Abstract
Introduction
Inadequate water and sanitation is a central challenge in global health. Since 2008, the Democratic Republic of Congo government has implemented a national programme, Healthy Villages and Schools (Villages et Ecoles Assainis (VEA), with support from UNICEF, financed by UK’s Foreign, Commonwealth and Development Office.
Methods
A cluster-level randomised controlled trial of VEA was implemented throughout 2019 across 332 rural villages, grouped into 50 treatment and 71 control clusters. Primary outcomes included time spent collecting water; quantity of water collected; prevalence of improved primary source of drinking water; and prevalence of improved primary defecation site. Secondary outcomes included child health, water governance, water satisfaction, handwashing practices, sanitation practices, financial cost of water, school attendance and water storage practices. All outcomes were self-reported. The primary analysis was on an intention-to-treat basis, using linear models. Outcomes were measured October–December 2019, median 5 months post-intervention.
Results
The programme increased access to improved water sources by 33 percentage points (pp) (95% CI 22 to 45), to improved sanitation facilities by 26 pp (95% CI 14 to 37), and improved water governance by 1.3 SDs (95% CI 1.1 to 1.5), water satisfaction by 0.6 SD (95% CI 0.4 to 0.9), handwashing practices by 0.5 SD (95% CI 0.3 to 0.7) and sanitation practices by 0.3 SD (95% CI 0.1 to 0.4). There was no significant difference in financial cost of water, school attendance, child health or water storage practices.
Conclusion
VEA produced large increases in access to and satisfaction with water and sanitation services, in self-reported hygiene and sanitation behaviour, and in measures of water governance.
Trial registration number
AEARCTR-0004648; American Economic Association RCT registry.
Keywords: randomised control trial, public health, health systems, health policy, environmental health
Key messages.
What is already known?
Inadequate water, sanitation and hygiene (WASH) contribute to over 800 000 deaths each year, the overwhelming majority of which are in low-income and middle-income countries.
Existing trials of WASH interventions either focus on one component at the group level (eg, community-led total sanitation) or multiple components at the household level (eg, recent WASH Benefits and Shine trials). Little evidence exists about the effectiveness of multicomponent group-level interventions, particularly in conflict settings.
What are the new findings?
A national community-led programme with WASH and governance components increased access to improved water sources and sanitation facilities, strengthened water governance, increased good handwashing and sanitation practices, and increased satisfaction with water access.
There were significant differences in the effects across four provinces, and by community remoteness, suggesting that programme impacts depend on initial conditions.
What do the new findings imply?
Multicomponent, community-led WASH programmes have the potential to address inadequate WASH in low-income, conflict-affected settings.
Additional research and intervention development are needed to further increase the effectiveness and efficiency of these programmes and to determine how their effects are modified by initial conditions in targeted communities.
Introduction
Water, sanitation and hygiene (WASH) services are critical to health but are inadequately provided in many developing countries. Globally, 2.3 billion people lack access to basic sanitation and 892 million practice open defecation.1 Prüss‐Ustün et al 2 estimate that there are over 500 000 deaths each year due to diarrhoea that results from inadequate drinking water, nearly 300 000 deaths due to inadequate sanitation, and another 300 000 deaths due to inadequate hand hygiene.2 Inadequate sanitation is hypothesised to be a key driver of the global stunting crisis,3 4 which has long-term negative impacts on health, education, cognition and human capital.5 6 Inadequate sanitation is also a leading risk factor for neglected tropical diseases, including soil-transmitted helminth infection. Rural residents spend large amounts of time collecting water, a burden that falls disproportionately on women and children,7 and illness linked to inadequate water and sanitation may contribute to school absenteeism for children.
The challenge of inadequate WASH services is pronounced in fragile and conflict-affected states,1 where instability and violence may hamper public and private efforts to build sustainable WASH systems. The World Bank projects that up to 2/3 of people living in extreme poverty in 2030 will live in fragile and conflict-affected settings.8 Sustainable development goal (SDG) 6 includes several WASH targets, such as ‘achieve universal and equitable access to safe and affordable drinking water for all’ by 2030 and ‘support and strengthen the participation of local communities in improving water and sanitation management’. Maximising the impact of WASH programmes, especially in fragile and conflict-affected settings, will be critical towards achieving this SDG as well as the other health-related and education-related SDGs.
We conducted a cluster-randomised trial of a national rural WASH programme in the Democratic Republic of Congo (DRC), where armed state and nonstate actors have been in conflict for over 20 years. DRC is home to approximately 80 million people, 70% of whom live in rural areas. The DRC ranked 176th in the Human Development Index in 2015. Life expectancy is 59.1 years and under-five mortality rate is 104 per 1000 live births.9 Despite being the most water-rich country in sub-Saharan Africa,10 only 31% of rural Congolese use an improved water source and only 29% use improved sanitation facilities.1 59% of rural households spend more than 30 min, on each round trip, to collect drinking water.
To address these gaps, in 2008, the Government of the DRC launched a national programme known as ‘Healthy Villages & Schools’ (in French ‘Villages et Ecoles Assainis’, abbreviated VEA), a WASH programme financed by UK’s Foreign, Commonwealth and Development Office (FCDO) and implemented by the DRC government’s Ministries of Public Health, and of Primary, Secondary and Professional Education, with support from UNICEF. Since 2008, approximately 6 500 000 people in several thousand villages in the DRC have been reached with WASH services through the programme.11 VEA is the largest WASH programme implemented by UNICEF globally and comprised 90% of total external funding committed to rural WASH in the DRC from 2005 to 2020.12
The VEA’s main objective is to support improved access to WASH, especially in rural areas. It does so via a four-pronged intervention: provision of new or improved water infrastructure; provision of new or improved sanitation infrastructure; strengthening of village-level WASH institutions and a behaviour change campaign. Communities that meet a set of water and sanitation norms through VEA are formally certified as ‘Healthy Villages’.
