(1):27-31. [Google Scholar]
NCT01506830 {unpublished data only}
- NCT01506830. Cervical restorations placed under two isolation methods [Influence of operatory field isolation techniques on the clinical performance of class V restorations]. clinicaltrials.gov/ct2/show/NCT01506830 (first received 10 January 2012).
Raskin 2000 {published data only}
- Raskin A, Setcos JC, Vreven J, Wilson NHF. Clinical evaluation of a posterior composite 10-year report. Journal of Dentistry 1999;27:13-9. [DOI] [PubMed] [Google Scholar]
- Raskin A, Setcos JC, Vreven J, Wilson NHF. Influence of the isolation method on the 10-year clinical behaviour of posterior resin composite restorations. Clinical Oral Investigations 2000;4(3):148-52. [DOI] [PubMed] [Google Scholar]
Sabbagh 2011 {published data only}
- Sabbagh J, Dagher S, El-Osta N, Souhaid P. One year clinical evaluation of vertise flow. In: 45th Meeting of the Continental European Division of the International Association for Dental Research; 2011 Aug 31- Sept 3; Budapest, Hungary. Alexandria (VA): International Association for Dental Research, 2011:Abstract No 232.
Smales 1993 {published data only}
- Smales RJ. Effect of rubber dam isolation on restoration deterioration. American Journal of Dentistry 1992;5(5):277-9. [PubMed] [Google Scholar]
- Smales RJ. Rubber dam usage related to restoration quality and survival. British Dental Journal 1993;174(9):330-3. [DOI] [PubMed] [Google Scholar]
Straffon 1985 {published data only}
- Straffon LH, Dennison JB, More FG. Three-year evaluation of sealant: effect of isolation on efficacy. Journal of the American Dental Association 1985;110(5):714-7. [DOI] [PubMed] [Google Scholar]
van Dijken 1987 {published data only}
- Dijken JWV, Hörstedt P. Effect of the use of rubber dam versus cotton rolls on marginal adaptation of composite resin fillings to acid-etched enamel. Acta Odontologica Scandinavica 1987;45:303-8. [DOI] [PubMed] [Google Scholar]
Additional references
Ahmad 2009
- Ahmad IA. Rubber dam usage for endodontic treatment: a review. International Endodontic Journal 2009;42(11):963-72. [DOI] [PubMed] [Google Scholar]
Al‐Amad 2017
- Al-Amad SH, Awad MA, Edher FM, Shahramian K, Omran TA. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. Journal of Infection and Public Health 2016;10(2):195-200. [DOI] [PubMed] [Google Scholar]
Atkins 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Begg 1994
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50(4):1088-101. [PubMed] [Google Scholar]
Berglund 1991
- Berglund A, Molin M. Mercury levels in plasma and urine after removal of all amalgam restorations: the effect of using rubber dams. Dental Materials 1991;13(5):297-304. [DOI] [PubMed] [Google Scholar]
Bhuva 2008
- Bhuva B, Chong BS, Patel S. Rubber dam in clinical practice. Endodontic Practice Today 2008;2(2):131-41. [Google Scholar]
Bücher 2015
- Bücher K, Metz I, Pitchika V, Hickel R, Kühnisch J. Survival characteristics of composite restorations in primary teeth. Clinical Oral Investigations 2015;19(7):1653-62. [DOI] [PubMed] [Google Scholar]
Cajazeira 2014
- Cajazeira MR, De Sabóia TM, Maia LC. Influence of the operatory field isolation technique on tooth-colored direct dental restorations. American Journal of Dentistry 2014;27(3):155-9. [PubMed] [Google Scholar]
Carrotte 2000
- Carrotte PV. Current practice in endodontics: 3. Access is success, and rubber dam is easy. Dental Update 2000;27(9):436-40. [DOI] [PubMed] [Google Scholar]
Carrotte 2004
- Carrotte P. Endodontics: Part 6. Rubber dam and access cavities. British Dental Journal 2004;197(9):527-34. [DOI] [PubMed] [Google Scholar]
Cochran 1989
- Cochran MA, Miller CH, Sheldrake MA. The efficacy of the rubber dam as a barrier to the spread of microorganisms during dental treatment. Journal of the American Dental Association 1989;119(1):141-4. [DOI] [PubMed] [Google Scholar]
Cohen 1987
- Cohen S, Schwartz S. Endodontic complications and the law. Journal of Endodontics 1987;13(4):191-7. [DOI] [PubMed] [Google Scholar]
Dalpian 2018
- Dalpian DM, Gallina CS, Nicoloso GF, Correa MB, Garcia-Godoy F, Araujo FB, et al. Patient- and treatment-related factors may influence the longevity of primary teeth restorations in high caries-risk children: a university-based retrospective study. American Journal of Dentistry 2018;31(5):261-6. [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140-9. [DOI] [PubMed] [Google Scholar]
Elderton 1971a
- Elderton RJ. A modern approach to use of rubber dam. 1. Dental Practitioner and Dental Record 1971;21(6):187-93. [PubMed] [Google Scholar]
Elderton 1971b
- Elderton RJ. A modern approach to use of rubber dam. 2. Dental Practitioner and Dental Record 1971;21(7):226-32. [PubMed] [Google Scholar]
Elderton 1971c
- Elderton RJ. A modern approach to use of rubber dam. 3. Dental Practitioner and Dental Record 1971;21(8):267-73. [PubMed] [Google Scholar]
GRADE 2004
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(1490):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 15 December 2020. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7650):924-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Halbach 2008
