Abstract
We evaluated COVID-19 stigma and medical mistrust among people living with HIV in South Africa. We conducted telephone interviews with participants in a prospective study of a decentralized antiretroviral therapy program. Scales assessing medical mistrust, conspiracy beliefs, anticipated and internalized stigma, and stereotypes specific to COVID-19 were adapted primarily from the HIV literature, with higher scores indicating more stigma or mistrust. Among 303 participants, the median stigma summary score was 4 [interquartile range (IQR) 0–8; possible range 0–24] and 6 (IQR 2–9) for mistrust (possible range 0–28). A substantial proportion of participants agreed or strongly agreed with at least one item assessing stigma (54%) or mistrust (43%). Higher COVID-19 stigma was associated with female gender and antecedent HIV stigma, and lower stigma with reporting television as a source of information on COVID-19. Further efforts should focus on effects of stigma and mistrust on protective health behaviors and vaccine hesitancy.
Keywords: COVID-19, Medical mistrust, Stigma, HIV, South Africa
Introduction
Over 100 million people worldwide have been infected with Severe Acute Respiratory Syndrome-Coronavirus 2 (SARS-CoV-2) since December 2019, leading to over two million deaths from COVID-19 [1]. South Africa has been significantly affected, with nearly 1.5 million COVID-19 cases by early February 2021 [1]. Non-pharmaceutical interventions, such as social distancing, wearing masks, and travel restrictions, are effective at reducing community spread of COVID-19 [2], and along with wide-spread testing and vaccine development, have formed the cornerstone of COVID-19 pandemic control worldwide. While non-pharmaceutical interventions, testing, and vaccination hold promise to curb the pandemic, these strategies rely in large part on individual uptake and adherence. Understanding the drivers of individual- and community-level adoption of preventive measures is critical to ongoing efforts to control the spread of COVID-19. Stigma and medical mistrust may impact COVID-19 protective health behaviors, particularly among populations already experiencing stigma, such as people living with HIV (PLWH).
Stigma—a social process that leads to devaluation or discrediting based on particular attributes [3, 4]—has been identified as a barrier to protective health behaviors across a range of health conditions [5–10]. Health-related stigma has been well characterized along the continuum of health-seeking behaviors for HIV, with impacts of HIV stigma ranging from avoidance of HIV testing [6] to decreased rates of antiretroviral therapy initiation and virologic suppression [11]. Since early in the COVID-19 pandemic, stigmatizing beliefs and behaviors towards people of Asian descent, health workers, COVID-19 patients, and marginalized populations have been reported, and have even culminated in violent action [12–18]. Stereotypes (beliefs about characteristics of a stigmatized group and its members [19]) and anticipated stigma (the expectation of future discrimination [19]) related to COVID-19 have been found to impact willingness to undergo COVID-19 testing [20]. Stigma is increasingly understood as intersectional [21], influenced by drivers such as misinformation, historical trauma, or systemic racism that can fuel stigma related to multiple health conditions, with the intersection of multiple stigmas in turn leading to social, economic, and health-related outcomes [22]. Understanding COVID-19 stigma among PLWH, a population already experiencing health-related stigma, is thus important for understanding the potential impacts of stigma on health-seeking behavior.
Medical mistrust may also undermine efforts to curb the pandemic by influencing health-protective behaviors and exacerbating existing inequities. Medical mistrust is defined as active distrust in healthcare systems and medical providers with the belief that they are acting against one’s best interest [23–25]. By contrast, trust in the healthcare system is not simply the opposite of mistrust but implies the belief that organizations or providers are acting in one’s best interest [24, 26]. Similar to stigma, both medical mistrust and conspiracy beliefs have been associated with decreased health-seeking behavior and poor health outcomes across a wide range of health conditions [27–33], and studies have demonstrated the mediating role of mistrust in the association between stigma or discrimination and health behaviors [34, 35]. Medical mistrust, and the related concept of conspiracy beliefs—theories about significant events that implicate dominant and usually malicious groups or individuals [36]—are rooted in historical mistreatment by medical institutions, systemic racism, and the perception and experience of discrimination in healthcare [25, 26, 37]. Medical mistrust and conspiracy beliefs can additionally stem from misinformation [25]. In South Africa, medical mistrust and conspiracy theories have been fueled by a long-standing history of racist policies and years of targeted government misinformation regarding the HIV epidemic [38, 39]. Since the beginning of the COVID-19 pandemic, there has been a preponderance of misinformation worldwide, often spread by social media [40–44], contributing to conspiracy theories [45, 46] and creating risk for increased medical mistrust.
Impacts of stigma and medical mistrust on preventive behaviors specific to COVID-19 have been reported, including protective health behaviors (e.g. social distancing, hand washing, wearing a mask) [36, 45] and vaccine hesitancy [47]. For PLWH, stigma and medical mistrust related to COVID-19 may exacerbate pre-existing impacts of HIV stigma and medical mistrust on health protective behaviors. Uncertainty about the risk and severity of COVID-19 and HIV coinfection could additionally fuel mistrust among PLWH. In South Africa, which has the world’s largest population of people living with HIV at 7.5 million people [48], the impacts of COVID-19 stigma and medical mistrust on health behaviors among PLWH could be particularly significant in national efforts to curb the spread of the pandemic. To implement effective public health messaging and interventions to promote health-protective behaviors, levels and characteristics of stigma and medical mistrust related to COVID-19 among PLWH must be better understood. We aimed to evaluate COVID-19 stigma and medical mistrust among people living with HIV enrolled in a decentralized ART distribution program in South Africa.