We are not aware of any randomised trials that test a WASH programme integrating the four components included in VEA. However, each component has been studied separately or in smaller combinations. Water quality improvements from point-of-use water treatment with filtration or chlorine have been shown to reduce diarrhoea among children,13 14 but evidence is weaker for health benefits of new water points without water treatment.15 One trial measured effects of reduced water collection time through provision of piped water,16 finding no effects on productive activities or school attendance, although observational evidence suggests that reduced collection time is associated with higher school attendance among children and greater leisure among adults.17–20
Systematic review and meta-analysis of sanitation programmes has found that latrine subsidy or provision increases the use of improved sanitation by 8%–24%.21 However, multiple recent randomised trials of sanitation interventions have found mixed and often null effects on nutrition and health: two trials in India and one in Indonesia found no effect on health outcomes,22–24 although two other trials found improvements in length-for-age.25 26 Notably, three recent large trials in Kenya, Bangladesh and Zimbabwe compared interventions to improve household-level water quality, sanitation, handwashing, nutrition, all three WASH components together, or the WASH components plus nutrition.27–29 Across these trials, WASH interventions had no effect on stunting and only affected diarrhoea in one trial.
Freeman et al 30’s meta-analysis estimated that only 14% of low-income and middle-income country residents wash hands after using a sanitation facility or having contact with faecal matter, and that handwashing reduces the risk of diarrhoea by 23%–40%. However, trials of large-scale efforts to increase handwashing behaviour by changing health beliefs have generally not been successful.31–35 The evidence base for interventions to sustainably improve rural water governance is also limited.36
Methods
Study design and participants
The trial was registered with the American Economics Association RCT registry, trial AEARCTR-0004648 (https://www.socialscienceregistry.org/trials/4648). The study protocol was approved by the Institutional Ethics Committee of the Institut Superieur des Techniques Médicales de Bukavu (DRC) (number 001/2019) and by Solutions IRB (USA) (number 2019/10/20). Respondents provided informed consent verbally.
Our goal was to estimate the causal effects of the core VEA programme with a randomised control trial. The programme intervention unit is the village; however, we grouped villages into clusters when they were within 2.5 km of each other (‘as-the-crow-flies’) to mitigate potential spillover effects. We relaxed this rule in South Kivu, where density is greater and we sought to include naturally occurring villages, rather than the smaller unit of VEA subvillages, in the sample. In cases where naturally occurring or administratively-defined villages were less than 1 km from each other, we aggregated these into a single village cluster.
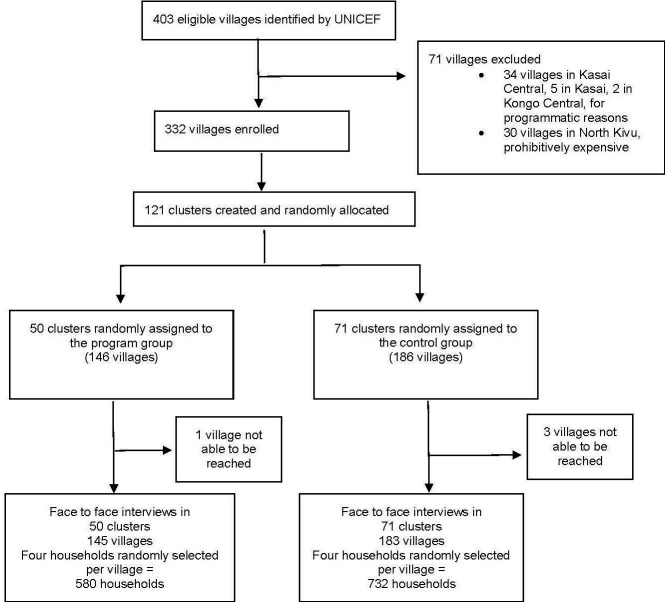
UNICEF generated a list of 403 candidate villages based on the programme criteria: being located in a secure, accessible Health Area not already served by other programmes, having Health Area staff who were interested in participating, and high incidence of diarrhoea, cholera and/or malnutrition in children and adults relative to other Health Areas. Health areas are subunits of the Congolese health system that include a health centre and cover approximately 10 000 residents. Thirty-four of the 403 villages were already implementing the programme, leaving 369 eligible villages in five provinces: Kongo Central, Kasai, Kasai Central, South Kivu and North Kivu. Based on the clustering method described above, we grouped those villages into 124 clusters. North Kivu had only three clusters, making it cost-prohibitive to work there, leaving a sample of 121 clusters in four provinces and 332 villages (figure 1).
Figure 1.
Trial profile.
Randomisation
We used statistical software (Stata V.16) to randomise the sample into 50 treatment clusters (containing 145 treatment villages) and 71 control clusters (183 control villages). Seven villages were randomly dropped to ensure that UNICEF’s operational targets were met, while maintaining treatment and control balance. Randomisation was stratified to ensure treatment and control balance with respect to (1) province and (2) the number of villages per cluster. Treatment clusters of villages received the VEA intervention. Control clusters of villages did not receive any intervention from VEA. Data collection procedures were identical in the two groups. Data collectors were blinded to treatment assignment, but one module in the questionnaire covered programme participation. Participants could not be blinded due to the participatory nature of the programme.
Intervention
The VEA is a comprehensive programme that mobilises communities to become a ‘Healthy Village’ with 3–6 months of support from government health officials and local NGOs, including approximately US$2000 of financing for new or improved water infrastructure, US$2000 for new or improved sanitation infrastructure and US$3000 for personnel costs, per village. The seven norms to become a Healthy Village are:
There is a dynamic village WASH committee.
At least 80% of the population has access to safe drinking water.
At least 80% of households use a hygienic latrine.
At least 80% of households dispose of their household waste hygienically.
At least 60% of the population washes their hands before eating and after going to the latrine.
At least 70% of the population is aware of faecal-oral disease transmission and how to prevent this.
The village is cleaned at least once a month.
The VEA programme is implemented in nine steps. (https://www.unicef.org/drcongo/media/2806/file/COD-Atlas2018.pdf). We focus on the village rather than the school component of the VEA programme. The nine steps are:
The community learns about the programme and collectively decides to adopt it before submitting a formal request to the relevant Health Zone. (A Health Zone is geographic unit of the Congolese health system that contains roughly 10 Health Areas and 100 000 residents, run by a chief medical officer (CMO)). Programme protocols state that the entire community should be involved in the decision to participate.
A statement of agreement between the community and the Health Zone is signed.