- Halbach S, Vogt S, Köhler W, Felgenhauer N, Welzl G, Kremers L, et al. Blood and urine mercury levels in adult amalgam patients of a randomized controlled trial: interaction of Hg species in erythrocytes. Environmental Research 2008;107(1):69-78. [DOI] [PubMed] [Google Scholar]
Harrel 2004
- Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. Journal of the American Dental Association 2004;135(4):429-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hickel 2007
- Hickel R, Roulet JF, Bayne S, Heintze SD, Mjör IA, Peters M, et al. Recommendations for conducting controlled clinical studies of dental restorative materials. Clinical Oral Investigations 2007;11(1):5-33. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2021
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
Hill 2008
- Hill EE, Rubel BS. Do dental educators need to improve their approach to teaching rubber dam use? Journal of Dental Education 2008;72(10):1177-81. [PubMed] [Google Scholar]
Koshy 2002
- Koshy S, Chandler NP. Use of rubber dam and its association with other endodontic procedures in New Zealand. New Zealand Dental Journal 2002;98(431):12-6. [PubMed] [Google Scholar]
Kremers 1999
- Kremers L, Halbach S, Willruth H, Mehl A, Welzl G, Wack FX, et al. Effect of rubber dam on mercury exposure during amalgam removal. European Journal of Oral Sciences 1999;107(3):202-7. [DOI] [PubMed] [Google Scholar]
Kumbargere 2020
- Kumbargere Nagraj S, Eachempati P, Paisi M, Nasser M, Sivaramakrishnan G, Verbeek JH. Interventions to reduce contaminated aerosols produced during dental procedures for preventing infectious diseases. Cochrane Database of Systematic Reviews 2020, Issue 10. Art. No: CD013686. [DOI: 10.1002/14651858.CD013686.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lynch 2003
- Lynch CD, McConnell RJ. The use of microabrasion to remove discolored enamel: a clinical report. Journal of Prosthetic Dentistry 2003;90:417-9. [DOI] [PubMed] [Google Scholar]
Lynch 2007
- Lynch CD, McConnell RJ. Attitudes and use of rubber dam by Irish general dental practitioners. International Endodontic Journal 2007;40(6):427-32. [DOI] [PubMed] [Google Scholar]
Mamoun 2002
- Mamoun J. A prosthesis for achieving dry-field isolation of molars with short clinical crowns. Journal of the American Dental Association 2002;133(8):1105-7. [DOI] [PubMed] [Google Scholar]
Mendes 2018
- Mendes ACB, Restrepo M, Azevedo ER, Cordeiro RCL, Santos-Pinto L, Zuanon ACC. Effect of rubber dam clamps on demineralized cervical enamel of permanent teeth. Journal of Dentistry for Children (Chicago, Ill) 2018;85(1):3-7. [PubMed] [Google Scholar]
Parmar 1998
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analysis of the published literature for survival endpoints. Statistics in Medicine 1998;17(24):2815-34. [DOI] [PubMed] [Google Scholar]
Perrine 2005
- Perrine GA. A simplified rubber-dam technique for preparing teeth for indirect restorations. Journal of the American Dental Association 2005;136(11):1560-1. [DOI] [PubMed] [Google Scholar]
Reid 1991
- Reid JS, Callis PD, Patterson CJW. Rubber Dam in Clinical Practice. 1st edition. London: Quintessence Publishing, 1991. [Google Scholar]
Reuter 1983
- Reuter JE. The isolation of teeth and the protection of patient during endodontic treatment. International Endodontic Journal 1983;16(4):173-81. [DOI] [PubMed] [Google Scholar]
Schuh 2019
- Schuh PL, Wachtel H, Bolz W, Maischberger C, Schenk A, Kühn M. "Teflon tape technique": synergy between isolation and lucidity. Quintessence International 2019;50(6):488-93. [DOI] [PubMed] [Google Scholar]
Stata 2017 [Computer program]
- Stata. Version 15. College Station, TX, USA: StataCorp, 2017. Available at www.stata.com.
Stewardson 2002
- Stewardson DA, McHugh ES. Patients' attitudes to rubber dam. International Endodontic Journal 2002;35(10):812-9. [DOI] [PubMed] [Google Scholar]
Susini 2007
- Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. International Endodontic Journal 2007;40(8):585-9. [DOI] [PubMed] [Google Scholar]
Sutton 1996
- Sutton J, Saunders WP. Effect of various irrigant and autoclaving regimes on the fracture resistance of rubber dam clamps. International Endodontic Journal 1996;29(5):335-43. [DOI] [PubMed] [Google Scholar]
Tiwana 2004
- Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: a 10-year institutional review. Journal of the American Dental Association 2004;135(9):1287-91. [DOI] [PubMed] [Google Scholar]
Whitworth 2000
- Whitworth JM, Seccombe GV, Shoker K, Steele JG. Use of rubber dam and irrigant selection in UK general dental practice. International Endodontic Journal 2000;33(5):435-41. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Wang 2012
- Wang Y, Li C, Yuan H, Wong MCM, Shi Z, Zhou X. Rubber dam isolation for restorative treatment in dental patients. Cochrane Database of Systematic Reviews 2012, Issue 5. Art. No: CD009858. [DOI: 10.1002/14651858.CD009858] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2016
- Wang Y, Li C, Yuan H, Wong MCM, Zou J, Shi Z, et al. Rubber dam isolation for restorative treatment in dental patients. Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No: CD009858. [DOI: 10.1002/14651858.CD009858.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