Methods
Study Population and Data Collection
We contacted a randomly selected subsample of participants enrolled in a prospective observational cohort study evaluating the implementation of the Central Chronic Medicines Dispensing and Distribution (CCMDD) program in Umlazi, KwaZulu-Natal. The CCMDD program, established by the South African National Department of Health (DOH), allows virologically stable PLWH to collect ART and/or medication for non-communicable diseases at pre-designated community-based pick-up points of their choice, including private pharmacies, churches, and schools [49]. People accessing HIV care in 9 DOH primary health clinics offering CCMDD enrollment in the urban township of Umlazi were recruited. Eligibility criteria included HIV positive serostatus, age 18 or older, and meeting clinical criteria for CCMDD participation as defined per program guidelines (not pregnant, on ART for ≥ 1 year, and virologically suppressed). Participants completed a baseline questionnaire at enrollment into the parent study assessing demographics, HIV care history, competing needs, mental health, social support, and HIV stigma.
We randomly selected 900 of the 2097 participants currently enrolled in the parent study, anticipating a 33% response rate for a target of 300 interviews. Selected participants were distributed evenly between those enrolled in the CCMDD program for 0–6 months, 6–12 months, and > 12 months. Between 28 April and 22 May 2020, bilingual research assistants contacted participants at the phone number provided at parent study enrollment and administered a questionnaire in the participants’ preferred language (isiZulu or English) to participants providing verbal consent. The questionnaire assessed participants’ sources of information about COVID-19, their concerns regarding COVID-19 and ART pick-up, changes in daily activities they had made as a result of the pandemic or national lockdown, measures of mental health and social support, medical mistrust related to COVID-19, and stigma related to COVID-19.
Measures
Sociodemographic Characteristics, HIV History, and Concerns Regarding COVID-19
We obtained basic demographic data, including age, gender, education level, employment, marital status, and years on ART from the baseline questionnaire of the parent study. We assessed participants’ sources of information on COVID-19 and primary concerns regarding the pandemic at the time of the telephone interview.
HIV Stigma
At enrollment into the parent study, we assessed HIV stigma using the 6 questions from the Internalized AIDS-related Stigma Scale [50], along with 6 questions from the HIV stigma scale by Berger et al. [51] that highlight disclosure concerns. Response options were 1—Agree and 0—Disagree. The frequency of “agree” responses per participant was calculated out of a possible total of 12. The scale had a Cronbach’s alpha of 0.94.
COVID-19 Stigma
During the telephone interview, we assessed stigma related to COVID-19 infection. We utilized 6 questions adapted from previously published stigma scales for HIV and chronic illness, with responses on a 5-point Likert scale, with scores ranging 0–4. Questions were selected to assess different domains of health-related stigma, including stereotypes (three questions), internalized stigma (two questions), and anticipated stigma (one question). Two of the questions were adapted from an HIV stigma scale designed for low- and middle-income country (LMIC) settings [52]: “a person with coronavirus must have done something wrong and deserves to be punished,” and “a person with coronavirus is cursed.” Two of the questions were adapted from the Internalized AIDS-related Stigma Scale [50]: “if I have coronavirus, it would be difficult to tell other people,” and “if I had coronavirus, I would feel ashamed”; the latter question had also been incorporated into the scale designed for use in LMIC by Genberg et al. [52]. We adapted one question from a chronic illness anticipated stigma scale [53]: “If I had coronavirus, my friends and family will be angry with me.” A final question, “if someone I knew had coronavirus and recovered, I would be afraid to visit them” was designed for this study. Scores on individual items were added to create a COVID-19 stigma summary score. Participants with missing data in individual items were categorized as having a missing stigma summary score. With regard to internal consistency, the scale had a Cronbach’s alpha of 0.67.
Medical Mistrust Related to COVID-19
We developed eight items assessing medical mistrust, trust in the formal healthcare system to address COVID-19, and conspiracy beliefs related to the COVID-19 pandemic. Two questions assessing mistrust of the government as an agent of healthcare and conspiracy beliefs were adapted from a published scale assessing conspiracy theories around HIV [54]: “The government cannot be trusted to tell the truth about coronavirus,” and “Information about coronavirus is being withheld from the public.” The remaining items were developed for the current study. Questions assessed trust in the government to address COVID-19 (“I trust the public health measures that the government is taking to combat coronavirus”), and trust in the media as an agent of public health messaging (i.e., “I trust the information that I am hearing on the radio and TV about coronavirus,” and “I trust the information that I am reading about coronavirus”). Additional questions assessed trust in healthcare providers and in the formal healthcare sector, by comparing trust in non-Western medicine with trust in clinic-based personnel: “I trust that the doctors and nurses in clinics know how to treat coronavirus,” “I trust traditional healers more than clinic workers to treat coronavirus,” and “I trust church leaders more than clinic workers to treat coronavirus.” Response choices were on a 5-point Likert scale, from ‘strongly disagree’ to ‘strongly agree,’ with scores for each answer option ranging 0–4. To maintain measurement of medical mistrust related to the formal healthcare sector, scores were reversed for the four questions that asked about trust in public health measures, trust in public messaging, and trust of doctors and clinic workers. Scores for individual items were added to produce a medical mistrust summary score; missing responses to individual items resulted in a missing summary score.
In terms of internal consistency, the full scale had a Cronbach’s alpha of 0.63. When the item least correlated with the remainder of the scale, “I trust that the doctors and nurses in clinics know how to treat coronavirus” was removed, the Cronbach’s alpha improved to 0.72. This question was subsequently removed from further analyses of medical mistrust.
Statistical Analysis
We used descriptive statistics [median, interquartile range (IQR), frequency] to report the characteristics of the study population at baseline and during the COVID-19 pandemic, concerns regarding the COVID-19 pandemic, and the distributions of scores for individual COVID-19 stigma and medical mistrust items and summary scores. We used univariate and multivariable logistic regression models to assess predictors of high COVID-19 medical mistrust and high COVID-19 stigma.