Health Zone officials survey 19 households on knowledge, attitudes and practices (KAP). The community self-evaluates on eight practices, including handwashing, water use and sanitation.
The community spends about 11 hours over 5 days creating calendars and maps, visiting water points, classifying hygiene practices as healthy or unhealthy, discussing faecal-oral disease transmission, calculating medical costs and assessing which individuals and organisations influence sanitation and hygiene in the community. This includes 1.5–2 hours in a facilitated activity around the question, ‘What are the hygiene practices that we want to change in our village?’
The Health Zone provides training for 20 volunteers on maintenance of latrines, water supply systems, and sanitation, conflict management and petty cash management. The community elects a village WASH committee.
The community spends 10 hours over 3 days describing a community vision, analysing the barriers to reducing diarrheal diseases, choosing improvements to drinking water, sanitation and hygiene, and formulating an action plan. The community is asked to identify practical, low-cost solutions with a minimum of outside assistance. New infrastructure is evaluated in terms of accessibility, technical feasibility and technical capacity.
The community builds new infrastructure over 90–180 days. Key messages about sanitation and hygiene are discussed during sensitization meetings or during visits to families by the WASH committee, community health workers or other volunteers. Health Zone staff are expected to visit the community monthly during this time; Health Area staff weekly.
The community self-evaluates again to measure progress since step 3. The Health Zone conducts additional KAP surveys and hosts 3 hours of meetings to assess the findings and make a plan to maintain progress.
The CMO spends 1 day in the community to assess whether or not the community completed its action plan and achieved the seven norms. If they have, a certification ceremony is held. The CMO and the village WASH committee develop a Community Action Plan for Maintenance.
Data collection
We interviewed households and village leaders concurrently in October–December 2019. In intervention villages, the median surveys occurred 151 days after new water and sanitation infrastructure was built. For the household survey, four households were randomly selected in each village by a team of four interviewers. From the centre of the village, the interviewers went in opposite directions to the nth household, where n was a randomly selected number from 1 to 20. The research team interviewed the head woman in the household. The questionnaire covered household demographics, water access, water governance, sanitation, health behaviours and time use. For the village and water leadership survey, the research team interviewed the village chief and the head of the village WASH committee and/or their representatives. If a WASH committee did not exist, the head of another village committee dealing with WASH-related issues was interviewed. The questionnaire covered leadership demographics, water infrastructure, water and sanitation interventions, other essential services and infrastructure, village history and village-state-society relations. The data collection team consisted of 46 interviewers, five supervisors and seven back-checkers.
Outcomes
We preregistered four primary outcomes: time spent collecting water in the day prior to the survey; water quantity collected in the day prior to the survey; whether or not the household’s primary water source is improved; and whether or not the household’s primary sanitation facility is improved. For the improved water source and sanitation variables, we use the Joint Monitoring Programme definitions.1 Improved water sources consist of water piped into a dwelling, piped into a plot, piped/public tap, tube well or borehole and protected spring. Improved sanitation indicates that the primary place of defecation is a ventilation-improved pit latrine, a pit latrine with slab or a composting latrine, or it flushes/pours to a piped sewer, septic tank or pit latrine. For the water time and quantity variables, outcomes are summed across all household members.
We also preregistered seven secondary outcomes: health behaviour and knowledge; child health; school attendance; functional water points; financial cost of water; satisfaction with water access and water governance. After seeing the data, health behaviour and knowledge was split into three outcomes: handwashing practices; sanitation practices and water storage practices. Thus, we report nine secondary outcomes. Two of the outcomes were measured at the village level. One was a count of the number of functional improved water points in the village. The other was a water governance index, comprised of questions about whether or not the village has an individual or group who reports about the management of water; has a WASH committee; number of WASH committee members; ratio of women to men on WASH committee; has a water maintenance system; is satisfied with health zone administration; time since last visit by health zone representative; is satisfied with health area administration and is satisfied with national government administration.
The remaining seven secondary outcomes were measured at the household level. The water satisfaction index had questions about satisfaction with water access and satisfaction with water point management. The financial cost of water index had questions about payment for water. The water storage index had four questions (does the household own a water pot?; is the water pot covered?; is the water pot clean?; are the water cups clean?). The handwashing index was based on how many of 12 situations (eg, ‘before eating’, ‘after touching animals’) the respondent reported the correct answer, unprompted, to the question, ‘When do you think it is necessary to wash your hands with soap?’ It also includes responses to ‘Have you used soap or any other relevant means (such as ashes) to wash your hands at least once since this time yesterday?’ The sanitation index had 11 questions about latrine cleaning, open defecation, faeces disposal, other garbage disposal, frequency of cleaning the living space and presence of flies or mosquitoes in the home. The school attendance index was based on the proportion of the household’s school-aged children enrolled in school and the number of days the children were present in school in the past week. Finally, we included as a secondary outcome a child health index comprised of questions about fever, cough and diarrheal illnesses among children 10–59 months old in the previous 2 weeks. This was included as a secondary outcome given our expectation that statistical power would be limited to detect effects on this outcome. All primary and secondary outcomes were self-reported.
Sample size
Power calculations focused on the primary outcome of whether the household uses an improved water source as their primary source of water. We limited the risk of type I errors (false positives) to 5% (alpha=0.05) and type II errors (false negatives) to 20% (beta=0.8), and we used a conservatively high intracluster correlation of 0.7, given shared village infrastructure. With four households per village and 121 clusters, the minimum detectable effect was an 8 percentage point increase in access to improved water sources.
Statistical analysis
We used intention-to-treat (ITT) analyses to test for differences in outcome measures between the intervention group and the control group. For both primary and secondary outcomes, we used linear models with the following general specification:
| (1) |
where is the outcome of interest for respondent i in household h in village v in cluster c at the follow-up survey, defined above. is the treatment indicator that takes value 1 for clusters that were randomly assigned to participate in VEA (‘treatment clusters’) and 0 for otherwise (‘control clusters’). X represents a set of randomization-strata-specific dummies where strata are based on province and number of villages in the cluster, which will equal 1 if the household falls in that stratum and 0 otherwise. is a vector of baseline covariates included in the analysis. Specifically we include gender and age (month) dummies for all child health outcomes; we do not include covariates for other outcomes. and are vectors of associated strata and covariate coefficients, respectively. is an idiosyncratic error term. Our main parameter of interest is , the ITT effect. SEs are clustered by the randomisation unit (clusters of villages).
For secondary outcomes consisting of multiple measures, we calculated a summary index to avoid over-rejection of the null hypothesis due to multiple inference. We rescaled each outcome, so that higher values implied better outcomes, and averaged standardised values relative to the control group.37 The index was calculated using all non-missing values for each observation (“greedy indexing”). Treatment effects were estimated as the difference in the summary index between treatment and control groups, implying that treatment effects are expressed in SD units relative to the control group.
We preregistered five subgroup analyses. For all four primary outcomes, this included tests of treatment effects by (1) education of household head, (2) village exposure to armed conflict, (3) village remoteness and (4) province. For time spent collecting water, we preregistered a test of effects by gender. For all subgroup analyses, we restricted the analysis to the subgroup of interest and fit the model described above.
Statistical analyses were conducted in Stata V.16.0.
Role of the funding source
This study was funded by a grant from the UK FCDO managed through the World Bank Group’s Development Impact Evaluation Department. VEA is a DRC Government national programme funded by UK’s FCDO and implemented with UNICEF’s support. The funder and implementing partners provided inputs at the design stage to ensure the study addressed policy and programme priorities of importance to them. However, the research was carried out independently and at no point did the partners attempt to influence field implementation, data collection, data analysis, manuscript preparation or the decision to publish findings.
Patient and public involvement
Neither patients nor the public were formally involved in the research process.
Results
Enrolment, baseline balance and attrition
From 11 October 2019 to 23 December 2019, we interviewed 1312 households in 328 villages in 121 clusters in four provinces (figure 1). Household and respondent characteristics that the programme was unlikely to have changed were similar in the intervention and control groups (table 1). Few households lived in homes with an improved roof (28% control; 37% intervention), improved wall (1% control; 1% intervention) or an improved floor (5% control; 5% intervention). The average control household had 7.0 members, compared with 6.8 members for intervention households. Respondents in both groups had similar ages, religions, levels of education and marital status.
Table 1.
Respondent and household characteristics by intervention group
| Variable |
Control group | Intervention group | Difference | t-test p value | ||
| N/(clusters) | Mean/(SE) | N/(clusters) | Mean/(SE) | (1)–(2) | (1)–(2) | |
| Household has improved roof | 732 | 0.276 | 580 | 0.372 | −0.096 | 0.559 |
| (71) | (0.054) | (50) | (0.075) | |||
| Household has improved wall | 732 | 0.007 | 580 | 0.009 | −0.002 | 0.770 |
| (71) | (0.003) | (50) | (0.003) | |||
| Household has improved floor | 732 | 0.046 | 580 | 0.050 | −0.004 | 0.768 |
| (71) | (0.011) | (50) | (0.020) | |||
| Household size | 732 | 6.958 | 580 | 6.809 | 0.149 | 0.153 |
| (71) | (0.178) | (50) | (0.197) | |||
| Respondent identifies as catholic | 732 | 0.190 | 580 | 0.219 | −0.029 | 0.338 |
| (71) | (0.019) | (50) | (0.022) | |||
| Respondent identifies as protestant | 732 | 0.342 | 580 | 0.376 | −0.034 | 0.1598 |
| (71) | (0.049) | (50) | (0.051) | |||
| Respondent identifies with other religion | 732 | 0.372 | 580 | 0.288 | 0.084 | 0.367 |
| (71) | (0.044) | (50) | (0.055) | |||
| Respondent age | 732 | 37.046 | 580 | 37.093 | −0.047 | 0.941 |
| (71) | (0.517) | (50) | (0.867) | |||
| Respondent has completed primary school | 732 | 0.295 | 580 | 0.310 | −0.015 | 0.579 |
| (71) | (0.029) | (50) | (0.036) | |||
| Respondent has completed secondary school | 732 | 0.044 | 580 | 0.053 | −0.010 | 0.823 |
| (71) | (0.007) | (50) | (0.012) | |||
| Respondent is married or cohabitating | 732 | 0.844 | 580 | 0.843 | 0.001 | 0.576 |
| (71) | (0.013) | (50) | (0.016) | |||
The value displayed for t-tests are the differences in the means across the groups, with controls for randomization strata. Standard errors are clustered by geographic cluster (group of villages). Improved roof=1 if roof is finished roofing (ie, metal, wood, calamine/cement fibre ceramic tiles, cement or roofing shingles); improved walls=1 if walls are ‘finished walls’; improved floor=1 if floor is ‘finished floor’.
Primary outcomes
In the intervention group, 83% of households reported that their primary water source was improved, compared with 43% in the control group (adjusted treatment effect 33% points; 95% CI 22 to 45) (table 2). In the intervention group, 46% of households reported that their primary sanitation facility was improved, compared with 18% in the control group (adjusted treatment effect 26% points; 95% CI 14 to 37). There was no statistically significant difference between the two groups in time spent collecting water (adjusted treatment effect −3 min; 95% CI −20 to 14) or in quantity of water collected (adjusted treatment effect 2.3 L; 95% CI −4.2 to 8.7).
Table 2.
Effect of the intervention on time spent collecting water, quantity of water collected, quality of water source and quality of sanitation facility
| Outcome | Control | Intervention | ITT | 95% CI | ||
| N | Mean | N | Mean | |||
| Time to collect water (min) | 732 | 70.7 | 580 | 61.5 | −3.0 | (−19.7 to 13.6) |
| Improved water source | 732 | 0.43 | 580 | 0.83 | 0.33 | (0.22 to 0.45) |
| Quantity of water collected (litres) | 732 | 37.2 | 580 | 41.5 | 2.3 | (−4.2 to 8.7) |
| Improved sanitation facility | 732 | 0.18 | 580 | 0.46 | 0.26 | (0.14 to 0.37) |
The model includes controls for randomisation blocks based on province and number of villages per cluster. There were 121 clusters in total. Time spent collecting water and total quantity of water collected were Winsorised at the 99th percentile.
ITT, intention-to-treat effect estimate.