For the outcome variables, we defined a high COVID-19 medical mistrust score as at or above the median score of 6, and a high stigma score as a score above the median score of 4. For predictors, we defined several combined categories of concerns regarding COVID-19. Using the responses to the question, “What are your concerns about coronavirus?”, we defined ‘economic concerns’ as any one or more of the responses, “unable to work,” “food running out,” and “money running out”; and ‘infection/illness concerns’ as any one or more of the responses, “becoming infected myself” and “family member becoming infected.” We defined ‘other’ concerns as any one or more of the remaining concerns unrelated to economic hardship or infection, which primarily included lack of transport, unavailable PPE or hand sanitizer, being afraid to move around, crime, and lack of information.
All multivariable models included age and gender. Other factors with p < 0.2 in univariate logistic regression models were also included in the specific multivariable model. All reported p-values were two-tailed, and p < 0.05 was considered statistically significant. Analyses were conducted using SAS software (version 9.4, SAS Institute, Cary, NC).
Ethical Considerations
The study protocol was approved by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal and by the Partners Healthcare Institutional Review Board (protocol 2017P001690).
Results
Participant Characteristics and Baseline HIV Stigma
Of the 638 enrollees contacted, 303 (47%) consented to and completed the interview. Sixty-six percent were female, 302 (99.7%) identified their ethnicity as Black, median age was 36 (IQR, 31–45), and 263 (86.8%) had completed at least some secondary school education (Table 1). Median time since initiation of ART was 3.0 years (IQR 1.0–6.0). Only 6 participants (2.0%) reported any competing needs at baseline, the majority (247, 81.8%) rated their ability to take HIV medication as “excellent,” and most (286, 94.4%) reported zero missed doses of ART in the preceding 7 days. At enrollment into the parent study, 54.6% of participants endorsed zero HIV stigma items. At the time of the telephone interview during the COVID-19 lockdown, half of participants (150, 49.5%) had been enrolled in the CCMDD program for fewer than six months, and 292 (96.4%) were continuing to receive their ART through the CCMDD program.
Table 1.
Participant demographics and characteristics at enrollment into the parent study
| Characteristic | Median, [IQR] or n, (%) |
|---|---|
| Gender | |
| Female | 200 (66.0) |
| Male | 103 (34.0) |
| Age, years | 36.0 [31.0–45.0] |
| 18–25 | 22 (7.3) |
| 26–40 | 166 (54.8) |
| > 40 | 115 (38.0) |
| Ethnic group (race) | |
| Black | 302 (99.7) |
| Coloured | 1 (0.3) |
| Years since initiation of ART | 3.0 [1.0–6.0] |
| Education level | |
| No school | 6 (2.0) |
| Primary | 34 (11.2) |
| Some high school | 123 (40.6) |
| Matric | 120 (39.6) |
| Tertiary | 20 (6.6) |
| Employed | |
| No | 164 (54.1) |
| Yes | 139 (45.9) |
| Marital status | |
| Never married | 237 (78.2) |
| Currently married | 58 (19.1) |
| Divorced/separated | 5 (1.7) |
| Widowed | 3 (1.0) |
| Ability to take HIV medication (n = 302) | |
| Very poor, poor, or fair | 0 |
| Good | 6 (2.0) |
| Very good | 49 (16.2) |
| Excellent | 247 (81.8) |
| Doses of ART missed in the preceding 7 days | |
| 0 doses missed | 286 (94.4) |
| 1–3 doses missed | 17 (5.6) |
| > 3 doses missed | 0 |
| Baseline competing needsa | |
| None | 297 (98.0) |
| Any | 6 (2.0) |
| Number of HIV stigma items endorsed at baseline, range 0–12 (n = 293) | |
| 0 | 160 (54.6) |
| 1–6 | 65 (22.2) |
| > 6 | 68 (23.2) |
| Time enrolled in CCMDD prior to COVID-19 interview, months | 7 [5–12] |
| 0–6 months | 150 (49.5) |
| 6–12 months | 81 (26.7) |
| > 12 months | 72 (23.8) |
n = 303 unless noted otherwise
aWhether the participant had gone without healthcare because they needed the money for basic needs, such as food, clothing, or housing, or if they had gone without basic needs because they needed the money for healthcare, in the preceding 6 months before enrollment in CCMDD
Sources of Information and Concerns about the Pandemic
Television and radio were the most common sources of information on COVID-19, reported by 249 (82.2%) and 219 (72.3%) participants, respectively, followed by social media (60, 19.8%) and friends/family (46, 15.2%) (Table 2). Participants’ most frequent concerns regarding the COVID-19 pandemic and national lockdown were food running out (121, 39.9%), becoming infected with COVID-19 (103, 34.0%), being unable to work/losing employment or income (102, 33.7%), and money running out (87, 28.7%) (Table 2). Only 4 (1.3%) participants spontaneously reported stigma as a concern during the pandemic when unprompted.
Table 2.