Among reported main sources of drinking water, protected springs were 28 pp more likely in the treatment group (53% vs 26%), and piped/public tap was 10 pp more likely (27% vs 18%), while unprotected springs were 26 pp less likely, and surface water was 12 pp less likely. Among reported main defecation sites, treatment households were 28 pp more likely to report pit latrine with slab (43% vs 15%). They were 20 pp less likely to report open pit (37% vs 57%) and 9 pp less likely to report no facilities (22% vs 9%).
Secondary outcomes
The programme increased the water governance index by 1.3 SDs (95% CI 1.1 to 1.5), the water satisfaction index by 0.6 SD (95% CI 0.4 to 0.9), the handwashing practices index by 0.5 SD (95% CI 0.3 to 0.7), and the sanitation index by 0.3 SD (95% CI 0.1 to 0.4) (table 3). There was no statistically significant difference between the two groups in the financial cost of water index, school attendance index, child health index, water storage practices index or water quality index. See online supplemental table 4 for effects on the individual variables within each index.
Table 3.
Effect of the intervention on indices of handwashing, sanitation practices, water storage, child health, school attendance, cost of water, water satisfaction, water quality and access, and water governance
| Indices | Control | Intervention | ITT | 95% CI | ||
| N | Mean | N | Mean | |||
| Handwashing | 732 | 0.00 | 580 | 0.61 | 0.48 | (0.25 to 0.71) |
| Sanitation practices | 732 | 0.00 | 580 | 0.48 | 0.28 | (0.12 to 0.44) |
| Water storage | 732 | 0.00 | 580 | −0.21 | −0.11 | (−0.28 to 0.05) |
| Child health | 742 | 0.00 | 646 | 0.14 | 0.04 | (−0.11 to 0.20) |
| School attendance | 702 | 0.00 | 558 | −0.02 | −0.09 | (−0.20 to 0.03) |
| Financial cost of water | 732 | 0.00 | 580 | 0.14 | 0.13 | (−0.10 to 0.36) |
| Water satisfaction | 732 | 0.00 | 580 | 0.65 | 0.64 | (0.43 to 0.85) |
| Water quality and access | 183 | 0.00 | 145 | 0.23 | 0.13 | (−0.18 to 0.44) |
| Water governance | 183 | 0.00 | 145 | 1.33 | 1.33 | (1.12 to 1.54) |
The model includes controls for randomisation blocks based on province and number of villages per cluster. Child health also includes controls for sex and age (months). There were 121 clusters in total. Indices are calculated by rescaling each variable in each index (eg, handwashing) so that higher values imply better outcomes, then standardising relative to the control group, following Kling et al 37. Effects are in standard deviation units. All indices are calculated at the household level except child health (child level), water quality and access (village level) and water governance (village level).
ITT, intention-to-treat effect estimate.
bmjgh-2021-005030supp001.pdf (93.5KB, pdf)
Subgroup analyses
There were several large differences in effects by province (table 4). In Kasai, the intervention increased the time spent collecting water by 43 min (95% CI 13 to 72), whereas in Kasai Central, the intervention decreased that time by 61 min (95% CI −95 to −26). However, in both provinces, the intervention increased the proportion of respondents with an improved water source: Kasai (49 pp increase; 95% CI 32 pp to 67 pp); Kasai Central (75 pp increase; 95% CI 55 pp to 96 pp). In Kasai Central, the intervention decreased the quantity of water collected the previous day by 13 L (95% CI −23 to −4) and increased access to improved sanitation by 74 pp (95% CI 58 to 90). In Kasai, there were no effects on those two outcomes.
Table 4.
Subgroup analysis by province: effect of the intervention on time spent collecting water, quantity of water collected, quality of water source and quality of sanitation facility
| Outcome | Province | Control | Intervention | ITT | 95% CI | ||
| N | Mean | N | Mean | ||||
| Time to collect water (min) | Kongo Central | 72 | 50 | 80 | 33 | −19 | (−51 to 13) |
| Kasai | 172 | 47 | 196 | 90 | 43 | (13 to 72) | |
| Kasai Central | 260 | 92 | 64 | 21 | −61 | (−95 to −26) | |
| South Kivu | 228 | 70 | 240 | 59 | −10 | (−35 to 16) | |
| Improved water source | Kongo Central | 72 | 0.51 | 80 | 0.79 | 0.24 | (−0.06 to 0.53) |
| Kasai | 172 | 0.24 | 196 | 0.73 | 0.49 | (0.32 to 0.67) | |
| Kasai Central | 260 | 0.15 | 64 | 0.83 | 0.75 | (0.55 to 0.96) | |
| South Kivu | 228 | 0.86 | 240 | 0.93 | 0.06 | (−0.04 to 0.17) | |
| Quantity of water collected (liters) | Kongo Central | 72 | 23 | 80 | 23 | 0 | (−14 to 15) |
| Kasai | 172 | 31 | 196 | 37 | 5 | (−2 to 12) | |
| Kasai Central | 260 | 32 | 64 | 18 | −13 | (−23 to −4) | |
| South Kivu | 228 | 52 | 240 | 58 | 7 | (−7 to 21) | |
| Improved sanitation facility | Kongo Central | 72 | 0.15 | 80 | 0.84 | 0.68 | (0.52 to 0.85) |
| Kasai | 172 | 0.24 | 196 | 0.38 | 0.14 | (−0.05 to 0.33) | |
| Kasai Central | 260 | 0.05 | 64 | 0.80 | 0.74 | (0.58 to 0.90) | |
| South Kivu | 228 | 0.29 | 240 | 0.30 | 0.01 | (−0.11 to 0.12) | |
The model includes controls for the number of villages per cluster. There were 121 clusters in total. Time spent collecting water and total quantity of water collected were Winsorised at the 99th percentile.
ITT, intention-to-treat effect estimate.
We found no evidence of any intervention effects on any of the primary outcomes in subgroup analyses of South Kivu province. In the Kongo Central subsample, the only significant effect was an increase in access to improved sanitation of 68 pp (95% CI 52 pp to 85 pp).