Sources of information on COVID-19 and concerns about the COVID-19 pandemic
| Sources of information on COVID-19 | n (%) |
|---|---|
| TV | 249 (82.2) |
| Radio | 219 (72.3) |
| Social Media | 60 (19.8) |
| Friends/family | 46 (15.2) |
| Newspapers/news websites | 38 (12.5) |
| Clinics (materials, staff) | 32 (10.6) |
| DOH/Government website | 30 (9.9) |
| At work | 15 (5.0) |
| Other websites | 8 (2.6) |
| Other | 19 (6.3) |
| Concerns about the COVID-19 pandemic | |
|---|---|
| Food running out | 121 (39.9) |
| Becoming infected myself | 103 (34.0) |
| Unable to work | 102 (33.7) |
| Money running out | 87 (28.7) |
| Family member becoming infected | 54 (17.8) |
| Lack of transport to work, clinic, or elsewhere | 39 (12.9) |
| Afraid to move | 33 (10.9) |
| Unavailable sanitizer/PPE | 24 (7.9) |
| Lack of transport to CCMDD pick-up point | 9 (3.0) |
| Crime | 8 (2.6) |
| Lack of information | 5 (1.7) |
| Stigma | 4 (1.3) |
| Other | 80 (26.4) |
COVID-19 Stigma
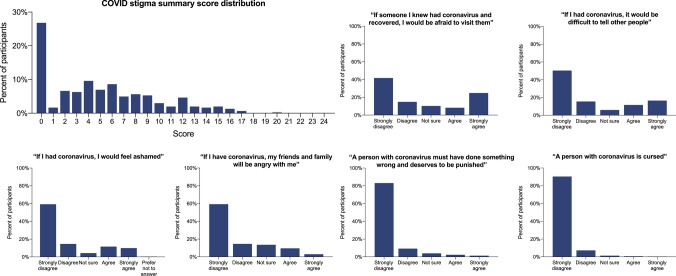
Of 301 participants with data available for all stigma items, over one quarter (81, 26.9%) of participants strongly disagreed with all items assessing stigma and thus had the lowest possible COVID-19 stigma summary score of 0. With a possible score range of 0–24, the median summary score was 4 with IQR 0–8, indicating overall low levels of stigma. The distribution of summary stigma scores and of answers for each individual stigma item are shown in Fig. 1. Of 302 participants with data available for any stigma items, a majority (164, 54.3%) agreed or strongly agreed with at least one item assessing stigma. The most frequently endorsed COVID-19 stigma item, at 33%, was, “If someone I knew had coronavirus and recovered, I would be afraid to visit them,” with the least frequently endorsed questions being, “A person with coronavirus must have done something wrong and deserves to be punished,” and “A person with coronavirus is cursed,” (4% and 1%, respectively). In multivariable analyses, female gender (aOR 1.88, 95% CI 1.10–3.20), having ‘other’ concerns about the COVID-19 pandemic (aOR 2.04, 95% CI 1.14–3.66), and endorsing greater than 6 HIV stigma items at baseline (aOR 2.09, 95% CI 1.11–3.93) were associated with having a COVID-19 stigma score above the median, while identifying television as a source of information on COVID-19 made one less likely to have a stigma score above the median (aOR 0.46, 95% CI 0.24–0.90) (Table 3).
Fig. 1.
COVID-19 stigma summary scores and distributions of responses for individual stigma items
Table 3.
Correlates of high COVID-19 stigma, n = 291
| OR, univariate analyses | p-value | aOR, multivariable analysis | p-value | |
|---|---|---|---|---|
| Gender (Ref = M) | ||||
| F | 1.97 (1.21–3.20) | 0.006 | 1.88 (1.10–3.20) | 0.02 |
| Age (Ref = > 40) | ||||
| 18–25 | 3.62 (1.31–10.00) | 0.01 | 2.02 (0.67–6.08) | 0.21 |
| 26–40 | 1.54 (0.95–2.49) | 0.08 | 1.21 (0.71–2.05) | 0.49 |
| Education level (Ref = no school) | ||||
| Primary | 0.70 (0.12–3.99 | 0.69 | ||
| Some high school | 0.81 (0.16–4.17) | 0.80 | ||
| Matric | 1.14 (0.22–5.89) | 0.87 | ||
| Tertiary | 1.57 (0.25–10.09) | 0.63 | ||
| Sources of information on COVID-19 | ||||
| Newspaper/news websites | 0.65 (0.32–1.30) | 0.22 | ||
| Radio | 0.63 (0.38–1.05) | 0.07 | 0.66 (0.37–1.15) | 0.14 |
| Television | 0.50 (0.27–0.91) | 0.02 | 0.46 (0.24–0.90) | 0.02 |
| DOH/government website | 0.78 (0.37–1.67) | 0.53 | ||
| Social media | 0.89 (0.50–1.59) | 0.70 | ||
| Friends/family | 0.63 (0.33–1.19) | 0.15 | 0.58 (0.28–1.19) | 0.14 |
| Clinics | 0.69 (0.33–1.45) | 0.33 | ||
| Other | 1.77 (0.90–3.47) | 0.10 | 1.59 (0.76–3.33) | 0.22 |
| Any economic concerns about COVID-19 | 0.88 (0.55–1.38) | 0.57 | ||
| Infection as a concern about COVID-19 | 0.80 (0.50–1.26) | 0.33 | ||
| Any other concerns about COVID-19 | 2.71 (1.58–4.66) | < 0.001 | 2.04 (1.14–3.66) | 0.02 |
| Number of HIV stigma items endorsed at baseline (Ref = 0) | ||||
| 1–6 | 1.44 (0.81–2.57) | 0.22 | 1.31 (0.70–2.43) | 0.40 |
| > 6 | 2.56 (1.42–4.61) | 0.002 | 2.09 (1.11–3.93) | 0.02 |
COVID-19 Medical Mistrust
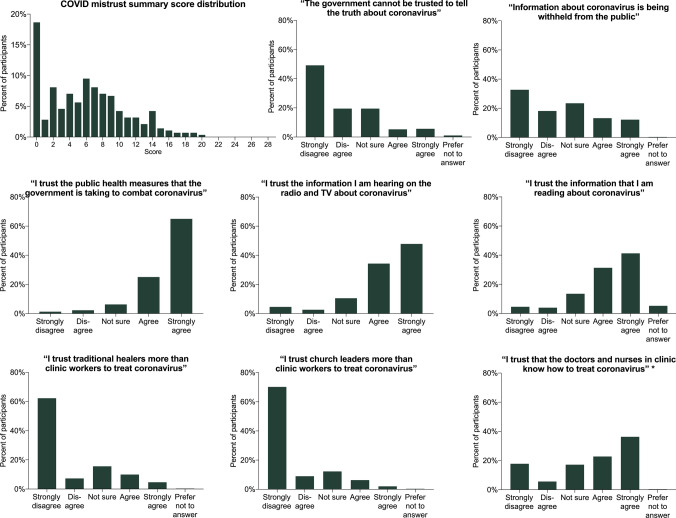
Among 283 participants with data available for all mistrust items, the median summary score for medical mistrust related to COVID-19 was 6 (interquartile range, 2–9) on a scale from 0–28. The distribution of summary medical mistrust scores and for each answer item are shown in Fig. 2. Fifty-three participants (18.7%) had the lowest score of 0, indicating that they strongly disagreed with all mistrust items and conspiracy beliefs, and strongly agreed with all ‘trust’ items. Only 26 participants (9.2%) had a summary score above 13, and nobody had a score above 20. However, 130 participants (42.9%) among those with data on any mistrust items available agreed or strongly agreed with at least one mistrust item. In multivariable analyses, identifying illness-related concerns regarding the COVID-19 pandemic was associated with lower medical mistrust (aOR 0.53, 95% CI 0.31–0.92). Medical mistrust was otherwise not associated with gender, age, education level, sources of information on COVID-19, or other categories of concerns about the COVID-19 pandemic (data not shown).