Some of the programme’s effects varied by the remoteness of the cluster, calculated as travel time to the territory capital (table 5) (in DRC, territory is the administrative unit below province). In clusters that were below median remoteness (420 min), the intervention decreased the amount of time spent collecting water by 25 min (95% CI −48 to −2). There was no effect in clusters above-median remoteness. The intervention’s positive effect on access to improved water was larger in more remote clusters (58 pp; 95% CI 45 to 71) than in less remote clusters (11 pp; 95% CI 1 pp to 21 pp). Point estimates for access to improved sanitation also differed but not significantly; there was a 30 pp increase in more remote clusters (95% CI 13 to 47) compared with a 22 pp increase in less remote clusters (95% CI 8 pp to 37 pp). There was no evidence of effects on the quantity of water collected at either level of remoteness. The median travel time in minutes to the territory capital, by province, was 180 in Kongo Central, 240 in South Kivu, 600 in Kasai Central and 840 in Kasai.
Table 5.
Subgroup analysis by remoteness: effect of intervention on time spent collecting water, quantity of water collected, quality of water source and quality of sanitation facility
| Outcome | Remoteness | Control | Intervention | ITT | 95% CI | ||
| N | Mean | N | Mean | ||||
| Time to collect water (min) | Less remote | 416 | 78.5 | 292 | 49.8 | −25.0 | (−48.3 to −1.7) |
| More remote | 316 | 63.5 | 288 | 74.4 | 23.5 | (−2.5 to 49.5) | |
| Improved water source | Less remote | 416 | 0.6 | 292 | 0.89 | 0.11 | (0.01 to 0.21) |
| More remote | 316 | 0.2 | 288 | 0.78 | 0.58 | (0.45 to 0.71) | |
| Quantity of water collected (litres) | Less remote | 416 | 40.9 | 292 | 49.9 | 4.4 | (−5.7 to 14.4) |
| More remote | 316 | 32.2 | 288 | 33.1 | 0.5 | (−5.7 to 6.7) | |
| Improved sanitation facility | Less remote | 416 | 0.2 | 292 | 0.47 | 0.22 | (0.08 to 0.37) |
| More remote | 316 | 0.1 | 288 | 0.44 | 0.30 | (0.13 to 0.47) | |
The model includes controls for randomisation blocks based on province and number of villages per cluster. There were 121 clusters in total. Time spent collecting water and total quantity of water collected were Winsorised at the 99th percentile. More remote = above median travel time to territory capital (median=420 min). Less remote = equal to or below median travel time to territory capital.
ITT, intention-to-treat effect estimate.
Effects on primary outcomes did not vary by exposure to conflict (online supplemental table 1) or respondent education level (online supplemental table 2). Restricting the sample to women and girls, there was no effect on the time spent collecting water the previous day (online supplemental table 3).
Discussion
The VEA programme was a comprehensive attempt to address multiple WASH gaps in rural DRC, combining construction and rehabilitation of water infrastructure and sanitation facilities, community mobilisation for behaviour change and support to community WASH institutions. It is a long-standing programme, operating at scale (over 6.5 million people have been reached since programme initiation), in a setting with multiple economic, geographic and conflict-related challenges. This combination of multiple water, sanitation and governance elements could be considered a ‘big push’ towards addressing multiple WASH constraints simultaneously at the community level.
This programme produced large increases in the percentage of households who use improved water sources and who use improved sanitation facilities, almost doubling access to improved water sources (from 43% to 83%) and more than doubling access to improved sanitation (from 18% to 46%). Respondents also reported large increases in adoption of healthy behaviours, especially handwashing and sanitation-related behaviours, better local governance of WASH facilities and greater satisfaction with and access to water. Yet, despite programmatic focus on the burden of water collection, especially for women and children, and the links between WASH-related childhood illness and school absenteeism, there was no significant effect on these outcomes.
A main conclusion of this study is that effective implementation of large-scale community-driven WASH programmes is possible even in highly conflict-affected settings. South Kivu, Kasai and Kasai Central provinces are among the regions of the DRC with the highest levels of armed conflict in recent years, yet the DRC government and UNICEF were able to produce large increases in WASH access. This highlights the possibility for effective action in similar settings globally.
Treatment effects on water source, water collection time and sanitation varied significantly across provinces. Given that the programme was, by design, responsive to community demands, some variation in community priorities (eg, more investment in water relative to sanitation or vice versa) may not be unexpected across provinces facing different needs at baseline. For the most part, treatment effects were higher in provinces with less WASH access in the control group. This may reflect greater ease of improvement from a low baseline (‘low-hanging fruit’). This is consistent with our findings that more remote villages, which have less WASH access in the control group, also experienced greater gains in water access, and with Gopalan and Rajan38, who find larger impacts of foreign aid on WASH in rural relative to urban areas.
This study is complementary to, but distinct from, several other recent large WASH RCTs.27–29 This study is closer to an at-scale effectiveness trial, with both the advantages and disadvantages that that implies. There is far less ability to disaggregate any distinct mechanism of action in the VEA trial than in the aforementioned studies, which separately tested water, sanitation and nutrition interventions. However, VEA is a national programme implemented at scale and seeks to address a full set of WASH gaps at the same time. As such it more closely mirrors the policy that might be available to a decision-maker in a developing country. Furthermore, in the VEA programme, the communities themselves decide on the specific components of the package, and the specific programme logic is that the village must achieve threshold levels of WASH behaviours in order to be labelled and celebrated as a ‘healthy village’. Thus, VEA has more in common with community-led total sanitation (CLTS) campaigns in its focus on community mobilisation. However, it differs from CLTS in its focus on water as well as sanitation and by pairing community mobilisation efforts with direct investments in water and sanitation infrastructure.
Sustainability was a major emphasis of the VEA programme, including activities to strengthen community institutions for managing water. The observed improvements in water governance included large increases in the proportion of villages with WASH committees as well as more gender balance on WASH committees. A critical question for follow-up surveys is the extent to which institutional changes, such as the functioning and improved gender balance of water committees, persist over time.
A limitation of this study as a comprehensive evaluation of the VEA programme is that there was limited collection of health outcome data in this survey round. A related limitation is that all outcomes were self-reported, including measures of behavioural change for water and sanitation. One factor which suggests that our results are not driven by social desirability bias is that such biases might lead us to expect uniformly positive responses for socially desirable sanitation behaviours, when, in fact, we find major heterogeneity within specific behavioural indices. For example, in the sanitation index, there was a 20 pp increase in nonfaecal garbage disposal versus 2 pp increase in latrine emptying (online supplemental table 4). In the handwashing index, there was a 17 pp increase in washing hands after toilet use compared with no statistically significant change in washing hands after coughing or before eating. Similarly, the large reported increases in satisfaction by village leaders with the performance of Health Zone officials do not appear to reflect desirability bias since similar improvements were not seen for broader health and political authorities (eg, Health Area staff, national government).
A further limitation is that although the VEA programme also delivers programming to schools, it was not practical to randomise the school component without disrupting programme implementation. Finally, the survey from which we report results here was conducted a median of approximately 5 months after the completion of programme activities. A follow-up survey, planned for late 2021, will measure longer-term effects.
Acknowledgments
The authors are indebted to the respondents, the data collection team from IHfRA, led by Luc Zanmenou, and our partners in the DRC Ministries of Public Health and of Primary, Secondary, and Professional Education, particularly Kwengani Mavard, Paul Mushiya, Willy Mude Manana, and Jean Jacques Diyabanza; at UNICEF, particularly Franck Abeille, Julie Aubriot, Lise Lacan, Frederic Unterreiner, Nicolas Rice Chudeau, Françoise Nseya, Thomas Dechentinnes, Adelard Mahamba and Pierre Fuamba; at UK FCDO, particularly Anne Joselin, Pete Howson, Maguy Makusudi Zabibu, Mark Dunn, Jolie Massay, Laura Mazal, Alex Marshall, Conor Doyle, Jonas Herman, and Federica di Batistia; and at the World Bank, particularly Evelyn De Castro, Chloe Fernandez, Julie Bousquet, Patricia Komina Dele, and Francoise Mukamana. We also thank Julia Bailey, Chloe Lewis, and Dana Olds for their comments on the study design and manuscript drafts.
Footnotes
Handling editor: Sanni Yaya
Contributors: JPQ was involved with conceptuatlisation, formal analysis, methodology, writing of the original draft, review and editing. AC was involved with conceptuatlisation, formal analysis, methodology, project administration, funding acquisition, manuscript review and editing. EM was involved with conceptuatlisation, formal analysis, methodology, project administration, funding acquisition, manuscript review and editing. CD was involved in data curation, formal analysis, methodology, project administration and reviewing and editing. FE was involved in data curation, methodology, project administration and reviewing and editing. BC was involved in data curation, formal analysis, methodology, and reviewing and editing. YBL was involved in data curation, methodology, project administration and reviewing and editing. KC was involved with conceptuatlisation, formal analysis, methodology, writing of the original draft, and review and editing.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon request. All de-identified data are available from the corresponding author upon request and will become available publicly on the World Bank’s microdata catalogue.
References
- 1. UNICEF/WHO JMP . Progress on drinking water, sanitation, and hygeine: 2017 update and SDG baselines. Geneva: World Health Organization; 2017: 1–116. https://washdata.org. 978-92-4-151289-3. [Google Scholar]
- 2. Prüss-Ustün A, Bartram J, Clasen T, et al. Burden of disease from inadequate water, sanitation and hygiene in low- and middle-income settings: a retrospective analysis of data from 145 countries. Trop Med Int Health 2014;19:894–905. 10.1111/tmi.12329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Adair LS, Fall CHD, Osmond C, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet 2013;382:525–34. 10.1016/S0140-6736(13)60103-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cumming O, Cairncross S. Can water, sanitation and hygiene help eliminate stunting? current evidence and policy implications. Matern Child Nutr 2016;12 Suppl 1:91–105. 10.1111/mcn.12258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grantham-McGregor S, Cheung YB, Cueto S, et al. Developmental potential in the first 5 years for children in developing countries. Lancet 2007;369:60–70. 10.1016/S0140-6736(07)60032-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Black MM, Walker SP, Fernald LCH, et al. Early childhood development coming of age: science through the life course. Lancet 2017;389:77–90. 10.1016/S0140-6736(16)31389-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kayser GL, Rao N, Jose R, et al. Water, sanitation and hygiene: measuring gender equality and empowerment. Bull World Health Organ 2019;97:438–40. 10.2471/BLT.18.223305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Corral P, Irwin A, Krishnan N. Fragility and conflict: on the front lines of the fight against poverty. Washington, DC.: World Bank Publications, 2020. [Google Scholar]
- 9. Ministère du Plan et Suivi de la Mise en œuvre de la Révolution de la Modernité, Ministère de la Santé Publique . République Démocratique Du Congo Enquête Démographique et de Santé (EDS-RDC) 2013-2014, 2014. Available: http://dhsprogram.com/publications/publication-FR300-DHS-Final-Reports.cfm
- 10. UNEP . Water issues in the Democratic Republic of the Congo challenges and opportunities. United nations environment programme (UNEP) Democratic Republic of the Congo, 2011. Available: https://reliefweb.int/sites/reliefweb.int/files/resources/DDB8149182AD305BC125785B00476984-Full_Report.pdf
- 11. Programme National Ecole et Village Assaini (PNEVA) . Atlas 2018 : Acces a L’eu potable, a l’hygeine et a l’assainaissement pour les commautes rurales et periurbaines de la republique democratique du Congo, 2018. Available: https://www.unicef.org/drcongo/media/2806/file/COD-Atlas2018.pdf