Fig. 2.
COVID-19 medical mistrust summary scores and distributions for individual mistrust items. The question, “I trust that the doctors and nurses in clinic know how to treat coronavirus” was not included in the summary score
Discussion
This study demonstrates that early in the COVID-19 pandemic in South Africa, a significant proportion of people living with HIV enrolled in a decentralized ART delivery program endorsed aspects of COVID-19 stigma and medical mistrust. Specifically, over half of participants agreed or strongly agreed with at least one item assessing anticipated stigma, internalized stigma, or stereotypes specific to COVID-19, and over two-fifths of participants agreed or strongly agreed with at least one item assessing mistrust in the government regarding COVID-19, conspiracy beliefs, or lack of trust in public messaging or healthcare providers. However, overall levels of stigma and medical mistrust were low when summed over all measures. While this is the first study, to our knowledge, to evaluate levels of COVID-19 stigma and medical mistrust among PLWH in South Africa, we found levels of stigma similar to findings from a general United States population [20], while levels of mistrust were somewhat lower than in a study of Black Americans living with HIV [47] and among the general population in the United Kingdom [55]. In light of the known negative associations of both stigma and mistrust with health-protective behaviors and health outcomes [5–11, 27–33], understanding the features of COVID-19 stigma and medical mistrust among PLWH can help elucidate potential impacts of these forces on health-seeking behaviors and guide intervention efforts.
Our findings shed additional light on the prevalence of medical mistrust and conspiracy beliefs related to COVID-19 among PLWH in South Africa. Participants who identified acquiring COVID-19 infection as a major concern during the pandemic demonstrated lower levels of medical mistrust. This association may indicate that individuals with more trust in the healthcare system had a heightened awareness of their risk for acquiring infection, or alternately that those more concerned about infection were more likely to trust public health systems and messaging in order to understand how to avoid exposure to COVID-19. Interestingly, we did not find an association between social media as a source of information on COVID-19 and medical mistrust, counter to previous studies in other settings [36, 45]; however, less than twenty percent of our cohort identified social media as a source of information on COVID-19, highlighting potential differences in dissemination of information regarding the pandemic in South Africa compared to higher-income countries.
We additionally identified characteristics associated with higher COVID-19 stigma, including female gender and higher levels of HIV stigma prior to the COVID-19 pandemic, and found a negative association between television as a source of information on COVID-19 and stigma. An association between gender and health-related stigma has been noted previously, demonstrating more perceived HIV stigma among women than men [56] and differential influences of HIV stigma on care-seeking behavior for men and women [57, 58]. The association of higher HIV stigma at baseline with higher COVID-19 stigma supports the notion that health-related stigma is not an isolated phenomenon specific to a single condition, but rather reflects the intersectionality of multiple health-related stigmas [19, 22] and suggests that structural determinants, such as poverty and systemic racism, may be contributing to multiple health-related stigmas for the same individual or group of people. Interestingly, participants who reported television as a source of information about COVID-19 were less likely to have high COVID-19 stigma; no other source of information was associated with higher or lower stigma or with medical mistrust. The use of television over social media for information in South Africa, with the latter linked frequently to COVID-19 misinformation [40–44] which can in turn fuel stigma, may provide access to more unbiased, comprehensive information on the virus that may counteract stigma.
Overall, endorsement of COVID-19 medical mistrust and conspiracy beliefs was somewhat lower than in recent studies among PLWH and people without HIV in the U.S. and U.K. [47, 55]. Our cohort included only participants who had achieved HIV virologic suppression and clinical stability on ART for at least one year. The baseline characteristics of this cohort (e.g., low rates of competing needs, near-universal self-report of very good or excellent ART adherence) demonstrate that this population is already actively, and successfully, engaging with the healthcare system, and thus potentially less likely to endorse medical mistrust even with regard to a new health condition such as COVID-19. However, a significant proportion of participants, over forty percent, did agree with at least one mistrust item, and one in four participants agreed or strongly agreed that information about coronavirus was being withheld from the public, which was also common among Black Americans living with HIV [47], suggesting the potential impacts of shared histories of intentional disinformation and systemic racism on medical mistrust. Similarly, while a significant proportion of participants disagreed with all items on the stigma scale and thus had the lowest possible summary score for COVID-19 stigma, there was a broad distribution of responses. Notably, over one quarter of participants agreed or strongly agreed that it would be difficult to tell other people if they were infected with COVID-19, and over one out of five people agreed or strongly agreed that they would feel ashamed if they had COVID-19. Both of these items assess internalized stigma, which has been associated with decreased care-seeking for HIV [11] and with negative impacts on mental health in the setting of HIV [50, 59].
Stigma and mistrust have been associated with decreased care-seeking behaviors for other health conditions [5, 8–10, 27–30], for COVID-19 [45, 55, 60], and with COVID-19 vaccine hesitancy [47]. Furthermore, COVID-19 stigma and medical mistrust could negatively impact care-seeking behavior for HIV, if mistrust in the protection against COVID-19 afforded by physical distancing and use of PPE in clinics, mistrust of transmission dynamics of the virus, or stigma associated with healthcare workers or others perceived to be at high risk of COVID-19 infection lead to avoidance of healthcare settings. As many nations worldwide, including South Africa, experience multiple surges of infections and the emergence of SARS-CoV-2 variants, ongoing adherence to mitigation measures to prevent recurrent surges, as well as encouragement of the uptake of effective vaccines, are increasingly important. Interventions to address stigma and medical mistrust related to COVID-19 among vulnerable populations such as PLWH are necessary and will require targeted efforts. Messages disseminated by healthcare providers, opinion leaders, and on television may be particularly effective, as television, a commonly reported source of information on COVID-19, was associated with lower COVID-19 stigma. Acknowledging and addressing structural racism and its impacts on health in this population are critical, including greater investment in healthcare delivery in historically underserved areas, which are often those most affected by HIV and COVID-19, prioritizing underrepresented racial and ethnic groups in healthcare leadership, and ensuring all population groups are represented equally in public health messaging. Additionally, recognizing the intersectionality of health-related stigmas and the differential stigma experienced by women and addressing the history of systematic misinformation on HIV will be important to increasing the trustworthiness of the public health system regarding COVID-19.
Limitations
This study is one of the first systematic evaluations of medical mistrust and stigma related to COVID-19 in a low- or middle-income country setting, thus there are no existing validated scales or measures in these populations. Our questions, adapted from existing stigma and mistrust scales for HIV and chronic disease or designed specifically for this study, may not comprehensively assess all dimensions of these constructs. Scales to be used more widely to assess COVID-19 mistrust and stigma will require more thorough psychometric evaluations; however, we did not have the capacity to conduct a full assessment in this study. The satisfactory internal consistency of these scales and the consistency of identified associations with other studies suggest, however, that we have measured at least certain dimensions of COVID-19 stigma and mistrust accurately. While many parallels can be drawn between the COVID-19 and HIV epidemics, COVID-19 also differs from HIV in important ways, including a lack of association with sexual risk behavior, possibility of cure, and the rapid accrual and dissemination of information about COVID-19. Our results may not be generalizable to other populations of people living with HIV who are not virally suppressed or clinically stable, those not enrolled in a decentralized ART distribution program, or people without HIV in South Africa. Furthermore, our results have to be interpreted within the circumstances of the early stages of the pandemic and national lockdown in South Africa, as the interviews were conducted over a one-month period spanning only the first two of five stages of the national lockdown. Subsequently, COVID-19 cases in South Africa increased exponentially, global knowledge about transmission dynamics and potential treatments for the infection increased significantly, and due to economic concerns, the South African government has transitioned the nation to lower levels of restrictions. Thus, it is anticipated that levels of stigma and mistrust will also respond in dynamic ways to the changing nature of the pandemic.
Conclusions
Among people living with HIV enrolled in a decentralized ART delivery program in South Africa, a substantial proportion endorsed at least one aspect of COVID-19 stigma or medical mistrust early in the COVID-19 pandemic. Female gender and higher baseline HIV stigma were associated with higher COVID-19 stigma, while obtaining COVID-19 information from television was associated with lower COVID-19 stigma, highlighting the intersectionality of multiple health-related stigmas and suggesting the potential for mass media to disseminate destigmatizing information about COVID-19. Stigma and medical mistrust could impede efforts to effectively control the COVID-19 pandemic at the population level and targeted interventions are needed.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by JJ, JY, SG, NN, ZMS, ARK, BAB, NJW, DZ, RAP, LMB, IVB. The first draft of the manuscript was written by JJ and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was funded by the National Institutes of Health: T32AI007433 (JJ), P30AI060354 (LMB), R01 MH114997 (IVB), K24 AI141036 (IVB), and the Weissman Family MGH Research Scholar Award (IVB). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or the Massachusetts General Hospital Executive Committee on Research.
Data Availability
Data are not posted online due to potentially identifiable information but are available from the principal investigator upon request.
Declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical Approval
The study protocol was approved by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal and by the Partners Healthcare Institutional Review Board (protocol 2017P001690).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. [cited 2020 Dec 15]. Available from: https://covid19.who.int
- 2.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goffman E. Stigma: notes on the management of spoiled identify. Englewood Cliffs: Prentice-Hall, Inc; 1963. [Google Scholar]
- 4.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalichman S, Simbayi L. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town. South Africa Sex Transm Infect. 2003;79(6):442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Skinner D, et al. AIDS-related stigma, HIV testing, and transmission risk among patrons of informal drinking places in Cape Town, South Africa. Ann Behav Med Publ Soc Behav Med. 2012;43(3):362–371. doi: 10.1007/s12160-012-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Golub SA, Gamarel KE. The impact of anticipated hiv stigma on delays in HIV testing behaviors: findings from a community-based sample of men who have sex with men and transgender women in New York City. AIDS Patient Care STDs. 2013;27(11):621–627. doi: 10.1089/apc.2013.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. 2014;15(2):37–70. doi: 10.1177/1529100614531398. [DOI] [PubMed] [Google Scholar]