- 12. Bank W. WASH poor in a water-rich Country: a diagnostic of water, sanitation, hygiene, and poverty in the Democratic Republic of Congo. Washington, DC: World Bank, 2017. [Google Scholar]
- 13. Waddington H, Snilstveit B. Effectiveness and sustainability of water, sanitation, and hygiene interventions in combating diarrhoea. J Dev Effect 2009;1:295–335. 10.1080/19439340903141175 [DOI] [Google Scholar]
- 14. Ahuja A, Kremer M, Zwane AP. Providing safe water: evidence from randomized evaluations. Annu Rev Resour Econ 2010;2:237–56. 10.1146/annurev.resource.012809.103919 [DOI] [Google Scholar]
- 15. Clasen TF, Alexander KT, Sinclair D, et al. Interventions to improve water quality for preventing diarrhoea. Cochrane Database Syst Rev 2015:CD004794. 10.1002/14651858.CD004794.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Devoto F, Duflo E, Dupas P, et al. Happiness on TAP: piped water adoption in urban Morocco. Am Econ J Econ Policy 2012;4:68–99. 10.1257/pol.4.4.68 [DOI] [Google Scholar]
- 17. Ilahi N, Grimard F. Public infrastructure and private costs: water supply and time allocation of women in rural Pakistan. Econ Dev Cult Change 2000;49:45–75. 10.1086/452490 [DOI] [Google Scholar]
- 18. Lokshin M, Yemtsov R. Has rural infrastructure rehabilitation in Georgia helped the poor? World Bank Econ Rev 2005;19:311–33. 10.1093/wber/lhi007 [DOI] [Google Scholar]
- 19. Koolwal G, van de Walle D, Walle D. Access to water, women’s work, and child outcomes. Econ Dev Cult Change 2013;61:369–405. 10.1086/668280 [DOI] [Google Scholar]
- 20. Nauges C, Strand J. Water hauling and girls’ school attendance: some new evidence from Ghana. Environ Resource Econ 2017;66:65–88. 10.1007/s10640-015-9938-5 [DOI] [Google Scholar]
- 21. Garn JV, Sclar GD, Freeman MC, et al. The impact of sanitation interventions on latrine coverage and latrine use: a systematic review and meta-analysis. Int J Hyg Environ Health 2017;220:329–40. 10.1016/j.ijheh.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clasen T, Boisson S, Routray P, et al. Effectiveness of a rural sanitation programme on diarrhoea, soil-transmitted helminth infection, and child malnutrition in Odisha, India: a cluster-randomised trial. Lancet Glob Health 2014;2:e645–53. 10.1016/S2214-109X(14)70307-9 [DOI] [PubMed] [Google Scholar]
- 23. Patil SR, Arnold BF, Salvatore AL, et al. The effect of India's total sanitation campaign on defecation behaviors and child health in rural Madhya Pradesh: a cluster randomized controlled trial. PLoS Med 2014;11:e1001709. 10.1371/journal.pmed.1001709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cameron L, Olivia S, Shah M. Scaling up sanitation: evidence from an RCT in Indonesia. J Dev Econ 2019;138:1–16. 10.1016/j.jdeveco.2018.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hammer J, Spears D. Village sanitation and child health: effects and external validity in a randomized field experiment in rural India. J Health Econ 2016;48:135–48. 10.1016/j.jhealeco.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pickering AJ, Djebbari H, Lopez C, et al. Effect of a community-led sanitation intervention on child diarrhoea and child growth in rural Mali: a cluster-randomised controlled trial. Lancet Glob Health 2015;3:e701–11. 10.1016/S2214-109X(15)00144-8 [DOI] [PubMed] [Google Scholar]
- 27. Null C, Stewart CP, Pickering AJ, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Kenya: a cluster-randomised controlled trial. Lancet Glob Health 2018;6:e316–29. 10.1016/S2214-109X(18)30005-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Luby SP, Rahman M, Arnold BF, et al. Effects of water quality, sanitation, handwashing, and nutritional interventions on diarrhoea and child growth in rural Bangladesh: a cluster randomised controlled trial. Lancet Glob Health 2018;6:e302–15. 10.1016/S2214-109X(17)30490-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Humphrey JH, Mbuya MNN, Ntozini R, et al. Independent and combined effects of improved water, sanitation, and hygiene, and improved complementary feeding, on child stunting and anaemia in rural Zimbabwe: a cluster-randomised trial. Lancet Glob Health 2019;7:e132–47. 10.1016/S2214-109X(18)30374-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Freeman MC, Stocks ME, Cumming O, et al. Hygiene and health: systematic review of handwashing practices worldwide and update of health effects. Trop Med Int Health 2014;19:906–16. 10.1111/tmi.12339 [DOI] [PubMed] [Google Scholar]
- 31. Biran A, Schmidt W-P, Varadharajan KS, et al. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): a cluster-randomised trial. Lancet Glob Health 2014;2:e145–54. 10.1016/S2214-109X(13)70160-8 [DOI] [PubMed] [Google Scholar]
- 32. Galiani SG, Orsola-Vidal P A. Promoting handwashing behavior in Peru: the effect of large-scale Mass-Media and community level interventions. Policy Res Work Pap World Bank 2012;74:1–75. [Google Scholar]
- 33. Chase CD, Quy T. Handwashing behavior change at scale: evidence from a randomized evaluation in Vietnam. Policy Res Work Pap World Bank 2012;6207:1–50. 10.1596/1813-9450-6207 [DOI] [Google Scholar]
- 34. Huda TMN, Unicomb L, Johnston RB, et al. Interim evaluation of a large scale sanitation, hygiene and water improvement programme on childhood diarrhea and respiratory disease in rural Bangladesh. Soc Sci Med 2012;75:604–11. 10.1016/j.socscimed.2011.10.042 [DOI] [PubMed] [Google Scholar]
- 35. Briceño B, Coville A, Gertler P, et al. Are there synergies from combining hygiene and sanitation promotion campaigns: evidence from a large-scale cluster-randomized trial in rural Tanzania. PLoS One 2017;12:0186228. 10.1371/journal.pone.0186228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. International Initiative for Impact Evaluation (3ie) . Water, sanitation, and hygiene (wash) evidence gap map: 2018 update, 2018. Available: https://gapmaps.3ieimpact.org/evidence-maps/water-sanitation-and-hygiene-wash-evidence-gap-map-2018-update
- 37. Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica 2007;75:83–119. 10.1111/j.1468-0262.2007.00733.x [DOI] [Google Scholar]
- 38. Gopalan S, Rajan RS. Has foreign aid been effective in the water supply and sanitation sector? Evidence from panel data. World Dev 2016;85:84–104. 10.1016/j.worlddev.2016.04.010 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2021-005030supp001.pdf (93.5KB, pdf)
Data Availability Statement
Data are available upon request. All de-identified data are available from the corresponding author upon request and will become available publicly on the World Bank’s microdata catalogue.