- 9.Scott N, Crane M, Lafontaine M, Seale H, Currow D. Stigma as a barrier to diagnosis of lung cancer: patient and general practitioner perspectives. Prim Health Care Res Dev. 2015;16(06):618–622. doi: 10.1017/S1463423615000043. [DOI] [PubMed] [Google Scholar]
- 10.DiIorio C, Osborne Shafer P, Letz R, Henry T, Schomer DL, Yeager K. The association of stigma with self-management and perceptions of health care among adults with epilepsy. Epilepsy Behav. 2003;4(3):259–267. doi: 10.1016/s1525-5050(03)00103-3. [DOI] [PubMed] [Google Scholar]
- 11.Earnshaw VA, Bogart LM, Laurenceau J, Chan BT, Maughan‐Brown BG, Dietrich JJ, et al. Internalized HIV stigma, ART initiation and HIV‐1 RNA suppression in South Africa: exploring avoidant coping as a longitudinal mediator. J Int AIDS Soc [Internet]. 2018 Oct 26 [cited 2021 Feb 5];21(10). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6202800/ [DOI] [PMC free article] [PubMed]
- 12.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report -35 [Internet]. 2020 Feb [cited 2020 Sep 10]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200224-sitrep-35-covid-19.pdf?sfvrsn=1ac4218d_2
- 13.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. 2020;20(7):782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Somse P, Eba PM. Lessons from HIV to guide COVID-19 responses in the Central African Republic. Health Hum Rights. 2020;22(1):371–374. [PMC free article] [PubMed] [Google Scholar]
- 15.Sotgiu G, Dobler CC. Social stigma in the time of coronavirus disease 2019. Eur Respir J. 2020;56(2):2002461. doi: 10.1183/13993003.02461-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mukumbang FC, Ambe AN, Adebiyi BO. Unspoken inequality: how COVID-19 has exacerbated existing vulnerabilities of asylum-seekers, refugees, and undocumented migrants in South Africa. Int J Equity Health. 2020;19(1):141. doi: 10.1186/s12939-020-01259-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Social Stigma associated with COVID-19: A guide to preventing and addressing social stigma [Internet]. 2020 Feb [cited 2020 Sep 8]. Available from: https://www.who.int/docs/default-source/coronaviruse/covid19-stigma-guide.pdf?sfvrsn=226180f4_2
- 18.Lubega M, Ekol JE. Preparing communities to receive persons recently suspected or diagnosed with COVID-19. Pan Afr Med J. 2020;35(Supp 2):21. doi: 10.11604/pamj.supp.2020.35.2.23202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stangl AL, Earnshaw VA, Logie CH, van Brakel WC, Simbayi L, Barré I, et al. The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31. doi: 10.1186/s12916-019-1271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Earnshaw VA, Brousseau NM, Hill EC, Kalichman SC, Eaton LA, Fox AB. Anticipated stigma, stereotypes, and COVID-19 testing. Stigma Health. 2020;5(4):390–3. [Google Scholar]
- 21.Logie CH. Lessons learned from HIV can inform our approach to COVID-19 stigma. J Int AIDS Soc. 2020;3(5):e25504. doi: 10.1002/jia2.25504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–21. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benkert R, Cuevas A, Thompson HS, Dove-Meadows E, Knuckles D. Ubiquitous yet unclear: a systematic review of medical mistrust. Behav Med Wash DC. 2019;45(2):86–101. doi: 10.1080/08964289.2019.1588220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Williamson LD, Bigman CA. A systematic review of medical mistrust measures. Patient Educ Couns. 2018;101(10):1786–94. doi: 10.1016/j.pec.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav Med Wash DC. 2019;45(2):79–85. doi: 10.1080/08964289.2019.1619511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pellowski JA, Price DM, Allen AM, Eaton LA, Kalichman SC. The differences between medical trust and mistrust and their respective influences on medication beliefs and ART adherence among African-Americans living with HIV. Psychol Health. 2017;32(9):1127–39. doi: 10.1080/08870446.2017.1324969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Earnshaw VA, Bogart LM, Klompas M, Katz IT. Medical mistrust in the context of Ebola: Implications for intended care-seeking and quarantine policy support in the United States. J Health Psychol. 2019;24(2):219–28. doi: 10.1177/1359105316650507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bickell NA, Weidmann J, Fei K, Lin JJ, Leventhal H. Underuse of breast cancer adjuvant treatment: patient knowledge, beliefs, and medical mistrust. J Clin Oncol. 2009;27(31):5160–7. doi: 10.1200/JCO.2009.22.9773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheppard VB, Mays D, LaVeist T, Tercyak KP. Medical mistrust and self-efficacy influence black women’s level of engagement in BRCA1/2 genetic counseling and testing. J Natl Med Assoc. 2013;105(1):17–22. doi: 10.1016/s0027-9684(15)30081-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical mistrust, and preventive health services delays among community-dwelling African-American men. J Gen Intern Med. 2010;25(12):1300–8. doi: 10.1007/s11606-010-1481-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dale SK, Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Medical mistrust is related to lower longitudinal medication adherence among African-American males with HIV. J Health Psychol. 2016;21(7):1311–21. doi: 10.1177/1359105314551950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44(6):2093–105. doi: 10.1111/j.1475-6773.2009.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bogart LM, Kalichman SC, Simbayi LC. Endorsement of a genocidal HIV conspiracy as a barrier to HIV testing in South Africa. J Acquir Immune Defic Syndr. 2008;49(1):115–6. doi: 10.1097/QAI.0b013e318181b889. [DOI] [PubMed] [Google Scholar]
- 34.Eaton LA, Driffin DD, Kegler C, Smith H, Conway-Washington C, White D, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health. 2015;105(2):e75–82. doi: 10.2105/AJPH.2014.302322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galvan FH, Bogart LM, Klein DJ, Wagner GJ, Chen Y-T. Medical mistrust as a key mediator in the association between perceived discrimination and adherence to antiretroviral therapy among HIV-positive Latino men. J Behav Med. 2017;40(5):784–93. doi: 10.1007/s10865-017-9843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Earnshaw VA, Eaton LA, Kalichman SC, Brousseau NM, Hill EC, Fox AB. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl Behav Med [Internet]. 2020 Sep 10 [cited 2021 Feb 5]; Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7499784/ [DOI] [PMC free article] [PubMed]
- 37.Jaiswal J, Singer SN, Siegel K, Lekas H-M. HIV-related ‘conspiracy beliefs’: lived experiences of racism and socio-economic exclusion among people living with HIV in New York City. Cult Health Sex. 2019;21(4):373–86. doi: 10.1080/13691058.2018.1470674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tun W, Kellerman S, Maimane S, Fipaza Z, Sheehy M, Vu L, et al. HIV-related conspiracy beliefs and its relationships with HIV testing and unprotected sex among men who have sex with men in Tshwane (Pretoria) South Africa AIDS Care. 2012;24(4):459–67. doi: 10.1080/09540121.2011.617412. [DOI] [PubMed] [Google Scholar]
- 39.Nattrass N. Understanding the origins and prevalence of AIDS conspiracy beliefs in the United States and South Africa. Sociol Health Illn. 2013;35(1):113–29. doi: 10.1111/j.1467-9566.2012.01480.x. [DOI] [PubMed] [Google Scholar]
- 40.Quinn EK, Fazel SS, Peters CE. The Instagram infodemic: cobranding of conspiracy theories, coronavirus disease 2019 and authority-questioning beliefs. Cyberpsychol Behav Soc Netw. 2020 doi: 10.1089/cyber.2020.0663. [DOI] [PubMed] [Google Scholar]
- 41.Love JS, Blumenberg A, Horowitz Z. The parallel pandemic: medical misinformation and COVID-19. J Gen Intern Med. 2020;14:1–2. doi: 10.1007/s11606-020-05897-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bowles J, Larreguy H, Liu S. Countering misinformation via WhatsApp: preliminary evidence from the COVID-19 pandemic in Zimbabwe. PLoS ONE. 2020;15(10):e0240005. doi: 10.1371/journal.pone.0240005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahinkorah BO, Ameyaw EK, Hagan JEJ, Seidu A-A, Schack T. Rising Above Misinformation or Fake News in Africa: Another Strategy to Control COVID-19 Spread. Front Commun [Internet]. 2020 [cited 2020 Sep 11]; 5(45). Available from: https://www.frontiersin.org/articles/10.3389/fcomm.2020.00045/full
- 44.Islam MS, Sarkar T, Khan SH, Mostofa Kamal A-H, Hasan SMM, Kabir A, et al. COVID-19–related infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hyg. 2020;103(4):1621–9. doi: 10.4269/ajtmh.20-0812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Allington D, Duffy B, Wessely S, Dhavan N, Rubin J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol Med. 2020 doi: 10.1017/S003329172000224X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schaeffer K. Nearly three-in-ten Americans believe COVID-19 was made in a lab [Internet]. Pew Research Center. [cited 2020 Sep 10]. Available from: https://www.pewresearch.org/fact-tank/2020/04/08/nearly-three-in-ten-americans-believe-covid-19-was-made-in-a-lab/
- 47.Bogart LM, Ojikutu BO, Tyagi K, Klein DJ, Mutchler MG, Dong L, et al. COVID-19 related medical mistrust, health impacts, and potential vaccine hesitancy among black americans living with HIV. JAIDS J Acquir Immune Defic Syndr. 2021;86(2):200–7. doi: 10.1097/QAI.0000000000002570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.UNAIDS. UNAIDS Data 2019: South Africa [Internet]. Geneva, Switzerland; 2019 [cited 2020 Jul 29]. Available from: https://www.unaids.org/en/regionscountries/countries/southafrica
- 49.Steel G. Alternative Chronic Medicine Access Programme for Public Sector Patients [Internet]. Civil Society Stakeholder Meeting; 2014 Apr 14 [cited 2020 Aug 17]. Available from: https://www.differentiatedcare.org/Portals/0/adam/Content/5zkRswkhdUCwztOtMVmPKg/File/DOH_CCMDD%20civil%20society%20presentation_20140512_TO%20MSF.pdf
- 50.Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-related stigma scale. AIDS Care. 2009;21(1):87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- 51.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–29. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 52.Genberg BL, Kawichai S, Chingono A, Sendah M, Chariyalertsak S, Konda KA, et al. Assessing HIV/AIDS stigma and discrimination in developing countries. AIDS Behav. 2008;12(5):772–80. doi: 10.1007/s10461-007-9340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Earnshaw VA, Quinn DM, Kalichman SC, Park CL. Development and psychometric evaluation of the chronic illness anticipated stigma scale. J Behav Med. 2013;36(3):270–82. doi: 10.1007/s10865-012-9422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bogart LM, Thorburn S. Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? JAIDS J Acquir Immune Defic Syndr. 2005;38(2):213–8. doi: 10.1097/00126334-200502010-00014. [DOI] [PubMed] [Google Scholar]
- 55.Freeman D, Waite F, Rosebrock L, Petit A, Causier C, East A, et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol Med. 2020 doi: 10.1017/S0033291720001890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Maragh-Bass AC, Gamble T, Tolley EE. ‘Either you float or you drown:’ the role of social ties and stigma in lived experiences of the HIV care continuum in HPTN 065. AIDS Behav. 2020;24(9):2532–45. doi: 10.1007/s10461-020-02811-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chimoyi L, Tshuma N, Muloongo K, Setswe G, Sarfo B, Nyasulu PS. HIV-related knowledge, perceptions, attitudes, and utilisation of HIV counselling and testing: a venue-based intercept commuter population survey in the inner city of Johannesburg, South Africa. Glob Health Action. 2015;28(8):26950. doi: 10.3402/gha.v8.26950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kalichman SC, Shkembi B, Wanyenze RK, Naigino R, Bateganya MH, Menzies NA, et al. Perceived HIV stigma and HIV testing among men and women in rural Uganda: a population-based study. Lancet HIV [Internet]. 2020 Sep [cited 2020 Sep 15]; Available from: https://linkinghub.elsevier.com/retrieve/pii/S2352301820301983 [DOI] [PMC free article] [PubMed]
- 59.Simbayi LC, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town. South Africa Soc Sci Med. 2007;64(9):1823–31. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Plohl N, Musil B. Modeling compliance with COVID-19 prevention guidelines: the critical role of trust in science. Psychol Health Med. 2020;1:1–12. doi: 10.1080/13548506.2020.1772988. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are not posted online due to potentially identifiable information but are available from the principal investigator upon request.